Abstract
Purpose:
The objective of the study was to assess the effect of increased screen time on ocular health during the coronavirus disease (COVID-19) crisis.
Materials and Method:
An online pretested, self-reported questionnaire with relevant details was generated through Google form and sent to participants. Chi-square or Fisher’s exact test was used to investigate the associations between the qualitative variables. The associated risk factors of number and frequency of ocular health problems were analysed by univariate and multivariate logistic regression.
Result:
A total of 435 responses were considered where 48.5% (N = 211) were female participants and 51.5% (N = 224) were male. Average age of the participants was 35 years. 89% of the participants reported an increase in the screen time during the during the lockdown period. Younger age group reported to have greater screen time than the older participants (p = 0.001) and hence experienced more symptoms of digital eye strain (DES) (p = 0.003). The most common symptoms associated with digital eye strain in our study were eyestrain 52.8% (N = 230) and headache 31.3% (N = 136). In total, 81.37% (354/435) of participants had experienced at least one symptom related to digital screen usage.
Conclusion:
DES is non-vision-threatening but discomfort caused due to it can have implications on overall physical, mental, and social well-being. The study highlights the increase in digital screen time during the pandemic and the resultant eye strain. There is need of spreading awareness regarding the adverse effects of digital device use and the preventive measures to safeguard our ocular health.
Keywords: COVID-19, computer vision syndrome, digital eye strain, ocular health
Introduction
Digital eye strain or computer vision syndrome are interchangeable terms and involve a spectrum of ocular and non-ocular symptoms among the users of visual display units.[1] Ocular symptoms include tearing, tired eyes, blurred vision, burning sensation, redness and double vision while non-ocular symptoms include neck pain, general fatigue, headache, and back pain. The prevalence of symptoms due to digital eye strain ranges from 25 to 93%, as reported in different studies.[2] These symptoms can be further aggravated by improper lighting conditions.[3] These days, many of us have jobs that require us to stare at computer screens for hours at a time. That can put a real strain on our eyes. Working adults aren’t the only ones affected. Kids who stare at smartphones or use computers can have issues, too, especially if the lighting and their posture are less than ideal.
The COVID-19 pandemic has caused widespread restriction in outdoor activities causing a lot of inconvenience for everyone. As a result, people across the world are using alternative ways for both work and leisure. Closure of offices and workplaces make the people work from home, attending online meetings, and video conferences resulting in increase in screen time.[4,5] To avoid gatherings and maintaining social distance, multiple webinars are being organized. Limitation of outdoor activities has also led people to look for alternative ways of entertainment at home like video games, television, and online streaming platforms. Inability to connect and physically interact with people has led to an increase in the usage of smart phones or other digital screen for social media, video calling, and online shopping. There has been a complete closure of schools and colleges and students are given alternative resources which are mostly online. These lifestyle changes are creating havoc in terms of deteriorating mental as well as physical health of people.[6,7]
India has crossed massive target of 100 crores vaccination and life of people has started coming back to track.[8] With gradual opening of schools and offices the online burden is slowly decreasing but still majority of population have adapted to this modern way of living at the cost of their health. This online survey mainly focuses on how this COVID-19 crisis has affected the ocular health and will also give an insight on the awareness regarding DES. The aim of the study was to assess the effect of increased screen time on ocular health of people during the COVID-19 crisis.
Material and Methods
It was an online-based cross-sectional survey aimed at individuals above 18 years of age who used digital device and could understand the purpose of survey as written in English language and willing to give consent to participate in the survey. Exclusion criteria included participants having congenital eye disease, or with history of previous eye trauma. Snow ball technique/chain sampling technique (non-probability technique) where existing study subjects recruit future subjects from among their acquaintances was used. The study was approved by the institutional ethics committee, and a written informed consent was obtained from all the participants. An online self-reported questionnaire with relevant details using Google forms was circulated through various online platforms such as email, WhatsApp, and other social media accounts to different known contacts of the investigators throughout the country. Different demographics of people were targeted so as to get a sample representative of each of the subgroups – students, medical and paramedical staff, nonmedical working professionals, and others. They were all further encouraged to send the form forward to their various known contacts. All the responses received within the time frame of 1 month were included in the study. The self-reported questionnaire consisted of following details- general introduction briefing the purpose of the survey, consent to participate, socio-demographic details, information relevant to reason for increased screen time, number of hours spent on digital screen, information relevant to common complaints faced, and measures taken to overcome strain. Only completed questionnaires were considered for the study. Data collected from the survey forms were analysed using SPSS software version 13. Pearson’s correlation was used to find the association between variables. Chi-square or Fisher’s exact test was used to investigate the associations between the qualitative variables. The associated risk factors of number and frequency of ocular health problems were analysed by univariate and multivariate logistic regression. A value of P ≤ 0.05 was considered significant.
Results
Demographic profile – A total of 550 responses were received from May to June 2021 out of which 435 responses were considered for analysis. Age of the participants who took the survey ranged from 18 to 79 years with a mean age of 35 years. There were 211 (48.5%) females and 224 (51.5%) males who participated in the survey. The demographic details of all the participants are given in Table 1.
Table 1.
Demographic details
| Demographic details | Number of participants |
|---|---|
| Gender | |
| Male | 224 |
| Female | 211 |
| Age | |
| 18-25 yrs | 82 |
| 25-45 yrs | 305 |
| >45 yrs | 48 |
| Marital status | |
| Married | 309 |
| Single/separated/widowed | 126 |
| Living with family | |
| Yes | 376 |
| No | 89 |
| Occupation | |
| Students | 43 |
| Medical profession | 8 |
| Non-medical | 355 |
| Unemployed | 29 |
Clinical profile – The participants were asked about their pre-existing ocular conditions. 412 (94.7%) participants had no history of medications/surgery for any eye problem and out of the remaining 23 respondents, 8 had undergone LASIK and 4 had cataract surgery. 61 participants had history of ocular allergy. Out of 435 participants, 243 wear glasses and 45 use contact lenses.
Digital screen Usage – Screen time had increased during the lockdown period for 387 (89%) participants. Majority (275/435) of the participants spent 2–6 hours on screen per day. For 117 (26.9%) participants screen time had increased for more than 6 hours and only 43 (9.9%) participants were using the digital screen for less than 2 hours and around 79 (18.2%) were spending time continuously on screen. [Table 2] There was a tendency of younger age group to spend greater time with gadgets than the older participants (p = 0.001).
Table 2.
Digital screen usage
| Number of participants | |
|---|---|
| Hours spent on screen | |
| <2 h | 43 |
| 2-4 h | 155 |
| 4-6 h | 120 |
| >6 h | 117 |
| Screen usage | |
| Continuous | 79 |
| Interrupted | 356 |
Viewing distance for digital screen was 25–40 cm for maximum participants (255/435), and only 70 (16.1%) used digital screen at a distance less than 25 cm. Smart phone was the most frequently used digital screen among the participants. 394 (90%) participants used smart phone and 259 (59.5%) participants used more than one device. [Table 3].
Table 3.
Digital device used (Screen used)
| Number of participants | |
|---|---|
| Digital device | |
| Smart phone | 394 |
| Desktop | 73 |
| Laptop | 170 |
| Tablet/iPad | 68 |
| T.V. | 154 |
| Multiple screen | 259 |
The increased screen time was mainly because of increased work online 75.6% (329), social media (54.5%) (237), online classes or education related 44.1% (192) and for entertainment 35.4% (154). Other reason for increased screen time included using video calling and online shopping. [Table 4].
Table 4.
Reason for increased screen time
| Number of participants | |
|---|---|
| Reason for increased screen time | |
| Webinars | 185 |
| Online shopping | 97 |
| Online streaming platforms | 106 |
| Social media | 237 |
| Assisting kids in online classes | 95 |
| Work from home | 103 |
| Online meetings/video conferencing | 130/96 |
Ocular complaints: Common ocular complaints after screen use reported by the participants were eye pain/fatigue (52.8%), headache (31.3%) and dry eyes/frequent blinking (19.7%). Non-ocular complaints registered were backache/neck pain (26.7%), dizziness, and vertigo (3.4%). On an average 2.3+-1.5 symptoms were reported by the participants. In total, 81.37% (354/435) of participants have experienced at least one symptom related to digital screen usage. [Figure 1].
Figure 1.
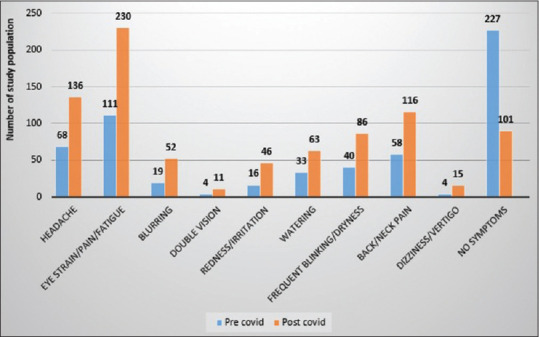
Symptoms of digital eye strain experienced by the study population in pre- and post-COVID-19 period
42.9% of the participants reported that the symptoms occurred often (either daily or 2–3 times a week), and 38.2% had symptoms occasionally (once in 1 or 2 weeks). [Figure 2] Majority (52.8%) of the participants did not have similar complaints in the past after using the digital screen. It is only after the increased screen time that occurred during the pandemic. The participants who had similar problem in the past reported a significant increase in number and frequency of symptoms during the pandemic (p = 0.00). Aggravated problems during pandemic were due to increased screen time according to 93.4% and were due to non-availability of medical care for 6.6% of the participants.
Figure 2.
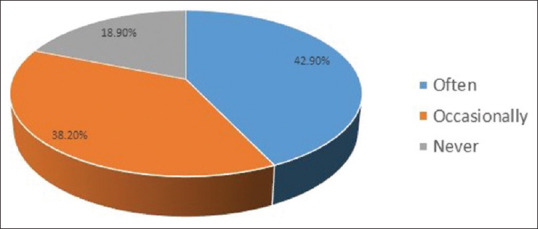
Frequency of symptoms of digital eye strain experienced by the study population
The correlation of increased screen time and number of symptoms were statistically significant (p = 0.00). There was positive correlation of number and frequency of symptoms with usage of multiple screens (p = 0.002), the time spent on digital screen (p = 0.00), and continuous screen time (p = 0.00). Increasing age had a negative correlation to number and frequency of symptoms. (p = 0.003).
Awareness: 354 (81.4%) of the participants were aware that increased screen time can cause harm to the eyes. Participants were also asked about if and what are the precautions/measures taken while using digital screen. 199 (45.7%) of the participants took some or the other precautions/measures while using screen in the form of antiglare glasses, screen filters, increasing the room illumination, and decreasing the screen brightness. The survey also asked about the remedial measures taken for the problems. 38.6% of the participants took break in between the screen time, 32.9% closed their eyes for a few seconds in between the screen time, 22.3% increased the blinking frequency, and 22.3% change focus from near to distance. 66 (15.2%) participants also used medications in the form of lubricating eye drops for their symptoms.
Discussion
COVID-19 pandemic has had an impact on physical as well as mental health of worldwide population. With a very high infectivity and mortality rate, it has hampered the normal functioning of the world, almost bringing a halt in everybody’s life. Home confinement during the pandemic has had a negative impact on the lifestyle in terms of psychosocial stress, decreased quantity as well as quality of sleep, weight issues, and many more.[9,10] According to this survey, around 89% of the participants had an increase in the screen time during the pandemic which is higher than found in study by Colley et al.[11] where over 50% of adults had increased their screen time on at least two different devices during the pandemic. However, a study conducted in China by Hu Z et al.[12] found that about 70% of 1033 participants spent more time looking at screens after the pandemic.
Digital eye strain as seen in this survey is directly related to the time spent on digital screen. 26.9% of the participants spent greater than 6 hours while 63% spent 2–6 hours on screen. The correlation of increased screen time and number of symptoms was found to be statistically significant (p = 0.00) as also found in the study by Gammoh Y et al.[13] DES was also more in those who have continuous screen time than those who take break in between (p = 0.00). This association could be due to accommodation lag on prolonged digital usage as reported by various researchers.[14,15] Use of multiple devices (dual or triple screening) is related to increase in DES symptoms as found in our study (P = 0.002). This is similar to 2016 Digital Eye Strain report where individuals using two or more devices simultaneously as compared to those using just one device at a time had prevalence of DES 75% and 53%, respectively.[16] Indian Academy of Paediatrics as well as WHO recommends no screen exposure for children less than 2 years of age and in 2 to 5 years’ age group screen time should not exceed 1 hour. For older children and adolescents no cut off limit is given but one has to balance screen time with other physical activities.[17,18]
In total, 81.37% (354/435) of participants have experienced at least one symptom related to digital screen usage. This is similar to the prevalence reported by previous studies.[19,20] On an average, 2.3+-1.5 symptoms were reported by the participants.
The most common symptom reported in our study was eye pain/strain affecting 52.8% of the participants. This is at par with prevalence of eye pain reported in various other studies, rather one of the most common computer-associated ocular complaints is asthenopia, experienced by an estimated 55% to 81% of digital device users.[21,22] Eye pain occurs due to increased accommodative effort putting undue strain on intraocular muscles without adequate relaxation at the viewing distance of digital devices.[23] Headache was second common symptom reported in our survey with a prevalence of 31.3%. Headache could also be a part of eye strain or uncorrected refractive error. Prevalence of headache was similar to as reported by R. Talwar et al.[20] In this survey, younger age group, unemployed and those not married or not living with family tend to spend more time on screen and hence suffer more from DES. The student population is considerably more symptomatic, and this can be attributed to the abrupt increase in screen time of students due to online classes and e-learning modules during the pandemic. The findings are similar to study by Badri et al.[24] where average time spent on social media by students was 5.2 h per day. M. Dubey et al.[25] concluded that 68% of adolescents have screen time for more than 2 hours. DES was also seen more commonly in participants who had similar complaints in the past and those with allergic eye disease (p = 0.00). Surprisingly, contact lens use was not associated with DES and hence not the risk factor which is similar to the results of a recently published survey.[26]
81.4% of the participants were aware that increased screen time can cause harm to the eyes however only 45.7% of the participants took some or the other precautions/measures while using screen. The association between DES and use of precautions/measures was not found to be statistically significant (p = 0.08). M Rosenfield et al.[27] found limited evidence to support use of blue-blocking filters as a clinical treatment for DES. Similar findings by B. Redondo et al.[28] found no effect of blue-blocking filters on accommodative dynamics or visual symptomatology. The AAO.[29] does not recommend any special eyewear for digital eye strain till date. Ergonomic tips such as keeping screen at an arm’s length distance, taking care of glare, defying dry eyes, taking frequent breaks from screen, adjusting environmental illumination, and increasing contrast of digital device has been emphasized.[30,31] The primary care physicians can play a pivotal role in creating awareness regarding ergonomic practices among the community. They can counsel the parents in developing digital etiquettes and also playing a role model for their kids. G Cardona et al.[32] suggested frequent breaks and blinking awareness training for visual display terminal users requiring prolonged periods of visually demanding dynamic computer play or work. M Hirayama et al.[33] recommended use of desktop humidifier for relief of ocular dryness and improvement of tear stability. Artificial tear drops can be used to combat DES in severe cases as also found in our study (p = 0.00).[34] The use of lubricants might be more essential in challenging environments with extremely high temperatures and low relative humidity levels as in India and this aspect needs more research.
The results of this study can be generalized to the Indian population during this COVID-19 lockdown period as the participants were from all over India and also gender distribution in our study was almost equal which makes it unique. Our study caters >18 years’ age group which is backbone of our employment, education, and social infrastructure. This study provides data on prevalence of eyestrain in this vulnerable age group which has tremendously increased during the pandemic, and will therefore help clinicians to understand the gravity of this emerging health threat.[35] However, the limitations of this study include those related to questionnaire studies: (i) recall bias, (ii) dishonest answers and interpretation issues, (iii) Online platform could confine the survey to educated people, (iv) Refractory error and other ocular surface disorders could not be objectively assessed.
Take home message – The recommendations from this study include: (i) screen time should be reduced to less than 4 hours per day with adequate breaks in between (20–20-20 rule). Adequate breaks during screen time can be ensured by putting an alarm for every 20 min, also there are certain apps which remind you of the same at fixed intervals.[36] Voluntary forceful blinking during screen time should be encouraged, which squeezes the Meibomian glands to secrete the lipid layer of the tear film. (ii) People should cut their other screen-related activities like social media, internet, video games and television to compensate for the screen time spent on work or studies. (iii) All teaching institutions should strictly comply with the ‘Pragyata’ guidelines chalked out for digital education by HRD Minister of India.[37,38] It is useful for a diverse set of stakeholders including school heads, teachers, parents, teacher educators, and students. Podcasts and audiobooks are an alternative option for online education and whenever possible, these can be used to reduce digital eye strain. (iv) Use of ergonomic practices should be encouraged. A preservative-free artificial tear preparation can also be recommended. The primary care physicians commonly encounter patients presenting with symptoms of asthenopia and headache in routine clinic. Before opting for an ophthalmology opinion they can inquire about screen habits and counsel for ergonomic practices. This approach can be saviour in terms of both time and money for the patient. Those not getting relief could be send for ophthalmological assessment in subsequent visits. Younger age group, unemployed and those not married or living alone must look out for other productive activities to avoid excessive screen time. Indoor games, reading books, physical exercises including yoga and meditation should be practised for overall betterment of an individual.
Conclusion
This study highlights the increase in digital screen time during the pandemic and the resultant eye strain. The study includes all age group with almost equal gender distribution thus the results can be generalised to the Indian population. It is understandable that for many people it is difficult to reduce the overall screen time during this pandemic. Gradual increase in screen time can be a suitable option than abrupt changes. This will give the eyes an adaption time and might suffer less harm. There is need of spreading awareness regarding the adverse effects of digital device use and the preventive measures to safeguard our ocular health. No screen usage guidelines are there for adults till date thus our study strongly recommends that guidelines should be formulated and strictly imposed. It is also responsibility of parents to guide their children by becoming role model as well as emphasize digital etiquette. DES is non vision-threatening but discomfort caused due to it is gruesome in majority of population. With joint efforts of parents, policymakers, teachers, and health workers this DES pandemic could be superseded.
Key points
Almost 89% of the participants had an increase in the screen time during the pandemic
Use of multiple devices (dual or triple screening) increases DES symptoms as found in our study (P = 0.002)
Younger age group, unemployed and those not married or living alone suffer more from DES
DES was a seen more commonly in participants who had similar complaints in the past and those with allergic eye disease (p = 0.00).
Contact lens use was not associated with DES.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Coles-Brennan C, Sulley A, Young G. Management of digital eye strain. Clin Exp Optom. 2019;102:18–29. doi: 10.1111/cxo.12798. [DOI] [PubMed] [Google Scholar]
- 2.Sheppard AL, Wolffsohn JS. Digital eye strain:Prevalence, measurement and amelioration. BMJ Open Ophthalmol. 2018;3:e000146. doi: 10.1136/bmjophth-2018-000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cole BL, Maddocks JD, Sharpe K. Effect of VDUs on the eyes:Report of a 6-year epidemiological study. Optom Vis Sci. 1996;73:512–28. doi: 10.1097/00006324-199608000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Usgaonkar U, Shet Parkar SR, Shetty A. Impact of the use of digital devices on eyes during the lockdown period of COVID-19 pandemic. Indian J Ophthalmol. 2021;69:1901–6. doi: 10.4103/ijo.IJO_3500_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohan A, Sen P, Shah C, Jain E, Jain S. Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic. Indian J Ophthalmol. 2021;69:140–4. doi: 10.4103/ijo.IJO_2535_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akkara JD, Kuriakose A. Commentary:Digital toxicity:Another side effect of COVID-19 pandemic. Indian J Ophthalmol. 2021;69:1907–8. doi: 10.4103/ijo.IJO_1362_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Twenge JM, Campbell WK. Associations between screen time and lower psychological well-being among children and adolescents:Evidence from a population-based study. Prev Med Rep. 2018;12:271–83. doi: 10.1016/j.pmedr.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.India hits 100-crore Covid vaccine milestone: Who said what-India News. [Last accessed on 2021 Nov 05]. Available from: https://www.indiatoday.in/india/story/india-100-crore-covid-vaccine-milestonewho-said-what-1867699-2021-10-21 .
- 9.Morin CM, Carrier J. The acute effects of the COVID-19 pandemic on insomnia and psychological symptoms. Sleep Med. 2021;77:346–7. doi: 10.1016/j.sleep.2020.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun QM, Qin QS, Chen BX, Shao RF, Zhang JS, Li Y. [Stress, anxiety, depression and insomnia in adults outside Hubei province during the COVID-19 pandemic. Zhonghua Yi Xue Za Zhi. 2020;100:3419–24. doi: 10.3760/cma.j.cn112137-20200302-00557. [DOI] [PubMed] [Google Scholar]
- 11.Colley RC, Bushnik T, Langlois K. Exercise and screen time during the COVID-19 pandemic. Health Rep. 2020;31:3–11. doi: 10.25318/82-003-x202000600001-eng. [DOI] [PubMed] [Google Scholar]
- 12.Hu Z, Lin X, Chiwanda Kaminga A, Xu H. Impact of the COVID-19 epidemic on lifestyle behaviors and their association with subjective well-being among the general population in Mainland China:Cross-sectional study. J Med Internet Res. 2020;22:e21176. doi: 10.2196/21176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gammoh Y. Digital eye strain and its risk factors among a university student population in Jordan:A cross-sectional study. Cureus. 2021;13:e13575. doi: 10.7759/cureus.13575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Collier JD, Rosenfield M. Accommodation and convergence during sustained computer work. Optometry. 2011;82:434–40. doi: 10.1016/j.optm.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 15.Wick B, Morse S. Accommodative accuracy of visual display monitors. Optom Vis Sci. 2002;79:218. [Google Scholar]
- 16.The Vision Council Shines Light on Protecting Sight –and Health –in a Multi-screen Era |The Vision Council. [Last accessed on 2021 Nov 05]. Available from: https://www.thevisioncouncil.org/blog/vision-council-shines-light-protecting-sight-and-health-multi-screen-era .
- 17. [Last accessed on 2021 Oct 28]. Available from: https://iapindia.org/pdf/Screentime-Guidelines-for-Parents-Ch-005.pdf .
- 18.To grow up healthy children need to sit less and play more. [Last accessed on 2021 Nov 05]. Available from: https://www.who.int/news/item/24-04-2019-to-grow-up-healthy-children-need-to-sit-less-and-play-more .
- 19.Logaraj M, Madhupriya V, Hegde S. Computer vision syndrome and associated factors among medical and engineering students in Chennai. Ann Med Health Sci Res. 2014;4:179–85. doi: 10.4103/2141-9248.129028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Talwar R, Kapoor R, Puri K, Bansal K, Singh S. A study of visual and musculoskeletal health disorders among computer professionals in NCR Delhi. Indian J Community Med. 2009;34:326–8. doi: 10.4103/0970-0218.58392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liat Gantz Mark Rosenfield;Digital eye strain symptoms during online university learning in Israel and the USA during the COVID-19 pandemic. Invest Ophthalmol Vis Sci. 2021;62:1975. [Google Scholar]
- 22.Fenga C, Di Pietro R, Di Nola C, Spinella R, Cacciola A, Germano D, et al. Asthenopia in VDT users:Our experience. G Ital Med Lav Ergon. 2007;29((Suppl 3)):500–1. [PubMed] [Google Scholar]
- 23.Parihar JK, Jain VK, Chaturvedi P, Kaushik J, Jain G, Parihar AK. Computer and visual display terminals (VDT) vision syndrome (CVDTS) Med J Armed Forces India. 2016;72:270–6. doi: 10.1016/j.mjafi.2016.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Badri M, Alnuaimi A, Al Rashedi A, Yang G, Temsah K. School children's use of digital devices, social media and parental knowledge and involvement –The case of Abu Dhabi Educ Inf Technol. 2017;22:2645–64. [Google Scholar]
- 25.Dubey M, Nongkynrih B, Gupta SK, Kalaivani M, Goswami AK, Salve HR. Screen-based media use and screen time assessment among adolescents residing in an Urban Resettlement Colony in New Delhi, India. J Family Med Prim Care. 2018;7:1236–42. doi: 10.4103/jfmpc.jfmpc_190_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mehra D, Galor A. Digital screen use and dry eye:A review. Asia Pac J Ophthalmol. 2020;9:491–7. doi: 10.1097/APO.0000000000000328. [DOI] [PubMed] [Google Scholar]
- 27.Rosenfield M, Li RT, Kirsch NT. A double-blind test of blue-blocking filters on symptoms of digital eye strain. Work. 2020;65:343–8. doi: 10.3233/WOR-203086. [DOI] [PubMed] [Google Scholar]
- 28.Redondo B, Vera J, Ortega-Sánchez A, Molina R, Jiménez R. Effects of a blue-blocking screen filter on accommodative accuracy and visual discomfort. Ophthalmic Physiol Opt. 2020;40:790–800. doi: 10.1111/opo.12738. [DOI] [PubMed] [Google Scholar]
- 29.Computer vision syndrome |AOA. [Last accessed on 2021 Nov 05]. Available from: https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/computer-vision-syndrome?sso=y .
- 30.Karoney MJ, Mburu SK, Ndegwa DW, Nyaichowa AG, Odera EB. Ergonomics in the computer workstation. East Afr Med J. 2010;87:382–4. [PubMed] [Google Scholar]
- 31.Ganne P, Najeeb S, Chaitanya G, Sharma A, Krishnappa NC. Digital eye strain epidemic amid COVID-19 Pandemic-A cross-sectional survey. Ophthalmic Epidemiol. 2021;28:285–92. doi: 10.1080/09286586.2020.1862243. [DOI] [PubMed] [Google Scholar]
- 32.Cardona G, García C, Serés C, Vilaseca M, Gispets J. Blink rate, blink amplitude, and tear film integrity during dynamic visual display terminal tasks. Curr Eye Res. 2011;36:190–7. doi: 10.3109/02713683.2010.544442. [DOI] [PubMed] [Google Scholar]
- 33.Hirayama M, Murat D, Liu Y, Kojima T, Kawakita T, Tsubota K. Efficacy of a novel moist cool air device in office workers with dry eye disease. Acta Ophthalmol. 2013;91:756–62. doi: 10.1111/j.1755-3768.2012.02485.x. [DOI] [PubMed] [Google Scholar]
- 34.Alabdulkader B. Effect of digital device use during COVID-19 on digital eye strain. Clin Exp Optom. 2021;104:698–704. doi: 10.1080/08164622.2021.1878843. [DOI] [PubMed] [Google Scholar]
- 35.Tawonkasiwattanakun P, Tonkerdmongkol D, Poyomtip T. To save our eyes, urgent public health policies are required after the COVID-19 pandemic. Public Health. 2021;197:e26. doi: 10.1016/j.puhe.2021.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Break Reminder –Apps on Google Play. [Last accessed 2021 Nov 05]. Available from: https://play.google.com/store/apps/details?id=bigfoot.dev.worksmart&hl=en_IN&gl=US .
- 37. [Last accessed on 2021 Nov 05]. Available from: https://www.education.gov.in/sites/upload_files/mhrd/files/pragyata-guidelines_0.pdf .
- 38.Mohan A, Sen P, Shah C, Datt K, Jain E. Binocular accommodation and vergence dysfunction in children attending online classes during the COVID-19 pandemic:Digital Eye Strain in Kids (DESK) study-2. J Pediatr Ophthalmol Strabismus. 2021;58:224–31. doi: 10.3928/01913913-20210217-02. [DOI] [PubMed] [Google Scholar]


