Abstract
Background
The initial clinical training has been reported by nursing students as the most challenging component of the nursing programs. Although progressive muscle relaxation and guided imagery have been reported to improve emotional and physical health, the use of such approaches among nursing students rarely exist.
Purpose
The purpose of this study was to examine the deferential effects of progressive muscle relaxation [PMR] and guided imagery [GI] on physical and emotional symptoms in nursing students taking their initial clinical training.
Methods
Using a three-group, randomized, single blinded study conducted in a large Jordanian university, 156 nursing students were randomly allocated into one of three study groups (PMR group, GI group, and control group). The physical symptoms and emotional symptoms of depression, anxiety, and stress were assessed at baseline and end of the intervention. The study protocol was registered in ClinicalTrail.gov, identifier: xxxxxx.
Results
Using one-way MANOVA and post-hoc comparisons, the results showed that PMR and GI significantly reduced more physical symptoms than control condition although PMR was more effective than GI in this regard. GI significantly decreased more emotional symptoms such as anxiety, depression, and stress than PMR and control condition. PMR decreased anxiety, depression, and stress but the results were not statistically significant.
Conclusion
The findings of this study support the ABC relaxation theory claiming that PMR im-proves better physical symptoms while GI improves better emotional symptoms. However, further studies using students from multiple settings are needed.
Keywords: Anxiety, Depression, Guided imagery, Nursing students, Physical symptoms, Progressive muscle relaxation, Stress
Anxiety; Depression; Guided imagery; Nursing students; Physical symptoms; Progressive muscle relaxation; Stress.
1. Introduction
The initial clinical training has been reported by nursing students as the most challenging component of the nursing programs, because nursing students taking initial clinical training are usually exposed to a variety of distinct stressors [1]. These stressors include lack of sufficient nursing knowledge and skills to provide healthcare services for patients, unfamiliarity with clinical environment, heavy workloads, and challenging assignments [1, 2]. Repeated exposure to these stressors over time can evoke emotional and physical symptoms, potentially resulting in increased suicidal tendency, impaired academic achievements, burnout, and inability to provide care for themselves and patients [3, 4]. Nursing students have commonly reported to experience various emotional and physical symptoms such as stress, depression, anxiety, headache, and sleep disturbances that need more attention [4, 5, 6, 7].
Although several mind-body relaxation approaches have been reported to improve emotional and physical health, the use of such approaches among nursing students rarely exist [8]. Mind-body relaxation approaches comprise a variety of cognitive behavioral methods used to increase the mind capacity to affect the functions of the body [8]. Among these approaches, progressive muscle relaxation (PMR) and guided imagery (GI) have been described as the easiest ones to be learnt and practiced. They have been also reported as inexpensive, available, and safe approaches [9].
Benson’s (1975) relaxation response hypothesis states that all mind-body relaxation approaches have similar effects on either physical or emotional health outcomes through evoking similar relaxation responses. Based on the relaxation response hypothesis, relaxation trainers are often used one general approach of mind-body relaxation to all patients with physical and emotional health problems [10]. However, Smith (2005) in the Attentional Behavioral Cognitive (ABC) Relaxation theory that explains the mechanisms of six families of relaxation approaches argues that although all approaches of mind-body relaxation are effective in improving physical and emotional health outcomes, each of them is associated with different degrees of effect on these outcomes [10]. For example, PMR, classified as somatic technique, has a greater effect in improving physical health outcomes. However, guided imagery is more effective in improving emotional health outcomes [10]. According to the ABC relaxation theory, the authors hypothesized that PMR and GI approaches could improve physical and emotional symptoms, compared to a control condition. Also, PMR may improve better physical symptoms than GI while GI could improve better emotional symptoms than PMR in nursing students having their initial clinical training.
1.1. Progressive muscle relaxation
PMR is a mind-body relaxation technique that involves tensing up and then relaxing [letting go] skeletal muscles progressively with cognitively attending to the feelings of muscles’ tension and relaxation [10]. This mind-body relaxation approach initially developed by Edmund Jacobson (1974) was described as long and time consuming. It involved several sessions a week for up to a year [11]. Since that time, various brief versions of PMR have been developed [12, 13]. Because the procedural variations of these versions limited comparisons of health outcomes across settings and populations, Smith [2005], who developed the ABC relaxation theory, proposed a detailed PMR training to standardize the procedure and explained its mechanism [10].
Smith proposes that PMR deploys and develops the access skill of tensing up-letting go (e.g., attending to a group of skeletal muscles, deliberately creating muscle tension, and then letting the muscle relax and the tension go). This developed access skill is associated with initial health effects; reductions in stressed skeletal muscles. Stressed skeletal muscle refers to increased skeletal muscle tension because of one’s exposure to stressful situations. The initial effects of reduced stressed muscles may result in reductions in other physical arousals [10]. As a rebound effect, for example, respiratory rate, heart rate and blood pressure will decline because relaxed muscles require less oxygen. Also, the normal blood flow and oxygenation to the relaxed muscles improve, leading to lesser discomfort, stiffness, pain, and fatigue and warmer hands and feet. This parasympathetic-mediated generalized physical relaxation state reduces sensory input (e.g., tension headache) to the brain that then triggers the hypothalamus to additionally reduce stress arousal and associated worrisome thoughts. Furthermore, it is argued that emotional symptoms such as anxiety and depression may be diminished because negative emotional states are absent in the existence of complete physical relaxation, although this proposition is still not enough empirically supported [10].
The existing research have demonstrated emotional and physical benefits in a variety of ill and healthy populations. Compared to aerobic exercise, PMR has been more effective in improving anxiety, fatigue, and sleep disorders in hemodialysis patients [14]. In patients with cancers, PMR resulted in significant greater reductions in anxiety, vomiting, nausea and pain as compared to control conditions [15, 16]. In comparison to control condition, PMR has significantly decreased more pain, sleep quality and physical activities in women after caesarean section [17]. PMR significantly improved more depression, anxiety, and sleep quality in patients with COVID-19 in comparison to routine treatment [18]. In educational settings, nursing students receiving PMR demonstrated lower levels of emotional symptoms such as anxiety, depression, and stress than those students in control groups [19, 20].
1.2. Guided imagery
GI is a mind-body relaxation technique in which one substitutes troubling memories and thoughts with relaxing mental imagery [10]. According to the ABC relaxation theory, GI involves deploying and developing the access skill of relaxing imagery, which facilitates the attentional shift from self-stressing verbal thoughts to nonverbal activity such as thinking about relaxing images, sounds, touch sensations, and smells. The instructional guidance by trainers and the sensory engagement by trainees are essential components of this technique that can achieve greater perceptual detail of the relaxing images created during the practice [10].
The emotional and physical benefits of guided imagery for ill and healthy populations have been empirically supported. In a systematic review, GI has been found to be effective in improving anxiety and pain in patients with critical illnesses [21]. In comprehensive narrative review, GI has been reported to be safe and non-invasive technique that can improve a variety of emotional and physical symptoms in patients with musculoskeletal disorders such as depression, anxiety, stress, fatigue, pain [22]. Hemodialysis patients receiving GI have shown significantly lower anxiety level and higher sleep quality level than those hemodialysis patients receiving routine care services [23]. In nurses working during the COVID-19, death anxiety in GI group was significantly less than that in control group [24]. Other studies have examined the effectiveness of GI in educational settings. For instance, nursing students receiving GI have shown lower levels of state anxiety, test anxiety, and stress than those students in control groups [25, 26].
In summary, the existing research have mainly supported the effectiveness and benefits of these two approaches on several emotional and physical symptoms in a variety of ill and healthy populations but rarely these approaches have been examined and compared side-by-side in experimental studies to assess relative effectiveness in promoting physical and emotional health in a comprehensive way for nursing students. It is known that these approaches are effective in decreasing emotional and physical symptoms, but not which approach is most effective in improving emotional or physical symptoms. It is critically necessary to understand which of mind-body relaxation approaches is more effective in terms of emotional and physical health because this will hopefully give healthcare providers tools for intelligently tailoring approaches to nursing students and other populations based on health problems they experience. Thus, the current study seeks to examine and compare the effectiveness of two common mind-body relaxation techniques on physical and emotional symptoms in nursing students taking their initial clinical training.
2. Materials and methods
2.1. Design
The current study used a three-arm pre-post test factorial single-blinded randomized controlled design.
2.2. Participants
The study subjects were 150 nursing students who were recruited from Jordan University of Science and Technology. Undergraduate nursing students were included in the present study if they were at least 18 years old and taking their initial clinical course (Adult health Nursing). Exclusion criteria included students who were performing any type of relaxation therapies, taking anxiolytic, sedatives, and antidepressant, or having current medical or mental illnesses.
The required sample size was determined by the G∗ Power software 3.1. given One-way MANOVA, a power of 0.8, an alpha of .05, the number of groups of 3, and an effect size of 0.06 as evident in a similar study [27], the sample size of 126 was generated. Approximately 25 % attrition rate was reported in an experimental study that examined the effectiveness of a mind-body intervention in population and setting similar to those in the present study [28]. Considering an expected attrition rate of 25 %, the required final total sample size was approximately 156 students.
2.3. Recruitment and randomization
After getting permission from the administration of the nursing faculty at XXXXX, the principal investigator (PI) visited the students in their clinical training settings and announced the study objectives, procedure, risks, and benefits. For students who were interested in the study, an initial meeting was arranged to meet with them on another day in a specious and private room at the university. At this meeting, informed consent was obtained from students who met the eligibility criteria once they were reassured that they can terminate participation at any time without any negative consequences. After that, one of the study authors with a PhD degree in nursing who did not participate in the data collection process randomly allocated students equally to the three study groups (PMR group, GI group, or control group) using a simple randomization method (computerized random numbers table). Finally, the study sessions were scheduled.
2.4. Interventions
In the present study, the ABC relaxation theory’s versions of PMR and GI were used, including five 30-minute weekly sessions of each version [10]. The subjects in the PMR and GI groups received separately an additional educational 3-hour workshop about their assigned interventions in private, noiseless, and large rooms at the university before the five actual intervention sessions to improve the subjects' understanding of their assigned interventions. In the educational workshop, the PI provided a presentation to subjects in the PMR and GI groups separately about the purposes and procedures of their assigned intervention and a demonstration of the intervention protocols. Subjects were asked briefly to practice their assigned intervention and then assessed by the PI to ensure the interventions have been performed accurately. The subjects were given the opportunity to ask questions about their assigned intervention during the educational workshop. The PI received training about mind-body relaxation techniques at the Psychology Department at a university in the USA 10 years ago. Since then, PI has been practicing these techniques.
The five sessions of PMR and GI were introduced by recorded verbal instructions that were developed by the PI according to the Smith’s protocols [10]. The subjects either in the PMR or GI groups were randomly divided into subgroups by the study author who randomly allocated subjects into the study groups, with 10 subjects in each subgroup. The subgroups received their assigned intervention separately in different large rooms at the university.
Several techniques were conducted to improve intervention fidelity. Quiet environments were kept, with a “Do Not Disturb” sign put on the doors of the rooms where the intervention sessions were conducted. The PI attended all sessions and randomly selected sessions from each intervention to assess the administration of the interventions using checklists developed in accordance with the interventions’ protocols. Participants in the PMR and GI groups were asked to avoid sharing any information about the interventions with other students during the study.
2.4.1. Progressive muscle relaxation
PMR involves a tense-let go exercise of 11 muscle groups including hand, arm, sides, back, shoulder, face, front of neck, stomach, chest, leg, and foot. This tense-let go exercise is performed twice for each muscle group. The tensing up phase for each muscle group should last for 5–10 s and the letting go phase for 20–30 s. Simultaneously, the subjects were asked to pay attention to the sensations of muscle tension and relaxation. After the tense-let go exercise, subjects were asked to systematically scan the muscle groups to notice and let go of any remaining muscle tension. The entire exercise took around 30 min, not including instructions and times of measurement [10].
2.4.2. Guided imagery
Guided imagery [Smith’s (2005) Version] involves creating in one’s mind or imagining a passive relaxing place or activity. In sense imagery, one simply imagines sensations associated with a relaxing setting or activity. The relaxation approach involves the sense of sight, sound, touch, and smell. The categories of stimuli consist of [1]: Travel such as boats, plains, trains, balloons, horses [2], outdoor nature settings such as mountains, gardens, and forest [3], water such as rivers, lakes, ocean, beach, rain, and [4] indoor settings such as childhood home, castle, religious institution, and cabin. The entire exercise took around 30 min, not including instructions and times of measurement [10].
2.4.3. Control group
Subjects in the control group were asked to sit calmly and relaxed during the PMR or GI sessions for 30 min.
2.5. Data collection and instruments
The data (questionnaire) were collected at baseline (after randomization and before the beginning of the initial training workshop) and immediately at the end of the interventions by two well-trained research assistants at spacious, quiet, and private rooms at the university. Those research assistants who had master’s degrees in nursing and approximately 20 years nursing experiences were blinded to the study groups. All the study data were approximately collected in similar time and conditions, including similar environment and room temperature. The collected data included the following parts:
2.5.1. Socio-demographic and behavioral variables
The socio-demographic and behavioral characteristics of the study subjects were evaluated by questions created by the study authors. These include gender, marital status, employment status, age, the number of cigarettes per day, and the number of sleeping hours per day.
2.5.2. Emotional symptoms
The emotional symptoms were measured by the Depression, Anxiety and Stress Scale - 21 (DASS-21) [29]. It includes three self-administered subscales developed to assess the negative emotions of depression, anxiety, and stress. Each DASS21 subscale consists of seven items, measured on a Likert-type scale that ranges from zero (does not apply to me at all) to three (applies to me very much). The total scores for each subscale ranges from zero to 21, with higher scores indicating higher levels of depression, anxiety, and stress [29, 30]. It has shown acceptable levels of construct validity and reliability when used in non-clinical populations [30]. In the present study, the Cronbach’s alphas for the stress, anxiety, and depression subscales were .73, .82, and .80 respectively, suggesting acceptable levels of internal consistency.
2.5.3. Physical symptoms
The physical symptoms were measured by the Patient Health Questionnaire- 15 (PHQ-15). It is a self-reported scale derived from the full Patient-Health-Questionnaire to measure the severity levels of physical symptoms [31]. It includes 15 items measured on a Likert-type scale that range from zero (not bothered at all) to two (bothered a lot). The total score ranges from zero to 30, with higher scores indicating severe levels of somatization. Evidence supports reliability and validity of the PHQ-15 as a measure of physical symptoms in general populations [31]. In the current study, the Cronbach’s alpha for the PHQ-15 was .88, suggesting acceptable levels of good internal consistency.
2.6. Statistical analysis
Statistical analysis was performed by SPSS software (version 25). Means, standard deviations and frequencies were used as measures to describe the study sample and variables. One-way ANOVA and Chi-squared tests were run to ensure that no significant differences between the study groups were detected in terms of sociodemographic characteristics and dependent variables at baseline.
One-way MANOVA was used for hypothesis testing. However, before conducting the MANOVA, normality using Kolmogorov-Smirnov and histograms were checked and managed appropriately. The correlation matrix was produced to assess and ensure that the dependent variables were not highly associated with each other.
Post hoc one-way ANOVA tests were used to evaluate whether the study groups were statically different on each of the dependent variables. Because of multiple testing, Bonferroni’s correction was used to adjust the significance level, and the p value of .05 was divided by four (i.e., the number of dependent variables), with p value of .0125 used as level of significance for all ANOVA tests.
2.7. Ethical considerations
The current study was reviewed and approved by the Institutional Review Board at Jordan University of Science and Technology and completed in accordance with the guidelines of the Declaration of Helsinki. Informed consent was obtained from all participants. The study protocol was registered in ClinicalTrail.gov, identifier: NCT05172804.
3. Results
3.1. Attrition
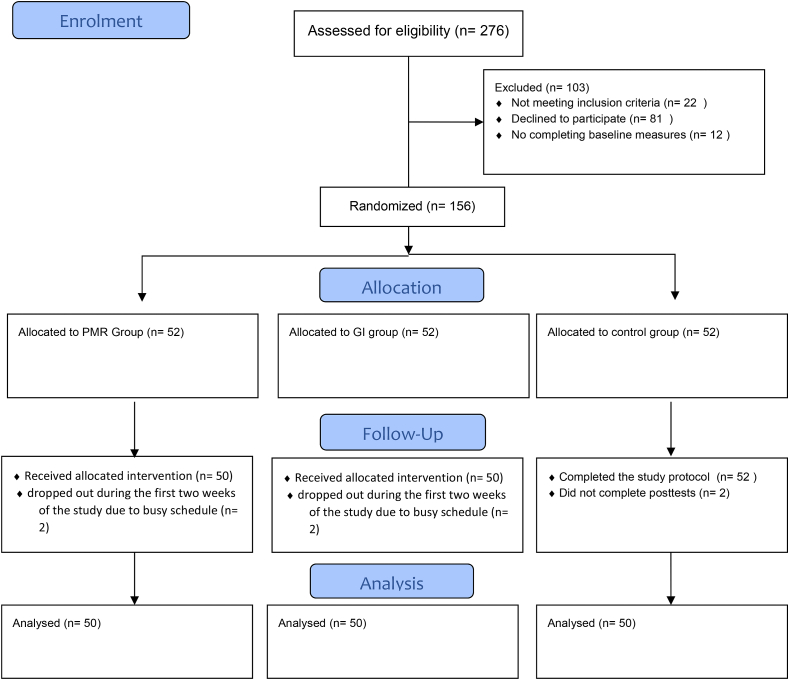
Of the 270 students who were asked to participate in the study, 168 were interested in participating and met the inclusion criteria. Of those students, 12 did not complete the pre-tests because of their tight schedule. The remaining 156 students were equally randomized to the PMR group (n = 52), the GI group (n = 52), and the control group (52). Of those students, two participants from the PMR group and two from the GI group dropped out during the first two weeks of the study. In the control group, two participants did not complete the post-tests. Accordingly, the analysis was conducted on 50 participants in each study group (see Figure 1). All participants who dropped out due to their tight schedule were not statistically different from those who completed the study.
Figure 1.
Study flow diagram for the study participants.
3.2. Descriptive statistics
3.2.1. PMR group
Of 50 participants in the PMR group, 21 were male, and 29 were female. They were predominantly unemployed (n = 45) and single (n = 49). The average age of the participants was 19.76 years (see Table1).
Table 1.
Sociodemographic characteristics and baseline scores of dependent variables (N = 150).
| Variables | n [%] |
x2 [p] | |||
|---|---|---|---|---|---|
| GI | PMR | Control | |||
| Sex | Male | 23 [46] | 21 [42] | 14 [28] | 3.76[.152] |
| Female | 27 [54] | 29 [58] | 36 [72] | ||
| Marital status | Single | 49 [98] | 49 [98] | 50 [100] | 1.01 [.602] |
| Married | 1 [2] | 1 [2] | 0 [0] | ||
| Employment status | Yes | 4 [8] | 5 [10] | 5 [10] | 4.19 [.650] |
| No | 46 [92] | 45 [90] | 45 [90] | ||
| Smoking status | Yes | 13 [26] | 12 [24] | 14 [28] | .20 [.901] |
| No | 37 [74] | 38 [76] | 36 [72] | ||
| Mean [SD] | F[p] | ||||
| Age | 19.57 [.53] | 19.76 [2.04] | 19.38 [.63] | 1.11 [.33] | |
| Physical Symptoms | 11.50 [7.25] | 11.14 [5.59] | 11.54 [5.97] | .06 [.941] | |
| Depression | 9.98 [2.52] | 10.42 [5.18] | 10.20 [4.52] | .13 [.874] | |
| Anxiety | 9.60 [3.07] | 7.94 [4.11] | 7.88 [4.75] | 2.91 [.057] | |
| Stress | 10.66 [2.75] | 10.50 [3.90] | 10.34 [4.19] | .09 [.910] | |
Note. GI = Guided imagery, PMR = Progressive muscle relaxation.
3.2.2. GI group
In the GI group (n = 50), 23 participants were male, and 27 were female. Most of them were single (n = 49) and unemployed (n = 46). The average age of the participants in the GI group was 19.57 years (see Table 1).
3.2.3. Control group
In the control group (n = 50), 14 of the participants were male and 36 were female. The majority were single (n = 50) and unemployed (n = 45). The average age of the participants was 19.38 years (see Table 1).
3.3. Comparison between groups at baseline on sociodemographic characteristics and dependent variables
Chi-squared and one-way ANOVA tests were used to examine any statistical differences between the study groups on the sociodemographic variables. The study groups were not statistically different in terms of sex (X2 (2) = 3.76, p = .152), marital status (X2 (2) = 1.014, p = .602), employment status (X2 (6) = 4.19, p = .650), age (F (2) = 1.11, p = .332), smoking status (X2 (2) = .20, p = .901), daily sleeping hours (F (2) = 2.79) (see Table 1).
One-way ANOVA tests were conducted to examine any significant differences between the study groups on the dependent variables at baseline. The results showed that there were no significant differences between the study groups on the pretest mean scores of physical symptoms (F(2) = .06, p = .941), depression (F(2) = .13, p = .874), anxiety (F(2) = 2.91, p = .057), or baseline stress scores (F(2) = .09, p = .91) (see Table 1).
3.4. Comparison between groups on dependent variables at end of interventions
One-Way Multivariate Analysis of Variance [MANOVA] tests were run to examine the mean differences between the three study groups in the mean post test scores of physical health, depression, anxiety, and stress. The results showed that there was a statistically significant difference between the three study groups on the combined scores of the four dependent variables (Pillais' Trace = .34, F (8, 290) = 7.47, p < .001). The effect size was 0.17, indicating that 17 % of the variance in the combined scores of the dependent variables was accounted for by the study groups (see Table 2).
Table 2.
Comparison between the study groups on dependent variables at the end of interventions (N = 150).
| Variables | Post-test Means [SD] |
ANOVA |
Mean difference [p] |
||||
|---|---|---|---|---|---|---|---|
| GI | PMR | Control | F [p] | GI vs Control | PMR vs Control | GI vs PMR | |
| Physical symptoms | 7.90 [3.61] | 6.62 [4.02] | 11.56 [6.44] | 13.91 [.00] | 3.66 [.001] | 4.94 [.00] | 1.28 [.57] |
| Depression | 4.28 [3.73] | 7.00 [4.64] | 8.20 [4.60] | 10.62 [.00] | 3.92 [.00] | 1.2 [.512] | 2.72 [.007] |
| Anxiety | 4.20 [3.69] | 7.24 [5.21] | 7.90 [4.98] | 8.88 [.00] | 3.70 [.00] | .66 [1.00] | 3.04 [.004] |
| Stress | 5.06 [3.77] | 8.08 [4.88] | 9.90 [4.93] | 14.36 [.00] | 4.84 [.00] | 1.82 [.144] | 3.02 [.004] |
Note: GI = Guided imagery, PMR = Progressive muscle relaxation.
At the end of interventions, the post hoc one-way ANOVA tests with Bonferroni corrections showed statistically significant mean differences between the three study groups on physical symptoms (F(2) = 13.91, p < .001, partial η2 = .159), depression (F(2) = 10.62, p < .001, partial η2 = .126), anxiety (F(2) = 8.88, p < .001, partial η2 = .108) and stress (F(2) = 14.36, p < .001, partial η2 = .1640 (see Table 2).
The results of post hoc comparisons between the study groups on each dependent variable using multiple t-tests with Bonferroni corrections showed that physical symptoms were significantly lower in the GI group (mean difference = 3.66, p = .001) and PMR group (mean difference = 4.94, p = .00) than in the control group. No significant differences between the PMR and GI groups were detected on physical symptoms score (mean difference = 1.28, p = .57). Mean depression score was significantly lower in the GI group than in the control group (mean difference = 3.92, p = .00) and the PMR group (mean difference = 2.72, p = .007).
No significant differences between the PMR and control groups were detected on depression score (mean difference = 1.2, p = .512). Mean anxiety score was significantly lower in the GI group than in the PMR group (mean difference = 3.04, p = .004) and control group (mean difference = 3.70, p = .00). No significant differences between the PMR and control groups were detected on anxiety score (mean difference = .66, p = 1.00). Finally, mean stress score was significantly lower in the GI than in the PMR group (mean difference = 3.02, p = .004) and control group (mean difference = 4.84, p = .00). No significant differences between the PMR and control groups were detected on stress score (mean difference = 1.82, p = .144) (see Table 2).
4. Discussion
The purpose of this study was to compare the differential treatment effects of GI and PMR on physical and emotional symptoms in nursing students taking their initial clinical training. Compared to control conditions, the results of the current study showed that GI and PMR resulted in significant greater reductions in physical symptoms even though the reduction in physical symptoms was larger in the PMR group. However, GI resulted in greater decreases in emotional symptoms such as depression, stress, and anxiety as compared to PMR and control conditions. It has not been possible to demonstrate that the PMR has a significant effect on emotional symptoms, only on physical symptoms.
The findings of the current study support and extend an existing body of knowledge about the potential benefits of PMR and GI on physical symptoms. Regarding PMR, the findings of the current study are consistent with other studies indicating that PMR was effective in improving fatigue and sleep disorders in patients with chronic renal failure undergoing hemodialysis [14], vomiting, nausea, and pain in cancer patients [15, 16], and pain, sleep quality, and physical activities in women after caesarean section [17]. Furthermore, the findings of the current study demonstrating the effectiveness of GI to decrease physical symptoms are in line with other studies showing that GI significantly decreased physical symptoms such as pain in critically ill patients [21], fatigue and pain in patients with musculoskeletal disorders [22], and sleep disorders in hemodialysis patients [23].
Moreover, the findings of the current study showed that PMR was more effective than GI in improving physical symptoms. These findings support the ABC relaxation theory arguing that PMR is a somatic relaxation technique which is more effective than any other relaxation techniques in decreasing physical symptoms [10]. According to the ABC relaxation theory, PMR deploys and develops the access skill of tensing up-letting go those results in reductions in stressed skeletal muscles. The initial effects of reduced stressed muscle could cause general physical relaxation that come in opposition to physical stressful arousals accompanied with physical symptoms [10].
Regarding emotional symptoms, the findings of the current study showed depression, anxiety, and stress were statistically lower in the GI group than the PMR group and the control group at the end of intervention. These findings come in line with previous studies. Compared to control conditions, GI resulted in greater reductions in anxiety in critically ill patients [21], depression, anxiety, and stress in patients with musculoskeletal disorders [22], anxiety in hemodialysis patients [23] state anxiety, test anxiety, and stress in nursing students [25, 26]. These findings support the ABC relaxation theory claiming that GI is more effective than PMR in improving emotional symptoms. According to the ABC relaxation theory, GI involves deploying and developing the access skill of relaxing imagery, which facilitates the attentional shift from self-stressing verbal thoughts to nonverbal activity such as thinking about relaxing images, sounds, touch sensations, and smells. This developed access skill can evoke relaxing emotions such as happiness and joy, rather than emotion-stirring thoughts primarily associated with feelings of anxiety, stress, and depression [10].
The findings of the current study showed that although PMR decreased stress, anxiety, and depression compared to the control condition, these findings did not reach statistically significant levels. These findings are inconsistent with previous studies showing that PMR produced statistically significant greater reductions in depression, anxiety, and stress in patients with chronic renal failure undergoing hemodialysis [14], patients with cancers [15, 16], patients with COVID-19 [18] and nursing students [19, 20] when compared to control conditions. These non-significant findings may be attributed to the idea that the participants in the PMR group were beginner relaxation practitioners, as most of those participants had not practiced PMR before this study. Thus, they may need to further practice PMR to develop the access skills of PMR and obtain more benefits from this relaxation technique [10].
4.1. Limitations
The study had limitations. The subjects in the current study were recruited from the same university, limiting generalizability to students from other universities. Therefore, it is recommended that future studies select students from multiple settings. Moreover, the long-term effects of the PMR and GI were not evaluated, and thus, it is recommended that future studies include follow-up evaluations. Also, two cross-sections (pre and post) have been done but that no longitudinal analysis (pre-post) has been done. Two subjects from each group dropped out during the study that might limit validity.
4.2. Implication for practice
To best of our knowledge, this is the first study to evidence the differential treatment effects of PMR and GI on physical and emotional symptoms in nursing students taking their initial clinical training. The current results may be used to guide nursing practice and education. The positive results regarding the deferential impacts of PMR and GI on emotional and physical symptoms give clinicians and nurses tools for intelligently tailoring relaxation approaches to nursing students and other populations based on health problems they experience. Also, the current results may encourage nursing educators to integrate these mind-body relaxation approaches into nursing curricula.
The use of mind-body programs such as PMR and GI may have important advantages over other stress-reduction programs among nursing students in Jordan. Nursing colleges in Jordan have considerably limited financial resources. Thus, the stress-reduction program in Jordan must be within the constraints of the colleges' budgets [32, 33]. Mind-body modalities such as PMR and GI are inexpensive stress-reduction modalities that do not requires therapist involvement, materials, or preparation once learned [10, 20, 34]. Also, mental health problems are stigmatized among Jordanian university students, considered as a significant barrier to seeking mental health services [32, 33]. However, once learned, PMR and GI can be self-practiced by students without visits to mental healthcare settings [10, 20, 34].
5. Conclusions
The findings of the present study provide evidence of the differential effectiveness of two commonly used mind-body relaxation approaches—PMR and GI on emotional and/or physical symptoms in nursing students taking their initial clinical training. The study findings showed that both PMR and GI produced significant improvements in physical symptoms although PMR was more effective in this regard. In respect of emotional symptoms, GI produced significant greater reductions in stress, depression, and anxiety than PMR and control conditions. It has not been possible to demonstrate that the PMR has a significant effect on emotional symptoms, only on physical symptoms, supporting the ABC relaxation theory [10].
Declarations
Author contribution statement
Hossam Alhawatmeh: Conceived and designed the experiments; Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Raya Albataineh: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Sawsan Abuhammad: Performed the experiments; Analyzed and interpreted the data.
Funding statement
Dr Hossam Alhawatmeh was supported by Jordan University of Science and Technology [377/2019].
Data availability statement
Data will be made available on request.
Competing interest statement
The authors declare no conflict of interest.
Additional information
The clinical trial described in this paper was registered at ClinicalTrials.gov under the registration number NCT05172804.
Supplementary content related to this article has been published online at https://doi.org/10.1016/j.heliyon.2022.e11147.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Shaban I.A., Khater W.A., Akhu-Zaheya L.M. Undergraduate nursing students’ stress sources and coping behaviors during their initial period of clinical training: a Jordanian perspective. Nurse Educ. Pract. 2012;12(4):204–209. doi: 10.1016/j.nepr.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 2.Chan C.K., So W.K., Fong D.Y. Hong Kong baccalaureate nursing students' stress and their coping strategies in clinical practice. J. Prof. Nurs. 2009;25(5):307–313. doi: 10.1016/j.profnurs.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 3.Jan L.K., Popescu L. Israel’s nursing students' stress sources and coping strategies during their first clinical experience in hospital wards-a qualitative research. Soc. Work Rev./Revista De Asistenta Sociala. 2014;13(4):163–188. [Google Scholar]
- 4.Gurková E., Zeleníková R. Nursing students' perceived stress, coping strategies, health and supervisory approaches in clinical practice: a Slovak and Czech perspective. Nurse Educ. Today. 2018;65:4–10. doi: 10.1016/j.nedt.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 5.Cheung T., Wong S.Y., Wong K.Y., Law L.Y., Ng K., Tong M.T., Wong K.Y., Ng M.Y., Yip P.S. Depression, anxiety and symptoms of stress among baccalaureate nursing students in Hong Kong: a cross-sectional study. Int. J. Environ. Res. Publ. Health. 2016;13(8):779. doi: 10.3390/ijerph13080779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Torres G.C., Paragas E.D. Social determinants associated with the quality of life of baccalaureate nursing students: a cross-sectional study. Nurs. Forum. 2019;54(2):137–143. doi: 10.1111/nuf.12306. [DOI] [PubMed] [Google Scholar]
- 7.Ekenze O.S., Ezeala-Adikaibe B.A., Orjioke C., Mbadiwe N., Ijoma U.N., Onyekonwu C., Ezeala-Adikaibe N.P., Onodugo O., Anyim O., Okpara T., Nwatu C.B. Prevalence and pattern of migraine, tension type headache and chronic daily headache among medical and nursing students in Enugu, southeast Nigeria. Health. 2018;10(10):1283–1293. [Google Scholar]
- 8.van Vliet M., Jong M.C., Jong M. A mind–body skills course among nursing and medical students: a pathway for an improved perception of self and the surrounding world. Glob. Qual. Nurs. Res. 2018;5:1–13. doi: 10.1177/2333393618805340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toussaint L., Nguyen Q.A., Roettger C., Dixon K., Offenbächer M., Kohls N., Hirsch J., Sirois F. Effectiveness of progressive muscle relaxation, deep breathing, and guided imagery in promoting psychological and physiological states of relaxation. Evid. Based Compl. Alternat. Med. 2021;2021 doi: 10.1155/2021/5924040. Article ID 5924040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith J.C. Springer Publishing Company; 2005. Relaxation, Meditation, & Mindfulness: A Mental Health Practitioner’s Guide to New and Traditional Approaches. [Google Scholar]
- 11.Jacobson E. The University of Chicago Press; Chicago, IL: 1974. Progressive Relaxation: A Physiological and Clinical Investigation of Muscular States and Their Significance in Psychology and Medical Practice. [Google Scholar]
- 12.Bernstein D.A., Borkovec T.D. Research Press; Champaign, IL: 1973. Progressive Relaxation Training: a Manual for the Helping Professions. [Google Scholar]
- 13.Ost L.G. Applied relaxation: description of a coping technique and review of controlled studies. Behav. Res. Ther. 1987;25(5):397–409. doi: 10.1016/0005-7967(87)90017-9. [DOI] [PubMed] [Google Scholar]
- 14.Amini E., Goudarzi I., Masoudi R., Ahmadi A., Momeni A. Effect of progressive muscle relaxation and aerobic exercise on anxiety, sleep quality, and fatigue in patients with chronic renal failure undergoing hemodialysis. Int. J. Pharmaceut. Chem. Res. 2016;8(12):1634–1639. [Google Scholar]
- 15.Gupta B., Kumari M., Kaur T. Effectiveness of progressive muscle relaxation technique on physical symptoms among patients receiving chemotherapy. Nurs. Midwifery Res. J. 2016;12:33–40. [Google Scholar]
- 16.kumari Samantaray K., Pahantasingh S., Pradhan J., Pradhan R. Progressive muscle relaxation therapy on anxiety among hospitalized cancer patients. Eur. J. Mol. Clin. Med. 2020;7(8):1485–1488. [Google Scholar]
- 17.Ismail N.I., Elgzar W.T. The effect of progressive muscle relaxation on post cesarean section pain, quality of sleep and physical activities limitation. Int. J. Stud. Nurs. 2018;3(3):14. [Google Scholar]
- 18.Xiao C.X., Lin Y.J., Lin R.Q., Liu A.N., Zhong G.Q., Lan C.F. Effects of progressive muscle relaxation training on negative emotions and sleep quality in COVID-19 patients: a clinical observational study. Medicine. 2020;99(47) doi: 10.1097/MD.0000000000023185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gangadharan M.P., Madani M.A. Effectiveness of progressive muscle relaxation techniques on depression, anxiety and stress among undergraduate nursing students. Int. J. Health Sci. Res. 2018;8(2):155–163. [Google Scholar]
- 20.Alhawatmeh, H. N. Effects of Abbreviated Progressive Muscle Relaxation on Stress in Jordanian Nursing Students (Doctoral dissertation, Kent State University). [DOI] [PubMed]
- 21.Hadjibalassi M., Lambrinou E., Papastavrou E., Papathanassoglou E. The effect of guided imagery on physiological and psychological outcomes of adult ICU patients: a systematic literature review and methodological implications. Aust. Crit. Care. 2018;31(2):73–86. doi: 10.1016/j.aucc.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 22.Kaplun A., Alperovitch-Najenson D., Kalichman L. Effect of guided imagery on pain and health-related quality of life in musculoskeletal medicine: a comprehensive narrative review. Curr. Pain Headache Rep. 2021;25 doi: 10.1007/s11916-021-00991-y. [DOI] [PubMed] [Google Scholar]
- 23.Afshar M., Mohsenzadeh A., Gilasi H., Sadeghi-Gandomani H. The effects of guided imagery on state and trait anxiety and sleep quality among patients receiving hemodialysis: a randomized controlled trial. Compl. Ther. Med. 2018;40:37–41. doi: 10.1016/j.ctim.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 24.Sanadgol S., Firouzkouhi M., Badakhsh M., Abdollahimohammad A., Shahraki-vahed A. Effect of guided imagery training on death anxiety of nurses at COVID-19 intensive care units: a quasi-experimental study. Neuropsychiatria i Neuropsychologia. 2020;15(3-4):83–88. [Google Scholar]
- 25.Suk M.H., Kil S.Y., Park H.J. The effects of guided imagery on nursing students performing intramuscular injections. J. Korean Acad. Nurs. 2002;32(6):784–791. [Google Scholar]
- 26.Maghaminejad F., Adib-Hajbaghery M., Nematian F., Akhavan Armaki M. The effects of guided imagery on test anxiety among the 1st-year nursing students: a randomized clinical trial. Nurs. Midwifery Stud. 2020;9(3):130–134. [Google Scholar]
- 27.Toussaint L., Nguyen Q.A., Roettger C., Dixon K., Offenbächer M., Kohls N., Hirsch J., Sirois F. Effectiveness of progressive muscle relaxation, deep breathing, and guided imagery in promoting psychological and physiological states of relaxation. Evid. Based Complement Alternat. Med. 2021;2021 doi: 10.1155/2021/5924040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alhawatmeh H.N., Rababa M., Alfaqih M., Albataineh R., Hweidi I., Awwad A.A. The benefits of mindfulness meditation on trait mindfulness, perceived stress, cortisol, and C-reactive protein in nursing students: a randomized controlled trial. Adv. Med. Educ. Pract. 2022;13:47–58. doi: 10.2147/AMEP.S348062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lovibond S.H., Lovibond P.F. Psychology Foundation; Sydney: 1995. Manual for the Depression Anxiety Stress Scales. [Google Scholar]
- 30.Henry J.D., Crawford J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005;44(2):227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- 31.Kocalevent R.D., Hinz A., Brähler E. Standardization of a screening instrument (PHQ-15) for somatization syndromes in the general population. BMC Psychiatr. 2013;13(1):1–8. doi: 10.1186/1471-244X-13-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hamdan-Mansour A.M., Pusak K., Bandak A.G. Effectiveness of cognitive-behavioral therapy on depressive symptomatology, stress and coping strategies among Jordanian university students. Issues Ment. Health Nurs. 2009;30(3):188–196. doi: 10.1080/01612840802694577. [DOI] [PubMed] [Google Scholar]
- 33.Nasir L.S., Al-Qutob R. Barriers to the diagnosis and treatment of depression in Jordan. J. Am. Board Fam. Med. 2005;18(2):125–131. doi: 10.3122/jabfm.18.2.125. [DOI] [PubMed] [Google Scholar]
- 34.National Centers for Complementary and Alternative Medicine Relaxation Techniques for Health: an Introduction. 2011. http://nccam.nih.gov Retrieved from.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.