Abstract
The prevalence of Attention Deficit Hyperactivity Disorder (ADHD) has seen a consistent rise in recent years. These numbers spark a debate over the reason for the observed trends, with some concerned about over diagnosis and over prescription of stimulant medications, and others raising the issue of diagnostic disparities, particularly in underrepresented populations. In this paper we look at both sides, starting with the history of ADHD and its diagnostic criteria changes, from early concepts of alterations in attention and hyperactivity in the 19th and 20th century, to its introduction in the Diagnostical and Statistical Manual of Mental Disorders (DSM), and its evolution into how it is defined today. The general broadening of ADHD diagnostically over time plays a role in the increased prevalence over the years, but it is not the only reason. Increased awareness of physicians and the public is also believed to play a big role, particularly in underrepresented minorities and women. However, there continues to be disparities in detection of ADHD in these groups. There are significant consequences to a patient’s social, interpersonal, and professional life when ADHD is left unrecognized and untreated. Thoughtful evaluation, accurate diagnosis, and adequate treatment can make a big difference.
Case History
Agatha has been struggling with school work since starting college in the fall. She always had difficulty paying attention in certain subjects, but did fairly well in high school. Lately she has been feeling more anxious because her study habits that worked throughout high school no longer seem to be effective. She feels completely inundated by the sheer volume and difficulty of her current assignments. She finds herself constantly procrastinating, regularly feeling guilty about her inability to adhere to deadlines. Problem sets are riddled with careless errors and papers contain numerous typos and grammatical errors. Sometimes, especially after doing poorly on an exam, guilt and anxiety about school become so high that she simply shuts down and avoids doing any work for the rest of the day. She has seen a lot of ADHD content on TikTok recently, and wonders if she may have ADHD herself. Her college friend has offered her Adderall, and while she hasn’t taken it without a prescription, she wonders if she may benefit from it.
Introduction
The past couple of decades have seen a continuous increase in attention deficit hyperactivity disorder (ADHD) diagnoses. National population surveys reflect an increase in the prevalence from 6.1% to 10.2% in the 20-year period from 1997 to 2016 and experts continue to debate and disagree on the causes for this trend.1 On the one hand, while there are children whose diagnoses are irrefutable and undeniably require treatment, some experts worry about the risk of overdiagnosis and subsequent over prescription of stimulants and other psychotropics. Like with most psychotropic medications, treatment consideration needs to be carefully weighed with regards to potential adverse outcomes. For stimulants there is also concern for diversion and misuse of the medication for performance enhancement rather than for treatment. On the other hand, diagnostic disparities and underdiagnosis exist in various communities, including women and underrepresented minorities, as seen with Agatha. In this article, we aim to better understand the debate about the growing number of those affected by reviewing how ADHD morphed into the diagnosis we know today, and the variability and disparities observed.
Attention Deficit Hyperactivity Disorder: The Basics
Attention Deficit Hyperactivity Disorder is a neurodevelopmental disorder that globally affects 5% – 7.2% of youth and 2.5% – 6.7% of adults.2–4 Recent estimates indicate that prevalence is even higher in children in the United States (U.S.), around 8.7% or 5.3 million.5 Although it has long been conceptualized as a disorder of childhood, up to 90% of children with ADHD continue to experience symptoms into adulthood.6 Obtaining a diagnosis in adulthood is also possible, as in one study, 75% of adults with ADHD were not previously diagnosed in childhood.7 While in childhood the male to female ratio is 4:1, the ratio is closer to 1:1 in adults.8
Attention Deficit Hyperactivity Disorder is thought to be caused by a combination of factors: genetic, neurobiologic, and environmental. Twin studies show that ADHD is highly hereditable (60–70%), and scientists have identified a number of genes believed to underlie vulnerability to the disorder.9 This includes genes that regulate the expression of Brain Derived Neurotrophic Factor, which plays a role in learning and memory, as well as those involved in modulation of the brain’s dopaminergic system.9 Environmental risk factors like perinatal complications and toxic exposures are also believed to play a role.9–10
ADHD is a clinical diagnosis, which is accomplished through questionnaires, clinical interview, and in some cases, neuropsychiatric testing. While neuroimaging studies suggest a potential correlation between ADHD and white matter volume abnormalities in cortico-striatal pathways and the prefrontal cortex in study samples, biomarkers are not currently sensitive enough to assist with diagnosis.
The treatment for ADHD is often a combination of medication, skill building, and psychotherapy. In the 1930s, Charles Bradley, MD, noticed a drastic improvement in children’s behavior and school performance after administration of amphetamine sulfate—a drug he was hoping would help treat headaches. That serendipitous discovery led to the development of other stimulants, a class of medications that is still considered the gold standard and first line ADHD treatment. Pharmacologic therapy is reported to be effective in up to 70% of cases, yet the benefits are not without risk.11 The most common side effects are decreased appetite, anxiety, nausea, headaches, and in children in particular, concern about tolerance, weight loss, and insomnia. Data on long-term stimulant use also remains limited. A recent literature review found long-term use to be generally safe, but authors did advise providers to use caution when prescribing stimulants to pre-school age children, adolescents at high risk of abuse, and children with tics and psychosis.12
There are also many non-pharmacological modalities of treatment for ADHD, including behavioral parent training and mindfulness-based attention training.13–14 Psychotherapy, especially cognitive behavioral techniques, has also been shown to be quite effective.11 Finally, a newer non-pharmacological approach, neurofeedback, has some benefits, though clinical application remains logistically challenging. More research is required into its efficacy.15
ADHD: Changes in Diagnostic Criteria Over Time
To understand its diagnostic trends, it is important to consider the origins of ADHD and its diagnostic criteria. In the Eighteenth century, Sir Alexander Crichton wrote one of the earliest documented clinical descriptions of a disorder in attention in his 1798 book On Attention and its Diseases. He described “morbid alterations” of attention that “render [individuals] incapable of attending with constancy to any one object of education.”16 Although not globally recognized and treated at the time, his observations bear striking similarities to modern descriptions of the inattention domains of ADHD.
In the early 1900s, British physician Sir George Frederic Still described a number of children with a “defect of moral control.”17 Although more similar to the modern concepts of conduct disorder (CD) or oppositional disorder (ODD), his description identified a number of features typically seen in ADHD like impulsivity and impaired frustration tolerance. Later, in the 1930s, physicians Kramer and Pollnow wrote about children with “hyperkinetic disease of infancy”, a syndrome that more closely resembled modern ADHD descriptions including both hyperactivity, emotional excitability and impulsivity, and inattention.17
ADHD made its first appearance in the Diagnostic and Statistical Manual of Mental Disorders (or DSM) in 1968, as “Hyperkinetic Reaction of Childhood.” As the name implies, the emphasis was on overactivity and distractibility. In the years that followed, and with subsequent editions of the DSM, there was a clear shift in focus towards attention deficit as the defining feature of the disorder. The publication of the DSM-III in 1980 gave rise to the diagnosis of “attention deficit disorder,” or ADD, a term that remains part of popular vernacular to this day. The DSM-III also introduced a cutoff for the number of symptoms to earn the diagnosis, as well as age at onset, symptom duration, and exclusion of confounding psychiatric disorders and substance use.
The label ADHD that we know and use today first appeared in 1987 with the DSM-III-R, and combined both inattention and hyperactivity domains into one diagnosis. Then, the DSM-IV iteration divided the diagnosis into three subtypes: predominantly inattentive, predominantly hyperactive-impulsive, and combined type. The release of the DSM-V in 2013 saw the definition of ADHD broaden significantly. The changes are summarized in Table 1. One such change allowed for autism spectrum disorder (ASD) and ADHD to coexist, which was not the case in previous iterations. Given the high comorbidity between ADHD and ASD, it is clear that this change, along with others (Table 1), contributed to the rise in ADHD prevalence, as it added a large group of children who were previously excluded.18
Table 1.
Changes in diagnostic determination for ADHD between the Diagnostic and Statistical Manual of Mental Disorders (DSM) IV and V editions
| DSM-IV | DSM-V | |
|---|---|---|
| Number of symptoms required | 6 or more in either inattention of hyperactivity domains | 6 or more in either domain if <17 years old, OR 5 or more in either domain if >17 years old |
| Age of symptom onset | <7 years | <12 years |
| Impairments at onset | Onset of impairment <7 years | Not required |
| Pervasiveness | “Evidence of impairment in 2 or more settings” | “Evidence of symptoms in 2 or more settings” |
| Autism exclusionary? | Yes | No |
Clearly, the evolution of the diagnostic criteria accounts for some of the rise in ADHD. In fact, Polanczyk and his collaborators have done a lot of work on ADHD epidemiology—and they have consistently demonstrated that the observed variability in prevalence rates across various studies was attributed largely to differences in measurement of outcomes, namely the criteria used to diagnose ADHD and the inclusion or exclusion of functional impairment.19–20
The changing criteria only makes clinical diagnosis more difficult. In the absence of biomarkers, diagnosis is made by signs and symptoms. Some helpful questions for screening by clinicians are suggested in Table 2. However, this leaves a lot up to the clinician, and may lead to under and over diagnosis. Due to the overlapping nature of psychiatric symptoms, ADHD is often missed, and patients end up with inaccurate psychiatric diagnoses and medication regimen. This latter point is important as we now know ADHD has high rates of psychiatric comorbidities, such as behavioral aberrances (52%), anxiety (33%), depression (17%), and autism (14%). While this may lead to overdiagnosis, more likely than not, ADHD can be misdiagnosed as a result, and subsequently inadequately treated.21 Screening tools have been developed and validated for detection of ADHD in adults such as WHO’s Adult ADHD Self Report Scales or ASRS and many clinicians will ask for reports from schools and loved ones as well.22 Referring to neuropsychiatric testing is also an option, though it is expensive and not required to make the diagnosis.
Table 2.
Example of questions clinicians can ask when assessing for ADHD. Adapted from “Integrative Treatment for Adult ADHD: A Practical, Easy-to-use Guide for Clinicians” by Ari Tuckman (New Harbinger Publications, 2007). Broader questions can often elicit more information and will allow clinicians to explore more in depth than a memorizable check-list.
| Helpful Diagnostic Questions for Clinicians |
|---|
| Could you describe how it feels when you have to sit through a long movie or meeting? |
| Tell me how you did with being attentive in class in middle school compared to other students? |
| What is your experience when you try to read or focus on work for an extended period of time? |
| Have you ever made a mistake on an exam or at work that could have easily been prevented? |
| Do you often lose things like your keys or cell phone? If so, what do you do to keep track of them? |
| How likely are you to remember to do a task without writing it down (make a phone call, water the plants, do the laundry etc..) |
| What happens when you have a lot of tasks to do and need to get them all done? |
| Tell me about your ability to focus on things you like and want to do as opposed to harder less exciting things. |
| Do your friends and family ever ask you if you are paying attention to them? Do you feel you need to ask them to repeat something? Do you sometimes pretend you heard the conversation but actually didn't? |
| Do you ever feel the urge to say whatever is on your mind right there and then, sometimes interrupt people? Does it ever get you in trouble with others? For example, losing friendships, or having difficulties with your boss? |
| Do you drink coffee? If so, how much and how do you notice it affects you? |
Note to clinicians: In addition to the questions mentioned above, you can rely on close observation of patient presentation to help in your diagnosis. A few things to consider include: Is the patient late? Have they missed any appointments before this one? Does the patient talk fast and is difficult to interrupt? Do they forget the question you asked and often ask you to repeat things? Are they constantly fidgeting or moving around? Do you see piles of papers in their bag, or on zoom, a mess behind them?
ADHD: Increased Awareness, Increased Prevalence
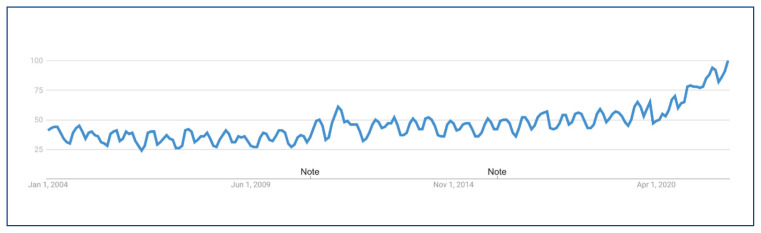
Outside of simply diagnostic changes, studies have provided other explanations for the rise in ADHD, including increased awareness and familiarity of physicians and the public with the diagnosis, geographic location and cultural differences, as well as other public health related factors such as improved access to care.23 ADHD has even earned its own Awareness Month as of October of 2004. A quick search on Google Trend shows a steady increase in ADHD-related searches throughout the years, with popularity in March 2022 at the highest it has ever been (Figure 1).
Figure 1.
Google search trends for the term “ADHD”, from 2004 to present
ADHD has also become prominent in popular culture. Characters with problems in attention and hyperactivity can be found all over early literary works - physician Heinrich Hoffman wrote short stories in the mid-1800s featuring characters like “Fidgety Philip” and “Johnny Look-in-the-Air,” the names of which alone indicate hyperactivity and inattention as core features of the characters.24 Today, a number of movies and television characters have ADHD as part of their plotline and defining features - from Barney Stinson on “How I Met Your Mother,” to Phil Dunphy on “Modern Family,” and even Bart Simpson. Social media has also propelled ADHD into popular awareness, as it has taken over platforms like TikTok and Twitter. As of May 2022, the hashtag #adhd has 11.4 billion views on TikTok. Many people credit these platforms with helping them realize they had the diagnosis and subsequently seeking treatment for it. However, as is always the case with the internet and social media, misinformation about ADHD is fairly prevalent. A recent study has found that more than half of ADHD content on TikTok was misleading, most of them posted by non-health care providers.25 That same study however did show that content posted by health care providers was overwhelmingly more accurate and useful to consumers.25
ADHD and Undertreatment
While there is concern from rising ADHD diagnoses, a U.S. national survey reported in 2006 that only 11% of adults with ADHD were being treated for it. This is critical as deficits in organization and time management can lead to major educational, professional, or financial problems, with higher drop-out rates, higher unemployment rates, and lower income attainment in adults with ADHD.26 Deficits can also have major interpersonal implications, with higher rates of divorce documented in adults with ADHD, for example.27 People with untreated ADHD are also at elevated risk of substance use, car accidents, unintentional injuries, depression, anxiety, and suicide.28 In other words, underdiagnosis has significant implications, far beyond inability to focus.
Some have raised concerns over non-medical use of stimulants. Non-medical use is most studied in student populations, where medications can function as either a cognitive enhancer, or are used recreationally. However, while some studies reported non-prescribed use of stimulants in about 7% of college students, most of the misuse was in the setting of attentional difficulties impairing the student’s ability to succeed in class.29 This is a possible indication that said student has undiagnosed ADHD, and not a desire to use the medication to get ahead. More importantly, a recent review has found that pharmacological treatment of ADHD was associated with a decreased risk of substance use, not the opposite.30
Disparities in ADHD Diagnosis in Minoritized Populations
Any discussion of ADHD diagnostic trends would be incomplete without a review of disparities among minoritized population. Increasing awareness of these disparities might be contributing to the increase in rates of diagnosis. Over the past 20 years, available literature showcases the presence of pervasive disparities in ADHD diagnosis related to both race and gender. For instance, between 2004–2006, Black students were more likely than their White counterparts to have ADHD symptoms (12% vs. 7% respectively), but were less likely to have received a diagnosis (9% vs. 14% respectively).31 During the following decade, rates of diagnosis among Black individuals grew at a rate 3 times higher than among White individuals.32 Similar trends have been seen among girls, who demonstrated a 3 times higher increase in diagnosis rates than boys over the past two decades.32–33 In fact, with regard to gender, experts have attributed changes in DSM-IV diagnostic criteria to recent diagnostic trends. Following changes that placed increased focus on inattention, rather than hyperactivity, there was a correspondingly significant increase in ADHD diagnosis among females.34 Specifically, between 1991 and 2008, diagnosis rates increased by a factor of 5.6 in girls compared to only 3.7 in boys.35 In other words, knowing girls and underrepresented groups are more likely to have missed diagnoses, and even present with different symptoms, patients and clinicians might be asking more questions as a result. The rise might be due to the fact that these groups are just simply finally diagnosed, rather than over-diagnosed.
Even still, the data suggests we still are missing groups and underdiagnosing ADHD for many. To date, recent findings indicate that ADHD continues to be less frequently diagnosed in youth who are Black Indigenous and Persons of Color (BIPOC) and female, compared to those who are White and male, even after controlling for potential confounders such as socioeconomic status and adverse childhood experiences.36–37 Girls continue to be diagnosed at older ages than boys and tend to endorse higher levels of perceived stress.38 Reasons for these disparities stem from a multitude of systems level factors, however racial and gender bias is likely to play a major role. For example, diagnosis of any mental illness, especially ADHD, depends on individual interpretations of behavior and the way that a clinician integrates multiple informant reports from parents, caregivers, and teachers. Studies have found that clinicians tend to be more responsive to White parents who solicit an ADHD diagnosis and treatment for their child compared to BIPOC parents.39 Further, BIPOC youth with ADHD are disproportionately more likely to be misdiagnosed with ODD or CD.40–41
ADHD manifests differently across gender, as there may be stronger social pressures for girls to sit quietly compared to boys. In fact, studies show that boys have historically been more likely to exhibit hyperactivity and disruptive behaviors, prompting earlier detection of the disorder, compared to those with inattentive symptoms, a group that most often includes girls.42 Interestingly, other studies have indicated there to be no true difference in level of hyperactivity across gender, rather a bias among teachers leading to under-recognition of hyperactive symptoms among girls.43 While some are concerned about the overdiagnosis of ADHD, there are still many groups who are underdiagnosed and unaccounted for in the data. Ultimately, focusing on the idea of “overdiagnosis” among providers may be harmful, particularly for these populations, as this may present additional barriers to them receiving appropriate care.
Conclusion
ADHD is not a new phenomenon, however its prevalence has increased significantly in the recent years. Given changing diagnostic criteria and increasing awareness of the disorder in marginalized populations, especially individuals of color and females, this finding is not surprising. The general public has become increasingly more aware of ADHD through the media and social media. People are more likely to bring up their concerns to a physician, which in turn might prompt more numbers of people to be diagnosed. While some may argue that the increase is concerning and due to intentional feigning of symptoms in order to gain access to stimulant medication or test accommodations, the evidence suggests these groups have a negligible impact on diagnostic trends. In fact, as medical providers, focus on the idea of “overdiagnosis” may instead be harmful, create additional barriers to care, and add to the stigma towards their requests for help. It is important, instead, to approach patients holistically, and with an understanding of both the risks of treatment and undertreatment in mind. For those who have been struggling with unrecognized ADHD, there are significant impacts to mental health, social life, and work life. Thoughtful diagnosis and subsequent treatment can make all the difference.
Footnotes
Elie Abdelnour, MD, (above) and Jessica A. Gold, MD, MS, are in the Department of Psychiatry, Washington University School of Medicine, St. Louis, Missouri. Madeline O. Jansen, MD, MPH, is with the Department of Psychiatry, Child and Adolescent Division, University of California-Los Angeles, Los Angeles, California.
Disclosure
None reported.
References
- 1.Xu G, Strathearn L, Liu B, Yang B, Bao W. Twenty-Year Trends in Diagnosed Attention-Deficit/Hyperactivity Disorder Among US Children and Adolescents, 1997–2016. JAMA Netw Open. 2018;1(4):e181471. doi: 10.1001/jamanetworkopen.2018.1471.. Published 2018 Aug 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Posner J, Polanczyk GV, Sonuga-Barke E. Attention-deficit hyperactivity disorder. Lancet. 2020;395(10222):450–462. doi: 10.1016/S0140-6736(19)33004-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and metaanalysis. Pediatrics. 2015;135(4):e994–e1001. doi: 10.1542/peds.2014-3482.. [DOI] [PubMed] [Google Scholar]
- 4.Song P, Zha M, Yang Q, Zhang Y, Li X, Rudan I. The prevalence of adult attention-deficit hyperactivity disorder: A global systematic review and meta-analysis. J Glob Health. 2021;11:04009. doi: 10.7189/jogh.11.04009.. Published 2021 Feb 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bozinovic K, McLamb F, O’Connell K, et al. U.S. national, regional, and state-specific socioeconomic factors correlate with child and adolescent ADHD diagnoses pre-COVID-19 pandemic. Sci Rep. 2021;2008;11(1):2. doi: 10.1038/s41598-021-01233-2.. Published 2021 Nov 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sibley MH, Arnold LE, Swanson JM, et al. Variable Patterns of Remission From ADHD in the Multimodal Treatment Study of ADHD. Am J Psychiatry. 2022;179(2):142–151. doi: 10.1176/appi.ajp.2021.21010032.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faraone SV, Spencer TJ, Montano CB, Biederman J. Attention-deficit/hyperactivity disorder in adults: a survey of current practice in psychiatry and primary care. Arch Intern Med. 2004;164(11):1221–1226. doi: 10.1001/archinte.164.11.1221.. [DOI] [PubMed] [Google Scholar]
- 8.Palladino VS, McNeill R, Reif A, Kittel-Schneider S. Genetic risk factors and gene-environment interactions in adult and childhood attention-deficit/hyperactivity disorder. Psychiatr Genet. 2019;29(3):63–78. doi: 10.1097/YPG.0000000000000220.. [DOI] [PubMed] [Google Scholar]
- 9.Núñez-Jaramillo L, Herrera-Solís A, Herrera-Morales WV. ADHD: Reviewing the Causes and Evaluating Solutions. J Pers Med. 2021;11(3):166. doi: 10.3390/jpm11030166.. Published 2021 Mar 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zayats T, Neale BM. Recent advances in understanding of attention deficit hyperactivity disorder (ADHD): how genetics are shaping our conceptualization of this disorder. F1000Res. 2019;8 doi: 10.12688/f1000research.18959.2.. F1000 Faculty Rev-2060. Published 2019 Dec 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jensen PS, Arnold LE, Swanson JM, et al. 3-year follow-up of the NIMH MTA study. J Am Acad Child Adolesc Psychiatry. 2007;46(8):989–1002. doi: 10.1097/CHI.0b013e3180686d48.. [DOI] [PubMed] [Google Scholar]
- 12.Krinzinger H, Hall CL, Groom MJ, et al. Neurological and psychiatric adverse effects of long-term methylphenidate treatment in ADHD: A map of the current evidence. Neurosci Biobehav Rev. 2019;107:945–968. doi: 10.1016/j.neubiorev.2019.09.023.. [DOI] [PubMed] [Google Scholar]
- 13.Ciesielski HA, Loren REA, Tamm L. Behavioral Parent Training for ADHD Reduces Situational Severity of Child Noncompliance and Related Parental Stress. J Atten Disord. 2020;24(5):758–767. doi: 10.1177/1087054719843181.. [DOI] [PubMed] [Google Scholar]
- 14.Modesto-Lowe V, Farahmand P, Chaplin M, Sarro L. Does mindfulness meditation improve attention in attention deficit hyperactivity disorder? World J Psychiatry. 2015;5(4):397–403. doi: 10.5498/wjp.v5.i4.397.. Published 2015 Dec 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Micoulaud-Franchi JA, Geoffroy PA, Fond G, Lopez R, Bioulac S, Philip P. EEG neurofeedback treatments in children with ADHD: an updated meta-analysis of randomized controlled trials. Front Hum Neurosci. 2014;8:906. doi: 10.3389/fnhum.2014.00906.. Published 2014 Nov 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crichton A. An inquiry into the nature and origin of mental derangement: on attention and its diseases. Reprint published in J Atten Disord. 2008;12(3):200–206. doi: 10.1177/1087054708315137.. [DOI] [PubMed] [Google Scholar]
- 17.Lange KW, Reichl S, Lange KM, Tucha L, Tucha O. The history of attention deficit hyperactivity disorder. Atten Defic Hyperact Disord. 2010;2(4):241–255. doi: 10.1007/s12402-010-0045-8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zablotsky B, Bramlett MD, Blumberg SJ. The Co-Occurrence of Autism Spectrum Disorder in Children With ADHD. J Atten Disord. 2020;24(1):94–103. doi: 10.1177/1087054717713638.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942–948. doi: 10.1176/ajp.2007.164.6.942.. [DOI] [PubMed] [Google Scholar]
- 20.Posner J, Polanczyk GV, Sonuga-Barke E. Attention-deficit hyperactivity disorder. Lancet. 2020;395(10222):450–462. doi: 10.1016/S0140-6736(19)33004-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McIntosh D, Kutcher S, Binder C, Levitt A, Fallu A, Rosenbluth M. Adult ADHD and comorbid depression: A consensus-derived diagnostic algorithm for ADHD. Neuropsychiatr Dis Treat. 2009;5:137–150. doi: 10.2147/ndt.s4720.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kessler RC, Adler L, Ames M, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35(2):245–256. doi: 10.1017/s0033291704002892. [DOI] [PubMed] [Google Scholar]
- 23.Xu G, Strathearn L, Liu B, Yang B, Bao W. Twenty-Year Trends in Diagnosed Attention-Deficit/Hyperactivity Disorder Among US Children and Adolescents, 1997–2016. JAMA Netw Open. 2018;1(4):e181471. doi: 10.1001/jamanetworkopen.2018.1471.. Published 2018 Aug 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoffmann Heinrich. The Story of Johnny Look-in-the-Air. Adam Matthew Digital. 2020 [Google Scholar]
- 25.Yeung A, Ng E, Abi-Jaoude E. TikTok and Attention-Deficit/Hyperactivity Disorder: A Cross-Sectional Study of Social Media Content Quality [published online ahead of print, 2022 Feb 23] Can J Psychiatry. 2022:7067437221082854. doi: 10.1177/07067437221082854.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bernfort L, Nordfeldt S, Persson J. ADHD from a socio-economic perspective. Acta Paediatr. 2008;97(2):239–245. doi: 10.1111/j.1651-2227.2007.00611.x.. [DOI] [PubMed] [Google Scholar]
- 27.Biederman J, Faraone SV, Spencer TJ, Mick E, Monuteaux MC, Aleardi M. Functional impairments in adults with self-reports of diagnosed ADHD: A controlled study of 1001 adults in the community. J Clin Psychiatry. 2006;67(4):524–540. doi: 10.4088/jcp.v67n0403.. [DOI] [PubMed] [Google Scholar]
- 28.Massuti R, Moreira-Maia CR, Campani F, et al. Assessing undertreatment and overtreatment/misuse of ADHD medications in children and adolescents across continents: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2021;128:64–73. doi: 10.1016/j.neubiorev.2021.06.001.. [DOI] [PubMed] [Google Scholar]
- 29.DuPaul GJ, Weyandt LL, O’Dell SM, Varejao M. College students with ADHD: current status and future directions. J Atten Disord. 2009;13(3):234–250. doi: 10.1177/1087054709340650.. [DOI] [PubMed] [Google Scholar]
- 30.Wilens TE, Woodward DW, Ko JD, Berger AF, Burke C, Yule AM. The Impact of Pharmacotherapy of Childhood-Onset Psychiatric Disorders on the Development of Substance Use Disorders. J Child Adolesc Psychopharmacol. 2022;32(4):200–214. doi: 10.1089/cap.2022.0016.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coker TR, Elliott MN, Toomey SL, et al. Racial and Ethnic Disparities in ADHD Diagnosis and Treatment. Pediatrics. 2016;138(3):e20160407. doi: 10.1542/peds.2016-0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fairman KA, Peckham AM, Sclar DA. Diagnosis and Treatment of ADHD in the United States: Update by Gender and Race. J Atten Disord. 2020;24(1):10–19. doi: 10.1177/1087054716688534.. [DOI] [PubMed] [Google Scholar]
- 33.Collins KP, Cleary SD. Racial and ethnic disparities in parent-reported diagnosis of ADHD: National Survey of Children’s Health (2003–2007 and 2011) J Clin Psychiatry. 2016;77(1):52–59. doi: 10.4088/JCP.14m09364.. [DOI] [PubMed] [Google Scholar]
- 34.Robison LM, Skaer TL, Sclar DA, Galin RS. Is attention deficit hyperactivity disorder increasing among girls in the US? Trends in diagnosis and the prescribing of stimulants. CNS Drugs. 2002;16(2):129–137. doi: 10.2165/00023210-200216020-00005.. [DOI] [PubMed] [Google Scholar]
- 35.Sclar DA, Robison LM, Bowen KA, Schmidt JM, Castillo LV, Oganov AM. Attention-deficit/hyperactivity disorder among children and adolescents in the United States: trend in diagnosis and use of pharmacotherapy by gender. Clin Pediatr (Phila) 2012;51(6):584–589. doi: 10.1177/0009922812439621.. [DOI] [PubMed] [Google Scholar]
- 36.Fadus MC, Ginsburg KR, Sobowale K, et al. Unconscious Bias and the Diagnosis of Disruptive Behavior Disorders and ADHD in African American and Hispanic Youth. Acad Psychiatry. 2020;44(1):95–102. doi: 10.1007/s40596-019-01127-6.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shi Y, Hunter Guevara LR, Dykhoff HJ, et al. Racial Disparities in Diagnosis of Attention-Deficit/Hyperactivity Disorder in a US National Birth Cohort. JAMA Netw Open. 2021;4(3):e210321. doi: 10.1001/jamanetworkopen.2021.0321.. Published 2021 Mar 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Isaksson J, Nilsson KW, Lindblad F. The Pressure-Activation-Stress scale in relation to ADHD and cortisol. Eur Child Adolesc Psychiatry. 2015;24(2):153–161. doi: 10.1007/s00787-014-0544-9.. [DOI] [PubMed] [Google Scholar]
- 39.Leslie LK, Plemmons D, Monn AR, Palinkas LA. Investigating ADHD treatment trajectories: listening to families’ stories about medication use. J Dev Behav Pediatr. 2007;28(3):179–188. doi: 10.1097/DBP.0b013e3180324d9a.. [DOI] [PubMed] [Google Scholar]