In this review, we summarize the design, feasibility, acceptability, and impact on health outcomes of culturally sensitive interventions developed for the pediatric primary care setting.
Abstract
CONTEXT
Culturally sensitive interventions in the pediatric primary care setting may help reduce health disparities. Less is known on the development of these interventions, their target groups, and their feasibility, acceptability, and impact on health outcomes.
OBJECTIVE
We conducted a systematic review to describe culturally sensitive interventions developed for the pediatric primary care setting.
DATA SOURCES
PubMed, Web of Science, Cumulative Index to Nursing and Allied Health Literature, and PsycInfo (January 2000 to July 2020).
STUDY SELECTION
Studies were eligible for inclusion if they were (1) original research on an intervention with an evaluation, (2) within a pediatric primary care setting, (3) not limited to education for providers, (4) not limited to interpreter use, and (5) based in the United States.
DATA EXTRACTION
The following were extracted: study topic, study design, intervention, cultural sensitivity strategies and terminology, setting, target group, sample size, feasibility, acceptability, and health outcomes.
RESULTS
Twenty-five studies described 23 interventions targeting a variety of health topics. Multiple cultural sensitivity strategies were used, most commonly sociocultural (83%). Most interventions (57%) were focused on Hispanic/Latino families. Interventions were generally reported as being feasible and acceptable; some also changed health outcomes.
LIMITATIONS
Small samples and heterogenous methods subject to bias were used. Relevant articles may have been missed because of the variety of terms used to describe cultural sensitivity.
CONCLUSIONS
The included articles provide preliminary evidence that culturally sensitive interventions can be feasible and effective and may help eliminate disparities for patients from communities with barriers to equitable care.
In pediatric primary care, disparities in access, quality, and care delivery exist for children and families of color,1 those living in poverty,2 and those whose primary language is not English.3 According to a review of pediatric health care access and quality, parents who identify as Indigenous, Black, Latino, Asian American, or Pacific Islander are less likely than non-Hispanic white parents to report receiving high-quality health care for their children.4 Many of these disparities are rooted in structural inequities, including racism,5 xenophobia,6 and poverty.2 Similarly, children whose parents’ primary language is not English face health care access and quality disparities7,8 and are less likely to have a medical home.9 Eliminating these disparities is a priority of the American Academy of Pediatrics,10 the American Board of Pediatrics,11 and the National Academy of Medicine.12,13
There has been a growing awareness that providing culturally sensitive pediatric primary care, especially during well-child visits, is a potentially modifiable way to address health care disparities and promote health equity.14,15 The American Academy of Pediatrics defines culturally sensitive care as “the delivery of care within the context of appropriate physician knowledge, understanding, and appreciation of all cultural distinctions leading to optimal health outcomes” and has recognized cultural sensitivity as an important aspect of providing all children high-quality comprehensive care.10 Two influential publications from the National Academy of Medicine, Crossing the Quality Chasm12 and Unequal Treatment,13 also describe how the provision of culturally sensitive care may help reduce racial and ethnic health care disparities. Culturally sensitive care is also a key component of the patient-centered medical home model.16 A recent study revealed that parent-reported culturally sensitive care within pediatric primary care settings was associated with higher-quality well-child care.17
Culturally sensitive interventions, defined here as interventions specifically incorporating tenets of culturally sensitive care, have been developed for the pediatric primary care setting over the past 2 decades in alignment with the call to action to address child health disparities.
An important example of a culturally sensitive intervention that is considered standard of care is ensuring that language supports (ie, professional medical interpreters or health care providers with professional language proficiency) are available to all patients.18,19 However, language represents only one component of delivering culturally sensitive pediatric health care.20 Kreuter et al21 provide a framework for how to develop culturally sensitive interventions more broadly, which includes the following strategies: peripheral (packaging materials in a way likely to appeal to a given group), evidential (providing evidence of a health issue’s impact on a given group), linguistic (providing health education in the dominant language of a group), constituent involving (drawing directly on experience of members of the target group), and sociocultural (framing health issues in relation to broader social or cultural values). In addition to the framework by Kreuter et al,21 addressing structural factors (ie, poverty, racism) is also a key tenet of culturally sensitive care.22
As reports of culturally sensitive interventions increase, a description about how culture is incorporated into intervention development, into groups included in these interventions, and into intervention feasibility, acceptability, and impact on health outcomes would allow pediatric health providers to assess the current state of the literature and identify opportunities for improvement in their own practices. In this systematic review, our objectives were to (1) summarize the existing primary literature on studies in which researchers applied culturally sensitive interventions in the pediatric primary care setting, (2) explore how authors used specific culturally sensitive strategies, and (3) assess whether these adaptations are feasible and acceptable and/or lead to a change in health outcomes.
Methods
Eligibility Criteria
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines to complete this systematic review.23 To be included in this review, studies were required to be (1) original research on an intervention or program, including evaluation; (2) within a pediatric primary care setting; (3) not limited to education for providers; (4) not limited to interpreter use; and (5) based in the United States. We excluded articles that described only provision of interpreters because it is now expected standard of care in all health care settings.18,19 Conference abstracts and dissertations were excluded. Because of the rapidly changing demographics in the United States in recent decades,24 only studies from 2000 or later were included.
Data Sources and Search Strategy
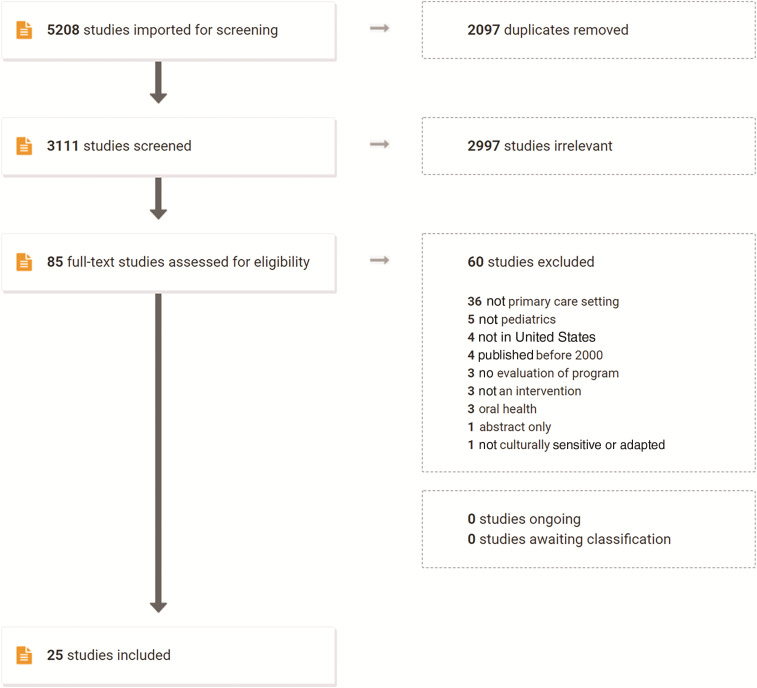
An electronic literature search was conducted in July 2020 by using PubMed, Web of Science, the Cumulative Index to Nursing and Allied Health Literature, and PsycInfo. A diagram of the search process can be found in Fig 1. The search terms used were as follows: (“cultural resilience” or “cultural sensitivity” or “culturally sensitive” or “cultural adaptation” or “culturally adapted” or “culturally humble” or “culturally appropriate” or “culturally competent” or “culturally grounded” or “cultural background” or “cultural values” or “cultural navigator” or “culturally responsive” or “culturally relevant”) AND (“pediatric” or “well-child” or “pediatric primary care” or “pediatric medical home” or “primary care”). Of 3111 unique titles and abstracts, 85 relevant articles were downloaded for further screening. Screening for inclusion was done independently by 2 study team members (W.O. and M.S.), who thoroughly reviewed each article to determine if each inclusion criterion was met. Discrepancies in terms of whether an article should be included were resolved by discussion and consensus, as well as arbitration by a third team member (M.R.) if necessary. Screening was performed in Covidence, an online tool for systematic reviews.25 Twenty-five studies on 23 unique interventions were included after screening by full text. The references for each article that met inclusion criteria were searched for additional relevant articles; no new articles were found.
FIGURE 1.
Flow diagram of study selection for the identification of peer-reviewed publications on culturally sensitive interventions in pediatric primary care settings in the United States, January 2000 to July 2020.
Data Extraction
Study interventions and results were abstracted and evaluated by 1 researcher (W.O.), with verification by 2 additional researchers (M.R. and M.S.). To summarize and synthesize articles, we developed an abstraction codebook that included the following topics: (1) populations studied, (2) intervention design, (3) how culturally sensitive care was defined, (4) how culturally sensitive care was incorporated into the intervention (considering the framework by Kreuter et al21 as well as structural factors), (5) evaluation design, and (6) feasibility, acceptability, and/or health outcomes reported. We used the evidence levels described in Table 1 to assess risk of bias for each study.26 Study quality and risk of bias were evaluated independently by 2 study team members (D.C.G and K.M.), with discrepancies resolved by discussion and consensus. We anticipated high variability and low standardization between studies, precluding meta-analysis and assessment of publication bias.
TABLE 1.
Evidence Quality Assessment (N = 25)
| Author (Year) | |
|---|---|
| Evidence level 1: systematic review of evidence level 2 studies | — |
| Evidence level 2: RCT | Chen et al30 (2019)a |
| Mirza et al43 (2013)a | |
| Evidence level 3-I: pseudo-RCT (ie, alternate allocation or some other method) | Arauz Boudreau et al27 (2013)b |
| O’Connor et al45 (2020)b | |
| La Roche et al38 (2006)b | |
| Mazzeo et al42 (2014)b | |
| Falbe et al33 (2015)b | |
| Evidence level 3-II: comparative study with concurrent controls (nonrandomized experimental trial, cohort study, case-control study, interrupted time series) | — |
| Evidence level 3-III: comparative study without concurrent controls (historical control study, ≥2 single-arm interrupted time series without a parallel control group) | Cronk et al31 (2011) |
| Evidence level 4: case series with either posttest or pre- and posttest outcomes or cross-sectional design | Bender et al29 (2014)c |
| D’Angelo et al32 (2009) | |
| Bender et al28 (2013) | |
| Herbst et al37 (2019) | |
| Falbe et al34 (2017)c | |
| Feutz and Andresen35 (2013) | |
| Hamilton et al36 (2013) | |
| Landback et al39 (2009) | |
| Lewin et al40 (2015) | |
| López et al41 (2018) | |
| Nitsos et al44 (2017) | |
| Reavy et al46 (2012) | |
| Rice et al47 (2003) | |
| Ryan et al48 (2020) | |
| Serpas et al49 (2013) | |
| Svetaz et al50 (2016) | |
| Valdez et al51 (2013) |
—, not applicable.
Described a power analysis.
No power analysis or authors stated they were underpowered.
Included here because the evaluation is described in another article.
The protocol for this systematic review was prospectively registered in the International Prospective Register of Systematic Reviews (identifier CRD42020083916). The University of Pittsburgh deemed this study non–human subjects research.
Results
Summary of Included Articles
Twenty-five articles were included in this review.27–51 Descriptions of study characteristics are shown in Tables 2 and 3. The most common study design was intervention arm only with pre-post assessment, which was used in 11 (44%) articles.* Seven studies (28%) used randomized controlled trial (RCT) designs.27,30,33,38,42,43,45 Two (8%) conducted fully powered RCTs,30,43 3 (12%) were pilot RCTs,38,42,45 and 2 (8%) RCTs were underpowered.27,33 Four (16%) studies used cross-sectional designs,34,36,46,50 1 (4%) used an adaptation scoring design,29 1 (4%) used an intervention arm with a historical control,31 and 1 (4%) used retrospective chart reviews.49 Per the description in each study’s methods section, 16 (64%) used primarily quantitative methods,† 1 (4%) was primarily qualitative,34 and 8 (32%) used mixed methods29,31,32,40,46,47,49,50 (Table 3). Evidence levels varied among the studies (Table 1). Studies describing the same intervention (those by Bender et al28,29 and by Falbe et al33,34) have been combined, resulting in a denominator of 23 (instead of 25) for percentages reported below.
TABLE 2.
Description of Included Interventions (n = 23)
| Author (Year) | Topic of Intervention | Target Population | Title and Brief Overview of Intervention | Setting | Timing | Participant Demographics |
|---|---|---|---|---|---|---|
| Arauz Boudreau et al27 (2013) | Obesity | Latino children | Children and caregivers received 6 total wk of “Power Up” group health classes and 6 mo of coaching designed to help families incorporate healthy lifestyles and address barriers to change | Urban community health primary care center (Boston, MA) | Power Up: 5 weekly sessions, sixth session 3 mo later; health coaching: 1 meeting followed by periodic contact over 6 mo | Latino children (N = 41) with BMI >85 percentile, aged 9–12 y, and their caregivers; average age 10, 62% female, >75% primary household language non-English, all participants first- (54%) or second-generation (46%) immigrants |
| Bender et al28 (2013) | Obesity | Low-income Hispanic mothers with preschool-aged children | Vida Saludable: 4 biweekly group classes on avoiding sugar-sweetened beverages, increasing physical activity, and maternal role-modeling, followed by 6 mo of community group activities | Urban community health center (San Diego, CA) | Phase 1: 4 biweekly group lessons | Mothers (N = 33): average age 27 y, 100% born in Mexico, 88% below poverty level, 97% Spanish speaking, 100% unemployed; children: average age 3.6, 52% female, 100% in preschool, 97% with MediCal insurance |
| Bender et al29 (2014) | — | — | — | — | Phase 2: 6 monthly group activities; delivered over 9 mo | — |
| Chen et al30 (2019) | Wt loss | Chinese-American adolescents | iStart Smart for Teens: online educational modules designed to increase self-efficacy and promote physical activity and healthy diets, followed by tailored biweekly text messages; Fitbit Flex devices were provided to monitor activity levels and track dietary intake | Community clinics; online (San Francisco, CA) | Online modules: 3 mo; tailored text messages: 3 mo; Fitbit: entire 6-mo period | Chinese-American adolescents (N = 40), mean age 14.9, 43% female, mean BMI 28.3, mean BMI percentile 94, 95% with family income <$40 000 |
| Cronk et al31 (2011) | BMI, quality of life | Spanish-speaking Latino families and children | Familias Sanas y Activas: family-centered, child-focused health presentations by bilingual and/or bicultural staff; emphasis on healthy lifestyles, not wt change, with family- and self-selected goals; staff support, coaching, and additional activities available | Community FQHC and/or local service organization community center (Milwaukee, WI) | 6 weekly sessions; follow-up at 6 and 12 mo | Spanish-speaking Latino families with children 8–11 y and BMI >85th percentile (N = 54): average age 9.4, 52% female, average parental age 36, 97% Mexican origin, average 11 y in United States, 68% children without insurance |
| D’Angelo et al32 (2009) | Depression | Latino families | Culturally adapted from the Beardslee Preventive Intervention Program for Depression: 6 modules with structured discussion topics delivered over a variable duration, designed to enhance strength and resilience in children whose parents are depressed | Mental health clinic (Boston, MA) | Flexible timing offered, range of 3–7 mo | Latino families with children 7–17 y and parent with depressive disorder (N = 9): child average age 11, 56% female, 78% bilingual, 22% English only; 100% parents female, average maternal age 40 y, 78% income <$20 000, average 14 y in United States, 78% Spanish only, 22% bilingual |
| Falbe et al33 (2015) and Falbe et al34 (2017) | Obesity | Latino children | Familias Activas y Saludables: weekly group classes led by a dietician, physician, and promotora covering healthy behaviors | Pediatric primary care FQHC (Martinez, CA) | Five 2-h group medical appointments, every other week for 10 wk | Spanish-speaking Latino families, child 5–12 y and BMI >85th percentile (N = 53): children 51% female, mean age 8.9 y, mean BMI 24.4, 87% BMI >95th percentile; parents 94% female, 67% first-generation immigrants, 76% food insecure |
| Feutz and Andresen35 (2013) | Sexual risk behaviors | Latino adolescents | Cuidate: modules on the Cuidate theme (“take care of yourself”) and safe and unsafe sex delivered in various formats, including small groups, music, videos, games, role-playing, and skill-building activities | Pediatric primary care center in federally designated medically underserved area (Urbana, IL) | Six 1-h modules, delivered over 2 d (3 h each day) | Latino adolescents 13–18 y, fluent in English |
| Hamilton et al36 (2013) | Care coordination | Children with special health care needs | Pediatric Medical Home Program: standard medical home requirements plus a focus on care coordination, a bilingual family liaison, and a pediatrician to develop and manage written patient care plans | Pediatric medical home (Los Angeles, CA) | Years | Children with low SES, minority racial and/or ethnic status, and serious chronic conditions |
| Herbst et al37 (2019) | Obesity | Racially diverse, low SES children in urban underserved area | Developed standardized, culturally tailored educational resources and used motivational interviewing to assess readiness for discussion of healthy diet and lifestyle changes and to develop SMART goals | Outpatient urban pediatric primary care center (Cincinnati, OH) | Provider training: 20-min monthly seminars over 9 mo; innovations: 6 mo | Racially diverse, low SES children (N = 137): mean age 44 mo, 61% female, 60% with overweight, 40% with obesity, 71% Black, 16% White, 10% multiracial, 93% with public insurance |
| La Roche et al38 (2006) | Asthma | Racial and/or ethnic minority, low SES, urban children | Multifamily Asthma Group Treatment: group modules discussed asthma prevention, treatment, and resources in an allocentric manner consistent with the allocentric orientation | Inner-city pediatric community health center (Boston, MA) | Three 1-h modules, conducted on different days | Racial and/or ethnic minority, low SES, urban children aged 7–13 y (N = 22): 73% Hispanic, 27% African American, 41% female |
| Landback et al39 (2009) | Depression | Adolescent patients with subthreshold depressive symptoms | Project CATCH-IT: Internet module–based intervention designed to enhance resiliency, coping skills, and prevent depression | Primary care clinic, and online (Chicago, IL) | 14 self-directed Internet modules, with 15-min motivational interviews before and after with PCP | Adolescents aged 14–21 y (N = 25): mean age 18 y, 68% female, 88% white, 8% African American, 4% Asian American, mean Center for Epidemiological Studies Depression Scale score 24 |
| Lewin et al40 (2015) | Depression | Urban, low-income minority teen-aged mothers and male partners | Strong Foundations: prenatal group educational sessions for married or cohabiting couples, led by a male and female facilitator, and individualized postnatal sessions integrated into well-child pediatric visits held over the course of the child’s first year | Primary care pediatrics (Chicago, IL) | Five 2-h prenatal group sessions; 9 individualized postnatal sessions in child’s first year | Prenatal pilot data: N = 32 couples: mothers average age 17 y, 83% Black, 90% in school; fathers average age 18 y, 85% Black, 55% in school, 35% employed |
| López et al41 (2018) | Child behavior | Latino families | Criando a Nuestros Niños hacio el Éxito: parenting program aimed to improve family dynamics, decrease problematic child behavior, and help manage stress through sessions with a promotora | Pediatric primary care clinic (rural SC) | Eight 2-h sessions conducted weekly | Sociodemographic data measured but not reported |
| Mazzeo et al42 (2014) | Obesity | African American children | Nourishing Our Understanding of Role Modeling to Improve Support and Health: parent-only group sessions emphasizing role-modeling of healthy eating and exercise, and enhancing parents’ self-efficacy in eating and exercise behaviors | Community-based clinic (VA) | Originally 12 weekly 90-min sessions, reduced to 6 after participant feedback | Baseline: N = 84 families; children mean age 8.6 y, 67% female, mean BMI percentile 98; caregivers mean age 40 y, 86% female, mean BMI 34; 61% African American, 37% White, 42% income <$35 000 |
| Mirza et al43 (2013) | Obesity | Hispanic American children and adolescents | LGD: nutrition modules on reducing carbohydrate intake and promoting intake of proteins and fats, weekly meetings with interventionist, and sessions designed to increase physical activity; LFD: identical to LGD but given nutritional information focused on reducing fat intake | Community-based pediatric clinic (Washington, DC) | Weekly modules and meetings for 12 wk; dietary intervention: 2 y | Hispanic American children and adolescents (n = 57 LGD, n = 56 LFD): mean age 12 y, mean BMI 31, mean age at obesity onset 6 y, 70% with obesity family history, mean income <$30 000 |
| Nitsos et al44 (2017) | Parent education | Latino parents with limited English proficiency | Tummy Time: education and educational materials in Spanish provided to parents on Tummy Time, in which adults play and interact with awake, prone infants to strengthen neck muscles and prevent musculoskeletal conditions | Obstetric clinic waiting rooms (West Columbia, SC [urban], and Lancaster, SC [rural]) | Single sessions while parents waiting in clinic, intervention run for 13 mo | Parents and expectant parents or caregivers of infants who self-identified as Latino or Hispanic, having limited English proficiency, and having Spanish as first language |
| O’Connor et al45 (2020) | Obesity | Hispanic children and fathers | Papas Saludables Ninos Saludables: group-based healthy lifestyle program that encourages fathers as healthy role models, teaches authoritative parenting, and recommends reciprocal reinforcement | Primary care pediatric clinic (Houston, TX) | Weekly 90-min sessions for 10 wk | Hispanic children (n = 64) and fathers (n = 36): children mean age 8.5 y, 56% female, 38% with overweight or obesity; fathers mean BMI 29, 39% with income <$25 000, 83% home Spanish speaking, 89% immigrants (70% from Mexico) |
| Reavy et al46 (2012) | Prenatal and pediatric clinic for refugees | US prenatal and pediatric refugees | Culturally Appropriate Resources and Education Clinic: nurse-led clinic model for prenatal and pediatric refugee patients, providing access to health care services and education, and implementing a designated CARE Clinic Health Advisor | Outpatient family center on medical campus (Boise, ID) | 2-h group visits; prenatal care: 6 times per month; well-infant care: 4 times per month | US prenatal and pediatric refugees |
| Rice et al47 (2003) | Smoking | Arab American adolescents | Project TNT: pilot focus, intervention, clinic, and school focused on smoking cessation; health educator met with teenagers in group setting to discuss tobacco use | Arab American teenager health clinic (Detroit, MI) | Pilot intervention: 1 h once a week for 4 wk | Arab American adolescents (N = 9), mean age 16 y, 78% male, 67% second-generation immigrants, 45% with Arabic as first language |
| Ryan et al48 (2020) | Bike helmet safety | Urban children | You Make the Call: a video on bike helmet use was shown to parent-child dyads during pediatric clinic visits, children were given a free helmet, and parents were given a handout to encourage helmet use | Primary care clinic (Baltimore, MD) | Single session, phone follow-up after 1 mo | Urban children |
| Serpas et al49 (2013) | Obesity | Latino children | San Diego Healthy Wt Collaborative: broad initiative that included primary care, public health, schools, and community organizations to reduce obesity. Primary care interventions included PDSA QI cycles, training on wt-related documentation, and creation of handout materials for families | Primary care clinic, as well as other medical and community centers, and schools (San Diego, CA) | Years | Chula Vista Family Clinic (N = 8106 patients): 79% Latino, obesity rate not available, 27% uninsured, 86% <200% federal poverty level |
| Svetaz et al50 (2016) | Family care | Latino immigrant teenagers | Aqui Para Ti: clinic-based program for youth and parents that provided family-centered, confidential, parallel care for Latino families; team consisted of a physician, health educator, and program coordinator | Primary care pediatrics (Minneapolis, MN) | Years | Latino immigrant youth (N = 30) and their families: youth 80% female, 63% older than 14 y; parents 73% female, 60% 40 y or younger; 67% from Mexico |
| Valdez et al51 (2013) | Functioning in maternal depression | Latina immigrant mothers with depression and families | Fortalezas Familiares: group meetings (adults and children separate) and booster sessions designed to improve communication and coping with maternal depression | 3 community outpatient clinics (Madison, WI) | 12 weekly sessions, with 2 booster sessions 1 mo apart | Latina immigrant mothers (n = 13) and children (n = 17): mothers mean age 36 y, 77% from Mexico, 92% income <$29 000; no data on children reported |
CARE, Culturally Appropriate Resources and Education; CATCH-IT, Competent Adulthood Transition with Cognitive-Behavioral, Humanistic, and Interpersonal Training; FQHC, Federally Qualified Health Centers; LFD, low-fat diet; LGD, low-glycemic diet; PCP, primary care physician; PDSA, plan-do-study-act; QI, quality improvement; SES, socioeconomic status; SMART, specific, measurable, achievable, relevant, timely: TNT, Toward No Tobacco Use; —, not applicable.
TABLE 3.
Intervention Evaluation Type, Feasibility, Acceptability, and Health Outcomes (n = 23)
| Author (Year) | Type of Study | Type of Method | Feasibility and Acceptability | Health Outcomes |
|---|---|---|---|---|
| Arauz Boudreau et al27 (2013) | RCT: underpowered | Quantitative | Feasibility: attendance rates averaged 79%, 63% completed follow-up; acceptability: not reported | Physical activity significantly increased in the intervention group (P = .03), but after demographic adjustment this effect was lost (P = .88); no differences found between groups for BMI, physical activity, or metabolic markers of obesity (lipids, glucose, insulin, HbA1C, AST and ALT, C-reactive protein, IL-6, TNF-α), health-related quality of life improved for both groups (P = .33) |
| Bender et al28 (2013) | Intervention arm only, pre-post assessment | Quantitative | Feasibility: 77% enrolled were included in the intervention; of the intervention group, 100% completed the program with 100% attendance and 91% completed 6-mo follow-up. Acceptability: high participant satisfaction and enjoyment of the program (no additional data reported) | Maternal BMI decreased (P < .05) and children’s BMI decreased (P > .05); sugary drink consumption decreased, and water and milk consumption increased (all P < .02) |
| Bender et al29 (2014) | Adaptation scoring | Mixed methods | Feasibility: no additional data reported (see Bender et al28); acceptability: participants highly complimented the promotora, bonded with each other, and continued to meet post intervention | No additional data reported; see Bender et al28 |
| Chen et al30 (2019) | RCT: fully powered | Quantitative | Feasibility: 75% reported accessing the Fitbit program several times a week, and 20% accessed once a week; 90% completed 6-mo follow-up. Acceptability: 100% would recommend this program to others; 100% reported the device was helpful in tracking physical activity, 88% found it helpful for tracking food intake; 91% shared Fitbit data with their PCP | Significantly greater decrease in BMI in the intervention group (−4.89 vs −4.72; P < .001), as well as sugar-sweetened drink consumption (P = .001) and television and/or computer time (P < .001) and increased self-efficacy in nutrition (P = .02) and physical activity (P = .05); no difference in quality of life physical health |
| Cronk et al31 (2011) | Intervention arm only, historical control | Mixed methods | Feasibility: 80% attended at least 4 of 6 sessions; home coaching occurred a median of 4 times over 12 mo; 57% completed 12-mo follow-up. Acceptability: the sessions created a sense of warmth and camaraderie; children enjoyed the structured physical activity and play sessions (qualitative) | Significant reduction in BMI z scores (average −0.13) in intervention compared with control (P < .001); >40% reduced their intake of chips, fries, and desserts, and increased milk intake; significant improvements were seen in all of the Pediatric Quality of Life subscales (all P < .001, except emotional subscale [P = .03]) |
| D’Angelo et al32 (2009) | Intervention arm only, pre-post assessment | Mixed methods | Feasibility: 100% completed the intervention; attendance was flexible, with participants averaging 7.3 sessions over 3–7 mo. Acceptability: mothers felt they had benefited from participation; 6 of 8 children were “glad to be involved”; only 1 child found the intervention stressful | Maternal ratings of therapeutic alliance averaged 6.97 of 7; parents reported improved ability to communicate and improved relationships and understanding with their child; children’s responses were similar; maternal GAS ratings revealed significant improvement (P = .02) |
| Falbe et al33 (2015) | RCT: underpowered | Quantitative | Feasibility: participants attended a mean of 3.5 of 5 sessions, 71% attended ≥4; 75% of randomly assigned participants were included in the final analysis. Acceptability: positive participant feedback was noted (no additional data reported) | Primary outcome: BMI, decreased at 10 wk in the AHF group (−0.50) and increased in the control group (+0.32; P = .004); triglyceride levels decreased in the AHF group compared with controls (P = .03); no differences found in SBP and DBP, LDL and HDL cholesterol, glucose, HOMA-IR, or HbA1C |
| Falbe et al34 (2017) | Cross-sectional | Qualitative | Feasibility: all 23 participants at the final session agreed to an exit interview, which 91% later completed. Acceptability: promotoras were felt to be an efficacious tool for helping clinicians provide bridging communication and to promote healthy behaviors; parents found the provider triad to enhance comfort and feel welcoming | Not reported |
| Feutz and Andresen35 (2013) | Intervention arm only, pre-post assessment | Quantitative | Feasibility: 15 of 24 (54%) registered for first session attended, with 5 additional unregistered participants (N = 20); 100% retention rate to second session; second program (n = 7) 70% attendance and 86% retention; and third program 0% attendance of 19 registered. Acceptability: participants evaluated the program positively; they enjoyed the activities and would strongly recommend Cuidate to others (no data reported) | There was a significant increase in HIV knowledge test scores (P = .001); improvement seen in intention to use condoms (P = .01), perceived self-efficacy in using condoms (P = .001), ability to say no to sex (P = .04) and to negotiate with partner (P = .03) |
| Hamilton et al36 (2013) | Cross-sectional | Quantitative | Feasibility: no data reported; acceptability: mean satisfaction scores for the 15 Spanish-speaking families were 8.5 points higher (more satisfied) than the mean scores from the 7 English-speaking families (P = .003) | Not reported |
| Herbst et al37 (2019) | Intervention arm only, pre-post assessment | Quantitative | Feasibility: family attendance of clinic follow-up improved from 11% to 34% pre and post innovation, respectively, retention data N/A; acceptability: not reported | Increases were seen in including: wt and BMI in the visit diagnosis (P < .001), HPI (P < .001), and plan (P = .006); providers were more likely to offer follow-up (P < .001); families were more likely to follow-up (P < .01) |
| La Roche et al38 (2006) | RCT: pilot | Quantitative | Feasibility: 100% completed the intervention, 92% completed 1 y follow-up; acceptability: not reported | Mean ED visits in the MFAGT group was 0.7, which was lower than the SPAI group (1.2) and control group (1.4) (P = .04); asthma management scale scores improved in both the MFAGT and SPAI groups (P > .05); no differences found by race and/or ethnicity |
| Landback et al39 (2009) | Intervention arm only, pre-post assessment | Quantitative | Feasibility: 92% of adolescents completed the final product intervention, which was improved significantly (P = .009) from the prototype (57%); retention not reported. Acceptability: participants rated that they would be willing to recommend the intervention to a peer (8.59/10) and that the program was useful in identifying thoughts and behaviors I would like to change (8.30/10) | Not reported |
| Lewin et al40 (2015) | Intervention arm only, pre-post assessment | Mixed methods | Feasibility: couples attended a mean of 3.2 of 5 prenatal sessions; 18% of couples completed the intervention. Acceptability: participants rated classes as very helpful (mean 4.4 of 5), and believed they were likely to use what they learned (mean 4.2 of 5) | Not reported |
| López et al41 (2018) | Intervention arm only, pre-post assessment | Quantitative | Feasibility: 100% of parents attended at least 1 session, 50% attended at least 75%; 92% retention for postintervention follow-up. Acceptability: participants rated their satisfaction with the program an average of 4.50 of 5 | No significant changes in child or parent coping competence; decrease in child behavior problems (P = .04) and parenting stress (P = .01) |
| Mazzeo et al42 (2014) | RCT: pilot | Quantitative | Feasibility: families attended an average of 52.9% of intervention sessions, 62% completed postintervention testing. Acceptability: 91.7% strongly agreed they would recommend this group to others | No changes reported in Child Feeding Questionnaire subscales; significant difference in BMI percentile, which decreased in the intervention group and did not change in the control group (P < .008); no significant changes in children’s quality of life |
| Mirza et al43 (2013) | RCT: fully powered | Quantitative | Feasibility: 79% of both groups completed 3 mo of treatment, 58% of LGD and 55% of LFD participants completed the final follow-up at 24 mo; acceptability: not reported | At 3 mo post intervention, LGD participants had decreased glycemic loads per meal compared with the LFD group (P = .02): not sustained at 12 and 24 mo, no between-group differences in glycemic loads or macronutrient intake; both groups decreased BMI z scores at all measurements post intervention (P = .0001, .003, and .002) and decreased metabolic syndrome (NS); no significant differences between groups in BMI or HOMA-IR |
| Nitsos et al44 (2017) | Intervention arm only, pre-post assessment | Quantitative | Feasibility: attendance and retention N/A; acceptability: not reported | Significant increase in Tummy Time–related knowledge (P = .04); all participants reported increased confidence |
| O’Connor et al45 (2020) | RCT: pilot | Quantitative | Feasibility: enrolled 90% of the goal sample size, retained 75% of participants for post assessment, and maintained 72% attendance; 72% had most anthropometric and behavioral data at follow-up. Acceptability: achieved 100% excellent or good satisfaction ratings among parents; almost all stated they would recommend the program to their friends | No statistically significant differences observed in wt, BMI, HR, BP, waist circumference, kilocalories (Food Frequency Questionnaire), moderate and/or vigorous physical activity, or sedentary time observed between groups in children |
| Reavy et al46 (2012) | Cross-sectional | Mixed methods | Feasibility: attendance and retention N/A; acceptability: advisors reported enhanced abilities for refugees to navigate and/or communicate with the health care system | Missed clinic appointments dropped from 25% to 2.5%; there was a drop in the no-show rate for clinic appointments; childhood immunizations rates at 100% compliance (no previous data) |
| Rice et al47 (2003) | Intervention arm only, pre-post assessment | Mixed methods | Feasibility: attendance was 100% at each of the sessions in the pilot intervention; 89% completed follow-up. Acceptability: participants evaluated the information provided as “very helpful” or “somewhat helpful” | Pilot intervention: validated tobacco quit rate of 37.5% at 1-mo follow-up |
| Ryan et al48 (2020) | Intervention arm only, pre-post assessment | Quantitative | Feasibility: attendance N/A, retention rate 60% for 1-mo follow-up; acceptability: not reported | Of those who reported riding their bikes post intervention, 100% “always” used helmets (compared with 0% preintervention); more parents required helmet use (35% preintervention, 67% post intervention); no outcomes reached statistical significance |
| Serpas et al49 (2013) | Chart reviews | Mixed methods | Feasibility: attendance and retention N/A; acceptability: not reported | Pediatric patients with wt assessments charted increased from 40% at baseline to 90% (no P value reported) |
| Svetaz et al50 (2016) | Cross-sectional | Mixed methods | Feasibility: attendance and retention N/A; acceptability: 100% reported being fully satisfied with clinic outcomes, and 29 of 30 would recommend Aqui Para Ti; adolescents reported high levels of comfort and trust | Not reported |
| Valdez et al51 (2013) | Intervention arm only, pre-post assessment | Quantitative | Feasibility: 76% of enrolled families attended >90% of the sessions; 76% of enrolled families completed the postintervention assessment. Acceptability: questionnaire ratings of satisfaction were highly favorable; overall quality of the intervention was rated at 4.92 of 5 and 4.56 of 5 by mothers and caregivers, respectively | Small improvements seen in child support–seeking behaviors, decreases in total conflict behavior with mothers, and improvements in conduct problems, emotional symptoms, and prosocial behavior; contrary to expectation, children reported an increase in peer problems (No P values reported) |
AHF, Active and Healthy Families; ALT, alanine aminotransferase ; AST, aspartate aminotransferase; BP, blood pressure; DBP, diastolic blood pressure; ED, emergency department; GAS, Global Assessment Scale; HbA1C, hemoglobin A1C; HDL, high-density lipoprotein; HOMA-IR, homeostatic model assessment estimate of insulin resistance; HR, heart rate; IL-6, interleukin 6; LDL, low-density lipoprotein; LFD, low-fat diet; LGD, low-glycemic diet; MFAGT, Multifamily Asthma Group Treatment; N/A, not applicable; NS, not significant; PCP, primary care provider; SBP, systolic blood pressure; SPAI, Standard Psychoeducational Asthma Intervention; TNF-α, tumor necrosis factor α.
Intervention Topics, Locations, and Timing
Interventions addressed a wide variety of topics. Ten (43%) were focused on obesity prevention‡ and 4 (17%) on depression.32,39,40,51 One (4%) each was focused on asthma,38 sexual health,35 smoking cessation,47 parental education for prevention of infant musculoskeletal disorders,44 bicycle helmet safety,48 child behavior,41 provision of family-centered primary care,50 care coordination,36 and development of a cultural health advisor position within a clinical practice.46 All interventions took place in primary care centers or clinics, with some including components located online,30 at schools,47,49 or at local community centers.31,49 For longitudinal interventions, session length ranged from 20 minutes50 to 2 hours,33,34,40,41,46 and intervention length ranged from a single session36,44,48 to sessions spread over 2 years43 (Table 2).
Terms Used to Describe Cultural Sensitivity
Authors used a total of 23 terms to describe how their interventions related to culture, with many studies including >1 term (Table 4). The 2 most frequent terms, “culturally sensitive”§ and “culturally appropriate,”‖ were each used in 12 (52%) interventions. Eight (35%) interventions used “culturally tailored,”28–31,33,34,37,41,44,48 8 (35%) used “culturally adapted,”28,29,32,40,41,43–45,51 7 (30%) used “culturally relevant,”27–29,32–34,39,41,48 7 (30%) used “culturally competent,”28,29,36,38,41,43,46,50 and 4 (17%) used “culturally specific.”31,33,34,41,51 Other terms included the following: culturally centered,45,51 culturally accepted or acceptable,35,44 culturally safe,46 culturally congruent,33,34 culturally aware,32 culturally inclusive,50 culturally familiar,31 culturally equivalent,51 culturally representative,51 culturally suitable,28,29 culturally modified,28,29 culturally effective,36 culturally respectful,33,34 culturally based,35 culturally targeted,44 and culturally accurate.49
TABLE 4.
Culturally Sensitive Strategies Used in Included Interventions (n = 23)
| Author (Year) | Cultural Terms Used | Constituent Strategies | Evidential Strategies | Linguistic Strategies | Peripheral Strategies | Sociocultural Strategies |
|---|---|---|---|---|---|---|
| Arauz Boudreau et al27 (2013) | Sensitive, relevant | Not described | Not described | Not described | Not described | Tailored sessions to be family centered to cater to participants’ sense of familismo |
| Bender et al28 (2013) and Bender et al29 (2014) | Sensitive, relevant, appropriate, adapted, tailored, competent, suitable, modified | Preprogram stakeholders’ input, incorporated to develop the culturally relevant intervention; an experienced promotora was recruited from the health center and trained by investigators | Not described | Study materials were forward- and back-translated into Spanish by 2 independent translators, according to Eremenco and colleagues’ guidelines.74 Surveys were linguistically tailored to participant education and literacy levels | Program materials included pictures of Hispanic children and families. Meetings were at familiar community locations and incorporated common cultural foods | Program materials and curriculum were designed with special attention to culture. Program attendance was extended to family members, and child care as well as supplemental health and social services assistance was provided |
| Chen et al30 (2019) | Appropriate, tailored | Not described | Not described | Not described | Presented opportunities for participants to sample healthy Chinese and Western foods | Modules discussed common Chinese and Western dietary practices, concepts, and beliefs regarding promoting balance in health |
| Cronk et al31 (2011) | Tailored, specific, familiar | The primary staff delivering the program were culturally Latino, usually born in a Latin American country, and native Spanish speakers with proficiency in English | Not described | The primary staff delivering the program were Spanish speakers with proficiency in English. Materials adapted and translated for use with Latino participants | Not described | Sessions were family centered and child focused, focusing on culturally familiar and acceptable approaches to increasing activity and decreasing caloric intake, rather than wt loss |
| D’Angelo et al32 (2009) | Sensitive, relevant, adapted, aware | A multidisciplinary, multiethnic group of researchers, including bilingual and/or bicultural preventionists, developed the adaptation; feedback from focus groups was incorporated | Information was provided to mothers about the similarities and differences about raising children in the United States versus their country of origin | Scales and interview questions were offered in both Spanish and English | Not described | Several modifications were made to better align with the target population’s values, such as placing more emphasis on respeto (respect) and confianza (trust) |
| Falbe et al33 (2015) and Falbe et al34 (2017) | Sensitive, relevant, tailored, specific, congruent | A promotora was involved in each intervention session. Feedback was incorporated on the basis of focus groups and interviews with parents | Not described | Promotoras and the dietician were bilingual native Spanish speakers. One of the 2 physicians was fluent in Spanish, and the other spoke basic Spanish | Module on immigration, focused on foods and recipes common in the target population | Targeted cultural perceptions and practices, such as viewing children with obesity as healthy. It was also designed to be family centered, with a focus on parenting |
| Feutz and Andresen35 (2013) | Appropriate, based, acceptable | Not described | Not described | Used culturally and linguistically appropriate materials and activities that relate Hispanic cultural values | Used music and videos relevant to the population | Emphasizes the Latino cultural beliefs of familismo, machismo, marianismo, respeto, and personalismo |
| Hamilton et al36 (2013) | Competent, effective | A parent advisory group that meets monthly provides a mechanism for families to participate in the development of the program | Not described | The family liaison is bilingual in English and Spanish | Not described | Not described |
| Herbst et al37 (2019) | Sensitive, appropriate, tailored | Not described | Not described | Handouts were written at a lower literacy level to facilitate greater understanding | Not described | Handouts were tailored to address common patient barriers associated with social determinants of health |
| La Roche et al38 (2006) | Competent | Not described | Framed patients’ asthma symptoms and problems within a historical and socioeconomic context in which health disparities are aggravated by social and economic force | Not described | Not described | Discussed topics in groups in a manner consistent with the allocentric orientation |
| Landback et al39 (2009) | Relevant | Preliminary tests in 2 clinics were done, which generated feedback from adolescents, which was used to adjust the intervention design | Not described | Not described | At the completion of each module, there was an Internet-based reward, which directed the adolescent to an Internet site on which they could play a game or listen to music | Each module lesson included teenager stories, skill-building exercises, and behavior change assignments |
| Lewin et al40 (2015) | Sensitive, appropriate, adapted | To inform the adaptation, focus groups and interviews were conducted with teen-aged fathers and mothers | Not described | Not described | Not described | Sessions were adapted to be more experiential and active than didactic to be more engaging for the teen-aged parents. Homework assignments were eliminated because of a negative connotation |
| López et al41 (2018) | Sensitive, relevant, adapted, tailored, competent, specific | The intervention was delivered by a clinic-employed promotora to help enhance trust between the clinic and participants | Not described | The PACE program was translated into Spanish and the promotora spoke Spanish with participants | Included videotapes, posters, and handouts as part of the intervention | The program specifically targeted traditional engagement barriers, such as child care, transportation, and food, to help ensure participation. The intervention of the program incorporated cultural differences in parenting |
| Mazzeo et al42 (2014) | Sensitive | Not described | Not described | Not described | Not described | Allowed all participants to consider how culture influences their behaviors and beliefs; the intervention was not exclusively tailored to African American participants |
| Mirza et al43 (2013) | Appropriate, adapted, competent | Not described | Not described | Not described | Not described | Hypothesized that a low-glycemic-load diet might be particularly useful for Hispanic children; the authors note that they adapted this intervention for the Hispanic culture but do not otherwise specify how this was done |
| Nitsos et al44 (2017) | Appropriate, adapted, tailored, acceptable, targeted | Not described | Not described | Materials were translated to Spanish for LEP participants | Educational handouts were provided to accompany intervention teaching | Not described |
| O’Connor et al45 (2020) | Adapted, centered | Not described | Not described | All facilitators were bilingual in Spanish and English. Families were given the option to participate in English or Spanish | Foods and games were modified to be common ones known to Hispanic families, and the program material’s reading level was lowered | The curriculum was enhanced with cultural values and addressed barriers for participation and engagement for Hispanic fathers; engaged mothers more by inviting them to a closed Facebook group for the program and sending them weekly videos of that week’s content |
| Reavy et al46 (2012) | Appropriate, safe, competent | Clinic peer health advisors were hired from refugee communities; used focus groups and individual interviews to elicit feedback from stakeholders | Not described | Peer health advisors and certified medical interpreters were available for the following languages: Arabic, Burmese, Dari, Farsi, French, Karen, Kirundi, Lingala, Nepali, Pashtu, Russian, Somali, Swahili, and Uzbek | The clinic is decorated with art from refugees’ native countries. A large map noting the native homes of all refugees hangs on a prominent wall | For the positions to be culturally safe, only women can apply for the position of health advisor for the prenatal and pediatric C.A.R.E. Clinic because refugee women in the C.A.R.E. Clinic have experienced trauma in their home countries |
| Rice et al47 (2003) | Appropriate | Incorporated feedback from stakeholders in 4 pilot focus groups, a pilot intervention, clinic, and school trials | Project TNT discusses epidemiology of tobacco-related diseases and prevalence of smoking and other tobacco use among youth and risk factors related to tobacco use. Participants were given smoking data tailored to Arab countries | Materials were provided in Arabic as well as English | Not described | Participants requested same-sex intervention sessions and a same-sex health educator |
| Ryan et al48 (2020) | Sensitive, relevant, tailored | The research team built a partnership with a local Baltimore public charter school and engaged youth in creating the content and filming | Not described | Not described | Not described | Not described |
| Serpas et al49 (2013) | Sensitive, appropriate, accurate | Met with community leaders and conducted focus groups to help inform strategy; adapted questionnaires were piloted with community representatives to ensure cultural and linguistic accuracy | Not described | The San Diego Healthy Wt Collaborative Web site was accessible in both English and Spanish, as were educational materials provided by the primary care clinic; translated health education in examination rooms | Not described | Not described |
| Svetaz et al50 (2016) | Sensitive, appropriate, competent, inclusive | Cultural concordance between patient and provider was a key element. Parents attended focus groups | Not described | Handouts are available in both English and Spanish; bilingual intervention facilitators | Not described | Interventions take into consideration Latino values and preferences, cultural navigation, and challenges related to immigration. Confidentiality was emphasized |
| Valdez et al51 (2013) | Sensitive, adapted, specific, equivalent, representative, centered | Focus groups were led by bilingual facilitators after delivery of the intervention for evaluation and future adaptation | Not described | Native Spanish speakers facilitated the adult groups in Spanish. Facilitators in the youth groups were trained graduate students in counseling psychology and social work who were bilingual in English and Spanish | A culturally representative meal was offered at each session | The 4 following sociocultural concepts were added: (1) acculturative and immigration stressors, (2) parental involvement and monitoring of children’s activities outside the home, (3) marital relationships in the context of acculturative stress and maternal depression, and (4) cultural assets, such as traditions, support from extended family, and ethnic socialization (ie, cultural pride and coping with discrimination) |
C.A.R.E., Culturally Appropriate Resources and Education; LEP, limited English proficiency; PACE, Parenting Our Children to Excellence; TNT, Toward No Tobacco Use.
Interventions were focused on a variety of cultural groups (Table 2), with the majority of interventions (19 [83%]) conceptualizing culture as race and/or ethnicity. Of these, 13 (57%) were focused on participants of Hispanic background¶ and 1 each on those of Chinese30 and Arab American47 backgrounds. Mazzeo et al42 were primarily interested in reaching African American children, although they allowed participants of any race and/or ethnicity to participate. La Roche et al38 focused on participants described as “ethnic and racial minority children.” Thirteen (57%) interventions included non–racial and/or ethnic elements of culture, including urban environment,37,38,40,48 income,28,29,37,40 adolescence,30,35,39,47,50 language proficiency,44 refugee status,46 and special health care needs.36
Cultural Adaptation Strategies
Eleven (48%) interventions were developed de novo,28–31,37–39,42,46,48,49 whereas the other 12 (52%) were culturally adapted from a previously existing intervention.# Examples of culturally adapted interventions include adaptation of the Beardslee Preventive Intervention Program for Depression for use with low-income Hispanic families by D’Angelo et al,32 adaptation of the Toward No Tobacco program for use with Arab American adolescents by Rice et al,47 and adaptation of Healthy Dads, Healthy Kids into Papás Saludables, Niños Saludables for Hispanic fathers and children by O’Connor et al.45
How Cultural Sensitivity Was Incorporated Into Interventions
For this review, we have categorized aspects of each intervention according to the framework by Kreuter et al21, which has been described above (Table 4). Nineteen (83%) interventions used sociocultural strategies.27–35,37–43,45–47,50,51 Nine (39%) included the provision of content appropriate to the target population,** 10 (40%) were focused on culturally relevant values and preferences,†† and 3 (13%) incorporated use of family-centered approaches.27,31,33,34 Four (17%) interventions explicitly discussed acculturative stress, or stress that emerges from the acculturation process.32–34,50,51 Examples of tailored sociocultural strategies include adaptation of sessions to be more experiential and active (rather than didactic) to promote parental engagement by Lewin et al,40 and Feutz and Andresen’s35 emphasis on the Hispanic/Latino cultural beliefs of familismo (the importance of family relationships), machismo and marianismo (men’s and women’s gender roles), and respeto (respect).
From a constituent-level perspective, 9 (39%) used focus groups to inform intervention development‡‡ and 7 (30%) used community-based intervention staff (Hamilton et al36 incorporated a family liaison).28,29,31–34,36,41,46 Three (13%) interventions that were focused on Hispanic families relied on the expertise of promotoras (community health workers).28,29,33,34,41 Other constituent-level strategies used to inform interventions included use of community advisory boards, such as the parent advisory group, which provided a monthly feedback mechanism for stakeholders in the medical home program for children with special health care needs by Hamilton et al.36 D’Angelo et al32 reported use of bicultural research staff for their multidisciplinary, multiethnic adaptation research team.
Linguistic strategies were primarily focused on conducting or having the option to conduct the intervention in a language other than English. Ten (43%) interventions included bilingual facilitators or research staff,31–34,36,41,45–47,50,51 and 9 (39%) involved translation of materials.§§ Two (9%) interventions adapted reading materials to improve accessibility and attend to health literacy.28,29,37
Ten (43%)‖‖ of the interventions used peripheral strategies, such as providing food commonly eaten by the target population28–30,45,51 or using culturally relevant images and materials.28,29,35,39,41,46 Examples include use of art from refugees’ native countries to decorate the clinic by Reavy et al,46 use of Internet-based rewards for adolescents who completed intervention modules by Landback et al,39 and opportunities for participants to sample healthy foods from both Chinese and Western cultures provided by Chen et al.30
Three (13%) interventions used evidential strategies.32,38,47 D’Angelo et al32 provided mothers with information regarding the similarities and differences about raising children in the United States versus their country of origin, Rice et al47 informed Arab American teenagers of tailored tobacco-related epidemiology and smoking data, and La Roche et al38 framed patients’ asthma symptoms and problems within a historical and socioeconomic context in which health disparities are aggravated by social and economic force.
Discussions of Structural Factors
Three (13%) interventions made explicit mentions of racism, poverty, or other structural inequities.32,38,51 La Roche et al38 used a social and economic lens to view health disparities as part of an evidential strategy within their intervention. D’Angelo et al32 and Valdez et al51 both studied depression and focused on structurally oppressive stressors, including discrimination, prejudice, poverty, and acculturative and immigration-related stressors.
Intervention Evaluations: Acceptability and Feasibility
Sample sizes for postintervention evaluations were generally small, ranging from 1732 to 227,46 with a mean of 50 and median of 28 (Lewin et al40 did not report an evaluation sample size). In 18 (78%) evaluations, authors reported feasibility data (Table 3).27–35,37–43,45,47,48,51 For example, Chen et al30 concluded that their Internet-based intervention was feasible on the basis of 75% of participants accessing the Fitbit program several times a week and 90% completing the 6-month follow-up. Herbst et al37 proposed that a motivational interviewing intervention was both feasible and sustainable on the basis of family attendance of clinic follow-up improving from 11% to 34% preintervention and post intervention. Sixteen evaluations (70%) described acceptability.28–36,39–42,45–47,50,51 Six (26%) surveyed whether participants would be willing to recommend the intervention to others; all or almost all participants recommended their respective interventions.30,35,39,42,45,50 The authors of another 6 (26%) reported high participant satisfaction.28,29,36,41,45,50,51 Specific examples include Svetaz et al50 stating that 100% of pediatric patients reported being fully satisfied with clinic outcomes and Feutz and Andresen35 reporting that intervention participants evaluated the program positively, enjoyed the activities, and would strongly recommend the intervention to others.
Intervention Evaluations: Health Outcomes
Data on health outcomes were reported in 19 (83%) evaluations (Table 3).27–35,37,38,41–49,51 Seventeen of these 19 described positive changes in health outcomes, with the authors of 13 reporting statistical significance.27–35,37,38,41–44 Examples include the validated tobacco quit rate of 37.5% reported by Rice et al,47 the decrease in child behavior problems (P = .04) and parenting stress (P = .01) reported by López et al,41 and the increase in childhood immunization rates to 100% (no baseline comparison rate reported) reported by Reavy et al.46 In other evaluations, authors reported positive outcomes but did not provide statistical analysis: Valdez et al51 reported improvement in child behaviors and decreased conflicts with mothers, and Serpas et al49 reported an increased proportion of pediatric weight assessments charted. Two (9%) evaluations with statistical analysis described no significant observed changes in health outcomes. O’Connor et al45 found no statistically significant differences in weight, BMI, heart rate, blood pressure, waist circumference, kilocalories (Food Frequency Questionnaire), moderate or vigorous physical activity, or sedentary time. The study by Ryan et al48 of helmet usage by children and parental requirement of helmet usage revealed no significant differences.
Cost-effectiveness
In one (4%) intervention,33,34 the authors examined cost-effectiveness, reporting that the Active and Healthy Families intervention series, with 10 participating families, would generate ∼$5000 in net income for a practice after reimbursement.
Discussion
The articles reviewed here offer preliminary evidence (of mixed quality) that culturally sensitive interventions may be feasible and acceptable, with some also revealing that these interventions were effective in changing in health outcomes. These results were observed in studies that used newly developed interventions as well as those that culturally adapted existing interventions. However, although many of the included interventions revealed promising preliminary data, few were randomized clinical trials powered to detect differences in outcomes.
Most of the strategies used to incorporate culturally sensitive care in interventions were aligned with the framework by Kreuter et al.21 In particular, many studies described including perspectives of community stakeholders in intervention development and testing (ie, constituent-level strategies). Previous literature has called for centering the voices of community members52 and inclusion of communities in cocreating and conceptualizing research.53 In addition, it has been suggested that to be effective, the patient-centered medical home should extend beyond the health care setting to the communities where patients and families live, work, and play.54 Results of the studies included in this review reinforce the feasibility of including community stakeholder perspectives when developing interventions for pediatric primary care settings.
The majority of studies developed interventions for specific racial and ethnic groups, particularly families identifying as Hispanic and/or Latino. Although a family’s racial and ethnic background may be an important factor in shaping their identity and lived experience, culture includes multiple interweaving identities and experiences. Intersectionality describes how various identities (eg, gender identity, income, immigration) intersect to determine social location, which, in turn, shapes health and health care quality and access.55,56 Although some interventions considered intersectional identities (eg, non–English-speaking Hispanic/Latino communities), many did not. In addition, the majority of interventions developed for families of specific racial and ethnic backgrounds considered groups in an aggregated way (eg, Hispanic/Latino, Asian American). There have been multiple calls to disaggregate racial and ethnic groups to better account for within-group diversity in disparities.57,58 Doing so in cultural sensitivity interventions would allow for a broader range of cultures, including many that do not appear in the summarized review, to be considered and supported through research and primary care provision.
Important gaps were noted from this review, such as few interventions that considered cultural differences between parents and children, included structural-level factors, and attended to health literacy. Children, parents, and other family members (ie, grandparents) may have different language preferences, cultural values and practices, intersectional identities, and experiences of acculturative stress.59–62 Considering these differences as part of culturally sensitive interventions may enhance communication between the family and the provider (as well as between family members), increase feelings of respect and trust, identify important nuances in how family members understand diagnoses and treatment recommendations, and ultimately improve the effectiveness of care. Additionally, in the majority of reviewed interventions, authors conceptualized “culture” as identities or values ascribed to specific communities without considering structural influences. For example, few of the interventions for Hispanic/Latino communities considered xenophobia and racist immigration policies and practices63 that may influence a family’s ability to access health care. However, structural-level oppressions, such as environmental injustice,64 police violence,65 mass incarceration,66 and redlining and/or racialized residential segregation,5,67,68 are deeply impactful on health and well-being. Finally, just 2 studies described attending to health literacy, a critical component of achieving health equity, per Healthy People 2030 guidelines.69 Future interventions should address health literacy on multiple levels to ensure families are able to make informed health-related decisions.
This review is subject to several limitations. Although we attempted to develop an inclusive search term strategy, we recognize that many terms are used to describe concepts related to cultural sensitivity.70 As a result, we may have missed articles that used a term related to cultural sensitivity that was not included in our search. Promising interventions that have not been published are also missing from this review. We focused on US-based studies, so these results may not be generalizable to pediatric health care settings in other countries. Furthermore, only a small number of cultural groups were addressed in reviewed studies. Culturally sensitive approaches are needed for a much broader range of cultural groups. Finally, this review was focused on the pediatric primary care setting. Future research is needed to better understand how to apply results from pediatric primary care to other pediatric health care settings. For example, inpatient and subspeciality settings may require different strategies for culturally sensitive interventions based on differences in length and frequency that a patient engages with those health care spaces. We were also unable to determine the effectiveness of specific aspects of culturally sensitive care because of the heterogeneity of the included interventions. Finally, although not a limitation of our review, we recognize that the included studies are subject to high risk of bias due to their sample sizes and methods. These studies nevertheless provide a foundation for future efforts to create and evaluate culturally sensitive interventions.
Conclusions
This review highlights how pediatric primary care settings have incorporated tenets of culturally sensitive practices into interventions for children and families and elucidates several areas for future research. More work rigorously testing culturally sensitive interventions is necessary. We recognize that RCTs, considered the gold standard for intervention evaluation, may be less feasible in primary care settings. Alternative designs (eg, stepped wedge [intervention implemented sequentially at different sites], interrupted time series) may be more feasible and less cost-prohibitive while still providing high-quality evidence for intervention efficacy and/or effectiveness.71 Additionally, use of hybrid effectiveness-implementation trials and adaptive trials may help measure clinical outcomes while also taking practical issues of implementation, scaling, and cost-effectiveness into consideration.72
Future researchers should examine similarities and differences among family members regarding their cultural needs and preferences as well as develop culturally sensitive interventions that disaggregate racial and ethnic groups and consider how intersecting identities may impact families’ needs. Future interventions focused on culturally sensitive care should also incorporate structural-level factors that underlie inequities. Examples include providing training for intervention facilitators on structural inequities (eg, for asthma interventions, facilitators should know about housing policies and poor air quality), including content on how structural inequities have impacted health, and measuring constructs such as racism as part of intervention evaluation. Additionally, institutional-level changes to dismantle structural inequities in health care (eg, recruitment, retention, and support of underrepresented minority medical staff) are essential to providing effective culturally sensitive interventions in pediatric health care settings (see study by Jindal et al73 for a more extensive discussion). This systematic review provides preliminary evidence to support how culturally sensitive interventions in pediatric primary care settings are feasible and acceptable and underscores how future work is needed to test, implement, and scale these interventions so they can be used as a tool to promote health equity.
Glossary
- RCT
randomized controlled trial
Footnotes
Dr Okoniewski screened and abstracted included articles, drafted the initial manuscript, and reviewed and revised the manuscript; Ms Sundaram screened included articles, supported abstraction, and provided critical edits to the manuscript; Drs Chaves-Gnecco and McAnany evaluated study quality and provided critical edits to the manuscript; Dr Cowden helped conceptualize the systematic review and reviewed and revised the manuscript; Dr Ragavan conceptualized the systematic review, provided arbitration for article inclusion and study quality evaluation, drafted portions of the manuscripts, and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
This trial has been registered with PROSPERO, the International Prospective Register of Systematic Reviews (https://www.crd.york.ac.uk/prospero/) (identifier CRD42020083916).
FUNDING: Dr Ragavan is supported by a National Center for Advancing Translational Sciences University of Pittsburgh KL2 grant (TR001856; Rubio). The funder had no role in this study. Funded by the National Institutes of Health (NIH).
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2021-052883.
References
- 1. Feagin J, Bennefield Z. Systemic racism and U.S. health care. Soc Sci Med. 2014;103:7–14 [DOI] [PubMed] [Google Scholar]
- 2. Chokshi DA. Income, poverty, and health inequality. JAMA. 2018;319(13):1312–1313 [DOI] [PubMed] [Google Scholar]
- 3. Diamond L, Izquierdo K, Canfield D, Matsoukas K, Gany F. A systematic review of the impact of patient-physician non-English language concordance on quality of care and outcomes. J Gen Intern Med. 2019;34(8):1591–1606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Flores G; Committee on Pediatric Research . Technical report--racial and ethnic disparities in the health and health care of children. Pediatrics. 2010;125(4). Available at: www.pediatrics.org/cgi/content/full/125/4/e979 [DOI] [PubMed] [Google Scholar]
- 5. Bailey ZD, Feldman JM, Bassett MT. How structural racism works - racist policies as a root cause of U.S. racial health inequities. N Engl J Med. 2021;384(8):768–773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Suleman S, Garber KD, Rutkow L. Xenophobia as a determinant of health: an integrative review. J Public Health Policy. 2018;39(4):407–423 [DOI] [PubMed] [Google Scholar]
- 7. Flores G. Families facing language barriers in healthcare: when will policy catch up with the demographics and evidence? J Pediatr. 2014;164(6):1261–1264 [DOI] [PubMed] [Google Scholar]
- 8. Cohen AL, Christakis DA. Primary language of parent is associated with disparities in pediatric preventive care. J Pediatr. 2006;148(2):254–258 [DOI] [PubMed] [Google Scholar]
- 9. DeCamp LR, Choi H, Davis MM. Medical home disparities for Latino children by parental language of interview. J Health Care Poor Underserved. 2011;22(4): 1151–1166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Britton CV; American Academy of Pediatrics Committee on Pediatric Workforce . Ensuring culturally effective pediatric care: implications for education and health policy. Pediatrics. 2004;114(6):1677–1685 [DOI] [PubMed] [Google Scholar]
- 11. The American Board of Pediatrics . National events intensify ABP’s commitment to diversity, inclusion. Available at: https://www.abp.org/news/national- events-intensify-abps-commitment- diversity-inclusion. Accessed July 1, 2021
- 12. Institute of Medicine Committee on Quality of Health Care in America . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001 [Google Scholar]
- 13. Smedley BD, Stith AY, Nelson AR, eds; Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care . Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003 [PubMed] [Google Scholar]
- 14. Brotanek JM, Seeley CE, Flores G. The importance of cultural competency in general pediatrics. Curr Opin Pediatr. 2008;20(6):711–718 [DOI] [PubMed] [Google Scholar]
- 15. Raphael JL. Observations from the balcony: directions for pediatric health disparities research and policy. J Appl Res Child. 2013;4(1):7. [PMC free article] [PubMed] [Google Scholar]
- 16. Stange KC, Nutting PA, Miller WL, et al. Defining and measuring the patient-centered medical home. J Gen Intern Med. 2010;25(6):601–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ragavan MI, Griffith KN, Cowden JD, Colvin JD, Bair-Merritt M. Parental perceptions of culturally sensitive care and well-child visit quality. Acad Pediatr. 2020;20(2):234–240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. American Academy of Pediatrics . Interpreter services. Available at: https://www.aap.org/en-us/professional-resources/practice- transformation/managing-patients/Pages/chapter-5.aspx. Accessed July 1, 2021
- 19. US Department of Health and Human Services, Office of Minority Health . National standards for culturally and linguistically appropriate services (CLAS) in health and health care. Available at: https://thinkculturalhealth.hhs.gov/assets/pdfs/EnhancedNational CLASStandards.pdf. Accessed July 1, 2021
- 20. Ragavan MI, Cowden JD. The complexities of assessing language and interpreter preferences in pediatrics. Health Equity. 2018;2(1):70–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003;30(2):133–146 [DOI] [PubMed] [Google Scholar]
- 22. Farmer PE, Nizeye B, Stulac S, Keshavjee S. Structural violence and clinical medicine. PLoS Med. 2006;3(10):e449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Flores A. How the U.S. Hispanic population is changing. Available at: https://www.pewresearch.org/fact-tank/2017/09/18/how-the-u-s-hispanic-population- is-changing/. Accessed July 1, 2021
- 25. Covidence Systematic Review Software [computer program]. Melbourne, Australia: Veritas Health Innovation [Google Scholar]
- 26. National Health and Medical Research Council . NHMRC levels of evidence and grades for recommendations for developers of guidelines. Available at: https://www.nhmrc.gov.au/sites/default/files/images/NHMRC%20Levels% 20and%20Grades%20(2009).pdf. Accessed July 1, 2021
- 27. Arauz Boudreau AD, Kurowski DS, Gonzalez WI, Dimond MA, Oreskovic NM. Latino families, primary care, and childhood obesity: a randomized controlled trial. Am J Prev Med. 2013;44(3, suppl 3):S247–S257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bender MS, Nader PR, Kennedy C, Gahagan S. A culturally appropriate intervention to improve health behaviors in Hispanic mother-child dyads. Child Obes. 2013;9(2):157–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bender MS, Clark MJ, Gahagan S. Community engagement approach: developing a culturally appropriate intervention for Hispanic mother-child dyads. J Transcult Nurs. 2014;25(4): 373–382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chen JL, Guedes CM, Lung AE. Smartphone-based healthy weight management intervention for Chinese American adolescents: short-term efficacy and factors associated with decreased weight. J Adolesc Health. 2019;64(4):443–449 [DOI] [PubMed] [Google Scholar]
- 31. Cronk CE, Hoffmann RG, Mueller MJ, Zerpa-Uriona V, Dasgupta M, Enriquez F. Effects of a culturally tailored intervention on changes in body mass index and health-related quality of life of Latino children and their parents. Am J Health Promot. 2011;25(4):e1–e11 [DOI] [PubMed] [Google Scholar]
- 32. D’Angelo EJ, Llerena-Ouinn R, Shapiro R, et al. Adaptation of the preventive intervention program for depression for use with predominantly low-income Latino families. Fam Process. 2009;48(2): 269–291 [DOI] [PubMed] [Google Scholar]
- 33. Falbe J, Cadiz AA, Tantoco NK, Thompson HR, Madsen KA. Active and healthy families: a randomized controlled trial of a culturally tailored obesity intervention for Latino children. Acad Pediatr. 2015;15(4):386–395 [DOI] [PubMed] [Google Scholar]
- 34. Falbe J, Friedman LE, Sokal-Gutierrez K, Thompson HR, Tantoco NK, Madsen KA. “She gave me the confidence to open up”: bridging communication by promotoras in a childhood obesity intervention for Latino families. Health Educ Behav. 2017;44(5):728–737 [DOI] [PubMed] [Google Scholar]
- 35. Feutz K, Andresen P. Cuidate: implementation of a culturally based sexual risk reduction program for Hispanic adolescents. Hisp Health Care Int. 2013;11(4):187–193 [DOI] [PubMed] [Google Scholar]
- 36. Hamilton LJ, Lerner CF, Presson AP, Klitzner TS. Effects of a medical home program for children with special health care needs on parental perceptions of care in an ethnically diverse patient population. Matern Child Health J. 2013;17(3):463–469 [DOI] [PubMed] [Google Scholar]
- 37. Herbst RB, Khalsa AS, Schlottmann H, Kerrey MK, Glass K, Burkhardt MC. Effective implementation of culturally appropriate tools in addressing overweight and obesity in an urban underserved early childhood population in pediatric primary care. Clin Pediatr (Phila). 2019;58(5):511–520 [DOI] [PubMed] [Google Scholar]
- 38. La Roche MJ, Koinis-Mitchell D, Gualdron L. A culturally competent asthma management intervention: a randomized controlled pilot study. Ann Allergy Asthma Immunol. 2006;96(1): 80–85 [DOI] [PubMed] [Google Scholar]
- 39. Landback J, Prochaska M, Ellis J, et al. From prototype to product: development of a primary care/internet based depression prevention intervention for adolescents (CATCH-IT). Community Ment Health J. 2009;45(5):349–354 [DOI] [PubMed] [Google Scholar]
- 40. Lewin A, Hodgkinson S, Waters DM, Prempeh HA, Beers LS, Feinberg ME. Strengthening positive coparenting in teen parents: a cultural adaptation of an evidence-based intervention. J Prim Prev. 2015;36(3):139–154 [DOI] [PubMed] [Google Scholar]
- 41. López CM, Davidson TM, Moreland AD. Reaching Latino families through pediatric primary care: outcomes of the CANNE parent training program. Child Fam Behav Ther. 2018;40(1):26–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mazzeo SE, Kelly NR, Stern M, et al. Parent skills training to enhance weight loss in overweight children: evaluation of NOURISH. Eat Behav. 2014;15(2): 225–229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mirza NM, Palmer MG, Sinclair KB, et al. Effects of a low glycemic load or a low-fat dietary intervention on body weight in obese Hispanic American children and adolescents: a randomized controlled trial. Am J Clin Nutr. 2013;97(2): 276–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Nitsos A, Estrada RD, Messias DKH. Tummy time for Latinos with limited English proficiency: evaluating the feasibility of a cultural and linguistically adapted parent education intervention. J Pediatr Nurs. 2017;36:31–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. O’Connor TM, Beltran A, Musaad S, et al. Feasibility of targeting Hispanic fathers and children in an obesity intervention: Papás Saludables Niños Saludables. Child Obes. 2020;16(6):379–392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Reavy K, Hobbs J, Hereford M, Crosby K. A new clinic model for refugee health care: adaptation of cultural safety. Rural Remote Health. 2012;12:1826. [PubMed] [Google Scholar]
- 47. Rice VH, Templin T, Kulwicki A. Arab-American adolescent tobacco use: four pilot studies. Prev Med. 2003;37(5): 492–498 [DOI] [PubMed] [Google Scholar]
- 48. Ryan LM, Solomon BS, Ziegfeld S, et al. Evaluation of a culturally tailored educational video intervention to promote bike helmet safety for urban children: a pilot study. Health Promot Pract. 2020;21(6):872–876 [DOI] [PubMed] [Google Scholar]
- 49. Serpas S, Brandstein K, McKennett M, Hillidge S, Zive M, Nader PR. San Diego Healthy Weight Collaborative: a systems approach to address childhood obesity. J Health Care Poor Underserved. 2013;24(2, suppl):80–96 [DOI] [PubMed] [Google Scholar]
- 50. Svetaz MV, Garcia-Huidobro D, Hurtado GA, et al. Can a healthy youth development clinic serving Latino families be youth friendly and family oriented? A mixed-methods evaluation. Int J Adolesc Med Health. 2016;28(1):61–68 [DOI] [PubMed] [Google Scholar]
- 51. Valdez CR, Padilla B, Moore SM, Magaña S. Feasibility, acceptability, and preliminary outcomes of the Fortalezas Familiares intervention for Latino families facing maternal depression. Fam Process. 2013;52(3):394–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hargraves M. Elevating the voices of rural minority women. Am J Public Health. 2002;92(4):514–515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gill S, Kuwahara R, Wilce M. Through a culturally competent lens: why the program evaluation standards matter. Health Promot Pract. 2016;17(1):5–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Franz BA, Murphy JW. The patient-centered medical home as a community-based strategy. Perm J. 2017;21:17–002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. 2014;110:10–17 [DOI] [PubMed] [Google Scholar]
- 56. Bowleg L. The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Read JG, Lynch SM, West JS. Disaggregating heterogeneity among non-Hispanic whites: evidence and implications for U.S. racial/ethnic health disparities. Popul Res Policy Rev. 2021;40(1):9–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Rubin V, Ngo D, Ross A, Butler D, Balaram N. Counting a diverse nation: disaggregating data on race and ethnicity to advance a culture of health. 2021. Available at: www.policylink.org/sites/default/files/Counting_a_Diverse_ Nation_08_15_18.pdf. Accessed July 1, 2021
- 59. Budiman A, Tamir C, Mora L, Noe-Bustamante L. Facts on U.S. immigrants, 2018. Available at: https://www.pewresearch.org/hispanic/2019/06/03/facts-on-u-s-immigrants/. Accessed July 1, 2021
- 60. Child Trends . Immigrant children. Available at: https://www.childtrends.org/?indicators=immigrant-children. Accessed July 1, 2021
- 61. Ayalew B, Dawson-Hahn E, Cholera R, et al. The health of children in immigrant families: key drivers and research gaps through an equity lens. Acad Pediatr. 2021;21(5):777–792 [DOI] [PubMed] [Google Scholar]
- 62. Schwartz SJ, Unger JB, Zamboanga BL, Szapocznik J. Rethinking the concept of acculturation: implications for theory and research. Am Psychol. 2010;65(4):237–251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Martinez O, Wu E, Sandfort T, et al. Evaluating the impact of immigration policies on health status among undocumented immigrants: a systematic review [published correction appears in J Immigr Minor Health. 2016;18(1):288]. J Immigr Minor Health. 2015;17(3):947–970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Landrigan PJ, Rauh VA, Galvez MP. Environmental justice and the health of children. Mt Sinai J Med. 2010;77(2): 178–187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Alang S, McAlpine D, McCreedy E, Hardeman R. Police brutality and Black health: setting the agenda for public health scholars. Am J Public Health. 2017;107(5):662–665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Blankenship KM, Del Rio Gonzalez AM, Keene DE, Groves AK, Rosenberg AP. Mass incarceration, race inequality, and health: expanding concepts and assessing impacts on well-being. Soc Sci Med. 2018;215:45–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Hardeman RR, Medina EM, Kozhimannil KB. Structural racism and supporting Black lives - the role of health professionals. N Engl J Med. 2016;375(22): 2113–2115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiol Rev. 2009;31:178–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Office of Disease Prevention and Health Promotion, US Department of Health and Human Services . Health literacy in healthy people 2030. 2020. Available at: https://health.gov/our-work/healthy- people/healthy-people-2030/health- literacy-healthy-people-2030. Accessed July 1, 2021
- 70. Curtis E, Jones R, Tipene-Leach D, et al. Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. Int J Equity Health. 2019;18(1):174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Sanson-Fisher RW, D’Este CA, Carey ML, Noble N, Paul CL. Evaluation of systems-oriented public health interventions: alternative research designs. Annu Rev Public Health. 2014;35:9–27 [DOI] [PubMed] [Google Scholar]
- 72. Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Jindal M, Heard-Garris N, Empey A, Perrin EC, Zuckerman KE, Johnson TJ. Getting “our house” in order: re-building academic pediatrics by dismantling the anti-black racist foundation. Acad Pediatr. 2020;20(8):1044–1050 [DOI] [PubMed] [Google Scholar]
- 74. Eremenco SL, Cella D, Arnold BJ. A comprehensive method for the translation and cross-cultural validation of health status questionnaires. Eval Health Prof. 2005;28(2):212–232 [DOI] [PubMed] [Google Scholar]