Abstract
Objectives
To elucidate the risk of cardiovascular event occurrence following Streptococcus pneumoniae infection.
Design
Retrospective cohort study using a LIFE Study database.
Setting
Three municipalities in Japan.
Participants
Municipality residents who were enrolled in either National Health Insurance or the Latter-Stage Elderly Healthcare System from April 2014 to March 2020.
Exposure
Occurrence of S. pneumoniae infection.
Primary outcome measures
Occurrence of one of the following cardiovascular events that led to hospitalisation after S. pneumoniae infection: (1) coronary heart disease (CHD), (2) heart failure (HF), (3) stroke or (4) atrial fibrillation (AF).
Results
S. pneumoniae-infected patients were matched with non-infected patients for each cardiovascular event. We matched 209 infected patients and 43 499 non-infected patients for CHD, 179 infected patients and 44 148 non-infected patients for HF, 221 infected patients and 44 768 non-infected patients for stroke, and 241 infected patients and 39 568 non-infected patients for AF. During follow-up, the incidence rates for the matched infected and non-infected patients were, respectively, 38.6 (95% CI 19.9 to 67.3) and 30.4 (29.1 to 31.8) per 1000 person-years for CHD; 69.6 (41.9 to 108.8) and 50.5 (48.9 to 52.2) per 1000 person-years for HF; 75.4 (48.3 to 112.2) and 35.5 (34.1 to 36.9) per 1000 person-years for stroke; and 34.7 (17.9 to 60.6) and 11.2 (10.4 to 12.0) per 1000 person-years for AF. Infected patients were significantly more likely to develop stroke (adjusted HR: 2.05, 95% CI 1.22 to 3.47; adjusted subdistribution HR: 1.94, 95% CI 1.15 to 3.26) and AF (3.29, 1.49 to 7.26; 2.74, 1.24 to 6.05) than their non-infected counterparts.
Conclusions
S. pneumoniae infections elevate the risk of subsequent stroke and AF occurrence. These findings indicate that pneumococcal infections have short-term effects on patients’ health and increase their midterm to long-term susceptibility to serious cardiovascular events.
Keywords: Epidemiology, Cardiac Epidemiology, EPIDEMIOLOGY
Strengths and limitations of this study.
This study comparatively examined both Streptococcus pneumoniae-infected patients and non-infected controls to elucidate the association between pneumococcal infections and subsequent cardiovascular events.
While prior studies mostly focused on short-term outcomes, our study period spanned from April 2014 to March 2020 to examine the midterm to long-term risks of cardiovascular events following pneumococcal infection.
Despite a relatively large study sample and long study period, S. pneumoniae infections and cardiovascular events were identified using only diagnosis codes in the claims data.
Our study did not account for patients’ lifestyle factors (eg, tobacco and alcohol consumption), socioeconomic factors or pneumococcal vaccination statuses.
Introduction
Community-acquired pneumonia is a major infectious disease that frequently leads to hospitalisation and exhibits high morbidity and mortality rates across numerous countries.1 2 Streptococcus pneumoniae is the causal pathogen for a large proportion of pneumonia cases that require hospital-based care.3 As older persons are more susceptible to pneumococcal pneumonia,4 this condition represents a particularly serious public health problem in countries with ageing populations. In addition to its acute effects, pneumonia is also known to increase the midterm to long-term health risks of infected patients, thereby placing a heavy clinical and economic burden on patients and society.2 5
Previous cohort studies have reported that pneumonia is associated with an increased risk of the following conditions: overall cardiac events,6–14 acute coronary syndrome,6 8 9 11 12 14–17 heart failure (HF),6 9–14 16 18 atrial fibrillation (AF)6 8–14 16 17 19 20 and stroke.11 12 17 However, the majority of these studies focused on pneumonia patients without comparisons with non-infected controls and generally used relatively short follow-up periods. Furthermore, only a few studies in the existing literature have explored the effects of pneumonia on subsequent cardiovascular disease.7 18 21
In order to accurately evaluate the impact of S. pneumoniae infection on subsequent cardiovascular disease, there is a need for long-term cohort studies that compare infected patients with matched non-infected controls. This study aimed to elucidate the risk of cardiovascular event occurrence following S. pneumoniae infection using administrative claims data acquired from infected and non-infected patients in three Japanese municipalities. The study also examined if these risks differ among age groups.
Methods
Study data
Data were provided by the Longevity Improvement & Fair Evidence (LIFE) Study, which is managed by Kyushu University (Fukuoka, Japan).22 In the LIFE Study, participating municipalities voluntarily provide administrative claims data for research purposes. These claims data are acquired from the municipalities’ residents who are enrolled in either National Health Insurance or the Latter-Stage Elderly Healthcare System, and encompass information on patient characteristics and reimbursement claims for all insurance-covered healthcare provided in the inpatient and outpatient settings. Enrollees in National Health Insurance include the self-employed, agricultural and fishery workers, part-time workers, retirees and their dependents. Enrollees in the Latter-Stage Elderly Healthcare System include residents aged ≥75 years. The number of municipalities participating in the LIFE Study varies over time owing to differences in agreement contracts, with the earliest participant providing data from April 2014. The majority of the participating municipalities provide data from April 2015 onward. As of 2021, the LIFE Study is able to conduct longitudinal studies with 5-year follow-up periods.
For this study, claims data from April 2014 to March 2020 were acquired from insurance enrollees who were residing in three municipalities (residential populations: 58 000, 121 600 and 305 200) in Fukuoka Prefecture. The claims datasets contained records of diagnoses (Japanese diagnosis codes and International Classification of Diseases, 10th revision (ICD-10) codes), dates of treatments and admissions and coexisting conditions. For the coexisting conditions, we analysed the list of comorbidities included in the Charlson comorbidity index using ICD-10 codes recorded in both inpatient and outpatient claims.
Study subjects
First, patients with S. pneumoniae infections were identified through combinations of ICD-10 codes and/or Japanese diagnosis codes developed by the Ministry of Health, Labour and Welfare. We used the combinations of codes proposed by Imai et al.23 In this study, we considered all types of S. pneumoniae infections, including invasive pneumococcal diseases. The occurrence of subsequent cardiovascular events leading to hospitalisation (coronary heart disease (CHD), HF, stroke and AF) was identified using ICD-10 codes. We excluded patients with records of previous in-hospital cardiovascular events from their earliest recorded dates within the observation period until S. pneumoniae infection, patients with records of cardiovascular events during the index hospitalisation for S. pneumoniae infection and patients without any claims data ≥12 months before S. pneumoniae infection.
Next, we set each infected patient’s index date as the last day of the month containing a recorded S. pneumoniae infection. The infected patients were then exactly matched with a cohort of non-infected patients according to age (within 5 years), sex, comorbidities and hospitalisation at the index date using sampling without replacement. The comorbidities included the following conditions: myocardial infarction, congestive HF, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatic disease, peptic ulcer disease, liver disease, diabetes with/without chronic complications, hemiplegia or paraplegia, malignancy, metastatic solid tumour and HIV/AIDS.24 When examining the occurrence of AF after S. pneumoniae infection, we also included the comorbidity of AF as a matching criterion. Infected patients who could not be matched with non-infected patients were excluded. The index date for each non-infected patient was set as the same date as his or her matched infected case. Each patient’s comorbidities were identified using claims data for 30 days before the index date. We also excluded non-infected patients who had experienced cardiovascular events that led to hospitalisation before their index dates.
Outcome measure
The outcome measure was the occurrence of a cardiovascular event that led to hospitalisation after the S. pneumoniae infection date. Among inpatients, the infection date was set as the first date of admission for the in-hospital treatment of an S. pneumoniae infection. Among outpatients, the infection date was set as the first date of any medical treatment with a diagnosis code indicating an S. pneumoniae infection. We focused on the first infection episode for patients who had multiple infection episodes during the observation period.
Next, we examined the subsequent occurrence of each of the following four cardiovascular events that led to hospitalisation: (1) CHD (ICD-10 codes: I20–25), (2) HF (I50), (3) stroke (I61–63, 65–66) and (4) AF (I48). The occurrence date of each cardiovascular event was set as the date of admission for the in-hospital treatment of that event.
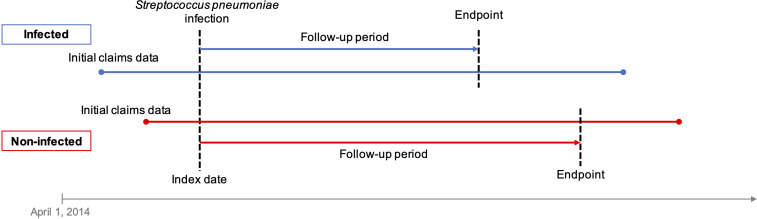
Patients who had died during the observation period without developing any cardiovascular event were followed up until the last date of medical treatments in the claims data. Patients who had died during the observation period after developing a cardiovascular event were followed up until the date of the cardiovascular event occurrence. All survivors were followed up until the end of their municipality’s observation period. The ends of the observation periods ranged from September 2019 to March 2020 among the municipalities. Figure 1 shows an overview of the follow-up process.
Figure 1.
Overview of the follow-up process for Streptococcus pneumoniae-infected and non-infected patients. Endpoints refer to the occurrence of a target cardiovascular event.
Statistical analysis
Our analysis was designed to examine the possible effects of S. pneumoniae infection on the subsequent occurrence of cardiovascular events and to determine if these effects differed among age groups. For each of the four target cardiovascular events, we calculated the number of events for the infected group and non-infected group during the observation period and estimated the incidence rates per 1000 person-years. Cox proportional hazards models were constructed to estimate the HR and 95% CIs of each cardiovascular event in the infected group relative to the non-infected group. Subdistribution HRs were also estimated with Cox proportional hazards models using the Fine-Gray competing risk approach in which death was regarded as a competing event. The Kaplan-Meier method was used to calculate the cumulative probability of cardiovascular event occurrence in the two groups. In addition, we analysed the patients stratified according to the following age groups: 0–49 years, 50–64 years and ≥65 years.
All statistical analyses were performed using R (V.4.1.0) and R Studio (V.1.4.1106) software. Two-tailed p values below 0.05 were considered statistically significant.
Patient and public involvement
Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Results
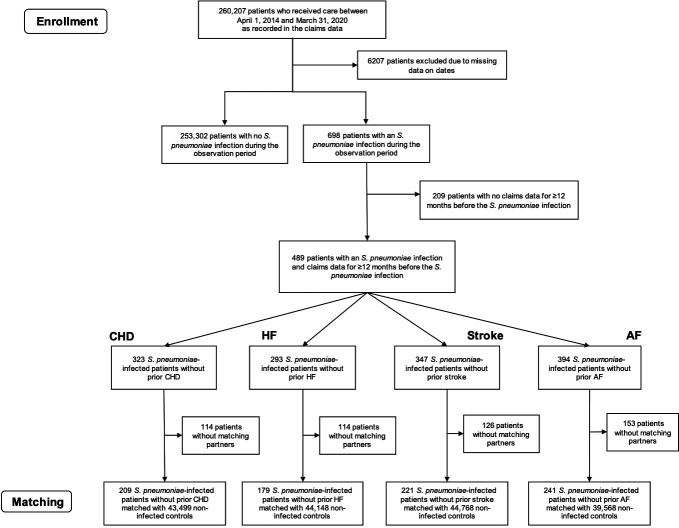
We first identified 698 S. pneumoniae-infected patients and 253 302 non-infected patients between 1 April 2014 and 31 March 2020 (figure 2). After applying the exclusion criteria, 489 eligible infected patients were included in the analysis. There were 22 invasive pneumococcal disease cases (4.5%) and 467 non-invasive pneumococcal disease cases (95.5%). Among the infected patients that could be successfully matched with non-infected patients for each cardiovascular event, we identified 209 infected patients without prior CHD, 179 infected patients without prior HF, 221 infected patients without prior stroke and 241 infected patients without prior AF. Using the various matching criteria, we matched 43 499, 44 148, 44 768, and 39 568 non-infected controls with the infected patients for CHD, HF, stroke and AF, respectively. The non-infected patients were followed up from the first S. pneumoniae infection date of their matched infected patients. Table 1 shows the characteristics and comorbidities of the infected and non-infected patients. The covariate balance summaries before and after matching for the target cardiovascular events are presented in online supplemental tables 1–4.
Figure 2.
Selection of Streptococcus pneumoniae-infected and non-infected patients for analysis. Prior CHD, HF, stroke and AF refer only to previous events with in-hospital treatments. AF, atrial fibrillation; CHD, coronary heart disease; HF, heart failure.
Table 1.
Characteristics and comorbidities of Streptococcus pneumoniae-infected and non-infected patients
| CHD | HF | Stroke | AF | |||||
| Non-infected | Infected | Non-infected | Infected | Non-infected | Infected | Non-infected | Infected | |
| N | 43 499 | 209 | 44 148 | 179 | 44 768 | 221 | 39 568 | 241 |
| Cardiovascular event incidence | 2090 (4.8%) | 12 (5.7%) | 3790 (8.6%) | 19 (11%) | 2502 (5.6%) | 24 (11%) | 703 (1.8%) | 12 (5.0%) |
| Age, mean (y) | 77.0 | 77.1 | 75.4 | 75.6 | 77.5 | 77.7 | 77.5 | 77.7 |
| Men | 22 062 (51%) | 106 (51%) | 24 417 (55%) | 99 (55%) | 22 890 (51%) | 113 (51%) | 20 523 (52%) | 125 (52%) |
| Women | 21 437 (49%) | 103 (49%) | 19 731 (45%) | 80 (45%) | 21 878 (49%) | 108 (49%) | 19 045 (48%) | 116 (48%) |
| Hospital admission | 30 595 (70%) | 147 (70%) | 29 103 (66%) | 118 (66%) | 31 804 (71%) | 157 (71%) | 29 224 (74%) | 178 (74%) |
| Myocardial infarction | 0 (0%) | 0 (0%) | 247 (0.6%) | 1 (0.6%) | 203 (0.5%) | 1 (0.5%) | 164 (0.4%) | 1 (0.4%) |
| Congestive heart failure | 4787 (11%) | 23 (11%) | 987 (2.2%) | 4 (2.2%) | 4051 (9.0%) | 20 (9.0%) | 4433 (11%) | 27 (11%) |
| Peripheral vascular disease | 1249 (2.9%) | 6 (2.9%) | 1233 (2.8%) | 5 (2.8%) | 1418 (3.2%) | 7 (3.2%) | 1149 (2.9%) | 7 (2.9%) |
| Cerebrovascular disease | 6036 (14%) | 29 (14%) | 5179 (12%) | 21 (12%) | 4254 (9.5%) | 21 (9.5%) | 5254 (13%) | 32 (13%) |
| Dementia | 6244 (14%) | 30 (14%) | 4933 (11%) | 20 (11%) | 5267 (12%) | 26 (12%) | 4761 (12%) | 29 (12%) |
| Chronic pulmonary disease | 12 488 (29%) | 60 (29%) | 14 305 (32%) | 58 (32%) | 12 762 (29%) | 63 (29%) | 11 000 (28%) | 67 (28%) |
| Rheumatic disease | 624 (1.4%) | 3 (1.4%) | 1233 (2.8%) | 5 (2.8%) | 810 (1.8%) | 4 (1.8%) | 985 (2.5%) | 6 (2.5%) |
| Peptic ulcer disease | 2914 (6.7%) | 14 (6.7%) | 3453 (7.8%) | 14 (7.8%) | 2633 (5.9%) | 13 (5.9%) | 2134 (5.4%) | 13 (5.4%) |
| Mild liver disease | 6868 (16%) | 33 (16%) | 7399 (17%) | 30 (17%) | 6685 (15%) | 33 (15%) | 4925 (12%) | 30 (12%) |
| Diabetes without chronic complications | 624 (1.4%) | 3 (1.4%) | 493 (1.1%) | 2 (1.1%) | 405 (0.9%) | 2 (0.9%) | 328 (0.8%) | 2 (0.8%) |
| Diabetes with chronic complications | 1249 (2.9%) | 6 (2.9%) | 1726 (3.9%) | 7 (3.9%) | 1215 (2.7%) | 6 (2.7%) | 1149 (2.9%) | 7 (2.9%) |
| Haemiplegia or paraplegia | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Renal disease | 416 (1.0%) | 2 (1.0%) | 493 (1.1%) | 2 (1.1%) | 810 (1.8%) | 4 (1.8%) | 657 (1.7%) | 4 (1.7%) |
| Malignancy | 3538 (8.1%) | 17 (8.1%) | 4686 (11%) | 19 (11%) | 4051 (9.0%) | 20 (9.0%) | 3284 (8.3%) | 20 (8.3%) |
| Moderate or severe liver disease | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Metastatic solid tumour | 833 (1.9%) | 4 (1.9%) | 987 (2.2%) | 4 (2.2%) | 608 (1.4%) | 3 (1.4%) | 657 (1.7%) | 4 (1.7%) |
| HIV/AIDS | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| AF | 328 (0.8%) | 2 (0.8%) | ||||||
Values are presented as number (percentage) unless stated otherwise.
AF, atrial fibrillation; CHD, coronary heart disease; HF, heart failure.
bmjopen-2021-059713supp001.pdf (84.2KB, pdf)
Table 2 summarises the risk of each cardiovascular event after S. pneumoniae infection. The observation periods of the matched infected and non-infected patients (weighted by the proportion of the infected patients) were, respectively, 311 and 68 706 person-years for CHD; 273 and 74 999 person-years for HF; 318 and 70 454 person-years for stroke; and 346 and 62 986 person-years for AF. The median observation periods of the matched infected and non-infected patients were 823 days for CHD, 827 days for HF, 820 days for stroke and 797 days for AF. During follow-up, the incidence rates for the infected and non-infected patients were, respectively, 38.6 (95% CI 19.9 to 67.3) and 30.4 (95% CI 29.1 to 31.8) per 1000 person-years for CHD; 69.6 (95% CI 41.9 to 108.8) and 50.5 (95% CI 48.9 to 52.2) per 1000 person-years for HF; 75.4 (95% CI 48.3 to 112.2) and 35.5 (95% CI 34.1 to 36.9) per 1000 person-years for stroke; and 34.7 (95% CI17.9 to 60.6) and 11.2 (95% CI 10.4 to 12.0) per 1000 person-years for AF. The unadjusted HRs for cardiovascular event occurrence in infected patients (relative to non-infected patients) were 1.27 (95% CI 95% CI 0.72 to 2.24) for CHD, 1.38 (95% CI 0.88 to 2.16) for HF, 2.12 (95% CI 1.42 to 3.17) for stroke and 3.11 (95% CI 1.76 to 5.50) for AF. After adjusting for age, sex, comorbidities and coexisting AF (only for the outcome of AF), infected patients were significantly more likely to develop stroke (adjusted HR: 2.05, 95% CI 1.22 to 3.47) and AF (adjusted HR: 3.29, 95% CI 1.49 to 7.26) than their non-infected counterparts. When death was regard as a competing event, the adjusted subdistribution HRs were 1.19 (95% CI 0.63 to 2.26) for CHD, 1.13 (0.60 to 2.13) for HF, 1.94 (1.15 to 3.26) for stroke and 2.74 (1.24 to 6.05) for AF. Infected patients were still significantly more likely to develop stroke and AF than their non-infected counterparts.
Table 2.
Cardiovascular events in Streptococcus pneumoniae-infected and non-infected patients
| CHD | HF | Stroke | AF | |||||
| Non-infected | Infected | Non-infected | Infected | Non-infected | Infected | Non-infected | Infected | |
| Overall | ||||||||
| N | 43 499 | 209 | 44 148 | 179 | 44 768 | 221 | 39 568 | 241 |
| Incidence, n (%) | 2090 (4.8%) | 12 (5.7%) | 3790 (8.6%) | 19 (11%) | 2502 (5.6%) | 24 (11%) | 703 (1.8%) | 12 (5.0%) |
| Person-years of follow-up | 68 706 | 311 | 74 999 | 273 | 70 454 | 318 | 62 986 | 346 |
| Incidence rate per 1000 person-years (95% CI) | 30.4 (29.1 to 31.8) | 38.6 (19.9 to 67.3) | 50.5 (48.9 to 52.2) | 69.6 (41.9 to 108.8) | 35.5 (34.1 to 36.9) | 75.4 (48.3 to 112.2) | 11.2 (10.4 to 12.0) | 34.7 (17.9 to 60.6) |
| Unadjusted HR (95% CI) | – | 1.27 (0.72 to 2.24) | – | 1.38 (0.88 to 2.16) | – | 2.12 (1.42 to 3.17) | – | 3.11 (1.76 to 5.50) |
| Adjusted HR* (95% CI) | – | 1.20 (0.60 to 2.39) | – | 1.18 (0.58 to 2.37) | – | 2.05 (1.22 to 3.47) | – | 3.29 (1.49 to 7.26) |
| Adjusted subdistribution HR* (95% CI) | – | 1.19 (0.63 to 2.26) | 1.13 (0.60 to 2.13) | 1.94 (1.15 to 3.26) | 2.74 (1.24 to 6.05) | |||
| By age group | ||||||||
| N (%) | ||||||||
| 0–49 years | 1958 (4.5%) | 9 (4.3%) | 2304 (5.2%) | 9 (5.0%) | 1895 (4.2%) | 9 (4.1%) | 1533 (3.9%) | 9 (3.7%) |
| 50–64 years | 3963 (9.1%) | 21 (10%) | 4080 (9.2%) | 18 (10%) | 3620 (8.1%) | 19 (8.6%) | 3305 (8.4%) | 22 (9.1%) |
| ≥65 years | 37 578 (86%) | 179 (86%) | 37 765 (86%) | 152 (85%) | 39 253 (88%) | 193 (87%) | 34 730 (88%) | 210 (87%) |
| Incidence rate per 1000 person-years (95% CI) | ||||||||
| 0–49 years | 8.0 (5.6 to 11.0) | 0 (0 to 200.4) | 15.0 (11.8 to 18.7) | 0 (0 to 200.4) | 3.0 (1.6 to 5.1) | 0 (0 to 200.4) | 1.2 (0.3 to 3.0) | 0 (0 to 200.4) |
| 50–64 years | 5.4 (4.0 to 7.0) | 21.8 (0.6 to 121.5) | 29.4 (26.1 to 33.1) | 24.3 (0.6 to 135.1) | 35.1 (31.3 to 39.3) | 69.7 (14.4 to 203.6) | 6.2 (4.6 to 8.2) | 21.4 (0.5 to 119.2) |
| ≥65 years | 36.7 (35.1 to 38.3) | 44.5 (22.2 to 79.7) | 57.1 (55.2 to 59.0) | 84.4 (50.0 to 133.4) | 38.0 (36.5 to 39.7) | 81.8 (50.6 to 125.0) | 12.6 (11.7 to 13.6) | 39.2 (19.6 to 70.1) |
| Adjusted HR* (95% CI) | ||||||||
| 0–49 years | – | 0 | – | 0 | – | 0 | – | 0 |
| 50–64 years | – | 4.06 (0.56 to 29.38) | – | 0.82 (0.12 to 5.86) | – | 1.98 (0.64 to 6.19) | – | 3.47 (0.48 to 25.02) |
| ≥65 years | – | 1.21 (0.64 to 2.10) | – | 1.48 (0.78 to 1.97) | – | 2.15 (1.29 to 3.04) | – | 3.11 (1.58 to 5.20) |
*Adjusted for age, sex, comorbidities and coexisting AF (only for the outcome of AF).
AF, atrial fibrillation; CHD, coronary heart disease; HF, heart failure.
In the age-stratified analysis, S. pneumonia infections were not significantly associated with a higher risk of the four cardiovascular events in patients aged 50–64 years. Among older patients aged ≥65 years, S. pneumonia infections were significantly associated with substantially higher risks of stroke and AF occurrence.
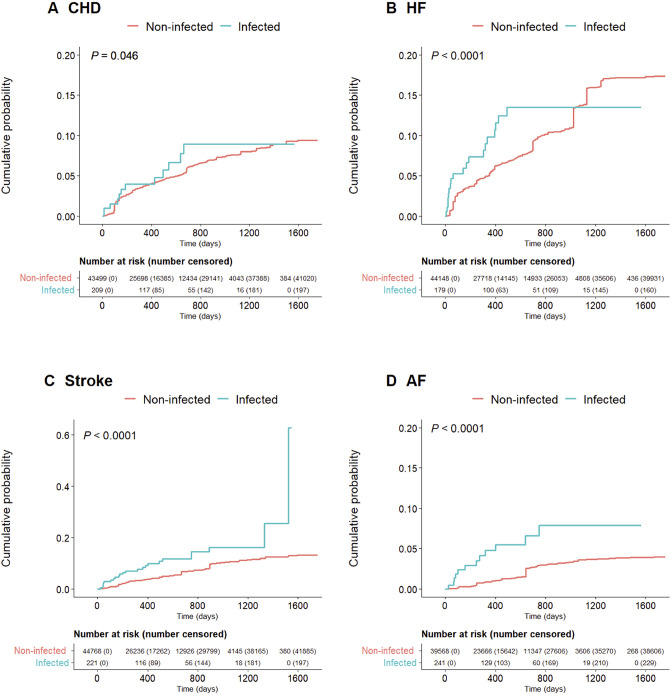
Figure 3 presents the Kaplan-Meier curves of each cardiovascular event. When compared with non-infected patients, infected patients had a significantly higher risk of incident HF, stroke and AF (all p<0.0001) but not CHD (p=0.046).
Figure 3.
Kaplan-Meier estimates for cardiovascular events in Streptococcus pneumoniae-infected and non-infected patients. (A) Coronary heart disease (CHD), (B) heart failure (HF), (C) stroke and (D) atrial fibrillation (AF).
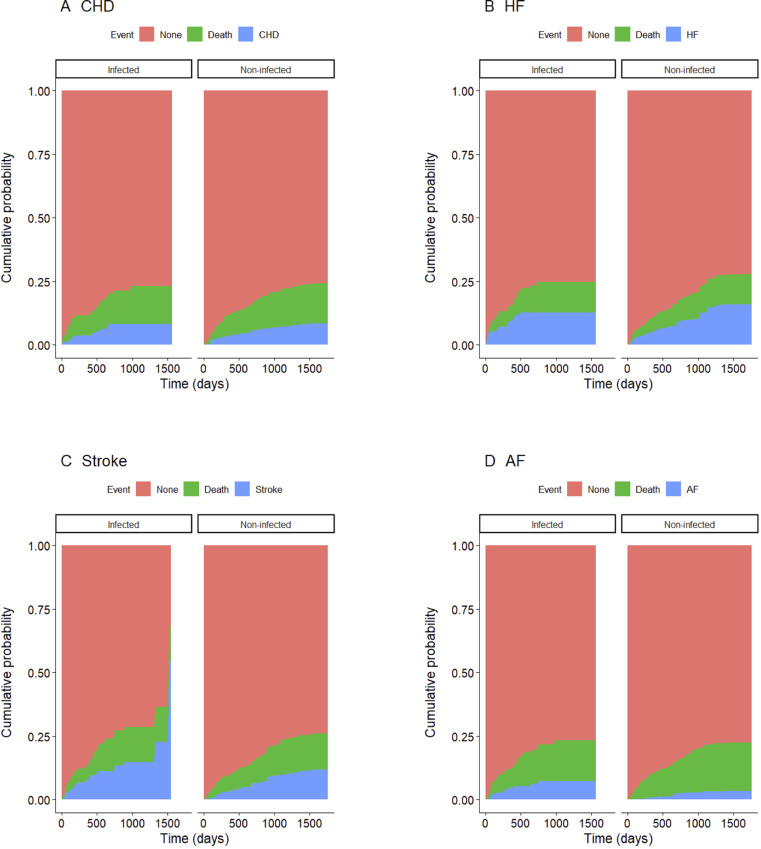
Figure 4 presents the cumulative incidence curves for cardiovascular events where death was regarded as a competing event.
Figure 4.
Cumulative incidence curves for cardiovascular events in Streptococcus pneumoniae-infected and non-infected patients. (A) Coronary heart disease (CHD), (B) heart failure (HF), (C) stroke and (D) atrial fibrillation (AF).
Discussion
Through an analysis of National Health Insurance and Latter-Stage Elderly Healthcare System enrollees residing in three Japanese municipalities, this study comparatively examined the incidence of cardiovascular events leading to hospitalisation between S. pneumoniae-infected patients and non-infected patients. Our results showed that the experience of S. pneumoniae infection significantly elevates the risk of subsequent stroke and AF. S. pneumoniae infection increased the risk of these cardiovascular events among older patients aged ≥65 years. While S. pneumonia infections were not significantly associated with a higher risk of these cardiovascular events in patients aged 50–64 years, the ratios were relatively high and more studies should be conducted. These findings may help to identify at-risk targets for expanded pneumococcal vaccination programmes.
Recent studies have shown that patients with community-acquired pneumonia have a higher frequency of cardiovascular events.8 10 11 16 18 21 25 26 Our estimated incidence of AF after S. pneumoniae infection was 5.0%. The incidence of arrhythmia (ICD-10 codes: I47–49) in this study was estimated to be 9.0%, which is slightly higher than that of a previous meta-analysis that estimated an overall incidence of 7.2% among inpatients with community-acquired pneumonia.25 This discrepancy may be explained by the fact that the meta-analysis had only included studies with short-term outcomes.
In our analysis, the estimated incidence of stroke after S. pneumoniae infection was considerably higher than those found in previous studies.11 16 Perry et al reported a stroke incidence of 0.17% in 40 979 patients during 90 days of admission for pneumonia, whereas Violi et al reported a stroke incidence of 1.0% in 1182 patients hospitalised for community-acquired pneumonia during in-hospital follow-up (median length of hospital stay: 11 days). Accordingly, those two studies had focused on the short-term incidence of stroke. However, the risk of stroke increases with age and longer follow-up periods after S. pneumoniae infection would therefore provide a more accurate depiction of its risks. Furthermore, Perry et al used ICD-9 codes to identify stroke, whereas Violi et al identified stroke cases through clinical manifestations confirmed by CT or MRI.11 16 Stroke diagnostic methods are generally reliant on imaging data, and many medical facilities in Japan are equipped with on-site CT and/or MRI scanners. This enables the accurate diagnosis of stroke, including cases of milder strokes, throughout Japan.
Among the studies that reported a high frequency of subsequent cardiovascular events in pneumonia patients, few have actually compared infected patients with non-infected controls. Eurich et al18 performed a long-term prospective cohort study of both inpatients and outpatients with community-acquired pneumonia and found that these infections substantially increased the risk of HF across different age groups and disease severity. During a median follow-up period of 9.9 years, 11.9% of patients with pneumonia developed incident HF compared with 7.4% of the non-infected controls; furthermore, 13.3% of patients with pneumococcal bacteraemia developed incident HF.18 In contrast, 13.0% of our infected patients developed incident HF compared with 12.0% of their non-infected counterparts, with no significant difference between the groups. This discrepancy may be influenced by the fact that Eurich et al used a control group that only controlled for age (5 year age bands) and sex, only investigated outpatients in emergency departments and focused on severe pneumonia infections. In contrast, our study included outpatients from all types of medical institutions, and our control group comprised patients without any S. pneumoniae infection. Our study also used a research design that differed from Eurich et al,18 which only matched for age and sex, and adjusted for the effects for coexisting conditions by including them as covariates in analytical models. However, we matched infected patients and non-infected controls by age and sex and by comorbidities.
To our knowledge, few studies have shown the long-term risks of subsequent stroke and AF after S. pneumoniae infection (including non-hospitalised cases) relative to non-infected controls. Severe cases of pneumonia require hospital-based care, especially among older adults. Therefore, studies that focus on hospitalised pneumonia patients would overlook the risks associated with less severe cases. For example, although patients aged ≤65 years may have milder S. pneumoniae infections and a correspondingly lower risk of hospitalisation than older patients, these infections could still elevate the risk of subsequent cardiovascular events in the younger age groups. As this study used insurance claims data that incorporated both inpatient and outpatient data, we were able to identify the risk of cardiovascular events after S. pneumoniae infection in patients regardless of whether they required hospitalisation. Moreover, our study excluded patients who had subsequent cardiovascular events during the index hospital stay for S. pneumoniae infection. For patients who were admitted to hospital due to S. pneumoniae infection, we only monitored for cardiovascular events that occurred after discharge. Most studies have reported the short-term risks of cardiovascular events during or after acute infections, and the long-term impact of pneumonia on subsequent cardiovascular disease occurrence is less clear. Therefore, our study provides new insight into the midterm to long-term effects of milder S. pneumoniae infections treated in outpatient settings as well as severe S. pneumoniae infections that require hospitalisation.
A previous study identified the major causative organisms of community-acquired pneumonia to be S. pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, Chlamydophila pneumoniae, Legionella pneumophila, Staphylococcus aureus and several viral pathogens (including influenza A and B).27 S. pneumoniae reportedly reduces cardiac contractility by increasing cardiomyocyte uptake of bacterial cell wall antigens.28 Many studies that seek to understand the pathogenesis of cardiovascular events following pneumonia focus on infections caused by S. pneumoniae.29 Several studies have proposed that S. pneumoniae cell wall components and pneumolysin (a pore-forming toxin) trigger proinflammatory mechanisms that ultimately result in cardiac damage.30–33 Furthermore, the infection-mediated hyperactivation of platelets can create a proinflammatory and prothrombotic environment that facilitates the occurrence of cardiovascular events and cardiac damage.31 Pneumonia and other infections can trigger fever, hypoxia and haemodynamic disturbance in patients, which are all risk factors of AF and its associated cardiac damage.34 In our analysis, S. pneumonia infections were significantly associated with higher risks of stroke and AF but not CHD and HF. These differences may be due to the presence of multiple mechanisms that differentially contribute to each type of cardiovascular event. Further studies are needed to explore these differences in greater depth.
The study limitations are as follows. First, S. pneumoniae infections and cardiovascular events were identified using diagnosis codes and ICD-10 codes, respectively. Therefore, our analysis may be vulnerable to coding errors. Second, our study could not account for patients’ lifestyle factors (eg, tobacco and alcohol consumption), socioeconomic factors or pneumococcal vaccination statuses. In addition, we also could not account for differences in medications and treatments (especially at discharge) among the patients. Third, our study population was limited to enrollees of Japan’s National Health Insurance and Latter-Stage Elderly Healthcare System, and the findings may not be extrapolatable to those enrolled in other insurance systems. Fourth, our study excluded patients with previous in-hospital cardiovascular events. However, the real-world population of patients would include those with such events. This approach could introduce selection bias and affect the comparability of our findings with real-world scenarios. Fifth, we excluded infected patients who were not matched with non-infected controls. With consideration to the relatively low number of infected patients, the exclusion of these non-matched patients could potentially reduce the power of our statistical analyses. Sixth, our study outcomes focused on cardiovascular events that resulted in hospitalisation and did not consider events without in-hospital care. Therefore, our study may overlook the impact of S. pneumoniae infection on subsequent occurrences of mild cardiovascular disease. Seventh, previous outpatient treatments were not included in the analysis, which could result in selection bias. Eighth, the index date for matching was set as the last day of the month with S. pneumoniae infection instead of the claims date, which could result in lead-time bias. Finally, we did not consider the random effects of hospitals or municipalities in our multivariate analyses. Patients treated in the same hospital or municipality may be similar to one another. However, all the study municipalities were located in the same prefecture, and there were no major differences in characteristics at the regional or hospital level. Additionally, pneumonia is a common disease that hospitals regularly treat, and it is unlikely that there would be a large bias at the hospital level.
Conclusion
S. pneumoniae infections elevate the risk of subsequent stroke and AF occurrence. These findings indicate that pneumococcal infections do have short-term effects on patient health and increase the midterm to long-term susceptibility to serious cardiovascular events. With a greater understanding of S. pneumoniae infection’s far-reaching impact, further studies are needed to explore the possible benefits of expanding current pneumococcal vaccination programmes.
Supplementary Material
Footnotes
Contributors: NN and HF designed the study. HF provided the data. NN analysed the data. NN prepared the first draft of the manuscript. HF made critical revisions to the manuscript. All authors reviewed and approved the final draft.
Funding: The construction of the LIFE Study database was funded by a Grant-in-Aid for Scientific Research by the Japan Society for the Promotion of Science (Grant No. JP20H00563). Data analysis and publication were funded by an Investigator-Sponsored Research grant from Pfizer Japan Inc.
Competing interests: HF received an Investigator-Sponsored Research grant from Pfizer Japan Inc.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. The data used in this study were acquired under agreements with the participating municipalities, which stipulate that the data can only be used by authorised research institutions and cannot be shared with third parties.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was approved by the Kyushu University Institutional Review Board for Clinical Research (Approval No. 2021-423).
References
- 1.Trotter CL, Stuart JM, George R, et al. Increasing hospital admissions for pneumonia, England. Emerg Infect Dis 2008;14:727–33. 10.3201/eid1405.071011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eurich DT, Marrie TJ, Minhas-Sandhu JK, et al. Ten-year mortality after community-acquired pneumonia. A prospective cohort. Am J Respir Crit Care Med 2015;192:597–604. 10.1164/rccm.201501-0140OC [DOI] [PubMed] [Google Scholar]
- 3.Musher DM. Streptococcus pneumoniae. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglass and Bennett’s principles and practice of infectious diseases. Philadelphia: Churchill Livingstone, 2005: 2392–411. [Google Scholar]
- 4.Fry AM, Shay DK, Holman RC, et al. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988-2002. JAMA 2005;294:2712–9. 10.1001/jama.294.21.2712 [DOI] [PubMed] [Google Scholar]
- 5.Jasti H, Mortensen EM, Obrosky DS, et al. Causes and risk factors for rehospitalization of patients hospitalized with community-acquired pneumonia. Clin Infect Dis 2008;46:550–6. 10.1086/526526 [DOI] [PubMed] [Google Scholar]
- 6.Postma DF, Spitoni C, van Werkhoven CH, et al. Cardiac events after macrolides or fluoroquinolones in patients hospitalized for community-acquired pneumonia: post-hoc analysis of a cluster-randomized trial. BMC Infect Dis 2019;19:17. 10.1186/s12879-018-3630-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corrales-Medina VF, Alvarez KN, Weissfeld LA, et al. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA 2015;313:264–74. 10.1001/jama.2014.18229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cangemi R, Calvieri C, Falcone M, et al. Relation of cardiac complications in the early phase of community-acquired pneumonia to long-term mortality and cardiovascular events. Am J Cardiol 2015;116:647–51. 10.1016/j.amjcard.2015.05.028 [DOI] [PubMed] [Google Scholar]
- 9.Griffin AT, Wiemken TL, Arnold FW. Risk factors for cardiovascular events in hospitalized patients with community-acquired pneumonia. Int J Infect Dis 2013;17:e1125–9. 10.1016/j.ijid.2013.07.005 [DOI] [PubMed] [Google Scholar]
- 10.Corrales-Medina VF, Musher DM, Wells GA, et al. Cardiac complications in patients with community-acquired pneumonia: incidence, timing, risk factors, and association with short-term mortality. Circulation 2012;125:773–81. 10.1161/CIRCULATIONAHA.111.040766 [DOI] [PubMed] [Google Scholar]
- 11.Violi F, Cangemi R, Falcone M, et al. Cardiovascular complications and short-term mortality risk in community-acquired pneumonia. Clin Infect Dis 2017;64:1486–93. 10.1093/cid/cix164 [DOI] [PubMed] [Google Scholar]
- 12.Aliberti S, Ramirez J, Cosentini R, et al. Acute myocardial infarction versus other cardiovascular events in community-acquired pneumonia. ERJ Open Res 2015;1:00020-2015. 10.1183/23120541.00020-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Viasus D, Garcia-Vidal C, Manresa F, et al. Risk stratification and prognosis of acute cardiac events in hospitalized adults with community-acquired pneumonia. J Infect 2013;66:27–33. 10.1016/j.jinf.2012.09.003 [DOI] [PubMed] [Google Scholar]
- 14.Cilli A, Cakin O, Aksoy E, et al. Acute cardiac events in severe community-acquired pneumonia: a multicenter study. Clin Respir J 2018;12:2212–9. 10.1111/crj.12791 [DOI] [PubMed] [Google Scholar]
- 15.Chen P-C, Liao W-I, Wang Y-C, et al. An elevated glycemic gap is associated with adverse outcomes in diabetic patients with community-acquired pneumonia. Medicine 2015;94:e1456. 10.1097/MD.0000000000001456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perry TW, Pugh MJV, Waterer GW, et al. Incidence of cardiovascular events after hospital admission for pneumonia. Am J Med 2011;124:244–51. 10.1016/j.amjmed.2010.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mandal P, Chalmers JD, Choudhury G, et al. Vascular complications are associated with poor outcome in community-acquired pneumonia. QJM 2011;104:489–95. 10.1093/qjmed/hcq247 [DOI] [PubMed] [Google Scholar]
- 18.Eurich DT, Marrie TJ, Minhas-Sandhu JK, et al. Risk of heart failure after community acquired pneumonia: prospective controlled study with 10 years of follow-up. BMJ 2017;356:j413. 10.1136/bmj.j413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cangemi R, Calvieri C, Taliani G, et al. Left atrium dilatation and left ventricular hypertrophy predispose to atrial fibrillation in patients with community-acquired pneumonia. Am J Cardiol 2019;124:723–8. 10.1016/j.amjcard.2019.05.051 [DOI] [PubMed] [Google Scholar]
- 20.Pieralli F, Biondo B, Vannucchi V, et al. Performance of the CHA2DS2-VASc score in predicting new onset atrial fibrillation during hospitalization for community-acquired pneumonia. Eur J Intern Med 2019;62:24–8. 10.1016/j.ejim.2019.01.012 [DOI] [PubMed] [Google Scholar]
- 21.Corrales-Medina VF, Serpa J, Rueda AM, et al. Acute bacterial pneumonia is associated with the occurrence of acute coronary syndromes. Medicine 2009;88:154–9. 10.1097/MD.0b013e3181a692f0 [DOI] [PubMed] [Google Scholar]
- 22.Fukuda H, Ishiguro C, Ono R, et al. The Longevity Improvement & Fair Evidence (LIFE) study: overview of the study design and baseline participant profile. J Epidemiol 2022;10.2188. 10.2188/jea.JE20210513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Imai K, Petigara T, Kohn MA, et al. Risk of pneumococcal diseases in adults with underlying medical conditions: a retrospective, cohort study using two Japanese healthcare databases. BMJ Open 2018;8:e018553. 10.1136/bmjopen-2017-018553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011;173:676–82. 10.1093/aje/kwq433 [DOI] [PubMed] [Google Scholar]
- 25.Tralhão A, Póvoa P. Cardiovascular events after community-acquired pneumonia: a global perspective with systematic review and meta-analysis of observational studies. J Clin Med 2020;9:414. 10.3390/jcm9020414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Musher DM, Rueda AM, Kaka AS, et al. The association between pneumococcal pneumonia and acute cardiac events. Clin Infect Dis 2007;45:158–65. 10.1086/518849 [DOI] [PubMed] [Google Scholar]
- 27.Chong CP, Street PR. Pneumonia in the elderly: a review of the epidemiology, pathogenesis, microbiology, and clinical features. South Med J 2008;101:1141–5. 10.1097/SMJ.0b013e318181d5b5 [DOI] [PubMed] [Google Scholar]
- 28.Fillon S, Soulis K, Rajasekaran S, et al. Platelet-activating factor receptor and innate immunity: uptake of gram-positive bacterial cell wall into host cells and cell-specific pathophysiology. J Immunol 2006;177:6182–91. 10.4049/jimmunol.177.9.6182 [DOI] [PubMed] [Google Scholar]
- 29.Feldman C, Anderson R. Platelets and their role in the pathogenesis of cardiovascular events in patients with community-acquired pneumonia. Front Immunol 2020;11:577303. 10.3389/fimmu.2020.577303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Feldman C, Normark S, Henriques-Normark B, et al. Pathogenesis and prevention of risk of cardiovascular events in patients with pneumococcal community-acquired pneumonia. J Intern Med 2019;285:635–52. 10.1111/joim.12875 [DOI] [PubMed] [Google Scholar]
- 31.Anderson R, Nel JG, Feldman C. Multifaceted role of pneumolysin in the pathogenesis of myocardial injury in community-acquired pneumonia. Int J Mol Sci 2018;19:1147. 10.3390/ijms19041147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shenoy AT, Beno SM, Brissac T, et al. Severity and properties of cardiac damage caused by Streptococcus pneumoniae are strain dependent. PLoS One 2018;13:e0204032. 10.1371/journal.pone.0204032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alhamdi Y, Neill DR, Abrams ST, et al. Circulating pneumolysin is a potent inducer of cardiac injury during pneumococcal infection. PLoS Pathog 2015;11:e1004836. 10.1371/journal.ppat.1004836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016;37:2893–962. 10.1093/eurheartj/ehw210 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-059713supp001.pdf (84.2KB, pdf)
Data Availability Statement
No data are available. The data used in this study were acquired under agreements with the participating municipalities, which stipulate that the data can only be used by authorised research institutions and cannot be shared with third parties.