Abstract
We explored the association between cholesterol levels and dementia risk according to the presence of diabetes and statin use. In this population-based longitudinal cohort study, the Korean National Health Insurance Service datasets (2002–2017) were used. Among individuals aged ≥ 40 years who underwent health examinations in 2009 (N = 6,883,494), the hazard of dementia was evaluated according to cholesterol levels. During a median 8.33 years, 263,185 dementia cases were detected. In statin non-users with or without diabetes, the hazards of all-cause dementia were highest for those in the lowest quartile or quintile of low-density lipoprotein-cholesterol (LDL-C) level, showing an inverted J-shaped relationship. Among statin users with or without diabetes, an advance in LDL-C group was associated with an increase in hazards of all-cause dementia. In statin users with diabetes, even very low LDL-C level was not associated with an increased risk of all-cause dementia. Although there was a seemingly paradoxical association between low LDL-C level and dementia risk in statin non-users, the trend was not observed in statin users and is not likely to be clinically relevant. Rather, an advance in LDL-C levels was associated with an increase in the hazard of all-cause dementia in statin users, regardless of the presence of diabetes.
Subject terms: Dementia, Dyslipidaemias
Introduction
Based on overwhelming evidence that statins reduce the risk of atherosclerotic cardiovascular disease (ASCVD), guidelines on ASCVD risk management have endorsed the intensification of statin therapy based on the ASCVD risk1. Emerging evidence indicates that a more aggressive lowering of low-density lipoprotein-cholesterol (LDL-C) and apolipoprotein B-containing lipoprotein particles further reduce ASCVD risk, with a benefit proportional to the absolute achieved reduction in LDL-C without a lower limit2–4.
However, concerns regarding adverse effects, not limited to proven ones but also controversial ones5, are frequent causes of non-compliance to statin therapy. Among the controversial ones, concerns have been raised on cognitive function because the brain is a cholesterol-rich organ, and cholesterol is a major constituent of the myelin sheath6. To our knowledge, few studies have specifically explored the association between absolute LDL-C level achieved by statin use and the risk of cognitive dysfunction.
The results of epidemiological studies on the association between cholesterol levels and the risk of dementia, including Alzheimer’s disease (AD) and vascular dementia (VD), have been conflicting7–12, failing to address the interaction between such an association and the presence of diabetes or the use of statins. Although high total cholesterol (TC) in late life has been suggested as protective against dementia10, and a weaker association between LDL-C level and dementia risk has been reported in older people (aged 65 years or above) compared with those aged less than 65 years12, the previous studies did not specifically examine whether such trends are valid in the association between absolute cholesterol levels achieved by statin therapy and the risk of dementia7–12. Since statin affects cholesterol levels potently, lipid levels in statin users and non-users would be markedly varied. Also, vascular risk profiles, closely related to the risk of dementia13,14, would be highly variable between statin users and non-users in the real-world since statins are more widely and actively prescribed to individuals at higher vascular risk. In addition, most previous studies did not explore whether the presence of diabetes could modify the association between LDL-C level and dementia risk. Given that diabetes is a profound modifier of lipid profiles15,16, a major risk factor for dementia13,14,17,18, and one of the most important indications for intensive statin therapy1, the discrepancy among previous epidemiological studies needs to be resolved by large-scale population-based research offering a stratified analysis according to the presence of diabetes and the use of statin.
Therefore, we explored trends in the association between baseline cholesterol levels and the risk of dementia according to the presence of diabetes and the use of statin.
Results
Baseline characteristics
A total of 6,883,494 individuals was included (Fig. 1). Individuals with LDL-C in the lower quartiles were more likely to be male, current smokers, and heavy drinkers, and to have higher baseline estimated glomerular filtration rate (eGFR), MI, and stroke prevalence (Table 1). With increasing quartiles of LDL-C, an increasing trend was observed in body mass index (BMI) and proportion of nondrinkers.
Figure 1.
Flowchart outlining selection of the study population.
Table 1.
Baseline characteristics according to quartile of low-density lipoprotein cholesterol level.
| LDL-C quartilea | Q1 | Q2 | Q3 | Q4 | p-value |
|---|---|---|---|---|---|
| N | 1,716,390 | 1,754,964 | 1,705,307 | 1,706,833 | |
| Age (years) | 54.18 ± 10.85 | 53.77 ± 10.54 | 54.21 ± 10.30 | 55.25 ± 10.08 | < 0.0001 |
| Age group [n (%)] | < 0.0001 | ||||
| 40–49 years | 705,863 (41.12) | 732,753 (41.75) | 654,268 (38.37) | 547,391 (32.07) | |
| 50–59 years | 474,681(27.66) | 515,717 (29.39) | 515,717 (29.39) | 604,004 (35.39) | |
| 60–69 years | 337,639 (19.67) | 324,201 (18.47) | 330,805 (19.4) | 369,539 (21.65) | |
| ≥ 70 years | 198,207 (11.55) | 182,293 (10.39) | 174,752 (10.25) | 185,899 (10.89) | |
| Male sex [n (%)] | 968,204 (56.41) | 898,167 (51.18) | 848,279 (49.74) | 765,580 (44.85) | < 0.0001 |
| BMI (kg/m2) | 23.71 ± 3.12 | 23.77 ± 3.01 | 24.04 ± 2.97 | 24.39 ± 2.94 | < 0.0001 |
| SBP (mmHg) | 124.27 ± 15.64 | 123.44 ± 15.32 | 124.05 ± 15.24 | 125.19 ± 15.41 | < 0.0001 |
| DBP (mmHg) | 77.10 ± 10.30 | 76.75 ± 10.11 | 77.15 ± 10.07 | 77.80 ± 10.08 | < 0.0001 |
| Current smoker [n (%)] | 419,102 (24.42) | 364,174 (20.75) | 341,647 (20.03) | 323,736 (18.97) | < 0.0001 |
| Alcohol consumption [n (%)] | < 0.0001 | ||||
| Nondrinkers (< 1 g/day) | 907,188 (52.85) | 1,007,182 (57.39) | 1,013,450 (59.43) | 1,090,459 (63.89) | |
| Moderate drinkers | 653,500 (38.07) | 639,773 (36.46) | 600,173 (35.19) | 540,400 (31.66) | |
| Heavy drinkers (≥ 30 g/day) | 155,702 (9.07) | 108,009 (6.15) | 91,684 (5.38) | 75,974 (4.45) | |
| Regular exercise [n (%)] | 854,519 (49.79) | 885,526 (50.46) | 859,533 (50.40) | 835,759 (48.97) | < 0.0001 |
| Low household income (lowest 25%) [n (%)] | 470,425 (27.41) | 470,309 (26.80) | 450,701 (26.43) | 455,916 (26.71) | < 0.0001 |
| Fasting glucose (mg/dl) | 101.23 ± 27.62 | 98.75 ± 23.6 | 99.11 ± 23.23 | 100.72 ± 24.85 | < 0.0001 |
| Triglycerides (mg/dl) | 127.84 (127.71–127.97) | 112.66 (112.57–112.75) | 115.04 (114.95–115.12) | 121.81 (121.72–121.89) | < 0.0001 |
| HDL-C (mg/dl) | 55.73 ± 22.70 | 55.16 ± 20.71 | 54.75 ± 21.42 | 54.91 ± 24.02 | < 0.0001 |
| LDL-C (mg/dl) | 74.28 ± 16.77 | 104.78 ± 6.30 | 126.4 ± 6.57 | 164.38 ± 51.24 | < 0.0001 |
| eGFR (ml/min/1.73 m2) | 86.27 ± 35.59 | 85.40 ± 36.65 | 84.44 ± 37.38 | 83.25 ± 37.89 | < 0.0001 |
| Diabetes [n (%)] | 275,743 (16.07) | 189,498 (10.80) | 169,484 (9.94) | 177,146 (10.38) | < 0.0001 |
| Hypertension [n (%)] | 681,650 (39.71) | 589,767 (33.61) | 574,166 (33.67) | 607,535 (35.59) | < 0.0001 |
| Statin use [n (%)] | 300,465 (17.51) | 147,115 (8.38) | 106,860 (6.27) | 152,125 (8.91) | < 0.0001 |
| Myocardial infarction [n (%)] | 16,497 (0.96) | 8,059 (0.46) | 5,903 (0.35) | 5,549 (0.33) | < 0.0001 |
| Stroke [n (%)] | 49,087 (2.86) | 35,494 (2.02) | 31,594 (1.85) | 31,426 (1.84) | < 0.0001 |
| Charlson Comorbidity Index | 1.93 ± 1.50 | 1.93 ± 1.50 | 1.93 ± 1.50 | 1.93 ± 1.50 | 0.1180 |
Values are presented as number (%), mean ± standard deviation, or geometric mean (95% confidence interval).
LDL-C low-density lipoprotein cholesterol, BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, HDL-C high-density lipoprotein cholesterol, eGFR estimated glomerular filtration rate.
aLDL-C quartile ranges: Q1 (LDL-C < 94 mg/dl), Q2 (94 mg/dl ≤ LDL-C < 116 mg/dl), Q3 (116 mg/dl ≤ LDL-C < 139 mg/dl), Q4 (LDL-C ≥ 139 mg/dl).
Incidence of dementia in the general population according to lipid parameters
During 55,849,826.75 person-years (median 8.33 years), 263,185 dementia cases were detected. In the general population, the hazards for all-cause dementia and AD were highest in the lowest quartiles (Q1) of LDL-C and high-density lipoprotein-cholesterol (HDL-C) (Table 2, Supplementary Table S1). When we used quintiles instead of quartiles for lipid stratifications and set the third quintile as the reference, the highest hazard of all-cause dementia was noted also in the lowest quintiles of LDL-C and HDL-C levels, demonstrating an inverted J-shaped relationship between quintiles of LDL-C or HDL-C and the hazard of all-cause dementia (Supplementary Table S2). With respect to VD, although a similar trend was observed in models 1 and 2, the Q2 and Q4 of LDL-C levels did not show a significantly lower hazard of VD compared to the Q1 of LDL-C level in model 4. Conversely, significantly higher hazards of all-cause dementia, AD, and VD were seen in higher triglycerides (TG) quartiles compared to the Q1 of TG. When the association between TC quartile and outcome incidence was assessed using Q1 as a reference, Q2 showed lower hazards of all-cause dementia, AD, and VD; and Q3 demonstrated lower hazards of all-cause dementia and AD. Compared to the Q1 of TC, Q4 did not exhibit significantly different hazards of all-cause dementia, AD, or VD, and Q3 did not differ in terms of the hazard of VD.
Table 2.
Hazard ratios for the incidence of all-cause dementia according to quartile of lipid parameters.
| Quartile of lipid parametersa | n | Events (n) | Follow-up duration (person-years) | Incidence rate (per 1000 person-years) | Hazard ratio (95% confidence interval) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 3–1 | Model 4 | |||||
| LDL-C | |||||||||
| Q1 | 1,716,390 | 70,173 | 13,812,376.82 | 5.08044 | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1(Ref.) | 1(Ref.) |
| Q2 | 1,754,964 | 62,949 | 14,259,651.33 | 4.41448 | 0.867 (0.858, 0.876) | 0.906 (0.897, 0.916) | 0.942 (0.932, 0.953) | 0.942 (0.932, 0.953) | 0.956 (0.945, 0.966) |
| Q3 | 1,705,307 | 60,825 | 13,890,566.36 | 4.37887 | 0.859 (0.850, 0.869) | 0.882 (0.872, 0.891) | 0.928 (0.918, 0.938) | 0.928 (0.917, 0.938) | 0.945 (0.935, 0.956) |
| Q4 | 1,706,833 | 69,238 | 13,887,232.24 | 4.98573 | 0.978 (0.968, 0.988) | 0.917 (0.907, 0.927) | 0.969 (0.959, 0.980) | 0.969 (0.959, 0.980) | 0.987 (0.976, 0.998) |
| HDL-C | |||||||||
| Q1 | 1,701,108 | 76,442 | 13,705,008.76 | 5.57767 | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1(Ref.) | 1(Ref.) |
| Q2 | 1,697,679 | 65,701 | 13,787,613.74 | 4.76522 | 0.853 (0.845, 0.862) | 0.939 (0.929, 0.949) | 0.960 (0.950, 0.970) | 0.960 (0.950, 0.970) | 0.958 (0.948, 0.968) |
| Q3 | 1,782,263 | 63,076 | 14,506,544.69 | 4.34811 | 0.779 (0.771, 0.787) | 0.921 (0.911, 0.931) | 0.949 (0.939, 0.959) | 0.949 (0.939, 0.959) | 0.946 (0.936, 0.956) |
| Q4 | 1,702,444 | 57,966 | 13,850,659.56 | 4.18507 | 0.751 (0.743, 0.759) | 0.933 (0.923, 0.943) | 0.965 (0.954, 0.975) | 0.964 (0.954, 0.975) | 0.961 (0.950, 0.971) |
| Triglycerides | |||||||||
| Q1 | 1,698,765 | 48,512 | 13,855,868.15 | 3.50119 | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1(Ref.) | 1(Ref.) |
| Q2 | 1,732,804 | 68,053 | 14,045,373.48 | 4.84523 | 1.384 (1.368, 1.400) | 1.037 (1.025, 1.050) | 1.027 (1.015, 1.039) | 1.027 (1.015, 1.040) | 1.027 (1.015, 1.039) |
| Q3 | 1,727,849 | 76,121 | 13,977,984.87 | 5.44578 | 1.556 (1.538, 1.573) | 1.068 (1.056, 1.080) | 1.048 (1.036, 1.061) | 1.049 (1.036, 1.061) | 1.048 (1.036, 1.060) |
| Q4 | 1,724,076 | 70,499 | 13,970,600.24 | 5.04624 | 1.442 (1.425, 1.459) | 1.145 (1.132, 1.158) | 1.096 (1.083, 1.109) | 1.096 (1.083, 1.109) | 1.096 (1.083, 1.109) |
| Total cholesterol | |||||||||
| Q1 | 1,720,451 | 71,228 | 13,836,389.14 | 5.14787 | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1(Ref.) | 1(Ref.) |
| Q2 | 1,713,211 | 61,467 | 13,928,119.96 | 4.41316 | 0.856 (0.846, 0.865) | 0.924 (0.914, 0.934) | 0.955 (0.944, 0.965) | 0.955 (0.944, 0.965) | 0.967 (0.957, 0.978) |
| Q3 | 1,710,041 | 60,823 | 13,933,296.61 | 4.36530 | 0.846 (0.837, 0.855) | 0.905 (0.895, 0.915) | 0.944 (0.934, 0.955) | 0.944 (0.934, 0.955) | 0.961 (0.950, 0.971) |
| Q4 | 1,739,791 | 69,667 | 14,152,021.04 | 4.92276 | 0.954 (0.944, 0.964) | 0.952 (0.942, 0.962) | 0.994 (0.984, 1.005) | 0.994 (0.983, 1.005) | 1.010 (0.999, 1.021) |
Model 1: unadjusted.
Model 2: adjusted for age and sex.
Model 3: model 2 plus body mass index, diabetes, hypertension, current smoking status, alcohol consumption status, regular exercise, and estimated glomerular filtration rate.
Model 3–1: model 3 plus monthly household income, and Charlson Comorbidity Index.
Model 4: model 3 plus statin use.
LDL-C low-density lipoprotein cholesterol, HDL-C high-density lipoprotein cholesterol.
aLDL-C quartile ranges: Q1 (LDL-C < 94 mg/dl), Q2 (94 mg/dl ≤ LDL-C < 116 mg/dl), Q3 (116 mg/dl ≤ LDL-C < 139 mg/dl), Q4 (LDL-C ≥ 139 mg/dl); HDL-C quartiles: Q1 (HDL-C < 45 mg/dl), Q2 (45 mg/dl ≤ HDL-C < 53 mg/dl), Q3 (53 mg/dl ≤ HDL-C < 63 mg/dl), Q4 (HDL-C ≥ 63 mg/dl); triglyceride quartiles: Q1 (triglyceride < 80 mg/dl), Q2 (80 mg/dl ≤ triglyceride < 115 mg/dl), Q3 (115 mg/dl ≤ triglyceride < 169 mg/dl), Q4 ( triglyceride ≥ 169 mg/dl); and total cholesterol quartiles: Q1 (total cholesterol < 174 mg/dl), Q2 (174 mg/dl ≤ total cholesterol < 197 mg/dl), Q3 (197 mg/dl ≤ total cholesterol < 222 mg/dl), Q4 (total cholesterol ≥ 222 mg/dl).
Incidence of dementia according to LDL-C level in individuals categorized by the presence of diabetes and statin use
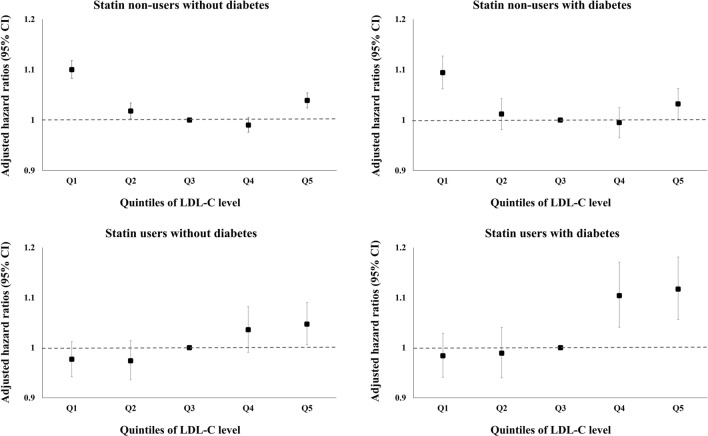
Consistent to previous reports that indicated diabetes as a major risk factor for dementia13,14,17,18, also in our dataset, individuals with diabetes exhibited a significantly higher hazard of all-cause dementia compared to those without (Supplementary Table S3), which provided one of the rationales for these stratified analyses. In statin non-users with or without diabetes, the hazards of all-cause dementia and AD were highest in the lowest quartile or quintile of LDL-C, exhibiting an inverted J-shaped relationship (Fig. 2, Supplementary Table S4). However, among statin users with or without diabetes, an advance in LDL-C quartile or quintile was associated with an increase in the hazard of all-cause dementia (hazard ratio, HR [95% confidence interval, CI] 1.010 [0.979–1.041] in Q2, 1.034 [1.000–1.070] in Q3, and 1.075 [1.042–1.108] in Q4 for those without diabetes; 1.015 [0.978–1.052] in Q2, 1.073 [1.028–1.121] in Q3, and 1.148 [1.103–1.196] in Q4 for those with diabetes) (Fig. 2, Supplementary Table S4). Additional adjustment for monthly household income and Charlson Comorbidity Index (CCI) demonstrated consistent findings with respect to the hazard of all-cause dementia. Regarding the hazard of AD, among statin users with or without diabetes, increasing trends of hazard according to the advance in LDL-C quartiles were shown after additional adjustment for these two factors.
Figure 2.
Hazard ratios for the incidence of all-cause dementia according to quintiles of low-density lipoprotein cholesterol levels in groups stratified according to the presence of diabetes and statin use. Adjusted for age, sex, body mass index, hypertension, current smoking status, alcohol consumption status, regular exercise, and estimated glomerular filtration rate. *LDL-C quintile ranges: Q1 (LDL-C < 89 mg/dl), Q2 (89 mg/dl ≤ LDL-C < 107 mg/dl), Q3 (reference, 107 mg/dl ≤ LDL-C < 124 mg/dl), Q4 (124 mg/dl ≤ LDL-C < 145 mg/dl), Q5 (LDL-C ≥ 145 mg/dl). LDL-C low-density lipoprotein cholesterol, CI confidence interval.
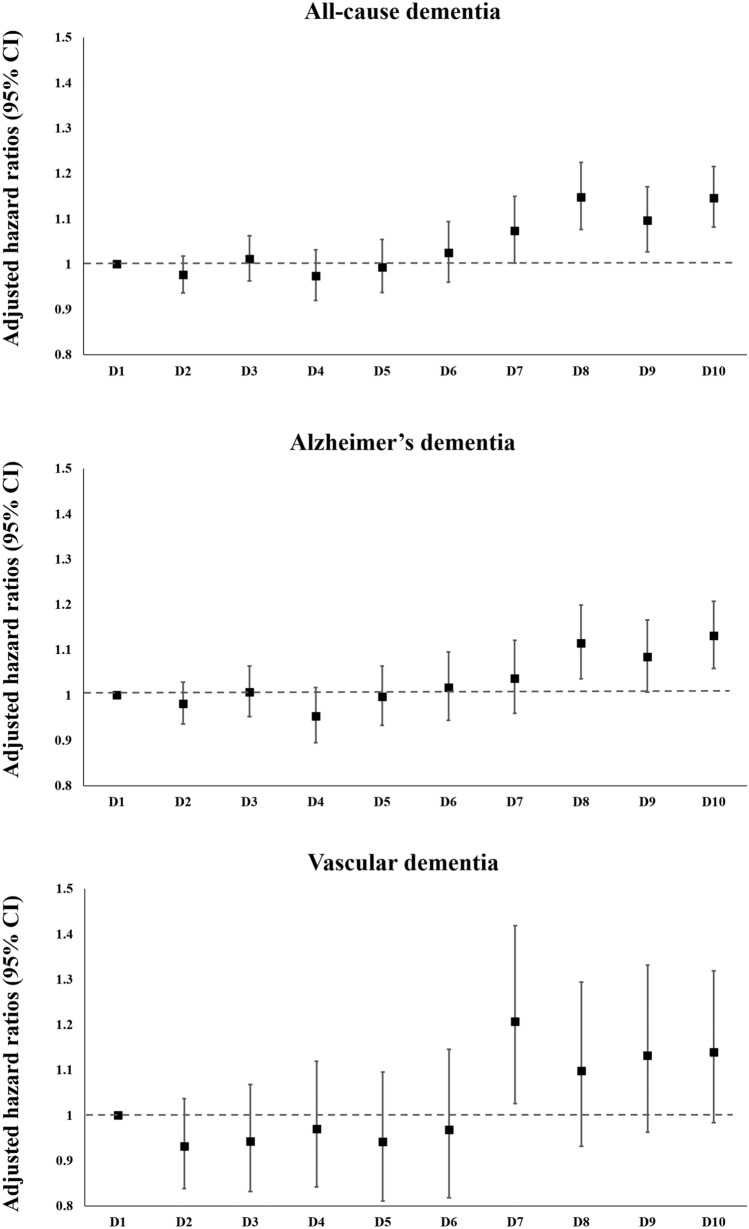
Incidence of dementia according to deciles of LDL-C level in statin users with diabetes
In subjects with diabetes using statins, the hazards of the outcomes were compared according to decile of LDL-C level to examine whether very low LDL-C level is associated with increased risk for dementia (Fig. 3). In statin users with diabetes, compared to the first decile group (D1, LDL-C < 75 mg/dl), the three highest decile groups (D8–D10, 133 mg/dl ≤ LDL-C) had a higher hazard of AD, and the highest four decile groups (D7–D10, 124 mg/dl ≤ LDL-C) presented a higher hazard of all-cause dementia.
Figure 3.
Hazard ratios for the incidence of all-cause dementia, Alzheimer’s disease, and vascular dementia among statin users with diabetes according to deciles of low-density lipoprotein cholesterol level. Adjusted for age, sex, body mass index, hypertension, current smoking status, alcohol consumption status, regular exercise, and estimated glomerular filtration rate. *LDL-C decile ranges: D1 (LDL-C < 75 mg/dl), D2 (75 mg/dl ≤ LDL-C < 89 mg/dl), D3 (89 mg/dl ≤ LDL-C < 99 mg/dl), D4 (99 mg/dl ≤ LDL-C < 107 mg/dl), D5 (107 mg/dl ≤ LDL-C < 116 mg/dl), D6 (116 mg/dl ≤ LDL-C < 124 mg/dl), D7 (124 mg/dl ≤ LDL-C < 133 mg/dl), D8 (133 mg/dl ≤ LDL-C < 145 mg/dl), D9 (145 mg/dl ≤ LDL-C < 162 mg/dl), D10 (LDL-C ≥ 162 mg/dl). LDL-C low-density lipoprotein cholesterol, CI confidence interval.
Similar trends were observed in statin users with ASCVD (Supplementary Fig. S1), which is another indication for intensive statin therapy, and in statin users aged ≥ 70 years, the age population in which the protective effect of high cholesterol levels was originally suggested10 (Supplementary Table S5).
Sensitivity analyses
Additional sensitivity analyses stratified by the statin use and restricting the subjects to individuals aged 40–60 years and to those aged ≥ 60 years demonstrated consistent results (Supplementary Tables S6 and S7). Sensitivity analyses in subpopulations categorized by the exposure duration to statins (never-users, irregular or short-term users, and continuous-users of statins) that accounted for the exposure duration to statins more in detail also yielded consistent findings, varied patterns of association according to statin exposure (Supplementary Table S8).
Discussion
In this study, the presence of diabetes did not affect trends in the association between LDL-C level and the risk of dementia. In statin non-users, an inverted J-shaped relation was noted between LDL-C level and dementia risk, showing a seemingly paradoxical increase in dementia risk in lower LDL-C levels, regardless of the presence of diabetes. However, this trend was not observed in statin users regardless of the presence of diabetes, with an increasing trend in the hazards of all-cause dementia according to increasing LDL-C quartile or quintile. Additional analyses conducted among never-users and continuous-users of statins also demonstrated consistent findings. In statin users with diabetes, the group with LDL-C level in the lowest decile (LDL-C < 75 mg/dl) did not present increased risk of all-cause dementia. Rather, those with LDL-C level ≥ 124 mg/dl showed increased risk of all-cause dementia compared to the lowest decile (LDL-C < 75 mg/dl).
In this study, the risk of all-cause dementia in the general population and in statin non-users was increased in those with LDL-C level in both the lowest and the highest quintiles, showing an inverted J-shaped relationship. However, the trend was not observed in the association between absolute cholesterol levels achieved by statins and the risk of dementia. As in other studies showing the ‘cholesterol paradox’ in various diseases19,20, an increase in the risk of dementia in statin non-users with LDL-C level in the lowest quintile does not indicate a causative role of low LDL-C level in dementia etiology but might represent secondary factors such as chronic inflammation, which results in decreased TC, LDL-C, and HDL-C levels and increased TG level19,21. Weight loss and an accompanying decrease in cholesterol levels are often observed alongside cognitive decline shortly before the diagnosis of dementia, which also could have affected the trends observed herein. Furthermore, considering that individuals in lower LDL-C quartiles were more likely to be current smokers and heavy drinkers and had a higher prevalence of ASCVD, the effects of these potential confounders might remain despite adjustment. On the other hand, the increased risk of all-cause dementia in those with LDL-C level in the highest quintile in the general population, which was consistent regardless of the statin use (Fig. 2), could be explained by an increasingly accepted notion that atherosclerosis is a key aspect in AD as well as VD13. A recent meta-analysis also suggested that high cholesterol values may play a role in the development of AD22.
It is reassuring that the lack of increase in the risk of dementia with LDL-C level in the lowest quartile or quintile was consistently observed in statin users, also in those with diabetes. In those with diabetes, moderate- or high-intensity statins would have been more frequently used than in the general population because recent guidelines have recommended statin therapy with adequate intensity regardless of baseline LDL-C level in people with diabetes1. In this study, statin users with diabetes and LDL-C level in the lowest decile (LDL-C < 75 mg/dl) did not present increased risks of all-cause dementia. A similar trend was observed in statin users with ASCVD, which is another indication for intensive statin therapy1; statin users in their midlife (40–60 years) or late-life (≥ 60 years); and especially in statin users aged ≥ 70 years, the age population in which the protective effect of high cholesterol levels was originally suggested10. The hypothesis that extremely low blood cholesterol levels can impair neuronal homeostasis has a caveat because cerebral cholesterol is primarily produced locally23, and cerebral cholesterol levels may be independent of plasma levels24. Indeed, a recent Mendelian randomization study in those with proprotein convertase subtilisin-kexin type 9 (PCSK9) and 3-hydroxy-3-methylglutaryl-CoA reductase genetic variations25 and recent randomized controlled trials of ezetimibe and anti-PCSK9 monoclonal antibodies indicated that very low LDL-C level does not increase the incidence of neurocognitive adverse events2,26. Therefore, the paradoxically increased hazards observed with LDL-C level in the lowest quartile or quintile among statin non-users with diabetes are not likely to be clinically relevant and at least should not be extrapolated to statin users with diabetes who achieved low LDL-C level with statin therapy.
The strength of this study was the large number of subjects (N = 6,883,494), representing the entire Korean population. The Korean National Health Insurance System (KNHIS) not only covers the entire Korean population, but also has strict reimbursement criteria that mandate documentation of evidence for cognitive dysfunction (assessed by the Mini-Mental State Exam [MMSE] and either the Clinical Dementia Rating or Global Deterioration Scale [GDS]) to prescribe anti-dementia drugs, which is highly likely to prevent misclassification or over-diagnosis of dementia. Although diverse variables including lifestyle, anthropometric, and laboratory measures were collected in this large population, only 3.8% of the eligible subjects were excluded for having missing values on at least one variable. The sufficient power enabled stratified analyses according to the presence of diabetes and statin use and provided insights on the specific association between absolute LDL-C level achieved by statin use and the risk of dementia.
The limitations of this study should be addressed. First, the study population was comprised of a single ethnicity, and extrapolation of the results to other ethnicities should be cautious. Second, the definition of statin use versus non-use was based on prescription records, which might be different from actual drug use. However, there have been reports on the correlation between prescriptions and real exposure to medications27,28. In Korea, a prescription by physicians is necessary to obtain statins, and a simple refill at pharmacies is prohibited. Third, analyses were based on lipid measures at a single timepoint (baseline). Repeated measurements and varied levels during follow-up were not reflected due to the data unavailability in most of the individuals. However, previous studies on the association between lipid levels and adverse outcomes also used a single baseline lipid level to produce meaningful findings29–34. Fourth, the diagnosis of dementia was based on the records of diagnostic codes and prescriptions, and brain imaging or in-depth cognitive tests were not used directly. However, to minimize the misclassification or over-diagnosis, we used the information on the prescription of anti-dementia medications as well as diagnostic codes. Considering the strict reimbursement criteria in Korea that require the documentation of evidence for cognitive dysfunction (assessed by MMSE and either Clinical Dementia Rating or GDS) to prescribe anti-dementia drugs, it is less likely that other conditions may have been misclassified or over-diagnosed as dementia. Fifth, data on factors that may have significant impact on dementia risk, such as educational attainment and/or baseline cognitive functions were unavailable. However, although we could not directly adjust for the educational attainment because of the data unavailability, additional adjustment for income, which are closely related to educational level35, demonstrated consistent findings. Lastly, we could not fully reflect the exact dosage or intensity of statins due to data unavailability.
Although there was a seemingly paradoxical association between low LDL-C level and dementia risk in statin non-users, such a trend was not observed in statin users and is not likely to be clinically relevant. Rather, an increase in LDL-C level was associated with an increase in the risk of all-cause dementia in statin users. This trend was consistent regardless of the presence of diabetes, also in people with diabetes who achieved very low LDL-C level with statin therapy.
Methods
Data sources
For this nationwide, longitudinal, population-based cohort study, we used the KNHIS datasets from January 2002 to December 2017. The KNHIS is a compulsory health insurance system for all citizens operated by the Korean government and recommends standardized health examinations at least every two years through the national health screening program36. The KNHIS provides a public database containing the health information of > 50 million people, including a qualification database (containing information regarding sex, age, household income, residential area, and types of qualification), claims data (diagnoses defined by International Classification of Diseases [ICD] codes and prescriptions), and death information36. In addition, results of biennial standardized health examinations promoted by the KNHIS through national health screening program are also assembled into the database. The protocol for this study was approved by the Institutional Review Board (IRB) of Samsung Medical Center (no. 2020-09-088), and all methods were performed in accordance with the relevant guidelines and regulations. An informed consent exemption was granted by the IRB of Samsung Medical Center because the KNHIS provided the researchers with de-identified data.
Study population
We included individuals aged ≥ 40 years who underwent health examinations between January and December 2009. The time point of the examination in 2009 was considered the baseline. We selected the year 2009 since lipid profiles including LDL-C, HDL-C, and TG were first introduced as components of standardized health examinations in 2009. In a total of 7,183,255 subjects, those with dementia at or before baseline (n = 24,772) and those with missing data for one or more variables (n = 274,989) were excluded (Fig. 1). Finally, 6,883,494 subjects were selected and followed from baseline until death, dementia diagnosis, or December 31, 2017, whichever came first.
Measurements and definitions
Standardized health examinations are conducted only in hospitals certified by the KNHIS. All health examination institutions undergo regular quality assessments according to the Basic Act on National Health Examination in Korea. Blood tests, including plasma glucose, TG, HDL-C, and LDL-C, were performed after an overnight fast. The eGFR was calculated by the Modification of Diet in Renal Disease Study equation37. BMI (kg/m2) was calculated by dividing body weight (kg) by height squared (m2). Blood pressure was measured by qualified medical personnel using sphygmomanometers or oscillometric devices at brachial levels after the examinee rested in a sitting position for at least 5 min. Questionnaires were conducted regarding smoking status, alcohol consumption history, and physical activity. Participants were classified into nondrinkers, moderate drinkers, and heavy drinkers according to alcohol consumption status. Individuals with an average alcohol intake < 1 g/day were considered as nondrinkers, while average alcohol ingestion ≥ 30 g/day was defined as heavy consumption38. Regular exercise was classified as high-intensity physical activity causing extreme shortness of breath for > 20 min per session ≥ 3 days per week or moderate-intensity physical activity causing substantial shortness of breath for > 30 min per session ≥ 5 days per week39.
The presence of diabetes mellitus was defined as either (1) at least one claim per year under ICD-10 codes E10-14 and at least one claim per year for prescription of anti-diabetes medication or (2) fasting glucose level ≥ 126 mg/dl. The presence of hypertension was defined as one or more claims per year under ICD-10 codes I10 or I11 and at least one claim per year for the prescription of antihypertensive agents, or systolic/diastolic blood pressure ≥ 140/90 mmHg40. Myocardial infarction (MI) was defined as one or more claims under ICD-10 codes I21–I22 during hospitalization or at least two claims under these codes40; stroke was determined as recording of ICD-10 codes I63–I64 during hospitalization with claims for brain computed tomography or magnetic resonance imaging40. CCI was defined according to established methods41 using previously provided diagnostic codes42. The participants were classified as statin users when they had been prescribed statins during the year before baseline. Those who had never been prescribed statins during the year before baseline were classified as statin non-users.
Study outcomes
The endpoint was incident all-cause dementia, and additional analyses were conducted after restricting the endpoint to AD or VD. Dementia was defined as the prescription of one or more anti-dementia medications and the presence of a claim for AD (ICD-10 F00 or G30), VD (ICD-10 F01), or another form of dementia (ICD-10 F02, F03, G23.1, G31)43. Anti-dementia medications included rivastigmine, galantamine, memantine, and donepezil hydrochloride. In Korea, strict reimbursement criteria require documentation of a MMSE score ≤ 26 and a Clinical Dementia Rating ≥ 1 or GDS stage ≥ 3 to file expense claims for anti-dementia drug prescriptions44. Identification of dementia type was based on diagnostic codes. If the codes for both AD and VD were present, the main diagnosis was considered the final diagnosis. When both codes for AD and VD were recorded as an additional diagnosis, the main diagnosis at the following visit was used as the final diagnosis43.
Statistical analyses
Subjects were stratified into quartiles of baseline lipid parameters. The baseline characteristics of the study population are presented according to quartile of LDL-C. Continuous variables with normal distributions are described as mean ± standard deviation, and those with non-normal distributions are described as geometric mean and 95% CI. Categorical variables are presented as frequency and percentage. The incidence rates of outcome (per 1000 person-years) were calculated as the number of incident cases divided by the total follow-up duration. Cox proportional hazards regression analysis was performed to evaluate the HRs and 95% CIs for the outcome incidence according to quartiles of lipid parameters. Model 1 was unadjusted, and model 2 was adjusted for age and sex. Model 3 was adjusted for age, sex, BMI, diabetes status, hypertension, current smoking, alcohol consumption, regular exercise, and eGFR. Model 3–1 was additionally adjusted for monthly household income and CCI in addition to the variables included in model 3. Model 4 was further adjusted for statin use in addition to the confounders in model 3. The proportional hazard assumptions of the Cox models were ensured by Schoenfeld residuals. We classified the study population according to the presence of diabetes and statin use. Stratified analyses according to statin use were performed in individuals with or without diabetes. To evaluate the effect of highest or lowest values of lipid parameters on outcome hazards, the main analyses were repeated using quintiles instead of quartiles for lipid stratifications and setting the third quintile as the reference. Among statin users with diabetes, the hazard of the outcome was calculated according to deciles of LDL-C levels, to examine the association between very low LDL-C level and the hazard of the outcome in individuals under intensive statin therapy due to high risk for subsequent ASCVD. P-values were considered significant at < 0.05, and all analyses were performed using SAS Version 9.4 (SAS Institute, Cary, NC, USA).
Sensitivity analyses
We conducted sensitivity analyses stratified by the statin use and restricting the subjects to individuals aged 40–60 years and to those aged ≥ 60 years considering previous suggestion that midlife (40–60 years) and late‐life (≥ 60 years) exposure to high cholesterol levels may have varied relation to dementia risk22. To account for the exposure duration to statins more in detail, we investigated the association between LDL-C levels and the hazard of dementia according to the presence of diabetes in subpopulations categorized by the exposure duration to statins (never-users, irregular or short-term users, and continuous-users of statins). Never-users of statins were defined as individuals who had never been prescribed for statins from 2002 to baseline. Those who had been prescribed statins for < 180 days, and for ≥ 180 days during the year before baseline were defined as irregular or short-term users, and continuous-users, respectively.
Supplementary Information
Acknowledgements
This work was performed using the database from the Korean National Health Insurance Service (KNHIS). The National Health Information Database constructed by the KNHIS was used, and the results do not necessarily represent the opinion of the KNHIS.
Abbreviations
- AD
Alzheimer’s disease
- ASCVD
Atherosclerotic cardiovascular disease
- BMI
Body mass index
- CI
Confidence interval
- eGFR
Estimated glomerular filtration rate
- GDS
Global Deterioration Scale
- HDL-C
High-density lipoprotein cholesterol
- HR
Hazard ratio
- ICD
International Classification of Diseases
- IRB
Institutional Review Board
- KNHIS
Korean National Health Insurance System
- LDL-C
Low-density lipoprotein-cholesterol
- MI
Myocardial infarction
- MMSE
Mini-Mental State Exam
- PCSK9
Proprotein convertase subtilisin-kexin type 9
- TC
Total cholesterol
- TG
Triglycerides
- VD
Vascular dementia
Author contributions
Conceptualization: K.H., J.H.K., and S.M.J. Data curation: B.K. and K.H. Formal analysis: B.K. and K.H. Methodology: J.P., G.K., K.Y.H., and K.H. Resources: K.H. Supervision: J.H.K. Validation: all authors. Writing—original draft: Y.B.L., M.Y.K., and S.M.J. Writing—review and editing: Y.B.L., S.M.J., and J.H.K. All authors read and approved the final version of the manuscript.
Data availability
The data that support the findings of this study are available from the Korean National Health Insurance Service (KNHIS) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the corresponding authors upon reasonable request and with permission of the KNHIS.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: You-Bin Lee and Min Young Kim.
Contributor Information
Jae Hyeon Kim, Email: jaehyeon@skku.edu.
Sang-Man Jin, Email: sangman.jin@samsung.com.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-24153-1.
References
- 1.Authors/Task Force Members, ESC Committee for Practice Guidelines & ESC National Cardiac Societies 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis. 2019;290:140–205. doi: 10.1016/j.atherosclerosis.2019.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Giugliano RP, et al. Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: A prespecified secondary analysis of the FOURIER trial. Lancet. 2017;390:1962–1971. doi: 10.1016/S0140-6736(17)32290-0. [DOI] [PubMed] [Google Scholar]
- 3.Silverman MG, et al. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: A systematic review and meta-analysis. JAMA. 2016;316:1289–1297. doi: 10.1001/jama.2016.13985. [DOI] [PubMed] [Google Scholar]
- 4.Cannon CP, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N. Engl. J. Med. 2015;372:2387–2397. doi: 10.1056/NEJMoa1410489. [DOI] [PubMed] [Google Scholar]
- 5.Mach F, et al. Adverse effects of statin therapy: Perception vs. the evidence—focus on glucose homeostasis, cognitive, renal and hepatic function, haemorrhagic stroke and cataract. Eur. Heart J. 2018;39:2526–2539. doi: 10.1093/eurheartj/ehy182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang J, Liu Q. Cholesterol metabolism and homeostasis in the brain. Protein Cell. 2015;6:254–264. doi: 10.1007/s13238-014-0131-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kivipelto M, et al. Apolipoprotein E epsilon4 allele, elevated midlife total cholesterol level, and high midlife systolic blood pressure are independent risk factors for late-life Alzheimer disease. Ann. Intern. Med. 2002;137:149–155. doi: 10.7326/0003-4819-137-3-200208060-00006. [DOI] [PubMed] [Google Scholar]
- 8.Tan ZS, et al. Plasma total cholesterol level as a risk factor for Alzheimer disease: The Framingham Study. Arch. Intern. Med. 2003;163:1053–1057. doi: 10.1001/archinte.163.9.1053. [DOI] [PubMed] [Google Scholar]
- 9.Mielke MM, et al. The 32-year relationship between cholesterol and dementia from midlife to late life. Neurology. 2010;75:1888–1895. doi: 10.1212/WNL.0b013e3181feb2bf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mielke MM, et al. High total cholesterol levels in late life associated with a reduced risk of dementia. Neurology. 2005;64:1689–1695. doi: 10.1212/01.WNL.0000161870.78572.A5. [DOI] [PubMed] [Google Scholar]
- 11.Reitz C, Tang MX, Luchsinger J, Mayeux R. Relation of plasma lipids to Alzheimer disease and vascular dementia. Arch. Neurol. 2004;61:705–714. doi: 10.1001/archneur.61.5.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iwagami M, et al. Blood cholesterol and risk of dementia in more than 1·8 million people over two decades: A retrospective cohort study. Lancet Healthy Longev. 2021;2:e498–e506. doi: 10.1016/S2666-7568(21)00150-1. [DOI] [PubMed] [Google Scholar]
- 13.Luchsinger JA, et al. Aggregation of vascular risk factors and risk of incident Alzheimer disease. Neurology. 2005;65:545–551. doi: 10.1212/01.wnl.0000172914.08967.dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Norton S, Matthews FE, Barnes DE, Yaffe K, Brayne C. Potential for primary prevention of Alzheimer's disease: An analysis of population-based data. Lancet Neurol. 2014;13:788–794. doi: 10.1016/s1474-4422(14)70136-x. [DOI] [PubMed] [Google Scholar]
- 15.Wu L, Parhofer KG. Diabetic dyslipidemia. Metabolism. 2014;63:1469–1479. doi: 10.1016/j.metabol.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 16.Taskinen MR. Quantitative and qualitative lipoprotein abnormalities in diabetes mellitus. Diabetes. 1992;41(Suppl 2):12–17. doi: 10.2337/diab.41.2.s12. [DOI] [PubMed] [Google Scholar]
- 17.Biessels GJ, Despa F. Cognitive decline and dementia in diabetes mellitus: Mechanisms and clinical implications. Nat. Rev. Endocrinol. 2018;14:591–604. doi: 10.1038/s41574-018-0048-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu JH, et al. Incidence and risk factors for dementia in type 2 diabetes mellitus: A nationwide population-based study in Korea. Diabetes Metab. J. 2020;44:113–124. doi: 10.4093/dmj.2018.0216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Myasoedova E, et al. Lipid paradox in rheumatoid arthritis: The impact of serum lipid measures and systemic inflammation on the risk of cardiovascular disease. Ann. Rheum. Dis. 2011;70:482–487. doi: 10.1136/ard.2010.135871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sittiwet C, Simonen P, Gylling H, Strandberg TE. Mortality and cholesterol metabolism in subjects aged 75 years and older: The Helsinki Businessmen Study. J. Am. Geriatr. Soc. 2020;68:281–287. doi: 10.1111/jgs.16305. [DOI] [PubMed] [Google Scholar]
- 21.Khovidhunkit W, et al. Effects of infection and inflammation on lipid and lipoprotein metabolism: Mechanisms and consequences to the host. J. Lipid Res. 2004;45:1169–1196. doi: 10.1194/jlr.R300019-JLR200. [DOI] [PubMed] [Google Scholar]
- 22.Zhu Y, Liu X, Zhu R, Zhao J, Wang Q. Lipid levels and the risk of dementia: A dose-response meta-analysis of prospective cohort studies. Ann. Clin. Transl. Neurol. 2022;9:296–311. doi: 10.1002/acn3.51516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dietschy JM, Turley SD. Cholesterol metabolism in the brain. Curr. Opin. Lipidol. 2001;12:105–112. doi: 10.1097/00041433-200104000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Lane RM, Farlow MR. Lipid homeostasis and apolipoprotein E in the development and progression of Alzheimer's disease. J. Lipid Res. 2005;46:949–968. doi: 10.1194/jlr.M400486-JLR200. [DOI] [PubMed] [Google Scholar]
- 25.Benn M, Nordestgaard BG, Frikke-Schmidt R, Tybjaerg-Hansen A. Low LDL cholesterol, PCSK9 and HMGCR genetic variation, and risk of Alzheimer's disease and Parkinson's disease: Mendelian randomisation study. BMJ. 2017;357:j1648. doi: 10.1136/bmj.j1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giugliano RP, et al. Long-term safety and efficacy of achieving very low levels of low-density lipoprotein cholesterol: A prespecified analysis of the IMPROVE-IT trial. JAMA Cardiol. 2017;2:547–555. doi: 10.1001/jamacardio.2017.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Choo PW, et al. Validation of patient reports, automated pharmacy records, and pill counts with electronic monitoring of adherence to antihypertensive therapy. Med. Care. 1999;37:846–857. doi: 10.1097/00005650-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Lee JK, et al. How should we measure medication adherence in clinical trials and practice? Ther. Clin. Risk Manag. 2007;3:685–690. [PMC free article] [PubMed] [Google Scholar]
- 29.Choe HJ, Park S, Han KD, Moon MK, Koo BK. Contribution of hypertriglyceridemia to ischemic cardiovascular disease in Korean women: A nationwide population-based study. J. Clin. Lipidol. 2022;16:83–93. doi: 10.1016/j.jacl.2021.11.008. [DOI] [PubMed] [Google Scholar]
- 30.Jo YS, et al. Relationship between total cholesterol level and tuberculosis risk in a nationwide longitudinal cohort. Sci. Rep. 2021;11:16254. doi: 10.1038/s41598-021-95704-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lim JH, et al. Nationwide cohort study: Cholesterol level is inversely related with the risk of gastric cancer among postmenopausal women. Gastr. Cancer. 2022;25:11–21. doi: 10.1007/s10120-021-01241-1. [DOI] [PubMed] [Google Scholar]
- 32.Nam GE, Huh Y, Jung JH, Han K, Kim SM. Association of high-density lipoprotein cholesterol phenotypes with the risk of cardiovascular diseases and mortality: A cohort study in Korea. Endocrinol. Metab. (Seoul) 2022;37:261–271. doi: 10.3803/EnM.2021.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Navarese EP, et al. Association between baseline LDL-C level and total and cardiovascular mortality after LDL-C lowering: A systematic review and meta-analysis. JAMA. 2018;319:1566–1579. doi: 10.1001/jama.2018.2525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang X, et al. Twenty-year epidemiologic study on LDL-C levels in relation to the risks of atherosclerotic event, hemorrhagic stroke, and cancer death among young and middle-aged population in China. J. Clin. Lipidol. 2018;12:1179–1189.e1174. doi: 10.1016/j.jacl.2018.06.011. [DOI] [PubMed] [Google Scholar]
- 35.Tamborini CR, Kim C, Sakamoto A. Education and lifetime earnings in the United States. Demography. 2015;52:1383–1407. doi: 10.1007/s13524-015-0407-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Seong SC, et al. Data resource profile: The National Health Information Database of the National Health Insurance Service in South Korea. Int. J. Epidemiol. 2017;46:799–800. doi: 10.1093/ije/dyw253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Levey AS, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann. Intern. Med. 2006;145:247–254. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 38.Stampfer MJ, Kang JH, Chen J, Cherry R, Grodstein F. Effects of moderate alcohol consumption on cognitive function in women. N. Engl. J. Med. 2005;352:245–253. doi: 10.1056/NEJMoa041152. [DOI] [PubMed] [Google Scholar]
- 39.Lee YB, et al. Hospitalization for heart failure incidence according to the transition in metabolic health and obesity status: A nationwide population-based study. Cardiovasc. Diabetol. 2020;19:77. doi: 10.1186/s12933-020-01051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim MK, et al. Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: A nationwide population-based study. Eur. Heart J. 2017;38:3560–3566. doi: 10.1093/eurheartj/ehx585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 42.Sundararajan V, et al. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J. Clin. Epidemiol. 2004;57:1288–1294. doi: 10.1016/j.jclinepi.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 43.Nam GE, et al. BMI, weight change, and dementia risk in patients with new-onset type 2 diabetes: A nationwide cohort study. Diabetes Care. 2019;42:1217–1224. doi: 10.2337/dc18-1667. [DOI] [PubMed] [Google Scholar]
- 44.Yoo JE, et al. Blood pressure variability and the risk of dementia: A nationwide cohort study. Hypertension. 2020;75:982–990. doi: 10.1161/hypertensionaha.119.14033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the Korean National Health Insurance Service (KNHIS) but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the corresponding authors upon reasonable request and with permission of the KNHIS.