This case series compares the number of adolescent/young adult patients seeking inpatient and outpatient eating disorder care before and after onset of the COVID-19 pandemic.
Key Points
Question
Did the volume of adolescent and young adult patients seeking care for eating disorders change after onset of the COVID-19 pandemic?
Findings
In this case series study, before and after onset of the COVID-19 pandemic eating disorder care volume, both inpatient and outpatient, across 14 geographically diverse academic adolescent medicine sites were compared. A significant increase in both inpatient and outpatient eating disorder volume after onset of the pandemic that surpassed prepandemic patient care trends was found, particularly through the first year.
Meaning
Programs throughout the US saw a significant, pandemic-associated increase in the number of patients seeking eating disorder–related care in both inpatient and outpatient settings.
Abstract
Importance
The COVID-19 pandemic has affected youth mental health. Increases in site-specific eating disorder (ED) care have been documented; however, multisite studies demonstrating national trends are lacking.
Objective
To compare the number of adolescent/young adult patients seeking inpatient and outpatient ED care before and after onset of the COVID-19 pandemic.
Design, Setting, and Participants
Using an observational case series design, changes in volume in inpatient and outpatient ED-related care across 15 member sites (14 geographically diverse hospital-based adolescent medicine programs and 1 nonhospital-based ED program) of the US National Eating Disorder Quality Improvement Collaborative was examined. Sites reported monthly volumes of patients seeking inpatient and outpatient ED care between January 2018 and December 2021. Patient volumes pre- and postpandemic onset were compared separately for inpatient and outpatient settings. Demographic data such as race and ethnicity were not collected because this study used monthly summary data.
Exposures
Onset of the COVID-19 pandemic.
Main Outcomes and Measures
Monthly number of patients seeking inpatient/outpatient ED-related care.
Results
Aggregate total inpatient ED admissions were 81 in January 2018 and 109 in February 2020. Aggregate total new outpatient assessments were 195 in January 2018 and 254 in February 2020. Before the COVID-19 pandemic, the relative number of pooled inpatient ED admissions were increasing over time by 0.7% per month (95% CI, 0.2%-1.3%). After onset of the pandemic, there was a significant increase in admissions over time of 7.2% per month (95% CI, 4.8%-9.7%) through April 2021, then a decrease of 3.6% per month (95% CI, −6.0% to −1.1%) through December 2021. Prepandemic, pooled data showed relative outpatient ED assessment volume was stable over time, with an immediate 39.7% decline (95% CI, −50.4% to −26.7%) in April 2020. Subsequently, new assessments increased by 8.1% (95% CI, 5.3%-11.1%) per month through April 2021, then decreased by 1.5% per month (95% CI, −3.6% to 0.7%) through December 2021. The nonhospital-based ED program did not demonstrate a significant increase in the absolute number of admissions after onset of the pandemic but did see a significant increase of 8.2 (95% CI, 6.2-10.2) additional inquiries for care per month in the first year after onset of the pandemic.
Conclusions and Relevance
In this study, there was a significant COVID-19 pandemic-related increase in both inpatient and outpatient volume of patients with EDs across sites, particularly in the first year of the pandemic. Given inadequate ED care availability prior to the pandemic, the increased postpandemic demand will likely outstrip available resources. Results highlight the need to address ED workforce and program capacity issues as well as improve ED prevention strategies.
Introduction
Eating disorders (EDs), such as anorexia nervosa, bulimia nervosa, avoidant/restrictive food intake disorder, and binge eating disorder, impact individuals of every age, race, socioeconomic status, gender identity, and sexual orientation.1 EDs are of particular concern in adolescence and young adulthood, which are critical stages of development that can be negatively affected by the consequences of EDs.2 EDs pose a significant public health burden, with up to 10% of the total US population struggling with an ED during their lifetime.3,4,5 The cost of ED care in the US is high, with a 2020 report revealing the annual cost to society of $64.7 billion.1 Restrictive EDs (eg, anorexia nervosa, avoidant/restrictive food intake disorder, and other specified feeding and eating disorder) in particular can have major health consequences, with the negative effects of malnutrition including bradycardia and electrolyte disturbances potentially necessitating hospitalization.3,6 Furthermore, EDs commonly co-occur with other mental health conditions such as anxiety, depression, and substance use, which can influence the trajectory of illness.4,7 Studies have shown that individuals with EDs have increased mortality rates compared with the general population, in part due to increased suicidality.4,7,8,9 Patients with EDs often require intensive treatment by multiple health care professionals, and this type of specialized care is not always available. Given the prevalence, cost, and effects on health, understanding factors that increase prevalence or worsen illness is essential.
The COVID-19 pandemic has affected the mental health of adolescents and young adults throughout the world. Increased rates of anxiety and depression have been attributed to the pandemic.10,11,12 Studies have also demonstrated worsening of symptoms and behaviors in those with EDs, eg, increased caloric restriction, compulsive exercise, binge eating, and purging.12,13,14,15 Multiple contributors to disordered eating and exercise behaviors during the pandemic have been proposed, such as uncertainty about the future, disruptions in daily routines, inconsistent access to food, increased time spent in triggering environments, influence from the media, and changes in access to treatment.12,14,15,16,17,18,19,20
While most of the studies on EDs during the COVID-19 pandemic have examined ED symptomatology, few have examined changes in patient volume (ie, the number of patients seeking ED-related care) during the pandemic, to our knowledge. Understanding trends in care needs is critical to project workforce and program needs and to raise awareness so that patients may be diagnosed and referred to treatment earlier. Reports from individual institutions in Australia, Pennsylvania, and Michigan have noted increased volumes of patients with EDs after the onset of the COVID-19 pandemic compared with prior to the pandemic.21,22,23 Another study showed that diagnosis codes for EDs in adults increased after onset of the pandemic, exceeding any increases noted in mood disorders or opioid use disorders.24 Boston Children’s Hospital noted significantly increased numbers of hospital admissions for patients with EDs in need of medical stabilization, as well as inquiries for and completed new outpatient ED assessments during the pandemic.25 However, multisite, geographically diverse studies that explore changes in volume of both inpatient and outpatient EDs for adolescents and young adults are lacking. Therefore, we aimed to examine the following in adolescent and young adult patients with EDs: (1) trends in patient volume for inpatient medical hospitalization before and after the onset of the COVID-19 pandemic and (2) trends in volume of patients seeking outpatient subspecialty care before and after the onset of the COVID-19 pandemic.
Methods
Sample and Measures
The National Eating Disorder Quality Improvement Collaborative (NEDQIC) was established in 2006 with the goal to compare treatment outcomes from adolescent and young adult ED programs across the US.26,27 For the current study, we used data from 14 medical centers throughout the United States as well as 1 nonhospital-based private ED program not affiliated with a medical center that has multiple levels of care including inpatient, residential, and partial day programs (Table). The nonhospital-based ED program site was included due to the author’s previous position and ongoing involvement in NEDQIC and with the intention of increasing institutional diversity. This study was granted exemption by the Boston Children’s Hospital Institutional Review Board due to the use of deidentified summary data. Each participating site received independent approval or exemption from their respective institutional review board. Analyses were conducted at Boston Children’s Hospital. This study has an observational case series design and follows Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Table. Geographic Location and Characteristics of Sites Used in Data Analysis.
| Site initial | Geographic location | Approximate No. of inpatient beds | Age range of patients, y | Site characteristics |
|---|---|---|---|---|
| A | West Coast | 300 | 8-20 | Freestanding children’s hospital |
| B | East Coast | 200 | 7-21 | Freestanding children’s hospital |
| C | East Coast | 150 | 10-24 | Freestanding children’s hospital |
| D | West Coast | 150 | 10-25 | Pediatric hospital within an adult hospital |
| E | East Coast | 400 | 11-26 | Freestanding children’s hospital |
| F | Midwest | 350 | 12-22 | Freestanding children’s hospital |
| G | East Coast | 120 | 11-26 | Pediatric hospital within an adult hospital |
| H | West Coast | 350 | 10-25 | Pediatrics and obstetrics hospital |
| I | Midwest | 350 | 8-22 | Freestanding children’s hospital |
| J | East Coast | 100 | 10-21 | Pediatric hospital within an adult hospital |
| K | Midwest | 300 | 9-18 | Freestanding children’s hospital |
| L | Midwest | 50 | 10-24 | Pediatric hospital within an adult hospital |
| M | Midwest | 320 | 5-22 | Pediatric hospital within an adult hospital |
| N | Midwest | 600 | 8-24 | Freestanding children’s hospital |
| Nonhospital-based eating disorder program | Southeast | 40 Inpatient/residential beds | 8-18 | Nonhospital-based eating disorder program with inpatient, residential, day, and evening program levels of care |
| 20 Day/evening program spots |
Primary outcomes include the number of patients requiring inpatient ED admission per month as well as the number of patients requiring a new outpatient ED assessment per month at the 14 hospital-based sites during the study period. Secondary outcomes include the number of admissions per month as well as the number of inquiries for care per month at the nonhospital-based ED program. Demographic data such as race and ethnicity were not collected because this study used monthly summary data. Each hospital-based site provided monthly summary data from January 2018 through December 2021 including inpatient admissions for patients with EDs and new outpatient ED assessments. For the nonhospital-based ED program, admissions data were available from January 2018 through November 2021, and inquiries for care data were available from January 2018 through August 2021. Each site also provided dates of COVID-19 restrictions taking effect at their state or local level including state-level school closures, stay-at-home orders, and any hospital or clinic restrictions put into place as a direct result of the pandemic. Data were provided by each site via a standard data entry form.
COVID-19–Related Restrictions
While not all sites had restrictions on inpatient admissions or outpatient visits, all sites were in states with school closures and stay-at-home orders. There was little variability in timing of these restrictions. School closures almost universally occurred in the third week of March 2020 and stay-at-home orders were issued in late March or the first week of April 2020.
Statistical Analysis
We examined trends in inpatient and outpatient volumes of patients with EDs before and after onset of the COVID-19 pandemic using segmented regression modeling, analyzing inpatient and outpatient data separately. Data for the private nonhospital-based program were analyzed separately.
For the purposes of this study, we defined before onset of the pandemic as January 1, 2018, through March 31, 2020. Visual inspection of the data and initial modeling indicated the potential for volumes leveling off or declining beginning in approximately the second year of the pandemic (ie, beginning May 2021); therefore, we defined the first year of the COVID-19 pandemic as April 2020 through April 2021, with COVID-19–related restrictions referring to April 2020 given the universal timing of school closures and stay-at-home orders. We defined the second year of the pandemic as May 2021, when volumes appeared to shift, through December 2021, our study end point. We tested for an immediate shift following restrictions (intercept) and allowed for a second shift following the first year after pandemic onset. We also tested for different slopes over time in the prepandemic onset period, the first year postpandemic onset, and second year postpandemic onset (interaction). Of note, the nonhospital-based ED program had admissions data available through November 2021 and care inquiry data through August 2021.
We performed 2 different analyses: (1) aggregated interrupted time series regression analysis to determine overall change in absolute total volume for the 14 hospital-based sites combined (and a similar model for the private nonhospital-based site separately) and (2) pooled analysis to examine overall mean and site-specific relative change within hospital-based sites. The pooled analysis used segmented mixed-effects negative binomial regression models to examine the changes in site-specific and overall mean volume over time as well as to specifically compare the time periods before onset of the pandemic, the first year after onset, and second year after onset of the pandemic. Pooled negative binomial model estimates were exponentiated and interpreted as a percent change. Models accounted for clustering by site over time using a heterogeneous autoregressive covariance structure and applied an offset for the reciprocal of the number of measurement months within a given period. Models included random intercepts for site as well as random coefficients for the immediate shift during each period as well as the change over time. All analyses were performed in SAS statistical software version 9.4 (SAS Institute) at an α level of P = .05. To maintain site confidentiality, we blinded site-specific results using an alphabetic code.
Results
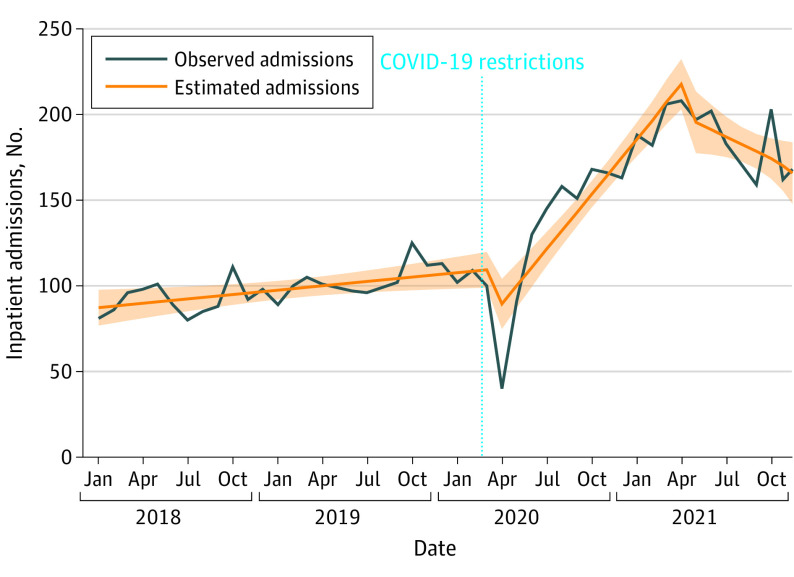
Inpatient Volume
Figure 1 shows the aggregate overall ED inpatient admission volume across sites over time. The aggregate total was 81 admissions in January 2018. Prior to the COVID-19 pandemic onset, admissions were increasing slightly over time by a mean of 0.85 (95% CI, 0.16-1.54) per month. In February 2020, the aggregate total inpatient ED admission volume was 109 admissions. In April 2020, there was a significant immediate decline of 30.6 (95% CI, −50.0 to −11.2) admissions, followed by a significant increase over time of a mean of 9.8 (95% CI, 7.66-12.0) admissions per month through April 2021. Beginning in May 2021, there was a nonsignificant immediate decline of 18.1 (95% CI, −44.1 to 8.12) admissions followed by a significant decrease over time of a mean of 5.08 (95% CI, −9.42 to −0.73) admissions per month through December 2021. The aggregate number of ED admissions across all sites reached 163 in December 2020, peaking at 208 in April 2021 with a mean of 181 per month through the last 8 months of 2021.
Figure 1. Aggregate Inpatient Eating Disorder Admissions Across 14 Sites Before and After Onset of the COVID-19 Pandemic .
Pooled results accounting for site showed that prior to the pandemic, inpatient ED-related admission volume was increasing by a mean of 0.7% (95% CI, 0.2%-1.3%) each month. In April 2020, there was a small, although not significant, immediate 14.6% decline (95% CI, −29.2% to 2.9%) on average in inpatient ED admissions followed by a significant 7.2% (95% CI, 4.8%-9.7%) per-month increase in volume on average through April 2021. Beginning in May 2021, there was an immediate, nonsignificant 15.5% decline (95% CI, −30.2% to 2.3%) in ED-related admissions followed by a significant decrease over time of 3.6% (95% CI, −6.0% to −1.1%) per month on average through December 2021. eFigure 1 in the Supplement shows model-estimated overall mean and site-specific observed and model-estimated number of inpatient ED admissions over time. Trends immediately after onset of the COVID-19 pandemic were highly variable by site; some sites saw a decline, while others did not and increases in the first year after onset were steeper for some sites than others. Site-specific trends in inpatient ED admission volumes over time are presented in eFigure 2 in the Supplement.
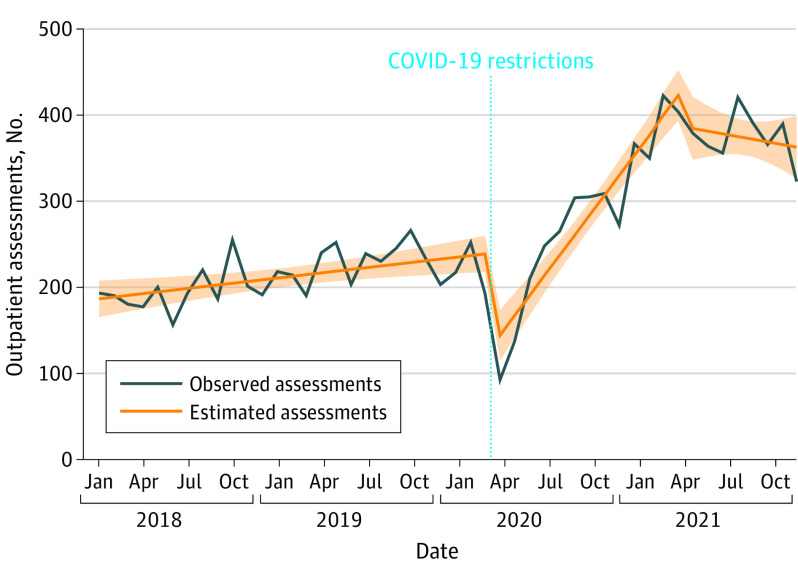
Outpatient Volume
Aggregate overall new outpatient ED assessment volume across sites over time is presented in Figure 2. Outpatient ED volume across sites totaled 195 assessments in January 2018. Prior to the COVID-19 pandemic, assessments were increasing slightly over time by 2.0 per month (95% CI, 0.62-3.40), and in February 2020, aggregate outpatient ED assessments totaled 254 assessments. In April 2020, there was an immediate decline of 118.1 (95% CI, −157.4 to −78.8) assessments. Subsequently, the number of new ED assessments increased significantly over time by a mean of 21.3 (95% CI, 16.9-25.7) per month through April 2021. Beginning in May 2021, there was an immediate nonsignificant decline of 35.5 (95% CI, −88.4 to 17.5) assessments followed by a nonsignificant decrease over time of a mean of 5.13 (95% CI, −13.9 to −3.68) assessments per month through December 2021. The aggregate number of assessments across all sites was 274 in December 2020, peaking at 425 in March 2021, and there was a mean of 376 per month through the last 8 months of 2021.
Figure 2. Aggregate Outpatient New Eating Disorder Assessments Across 14 Sites Before and After Onset of the COVID-19 Pandemic .
Pooled results accounting for site showed that before onset of the pandemic outpatient assessment volume was stable over time, increasing by a mean of 0.6% (95% CI, −0.2% to 1.4%) per month. Immediately postpandemic onset, outpatient ED assessment volume declined by 39.7% (95% CI, −50.4% to −26.7%) but then increased significantly over time by a mean of 8.1% (95% CI, 5.3%-11.1%) per month through April 2021. Starting in May 2021, there was a significant immediate decline of 22.0% (95% CI, −36.4% to −4.4%) in the number of assessments followed by a nonsignificant decrease over time of a mean of 1.5% (95% CI, −3.6% to 0.7%) per month through December 2021. eFigure 3 in the Supplement shows model-estimated overall mean and site-specific observed and estimated number of outpatient new ED assessments over time. There was variability seen from site to site immediately postpandemic onset; some sites saw dramatic declines in outpatient ED assessments and others saw very little change. Trends in outpatient new ED assessments over time for individual sites can be seen in eFigure 4 in the Supplement.
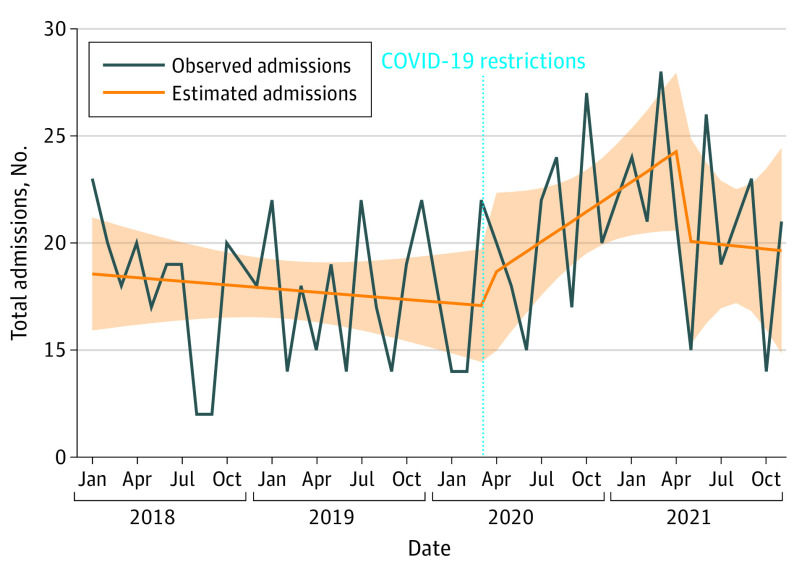
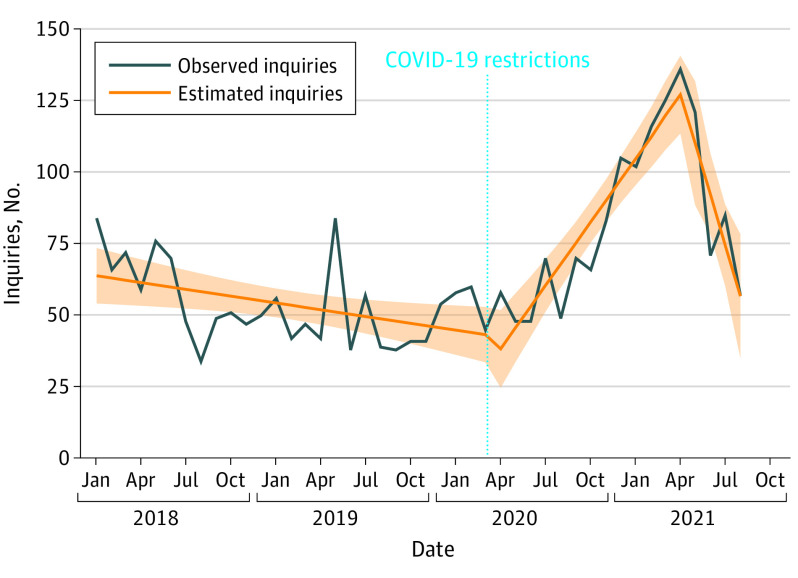
Nonhospital-Based Eating Disorder Program Volume
Total admissions at the nonhospital-based ED program were stable over time pre-pandemic (slope = −0.06 per month; 95% CI, −0.23 to 0.12) with no evidence of an immediate shift (slope = 1.12 per month; 95% CI, −3.79 to 6.02) or significant change over time in the first year after onset of the pandemic (slope = 0.52 per month; 95% CI, −0.03 to 1.07; Figure 3). Beginning in May 2021, there was a small but nonsignificant immediate decline of 4.2 (95% CI, −11.1 to 2.87) admissions with no evidence of a change over time through the end of the study period (slope = −0.015 admissions per month; 95% CI, −1.35 to 1.33; Figure 3). This pattern was similar for all levels of care. The total number of inquiries for care were declining slightly over time prepandemic (slope = −0.79 per month; 95% CI, −1.43 to −0.15). In April 2020, there was a nonsignificant decline of 12.3 (95% CI, −30.4 to 5.67) inquiries (Figure 4) followed by a significant increase in inquiries for care over time, with a mean of 8.2 (95% CI, 6.2-10.2) additional inquiries per month through April 2021. Starting in May 2021, there was no evidence of an immediate shift (slope = 0.86; 95% CI, −33.6 to 35.3); however, the number of inquiries decreased significantly over time by a mean of 17.0 (95% CI, −28.6 to −5.4) per month through the end of the study period (Figure 4).
Figure 3. Overall Admissions to a Single Nonhospital-Based Private Eating Disorder Program Before and After Onset of the COVID-19 Pandemic .
Figure 4. Overall Inquiries for Admission to a Single Nonhospital-Based Private Eating Disorder Program Before and After Onset of the COVID-19 Pandemic.
Discussion
We found marked increases in both inpatient and outpatient volumes of patients with EDs after onset of the COVID-19 pandemic, particularly within the first year, and our findings are in keeping with other single-site studies.21,22,23,24,25 These increases started to level off, and in some instances decline, in the second year of the pandemic; however, both ED-related inpatient admissions and new ED outpatient assessments remained above prepandemic baselines. To our knowledge, this is one of the only multisite studies to examine inpatient and outpatient changes in adolescent/young adult volume of patients with EDs before and after onset of the pandemic through the end of 2021.
While there was some site-to-site variation, overall, the volume of ED-related admissions and outpatient assessments declined immediately following the implementation of pandemic-related restrictions, which is not overall surprising. Local governments and health care facilities throughout the US put into effect shelter-in-place advisories and limitations on outpatient appointments after the onset of the pandemic, and there was widespread fear of contracting COVID-19 that may have impacted the number of patients presenting for admission.28 In the first year postpandemic onset, both inpatient and outpatient volumes of patients with EDs increased to above prepandemic levels, indicating that ED care needs were increasing. This contrasts with emerging literature suggesting that outpatient and emergency department visits for many other non-COVID-19–related diagnoses increased after an initial decline but remained below prepandemic baselines during 2020.29,30,31,32 Thus, ED-related care increases seem to represent a unique pandemic-associated trend. Our findings also indicate that in the second year after onset of the pandemic, both inpatient and outpatient ED volumes began to decline slightly but remained above prepandemic baselines. This suggests that while there may have been an improvement in the number of patients presenting for ED care, it may take quite some time for these numbers to return to prepandemic levels.
There was site-to-site variation in both inpatient and outpatient ED volume trends after onset of the pandemic, with some sites seeing sharper increases than others (eFigures 1-4 in the Supplement). This may be associated with geographic differences in access to ED care including the number of ED programs and practitioners with ED expertise, as well as local differences in pandemic response (eg, timing of mask mandates, school and business closures) and differences in the ability of sites to quickly accommodate greater numbers of patients.
The nonhospital-based program saw different patterns; there was not a significant change in numbers of admissions after onset of the pandemic compared with prepandemic. This may be because nonhospital-based ED programs cannot rapidly increase their number of beds to accommodate changing numbers, compared with medical hospitals that often have the ability to do so if needed. The nonhospital-based ED program did, however, see a significant increase in requests for care after onset of the pandemic, possibly demonstrating that need outpaced bed availability at that time. This portends a future of unmet need with respect to nonhospital-based ED program placement for patients.
We believe that our findings indicate that the current health care system for patients with EDs may quickly become overwhelmed by the pandemic-associated increase in volume of patients with EDs. Prepandemic, there was already a lack of available medical, nutrition, and mental health clinicians with specific ED-related training. Nonhospital-based ED programs frequently had waiting lists given limited space. With the rise in patients with EDs seeking care postpandemic onset, there has been further strain on systems already struggling to serve this vulnerable population. Our results show volumes starting to stabilize in the second year of the pandemic; however, recovery from EDs can take years, with patients at risk for relapses. Thus, the increases associated with the pandemic are likely to be of consequence for the foreseeable future. Timely diagnosis and treatment are essential for improved prognosis for patients with EDs. The scarcity of supports seen in association with the pandemic may lead to patients gaining access to care later than they should, which can increase the risk of medical hospitalizations for patients who have decompensated physically due to unchecked ED behaviors. While telehealth visits increased access for some patients, some patients with EDs may not benefit from this method and there were barriers for clinicians to adopting this method early on.12,33,34,35 In the future, increased access to outpatient ED assessments and ED program intakes could be made possible by a larger workforce with ED expertise; this increased access could help avoid medical hospitalizations and potentially shorten hospital stays as well.
Strengths and Limitations
From a strength standpoint, this study examined patterns of ED-related care volume in association with the COVID-19 pandemic in a geographically diverse sample with sites ranging in size. The inclusion of a nonhospital-based ED program allowed for a glimpse into the changes seen in program availability and inquiries for care associated with the pandemic. Additionally, our study was able to provide data focused on the adolescent/young adult population, who are especially vulnerable to lifelong problems if unable to access timely ED diagnosis and treatment.
There are limitations to this study. Because this study is observational in nature, we cannot determine causation from this type of study design. All sites had similar timing for shutdowns; however, reopening has varied by state and individual behavior influenced by state-by-state regulations could have affected volumes. Some sites may have caps on total admissions, which could underestimate potential increases in volume. Similarly, some sites may have had to divert pediatric patients to other hospitals to allow for available adult beds during the height of COVID-19 cases, a common practice across the country. Some hospital or program specific staffing and COVID-19 adaptations may have affected wait times for ED services. Although evidence supports a decrease in admissions for many common pediatric illnesses during the pandemic,30,31 this study did not specifically examine hospital admission totals compared with ED-specific admissions. Finally, the data presented in this article are summary volume data and we did not collect information on demographic characteristics, specific ED diagnosis, or severity. Therefore, we were unable to account for these risk factors associated with ED prevention and treatment or examine whether trends in volume were driven by certain diagnoses, severity, or demographic factors. This is important to consider in future studies examining the impact of the pandemic on patients with EDs.
Conclusions
In this study, programs serving adolescents and young adults with EDs had significant increases in both medical inpatient and outpatient volume after onset of the COVID-19 pandemic. These findings are critical for understanding potential effects of COVID-19 and to aid workforce and other planning essential for the management of long-term trends in volume and care of patients with EDs.
eFigure 1. Overall average and site-specific observed and model-estimated number of inpatient eating disorder admissions pre- and post-onset of the COVID-19 pandemic (N=14 sites)
eFigure 2. Number of inpatient eating disorder medical admissions by site pre- and post-onset of the COVID-19 pandemic (N=14 sites)
eFigure 3. Overall average and site-specific observed and model-estimated number of outpatient new eating disorder assessments pre- and post-onset of the COVID-19 pandemic (N=14 sites)
eFigure 4. Number of outpatient new eating disorder assessments by site pre- and post-onset of the COVID-19 pandemic (N=14 sites)
References
- 1.Harvard T.H. Chan School of Public Health. Report: economic costs of eating disorders. Published June 2020. Accessed October 3, 2022. https://www.hsph.harvard.edu/striped/report-economic-costs-of-eating-disorders/
- 2.Herpertz-Dahlmann B, Bonin E, Dahmen B. Can you find the right support for children, adolescents and young adults with anorexia nervosa: access to age-appropriate care systems in various healthcare systems. Eur Eat Disord Rev. 2021;29(3):316-328. doi: 10.1002/erv.2825 [DOI] [PubMed] [Google Scholar]
- 3.Herpertz-Dahlmann B. Adolescent eating disorders: update on definitions, symptomatology, epidemiology, and comorbidity. Child Adolesc Psychiatr Clin N Am. 2015;24(1):177-196. doi: 10.1016/j.chc.2014.08.003 [DOI] [PubMed] [Google Scholar]
- 4.Hudson JI, Hiripi E, Pope HG Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348-358. doi: 10.1016/j.biopsych.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galmiche M, Déchelotte P, Lambert G, Tavolacci MP. Prevalence of eating disorders over the 2000-2018 period: a systematic literature review. Am J Clin Nutr. 2019;109(5):1402-1413. doi: 10.1093/ajcn/nqy342 [DOI] [PubMed] [Google Scholar]
- 6.Hornberger LL, Lane MA; COMMITTEE ON ADOLESCENCE . Identification and management of eating disorders in children and adolescents. Pediatrics. 2021;147(1):e2020040279. doi: 10.1542/peds.2020-040279 [DOI] [PubMed] [Google Scholar]
- 7.Lin JA, Jhe G, Vitagliano JA, et al. The Association of Malnutrition, illness duration, and pre-morbid weight status with anxiety and depression symptoms in adolescents and young adults with restrictive eating disorders: a cross-sectional study. J Eat Disord. 2021;9(1):60. doi: 10.1186/s40337-021-00415-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nielsen S, Vilmar JW. What can we learn about eating disorder mortality from eating disorder diagnoses at initial assessment? a Danish nationwide register follow-up study using record linkage, encompassing 45 years (1970-2014). Psychiatry Res. 2021;303:114091. doi: 10.1016/j.psychres.2021.114091 [DOI] [PubMed] [Google Scholar]
- 9.Smink FRE, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep. 2012;14(4):406-414. doi: 10.1007/s11920-012-0282-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hossain MM, Tasnim S, Sultana A, et al. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020;9:636. doi: 10.12688/f1000research.24457.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu T, Jia X, Shi H, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2021;281:91-98. doi: 10.1016/j.jad.2020.11.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Termorshuizen JD, Watson HJ, Thornton LM, et al. Early impact of COVID-19 on individuals with self-reported eating disorders: a survey of ~1,000 individuals in the United States and the Netherlands. Int J Eat Disord. 2020;53(11):1780-1790. doi: 10.1002/eat.23353 [DOI] [PubMed] [Google Scholar]
- 13.Phillipou A, Meyer D, Neill E, et al. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: initial results from the COLLATE project. Int J Eat Disord. 2020;53(7):1158-1165. doi: 10.1002/eat.23317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scharmer C, Martinez K, Gorrell S, Reilly EE, Donahue JM, Anderson DA. Eating disorder pathology and compulsive exercise during the COVID-19 public health emergency: examining risk associated with COVID-19 anxiety and intolerance of uncertainty. Int J Eat Disord. 2020;53(12):2049-2054. doi: 10.1002/eat.23395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schlegl S, Maier J, Meule A, Voderholzer U. Eating disorders in times of the COVID-19 pandemic: results from an online survey of patients with anorexia nervosa. Int J Eat Disord. 2020;53(11):1791-1800. doi: 10.1002/eat.23374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodgers RF, Lombardo C, Cerolini S, et al. The impact of the COVID-19 pandemic on eating disorder risk and symptoms. Int J Eat Disord. 2020;53(7):1166-1170. doi: 10.1002/eat.23318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zeiler M, Wittek T, Kahlenberg L, et al. Impact of covid-19 confinement on adolescent patients with anorexia nervosa: a qualitative interview study involving adolescents and parents. Int J Environ Res Public Health. 2021;18(8):4251. doi: 10.3390/ijerph18084251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nutley SK, Falise AM, Henderson R, Apostolou V, Mathews CA, Striley CW. Impact of the COVID-19 pandemic on disordered eating behavior: qualitative analysis of social media posts. JMIR Ment Health. 2021;8(1):e26011. doi: 10.2196/26011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cooper M, Reilly EE, Siegel JA, et al. Eating disorders during the COVID-19 pandemic and quarantine: an overview of risks and recommendations for treatment and early intervention. Eat Disord. 2020;30(1):54-76. doi: 10.1080/10640266.2020.1790271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simone M, Emery RL, Hazzard VM, Eisenberg ME, Larson N, Neumark-Sztainer D. Disordered eating in a population-based sample of young adults during the COVID-19 outbreak. Int J Eat Disord. 2021;54(7):1189-1201. doi: 10.1002/eat.23505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haripersad YV, Kannegiesser-Bailey M, Morton K, et al. Outbreak of anorexia nervosa admissions during the COVID-19 pandemic. Arch Dis Child. 2021;106(3):e15. doi: 10.1136/archdischild-2020-319868 [DOI] [PubMed] [Google Scholar]
- 22.Otto AK, Jary JM, Sturza J, et al. Medical admissions among adolescents with eating disorders during the COVID-19 pandemic. Pediatrics. 2021;148(4):e2021052201. doi: 10.1542/peds.2021-052201 [DOI] [PubMed] [Google Scholar]
- 23.Schwartz MD, Costello KL. Eating disorder in teens during the COVID-19 pandemic. J Adolesc Health. 2021;68(5):1022. doi: 10.1016/j.jadohealth.2021.02.014 [DOI] [PubMed] [Google Scholar]
- 24.Asch DA, Buresh J, Allison KC, et al. Trends in US patients receiving care for eating disorders and other common behavioral health conditions before and during the COVID-19 pandemic. JAMA Netw Open. 2021;4(11):e2134913. doi: 10.1001/jamanetworkopen.2021.34913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin JA, Hartman-Munick SM, Kells MR, et al. The impact of the COVID-19 pandemic on the number of adolescents/young adults seeking eating disorder-related care. J Adolesc Health. 2021;69(4):660-663. doi: 10.1016/j.jadohealth.2021.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Forman SF, McKenzie N, Hehn R, et al. Predictors of outcome at 1 year in adolescents with DSM-5 restrictive eating disorders: report of the national eating disorders quality improvement collaborative. J Adolesc Health. 2014;55(6):750-756. doi: 10.1016/j.jadohealth.2014.06.014 [DOI] [PubMed] [Google Scholar]
- 27.Forman SF, Grodin LF, Graham DA, et al. ; National Eating Disorder QI Collaborative . An eleven site national quality improvement evaluation of adolescent medicine-based eating disorder programs: predictors of weight outcomes at one year and risk adjustment analyses. J Adolesc Health. 2011;49(6):594-600. doi: 10.1016/j.jadohealth.2011.04.023 [DOI] [PubMed] [Google Scholar]
- 28.Moreland A, Herlihy C, Tynan MA, et al. ; CDC Public Health Law Program; CDC COVID-19 Response Team, Mitigation Policy Analysis Unit . Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement: United States, March 1-May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(35):1198-1203. doi: 10.15585/mmwr.mm6935a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nourazari S, Davis SR, Granovsky R, et al. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am J Emerg Med. 2021;42:203-210. doi: 10.1016/j.ajem.2020.11.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pelletier JH, Rakkar J, Au AK, Fuhrman D, Clark RSB, Horvat CM. Trends in US pediatric hospital admissions in 2020 compared with the decade before the COVID-19 pandemic. JAMA Netw Open. 2021;4(2):e2037227. doi: 10.1001/jamanetworkopen.2020.37227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mehrotra A, Chernew ME, Linetsky D, Hatch H, Cutler DA, Schneider EC. The impact of COVID-19 on outpatient visits in 2020: visits remained stable, despite a late surge in cases. The Commonwealth Fund. Published February 22, 2021. Accessed November 15, 2021. https://www.commonwealthfund.org/publications/2021/feb/impact-covid-19-outpatient-visits-2020-visits-stable-despite-late-surge
- 32.Hartnett KP, Kite-Powell A, DeVies J, et al. ; National Syndromic Surveillance Program Community of Practice . Impact of the COVID-19 pandemic on emergency department visits: United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699-704. doi: 10.15585/mmwr.mm6923e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Datta N, Derenne J, Sanders M, Lock JD. Telehealth transition in a comprehensive care unit for eating disorders: challenges and long-term benefits. Int J Eat Disord. 2020;53(11):1774-1779. doi: 10.1002/eat.23348 [DOI] [PubMed] [Google Scholar]
- 34.Shaw H, Robertson S, Ranceva N. What was the impact of a global pandemic (COVID-19) lockdown period on experiences within an eating disorder service? a service evaluation of the views of patients, parents/carers and staff. J Eat Disord. 2021;9(1):14. doi: 10.1186/s40337-021-00368-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brothwood PL, Baudinet J, Stewart CS, Simic M. Moving online: young people and parents’ experiences of adolescent eating disorder day programme treatment during the COVID-19 pandemic. J Eat Disord. 2021;9(1):62. doi: 10.1186/s40337-021-00418-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Overall average and site-specific observed and model-estimated number of inpatient eating disorder admissions pre- and post-onset of the COVID-19 pandemic (N=14 sites)
eFigure 2. Number of inpatient eating disorder medical admissions by site pre- and post-onset of the COVID-19 pandemic (N=14 sites)
eFigure 3. Overall average and site-specific observed and model-estimated number of outpatient new eating disorder assessments pre- and post-onset of the COVID-19 pandemic (N=14 sites)
eFigure 4. Number of outpatient new eating disorder assessments by site pre- and post-onset of the COVID-19 pandemic (N=14 sites)