Abstract
The Histoplasma capsulatum URA5 gene, which has recently been cloned and disrupted by allelic replacement, encodes orotidine-5′-monophosphate pyrophosphorylase. Inactivation of URA5 by either targeted or UV mutagenesis results in disruption of the pyrimidine biosynthetic pathway and uracil auxotrophy. We examined the effect of uracil auxotrophy due to a ura5 mutation on H. capsulatum virulence in both cell culture and whole-animal models. Uracil auxotrophs of two H. capsulatum restriction fragment length polymorphism classes were found to be avirulent in cultured murine and human cells, as well as in mice. Moreover, virulence could be restored either by supplying a functional URA5 gene in trans or by supplying exogenous uracil during infection in vitro. These experiments demonstrate that the pyrimidine biosynthetic pathway is essential for H. capsulatum growth and virulence.
The dimorphic fungus Histoplasma capsulatum is the causative agent of the most common systemic mycosis in the United States, histoplasmosis (9, 13, 46). Endemic to the Mississippi and Ohio River valleys, infection with H. capsulatum most often manifests itself as a mild respiratory infection with flu-like symptoms. However, H. capsulatum infection can lead to severe systemic infection and even death in immunocompromised hosts, such as AIDS or cancer patients (4, 15, 17, 18, 47). H. capsulatum is thermally dimorphic, existing as a saprophytic mold in the soil or at room temperature in the laboratory and as a yeast in the host or at 37°C in the laboratory. Upon inhalation of the mold form, the organism enters pulmonary macrophages, where it converts to the yeast form, replicating inside the phagolysosome and eventually lysing the cell (19, 31, 36). In immunocompetent individuals infection is limited by the cell-mediated immune response; however, the response is fungistatic rather than fungicidal (3, 6). It is thought that persistent infection may be reactivated when the patient becomes immunocompromised, resulting in a severe, potentially fatal systemic infection (7). Therefore, the identification of gene products essential for survival and growth of H. capsulatum in the host is important for the development of antifungal treatments. Although there have been reports of virulence differences between strains (24, 29), between variants of strains (5, 44, 50, 54), or after chemical treatment (28, 30), the previous lack of molecular genetic tools for this pathogen has precluded the construction of isogenic strains and definitive identification of genes necessary for virulence.
It has been demonstrated for several bacterial and fungal pathogens, including Bacillus anthracis (16), Listeria monocytogenes (27), Yersinia pestis (43), Salmonella typhimurium (1, 2, 14), Cryptococcus neoformans (37, 38, 45), and Candida albicans (11, 20, 23, 26, 40, 41), that organisms with mutations involving components of the purine or pyrimidine biosynthetic pathway are less virulent in cultured cells or whole animals. The H. capsulatum URA5 gene encodes orotidine-5′-monophosphate pyrophosphorylase (OMPpase), a component of the pyrimidine biosynthetic pathway, and ura5 mutants require exogenous uracil for growth in culture (54). In this study, we examined the ability of two H. capsulatum strains that lack a functional URA5 gene due to UV mutagenesis (G217B ura5-23) or targeted gene disruption (G184AS Δura5::hph) to infect cultured cells and mice. For these experiments, we developed a nonradioactive cell proliferation assay to examine the virulence of H. capsulatum in the mouse macrophage-like cell line RAW264.7, as well as a cytotoxicity assay to examine H. capsulatum virulence in the human monocyte line U937, which does not proliferate following phorbol myristate acetate (PMA) treatment to induce monocyte-to-macrophage differentiation. We found that the URA5 gene is essential for virulence in both murine and human cell lines, as well as in a mouse infection model, and that either resupplying URA5 by transformation or supplying exogenous uracil during infection of cultured cells restores virulence. This study is the first demonstration of Koch’s molecular postulates for a gene essential for virulence for this fungus. Moreover, it provides the basis for future examination of H. capsulatum genes essential for growth of the organism in the host cell by exploiting the absolute requirement for uracil during infection.
MATERIALS AND METHODS
Fungal strains.
H. capsulatum G217B, G184AS, and G184AS Δura5::hph have been described previously (52, 53). G217B (ATCC 26032) is a clinical isolate of restriction fragment length polymorphism (RFLP) class 2; G184AS is derived from the clinical isolate G184A (ATCC 26027) (RFLP class 3), and G184AS Δura5::hph was constructed by using allelic replacement with a hygromycin resistance marker which insertionally inactivated the URA5 gene (53). For this study, we isolated G217B ura5-23, a uracil-auxotrophic mutant of G217B, by UV mutagenesis and 5-fluoroorotic acid selection as described previously (54). We transformed both G217B ura5-23 and G184AS Δura5::hph with plasmid pWU45, a pBR328 derivative containing the Podospora anserina URA5 gene. This plasmid is identical to the previously described telomeric shuttle plasmid pWU44 (51), except for moving of the telomeric repeats from the BamHI site to the BclI site of the base plasmid pBR328, restoring a functional tetracycline resistance gene. We used the P. anserina URA5 gene for complementation due to the ease of detecting transforming DNA by Southern hybridization since it does not detectably hybridize to H. capsulatum genomic DNA (50, 51). This gene encodes the same OMPpase enzyme activity as the H. capsulatum URA5 gene and has not shown any differences from the native gene in transformation efficiency or the fate of transforming DNA (50, 51). Although pWU45 is a telomeric plasmid, for this study we used transformants (one from G217B ura5-23 and two from G184AS Δura5::hph) in which the transforming marker was chromosomally integrated and mitotically stable without selection.
Mammalian cells.
The mammalian cell lines used in this study were RAW264.7 (ATCC TIB-71), a murine macrophage-like cell line, and U937 (ATCC CRL-1593.2), a human monocyte line, both acquired from the American Type Culture Collection.
Growth media.
HMM, which has been described previously (52), was used for growth of H. capsulatum strains. HMM was supplemented with 0.1 mg of uracil/ml for the growth of uracil auxotrophs. RPMI medium (Gibco-BRL or Cellgro) supplemented with 10% heat-inactivated fetal calf serum (Gibco-BRL) (complete medium) was used for the growth of RAW264.7 and U937 cells. RPMI medium was supplemented with 0.1 mg of uracil/ml during infection with H. capsulatum when indicated. Penicillin and streptomycin (10 μg/ml each) were added to both HMM and RPMI medium. All cells were grown at 37°C with 5% CO2.
Virulence assays.
The virulence of H. capsulatum in RAW264.7 cells was measured as a percentage of host cell viability by using a nonradioactive cell proliferation kit (Boehringer Mannheim) based upon incorporation of the thymidine analogue bromodeoxyuridine (BrdU). RAW264.7 cells were plated at a density of 2 × 104 cells per well in 96-well plates (Costar) and allowed to adhere overnight. H. capsulatum strains were grown to approximately mid-log phase (2 days), and yeast cells were enumerated with a hemocytometer following 1/10 dilution in serum-free RPMI medium and vortexing to disperse aggregated cells. If the aggregates could not be completely dispersed, each small group of cells, usually containing two to six yeast cells, was counted as one infectious unit. Yeast cells were diluted in complete RPMI medium (with or without 0.1 mg of uracil/ml) and added to triplicate wells for a multiplicity of infection (MOI) of 0.5 yeast/mammalian cell. The plates were placed on a nutator (for gentle agitation) at 37°C, and infection was allowed to proceed for 4 h. Following removal of the extracellular yeast cells by washing with serum-free RPMI medium, complete RPMI medium (with or without 0.1 mg of uracil/ml) was added to each well and the plates were incubated for 4 days on a nutator at 37°C. The proliferation assay was carried out according to the manufacturer’s protocol. Briefly, extracellular yeast cells were removed by washing with serum-free RPMI medium, and surviving RAW264.7 cells were incubated with BrdU for 2 h. The RAW264.7 cells were then fixed and incubated with an anti-BrdU antibody conjugated to alkaline phosphatase, which was later quantitated by using a colorimetric substrate and reading the A370. The A370 of wells containing uninfected cells was set at 100% viability, and the A370 of wells containing medium only was set at 0%. Control experiments indicated that there was no detectable incorporation of BrdU by H. capsulatum during a 2-h incubation designed to mimic these experimental conditions (data not shown).
To prepare U937 cells for infection, 10 mM PMA was added to cells at a concentration of 1.5 × 103 cells/ml. This treatment has been shown to induce monocyte-to-macrophage differentiation in these cells (39). Treated cells are adherent to plastic and no longer proliferate. Adherent cells were collected after 24 h, counted, plated in 96-well plates at a concentration of 6 × 104 cells/well, and allowed to adhere for 48 h. H. capsulatum strains were grown to mid-log phase (2 days), and yeast cells were prepared for infection as described above. Infections were performed in triplicate wells at an MOI of 0.5 for 4 h, extracellular yeast cells were removed by washing with serum-free RPMI medium, and complete RPMI medium (with or without 0.1 mg of uracil/ml) was added to each well. The plates were incubated for 7 days on a nutator at 37°C, and fresh complete RPMI medium was added to each well on day 4. On day 7, viable U937 cells were stained with a solution of 0.2% crystal violet in 2% ethanol. After wells were washed six times with serum-free RPMI medium, 100 μl of the stain was added to each well for 10 min, and then excess stain was removed by washing the plate with distilled H2O. Stained cells were solubilized with 1% sodium dodecyl sulfate for 30 min before A590 was read. The A590 of wells containing uninfected cells was set at 100% viability, and the A590 of wells containing medium only was set at 0%.
For infection of both cell lines in the presence of exogenous uracil, uracil was included in the control uninfected wells used to establish 100% viability. We have not observed any deleterious effect of uracil on mammalian cells. However, uracil was added to control cells in these experiments to allow us to evaluate the effect of uracil solely on the infecting H. capsulatum yeast.
Infection of mice with H. capsulatum.
Male C57BL/6 mice were purchased from Jackson Laboratories (Bar Harbor, Maine). Groups of mice (n = 6) were infected intranasally with 2.5 × 105 H. capsulatum yeast cells in a 50-μl volume.
Organ culture for H. capsulatum.
Lungs and spleens were homogenized in balanced salt solution and serially diluted and dispensed (100 μl) onto plates containing brain heart infusion agar (2% agar [wt/vol]) supplemented with 5% (vol/vol) defibrinated sheep erythrocytes, 1% glucose, 0.1 mg of uracil/ml, and 0.01% (wt/vol) cysteine hydrochloride. Plates were incubated at 30°C, and CFU were enumerated after 7 to 10 days. Data are expressed as means ± standard errors of the means per organ.
RESULTS
Effect of uracil auxotrophy on H. capsulatum virulence in a murine cell line.
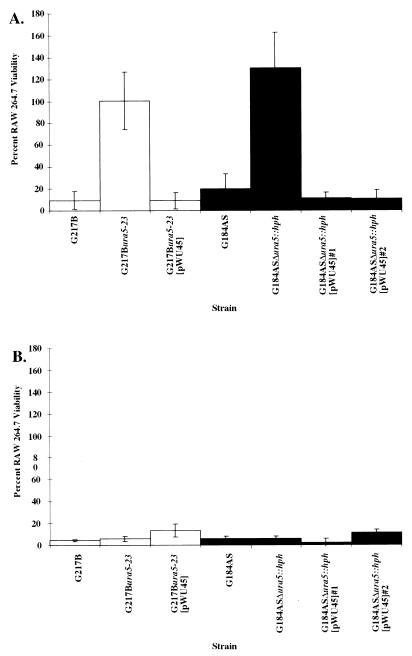
We examined the effect of uracil auxotrophy on the virulence of H. capsulatum strains of two different RFLP classes in the murine macrophage-like cell line RAW264.7. G217B, which belongs to RFLP class 2, has previously been shown to be virulent in murine macrophages, both primary isolates (8, 42, 48, 49) and the cell line P388D1 (10); however, its virulence in RAW264.7 cells has not previously been tested. Although to our knowledge the virulence of G184AS, RFLP class 3, in RAW264.7 cells has not been tested, previous studies have shown that G184AS is avirulent in the murine cell line P388D1 (10). To examine virulence in RAW264.7 cells, we adapted a nonradioactive cell proliferation assay to measure the number of RAW264.7 cells viable after infection with H. capsulatum, presuming that virulence of H. capsulatum strains is inversely proportional to the viability of the RAW264.7 host cell. As shown in Fig. 1A, both G217B and G184AS were virulent, that is, infection resulted in low RAW264.7 cell viability, at an MOI of 0.5, with G217B exhibiting slightly greater virulence (10% viability) than G184AS (20% viability). However, the uracil auxotrophs G217B ura5-23 and G184AS Δura5::hph were found to be avirulent in RAW264.7 cells (Fig. 1A). Infection with these strains resulted in high RAW264.7 cell viability, often at values of greater than 100%. These high values were not a result of yeast cell incorporation of BrdU and may be due to the activation of RAW264.7 cell proliferation resulting from the presence of avirulent yeast. To determine if a lack of available uracil was responsible for the reduced virulence of the URA5 mutants, we supplied uracil in the medium during infection. The addition of 0.1 mg of uracil/ml restored virulence to both G217B ura5-23 and G184AS Δura5::hph, each resulting in approximately 6% RAW264.7 cell viability (Fig. 1B). Resupply of a functional URA5 gene on a plasmid, pWU45, in addition to restoring uracil prototrophy to the yeast in vitro, restored virulence to a G217B ura5-23 transformant (∼9% viability) and two independent G184AS Δura5::hph transformants (∼10 to 11% viability) (Fig. 1A). These results indicate that avirulence of the ura5 mutants was due to uracil auxotrophy and could be complemented by addition of exogenous uracil or by supply of a functional URA5 gene in this infection model.
FIG. 1.
Effect of uracil auxotrophy on the virulence of H. capsulatum in RAW264.7 cells. Virulence is expressed as a function of RAW264.7 cell viability after infection. Viability was assessed by measuring the incorporation of the thymidine analogue BrdU, with the amount of BrdU taken up by uninfected RAW264.7 cells set at 100% viability. Each bar represents RAW264.7 viability after infection with the indicated H. capsulatum strain. The averages of triplicate wells from a representative experiment are shown, with standard deviations indicated by error bars. Similar results were observed in three independent experiments. (A) RAW264.7 cell viability resulting from infection with H. capsulatum without the addition of uracil to the culture medium. (B) RAW264.7 cell viability resulting from infection with H. capsulatum with the addition of uracil to the culture medium, including the uninfected wells used to establish 100% viability.
Effect of uracil auxotrophy on H. capsulatum virulence in mice.
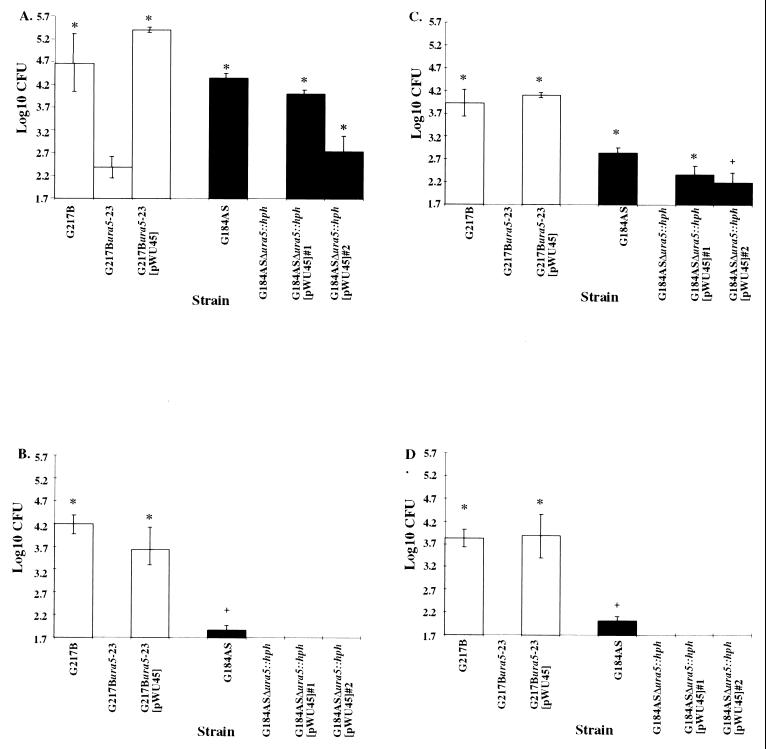
Since uracil-auxotrophic H. capsulatum strains were avirulent in cultured murine macrophage-like cells, we next examined whether these results were indicative of avirulence in whole-animal infections. Twelve mice were infected intranasally with the H. capsulatum strains indicated in Fig. 2. After 7 and 14 days, six mice were sacrificed, and the lungs and spleens were examined for the presence of H. capsulatum by plate culture. The level of G217B remained fairly constant (∼4 log10 CFU) in both lung and spleen cultures at weeks 1 and 2 postinfection. The results at 1 week postinfection show that G184AS, which was previously found to be avirulent in an intravenous mouse infection model (21), yielded only 0.3 log10 fewer CFU in the lung than G217B (Fig. 2A). However, G184AS yielded 1.1 log10 fewer CFU than G217B in the spleen at week 1 (Fig. 2C). The number of CFU present the second week after infection with G184AS indicates that the yeast was being cleared from the lung (∼2.5 log10 fewer CFU) (Fig. 2B), though CFU levels in the spleen were similar to those at week 1 (Fig. 2D). Although G184AS was clearly less virulent than G217B, levels of yeast recoverable at 1 week postinfection were high enough to detect differences between infection with the wild-type and uracil-auxotrophic strains. Consistent with results with RAW264.7 cells, the uracil auxotrophs G217B ura5-23 and G184AS Δura5::hph exhibited greatly diminished virulence. Only cultures from lungs 1 week after infection with G217B ura5-23 produced any CFU (Fig. 2A), but complete clearance occurred by week 2 (Fig. 2B). The reduced virulence of the uracil auxotrophs was also shown to be due to the lack of a functional URA5 gene in this infection model. Infection of mice with G217B ura5-23 and G184AS Δura5::hph pWU45 transformants showed complete or substantial restoration of virulence, reflected by the CFU cultured from both the spleen and lung. The G217B ura5-23 transformant had a level of CFU slightly higher than the wild type in the lung (5.4 log10 CFU) (Fig. 2A) and spleen (4.1 log10 CFU) (Fig. 2C) at week 1, with some reduction in CFU at week 2 (Fig. 2B and D). Although the number of CFU present in the lung at week 1 resulting from infection with G184AS Δura5::hph [pWU45]#2 was greater than that of the parental strain, it was ∼1.6 log10 unit lower than that of G184AS (Fig. 2A). However, infection with G184AS Δura5::hph [pWU45]#1 did show a more complete restoration of virulence, with 4 log10 CFU recovered from the lung and 2.4 log10 CFU recovered from the spleen at week 1 (Fig. 2A and C). Similar to G184AS, transformant yeasts were cleared from the lung and spleen by week 2 (Fig. 2B and D).
FIG. 2.
CFU recovered from mice infected with H. capsulatum. Shown are the CFU obtained from homogenates of the lungs (A and B) and spleens (C and D) of six mice at 1 week (A and C) and 2 weeks (B and D) postinfection. The lower limit of detection for this experiment was 50 CFU, or 1.7 log 10 CFU. Error bars represent standard errors of the means. +, P < 0.05 relative to the value for the corresponding uracil auxotroph, as determined by the Student t test; ∗, P < 0.01 relative to the value for the corresponding uracil auxotroph, as determined by the Student t test.
H. capsulatum infection of a human cell line.
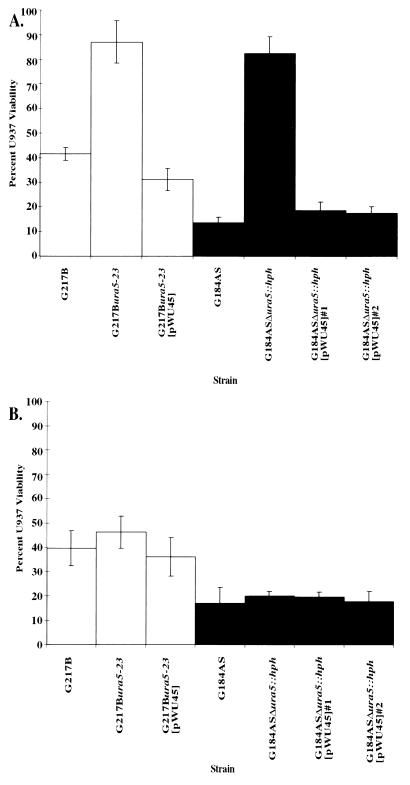
A long-term goal of our studies is to uncover those factors important for H. capsulatum infection and persistence in humans. Although murine infections are a useful model, allowing examination of both cell culture and whole-animal infections, it is important to examine the effect of H. capsulatum uracil auxotrophy on the infection of human cells and in particular human mononuclear phagocytes. Previous studies involving H. capsulatum infection of human monocytes have relied upon explanted cells from human volunteers (32–35). For ease of acquisition and consistency between experiments, we examined the effect of H. capsulatum uracil auxotrophy on the infection of the human monocyte line U937, which is both differentiable and activable. U937 cells were differentiated with the phorbol ester PMA, and adherent cells were infected with the H. capsulatum strains. Because the cells are terminally differentiated, and therefore do not replicate, we could not use the nonradioactive cell proliferation assay as a measure of host cell viability. Instead, viable cells were stained with crystal violet after infection. A longer infection period (7 days) than used for RAW264.7 cells (4 days) was necessary since lysis of U937 cells was not observed until at least day 6. Similar to the infection of RAW264.7 cells, both G217B and G184AS were found to be virulent at an MOI of 0.5 (Fig. 3A). However, unlike the infection of RAW264.7 cells, G184AS was found to be slightly more virulent, yielding only 14% U937 cell viability, than G217B, which yielded 42% U937 cell viability. Consistent with the previous experiments utilizing murine cell culture and whole-animal infections, the uracil auxotrophs G217B ura5-23 and G184AS Δura5::hph were found to be avirulent in U937 cells (Fig. 3A). Infection with either auxotroph resulted in 85% U937 cell viability. However, supplying uracil (0.1 mg/ml) exogenously restored virulence of G217B ura5-23 and G184AS Δura5::hph to wild-type levels (46 and 20% U937 cell viability, respectively) (Fig. 3B). Moreover, resupplying a functional URA5 gene in trans also restored the virulence of the uracil-auxotrophic strains G217B ura5-23 and G184AS Δura5::hph (31% and ∼18 to 20% U937 cell viability, respectively) (Fig. 3A).
FIG. 3.
Effect of uracil auxotrophy on the virulence of H. capsulatum in U937 cells. Virulence is expressed as a function of U937 cell viability after infection. Viability was assessed by staining with crystal violet. Dye uptake by uninfected cells was set at 100% viability. Each bar represents U937 cell viability after infection with the indicated H. capsulatum strain. The averages of triplicate wells from a representative experiment are shown, with standard deviations indicated by error bars. Similar results were observed in three independent experiments. (A) U937 cell viability resulting from infection with H. capsulatum without the addition of uracil to the culture medium. (B) U937 cell viability resulting from infection with H. capsulatum with the addition of uracil to the culture medium, including the uninfected wells used to establish 100% viability.
DISCUSSION
The ability of a pathogen to survive within the host cell involves the activity of many gene products, including those that enable the organism to acquire nutrients within the harsh intracellular environment. By studying the effect of auxotrophic mutations on the survival of H. capsulatum in host cells, we hope to gain insight into the factors necessary for pathogenicity of the fungus. In this study, we showed that uracil auxotrophy due to loss of a functional URA5 gene product, OMPpase, results in loss of virulence for at least two RFLP classes of H. capsulatum. Infection of murine (RAW264.7) or human (U937) cells with the UV-generated auxotrophic mutant G217B ura5-23 or the targeted URA5 mutant G184AS Δura5::hph results in high viability of the host cell compared to infection with the corresponding prototrophic strain, indicating reduced virulence. Similar results were observed during mouse infections. Although G184AS exhibits lower levels of virulence in mice than does G217B, with lower numbers of CFU recovered from both the lung and spleen, the number of CFU observed after infection with G184AS is significantly different than that observed after infection with G184AS Δura5::hph.
Resupply of a functional URA5 gene in trans restored virulence, thus fulfilling Koch’s molecular postulates, with the caveat that a P. anserina URA5 gene, encoding the same OMPpase activity, was used for complementation. Virulence equal to that of the corresponding uracil-prototrophic strains was observed upon infection of either RAW264.7 or U937 cells with transformants of the uracil-auxotrophic strains carrying the plasmid pWU45, which contains a functional URA5 gene. These data are consistent with the auxotrophic defect being the sole cause of the reduction in virulence in these infection models. Full or partial restoration of virulence by transformation with pWU45 was also observed in the infection of whole animals. Similar numbers of CFU were recovered from mice infected with the wild-type strain, G217B, and the transformed uracil-prototrophic strain, G217B ura5-23 [pWU45], in both the lung and spleen. Although G184AS Δura5::hph [pWU45]#1 and G184AS Δura5::hph [pWU45]#2 did not show a level of virulence equal to that of the wild-type strain, G184AS, and in fact showed levels of virulence different from each other, the number of CFU observed after infection with these two strains was greater than that of the parental uracil-auxotrophic strain, G184AS Δura5::hph, indicating that some level of virulence was restored. One explanation for the lack of full restoration of virulence could be that the P. anserina URA5 gene used to complement uracil auxotrophy may exhibit diminished expression, or OMPpase activity, in the mouse infection model for G184AS. Alternately, there may be a relatively greater requirement for P. anserina URA5 expression or OMPpase activity specifically in this model system. It has been reported that transformation with a different plasmid containing this marker results in incomplete restoration of OMPpase activity (55). However, there was no evidence for this phenomenon with G217B derivatives and no indication of suboptimal expression in G184AS derivatives during in vitro growth or infection of cultured cells. Another explanation for the incomplete restoration of virulence of the two G184AS Δura5::hph transformants is that the integration site of the plasmid may have an effect on other factors involved in the infection process. However, both transformants exhibit lower levels of virulence than G184AS. Such incomplete complementation following gene disruption and restoration of the wild-type gene by transformation has been observed in pathogenic fungi previously (12, 22, 25). Obviously such phenomena merit careful consideration of the particular infection model and the microbial strain background used for testing effects on virulence.
The addition of exogenous uracil during the infection of cultured cells also restored virulence, indicating that the yeast cells are able to acquire and utilize uracil during infection of macrophages but that uracil is perhaps either not present in the intracellular environment or present in concentrations too low to support the growth of H. capsulatum under normal infection conditions. The low level of RAW264.7 and U937 cell viability resulting from infection in the presence of uracil was not due to some toxic effect of uracil itself, since control uninfected cells grown in the presence of uracil were viable after mock infection. In fact, the viability of these cells as measured by BrdU or crystal violet uptake was set at 100%, and the viability of infected cells was compared to that of these cells.
These results serve to reinforce the importance of pyrimidine biosynthesis for survival and virulence. Several purine- and pyrimidine-auxotrophic mutants of both bacterial and fungal pathogens have been shown to have reduced virulence. Adenine auxotrophs of S. typhimurium (1, 2, 14), B. anthracis (16), and L. monocytogenes (27) have proved avirulent in mice. Likewise, a C. neoformans strain auxotrophic for adenine exhibits reduced virulence in rabbits (37), while some C. neoformans strains auxotrophic for uracil (45) or the amino acid arginine (38) have shown decreased virulence in mice. pur mutants of Y. pestis, Yersinia pseudotuberculosis, and Yersinia enterocolitica, which require guanine for growth, are also avirulent in mice (43). Decreased pathogenicity has been observed for proline (20, 41), lysine (20, 41), serine (20, 26), adenine (20, 23, 40, 41), and uracil (11, 20) auxotrophs of C. albicans. These results, together with those presented in this paper, strongly suggest that biosynthetic pathways may serve as excellent targets for antifungal therapy. Moreover, genes encoding proteins involved in purine and pyrimidine biosynthetic pathways may serve as markers for expression during infection. We are currently investigating the use of the URA5 gene as a reporter for testing promoter activity during macrophage infection.
ACKNOWLEDGMENTS
This work was supported by Public Health Service grant HL55949 from the National Heart, Lung, and Blood Institute. D.M.R. was supported by National Research Service award F32 AI09720 from the National Institute of Allergy and Infectious Diseases and by a Basic Biomedical Research grant from the Life and Health Insurance Medical Research Fund.
REFERENCES
- 1.Bacon G A, Burrows T W, Yates M. The effects of biochemical mutation on the virulence of Bacterium typhimosum: the loss of virulence in certain mutants. Br J Exp Pathol. 1951;32:85–96. [PMC free article] [PubMed] [Google Scholar]
- 2.Buchmeier N A, Libby S J. Dynamics of growth and death within a Salmonella typhimurium population during infection of macrophages. Can J Microbiol. 1996;43:29–34. doi: 10.1139/m97-005. [DOI] [PubMed] [Google Scholar]
- 3.Bullock W E. Interaction between human phagocytic cells and Histoplasma capsulatum. Arch Med Res. 1993;24:219–223. [PubMed] [Google Scholar]
- 4.Chaturvedi S, Frame P, Newman S L. Macrophages from human immunodeficiency virus-positive persons are defective in host defense against Histoplasma capsulatum. J Infect Dis. 1995;171:320–327. doi: 10.1093/infdis/171.2.320. [DOI] [PubMed] [Google Scholar]
- 5.Daniels L S, Berliner M D, Campbell C C. Varying virulence in rabbits infected with different filamentous types of Histoplasma capsulatum. J Bacteriol. 1968;96:1535–1539. doi: 10.1128/jb.96.5.1535-1539.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deepe G S., Jr The immune response to Histoplasma capsulatum: unearthing its secrets. J Clin Med. 1994;123:201–205. [PubMed] [Google Scholar]
- 7.Deepe G S., Jr Histoplasma capsulatum: darling of the river valleys. ASM News. 1997;63:599–604. [Google Scholar]
- 8.Eissenberg L G, Goldman W E. Histoplasma capsulatum fails to trigger release of superoxide from macrophages. Infect Immun. 1987;55:29–34. doi: 10.1128/iai.55.1.29-34.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eissenberg L G, Goldman W E. Histoplasma variation and adaptive strategies for parasitism: new perspectives on histoplasmosis. Clin Microbiol Rev. 1991;4:411–421. doi: 10.1128/cmr.4.4.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eissenberg L G, West J L, Woods J P, Goldman W E. Infection of P388D1 macrophages and respiratory epithelial cells by Histoplasma capsulatum: selection of avirulent variants and their potential role in persistent histoplasmosis. Infect Immun. 1991;59:1639–1646. doi: 10.1128/iai.59.5.1639-1646.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fasoli M O F, Kerridge D, Ryley J F. Pathogenicity of 5-fluorocytosine resistant strains of Candida albicans. J Med Vet Mycol. 1990;28:27–34. doi: 10.1080/02681219080000041. [DOI] [PubMed] [Google Scholar]
- 12.Gale C A, Bendel C M, McClellan M, Hauser M, Becker J M, Berman J, Hostetter M K. Linkage of adhesion, filamentous growth, and virulence in Candida albicans to a single gene, INT1. Science. 1998;279:1355–1358. doi: 10.1126/science.279.5355.1355. [DOI] [PubMed] [Google Scholar]
- 13.Goodwin R A, Jr, Des Prez R M. Histoplasmosis. Am Rev Respir Dis. 1978;117:929–956. doi: 10.1164/arrd.1978.117.5.929. [DOI] [PubMed] [Google Scholar]
- 14.Gowen J W, Stadler J, Plough H H, Miller H N. Virulence and immunizing capacity of Salmonella typhimurium as related to mutations in metabolic requirements. Genetics. 1953;38:531–549. doi: 10.1093/genetics/38.6.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Graybill J R. Histoplasmosis and AIDS. J Infect Dis. 1988;158:623–626. doi: 10.1093/infdis/158.3.623. [DOI] [PubMed] [Google Scholar]
- 16.Ivanovics G, Marjai E, Dobozy A. The growth of purine mutants of Bacillus anthracis in the body of the mouse. J Gen Microbiol. 1968;53:147–162. doi: 10.1099/00221287-53-2-147. [DOI] [PubMed] [Google Scholar]
- 17.Johnson P C, Khardori N, Najjar A F, Butt F, Mansell P W A, Sarosi G A. Progressive disseminated histoplasmosis in patients with acquired immunodeficiency syndrome. Am J Med. 1988;85:152–157. doi: 10.1016/s0002-9343(88)80334-6. [DOI] [PubMed] [Google Scholar]
- 18.Kauffman C A, Isreal K S, Smith J W, White A C, Schwartz J, Brooks G F. Histoplasmosis in immunosuppressed patients. Am J Med. 1978;64:923–932. doi: 10.1016/0002-9343(78)90445-x. [DOI] [PubMed] [Google Scholar]
- 19.Kimberlin C L, Hairiri A R, Hempel H O, Goodman N L. Interactions between Histoplasma capsulatum and macrophages from normal and treated mice: comparison of mycelial and yeast phases in alveolar macrophages. Infect Immun. 1981;34:6–10. doi: 10.1128/iai.34.1.6-10.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirsch D R, Whitney R R. Pathogenicity of Candida albicans auxotrophic mutants in experimental infections. Infect Immun. 1991;59:3297–3300. doi: 10.1128/iai.59.9.3297-3300.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Klimpel K R, Goldman W E. Isolation and characterization of spontaneous avirulent variants of Histoplasma capsulatum. Infect Immun. 1987;55:528–533. doi: 10.1128/iai.55.3.528-533.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kohler J R, Fink G R. Candida albicans strains heterozygous and homozygous for mutations in mitogen-activated protein kinase signaling components have defects in hyphal development. Proc Natl Acad Sci USA. 1996;93:13223–13228. doi: 10.1073/pnas.93.23.13223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kwon-Chung K J, Hill W B. Studies on the pink adenine-deficient strains of Candida albicans. I. Cultural and morphological characteristics. Sabouraudia. 1970;8:48–59. [PubMed] [Google Scholar]
- 24.Lambowitz A M, Kobayashi G S, Painter A, Medoff G. Possible relationship of morphogenesis in the pathogenic fungus, Histoplasma capsulatum, to heat shock response. Nature. 1983;303:806–808. doi: 10.1038/303806a0. [DOI] [PubMed] [Google Scholar]
- 25.Lo H J, Kohler J R, DiDomenico B, Loebenberg D, Cacciapuoti A, Fink G R. Nonfilamentous C. albicans mutants are avirulent. Cell. 1997;90:939–949. doi: 10.1016/s0092-8674(00)80358-x. [DOI] [PubMed] [Google Scholar]
- 26.Manning M, Snoddy C B, Fromtling R A. Comparative pathogenicity of auxotrophic mutants of Candida albicans. Can J Microbiol. 1983;30:31–35. doi: 10.1139/m84-005. [DOI] [PubMed] [Google Scholar]
- 27.Marquis H, Bouwer H G A, Hinrichs D J, Portnoy D A. Intracytoplasmic growth and virulence of Listeria monocytogenes auxotrophic mutants. Infect Immun. 1993;61:3756–3760. doi: 10.1128/iai.61.9.3756-3760.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Medoff G, Kobayashi G S, Painter A, Travis S. Morphogenesis and pathogenicity of Histoplasma capsulatum. Infect Immun. 1987;55:1355–1358. doi: 10.1128/iai.55.6.1355-1358.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Medoff G, Maresca B, Lambowitz A M, Kobayashi G, Painter A, Sacco M, Carratu L. Correlation between pathogenicity and temperature sensitivity in different strains of Histoplasma capsulatum. J Clin Investig. 1986;78:1638–1647. doi: 10.1172/JCI112757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Medoff G, Sacco M, Maresco B, Schlessinger D, Painter A, Kobayashi G S, Carratu L. Irreversible block of the mycelial-to-yeast phase transition of Histoplasma capsulatum. Science. 1986;231:476–479. doi: 10.1126/science.3001938. [DOI] [PubMed] [Google Scholar]
- 31.Newman S L, Bucher C, Rhodes J, Bullock W E. Phagocytosis of Histoplasma capsulatum yeasts and microconidia by human cultured macrophages and alveolar macrophages. Cellular cytoskeleton required for attachment and ingestion. J Clin Investig. 1990;85:223–230. doi: 10.1172/JCI114416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Newman S L, Gootee L. Colony-stimulating factors activate human macrophages to inhibit growth of Histoplasma capsulatum yeasts. Infect Immun. 1992;60:4593–4597. doi: 10.1128/iai.60.11.4593-4597.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Newman S L, Gootee L, Brunner G, Deepe G S., Jr Chloroquine induces human macrophage killing of Histoplasma capsulatum by limiting the availability of intracellular iron and is therapeutic in a murine model of histoplasmosis. J Clin Investig. 1994;93:1422–1429. doi: 10.1172/JCI117119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Newman S L, Gootee L, Bucher C, Bullock W E. Inhibition of intracellular growth of Histoplasma capsulatum yeast cells by cytokine-activated human monocytes and macrophages. Infect Immun. 1991;59:737–741. doi: 10.1128/iai.59.2.737-741.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Newman S L, Gootee L, Kidd C, Ciraolo G M, Morris R. Activation of human macrophage fungistatic activity against Histoplasma capsulatum upon adherence to type 1 collagen matrices. J Immunol. 1997;158:1779–1786. [PubMed] [Google Scholar]
- 36.Newman S L, Gootee L, Morris R, Bullock W E. Digestion of Histoplasma capsulatum yeasts by human macrophages. J Immunol. 1981;149:574–580. [PubMed] [Google Scholar]
- 37.Perfect J R, Toffaletti D L, Rude T H. The gene encoding phosphoribosylaminoimidazole carboxylase (ADE2) is essential for growth of Cryptococcus neoformans in cerebrospinal fluid. Infect Immun. 1993;61:4446–4451. doi: 10.1128/iai.61.10.4446-4451.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rhodes J C, Howard D H. Isolation and characterization of arginine auxotrophs of Cryptococcus neoformans. Infect Immun. 1980;27:910–914. doi: 10.1128/iai.27.3.910-914.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rodgers F G, Gibson F C., III Opsonin-independent adherence and intracellular development of Legionella pneumophila within U-937 cells. Can J Microbiol. 1993;39:718–722. doi: 10.1139/m93-103. [DOI] [PubMed] [Google Scholar]
- 40.Sarachek A. Promotion or retardation of the growth of adenine auxotrophs of Candida albicans. Antonie Leeuwenhoek. 1964;30:289–302. doi: 10.1007/BF02046735. [DOI] [PubMed] [Google Scholar]
- 41.Shepherd M G. Pathogenicity of morphological and auxotrophic mutants of Candida albicans in experimental infections. Infect Immun. 1985;50:541–544. doi: 10.1128/iai.50.2.541-544.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smith J G, Magee D M, Williams D M, Graybill J R. Tumor necrosis factor-α plays a role in host defense against Histoplasma capsulatum. J Infect Dis. 1990;162:1349–1353. doi: 10.1093/infdis/162.6.1349. [DOI] [PubMed] [Google Scholar]
- 43.Straley S C, Brubaker R R. Localization in Yersinia pestis of peptides associated with virulence. Infect Immun. 1982;36:129–135. doi: 10.1128/iai.36.1.129-135.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tewari R P, Berkout F J. Comparative pathogenesis of albino and brown types of Histoplasma capsulatum for mice. J Infect Dis. 1972;125:504–508. doi: 10.1093/infdis/125.5.504. [DOI] [PubMed] [Google Scholar]
- 45.Varma A, Edman J C, Kwon-Chung K J. Molecular and genetic analysis of URA5 transformants of Cryptococcus neoformans. Infect Immun. 1992;60:1101–1108. doi: 10.1128/iai.60.3.1101-1108.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wheat L J. Histoplasmosis. Infect Dis Clin N Am. 1988;2:841–859. [PubMed] [Google Scholar]
- 47.Wheat L J. Endemic mycosis in AIDS: a clinical review. Clin Microbiol Rev. 1995;8:146–159. doi: 10.1128/cmr.8.1.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wolf J E, Abegg A L, Travis S J, Kobayashi G S, Little J R. Effects of Histoplasma capsulatum on murine macrophage functions: inhibition of macrophage priming, oxidative burst, and antifungal activities. Infect Immun. 1989;57:513–519. doi: 10.1128/iai.57.2.513-519.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wolf J E, Kerchberger V, Kobayashi G S, Little J R. Modulation of the macrophage oxidative burst by Histoplasma capsulatum. J Immunol. 1987;138:582–586. [PubMed] [Google Scholar]
- 50.Woods J P, Goldman W E. In vivo generation of linear plasmids with addition of telomeric sequences by Histoplasma capsulatum. Mol Microbiol. 1992;6:3603–3610. doi: 10.1111/j.1365-2958.1992.tb01796.x. [DOI] [PubMed] [Google Scholar]
- 51.Woods J P, Goldman W E. Autonomous replication of foreign DNA in Histoplasma capsulatum: role of native telomeric sequences. J Bacteriol. 1993;175:636–641. doi: 10.1128/jb.175.3.636-641.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Woods J P, Heinecke E L, Goldman W E. Electrotransformation and expression of bacterial genes encoding hygromycin phosphotransferase and β-galactosidase in the pathogenic fungus Histoplasma capsulatum. Infect Immun. 1998;66:1697–1707. doi: 10.1128/iai.66.4.1697-1707.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Woods J P, Retallack D M, Heinecke E L, Goldman W E. Rare homologous gene targeting in Histoplasma capsulatum: disruption of the URA5Hc gene by allelic replacement. J Bacteriol. 1998;180:5135–5143. doi: 10.1128/jb.180.19.5135-5143.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Worsham P L, Goldman W E. Selection and characterization of ura5 mutants of Histoplasma capsulatum. Mol Gen Genet. 1988;214:348–352. doi: 10.1007/BF00337734. [DOI] [PubMed] [Google Scholar]
- 55.Worsham P L, Goldman W E. Development of a genetic transformation system for Histoplasma capsulatum: complementation of uracil auxotrophy. Mol Gen Genet. 1990;221:358–362. doi: 10.1007/BF00259400. [DOI] [PubMed] [Google Scholar]