Abstract
Simple Summary
Cyclin-dependent kinase inhibitors (palbociclib (Ibrance), ribociclib (Kisqali), and abemaciclib (Verzenio)), targeting aberrant cell-cycle activity have been evaluated extensively in clinical trials. Significant delays in progression free survival and overall survival are now documented with each agent in estrogen receptor positive and human epidermal growth factor receptor two negative advanced breast cancer including luminal B breast cancer. Therapy resistance, driven by chromosomal instability, results in genomic rearrangements, activation of cell-cycle components (cyclin E/cdk2 in Rb− tumors, cyclin D1 in growth factor activated pathways), and the immune response. Molecular analysis of therapy resistant tumors may provide the rational basis for new therapies (brivanib, CYC065, WEE1 kinase and other inhibitors). Luminal B breast cancer is enriched for cyclin D1 overexpression and the chromosomal instability gene signature. The molecular mechanisms governing chromosomal instability in luminal B breast cancer remain poorly understood. Co-targeting of chromosomal instability may potentially reduce the prevalent escape mechanisms that reduce the effectiveness of cyclin-dependent kinase inhibitors.
Abstract
Cyclin-dependent kinases (CDKs) govern cell-cycle checkpoint transitions necessary for cancer cell proliferation. Recent developments have illustrated nuanced important differences between mono CDK inhibitor (CDKI) treatment and the combination therapies of breast cancers. The CDKIs that are currently FDA-approved for breast cancer therapy are oral agents that selectively inhibit CDK4 and CDK6, include palbociclib (Ibrance), ribociclib (Kisqali), and abemaciclib (Verzenio). CDKI therapy is effective in hormone receptor positive (HR+), and human epidermal growth factor receptor two negative (HER2−) advanced breast cancers (ABC) malignancies, but remains susceptible due to estrogen and progesterone receptor overexpression. Adding a CDK4/6I to endocrine therapy increases efficacy and delays disease progression. Given the side effects of CDKI, identifying potential new treatments to enhance CDKI effectiveness is essential. Recent long-term studies with Palbociclib, including the PALLAS and PENELOPE B, which failed to meet their primary endpoints of influencing progression-free survival, suggest a deeper mechanistic understanding of cyclin/CDK functions is required. The impact of CDKI on the anti-tumor immune response represents an area of great promise. CDKI therapy resistance that arises provides the opportunity for specific types of new therapies currently in clinical trials.
Keywords: abemaciclib, advanced breast cancer, CDK4/6 inhibitor, hormone receptor-positive, palbociclib, ribociclib
1. Introduction
Despite the extensive use of anti-hormonal endocrine therapy and chemotherapy, therapy resistance and long-term side effects have led to the introduction of alternative treatments targeting the cell-cycle machinery. The essential role of CDKs in promoting cell cycle progression (through phosphorylation of Retinoblastoma (Rb)) established CDK4/6Is as a selective target therapy to influence outcomes in breast cancer, especially therapy-resistant breast cancer [1]. In clinical practice, the most commonly used CDK4/6Is include palbociclib, ribociclib, and abemaciclib for HR+ advanced breast malignancies. Developments of these agents derive from carefully controlled research trials. Three FDA-approved CDK4/6 inhibitors are palbociclib, ribociclib, and abemaciclib. Ribociclib is very similar to palbociclib in structure, but abemaciclib is different. In vitro studies indicated that palbociclib has an almost equivalent inhibition effect on CDK4 and CDK6, while abemaciclib and ribociclib are more potent against CDK4 than CDK6 [2,3,4]. Other inhibitors of CDK including CDK5 are in development and have been reviewed elsewhere [5]. The current review focuses on CDK4/6 inhibitors, to provide a clinical update noting the recent disappointments and a synopsis of the mechanisms governing therapy resistance and potential alternative approaches for the treatment of such resistance.
Several clinical trials formed a platform upon which the clinical utility of CDKI are based, including the PALOMA (Palbociclib Ongoing Trials in the Management of Breast Cancer) studies, showed significant results for palbociclib use, whereas the “Mammary Oncology assessment of LEE011’s (ribociclib’s) Efficacy and Safety” (MONALEESA) trials have proven ribociclib therapy as a viable treatment option. In addition, the MONARCH research studies have revealed improved survival outcomes on abemaciclib therapy in ABC patients.
2. Breast Cancer and Existing Targeted Therapy
Only to certain dermatologic malignancies, breast cancer leads to female mortality in the United States [6]. Breast cancer may be characterized based on coding [7] or non-coding genome [8]. The three most common molecular subtypes of breast cancers based on the coding genome are HR+ malignancies (estrogen receptor-positive (ER+) and progesterone receptor positive (PR+) breast cancers) [9], HER2+, and triple-negative breast cancer (TNBC) malignancies. HR+ breast cancer cells retain sensitivity to estrogen/progesterone-blocking endocrine therapy. HR− breast cancer types are without a rational basis for endocrine treatments. HER2+ breast cancer cells display amplified expression of HER2 receptors that is targeted by antibodies, including the humanized monoclonal antibody trastuzumab (Herceptin) [10,11,12,13]. In contrast, TNBC malignancies which have the worst prognosis, do not express estrogen receptor (ER), progesterone receptor (PR), or HER2/neu, and are now being assessed for new targeted therapies to PARP, Trop2, CCR5 [14], DNMT1, VEGF and immune checkpoints [15,16].
Luminal A breast cancers express hormone receptors (ER+ and PR+/−) but lack expression of HER2 and have low levels of Ki-67 protein (a marker of proliferation). These subtypes grow slowly, are low-grade, with the best prognosis, and are most likely to benefit from hormone therapy but may not benefit from chemotherapy [17], and side effects from chemotherapy may outweigh the value of chemotherapy in this population [18]. Luminal B breast tumors are ER+ and PR+/− and HER2+/−, with increased levels of Ki-67. Such subtypes grow faster with a slightly worse prognosis than Luminal A, with the best response to endocrine therapy, chemotherapy, and targeted anti-HER2 therapy in HER2+ patients [17,19,20]. HER2+ tumors are HER2-enriched, PR−/HR−, and tend to grow faster and benefit most from targeted therapies against HER2. Basal-like breast cancer, often referred to as TNBC due to its lack of ER, PR, and HER2 expression, is the most common subtype amongst patients with breast cancer gene 1 (BRCA1) mutations (early-onset) and African American women [21].
Factors contributing to breast cancer development include strong family history, BRCA1 and breast cancer gene 2 (BRCA2) gene mutations, a history of atypical hyperplasia, alcohol intake, and increased age. Ethnicity also plays a role, with TNBC being most prevalent in African American women. In contrast, Caucasian women are more susceptible to other breast cancer subtypes, particularly infiltrating ductal carcinoma, lobular carcinoma, and tubular adenocarcinoma [15]. In addition, higher estrogen exposure throughout a patient’s lifetime (i.e., early menstruation, late menopause, nulliparity, postmenopausal obesity, the elevated total number of menstrual cycles, absence of breastfeeding, later age of first pregnancy, alcohol intake, Klinefelter syndrome in men, etc.) can increase the risk of breast cancer [22].
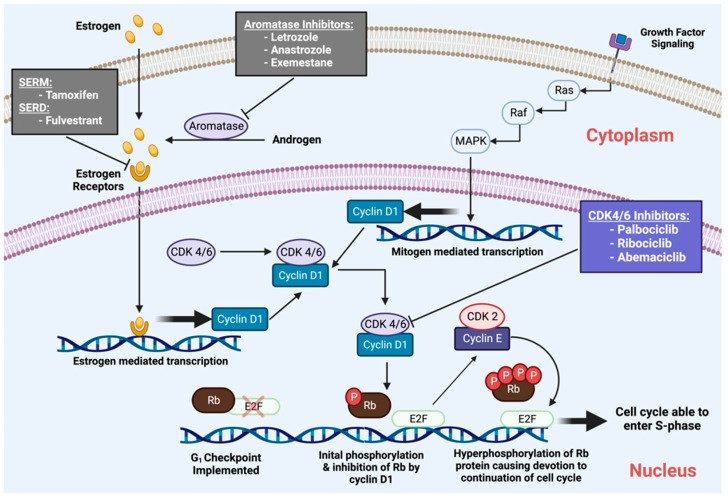
Anti-estrogen treatments include aromatase inhibitors, such as letrozole, and estrogen receptor antagonists, such as fulvestrant. However, a consequence of these long-term therapies is acquired resistance. Therefore, additional agents are required to attenuate the mechanisms of resistance and its associated rise in breast cancer mortality rates. To prevent therapeutic resistance, long-term therapies for breast malignancies must be consistent, stable, and, most importantly, selective to the target cancer cells [23]. The specificity of the CDK4/6Is, and evidence for increased CDK activity in HR+ breast cancers suggested the potential utility of CDK4/6Is in combination with endocrine therapy for therapy-specific breast cancer subtypes [24,25] (Figure 1).
Figure 1.
CDK in Breast Cancer therapy.
3. The Regulatory Cyclin D Subunit Are Frequently Amplified in Human Breast Cancer
The cyclin regulatory subunit together with the catalytic CDK subunit generates a holoenzyme that phosphorylates gatekeeper proteins coordinating cell cycle progression [26]. The cell cycle is divided into phases, controlled by checkpoint transitions that proceed in an orderly and precise manner to ensure cellular growth and proliferation. Cyclin/CDK complexes must be activated and inactivated at appropriate times to ensure carefully timed progress through the cell cycle [26]. The holoenzymes are serine and threonine kinases that regulate cell cycle progression via selective phosphorylation of target substrates [27]. CDK4, and CDK6, together, with their cyclin-D regulatory subunits, promote the G1/S phase progression of the cell cycle [28]. The cyclin-CDK holoenzyme complexes phosphorylate the Rb protein to release elongation factor two (E2F) and promote DNA synthesis [28].
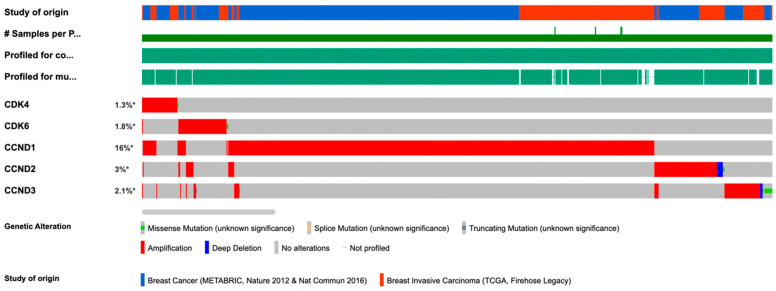
The CCND1 gene encodes cyclin D1 is frequently amplified in human breast cancers [2]. Analysis of 3617 samples, combining the METABRIC and TCGA (Firehose Legacy data) showed amplification of CDK4 is a rare event (1.3%) co-occurring with cyclin D1 amplification (Figure 2). Cyclin D1 protein abundance is increased as a consequence of overexpression, gene amplification, transcriptional induction or post-transcriptional induction, in >50% of breast cancers [2].
Figure 2.
Infrequent CDK4/6 amplification in Breast Cancer therapy. Analysis of 3617 breast cancer samples from CBIOPORTSAL, combining the METABRIC and TCGA (Firehose Legacy data) showed amplification of CDK4 is a rare event (1.3%), co-occurring with cyclin D1 amplification. Frequent amplification of the regulatory subunit of the cyclin D/CDK complexes (cyclin D1, CCND1) occurs in human breast cancer. # number of samples. * percentage of patients in the population with the particular genetic abnormality.
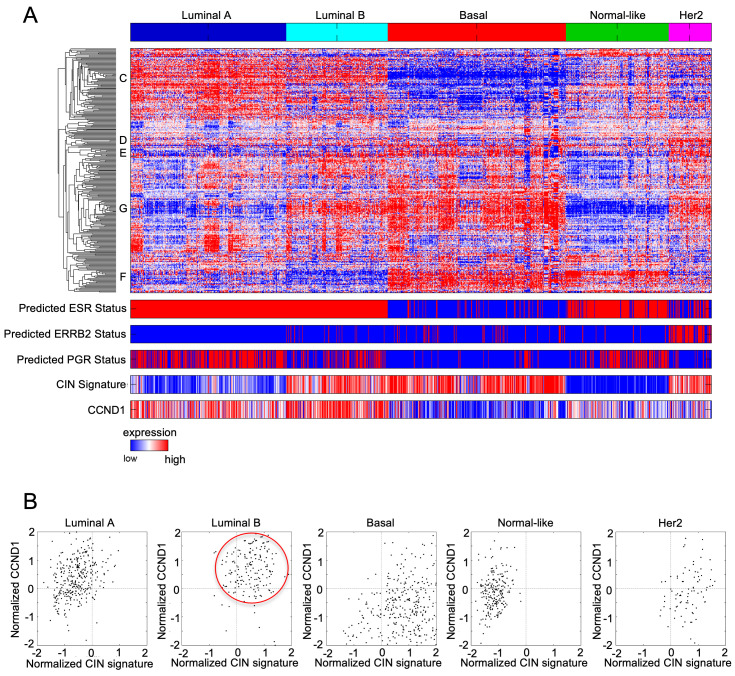
Cyclin D1 is overexpressed primarily in luminal breast cancer (luminal A and luminal B) associated with ERα+ breast cancer (Figure 3A). Consistent with the model in which cyclin D1 induces chromosomal instability, increased cyclin D1 correlates with the expression of chromosomal instability signature (Figure 3B). In tissue culture, CDKI reduces RB protein phosphorylation, reducing the release E2F from binding to Rb and G1 cell cycle arrest [29,30,31]. In addition, CDKIs have additional anticancer effects in breast cancer, including enhancing cancer cell immunogenicity and promoting cellular senescence [32].
Figure 3.
Chromosomal instability signature and cyclin D1 expression in breast cancer subtypes. (A) Heatmap of breast cancer microarray datasets assigned to the breast cancer coding genome expression subtypes. The predicted ESR1, epidermal growth factor receptor (ERBB2), and progesterone receptor (PGR) statuses are shown together with a chromosomal instability gene signature (CIN) signature score and CCND1 expression level across the 5 subtypes. The CIN signature score, and cyclin D1 expression level are outlined for the luminal B subtype. (B) CCND1 transcript level plotted vs. CIN signature expression level show a correlation between high CIN score and high cyclin D1 expression in luminal B subtype specific (red circle).
4. CDK Inhibitors
Early efforts to produce CDKIs resulted in relatively non-selective targeting of several CDKs. However, the current generation CDKIs more specifically target CDK4 and CDK6, allowing for better toleration and reduced toxicity. The current FDA-approved CDKIs decrease phosphorylation of the RB tumor suppressor, promoting cell cycle arrest at the G1/S transition checkpoint. Current NCCN Guideline recommendations for metastatic HR+/HER2−, breast cancer include the addition of CDK4/6Is with hormonal therapy (letrozole, fulvestrant) in postmenopausal and for premenopausal patients as a preferred first-line treatment (Table 1, [33]). Palbociclib is a highly specific inhibitor of cyclin-dependent kinase 4 (Cdk4) (IC50, 0.011 µM) and Cdk6 (IC50, 0.016 µM).
Table 1.
Summary of FDA approved CDK4/6 Inhibitors.
| Drug | Mechanism of Action IC50 (nM) |
Recommended Dose Half-Life Tmax |
Drug Interactions IC50 against Bone Marrow Mononuclear Cells (nM) |
References |
|---|---|---|---|---|
| Palbociclib | Similar potency against cyclin D1/CDK4 and cyclin D2/CDK6 | 125 mg po once a day for 21 days in a 28-day cycle with food | CYP3A4 substrate 240 ± 43 |
[34,35,36,37,38] |
| CDK4–cyclin D1 | 11 | |||
| CDK6–cyclin D1/2/3 | 16 | Half-life | ||
| CDK1–cyclin B | >10,000 | 26–27 h | ||
| CDK2–cyclin A/E | >10,000 | Tmax | ||
| CDK5–p25 | >10,000 | 6–12 h | ||
| Ribociclib | Greater potency against CDK4 than CDK 6 | 600 mg po once daily for 21 days in a 28- day cycle with or without food | CYP3A4 substrate 1700 ± 231 |
[39,40] |
| CDK4–cyclin D1 | 10 | |||
| CDK6–cyclin D1/2/3 | 39 | Half-life | ||
| CDK1–cyclin B | 113,000 | 33–42 h | ||
| CDK2–cyclin A/E | 76,000 | Tmax | ||
| CDK5–p25 | 43,900 | 1–5 h | ||
| Abemaciclib | Greater potency against CDK4 than CDK 6 (CDK4 and CDK6 with IC50 of 2 nM and 10 nM | 150 mg or 200 mg po BID with or without food. | CYP3A4 substrate, BCRP, Pgp 230 ± 27 |
[4,41,42,43] |
| CDK4–cyclin D1 | 2 | |||
| CDK6–cyclin D1/2/3 | 10 | Half-life | ||
| CDK1–cyclin B | 1627 | 17–38 h | ||
| CDK2–cyclin A/E | 504 | Tmax | ||
| CDK5–p25 | 355 | 4–6 h |
Palbociclib. Palbociclib is a specific CDK4/6I. Palbociclib-responsive breast tumors are ER+, Rb+ with cyclin D1 overexpression. Palbociclib is best used with an aromatase inhibitor, frequently used in postmenopausal women and men who have not had prior hormonal therapy [44]. The aromatase inhibitors regularly used in combination therapy include Arimidex/anastrozole, Aromasin/exemestane, and Femara/letrozole. However, in all patients with previous hormonal therapy, palbociclib is best combined with the ER antagonist Faslodex/fulvestrant [45,46,47,48,49,50,51,52]. Female patients on this latter regimen must be on an LHRH (luteinizing hormone releasing-hormone) agonist to suppress ovarian function as the palbociclib/ER antagonist combination therapy results in continuous stimulation of the hypothalamic–pituitary–ovarian axis feedback loop, thereby inhibiting ovarian estrogen production, allowing tumor growth suppression [53].
PALOMA-1 was the first of many trials to analyze the therapeutic effects of combination therapy with palbociclib and letrozole in advanced breast cancer (ABC). The PALOMA-1 trial randomized postmenopausal women with ER+/HER2− ABC to letrozole alone (2.5 milligrams (mg) daily) or in combination with palbociclib (125 mg daily). Palbociclib augmented progression-free survival (PFS) in the patients taking letrozole combination therapy, (Table 2 [54]) resulting in FDA approval (April 2013 [37]).
Table 2.
Summary of CDK4/6 Inhibitors and Corresponding Research Trials.
| DRUG | TRIAL | TARGET POPULATION | EXPERIMENTALGROUP | CONTROL GROUP | CHANGE IN PFS | CHANGE IN OS |
|---|---|---|---|---|---|---|
| PALBOCICLIB | PALOMA-1 | 165 postmenopausal | +Letrozole | Letrozole monotherapy | 20.2 vs. 12.9 months [34,35,53,54,61] |
[34,35,53,54,61] |
| PALOMA-2 | 666 postmenopausal | Placebo + Letrozole | 24.8 vs. 14.5 months [34,35,53,61] |
|||
| PALOMA-3 | 521 pre/peri/post-menopausal | +Fulvestrant | Placebo + Fulvestrant | 9.2 vs. 3.8 months [34,35,53,57,61] |
6 years OS, 19.1% vs. 12.9% [62] | |
| PALLAS | 5796 (5761 included in analysis) | +Endocrine adjuvant | Endocrine adjuvant | N/A [34,35,53,59] |
||
| PENELOPE-B | 1250 included in analysis | +standard endocrine adjuvant | Placebo + standard endocrine adjuvant | N/A [60] |
||
| RIBOCICLIB | MONALEESA-2 | 668 postmenopausal | +Letrozole | Placebo + Letrozole | 20.5 vs. 12.8 months [53,61,63,64] [53,63,64] |
|
| MONALEESA-3 | 726 men and postmenopausal women with prior exposure to ET | +Fulvestrant | Placebo + Fulvestrant | 42 months OS 57.8% vs. 45.9% [65] |
||
| MONALEESA-7 | 672 pre/peri-menopausal | +Fulvestrant + Goserelin | ET + Goserelin | 23.8 vs. 13.0 months [53,61,63,64] |
||
| ABEMACICLIB | MONARCH-1 | 132 with prior ET or chemo exposure | Monotherapy | N/A | 16.4 vs. 9.3 months [42,53,61] [53,66] |
|
| MONARCH-2 | 669 with prior ET exposure | +Fulvestrant | Placebo + Fulvestrant | 46.7 months OS vs. 37.3 months [67] | ||
| MONARCH-3 | 493 postmenopausal | +Letrozole | Placebo + Letrozole | 28.2 vs. 14.8 months [53,61,68] |
* ET = endocrine therapy [69]. N/A primary end point not achieved.
PALOMA-2, a phase III double-blind research study, was performed to further evaluate the outcomes of PALOMA-1. PALOMA-2 employed the exact dosage and scheduling of Palbociclib as PALOMA-1. Palbociclib treatment resulted in the extension of PFS compared to the placebo-controlled group, as shown in Table 2. Due to the greater number of patients, there was a more significant benefit observed in all breast cancer patient subgroups in PALOMA-2. This includes patients with lobular carcinoma and those who developed metastasis within 12 months of diagnosis, considered advanced breast cancer [55], resulting in FDA accelerated approval for palbociclib in February 2015.
The double-blinded phase III PALOMA-3 trial sought to assess the potential for combination therapy with palbociclib and the most common selective estrogen receptor degraders, fulvestrant. The patients treated were ER+, HER2− breast cancers. The palbociclib group experienced extension to PFS and OS compared to placebo (Table 2) [56]. In addition, although palbociclib toxicity was frequent, improvement in global quality of life was noted [56,57,58].
The “Palbociclib Collaborative Adjuvant Study” (PALLAS) was initiated in 2015. to determine disease-free survival (iDFS) in patients who received palbociclib with an endocrine therapy versus a standalone endocrine therapy. Ultimately, 5761 patients were randomly assigned to either treatment group, with 2884 receiving palbociclib and endocrine therapy, and 2877 received only endocrine therapy, with each group receiving treatment for at least 5 years. The palbociclib was dosed at 125 mg orally given once daily for 21 days, followed by a 7-day break from treatment in a cycle of 28 days, and this continued for 2 years, along with a standard endocrine adjuvant for 5 years. At the median follow-up period of 31 months, the iDFS were compared for both treatment groups. The results showed that iDFS occurred at a rate of 8.8% in the patients receiving palbociclib plus the endocrine adjuvant and at a rate of 9.1% in patients just receiving the standard endocrine therapy on its own. Palbociclib added to an adjuvant endocrine therapy did not significantly improve compared to endocrine therapy on its own [59]. Palbociclib is not recommended in the adjuvant setting of stage II/III h ERα+, HER2− breast cancer because the addition of Palbociclib to standard endocrine therapy (ET) did not improve outcomes. The molecular mechanisms governing this outcome is investigated through assessment of the Trans-PALLAS program samples.
The PENELOPE-B trials were conducted to assess the efficacy of combining palbociclib with adjuvant chemotherapy in breast cancer treatment outcomes. The PENELOPE-B trials randomly assigned patients to either 13 cycles for 4 weeks at a time of palbociclib or placebo treatment. The palbociclib group received 125 mg given once daily given from days 1 to 21, followed by a 7-day break in a 28-day cycle of treatment. The placebo group also followed this dosing schedule. Both groups were also given standard neoadjuvant chemotherapy alongside palbociclib or the placebo. The primary outcome of interest was iDFS based on the random assignment of 1250 patients. The end of the trial showed that the use of palbociclib did not improve the iDFS compared to the use of a placebo, ultimately leading to the conclusion that the use of palbociclib for 1 year alongside estrogen therapy did not lead to improvement in iDSF [60]. The primary endpoint, of improving invasive disease-free survival (iDFS) in ERα+, HER2− breast cancer patients who had residual invasive disease after completing neoadjuvant chemotherapy (the phase 3 PENELOPE-B) was not met.
Ribociclib. Ribociclib, the second CDK4/6I to become FDA approved, is structurally and functionally similar to palbociclib, and can be used in premenopausal, perimenopausal or postmenopausal women. It is most effective when combined with aromatase inhibitors, including anastrozole, exemestane, and letrozole. Like palbociclib, ribociclib requires fulvestrant adjunct therapy to suppress ovarian function, particularly in postmenopausal patients without prior endocrine therapy [40,70,71,72,73,74]. The most concerning adverse effect of ribociclib use is cardiotoxicity, monitored with electrocardiograms (EKGs).
The MONALEESA trial was a randomized, double-blinded study using oral dosing of ribociclib [63]. The MONALEESA-2 trial examined the clinical benefits of ribociclib (600 mg and higher) over standard therapy with letrozole in patients with advanced metastatic disease (all subtypes and/or ≥1 lytic bone lesion) [39]. Patients were then stratified by either the presence or absence of visceral malignant advancement.
The MONALEESA-3 study was a randomized, placebo-controlled phase III study designed to assess the benefits of ribociclib in combination with fulvestrant for patients with confirmed HR+/HER2− ABC, including men and postmenopausal women and patients with advanced metastatic disease (all subtypes and/or ≥1 lytic bone lesion). Combination therapy of ribociclib plus fulvestrant significantly prolonged PFS and OS compared to placebo plus fulvestrant, (Table 2 [64]). The MONALEESA-7 trial extended these findings to examine the effect of ribociclib on PFS rates in comparison to endocrine therapy alone in premenopausal or perimenopausal patients with HR+/HER2− ABC [63].
Although CDKIs have been shown to have the best results in conjunction with endocrine therapy, palbociclib and ribociclib in particular, synergize well in combination with phosphoinositide 3-kinase (PI3K) and mammalian target of rapamycin (mTOR) inhibitors. Similar to the effects of CDKIs, antagonism of protein kinase B (AKT) and 3-phosphoinositide-dependent protein kinase 1 (PDK1) produce a similar reduction in tumor growth and progression via cancer cell senescence. Moreover, pairing ribociclib with PI3K/mTOR inhibitors reduced ribociclib resistance, especially in ER+/HER2− breast cancer patients, which is mediated by the PI3K/AKT pathway [75].
Abemaciclib. A third FDA-approved CDK4/6I for breast cancer management is abemaciclib. Abemaciclib has different clinical features than other CDKIs, presumably due to its more significant inhibition of CDK4 than CDK6 and inhibition of CDK9 [76]. Administration of abemaciclib is provided continuously daily if well tolerated (a twice-daily regimen is permitted), which differs from the dosing schedule for other CDKIs [41,42].
The FDA approved abemaciclib for use in HR+/HER2− ABC treatment in 2017 as either monotherapy in patients receiving endocrine therapy or chemotherapy or used in conjunction with fulvestrant in those with prior exposure to hormonal therapy. The MONARCH trials were initiated to investigate abemaciclib therapy’s results in different potential breast cancer management regimens. MONARCH-1, a phase II research trial, examined abemaciclib monotherapy (200 mg twice daily) in HR+/HER2− ABC patients with previously significant exposure to treatment with endocrine therapy and chemotherapy [42].
The MONARCH-2 phase III trial randomized patients with HR+/HER2− ABC to either fulvestrant plus abemaciclib (150 mg twice daily) or placebo [66]. PFS and OS of the combined therapy group was significantly greater than placebo (Table 2). In addition, the combination of fulvestrant with abemaciclib conveyed beneficial results in patients with primary endocrine therapy resistance, significantly increasing overall survival [66]. The MONARCH-3 trial demonstrated similar effectiveness of combination abemaciclib therapy with aromatase inhibitors in the same patient demographic as MONARCH-2 [68].
The MONARCH trial indicated the use of abemaciclib with aromatase inhibitors for postmenopausal women without prior hormonal therapy exposure. There was also robust evidence for combining abemaciclib with fulvestrant to suppress ovarian functions in premenopausal and perimenopausal women. Lastly, there was supporting evidence that both male and female patients should receive abemaciclib as monotherapy after ineffective use of anti-hormonal and chemotherapy for the management of metastatic breast cancer [67].
Further differences between abemaciclib and other CDKIs result from its capacity to cross the blood–brain barrier (BBB), thus allowing penetration into the cerebrospinal fluid (CSF). This characteristic is essential for the treatment of brain metastasis in breast cancer patients [77,78,79,80,81,82]. Abemaciclib’s ability to adequately reach the central nervous system results in substantial improvement in morbidity of metastatic breast cancer patients and potentially for other primary CNS malignancies. The ability of CDKIs to accumulate in CSF depends on many factors, particularly the presence of p-glycoprotein (P-gp) and breast cancer resistance proteins in the CNS. These proteins act to extract and dispose of certain drugs from the brain, including palbociclib and abemaciclib [77]. Although both these drugs can penetrate the BBB, they display different levels of accumulated CSF concentrations due to palbociclib’s greater efflux by P-gp. Thus, abemaciclib is the most effective CDKI to manage brain metastasis of breast malignancies [41]. Pharmacodynamic markers are used to monitor patient response to abemaciclib therapy to observe treatment efficacy. These markers include the expected decline in phosphorylated-Rb protein and topoisomerase II-alpha, which are associated with treatment competence [41].
5. Dose-Limiting Side Effects
Although each CDKI can produce side effects, the most common ones seen with these drugs include bone marrow suppression, cardiotoxicity, hepatotoxicity, and gastric toxicity, and most are contraindicated in pregnant patients. Common side effects of CDKIs include pancytopenia, particularly neutropenia, lethargy, fatigue, nausea, diarrhea, and low-grade alopecia. The high rates of febrile neutropenia are monitored by complete blood counts (CBCs) with differential. These effects are generally resolved after discontinuation of CDKI therapy [34,35,36].
The PALOMA trials highlighted side effects and precise dosing as essential in obtaining the most therapeutic value with palbociclib. The most significant side effect of palbociclib is acute neutropenia (up to 62% of patients), resulting in immunosuppression and infections managed with antibiotics [83]. The time taken for the appearance of neutropenia from initiation of treatment was 20 days, with the recurrence slowly reducing over therapy use [37]. Monitoring for adverse effects via CBCs with differential is conducted regularly, recommended on day 14 and performed if any complications arise within the treatment period [34,35,36].
Toxic effects of ribociclib are similar to those of palbociclib, with the addition of cardiotoxic side effects with ribociclib. These effects are monitored with routine EKGs. Dose-dependent prolongation of the QT interval is seen at a dose of 600 mg. Detection of QT interval with Fridericia’s correction (QTcF) was observed to be >480 milliseconds (ms), whereas the standard length of this period is ideally 400–440 ms. This conduction abnormality can lead to irregular heartbeats and eventually life-threatening arrhythmias. As such, patients with prior cardiac disease, prolonged QTcF or those taking any other medications that increase the risk of QT lengthening are not approved to be involved in this study (30). Routine monitoring of hepatic transaminases with liver function tests (LFTs) and bilirubin levels is required to prevent liver complications. These effects are generally resolved after discontinuation of ribociclib (30).
A significant distinction between abemaciclib and other CDKIs is its minimal hematologic adverse effects, with mild leukopenia seen in patients rather than the expected high-grade neutropenia [4,41,42]. The more common and more favorable side effects seen with abemaciclib use include fatigue and gastrointestinal toxicity, particularly abdominal pain, diarrhea, and nausea [66]. These may lead to dehydration and infection; however, management with Imodium (loperamide), greater fluid intake, and changes in diet can relieve these symptoms. Abemaciclib is not recommended in patients with any underlying gastrointestinal conditions such as irritable bowel syndrome, colitis, or diverticulitis [84,85]. Additionally, an observed elevation of creatinine is seen with abemaciclib use; however, it may not be directly associated with renal impairment but due to drug interference with creatinine tubular secretion [41]. These benign adverse effects are managed with dose reductions or modifications, particularly during the first two months of initial therapy. Intolerance to side effects may require a break from treatment, as with any serious complications [86].
The dosage for palbociclib and ribociclib administration follows the same schedule, with intake for three weeks (21 days) followed by a one-week (7-day) interval without CDKI use to complete a 28-day cycle. However, letrozole (2.5 mg) is taken continuously throughout the four weeks of the combination drug regimen. Initial palbociclib dosing begins at 125 mg, and ribociclib is dosed at 600 mg (dispensed as three 200 mg tablets). Fulvestrant administration is given intramuscularly (500 mg) on the first day of every 28-day cycle, administered as two injections in each gluteal muscle. Additionally, in the first cycle, an extra fulvestrant dose is provided for day 15 [63,64,87]. Abemaciclib administration is provided continuously daily, permitting a 150 to 200 mg dosing regimen every 12 h (twice daily) if well tolerated [41,42].
6. Mechanisms of Resistance to CDK4/6 Inhibitors
A review of the clinical trials (Table 2) illustrates the vital impact the new generation of CDK inhibitors has had, yet raises several important questions. Firstly, CDK activity remains inhibited in the patients’ tumors, yet the tumors progress. The reduction in RB phosphorylation as the tumor progress suggests CDK independent pathways maintain tumor growth. The development of resistance to CDK4/6I is typical in most patients. The tumors being treated have high levels of chromosomal instability, and consequent genomic instability [29] as cyclin D1 overexpression is a driver of chromosomal instability [29,88,89]. Consistent with the high level of CIN, genomic alterations occur with CDKI therapy, including loss of the RB gene, altered cyclin E1 expression [90], p27 inhibition [91], and activation of the Phosphatidylinositol-4,5-Bisphosphate 3-Kinase Catalytic Subunit Alpha (PIK3CA) pathway [92].
Genetic loss and mutations of RB. RB is a tumor suppressor protein that acts as a critical checkpoint regulator of the G1/S phase of the cell cycle and is, therefore the main target of CDK4/6Is to cause cell-autonomous G1 arrest. Rb regulates E2F, a downstream transcription factor. E2F bound to Rb restrains induction of the G1 to S phase cell cycle. RB genetic loss or silencing causes CDKI resistance [93,94,95,96]. Loss of RB is associated with increased E2F expression leading to constitutive activation of downstream proteins. E2F can upregulate AKT signaling via GRB2 Associated Binding Protein 2 (Gab2) [97]. In tumors where Rb is inactivated, the targeted inhibition of the cyclin E-CDK2 axis in combination with CDK4/6Is may effectively overcome resistance to CDK4/6Is [54,98].
Cyclin E1 and cyclin E2 as biomarkers of response to CDK4/6 inhibitors. Cyclin E1 overexpression may constitute a resistance mechanism in patients treated with fulvestrant + palbociclib. CDK4/6 inhibitor resistance is associated with increased CDK2 activation (reviewed in [99]. In such circumstances, CDK2/cyclin E inhibitors such as Cyclacel (CYC065) may be of use [100]. The PALOMA-2 and PALOMA-3 trials showed that palbociclib addition to endocrine therapy benefited recurrence-free survival irrespective of CCNE1 and CCNE2 levels in the pre-treated primary tumor samples. However, the expression of CCNE1 distinguished patients with the longest vs. the shortest recurrence-free survival. Cyclin E1 is not amplified in ERα+ breast cancer, nor does amplification appear to occur during progression to resistance [101]. In both the MONALEESA-2 (letrozole/ribociclib) and the PALOMA-3 (fulvestrant/palbociclib) trials, high expression of CCNE1 mRNA was associated with poor progression-free survival [100]. In the PALOMA-3 trial, high pre-existing CCNE2 mRNA expression was not associated with any difference in progression-free survival [101], nor did CCNE2 amplification increase during disease progression [102]. In the MONALEESA-7 and CLEE011X2106 trials there was a trend for CCNE1-high patients to have poor progression-free survival. Furthermore, patients expressing cytoplasmic cyclin E1 protein, reflecting a low molecular weight form of cyclin E1, had worse survival than patients expressing only nuclear cyclin E1 protein [103]. In the POP trial of pre-operative palbociclib, CCNE2 expression was significantly decreased in antiproliferative responders vs. non-responders measured over 15 days (p = 0.006) [104]. CCNE1 was high in patients who maintained high Ki67 after 15 days of treatment in the NeoPalAna study [44] in the PALOMA-3 trial [102].
p16 Amplification. The tumor suppressor p16INK4a, a member of the inhibitors of the CDK4 (INK4) family and a natural inhibitor of CDK4, is involved in cell cycle control and regulation [92]. Since CDK4/6 (a p16 target) requires Rb for its kinase activity, p16 acts as a tumor suppressor when functional Rb is present [105]. p16 overexpression occurs during oncogenic stress in the presence or absence of Rb [106,107]. In human breast cancer, p16INK4a is inversely correlated with cyclin D1 and ERα expression [108]. p16 expression lacked prognostic relevance in TNBC [109]. p16INK4a inactivation by DNA methylation occurs in ≤30% of human breast cancers [110] however increased abundance is also reported [109]. In mouse models of tumorigenesis Ink4a/Arf+/− mice have increased Eμ-Myc-induced lymphomagenesis and epidermal growth factor receptor-induced gliomagenesis. In ErbB2-induced mammary tumorigenesis, Ink4a/Arf+/− mice showed decreased p16INK4a, increased Ki-67 expression, increased cyclin D1 protein but decreased mammary tumor apoptosis [111]. Currently, two theories exist involving loss of Rb and amplification of p16 [112]. Further studies might be beneficial in designing the strategies to overcome acquired resistance to CDK4/6Is.
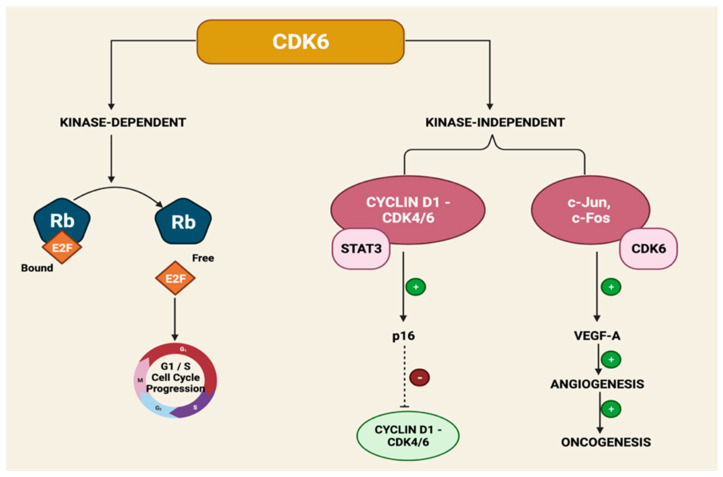
CDK6 Amplification. The catalytic subunit CDK6 conveys both kinase-dependent and kinase-independent roles via gene transcription [113]. CDK6 upregulates p16INK4a in the presence of STAT3 and cyclin D1 [114]. CDK6 increases vascular endothelial growth factor A (VEGF-A) and c-Jun, promoting angiogenesis to allow the promotion of breast cancer progression and CDK4/6I resistance [115] (Figure 4).
Figure 4.
Mechanism of CDK6 Amplification in Resistance to CDK4/6 Inhibitors.
CDK4 Amplification. CDK4 can be amplified via gene amplification, mutations, and epigenetic alterations, which allows overactivation of the cyclin D1-CDK4/6-Rb pathways. Although CDK4 overexpression has been seen in several cancers and may limit the therapeutic efficacy of CDK4/6Is [116,117], this is an uncommon event in breast cancer.
Activation of the FGFR Pathway. The fibroblast growth factor receptor (FGFR) leads to a signaling pathway that plays a vital role in proliferation, differentiation, and cell survival [118]. The FGFR pathways, particularly FGFR1-4, are overactivated in breast cancer and other malignancies and are implicated in cancer progression [119]. Therefore, FGFR1 and FGFR2 are associated with CDK4/6I resistance development and endocrine therapy resistance. FGFR1 amplification activates of the PI3K/AKT and RAS/MEK/ERK signaling pathways, specifically in endocrine-resistant breast cancer cells [120,121]. Laboratory-induced FGFR1 overexpression showed resistance to combination therapy with palbociclib/fulvestrant and fulvestrant monotherapy [122]. FGFR2 is the main activating factor of the FGFR pathway and functions to promote endocrine resistance. Therefore, a potential option in overcoming CDKI resistance may require combined inhibition of both CDK4/6 and FGFR pathways by combining brivanib, an FGFR-1/VEGFR-2 kinase inhibitor, with tamoxifen, which could potentially maximize the therapeutic efficacy and rescue cells’ sensitivity to endocrine therapy [121].
Activation of the PI3K/AKT/mTOR Pathway. In approximately 30–40% of breast cancer cases, especially HR+ subtypes, activation of the PI3K/AKT/mTOR signaling pathways are seen [93,122]. Dysregulation of this pathway can lead to critical resistance to endocrine therapy and was recently reported to be associated with CDK4/6I resistance [75]. Patients with CDKI-resistant breast cancer cells have become more dependent on PI3K/AKT/mTOR signaling pathways rather than ERα signaling for oncogenesis. CDK4/6I phosphorylate AKT via PDK1 to activate PI3K/AKT/mTOR pathways in ribociclib-resistant breast cancer cells. CDK4/6I-resistant breast cancer cell lines show reactivation of phosphorylated-Rb and E2F, which may occur via the CDK or the mTOR pathways [123]. A recent study suggested that PI3K inhibitors may downregulate cyclin D1 expression and promote resistance to CDK4/6Is. Therefore, there are potential therapeutic benefits in combination therapy of PI3K/AKT/mTOR inhibitors and CDK4/6Is in addressing CDKI resistance and enhancing the anticancer effect in CDKI-sensitive cases [93].
Loss of ERα or PR Expression. A critical factor in the progression of breast carcinogenesis is cyclin D1-CDK4/6 activity which allows hormone-mediated activation of ER [37]. Abemaciclib-resistant breast cancer cell lines exhibited loss of ER/PR expression [115]. This results in the loss of the estrogen-dependent driver of tumor growth; however, this can also lead to a mechanism of resistance to CDK4/6I therapy. In addition, patients who develop resistance mechanisms to CDKI treatment may require treatment methods beneficial in HR− subtypes of breast cancers.
Higher transcriptional activity of AP-1 transcription factor. The structure of activator protein 1 (AP-1) is a heterodimer composed of proteins belonging to the c-Fos, c-Jun, activation transcription factor (ATF), and transcription factor MAF sub-families [124]. Approximately 20–40% of breast cancers have increased c-Jun activity [125]. Selective c-jun gene deletion in mice evidenced a role for c-Jun in maintaining breast epithelial cell survival [126]. Laser capture microdissection demonstrated endogenous c-Jun inhibited expression of apoptosis-inducing genes and reactive oxygen species (ROS)-reducing genes (MnSOD, catalase) [126]. In breast tumors c-Jun is expressed at the invading edge [127], suggesting a role for c-Jun in tumor migration. Consistent with this clinical observation, somatic deletion of the c-jun gene, conducted using floxed c-jun (c-junf/f) conditional knockout mice, showed c-Jun promoted cellular migration and invasion via increasing expression of CCL5 [128] and stem cell factor (SCF) [129], increasing c-Src abundance and suppressing Rock kinase signaling [130]. Increased transcriptional activity of AP-1 and increased c-Fos levels were noted to lead to acquired resistance to palbociclib and tamoxifen (96). Inhibiting AP-1 in combination with palbociclib and fulvestrant was ultimately more productive dual or mono-treatment (96). One c-Fos/AP-1 inhibitor (T-5224) has reached Stage II of trials [124].
Immune Mechanisms of CDKI therapy resistance. CDKi have significant and diverse effects on the breast cancer tumor immune microenvironment (reviewed in: [2]). Stromal cyclin D1 is increased in human breast cancer, correlating with poor outcome, and is known to augment the recruitment of macrophages into the breast cancer tumor microenvironment [131]. Treatment with immune checkpoint inhibitors is being explored for TNBC [132]. Compared with HER2-positive breast cancer and TNBC, ERα-positive breast cancer is not an immunogenic cancer type. Luminal breast cancers have the lowest level of tumor PD-L1 expression compared with basal-like and HER2-positive tumors. However, CDK4/6I-resistant breast cancer cells demonstrated upregulation of IFN-ɑ and IFN-β activity in immune-related signaling pathways [125,133]. DNA methyltransferase is an E2F target protein that promotes cytotoxic T-cell-mediated tumor inhibition when CDK4/6Is inhibit its activity [134]. CDK6 phosphorylates and thereby inhibits the nuclear factor of activated T-cell 4 (NFAT4), [135], reducing interleukin 2 (IL-2) levels. CDK4/6Is dephosphorylate NFAT4, enhancing its activity and increasing IL-2 levels [135]. CDKIs can potentiate anti-tumor immunity via augmenting the response to programmed cell death protein 1 (PD-1) blockade. Combining therapy with CDK4/6Is and PD-1 inhibitors may be a useful approach to overcome CDK4/6Is resistance.
7. Identifying Targeted Therapies for CDK4/6 Inhibitor-Resistant ER+ Breast Cancer
It has been proposed CDKI resistant cells have increased dependency upon the G2/M checkpoint [136]. WEE1 is an important G2 checkpoint regulator. In ER+ breast cancer cell models made resistant to ribociclib, the combination of AZD1775 (WEE1 inhibitor) and ribociclib inhibited proliferation in resistant cells [136]. Inhibiting WEE1 kinase decreased cell proliferation and increased G2/M arrest, apoptosis, and gamma H2AX levels (a marker for DNA double-strand breaks), in resistant cells compared with sensitive cells [136]. WEE1 kinase is thus a promising anticancer target in therapy-resistant ERα+ breast cancer [136].
8. Conclusions
Breast cancers, particularly metastatic HR+/HER2− advanced breast carcinomas, are currently treated with CDK4/6I [39,55,56]. However, tumor progression occurs frequently despite CDKi therapy. Recent studies, including the phase 3 PENELOPE-B trial, which did not meet the primary endpoint of improved invasive disease-free survival (iDFS) suggest there is much more to be understood about the role of CDK in breast cancer.
The variety of distinct genetic mechanisms giving rise to therapy resistance may, in part, reflect the intrinsic genomic instability of cyclin D1 overexpressing breast tumors [88] (Figure 3A). Cyclin D1 induced chromosomal instability (CIN) in murine mammary epithelium [29,88], and in other species [89]. Cyclin D1 is induced early in breast cancer and CIN is an early feature of tumorigenesis that may precede tumor suppressor loss [137,138]. Cyclin D1 [88] and cyclin E, are both capable of inducing CIN [139], and the induction of cyclin E in CDKI-resistant tumors may sustain CIN. Cyclin D1 induction of CIN is in mouse hepatocytes [140], lymphoid tumors [141] and bladder cancer [142]. The recent identification of drugs targeting CIN [143,144] may provide a rational basis for therapeutic substratification, supplementing with compounds targeting CIN in the luminal B subtype of breast cancer.
Multiple cell-cycle states have cell-cycle states have specific genetic and pharmaceutical vulnerabilities and a high degree of heterogeneity within tumor types [145]. RB loss for example, results in specific new vulnerabilities for therapeutic intervention, such as the use of the XIAP/CIAP inhibitor birinapant [146]. Furthermore, the combination of AURK and WEE1 inhibitors, yields synergistic cell death selectively in RB-deleted ERα+ breast cancer cells. WEE1 is targeted to inhibit the growth of breast cancer cells resistant to endocrine therapy and CDK4/6 inhibitors [136]. Although remarkable progress has been made in understanding the utility of CDKI for breast cancer,
Author Contributions
Conceptualization, R.P.; project administration, X.J.; writing—original draft preparation, R.P., M.A. (Mary Abdelmalak), R.S., M.A. (Mohammed Anwer), P.I., A.R. and M.A. (Myra Ahmed); writing—review and editing, R.P., X.J., A.W.A. and Y.D.; Supervision, R.P., X.J. and A.W.A. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
R.G.P. has ownership positions in the companies CytoDyn, EcoGenome, LightSeed, and StromaGenesis. Other authors declare no conflict of interest.
Funding Statement
This work was supported in part by an award from the National Institutes of Health (R01 CA132115, R21 CA235139-01 to R.G.P.), and the Breast Cancer Research Breakthrough Program (#W81XWH1810605) (R.G.P.) from US Department of Defense.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mayer E.L. Targeting breast cancer with CDK inhibitors. Curr. Oncol. Rep. 2015;17:443. doi: 10.1007/s11912-015-0443-3. [DOI] [PubMed] [Google Scholar]
- 2.Di Sante G., Page J., Jiao X., Nawab O., Cristofanilli M., Skordalakes E., Pestell R.G. Recent advances with cyclin-dependent kinase inhibitors: Therapeutic agents for breast cancer and their role in immuno-oncology. Expert Rev. Anticancer Ther. 2019;19:569–587. doi: 10.1080/14737140.2019.1615889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu H., Yu S., Liu Q., Yuan X., Mani S., Pestell R.G., Wu K. Recent advances of highly selective CDK4/6 inhibitors in breast cancer. J. Hematol. Oncol. 2017;10:97. doi: 10.1186/s13045-017-0467-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sherr C.J., Beach D., Shapiro G.I. Targeting CDK4 and CDK6: From Discovery to Therapy. Cancer Discov. 2016;6:353–367. doi: 10.1158/2159-8290.CD-15-0894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shupp A., Casimiro M.C., Pestell R.G. Biological functions of CDK5 and potential CDK5 targeted clinical treatments. Oncotarget. 2017;8:17373–17382. doi: 10.18632/oncotarget.14538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siegel R.L., Miller K.D., Jemal A. Cancer Statistics, 2017. CA Cancer J. Clin. 2017;67:7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 7.Cancer Genome Atlas N. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490:61–70. doi: 10.1038/nature11412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang G., Gormley M., Qiao J., Zhao Q., Wang M., Di Sante G., Deng S., Dong L., Pestell T., Ju X., et al. Cyclin D1-mediated microRNA expression signature predicts breast cancer outcome. Theranostics. 2018;8:2251–2263. doi: 10.7150/thno.23877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schreiber M., Kolbus A., Piu F., Szabowski A., Möhle-Steinlein U., Tian J., Karin M., Angel P., Wagner E.F. Control of cell cycle progression by c-Jun is p53 dependent. Genes Dev. 1999;13:607–619. doi: 10.1101/gad.13.5.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fouad Y.A., Aanei C. Revisiting the hallmarks of cancer. Am. J. Cancer Res. 2017;7:1016–1036. [PMC free article] [PubMed] [Google Scholar]
- 11.Csermely P., Korcsmaros T., Nussinov R. Intracellular and intercellular signaling networks in cancer initiation, development and precision anti-cancer therapy: RAS acts as contextual signaling hub. Semin. Cell Dev. Biol. 2016;58:55–59. doi: 10.1016/j.semcdb.2016.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gradishar W.J., Anderson B.O., Abraham J., Aft R., Agnese D., Allison K.H., Blair S.L., Burstein H.J., Dang C., Elias A.D., et al. Breast Cancer, Version 3.2020, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2020;18:452–478. doi: 10.6004/jnccn.2020.0016. [DOI] [PubMed] [Google Scholar]
- 13.Stracquadanio G., Wang X., Wallace M.D., Grawenda A.M., Zhang P., Hewitt J., Zeron-Medina J., Castro-Giner F., Tomlinson I.P., Goding C.R., et al. The importance of p53 pathway genetics in inherited and somatic cancer genomes. Nat. Rev. Cancer. 2016;16:251–265. doi: 10.1038/nrc.2016.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Upadhyaya C., Jiao X., Ashton A., Patel K., Kossenkov A.V., Pestell R.G. The G protein coupled receptor CCR5 in cancer. Adv. Cancer Res. 2020;145:29–47. doi: 10.1016/bs.acr.2019.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aine M., Boyaci C., Hartman J., Hakkinen J., Mitra S., Campos A.B., Nimeus E., Ehinger A., Vallon-Christersson J., Borg A., et al. Molecular analyses of triple-negative breast cancer in the young and elderly. Breast Cancer Res. 2021;23:20. doi: 10.1186/s13058-021-01392-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Y., Zhan Z., Yin X., Fu S., Deng X. Targeted Therapeutic Strategies for Triple-Negative Breast Cancer. Front. Oncol. 2021;11:731535. doi: 10.3389/fonc.2021.731535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gao J.J., Swain S.M. Luminal A Breast Cancer and Molecular Assays: A Review. Oncologist. 2018;23:556–565. doi: 10.1634/theoncologist.2017-0535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Y., Ma L. Efficacy of chemotherapy for lymph node-positive luminal A subtype breast cancer patients: An updated meta-analysis. World J. Surg. Oncol. 2020;18:316. doi: 10.1186/s12957-020-02089-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roulot A., Hequet D., Guinebretiere J.M., Vincent-Salomon A., Lerebours F., Dubot C., Rouzier R. Tumoral heterogeneity of breast cancer. Ann. Biol. Clin. 2016;74:653–660. doi: 10.1684/abc.2016.1192. [DOI] [PubMed] [Google Scholar]
- 20.Navale P., Bleiweiss I.J., Jaffer S., Nayak A. Evaluation of Biomarkers in Multiple Ipsilateral Synchronous Invasive Breast Carcinomas. Arch. Pathol. Lab. Med. 2019;143:190–196. doi: 10.5858/arpa.2017-0494-OA. [DOI] [PubMed] [Google Scholar]
- 21.Afghahi A., Timms K.M., Vinayak S., Jensen K.C., Kurian A.W., Carlson R.W., Chang P.J., Schackmann E., Hartman A.R., Ford J.M., et al. Tumor BRCA1 Reversion Mutation Arising during Neoadjuvant Platinum-Based Chemotherapy in Triple-Negative Breast Cancer Is Associated with Therapy Resistance. Clin. Cancer Res. 2017;23:3365–3370. doi: 10.1158/1078-0432.CCR-16-2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sun Y.S., Zhao Z., Yang Z.N., Xu F., Lu H.J., Zhu Z.Y., Shi W., Jiang J., Yao P.P., Zhu H.P. Risk Factors and Preventions of Breast Cancer. Int. J. Biol. Sci. 2017;13:1387–1397. doi: 10.7150/ijbs.21635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sobhani N., D’Angelo A., Pittacolo M., Roviello G., Miccoli A., Corona S.P., Bernocchi O., Generali D., Otto T. Updates on the CDK4/6 Inhibitory Strategy and Combinations in Breast Cancer. Cells. 2019;8:321. doi: 10.3390/cells8040321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haque M.M., Desai K.V. Pathways to Endocrine Therapy Resistance in Breast Cancer. Front. Endocrinol. 2019;10:573. doi: 10.3389/fendo.2019.00573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rani A., Stebbing J., Giamas G., Murphy J. Endocrine Resistance in Hormone Receptor Positive Breast Cancer-From Mechanism to Therapy. Front. Endocrinol. 2019;10:245. doi: 10.3389/fendo.2019.00245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goel S., DeCristo M.J., McAllister S.S., Zhao J.J. CDK4/6 Inhibition in Cancer: Beyond Cell Cycle Arrest. Trends Cell Biol. 2018;28:911–925. doi: 10.1016/j.tcb.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Di Sante G., Di Rocco A., Pupo C., Casimiro M.C., Pestell R.G. Hormone-induced DNA damage response and repair mediated by cyclin D1 in breast and prostate cancer. Oncotarget. 2017;8:81803–81812. doi: 10.18632/oncotarget.19413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sherr C.J., Roberts J.M. CDK inhibitors: Positive and negative regulators of G1-phase progression. Genes Dev. 1999;13:1501–1512. doi: 10.1101/gad.13.12.1501. [DOI] [PubMed] [Google Scholar]
- 29.Casimiro M.C., Di Sante G., Crosariol M., Loro E., Dampier W., Ertel A., Yu Z., Saria E.A., Papanikolaou A., Li Z., et al. Kinase-independent role of cyclin D1 in chromosomal instability and mammary tumorigenesis. Oncotarget. 2015;6:8525–8538. doi: 10.18632/oncotarget.3267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Piezzo M., Cocco S., Caputo R., Cianniello D., Gioia G.D., Lauro V.D., Fusco G., Martinelli C., Nuzzo F., Pensabene M., et al. Targeting Cell Cycle in Breast Cancer: CDK4/6 Inhibitors. Int. J. Mol. Sci. 2020;21:6479. doi: 10.3390/ijms21186479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson J., Thijssen B., McDermott U., Garnett M., Wessels L.F., Bernards R. Targeting the RB-E2F pathway in breast cancer. Oncogene. 2016;35:4829–4835. doi: 10.1038/onc.2016.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schoninger S.F., Blain S.W. The Ongoing Search for Biomarkers of CDK4/6 Inhibitor Responsiveness in Breast Cancer. Mol. Cancer Ther. 2020;19:3–12. doi: 10.1158/1535-7163.MCT-19-0253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spring L.M., Wander S.A., Zangardi M., Bardia A. CDK 4/6 Inhibitors in Breast Cancer: Current Controversies and Future Directions. Curr. Oncol. Rep. 2019;21:25. doi: 10.1007/s11912-019-0769-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DeMichele A., Cristofanilli M., Brufsky A., Liu X., Mardekian J., McRoy L., Layman R.M., Emir B., Torres M.A., Rugo H.S., et al. Comparative effectiveness of first-line palbociclib plus letrozole versus letrozole alone for HR+/HER2- metastatic breast cancer in US real-world clinical practice. Breast Cancer Res. 2021;23:37. doi: 10.1186/s13058-021-01409-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Finn R.S., Boer K., Bondarenko I., Patel R., Pinter T., Schmidt M., Shparyk Y.V., Thummala A., Voitko N., Bananis E., et al. Overall survival results from the randomized phase 2 study of palbociclib in combination with letrozole versus letrozole alone for first-line treatment of ER+/HER2- advanced breast cancer (PALOMA-1, TRIO-18) Breast Cancer Res. Treat. 2020;183:419–428. doi: 10.1007/s10549-020-05755-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilson F.R., Varu A., Mitra D., Cameron C., Iyer S. Systematic review and network meta-analysis comparing palbociclib with chemotherapy agents for the treatment of postmenopausal women with HR-positive and HER2-negative advanced/metastatic breast cancer. Breast Cancer Res. Treat. 2017;166:167–177. doi: 10.1007/s10549-017-4404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Finn R.S., Aleshin A., Slamon D.J. Targeting the cyclin-dependent kinases (CDK) 4/6 in estrogen receptor-positive breast cancers. Breast Cancer Res. 2016;18:17. doi: 10.1186/s13058-015-0661-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fry D.W., Harvey P.J., Keller P.R., Elliott W.L., Meade M., Trachet E., Albassam M., Zheng X., Leopold W.R., Pryer N.K., et al. Specific inhibition of cyclin-dependent kinase 4/6 by PD 0332991 and associated antitumor activity in human tumor xenografts. Mol. Cancer Ther. 2004;3:1427–1438. doi: 10.1158/1535-7163.1427.3.11. [DOI] [PubMed] [Google Scholar]
- 39.Hortobagyi G.N., Stemmer S.M., Burris H.A., Yap Y.S., Sonke G.S., Paluch-Shimon S., Campone M., Blackwell K.L., Andre F., Winer E.P., et al. Ribociclib as First-Line Therapy for HR-Positive, Advanced Breast Cancer. N. Engl. J. Med. 2016;375:1738–1748. doi: 10.1056/NEJMoa1609709. [DOI] [PubMed] [Google Scholar]
- 40.Tripathy D., Bardia A., Sellers W.R. Ribociclib (LEE011): Mechanism of Action and Clinical Impact of This Selective Cyclin-Dependent Kinase 4/6 Inhibitor in Various Solid Tumors. Clin. Cancer Res. 2017;23:3251–3262. doi: 10.1158/1078-0432.CCR-16-3157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Patnaik A., Rosen L.S., Tolaney S.M., Tolcher A.W., Goldman J.W., Gandhi L., Papadopoulos K.P., Beeram M., Rasco D.W., Hilton J.F., et al. Efficacy and Safety of Abemaciclib, an Inhibitor of CDK4 and CDK6, for Patients with Breast Cancer, Non-Small Cell Lung Cancer, and Other Solid Tumors. Cancer Discov. 2016;6:740–753. doi: 10.1158/2159-8290.CD-16-0095. [DOI] [PubMed] [Google Scholar]
- 42.Dickler M.N., Tolaney S.M., Rugo H.S., Cortes J., Dieras V., Patt D., Wildiers H., Hudis C.A., O’Shaughnessy J., Zamora E., et al. MONARCH 1, A Phase II Study of Abemaciclib, a CDK4 and CDK6 Inhibitor, as a Single Agent, in Patients with Refractory HR(+)/HER2(−) Metastatic Breast Cancer. Clin. Cancer Res. 2017;23:5218–5224. doi: 10.1158/1078-0432.CCR-17-0754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gelbert L.M., Cai S., Lin X., Sanchez-Martinez C., Del Prado M., Lallena M.J., Torres R., Ajamie R.T., Wishart G.N., Flack R.S., et al. Preclinical characterization of the CDK4/6 inhibitor LY2835219: In-vivo cell cycle-dependent/independent anti-tumor activities alone/in combination with gemcitabine. Investig. New Drugs. 2014;32:825–837. doi: 10.1007/s10637-014-0120-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ma C.X., Gao F., Luo J., Northfelt D.W., Goetz M., Forero A., Hoog J., Naughton M., Ademuyiwa F., Suresh R., et al. NeoPalAna: Neoadjuvant Palbociclib, a Cyclin-Dependent Kinase 4/6 Inhibitor, and Anastrozole for Clinical Stage 2 or 3 Estrogen Receptor-Positive Breast Cancer. Clin. Cancer Res. 2017;23:4055–4065. doi: 10.1158/1078-0432.CCR-16-3206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bisi J.E., Sorrentino J.A., Jordan J.L., Darr D.D., Roberts P.J., Tavares F.X., Strum J.C. Preclinical development of G1T38: A novel, potent and selective inhibitor of cyclin dependent kinases 4/6 for use as an oral antineoplastic in patients with CDK4/6 sensitive tumors. Oncotarget. 2017;8:42343–42358. doi: 10.18632/oncotarget.16216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lukasik P., Baranowska-Bosiacka I., Kulczycka K., Gutowska I. Inhibitors of Cyclin-Dependent Kinases: Types and Their Mechanism of Action. Int. J. Mol. Sci. 2021;22:2806. doi: 10.3390/ijms22062806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liao X., Hong Y., Mao Y., Chen N., Wang Q., Wang Z., Zhang L., Wang L., Shi C., Shi W., et al. SPH3643: A novel cyclin-dependent kinase 4/6 inhibitor with good anticancer efficacy and strong blood-brain barrier permeability. Cancer Sci. 2020;111:1761–1773. doi: 10.1111/cas.14367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen F., Liu C., Zhang J., Xu W., Zhang Y. Progress of CDK4/6 Inhibitor Palbociclib in the Treatment of Cancer. Anticancer Agents Med. Chem. 2018;18:1241–1251. doi: 10.2174/1871521409666170412123500. [DOI] [PubMed] [Google Scholar]
- 49.Roskoski R., Jr. Cyclin-dependent protein kinase inhibitors including palbociclib as anticancer drugs. Pharmacol. Res. 2016;107:249–275. doi: 10.1016/j.phrs.2016.03.012. [DOI] [PubMed] [Google Scholar]
- 50.Xu B., Li H., Zhang Q., Sun W., Yu Y., Li W., Wang S., Liao N., Shen P., Liu Y., et al. Pharmacokinetics, safety, activity, and biomarker analysis of palbociclib plus letrozole as first-line treatment for ER+/HER2− advanced breast cancer in Chinese women. Cancer Chemother. Pharmacol. 2021;88:131–141. doi: 10.1007/s00280-021-04263-9. [DOI] [PubMed] [Google Scholar]
- 51.Saha S., Dey S., Nath S. Steroid Hormone Receptors: Links with Cell Cycle Machinery and Breast Cancer Progression. Front. Oncol. 2021;11:620214. doi: 10.3389/fonc.2021.620214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Palumbo R., Torrisi R., Sottotetti F., Presti D., Rita Gambaro A., Collova E., Ferzi A., Agostinetto E., Maria Teragni C., Saltalamacchia G., et al. Patterns of treatment and outcome of palbociclib plus endocrine therapy in hormone receptor-positive/HER2 receptor-negative metastatic breast cancer: A real-world multicentre Italian study. Ther. Adv. Med. Oncol. 2021;13:1758835920987651. doi: 10.1177/1758835920987651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rossi V., Berchialla P., Giannarelli D., Nistico C., Ferretti G., Gasparro S., Russillo M., Catania G., Vigna L., Mancusi R.L., et al. Should All Patients with HR-Positive HER2-Negative Metastatic Breast Cancer Receive CDK 4/6 Inhibitor As First-Line Based Therapy? A Network Meta-Analysis of Data from the PALOMA 2, MONALEESA 2, MONALEESA 7, MONARCH 3, FALCON, SWOG and FACT Trials. Cancers. 2019;11:1661. doi: 10.3390/cancers11111661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Finn R.S., Crown J.P., Lang I., Boer K., Bondarenko I.M., Kulyk S.O., Ettl J., Patel R., Pinter T., Schmidt M., et al. The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): A randomised phase 2 study. Lancet Oncol. 2015;16:25–35. doi: 10.1016/S1470-2045(14)71159-3. [DOI] [PubMed] [Google Scholar]
- 55.Finn R.S., Martin M., Rugo H.S., Jones S., Im S.A., Gelmon K., Harbeck N., Lipatov O.N., Walshe J.M., Moulder S., et al. Palbociclib and Letrozole in Advanced Breast Cancer. N. Engl. J. Med. 2016;375:1925–1936. doi: 10.1056/NEJMoa1607303. [DOI] [PubMed] [Google Scholar]
- 56.Turner N.C., Ro J., Andre F., Loi S., Verma S., Iwata H., Harbeck N., Loibl S., Huang Bartlett C., Zhang K., et al. Palbociclib in Hormone-Receptor-Positive Advanced Breast Cancer. N. Engl. J. Med. 2015;373:209–219. doi: 10.1056/NEJMoa1505270. [DOI] [PubMed] [Google Scholar]
- 57.Loibl S., Turner N.C., Ro J., Cristofanilli M., Iwata H., Im S.A., Masuda N., Loi S., Andre F., Harbeck N., et al. Palbociclib Combined with Fulvestrant in Premenopausal Women with Advanced Breast Cancer and Prior Progression on Endocrine Therapy: PALOMA-3 Results. Oncologist. 2017;22:1028–1038. doi: 10.1634/theoncologist.2017-0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Turner N.C., Slamon D.J., Ro J., Bondarenko I., Im S.A., Masuda N., Colleoni M., DeMichele A., Loi S., Verma S., et al. Overall Survival with Palbociclib and Fulvestrant in Advanced Breast Cancer. N. Engl. J. Med. 2018;379:1926–1936. doi: 10.1056/NEJMoa1810527. [DOI] [PubMed] [Google Scholar]
- 59.Gnant M., Dueck A.C., Frantal S., Martin M., Burstein H.J., Greil R., Fox P., Wolff A.C., Chan A., Winer E.P., et al. Adjuvant Palbociclib for Early Breast Cancer: The PALLAS Trial Results (ABCSG-42/AFT-05/BIG-14-03) J. Clin. Oncol. 2022;40:282–293. doi: 10.1200/JCO.21.02554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Loibl S., Marme F., Martin M., Untch M., Bonnefoi H., Kim S.B., Bear H., McCarthy N., Mele Olive M., Gelmon K., et al. Palbociclib for Residual High-Risk Invasive HR-Positive and HER2-Negative Early Breast Cancer-The Penelope-B Trial. J. Clin. Oncol. 2021;39:1518–1530. doi: 10.1200/JCO.20.03639. [DOI] [PubMed] [Google Scholar]
- 61.Schettini F., Giudici F., Giuliano M., Cristofanilli M., Arpino G., Del Mastro L., Puglisi F., De Placido S., Paris I., De Placido P., et al. Overall Survival of CDK4/6-Inhibitor-Based Treatments in Clinically Relevant Subgroups of Metastatic Breast Cancer: Systematic Review and Meta-Analysis. J. Natl. Cancer Inst. 2020;112:1089–1097. doi: 10.1093/jnci/djaa071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cristofanilli M., Rugo H.S., Im S.A., Slamon D.J., Harbeck N., Bondarenko I., Masuda N., Colleoni M., DeMichele A., Loi S., et al. Overall Survival with Palbociclib and Fulvestrant in Women with HR+/HER2− ABC: Updated Exploratory Analyses of PALOMA-3, a Double-blind, Phase III Randomized Study. Clin. Cancer Res. 2022;28:3433–3442. doi: 10.1158/1078-0432.CCR-22-0305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Im S.A., Lu Y.S., Bardia A., Harbeck N., Colleoni M., Franke F., Chow L., Sohn J., Lee K.S., Campos-Gomez S., et al. Overall Survival with Ribociclib plus Endocrine Therapy in Breast Cancer. N. Engl. J. Med. 2019;381:307–316. doi: 10.1056/NEJMoa1903765. [DOI] [PubMed] [Google Scholar]
- 64.Slamon D.J., Neven P., Chia S., Fasching P.A., De Laurentiis M., Im S.A., Petrakova K., Bianchi G.V., Esteva F.J., Martin M., et al. Phase III Randomized Study of Ribociclib and Fulvestrant in Hormone Receptor-Positive, Human Epidermal Growth Factor Receptor 2-Negative Advanced Breast Cancer: MONALEESA-3. J. Clin. Oncol. 2018;36:2465–2472. doi: 10.1200/JCO.2018.78.9909. [DOI] [PubMed] [Google Scholar]
- 65.Slamon D.J., Neven P., Chia S., Fasching P.A., De Laurentiis M., Im S.A., Petrakova K., Bianchi G.V., Esteva F.J., Martin M., et al. Overall Survival with Ribociclib plus Fulvestrant in Advanced Breast Cancer. N. Engl. J. Med. 2020;382:514–524. doi: 10.1056/NEJMoa1911149. [DOI] [PubMed] [Google Scholar]
- 66.Sledge G.W., Jr., Toi M., Neven P., Sohn J., Inoue K., Pivot X., Burdaeva O., Okera M., Masuda N., Kaufman P.A., et al. MONARCH 2: Abemaciclib in Combination with Fulvestrant in Women with HR+/HER2- Advanced Breast Cancer Who Had Progressed While Receiving Endocrine Therapy. J. Clin. Oncol. 2017;35:2875–2884. doi: 10.1200/JCO.2017.73.7585. [DOI] [PubMed] [Google Scholar]
- 67.Sledge G.W., Jr., Toi M., Neven P., Sohn J., Inoue K., Pivot X., Burdaeva O., Okera M., Masuda N., Kaufman P.A., et al. The Effect of Abemaciclib Plus Fulvestrant on Overall Survival in Hormone Receptor-Positive, ERBB2-Negative Breast Cancer That Progressed on Endocrine Therapy-MONARCH 2: A Randomized Clinical Trial. JAMA Oncol. 2020;6:116–124. doi: 10.1001/jamaoncol.2019.4782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Goetz M.P., Toi M., Campone M., Sohn J., Paluch-Shimon S., Huober J., Park I.H., Tredan O., Chen S.C., Manso L., et al. MONARCH 3: Abemaciclib As Initial Therapy for Advanced Breast Cancer. J. Clin. Oncol. 2017;35:3638–3646. doi: 10.1200/JCO.2017.75.6155. [DOI] [PubMed] [Google Scholar]
- 69.Lam S.Y., Liu W.S.A., Lee C.-S. A Review of CDK4/6 Inhibitors. [(accessed on 12 April 2021)]. Available online: https://www.uspharmacist.com/article/a-review-of-cdk4-6-inhibitors.
- 70.Yip H.Y.K., Papa A. Signaling Pathways in Cancer: Therapeutic Targets, Combinatorial Treatments, and New Developments. Cells. 2021;10:659. doi: 10.3390/cells10030659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lee H.J., Lee W.K., Kang C.W., Ku C.R., Cho Y.H., Lee E.J. A selective cyclin-dependent kinase 4, 6 dual inhibitor, Ribociclib (LEE011) inhibits cell proliferation and induces apoptosis in aggressive thyroid cancer. Cancer Lett. 2018;417:131–140. doi: 10.1016/j.canlet.2017.12.037. [DOI] [PubMed] [Google Scholar]
- 72.Li T., Xiong Y., Wang Q., Chen F., Zeng Y., Yu X., Wang Y., Zhou F., Zhou Y. Ribociclib (LEE011) suppresses cell proliferation and induces apoptosis of MDA-MB-231 by inhibiting CDK4/6-cyclin D-Rb-E2F pathway. Artif. Cells Nanomed. Biotechnol. 2019;47:4001–4011. doi: 10.1080/21691401.2019.1670670. [DOI] [PubMed] [Google Scholar]
- 73.Konecny G.E. Cyclin-dependent kinase pathways as targets for women’s cancer treatment. Curr. Opin. Obstet. Gynecol. 2016;28:42–48. doi: 10.1097/GCO.0000000000000243. [DOI] [PubMed] [Google Scholar]
- 74.Kumarasamy V., Vail P., Nambiar R., Witkiewicz A.K., Knudsen E.S. Functional Determinants of Cell Cycle Plasticity and Sensitivity to CDK4/6 Inhibition. Cancer Res. 2021;81:1347–1360. doi: 10.1158/0008-5472.CAN-20-2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jansen V.M., Bhola N.E., Bauer J.A., Formisano L., Lee K.M., Hutchinson K.E., Witkiewicz A.K., Moore P.D., Estrada M.V., Sanchez V., et al. Kinome-Wide RNA Interference Screen Reveals a Role for PDK1 in Acquired Resistance to CDK4/6 Inhibition in ER-Positive Breast Cancer. Cancer Res. 2017;77:2488–2499. doi: 10.1158/0008-5472.CAN-16-2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen P., Lee N.V., Hu W., Xu M., Ferre R.A., Lam H., Bergqvist S., Solowiej J., Diehl W., He Y.A., et al. Spectrum and Degree of CDK Drug Interactions Predicts Clinical Performance. Mol. Cancer Ther. 2016;15:2273–2281. doi: 10.1158/1535-7163.MCT-16-0300. [DOI] [PubMed] [Google Scholar]
- 77.Raub T.J., Wishart G.N., Kulanthaivel P., Staton B.A., Ajamie R.T., Sawada G.A., Gelbert L.M., Shannon H.E., Sanchez-Martinez C., De Dios A. Brain Exposure of Two Selective Dual CDK4 and CDK6 Inhibitors and the Antitumor Activity of CDK4 and CDK6 Inhibition in Combination with Temozolomide in an Intracranial Glioblastoma Xenograft. Drug Metab. Dispos. 2015;43:1360–1371. doi: 10.1124/dmd.114.062745. [DOI] [PubMed] [Google Scholar]
- 78.Cersosimo R.J. Cyclin-dependent kinase 4/6 inhibitors for the management of advanced or metastatic breast cancer in women. Am. J. Health Syst. Pharm. 2019;76:1183–1202. doi: 10.1093/ajhp/zxz121. [DOI] [PubMed] [Google Scholar]
- 79.Knudsen E.S., Hutcheson J., Vail P., Witkiewicz A.K. Biological specificity of CDK4/6 inhibitors: Dose response relationship, in vivo signaling, and composite response signature. Oncotarget. 2017;8:43678–43691. doi: 10.18632/oncotarget.18435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Spring L.M., Zangardi M.L., Moy B., Bardia A. Clinical Management of Potential Toxicities and Drug Interactions Related to Cyclin-Dependent Kinase 4/6 Inhibitors in Breast Cancer: Practical Considerations and Recommendations. Oncologist. 2017;22:1039–1048. doi: 10.1634/theoncologist.2017-0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Braal C.L., Jongbloed E.M., Wilting S.M., Mathijssen R.H.J., Koolen S.L.W., Jager A. Inhibiting CDK4/6 in Breast Cancer with Palbociclib, Ribociclib, and Abemaciclib: Similarities and Differences. Drugs. 2021;81:317–331. doi: 10.1007/s40265-020-01461-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tate S.C., Burke T.F., Hartman D., Kulanthaivel P., Beckmann R.P., Cronier D.M. Optimising the combination dosing strategy of abemaciclib and vemurafenib in BRAF-mutated melanoma xenograft tumours. Br. J. Cancer. 2016;114:669–679. doi: 10.1038/bjc.2016.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Finn R.S., Crown J.P., Ettl J., Schmidt M., Bondarenko I.M., Lang I., Pinter T., Boer K., Patel R., Randolph S., et al. Efficacy and safety of palbociclib in combination with letrozole as first-line treatment of ER-positive, HER2-negative, advanced breast cancer: Expanded analyses of subgroups from the randomized pivotal trial PALOMA-1/TRIO-18. Breast Cancer Res. 2016;18:67. doi: 10.1186/s13058-016-0721-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Johnston S.R.D., Harbeck N., Hegg R., Toi M., Martin M., Shao Z.M., Zhang Q.Y., Martinez Rodriguez J.L., Campone M., Hamilton E., et al. Abemaciclib Combined with Endocrine Therapy for the Adjuvant Treatment of HR+, HER2-, Node-Positive, High-Risk, Early Breast Cancer (monarchE) J. Clin. Oncol. 2020;38:3987–3998. doi: 10.1200/JCO.20.02514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tamura K. Differences of cyclin-dependent kinase 4/6 inhibitor, palbociclib and abemaciclib, in breast cancer. Jpn. J. Clin. Oncol. 2019;49:993–998. doi: 10.1093/jjco/hyz151. [DOI] [PubMed] [Google Scholar]
- 86.Corona S.P., Generali D. Abemaciclib: A CDK4/6 inhibitor for the treatment of HR+/HER2- advanced breast cancer. Drug Des. Devel. Ther. 2018;12:321–330. doi: 10.2147/DDDT.S137783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Fasching P.A., Beck J.T., Chan A., De Laurentiis M., Esteva F.J., Jerusalem G., Neven P., Pivot X., Bianchi G.V., Martin M., et al. Ribociclib plus fulvestrant for advanced breast cancer: Health-related quality-of-life analyses from the MONALEESA-3 study. Breast. 2020;54:148–154. doi: 10.1016/j.breast.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Casimiro M.C., Crosariol M., Loro E., Ertel A., Yu Z., Dampier W., Saria E.A., Papanikolaou A., Stanek T.J., Li Z., et al. ChIP sequencing of cyclin D1 reveals a transcriptional role in chromosomal instability in mice. J. Clin. Investig. 2012;122:833–843. doi: 10.1172/JCI60256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Duffy S., Fam H.K., Wang Y.K., Styles E.B., Kim J.H., Ang J.S., Singh T., Larionov V., Shah S.P., Andrews B., et al. Overexpression screens identify conserved dosage chromosome instability genes in yeast and human cancer. Proc. Natl. Acad. Sci. USA. 2016;113:9967–9976. doi: 10.1073/pnas.1611839113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Caruso J.A., Duong M.T., Carey J.P.W., Hunt K.K., Keyomarsi K. Low-Molecular-Weight Cyclin E in Human Cancer: Cellular Consequences and Opportunities for Targeted Therapies. Cancer Res. 2018;78:5481–5491. doi: 10.1158/0008-5472.CAN-18-1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Guiley K.Z., Stevenson J.W., Lou K., Barkovich K.J., Kumarasamy V., Wijeratne T.U., Bunch K.L., Tripathi S., Knudsen E.S., Witkiewicz A.K., et al. p27 allosterically activates cyclin-dependent kinase 4 and antagonizes palbociclib inhibition. Science. 2019;366:eaaw2106. doi: 10.1126/science.aaw2106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gomatou G., Trontzas I., Ioannou S., Drizou M., Syrigos N., Kotteas E. Mechanisms of resistance to cyclin-dependent kinase 4/6 inhibitors. Mol. Biol. Rep. 2021;48:915–925. doi: 10.1007/s11033-020-06100-3. [DOI] [PubMed] [Google Scholar]
- 93.Herrera-Abreu M.T., Palafox M., Asghar U., Rivas M.A., Cutts R.J., Garcia-Murillas I., Pearson A., Guzman M., Rodriguez O., Grueso J., et al. Early Adaptation and Acquired Resistance to CDK4/6 Inhibition in Estrogen Receptor-Positive Breast Cancer. Cancer Res. 2016;76:2301–2313. doi: 10.1158/0008-5472.CAN-15-0728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.O’Leary B., Finn R.S., Turner N.C. Treating cancer with selective CDK4/6 inhibitors. Nat. Rev. Clin. Oncol. 2016;13:417–430. doi: 10.1038/nrclinonc.2016.26. [DOI] [PubMed] [Google Scholar]
- 95.Guarducci C., Bonechi M., Boccalini G., Benelli M., Risi E., Di Leo A., Malorni L., Migliaccio I. Mechanisms of Resistance to CDK4/6 Inhibitors in Breast Cancer and Potential Biomarkers of Response. Breast Care. 2017;12:304–308. doi: 10.1159/000484167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Malorni L., Piazza S., Ciani Y., Guarducci C., Bonechi M., Biagioni C., Hart C.D., Verardo R., Di Leo A., Migliaccio I. A gene expression signature of retinoblastoma loss-of-function is a predictive biomarker of resistance to palbociclib in breast cancer cell lines and is prognostic in patients with ER positive early breast cancer. Oncotarget. 2016;7:68012–68022. doi: 10.18632/oncotarget.12010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Condorelli R., Spring L., O’Shaughnessy J., Lacroix L., Bailleux C., Scott V., Dubois J., Nagy R.J., Lanman R.B., Iafrate A.J., et al. Polyclonal RB1 mutations and acquired resistance to CDK 4/6 inhibitors in patients with metastatic breast cancer. Ann. Oncol. 2018;29:640–645. doi: 10.1093/annonc/mdx784. [DOI] [PubMed] [Google Scholar]
- 98.Gao X., Leone G.W., Wang H. Cyclin D-CDK4/6 functions in cancer. Adv. Cancer Res. 2020;148:147–169. doi: 10.1016/bs.acr.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 99.Milioli H.H., Alexandrou S., Lim E., Caldon C.E. Cyclin E1 and cyclin E2 in ER + breast cancer: Prospects as biomarkers and therapeutic targets. Endocr. Relat. Cancer. 2020;27:R93–R112. doi: 10.1530/ERC-19-0501. [DOI] [PubMed] [Google Scholar]
- 100.Turner N.C., Liu Y., Zhu Z., Loi S., Colleoni M., Loibl S., DeMichele A., Harbeck N., Andre F., Bayar M.A., et al. Cyclin E1 Expression and Palbociclib Efficacy in Previously Treated Hormone Receptor-Positive Metastatic Breast Cancer. J. Clin. Oncol. 2019;37:1169–1178. doi: 10.1200/JCO.18.00925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Finn R.S., Liu Y., Zhu Z., Martin M., Rugo H.S., Dieras V., Im S.A., Gelmon K.A., Harbeck N., Lu D.R., et al. Biomarker Analyses of Response to Cyclin-Dependent Kinase 4/6 Inhibition and Endocrine Therapy in Women with Treatment-Naive Metastatic Breast Cancer. Clin. Cancer Res. 2020;26:110–121. doi: 10.1158/1078-0432.CCR-19-0751. [DOI] [PubMed] [Google Scholar]
- 102.O’Leary B., Cutts R.J., Liu Y., Hrebien S., Huang X., Fenwick K., Andre F., Loibl S., Loi S., Garcia-Murillas I., et al. The Genetic Landscape and Clonal Evolution of Breast Cancer Resistance to Palbociclib plus Fulvestrant in the PALOMA-3 Trial. Cancer Discov. 2018;8:1390–1403. doi: 10.1158/2159-8290.CD-18-0264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wei G., Wang Y., Zhang P., Lu J., Mao J.H. Evaluating the prognostic significance of FBXW7 expression level in human breast cancer by a meta-analysis of transcriptional profiles. J. Cancer Sci. Ther. 2012;4:299–305. doi: 10.4172/1948-5956.1000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Arnedos M., Bayar M.A., Cheaib B., Scott V., Bouakka I., Valent A., Adam J., Leroux-Kozal V., Marty V., Rapinat A., et al. Modulation of Rb phosphorylation and antiproliferative response to palbociclib: The preoperative-palbociclib (POP) randomized clinical trial. Ann. Oncol. 2018;29:1755–1762. doi: 10.1093/annonc/mdy202. [DOI] [PubMed] [Google Scholar]
- 105.Li Z., Zou W., Zhang J., Zhang Y., Xu Q., Li S., Chen C. Mechanisms of CDK4/6 Inhibitor Resistance in Luminal Breast Cancer. Front. Pharmacol. 2020;11:580251. doi: 10.3389/fphar.2020.580251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Pandey K., Park N., Park K.S., Hur J., Cho Y.B., Kang M., An H.J., Kim S., Hwang S., Moon Y.W. Combined CDK2 and CDK4/6 Inhibition Overcomes Palbociclib Resistance in Breast Cancer by Enhancing Senescence. Cancers. 2020;12:3566. doi: 10.3390/cancers12123566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sharifi M.N., Anandan A., Grogan P., O’Regan R.M. Therapy after cyclin-dependent kinase inhibition in metastatic hormone receptor-positive breast cancer: Resistance mechanisms and novel treatment strategies. Cancer. 2020;126:3400–3416. doi: 10.1002/cncr.32931. [DOI] [PubMed] [Google Scholar]
- 108.Hui R., Macmillan R.D., Kenny F.S., Musgrove E.A., Blamey R.W., Nicholson R.I., Robertson J.F., Sutherland R.L. INK4a gene expression and methylation in primary breast cancer: Overexpression of p16INK4a messenger RNA is a marker of poor prognosis. Clin. Cancer Res. 2000;6:2777–2787. [PubMed] [Google Scholar]
- 109.Lebok P., Roming M., Kluth M., Koop C., Özden C., Taskin B., Hussein K., Leveau A., Witzel I., Wölber L., et al. p16 overexpression and 9p21 deletion are linked to unfavorable tumor phenotype in breast cancer. Oncotarget. 2016;7:81322–81331. doi: 10.18632/oncotarget.13227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Herman J.G., Merlo A., Mao L., Lapidus R.G., Issa J.P., Davidson N.E., Sidransky D., Baylin S.B. Inactivation of the CDKN2/p16/MTS1 gene is frequently associated with aberrant DNA methylation in all common human cancers. Cancer Res. 1995;55:4525–4530. [PubMed] [Google Scholar]
- 111.D’Amico M., Wu K., Di Vizio D., Reutens A.T., Stahl M., Fu M., Albanese C., Russell R.G., Muller W.J., White M., et al. The role of Ink4a/Arf in ErbB2 mammary gland tumorigenesis. Cancer Res. 2003;63:3395–3402. [PubMed] [Google Scholar]
- 112.Hart C.D., Migliaccio I., Malorni L., Guarducci C., Biganzoli L., Di Leo A. Challenges in the management of advanced, ER-positive, HER2-negative breast cancer. Nat. Rev. Clin. Oncol. 2015;12:541–552. doi: 10.1038/nrclinonc.2015.99. [DOI] [PubMed] [Google Scholar]
- 113.Kollmann K., Heller G., Schneckenleithner C., Warsch W., Scheicher R., Ott R.G., Schafer M., Fajmann S., Schlederer M., Schiefer A.I., et al. A kinase-independent function of CDK6 links the cell cycle to tumor angiogenesis. Cancer Cell. 2013;24:167–181. doi: 10.1016/j.ccr.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Gacche R.N., Assaraf Y.G. Redundant angiogenic signaling and tumor drug resistance. Drug Resist. Updates. 2018;36:47–76. doi: 10.1016/j.drup.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 115.Yang C., Li Z., Bhatt T., Dickler M., Giri D., Scaltriti M., Baselga J., Rosen N., Chandarlapaty S. Acquired CDK6 amplification promotes breast cancer resistance to CDK4/6 inhibitors and loss of ER signaling and dependence. Oncogene. 2017;36:2255–2264. doi: 10.1038/onc.2016.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kwon N.H., Lee J.Y., Ryu Y.L., Kim C., Kong J., Oh S., Kang B.S., Ahn H.W., Ahn S.G., Jeong J., et al. Stabilization of Cyclin-Dependent Kinase 4 by Methionyl-tRNA Synthetase in p16(INK4a)-Negative Cancer. ACS Pharmacol. Transl. Sci. 2018;1:21–31. doi: 10.1021/acsptsci.8b00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Du Q., Guo X., Wang M., Li Y., Sun X., Li Q. The application and prospect of CDK4/6 inhibitors in malignant solid tumors. J. Hematol. Oncol. 2020;13:41. doi: 10.1186/s13045-020-00880-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Jafarzadeh M., Mousavizadeh K., Joghataei M.T., Bahremani M.H., Safa M., Asghari S.M. A Fibroblast Growth Factor Antagonist Peptide Inhibits Breast Cancer in BALB/c Mice. Open Life Sci. 2018;13:348–354. doi: 10.1515/biol-2018-0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sahores A., May M., Sequeira G.R., Fuentes C., Jacobsen B., Lanari C., Lamb C.A. Targeting FGFR with BGJ398 in Breast Cancer: Effect on Tumor Growth and Metastasis. Curr. Cancer Drug Targets. 2018;18:979–987. doi: 10.2174/1568009618666171214114706. [DOI] [PubMed] [Google Scholar]
- 120.Drago J.Z., Formisano L., Juric D., Niemierko A., Servetto A., Wander S.A., Spring L.M., Vidula N., Younger J., Peppercorn J., et al. FGFR1 Amplification Mediates Endocrine Resistance but Retains TORC Sensitivity in Metastatic Hormone Receptor-Positive (HR(+)) Breast Cancer. Clin. Cancer Res. 2019;25:6443–6451. doi: 10.1158/1078-0432.CCR-19-0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lv Q., Guan S., Zhu M., Huang H., Wu J., Dai X. FGFR1 Is Associated with Tamoxifen Resistance and Poor Prognosis of ER-Positive Breast Cancers by Suppressing ER Protein Expression. Technol. Cancer Res. Treat. 2021;20:15330338211004935. doi: 10.1177/15330338211004935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Takeshita T., Yamamoto Y., Yamamoto-Ibusuki M., Tomiguchi M., Sueta A., Murakami K., Iwase H. Clinical significance of plasma cell-free DNA mutations in PIK3CA, AKT1, and ESR1 gene according to treatment lines in ER-positive breast cancer. Mol. Cancer. 2018;17:67. doi: 10.1186/s12943-018-0808-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Michaloglou C., Crafter C., Siersbaek R., Delpuech O., Curwen J.O., Carnevalli L.S., Staniszewska A.D., Polanska U.M., Cheraghchi-Bashi A., Lawson M., et al. Combined Inhibition of mTOR and CDK4/6 Is Required for Optimal Blockade of E2F Function and Long-term Growth Inhibition in Estrogen Receptor-positive Breast Cancer. Mol. Cancer Ther. 2018;17:908–920. doi: 10.1158/1535-7163.MCT-17-0537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ye N., Ding Y., Wild C., Shen Q., Zhou J. Small molecule inhibitors targeting activator protein 1 (AP-1) J. Med. Chem. 2014;57:6930–6948. doi: 10.1021/jm5004733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Pandey K., An H.J., Kim S.K., Lee S.A., Kim S., Lim S.M., Kim G.M., Sohn J., Moon Y.W. Molecular mechanisms of resistance to CDK4/6 inhibitors in breast cancer: A review. Int. J. Cancer. 2019;145:1179–1188. doi: 10.1002/ijc.32020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Katiyar S., Casimiro M.C., Dettin L., Ju X., Wagner E.F., Tanaka H., Pestell R.G. C-jun inhibits mammary apoptosis in vivo. Mol. Biol. Cell. 2010;21:4264–4274. doi: 10.1091/mbc.e10-08-0705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Vleugel M.M., Greijer A.E., Bos R., van der Wall E., van Diest P.J. c-Jun activation is associated with proliferation and angiogenesis in invasive breast cancer. Hum. Pathol. 2006;37:668–674. doi: 10.1016/j.humpath.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 128.Jiao X., Katiyar S., Willmarth N.E., Liu M., Ma X., Flomenberg N., Lisanti M.P., Pestell R.G. c-Jun induces mammary epithelial cellular invasion and breast cancer stem cell expansion. J. Biol. Chem. 2010;285:8218–8226. doi: 10.1074/jbc.M110.100792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Katiyar S., Jiao X., Wagner E., Lisanti M.P., Pestell R.G. Somatic excision demonstrates that c-Jun induces cellular migration and invasion through induction of stem cell factor. Mol. Cell Biol. 2007;27:1356–1369. doi: 10.1128/MCB.01061-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Jiao X., Katiyar S., Liu M., Mueller S.C., Lisanti M.P., Li A., Pestell T.G., Wu K., Ju X., Li Z., et al. Disruption of c-Jun reduces cellular migration and invasion through inhibition of c-Src and hyperactivation of ROCK II kinase. Mol. Biol. Cell. 2008;19:1378–1390. doi: 10.1091/mbc.e07-08-0753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Pestell T.G., Jiao X., Kumar M., Peck A.R., Prisco M., Deng S., Li Z., Ertel A., Casimiro M.C., Ju X., et al. Stromal cyclin D1 promotes heterotypic immune signaling and breast cancer growth. Oncotarget. 2017;8:81754–81775. doi: 10.18632/oncotarget.19953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gaynor N., Crown J., Collins D.M. Immune checkpoint inhibitors: Key trials and an emerging role in breast cancer. Semin. Cancer Biol. 2022;79:44–57. doi: 10.1016/j.semcancer.2020.06.016. [DOI] [PubMed] [Google Scholar]
- 133.Demuth C., Andersen M.N., Jakobsen K.R., Madsen A.T., Sorensen B.S. Increased PD-L1 expression in erlotinib-resistant NSCLC cells with MET gene amplification is reversed upon MET-TKI treatment. Oncotarget. 2017;8:68221–68229. doi: 10.18632/oncotarget.19920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Goel S., DeCristo M.J., Watt A.C., BrinJones H., Sceneay J., Li B.B., Khan N., Ubellacker J.M., Xie S., Metzger-Filho O., et al. CDK4/6 inhibition triggers anti-tumour immunity. Nature. 2017;548:471–475. doi: 10.1038/nature23465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Deng J., Wang E.S., Jenkins R.W., Li S., Dries R., Yates K., Chhabra S., Huang W., Liu H., Aref A.R., et al. CDK4/6 Inhibition Augments Antitumor Immunity by Enhancing T-cell Activation. Cancer Discov. 2018;8:216–233. doi: 10.1158/2159-8290.CD-17-0915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Fallah Y., Demas D.M., Jin L., He W., Shajahan-Haq A.N. Targeting WEE1 Inhibits Growth of Breast Cancer Cells That Are Resistant to Endocrine Therapy and CDK4/6 Inhibitors. Front. Oncol. 2021;11:681530. doi: 10.3389/fonc.2021.681530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Shih I.M., Zhou W., Goodman S.N., Lengauer C., Kinzler K.W., Vogelstein B. Evidence that genetic instability occurs at an early stage of colorectal tumorigenesis. Cancer Res. 2001;61:818–822. [PubMed] [Google Scholar]
- 138.Kops G.J., Weaver B.A., Cleveland D.W. On the road to cancer: Aneuploidy and the mitotic checkpoint. Nat. Rev. Cancer. 2005;5:773–785. doi: 10.1038/nrc1714. [DOI] [PubMed] [Google Scholar]
- 139.Spruck C.H., Won K.A., Reed S.I. Deregulated cyclin E induces chromosome instability. Nature. 1999;401:297–300. doi: 10.1038/45836. [DOI] [PubMed] [Google Scholar]
- 140.Nelsen C.J., Kuriyama R., Hirsch B., Negron V.C., Lingle W.L., Goggin M.M., Stanley M.W., Albrecht J.H. Short term cyclin D1 overexpression induces centrosome amplification, mitotic spindle abnormalities, and aneuploidy. J. Biol. Chem. 2005;280:768–776. doi: 10.1074/jbc.M407105200. [DOI] [PubMed] [Google Scholar]
- 141.Aggarwal P., Lessie M.D., Lin D.I., Pontano L., Gladden A.B., Nuskey B., Goradia A., Wasik M.A., Klein-Szanto A.J., Rustgi A.K., et al. Nuclear accumulation of cyclin D1 during S phase inhibits Cul4-dependent Cdt1 proteolysis and triggers p53-dependent DNA rereplication. Genes Dev. 2007;21:2908–2922. doi: 10.1101/gad.1586007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Del Rey J., Prat E., Ponsa I., Lloreta J., Gelabert A., Algaba F., Camps J., Miro R. Centrosome clustering and cyclin D1 gene amplification in double minutes are common events in chromosomal unstable bladder tumors. BMC Cancer. 2010;10:280. doi: 10.1186/1471-2407-10-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Manchado E., Malumbres M. Targeting aneuploidy for cancer therapy. Cell. 2011;144:465–466. doi: 10.1016/j.cell.2011.01.037. [DOI] [PubMed] [Google Scholar]
- 144.Tang Y.C., Williams B.R., Siegel J.J., Amon A. Identification of aneuploidy-selective antiproliferation compounds. Cell. 2011;144:499–512. doi: 10.1016/j.cell.2011.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Knudsen E.S., Kumarasamy V., Nambiar R., Pearson J.D., Vail P., Rosenheck H., Wang J., Eng K., Bremner R., Schramek D., et al. CDK/cyclin dependencies define extreme cancer cell-cycle heterogeneity and collateral vulnerabilities. Cell Rep. 2022;38:110448. doi: 10.1016/j.celrep.2022.110448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kumarasamy V., Nambiar R., Wang J., Rosenheck H., Witkiewicz A.K., Knudsen E.S. RB loss determines selective resistance and novel vulnerabilities in ER-positive breast cancer models. Oncogene. 2022;41:3524–3538. doi: 10.1038/s41388-022-02362-2. [DOI] [PMC free article] [PubMed] [Google Scholar]