Abstract
Alcoholic liver disease is one of the most common chronic liver diseases in the world. It is a liver disease caused by prolonged heavy drinking and its main clinical features are nausea, vomiting, enlargement of the liver, and jaundice. Recent studies suggest that Kupffer cell-mediated inflammatory response is a core driver in the development of alcoholic steatohepatitis and alcoholic liver fibrosis. As a danger signal, extracellular ATP activates the assembly of NLPR3 inflammasome by acting on purine P2X7 receptor, the activated NLRP3 inflammasome prompts ASC to cleave pro-cCaspase-1 into active caspase-1in KCs. Active caspase-1 promotes the conversion of pro-IL-1β to IL-1β, which further enhances the inflammatory response. Here, we briefly review the role of the P2X7R-NLRP3 inflammasome axis in the pathogenesis of alcoholic liver disease and the evolution of alcoholic steatohepatitis and alcoholic liver fibrosis. Regulation of the inflammasome axis of P2X7R-NLRP3 may be a new approach for the treatment of alcoholic liver disease.
Keywords: ATP, P2X7 receptor, Kupffer cells, NLRP3 inflammasome, Alcoholic steatohepatitis, Alcoholic liver fibrosis
Introduction
Alcoholic liver disease (ALD) is one of the most common chronic liver diseases in the world.1 It is caused by prolonged heavy drinking and its main clinical features are nausea, vomiting, enlargement of the liver, and jaundice.2 About 2 billion people around the world drink alcohol and ALD affects more than 75 million people worldwide, with its incidence and fatality rate increasing year by year.3 Statistics show that ALD accounts for 48% of cirrhosis-related deaths in the USA.4,5 ALD presents hepatic steatosis in the early stage of the disease, which will develop into alcoholic steatohepatitis (ASH) and alcoholic liver fibrosis if not controlled, and can even lead to cirrhosis in severe cases. In the course of the disease, this can also be accompanied by serious complications, such as gastrointestinal bleeding and liver failure.1,6 There are many factors affecting the development of ALD, and the risk factors studied at home and abroad mainly include alcohol consumption, drinking years, sex, race, obesity, genetic factors, nutritional status, and hepatitis virus infection.7–9 In addition, studies have found that there are considerable individual differences in risk factors of ALD, and different individuals have different sensitivity to the various risk factors.10,11 At present, the mainstream view is that ALD is mainly the result of the interaction of many factors, such as oxidative stress, enterogenic endotoxin, inflammatory mediators and nutritional imbalance (especially protein-caloric malnutrition), which is directly or indirectly induced by the metabolic process of ethanol and its derivatives.12–14 Activated Kupffer cells (KCs) play an important role in the development and progression of ALD and are considered to be important conditions leading to ASH and alcoholic fibrosis, but the cascade of events that regulate these processes has not been fully identified.15
The purpose of this work was to review how P2X7R activates KCs and exacerbates the transition from ASH to alcoholic liver fibrosis. ATP and alcohol as mediators of extracellular inflammation and the role of the NLRP3 inflammasome are also reviewed.
Activated extracellular inflammatory mediators of P2X7R
Liver is the main organ for ethanol metabolism. After ethanol is ingested orally, most of it is simply diffused and absorbed into the blood through the gastrointestinal tract, and more than 90% of ethanol in the blood depends on the metabolism of hepatocytes.16 Ethanol entering the liver is converted to acetaldehyde and then to acetate by alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH). The conversion of acetaldehyde to acetate results in the conversion of coenzyme I (NAD) to reduced coenzyme I (NADH), thus increasing the content of NADH in hepatocytes. On the one hand, increased NADH inhibits the mitochondrial tricarboxylic acid cycle, thus reducing the oxidation capacity of liver cells for fatty acids and causing fat accumulation in the liver. On the other hand, increased NADH leads to the increase of reoxidation of NADH and increased oxygen consumption of mitochondria, resulting in hypoxic stress response of hepatocytes.17,18 Excessive NADH and acetaldehyde can lead to excessive production of mitochondrial reactive oxygen (ROS), which can cause oxidative stress, endoplasmic reticulum (ER) stress, and steatosis.19 In addition, acetaldehyde exerts a strong biochemical reaction and toxicity, which leads to glutathione depletion and makes hepatocytes more sensitive to oxidative stress; it can also affect the character of the liver cell membrane and inhibit the protein secretion and synthesis of liver cells.20,21 The cytotoxic effects of ethanol metabolism and ROS lead to hepatocyte death. With the death of hepatocytes, the integrity of their membrane is destroyed; rupture of the cytoplasmic membrane ultimately leads to cell lysis, death of intracellular organelles, and release of enzymes into the cytoplasmic fluid. Damage-related molecular pattern (DAMP) molecules are also released after cell death (mainly necrosis) and trigger macrophage and neutrophil activation, fibrosis, and liver regeneration.22 Common DAMPs contain high mobility group protein B1 (HGMB1), formyl-peptide, DNA, ATP, and so on.22
Adenine nucleoside triphosphate is an unstable, high-energy phosphoric acid compound, which is composed of one molecule of adenine, one molecule of ribose and three molecules of phosphoric acid groups. It is also known as adenosine triphosphate, abbreviated as ATP. General knowledge of ATP has expanded considerably since its discovery in 1929, and it is well known as a substrate for muscle contraction. ATP is widely regarded as an energy exchange factor linking anabolism and catabolism, and is also involved in active transport, motor contraction, phosphorylation, etc.23 In recent years, it has been found that ATP not only plays an important role in cellular energy metabolism but also plays an important role in the physiological and pathological process of chronic liver diseases, including ALD, acting as a “danger signal”.24–26 It activates intracellular signaling cascades by acting on p2 purine receptors on the cell surface.24,27 Current studies have found that the body will release high levels of intracellular nucleotides (such as ATP) into the extracellular environment when receiving such external stimuli as ethanol, which itself acts as a danger signal to prompt the body to initiate its own immune defense. Studies have found that in the process of ALD, in addition to releasing cytokines/inflammatory factors, a large amount of ATP will be released, as an endogenous danger signal to activate the inflammatory complex through p2 purine receptors and further magnify the inflammatory response.28 The inflammation, which occurs in the absence of external pathogens in response to various stimuli of tissue stress and injury, is known as sterile inflammation (SI). In SI, endogenous DAMPs, normally hidden outside the extracellular environment, are released when tissue is damaged and activate receptors on immune cells. ATP is a DAMP, and the extracellular ATP (eATP)-induced inflammatory response is SI. This SI is a key process in drug-induced liver injury, non-ASH, and ASH, and is a major determinant of fibrosis and cancer.29
Purine receptors are divided into P1 and P2 receptors. P2X7 purine receptor (P2X7R) belongs to the P2X family of P2 purine receptors and is an ATP-gated, non-selective cation channel receptor. P2X7R exists in a variety of cell types, including exocrine cells, stem cells, glial cells, nerve cells, endothelial cells, and KCs. P2X7R is also expressed by almost all innate and adaptive immune cells. P2X7R induces a variety of intracellular cascade reactions in a cell-specific manner, including inflammatory molecule release, phagocytosis, cell proliferation, and cell death.30,31 Current studies have found that P2X7R plays an important role in the physiological and pathological processes of a variety of chronic liver diseases, and ATP activated P2X7R induces intracellular cascade reactions. Studies have found that eATP intensifies inflammation by activating P2X7R and increasing cytokine release, and aggravates liver damage caused by sepsis.32 Hoque et al.33 showed that ATP-activated P2X7R aggravated the liver injury induced by acetaminophen hepatotoxicity, while acetaminophen-induced liver necrosis was significantly reduced in P2X7−/− mice. Toki et al.34 showed that eATP induces activation of the P2X7 receptor on KCs, resulting in the release of interleukin-1β (IL-1β), HMGB1 and prostaglandin E2 (PGE2), and is involved in various inflammatory responses in the liver.
As a transmembrane hydrolytic enzyme, ecto-nucleoside triphosphate diphosphohydrolase (CD39/ENTPD1) plays an important role in many pathophysiological processes. When ATP is released extracellularly by stressed or damaged cells, it is rapidly hydrolyzed to adenosine monophosphate (AMP) and phosphoric acid by CD39 expressed on the cell surface, releasing energy, after which it is further hydrolyzed to adenosine by extracellular 5′-nucleotide enzyme (CD73/NT5E).35 It has been found that ATP can enhance the phagocytosis of macrophages through P2X7R-induced intercellular Ca2+ signal transduction, while CD39 expression can effectively inhibit this process.36 Sun et al.37 found that, in CD39 knockout mice, genetic deletion of CD39 aggravates the systemic inflammatory response and liver damage. Furthermore, Savio et al.32 found that CD39 can limit the inflammatory signal transduction of P2X7R by hydrolyzing eATP and reduce liver injury caused by sepsis. CD39 also mitigated P2X7R-mediated inflammatory response by hydrolyzing ATP.
It is also worth noting that, in recent years, it has been found that ethanol can directly or indirectly activate P2X7R with its metabolite acetaldehyde. For example, long-term exposure to ethanol has been found to induce activation of the NLRP3 inflammasome by upregulating P2X7R expression in human macrophages.38 Wu et al.39 found that P2X7R mediates acetaldehyde-induced hepatic stellate cell (HSC) activation via a PKC-dependent GSK3β pathway. Similarly, Liana et al.40 found that ethanol can enhance p2X7R-mediated IL-1β secretion in BV2 microglia cells. In patients with alcoholic liver, P2X7R may be early responsive to ethanol and metabolite stimulation, rather than completely secondary to alcohol and metabolite-induced liver injury.
The purine P2X4 receptor (P2X4R) is another subtype belonging to the P2X family. There seems to be some potential interaction between P2X4R and P2X7R. It has been reported that the heterotrimeric P2X4/P2X7 receptor can be formed by P2X4R and P2X7R.41 It has also been reported that the synergistic action of P2X4R and P2X7 plays an important role in Ca2+ signaling.36,42 Interestingly, studies have found that P2X4R and P2X7R have different sensitivities to ethanol and ATP. High concentration of ethanol was found to inhibit P2X4R but to not affect the activity of P2X7R.40 P2X4R is one of the most sensitive purinergic receptors and its sensitivity to ATP is much higher than that of P2X7R.43 The synergistic effect of P2X4R and P2X7R is worthy of further investigation.
Activated NLRP3 inflammasome
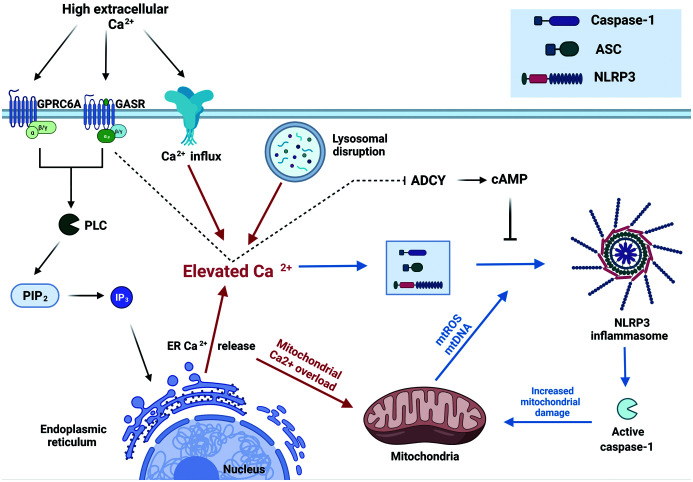
NLRP3 is a NOD-like receptor thermal protein domain associated protein 3, which is an important member of the NOD-like receptor family. The NLRP3 inflammasome is composed of NLRP3, apoptosis-associated speck-like protein containing a CARD (ASC) and pro-cysteinyl aspartate specific proteinase-1 (pro-caspase-1).44,45 Studies have found that the activation mechanism of NLRP3 involves multiple aspects, including extracellular Ca2+ influx, K+ efflux, Ca2+ release from the ER, Ca2+ uptake by mitochondria, and mitochondrial dysfunction.46–48 There is considerable evidence that intracellular Ca2+ signal transduction plays an important role in NLRP3 inflammasome activation. Studies have shown that the cholesterol-dependent cytolysin-induced activation of NLRP3 inflammasome in mouse macrophages requires Ca2+ influx.49 Ca2+ signal transduction can trigger mitochondrial instability and production of the mitochondrial associated ligand (mtROS, mtDNA) that activates NLRP3 inflammasome.47,50,51 Unstable mitochondria also affect the Ca2+ uptake and lead to cardiolipin externalization, which also plays an important role in NLRP3 inflammasome activation.52 Studies have shown that the use of Ca2+ channel inhibitors can effectively inhibit NLRP3 inflammasome activation, which also indicates that Ca2+ influx plays an important role in NLRP3 inflammasome activation.53,54 In addition, it has been suggested that Ca2+ activated Ca2+-sensing receptor (CASR) and the GPCR family C group 6 member A (GPRC6A) lead to the activation of phospholipase C (PLC), which then hydrolyzes phosphatidylinositol diphosphate (PIP2) into inositol triphosphate (IP3) and diacylglycerol (DG); IP3 activates the IP3 ligand gate Ca2+ channel in the ER, resulting in the release of Ca2+ from the ER.55,56 See Figure 1 for details. K+ efflux also plays an important role in NLRP3 activation.57 It has been found that K+ flux may affect Ca2+ flux and seems to respond to mitochondrial destruction and cell volume regulation, which provide conditions for the activation of NLRP3 inflammasome as well as the study of Groß etc.46,58–60
Fig. 1. Regulation of NLRP3 activation by Ca2+ signaling.
High extracellular Ca2+ concentration activates CASR and the GPRC6A. The activation of GASR and GPRC6A leads to the activation of PLC, which hydrolyzes PIP2 into IP3 and DG, and IP3 activates the IP3 ligand gate Ca2+ channel in the ER, resulting in the release of Ca2+ from the ER. Activated CASR also inhibits adenylate cyclase (ADCY), thereby alleviating the inhibition of cAMP on the NLRP3 inflammasome assembly. Ca2+ released by the ER, Ca2+ flowing through the P2X7R channel, and Ca2+ released by unstable lysosomes, all provide important conditions for the high concentration of Ca2+ in the intracellular environment. In addition, high intracellular Ca2+ concentration (especially Ca2+ released from the ER) leads to mitochondrial Ca2+ uptake overload, and mitochondrial damage leads to increased mtROS and mtDNA release, which are required for NLRP3 inflammasome activation. In addition, the activated NLRP3 inflammasome activates caspase-1, which further enhances mitochondrial damage. Created with BioRender.com
In addition, ATP-mediated P2X7R has received increasing attention in recent years due to its activation of the NLRP3 inflammasome, which is involved in the pathophysiological regulation of various diseases, including liver disease. It has been found that ATP-induced P2X7R mediates NLRP3 inflammasome-dependent IL-1β secretion in neutrophils.61 It has also been reported that NLRP3 inflammasome activated by P2X7R in hippocampal glial cells mediates chronic stress-induced depressive-like behaviors.62 The study of Jiang et al.63 showed that the activation degree of eATP for HSCs depends on activation of the NLRP3 inflammasome mediated by P2X7R, and proposed that blocking the axis of the P2X7R-NLRP3 inflammasome is a potential target for the treatment of hepatic fibrosis. ATP-activated P2X7R provides a critical channel basis for K+ efflux and Ca2+ influx and is an important condition for NLRP3 inflammasome activation.
Studies have shown elevated levels of NLRP3, IL-1β and caspase-1 in the livers of ALD patients,64 and significantly elevated levels of IL-1β in the serum of patients with severe ASH.65 Similarly, the expression of NLRP3 and IL-1β was significantly increased in the liver of alcohol-fed mice.66 Activation of the p2X7R-NLRP3 inflammasome has been reported to influence alcoholic steatosis by modulating AMPK-dependent adipogenesis.67 ALD inchoate disease exhibits the main characteristic of liver adipose denaturation. Excess free fatty acids (FFAs) are esterified into triglyceride (TG), which is present in hepatocytes as lipid droplets. When the amount of FFAs exceeds the storage capacity of lipid droplets, FFAs produce lipid toxicity to hepatocytes and cause oxidative stress and ER stress.1,68 The stress response further causes lipid metabolism disorder of hepatocytes. FFAs also activate transcription factors such as nuclear factor kappa-B (NF-κB), which supports secretion of pro-inflammatory factors and chemokines, activate liver-resident macrophages such as KCs, and recruits circulating monocytes/macrophages into the liver to enhance liver inflammation.68 What is more, the activated NLRP3 inflammasome prompts ASC to cleave pro-caspase-1 into active caspase-1in KCs. Active caspase-1 promotes the conversion of pro-IL-1β to IL-1β, which further enhances the inflammatory response.44,69 This is the main intracellular mechanism by which the NLRP3 inflammasome is known to promote the development of ASH.70 In addition, few studies have investigated the intracellular mechanisms involved in NLRP3 inflammasome activation in ALD. Further studies suggest that inhibition of NLRP3 inflammasome activation can effectively inhibit the further deterioration of ASH and alleviate alcohol-induced liver damage. For example, Zhou et al.71 found that cyanidin-3-O-β-glucoside inactivates the NLRP3 inflammasome and alleviates ASH via the SirT1/NF-κB signaling pathway. Liu et al.72 found that magnolol prevents acute alcoholic liver damage by activating PI3K/Nrf2/PPARγ and inhibiting the NLRP3 signaling pathway.
KCs, HSCs, ASH and alcoholic liver fibrosis
ASH (ASH) is one of the important types of ALD, and is characterized by jaundice and signs of liver failure.1,73 Alcoholic liver fibrosis is a pathophysiological process, involving excessive deposition of diffuse extracellular matrix (ECM) (especially collagen) in the liver during chronic liver injury caused by alcohol.74,75 The alcohol-induced inflammatory immune response plays a central role in the development of ALD. It disrupts the balance of pro- and anti-inflammatory functions in the liver, causing it to remain chronically inflamed.76 There is evidence that alcohol-induced inflammatory immune responses play an important role in the development of ASH and alcoholic fibrosis.77
KCs are liver-resident macrophages that recognize, ingest, and degrade cell debris, foreign bodies, and pathogens.78 KCs are also highly secretory, with the ability to secrete a variety of active mediators to regulate homeostasis and participate in inflammatory responses and various immune responses.79,80 There are two main sources: one is KCs inherent in the liver, and the other is KCs formed after hematopoietic stem cells from bone marrow differentiate into monocytes and migrate to the liver.15,81 Studies have shown that liver injury caused by ethanol metabolism in ALD can be sensed and triggered by KCs, which then release pro-inflammatory cytokines and inflammatory chemokines, and recruit free monocytes into blood vessels to converge to the liver and reside as KCs.19,81 KCs are usually the first response to immunogenicity cells derived from alcohol-induced gut microbes (especially the microbe’s lipopolysaccharide [LPS]).82 KCs express toll-like receptors that trigger pro-inflammatory pathways in response to LPS, and also express P2X7R that activates KCs and triggers pro-inflammatory pathways when stimulated by eATP.32,34 The mainstream view is that KCs release inflammatory cytokines and chemokines extracellularly, mainly through the NF-κB pathway.68 However, it has been found in recent years that the NLRP3 inflammasome plays an important role in the KC-mediated inflammatory response, and KCs can also release pro-inflammatory cytokines into the extracellular space by activating the NLRP3 inflammasome.66,83 A study found that blocking the NLRP3 inflammasome in KCs reduced liver inflammation in mice.84 Another study showed that, in NLRP3 knockout mice, the KC-mediated inflammatory response can be effectively suppressed.85 Interestingly, ROS and cytokines released by KCs during inflammation can further exacerbate liver damage, leading to a vicious cycle.68,86 In addition, it has been reported that activated KCs can produce a variety of chemokines and cytokines that directly affect the activation of HSCs, including TGF-β, tumor necrosis factor-alpha (TNF-α), IL-1β, monocyte chemoattractant protein (MCP1) and platelet-derived growth factor (PDGF). For example, the Pradere et al.87 study demonstrated that KCs can enhance the survival rate of HSCs in a NF-κB-dependent manner, thus promoting liver fibrosis. The Purohit et al.88 study also showed that KCs can promote the activation of HSCs by releasing ROS and TGF-β, and this is an indispensable part of the mechanism of alcohol-induced liver fibrosis. In conclusion, the KC-mediated inflammatory response plays an important role in the development of ASH and alcoholic liver fibrosis.
HSCs are a kind of nonparenchymal cells, characterized by the storage of retinol in lipid droplets in the cytoplasm.89 In normal liver, HSCs appear as non-proliferating resting cells, but after liver injury, HSCs can be transformed into myofibroblasts, which can proliferate, contract, and secrete large amounts of ECM.90,91 The process of HSC transdifferentiation from retinol-storage cells to myofibroblasts is called the activation of HSC.92 TGF-β is considered to be the most effective fibrosis cytokine, which plays a key role in activating HSCs and liver ECM deposition, including inducing the synthesis and release of ECM components and inhibiting ECM degradation.92,93 In activated HSCs, TGF-β can promote the transcription of type I collagen and III collagen by activating the SMAD pathway.94 TGF-β also participates in TGF-β-induced gene expression to promote HSC activation by activating the mitogen-activated protein kinase (TAK1) signaling pathway.95 ROS produced by KCs can also act as inducers or effectors of the TGF-β signaling pathway, thereby promoting the activation of HSCs and exacerbating the process of liver fibrosis.96 ROS can induce TGF-β signaling through various mechanisms, including activation of matrix metalloproteinases, induction of TGF-β expression, and increase of TGF-β release through activation of the latency-associated protein (LAP). At the same time, TGF-β can increase the production of ROS and inhibit antioxidant enzymes, thereby leading to redox imbalance.96,97 Activated HSCs can also secrete vascular endothelial growth factor (VEGF) and TGF-β, thus promoting the activation and proliferation of HSC itself.91,98 In addition, damaged hepatocytes also produce ROS, nucleotides, lipid peroxides, and cytokines (VEGF, insulin-like growth factor 1 [IGF1]) to promote HSC activation.77,93
Purinergic signaling pathway as a therapeutic target in ASH and alcoholic liver fibrosis
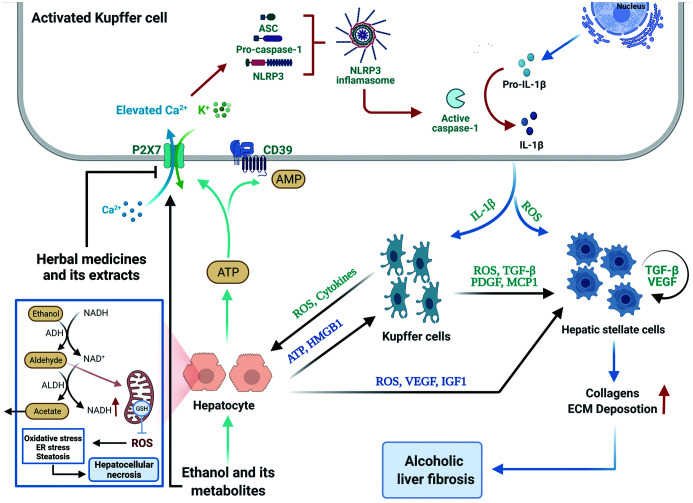
Due to the important role of the purinergic signaling pathway in the inflammatory development of ASH and alcoholic liver fibrosis, interference of the purinergic signaling pathway may be a new therapeutic strategy for ALD. This purine signaling pathway includes ATP, CD39, P2X7R and the NLRP3 inflammasome downstream of P2X7R, all of which are involved in the activation, maintenance, and amplification of inflammatory signals, and are core drivers in the development of alcoholic steatosis and alcoholic liver fibrosis. As shown in Figure 2, the toxic effects of ethanol, oxidative metabolites of ethanol and lipid metabolism disorders on hepatocyte cells cause the extracellular release of ATP, which activates P2X7R on KCs, thus opening cationic channels and mediating K+ efflux and Ca2+ influx.25,34,36 K+ efflux and Ca2+ influx in the intracellular environment activate NLRP3 inflammasome assembly, further activating caspase-1 and mediating IL-1β production and release.44,58 Therefore, targeted therapy of the purinergic pathway may be an effective means to eliminate the inflammatory response induced by liver injury. More and more attention has been paid to the purine signaling pathway in ALDs, especially after the P2X7R-NLRP3 signaling pathway was found to be involved in ALD.
Fig. 2. Schematic diagram of the P2X7 receptor/NLRP3 inflammasome axis involved in the pathogenesis of ALD and evolution into ASH and alcoholic liver fibrosis.
Ethanol, oxidative metabolites of ethanol and lipid metabolism disorders can cause excessive production of mtROS, resulting in oxidative stress, ER stress, and steatosis of liver cells; acetaldehyde depletes the glutathione in the mitochondria, making hepatocytes more sensitive to oxidative stress, and ultimately leads to hepatocellular necrosis. The necrotic hepatocytes can release ATP, which activates P2X7R on KCs, thus opening cationic channels and mediating K+ efflux and Ca2+ influx. K+ efflux and Ca2+ influx in the intracellular environment activate the NLRP3 inflammasome assembly, further activating caspase-1 and mediating IL-1β production and release. Il-1β secreted by activated KCs activates resting KCs, further amplifying the alcohol-induced inflammatory response. The ROS and cytokines secreted by it can further aggravate the damage to hepatocytes, and the secreted ROS, TGF-β and PDGF can promote the activation and proliferation of HSCs. In addition, necrotic hepatocytes release HMPB1, which promotes the inflammatory response of macrophages. Necrotic hepatocytes also secrete ROS, VEGF and IGF1 to promote the active proliferation of HSCs. Activated HSCs (myofibroblasts) secrete excessive collagen and ECM, leading to alcoholic liver fibrosis. Created with BioRender.com
In recent years, this hypothesis has been further supported by evidentiary research findings. For example, it has been suggested that eATP-enhanced HSC activation via the P2X7R-mediated NLRP3 pathway enhanced HSC collagen expression and promoted ECM deposition.63 It has also been found that P2X7R is increased in an acetaldehyde-induced HSC activation model and promotes acetaldehyde induction through the pkC-GSK3β pathway-induced HSC activation.39 Dihydroquercetin has been shown to ameliorate alcoholic steatosis by signaling the P2X7R-NLRP3 inflammasome activation pathway.67 Su et al.99 found that P2X7R blocker could reduce ASH and liver injury in alcohol-fed mice, and further studies showed that P2X7R blocker inhibited meK1/2-ERK1/2 phosphorylation and EGR-1 expression in the liver and intestine tissue of alcohol-fed mice. Current studies on the mechanism of inhibiting P2X7R to reduce alcoholic steatosis and alcohol-induced liver injury mostly focus on inhibiting Ca2+ influx and K+ outflow by inhibiting P2X7R, so as to avoid a series of signal cascade reactions caused by intracellular Ca2+ and K+ disturbance.99,100 One of the most representative is the activation of the NLRP3 inflammasome due to intracellular Ca2+ and K+ disturbance, which leads to a series of inflammatory responses.101 Few studies have explored the intracellular mechanism of P2X7R activation in ALD, and this aspect needs to be further studied.
At present, it has been reported that P2X7R inhibitors are useful to relieve ASH and alcoholic liver injury; moreover, P2X7R inhibitors can effectively relieve the alcohol-induced inflammatory response and liver injury in mice and zebrafish.99,100 Recent studies suggest that the P2X7R-NLRP3 inflammasome axis may be an effective target for the treatment of ASH and alcoholic liver fibrosis. Drug development based on blocking the P2X7R-NLRP3 inflammasome axis may be a practical and effective research direction. It should be noted that there are many subtypes of the P2X family, and the drugs currently used to study P2X7 blockade are not highly specific; however, chemically synthesized P2X7R-specific blockers are highly toxic. Moreover, P2X7R plays an important role in a variety of inflammatory and immune responses, and systemic application of P2X7R blockade may bring about a series of systemic chain reactions.30,102 Therefore, drugs that are highly selective for P2X7R and have liver targeting may be an important direction of future research, and how to achieve safe and effective application is also a problem to be solved. Most importantly, although P2X7R blockade has achieved good results in alleviating ASH and alcohol-induced liver injury at present, most of the current studies are limited to animal samples, and there is no clinical study data on human samples. Whether P2X7R blockers are effective in humans and the possible adverse clinical symptoms are not clear, and further studies in humans need to confirm the observation results from cells and animals.
In addition, in recent years, the international research on herbal medicine and its extracts has attracted extensive attention. Several herbal medicine and their extracts have been shown to protect against alcohol-induced liver damage. For example, quercetin alleviates chronic ethanol-induced liver mitochondrial damage by enhancing mitochondrial phagocytosis.103 Xiao et al.104 found that Lycium barbarum polysaccharide reduces alcohol-induced liver injury through the TXNIP-NLRP3 inflammasome pathway. Yang et al.105 found that betaine attenuates chronic alcohol-induced fatty liver by broadly regulating hepatic lipid metabolism. It has been suggested that leucodin (a sesquiterpene lactone from Artemisia capillaris) can inhibit inflammatory responses in macrophages and lipid accumulation in liver cells through p2X7R-NLRP3 inflammasome activation.101 Herbal medicines and their extracts seem to have a unique advantage in protecting against alcohol-induced liver damage. For the protection of liver injury caused by alcohol, the study of herbal medicine and its extracts may be an effective direction, but it still needs further research and development.
Conclusions
The incidence and mortality of ALD worldwide are increasing year by year, but the treatment of patients with ALD is still challenging and controversial.3,106 Due to the complex pathogenesis of ALD, there is still no effective prevention and treatment in addition to alcohol withdrawal and nutritional treatment, so there remains an urgent need to develop new targeted treatment methods for ALD.64,107,108 This review briefly discussed the involvement of the inflammatory body axis of P2X7R-NLRP3 in the pathogenesis of ALD and the evolution to ASH and alcoholic liver fibrosis. The P2X7R-NLRP3 inflammasome axis may still be an effective therapeutic target, although the cascade of events that regulate the p2X7R-NLRP3 inflammasome axis has not been fully identified and further studies are needed to understand it. These recent advances in our understanding of the P2X7R-NLRP3 axis may bring new target foci for modulating KC activation to help alleviate inflammatory responses and ALD.
Abbreviations
- ADCY
adenylate cyclase inhibitor
- ADH
alcohol dehydrogenase
- ALD
Alcoholic liver disease
- ALDH
aldehyde dehydrogenase
- AMP
adenosine monophosphate
- ASH
alcoholic steatohepatitis
- CD39
ecto-nucleoside triphosphate diphosphohydrolase
- DAMP
Damage-related molecular pattern
- eATP
extracellular ATP
- ECM
extracellular matrix
- ER
endoplasmic reticulum
- HSC
hepatic stellate cell
- IL-1β
interleukin-1β
- KCs
Kupffer cells
- MCP1
monocyte chemoattractant protein 1
- PDGF
platelet-derived growth factor
- PEG2
prostaglandin E2
- P2X4R
purine P2X4 receptor
- P2X7R
P2X7 purine receptor
- ROS
reactive oxygen
- VEGF
vascular endothelial growth factor
References
- 1.Seitz HK, Bataller R, Cortez-Pinto H, Gao B, Gual A, Lackner C, et al. Alcoholic liver disease. Nat Rev Dis Primers. 2018;4(1):16. doi: 10.1038/s41572-018-0014-7. [DOI] [PubMed] [Google Scholar]
- 2.Singal AK, Bataller R, Ahn J, Kamath PS, Shah VH. ACG Clinical Guideline: Alcoholic Liver Disease. Am J Gastroenterol. 2018;113(2):175–194. doi: 10.1038/ajg.2017.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70(1):151–171. doi: 10.1016/j.jhep.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 4.Shirazi F, Singal AK, Wong RJ. Alcohol-associated Cirrhosis and Alcoholic Hepatitis Hospitalization Trends in the United States. J Clin Gastroenterol. 2021;55(2):174–179. doi: 10.1097/mcg.0000000000001378. [DOI] [PubMed] [Google Scholar]
- 5.Moon AM, Singal AG, Tapper EB. Contemporary Epidemiology of Chronic Liver Disease and Cirrhosis. Clin Gastroenterol Hepatol. 2020;18(12):2650–2666. doi: 10.1016/j.cgh.2019.07.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stickel F, Datz C, Hampe J, Bataller R. Pathophysiology and Management of Alcoholic Liver Disease: Update 2016. Gut Liver. 2017;11(2):173–188. doi: 10.5009/gnl16477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gramenzi A, Caputo F, Biselli M, Kuria F, Loggi E, Andreone P, et al. Review article: alcoholic liver disease—pathophysiological aspects and risk factors. Aliment Pharmacol Ther. 2006;24(8):1151–1161. doi: 10.1111/j.1365-2036.2006.03110.x. [DOI] [PubMed] [Google Scholar]
- 8.Rocco A, Compare D, Angrisani D, Sanduzzi Zamparelli M, Nardone G. Alcoholic disease: liver and beyond. World J Gastroenterol. 2014;20(40):14652–14659. doi: 10.3748/wjg.v20.i40.14652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu BB, Li YL, Wang BY. Research advances in risk factors for alcoholic liver disease. Zhonghua Gan Zang Bing Za Zhi. 2017;25(5):397–400. doi: 10.3760/cma.j.issn.1007-3418.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 10.Choudhary NS, Duseja A. Genetic and epigenetic disease modifiers: non-alcoholic fatty liver disease (NAFLD) and alcoholic liver disease (ALD) Transl Gastroenterol Hepatol. 2021;6:2. doi: 10.21037/tgh.2019.09.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Llopis M, Cassard AM, Wrzosek L, Boschat L, Bruneau A, Ferrere G, et al. Intestinal microbiota contributes to individual susceptibility to alcoholic liver disease. Gut. 2016;65(5):830–839. doi: 10.1136/gutjnl-2015-310585. [DOI] [PubMed] [Google Scholar]
- 12.Gao B, Bataller R. Alcoholic liver disease: pathogenesis and new therapeutic targets. Gastroenterology. 2011;141(5):1572–1585. doi: 10.1053/j.gastro.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunn W, Shah VH. Pathogenesis of Alcoholic Liver Disease. Clin Liver Dis. 2016;20(3):445–456. doi: 10.1016/j.cld.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kourkoumpetis T, Sood G. Pathogenesis of Alcoholic Liver Disease: An Update. Clin Liver Dis. 2019;23(1):71–80. doi: 10.1016/j.cld.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Dixon LJ, Barnes M, Tang H, Pritchard MT, Nagy LE. Kupffer cells in the liver. Compr Physiol. 2013;3(2):785–797. doi: 10.1002/cphy.c120026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Norberg A, Jones AW, Hahn RG, Gabrielsson JL. Role of variability in explaining ethanol pharmacokinetics: research and forensic applications. Clin Pharmacokinet. 2003;42(1):1–31. doi: 10.2165/00003088-200342010-00001. [DOI] [PubMed] [Google Scholar]
- 17.Chakrabarty RP, Chandel NS. Mitochondria as Signaling Organelles Control Mammalian Stem Cell Fate. Cell Stem Cell. 2021;28(3):394–408. doi: 10.1016/j.stem.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Navas LE, Carnero A. NAD(+) metabolism, stemness, the immune response, and cancer. Signal Transduct Target Ther. 2021;6(1):2. doi: 10.1038/s41392-020-00354-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Louvet A, Mathurin P. Alcoholic liver disease: mechanisms of injury and targeted treatment. Nat Rev Gastroenterol Hepatol. 2015;12(4):231–242. doi: 10.1038/nrgastro.2015.35. [DOI] [PubMed] [Google Scholar]
- 20.Tuma DJ. Role of malondialdehyde-acetaldehyde adducts in liver injury. Free Radic Biol Med. 2002;32(4):303–308. doi: 10.1016/s0891-5849(01)00742-0. [DOI] [PubMed] [Google Scholar]
- 21.Jokelainen K, Parkkila S, Salaspuro M, Niemelä O. Covalent adducts of proteins with acetaldehyde in the liver as a result of acetaldehyde administration in drinking water. J Hepatol. 2000;33(6):926–932. doi: 10.1016/s0168-8278(00)80124-5. [DOI] [PubMed] [Google Scholar]
- 22.Luedde T, Kaplowitz N, Schwabe RF. Cell death and cell death responses in liver disease: mechanisms and clinical relevance. Gastroenterology. 2014;147(4):765–783.e764. doi: 10.1053/j.gastro.2014.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bonora M, Patergnani S, Rimessi A, De Marchi E, Suski JM, Bononi A, et al. ATP synthesis and storage. Purinergic Signal. 2012;8(3):343–357. doi: 10.1007/s11302-012-9305-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vaughn BP, Robson SC, Burnstock G. Pathological roles of purinergic signaling in the liver. J Hepatol. 2012;57(4):916–920. doi: 10.1016/j.jhep.2012.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Petrasek J, Iracheta-Vellve A, Saha B, Satishchandran A, Kodys K, Fitzgerald KA, et al. Metabolic danger signals, uric acid and ATP, mediate inflammatory cross-talk between hepatocytes and immune cells in alcoholic liver disease. J Leukoc Biol. 2015;98(2):249–256. doi: 10.1189/jlb.3AB1214-590R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang S, Gao S, Zhou D, Qian X, Luan J, Lv X. The role of the CD39-CD73-adenosine pathway in liver disease. J Cell Physiol. 2021;236(2):851–862. doi: 10.1002/jcp.29932. [DOI] [PubMed] [Google Scholar]
- 27.Ayata CK, Ganal SC, Hockenjos B, Willim K, Vieira RP, Grimm M, et al. Purinergic P2Y2 receptors promote neutrophil infiltration and hepatocyte death in mice with acute liver injury. Gastroenterology. 2012;143(6):1620–1629.e1624. doi: 10.1053/j.gastro.2012.08.049. [DOI] [PubMed] [Google Scholar]
- 28.Iracheta-Vellve A, Petrasek J, Satishchandran A, Gyongyosi B, Saha B, Kodys K, et al. Inhibition of sterile danger signals, uric acid and ATP, prevents inflammasome activation and protects from alcoholic steatohepatitis in mice. J Hepatol. 2015;63(5):1147–1155. doi: 10.1016/j.jhep.2015.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kubes P, Mehal WZ. Sterile inflammation in the liver. Gastroenterology. 2012;143(5):1158–1172. doi: 10.1053/j.gastro.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 30.Di Virgilio F, Dal Ben D, Sarti AC, Giuliani AL, Falzoni S. The P2X7 Receptor in Infection and Inflammation. Immunity. 2017;47(1):15–31. doi: 10.1016/j.immuni.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 31.Sluyter R. The P2X7 Receptor. Adv Exp Med Biol. 2017;1051:17–53. doi: 10.1007/5584_2017_59. [DOI] [PubMed] [Google Scholar]
- 32.Savio LEB, de Andrade Mello P, Figliuolo VR, de Avelar Almeida TF, Santana PT, Oliveira SDS, et al. CD39 limits P2X7 receptor inflammatory signaling and attenuates sepsis-induced liver injury. J Hepatol. 2017;67(4):716–726. doi: 10.1016/j.jhep.2017.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoque R, Sohail MA, Salhanick S, Malik AF, Ghani A, Robson SC, et al. P2X7 receptor-mediated purinergic signaling promotes liver injury in acetaminophen hepatotoxicity in mice. Am J Physiol Gastrointest Liver Physiol. 2012;302(10):G1171–1179. doi: 10.1152/ajpgi.00352.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Toki Y, Takenouchi T, Harada H, Tanuma S, Kitani H, Kojima S, et al. Extracellular ATP induces P2X7 receptor activation in mouse Kupffer cells, leading to release of IL-1β, HMGB1, and PGE2, decreased MHC class I expression and necrotic cell death. Biochem Biophys Res Commun. 2015;458(4):771–776. doi: 10.1016/j.bbrc.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 35.Linden J, Koch-Nolte F, Dahl G. Purine Release, Metabolism, and Signaling in the Inflammatory Response. Annu Rev Immunol. 2019;37:325–347. doi: 10.1146/annurev-immunol-051116-052406. [DOI] [PubMed] [Google Scholar]
- 36.Zumerle S, Calì B, Munari F, Angioni R, Di Virgilio F, Molon B, et al. Intercellular Calcium Signaling Induced by ATP Potentiates Macrophage Phagocytosis. Cell Rep. 2019;27(1):1–10.e14. doi: 10.1016/j.celrep.2019.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sun X, Imai M, Nowak-Machen M, Guckelberger O, Enjyoji K, Wu Y, et al. Liver damage and systemic inflammatory responses are exacerbated by the genetic deletion of CD39 in total hepatic ischemia. Purinergic Signal. 2011;7(4):427–434. doi: 10.1007/s11302-011-9239-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Le Daré B, Victoni T, Bodin A, Vlach M, Vene E, Loyer P, et al. Ethanol upregulates the P2X7 purinergic receptor in human macrophages. Fundam Clin Pharmacol. 2019;33(1):63–74. doi: 10.1111/fcp.12433. [DOI] [PubMed] [Google Scholar]
- 39.Wu X, Wang Y, Wang S, Xu R, Lv X. Purinergic P2X7 receptor mediates acetaldehyde-induced hepatic stellate cells activation via PKC-dependent GSK3β pathway. Int Immunopharmacol. 2017;43:164–171. doi: 10.1016/j.intimp.2016.12.017. [DOI] [PubMed] [Google Scholar]
- 40.Asatryan L, Ostrovskaya O, Lieu D, Davies DL. Ethanol differentially modulates P2X4 and P2X7 receptor activity and function in BV2 microglial cells. Neuropharmacology. 2018;128:11–21. doi: 10.1016/j.neuropharm.2017.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schneider M, Prudic K, Pippel A, Klapperstück M, Braam U, Müller CE, et al. Interaction of Purinergic P2X4 and P2X7 Receptor Subunits. Front Pharmacol. 2017;8:860. doi: 10.3389/fphar.2017.00860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brock VJ, Wolf IMA, Er-Lukowiak M, Lory N, Stähler T, Woelk LM, et al. P2X4 and P2X7 are essential players in basal T cell activity and Ca(2+) signaling milliseconds after T cell activation. Sci Adv. 2022;8(5):eabl9770. doi: 10.1126/sciadv.abl9770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Suurväli J, Boudinot P, Kanellopoulos J, Rüütel Boudinot S. P2X4: A fast and sensitive purinergic receptor. Biomed J. 2017;40(5):245–256. doi: 10.1016/j.bj.2017.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.He Y, Hara H, Núñez G. Mechanism and Regulation of NLRP3 Inflammasome Activation. Trends Biochem Sci. 2016;41(12):1012–1021. doi: 10.1016/j.tibs.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mangan MSJ, Olhava EJ, Roush WR, Seidel HM, Glick GD, Latz E. Targeting the NLRP3 inflammasome in inflammatory diseases. Nat Rev Drug Discov. 2018;17(8):588–606. doi: 10.1038/nrd.2018.97. [DOI] [PubMed] [Google Scholar]
- 46.Elliott EI, Sutterwala FS. Initiation and perpetuation of NLRP3 inflammasome activation and assembly. Immunol Rev. 2015;265(1):35–52. doi: 10.1111/imr.12286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Murakami T, Ockinger J, Yu J, Byles V, McColl A, Hofer AM, et al. Critical role for calcium mobilization in activation of the NLRP3 inflammasome. Proc Natl Acad Sci U S A. 2012;109(28):11282–11287. doi: 10.1073/pnas.1117765109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rizzuto R, De Stefani D, Raffaello A, Mammucari C. Mitochondria as sensors and regulators of calcium signalling. Nat Rev Mol Cell Biol. 2012;13(9):566–578. doi: 10.1038/nrm3412. [DOI] [PubMed] [Google Scholar]
- 49.Chu J, Thomas LM, Watkins SC, Franchi L, Núñez G, Salter RD. Cholesterol-dependent cytolysins induce rapid release of mature IL-1beta from murine macrophages in a NLRP3 inflammasome and cathepsin B-dependent manner. J Leukoc Biol. 2009;86(5):1227–1238. doi: 10.1189/jlb.0309164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Horng T. Calcium signaling and mitochondrial destabilization in the triggering of the NLRP3 inflammasome. Trends Immunol. 2014;35(6):253–261. doi: 10.1016/j.it.2014.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shimada K, Crother TR, Karlin J, Dagvadorj J, Chiba N, Chen S, et al. Oxidized mitochondrial DNA activates the NLRP3 inflammasome during apoptosis. Immunity. 2012;36(3):401–414. doi: 10.1016/j.immuni.2012.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu Q, Zhang D, Hu D, Zhou X, Zhou Y. The role of mitochondria in NLRP3 inflammasome activation. Mol Immunol. 2018;103:115–124. doi: 10.1016/j.molimm.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 53.Chang YY, Jean WH, Lu CW, Shieh JS, Chen ML, Lin TY. Nicardipine Inhibits Priming of the NLRP3 Inflammasome via Suppressing LPS-Induced TLR4 Expression. Inflammation. 2020;43(4):1375–1386. doi: 10.1007/s10753-020-01215-y. [DOI] [PubMed] [Google Scholar]
- 54.Fan Y, Xue G, Chen Q, Lu Y, Dong R, Yuan H. CY-09 Inhibits NLRP3 Inflammasome Activation to Relieve Pain via TRPA1. Comput Math Methods Med. 2021;2021:9806690. doi: 10.1155/2021/9806690. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 55.Lee GS, Subramanian N, Kim AI, Aksentijevich I, Goldbach-Mansky R, Sacks DB, et al. The calcium-sensing receptor regulates the NLRP3 inflammasome through Ca2+ and cAMP. Nature. 2012;492(7427):123–127. doi: 10.1038/nature11588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rossol M, Pierer M, Raulien N, Quandt D, Meusch U, Rothe K, et al. Extracellular Ca2+ is a danger signal activating the NLRP3 inflammasome through G protein-coupled calcium sensing receptors. Nat Commun. 2012;3:1329. doi: 10.1038/ncomms2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Le Daré B, Ferron PJ, Gicquel T. The Purinergic P2X7 Receptor-NLRP3 Inflammasome Pathway: A New Target in Alcoholic Liver Disease? Int J Mol Sci. 2021;22(4):2139. doi: 10.3390/ijms22042139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Groß CJ, Mishra R, Schneider KS, Médard G, Wettmarshausen J, Dittlein DC, et al. K(+) Efflux-Independent NLRP3 Inflammasome Activation by Small Molecules Targeting Mitochondria. Immunity. 2016;45(4):761–773. doi: 10.1016/j.immuni.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 59.Muñoz-Planillo R, Kuffa P, Martínez-Colón G, Smith BL, Rajendiran TM, Núñez G. K+ efflux is the common trigger of NLRP3 inflammasome activation by bacterial toxins and particulate matter. Immunity. 2013;38(6):1142–1153. doi: 10.1016/j.immuni.2013.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Di A, Xiong S, Ye Z, Malireddi RKS, Kometani S, Zhong M, et al. The TWIK2 Potassium Efflux Channel in Macrophages Mediates NLRP3 Inflammasome-Induced Inflammation. Immunity. 2018;49(1):56–65.e54. doi: 10.1016/j.immuni.2018.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Karmakar M, Katsnelson MA, Dubyak GR, Pearlman E. Neutrophil P2X7 receptors mediate NLRP3 inflammasome-dependent IL-1β secretion in response to ATP. Nat Commun. 2016;7:10555. doi: 10.1038/ncomms10555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yue N, Huang H, Zhu X, Han Q, Wang Y, Li B, et al. Activation of P2X7 receptor and NLRP3 inflammasome assembly in hippocampal glial cells mediates chronic stress-induced depressive-like behaviors. J Neuroinflammation. 2017;14(1):102. doi: 10.1186/s12974-017-0865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jiang S, Zhang Y, Zheng JH, Li X, Yao YL, Wu YL, et al. Potentiation of hepatic stellate cell activation by extracellular ATP is dependent on P2X7R-mediated NLRP3 inflammasome activation. Pharmacol Res. 2017;117:82–93. doi: 10.1016/j.phrs.2016.11.040. [DOI] [PubMed] [Google Scholar]
- 64.Voican CS, Njiké-Nakseu M, Boujedidi H, Barri-Ova N, Bouchet-Delbos L, Agostini H, et al. Alcohol withdrawal alleviates adipose tissue inflammation in patients with alcoholic liver disease. Liver Int. 2015;35(3):967–978. doi: 10.1111/liv.12575. [DOI] [PubMed] [Google Scholar]
- 65.McClain CJ, Cohen DA, Dinarello CA, Cannon JG, Shedlofsky SI, Kaplan AM. Serum interleukin-1 (IL-1) activity in alcoholic hepatitis. Life Sci. 1986;39(16):1479–1485. doi: 10.1016/0024-3205(86)90554-0. [DOI] [PubMed] [Google Scholar]
- 66.Petrasek J, Bala S, Csak T, Lippai D, Kodys K, Menashy V, et al. IL-1 receptor antagonist ameliorates inflammasome-dependent alcoholic steatohepatitis in mice. J Clin Invest. 2012;122(10):3476–3489. doi: 10.1172/jci60777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang Y, Jin Q, Li X, Jiang M, Cui BW, Xia KL, et al. Amelioration of Alcoholic Liver Steatosis by Dihydroquercetin through the Modulation of AMPK-Dependent Lipogenesis Mediated by P2X7R-NLRP3-Inflammasome Activation. J Agric Food Chem. 2018;66(19):4862–4871. doi: 10.1021/acs.jafc.8b00944. [DOI] [PubMed] [Google Scholar]
- 68.Gao B, Ahmad MF, Nagy LE, Tsukamoto H. Inflammatory pathways in alcoholic steatohepatitis. J Hepatol. 2019;70(2):249–259. doi: 10.1016/j.jhep.2018.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Latz E, Xiao TS, Stutz A. Activation and regulation of the inflammasomes. Nat Rev Immunol. 2013;13(6):397–411. doi: 10.1038/nri3452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.de Carvalho Ribeiro M, Szabo G. Role of the Inflammasome in Liver Disease. Annu Rev Pathol. 2022;17:345–365. doi: 10.1146/annurev-pathmechdis-032521-102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhou Y, Wang S, Wan T, Huang Y, Pang N, Jiang X, et al. Cyanidin-3-O-β-glucoside inactivates NLRP3 inflammasome and alleviates alcoholic steatohepatitis via SirT1/NF-κB signaling pathway. Free Radic Biol Med. 2020;160:334–341. doi: 10.1016/j.freeradbiomed.2020.08.006. [DOI] [PubMed] [Google Scholar]
- 72.Liu X, Wang Y, Wu D, Li S, Wang C, Han Z, et al. Magnolol Prevents Acute Alcoholic Liver Damage by Activating PI3K/Nrf2/PPARγ and Inhibiting NLRP3 Signaling Pathway. Front Pharmacol. 2019;10:1459. doi: 10.3389/fphar.2019.01459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stickel F, Seitz HK. Alcoholic steatohepatitis. Best Pract Res Clin Gastroenterol. 2010;24(5):683–693. doi: 10.1016/j.bpg.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 74.Parola M, Pinzani M. Liver fibrosis: Pathophysiology, pathogenetic targets and clinical issues. Mol Aspects Med. 2019;65:37–55. doi: 10.1016/j.mam.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 75.Bataller R, Brenner DA. Liver fibrosis. J Clin Invest. 2005;115(2):209–218. doi: 10.1172/jci24282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang HJ, Gao B, Zakhari S, Nagy LE. Inflammation in alcoholic liver disease. Annu Rev Nutr. 2012;32:343–368. doi: 10.1146/annurev-nutr-072610-145138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hernandez-Gea V, Friedman SL. Pathogenesis of liver fibrosis. Annu Rev Pathol. 2011;6:425–456. doi: 10.1146/annurev-pathol-011110-130246. [DOI] [PubMed] [Google Scholar]
- 78.Varol C, Mildner A, Jung S. Macrophages: development and tissue specialization. Annu Rev Immunol. 2015;33:643–675. doi: 10.1146/annurev-immunol-032414-112220. [DOI] [PubMed] [Google Scholar]
- 79.Krenkel O, Tacke F. Liver macrophages in tissue homeostasis and disease. Nat Rev Immunol. 2017;17(5):306–321. doi: 10.1038/nri.2017.11. [DOI] [PubMed] [Google Scholar]
- 80.Bennett H, Troutman TD, Sakai M, Glass CK. Epigenetic Regulation of Kupffer Cell Function in Health and Disease. Front Immunol. 2020;11:609618. doi: 10.3389/fimmu.2020.609618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tacke F. Targeting hepatic macrophages to treat liver diseases. J Hepatol. 2017;66(6):1300–1312. doi: 10.1016/j.jhep.2017.02.026. [DOI] [PubMed] [Google Scholar]
- 82.Nagy LE. The Role of Innate Immunity in Alcoholic Liver Disease. Alcohol Res. 2015;37(2):237–250. [PMC free article] [PubMed] [Google Scholar]
- 83.Yu X, Lan P, Hou X, Han Q, Lu N, Li T, et al. HBV inhibits LPS-induced NLRP3 inflammasome activation and IL-1β production via suppressing the NF-κB pathway and ROS production. J Hepatol. 2017;66(4):693–702. doi: 10.1016/j.jhep.2016.12.018. [DOI] [PubMed] [Google Scholar]
- 84.Mridha AR, Wree A, Robertson AAB, Yeh MM, Johnson CD, Van Rooyen DM, et al. NLRP3 inflammasome blockade reduces liver inflammation and fibrosis in experimental NASH in mice. J Hepatol. 2017;66(5):1037–1046. doi: 10.1016/j.jhep.2017.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cai C, Zhu X, Li P, Li J, Gong J, Shen W, et al. NLRP3 Deletion Inhibits the Non-alcoholic Steatohepatitis Development and Inflammation in Kupffer Cells Induced by Palmitic Acid. Inflammation. 2017;40(6):1875–1883. doi: 10.1007/s10753-017-0628-z. [DOI] [PubMed] [Google Scholar]
- 86.Malik R, Selden C, Hodgson H. The role of non-parenchymal cells in liver growth. Semin Cell Dev Biol. 2002;13(6):425–431. doi: 10.1016/s1084952102001301. [DOI] [PubMed] [Google Scholar]
- 87.Pradere JP, Kluwe J, De Minicis S, Jiao JJ, Gwak GY, Dapito DH, et al. Hepatic macrophages but not dendritic cells contribute to liver fibrosis by promoting the survival of activated hepatic stellate cells in mice. Hepatology. 2013;58(4):1461–1473. doi: 10.1002/hep.26429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Purohit V, Brenner DA. Mechanisms of alcohol-induced hepatic fibrosis: a summary of the Ron Thurman Symposium. Hepatology. 2006;43(4):872–878. doi: 10.1002/hep.21107. [DOI] [PubMed] [Google Scholar]
- 89.Hellerbrand C. Hepatic stellate cells—the pericytes in the liver. Pflugers Arch. 2013;465(6):775–778. doi: 10.1007/s00424-012-1209-5. [DOI] [PubMed] [Google Scholar]
- 90.Puche JE, Saiman Y, Friedman SL. Hepatic stellate cells and liver fibrosis. Compr Physiol. 2013;3(4):1473–1492. doi: 10.1002/cphy.c120035. [DOI] [PubMed] [Google Scholar]
- 91.Dewidar B, Meyer C, Dooley S, Meindl-Beinker AN. TGF-β in Hepatic Stellate Cell Activation and Liver Fibrogenesis-Updated 2019. Cells. 2019;8(11):1419. doi: 10.3390/cells8111419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Higashi T, Friedman SL, Hoshida Y. Hepatic stellate cells as key target in liver fibrosis. Adv Drug Deliv Rev. 2017;121:27–42. doi: 10.1016/j.addr.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Tsuchida T, Friedman SL. Mechanisms of hepatic stellate cell activation. Nat Rev Gastroenterol Hepatol. 2017;14(7):397–411. doi: 10.1038/nrgastro.2017.38. [DOI] [PubMed] [Google Scholar]
- 94.Friedman SL. Hepatic stellate cells: protean, multifunctional, and enigmatic cells of the liver. Physiol Rev. 2008;88(1):125–172. doi: 10.1152/physrev.00013.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hanafusa H, Ninomiya-Tsuji J, Masuyama N, Nishita M, Fujisawa J, Shibuya H, et al. Involvement of the p38 mitogen-activated protein kinase pathway in transforming growth factor-beta-induced gene expression. J Biol Chem. 1999;274(38):27161–27167. doi: 10.1074/jbc.274.38.27161. [DOI] [PubMed] [Google Scholar]
- 96.Liu RM, Desai LP. Reciprocal regulation of TGF-β and reactive oxygen species: A perverse cycle for fibrosis. Redox Biol. 2015;6:565–577. doi: 10.1016/j.redox.2015.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Koli K, Myllärniemi M, Keski-Oja J, Kinnula VL. Transforming growth factor-beta activation in the lung: focus on fibrosis and reactive oxygen species. Antioxid Redox Signal. 2008;10(2):333–342. doi: 10.1089/ars.2007.1914. [DOI] [PubMed] [Google Scholar]
- 98.DeLeve LD. Liver sinusoidal endothelial cells in hepatic fibrosis. Hepatology. 2015;61(5):1740–1746. doi: 10.1002/hep.27376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Su QQ, Tian YY, Liu ZN, Ci LL, Lv XW. Purinergic P2X7 receptor blockade mitigates alcohol-induced steatohepatitis and intestinal injury by regulating MEK1/2-ERK1/2 signaling and egr-1 activity. Int Immunopharmacol. 2019;66:52–61. doi: 10.1016/j.intimp.2018.11.012. [DOI] [PubMed] [Google Scholar]
- 100.Zhao X, Gong L, Wang C, Liu M, Hu N, Dai X, et al. Quercetin mitigates ethanol-induced hepatic steatosis in zebrafish via P2X7R-mediated PI3K/ Keap1/Nrf2 signaling pathway. J Ethnopharmacol. 2021;268:113569. doi: 10.1016/j.jep.2020.113569. [DOI] [PubMed] [Google Scholar]
- 101.Shang Y, Li XF, Jin MJ, Li Y, Wu YL, Jin Q, et al. Leucodin attenuates inflammatory response in macrophages and lipid accumulation in steatotic hepatocytes via P2x7 receptor pathway: A potential role in alcoholic liver disease. Biomed Pharmacother. 2018;107:374–381. doi: 10.1016/j.biopha.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 102.Savio LEB, de Andrade Mello P, da Silva CG, Coutinho-Silva R. The P2X7 Receptor in Inflammatory Diseases: Angel or Demon? Front Pharmacol. 2018;9:52. doi: 10.3389/fphar.2018.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yu X, Xu Y, Zhang S, Sun J, Liu P, Xiao L, et al. Quercetin Attenuates Chronic Ethanol-Induced Hepatic Mitochondrial Damage through Enhanced Mitophagy. Nutrients. 2016;8(1):27. doi: 10.3390/nu8010027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Xiao J, Zhu Y, Liu Y, Tipoe GL, Xing F, So KF. Lycium barbarum polysaccharide attenuates alcoholic cellular injury through TXNIP-NLRP3 inflammasome pathway. Int J Biol Macromol. 2014;69:73–78. doi: 10.1016/j.ijbiomac.2014.05.034. [DOI] [PubMed] [Google Scholar]
- 105.Yang W, Huang L, Gao J, Wen S, Tai Y, Chen M, et al. Betaine attenuates chronic alcohol-induced fatty liver by broadly regulating hepatic lipid metabolism. Mol Med Rep. 2017;16(4):5225–5234. doi: 10.3892/mmr.2017.7295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bajaj JS. Alcohol, liver disease and the gut microbiota. Nat Rev Gastroenterol Hepatol. 2019;16(4):235–246. doi: 10.1038/s41575-018-0099-1. [DOI] [PubMed] [Google Scholar]
- 107.García ML, Blasco-Algora S, Fernández-Rodríguez CM. Alcohol liver disease: A review of current therapeutic approaches to achieve long-term abstinence. World J Gastroenterol. 2015;21(28):8516–8526. doi: 10.3748/wjg.v21.i28.8516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Stickel F, Hoehn B, Schuppan D, Seitz HK. Review article: Nutritional therapy in alcoholic liver disease. Aliment Pharmacol Ther. 2003;18(4):357–373. doi: 10.1046/j.1365-2036.2003.01660.x. [DOI] [PubMed] [Google Scholar]