Abstract
There is a considerable burden of children being hospitalized due to infectious diseases worldwide. The COVID-19 pandemic provided a unique opportunity to examine effects of worldwide efforts to control spread of infection. We aimed to investigate overall age-specific hospitalizations due to viral and bacterial infections and diseases triggered by respiratory tract infections during and after lockdown. This nationwide register–based observational study included children from 29 days to 17 years old hospitalized in all Danish pediatric emergency departments during the years 2015–2021. Main outcomes were ICD-10 diagnoses for infectious diseases and infection triggered illnesses. Fluctuations in hospitalization events were explored using figures with weekly events per 100,000. Total events followed a predictable pattern during 2015–2019. In 2020–2021, there was a drop in hospital encounters after lockdowns and surge after reopenings. In 2021, there was a surge of hospital encounters in the late summer due to respiratory syncytial virus infections and asthmatic bronchitis mostly in infants from 29 days to 2 years. For the infectious diseases, there was a dramatic decrease in events after lockdowns and immediate increase in cases that followed the same pattern of previous years after reopenings. Bacterial infections, like urinary tract infections, sepsis, and meningitis followed a steady pattern throughout all calendar-years.
Conclusions: Nationwide efforts to minimize infectious disease spread like lockdowns have a preventative and period lasting effect but reopenings/reunions result in surges of infectious diseases. This might be due to children not getting immunized steadily thereby increasing the pool of possible hosts for potential viral infections.
|
What is Known: • There is a seasonal fluctuation in viral/respiratory infections in children with higher infection rates in the winter and lower rates in the summer. • RSV infection is a major source of concern. | |
|
What is New: • Major lockdowns and reopenings disrupt the seasonal fluctuations which can result in high surges in infections that increases the burden of children emergency departments and the risk of serious complications. |
Supplementary Information
The online version contains supplementary material available at 10.1007/s00431-022-04682-7.
Keywords: Pandemic, Viral infections, Children, Respiratory syncytial virus, Seasons, Coronavirus disease
Introduction
Worldwide, there is a considerable burden of children being hospitalized, morbidity, and mortality due to viral respiratory tract infections (RTI) and infectious diseases in general [1–4]. Lower RTIs (viral and bacterial) are the number one infectious cause of death in children worldwide [1]. Children below 3 years of age are at risk of having several infection related hospitalizations [5]. Respiratory syncytial virus infection (RSV) is one of the major causes of hospital admissions in children under 5 years of age [6, 7]. Early childhood RTIs are associated to childhood and early adulthood asthma [8]. There is a considerable burden of urinary tract infections (UTI) that are some of the most frequent bacterial infections in infants and children with an overall prevalence of 7% among infants with fever [9].
Research on efforts to control or minimize spread of viral respiratory infections is scarce and of low quality because of general low compliance with interventions [10, 11]. The Coronavirus disease (COVID-19) pandemic provided a unique opportunity to explore effects and consequences of country wide efforts to attempt infectious disease control through major lockdowns, social distancing, and increase of sanitary precautions on the general spread of infections, infectious disease patterns, and infectious disease mortality [12].
We aimed to investigate overall and age-specific short and long pediatric emergency hospitalization contacts (events) due to both viral and bacterial infections and diseases triggered by infections during and after lockdowns during the pandemic compared to five calendar-years before (2015–2021).
Materials and methods
Setting
This nationwide register–based observational study used information from Danish registers. The Danish Civil Registration System provided birth dates, deaths, sex, and migration status [13]. The Danish National Patient Register provided data on pediatric emergency hospitalization events with main diagnoses according to the International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) [14]. The Danish nationwide register setup has previously been described in detail [15].
Subjects and variables
All children living in Denmark aged 29 days to 17 years and 364 days were included from 2015 to 2021. Data on migration and death were adjusted for each year on the 31st of December the previous year until 2019. Migration data after 2019 was not available at the time of the study, but the yearly migration numbers were so small in Denmark that it was considered to not affect results.
Nationwide emergency hospital events were used as an inclusion criterion, and all planned admissions and outpatient contacts were excluded. Hospital events included both short visits for assessment and longer stays in the hospital. Multiple events for one child were accepted to assess hospital burden, but only the first contact in each day for the same patient was included. Multiple observations for a series of overlapping hospital events were considered as one and combined as one in-date and one out-date. Overlapping events could occur when children were transferred between hospitals, e.g., to a tertiary center for more intensive care and then transferred back to a secondary hospital.
Main outcomes were ICD-10 diagnoses for infectious diseases and diseases triggered by infections and were chosen as presented in Online Table 1.
Statistical analysis
Descriptive data was calculated for each year. Data was stratified by sex and age groups. Age groups were defined as < 1, 1–2, 3–5, 6–14, and 15–17 years. The chi-squared test was used on weekly and yearly events comparing calendar-years; 2021 and 2020 to the mean of pre-pandemic years 2015–2019 and Poisson regression was done comparing differences between sexes in 2019–2021.
Weekly rates of events per 100,000 children were calculated for each calendar-year. Rates for weekly total events (total events, including all primary ICD-10 diagnoses in children and adolescents), weekly rates for infection diagnoses (infection events, including primary ICD-10 diagnoses for bacterial, viral, parasitic, and fungal infections in children and adolescents), and weekly rates for each predefined condition (ICD-10 diagnoses for asthma, asthmatic bronchitis (AB), RSV, UTI, gastrointestinal infections (GI), pneumonia and meningitis/encephalitis, sepsis and osteoarticular infections combined as (SI)) were plotted in figures for each calendar-year and specifically for 2020–2021 with a clear marking of time of lockdown and time of reopening/reunion in Denmark. Reopening markings were shown when specifically, schools were reopened. Weekly events < 4 were all adjusted to equal 4 in the figures to adhere to the data anonymity requirements from Statistics Denmark. Data management and statistical analysis were performed using R, v. 4.0.3 [16].
The political definition of Lockdown and reopening in Denmark is presented in Online Supplements.
Results
In total, 2,640,942 hospital events were recorded during the study period (2015–2021); 1,417,571 (53.7%) boys and 1,223,371 (46.3%) girls. In 2020 and 2021, there were 187,771 (53.6%) and 195,069 (53.9%) events respectively for boys and 162,278 (46.4%) and 166,550 (46.3%) events respectively for girls. Total events in year 2020 and 2021 were significantly lower compared to 2015–2019, P < 0.001.
Infection events in total and stratified by sex and predefined condition in calendar-years 2015–2021 are presented in Table 1. Notably, infection events in calendar-years 2020 and 2021 were lower in total and for boys and girls compared to pre-pandemic years (P < 0.001). In all calendar-years, there were more events for boys than for girls by around 5000–6000.
Table 1.
Total infection hospital emergency encounter events for children stratified by sex and selected predefined condition in 2015–2021
| Variables | Levels | Calendar-Years | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | |||
| Total Infections | 74,739 | 79,365 | 79,874 | 74,958 | 77,495 | 49,978 | 66,161 | 502,570 | |
| Sex | Male | 40,930 (54.8) | 43,444 (54.7) | 43,638 (54.6) | 41,012 (54.7) | 42,471 (54.8) | 27,638 (55.3) | 36,783 (55.6) | 275,916 (54.9) |
| Female | 33,809 (45.2) | 35,921 (45.3) | 36,236 (45.4) | 33,946 (45.3) | 35,024 (45.2) | 22,340 (44.7) | 29,378 (44.4) | 226,654 (45.1) | |
| Condition | URTI | 29,663 (39.7) | 30,863 (38.9) | 32,610 (40.8) | 31,546 (42.1) | 33,172 (42.8) | 22,993 (46.0) | 26,555 (40.1) | 207,402 (41.3) |
| Pneumonia | 6842 (9.2) | 7173 (9.0) | 5848 (7.3) | 4754 (6.3) | 4621 (6.0) | 2107 (4.2) | 3237 (4.9) | 34,582 (6.9) | |
| Skin | 5690 (7.6) | 5780 (7.3) | 6447 (8.1) | 5860 (7.8) | 5669 (7.3) | 4451 (8.9) | 4332 (6.5) | 38,229 (7.6) | |
| SI | 887 (1.2) | 860 (1.1) | 854 (1.1) | 790 (1.1) | 680 (0.9) | 514 (1.0) | 518 (0.8) | 5103 (1.0) | |
| Asthma | 4426 (5.9) | 4691 (5.9) | 3646 (4.6) | 3063 (4.1) | 3628 (4.7) | 2949 (5.9) | 3289 (5.0) | 25,692 (5.1) | |
| UTI | 2123 (2.8) | 2104 (2.7) | 2190 (2.7) | 2204 (2.9) | 2075 (2.7) | 2137 (4.3) | 2058 (3.1) | 14,891 (3.0) | |
| GI | 7987 (10.7) | 8058 (10.2) | 8594 (10.8) | 7929 (10.6) | 9302 (12.0) | 3575 (7.2) | 6596 (10.0) | 52,041 (10.4) | |
| Eye | 1408 (1.9) | 3538 (4.5) | 4425 (5.5) | 3963 (5.3) | 3342 (4.3) | 1520 (3.0) | 2338 (3.5) | 20,534 (4.1) | |
| Ear | 7596 (10.2) | 7223 (9.1) | 7776 (9.7) | 7169 (9.6) | 7038 (9.1) | 4552 (9.1) | 5418 (8.2) | 46,772 (9.3) | |
| AB | 5339 (7.1) | 6017 (7.6) | 4905 (6.1) | 4705 (6.3) | 4617 (6.0) | 3020 (6.0) | 5024 (7.6) | 33,627 (6.7) | |
| RSV | 2277 (3.0) | 2703 (3.4) | 2273 (2.8) | 2724 (3.6) | 3084 (4.0) | 1676 (3.4) | 5723 (8.7) | 20,460 (4.1) | |
| COVID-19 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 186 (0.4) | 773 (1.2) | 959 (0.2) | |
| IBD | 501 (0.7) | 355 (0.4) | 306 (0.4) | 251 (0.3) | 267 (0.3) | 298 (0.6) | 300 (0.5) | 2278 (0.5) | |
URTI Upper respiratory tract infections, Skin skin infections, Eye eye infections, Ear ear infections, IBD inflammatory bowel disease, AB asthmatic bronchitis, RSV respiratory syncytial virus, UTI urinary tract infections, GI gastrointestinal infections and SI meningitis/encephalitis, sepsis, and osteoarticular infections combined.
Total pediatric emergency hospital events and infection events
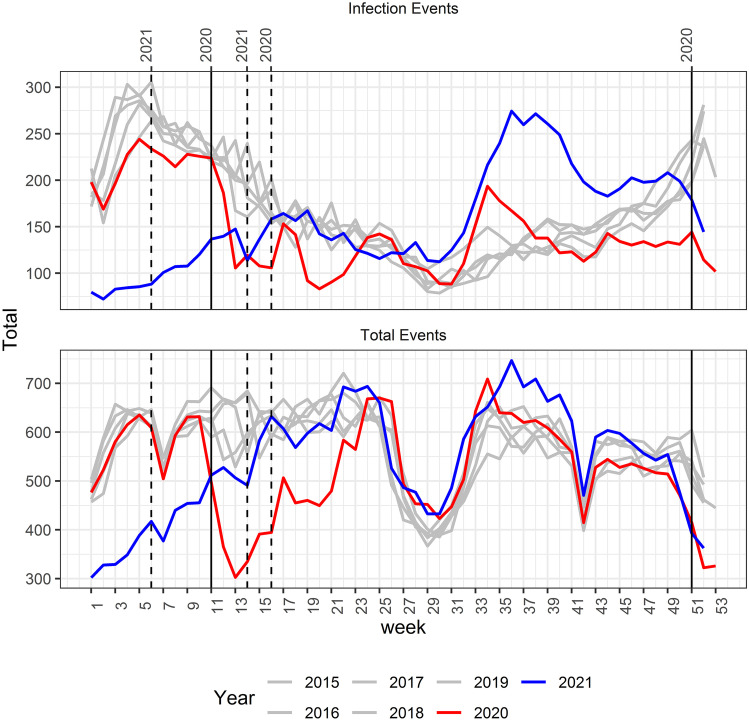
All emergency hospital events in years 2015–2021 are displayed in Fig. 1 and show similar trends and patterns for years 2015–2019.
Fig. 1.
Infection hospital emergency event rates and total weekly hospital emergency event rates for children and adolescents during 2015–2021. Solid lines marking lockdowns. Dotted lines marking reopenings. Specifically, school reopenings are marked
In calendar-year 2020, Fig. 1 shows the year started off in the winter with event rates following those of pre-pandemic years but around week 11 total event (P < 0.001) rates and infection events (P < 0.001) fell drastically and reached the lowest level in week 13 (total P < 0.001 and infection P < 0.001). From there, the curve rose again to around week 24 from where events (infection and total) largely followed the patterns of pre-pandemic years. After week 45, 2020 infection event rates stayed around the same level while previous calendar-years’ rates rose gradually.
Figure 1 shows that the year 2021 began with low rates, around half those of the previous calendar-years in total (week 1 P < 0.001) and infection (week 1 P < 0.001) events, then slowly increased during the spring to around week 15. From then, the curve for 2021 followed trends of pre-pandemic years until week 32–34 where we observed a rise in events most dramatic in the infection events curve (P < 0.001 for weeks 32–34). After week 41, the total events curve returned to following pre-pandemic patterns.
All RTI event rates during 2015–2021 are shown in Online Figure 3.
Infection events stratified by sex and age
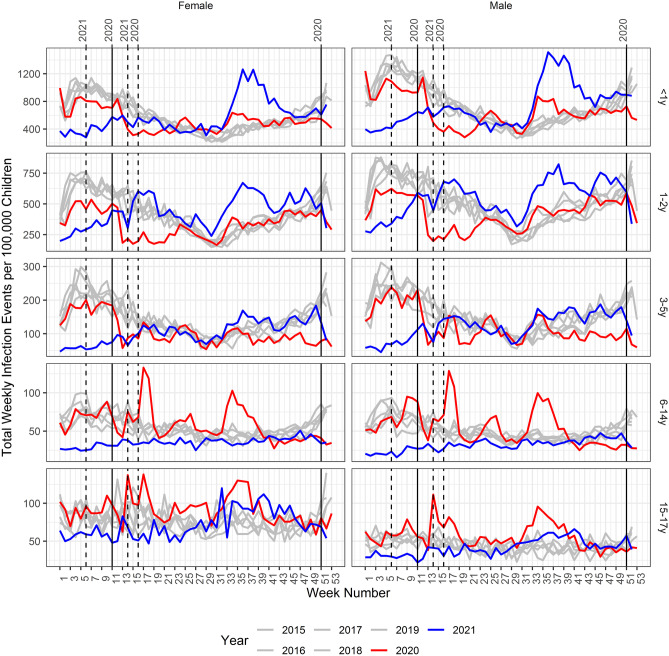
Figure 2 shows infection event rates in years 2015–2021 stratified by sex and age groups. In pre-pandemic years, event rates were the highest in < 1-year-old children with rates up to 1400/100,000 in the winter for boys. Event rates were lowest in 6–14-year-olds and in the 15–17-year-old boys’ group with rates only reaching 25–50/100,000 in pre-pandemic years in the summer. The seasonal trend seemed to be more expressed in up to the 6–14 years’ groups. There were higher event rates for boys up to 3–5 years, and then, it looked like boys’ and girls’ events were equal in the 6–14 years group. There were higher event rates for girls in 15–17-year-olds.
Fig. 2.
Total weekly infections hospital emergency events stratified by sex and age group in years 2015–2021. Solid lines marking lockdowns and dotted lines marking reopenings. Specifically, school reopenings are marked
Lockdown in 2020 reduced infection rates most for children up to 5 years old and had least effect on events for 15–17-year-olds. Reopening in 2020 resulted in spikes most obvious in 3–14-year-olds. Another spike in events was observed in 2020 mostly for the 6–17-year-olds in week 34.
Lockdown in 2021 had an effect for all groups apart from the last with 15–17-year-olds. Reopening in 2021 resulted in curves following the same trends as pre-pandemic years in all groups apart from < 1 to 2-year-olds (P = 0.005) where there was a rise in event rates to around 1400/100,000 for boys < 1 year in week 34 and to 750/100,000 for boys 1–2 years old in week 34. Similar patterns were observed for girls in these age groups.
Selected predefined events
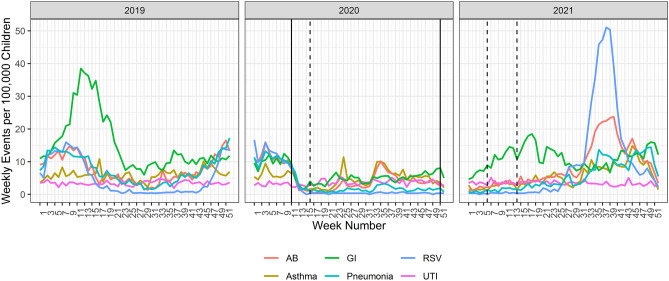
Figure 3 presents graphs for each predefined condition’s event rate in 2020. The calendar-year started off with high event rates for GI’s (13/100,000) and respiratory illnesses like pneumonia (13/100,000), AB (> 15/100,000), asthma (9/100,000), and RSV infection (> 15/100,000) and in week 13 which was 2 weeks after lockdown the rates decreased to around 3 cases per 100,000. There were spikes in asthma cases in week 25 and spikes in both asthma and AB in weeks 33–44. UTI’s stayed on the same levels around 4/100,000 the entire calendar-year.
Fig. 3.
Weekly infectious hospital emergency event rates for selected predefined infection events for children and adolescents during 2019, 2020, and 2021. GI is gastroenteritis. RSV is respiratory syncytial virus. AB is asthmatic bronchitis. UTI is urinary tract infection. Solid lines are marking lockdowns. Dotted lines are marking reopenings
Figure 3 also depicts predefined conditions’ event rates for the calendar-year 2021. Here, GI event rates increased from around 5/100,000 to reach a peak around week 18 of 18/100,000 then declined again to 7/100,000 by week 30. By the end of the calendar-year, there was another peak in GI events of about 15/100,000. The curve for RSV showed rates around zero in the beginning of the calendar-year that increased from week 25 to reach rates around 50/100,000 by week 38. The remaining conditions’ rates seemed to increase gradually after the first and second reopening. AB mirrors the RSV spike and tops in week 35–40 with around 23/100,000 events per week.
Comparatively, Fig. 3 also has rates for the most common conditions in 2019 that showed a rise in GI events weeks 3–24 with rates reaching more than 35/100,000 per week in the peak. The respiratory illnesses in 2019 showed the same levels in the beginning of the calendar-year, but there was a slower decline in cases for pneumonia, RSV infection, and AB whereas asthma rates stayed under 12/100,000 the whole calendar-year. From week 43, there was an increase in rates for airway infections for the rest of 2019 that was not seen in the winter of years 2020 or 2021.
A difference was found for all respiratory illnesses in week 43 between the average admission of years 2015–2019 and years 2020 and 2021 respectively (P < 0.001).
Figures for years 2021, 2020, and 2019 were done (Online supplements) for the rarest conditions (Inflammatory bowel disease, COVID-19, and SI) and weekly rates stayed constant around 0–2 cases per 100,000 for all three calendar-years. In 2021, there was a rise in COVID-19 events to around 11/100,000 per week.
Discussion
This nationwide register–based observational study explored all Danish pediatric emergency hospital events in total and in particular events due to infections and diseases triggered by infections, during and after lockdown (week 11–16 in 2020 and week 50 in 2020 to weeks 6 and 14 in 2021), compared to trends in pre-pandemic years (2015–2019). Before the pandemic, there was a seasonal trend in hospital events showing higher rates during winter times and lower rates in the summer especially for respiratory tract diseases. During the pandemic (2020–2021) and shortly after major lockdowns, there was a trend of decreasing event rates that flared up to normal patterns shortly after reopening of schools (week 16 in 2020 and weeks 6 and 14 in 2021) in total and in infection events. Lockdowns and reopenings resulted in out of season surges in RTIs like RSV infection most likely due to non-stable immunization of susceptible hosts. Boys were more likely to have infection events than girls until age 6–14 where older girls were more likely to have infection events. Upper respiratory tract infections (URTI)/viral infections seemed to be responsible for most pediatric event trends during the study period. Bacterial infections, aside from pneumonia, had a constant rate throughout all calendar-years.
Trends in pre-pandemic years
In this study, there was a trend of less overall hospitalization events during the summer holidays in Denmark. There was also a clear trend of seasonal variations in RTIs and pulmonary diseases like asthma and AB event rates in pre-pandemic years. This is a well-known trend in Denmark as well as in other countries [4–7, 17, 18].
Lockdown and reopening effects on total and infection events
Event rates/hospitalizations were largely affected by lockdowns in 2020. As expected, rates decreased shortly after schools were closed (week 11). The effect appeared stronger in the total events graph, but this graph included all injuries and psychiatric events as well that were affected by lockdowns and reopenings [19]. Lockdowns also reduced hospitalizations in the USA especially for communicable diseases like RTIs [20]. URTIs were by far the most common in this study as in other studies [4].
We found a definite effect of lockdown on infection rates which was also found by others [12, 20, 21]. The infection rate stayed steady during late autumn and winter and did not increase like previous calendar-years. This could be explained by hand washing, social distance, sanitizing surfaces, being more outside, children playing in small groups that did not mix, etc. as was recommended by the government. A modest effect of handwashing and an effect of sanitizing objects and surfaces was found [10, 11]. Social distance in addition to other measures showed reduced contact and therefore reduced incidence of COVID-19 [12].
Infection rate in year 2021 started to increase right after the first reopening where students in 1st-4th grade were back in school and accelerated after the second reopening where all remaining students were 50% back in school (Online Fig. 2). Event rates began following trends of pre-pandemic years just 2 weeks after reopening. Other countries also observed returns to normal patterns immediately after reopenings [22].
Infection events in year 2021 increased drastically from week 32 (Summer) to heights not seen before. Figure 2 shows that the most affected group was children < 1 years and then children 1–2 years. Children < 1 years old were probably not immunized slowly since birth during 2020 where infection rates were unusually low, and when they were exposed to these unknown viruses, they started getting ill over a very short period [23]. Another explanation could be simply their age, as children < 1 year are more at risk of hospitalization because of infectious disease than older children [5, 24]. RSV infection and AB were mostly responsible for the surge in events (Fig. 3). Here, we could theorize that the group of children 1–2 years old were those likely admitted because of AB and children < 1 year old were more likely affected by RSV infection which has been observed before [25].
Most of the year 2021 after reopening, apart from the surge in the late summer, followed the curve of pre-pandemic years where in 2020 events stayed steady. A report from the same period in Denmark showed that people stopped upholding other measures of transmission control as strictly as in the beginning of the pandemic [26].
Events stratified by sex
Events were in general higher for boys than girls in all calendar-years as shown in other studies in Denmark (1997–2015) although that difference disappeared in older children [4, 7]. Suggested explanations for this are differences in immunity response and/or differences in anatomical build, e.g., it has been shown that pre-pubertal boys have smaller airways than girls [27].
Viral/respiratory infections and infection triggered conditions
Effects of lockdown were also apparent in the curves for our predefined conditions (Fig. 3). GI event rates mostly followed the same trend in year 2020 as other viral infections. There seemed to be a spring outbreak of GI infections in years 2019 and 2021 which has been seen before [5, 28].
In year 2020, it was clear that asthma and AB rates dropped immediately after lockdown in week 11 then spiked probably as a result of the grass pollen season and the after school holiday reunion in the spring and summer respectively. In year 2021 though, events rose gradually after the first and second reopenings to peak in week 45 for asthma and week 40 for AB. It is well-known that asthma can be triggered by viral infections and the definition of AB is that it occurs during viral RTIs which explains the increase in event rates following trends of viral infections [29].
There was an unusual surge in RSV infection in the late summer of year 2021. RSV infection season is usually in the winter as seen before [6, 7]. But our results, in congruence with others’, showed that other factors than the season had a larger effect on RSV infection rates’ rising, maybe the host susceptibility to infection either because of no prior immunization and/or low age thus a worse response to infection [23, 30, 31].
Viral vs. bacterial infections
Other bacterial infections than pneumonia did not fluctuate seasonally in our data. We did not show any pattern changes in rates between pre-pandemic and pandemic years. This might be explained by transmission ways as studies have shown that unknown host factors rather than exposure account for most of the risk of infection in children [5]. In the USA, declines in emergency hospital visits were observed in 2020 for septicemia and UTI’s compared to the same period in 2019 [20]. This could propose the question that fear of contagion might have kept people away from the hospital more in the USA than in Denmark [32]. Pneumonia showed a more seasonal trend like other RTIs which might be because children mostly have viral pneumonia or opportunistic bacterial pneumonias because of viral infections [33].
Strengths and limitations
This study included all children hospital emergency contacts in Denmark which minimized selection bias. The study period was long as we included observations for 2 calendar-years (2020–2021) of the COVID-19 pandemic compared with 5 calendar-years before (2015–2019). This helped to validate the data and highlighted strong trends that were not affected by small periods of change. Using rates for events calculated per 100,000, allowed for comparing results to other studies in smaller/larger populations.
A limitation is that details on hospitalizations were not available in the registers. This allowed for examining overall trends but slight changes in rates were not explained. Migration data for 2020–2021 was not available, so there might be a slight overestimation of rates in these calendar-years as migration was adjusted for previous calendar-years. During the pandemic, some pediatric emergency departments used telemedicine to evaluate patients’ need for a hospital visit. This might have prevented more hospital events and an underestimation of our event rates as telemedicine events were not included.
Conclusion
Generally, there was a seasonal fluctuation of infections with more infections during the winter. Lockdowns were an effective measure to bring down emergency infection rates and had a period lasting effect, but reopenings made for an instant return to regular infection patterns. RTIs and/or viral infections were seasonal in pre-pandemic years, but other types of infections did not follow a seasonal trend. Lockdowns and reopenings disrupted seasonal trends of respiratory infections like RSV infections resulting in large surges of infections out of season most likely due to unsteady immunization.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The Nordsjaellands Hospital Research Found: Section for Infectious Diseases.
Abbreviations
- AB
Asthmatic bronchitis
- COVID-19
Coronavirus disease
- GI
Gastrointestinal infections
- ICD-10
International Statistical Classification of Diseases and Related Health Problems, 10th Revision
- SI
Meningitis/encephalitis, sepsis, and osteoarticular infections combined
- RSV
Respiratory syncytial virus
- RTI
Respiratory tract infections
- Events
Short and long pediatric emergency hospitalization contacts
- URTI
Upper respiratory tract infections
- UTI
Urinary tract infections
Authors' contribution
All authors contributed to the study conception and design. Data access was provided by Statistics Denmark through Christian Torp-Pedersen and Mikkel Porsborg Andersen. Data cleaning and analysis were performed by Elisabeth Helen Anna Mills and Rada Faris Al-Jwadi. The first draft of the manuscript was written by Rada Faris Al-Jwadi, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Author Rada Faris Al-Jwadi has received funding from The Nordsjaellands Hospital Research Found: Section for Infectious Diseases.
Declarations
Ethics approval
In Denmark, retrospective register–based studies conducted for the purpose of statistics and scientific research do not require patient consent or ethical approval by law [34]. The project was approved by the data responsible institute in the Capital Region of Denmark reference number P-2019–191.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.GBD 2017 Child and Adolescent Health Collaborators, Reiner RC Jr, Olsen HE, Ikeda CT, Echko MM, Ballestreros KE, Manguerra H, Martopullo I, Millear A, Shields C, Smith A, Strub B, Abebe M, Abebe Z, Adhena BM, Adhikari TB, Akibu M, Al-Raddadi RM, Alvis-Guz KN (2019) Diseases, injuries, and risk factors in child and adolescent health, 1990 to 2017: findings from the global burden of diseases, injuries, and risk factors 2017 study. JAMA Pediatr 173:e190337. 10.1001/jamapediatrics.2019.0337 [DOI] [PMC free article] [PubMed]
- 2.Toivonen L, Karppinen S, Schuez-Havupalo L, Teros-Jaakkola T, Vuononvirta J, Mertsola J, He Q, Waris M, Peltola V. Burden of recurrent respiratory tract infections in children: a prospective cohort study. Pediatr Infect Dis J. 2016;35:e362–e369. doi: 10.1097/INF.0000000000001304. [DOI] [PubMed] [Google Scholar]
- 3.Moe N, Stenseng IH, Krokstad S, Christensen A, Skanke LH, Risnes KR, Nordbø SA, Døllner H. The burden of human metapneumovirus and respiratory syncytial virus infections in hospitalized Norwegian children. J Infect Dis. 2017;216:110–116. doi: 10.1093/infdis/jix262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Larsen JWW, Sørensen AF, Jensen AKG, Poulsen A, Gehrt L, Benn CS, Sørup S. Hospitalizations for infections by age and sex: register-based study of Danish children 1977–2014. Infect Dis (Auckl) 2020;52:97–106. doi: 10.1080/23744235.2019.1682657. [DOI] [PubMed] [Google Scholar]
- 5.Vissing NH, Chawes BL, Rasmussen MA, Bisgaard H (2018) Epidemiology and risk factors of infection in early childhood. Pediatrics 141. 10.1542/peds.2017-0933 [DOI] [PubMed]
- 6.Heikkinen T, Ojala E, Waris M. Clinical and socioeconomic burden of respiratory syncytial virus infection in children. J Infect Dis. 2017;215:17–23. doi: 10.1093/INFDIS/JIW475. [DOI] [PubMed] [Google Scholar]
- 7.Jepsen MT, Trebbien R, Emborg HD, Krause TG, Schønning K, Voldstedlund M, Nielsen J, Fischer TK. Incidence and seasonality of respiratory syncytial virus hospitalisations in young children in Denmark, 2010 to 2015. Eurosurveillance. 2018;23:1. doi: 10.2807/1560-7917.ES.2018.23.3.17-00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rantala AK, Jaakkola MS, Mäkikyrö EMS, Hugg TT, Jaakkola JJK. Early respiratory infections and the development of asthma in the first 27 years of life. Am J Epidemiol. 2015;182:615–623. doi: 10.1093/aje/kwv093. [DOI] [PubMed] [Google Scholar]
- 9.Shaikh N, Morone NE, Bost JE, Farrell MH. Prevalence of urinary tract infection in childhood: a meta-analysis. Pediatr Infect Dis J. 2008;27:302–308. doi: 10.1097/INF.0b013e31815e4122. [DOI] [PubMed] [Google Scholar]
- 10.Jefferson T, Del Mar CB, Dooley L, Ferroni E, Al-Ansary LA, Bawazeer GA, van Driel ML, Jones MA, Thorning S, Beller EM et al (2020) Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev [DOI] [PMC free article] [PubMed]
- 11.Jefferson T, Del Mar CB, Dooley L, Ferroni E, Al-Ansary LA, Bawazeer GA, van Driel ML, Nair NS, Jones MA, Thorning S et al (2011) Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev 2020. 10.1002/14651858.CD006207.pub4 [DOI] [PMC free article] [PubMed]
- 12.Girum T, Lentiro K, Geremew M, Migora B, Shewamare S, Shimbre MS (2021) Optimal strategies for COVID-19 prevention from global evidence achieved through social distancing, stay at home, travel restriction and lockdown: a systematic review. Public Heal Arch 79 [DOI] [PMC free article] [PubMed]
- 13.Pedersen CB. The Danish civil registration system. Scand J Public Health. 2011;39:22–25. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 14.Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sørensen HT. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol. 2011;11:1–6. doi: 10.1186/1471-2288-11-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmidt M, Schmidt SAJ, Adelborg K, Sundbøll J, Laugesen K, Ehrenstein V, Sørensen HT. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563–591. doi: 10.2147/CLEP.S179083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.R Core Team (2017) R: A language and environment for statistical computing. R Found. Stat Comput Vienna, Austria.
- 17.Du Prel JB, Puppe W, Gröndahl B, Knuf M, Weigl JAI, Schaaff F, Schmitt HJ. Are meteorological parameters associated with acute respiratory tract infections? Clin Infect Dis. 2009;49:861–868. doi: 10.1086/605435. [DOI] [PubMed] [Google Scholar]
- 18.Viegas M, Barrero PR, Maffey AF, Mistchenko AS. Respiratory viruses seasonality in children under five years of age in Buenos Aires. Argentina A five-year analysis J Infect. 2004;49:222–228. doi: 10.1016/j.jinf.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 19.Gilmartin S, Barrett M, Bennett M, Begley C, Chroinin CN, O’toole P, Blackburn C (1971) The effect of national public health measures on the characteristics of trauma presentations to a busy paediatric emergency service in Ireland: a longitudinal observational study. Irish J Med Sci 1:3. 10.1007/s11845-021-02593-4 [DOI] [PMC free article] [PubMed]
- 20.Pines JM, Zocchi MS, Black BS, Carlson JN, Celedon P, Moghtaderi A, Venkat A. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am J Emerg Med. 2021;41:201–204. doi: 10.1016/j.ajem.2020.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Polcwiartek LB, Polcwiartek C, Andersen MP, Østergaard L, Broccia MD, Gislason GH, Køber L, Torp-Pedersen C, Schou M, Fosbøl E, et al. Consequences of coronavirus disease-2019 (COVID-19) lockdown on infection-related hospitalizations among the pediatric population in Denmark. Eur J Pediatr. 2021;180:1955–1963. doi: 10.1007/s00431-021-03934-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kuitunen I, Artama M, Haapanen M, Renko M. Rhinovirus spread in children during the COVID-19 pandemic despite social restrictions—a nationwide register study in Finland. J Med Virol. 2021;93:6063–6067. doi: 10.1002/jmv.27180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Di Mattia G, Nenna R, Mancino E, Rizzo V, Pierangeli A, Villani A, Midulla F. During the COVID-19 pandemic where has respiratory syncytial virus gone? Pediatr Pulmonol. 2021;56:3106–3109. doi: 10.1002/ppul.25582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kamper-Jørgensen M, Wohlfahrt J, Simonsen J, Thrane N, Benn CS. Temporal trend in paediatric infections in Denmark. Arch Dis Child. 2006;91:401–404. doi: 10.1136/adc.2005.085787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Wijhe M, Johannesen CK, Simonsen L, Jørgensen IM, Fischer TK (2022) A retrospective cohort study on infant respiratory tract infection hospitalizations and recurrent wheeze and asthma risk: impact of respiratory syncytial virus. J Infect Dis 10.1093/infdis/jiac141 [DOI] [PubMed]
- 26.Bor A (2021) Estimating local protective behavior in Denmark with dynamic MRP- July 6 2021. Available from: https://hope-project.dk/#/reports/estimating_local_protective_behaviour/versions/06-07-2021
- 27.Muenchhoff M, Goulder PJR (2014) Sex differences in pediatric infectious diseases. J Infect Dis 209. 10.1093/infdis/jiu232 [DOI] [PMC free article] [PubMed]
- 28.Schrijver TV, Brand PLP, Bekhof J. Seasonal variation of diseases in children: a 6-year prospective cohort study in a general hospital. Eur J Pediatr. 2016;175:457–464. doi: 10.1007/s00431-015-2653-y. [DOI] [PubMed] [Google Scholar]
- 29.Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2022. Available from: www.ginasthma.org
- 30.Williams TC, Sinha I, Barr IG, Zambon M (2021) Transmission of paediatric respiratory syncytial virus and influenza in the wake of the COVID-19 pandemic. Euro Surveill 26. 10.2807/1560-7917.ES.2021.26.29.2100186 [DOI] [PMC free article] [PubMed]
- 31.Foley DA, Yeoh DK, Minney-Smith CA, Martin AC, Mace AO, Sikazwe CT, Le H, Levy A, Moore HC, Blyth CC. The interseasonal resurgence of respiratory syncytial virus in Australian children following the reduction of coronavirus disease 2019-related public health measures. Clin Infect Dis. 2021;73:E2829–E2830. doi: 10.1093/cid/ciaa1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Macy ML, Smith TL, Cartland J, Golbeck E, Davis MM. Parent-reported hesitancy to seek emergency care for children at the crest of the first wave of COVID-19 in Chicago. Acad Emerg Med. 2021;28:355–358. doi: 10.1111/acem.14214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jain S, Williams DJ, Arnold SR, Ampofo K, Bramley AM, Reed C, Stockmann C, Anderson EJ, Grijalva CG, Self WH, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372:835–845. doi: 10.1056/nejmoa1405870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Andersen MP, Valeri L, Starkopf L, Mortensen RN, Sessa M, Kragholm KH, Vardinghus-Nielsen H, Bøggild H, Lange T, Torp-Pedersen C. The mediating effect of pupils’ physical fitness on the relationship between family socioeconomic status and academic achievement in a Danish school cohort. Sport Med. 2019;49:1291–1301. doi: 10.1007/s40279-019-01117-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.