Abstract
Study Objectives:
Short sleep duration and evening chronotype are independently associated with negative health outcomes. However, it is unclear how adolescent sleep duration and chronotype are longitudinally associated with health outcomes during early adulthood.
Methods:
Participants from the NEXT Generation Health Study (n = 2,783; 54.5% female) completed measures of sleep duration (scheduled day and unscheduled day) and chronotype in high school. Sleep duration, chronotype, general health, depressive symptoms, and psychosomatic symptoms were also assessed 4 years after high school. Latent variables estimated high school scheduled-day sleep duration, unscheduled-day sleep duration, and chronotype using the during high school measures. Two path analyses tested the prospective associations between high school sleep duration (separate models for scheduled and unscheduled days) and chronotype with 4 years after high school health outcomes as mediated by concurrent sleep duration and chronotype.
Results:
In the scheduled-day model, longer high school sleep duration and later chronotype were associated with longer duration and later chronotype in early adulthood. Longer high school sleep duration was directly associated with fewer psychosomatic symptoms and indirectly associated with fewer depressive and psychosomatic symptoms through longer sleep duration in early adulthood. Later chronotype in high school was indirectly associated with poorer general health, greater depressive symptoms, and greater psychosomatic symptoms in early adulthood through later chronotype.
Conclusions:
Findings highlight the roles of scheduled-day sleep duration and evening chronotype in shaping health outcomes and suggest the importance of chronotype and optimal sleep habits among adolescents.
Citation:
Maultsby KD, Temmen CD, Lewin D, et al. Longitudinal associations between high school sleep characteristics and young adult health outcomes. J Clin Sleep Med. 2022;18(11):2527–2536.
Keywords: adolescence, sleep duration, sleep timing, chronotype, longitudinal mediation models
BRIEF SUMMARY
Current Knowledge/Study Rationale: Short sleep duration and evening chronotype both contribute to adverse physical and mental health outcomes, but research has yet to examine the independent longitudinal effects of sleep duration and chronotype at the transition from adolescence to adulthood. This study sought to examine longitudinal health outcomes associated with sleep duration and chronotype from adolescence to early adulthood using a nationally representative sample.
Study Impact: Findings highlight short scheduled-day sleep duration and evening chronotype in adolescence as contributing to increased depressive and psychosomatic symptoms and poorer general health in early adulthood. Furthermore, findings suggest that sleep timing and duration habits developed in adolescence persist into early adulthood, raising important questions about the types and timing of intervention to address high value modifiable health behaviors.
INTRODUCTION
The majority of adolescents experience deficiencies in sleep duration (< 8 h/night) and less optimal timing due to conflicts between their intrinsic evening chronotype, early school and work start times, and other social and environmental demands.1,2 At the onset of puberty, circadian clocks slow, resulting in a longer biological day and a drive to go to bed later and wake later.3 Thus, relative to young children and adults, adolescents typically do not go to bed earlier to accommodate early rise times necessitated by school or other morning commitments because of their biological circadian phase delay.4 While in general, early adulthood is a period of relatively good health,5 a notable proportion of this age group report experiences of depressive and psychosomatic symptoms.6,7 Data from the National Survey on Drug Use and Health (NSDUH) indicate that almost 10% of individuals aged 18–25 report 12-month prevalence of a major depressive episode.6 Young people also report mild but frequent psychosomatic symptoms, including headache and back ache.7 Using a prospective design, we examine how both deficient sleep duration and timing in adolescence contribute to early adult indicators of depressive symptoms, psychosomatic symptoms, and general health.
Much literature demonstrates the adverse health consequences of short sleep duration among adolescents. For example, a study of cross-sectional data from the Youth Risk Behavior Survey found that high school students who reported < 8 hours of sleep on school nights had higher odds of reporting substance use, risk behavior, poor dietary habits, and feelings of depression than students reporting sufficient school night sleep duration.8 Short sleep duration is also cross-sectionally associated with poorer self-rated health, increased odds of being overweight, frequent or severe headaches, and atopic conditions.9,10 Using a longitudinal design, Roberts and Duong11 found that sleep deprivation (≤ 6 h/night) predicted depressive symptoms 1 year later when accounting for baseline symptoms. Additionally, short sleep duration is associated with longitudinal risk of low self-esteem, low life satisfaction, and increased physical health risk among youth.12,13
Chronotype refers to an individual’s biologically preferred timing of sleep during the 24-hour day and is an important component of sleep health.3,4 Adolescence is marked by a shift to later chronotype, peaking around age 20.4 Later chronotype (ie, a preference for later bed and wake times) is cross-sectionally associated with increased mental health symptoms, poor emotion regulation, and adverse behavioral outcomes.14–16 Longitudinal studies evaluating consequences of poor sleep timing in adolescence largely focus on substance use.17,18 There is only 1 longitudinal study among youth that examines chronotype and mental health, which focuses on depressive symptoms, and it found that later chronotype predicts greater depressive symptoms.19 Similar findings have been found in longitudinal samples of adults.20,21
As evening chronotype and short sleep duration are both common among adolescents and have well-established associations with poorer health outcomes, studies have proposed a broader conceptualization of deficient sleep in adolescents that incorporates both duration and timing.16 Accordingly, various studies have examined these factors together,14,16,22 but research regarding the joint effects among high school students is mixed. Some studies suggest a more prominent contribution of chronotype on psychological health and other outcomes, including academic performance and self-regulation,14,16,22 although there is also evidence indicating independent roles of both sleep duration and chronotype.23 Notably, this work is cross-sectional,14,16,22,23 highlighting the importance of investigating these potential independent associations with a longitudinal study. Moreover, despite being health concerns among adolescents, independent contributions of chronotype and sleep duration on psychosomatic symptoms and self-rated health have not been explored.
Additionally, it remains unclear if longitudinal sequelae of short sleep duration and evening chronotype are due to the unique effects of poor sleep health during adolescence or because poor sleep health becomes habitual and persists throughout early adulthood. Research indicates that year-to-year sleep duration is stable among adolescents24 even in times of transition.25 Similar research has not been conducted examining stability of chronotype across adolescence and into early adulthood, although research suggests stability in chronotype among adults.20 Extant cross-sectional research indicates that the overall distribution of chronotype shifts later in adolescence and the distribution of individual chronotypes remains normal within each age group.4,20,26
Because adolescence is marked by change and growing independence from caregivers,27 it is a critical period for youth to develop healthful lifestyle habits, including adequate sleep duration and sleep/wake times. Sleep habits developed in adolescence can persist into adulthood and influence subsequent health behaviors, as is seen with dietary habits28 and substance use.29 To address the dearth of research on longer term stability of sleep and circadian characteristics and impacts on subsequent wellbeing, this study investigated potential pathways to longitudinal sleep-related and circadian-related health outcomes from high school through early adulthood.
We examined associations of high school sleep duration and high school chronotype with general health, depressive symptoms, and psychosomatic symptoms 4 years after high school. First, we hypothesized that adolescents with shorter sleep duration and later chronotype during high school would experience greater depressive symptoms, greater psychosomatic symptoms, and poorer physical health 4 years after high school. Additionally, we examined if young adult sleep duration and chronotype accounted for indirect pathways from high school sleep duration and chronotype to young adult health outcomes. We hypothesized that sleep duration and chronotype in early adulthood would mediate the relations between high school sleep duration and chronotype and health outcomes in early adulthood.
METHODS
All data came from the NEXT Generation Health Study, a 7-year cohort study of multiple health indicators and behaviors in a nationally representative sample of US adolescents. School districts were randomly selected from each of the 9 US census divisions, and schools were randomly selected within participating school districts; the probability of selection at each level was proportional to enrollment. Out of 137 schools selected, 81 (64%) agreed to participate and all students within 1 to 5 randomly selected 10th grade classrooms within schools were eligible for inclusion. Baseline data were collected during the 2009–2010 school year for all but 1 school; due to timing of school approval for participation, baseline assessments for that school (261 participants) occurred during the second wave (2010–2011, 11th grade). Parents provided informed consent; participant consent was obtained when they turned 18 years old. In total, 2,783 participants from 22 states were surveyed annually until early adulthood. In the first year (T1) participants completed surveys during in their classroom. From T2 onward, participants were contacted by email, provided a unique password to access their survey, which was completed online. Multiple outreach efforts were employed (eg, Facebook and text messages) to encourage participants to complete their surveys. The present study focused on 10th, 11th, and 12th grades (T1–T3) and the fourth year after high school (T7). The study protocol was approved by the institutional review board at the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Measures
Sleep variables (T1–T3, T7)
Sleep duration.
Participants reported what time they “usually wake up” and “usually go to sleep the night or day before” (hour, minute, AM/PM designation) on scheduled (ie, go to school, work, or have similar activities) and unscheduled (ie, do not have to get up at a certain time) days using items from the National Longitudinal Study of Adolescent Health.30 To address questionable AM vs PM designations, we followed the methodology utilized in analyzing sleep duration data in the NEXT study: wake time hours of 5–11 were designated as “AM” and wake times of 12, 1, and 2 were designated as “PM,” whereas sleep time hours of 8–11 were designated as “PM” and 12 and 1–4 were designated as “AM”.31 This resulted in changing AM/PM designations for 0.06–2.50% of wake times and 2.70–8.21% of sleep times at each wave. Sleep duration for scheduled and unscheduled days was the length of time between reported sleep and wake times.
Chronotype.
Chronotype was derived from self-reported free-day sleep period. The midpoint between the wake time and bedtime was corrected for oversleeping due to sleep debt to calculate chronotype for each participant [chronotype = free-day sleep midpoint − 0.5 * (scheduled-day sleep duration − weekly sleep duration)].4 Higher values indicate later chronotype or more eveningness (ie, worse sleep timing). This method of assessment yields a validated quantitative measure of sleep phase32 and derivation of chronotype for adolescents.4
Young adult mental health and wellbeing (T7)
General health.
Participants answered the single item question, “Would you say your health is…?” (1 = poor to 4 = excellent). A single-item global assessment of self-perception is a consistent predictor of mortality, independent of other more specific health indicators.33 This assessment method has been used previously with adolescent samples in the Health Behavior in School-Aged Children (HBSC) study34
Depressive symptoms.
Participants completed the 8-item Patient-Reported Outcomes Measurement Information System (PROMIS) pediatric depressive symptoms scale.35 Participants indicated how often each item (eg, I felt lonely) was true over the past 7 days from 1 (never) to 5 (almost always). Scores were converted to t-scores normed to distributions of scores in the national pediatric population (mean = 50, standard deviation = 10) with higher scores indicating higher depressive symptoms (α = .96).
Psychosomatic symptoms.
Participants indicated how often they experienced 8 symptoms: headache, stomach ache, back ache, feeling low, irritability or bad temper, feeling nervous, difficulties in getting to sleep, and feeling dizzy (1 = rarely/never to 5 = about every day) using a validated measure with prior use in the HBSC study.36 A mean score was calculated, with higher scores indicating more psychosomatic symptoms (α = .84).
Covariates (T1, T7)
T1 measures of depressive symptoms, general health, and psychosomatic symptoms were included as covariates to account for baseline health in adolescence. At T1, the NEXT Generation Health Study assessed depressive symptoms with the Modified Depression Scale.37 Participants reported how often they felt 6 symptoms (eg, grouchy or irritable or in a bad mood) in the past 30 days on a scale of 1 (never) to 5 (always). Since PROMIS scores were used to assess depressive at T7, scores were standardized (mean = 50, standard deviation = 10) to be consistent with the PROMIS scores, with higher scores indicating higher depressive symptoms.38 The T1 measures of general health and psychosomatic symptoms were the same as those used at T7.
Models also included T7 college status (not enrolled or enrolled in higher education), T7 employment status (not full-time employed, full-time employed), and baseline demographic variables, including sex, race/ethnicity (White, African American, Hispanic, other), and perceived family affluence (high, medium, and low) using the Family Affluence scale, which inquired about family car and computer ownership, child having their own bedroom, and holiday travel.39
Analysis plan
First, bivariate associations among scheduled-day and unscheduled-day sleep duration, chronotype, and health outcome variables in adolescence and early adulthood were investigated. Next, measurement models estimated separate latent structures for high school scheduled-day sleep duration, unscheduled-day sleep duration, and chronotype using the T1, T2, and T3 measures. Then 2 path models were estimated. The first model estimated the direct effects of high school scheduled-day sleep duration and chronotype on each T7 health outcome and the indirect effects of high school scheduled-day sleep duration and chronotype through T7 scheduled-day sleep duration and chronotype, respectively. The second model paralleled the first but replaced the scheduled-day sleep duration with unscheduled-day sleep duration. The residual variances between all outcome variables were correlated. Survey design variables, sex (referent = female), race/ethnicity (referent = White), family affluence (referent = high), employment status (referent = not full-time employed), and college enrollment (referent = not enrolled) were included as controls. In addition, measures of depressive symptoms, general health, and psychosomatic symptoms in adolescence were covaried in each path model to account for health symptoms at baseline. Descriptive statistics were conducted in SAS 9.4 (Cary, NC); the latent structures and path model were estimated in Mplus 8.40 The path model used bootstrapping resampling methods to estimate the bias-corrected confidence intervals of each indirect effect, which maximizes power and does not assume normal distributions in the data.41 To make use of all available data and account for missing data, all models were estimated using full information maximum likelihood. We used 3 goodness-of-fit indexes to determine model fit adequacy: comparative fit index (CFI), Tucker-Lewis index (TLI), and root mean square error of approximation (RMSEA). CFI and TLI > .95 and RMSEA ≤ .06 indicate acceptable fit.42
RESULTS
Sample characteristics are reported in Table 1, and descriptive statistics and correlations of model variables are reported in Table 2. Average scheduled-day sleep duration ranged from 7 hours, 20 minutes to 7 hours, 50 minutes; average unscheduled-day sleep duration ranged from 8 hours, 53 minutes to 9 hours, 17 minutes across time points. Average chronotype, or midsleep time, ranged from 4:27 AM (4.45) to 4:38 AM (4.63) across time points, where greater chronotype reflects more eveningness or later (ie, worse) sleep timing.
Table 1.
Sample characteristics (n = 2,783).
| n | Weighted % | ||
|---|---|---|---|
| Sex | Male | 1,254 | 45.49% |
| Female | 1,524 | 54.51% | |
| Race/Ethnicity | Latinx | 835 | 19.27% |
| African American | 687 | 20.19% | |
| White | 1,106 | 55.72% | |
| Other (eg, Asian, Hawaiian/Pacific Islander, and American Indian/Alaskan Native) | 142 | 4.82% | |
| Family Affluence | Low | 920 | 24.92% |
| Moderate | 1,285 | 48.53% | |
| High | 578 | 26.55% | |
| T7 Employment Status | Employed Full Time | 1,063 | 49.29% |
| Not Employed Full Time | 1,251 | 50.71% | |
| T7 College Enrollment Status | Enrolled in Higher Education | 990 | 38.13% |
| Not Enrolled in Higher Education | 1,326 | 61.87% |
Fluctuating n values are due to missing data on demographic variables.
Table 2.
Descriptive statistics and correlations of model variables.
| M | (SE) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scheduled-Day Sleep Duration | |||||||||||||||||||||
| 1. | T1 | 7.46 | (1.29) | — | |||||||||||||||||
| 2. | T2 | 7.44 | (1.40) | .42* | — | ||||||||||||||||
| 3. | T3 | 7.33 | (1.35) | .34* | 39* | — | |||||||||||||||
| 4. | T7 | 7.83 | (2.02) | .09* | .10* | .14* | — | ||||||||||||||
| Unscheduled-Day Sleep Duration | |||||||||||||||||||||
| 5. | T1 | 9.28 | (1.83) | .16* | .10* | .10* | .12* | — | |||||||||||||
| 6. | T2 | 9.29 | (1.92) | .12* | .23* | .10* | .12* | .35* | — | ||||||||||||
| 7. | T3 | 9.04 | (1.71) | .16* | .12* | .28* | .06* | .34* | .39* | — | |||||||||||
| 8. | T7 | 8.89 | (1.97) | .02 | .05 | .07* | .26* | .14* | .18* | .21* | — | ||||||||||
| Chronotype | |||||||||||||||||||||
| 9. | T1 | 4.47 | (1.39) | −.11* | −.10* | −.07* | −.03 | −.25* | −.06* | −.04 | .02 | — | |||||||||
| 10. | T2 | 4.45 | (1.40) | −.12* | −.06* | −.11* | −.02 | −.06* | −.23* | −.05 | .00 | .52* | — | ||||||||
| 11. | T3 | 4.47 | (1.37) | −.11* | −.11* | −.04 | −.06* | −.06* | −.10* | −.26* | −.03 | .47* | .49* | — | |||||||
| 12. | T7 | 4.63 | (1.67) | −.11* | −.10* | −.14* | .21* | .01 | .02 | −.01 | −.16* | .19* | .21* | .22* | — | ||||||
| General Health | |||||||||||||||||||||
| 13. | T1 | 2.17 | (.83) | −.06 | −.05 | −.02 | −.01 | −.02 | .01 | .01 | .01 | −.01 | .01 | −.01 | .04 | — | |||||
| 14. | T7 | 2.78 | (.76) | .05 | .04 | .09* | .02 | .02 | .02 | .03 | .01 | −.02 | −.02 | −.01 | −.12* | .29* | — | ||||
| Depressive Symptoms | |||||||||||||||||||||
| 15. | T1 | 51.12 | (9.97) | −.10* | −.07 | −.07 | .03 | .03 | −.01 | −.06 | −.01 | .07 | .04 | .04 | .07 | .31* | .20* | — | |||
| 16. | T7 | 49.76 | (11.96) | −.10* | −.04 | −.06* | −.04 | −.03 | .03 | −.02 | −.08* | .04 | .05 | .02 | .15* | .14* | −.32* | .30* | — | ||
| Psychosomatic Symptoms | |||||||||||||||||||||
| 17. | T1 | 2.22 | (.83) | −.07 | −.04 | −.05 | −.02 | .01 | −.01 | −.03 | −.06 | .06 | .05 | .05 | .01 | .25* | .14* | .63* | .27 | — | |
| 18. | T7 | 1.88 | (.79) | −.12* | −.05 | −.09* | −.02 | −.04 | −.01 | −.03 | −.04 | .08* | .08* | .05 | .08* | .19* | −.33* | .34* | .61* | .42* | — |
*P < .001. T1 = assessment during the 10th grade, T2 = assessment during 11th grade, T3 = assessment during 12th grade, T7 = assessment 4 years after the last year of high school.
The bivariate relations of high school sleep duration and chronotype with health outcomes in early adulthood indicated overall patterns in the longitudinal relations (see Table 2): (1) longer scheduled-day sleep duration in high school (T1–T3) was associated with better general health, fewer depressive symptoms, and fewer psychosomatic symptoms in early adulthood (T7); (2) unscheduled sleep duration in high school (T1–T3) was not associated with general health, depressive symptoms, or psychosomatic symptoms in early adulthood (T7); and (3) high school chronotype (T1–T3) was overall not related to general health or depressive symptoms, but a later high school chronotype was associated with more psychosomatic symptoms in early adulthood (T7). Additionally, longer scheduled-day sleep duration in high school (T1–T3) was associated with longer scheduled-day sleep duration in early adulthood (T7), longer unscheduled-day sleep duration in high school (T1–T3) was associated with longer unscheduled-day sleep duration in early adulthood (T7), and later high school chronotype (T1–T3) was associated with later young adult chronotype (T7). When examining the cross-sectional bivariate results of chronotype and scheduled and unscheduled sleep duration in early adulthood (T7) with health outcomes in early adulthood (T7; for correlation plots, see Figure S1 (373.1KB, pdf) , Figure S2 (373.1KB, pdf) , Figure S3 (373.1KB, pdf) in the supplemental material), longer scheduled-day and unscheduled-day sleep duration were each significantly associated with more depressive symptoms, and later chronotype was associated with poorer general health and more depressive and psychosomatic symptoms.
Three measurement models were estimated to create the latent structures for high school sleep duration and high school chronotype. Because all 3 models were just-identified (ie, models with no available degrees of freedom), the process provided no meaningful global fit statistics (Chi square, CFI, TLI, RMSEA). Instead, we examined the component fit of each latent structure to evaluate the standardized factor loadings of each observed measure. In the measurement models for high school sleep, the T1, T2, and T3 standardized factor loadings for the latent structures were .61, .68, and .45 for scheduled-day sleep duration; .60, .63, and .43 for unscheduled sleep duration; and .72, .76, and .65 for chronotype. Thus, all 3 time points for high school sleep duration and chronotype loaded adequately onto their respective latent structures.
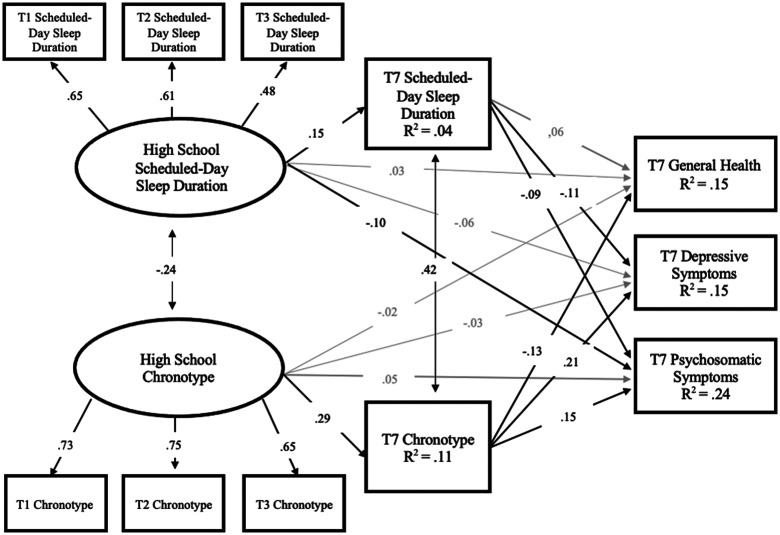
Results of the path model predicting health outcomes from high school scheduled-day sleep duration and high school chronotype while accounting for baseline health symptoms are found in Figure 1. The final model fit was adequate (CFI = 0.98; TLI = .95; RMSEA = 0.01). Longer high school scheduled-day sleep duration was associated with longer T7 sleep duration and with fewer T7 psychosomatic symptoms. Longer T7 scheduled-day duration was related to fewer depressive and psychosomatic symptoms. Indirect pathways were present for high school scheduled-day sleep duration through T7 sleep duration to depressive and psychosomatic symptoms (Table 3), such that longer high school duration was associated with fewer depressive symptoms and psychosomatic symptoms through longer T7 sleep duration. For high school chronotype, there was a positive association with T7 chronotype, such that later high school chronotype predicted later T7 chronotype, but no significant direct paths to the T7 health outcomes. Later T7 chronotype was associated with poorer T7 general health and increased T7 depressive and psychosomatic symptoms. All 3 indirect paths of high school chronotype through T7 chronotype to T7 health outcomes were significant (Table 3), such that later high school chronotype was associated with worse outcomes through later T7 chronotype. The model accounted for 15%, 15%, and 24% of the variance in T7 general health, depressive symptoms, and psychosomatic symptoms, respectively.
Figure 1. Path model predicting health outcomes from high school scheduled-day sleep duration and high school chronotype.
Standardized estimates are reported. Sex, race/ethnicity, family affluence, T1 general health, depressive symptoms, and psychosomatic symptoms and T7 college status and employment status are included as covariates. T1 = assessment during the 10th grade, T2 = assessment during 11th grade, T3 = assessment during 12th grade, T7 = assessment 4 years after the last year of high school.
Table 3.
Indirect effects from Figure 1.
| Predictors (latent variables) | Mediators | Health Outcomes | 95% CI | ||||
|---|---|---|---|---|---|---|---|
| Lower | β | Upper | |||||
| High School Scheduled-Day Sleep Duration | → | T7 Scheduled-Day Sleep Duration | → | General Health | .000 | .008 | .032 |
| High School Scheduled-Day Sleep Duration | → | T7 Scheduled-Day Sleep Duration | → | Psychosomatic Symptoms | −.039 | −.014 | −.005 |
| High School Scheduled-Day Sleep Duration | → | T7 Scheduled-Day Sleep Duration | → | Depressive Symptoms | −.046 | −.016 | −.003 |
| High School Chronotype | → | T7 Chronotype | → | General Health | −.078 | −.036 | −.009 |
| High School Chronotype | → | T7 Chronotype | → | Psychosomatic Symptoms | .019 | .043 | .076 |
| High School Chronotype | → | T7 Chronotype | → | Depressive Symptoms | .039 | .062 | .095 |
Bold values indicate a significant indirect effect. T1 = assessment during the 10th grade, T2 = assessment during 11th grade, T3 = assessment during 12th grade, T7 = assessment 4 years after the last year of high school.
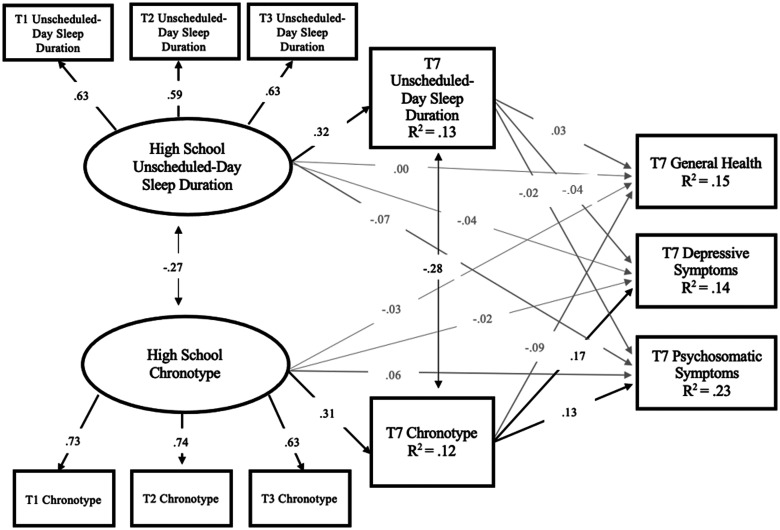
Results of the path model predicting health outcomes from high school unscheduled-day sleep duration and high school chronotype while accounting for baseline health symptoms are found in Figure 2. The final model fit was marginal (CFI = 0.88; TLI = .71; RMSEA = 0.035). Longer high school unscheduled-day sleep duration was related to longer T7 sleep duration. T7 sleep duration was not associated with T7 health outcomes, and there were no indirect effects present (Table 4). There was a positive association between later high school chronotype and later T7 chronotype, but there were no direct paths from high school chronotype to the T7 health outcomes. Later T7 chronotype was significantly associated with increased depressive symptoms and increased psychosomatic symptoms. Significant indirect pathways were found for high school chronotype through T7 chronotype to depressive and psychosomatic symptoms (Table 4), such that later high school chronotype was associated with greater depressive symptoms and psychosomatic symptoms through later T7 chronotype. The model accounted for 15%, 14%, and 23% of the variance in general health, depressive symptoms, and psychosomatic symptoms, respectively.
Figure 2. Path model predicting health outcomes from high school unscheduled-day sleep duration and high school chronotype.
Standardized estimates are reported. Sex, race/ethnicity, family affluence, T1 general health, depressive symptoms, and psychosomatic symptoms and T7 college status and employment status are included as covariates. T1 = assessment during the 10th grade, T2 = assessment during 11th grade, T3 = assessment during 12th grade, T7 = assessment 4 years after the last year of high school.
Table 4.
Indirect effects from Figure 2.
| Predictors (latent variables) | Mediators | Health Outcomes | 95% CI | ||||
|---|---|---|---|---|---|---|---|
| Lower | β | Upper | |||||
| High School Unscheduled-Day Sleep Duration | → | T7 Unscheduled-Day Sleep Duration | → | General Health | −.015 | .008 | .033 |
| High School Unscheduled-Day Sleep Duration | → | T7 Unscheduled-Day Sleep Duration | → | Psychosomatic Symptoms | −.033 | −.005 | .016 |
| High School Unscheduled-Day Sleep Duration | → | T7 Unscheduled-Day Sleep Duration | → | Depressive Symptoms | −.041 | −.013 | .005 |
| High School Chronotype | → | T7 Chronotype | → | General Health | −.067 | −.028 | .002 |
| High School Chronotype | → | T7 Chronotype | → | Psychosomatic Symptoms | .014 | .039 | .074 |
| High School Chronotype | → | T7 Chronotype | → | Depressive Symptoms | .032 | .053 | .081 |
Bold values indicate a significant indirect effect. T1 = assessment during the 10th grade, T2 = assessment during 11th grade, T3 = assessment during 12th grade, T7 = assessment 4 years after the last year of high school.
DISCUSSION
This study extended previous research by investigating longitudinal associations between high school scheduled-day and unscheduled-day sleep duration and chronotype with subsequent sleep duration, chronotype, and wellbeing outcomes 4 years after high school while accounting for baseline health outcomes in high school. Consistent with other adolescent samples,2 our sample reported insufficient average sleep duration on scheduled days (ie, when they go to school or work). However, on days in which they do not have to get up at a certain time (ie, unscheduled days), our sample reported adequate sleep duration. Scheduled-day sleep duration and chronotype uniquely contributed to measures of young adult health, highlighting the important roles of these behaviors in relation to physical and psychological health outcomes.
Findings build upon previous longitudinal research evidencing adverse health impacts of evening chronotype19 and short sleep duration11,13 in adolescence and indicate that both scheduled-day duration and chronotype demonstrate independent relations with general health, depressive symptoms, and psychosomatic symptoms 4 years after high school. Interestingly, findings build upon mixed cross-sectional literature about this definition of deficient sleep that incorporates both duration and timing14,16,23 by using longitudinal evidence to evaluate independent associations. The present longitudinal findings suggest that though a focus on sleep timing is important, sleep duration also remains a critical component of developing sleep health.
Findings also indicate that sleep duration and chronotype measured at the same time point are related to one another. In high school, shorter scheduled-day and unscheduled-day sleep duration were modestly associated with later chronotype. Prior research has attributed this to social/contextual factors in high school such as early school start times, increasingly demanding school curricula, and other demands.1,26 Four years after high school this relation changed, such that longer scheduled-day sleep duration was related to later chronotype, which may reflect the way young adults use the greater flexibility in their scheduled-day habits to match their preferred sleep period.
The longitudinal findings in this study corroborate those from previous studies indicating that sleep duration is generally stable.24–26 Further, these findings also build upon results from Druiven et al,20 which indicate longitudinal stability in chronotype among adults, and suggest that chronotype remains stable during the transition from adolescence to early adulthood. The significant indirect pathways from high school weekday sleep duration and chronotype to later health outcomes through concurrent sleep characteristics may reflect consistent sleep habits that persist across development and shape young adult health outcomes. Specifically, our findings that consistency in sleep duration and chronotype are associated with greater depressive symptoms, psychosomatic symptoms, and general health are supported by cross-sectional empirical evidence that concurrent sleep habits are associated with adverse health outcomes.8,15,22 However, our findings indicate that not all sleep characteristics follow this pattern; neither high school nor young adult unscheduled-day sleep duration was associated with health outcomes. Discrepancies in outcomes associated with scheduled-day and unscheduled-day duration may be due to differences in reported sleep duration. As is well-documented in the literature,1,2,8 high school students reported sleeping an insufficient duration on scheduled days. However, they reported sufficient duration (ie, 8 hours a night) on unscheduled days. Indeed, on unscheduled days, adolescents are not bound to early rise times due to school or other morning commitments and therefore may be better able to meet their sleep need. Notably, this pattern remained throughout young adulthood and highlights the clinical utility of examining scheduled-day and unscheduled-day sleep duration separately.
Prior research shows associations between deficient sleep and decrements in mood,14 emotion regulation,16 headache severity,9 and general health.10 Long-term deficits in scheduled-day sleep duration and chronotype may exacerbate such effects, which may contribute to greater depressive symptoms, psychosomatic symptoms, and poorer general health. The biological nature of chronotype may make it a difficult intervention target outside of clinical settings,4 but our independent findings suggest that a focus on improving sleep duration through sleep hygiene and consistency in sleep schedules43,44 may have the potential to mitigate adverse long-term outcomes, including emotional and physical health.
Adolescence is a sensitive period for the development of healthful behavioral habits. Importantly, prior research has identified adolescence as an important time to develop healthy eating behavior28 and substance use29 patterns, and this study provides similar evidence for sleep. Adolescents who report short scheduled-day sleep duration and evening chronotype are at heightened risk for worse longitudinal health outcomes in early adulthood, highlighting that cultivating adequate scheduled-day sleep schedules and maintaining optimal sleep timing in adolescence is foundational to long-term positive health development. An identified barrier to motivating adolescents to prioritize healthful lifestyles45 is a common perception that consequences from unhealthy lifestyles are too far in the future to impact their current behavior.46 This study provides evidence that there are long-term consequences rooted in adolescence (or earlier). This message should be incorporated into community educational efforts and policy considerations, such as setting of later school start times.
The present study utilized a large, nationally representative longitudinal sample of US students to examine sleep characteristics over multiple years, accounted for temporal precedence in sleep measures, and included important baseline control variables. However, there are notable limitations. All measures were self-reported, which are prone to social desirability and overestimation of sleep duration from conflating bed and sleep times.47 Sleep duration and timing were the only sleep variables included and were derived from single-item questions. We also measured general health with one item, without domain specific (ie mental, physical) assessments. More comprehensive assessments of mental and physical health could have provided a broader scope of health outcomes. Further, although this study accounts for health outcomes at baseline in the longitudinal relations of high school sleep and chronotype with young adult health outcomes, we cannot conclude a causal link in these relations from observational data due to the possibility of other unmeasured influences.
Future research should include additional sleep parameters, such as daytime sleepiness, sleep quality, insomnia symptoms,15,48,49 and more comprehensive measures of general health. The associations found here could be tested using actigraphic data, an objective measure of sleep, which may be a more reliable estimate than self-reports. Given present findings regarding the importance of adolescence as a period to develop healthful sleep habits, it is the authors’ opinions that future research could explore educational efforts or motivational interviewing as a mechanism to encourage youth, families, and policy makers to prioritize youth sleep. Other avenues of interest include longitudinal examinations of bedtime procrastination to disentangle biological vs behavioral reasons for delaying sleep timing50,51 and night time use of social networking sites and other digital media in association with both sleep parameters and psychological health.52 In addition, specific evaluation of the efficacy of sleep health interventions and investigation of durable changes in sleep and long-term physical and mental health outcomes may be justified investment given the findings of this study.
CONCLUSIONS
This study identified adolescence as a critical time to establish healthful sleep timing and duration habits given the association between late chronotype and scheduled sleep (resulting in sleep insufficiency) in high school and these sleep characteristics 4 years later, which, in turn, were associated with health outcomes. Moreover, sleep duration during high school was directly associated with psychosomatic symptoms 4 years later, when accounting for high school chronotype, baseline symptoms, and later sleep characteristics. The independent effects of duration and chronotype on health outcomes warrant more attention in longitudinal studies to best target intervention efforts.
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. This study was funded by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (contract HHSN275201200001I)t; the National Heart, Lung, and Blood Institute; the National Institute on Alcohol Abuse and Alcoholism; the National Institute on Drug Abuse; and the Maternal and Child Health Bureau of the Health Resources and Services Administration. The authors report no conflicts of interest.
ABBREVIATIONS
- CFI
comparative fit index
- HBSC
Health Behaviour in School-Aged Children
- PROMIS
Patient-Reported Outcomes Measurement Information
- RMSEA
root mean square error of approximation
- T1
assessment during the 10th grade
- T2
assessment during 11th grade
- T3
assessment during 12th grade
- T7
assessment four years after the last year of high school
- TLI
Tucker-Lewis index
REFERENCES
- 1. Carskadon MA . Sleep in adolescents: the perfect storm . Pediatr Clin North Am. 2011. ; 58 ( 3 ): 637 – 647 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Owens J , Adolescent Sleep Working GroupCommittee on Adolescence . Insufficient sleep in adolescents and young adults: an update on causes and consequences . Pediatrics. 2014. ; 134 ( 3 ): e921 – e932 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Crowley SJ , Acebo C , Carskadon MA . Sleep, circadian rhythms, and delayed phase in adolescence . Sleep Med. 2007. ; 8 ( 6 ): 602 – 612 . [DOI] [PubMed] [Google Scholar]
- 4. Roenneberg T , Kuehnle T , Pramstaller PP , et al . A marker for the end of adolescence . Curr Biol. 2004. ; 14 ( 24 ): R1038 – R1039 . [DOI] [PubMed] [Google Scholar]
- 5. Allen CD , McNeely CA , Orme JG . Self-rated health across race, ethnicity, and immigration status for US adolescents and young adults . J Adolesc Health. 2016. ; 58 ( 1 ): 47 – 56 . [DOI] [PubMed] [Google Scholar]
- 6. Mojtabai R , Olfson M , Han B . National trends in the prevalence and treatment of depression in adolescents and young adults . Pediatrics. 2016. ; 138 ( 6 ): e20161878 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kröner-Herwig B , Gorbunova A , Maas J . Predicting the occurrence of headache and back pain in young adults by biopsychological characteristics assessed at childhood or adolescence . Adolesc Health Med Ther. 2017. ; 8 : 31 – 39 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McKnight-Eily LR , Eaton DK , Lowry R , Croft JB , Presley-Cantrell L , Perry GS . Relationships between hours of sleep and health-risk behaviors in US adolescent students . Prev Med. 2011. ; 53 ( 4-5 ): 271 – 273 . [DOI] [PubMed] [Google Scholar]
- 9. Smaldone A , Honig JC , Byrne MW . Sleepless in America: inadequate sleep and relationships to health and well-being of our nation’s children . Pediatrics. 2007. ; 119 ( Suppl 1 ): S29 – S37 . [DOI] [PubMed] [Google Scholar]
- 10. Yeo SC , Jos AM , Erwin C , et al . Associations of sleep duration on school nights with self-rated health, overweight, and depression symptoms in adolescents: problems and possible solutions . Sleep Med. 2019. ; 60 : 96 – 108 . [DOI] [PubMed] [Google Scholar]
- 11. Roberts RE , Duong HT . The prospective association between sleep deprivation and depression among adolescents . Sleep. 2014. ; 37 ( 2 ): 239 – 244 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fatima Y , Doi SAR , Mamun AA . Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis . Obes Rev. 2015. ; 16 ( 2 ): 137 – 149 . [DOI] [PubMed] [Google Scholar]
- 13. Shochat T , Cohen-Zion M , Tzischinsky O . Functional consequences of inadequate sleep in adolescents: a systematic review . Sleep Med Rev. 2014. ; 18 ( 1 ): 75 – 87 . [DOI] [PubMed] [Google Scholar]
- 14. Antypa N , Vogelzangs N , Meesters Y , Schoevers R , Penninx BWJH . Chronotype associations with depression and anxiety disorders in a large cohort study . Depress Anxiety. 2016. ; 33 ( 1 ): 75 – 83 . [DOI] [PubMed] [Google Scholar]
- 15. Li SX , Chan NY , Man Yu MW , et al . Eveningness chronotype, insomnia symptoms, and emotional and behavioural problems in adolescents . Sleep Med. 2018. ; 47 : 93 – 99 . [DOI] [PubMed] [Google Scholar]
- 16. Owens JA , Dearth-Wesley T , Lewin D , Gioia G , Whitaker RC . Self-regulation and sleep duration, sleepiness, and chronotype in adolescents . Pediatrics. 2016. ; 138 ( 6 ): e20161406 . [DOI] [PubMed] [Google Scholar]
- 17. Hasler BP , Franzen PL , de Zambotti M , et al . Eveningness and later sleep timing are associated with greater risk for alcohol and marijuana use in adolescence: initial findings from the National Consortium on Alcohol and Neurodevelopment in Adolescence Study . Alcohol Clin Exp Res. 2017. ; 41 ( 6 ): 1154 – 1165 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nguyen-Louie TT , Brumback T , Worley MJ , et al . Effects of sleep on substance use in adolescents: a longitudinal perspective . Addict Biol. 2018. ; 23 ( 2 ): 750 – 760 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Haraden DA , Mullin BC , Hankin BL . The relationship between depression and chronotype: a longitudinal assessment during childhood and adolescence . Depress Anxiety. 2017. ; 34 ( 10 ): 967 – 976 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Druiven SJM , Hovenkamp-Hermelink JHM , Knapen SE , et al . Stability of chronotype over a 7-year follow-up period and its association with severity of depressive and anxiety symptoms . Depress Anxiety. 2020. ; 37 ( 5 ): 466 – 474 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Van den Berg JF , Kivelä L , Antypa N . Chronotype and depressive symptoms in students: an investigation of possible mechanisms . Chronobiol Int. 2018. ; 35 ( 9 ): 1248 – 1261 . [DOI] [PubMed] [Google Scholar]
- 22. Short MA , Gradisar M , Lack LC , Wright HR . The impact of sleep on adolescent depressed mood, alertness and academic performance . J Adolesc. 2013. ; 36 ( 6 ): 1025 – 1033 . [DOI] [PubMed] [Google Scholar]
- 23. Ojio Y , Kishi A , Sasaki T , Togo F . Association of depressive symptoms with habitual sleep duration and sleep timing in junior high school students . Chronobiol Int. 2020. ; 37 ( 6 ): 877 – 886 . [DOI] [PubMed] [Google Scholar]
- 24. Roberts RE , Roberts CR , Xing Y . Restricted sleep among adolescents: prevalence, incidence, persistence, and associated factors . Behav Sleep Med. 2011. ; 9 ( 1 ): 18 – 30 . [DOI] [PubMed] [Google Scholar]
- 25. Perlus JG , O’Brien F , Haynie DL , Simons-Morton BG . Adolescent sleep insufficiency one year after high school . J Adolesc. 2018. ; 68 ( 1 ): 165 – 170 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fischer D , Lombardi DA , Marucci-Wellman H , Roenneberg T . Chronotypes in the US - Influence of age and sex . PLoS One. 2017. ; 12 ( 6 ): e0178782 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steinberg L, Silk JS. Parenting adolescents. In: Bornstein MH ed. Handbook of parenting: Children and parenting. Mahwah: Lawrence Erlbaum Associates Publishers; 2002; 103–133.
- 28. Moreno LA , Gottrand F , Huybrechts I , Ruiz JR , González-Gross M , DeHenauw S ; HELENA Study Group . Nutrition and lifestyle in european adolescents: the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) study . Adv Nutr. 2014. ; 5 ( 5 ): 615S – 623S . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Schulte MT , Hser Y-I . Substance use and associated health conditions throughout the lifespan . Public Health Rev. 2013. ; 35 ( 2 ): 3 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Asarnow LD , McGlinchey E , Harvey AG . The effects of bedtime and sleep duration on academic and emotional outcomes in a nationally representative sample of adolescents . J Adolesc Health. 2014. ; 54 ( 3 ): 350 – 356 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Haynie DL , Lewin D , Luk JW , et al . Beyond sleep duration: bidirectional associations among chronotype, social jetlag, and drinking behaviors in a longitudinal sample of US high school students . Sleep. 2018. ; 41 ( 2 ): zsx202 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Roenneberg T , Wirz-Justice A , Merrow M . Life between clocks: daily temporal patterns of human chronotypes . J Biol Rhythms. 2003. ; 18 ( 1 ): 80 – 90 . [DOI] [PubMed] [Google Scholar]
- 33. Idler EL , Benyamini Y . Self-rated health and mortality: a review of twenty-seven community studies . J Health Soc Behav. 1997. ; 38 ( 1 ): 21 – 37 . [PubMed] [Google Scholar]
- 34. Marques A , Peralta M , Santos T , Martins J , Gaspar de Matos M . Self-rated health and health-related quality of life are related with adolescents’ healthy lifestyle . Public Health. 2019. ; 170 : 89 – 94 . [DOI] [PubMed] [Google Scholar]
- 35. Irwin DE , Stucky B , Langer MM , et al . An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales . Qual Life Res. 2010. ; 19 ( 4 ): 595 – 607 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Haugland S , Wold B . Subjective health complaints in adolescence–Reliability and validity of survey methods . J Adolesc. 2001. ; 24 ( 5 ): 611 – 624 . [DOI] [PubMed] [Google Scholar]
- 37. Dunn EC , Johnson RM , Green JG . The Modified Depression Scale (MDS): a brief, no-cost assessment tool to estimate the level of depressive symptoms in students and schools . School Ment Health. 2012. ; 4 ( 1 ): 34 – 45 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Goldstein RB , Lee AK , Haynie DL , et al . Neighbourhood disadvantage and depressive symptoms among adolescents followed into emerging adulthood . J Epidemiol Community Health. 2019. ; 73 ( 7 ): 590 – 597 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Currie CE , Elton RA , Todd J , Platt S . Indicators of socioeconomic status for adolescents: the WHO Health Behaviour in School-aged Children Survey . Health Educ Res. 1997. ; 12 ( 3 ): 385 – 397 . [DOI] [PubMed] [Google Scholar]
- 40. Muthen M . MPlus User’s Guide. 8th ed. Los Angeles, CA: : Muthén & Muthén; ; 2017. . [Google Scholar]
- 41. Shrout PE , Bolger N . Mediation in experimental and nonexperimental studies: new procedures and recommendations . Psychol Methods. 2002. ; 7 ( 4 ): 422 – 445 . [PubMed] [Google Scholar]
- 42. Hu L , Bentler PM . Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria vs new alternatives . Struct Equ Model Multidiscip J. 1999. ; 6 ( 1 ): 1 – 55 . [Google Scholar]
- 43. Micic G , Richardson C , Cain N , et al . Readiness to change and commitment as predictors of therapy compliance in adolescents with delayed sleep-wake phase disorder . Sleep Med. 2019. ; 55 : 48 – 55 . [DOI] [PubMed] [Google Scholar]
- 44. Richardson C , Micic G , Cain N , Bartel K , Maddock B , Gradisar M . Cognitive “insomnia” processes in delayed sleep-wake phase disorder: do they exist and are they responsive to chronobiological treatment? J Consult Clin Psychol. 2019. ; 87 ( 1 ): 16 – 32 . [DOI] [PubMed] [Google Scholar]
- 45. Blunden SL , Chapman J , Rigney GA . Are sleep education programs successful? The case for improved and consistent research efforts . Sleep Med Rev. 2012. ; 16 ( 4 ): 355 – 370 . [DOI] [PubMed] [Google Scholar]
- 46. Koehn S , Gillison F , Standage M , Bailey J . Life transitions and relevance of healthy living in late adolescence . J Health Psychol. 2016. ; 21 ( 6 ): 1085 – 1095 . [DOI] [PubMed] [Google Scholar]
- 47. Gradisar M , Gardner G , Dohnt H . Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep . Sleep Med. 2011. ; 12 ( 2 ): 110 – 118 . [DOI] [PubMed] [Google Scholar]
- 48. Bonvanie IJ , Oldehinkel AJ , Rosmalen JGM , Janssens KAM . Sleep problems and pain: a longitudinal cohort study in emerging adults . Pain. 2016. ; 157 ( 4 ): 957 – 963 . [DOI] [PubMed] [Google Scholar]
- 49. Schlarb AA , Claßen M , Hellmann SM , Vögele C , Gulewitsch MD . Sleep and somatic complaints in university students . J Pain Res. 2017. ; 10 : 1189 – 1199 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Chung SJ , An H , Suh S . What do people do before going to bed? A study of bedtime procrastination using time use surveys . Sleep. 2020. ; 43 ( 4 ): zsz267 . [DOI] [PubMed] [Google Scholar]
- 51. Nauts S , Kamphorst BA , Stut W , De Ridder DTD , Anderson JH . The explanations people give for going to bed late: a qualitative study of the varieties of bedtime procrastination . Behav Sleep Med. 2019. ; 17 ( 6 ): 753 – 762 . [DOI] [PubMed] [Google Scholar]
- 52. Twenge JM , Martin GN , Campbell WK . Decreases in psychological well-being among American adolescents after 2012 and links to screen time during the rise of smartphone technology . Emotion. 2018. ; 18 ( 6 ): 765 – 780 . [DOI] [PubMed] [Google Scholar]