Abstract
Background:
Maximizing uptake of SARS-CoV-2 vaccines among people in prison is essential in mitigating future outbreaks. We aimed to determine factors associated with willingness to receive SARS-CoV-2 vaccination before vaccine availability.
Methods:
We chose 3 Canadian federal prisons based on their low uptake of influenza vaccines in 2019–2020. Participants completed a self-administered questionnaire on knowledge, attitude and beliefs toward vaccines. The primary outcome was participant willingness to receive a SARS-CoV-2 vaccine, measured using a 5-point Likert scale to the question, “If a safe and effective COVID-19 vaccine becomes available in prison, how likely are you to get vaccinated?” We calculated the association of independent variables (age, ethnicity, chronic health conditions, 2019–2020 influenza vaccine uptake and prison security level), identified a priori, with vaccine willingness using logistic regression and crude and adjusted odds ratios (ORs) with 95% confidence intervals (CIs).
Results:
We recruited 240 participants from Mar. 31 to Apr. 19, 2021 (median age 46 years; 19.2% female, 25.8% Indigenous). Of these, 178 (74.2%) were very willing to receive a SARS-CoV-2 vaccine. Participants who received the 2019–2020 influenza vaccine (adjusted OR 5.20, 95% CI 2.43–12.00) had higher odds of vaccine willingness than those who did not; those who self-identified as Indigenous (adjusted OR 0.27, 95% CI 0.11–0.60) and in medium- or maximum-security prisons (adjusted OR 0.36, 95% CI 0.12–0.92) had lower odds of vaccine willingness than those who identified as white or those in minimum-security prisons, respectively.
Interpretation:
Most participants were very willing to receive vaccination against SARS-CoV-2 before vaccine roll-out. Vaccine promotion campaigns should target groups with low vaccine willingness (i.e., those who have declined influenza vaccine, identify as Indigenous or reside in high-security prisons).
Canadian correctional settings have witnessed several large SARS-CoV-2 outbreaks since the start of the COVID-19 pandemic.1–3 Many of the risk factors that predispose correctional settings to SARS-CoV-2 outbreaks — close living conditions,4,5 an aging and comorbid population,5,6 and limited autonomy that affects access to health care7,8 — are nonmodifiable, underscoring the importance of SARS-CoV-2 vaccination.9 The Canadian National Advisory Committee on Immunization prioritized residents and staff of congregate settings, such as correctional settings, for early SARS-CoV-2 vaccination in December 2020.10 However, rates of vaccine uptake have remained historically low in Canadian prisons despite the routine availability and promotion of vaccination since the 1990s.11 Given the disproportionate incarceration of people experiencing social and health inequities,12–16 maximizing vaccine acceptance is essential in preventing morbidity and death from vaccine-preventable diseases among the 30 000 adults currently incarcerated in Canadian federal and provincial or territorial prisons.13
Very few studies have sought to understand predictors of SARS-CoV-2 vaccine acceptance among people incarcerated in prison. The few existing studies have found that race and ethnicity,17,18 age,18 correctional facility type and security level,17,18 presence of chronic health conditions17 and a history of COVID-1917 were associated with vaccine willingness or acceptance. In addition to these factors,19–21 higher socioeconomic status and level of education,22 previous influenza vaccination23,24 and acceptance of other routine vaccines25 were predictors of SARS-CoV-2 vaccine acceptance in the general population. Understanding determinants of SARS-CoV-2 vaccine acceptance is crucial in preventing severe cases, hospital admissions and deaths, and in mitigating future outbreaks and the consequent harms in correctional settings. Additional studies are needed to understand who remains at risk of SARS-CoV-2 vaccine hesitancy such that targeted interventions can be designed to improve vaccination uptake. Cognizant of the knowledge gaps that exist in correctional settings, we sought to determine factors associated with SARS-CoV-2 vaccine willingness in Canadian federal prisons.
Methods
Study design and setting
We conducted an observational cross-sectional study in 3 Canadian federal prisons. Correctional Service Canada (CSC) oversees 43 federal corrections, where incarcerated adults serve sentences of 2 years or more.13 Three Canadian federal correctional facilities with low uptake of the influenza vaccine in 2019–2020 (and thus hypothesized to have lower willingness toward SARS-CoV-2 vaccination), served as the study sites, namely the Matsqui Institution in British Columbia, the Grand Valley Institution for Women in Ontario and the Federal Training Centre in Quebec. Matsqui Institution is a minimum- and medium-security prison that houses 313 men. More than one-third (n = 112, 36%) of incarcerated people in this facility are Indigenous and one-fifth (n = 65, 20%) are from other ethnic minority groups (Asian, Black, Hispanic and other) (Correctional Service Canada: unpublished data, 2022). Grand Valley Institution for Women is a multisecurity-level prison (with minimum, medium and maximum levels) that houses 169 incarcerated women. About one-third (n = 53, 31%) of incarcerated people in this facility are Indigenous and one-quarter (n = 42, 25%) are from other minority groups. Federal Training Centre is a minimum- and medium-security prison that houses 420 incarcerated men; fewer than one-fifth of incarcerated people in this facility are Indigenous (n = 70, 17%) or from other minority groups (n = 57, 14%). Both Grand Valley Institution for Women and Federal Training Centre were sites of previous COVID-19 outbreaks; 8 and 163 people tested positive for SARS-CoV-2, respectively.26
We included individuals aged 18 years or older who were able and willing to consent to study participation in either English or French. We excluded those who had been previously vaccinated with a SARS-CoV-2 vaccine (as older, medically vulnerable federal inmates were offered SARS-CoV-2 vaccination in January 2021),27 those whose sentences would end within 14 days and those who posed a security risk to the research team, as determined by facility staff. Participants did not receive compensation for their participation as per CSC regulations.
Data collection
We undertook systematic sampling of individuals meeting the eligibility criteria. After consultation with CSC, site-level CSC nurses sequentially approached potential participants in every second cell.28 Given visitation restrictions during the COVID-19 pandemic, we trained CSC nurses to describe the study to prospective participants, review the information and consent forms, and obtain verbal consent. We asked nurses to recruit 1 in 5 individuals older than 60 years at each study site. To reduce response bias, participants who agreed to participate were given self-administered paper questionnaires focused on their knowledge, attitude and beliefs toward vaccines in general and, more specifically, the SARS-CoV-2 vaccine (Appendix 1, available at www.cmajopen.ca/content/10/4/E922/suppl/DC1). We adapted the questionnaire from survey questions from the World Health Organization Strategic Advisory Group of Experts Working Group on Vaccine Hesitancy,29 Leger’s North American Tracker — Concerns about COVID-19,30 and Statistics Canada’s Canadian Perspectives Survey Series 3.31 We pilot-tested the questionnaire among 15 people in prison to ensure clarity before the study. Participants who required assistance with reading and writing could request nursing support to complete their questionnaires. We recruited people across the 3 sites between Mar. 31 and Apr. 19, 2021, until 240 were consented — a sample size chosen for an alternative primary end point (change in willingness to receive a SARS-CoV-2 vaccine after an educational intervention). However, on Apr. 20, 2021, the Moderna SARS-CoV-2 vaccine was made available across the 43 federal sites, precluding the evaluation of our intended primary outcome. With 240 participants, the confidence interval for estimating the proportion willing to be vaccinated would be estimated at 6%.32
Outcome
The primary outcome measure was “willingness to receive a COVID-19 vaccine.” We measured willingness by participants’ responses to the question “If a safe and effective COVID-19 vaccine becomes available in prison, how likely are you to get vaccinated?” Participants responded on a 5-point Likert scale (very willing, somewhat willing, uncertain, somewhat unwilling, very unwilling). Self-reported willingness to be vaccinated served as a proxy for vaccine acceptance, as mass vaccination (i.e., of everyone who was not an older, medically vulnerable federal inmate) across CSC sites began after recruitment. For our primary outcome, we dichotomized responses into “willing” (very willing) and “not willing” (all other responses). We determined independent variables a priori using published literature on vaccine hesitancy among incarcerated people and the general population. These included age,18,19 ethnicity,17,18,20,21 chronic health conditions related to COVID-19 severity (asthma, cancer, chronic blood disorder, congestive heart disease, chronic kidney disease, chronic lung disease, chronic neurologic disorders, diabetes, HIV, hypertension, other immunocompromised condition and liver disease),17 self-reported receipt of the 2019–2020 seasonal influenza vaccine24 and facility security level (minimum v. medium and maximum).17,18 Although factors related to socioeconomic status (i.e., housing security, high gross yearly income and stable income source) have been found to be associated with vaccine acceptance,22 they were excluded from the analysis as they do not apply to our study population given long incarceration periods.
Statistical analysis
We calculated summary statistics, medians and interquartile ranges (IQRs) for continuous variables, and counts and proportions for categorical variables to describe the study sample. We classified participants who reported multiple ethnicities, including Indigenous ethnicity, as Indigenous. We classified those who selected “visible minority other than Indigenous” (e.g., Black, Asian, Arab) or “other ethnicity” as other. We made conservative assumptions to address participants who indicated “prefer not to answer” or “don’t know” such that any misclassification would bias any effect to the null. We categorized participants who did not know or preferred not to answer regarding receipt of the 2019–2020 influenza vaccine as not having received it. Remaining participants who “preferred not to answer” on any other question were removed from the regression analysis. We included independent variables identified a priori in the final logistic regression analysis, and calculated crude and adjusted odds ratios (ORs) with 95% confidence intervals (CIs) to determine factors associated with willingness to receive SARS-CoV-2 vaccination. We performed all analyses using R statistical software (version 4.0.3).
Ethics approval
This study was approved by the McGill University Health Centre Research Ethics Board (REB #2021–7547). Consequently, additional REB approval by CSC was not required.
Results
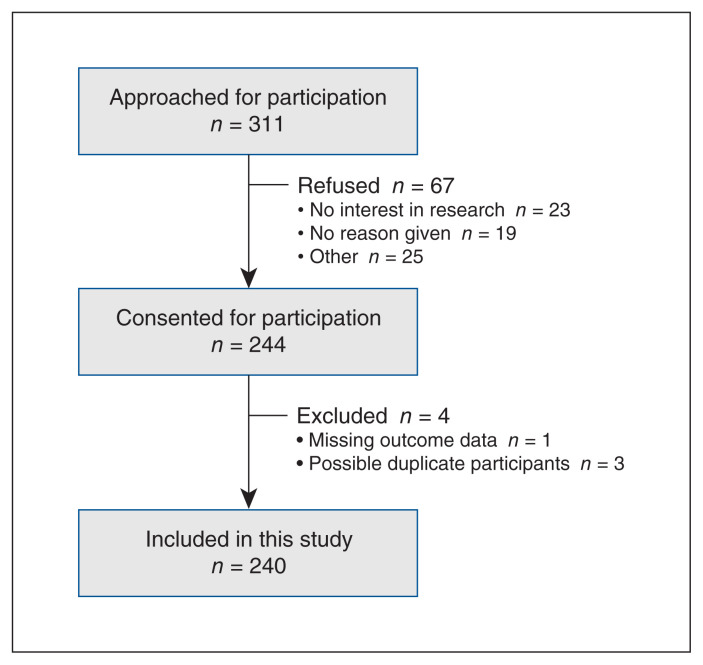
Overall, 311 people across the 3 federal prisons were invited to participate (n = 88 at Matsqui Institution, n = 74 at Grand Valley Institution for Women and n = 149 at Federal Training Centre). Of these, 67 (21.5%) declined participation (Figure 1). An additional 4 participants were excluded as they either had missing outcome data (n = 1) or represented possibly duplicate participants (n = 3), leaving a total of 240 participants in the analysis (n = 88 at Matsqui Institution, n = 47 at Grand Valley Institution for Women and n = 105 at Federal Training Centre).
Figure 1:
Participant flow chart.
Overall, the median age was 46 years (Table 1). Forty-six (19.2%) participants self-identified as female, all of whom were incarcerated at Grand Valley Institution for Women. Indigenous people made up 25.8% (n = 62) of the study sample and more than one-third of participants at Matsqui Institution and Grand Valley Institution for Women; less than one-fifth of participants were from other visible minority groups. Nearly half of participants reported no chronic health conditions related to COVID-19 morbidity and mortality. About half had received the influenza vaccine in 2019–2020. Overall, 181 (75.4%) participants were housed in a medium-security facility. The median length of incarceration was 4.1 years. Participant sociodemographic and clinical characteristics differed across correctional facilities (data not shown).
Table 1:
Participant characteristics
| Characteristic | No. (%) of participants* | ||
|---|---|---|---|
| Not willing to receive vaccine n = 62 |
Willing to receive vaccine n = 178 |
Total n = 240 |
|
| Demographic characteristics | |||
| Age, yr, median (IQR) | 39 (23–83) | 50 (21–81) | 46 (21–83) |
| Biological sex | |||
| Female | 17 (37.0) | 29 (63.0) | 46 (19.2) |
| Male | 44 (22.8) | 149 (77.2) | 193 (80.4) |
| Prefer not to answer | 1 (100.0) | 0 (0.0) | 1 (0.4) |
| Ethnicity | |||
| White | 21 (15.9) | 111 (84.1) | 132 (55.0) |
| Indigenous† | 27 (43.5) | 35 (56.5) | 62 (25.8) |
| Other‡ | 11 (25.6) | 32 (74.4) | 43 (17.9) |
| Prefer not to answer | 3 (100.0) | 0 (0.0) | 3 (1.2) |
| Education level | |||
| Secondary or less | 43 (29.3) | 104 (70.7) | 147 (61.2) |
| Higher education | 15 (18.5) | 66 (81.5) | 81 (33.8) |
| Prefer not to answer | 4 (33.3) | 8 (66.7) | 12 (5.0) |
| Clinical characteristics | |||
| Chronic health conditions§ | |||
| None | 35 (33.3) | 70 (66.7) | 105 (43.8) |
| ≥ 1 | 22 (18.3) | 98 (81.7) | 120 (50.5) |
| Prefer not to answer | 5 (33.3) | 10 (66.7) | 15 (6.2) |
| Vaccine-related characteristics | |||
| Receipt of the influenza vaccination in 2019–2020 | |||
| No¶ | 48 (38.7) | 76 (61.3) | 124 (51.7) |
| Yes | 13 (11.5) | 100 (88.5) | 113 (47.1) |
| Prefer not to answer | 1 (33.3) | 2 (66.7) | 3 (1.2) |
| Carceral characteristics | |||
| Correctional facility | |||
| FTC | 12 (11.4) | 93 (88.6) | 105 (43.8) |
| GVIW | 17 (36.2) | 30 (63.8) | 47 (19.6) |
| MI | 33 (37.5) | 55 (62.5) | 88 (36.7) |
| Security level | |||
| Minimum | 7 (12.3) | 50 (87.7) | 57 (23.8) |
| Medium | 54 (29.8) | 127 (70.2) | 181 (75.4) |
| Maximum | 1 (50.0) | 1 (50.0) | 2 (0.8) |
Note: FTC = Federal Training Centre, GVIW = Grand Valley Institution for Women, IQR = Interquartile range, MI = Matsqui Institution.
Unless indicated otherwise. Row percentages are provided for vaccine willingness subgroups.
Includes 14 participants who selected multiple ethnicities including Indigenous ethnicity.
Includes 25 participants who selected “visible minority other than Indigenous” (e.g., Black, Asian, Arab) and 18 who selected “other ethnicity.”
Chronic health conditions include asthma, cancer, chronic blood disorder, congestive heart disease, chronic kidney disease, chronic lung disease, chronic neurologic disorders, diabetes, HIV, hypertension, other immunocompromised conditions and liver disease.
One person did not know whether or not they had received the influenza vaccine.
SARS-CoV-2 vaccine willingness
A total of 178 (74.2%) participants were willing to receive a SARS-CoV-2 vaccine (n = 55 [62.5%] at Matsqui Institution, n = 30 [63.8%] at Grand Valley Institution for Women and n = 93 [88.6%] at Federal Training Centre), and 62 (25.8%) participants were not willing to receive a SARS-CoV-2 vaccine. This included 178 participants who were very willing, 18 who were somewhat willing, 30 who were uncertain, 4 who were somewhat unwilling and 10 who were very unwilling.
In the multivariable analyses, we found no significant association between willingness to receive a SARS-CoV-2 vaccine and age or number of chronic health conditions (Table 2). Participants who received the influenza vaccine in 2019–2020 had higher odds of being willing to receive a SARS-CoV-2 vaccine than those who did not receive the influenza vaccine (adjusted OR 5.20, 95% CI 2.43–12.00). Conversely, those who self-identified as Indigenous (adjusted OR 0.27, 95% CI 0.11–0.60) and those in medium- or maximum-security facilities (adjusted OR 0.36, 95% CI 0.12–0.92) had lower odds of being willing to receive a SARS-CoV-2 vaccine than those who identified as white or those in minimum-security facilities, respectively.
Table 2:
Multivariable analysis of factors associated with willingness to receive SARS-CoV-2 vaccination among adults incarcerated in Canada (n = 222)
| Variable | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Demographic characteristics | ||
| Age | 1.05 (1.03–1.08) | 1.03 (1.00–1.06) |
| Ethnicity | ||
| White | Reference | Reference |
| Indigenous | 0.22 (0.11–0.46) | 0.27 (0.11–0.60) |
| Other* | 0.51 (0.22–1.20) | 0.59 (0.24–1.51) |
| Clinical characteristics | ||
| Chronic health conditions† | ||
| None | Reference | Reference |
| ≥ 1 | 2.43 (1.30–4.61) | 1.65 (0.80–3.47) |
| Vaccine-related characteristics | ||
| Receipt of the seasonal influenza vaccination in 2019–2020 | ||
| No | Reference | Reference |
| Yes | 5.41 (2.69–11.70) | 5.20 (2.43–12.00) |
| Carceral characteristics | ||
| Security level | ||
| Minimum | Reference | Reference |
| Medium and maximum‡ | 0.30 (0.11–0.71) | 0.36 (0.12–0.92) |
Note: CI = confidence interval, OR = odds ratio.
Other includes all other ethnicities (i.e., Black, Latin American, Arab, Asian).
Chronic health conditions include asthma, cancer, chronic blood disorder, congestive heart disease, chronic kidney disease, chronic lung disease, chronic neurologic disorders, diabetes, HIV, hypertension, other immunocompromised conditions and liver disease.
Includes 2 participants in maximum-security facilities.
Interpretation
In this cross-sectional study, we explored factors associated with willingness to receive a SARS-CoV-2 vaccine among people incarcerated in 3 Canadian federal prisons with historically low influenza vaccine uptake and, as such, expected to be less receptive toward SARS-CoV-2 vaccination. Our study found that incarcerated adults who had previously received influenza vaccination had about 5 times higher odds of being willing to receive a SARS-CoV-2 vaccine. These findings may be explained by increased contact with health care providers, targeted messaging and education to those at higher risk of morbidity and mortality related to SARS-CoV-2 or a higher perceived risk of COVID-19.17,33 Similar to previous studies,17,18 we also found that individuals in higher-security settings (i.e., medium and maximum security v. minimum security) and those who self-reported as Indigenous had 64% and 73% lower odds of being willing to receive a SARS-CoV-2 vaccine, respectively. Recent qualitative studies by the research team showed that these findings may be explained by feelings of distrust toward correctional employees, limited access to information and a lower perceived risk of SARS-CoV-2 owing to restricted visits and interactions;34,35 however, additional research is needed to better understand and address reasons why incarcerated individuals are unwilling to receive SARS-CoV-2 vaccination.
Despite historically low uptake of the influenza vaccine at the selected study sites, 74% of participants reported being willing to receive a SARS-CoV-2 vaccine. This proportion is comparable to the Canadian adult population; 74% of the general population had received at least 1 dose of a SARS-CoV-2 vaccine by Sept. 10, 2021.36 The relatively high proportion of participants who reported being willing to receive a SARS-CoV-2 vaccine may in part be explained by a study population that is almost exclusively housed in minimum- and medium-security prisons or owing to selection bias during recruitment. Among individuals approached by CSC nurses, only 22% declined participation, a proportion that is considerably lower than most Canadian prison-based studies. This suggests the possibility of selection bias, resulting in a recruited population that may have been more representative of the Canadian general population rather than the general prison population. We did not collect demographic information among those who declined participation, which could have informed how our sample deviated from the overall prison populations, as well as possible selection bias. Certainly, although the proportion that reported willingness to get vaccinated was higher than what has been found in other prison-based studies,17,37 this may also highlight that prison-based outreach efforts, as was done by CSC nurses at all sites, can be effective in increasing uptake of the SARS-CoV-2 vaccine. Furthermore, people with greater contacts — namely those in minimum-security facilities — were more willing to receive the SARS-CoV-2 vaccine, underscoring that a stepwise approach (from highest to lowest risk) to SARS-CoV-2 vaccination in correctional settings could be considered where vaccine supply is limited. That said, given the non-modifiable risk factors that predispose correctional settings to COVID-19 outbreaks, all incarcerated people should be prioritized for SARS-CoV-2 vaccination,5,12 particularly in settings where decarceration (i.e., the early release of incarcerated individuals) is uncommon.13
Studies of the determinants of vaccination decision-making have resulted in several proposed models of acceptance and refusal.38–46 The various models illustrate the difficulty of categorizing attitudes about vaccination. That said, it is clear that attitudes toward vaccination are the result of complex interactions between different social, cultural, political and personal factors in vaccine decision-making.33 Additional studies are urgently needed to better understand the reasons that contribute to vaccine hesitancy among incarcerated populations.34,35 Given the unique environment, these reasons (e.g., trust with correctional employees, risk perception in congregate settings) are expected to differ substantially from those in the general population, precluding the generalizability of population-based studies to people in prison. Using the data generated from prison-based studies, focused interventions may seek to address modifiable individual-, interpersonal- and system-level factors. In addition, vaccine-hesitant people may refuse some vaccines, but agree to others. These future studies may contribute to our understanding of vaccine hesitancy for other vaccines routinely offered in prison as well, such as hepatitis A and B or influenza vaccines, thereby potentially affecting overall vaccine uptake. Finally, vaccine hesitancy is not fixed and may change with shifting contexts or when a vaccine and its related information are offered multiple times. Therefore, consideration must be given to different multi-modal approaches for offering SARS-CoV-2 vaccination, particularly among vaccine-hesitant populations.
Although we found that vaccine willingness among incarcerated people was relatively high, ongoing efforts are needed to increase uptake and prevent outbreaks in these congregate settings. Experts have argued that educational interventions will be key to reinforce trust in science-based interventions like vaccination,47,48 particularly as a result of the medical mistrust that emerged from disruptions caused by the COVID-19 pandemic. In fact, studies have confirmed that prison-based vaccination programs have the potential to increase vaccine uptake if partnered with education.49–51 However, although education may be necessary, studies have shown only modest improvements in vaccine uptake with education,52,53 underscoring that education will likely need to be paired with other interventions to achieve increased uptake. Although alternative strategies (e.g., peers, media or content) could be developed simultaneously and tailored to the needs of incarcerated people who express vaccine hesitancy,54,55 building trust with those incarcerated will be critical moving forward.56 Nurses, Indigenous Elders and peer educators could also be considered valuable resources to increasing rates of SARS-CoV-2 vaccination in Canadian correctional settings.
Limitations
We restricted our study sample to people incarcerated in 3 of 43 Canadian correctional facilities. Our results may thus not be generalizable to other CSC correctional facilities, including maximum-security facilities, and where the demographic characteristics of those incarcerated differs from our sample. The proportion of participants who were willing to receive a SARS-CoV-2 vaccine was higher than what has been found in other prison-based studies,17,37 which may be attributable to outreach efforts (information pamphlets, individual and group educational sessions, etc.) made by CSC and selection bias owing to the inclusion of 1 in 5 high-risk individuals older than 60 years. Thus, our findings may not be generalizable to Canadian provincial prisons, where the turnover of incarcerated people is much higher, and ORs should be interpreted with caution. Study consent and data collection were obtained by CSC nurses, which may have introduced response biases such as acquiescence, social desirability and dissent biases; however, the impact of these biases was limited with the use of self-administered questionnaires.57 The primary outcome, SARS-CoV-2 vaccine willingness, was used as a proxy for vaccine acceptance. As individual-level data were not available, we could not perform a sensitivity analysis using SARS-CoV-2 vaccine uptake as the dependent variable. Finally, our study was not initially designed to study factors associated with vaccine willingness. Thus, we may not be adequately powered to identify such factors. Despite these limitations, our study adds to the dearth of data regarding willingness to receive the SARS-CoV-2 vaccine in an understudied population.
Conclusion
We identified possible factors associated with willingness to receive the SARS-CoV-2 vaccine among people incarcerated in 3 Canadian federal prisons. Vaccine promotion campaigns should target groups with low vaccine willingness (i.e., those who have declined influenza vaccine, identify as Indigenous, or reside in high-security prisons).
Supplementary Material
Acknowledgements
The authors thank the site teams at Matsqui Institution, Grand Valley Institution for Women and Federal Training Centre for assisting with recruitment.
Footnotes
Competing interests: Joseph Cox reports research funding from ViiV Healthcare, Gilead Sciences and the Canadian Institutes of Health Research (CIHR), as well as remuneration for advisory work from ViiV Healthcare, Gilead Sciences and Merck Canada. Nicole Basta reports research funding from the National Institutes of Health, CIHR and McGill University’s Interdisciplinary Initiative in Infection and Immunity (MI4). Bertrand Lebouché reports research funding, consulting fees and honoraria from Gilead Sciences, Merck and ViiV Healthcare. Nadine Kronfli reports research funding from Gilead Sciences, as well as advisory fees and speaker fees from Gilead Sciences, ViiV Healthcare, Merck and AbbVie.
This article has been peer reviewed.
Contributors: Nadine Kronfli and Nicole Basta were involved in study conceptualization and design. Kathryn Romanchuk analyzed the data. All of the authors interpreted the data. Kathryn Romanchuk and Nadine Kronfli drafted the manuscript. All of the authors critically reviewed the manuscript for important intellectual content and approved the final manuscript as submitted.
Funding: This work was supported by a grant from the McGill Interdisciplinary Initiative in Infection and Immunity. Nicole Basta is supported by a Canada Research Chair (Tier 2) in Infectious Disease Prevention. Bertrand Lebouché holds a Canadian Institutes of Health Research, Strategy for Patient-Oriented Research Mentorship Chair in Innovative Clinical Trials for HIV Care and is also supported by a career award, LE 250, from Quebec’s Ministry of Health for researchers in Family Medicine. Nadine Kronfli is supported by a career award from the Fonds de Recherche Québec – Santé.
Data sharing: The study protocol, statistical analysis plan, and informed consent forms are available on request to the corresponding author. Individual-level data cannot be made available by the authors.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/10/4/E922/suppl/DC1.
References
- 1.Testing of inmates in federal correctional institutions for COVID-19. Ottawa: Correctional Service Canada; 2021. [accessed 2021 Jan. 6]. Available: https://www.csc-scc.gc.ca/001/006/001006-1014-fr.shtml. [Google Scholar]
- 2.Number of cases in detention facilities [article in French] Quebec: Gouvernement du Québec; 2021. [accessed 2021 Jan. 6]. Available: https://www.quebec.ca/sante/problemes-de-sante/a-z/coronavirus-2019/situation-coronavirus-quebec/#c57309. [Google Scholar]
- 3.Coronavirus disease 2019 (COVID-19): epidemiology update. Ottawa: Government of Canada; 2021. [accessed 2021 Jan. 6]. Available: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.htm. [Google Scholar]
- 4.Saloner B, Parish K, Ward JA, et al. COVID-19 cases and deaths in federal and state prisons. JAMA. 2020;324:602–3. doi: 10.1001/jama.2020.12528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beaudry G, et al. Managing outbreaks of highly contagious diseases in prisons: a systematic review. BMJ Glob Health. 2020;5:e003201. doi: 10.1136/bmjgh-2020-003201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blair A, Parnia A, Siddiqi A. Testing lags and emerging COVID-19 outbreaks in federal penitentiaries: a view from Canada. medRxiv [preprint] 2020 May 8; doi: 10.1101/2020.05.02.20086314. [DOI] [Google Scholar]
- 7.Kouyoumdjian F, Schuler A, Matheson FI, et al. Health status of prisoners in Canada: Narrative review. Can Fam Physician. 2016;62:215–22. [PMC free article] [PubMed] [Google Scholar]
- 8.Scallan E, Lancaster K, Kouyoumdjian F. The “problem” of health: an analysis of health care provision in Canada’s federal prisons. Health. 2021;25:3–20. doi: 10.1177/1363459319846940. [DOI] [PubMed] [Google Scholar]
- 9.Kronfli N, Dussault C, Maheu-Giroux M, et al. Seroprevalence and risk factors for SARS-CoV-2 among incarcerated adult men in Quebec, Canada. Clin Infect Disease. 2022;75:e165–73. doi: 10.1093/cid/ciac031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Preliminary guidance on key populations for early COVID-19 immunization [archived content] Ottawa: Government of Canada; 2020. [accessed 2021 Jan. 6]. Available: https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/guidance-key-populations-early-covid-19-immunization.html. [Google Scholar]
- 11.Vicente-Alcalde N, Ruescas-Escolano E, Barrella Harboe Z, et al. Vaccination coverage among prisoners: a systematic review. Int J Environ Res Public Health. 2020;17:7589. doi: 10.3390/ijerph17207589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kronfli N, Akiyama MJ. Prioritizing incarcerated populations for COVID-19 vaccination and vaccine trials. EClinicalMedicine. 2020;31:100659. doi: 10.1016/j.eclinm.2020.100659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malakieh J. Adult and youth correctional statistics in Canada, 2018/2019. Juristat: Canadian Centre for Justice Statistics; 2020. pp. 3–23. [Google Scholar]
- 14.Nowotny KM, Kuptsevych-Timmer A. Health and justice: framing incarceration as a social determinant of health for Black men in the United States. Sociol Compass. 2018;12:e12566. [Google Scholar]
- 15.Singh D, Prowse S, Anderson M. Overincarceration of Indigenous people: a health crisis. CMAJ. 2019;191:E487–8. doi: 10.1503/cmaj.181437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang EA, Zenilman J, Brinkley-Rubinstein L. Ethical considerations for COVID-19 vaccine trials in correctional facilities. JAMA. 2020;324:1031–2. doi: 10.1001/jama.2020.15589. [DOI] [PubMed] [Google Scholar]
- 17.Chin ET, Leidner D, Ryckman T, et al. COVID-19 vaccine acceptance in California state prisons [letter] N England J Med. 2021;385:4. doi: 10.1056/NEJMc2105282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stern MF, Piasecki AM, Strick LB, et al. Willingness to receive a COVID-19 vaccination among incarcerated or detained persons in correctional and detention facilities: four states, September–December 2020. MMWR Morb Mortal Wkly Rep. 2021;70:473–7. doi: 10.15585/mmwr.mm7013a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kourlaba G, Kourkouni E, Maistreli S, et al. Willingness of Greek general population to get a COVID-19 vaccine. Glob Health Res Policy. 2021;6:3. doi: 10.1186/s41256-021-00188-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Quach S, Hamid JS, Pereira JA, et al. Influenza vaccination coverage across ethnic groups in Canada. CMAJ. 2012;184:1673–81. doi: 10.1503/cmaj.111628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thorneloe R, Wilcockson H, Lamb M, et al. Willingness to receive a COVID-19 vaccine among adults at high-risk of COVID-19: a UK-wide survey. PsyArXiv [preprint] 2020 July 20; doi: 10.31234/osf.io/fs9wk. [DOI] [Google Scholar]
- 22.Lazarus JV, Ratzan SC, Palayew A, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nature Med. 2021;27:225–8. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fisher KA, Bloomstone SJ, Walder J, et al. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann Intern Med. 2020;173:964–73. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crawshaw J, Konnyu K, Castillo G, et al. Factors affecting COVID-19 vaccination acceptance and uptake among the general public: a living behavioural science evidence synthesis. Ottawa: The Ottawa Hospital Research Institute; 2021. [accessed 2021 May 27]. Available: https://www.mcmasterforum.org/docs/default-source/product-documents/living-evidence-syntheses/covid-19-living-evidence-synthesis-4.1---factors-affecting-covid-19-vaccination-acceptance-and-uptake-among-the-general-public.pdf?sfvrsn=5368712f_7. [Google Scholar]
- 25.Fridman A, Gershon R, Gneezy A. COVID-19 and vaccine hesitancy: a longitudinal study. PLoS One. 2021;16:e0250123. doi: 10.1371/journal.pone.0250123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Testing of inmates in federal correctional institutions for COVID-19. Ottawa: Government of Canada; 2021. [accessed 2022 Feb. 27]. Available: https://www.canada.ca/en/correctional-service/campaigns/covid-19/inmate-testing.html. [Google Scholar]
- 27.Correctional Service Canada COVID-19 vaccine roll-out. Ottawa: Government of Canada; 2021. [accessed 2022 Feb. 27]. Available: https://www.canada.ca/en/correctional-service/news/2021/01/correctional-service-canada-covid-19-vaccine-roll-out.html. [Google Scholar]
- 28.Abbott P, DiGiacomo M, Magin P, et al. A scoping review of qualitative research methods used with people in prison. Int J Qual Methods. 2018;17 [Google Scholar]
- 29.Strategic Advisory Group of Experts (SAGE) on Vaccine Hesitancy Report of the SAGE Working Group on vaccine hesitancy. World Health Organization; 2014. [accessed 2022 Feb. 27]. Available https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf. [Google Scholar]
- 30.Concerns about COVID-19 — March 24, 2020 [posted on North American Tracker, Surveys] Leger. 2020. Mar 24, [accessed 2022 Feb. 27]. Available: https://leger360.com/surveys/concerns-about-covid-19-march-24-2020/
- 31.Canadian Perspectives Survey Series 3 — resuming economic and social activities during COVID-19 June 15, 2020 to June 21, 2020. Ottawa: Statistics Canada; 2020. [accessed 2022 Feb. 27]. Available https://www23.statcan.gc.ca/imdb/p3Instr.pl?Function=assembleInstr&lang=en&Item_Id=1282314. [Google Scholar]
- 32.Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. 2013;35:121–6. doi: 10.4103/0253-7176.116232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dubé E, Laberge C, Guay M, et al. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9:1763–73. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ortiz-Paredes D, Varsaneux O, Worthington J, et al. Reasons for COVID-19 vaccine refusal among people incarcerated in Canadian federal prisons. PLoS One. 2022;17:e0264145. doi: 10.1371/journal.pone.0264145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lessard D, Ortiz-Paredes D, Park H, et al. Barriers and facilitators to COVID-19 vaccine acceptability among people incarcerated in Canadian federal prisons: a qualitative study. Vaccine X. 2022;10:100150. doi: 10.1016/j.jvacx.2022.100150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.COVID-19 vaccination in Canada. Ottawa: Government of Canada; 2021. [accessed 2022 Feb. 27]. Available: https://health-infobase.canada.ca/covid-19/vaccination-coverage/ [Google Scholar]
- 37.Berk J, Chan P, Brinkley-Rubinstein L. SARS-CoV-2 vaccination uptake in a correctional setting. MIRx Med. 2021;2:e30176. doi: 10.2196/30176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kashyap VK, Dhasmana A, Massey A, et al. Smoking and COVID-19: adding fuel to the flame. Int J Mol Sci. 2020;21:6581. doi: 10.3390/ijms21186581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Benin AL, Wisler-Scher DJ, Colson E, et al. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117:1532–41. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- 40.Brown K, Fraser G, Ramsay M, et al. Attitudinal and demographic predictors of measles-mumps-rubella vaccine (MMR) uptake during the UK catch-up campaign 2008-09 cross-sectional survey. PLoS One. 2011;6:e19381. doi: 10.1371/journal.pone.0019381. [Epub 2011 May 13]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Burton-Jeangros C, Golay M, Sudre P. Compliance and resistance to child vaccination: a study among Swiss mothers. Rev Epidemiol Sante Publique. 2005;53:341–50. doi: 10.1016/s0398-7620(05)84616-4. [DOI] [PubMed] [Google Scholar]
- 42.Gust D, Brown C, Sheedy K, et al. Immunization attitudes and beliefs among parents: beyond a dichotomous perspective. Am J Health Behav. 2005;29:81–92. doi: 10.5993/ajhb.29.1.7. [DOI] [PubMed] [Google Scholar]
- 43.Halperin SA. How to manage parents unsure about immunization. Can J Contin Med Educ. 2000;2000:62–75. [Google Scholar]
- 44.Nichter M. Vaccinations in the Third World: a consideration of community demand. Soc Sci Med. 1995;41:617–32. doi: 10.1016/0277-9536(95)00034-5. [DOI] [PubMed] [Google Scholar]
- 45.Rogers A, Pilgrim D, Gust ID, et al. The pros and cons of immunisation. Health Care Anal. 1995;3:99–115. doi: 10.1007/BF02198210. [DOI] [PubMed] [Google Scholar]
- 46.Streefland P, Chowdhury AMR, Ramos-Jimenez P. Patterns of vaccination acceptance. Soc Sci Med. 1999;49:1705–16. doi: 10.1016/s0277-9536(99)00239-7. [DOI] [PubMed] [Google Scholar]
- 47.Dawson A, et al. Key ethical concepts and their application to COVID-19 research. Public Health Ethics. 2020;13:127–32. [Google Scholar]
- 48.Rutjens BT, van der Linden S, van der Lee R. Science skepticism in times of COVID-19. Group Process Intergroup Relat. 2021;24:276–83. [Google Scholar]
- 49.Buck J, et al. Hepatitis B vaccination in prison: the perspectives of formerly incarcerated men. J Correct Health Care. 2006;12:12–23. [Google Scholar]
- 50.Devine A, Karvelas M, Sundararajan V. Evaluation of a prison-based hepatitis B immunisation pilot project. Aust N Z J Public Health. 2007;31:127–30. doi: 10.1111/j.1753-6405.2007.00029.x. [DOI] [PubMed] [Google Scholar]
- 51.Winter RJ, et al. A nurse-led intervention improved blood-borne virus testing and vaccination in Victorian prisons. Aust N Z J Public Health. 2016;40:592–4. doi: 10.1111/1753-6405.12578. [DOI] [PubMed] [Google Scholar]
- 52.Piedimonte S, et al. Impact of an HPV education and vaccination campaign among canadian university students. J Obstet Gynaecol Can. 2018;40:440–6. doi: 10.1016/j.jogc.2017.07.028. [DOI] [PubMed] [Google Scholar]
- 53.Hu Y, Qian L, Yaping C. Evaluation of two health education interventions to improve the varicella vaccination: a randomized controlled trial from a province in the east China. BMC Public Health. 2018;18:144. doi: 10.1186/s12889-018-5070-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cataldi JR, Kerns ME, O’Leary ST. Evidence-based strategies to increase vaccination uptake: a review. Curr Opin Pediatr. 2020;32:151–9. doi: 10.1097/MOP.0000000000000843. [DOI] [PubMed] [Google Scholar]
- 55.Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg Health Eur. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gagnon D, Dubé È. Literature review on effective strategies to improve vaccine acceptance and uptake. Ottawa: Canadian Public Health Association — CAN-Vax; 2019. [accessed 2021 July 2]. Available: https://canvax.ca/sites/default/files/2019-02/Literature%20Review%20on%20Effective%20Strategies%20to%20Improve%20VAU_3.pdf. [Google Scholar]
- 57.Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health. 2005;27:281–91. doi: 10.1093/pubmed/fdi031. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.