Abstract
Background: Elective culinary medicine education has become popular to help fill important gaps in physician nutrition training. The implementation and outcomes among the inaugural cohort of medical students who received culinary medicine training as a required component of medical school curriculum at the University of Maryland School of Medicine are described. Methods: Following a series of elective pilot sessions, culinary medicine training was provided to all first-year medical students in the 2019-2020 academic year. The 3-hour training included evidence-based nutrition lecture, cooking simple recipes, and group discussion of the application to personal and patient care. Pre-/postsession questionnaires assessed nutrition knowledge, skills, and attitudes as well as nutritional counseling confidence. Paired t-tests estimated mean differences in outcomes pre- and posttraining. Qualitative data were subjected to thematic analysis. Results: Overall, 119 of 125 (95.2%) students provided pre- and posttraining outcomes data. All nutritional and patient counseling outcomes improved (P < .05). Themes of being better prepared to address healthy eating barriers in patient care and personal ability to make healthy dietary changes were noted in qualitative analysis. Conclusion: One session of culinary medicine training in core medical student curriculum was feasible and improved medical student nutrition knowledge, skills, and attitudes and confidence in patient nutrition counseling.
Keywords: culinary medicine, nutrition education, Mediterranean diet, plant-based diet, paleolithic diet, low-fat diet, low-carbohydrate diet
‘. . . current medical practice and education do not adequately reflect the important role of the physician in nutritional aspects of patient care.’
The 2019 Global Burden Disease Study of 195 countries revealed that poor diet quality is the greatest risk factor for mortality, surpassing even the health burden of smoking.1-3 It has been estimated that 20% of deaths worldwide could potentially be prevented with improved dietary habits, highlighting the global need for improved dietary education and intervention. 1 A great deal of nutrition research has accordingly focused on dietary approaches to reduce the risk and mitigate the symptoms of chronic disease. Systematic reviews and meta-analysis of randomized control trials have revealed that a variety of dietary approaches, including low-fat, low-carbohydrate, plant-based, paleolithic, and Mediterranean diets, can improve lipid profiles; decrease systolic and diastolic blood pressure; reduce markers of inflammation; lower weight among obese and overweight adults; reduce the risk of cancers, cognitive decline, and frailty; lower cardiovascular disease incidence and mortality, and decrease risk of all-cause mortality.4-13
Despite this extensive evidence base supporting numerous dietary approaches to help mitigate the burden of chronic disease, current medical practice and education do not adequately reflect the important role of the physician in nutritional aspects of patient care. Only 29% of US medical schools met the minimum 25 hours of required nutrition education. 14 On average, medical students receive only 19 hours of nutrition training over their 4 years in medical school. Furthermore, the majority of the curricular hours in most institutions in the United States emphasize nutritional biochemistry and nutrient-deficiency disorders, which while important, do not address the pressing needs of chronic disease prevention and management in clinical care.15-17 This dilemma persists into residency and fellowship training, where nutrition education is either minimal or completely absent. Nutrition education is not included in the 2018 Accreditation Council for Graduate Medical Education Common Program Requirements for residency and fellowship.15,17,18 The trend of meager incorporation of nutrition into medical practice continues with practicing physicians. A 2017 survey of cardiologists revealed that the majority of participating physicians felt that their nutrition training was inadequate (90%) and that such training was a personal responsibility (95%). 19
A number of barriers to improving nutrition education in medical training have been identified. These include a perceived lack of interest and expertise among faculty members in nutrition, few opportunities created for nutritional counseling during clinical years, and a general lack of curricular priority for nutrition training. 20 Medical students across the globe, including in the United States, Europe, Middle East, Africa, Australia, and New Zealand, consequently do not perceive themselves to have adequate nutrition knowledge and confidence in nutrition counseling. 21 Interest in nutrition has been shown to be high among incoming medical students, but often wanes by the time of graduation22,23. This is likely attributable in part to the fact that medical students receive limited clinically relevant nutrition education in the core curriculum and their preceptors rarely include nutritional interventions into care plans throughout their training.
Culinary medicine, which combines evidence-based nutritional education with experiential group cooking instruction based on the lecture, has become increasingly popular at medical schools across the United States to help fill these training gaps. Medical students who received experiential culinary medicine education at numerous academic medical institutions, including Tulane University, Stanford University, the University of Pennsylvania, the University of Southern California, UT Southwestern, and Texas Tech University among others, have demonstrated improvements in nutrition knowledge, skills, and attitudes for both patient care and self-care as well as improved personal dietary habits.24-36 In light of the promise of these findings across numerous institutions, a culinary medicine curriculum for health care professionals has been published recently. 37
While promising and serving as the inspiration for this study, most culinary medicine training is offered on an elective basis and no data have been published on culinary medicine as part of the core medical student curriculum to the authors’ knowledge. This article reports on the implementation, curricular content, and mixed methods outcomes evaluation from the first cohort of first-year medical students at the University of Maryland School of Medicine (UMSOM) receiving culinary medicine as a component of core medical student curriculum.
Methods
Pilot and Implementation Process of Incorporating Culinary Medicine Training Into Core Medical Student Curriculum
In light of the challenge of securing new educational content into the core curriculum of most medical schools, the culinary medicine training was first piloted in the 2018-2019 academic year on an elective, noncredit basis among a group of 12 second- and third-year medical students interested in nutrition.
Two sessions were offered to the medical students participating in the pilot training. Each session was 3 hours in length and was offered at the teaching kitchen of the Institute for Integrative Health, a community-based nonprofit in Baltimore that had previously been involved in nutrition research.38-42 The training featured evidence-based nutrition instruction, group cooking of recipes based on the concepts of the lecture, and eating the prepared meals together while discussing the potential application of the training to both patient care and the students’ self-care.
The lecture featured a practical overview of nutrients and foods that contain them, an introduction to the concept of “nutrient density” that can accommodate many seemingly conflicting popular dietary approaches (eg, Mediterranean, low-fat, low-carbohydrate, plant-based, paleolithic), practical methods to overcome barriers to healthy eating, and a focus on published evidence on plant-based and paleolithic diets. Plant-based and paleolithic diets were selected for the pilot due to both the popularity and the many misconceptions and perceived conflicts among these 2 dietary approaches. As a demonstration of the core commonalities among the seemingly conflicting popular diets when approached through a more unifying lens of nutrient density, one of the two meals that was cooked in the pilot training (consisting of portobello mushrooms steaks, cauliflower fried rice, and chocolate avocado mousse) satisfied the tenets of both plant-based and paleolithic approaches.
The pilot culinary medicine training was well-received by participating students and the positive feedback was conveyed by several of the medical students who had participated to the course directors of the Introduction to Clinical Medicine courses in the core curriculum at UMSOM. This student advocacy was accompanied by faculty advocacy, including a presentation by the faculty leader of the culinary medicine training to the UMSOM Medical Education Committee describing the evidence supporting culinary medicine at other institutions, the content of the culinary medicine pilot training, and the positive reception of the training that had been noted among participating medical students at UMSOM.
This multifaceted student and faculty advocacy culminated in a decision to offer 2 sessions of culinary medicine for first-year medical students in the Introduction to Clinical Medicine course during the 2019-2020 academic year.
Delivery and Content of Culinary Medicine Training in Core Medical Student Curriculum
A single 3-hour culinary medicine training session was offered in the first few weeks of the first-year medical student core curriculum. The structure of this culinary medicine training was identical to that of the successful pilot training. The session consisted of evidence-based nutrition lecture, followed by group cooking of 3 recipes based on the lecture content, followed by eating the meal together and group discussion on the potential applications of the training to patient care and self-care.
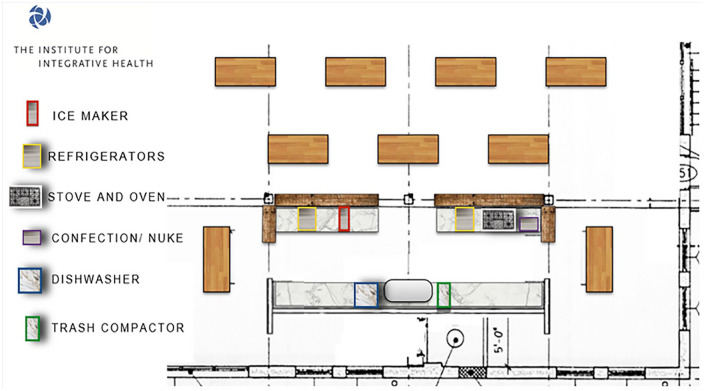
The 125 first-year medical students at UMSOM were split into 5 separate classes of 25 students for the culinary medicine training. The lecture was provided to all students in each class as a group. Students cooked in groups of 5 students. This class and cooking group size was deemed to be feasible to accommodate the footprint and equipment of the teaching kitchen (see Figure 1) and to allow for an environment conducive for active participation in group discussion.
Figure 1.
Layout of the teaching kitchen at the Institute for Integrative Health where culinary medicine training was offered.
The 1-hour lecture was provided by the UMSOM faculty lead of the culinary medicine training and included basic concepts of human nutrition (macronutrients, micronutrients, etc), introduction to the concept nutrient density as a unifying approach to accommodate the supportive evidence of numerous seemingly conflicting popular diets, practical ways to address common barriers to healthy eating (eg, time, taste, and cost), and a specific focus on Mediterranean diets. The Mediterranean diets lecture content included description of the philosophy, practical implementation, common misconceptions, and clinical evidence supporting this dietary approach. Mediterranean diets were chosen as the focus for the session due to the abundance of evidence in systematic reviews and meta-analyses supporting human health, the previous success with this dietary approach in an elective medical student course at the University of Pennsylvania School of Medicine, 35 as well as the relatively high compliance of the diet noted in systematic reviews among adults and children,43,44 making it a feasible option for both the medical students and their future patients.
Following the lecture, students then split into groups of 5 to prepare a 3-course meal inspired by the particular dietary approach of focus. A basic cooking primer, including kitchen safety, kitchen tools introduction, and knife skills was provided in the first session prior to the preparation of the meals. The cooking instruction was led by personnel from the UMSOM, the Institute for Integrative Health, and Maryland University of Integrative Health. In light of the importance of cost as a barrier to healthy eating among students45-48 and the disproportionately high burden of diet- and lifestyle-related chronic disease among economically underserved49-54 patients that many of the students would ultimately be treating, the cost of the meal (consisting primarily of frozen salmon, vegetables, and berries) was less than $10.
After the meals were prepared, the students then reassembled as a full group to eat meals together and participate in group discussion with the UMSOM faculty leader of the training to discuss their experiences with the training and potential applications to clinical and self-care. In order to provide visual context, Figure 2 provides pictures of the medical students cooking in the teaching kitchen, a meal that was prepared by a student, and the group discussion with UMSOM faculty.
Figure 2.
Photographs of a medical student pilot session, cooking instruction, medical students cooking, group discussion and eating together, and a meal that a medical student prepared.
Outcomes Evaluation
Approval was obtained by the institutional review board of the UMSOM to conduct a mixed-methods outcomes evaluation of the first year of core curriculum culinary medicine training.
Pre- and posttraining quantitative questionnaires and open-ended qualitative questions were administered to all 125 first-year medical students. Two additional survey questions reflecting on the applicability of the culinary medicine training to patient care and self-care, with open-ended options to elaborate, were asked only at the posttraining assessment.
The questionnaires assessed a variety of nutrition knowledge, skills, and attitudes as well as specific understanding of the evidence and application of the Mediterranean diets that were the dietary approach of focus of the session. Students were also asked how prepared they felt to help patients overcome 5 common barriers to healthy eating: lack of confidence in ability to prepare healthy food, overcoming food cravings, challenge of eating healthy on a budget, perception of insufficient time to eat healthy, and palatability of eating healthy without excessive added sugar or salt. All questionnaire and qualitative responses were deidentified prior to statistical analysis.
Statistical Methods
Surveys were scored on a 1 to 5 Likert-type scale for the various preparation, knowledge, and confidence domains that were assessed (eg, “very prepared,” “prepared,” “somewhat prepared,” “not prepared,” “not at all prepared”).
Student responses were deidentified and pre- and postsession responses to each question were compared. Paired t-tests were employed to estimate mean differences in pre-/postsession outcomes. Folded F tests were utilized to compare the pre-/postsession variance in outcomes to evaluate potential changes in the discrepancies in baseline nutrition knowledge, skills, and attitudes and patient nutrition counseling confidence on entering medical school.
Survey responses were also collapsed into dichotomous preparation, knowledge, and confidence categories (eg, “at least somewhat knowledgeable” [consisting of “very knowledgeable,” “knowledgeable,” and “somewhat knowledgeable”] vs. “not knowledgeable” [consisting of “not at all knowledgeable” and “not knowledgeable”].
This dichotomous categorization of the study outcomes was in accordance with the goal of this brief 3-hour training to provide basic knowledge, preparation, and confidence in nutrition counseling and self-care, with opportunities for further development in additional culinary medicine training currently being offered in subsequent years of medical school. The pre-/posttraining relative risk (RR) of being at least somewhat knowledgeable, confident, or prepared was calculated for each survey question.
Statistical significance was defined as P < .05. All statistical analyses were performed in SAS Version 9.4.1 (SAS Institute). Qualitative data were subjected to thematic analysis.
Results
Pre– and post–culinary medicine training outcomes data were collected from 119 of 125 (95.2%) UMSOM first-year students. The class was 61.4% female, 56.6% White, 26.2% Asian, 11.7% Black or African American, and 5.5% other race/not reported, and mean age 23.8 years.
The pre– and post–culinary medicine training questionnaire responses and statistical comparison of mean changes are provided in Table 1. Statistically significant improvements were noted in mean scores of all survey questions, spanning the entirety of the nutrition knowledge, skills, and attitudes as well as patient nutrition counseling confidence that were assessed (P < .0001). There was also a statistically significant decrease in the variance of all survey questions after the culinary medicine training (P < .02), reflecting a reduction in the baseline disparity in nutrition knowledge, skills, and attitudes and patient nutrition counseling confidence among incoming medical students.
Table 1.
Questions Assessing Perceived Nutrition Preparation, Confidence, and Knowledge in Clinical Care.
| Question | Pretraining (n = 119) | Posttraining (n = 125) | P a | ||
|---|---|---|---|---|---|
| Frequency (%) | Mean (SD) | Frequency (%) | Mean (SD) | ||
| How prepared do you feel you are to provide healthy eating recommendations to patients in clinical care? | |||||
| Very prepared | 6 (5.0) | 3.25 (0.83) | 15 (12.0) | 3.78 (0.67) | <.0001 |
| Prepared | 40 (33.6) | 69 (55.2) | |||
| Somewhat prepared | 52 (43.7) | 39 (31.2) | |||
| Not prepared | 20 (16.8) | 2 (1.6) | |||
| Not at all prepared | 1 (0.8) | 0 (0.0) | |||
| How confident are you in your ability to make healthy dietary recommendations that accommodate varying patient food preferences? | |||||
| Very confident | 3 (2.5) | 2.9 (0.87) | 9 (7.2) | 3.6 (0.70) | <.0001 |
| Confident | 22 (18.5) | 59 (47.2) | |||
| Somewhat confident | 57 (47.9) | 51 (40.8) | |||
| Not confident | 30 (25.2) | 6 (4.8) | |||
| Not at all confident | 7 (5.9) | 0 (0.0) | |||
| How knowledgeable are you with the clinical evidence, practical application, and misconceptions surrounding popular diets? | |||||
| Very knowledgeable | 5 (4.2) | 2.82 (0.89) | 15 (12.0) | 3.61 (0.71) | <.0001 |
| Knowledgeable | 17 (14.3) | 55 (44.0) | |||
| Somewhat knowledgeable | 54 (45.4) | 46 (36.8) | |||
| Not knowledgeable | 37 (31.1) | 9 (7.2) | |||
| Not at all knowledgeable | 6 (5.0) | 0 (0.0) | |||
| How knowledgeable are you with the clinical evidence, practical applications, and misconceptions of the Mediterranean diet, in particular? | |||||
| Very knowledgeable | 2 (1.7) | 2.26 (0.90) | 15 (12.0) | 3.74 (0.69) | <.0001 |
| Knowledgeable | 7 (5.9) | 66 (52.8) | |||
| Somewhat knowledgeable | 34 (28.6) | 41 (32.8) | |||
| Not knowledgeable | 53 (44.5) | 3 (2.4) | |||
| Not at all knowledgeable | 23 (19.3) | 0 (0.0) | |||
P values determined by paired t tests.
No medical students reported being “not at all” knowledgeable, prepared, or confident in any of the nutrition domains assessed after the culinary medicine training, as contrasted with 4.7% of responses of being “not at all” knowledgeable, prepared, or confident prior to the training. Questions assessing preparation to address common barriers to healthy eating among patients are provided in Table 2. Table 3 provides the frequencies of the dichotomous outcomes as well as the RR of being at least somewhat knowledgeable, prepared, or confident after the culinary medicine training. There was an increased pre-/posttraining RR of being at least somewhat knowledgeable, prepared, or confident in each of the nutrition domains that were assessed (RR > 1.83, P < .0001).
Table 2.
Questions Assessing Preparation to Address Common Barriers to Healthy Eating Among Patients.
| How prepared do you feel you are to help patients overcome the following common barriers to healthy eating: | Pretraining (n = 119) | Posttraining (n = 125) | P a | ||
|---|---|---|---|---|---|
| Frequency (%) | Mean (SD) | Frequency (%) | Mean (SD) | ||
| 1. Lack of patient confidence in ability to prepare healthy food | |||||
| Very prepared | 2 (1.7) | 2.95 (0.80) | 13 (10.4) | 3.70 (0.70) | <.0001 |
| Prepared | 26 (21.8) | 65 (52.0) | |||
| Somewhat prepared | 58 (48.7) | 43 (34.4) | |||
| Not prepared | 30 (25.2) | 4 (3.2) | |||
| Not at all prepared | 3 (2.5) | 0 (0.0) | |||
| 2. Unwillingness to give up unhealthy foods that the patient craves | |||||
| Very prepared | 2 (1.7) | 2.91 (0.91) | 12 (9.6) | 3.65 (0.71) | <.0001 |
| Prepared | 32 (26.9) | 62 (49.6) | |||
| Somewhat prepared | 45 (37.8) | 46 (36.8) | |||
| Not prepared | 34 (28.6) | 5 (4.0) | |||
| Not at all prepared | 6 (5.0) | 0 (0.0) | |||
| 3. Belief that eating healthy on a budget is impossible | |||||
| Very prepared | 9 (7.6) | 3.27 (0.92) | 14 (11.2) | 3.67 (0.74) | .0002 |
| Prepared | 41 (34.5) | 62 (49.6) | |||
| Somewhat prepared | 44 (37.0) | 43 (34.4) | |||
| Not prepared | 23 (19.3) | 6 (4.8) | |||
| Not at all Prepared | 2 (1.7) | 0 (0.0) | |||
| 4. Perception of insufficient time to eat healthy | |||||
| Very prepared | 6 (5.0) | 3.16 (0.86) | 21 (16.8) | 3.79 (0.74) | <.0001 |
| Prepared | 35 (29.4) | 60 (48.0) | |||
| Somewhat prepared | 52 (43.7) | 41 (32.8) | |||
| Not prepared | 24 (20.2) | 3 (2.4) | |||
| Not at all prepared | 2 (1.7) | 0 (0.0) | |||
| 5. Flavor enhancement without excessive sugar or salt | |||||
| Very prepared | 9 (7.6) | 3.13 (0.90) | 21 (16.8) | 3.76 (0.78) | <.0001 |
| Prepared | 29 (24.4) | 58 (46.4) | |||
| Somewhat prepared | 49 (41.2) | 41 (32.8) | |||
| Not prepared | 32 (26.9) | 5 (4.0) | |||
| Not at all prepared | 0 (0.0) | 0 (0.0) | |||
P values determined by paired t tests.
Table 3.
Relative Risk of Medical Students Reporting Being at Least Somewhat Knowledgeable/Confident/Prepared in Nutritional Domains Before and After Culinary Medicine Training.
| Question | Relative risk at least somewhat knowledgeable/confident/prepared | 95% confidence interval | P a |
|---|---|---|---|
| How prepared do you feel you are to provide healthy eating recommendations to patients in clinical care? | 2.06 | [1.70, 2.50] | <.0001 |
| How confident are you in your ability to make healthy dietary recommendations that accommodate varying patient food preferences? | 2.11 | [1.71, 2.59] | <.0001 |
| How knowledgeable are you with the clinical evidence, practical application, and misconceptions surrounding popular diets? | 2.09 | [1.69, 2.59] | <.0001 |
| How knowledgeable are you with the clinical evidence, practical applications, and misconceptions of the Mediterranean diet, in particular? | 3.69 | [2.84, 4.79] | <.0001 |
| How prepared do you feel you are to help patients overcome the following common barriers to healthy eating: | |||
| 1. Lack of patient confidence in ability to prepare healthy food | 2.15 | [1.76, 2.61] | <.0001 |
| 2. Unwillingness to give up unhealthy foods that the patient craves | 2.24 | [1.83, 2.74] | <.0001 |
| 3. Belief that eating healthy on a budget is impossible | 1.83 | [1.45, 2.30] | <.0001 |
| 4. Perception of insufficient time to eat healthy | 2.07 | [1.70, 2.52] | <.0001 |
| 5. Flavor enhancement without excessive sugar or salt | 2.06 | [1.68, 2.53] | <.0001 |
P values determined via chi-square tests.
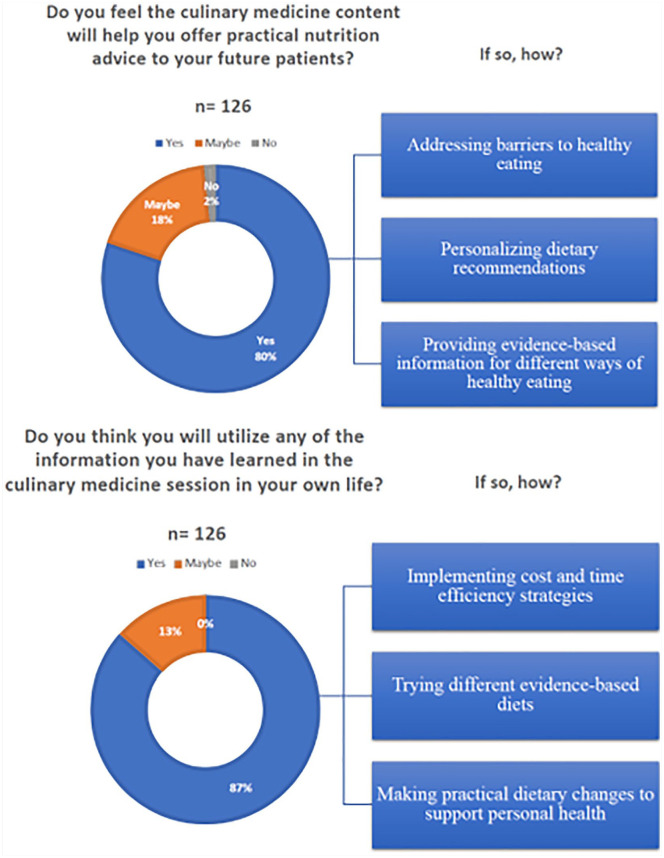
Several themes emerged from the qualitative data analysis as depicted visually in Figure 2. In brief, when asked “How will you offer practical nutrition advice to your future patients?” 3 key themes were revealed: (1) addressing barriers to healthy eating, (2) personalizing dietary recommendations, and (3) providing evidence-based information for different ways of healthy eating.
Addressing barriers to healthy eating was characterized by the students’ increased sense of preparation, confidence, and comfort in addressing possible barriers to healthy eating such as misconceptions about popular diets, how to make healthy food flavorful with spices and herbs and basic cooking techniques, and food access and other equity issues. Personalizing dietary recommendations was evident in student reporting that they felt they can better relate and connect to patients and their unique dietary obstacles. Providing evidence-based information supporting various ways of eating was marked by the ability of the students to provide their patients broad guidelines for healthy eating, understand and explain different dietary approaches to patients, and offer strategies to transition from unhealthy familiar ways of eating.
Some relevant quotes that reflect the themes are as follows:
I learned about the real-life barriers to accessing or switching diets, which helped frame the perspective of future patients so that I can better address their needs and concerns. The training also provided practical solutions to getting affordable fresh produce and making tasty meals that patients will enjoy to improve their health.
There is so much information out there online about what you should be eating and why. It is helpful to be able to discern the pros/cons of “strict” diets. The more nutrition training we have, the better we can personalize recommendations to patients. Diet cannot just prevent illness but also help one heal from it, and as physicians we should be fully equipped to advise our patients on how to maximize their health.
When posed with the question “How do you think you will utilize the information you have learned in the culinary medicine session in your own life?,” 3 key themes emerged: (1) implementing cost and time efficiency strategies, (2) trying different evidence-based diets, and (3) making practical dietary changes to support personal health.
Implementing cost- and time-efficiency strategies was hallmarked by feelings that healthy eating on a student’s budget and with limited time were major barriers. Students commonly expressed that they learned practical tactics and prioritized addressing both of these barriers in their own lives. Trying different evidence-based diets was marked by a commonly expressed desire to experience which nutrient-dense approach would resonate best with them and how their own body would respond to different methods. Making practical changes to support their health was reflected in basic strategies such as carefully reading the nutrition label before buying a product, using spices and herbs to enhance the taste of healthy food, and knowing how to prioritize healthy food shopping while on limited budgets.
These themes are reflected in the following student quotes:
It’s helpful to be reminded that the quality of food matters so much for our overall health—there is so much focus on maintaining a “caloric deficit” to lose weight, it is easy to lose sight of the fact that food provides us with vital nutrients that we can’t produce ourselves.
One of the barriers to healthy eating that I face is time, both the time necessary to cook food and also how long fresh produce lasts after purchase. Buying frozen foods in bulk (eg, vegetables) and also cooking in bulk and storing for later are skills I plan to apply to my own life.
Discussion
The incorporation of a single session of culinary medicine training into the core curriculum of first-year medical students at the UMSOM was feasible, well-accepted, and associated with improvements in medical student nutrition knowledge, skills, and attitudes as well as confidence in providing nutrition counseling to patients. Pre-/posttraining improvements were noted in mean scores of all nutrition questionnaires and themes of being better prepared to address barriers to healthy eating in patient care, familiarity with numerous evidence-based popular diets to provide a variety of choices for patients to eat healthier diets, and confidence to make healthy eating behavior changes in the medical students’ personal lives were revealed in qualitative analysis. It was particularly encouraging that no medical students reported being not at all knowledgeable, prepared, or confident in any of the nutritional outcomes assessed after the single culinary medicine session.
The ultimate goals of the 3-hour training session were 2-fold. The first goal was to offer sufficient practical nutrition knowledge and skills in the limited time available in core curriculum to fill well-established nutritional training gaps and prepare future physicians for basic nutrition counseling at the point of clinical care. The decreases in the variance of all questionnaire scores and increases in being at least somewhat knowledgeable, prepared, and confident in all domains assessed further reflect attainment of the goal of basic nutrition counseling competency. More intensive elective training in culinary medicine similar to those offered at other academic medical institutions is being planned for the third and fourth years of medical students who may choose to focus on nutrition in clinical practice or research. The intention of this training was to provide enough basic instruction to all medical students to confidently address common nutritional concerns in patient care. While nutritional biochemistry plays an important role in physician understanding of health and disease, patients are more likely to inquire about the many seemingly conflicting popular diets that are recommended to them by acquaintances outside of the clinic or that they encounter online. Many patients often begin such popular diets without any communication with their physician. This can be problematic as popular diets are often implemented improperly, and in some cases, may be inappropriate for the patient’s health status. Thus, the training was intended to familiarize future physicians with the basic tenets and clinical evidence supporting a variety of the most popular diets (low-fat, low-carbohydrate, plant-based, and paleolitihic) while provided more in-depth analysis of Mediterranean diets, due to the robust evidence base and versatility of this dietary approach for most patients.
The second goal of the culinary medicine training was to equip the medical students at the onset of medical school with practical strategies to eat healthy diets that they could carry with them throughout the course of their medical training. Medical school has been established in many previous studies to be physically and psychologically stressful for many students. 55 This level of distress can negatively affect students’ personal and professional lives by contributing to poor academic performance, increased dropout rates from medical school, broken relationships, substance abuse, burnout, depressive symptoms, suicide, depersonalization, as well as a reduced quality of patient care.56,57 Healthy eating and other self-care modalities have been shown to help reduce this stress among medical students.55,58 Higher adherence to nutrient-dense diets has been associated with lower depression risk and higher positive emotional state and more resilience to stress, while lower fruit and vegetable intake has been associated with a higher Perceived Stress Score.59-61 The strategies presented in the culinary medicine training for overcoming patient barriers to healthy eating—including time, taste, and cost—are also applicable to medical students and were communicated as being relevant to their own lives. The importance of overcoming barriers to healthy eating, both among medical students themselves and future patients, were common topics of conversation when eating meals together. The increased confidence engendered in the medical students’ ability to cook simple, healthy, and flavorful recipes after cooking the Mediterranean meal together was reflected in the improved questionnaire outcomes and qualitative data.
The results of this first outcomes evaluation of culinary medicine training offered as a component of core medical student education are aligned with previously published data of culinary medicine education that was offered on an elective basis.24-36 It is encouraging that the improvements that have consistently been noted in nutrition knowledge, skills, and attitudes and increased confidence in nutritional patient counseling and personal ability to eat a healthy diet while in medical school appear to extend beyond self-selected populations of medical students who elected to receive more intensive culinary medicine training. More benefit is likely to be seen with repeated exposures and reinforcement with more training sessions, but these findings in a single session of training reduce some of the potential for selection bias and extend the generalizability of previous work to medical students at large in core curriculum.
While the delivery model of a single 3-hour culinary medicine session incorporated into core curriculum is likely to be feasible in other academic medical settings, there are several limitations to the replicability and inference of the results of this study that are worthy of mention. One key limitation is that most medical schools do not have a dedicated teaching kitchen. However, extensive on-site kitchen equipment is not necessary at the medical school to offer this type of training. In fact, UMSOM does not have a teaching kitchen and the pilot culinary medicine training was held within the basement of a local office building. There are also community kitchens, similar to that of the Institute for Integrative Health where the training was offered, located within reasonable proximity of many academic medical centers. Even within the well-equipped teaching kitchen in this training, the primary pieces of equipment utilized for the class were widely accessible portable induction burners, food processors, and blenders predominantly used at portable group cooking stations (see Figure 3).
Figure 3.
Culinary medicine posttraining questionnaire responses and qualitative themes.
Another limitation related to the feasibility of culinary medicine training when offered in core medical student curriculum are the costs of food, kitchen materials, kitchen space, and preparation time for large cohorts of students. These costs can be contained through several measures. The Institute for Integrative Health donated the kitchen space for the training, which may be a feasible option at other community-kitchens. The cost of food was limited by cooking bulk-purchased and frozen salmon, vegetables, berries, and other ingredients. The cost of the entire meal was intentionally designed to be less than $10 (approximately $8) to demonstrate the economic feasibility for both students and future patients. Graduate students in nutrition and dietetics with required hours for licensure volunteered to assist with the preparation of meals and cooking instruction. Finally, making video recording of the cooking instruction available to students may help further reduce the cost of food and other ingredients for a large cohort of medical students. COVID-19 has required remote delivery of the culinary medicine curriculum to first-year medical students thus far in the 2020-2021 academic year. While outcomes data from the remote culinary medicine training are still being collected, the resources required have been reduced considerably, the training has been well-accepted by students, and the live Q&A via video conferencing has been similarly as engaging as in-person. Collectively, these strategies helped limit the cost of training and other measures are being explored.
There are also several limitations related to the pilot outcomes evaluation of the training. To the authors’ knowledge, there are no previously validated metrics available to assess medical student knowledge, nutrition, and attitudes toward nutrition counseling in patient care. As such, a relatively brief set of questions utilizing a 5-point Likert-type scale was created to evaluate changes in these areas before and after the culinary medicine training. A related limitation is the lack of long-term follow up data to determine whether the improvements noted in nutrition knowledge, skills, and attitudes specific to patient counseling and increased personal confidence to eat healthy while in medical school persist over time. Longitudinal evaluation of changes in these important areas is underway at UMSOM as a session of culinary medicine training is being offered to second-year medical students in the 2020-2021 academic year. Repeated survey distribution will help evaluate the potential of culinary medicine training to elicit sustained behavior change and confidence in nutrition counseling for patients throughout the course of medical school.
Culinary medicine appears to be a valuable addition to core medical student curriculum to help fill well-established gaps in medical student nutrition education that have been shown to persist into clinical practice. Institutional pilot testing, medical student advocacy, relatively brief curriculum, and a variety of cost containment measures are likely to be helpful in supporting feasible replicability at other medical schools across the country.
Supplemental Material
Supplemental material, sj-xlsx-1-ajl-10.1177_15598276211021749 for Culinary Medicine Training in Core Medical School Curriculum Improved Medical Student Nutrition Knowledge and Confidence in Providing Nutrition Counseling by Christopher R. D’Adamo, Kayli Workman, Christine Barnabic, Norman Retener, Bernadette Siaton, Gabriela Piedrahita, Brandin Bowden, Nicola Norman and Brian M. Berman in American Journal of Lifestyle Medicine
Acknowledgments
The authors express their sincere gratitude to the medical students for their enthusiastic engagement in the culinary medicine training. We would also like to thank the Office of Medical Education at the University of Maryland School of Medicine for their vision and support in offering this training. We greatly appreciate the outstanding nutrition teaching and other comprehensive contributions to the culinary medicine training provided by David Feuz, MS, Susan Sullivan, MS, and Gina Weires, MS from Maryland University of Integrative Health. The authors are appreciative of the food and supplies that were generously donated by Performance Food Services Group. Last, the authors would like to thank the leadership and staff of the Institute for Integrative Health for their essential partnership in helping catalyze this training, both in providing the teaching kitchen space and their valuable support in the day-to-day operations of the training.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Approval was obtained by the institutional review board of the University of Maryland School of Medicine (HP-00090749).
ORCID iD: Christopher R. D’Adamo  https://orcid.org/0000-0002-2415-8158
https://orcid.org/0000-0002-2415-8158
Contributor Information
Christopher R. D’Adamo, Department of Family & Community Medicine, University of Maryland School of Medicine, Baltimore, Maryland; Department of Epidemiology & Public Health, University of Maryland School of Medicine, Baltimore, Maryland.
Kayli Workman, Department of Family & Community Medicine, University of Maryland School of Medicine, Baltimore, Maryland.
Christine Barnabic, Department of Family & Community Medicine, University of Maryland School of Medicine, Baltimore, Maryland.
Norman Retener, Department of Medicine, University of Maryland School of Medicine, Baltimore, Maryland.
Bernadette Siaton, Department of Medicine, University of Maryland School of Medicine, Baltimore, Maryland.
Gabriela Piedrahita, The Institute for Integrative Health, Baltimore, Maryland.
Brandin Bowden, The Institute for Integrative Health, Baltimore, Maryland.
Nicola Norman, Department of Medicine, University of Maryland School of Medicine, Baltimore, Maryland; The Institute for Integrative Health, Baltimore, Maryland.
Brian M. Berman, The Institute for Integrative Health, Baltimore, Maryland.
References
- 1.GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393:1958-1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2013 Risk Factors Collaborators; Forouzanfar MH, Alexander L, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries. 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287-2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risk or clusters of risks. 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1659-1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu M, Wan Y, Yang B, Huggins CE, Li D. Effects of low-fat compared with high-fat diet on cardiometabolic indicators in people with overweight and obesity without overt metabolic disturbance: a systematic review and meta-analysis of randomized control trials. Br J Nutr. 2018;119:96-108. [DOI] [PubMed] [Google Scholar]
- 5.Mancini JG, Filion KB, Atallah R, Eisenberg MJ. Systematic review of the Mediterranean diet for long-term weight loss. Am J Med. 2016;129:407-415.e4. [DOI] [PubMed] [Google Scholar]
- 6.Santos FL, Esteves SS, da Costa Pereira A, Yancy WS, Jr, Nunes JP. Systematic review and meta-analysis of clinical trials of the effects of low carbohydrate diets on cardiovascular risk factors. Obes Rev. 2012;13:1048-1066. [DOI] [PubMed] [Google Scholar]
- 7.Chiavaroli L, Nishi SK, Khan TA, et al. Portfolio dietary pattern and cardiovascular disease: a systematic review and meta-analysis of controlled trials. Prog Cardiovasc Dis. 2018;61:43-53. [DOI] [PubMed] [Google Scholar]
- 8.Manheimer EW, van Zuuren EJ, Fedorowicz Z, Pijl H. Paleolithic nutrition for metabolic syndrome: systematic review and meta-analysis. Am J Clin Nutr. 2015;102:922-932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwingshackl L, Schwedhelm C, Galbete C, Hoffmann G. Adherence to Mediterranean diet and risk of cancer: an updated systematic review and meta-analysis. Nutrients. 2017;9:1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu L, Sun D. Adherence to Mediterranean diet and risk of developing cognitive disorders: an updated systematic review and meta-analysis of prospective cohort studies. Sci Rep. 2017;7:41317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Y, Hao Q, Su L, Liu S, Dong B. Adherence to the mediterranean diet and the risk of frailty in old people: a systematic review and meta-analysis. J Nutr Health Aging. 2018;22:613-618. [DOI] [PubMed] [Google Scholar]
- 12.Becerra-Tomás N, Blanco Mejía S, Viguiliouk E, et al. Mediterranean diet, cardiovascular disease and mortality in diabetes: a systematic review and meta-analysis of prospective cohort studies and randomized clinical trials. Crit Rev Food Sci Nutr. 2020;60:1207-1227. [DOI] [PubMed] [Google Scholar]
- 13.Soltani S, Jayedi A, Shab-Bidar S, Becerra-Tomas N, Salas-Salvado J. Adherence to the Mediterranean diet in relation to all-cause mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Adv Nutr. 2019;10:1029-1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adams KM, Butsch WS, Kohlmeier M. The State of Nutrition Education at US Medical Schools. J Biomed Educ. 2015;2015:357627. [Google Scholar]
- 15.Devries S, Willett W, Bonow RO. Nutrition education in medical school, residency training, and practice. JAMA. 2019;321:1351-1352. [DOI] [PubMed] [Google Scholar]
- 16.Irl BH, Evert A, Fleming A, et al. Culinary medicine: advancing a framework for healthier eating to improve chronic disease management and prevention. Clin Ther. 2019;41:2184-2198. [DOI] [PubMed] [Google Scholar]
- 17.Accreditation Council for Graduate Medical Education. ACGME Common Program Requirements (Residency). Accreditation Council for Graduate Medical Education; 2018. Accessed March 29, 2020. http://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRResidency2019.pdf [Google Scholar]
- 18.Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Internal Medicine. Chicago, IL: Accreditation Council for Graduate Medical Education; 2017. [Google Scholar]
- 19.Devries S, Agatston A, Aggarwal M, et al. A deficiency of nutrition education and practice in cardiology. Am J Med. 2017;130:1298-1305. [DOI] [PubMed] [Google Scholar]
- 20.Mogre V, Stevens FCJ, Aryee PA, Amalba A, Scherpbier AJJA. Why nutrition education is inadequate in the medical curriculum: a qualitative study of students’ perspectives on barriers and strategies. BMC Med Educ. 2018;18:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crowley JJ, Ball I, Hiddinks GJ. Nutrition in medical education: a systematic review. Lancet Plan Health. 2019;3:e379-e389. [DOI] [PubMed] [Google Scholar]
- 22.Weinsier RL, Boker JR, Morgan SL, et al. Cross-sectional study of nutrition knowledge and attitudes of medical students at three points in their medical training at 11 southeastern medical schools. Am J Clin Nutr. 1988;48:1-6. [DOI] [PubMed] [Google Scholar]
- 23.Devries S. A global deficiency of nutrition education in physician training: the low hanging fruit in medicine remains on the vine. Lancet Planetary Health. 2019;3:e371-e372. [DOI] [PubMed] [Google Scholar]
- 24.Pang B, Memel Z, Diamant C, Clark E, Chou S, Gregory H. Culinary Medicine and community partnership: hands-on culinary skills training to empower medical students to provide patient-centered nutrition education. Med Educ Online. 2019;24:1630238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.La Puma J. What is culinary medicine and what does it do? Popul Health Manag. 2016;19:1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.La Puma J, Marx RM. ChefMD’s Big Book of Culinary Medicine. Crown; 2008. [Google Scholar]
- 27.LeBlanc-Morales N. Culinary medicine: patient education for therapeutic lifestyle changes. Crit Care Nurs Clin North Am. 2019;31:109-123. [DOI] [PubMed] [Google Scholar]
- 28.Monlezun DJ, Leong B, Joo E, Birkhead AG, Sarris L, Harlan TS. Novel longitudinal and propensity score matched analysis of hands-on cooking and nutrition education versus traditional clinical education among 627 medical students. Adv Prev Med. 2015;2015:656780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jaroudi SS, Sessions WS, 2nd, Wang VS, et al. Impact of culinary medicine elective on medical students’ culinary knowledge and skills. Proc (Baylor Univ Med Cent). 2018;31:439-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Razavi AC, Monlezun DJ, Sapin A, et al. Multisite culinary medicine curriculum is associated with cardioprotective dietary patterns and lifestyle medicine competencies among medical trainees. Am J Lifestyle Med. 2020;14:225-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fredericks L, Koch PA, Liu A, Galitzdorfer L, Costa A, Utter J. Experiential features of culinary nutrition education that drive behavior change: frameworks for research and practice. Health Promot Pract. 2020;21:331-335. [DOI] [PubMed] [Google Scholar]
- 32.Hauser ME. A novel culinary medicine course for undergraduate medical education. Am J Lifestyle Med. 2019;13:262-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hauser ME. Culinary medicine basics and applications in medical education in the United States. Nestle Nutr Inst Workshop Ser. 2019;92:161-170. [DOI] [PubMed] [Google Scholar]
- 34.Conroy MB, Delichatsios HK, Hafler JP, Rigotta NA. Impact of a preventative medicine and nutrition curriculum for medical students. Am J Prev Med. 2004;27:77-80. [DOI] [PubMed] [Google Scholar]
- 35.Rothman JM, Bilici N, Mergler B, et al. A culinary medicine elective for clinically experienced medical students: a pilot study. J Altern Complement Med. 2020;26:636-644. [DOI] [PubMed] [Google Scholar]
- 36.Magallanes E, Sen A, Siler M, Albin J. Nutrition from the kitchen: culinary medicine impacts students’ counseling confidence. BMC Med Educ. 2021;21:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hauser ME, Nordgren JR, Adam M, et al. The first, comprehensive, open-source culinary medicine curriculum for health professional training programs: a global reach. Am J Lifestyle Med. 2020;14:369-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.D’Adamo CR, McArdle PF, Balick L, et al. Spice MyPlate: nutrition education focusing upon spices and herbs improved diet quality and attitudes among urban high school students. Am J Health Promot. 2016;30:346-356. [DOI] [PubMed] [Google Scholar]
- 39.Pierce B, Bowden B, McCullagh M, et al. A summer health program for African-American high school students in Baltimore, Maryland: community partnership for integrative health. Explore (NY). 2017;13:186-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parker EA, Feinberg TM, Bowden B, et al. Spices and herbs increased vegetable palatability among underserved urban adolescents. Health Behav Policy Rev. 2018;5:76-89. [Google Scholar]
- 41.Parker EA, McArdle PF, Gioia D, et al. An onsite fitness facility and integrative wellness program positively impacted health-related outcomes among teachers and staff at an urban elementary/middle school. Glob Adv Health Med. 2019;8:2164956119873276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.D’Adamo CR, Parker EA, McArdle PF, et al. The addition of spices and herbs to vegetables in the National School Lunch Program increased vegetable intake at an urban, economically-underserved, and predominantly African-American high school. Food Qual Prefer. 2021;88:104076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sofi F, Macchi C, Abbate R, Gensini GF, Casini A. Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014;17:2769-2782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Idelson PI, Scalfi L, Valerio G. Adherence to the Mediterranean diet in children and adolescents: a systematic review. Nutr Metab Cardiovasc Dis. 2017;27:283-299. [DOI] [PubMed] [Google Scholar]
- 45.Vélez-Toral M, Rodríguez-Reinado C, Ramallo-Espinosa A, Andrés-Villas M. “It’s important but, on what level?” Healthy cooking meanings and barriers to healthy eating among university students. Nutrients. 2020;12:2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abdelhafez AI, Akhter F, Alsultan AA, Jalal SM, Ali A. Dietary practices and barriers to adherence to healthy eating among King Faisal University Students. Int J Environ Res Public Health. 2020;17:8945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Amore L, Buchthal OV, Banna JC. Identifying perceived barriers and enablers of healthy eating in college students in Hawai’i: a qualitative study using focus groups. BMC Nutr. 2019;5:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hilger J, Loerbroks A, Diehl K. Eating behaviour of university students in Germany: dietary intake, barriers to healthy eating and changes in eating behaviour since the time of matriculation. Appetite. 2017;109:100-107. [DOI] [PubMed] [Google Scholar]
- 49.Quiñones J, Hammad Z. Social determinants of health and chronic kidney disease. Cureus. 2020;12:e10266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nicholas SB, Kalantar-Zadeh K, Norris KC. Socioeconomic disparities in chronic kidney disease. Adv Chronic Kidney Dis. 2015;22:6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cockerham WC, Hamby BW, Oates GR. The social determinants of chronic disease. Am J Prev Med. 2017;52(1 suppl 1):S5-S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ibe CA, Alvarez C, Carson KA, et al. Social determinants of health as potential influencers of a collaborative care intervention for patients with hypertension. Ethn Dis. 2021;31:47-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rahman S, Mirza AS, Wathington D, et al. Chronic disease and socioeconomic factors among uninsured patients: a retrospective study. Chronic Illn. 2021;17:53-66. [DOI] [PubMed] [Google Scholar]
- 54.Williams J, Allen L, Wickramasinghe K, Mikkelsen B, Roberts N, Townsend N. A systematic review of associations between non-communicable diseases and socioeconomic status within low- and lower-middle-income countries. J Glob Health. 2018;8:020409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Slonim J, Kienhuis M, Di Benedetto M, Reece J. The relationships among self-care, dispositional mindfulness, and psychological distress in medical students. Med Educ Online. 2015;20:27924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80:1613-1622. [DOI] [PubMed] [Google Scholar]
- 57.Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among US and Canadian medical students. Acad Med. 2006;81:354-373. [DOI] [PubMed] [Google Scholar]
- 58.Coplan J. An Empirical Investigation of The Lifestyle Profile Of Graduate Students [master’s thesis]. ProQuest Dissertations & Theses database (UMI No.: 1502393). Washington, DC: The George Washington University; 2011. [Google Scholar]
- 59.Antonopoulou M, Mantzorou M, Serdari A, et al. Evaluating Mediterranean diet adherence in university student populations: does this dietary pattern affect students’ academic performance and mental health? Int J Health Plann Manage. 2020;35:5-21. [DOI] [PubMed] [Google Scholar]
- 60.Lesani A, Mohammadpoorasl A, Javadi M, Esfeh JM, Fakhari A. Eating breakfast, fruit and vegetable intake and their relation with happiness in college students. Eat Weight Disord. 2016;21:645-651. [DOI] [PubMed] [Google Scholar]
- 61.López-Olivares M, Mohatar-Barba M, Fernández-Gómez E, Enrique-Mirón C. Mediterranean diet and the emotional well-being of students of the Campus of Melilla (University of Granada). Nutrients. 2020;12:1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-xlsx-1-ajl-10.1177_15598276211021749 for Culinary Medicine Training in Core Medical School Curriculum Improved Medical Student Nutrition Knowledge and Confidence in Providing Nutrition Counseling by Christopher R. D’Adamo, Kayli Workman, Christine Barnabic, Norman Retener, Bernadette Siaton, Gabriela Piedrahita, Brandin Bowden, Nicola Norman and Brian M. Berman in American Journal of Lifestyle Medicine