Objective:
To characterize diet quality across a global cohort of people with HIV (PWH).
Design:
Cross-sectional analysis.
Methods:
Leveraging REPRIEVE data from baseline across five Global Burden of Disease (GBD) regions, we analyzed participant responses to the Rapid Eating Assessment for Participants questionnaire. An overall diet quality score and scores for specific diet components were generated. Higher scores indicate better diet quality.
Results:
Among 7736 participants (median age 50 years, 30% women, median BMI 25.8 kg/m2) overall diet quality score (max score 30) was optimal in 13% of participants and good, suboptimal or poor in 45%, 38%, and 4% of participants, respectively; saturated fat score (max score 18) was good, suboptimal, or poor in 38%, 40%, or 7% of participants, respectively. Diet quality scores differed across GBD region with the highest scores reported in the South Asia region [median 23 (21–25)] and lowest in the sub-Saharan Africa region [median 15 (12–18)]; 61% of participants in the South Asia region reported optimal diet quality compared with only 6% in the sub-Saharan Africa region. Higher atherosclerotic cardiovascular risk scores were seen with worsening diet quality.
Conclusion:
Among PWH eligible for primary CVD prevention, diet quality was suboptimal or poor for almost half of participants, and there were substantial variations in diet quality reported by GBD region.
TRIAL REGISTRATION:
Keywords: cardiovascular disease, diet quality, global, HIV
Introduction
Chronic comorbid diseases have emerged as major challenges for the large global population of people with HIV (PWH). Diet is an important, but poorly understood risk factor for cardiometabolic disease and other chronic comorbid conditions in PWH. Indeed, preventing onset of cardiometabolic comorbidities may be possible by optimizing lifestyle habits including diet. Poor-quality diets are high in unhealthy fats, refined grains, sodium, added sugars, and animal-source foods, and low in fruits, vegetables, whole grains, legumes, fish, and nuts. Low-quality diets are associated with noncommunicable diseases in the general population [1], and globally, unhealthy diet is a top contributor to cardiovascular disease (CVD) burden and death [2]. In PWH, diet quality has been found to be low compared with people without HIV, although studies evaluating diet in PWH to date have been conducted in relatively small, homogenous, site-specific cohorts [3–5]. Importantly, diet quality has not been previously characterized across a global cohort of PWH.
The current analysis leveraged data collected on diet across a global cohort of PWH. REPRIEVE, the Randomized Trial to Prevent Vascular Events in HIV, is an ongoing trial evaluating a primary CVD prevention strategy in PWH. The multinational population of PWH with low-to-moderate traditional CVD risk provides the first opportunity to evaluate diet quality across global regions. The primary objective of the current analysis was to characterize overall diet quality and dietary components as determined by the Rapid Eating Assessment for Participants (REAP) questionnaire in the REPRIEVE cohort. The secondary objective was to evaluate cardiometabolic characteristics by diet quality.
Methods
REPRIEVE (NCT02344290) is a randomized, multicenter, phase III trial of pitavastatin calcium vs. placebo [6,7]. REPRIEVE enrolled 7770 participants between March 2015 and July 2019 at over 100 sites globally [7]. PWH, without known atherosclerotic cardiovascular disease (ASCVD), 40–75 years of age, receiving antiretroviral therapy (ART), with low-to-moderate ASCVD risk (≤15%) were enrolled using the 2013 ACC/AHA Pooled Cohort Equations and specific low-density lipoprotein (LDL) cholesterol thresholds. Full eligibility criteria and design details are described elsewhere [6]. Enrollment sites were grouped by Global Burden of Disease (GBD) super region subgroups using classifications developed by the WHO [8] as previously described [9].
At study entry, diet information was collected utilizing the REAP questionnaire [10], a 31-item questionnaire developed to assess diet quality in primary care settings. REAP was administered as instructed; translation was available in Spanish and at the discretion of each individual site. A diet quality score was calculated based on participant responses to 15 questions (Supplemental Material 1a) from the questionnaire, higher scores reflected better diet quality and eating habits. To further evaluate dietary components (saturated fat, sodium, fiber, and added sugar), component scores were developed based on groupings of questions. Diet quality score was analyzed on a continuous scale with a maximum score of 30 and grouped on an ordinal scale with four categories: optimal, good, suboptimal, or poor (Supplemental Material 1b for cut points), and likewise for the key dietary components. In a calibration study, REAP had excellent test–retest reliability (r = 0.86, P < 0.0001) and has been validated with the Healthy Eating Index (a summary measure of diet quality assessing conformance to dietary recommendations) (r = 0.49, P = 0.0007) [10].
Statistical analysis
Distributions of diet quality scores were evaluated by GBD region and other baseline demographics. Continuous variables are summarized as median (Q1–Q3). For binary or categorical variables, N and percentage are provided. In the calculation of percentages, participants with missing data were excluded from the denominator. A priori selected characteristics (sex, age, BMI, alcohol use, race, and GBD region) were individually assessed for their association with diet quality score using linear regression models; all variables listed in Supplemental Figure 1 were included in adjusted analyses. Covariates were analyzed on the categorical scales to allow for clearer assessment of both linear and nonlinear trends. In these cases, type-three P values are provided as an overall assessment of the association; estimates are shown with 95% confidence intervals. The analysis was conducted using SAS software, version 9.4M5 for Linux (SAS Institute).
Role of the funding source
The funders had no role in the study design, data collection, analysis, interpretation, or writing of the article.
Ethics statement
Each clinical research site obtained institutional review board/ethics committee approval and any other applicable regulatory entity approvals. Participants were provided with study information, including discussion of risks and benefits, and signed the approved declaration of informed consent.
Results
Baseline characteristics
Seven thousand seven-hundred and thirty-six participants completed the baseline REAP questionnaire and were included in the analysis. Median age was 50 years, ASCVD risk score 4.5%, and BMI 25.8 kg/m2 (Table 1). Demographic and clinical characteristics are available in Supplemental Table 1.
Table 1.
Cardiometabolic characteristics by diet quality scorea
| Characteristic | Total (N = 7736) | Optimal (N = 1020) | Good (N = 3488) | Suboptimal (N = 2941) | Poor (N = 287) |
| Cardiovascular and metabolic | |||||
| Hypertensionb | 2774 (36%) | 353 (35%) | 1218 (35%) | 1089 (37%) | 114 (40%) |
| ASCVD risk score (%) | 4.5 (2.1–7.0) | 3.9 (1.9–6.6) | 4.3 (2.0–6.8) | 4.9 (2.4–7.3) | 5.1 (2.7–7.4) |
| 0 to <2.5 | 2150 (28%) | 317 (31%) | 1025 (29%) | 744 (25%) | 64 (22%) |
| 2.5 to <5 | 2046 (26%) | 289 (28%) | 943 (27%) | 740 (25%) | 74 (26%) |
| 5 to <7.5 | 1881 (24%) | 223 (22%) | 827 (24%) | 753 (26%) | 78 (27%) |
| 7.5–10 | 1097 (14%) | 125 (12%) | 464 (13%) | 462 (16%) | 46 (16%) |
| >10 | 562 (7%) | 66 (6%) | 229 (7%) | 242 (8%) | 25 (9%) |
| BMI (kg/m2) | 25.8 (22.7–29.4) | 24.9 (22.1–28.2) | 25.7 (22.9–29.2) | 26.1 (22.8–30.0) | 26.5 (22.7–29.8) |
| <18.5 | 287 (4%) | 51 (5%) | 120 (3%) | 107 (4%) | 9 (3%) |
| 18.5–24.9 | 3108 (40%) | 464 (45%) | 1421 (41%) | 1117 (38%) | 106 (37%) |
| 25–29.9 | 2648 (34%) | 346 (34%) | 1218 (35%) | 980 (33%) | 104 (36%) |
| 30–34.9 | 1066 (14%) | 108 (11%) | 467 (13%) | 451 (15%) | 40 (14%) |
| 35–39.9 | 412 (5%) | 34 (3%) | 175 (5%) | 189 (6%) | 14 (5%) |
| 40+ | 209 (3%) | 17 (2%) | 86 (2%) | 92 (3%) | 14 (5%) |
| Waist circumference (cm) | 92 (84–101) | 90 (84–98) | 91 (84–100) | 93 (84–102) | 94 (85–102) |
| Fasting cholesterol and fasting glucose | |||||
| Total cholesterol (mmol/l) | 4.74 (4.14–5.39) | 4.77 (4.17–5.39) | 4.79 (4.17–5.44) | 4.69 (4.12–5.34) | 4.61 (4.07–5.15) |
| Glucose (mmol/l) | 5.00 (4.66–5.38) | 4.94 (4.61–5.33) | 5.00 (4.66–5.38) | 5.00 (4.61–5.33) | 4.94 (4.61–5.33) |
Frequency (%) are presented for categorical measures; median with lower and upper quartiles (Q1–Q3) are presented for continuous measures. ASCVD, atherosclerotic cardiovascular disease.
All statistics are calculated out of participants with data collected. Missing data include: BMI (n = 6); waist circumference (n = 103); total cholesterol (n = 357); glucose (n = 402). Thirty-four participants are missing the REAP questionnaire at the time of analysis and are excluded in Total by Diet Quality Score.
Hypertension is defined as any of the following: hypertension diagnosis, use of antihypertensive treatment for elevated blood pressure, SBP at least 140 mmHg, DBP at least 90 mmHg.
Factors associated with diet quality and differences by GBD region
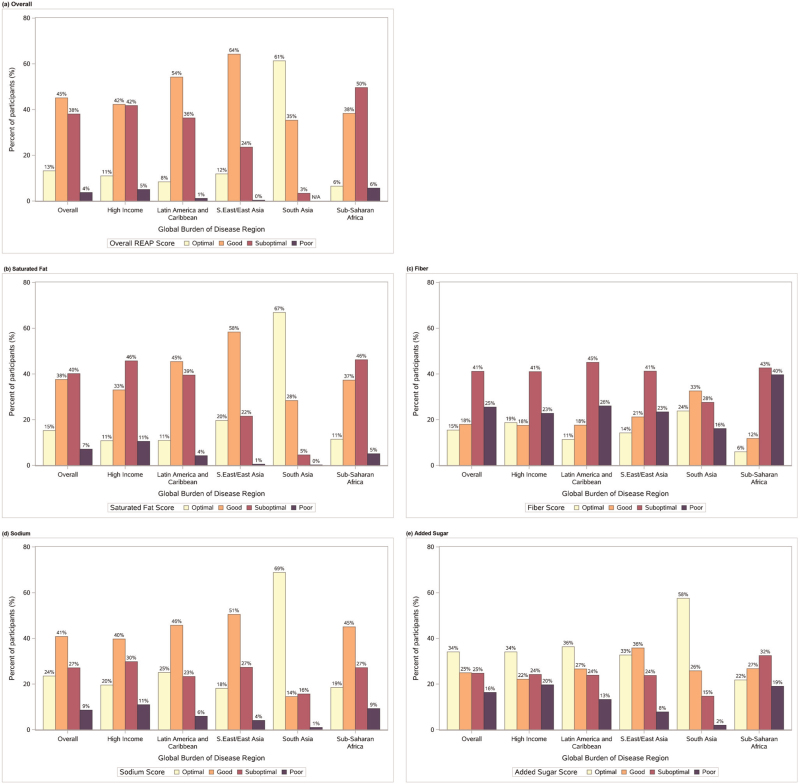
Among all participants, median diet quality score was 17 points (Q1–Q3: 13–20) (Supplemental Table 2), with higher values indicative of better diet quality (score range from 1 to 30). When diet quality scores were grouped by category, 13% of participants had optimal, 45% good, 38% suboptimal, and 4% poor diet quality (Fig. 1a). Suboptimal diet quality was more frequently reported by younger participants compared with older participants, Blacks or African Americans, current smokers, and participants reporting most frequent alcohol use (Supplemental Table 1).
Fig. 1.
Diet quality score and diet component scores by global burden of disease region.
Distribution of diet quality score by global burden of disease region. Score categorizations are as follows: max score = 30; optimal 22.5–30; good 15 < to <22.5; suboptimal 7.5 < to ≤15; poor 0–7.5. Distribution of diet component scores by global burden of disease region; component score for (a) saturated fat, (b) fiber, (c) sodium, (d) added sugar. Categorization of component scores is as follows: saturated fat: max score = 18; optimal greater than 13.5; good 9 < to ≤13.5; suboptimal 4.5 < to ≤9; poor 4.5 or less; fiber: max score = 6; optimal greater than 4.5; good 3 < to ≤ 4.5; suboptimal 1.5 < to ≤3; poor 1.5 or less; sodium: max score = 8; optimal greater than 6; good 4 < to ≤ 6; suboptimal 2 < to ≤ 4; poor 2 or less; added sugar: max score = 4; optimal greater than 3; good 2 < to ≤ 3; suboptimal 1 < to ≤ 2; poor 1 or less.
Diet quality scores differed across GBD region with highest diet quality reported in the South Asia region [median 23 (21–25)] and lowest diet quality reported in the sub-Saharan Africa region [median 15 (12–18)] (Supplemental Table 2). Similarly, 61% of participants in the South Asia region reported optimal diet quality compared with only 6% of participants in the sub-Saharan Africa region (Fig. 1a).
In single-variable analyses exploring associations between covariates and diet quality, factors associated with higher diet quality score were older age (≥60 years), Asian race, and region of enrollment in South Asia, Southeast/East Asia, or Latin America/Caribbean GBD regions (compared with high-income GBD region). Characteristics associated with lower diet quality score included BMI at least 30 kg/m2, more frequent alcohol use, black or African American race, and sub-Saharan Africa GBD region of enrollment (compared with high-income GBD region) (Supplemental Figure 1, left panel). In the adjusted analysis, the associations with BMI and Asian race were no longer apparent, and a stronger relationship between higher diet quality score and increasing age emerged (Supplemental Figure 1, right panel). Given population differences across regions, the race effect in the adjusted model is estimated only among the high-income region.
We explored cardiometabolic characteristics by diet quality score category (Table 1). ASCVD risk scores, BMI, and waist circumference increased with worsening category of diet quality while there were no clinical differences in glucose or total cholesterol across worsening diet quality score category. Participants with diet quality scores categorized as poor had the highest percentage of hypertension compared with the other diet quality categories.
Diet component scores
Diet component scores for saturated fat, fiber, sodium, and added sugar are shown in Fig. 1b–e, with variations in consumption noted by GBD region. Among all participants, 47% had saturated fat scores categorized as suboptimal or poor, 66% of participants had fiber component scores categorized as suboptimal or poor, 36% of participants had sodium scores categorized as suboptimal or poor, and 41% of participants had an added sugar component score categorized as suboptimal or poor.
Discussion
The REPRIEVE cohort provides global data on risk factors for cardiometabolic disease among PWH. In this diverse population, we evaluated diet quality over multiple GBD regions and assessed demographic and CVD risk factors by diet quality. We utilized the REAP questionnaire, a validated questionnaire developed to assess diet quality in clinical settings and summed a score from responses to represent diet quality as previously reported [10–12]. A high percentage of participants reported suboptimal or poor diet quality (42%), and there were notable variations in diet quality by GBD region. Moreover, established CVD risk factors increased with worsening category of diet quality.
Smaller studies in the United States [3,5], Uganda [13,14], Brazil [15,16], and India [17,18] have demonstrated the need to address nutrition among PWH. We leveraged REPRIEVE to address this knowledge gap, simultaneously comparing diet quality across multiple GBD regions, to better understand how CVD risk relates to diet quality in PWH.
We found that poor or suboptimal diets were more commonly reported in the sub-Saharan Africa region (Botswana, South Africa, Uganda, Zimbabwe). Of additional interest, in the distributions of diet component scores stratified by GBD region, component scores for saturated fat, fiber, and added sugar were suboptimal or poor in well over half of participants in this region. Diet quality among PWH in sub-Saharan Africa may be low because of economic factors, urbanization, limited access to healthy food, impacts of climate change, as well as absence of population level strategies, such as dietary guidelines to improve diet quality [19]. Notably, the component score for sodium was optimal or good in over half of participants in the sub-Saharan Africa region and may reflect recent population level efforts to raise awareness about and take action to decrease sodium intake [20]. Our findings are important as CVD risk factors including hypertension, diabetes, and obesity in PWH in sub-Saharan Africa are increasingly prevalent [21] and are attributed in part to lifestyle behaviors including diet [22]. A recent systematic review by Shah et al. [23] found the highest HIV-associated CVD burden to be in sub-Saharan Africa. Developing and supporting care models that incorporate nutrition assessment and counseling, as well as improving availability of and access to affordable, healthy foods is essential in this region. These activities may be effective to lessen the burden of CVD in PWH in sub-Saharan Africa.
Markers of traditional CVD risk tracked with diet quality categories such that higher BMI, higher WC, and higher ASCVD risk score were observed with lower diet quality. Although factors unique to HIV, including persistent vascular inflammation and immune activation, play a role in increased CVD risk [24], traditional CVD risk factors are important as well [25,26]. These findings enrich our understanding of modifiable risk factors and highlight that diet quality, while not often assessed in CVD risk assessment, may be an important factor in the large global population of PWH as has been demonstrated in REPRIEVE [27]. Interestingly, total cholesterol and glucose did not demonstrate clinically meaningful changes across diet quality categories.
Our findings show poor nutrient profiles for fiber, saturated fat, and added sugar and may reflect food-supply systems that are dominated by large industrial food processors and/or restaurant chains/fast food type venues [28]. Although in South Asia and, to a lesser extent, Southeast/East Asia, individual component scores demonstrated better nutrient profiles, which may reflect preservation of traditional diets high in vegetables, nuts/legumes, and low in red meat and processed meat [29]. GBD 2017 Diet Collaborators found that intake of foods known to be low in fiber was a leading dietary risk factor for morbidity and mortality [2]. Diets high in saturated fat and added sugars are associated with poor CVD outcomes. Dietary fiber has been negatively associated with inflammatory markers associated with CVD in the general population [30] and may also be related to CVD in the setting of HIV, but further studies are needed.
This current investigation has several strengths, notably its large size, global reach, and diverse population all assessed uniformly by a rapid diet assessment tool, and some limitations. The trial recruited a primary prevention population with a lower range of LDL levels and less diabetes than a group with known CVD. Despite this, poor diet was common and related to traditional risks, highlighting the importance of targeting PWH before the occurrence of cardiovascular disease. Dietary data obtained in REPRIEVE were obtained through participant self-assessment but tracked well with CVD risk, suggesting the utility and feasibility of capturing data on diet quality to assess this key understudied aspect of cardiovascular risk. Only a small number of participants had a low BMI, and thus undernutrition was not a focus of this analysis. Future studies are needed to further assess the utility of dietary data obtained in this manner in global populations with different diet customs and practices. Importantly, these data informing us of poor diet quality among PWH will be analyzed with respect to CVD events upon the completion of REPRIEVE.
The current study analyzes diet quality at entry among participants in REPRIEVE, a multinational primary prevention trial assessing for statin effects on major adverse cardiovascular events. In this study, we show that diet quality was suboptimal or poor in almost half of participants with differences observed across GBD region. These data suggest the need to focus on diet quality as a potential modifiable risk for CVD in PWH.
Acknowledgements
The study investigators would like to thank the study participants, site staff, and study-associated personnel for their ongoing participation in the trial. Additionally, AIDS Clinical Trial Group (ACTG) for clinical site support; ACTG Clinical Trials Specialists (Jhoanna Roa) for regulatory support; the data management center, Frontier Science Foundation, for data support; the Center for Biostatistics in AIDS Research for statistical support.
The authors’ contributions were as follows: K.V.F.: design/implementation, project administration, data interpretation, prepared original draft, review/editing, primary responsibility for final content; S.A.M.: design, data analysis/interpretation/verification, review/editing; K.M.E.: design/implementation, data interpretation, review/editing; E.T.O.: design/implementation, performance, data interpretation, review/editing; M.V.Z.: design/implementation, review/editing; C.F.: design/implementation, performance, review/editing; J.A.A.: design/implementation, performance, review/editing; E.S.F.: implementation, review/editing; E.M.K.: implementation, data interpretation, review/editing; L.E.M.: design/implementation, review/editing; G.S.B.: design/implementation, review/editing; R.M.N.: implementation, performance, review/editing; S.P.F.: implementation, performance, review/editing; A.A.D.: implementation, performance, review/editing; N.K.: implementation, performance, review/editing; K.R.: implementation, performance, review/editing; R.M.: implementation, performance, review/editing; P.S.D.: design/implementation, funding acquisition, project administration, review/editing; H.J.R.: design/implementation, funding acquisition, data analysis/interpretation/verification, review/editing; SKG: design/implementation, funding acquisition, project administration, data interpretation, review/editing, final approval. All authors read and approved the final manuscript.
Previous presentation: Conference on Retroviruses and Opportunistic Infections (CROI), 2021, Science Spotlight; REPRIEVE Investigator Meeting, 2021.
This work was supported through National Institutes of Health, National Institute of Heart, Lung, and Blood Institute grants U01HL123336, to the REPRIEVE Clinical Coordinating Center, and U01HL123339, to the REPRIEVE Data Coordinating Center, as well as through funding from Kowa Pharmaceuticals America, Inc. and Gilead Sciences, Inc. National Institute of Allergy and Infectious Diseases has supported this study through grants UM1 AI068636, which supports the AIDS Clinical Trials Group (ACTG) Leadership and Operations Center; and UM1 AI106701, which supports the ACTG Laboratory.
The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute or the National Institute of Allergy and Infectious Diseases; the National Institutes of Health; or the U.S. Department of Health and Human Services.
Conflicts of interest
K.V.F., S.A.M., E.S.F., E.M.K., L.E.M., G.S.B., A.A.D., G.P., N.K., K.R., R.M., P.S.D., and H.J.R. have no disclosures to report; K.M.E. reports grants and personal fees from Gilead, personal fees from ViiV, Janssen, and Theratechnologies, outside the submitted work (all paid to her institution); E.T.O. reports personal fees and nonfinancial support from ViiV, personal fees and nonfinancial support from Merck, nonfinancial support from Bavarian Nordic, personal fees and nonfinancial support from Gilead, nonfinancial support from Janssen, outside the submitted work; M.V.Z. reports serving as PI of an investigator-initiated research grant from Gilead to Institution (MGH); C.F. reports grants from Gilead Sciences, ViiV Healthcare, GSK, Merck, Janssen, and Amgen unrelated to this work; J.A.A. reports grants from Atea, Emergent Biosolutions, Frontier Technologies, Gilead Sciences, grants and personal fees from Glaxo Smith Kline, grants from Janssen, grants and personal fees from Merck, grants from Pfizer, grants from Regeneron, grants from ViiV Healthcare, outside the submitted work; R.M.N. reports personal fees from Gilead Sciences, personal fees from ViiV Pharma, outside the submitted work; S.P.F. reports personal fees from Gilead Sciences unrelated to this work; S.K.G. reports grants and personal fees from Theratechnologies, grants and personal fees from ViiV, grants from Gilead, grants from Kowa, during the conduct of the study.
Supplementary Material
Footnotes
Supplemental digital content is available for this article.
References
- 1.Sotos-Prieto M, Bhupathiraju SN, Mattei J, Fung TT, Li Y, Pan A, et al. Changes in diet quality scores and risk of cardiovascular disease among US men and women. Circulation 2015; 132:2212–2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019; 393:1958–1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weiss JJ, Sanchez L, Hubbard J, Lo J, Grinspoon SK, Fitch KV. Diet quality is low and differs by sex in people with HIV. J Nutr 2019; 149:78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muhammad JN, Fernandez JR, Clay OJ, Saag MS, Overton ET, Willig AL. Associations of food insecurity and psychosocial measures with diet quality in adults aging with HIV. AIDS Care 2019; 31:554–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webel AR, Moore SM, Longenecker CT, Currie J, Horvat Davey C, Perazzo J, et al. Randomized controlled trial of the SystemCHANGE Intervention on Behaviors Related to Cardiovascular Risk in HIV+ Adults. JAIDS J Acquir Immune Deficiency Syndr 2018; 78:23–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grinspoon SK, Fitch KV, Overton ET, Fichtenbaum CJ, Zanni MV, Aberg JA, et al. REPRIEVE Investigators. Rationale and design of the Randomized Trial to Prevent Vascular Events in HIV (REPRIEVE). Am Heart J 2019; 212:23–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grinspoon SK, Douglas PS, Hoffmann U, Ribaudo HJ. Leveraging a landmark trial of primary cardiovascular disease prevention in human immunodeficiency virus: introduction from the REPRIEVE Coprincipal Investigators. J Infect Dis 2020; 222: (Suppl 1): S1–S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.GBD 2017 Mortality Collaborators. Global, regional, and national age-sex-specific mortality and life expectancy, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392:1684–1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smeaton LM, Kileel EM, Grinsztejn B, Gardner EM, Starr K, Murry ML, et al. Characteristics of REPRIEVE Trial Participants Identifying Across the Transgender Spectrum. J Infect Dis 2020; 222: (Suppl 1): S31–S40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gans KM, Risica PM, Wylie-Rosett J, Ross EM, Strolla LO, McMurray J, Eaton CB. Development and evaluation of the nutrition component of the Rapid Eating and Activity Assessment for Patients (REAP): a new tool for primary care providers. J Nutr Educ Behav 2006; 38:286–292. [DOI] [PubMed] [Google Scholar]
- 11.Segal-Isaacson CJ, Wylie-Rosett J, Gans KM. Validation of a short dietary assessment questionnaire: the Rapid Eating and Activity Assessment for Participants short version (REAP-S). Diabetes Educ 2004; 30:774.776, 778 passim. [DOI] [PubMed] [Google Scholar]
- 12.Johnston CS, Bliss C, Knurick JR, Scholtz C. Rapid eating assessment for participants [shortened version] scores are associated with Healthy Eating Index-2010 scores and other indices of diet quality in healthy adult omnivores and vegetarians. Nutr J 2018; 17:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rawat R, McCoy SI, Kadiyala S. Poor Diet Quality Is Associated With Low CD4 Count and Anemia and Predicts Mortality Among Antiretroviral Therapy–Naive HIV-Positive Adults in Uganda. J Acquir Immune Defic Syndr 2013; 62:246–253. [DOI] [PubMed] [Google Scholar]
- 14.Kadiyala S, Rawat R. Food access and diet quality independently predict nutritional status among people living with HIV in Uganda. Public Health Nutrition 2013; 16:164–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silva EFR, Lewi DS, Vedovato GM, Garcia VRS, Tenore SB, Bassichetto KC. Nutritional and clinical status, and dietary patterns of people living with HIV/AIDS in ambulatory care in Sao Paulo, Brazil. Rev Bras Epidemiol 2010; 13:677-688. [DOI] [PubMed] [Google Scholar]
- 16.Duran ACFL, Almeida LB, Segurado AAC, Jaime PC. Diet quality of persons living with HIV/AIDS on highly active antiretroviral therapy. J Hum Nutr Diet 2008; 21:346–350. [DOI] [PubMed] [Google Scholar]
- 17.Sachdeva RK, Sharma A, Wanchu A, Dogra V, Singh S, Varma S. Dietary adequacy of HIV infected individuals in north India--a cross-sectional analysis. Indian J Med Res 2011; 134:967–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anand D, Puri S. Anthropometric and nutritional profile of people living with HIV and AIDS in India: an assessment. Indian J Community Med 2014; 39:161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moyo N, Maharaj P, Mambondiani L. Food challenges facing people living with HIV/AIDS in Zimbabwe. Afr J AIDS Res 2017; 16:225–230. [DOI] [PubMed] [Google Scholar]
- 20.Sookram C, Munodawafa D, Phori PM, Varenne B, Alisalad A. WHO's supported interventions on salt intake reduction in the sub-Saharan Africa region. Cardiovasc Diagn Ther 2015; 5:186–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu Y, Chen X, Wang K. Global prevalence of hypertension among people living with HIV: a systematic review and meta-analysis. J Am Soc Hypertens 2017; 11:530–540. [DOI] [PubMed] [Google Scholar]
- 22.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004; 27:1047–1053. [DOI] [PubMed] [Google Scholar]
- 23.Shah ASV, Stelzle D, Lee KK, Beck EJ, Alam S, Clifford S, et al. Global burden of atherosclerotic cardiovascular disease in people living with HIV. Circulation 2018; 138:1100–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nou E, Lo J, Grinspoon SK. Inflammation, immune activation, and cardiovascular disease in HIV. AIDS 2016; 30:1495–1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bijker R, Jiamsakul A, Uy E, Kumarasamy N, Ditag R, Chaiwarith R, et al. TREAT Asia HIV Observational Database (TAHOD) of IeDEA Asia-Pacific. Cardiovascular disease-related mortality and factors associated with cardiovascular events in the TREAT Asia HIV Observational Database (TAHOD). HIV Med 2019; 20:183–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boettiger DC, Escuder MM, Law MG, Veloso V, Souza RA, Ikeda MLR, et al. Cardiovascular disease among people living with HIV in Brazil. Trop Med Int Health 2020; 25:886–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Douglas PS, Umbleja T, Bloomfield GS, Fichtenbaum CJ, Zanni MV, Overton ET, et al. Cardiovascular risk and health among people with HIV eligible for primary prevention: insights from the REPRIEVE Trial. Clin Infect Dis 2021; 7:2009–2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Popkin BM, Reardon T. Obesity and the food system transformation in Latin America. Obes Rev 2018; 19:1028–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gulati S, Misra A, Sharma M. Dietary fats and oils in India. Curr Diabetes Rev 2017; 13:438–443. [DOI] [PubMed] [Google Scholar]
- 30.Ma Y, Hebert JR, Li W, Bertone-Johnson ER, Olendzki B, Pagoto SL, et al. Association between dietary fiber and markers of systemic inflammation in the Women's Health Initiative Observational Study. Nutrition 2008; 24:941–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.