Abstract
Waning immunity following mRNA vaccination and the emergence of SARS-CoV-2 variants has led to reduced mRNA vaccine efficacy against both symptomatic infection and severe disease. Bivalent mRNA boosters expressing the Omicron BA.5 and ancestral WA1/2020 Spike proteins have been developed and approved, because BA.5 is currently the dominant SARS-CoV-2 variant and substantially evades neutralizing antibodies (NAbs). Our data show that BA.5 NAb titers were comparable following monovalent and bivalent mRNA boosters.
Waning immunity following mRNA vaccination and the emergence of SARS-CoV-2 variants has led to reduced mRNA vaccine efficacy against both symptomatic infection and severe disease1,2. Bivalent mRNA boosters expressing the Omicron BA.5 and ancestral WA1/2020 Spike proteins have been developed and approved, because BA.5 is currently the dominant SARS-CoV-2 variant and substantially evades neutralizing antibodies (NAbs)3. However, the immunogenicity of the BA.5-containing bivalent mRNA boosters remains unknown.
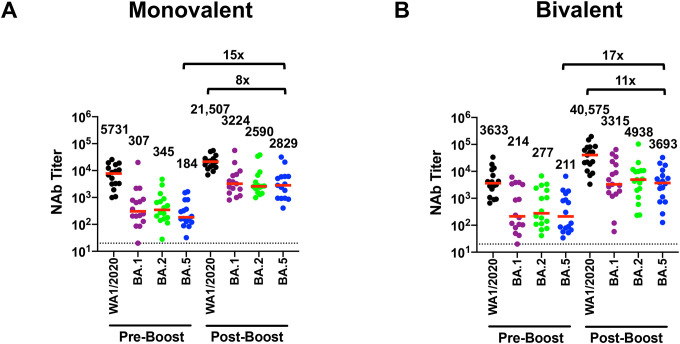
We evaluated humoral and cellular immune responses in 15 individuals who received the original monovalent mRNA boosters and in 18 individuals who received the bivalent mRNA boosters (Table S1). Participants had a median of 3 (range 2–4) prior COVID-19 vaccine doses, and 33% had documented SARS-CoV-2 infection during the Omicron surge, although it is likely that the majority of participants had hybrid immunity prior to boosting given the high prevalence and limited severity of Omicron infection. Both the monovalent and bivalent mRNA boosters led to preferential expansion of WA1/2020 NAb titers and lower BA.1, BA.2, and BA.5 NAb titers (Fig. 1A, B). Median BA.5 NAb titers increased from 184 to 2,829 following monovalent mRNA boosting and from 211 to 3,693 following bivalent mRNA boosting. The Pfizer and Moderna bivalent mRNA boosters induced similar NAb profiles (Fig. S1). Binding antibody responses by ELISA and electrochemiluminescence assays were comparable following monovalent and bivalent mRNA boosting (Fig. S2, S3).
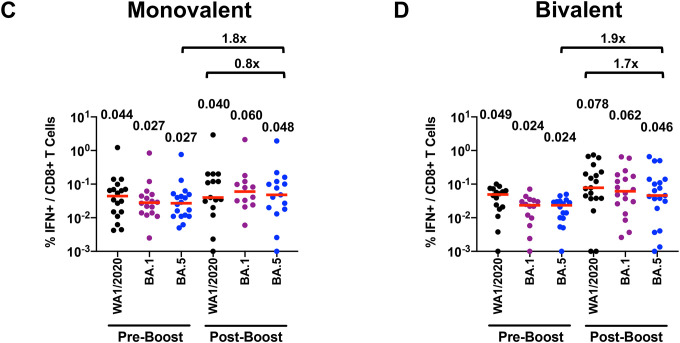
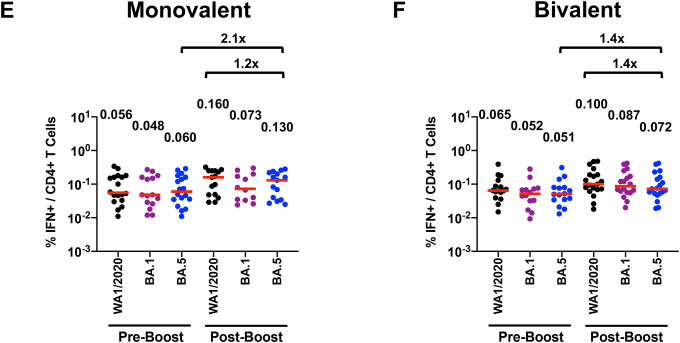
Figure 1. Neutralizing antibody and T cell responses following monovalent and bivalent mRNA boosting.
A, B. Neutralizing antibody (NAb) titers by luciferase-based pseudovirus neutralization assays in individuals following monovalent or bivalent mRNA boosting. C, D. Spike-specific CD8+ T cell responses by intracellular cytokine staining assays in individuals following monovalent or bivalent mRNA boosting. E, F. Spike-specific CD4+ T cell responses by intracellular cytokine staining assays in individuals following monovalent or bivalent mRNA boosting. Responses were measured against the SARS-CoV-2 WA1/2020, Omicron BA.1, BA.2, and BA.5 variants. Medians (red bars) are depicted and shown numerically with fold differences.
Spike-specific CD8+ and CD4+ T cell responses increased only modestly following monovalent and bivalent mRNA boosting. Median BA.5 CD8+ T cell responses increased from 0.027% to 0.048% following monovalent mRNA boosting and from 0.024% to 0.046% following bivalent mRNA boosting (Fig. 1C, 1D). Median BA.5 CD4+ T cell responses increased from 0.060% to 0.130% following monovalent mRNA boosting and from 0.051% to 0.072% following bivalent mRNA boosting (Fig. 1E, 1F). Median BA.5 memory B cell responses were 0.079% following monovalent mRNA boosting and 0.091% following bivalent mRNA boosting (Fig. S4).
Our data demonstrate that both monovalent and bivalent mRNA boosters markedly increased antibody responses but did not substantially augment T cell responses. BA.5 NAb titers were comparable following monovalent and bivalent mRNA boosters, with a modest and nonsignificant trend favoring the bivalent booster by a factor of 1.3. These findings are consistent with data recently reported for a BA.1-containing bivalent mRNA booster4. Our findings suggest that immune imprinting by prior antigenic exposure5 may pose a greater challenge than currently appreciated for inducing robust immunity to SARS-CoV-2 variants.
Supplementary Material
Funding
The authors acknowledge NIH grant CA260476, the Massachusetts Consortium for Pathogen Readiness, the Ragon Institute, and the Musk Foundation (D.H.B.), as well as NIH grant AI69309 (A.Y.C.).
Role of Sponsor
The sponsor did not have any role in design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Conflicts of Interest
The authors report no conflicts of interest.
Data sharing
A.Y.C. and D.H.B. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All data are available in the manuscript or the supplementary material. Correspondence and requests for materials should be addressed to D.H.B. (dbarouch@bidmc.harvard.edu).
References
- 1.Lin DY, Gu Y, Xu Y, et al. Association of Primary and Booster Vaccination and Prior Infection With SARS-CoV-2 Infection and Severe COVID-19 Outcomes. JAMA 2022;328:1415–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collie S, Nayager J, Bamford L, Bekker LG, Zylstra M, Gray G. Effectiveness and Durability of the BNT162b2 Vaccine against Omicron Sublineages in South Africa. N Engl J Med 2022;387:1332–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hachmann NP, Miller J, Collier AY, et al. Neutralization Escape by SARS-CoV-2 Omicron Subvariants BA.2.12.1, BA.4, and BA.5. N Engl J Med 2022;387:86–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chalkias S, Harper C, Vrbicky K, et al. A Bivalent Omicron-Containing Booster Vaccine against Covid-19. N Engl J Med 2022;387:1279–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reynolds CJ, Pade C, Gibbons JM, et al. Immune boosting by B.1.1.529 (Omicron) depends on previous SARS-CoV-2 exposure. Science 2022;377:eabq1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
A.Y.C. and D.H.B. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All data are available in the manuscript or the supplementary material. Correspondence and requests for materials should be addressed to D.H.B. (dbarouch@bidmc.harvard.edu).