Abstract
Socioeconomic gaps in life expectancy have widened substantially in the United States since 2000. Yet the contribution of specific causes to these growing disparities remains unknown. We used death records from the National Vital Statistics System and population data from Current Population Surveys to quantify the contribution of alcohol-attributable causes of death to changes in US life expectancy between 2000 and 2018 by sex and socioeconomic status (as measured by educational attainment). During the study period, the gap in life expectancy between people with low (high school diploma or less) compared with high (college degree) levels of education increased by three years among men and five years among women. Between 2000 and 2010 declines in cardiovascular disease mortality among people with high education made major contributions to growing inequalities. In contrast, between 2010 and 2018 deaths from a cause with an alcohol-attributable fraction of 20 percent or more were a dominant driver of socioeconomic divergence. Increased efforts to implement cost-effective alcohol control policies will be essential for reducing health disparities.
In stark contrast to the overall global trend of increasing life expectancy during the past several decades,1,2 the United States has experienced stagnation and then declines in life expectancy at birth since about 2010.3,4 These trends constitute a severe public health concern, as prolonged stagnation of and declines in life expectancy are rare globally and have only been seen during times of crisis.2
Looking at the trends preceding declines in life expectancy reveals that gains in life expectancy between 2001 and 2014 were highly unequal across socioeconomic groups.5 Although men and women in the top 5 percent of the income distribution experienced increases of 2.3 and 2.9 years, respectively, their counterparts in the bottom 5 percent gained only 0.3 and less than 0.1 years, respectively. These socioeconomic inequalities are an important contributor to the overall recent stagnation in US life expectancy.
It is not yet fully understood which causes of death contributed to the overall stagnation or to these increasing disparities in life expectancy. Anne Case and Angus Deaton6 were the first to demonstrate that rising mortality from “deaths of despair”—causes of death related to drug and alcohol poisoning, suicide, and alcohol-related liver disease—was a major contributor to stagnating US life expectancy, especially among groups with lower socioeconomic status (SES). However, the importance of these causes in explaining overall trends in mortality at the population level has been criticized as overstated.7 Other causes of death that have been found to contribute to the trends in life expectancy during the past decade are motor vehicle–related injuries, liver diseases, pneumonia, and diabetes mellitus,8 all of which can be causally linked to alcohol use.9 We note that the period of time we are examining predates the COVID-19 pandemic.
Current evidence suggests that about 5 percent of all deaths in the US can be attributed to alcohol use.10,11 Furthermore, findings from meta-analyses show that alcohol use disproportionally affects those with low SES, leading to a relative risk of dying from a 100 percent alcohol-attributable cause of death for low compared with high SES that is about 1.5 to 2 times as large as the corresponding relative risk for all-cause mortality.12
However, it remains unknown to what extent alcohol-attributable causes of death contributed to the overall trends and growing socioeconomic divide in US life expectancy since 2000. The objectives of this study were to investigate changes in US life expectancy at age eighteen between 2000 and 2018 by SES and sex and to quantify how causes of death for which alcohol use is a risk factor have contributed to these changes.
Study Data And Methods
We adhered to the standards set out in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement (see online appendix exhibit A1).13
DEFINITIONS
Life expectancy at age eighteen was defined as the average age of death among people who survived to age eighteen, assuming that mortality conditions of the period prevailed over the rest of their lifetimes.14 Age was categorized into five-year age groups (with the youngest age group being ages 18–24 and the oldest age group being ages 80 and older). SES was operationalized via educational attainment and grouped into three categories: low education (high school diploma or less), middle education (some college but no college degree), and high education (college degree or more).
We included all major causes of death that are causally linked to alcohol use according to Jürgen Rehm and coauthors’ 2017 review9 and the Centers for Disease Control and Prevention:15 alcohol use disorders; liver disease and cirrhosis; pancreatitis; motor vehicle accidents; other unintentional injuries; suicide; cancer (female breast cancer, liver cancer, pancreatic cancer, and cancers of the digestive tract); hemorrhagic stroke; hypertensive heart disease; ischemic heart disease and ischemic stroke; diabetes mellitus; and lower respiratory infections (pneumonia).We classified these causes of death using the alcohol-attributable fraction, which is an indicator of the degree to which causes of death are affected by alcohol use at the population level. Alcohol-attributable fractions are informed by the prevalence, pattern, and level of alcohol use in the geography of interest and the relative risk function linking alcohol use to mortality risks. They indicate the proportion of deaths from a specific cause that would not have occurred in a counterfactual scenario of everyone being a lifetime abstainer. The International Model of Alcohol Harms and Policies, an open-access alcohol harms estimator, was used to calculate alcohol-attributable fractions,16,17 using exposure estimates published by Jakob Manthey and colleagues.18 International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10), codes, along with their corresponding alcohol-attributable fractions, are shown in appendix exhibit A2.13 All remaining causes of death were included in one “rest” category. In addition to mental and behavioral disorders due to use of alcohol (F10), the alcohol use disorders category included other causes of death that are fully attributable to alcohol use (such as alcohol poisoning, X45). To facilitate interpretation and communication of the results, the causes of death were grouped according to their alcohol-attributable fraction, as follows: less than 20 percent: cancer, hemorrhagic stroke, hypertensive heart disease, ischemic heart disease and ischemic stroke, diabetes mellitus, and lower respiratory infections; 20 percent to less than 50 percent: pancreatitis, motor vehicle accidents, other unintentional injuries, and suicide; and 50–100 percent: alcohol use disorders and liver disease and cirrhosis.
DATA SOURCES
The study used individual death records for 2000–18 obtained from the National Vital Statistics System.19 Specifically, we used the Multiple Cause-of-Death Files, which contain all deaths and information on education, age, and sex of the deceased, in addition to the underlying cause of death coded according to ICD-10.20 The data contained a total of 50,146,136 adult deaths. There were no missing data on age and sex, but education level was missing for 3.8 percent of the decedents. To ensure the inclusion of all observed deaths and prevent underestimation of mortality rates, these deaths were randomly assigned to an education category based on the observed proportion of deaths in each education group by age group, year, sex, and cause of death.3
We calculated population estimates for 2000–18 by educational attainment, age, and sex, using data from the Current Population Surveys, also known as the March CPS.21,22 The CPS sample is based on the US civilian, noninstitutionalized population, and it is representative at the national and state levels. The CPS recruits a probability sample of about 60,000 occupied households. Each year a computerized questionnaire is administered through both in-person and telephone interviews to about 150,000 adults. Education is classified by the highest level of education completed. The sample for our study period included 2,602,919 adults with no missing information on education, age, and sex.
STATISTICAL ANALYSES
First, we aggregated mortality counts obtained from the National Vital Statistics System by year, cause of death, education, age group, and sex, and we divided by respective population counts to generate mortality rates. Population counts were calculated as the sum of the survey weights (person weight) in each subgroup, using March CPS data. For presentation, we age-standardized mortality rates using the age distribution of the overall population in 2018. Life expectancy at age eighteen by year, education, and sex was calculated using standard life table techniques.23 Mortality data and population estimates were processed using STATA software, version 15.1; all further statistical analyses were conducted using R statistical software, version 3.6.1.
DECOMPOSITION
For the decomposition of cause-specific contributions to changes in life expectancy, we applied the continuous change decomposition method described by Shiro Horiuchi and colleagues.24 Intuitively, this method estimates the contribution of changes in mortality rates due to a specific cause of death to the change in life expectancy between two time points by holding mortality rates from all other causes of death fixed at their initial level, changing just the mortality rates for the cause of interest to their final levels, and seeing how many years of life expectancy would be gained or lost after recomputing on the basis of these updated rates. This process is then repeated for each cause-of-death group. In practice, the method is applied through numerical integration and by assuming that all of the age-cause-specific rates change proportionately between each year. This is to prevent residual contribution estimates that arise because life expectancy is a nonlinear function of mortality rates.25 To facilitate interpretation, contributions were aggregated over the course of four periods: 2000–05, 2005–10, 2010–15, and 2015–18 (periods overlap because the first year in each period is the baseline year.)
CONTRIBUTION TO INEQUALITIES
To quantify the contribution that different causes of death made to changes in inequality in life expectancy, we calculated the proportion of total changes in inequality that was contributed by each of the causes of death in each period. For example, if the high-SES group gained 0.1 years of life expectancy because of cause X over the course of 2000–05 and the low-SES group lost 0.2 years because of cause X during the same period, the increase in inequality in life expectancy between high and low SES because of cause X would be 0.3 years. If the total gain (from all causes of death) was 1.0 years for people with high SES and 0.1 years for those with low SES, the increase in inequality in life expectancy for all causes would be 0.9 years. Cause X would thereby have contributed 33 percent to this increase.
LIMITATIONS
We note several limitations to this work. First, SES is a multifaceted concept that refers to “social and economic factors that influence what position(s) individuals and groups hold within the structure of society.”26 Educational attainment hence represents only one facet of SES, which is also affected by aspects of income, wealth, housing conditions, employment, and occupation.27,28 However, as it is the only SES-related information available in national mortality statistics,19,29 it was used as an indicator of SES in our study.
Also, our study relied on separate data sources to inform mortality and population counts by education, age, and sex. Information on education in mortality data may introduce error, as it is assigned by funeral directors or the next of kin.30 This “dual data” bias can lead to measurement error in the size of SES mortality differentials.31,32 Although an alternative would be to use mortality-linked survey data,32–34 this approach has two important limitations: Publicly available linked data are available for selected causes of death and all-cause mortality only, limiting their utility for the present study, and the smaller sample sizes in linked data sources lead to large sampling errors around mortality estimates for individual causes.35 Linked mortality surveys may also be less representative, as response rates vary between 50 percent and 60 percent.36
The distribution of levels of educational attainment and the opportunities attached to each level have shifted over time, introducing bias in comparisons of education levels over time.32,33 In addition, stigmatized disease categories such as alcohol use disorders may be differentially assigned to people with lower levels of education.7
Finally, although alcohol-attributable fractions were used to describe the strength of the causal link between alcohol use and specific causes of death at the population level, they constitute a relatively coarse indicator. An individual-level determination of the role that alcohol played in the occurrence of a death was not possible. Furthermore, it should be noted that cause-specific mortality rates differ regarding their timeline of being affected by changes in consumption. Cancer mortality, for example, has a long latency in which effects of increased exposure to alcohol use would only appear about a decade later.37
Study Results
The proportion of men and women with low education declined from 49 percent and 50 percent, respectively, in 2000 to 41 percent and 38 percent, respectively, in 2018, whereas the proportion of men and women with high education increased between 2000 (25 percent and 23 percent, respectively) and 2018 (32 percent and 33 percent, respectively) (see appendix exhibit A3).13
There was considerable variation in gains in life expectancy between educational levels and sexes. During the total observation period, life expectancy among men with high education increased by 3.7 years, from 80.2 years in 2000 to 83.9 years in 2018 (exhibit 1). In contrast, life expectancy for men with low education was much lower in 2000, at 71.2 years, and increased only by 0.7 years, to 71.9 years, in 2018.With this, the gap in life expectancy between men with low and high education increased by 3.0 years, from 9.0 years in 2000 to 12.0 years in 2018.
EXHIBIT 1. Life expectancy at age 18 for men in the US, by educational attainment, 2000–18.
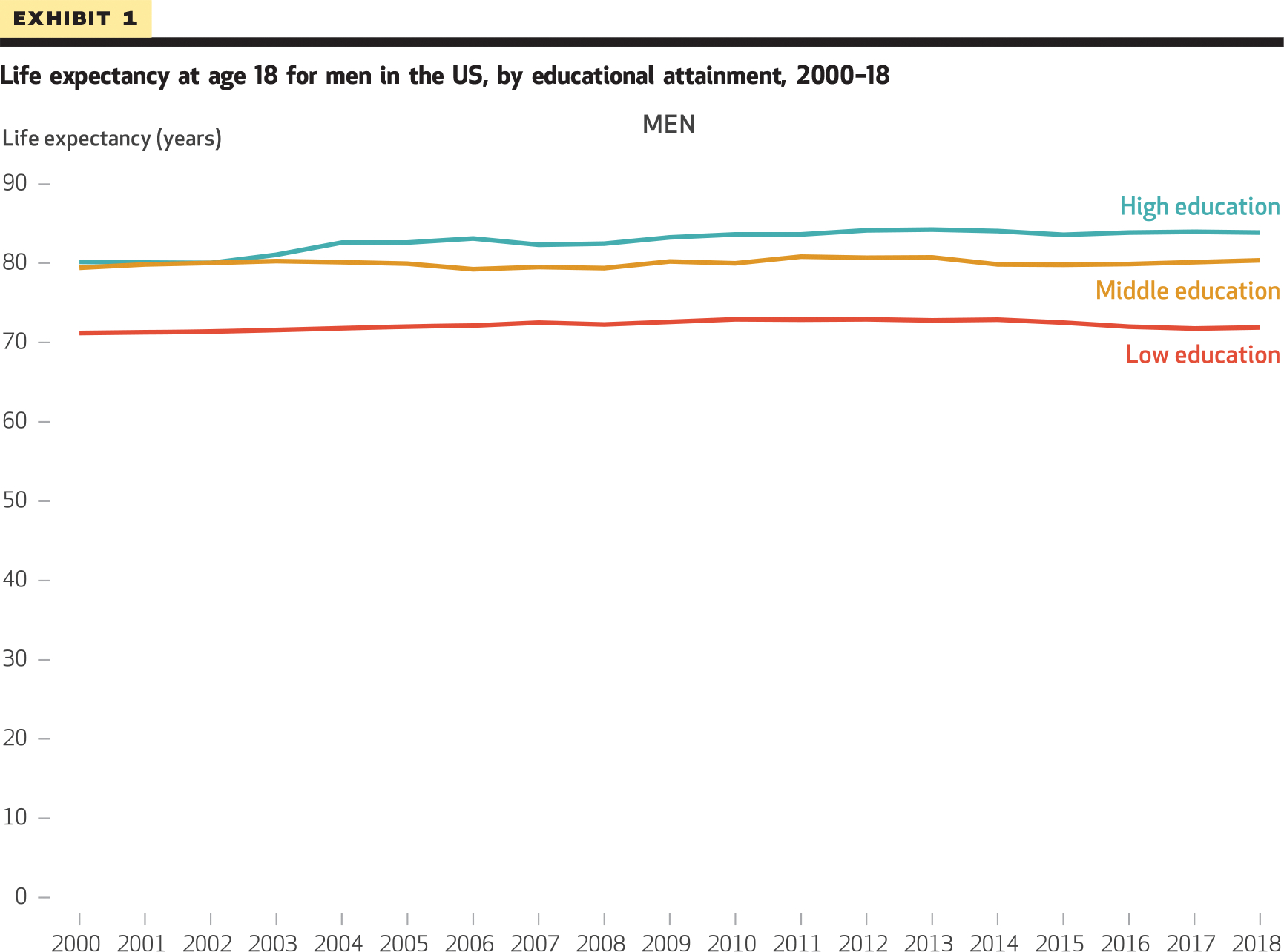
SOURCE Authors’ analysis of mortality data from the National Vital Statistics System and population data from Current Population Surveys, 2000–18. NOTES “Low education” means high school diploma or less, “middle education” means some college but no college degree, and “high education” means college degree or more. Educational attainment is used here as an indicator of socioeconomic status.
Among women, those with high education had a life expectancy of 81.5 years in 2000, which increased by 5.5 years to 87.0 years in 2018 (exhibit 2). Among women with low education, life expectancy increased by 0.5 years, from 77.4 years in 2000 to 77.9 years in 2018. The gap in life expectancy between women with low and high education thereby increased by 5.0 years, from 4.1 years in 2000 to 9.1 years in 2018.
EXHIBIT 2. Life expectancy at age 18 for women in the US, by educational attainment, 2000–18.
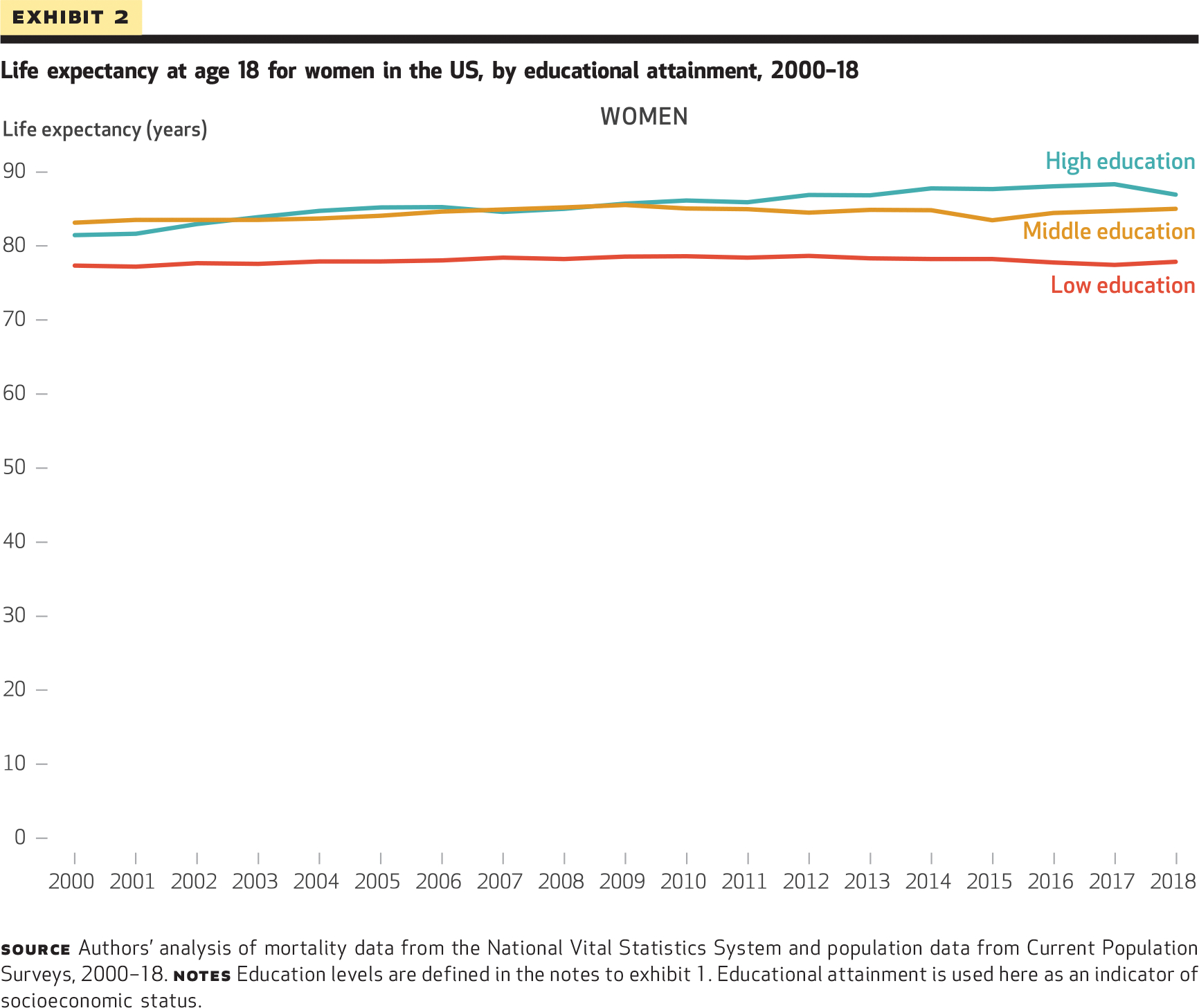
SOURCE Authors’ analysis of mortality data from the National Vital Statistics System and population data from Current Population Surveys, 2000–18. NOTES Education levels are defined in the notes to exhibit 1. Educational attainment is used here as an indicator of socioeconomic status.
Changes in mortality rates underlying the observed changes in life expectancy and inequalities differed greatly by cause of death (appendix exhibits A4 and A5).13 Complete data on mortality rates by cause of death, SES, and sex are in appendix exhibit B1.13
CAUSE-SPECIFIC CONTRIBUTIONS TO CHANGES IN LIFE EXPECTANCY
Exhibit 3 presents the cause-specific contributions to gains and losses in life expectancy at age eighteen in US men and women with high and low education during selected periods. The complete results are in appendix exhibit A6.13 Values above zero represent the positive contributions of cause-specific changes in life expectancy (years gained), whereas values below zero show negative contributions (years lost).
EXHIBIT 3.
Cause-specific contributions (in years) to annual changes in life expectancy among US adult men and women, by educational attainment, 2000–05 and 2015–18
| High education |
Low education |
|||
|---|---|---|---|---|
| Causes of death | 2000–05 | 2015–18 | 2000–05 | 2015–18 |
| MEN | ||||
| Alcohol use disorder | 0.00 | −0.01 | 0.00 | −0.02 |
| Liver disease and cirrhosis | 0.03 | −0.01 | 0.03 | −0.02 |
| Pancreatitis | 0.00 | 0.00 | 0.00 | 0.00 |
| Suicide | 0.01 | −0.02 | 0.00 | −0.08 |
| Motor vehicle accident | 0.03 | 0.02 | 0.00 | −0.05 |
| Unintentional injurya | 0.02 | −0.01 | 0.01 | −0.02 |
| IHD and ischemic stroke | 0.98 | 0.05 | 0.54 | −0.01 |
| Hemorrhagic stroke | 0.04 | 0.01 | 0.02 | 0.00 |
| Hypertensive heart disease | 0.00 | −0.04 | −0.03 | −0.04 |
| Diabetes mellitus | 0.03 | 0.00 | −0.02 | −0.04 |
| Cancer | 0.13 | 0.04 | 0.02 | 0.01 |
| Lower respiratory infections | 0.01 | −0.03 | 0.00 | −0.03 |
| Restb | 1.17 | 0.28 | 0.23 | −0.30 |
| Total | 2.45 | 0.31 | 0.80 | −0.59 |
| WOMEN | ||||
| Alcohol use disorder | 0.00 | 0.00 | 0.00 | −0.01 |
| Liver disease and cirrhosis | 0.03 | 0.00 | 0.00 | −0.02 |
| Pancreatitis | 0.00 | 0.00 | 0.00 | 0.00 |
| Suicide | 0.00 | 0.00 | −0.01 | −0.02 |
| Motor vehicle accident | 0.03 | 0.01 | 0.00 | −0.03 |
| Unintentional injurya | 0.03 | −0.04 | −0.02 | −0.02 |
| IHD and ischemic stroke | 1.22 | −0.10 | 0.52 | 0.01 |
| Hemorrhagic stroke | 0.07 | 0.00 | 0.02 | 0.00 |
| Hypertensive heart disease | 0.03 | −0.07 | −0.02 | −0.03 |
| Diabetes mellitus | 0.06 | −0.01 | 0.02 | −0.01 |
| Cancer | 0.32 | −0.01 | 0.10 | 0.00 |
| Lower respiratory infections | 0.01 | −0.03 | 0.00 | −0.03 |
| Restb | 1.96 | −0.52 | −0.06 | −0.21 |
| Total | 3.77 | −0.76 | 0.55 | −0.38 |
SOURCE Authors’ analysis of mortality data from the National Vital Statistics System and population data from Current Population Surveys, 2000–18.
NOTES Education levels are defined in the notes to exhibit 1. Educational attainment is used here as an indicator of socioeconomic status. IHD is ischemic heart disease.
Other than motor vehicle accidents.
Includes all remaining causes of death.
There are two main trends. First, causes of death with an alcohol-attributable fraction of 20 percent or more made overall negative contributions to life expectancy, especially among men and women with middle and low education. These causes included alcohol use disorders, liver diseases and cirrhosis, pancreatitis, suicide, motor vehicle accidents, and other unintentional injuries. Together, they accounted for a net loss in life expectancy of 0.38 years in men with low education and 0.23 years in women with low education between 2010 and 2018. In comparison, the net loss in life expectancy among men and women with high education from these causes during this period was only 0.04 and 0.03 years, respectively. The second main trend was a large but decreasing gain in life expectancy resulting from reductions in mortality from cardiovascular diseases—ischemic heart disease and ischemic stroke in particular—across all groups. During the whole observation period (2000–18), men and women with high education experienced a gain of 1.80 years and 2.08 years of life expectancy, respectively, attributable to reductions in mortality from ischemic heart disease and ischemic stroke. Among men and women with low education, these gains were lower, at just 1.16 years and 1.19 years, respectively. However, across all educational groups and both sexes, gains from progress against ischemic heart disease and ischemic stroke decreased considerably during the observation period and nearly disappeared completely after 2015 (appendix exhibit A6).
Finally, it should be noted that considerable changes in life expectancy were observed that were due to the remaining causes of death, which were not individually accounted for in this analysis. For example, among both men and women with low education, more than 0.6 years of life were lost between 2010 and 2018 because of the remaining causes of death (appendix exhibit A6).
CONTRIBUTION TO CHANGES IN INEQUALITY IN LIFE EXPECTANCY
Exhibit 4 illustrates the absolute contribution of each cause of death, grouped by alcohol-attributable fraction, to increases or decreases in life expectancy inequality between people with low, middle, and high levels of educational attainment. (Detailed results are in appendix exhibit B2.)13
EXHIBIT 4. Absolute contribution to increases and decreases in inequality in life expectancy at age 18 for people with middle and low education compared with high education in the US, by cause of death, time period, and sex, 2000–18.
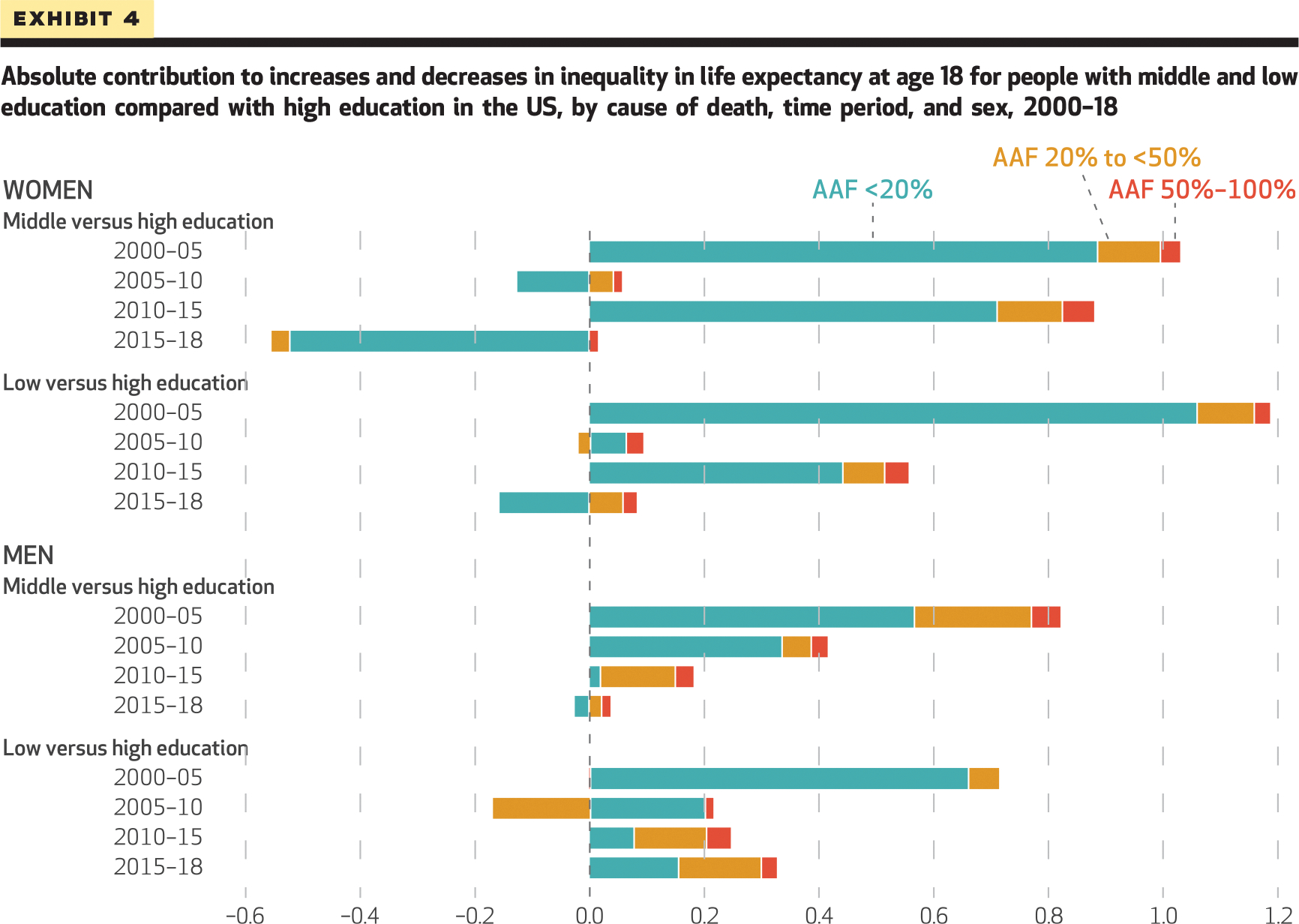
SOURCE Authors’ analysis of mortality data from the National Vital Statistics System and population data from Current Population Surveys, 2000–18. NOTES Positive numbers indicate an increase in absolute socioeconomic inequalities (difference) in life expectancy in years; negative numbers indicate a decline in the inequality in life expectancy. Education levels are defined in the notes to exhibit 1. Educational attainment is used here as an indicator of socioeconomic status. Cause-of-death categories are defined by alcohol-attributable fraction (AAF). Diseases in each of the three categories are defined in the text.
In the first period (2000–05), a stark increase in the inequalities in life expectancy between low and high education was observed for both men (1.65 years) and women (3.21 years). In this first period, changes in causes of death with an alcohol-attributable fraction of 20 percent or more contributed less than 5 percent to the total increase in the gap in life expectancy between both men (0.05 years) and women (0.13 years) with low and high education. However, changes in ischemic heart disease and ischemic stroke alone explained more than 20 percent of this increase in inequality among both sexes (0.45 years among men, 0.70 years among women). Among men, the second-largest increase in the gap in life expectancy between low and high education was observed for the period 2015–18 (0.90 years). In this period, changes in causes of death with an alcohol-attributable fraction of 20 percent or more contributed nearly 20 percent to the changes in inequality in life expectancy (0.17 years), whereas changes in ischemic heart disease and ischemic stroke contributed about 7 percent (0.06 years). Among women, the second-largest increase in the gap in life expectancy between low and high education was observed for the period 2010–15, with an increase of 1.94 years. Changes in causes of death with an alcohol-attributable fraction of 20 percent or more contributed about 5 percent to this increase (0.11 years). However, changes in ischemic heart disease and ischemic stroke contributed about 15 percent (0.28 years).
Discussion
We found that especially during the period 2010–18, alcohol-attributable causes of death were a major contributor to the widening SES gap, as indicated by educational attainment, in US life expectancy. During this period deaths from liver disease and cirrhosis, suicides, and motor vehicle accidents were substantially more concentrated among men and women without college degrees than among those with a college degree or more and were a dominant cause of the rapid socioeconomic divergence in US life expectancy. Alarmingly, the large negative contributions of alcohol-attributable causes of death to life expectancy changes among people without degrees were a relatively recent phenomenon, only emerging as an important explanation for why lower educational groups experienced stagnating and reversing life expectancy trends in 2010 and later. Beyond educational differences, slowing progress against ischemic heart disease and ischemic stroke mortality was an important contributor to stagnating life expectancy for all groups. Overall, our findings draw attention to the important and growing role that alcohol-attributable causes of death play in social and economic disparities in US life expectancy.
The findings of this study are in line with findings in previous research6,12 that showed a widening socioeconomic gap in mortality in the US.38 Our finding that overall stagnation across all groups was driven by a rapid slowdown in progress in ischemic heart disease and ischemic stroke mortality is also consistent with recently published research indicating that slowing progress against cardiovascular disease mortality is the main reason for recent trends in US mortality.39,40 To our knowledge, however, this is the first study to investigate and reveal the contribution of alcohol-attributable causes of death to widening mortality inequalities in the US. The results from these analyses are consistent with studies conducted in Scandinavia and the United Kingdom that found that more deprived socioeconomic groups experience a shorter life expectancy because of alcohol consumption or alcohol-attributable causes of death.41,42
Taken together, these findings suggest that although policy attention needs to be given to improving cardiovascular disease–related mortality to reverse mortality stagnation for all groups, such efforts alone might not result in reduced mortality disparities without additional attention to reducing alcohol-attributable deaths in lower-SES groups. These efforts seem especially important in times of COVID-19, during which overall life expectancy losses in the US have reached an unprecedented high.43 First evidence on the impact of the COVID-19 pandemic shows a 25.9 percent increase in alcohol-attributable mortality from 2019 to 2020, surpassing the respective 16.6 percent increase in all-cause mortality.44
Implications
Many recent studies have held so-called deaths of despair and stagnating cardiovascular disease mortality responsible for trends in US mortality.39,40,45 However, we found that the role of specific causes of death varied substantially by level of education during our study period. Our results call attention to the disproportionate role of alcohol-attributable causes of death among less educated groups and the impact of these causes on the recent widening disparities in mortality. Immediate action is needed to address alcohol-attributable causes of death, especially among people with low education. Even though cost-effective alcohol control policies are available,46 current data from the US show that they are vastly underused.47 There have been practically no improvements in alcohol policies directed at the general adult population, such as taxation or restriction of availability, and existing excise taxes are in most cases not being corrected for inflation, leading to a de facto erosion of alcohol taxes. Policies such as minimum unit pricing, which has some evidence supporting its ability to reach drinkers with low SES and risky drinking patterns in particular,48 are, to the best of our knowledge, currently not implemented at all in the US. Expanding the implementation of such policies while also addressing the broader social and economic determinants of health will be essential for reducing the large and growing gap in life expectancy between less- and more-well-off Americans.49 ∎
Supplementary Material
Acknowledgments
Charlotte Probst and Jürgen Rehm were supported by a research grant from the National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health (Grant No. R01AA028009). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Nikkil Sudharsanan was supported by the Alexander von Humboldt Foundation. Probst is also affiliated with Heidelberg University, Heidelberg, Germany; and the University of Toronto, Toronto, Ontario, Canada. Rehm is also affiliated with the University of Toronto; the University of Dresden, Dresden, Germany; the I. M. Sechenov First Moscow State Medical University, Moscow, Russia; and the University of Hamburg, Hamburg, Germany. Sudharsanan is also affiliated with Heidelberg University.
Contributor Information
Charlotte Probst, Centre for Addiction and Mental Health, Toronto, Ontario, Canada..
Miriam Könen, Heidelberg University, Heidelberg, Baden-Württemberg, Germany..
Jürgen Rehm, Centre for Addiction and Mental Health..
Nikkil Sudharsanan, Technical University of Munich, Munich, Bavaria, Germany..
References
- 1.Riley JC. Rising life expectancy: a global history. Cambridge: Cambridge University Press; 2001. [Google Scholar]
- 2.Deaton A The great escape: health, wealth, and the origins of inequality. Princeton (NJ): Princeton University Press; 2013. [Google Scholar]
- 3.Case A, Deaton A. Mortality and morbidity in the 21st century. Brookings Pap Econ Act. 2017;2017: 397–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kochanek KD, Anderson RN, Arias E. Changes in life expectancy at birth, 2010–2018 [Internet]. Hyattsville (MD): National Center for Health Statistics; 2020. Jan 30 [cited 2022 June 16]. Available from: https://www.cdc.gov/nchs/data/hestat/life-expectancy/life-expectancy-2018.htm [Google Scholar]
- 5.Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315(16): 1750–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harper S, Riddell CA, King NB. Declining life expectancy in the United States: missing the trees for the forest. Annu Rev Public Health. 2021;42(1):381–403. [DOI] [PubMed] [Google Scholar]
- 8.Shiels MS, Chernyavskiy P, Anderson WF, Best AF, Haozous EA, Hartge P, et al. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. Lancet. 2017;389(10073):1043–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rehm J, Gmel GE Sr, Gmel G, Hasan OSM, Imtiaz S, Popova S, et al. The relationship between different dimensions of alcohol use and the burden of disease—an update. Addiction. 2017;112(6):968–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shield K, Manthey J, Rylett M, Probst C, Wettlaufer A, Parry CDH, et al. National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: a comparative risk assessment study. Lancet Public Health. 2020;5(1): e51–61. [DOI] [PubMed] [Google Scholar]
- 11.National Center for Chronic Disease Prevention and Health Promotion. Alcohol-related disease impact (ARDI) application [Internet]. Atlanta (GA): Centers for Disease Control and Prevention; 2019. [cited 2022 Jun 16]. Available from: https://nccd.cdc.gov/DPH_ARDI/default/default.aspx [Google Scholar]
- 12.Probst C, Roerecke M, Behrendt S, Rehm J. Socioeconomic differences in alcohol-attributable mortality compared with all-cause mortality: a systematic review and meta-analysis. Int J Epidemiol. 2014;43(4):1314–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.To access the appendix, click on the Details tab of the article online. [Google Scholar]
- 14.Jung-Choi K, Khang Y-H, Cho H-J, Yun S-C. Decomposition of educational differences in life expectancy by age and causes of death among South Korean adults. BMC Public Health. 2014;14:560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Alcohol-related ICD codes: alcohol-related disease impact (ARDI) International Classification of Diseases (ICD) codes and alcohol-attributable fraction (AAF) sources [Internet]. Atlanta (GA): CDC; 2021. Jul 6 [cited 2022 Jun 16]. Available from: https://www.cdc.gov/alcohol/ardi/alcohol-related-icd-codes.html [Google Scholar]
- 16.Sherk A, Stockwell T, Rehm J, Dorocicz J, Shield KD, Churchill S. The International Model of Alcohol Harms and Policies: a new method for estimating alcohol health harms with application to alcohol-attributable mortality in Canada . J Stud Alcohol Drugs. 2020;81(3): 339–51. [PubMed] [Google Scholar]
- 17.Sherk A, Stockwell T, Rehm J, Dorocicz J, Shield KD. InterMAHP: The International Model of Alcohol Harms and Policies: a comprehensive guide to the estimation of alcohol-attributable morbidity and mortality. Victoria (BC): University of Victoria, Canadian Institute for Substance Use Research; 2017. [Google Scholar]
- 18.Manthey J, Shield KD, Rylett M, Hasan OSM, Probst C, Rehm J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: a modelling study. Lancet. 2019;393(10190):2493–502. [DOI] [PubMed] [Google Scholar]
- 19.National Center for Health Statistics. National Vital Statistics System [home page on the Internet]. Hyattsville (MD): NCHS; 2018. [last updated 2022 May 26; cited 2022 Jun 16]. Available from: https://www.cdc.gov/nchs/nvss/index.htm [Google Scholar]
- 20.World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: clinical descriptions and diagnostic guidelines [Internet]. Geneva: WHO; 1992. [cited 2022 Jun 16]. Available from: https://cdn.who.int/media/docs/default-source/classification/other-classifications/9241544228_eng.pdf [Google Scholar]
- 21.Center for Economic and Policy Research. CPS ASEC (March) data [Internet]. Washington (DC): CEPR; 2018. [cited 2022 Jun 16]. Available from: http://ceprdata.org/cps-uniform-data-extracts/march-cps-supplement/march-cps-data/ [Google Scholar]
- 22.Census Bureau. Design and methodology: Current Population Survey [Internet].Washington (DC): Census Bureau; 2006. Oct [cited 2022 Jun 30]. (Technical Paper 66). Available from: https://cps.ipums.org/cps/resources/earner/tp-66.pdf [Google Scholar]
- 23.Preston SH, Heuveline P, Guillot M. Demography: measuring and modeling population processes. Oxford: Blackwell Publishers Ltd.; 2001. [Google Scholar]
- 24.Horiuchi S, Wilmoth JR, Pletcher SD. A decomposition method based on a model of continuous change. Demography. 2008;45(4):785–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riffe T DemoDecomp: decompose demographic functions [Internet]. [location unknown]: Comprehensive R Archive Network; 2018. Aug 14 [cited 2022 Jun 16]. Available from: https://cran.r-project.org/web/packages/DemoDecomp/index.html [Google Scholar]
- 26.Lynch J, Kaplan G. Socioeconomic position. In: Berkman LF, Kawachi I, editors. Social epidemiology. New York (NY): Oxford University Press; 2000. p. 13–35. [Google Scholar]
- 27.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 1). J Epidemiol Community Health. 2006;60(1):7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (part 2). J Epidemiol Community Health. 2006;60(2):95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murphy SL, Xu J, Kochanek KD, Curtin SC, Arias E. Deaths: final data for 2015. Natl Vital Stat Rep. 2017; 66(6):1–75. [PubMed] [Google Scholar]
- 30.Rostron BL, Boies JL, Arias E. Education reporting and classification on death certificates in the United States. Vital Health Stat 2. 2010; (151):1–21. [PubMed] [Google Scholar]
- 31.Kunst AE, Groenhof F, Borgan JK, Costa G, Desplanques G, Faggiano F, et al. Socio-economic inequalities in mortality. Methodological problems illustrated with three examples from Europe. Rev Epidemiol Sante Publique. 1998;46(6):467–79. [PubMed] [Google Scholar]
- 32.Hendi AS. Trends in education-specific life expectancy, data quality, and shifting education distributions: a note on recent research. Demography. 2017;54(3):1203–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hendi AS. Trends in U.S. life expectancy gradients: the role of changing educational composition. Int J Epidemiol. 2015;44(3):946–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vierboom YC. Trends in alcohol-related mortality by educational attainment in the U.S., 2000–2017. Popul Res Policy Rev. 2020;39(1): 77–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sasson I Reply to trends in education-specific life expectancy, data quality, and shifting education distributions: a note on recent research. Demography. 2017;54(3):1215–9. [DOI] [PubMed] [Google Scholar]
- 36.National Center for Health Statistics. National Health Interview Survey: NHIS data, questionnaires, and related documentation [Internet]. Hyattsville (MD): NCHS; [last reviewed 2022 Feb 8; cited 2022 Jun 30]. Available via query from: https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm [Google Scholar]
- 37.Rumgay H, Shield K, Charvat H, Ferrari P, Sornpaisarn B, Obot I, et al. Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study. Lancet Oncol. 2021;22(8):1071–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Singh GK, Siahpush M. Widening socioeconomic inequalities in US life expectancy, 1980–2000. Int J Epidemiol. 2006;35(4):969–79. [DOI] [PubMed] [Google Scholar]
- 39.Mehta NK, Abrams LR, Myrskylä M. US life expectancy stalls due to cardiovascular disease, not drug deaths. Proc Natl Acad Sci U S A. 2020;117(13):6998–7000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bennett JE, Kontis V, Mathers CD, Guillot M, Rehm J, Chalkidou K, et al. NCD Countdown 2030: path-ways to achieving Sustainable Development Goal target 3.4. Lancet. 2020;396(10255):918–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Angus C, Pryce R, Holmes J, de Vocht F, Hickman M, Meier P, et al. Assessing the contribution of alcohol-specific causes to socio-economic inequalities in mortality in England and Wales 2001–16. Addiction. 2020;115(12):2268–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Östergren O, Martikainen P, Tarkiainen L, Elstad JI, Brønnum-Hansen H. Contribution of smoking and alcohol consumption to income differences in life expectancy: evidence using Danish, Finnish, Norwegian, and Swedish register data. J Epidemiol Community Health. 2019;73(4):334–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aburto JM, Schöley J, Kashnitsky I, Zhang L, Rahal C, Missov TI, et al. Quantifying impacts of the COVID-19 pandemic through life-expectancy losses: a population-level study of 29 countries. Int J Epidemiol. 2022; 51(1):63–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.White AM, Castle IP, Powell PA, Hingson RW, Koob GF. Alcohol-related deaths during the COVID-19 pandemic. JAMA. 2022;327(17): 1704–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Case A, Deaton A. Deaths of despair and the future of capitalism. Princeton (NJ): Princeton University Press; 2020. [Google Scholar]
- 46.Chisholm D, Moro D, Bertram M, Pretorius C, Gmel G, Shield K, et al. Are the “Best Buys” for alcohol control still valid? An update on the comparative cost-effectiveness of alcohol control strategies at the global level. J Stud Alcohol Drugs. 2018; 79(4):514–22. [PubMed] [Google Scholar]
- 47.Blanchette JG, Lira MC, Heeren TC, Naimi TS. Alcohol policies in U.S. states, 1999–2018. J Stud Alcohol Drugs. 2020;81(1):58–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.O’Donnell A, Anderson P, Jané-Llopis E, Manthey J, Kaner E, Rehm J. Immediate impact of minimum unit pricing on alcohol purchases in Scotland: controlled interrupted time series analysis for 2015–18. BMJ. 2019;366:l5274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Loring B Alcohol and inequities: guidance for addressing inequities in alcohol-related harm. Copenhagen: World Health Organization, Regional Office for Europe; 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


