Abstract
Cancer remains the leading cause of death worldwide despite advances in treatment options for patients. As such, safe and effective therapeutics are required. Short peptides provide advantages to be used in cancer management due to their unique properties, amazing versatility, and progress in biotechnology to overcome peptide limitations. Several appealing peptide-based therapeutic strategies have been developed. Here, we provide an overview of peptide conjugates, the better equivalents of antibody-drug conjugates, as the next generation of drugs for required precise targeting, enhanced cellular permeability, improved drug selectivity, and reduced toxicity for the efficient treatment of cancers. We discuss the basic components of drug conjugates and their release action, including the release of cytotoxins from the linker. We also present peptide-drug conjugates under different stages of clinical development as well as regulatory and other challenges.
Keywords: short peptides, peptide-drug conjugates, drug delivery, cancer
1. Introduction
Cancer remains one of the major diseases with a high mortality rate despite advances in enhanced diagnostics and treatments. In women, the leading cancer is breast cancer, and in men, it is prostate cancer [1]. At the genetic level, cellular DNA is altered, leading to abnormal gene expression patterns [2]. Consequently, the effects of normal genes which control normal cellular functions such as growth and survival of the cell and invasion/motility, are accentuated [3]. Accumulation of mutations is the main mechanism of alteration. However, non-mutational(epigenetic) changes occur through the DNA methylation process, which is recognized as central to the process [4]. Primarily, cancer can be treated by various approaches including surgery, chemotherapy, radiotherapy, and immunotherapy [5]. Chemotherapeutic drugs generally have a low capacity to penetrate the parenchyma of solid tumors, hence, improvements are vital [6,7]. In addition, the overexpression of cancer associated antigens allows targeted approaches for drugs to be delivered as antibody–drug conjugates or peptide-drug conjugates [8,9], with minimal effects on healthy cells [10].
As we know, communication between cells and their cell surface proteins is required for their survival. In a single organism, numerous cells are connected to form an interactome. The interactome is an extensive network system composed of protein–protein interactions(PPIs) and an array of molecular interactions [11]. Hydrophobic effects hold hydrogen bonding and electrostatic forces together. PPIs networks are formed via the correlation between the human interactome and 130,000–600,000 PPIs. These PPIs are necessary for chemical biology and medicinal chemistry, and modulate signaling pathways and the cells’ systemic functions. Some cellular processes such as transcription, translation, transduction, and replication are catalyzed by PPIs [12]. In living cells, PPIs and proteins play a role in functional building blocks. Diseases such as cancer, infectious and neurodegenerative diseases, and disturbances in cell homeostasis can be caused by errors in a central node/hub of the PPIs network [13]. For the development of new drugs and novel diagnostics, PPIs are attractive targets and have efficient therapeutic potential [14,15].
Peptides, as constituents of proteins, are promising, safe, and effective anti-cancer therapeutics and are engaged in nearly all biological functions. Short peptides do not induce an undesired autoimmune response; they have high selectivity and specificity, are able to cross cell membranes, and penetrate tumors more efficiently [16,17,18,19,20,21,22,23,24,25,26,27]. Herein, applications of peptide-drug conjugates, their basic components, conjugation chemistry, release action, and different stages of their clinical development, regulatory procedures, and other challenges are presented.
2. Peptide-Drug Conjugates
In peptide-drug approaches for cancer, it is important to identify a target for cancer cells and a method to target the drug to such cells [28]. Peptides facilitate the penetration of drugs into the body. A chemical modification of peptide and protein drugs improves their enzymatic stability and/or membrane penetration of peptides and proteins [29]. Thus, much focus has been on tumor-targeting peptides. For example, cancer cells, and the tripeptide arginyl-glycyl-aspartic acid (RGD) express adhesion receptors, αvβ3, and αvβ5 integrins-peptides selectively bind to these integrins, allowing drug delivery [30]. In the parenchyma of the tumor, peptides show limited loading capacity but can deliver drugs, biologics, viruses, and nanoparticles to blood vessels successfully [31]. While the molecular targets in non-targeted approaches are not clear, natural and synthetic molecules are screened based on their ability to produce a sufficient phenotypic change in cells, including depletion of mitotic and motility defects and initiation of apoptosis. As such, the final hit compounds are selected based on efficacy to restrict the desired phenotypic properties with minimal side effects [32].
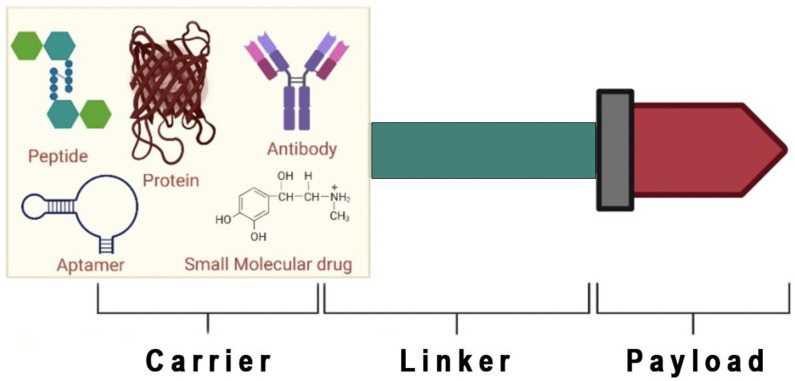
Currently, peptides are used for several diseases, representing a powerful class of medicines [16,22]. Short peptides are advantageous over biologics and small molecules, as they can interact with unknown targets, have a straightforward design, are relatively cheaper to synthesize, and have enhanced tissue penetration [33]. Peptides show excellent performance in transporting molecules to desired targets. Thus, such advantages lead to the identification of several naturally occurring and modified peptides, in addition to their combination with other systems, such as peptide–nanoparticles and peptide-drug conjugates [34]. Countless strategies are available for identifying peptides with anti-cancer activity for targeted and non-targeted approaches. The non-targeted approaches are evaluated from natural sources such as plant extracts, algae, toxins, animal venom, microbes, or screening of synthetic libraries. A targeted approach uses a direct evolution technique for rationally designed peptides (combined principles of biology with materials science) for selected targets [35,36]. Peptide-drug conjugates (PDCs) are composed of different components, which include a homing peptide or device, cytotoxic payload, and a linker that works synergistically to deliver cytotoxins to the targeted receptor on cancer cells (Figure 1) [37]. Each component’s role and mechanisms of action are important considerations when assembling PDCs [38].
Figure 1.
Schematic diagram of the components of peptide-drug conjugates (Created with Biorender.Com). Peptide, protein, antibody, small molecular drug, and aptamer is used as a carrier. If a peptide is used as a carrier, it is known as a peptide-drug conjugate.
An example of PDCs includes the use of gemcitabine, a chemotherapeutic drug. Gemcitabine is attached to a glutaryl linker by an ester bond, which is then attached to the peptide ([D-Lys6]-GnRH) (Gonadotropin hormone-releasing hormone (GnRH)) by an amide bond [37]. Notably, PDCs have much broader applications and advantages over antibody–drug conjugates. They are smaller, and consequently, have a better profile in terms of cellular uptake, stability, selectivity, immunogenicity, cellular permeability, tissue penetration, and lower manufacturing costs [39]. However, unlike antibody–drug conjugates, PDCs are not fast-paced in the market due to the poor intrinsic pharmacokinetic properties of the peptides [40]. PDCs have a shorter half-life of minutes, whilst antibody–drug conjugates have a half-life of days to weeks [41]. However, new methodologies are being developed to overcome such factors. Thus far, two PDCs are available in the market, (i) Lu177-dotatate (somatostatin as homing peptide conjugates with a radio-therapeutic agent) used for the treatment of gastroenteropancreatic neuroendocrine tumors [42], and (ii) melphalan flufenamide (melflufen), an allogeneic first-in-class peptide-drug conjugate, approved by the US Food and Drug Administration (USFDA) in 2021 for the treatment of multiple myeloma [42], with several others in various phases of development (Table 1).
Table 1.
Some peptide-drug conjugates against cancer in different developmental phases.
| Development Phase | Peptide-Drug-Conjugates | References | ||
|---|---|---|---|---|
| US FDA approved |
Lu177 dotatate | Peptide | Somatostatin analogue | [43,44,45,46] |
| Drug | Radio-therapeutic agent | |||
| Linker | Amide (chelating agent Lu177 chelates with meta-chelating agent DOTA) | |||
| Action | Somatostatin receptor-2 mediated delivery of nucleotide | |||
| Indication | Neuroendocrine cancer | |||
| Melflufen (melphalan flufenamide) amino peptide | Peptide | [47,48] | ||
| Drug | ||||
| Linker | Enzymatically cleaved linker | |||
| Action | Targets aminopeptidases. Rapidly releases alkylating agent into cancer cells | |||
| Indication | Multiple myeloma, ovarian cancer, breast cancer, acute myeloid leukemia, hematologic malignancies, and solid tumors | |||
| Clinical development | Paclitaxel with Angiopep-2 | Peptide | Angiopep-2 | [49,50] |
| Drug | Paclitaxel | |||
| Linker | Ester | |||
| Action | LPR-1 mediated brain uptake | |||
| Indication | Brain cancer | |||
| Paclitaxel with Poliglumex | Peptide | Poliglumex | [51,52,53] | |
| Drug | Paclitaxel | |||
| Linker | Ester | |||
| Action | Prolongs the exposure of the tumour to the active form of drug by minimizing the systemic enhancing the permeability of tumor vasculature | |||
| Indication | To treat a wide variety of cancers | |||
| Thapsigargin with Tetrapeptide | Peptide | Tetrapeptide | [52,53] | |
| Drug | Thapsigargin | |||
| Linker | Ester | |||
| Action | Tumor activation (extracellularly) | |||
| Indication | To treat a wide variety of cancers | |||
| Doxorubicin-GnRH | Peptide | GnRH | [54] | |
| Drug | Doxorubicin | |||
| Linker | Ester | |||
| Action | GnRH-mediated delivery to cancer cells | |||
| Indication | Ovarian and endometrial cancer | |||
| Maytansinoid with Bicyclic peptide | Peptide | Bicyclic peptide | [55] | |
| Drug | Maytansinoid | |||
| Linker | Disulfide | |||
| Action | Membrane type-1 matrixmetalloproteinase delivery to toxin material | |||
| Indication | Cancer | |||
| Doxorubicin-Tetrapeptide | Peptide | Tetrapeptide | [56,57] | |
| Drug | Doxorubicin | |||
| Linker | Amide | |||
| Action | Tumor activation (extracellularly) | |||
| Indication | Cancer | |||
| 123I-Glutamate urea lysine | Peptide | Glutamate urea lysine | [58] | |
| Drug | Radiotherapeutic agent (123I) | |||
| Linker | Amide | |||
| Action | Prostate-specific membrane antigen-mediated delivery of nucleotide | |||
| Indication | Specifically used for prostate cancer | |||
| 111In-DTPA-D-Phe-1-octreotide | Peptide | D-phe-1-octreotide | [59] | |
| Drug | 111In-DTPA | |||
| Linker | Amido bond | |||
| Action | Diagnosis of neuroendocrine tumors (somatostatin receptor-positive tumors) using SPECT or planar scintigraphy | |||
| Indication | Diagnostic Radiology | |||
| Aminopeptides N (CD13) peptide-hTumour Necrosis Factor (NGR-TNF) |
Peptide | NGR | [60] | |
| Drug | hTNFα | |||
| Linker | Amido bond | |||
| Action | Targets angiogenic tumor blood vessels (vasculature), through the NGR motif | |||
| Indication | Elapsed ovarian cancer | |||
| Paclitaxel-Poliglumex conjugate CT2103 (Opaxio™) |
Peptide | Poliglumex | [61] | |
| Drug | Paclitaxel (chemotherapeutic drug) | |||
| Linker | Ester bond | |||
| Action | Paclitaxel therapeutic index is restricted due to poor tumor exposure and high systemic exposure. Paclitaxel poliglumex (PPX) combination increases tumor exposure by taking advantage of tumor tissue’s hyperpermeable vasculature and reduced lymphatic clearance. The release of paclitaxel is dependent, at least in part, on PPX metabolism by the lysosomal protease cathepsin B, which is increased in many tumor types. | |||
| Indication | Metastatic breast cancer | |||
| Paclitaxel linked to brain delivery vector angiopep-2 (ANG1005) |
Peptide | Angiopep-2 | [62] | |
| Drug | Paclitaxel | |||
| Linker | Ester bond | |||
| Action | Paclitaxel is blocked from attaining its target in malignant gliomas by the presence of the efflux pump P-glycoprotein (P-gp) at the blood-brain barrier. Angiopep-2 peptide vectors have the potential to improve their efficacy in the treatment of brain tumors. | |||
| Indication | Recurrent malignant glioma | |||
| Natural luteinizing hormone-releasing hormone (LHRH) ligand linked to a cationic membrane disrupting peptide (EP-100) |
Peptide | LHRH | [63] | |
| Drug | CLIP71 | |||
| Linker | Amino bond | |||
| Action | EP-100 interacts with the negatively charged membrane upon accumulation on the cell membrane via LHRH receptor targeting, resulting in lysis and cell death. | |||
| Indication | LHRH-receptor-expressing solid tumors | |||
| Preclinical development | Gemcitabine conjugation to an integrin binding knotting peptide-Ecbellium elaterium trypsin inhibitor (EETI)-2.5Z, via Val-Ala-PABC linker (EETI-2.5Z-Val-Ala-PABC-genciabine) |
Peptide | Knotting peptide | [64,65] |
| Drug | Gemcitabine | |||
| Linker | Amide, ester, cathepsin-B, carbamate | |||
| Action | DNA replication block assisted by integrin knotting peptide that specifically allows tumor delivery | |||
| Indication | Breast cancer, ovarian cancer, geo-blastoma, and pancreatic cancer | |||
| DOTA (bifunctional chelating ligand; 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid) linked to bombesin (BBN) (DOTA-GABA-BBN) |
Peptide | Bombesin 7–14, from frog skin | [66] | |
| Drug | DOTA | |||
| Linker | g-aminobutyric acid | |||
| Action | Bombesin is overexpressed on cancer cells. DOTA-GABA-BBN is a specific radioligand for gastrin-releasing peptide-positive tumors. Used in targeted PET imaging |
|||
| Indication | Used for diagnostic radiology | |||
| MTX-YTA2 | Peptide | Acetyl-YTAIAWVKAFIRKLRK -amide |
[67] | |
| Drug | Methotrexate (MTX) | |||
| Linker | Amino bond | |||
| Action | Cell-penetrating peptide (YTA2) conjugated to MTX as therapeutic for drug-resistant cancer cells | |||
| Indication | Breast cancer | |||
Another example of a PDC involves the 12-mer exacyclic mimetic peptide(H-FCDGFYACYKDV-OH) of the heavy chain 3 of trastuzumab (a recombinant anti-human epidermal growth factor 2 (HER2) receptor antibody) known as AHNP, which shows high affinity and similar potency as trastuzumab regarding binding affinity (REF). In addition, AHNP linked to the chemotherapeutic drug, doxorubicin, forms an ester bond with the matrix metalloproteinase (MMP-2) cleavage (which is linked to AHNP via an amide bond) [68]. In addition, via carbamate linkage of lysine amino groups between the peptide and drugs, several PDCs targeting somatostatin receptors (SSTR) and other receptors have been designed [69]. However, PDCs with ester linkers have been shown to release the drug faster compared to PDCs with a carbamate linkage [43].
3. Components of Peptide-Drug Conjugates
Several approaches have been explored for the selective delivery of effector molecules to cancer cells. PDCs are composed of three main components, including homing peptide, linker, and payload (Figure 1).
3.1. Homing Peptide
The first component of PDCs is the carrier or the homing peptide, which eases tumor targeting [40]. Several biologics, including antibodies, proteins, peptides, and small molecules have been investigated in addition to aptamers to facilitate tumor selectivity [70]. The homing peptide is a selected peptide that has a specificity for targeting molecules to specific protein receptors expressed on cancer cells, and often displays high affinity to the target receptor site [71]. Thus, the homing peptide directs the PDC at the desired targeted cell or tissue (as they have enhanced binding affinity for targets) and limits off-target delivery. The binding affinity of homing peptides is an important feature, and it depends on the secondary structure of homing devices such as random coil, β-sheet, and α-helix. This allows greater binding affinity through enhanced stabilization of the secondary structure of the homing peptide [72]. However, this approach has certain disadvantages, such as chemical instability, degradation by enzymes, and fast renal clearance. However, it is possible to gain control over such types of drawbacks by developing modifications of the peptide such as cyclization techniques or non-natural amino acids. Cyclization is achieved either via side chain to side chain, head-tail chain to side chain, or head-to-tail modifications, which are more stable and active compared to their linear counterparts, as seen in various studies [73,74,75,76,77,78]. To produce peptide-drug conjugates, several homing peptides have been used (Table 2).
Table 2.
Homing peptides used for the development of Peptide-drug-conjugates.
| Homing Peptide | Receptor Site [71,73,73,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93] |
|---|---|
| Somatostatin (SST) | Somatostatin receptor |
| Gonadotropin-releasing hormone (GnRH) | Receptor version of hormone-GnRH-R |
| Angiopep-2 | Low-density lipoprotein receptor-related protein (LRP-1) |
| Epidermal growth factor (EGF) | Epidermal growth factor receptor (EGFR): HER1, HER2, HER3, HER4 |
| REG | Integrin αvβ3 receptor |
| iREG | Integrin αvβ3/αvβ5 receptor |
| GE11 | Epidermal growth factor receptor (EGFR): ErbB1 |
| D-Lys6-LHRH | Luteinizing hormone-releasing hormone receptor (LHRH-R) |
| Octreotide | Somatostatin receptor 2/5 (SSTR2/5) |
Peptides can be used as therapeutic agents and as drug carriers [79], but the criteria for action and selection of peptides are quite different. Herein, we discuss all the aspects of peptides. They are used in biotechnology for diagnostic and therapeutic purposes [80]. As an example, calcitonin gene-related peptide is used for migraines, bombesin is used in prostate cancer, somatropin pegol is used in growth hormone deficiency, and BPI-3016 is used in type-2 diabetes as a therapeutic agent [81]. In recent years, peptides have demonstrated improved binding affinity and specificity for challenging binding interfaces due to their smaller size and balance of conformational rigidity and flexibility. There needs to be an understanding and characterization of peptide–protein recognition mechanisms to develop new peptide-based strategies to interfere with endogenous protein interactions or to improve the affinity and specificity of existing approaches. It has been shown that peptide therapeutics can be rationally developed using computational-aided rational design methods. As such, over 60 peptides in clinical trials have been approved worldwide [82]. Delivering biologically active molecules into cells with peptide carriers is one of the most promising approaches. In addition, cancer and infectious diseases could benefit from protein/peptide delivery for efficient and safer vaccines and therapies, as has been shown in models of cancer and multiple sclerosis (REF) [94,95,96,97,98,99]. In recent years, PTD-mediated transfection has demonstrated that future treatments can benefit from ‘protein therapy’ [100]. The blood-brain barrier limits the transport of most therapeutic compounds to the brain in several conditions, such as brain cancers and other neurological disorders. It was previously shown that a synthetic peptide carrier, K16ApoE, resembled the ligand-receptor system that enabled protein transport into the brain. Cisplatin, methotrexate, and other drugs can be delivered non-covalently to the brain with the peptide carrier, by generating transient blood brain barrier permeability [83]. In addition, the interaction between S protein and hACE2 can be potently inhibited by several peptide-based inhibitors, which can be useful for the treatment of COVID-19(REF) [101,102].
In the same way, lactoferrin, an antiviral peptide, is an important drug candidate against COVID-19. Phase II human clinical trials are in progress for RhACE2-APN01, a drug candidate based on recombinant hACE2 peptide. Peptide-based therapeutics for the treatment of COVID-19 include SBP1; Spikeplug target SARS-CoV-2 RBD, EK1; EK1C4; IBP01 and 2019-nCoV-HR1P & HR2P target protein-HR1 [84].
3.2. Linker
In peptide-drug conjugations, linkers play a crucial role by linking small drug molecules to peptides and maintaining the structural integrity of PDCs [103]. Based on the mechanisms of PDC, the linker should be selected based on its stability within the circulation to prevent non-specific and premature releasing of the drug at receptor sites, which may result in adverse effects [104]. As such, several conditions are considered when determining which linker to use including pH, enzyme responsiveness, redox responsiveness, and non-covalent linkers (Figure 2) [105].
Figure 2.
Different types of polypeptide-drug linkers commonly used in the rational design of poly peptide-drug conjugates (Adopted under CC BY 4.0 from [103]). In the figure, white bubble indicates PDCs. The green triangle is a therapeutic agent. The red colored line indicates the linker and the green colored ribbon type structure indicates polypeptide. In the linker, different types of linkers are discussed.
3.2.1. pH-Responsive Linkers
pH-responsive linkers are the most widely used, and low pH of the tumor microenvironment, intracellular vesicles and organelles, and inflammatory sites play a central role in the release of drugs from PDCs [106]. pH-sensitive linkers which form imine, cis-aconityl, hydrazone, and ketal/acetal bonds are used for drug conjugations [107]. Due to their straightforward reaction between carbonyl groups (aldehydes or ketones) and amines or hydrazides under mild acid conditions, amine and hydrazone linkers are most used. Materials that are capable of releasing their payloads in acidic conditions, such as tumors or infection sites, have been designed using various chemical functionalities including acetal, ortho ester, amine, and hydrazone. Hydrazone linkages are important synthons for a variety of transformations, and they have acquired prominence in pharmaceutical sciences due to their many biological and clinical uses [108]. A series of six molecules comprising 18 different molecules are designed, synthesized, and studied to investigate the effect of structural differences on the degradation kinetics of acetal- and ketal-based linkers [109]. Thus, PDCs have some limitations for targeted drug delivery as the difference [110] in pH between normal and tumor cells may not be sufficient [106].
3.2.2. Enzyme Responsive Linkers
In the progressive early stages of diseases such as cancer, proteolytic enzymes including proteases can affect their role [111]. This involves the progression of the disease by cleavage of biologically important molecules into the cellular microenvironment [112]. Further, their stability is enhanced by adding several alkyl groups such as methyl, adjacent to disulfide bonds. As an example, cathepsin-B or lysosomal cysteine proteases papain regulate the adaptive and innate immune systems, which are unregulated in the tumor microenvironment of some types of cancers [113]. Non-invasive protease activity imaging in vivo with protease-specific cleavable agents offers unique possibilities for the monitoring of disease states. A polymeric carrier with a fluorescent reporter is used to develop protease-sensitive activatable ligands [114,115,116].
3.2.3. Redox Responsive Linkers
In some PDCs, redox sensitivity is provided by the presence of disulfide-containing linkers. The stability of disulfide linkers can be enhanced by adding electron-donating groups such as methyl groups, while the introduction of aromatic groups can lead to bond dissociation [117]. When glutathione levels increase to 1–10 mM/L, it reduces in the cytosol of tumor cells, whereas in the plasma, glutathione is stable at 5 µM/L [118]. This strategy relies on the higher concentration of reducing molecules such as glutathione in the cytoplasm (1–10 mM/L) [119]. In tumor cells, glutathione levels are four times higher than that of normal cells, enabling the selection of an antitumorigenic PDC linker [120]. Diselenide bonds have recently developed as a novel reduction-sensitive linkage. However, its reduced sensitivity has not been observed systemically [121].
3.2.4. Non-Covalent Interaction Linkers
A strong ionic bond between a carboxylic group and metal is widely employed in nanomedicines. Some platinum-based PDCs are in clinical trials in which the metal complexation method is used as the alkylating agent [122]. Metal complexation by using PDCs is used as a potent anti-cancer therapy as a result of their unique properties such as redox activity, variable coordination modes, and reactivity toward organic substrates; metal complexes have attracted a great deal of attention as cancer therapy agents, and have shown to be effective in apoptosis-inducing phase lock loop-based conjugates (removes differences in frequency and phase among input and output signals) [123]. The use of PDCs as metal complexation catalysts is a potent anti-cancer therapy for PLL-based conjugates that induce apoptosis. The simultaneous action of this example suppressed cell migration and invasion on intracellular Ca2+ homeostasis perturbation and synergetic apoptosis [124]. As a result, metal complexation with PDCs, RadProtect® (in phase I clinical evaluation, also known as CC-AMI, developed by Original BioMedicals, Taipei, Taiwan) has also been used to treat acute radiation syndrome. PEG-b-PGA micelles connected by ferrous ions chelate the -COOH and -SPO3H of amifostine, releasing the drug into the bloodstream with controlled release [125,126]. In addition, the linker’s fate factor (denotes a substance’s total persistence) is considered to demonstrate the drug metabolism effects on the body, and hence resulting toxicity is formed [127]. An ideal linker for selective killing would release the drug only after the intracellular uptake of the conjugates via cancer cells [37]. Upon decomposition of PDCs, cancer cells absorb whatever remains (intact PDCs) for intracellular delivery of the drug. In the synthesis process of drug conjugates, linkers form two chemical bonds: one bond is formed between the peptide and the linker, and another bond is formed between the drug and the linker [128]. A non-cleavable linker is triggered by environmental changes of diseased tissue stimuli such as tripeptide glutathione, or other enzymes present in the tumor microenvironment, and change in pH [103,129].
For improvement in the efficacy of PDCs, the chemistry of the linker plays an important role. Non-cleavable linkers are less preferred over cleavable ones, even though they are more stable [130]. Nevertheless, the linkers should specifically and efficiently release the drug once the targets activate the pharmacological effect (Table 3). Thus, it is obvious to study their chemical effects in the plasma for desirable choice of linkers according to peptide and drug molecules. For example, hydrazones are mainly unstable under acidic conditions (pH 4.5–6.0), and in conditions greater than pH 6.0 the linker is not completely stable in the plasma [131]. Esters are commonly preferred for the conjugation of PDCs due to their ability to be cleaved by the esterase enzyme under acidic conditions. Even though esters do not provide much stability in the plasma, they are still used as a medicinal agent [131]. Carbamates also function similarly to that of esters with relatively higher stability in the plasma. Amides are preferred for the extended duration of action along with the increased therapeutic index due to the release of an active form of conjugated small molecules in the biological system, as amide bonds help and facilitate them in the lysosome with the help of multiple protease enzymes [103,131,132]. In addition, dipeptide linkers are considered, such as Val-Cit and related derivatives if there is no cleavage, as they are cleaved by intracellular proteases [133]. Similarly, tripeptides such as Glu-Val-Cit have been utilized to further enhance the efficacy and stability over dipeptide linkers. Initially, the stability and efficacy of dipeptides and tripeptides were evaluated in mice. However, it was noted that peptide linkers had higher stability in human plasma compared to mouse plasma. This is due to the cleavage of extracellular carboxyl-esterase enzymes in mice, and translation errors may occur when comparing preclinical and clinical data. Thus, the amide bond linker confers suitable plasma stability [133,134]. β-glucuronide is another example of a cleavable linker and has a high advantage of easy drug release, aqueous solubility, and high serum stability [135]. Disulfide linkers are also involved in the formation of peptide conjugates with higher plasma stability. Thus, to achieve the appropriate targeted delivery, hydrazones, esters, carbamates, amides, dipeptides, tripeptides, β-glucuronide, and disulfide bonds provide a diverse set of linkers that are preferably utilized in the development of PDCs (Table 3) [136].
Table 3.
Different types of linkers used in peptide-drug conjugates.
| Type of Linker | Name | Comment |
|---|---|---|
| pH-responsive | Acetal/Ketal bond | An acidic environment in endosomes |
| Hydrazone bond | ||
| Vinyl ether bond | ||
| Enzyme responsive | Gly-Phe-Leu-Gly | Cathepsin B |
| Phe-Lys | ||
| Val-Citrulline | ||
| Redox responsive | Disulfide bond | Reduction in endosomes by glutathione |
| Non-covalent interaction | Amido bond | The potential of modifying the particle’s surface peptide layer to stabilize the particle for systemic in vivo injection or for targeting opens fascinating possibilities for improving cargo trafficking |
| Carbon chain | ||
| Ether bond |
3.3. Payloads
The main and third component of PDCs is the drug itself, which can persuade a variety of biological functions. However, in the treatment of cancer, radionuclides and cytotoxic molecules are widely used [137].
3.3.1. Radionuclides
Radionuclides are the second most important type of payload in PDCs. It can be used for two main purposes, that of diagnosis or in therapeutic settings. Various types of PDCs such as [18F] Galacto-RGD, 68Ga-labeled bombesin analog (RM2) and 99mTc-labeled [Phe7, Pro34] NPY have been investigated under clinical settings as molecular imaging agents. Most commonly, indium-111(111In), lutetium-177(177Lu), and yttrium-90(90Y) are used as radionuclides [138].
3.3.2. Chemotherapeutic Agents
Based on the general mechanism of action, cytotoxic agents are classified as the first group of cytotoxic agents which interfere with the DNA protein complexes/cellular DNA and lead to apoptosis. Anthracyclines such as daunorubicin (DAU) or doxorubicin (DOX) and camptothecin (CPT) are widely used in PDCs. The second group of agents act by inhibiting the biosynthesis of DNA. It is a class of antimetabolites. Folate derivative methotrexate (MTX), nucleoside analog of deoxycytidine, and gemcitabine are widely used. The third group of agents act on microtubules with anti-mitotic abilities. Vinka alkaloid analogs and paclitaxel (PTX) belong to this class of agents [138].
There are thousands of anti-tumor agents available and a wide range of cytotoxic drugs on the market, and each of them come with different limitations including poor pharmacokinetic properties and generation of toxicity to nearby healthy cells whilst targeting an affected one [139]. To overcome these unwanted effects, cytotoxins are attached to peptides with the reduced dose, since peptides provide a specific targeted delivery, and hence the greater proportion of the drug being reached to the specific target site. There are certain criteria for the selection of suitable payloads with respect to PDCs including potency, release through a linker, and stability within the circulation. The payloads are usually chosen with lower IC50 within the nM range due to some cytotoxic agents being more toxic, and as such, picometer range is used. The common payloads which are used include daunorubicin, doxorubicin, taxol, and Gemzar [40,140].
4. Delivery of Peptide–Drug-Conjugates to the Desired Targeted Tissue
When delivering drugs to cancer cells, the primary goal is to minimize their impact on healthy tissues and ensure that a sufficient amount of the drug reaches the target. This is achieved using two main approaches, both of which aim to alter the pharmacokinetic properties of the drug [141]; (i) use of a delivery vehicle such as nanoparticles, which encapsulate the drug and can dictate its biodistribution through its physicochemical properties, and (ii) to covalently modify the drug with a small moiety that masks the drug’s bioactivity or limits its pharmacokinetic properties [43]. Using peptides, PDCs can have a great degree of functionality, as they can be controlled physiochemically and actively target a particular receptor on cancer cells [142]. The peptides in PDCs are generally short in length and biodegradable, to avoid unwanted immune reactions [143]. By combining different amino acids, a wide variety of PDCs are easily prepared. The sequence controls both the hydrophobicity and the ionization of the conjugate, which affects bioavailability in vitro and in vivo [144].
The physiological action of PDCs depends on several factors including the homing peptide and the linker. Cancer-targeted therapeutic approaches rely on cell surface receptors because they provide specific targeting properties for tumors. To achieve sufficient selectivity, cell surface receptor overexpression is required. It is usually desirable to have a normal cell-to-tumor expression ratio above 1:3 [145]. As discussed, the linker prevents premature release or unwanted release of cytotoxins that can be responsible for the adverse effects. Thus, it is important to gain control over the release of cytotoxins from the linker [146]. A cleavable linker should be cleaved in the presence of a suitable pH or enzymes. Two alternates are available; in the first approach, PDCs follow a similar kind of action to that of antibody-drug conjugates such as the first internalization and then release of a cytotoxin from the linker by cleavage, while the second approach includes cleavage release of a cytotoxin outside the cell followed by internalization [147]. Homing peptides play an important role in targeting the PDCs at specific receptors as they can be a non-penetrating or penetrating peptide. Generally, non-penetrating homing peptides bind with the targeted receptor site and initiate receptor-mediated internalization and endocytosis [148]. PDCs are transported from early endosomes to late endosomes and enter lysosomes, where the pH is low and which contain specific enzymes, where the PDC is cleaved and releases the cytotoxin [132]. As a result, peptide-binding receptors are potential drug carriers with tumor-specific properties due to the properties associated with their activating peptide ligands. Additionally, small molecules or antibodies can also be used to target peptide-binding receptors. As such, the drug compound can be covalently linked to the receptor-binding molecule, making it possible to deliver the drug in a targeted manner. Furthermore, the main demerits are fast renal clearance and poor stability of PDCs in circulation [149]. To overcome these drawbacks, gold nanoparticles and conjugation to antibody Fc or albumin have been used together with the PDCs due to their longer circulation half-life, reliable physicochemical properties, and safety properties which enhance the overall stability of PDCs [150]. One of the greatest advantages of PDCs is that they may overcome/bypass the development of drug resistance in cancer cells. As such, branched cell penetration of peptide-drug conjugates have been studied to overcome drug resistance. Many valuable anti-cancer drugs have undesirable side effects in the current clinical setting, including drug resistance and inefficient cellular uptake. There are several strategies for overcoming limitations in therapeutic research, such as the construction of high-affinity multivalent ligands for drug delivery or selective tumor targeting of chemotherapeutics [151]. Cell-penetrating peptides are particularly effective delivery vehicles, and conjugates of these peptides with anti-cancer medicines have been used to improve cellular uptake. They concluded that in comparison to their linear analogue and doxorubicin, new branched doxorubicin–oligoarginine conjugates demonstrated superior efficacy against wild-type and resistant neuroblastoma tumor cell lines. For the first time, these novel conjugates confirm the effect of high local concentrations on cellular uptake and cytotoxicity in resistant cells [152]. Radiotherapy is mostly used as a treatment of cancer, but it increases normal tissue damage, so it is conjugated with peptides. Peptides linked to radiosensitizing monomethyl auristatin E selectively stimulates CD8+ T cells and are reliant on long-term tumor control and immunological memory in irradiated cells. Monomethyl auristatin-E sculpts the tumor immune infiltration in conjunction with ionizing radiation to enhance immune checkpoint inhibition. This is how drug resistance is overcome by PDCs, which will be beneficial for treating trimodal cancers [153]. Efficiency of PDCs depends on the targeted receptor, the pathway of receptor-mediated-endocytosis, and intracellular trafficking. For the treatment of cancer, several cancer-specific receptors or markers are targeted by PDCs such as the integrin (αvβ3) receptor for ovarian cancer, EGFR receptor and MUC1 (CD227) for lung, breast, bladder, and ovarian cancer, NPY(Hy1R) receptor for breast cancer and Ewing sarcoma, and MC1R receptor for melanoma (REFS) [154,155,156]. By the targeted drug delivery approach, side-effects can be reduced, and the efficacy of the drug can be increased [38]. Trafficking of extracellular macromolecules into cells (endocytosis) and across cells (transcytosis) is facilitated by receptor-mediated transport mechanisms. During this process, ligands bind to specific cell-surface receptors, cluster together within endocytic vesicles, and sort into their respective vesicles [157]. Internalization and trafficking of CSPG-bound recombinant VAR2CSA lectins are examples and used in cancer treatment [158].
5. Applications
PDCs have a broad range of applications (Table 4). They can be applied against viruses such as SARS-CoV-2 [159,160] or multi-resistant bacteria [161]. PDCs also have relevance in the development of efficient vaccines. CoVac501, a self-adjuvanting peptide vaccine conjugated to a toll-like receptor (TLR)-7 agonist is a promising therapeutic against SARS-CoV-2 [162] with antifungal applications [163]. Likewise, in cancer, a self-adjuvanting multicomponent vaccine combining per-glycosylated MUC1 peptide and TLR2 agonist Pam3CysSer shows strong antibody generation in animal models (REF) [164]. Moving forward, peptide conjugates with a fluorescent dye can be used in diagnostic applications i.e., cancer imaging. In addition, polyanionic peptides conjugated with anti-inflammatory drugs are delivered into bones and other tumor cells [165]. Peptide conjugates acting on the central nervous system [166] or in gene delivery [167] are promising.
Table 4.
Selected applications of peptide-drugconjugates.
| Peptide | Drug/Vaccine | Indications | Reference |
|---|---|---|---|
| Somatostatin peptide analogue | 177Lu-dotate | Gastroenteropancreatic neuroendocrine tumors | [168] |
| Di-amino acid | Melflufen | Multiple myeloma | [169] |
| Arginine-glycine-aspartic acid | Naproxen/Ibuprofen | Anti-inflammatory/additives therapy with anti-cancer drugs to provide specific targeted delivery | [170] |
| Asparagine-glycine-arginine | Naproxen/ Ibuprofen |
||
| Arginine-glycine-aspartic acid/Asparagine-glycine-arginine | Ketoprofen | Anti-cancer therapy | [171] |
| AE147 peptide | Docetaxel | Advanced therapy for metastatic tumor | [172] |
| Gonadotropin-releasing hormone I/II | Daunorubicin | Targeted tumor therapy with high binding affinity and provides apoptotic effects | [173] |
| Dimethylmaleic anhydride | Doxorubicin | Targeted tumor therapy | [174] |
| Lysine | Neomycin-B | Antibiotics mainly evaluate their activity against gram-positive bacteria | [175] |
| Disulfide | Kanamycin | Successfully shows the activity in Mycobacterium tuberculosis | [176] |
| Polylactide-co-glycolide | Pyridopyrimidine derivatives | Anti-tubercular activity | [177] |
| Dipeptide | Cinnamic acid | Anti-protozoal agent | [178] |
| Ubiquicidin | Coumarin derivatives | Anti-fungal agent | [179] |
| Self-adjuvanting peptide vaccine conjugated toll-like receptor 7 agonists | CoVac501 | SARS-CoV-2 and other infectious diseases | [162] |
5.1. Anti-Cancer Therapy
In the context of applications of conjugated peptides for anti-cancer therapy, apoptosis and tumor accumulation-related peptides as well as the role of peptide-based nanotechnology, are discussed.
5.2. Apoptosis
Peptide-inducing apoptosis in tumor cells include Ra-V (deoxybouvardin) against breast cancer [180], and Hodgkin lymphoma [181]. DEVD (Asp-Glu-Val-Asp)-monomethyl auristatin-E conjugate shows strong therapeutic effects with minimal toxicity. More specifically, self-assembled nanoparticles deliver large amounts of monomethyl auristatin-E [182]. Self-assembled nanoparticles are advantageous as they show diversity in their chemical makeup, are biocompatible, enable high loading capacity of peptides and/or drugs, and can target sites on cancer cells. In fact, the peptide KLA (acetyl-KLAKLAK)2-NH2) conjugated with a tumor-homing peptide iRGD (CRGDKGPDC) has improved penetration of low-grade tumor tissue and cells with high selectivity and low systemic toxicity [42,183].
5.3. Tumor Accumulation
Diverse techniques for targeting tumors with peptides have been introduced. For example, non-RGD (arginine-glycine-aspartate) disulfide(SS)-bridged cyclo-peptide (ALOS-4) has specificity for integrin avβ3, overexpressed on several cancers including human metastatic melanoma. ALOS-4 conjugated with a topoisomerase I inhibitor, camptothecin, revealed increased cytotoxicity in human metastatic melanoma cells and decreased cytotoxicity in normal cells [184]. The tetra-branched peptide NT4 conjugated with paclitaxel binds to tumor membrane-sulfated glycosaminoglycans with strong selectivity showing more effective tumor regression [185]. Dimeric 123B9 peptide, targeting EphA2 (related to cancer metastasis, overexpressed in melanomas, ovarian, prostate, lung, and breast cancers), conjugated with paclitaxel inhibits lung metastasis in breast cancer models [186]. A protein-G-derived albumin-binding domain (ABD) conjugated with doxorubicin via a pH-sensitive linker demonstrates a longer half-life in the plasma and four times higher accumulation within the tumor [182]. Albumin-binding peptide (DICLPRWGCLW)-based bioconjugates are stable complexes for tumor-targeting effect [42,182].
5.4. Cancer Immunotherapy
The treatment of cancer can be possible by controlling the function of immune cells [42]. Programmed cell death ligand (PD-L1) is overexpressed on several cancer cells [187,188,189,190]. Interaction with programmed cell death protein 1 (PD-1; CD279), overexpressed on activated T cells, enables immune evasion of cancer cells. Inhibiting PD-1/PD-L1 interactions is a promising therapeutic approach. D-PPA [NYSKPTDRQYHF], a PD-L1-binding peptide, is an immune-related peptide (immunomodulating peptide). Interestingly, the hydrophilic D-type polypeptide (D-PPA) does not show cytotoxicity, but it can inhibit tumor growth and prolong survival by blocking the PD-1/PD-L1 interaction. In comparison to the equivalent L-peptide, D-peptides improve enzymatic stability, increase plasma half-life, improve oral bioavailability, binding activity, and specificity with the receptor of target proteins [191]. PD-L1-binding nanoparticles can be conjugated with doxorubicin leading to minimal toxicity and enhanced internalization [192]. Melittin peptide [GIGAVLKVLTTGLPALISWIKRKRQQ] can be conjugated with IL-2, improving the antitumor effect, and reducing side effects [193]. Macrophages play an essential role in innate and adaptive immunity, such that M2pep [Cys-YEQDPWGVKWWY] can be modified to increase specificity to target M2 tumor-associated macrophages. Co-encapsulation of CSF-1R siRNA and M2pep can target M2 tumor-associated macrophages for reprogramming to the M1 type, resulting in increased anti-tumor immune responses. Consequently, synergistically therapeutic effects in pancreatic cancer cells have been noted [194].
5.5. Nanotechnology
Peptides provide different advantages as drugs such as low toxicity, potency, and specificity. However, several practical challenges exist, such as short half-life, poor stability, and susceptibility to protease digestion. Nanotechnology has shown great potential in overcoming many traditional challenges of medicines. By using nano-drug delivery systems, numerous traditional pharmaceuticals have successfully passed into clinical trials and clinics. The combination of nanotechnology and peptides in nanomedicine offers excellent opportunities for developing novel, safe, and more efficient treatments against many diseases, including different types of cancers. Nanotechnology is an appealing strategy for maintaining functional forms of peptide biomolecules (biorecognition, signal transduction for treatment, toxicity) that otherwise could be degraded by digestive enzymes. Conjugation of peptides to nanoparticles enhances the stability and cellular uptake, leading to excellent efficacy and reduced toxicity. Protease-activatable liposomes were one of the earliest combinations of nanotechnology and peptides. It was designed by conjugating an acetylated dipeptide substrate (N-Ac-AA) through its carboxyl terminus to the amino group of 1,2-dioleoyl-sn-glycero-3-phosphoethanolamine (DOPE) to promote cellular internalization [195]. The resulting (N-Ac-AA-DOPE), together with dioleoyl trimethylammonium propane (DOTAP) and phosphatidyl-ethanolamine (PE), was assembled into non-fusogenic liposomes. The nanoparticles were activated by elastase or proteinase K to become fusogenic to improve intracellular delivery. Since then, tumor-targeting peptides have been successfully incorporated in nano-carriers that deliver small-molecule drugs, targeted imaging agents, liposomes, oligonucleotides, and inorganic nanoparticles to tumors. Moreover, peptide-related nanoparticles, such as peptidomimetic self-assembled nanoparticles and peptide aptamers, have also shown promising results in targeted drug delivery for cancer treatment [196,197].
The cell-penetrating peptide, KT2(NGVQPKYKWWKWWKKWW-NH2), conjugated to gold nanoparticles against breast cancer is a good example [198]. Notably, peptide-based bioconjugates can form nanoparticles by self-assembly resulting in increased permeability and retention effects at the tumor site [199,200]. Curcumin, a polyphenol derived from Curcuma longa(turmeric) root, has relevance either in terms of targeting or nano-formulation. The encapsulation of curcumin with albumin overcomes shortcomings of curcumin (low water solubility and bioavailability). In addition, the conjugation of nanoparticles with RK-10 (GSGSGSTYLCGAISLAPKAQIKESL), a PDL1-targeting peptide, leads to increased cytotoxicity against breast cancer [201]. Self-assembling peptides can be used as scaffolds for cell regeneration or carriers for the delivery of drugs and can be utilized to target the controlled release of stable drugs with less toxicity [202]. Moreover, studies showed tumor lymphatic vessel-targeting peptides present a novel approach for targeted drug delivery for cancer treatment [203].
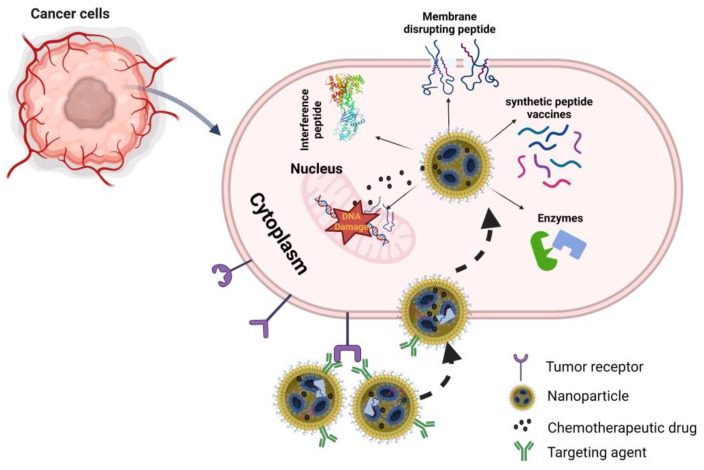
Recently, the number of targeting peptide–nanoconjugate drugs has significantly increased [204,205]. Using nanotechnology, new approaches are available to combine targeting peptides with other functional peptides and various diagnostic or therapeutic molecules. Peptide targeting itself is becoming combinatorial with the use of more than one peptide in a single entity, the use of peptides that also serve as proteolytic substrates to provide more function [206]. The further development of self-assembly peptide-based nanotechnology can promise highly effective anti-cancer therapeutic options [42]. Figure 3 presents different types of peptides which nanoparticles can deliver and provide a more efficient therapeutic impact for cancer treatment.
Figure 3.
Summary of different types of peptides that nanoparticles can deliver to cancer cells. Figure was created using biorender.com.
5.6. Bicycle–Toxin Conjugates
A bicycle peptide is a new modality consisting of 9–20 amino acids, including three cysteine residues reacting with a linker to form a rigid conformation of the peptide [207]. A bicycle can act as a transporter of drugs by bicycle-toxin conjugates. This approach offers some advantages such as slower renal clearance, deeper tumor penetration, and rapid extravasation [207].
5.7. Peptide–Dendrimer Conjugates
Peptide dendrimers, covalent (type I and II), built from (un)natural amino acids, and noncovalent (type III) that are not attached to multiple frameworks through the periphery, have a highly branched construction and unique properties-thermal performance, viscosity, and use for encapsulation. In the drug delivery mechanism, the drug is attached by (non)covalent (encapsulation)/bond. Peptide dendrimers have good biocompatibility and tunable amino acid features [208]. They can selectively deliver doxorubicin to the target cancer site [209]. Polyethylene glycol (PEG) incorporated into the dendrimer leads to an increased half-life. In the case of breast cancer, a dendrimer nanoparticle with doxorubicin is efficiently reduces tumor size [209]. Peptide dendrimers can also be used in the treatment of colorectal cancer with controlled gemcitabine drug delivery [210,211]. Further, dendrimers have also been shown to deliver cancer peptides and proteins to the immune system for effective stimulation and activation for immunotherapeutic approaches [212,213].
5.8. Cell-Penetrating Peptides
Membrane translocating peptides, such as penetratin from Antennapedia with sequence RQIKIWFQNRRMKWKK when tandemly linked to cancer peptides can stimulate anti-cancer immune responses [214,215,216,217]. The mechanisms by which cell-penetrating peptides enter cells and delivery of drugs, peptides, proteins, and DNA, is via a combination of energy-independent (membrane fusion) and energy-dependent pathways (endocytosis). Some peptides are also fully energy-independent in their uptake [218]. Cell-penetrating peptides are arginine-rich peptides, and due to their positive charge, they interact with negatively charged drug molecules and cell membranes through non-covalent interaction, including electrostatic interactions. As such, the application of these arginine-rich peptides has been used to deliver biosensors, drugs, and vaccines and allows entry through the blood-brain barrier [219]. An example is the use of these peptides linked to chemotherapeutic drugs, such as doxorubicin, for its specific delivery to triple-negative breast cancers [220].
6. Human Clinical Trials
We note that over twenty PDCs are currently in human clinical trials (some are summarized in Table 5 at different stages of clinical development). Zoptarelin against metastatic endometrial cancer [221,222], polyglutamic acid-paclitaxel conjugate for therapy of non-small cell lung cancer [223], and Vitafolid, a folic acid-vinca alkaloid conjugated with a peptide moiety against epithelial ovarian cancer [224], which reached phase III trial, are good examples [225].
Table 5.
Various PDCs under different stages of clinical development.
| Name of PDCs | TTP | Payload | Linker | Indication | Development Phase | Clinical Trials Registry |
|---|---|---|---|---|---|---|
| ANG1005 | Angiopep-2 | Paclitaxel | Succinic acid | Leptomeningeal disease from breast cancer | Phase III | NCT02048059 NCT03613181 |
| NGR015, NGR-hTNF | CNGRCG (1,5SS) | Human TNF | Amide | Malignant pleural mesothelioma | Phase III | NCT01098266 NCT03804866 NCT00484276 NCT00483080 |
| [18F]-AlF-NOTA-octreotide | Octreotide | 18F | NOTA | PET or GEP-NETs | Phase II/III | NCT04552847 |
| BT1718 | MT1-MMP binder | DM1 | Disulfide | Solid tumors | Phase II | NCT03486730 |
| [18F]-Fluciclatide | RGD | 18F | PEG | PET imaging | Phase II | NCT00918281 NCT00565721 NCT01176500 NCT01633255 NCT01788280 |
| [18F]-RGD-K5 | Cyclo-(RGDfK) | 18F | NOTA | PET imaging | Phase II | NCT00988936 NCT02490891 NCT03364270 |
| G-202 (mipsagargin) | DγEγEγEγE | Thapsigargin | Amide | Solid tumors | Phase II | NCT02381236 NCT02067156 NCT02607553 NCT01777594 NCT01056029 |
| 68Ga-NODAGA-E[cyclo(RGDyK)] 2 | E[cyclo(RGDyK)]2 | 68Ga | NODAGA | PET imaging | Phase II | NCT03445884 NCT03271281 |
| PEN-221 | fCYwKTCC (2,7 SS) | DM-1 | Disulfide | Neuroendocrine and small cell lung cancers | Phase II | NCT02936323 |
| 90Y-DOTATOC | 3 Tyr-octreotat | 90Y | DOTA | PRRT | Phase II | NCT03273712 |
| GRN1005 | Trevatide | Paclitaxel | Ester | Non-small Cell Lung Cancer (NSCLC) With Brain Metastases | Phase II | NCT01497665 |
| BT5528 | EphA2 binder | MMAE | Amide | EphA2-positive NSCLC | Phase I/II | NCT04180371 |
| 68Ga-NOTA-BBN-RGD | cyclo(RGDyK) and BBN | 68Ga | NOTA | PET/CT and PET imaging | Phase I | NCT02749019 NCT02747290 |
| tTF-NG | GNGRAHA | tTF | Amide | Malignant solid tumors | Phase I | NCT02902237 |
| TH1902 | Docetaxel peptide–drug conjugate | Alexa488 | Cleavable ester linker | Solid Tumor, TNBC-Triple-Negative Breast Cancer, Hormone Receptor-positive Breast Cancer, Epithelial Ovarian Cancer, Endometrial Cancer, Cutaneous Melanoma, Thyroid Cancer, Small-cell Lung Cancer, Prostate Cancer | Phase I | NCT04706962 |
| MB1707 | CXC | Paclitaxel | Ester | Advanced Solid Tumor, Breast Cancer, Non-Small Cell Lung Cancer, Ovary Cancer, Pancreatic Neoplasms |
Early Phase I | NCT05465590 |
Abbreviations: AlF, aluminum fluoride; AMBF3, ammonimethyltrifluoroborate; DγEγEγEγE, Asp-γ-(Glu)4-OH; DM-1, a maytansine derivative; DOTA, cyclododecyltetraacetic acid; f, D-Phe; 18F, fluorine-18; 68Ga, gallium-68; GEP-NETs, gastroenteropancreatic neuroendocrine tumors; MMAE, monomethyl auristatin E; NODAGA, 1,4,7-triazacyclononane,1-glutaric acid-4,7-acetic acid; NOTA, 1,4,7-triazacyclononane-1,4-7-triacetic acid; NSCLC, non-small cell lung cancer; SCN-Bz, 2-pisothiocyanatobenzyl; SN-38, 7-ethyl-10-hydroxycamptothecin; TATE, [3 Tyr]octreotate; TTP, tumor-targeting peptide; w, D-Trp; y, D-Tyr; 90Y, yttrium-90. bNCT numbers: ClinicalTrials.gov, USA.
In addition, appealing next-generation bicycle–toxin and peptide–dendrimer conjugates are in the pipeline, and their diverse variations are undergoing clinical trials [211]. BT1718, BT5528, and BT8009 [226] are worth mentioning. BT1718 consists of the specific targeting bicycle conjugated to the MD1 cytotoxin via a cleavable disulfide bond. Its target is 1 matrix metalloproteinase related to bladder, lung, breast, ovarian, and endometrial cancer. Phase I of clinical trials revealed good tolerability and stability and allowed the progression to Phase II [226]. BT5528 is formed from bicycle conjugation, via an enzyme cleavable Val-Cit linker, to an MMAE payload. It targets Ephrin type A receptor 2 related to several tumors and tyrosine kinase, which is responsible for cell adhesion, migration, proliferation, and differentiation. Phase I/II showed well tolerability [207,226]. BT8009, like BT5528 (but with a Val-Cit cleavable linker), targets Nectin-4, overexpressed in breast, bladder, lung, or pancreatic cancer. This bicyclic toxin conjugate presented promising results, including limited off-target toxicity in clinical trials [210,211]. Furthermore, it could be highlighted that nanotechnology offers excellent potential for PDCs to obtain clinical trials. The nanostructures of modified drugs, such as camptothecins, 10-hydroxycamptothecin, hydroxychloroquine, paclitaxel, doxorubicin, and dexamethasone via conjugation with peptides can be successfully used to treat a plethora of cancers, overcoming the drawbacks of drugs and enhancing their efficacy and efficiency [43,69,227]. The self-assembled PDCs, despite the last progress, have not been accepted either by the FDA or for clinical trials so far [227]. Nevertheless, in the coming years, rapid approval of anti-cancer PDCs is expected, thanks to the high investment in clinical trials by big Pharmaceutical Corporations (Pfizer, Oncopeptides, Pepgen Corporation, Bicycle Therapeutics, AstraZeneca).
7. Challenges for the Delivery of Peptide-Drug Conjugates: The Way Forward
Despite the remarkable progress in the research of PDCs, they still face challenges such as poor stability, rapid renal clearance [228], and translation of their favorable features into clinical outcomes for patients. PDCs often fail in clinical trials due to difficulty in translating rational drug conjugate designs into effective anti-cancer therapies [44]. The question of how and when PDCs are is released after entering the cell remains open. Thus, PDCs must be designed and synthesized more efficiently. Notably, fluorescent probes (such as fluorogenic with aggregation-induced emission feature) can be incorporated into PDCs to monitor this process [43]. Another problem is the oral administration of peptides as a new strategy for utilizing potential PDCs in human clinical trials. In this context, a new self-assembly method to form pectindiydroartemis in hydroxycamptothecin nanoparticles to PDC delivery by the oral route is worth mentioning. It could improve drug loading and release [209,229].
8. Conclusions
Peptide-drug conjugates are a great promise for cancer management, with two compounds, Melluflen and Lu177-dotatate, on the market and many others, such as peptide–dendrimer or bicycle–toxin conjugates, undergoing clinical trials. PDCs are a next-generation of targeted therapeutic agents as the equivalent antibody-drug conjugates, offering many advantages such as enhanced tumor penetration, selective delivery of cytotoxic payloads to target cells, improved efficacy, multifunctionality, biodegradability, reduced immunogenicity, and systemic toxicity, simplicity, easy structural modification, and lower costs of synthesis. Nevertheless, there are still challenges to overcome such as stability, bioactivity, and renal clearance. On the other hand, new innovative technologies such as nanotechnology are a promising prospect for potentiating anti-cancer efficacy, with potentially fewer side effects in terms of PDCs, thus driving the development of the field.
Author Contributions
All authors contributed to the concept of the article, writing of the article, and critically revising the article. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Sample Availability
Samples of the compounds are not available from the authors.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chavda V.P., Ertas Y.N., Walhekar V., Modh D., Doshi A., Shah N., Anand K., Chhabria M. Advanced Computational Methodologies Used in the Discovery of New Natural Anticancer Compounds. Front. Pharmacol. 2021;12:702611. doi: 10.3389/fphar.2021.702611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chavda V.P., Patel A.B., Mistry K.J., Suthar S.F., Wu Z.X., Chen Z.S., Hou K. Nano-Drug Delivery Systems Entrapping Natural Bioactive Compounds for Cancer: Recent Progress and Future Challenges. Front. Oncol. 2022;12:867655. doi: 10.3389/fonc.2022.867655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hanahan D., Weinberg R.A. Hallmarks of Cancer: The Next Generation. Cell. 2011;144:646. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 4.Baylin S.B., Jones P.A. Epigenetic Determinants of Cancer. Cold Spring Harb. Perspect. Biol. 2016;8:a019505. doi: 10.1101/cshperspect.a019505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu B., Zhou H., Tan L., Siu K.T.H., Guan X.-Y. Exploring treatment options in cancer: Tumor treatment strategies. Signal Transduct. Target. Ther. 2024;9:175. doi: 10.1038/s41392-024-01856-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takeshima H., Ushijima T. Accumulation of genetic and epigenetic alterations in normal cells and cancer risk. NPJ. Precis. Oncol. 2019;3:7. doi: 10.1038/s41698-019-0079-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kang S., Lee S., Park S. iRGD Peptide as a Tumor-Penetrating Enhancer for Tumor-Targeted Drug Delivery. Polymers. 2020;12:1906. doi: 10.3390/polym12091906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chavda V.P. Applications of Targeted Nano Drugs and Delivery Systems. Elsevier; Amsterdam, The Netherlands: 2019. Nanotherapeutics, and Nanobiotechnology; pp. 1–13. [Google Scholar]
- 9.Chavda V.P., Vihol D., Mehta B., Shah D., Patel M., Vora L.K., Pereira-Silva M., Paiva-Santos A.C. Phytochemical-loaded liposomes for anti-cancer therapy: An updated review. Nanomedicine. 2022;7:547. doi: 10.2217/nnm-2021-0463. [DOI] [PubMed] [Google Scholar]
- 10.Puig-Saus C., Rojas L.A., Laborda E., Figueras A., Alba R., Fillat C., Alemany R. iRGD tumor-penetrating peptide-modified oncolytic adenovirus shows enhanced tumor transduction, intratumoral dissemination, and antitumor efficacy. Gene Ther. 2014;21:767. doi: 10.1038/gt.2014.52. [DOI] [PubMed] [Google Scholar]
- 11.Safari-Alighiarloo N., Taghizadeh M., Rezaei-Tavirani M., Goliaei B., Peyvandi A.A. Protein-protein interaction networks (PPI) and complex diseases. Gastroenterol Hepatol. Bed Bench. 2014;7:17. [PMC free article] [PubMed] [Google Scholar]
- 12.De Las Rivas J., Fontanillo C. Protein–Protein Interactions Essentials: Key Concepts to Building and Analyzing Interactome Networks. PLoS Comput. Biol. 2010;6:e1000807. doi: 10.1371/journal.pcbi.1000807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rao V.S., Srinivas K., Sujini G.N., Kumar G.N.S. Protein-protein interaction detection: Methods and analysis. Int. J. Proteom. 2014;2014:147648. doi: 10.1155/2014/147648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hashemi Z.S., Zarei M., Fath M.K., Ganji M., Farahani M.S., Afsharnouri F., Pourzardosht N., Khalesi B., Jahangiri A., Rahbar M.R., et al. In silico Approaches for the Design and Optimization of Interfering Peptides Against Protein–Protein Interactions. Front. Mol. Biosci. 2021;8:669431. doi: 10.3389/fmolb.2021.669431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chavda V.P., Patel Z., Parmar Y., Chavda D. In Silico Protein Design and Virtual Screening. Comput. Bioinform. 2021;5:85–99. [Google Scholar]
- 16.Apostolopoulos V., Bojarska J., Chai T.-T., Elnagdy S., Kaczmarek K., Matsoukas J., New R., Parang K., Lopez O.P., Parhiz H., et al. A Global Review on Short Peptides: Frontiers and Perspectives. Molecules. 2021;26:430. doi: 10.3390/molecules26020430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Apostolopoulos V., Bojarska J., Feehan J., Matsoukas J., Wolf W.M. Smart therapies for pandemics: A potential of short peptides. Front. Pharmacol. 2022;13:914467–914475. doi: 10.3389/fphar.2022.914467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Apostolopoulos V., Bojarska J., Chai T.-T., Feehan J., Kaczmarek K., Matsoukas J.M., Paredes Lopez O., Saviano M., Skwarczynski M., Smith-Carpenter J., et al. New Advances in Short Peptides: Looking Forward. Molecules. 2022;27:3635. doi: 10.3390/molecules27113635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bojarska J., Mieczkowski A., Ziora Z.M., Skwarczynski M., Toth I., Shalash A.O., Parang K., El-Mowafi S.A., Mohammed E.H.M., Elnagdy S., et al. Cyclic Dipeptides: The Biological and Structural Landscape with Special Focus on the Anti-Cancer Proline-based Scaffold. Biomolecules. 2021;11:1515. doi: 10.3390/biom11101515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bojarska J., Wolf W.M. Ultra-short cyclo-peptides as bio-inspired therapeutics: Proline-based 2,5-diketopiperazines (DKP) Proceedings. 2021;79:10. [Google Scholar]
- 21.Bojarska J., Breza M., Remko M., Czyz M., Gajos-Michniewicz A., Zimecki M., Kaczmarek K., Madura I.D., Wojciechowski J.M., Wolf W.M. Structural and Biofunctional Insights into the Cyclo(Pro-Pro-Phe-Phe-) Scaffold from Experimental and In Silico Studies: Melanoma and Beyond. Int. J. Mol. Sci. 2022;23:7173. doi: 10.3390/ijms23137173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bojarska J. Advances in Research of Short Peptides. Molecules. 2022;27:2446. doi: 10.3390/molecules27082446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bojarska J., New R., Borowiecki P., Remko M., Breza M., Madura I.D., Fruzinski A., Pietrzak A., Wolf W.M. The First Insight Into the Supramolecular System of D,L-α-Difluoromethylornithine: A New Antiviral Perspective. Front. Chem. 2021;9:679776. doi: 10.3389/fchem.2021.679776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bojarska J., Remko M., Breza M., Madura I., Fruzinski A., Wolf W.M. A Proline-Based Tectons and Supramolecular Synthons for Drug Design 2.0: A Case Study of ACEI. Pharmaceuticals. 2020;13:338. doi: 10.3390/ph13110338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bojarska J., Remko M., Madura I.D., Kaczmarek K., Zabrocki J., Wolf W.M. Synthesis, Experimental and in Silico Studies of N-Fluorenylmethoxycarbonyl-O-Tert-Butyl-N-Methyltyrosine, Coupled with CSD Data: A Survey of Interactions in the Crystal Structures of Fmoc-Amino Acids. Acta Crystallogr. C. 2020;76:328–345. doi: 10.1107/S2053229620003009. [DOI] [PubMed] [Google Scholar]
- 26.Bojarska J., Remko M., Madura I.D., Wojciechowski J.M., Olczak A., Kaczmarek K., Zabrocki J., Wolf W.M. Supramolecular Synthon Polymorphism in Modified Amino Acids. Structural, Conformational and Energy Landscapes of N-Benzoyl-20-Hydroxy-3-Methylisovaline. J. Mol. Struct. 2019;1190:11–22. doi: 10.1016/j.molstruc.2019.04.045. [DOI] [Google Scholar]
- 27.Bojarska J., Remko M., Breza M., Madura I.D., Kaczmarek K., Zabrocki J., Wolf W.M. A Supramolecular Approach to Structure-Based Design with A Focus on Synthons Hierarchy in Ornithine-Derived Ligands: Review, Synthesis, Experimental and in Silico Studies. Molecules. 2020;25:1135. doi: 10.3390/molecules25051135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhao Z., Ukidve A., Kim J., Mitragotri S. Targeting Strategies for Tissue-Specific Drug Delivery. Cell. 2020;181:151. doi: 10.1016/j.cell.2020.02.001. [DOI] [PubMed] [Google Scholar]
- 29.Shaji J., Patole V. Protein and peptide drug delivery: Oral approaches. Indian J. Pharm. Sci. 2008;70:269–277. doi: 10.4103/0250-474X.42967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ludwig B.S., Kessler H., Kossatz S., Reuning U. RGD-Binding Integrins Revisited: How Recently Discovered Functions and Novel Synthetic Ligands (Re-)Shape an Ever-Evolving Field. Cancers. 2021;13:1711. doi: 10.3390/cancers13071711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Habault J., Poyet J.L. Recent Advances in Cell Penetrating Peptide-Based Anticancer Therapies. Molecules. 2019;24:927. doi: 10.3390/molecules24050927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yan L., Rosen N., Arteaga C. Targeted cancer therapies. Chin. J. Cancer. 2011;30:1. doi: 10.5732/cjc.010.10553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Craik D.J., Fairlie D.P., Liras S., Price D. The future of peptide-based drugs. Chem. Biol. Drug Des. 2013;81:136. doi: 10.1111/cbdd.12055. [DOI] [PubMed] [Google Scholar]
- 34.Tsomaia N. Peptide therapeutics: Targeting the undruggable space. Eur. J. Med. Chem. 2015;94:459. doi: 10.1016/j.ejmech.2015.01.014. [DOI] [PubMed] [Google Scholar]
- 35.Moffat J.G., Rudolph J., Bailey D. Phenotypic screening in cancer drug discovery—Past, present and future. Nat. Rev. Drug Discov. 2014;13:588. doi: 10.1038/nrd4366. [DOI] [PubMed] [Google Scholar]
- 36.Guzmán-Rodríguez J.J., Ochoa-Zarzosa A., López-Gómez R., López-Meza J.E. Plant antimicrobial peptides as potential anticancer agents. Biomed. Res. Int. 2015;2015:735087. doi: 10.1155/2015/735087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alas M., Saghaeidehkordi A., Kaur K. Peptide-Drug Conjugates with Different Linkers for Cancer Therapy. J. Med. Chem. 2021;64:216. doi: 10.1021/acs.jmedchem.0c01530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chavda V.P., Ajabiya J., Teli D., Bojarska J., Apostolopoulos V. Tirzepatide, a New Era of Dual-Targeted Treatment for Diabetes and Obesity: A Mini-Review. Molecules. 2022;27:4315. doi: 10.3390/molecules27134315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hoppenz P., Els-Heindl S., Beck-Sickinger A.G. Peptide-Drug Conjugates and Their Targets in Advanced Cancer Therapies. Front. Chem. 2020;8:571. doi: 10.3389/fchem.2020.00571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Das S., Al-Toubah T., El-Haddad G., Strosberg J. (177)Lu-DOTATATE for the treatment of gastroenteropancreatic neuroendocrine tumors. Expert Rev. Gastroenterol. Hepatol. 2019;13:1023. doi: 10.1080/17474124.2019.1685381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Deonarain M.P., Yahioglu G., Stamati I., Pomowski A., Clarke J., Edwards B.M., Diez-Posada S., Stewart A.C. Small-format drug conjugates: A viable alternative to ADCs for solid tumors? Antibodies. 2018;7:16. doi: 10.3390/antib7020016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang S.B., Banik N., Han B., Lee D.-N., Park J. Peptide-Based Bioconjugates and Therapeutics for Targeted Anticancer Therapy. Pharmaceutics. 2022;14:1378. doi: 10.3390/pharmaceutics14071378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang Y., Cheetham A.G., Angacian G., Su H., Xie L., Cui H. Peptide-drug conjugates as effective prodrug strategies for targeted delivery. Adv. Drug Deliv. Rev. 2017;110:112. doi: 10.1016/j.addr.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jong M.D., Valkema R., Jamar F., Kvols L.K., Kwekkeboom D.J., Breeman W.A.P., Bakker W.H., Smith C., Pauwels S., Krenning E.P. Somatostatin receptor-targeted radionuclide therapy of tumors: Preclinical and clinical findings. Semin. Nucl. Med. 2002;32:133. doi: 10.1053/snuc.2002.31027. [DOI] [PubMed] [Google Scholar]
- 45.Jamous M., Haberkorn U., Mier W. Synthesis of Peptide Radiopharmaceuticals for the Therapy and Diagnosis of Tumor Diseases. Molecules. 2013;18:3379. doi: 10.3390/molecules18033379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Capper C.P., Rae J.M., Auchus R.J. The Metabolism, Analysis, and Targeting of Steroid Hormones in Breast and Prostate Cancer. Horm. Cancer. 2016;7:149. doi: 10.1007/s12672-016-0259-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mateos M.V., Blade J., Bringhen S., Ocio E.M., Efebera Y., Pour L., Gay F., Sonneveld P., Gullbo J., Richardson P.G. Melflufen: A peptide-drug conjugtae for the treatment of multiple myeloma. J. Clin. Med. 2020;9:3120. doi: 10.3390/jcm9103120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lindberg J., Nilvebrant J., Lehmann F. Progress and future directions with peptide-drug conjugates for targeted cancer therapy. Molecules. 2021;26:6042. doi: 10.3390/molecules26196042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kurzock R., Gabrail N., Chandhasin C., Moulder S., Smith C., Brenner A., Sankhala K., Mita A., Elian K., Bouchard D., et al. Safety, pharmacokinetics, and activity of GRN1005, a novel conjugate of angiopep-2, a peptide facilitating brain penetration, and paclitaxel, in patients with advanced solid tumours. Mol. Cancer Ther. 2012;11:308. doi: 10.1158/1535-7163.MCT-11-0566. [DOI] [PubMed] [Google Scholar]
- 50.Li F., Tang S.C. Targeting metastatic breast cancer with ANG1005, a novel peptide-paclitaxel conjugate that crosses the blood-brain-barrier (BBB) Genes Dis. 2017;4:1–3. doi: 10.1016/j.gendis.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Northfelt D.W., Allred J.B., Liu H., Hobday T.J., Rodacker M.W., Lyss A.P., Fitch T.R., Perez E.A. Phase 2 trial of paclitaxel polyglumex with capecitabine for metastatic breast cancer. Am. J. Clin. Oncol. 2014;37:167–171. doi: 10.1097/COC.0b013e31826e0550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mahalingam D., Wilding G., Denmeade S., Sarantopoulas J., Cosgrove D., Cetnar J., Azad N., Bruce J., Kurman M., Allgood V.E., et al. Mipsagargin, a novel thapsigargin-based PSMA-activated prodrug: Results of a first-in-man phase I clinical trial in patients with refractory, advanced or metastatic solid tumours. Br. J. Cancer. 2016;114:9. doi: 10.1038/bjc.2016.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Andersen T.B., López C.Q., Manczak T., Martinez K., Simonsen H.T. Thapsigargin—From Thapsia L. to Mipsagargin. Molecules. 2015;20:6113. doi: 10.3390/molecules20046113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Emos G., Gorchev G., Sehouli J., Wimberger P., Stahle A., Hanker L., Hilpert F., Sindermann H., Grundker C., Harter P. Efficacy and safety of AEZS-108 (INN: Zoptarelin doxorubicin acetate) an LHRH agonist linked to doxorubicin in women with platinum refractory or resistant ovarian cancer expressing LHRH receptors: A multicenter phase II trial of the ago-study group (AGO GYN 5) Gynecol. Oncol. 2014;133:427. doi: 10.1016/j.ygyno.2014.03.576. [DOI] [PubMed] [Google Scholar]
- 55.BT1718 in Patients with Advanced Solid Tumours. [(accessed on 30 August 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03486730.
- 56.Schoffski P., Delord J.P., Brain E., Robert J., Dumez H., Gasmi J., Trouet A. First-in-man phase I study assessing the safety and pharmacokinetics of a 1-hour intravenous infusion of the doxorubicin prodrug DTS-201 every 3 weeks in patients with advanced or metastatic solid tumours. Eur. J. Cancer. 2017;86:240. doi: 10.1016/j.ejca.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 57.Clinical Trials Register—Search for DTS-201. [(accessed on 29 April 2008)]. Available online: https://www.clinicaltrialsregister.eu/ctr-search/search?query=DTS-201.
- 58.Pinato D.J., Black J.R.M., Ramaswami R., Tan T.M., Adjogatse D., Sharma R. Peptide receptor radionuclide therapy for metastatic paragangliomas. Med. Oncol. 2016;33:47. doi: 10.1007/s12032-016-0737-9. [DOI] [PubMed] [Google Scholar]
- 59.Forsell-Aronsson E., Bernhardt P., Nilsson O., Tisell L.E., Wangberg B., Ahlman H. Biodistribution data from 100 patinets i.v. injected with In-111-DTPA-D-Phe(1)-octreotide. Acta Oncolog. 2004;43:436–442. doi: 10.1080/02841860410030670. [DOI] [PubMed] [Google Scholar]
- 60.Lorusso D., Scambia G., Amadio G., di Legge A., Pietragalla A., De Vincenzo R., Masciullo V., Stefano M.D., Mangili G., Citterio G., et al. Phase II study of NGR-hTNF in combination with doxorubicin in relapsed ovarian cancer patients. Br. J. Cancer. 2012;107:37–42. doi: 10.1038/bjc.2012.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Abu Samaan T.M., Samec M., Liskova A., Kubatka P., Busselberg D. Paclitaxel`s mechanistic and clinical effects on breast cancer. Biomolecules. 2019;9:789. doi: 10.3390/biom9120789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Drappatz J., Brenner A., Wong E.T., Eichler A., Schiff D., Groves M.D., Mikkelsen T., Rosenfeld S., Sarantopoulos J., Meyers C.A., et al. Phase I study of GRN1005 in recurrent malignant glioma. Clin. Cancer Res. 2013;19:1567–1576. doi: 10.1158/1078-0432.CCR-12-2481. [DOI] [PubMed] [Google Scholar]
- 63.Curtis K.K., Sarantopoulos J., Northfelt D.W., Weiss G.J., Barnhart K.M., Whisnant J.K., Leuschner C., Alila H., Borad M.J., Ramanathan R.K. Novel LHRH-receptor-targeted cytolytic peptide, EP-100: First-in-human phase I study in patients with advanced LHRH-receptor-expressing solid tumors. Cancer Chemother. Pharm. 2014;73:931–941. doi: 10.1007/s00280-014-2424-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ley K., Rivera-Nieves J., Sandborn W.J., Shattil S. Integrin-based therapeutics: Biological basis, clinical use and new drugs. Nat. Rev. Drug Discov. 2016;15:173. doi: 10.1038/nrd.2015.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Toschi L., Finocchiaro G., Bartolini S., Gioia V., Cappuzzo F. Role of gemcitabine in cancer therapy. Future Oncol. 2005;1:7. doi: 10.1517/14796694.1.1.7. [DOI] [PubMed] [Google Scholar]
- 66.Pezhman Shirmardi S., Gandomkar M., Maragheh M.G., Shamsaei M. Preclinical evaluation of a new bombesin analog for imaging of gastrin-releasing peptide receptors. Cancer Biother. Radiopharm. 2011;26:309–316. doi: 10.1089/cbr.2010.0912. [DOI] [PubMed] [Google Scholar]
- 67.Lindgren M., Rosenthal-Aizman K., Saar K., Eiriksdottir E., Jiang Y., Sassian M., Ostlund P., Hallbrink M., Langel U. Overcoming methotrexate resistance in breast cancer tumour cells by the use of a new cell-penetrating peptide. Biochem. Pharmacol. 2006;71:416–425. doi: 10.1016/j.bcp.2005.10.048. [DOI] [PubMed] [Google Scholar]
- 68.Biri-Kovács B., Adorján A., Szabó I., Szeder B., Bősze S., Mező G. Structure-Activity Relationship of HER2 Receptor Targeting Peptide and Its Derivatives in Targeted Tumor Therapy. Biomolecules. 2020;10:183. doi: 10.3390/biom10020183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hernandez Vargas S., Kossatz S., Voss J., Ghosh S.C., Tran Cao H.S., Simien J., Reiner T., Dhingra S., Fisher W.E., Azhdarinia A. Specific Targeting of Somatostatin Receptor Subtype-2 for Fluorescence-Guided Surgery. Clin. Cancer Res. 2019;25:4332. doi: 10.1158/1078-0432.CCR-18-3312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhou J., Rossi J. Aptamers as targeted therapeutics: Current potential and challenges. Nat. Rev. Drug Discov. 2017;16:181–202. doi: 10.1038/nrd.2016.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kondo E., Iioka H., Saito K. Tumor-homing peptide and its utility for advanced cancer medicine. Cancer Sci. 2021;112:2118–2125. doi: 10.1111/cas.14909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fujiwara K., Toda H., Ikeguchi M. Dependence of α-helical and β-sheet amino acid propensities on the overall protein fold type. BMC Struct. Biol. 2012;12:18. doi: 10.1186/1472-6807-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bouayad-Gervais S., St-Cyr D.J., Courcelles M., Bonneil É., Gohard F.H., Thibault P., Earnshaw C., Tyers M. Head-to-tail cyclization of side chain-protected linear peptides to recapitulate genetically-encoded cyclized peptides. Pept. Sci. 2022;114:e24254. doi: 10.1002/pep2.24254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Katsara M., Tselios T., Deraos S., Deraos G., Matsoukas M.T., Lazoura E., Matsoukas J., Apostolopoulos V. Round and round we go: Cyclic peptides in disease. Curr. Med. Chem. 2006;13:2221–2232. doi: 10.2174/092986706777935113. [DOI] [PubMed] [Google Scholar]
- 75.Katsara M., Deraos G., Tselios T., Matsoukas J. Apostolopoulos. Design of novel cyclic altered peptide ligands of myelin basic protein MBP83-99 that modulate immune responses in SJL/J mice. J. Med. Chem. 2008;51:3971–3978. doi: 10.1021/jm8000554. [DOI] [PubMed] [Google Scholar]
- 76.Deraos G., Chatzantoni K., Matsoukas M.T., Tselios T., Deraos S., Katsara M., Papathanasopoulos P., Vynios D., Apostolopoulos V., Mouzaki A., et al. Cittrulination of linear and cyclic altered peptide ligands from myelin basic protein (MBP87-99) epitope elicits a Th1 polarized responses by T cells isolated from multiple sclerosis patients: Implications in triggering disease. J. Med. Chem. 2008;51:7834–7842. doi: 10.1021/jm800891n. [DOI] [PubMed] [Google Scholar]
- 77.Katsara M., Deraos G., Tselios T., Matsoukas M.T., Friligou I., Matsoukas J., Apostolopoulos V. Design and synthesis of a cyclic double mutant peptide (cyclo(87-99)[A91,A96]MBP87-99) induces altered responses in mice after conjugation to mannan: Implications in the immunotherapy of multiple sclerosis. J. Med. Chem. 2009;52:214–218. doi: 10.1021/jm801250v. [DOI] [PubMed] [Google Scholar]
- 78.Lourbopoulos A., Matsoukas M.T., Katsara M., Deraos G., Giannakopoulos A., Lagoudaki R., Grigoriadis N., Matsoukas J., Apostolopoulos V. Cyclization of PLP139-151 peptide reduces its encephalitogenic potential in experimental autoimmune encephalomyelitis. Bioorg. Med. Chem. 2018;26:2221–2228. doi: 10.1016/j.bmc.2017.12.024. [DOI] [PubMed] [Google Scholar]
- 79.Garg C., Priyam A., Kumar P., Kumar Sharma A., Gupta A. In vitro assessment of core-shell micellar nanostructures of amphiphilic cationic polimer-peptide conjugates as efficient gene and drug carriers. J. Pharm. Sci. 2020;109:2847–2853. doi: 10.1016/j.xphs.2020.05.016. [DOI] [PubMed] [Google Scholar]
- 80.Tesauro D., Accardo A., Diaferia C., Milano V., Guillon J., Ronga L., Rossi F. Peptide-based drug-delivery systems in biotechnological applications: Recent advances and perspectives. Molecules. 2019;24:351. doi: 10.3390/molecules24020351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang L., Wang N., Zhang W., Cheng X., Yan Z., Shao G., Wang X., Wang R., Fu C. Therapeutic peptides: Current applications and future directions. Signal Transduct. Target. Ther. 2022;7:48. doi: 10.1038/s41392-022-00904-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chi-Lung Lee A., Harris J.L., Khanna K.K., Hong J.H. A comprehensive review on current advances in peptide drug development and design. Int. J. Mol. Sci. 2019;20:2383. doi: 10.3390/ijms20102383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sarkar G., Curran G.L., Sarkaria J.N., Lowe V.J., Jenksins R.B. Peptide carrier-mediated non-covalent delivery of unmodified cisplatin, methotrexate and other agents via intravenous route to the brain. PLoS ONE. 2014;9:e979655. doi: 10.1371/journal.pone.0097655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shah J.N., Guo G.Q., Krishnan A., Ramesh M., Kumar Katari N., Shahbaaz M., Abdellattif M.H., Singh S.K., Dua K. Peptide-based therapeutics: Emerging potential therapeutic agents for COVID-19. Therapie. 2022;77:319–328. doi: 10.1016/j.therap.2021.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.King A., Ndifon C., Lui S., Widdows K., Kotamraju V.R., Agemy L., Teesalu T., Glazier J.D., Cellesi F., Harris L.K., et al. Tumor-homing peptides as tools for targeted delivery of payloads to the placenta. Sci. Adv. 2022;2:e1600349. doi: 10.1126/sciadv.1600349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Anti-Cancer Peptide Drug Conjugates: An Overwiew (2021) [(accessed on 9 July 2021)]. Available online: https://www.biochempeg.com/article/199.html.
- 87.Sharma A., Kapoor P., Gautam A., Chaudhary K., Kumar R., Chauhan J.S., Tyagi A., Raghava G.P.S. Computational approach for designing tumor homing peptides. Sci. Rep. 2013;3:srep01607. doi: 10.1038/srep01607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Laakonen P., Porkka K., Hoffman J.A., Ruoslahti E. A tumor-homing peptide with a targeting specificity related to lymphatic vessels. Nat. Med. 2002;8:751–755. doi: 10.1038/nm720. [DOI] [PubMed] [Google Scholar]
- 89.Kapoor P., Singh H., Gautam A., Chaudhary K., Kumar R., Raghava G.P.S. TumorHoPe: A database of tumor homing peptides. PLoS ONE. 2012;7:e35187. doi: 10.1371/journal.pone.0035187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Acharya B., Meka R.R., Venkatesha S.H., Lees J., Teesalu T., Moudgil K.D. A novel CNS-homing peptide for targeting neuroinflammatory lesions in experimental autoimmune encephalomyelitis. Mol. Cell. Probes. 2020;51:101530. doi: 10.1016/j.mcp.2020.101530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Khandia R., Sachan S., Munjal A.K., Tiwari R., Dhama K. Topics in Anti-Cancer Research. Volume 44. Bentham Science Publishers; Sharjah, United Arab Emirates: 2016. Tumor homing peptides: Promising futuristic hope for cancer therapy; pp. 43–86. [Google Scholar]
- 92.Ruoslahti E. Homing peptides. Encycl. Ref. Cancer. 2001:417–418. [Google Scholar]
- 93.Cho C.-F., Farquhar C.E., Fadzen C.M., Scott B., Zhuang P., von Spreckelsen N., Loas A., Hartrampf N., Pentelute B.L., Lawler S.E. A Tumor-Homing Peptide Platform Enhances Drug Solubility, Improves Blood–Brain Barrier Permeability and Targets Glioblastoma. Cancers. 2022;14:2207. doi: 10.3390/cancers14092207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Katsara M., Yuriev E., Ramsland P.A., Tselios T., Deraos G., Lourbopoulos A., Grigoriadis N., Matsoukas J., Apostolopoulos V. Altered peptide ligands of myelin basic protein (MBP87-99) conjugated to reduces mannan modulate immune responses in mice. Immunology. 2009;128:521–533. doi: 10.1111/j.1365-2567.2009.03137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Xing P., Michael M., Apostolopulos V., Prenzoska J., Marshall C., Bishop J., McKenzie I.F.C. Phase-I study of synthetic MUC1 peptides in breast-cancer. Int. J. Oncol. 1995;6:1283–1289. doi: 10.3892/ijo.6.6.1283. [DOI] [PubMed] [Google Scholar]
- 96.Karanikas V., Hwang L.A., Pearson J., Ong C.S., Apostolopoulos V., Vaughan H., Xing P.X., Jamieson G., Pietersz G., Tait B., et al. Antibody and T cell responses of patients with adenocarcinoma immunized with manna-MUC1 fusion protein. J. Clin. Investig. 1997;100:2783–2792. doi: 10.1172/JCI119825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Apostolopoulos V., Pietersz G.A., Tsibanis A., Tsikkinis A., Stojanovska L., McKenzie I.F.C., Vassilaros S. Dendritic cell immunotherapy: Clinical outcomes. Clin. Transl. Immunol. 2014;3:e21. doi: 10.1038/cti.2014.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Apostolopoulos V., Lofthouse S.A., Popovski V., Chelvanayagam G., Sandrim M.S., McKenzie I.F.C. Peptide mimics of a tumor antigen induce functional cytotoxic T cells. Nat. Biotechnol. 1998;16:276–280. doi: 10.1038/nbt0398-276. [DOI] [PubMed] [Google Scholar]
- 99.Wilsinso B.L., Day S., Chapman R., Perrier S., Apostolopoulos V., Payne R.J. Synthesis and immunological evaluation of self-assebing and self-adjuvanting tricomponent glycopeptide cancer-vaccine candidates. Chem. Eur. J. 2012;18:16540–16548. doi: 10.1002/chem.201202629. [DOI] [PubMed] [Google Scholar]
- 100.Morris M.C., Depollier J., Heitz F., Divita G. A peptide carrier from the delivery of biologiclly active protein sinto mammalian cells. Nat. Biotechnol. 2001;19:1173–1176. doi: 10.1038/nbt1201-1173. [DOI] [PubMed] [Google Scholar]
- 101.Ridgway H., Moore G.J., Mavromoustakos T., Tsiodras S., Ligielli I., Kelaidonis K., Chasapis C.T., Gadanec L.K., Zulli A., Apostolopoulos V., et al. Discovery of a new generation of angiotensyn receptor blocking drugs: Receptor mechanisms and in silico binding to enzymes relevant to SARS-CoV-2. Comput. Struct. Biotechnol. J. 2022;20:2091–2111. doi: 10.1016/j.csbj.2022.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Matsoukas J.M., Gadanec L.K., Zulli A., Apostolopoulos V., Kelaidonis K., Ligielli I., Moschovou K., Georgiou N., Plotas P., Chasapis C.T., et al. Diminazene Aceturate Reduces Angiotensin II Constriction and Interacts with the Spike Protein of Severe Acute Respiratory Syndrome Coronavirus 2. Biomedicines. 2022;10:1731. doi: 10.3390/biomedicines10071731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Melnyk T., Dordevic S., Conejos-Sanchez I., Vincent M.J. Therapeutic potential of polypeptide-based conjugates: Rational design and analytical tools that can boost clinical translation. Adv. Drug Deliv. Rev. 2020;160:136–169. doi: 10.1016/j.addr.2020.10.007. [DOI] [PubMed] [Google Scholar]
- 104.Tang H., Liu Y., Yu Z., Sun M., Lin L., Liu W., Han Q., Wei M., Jin Y. The Analysis of Key Factors Related to ADCs Structural Design. Front. Pharmacol. 2019;10:373. doi: 10.3389/fphar.2019.00373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ding H., Gangalum P.R., Galstyan A., Fox I., Patil R., Hubbard P., Murali R., Ljubimova J.Y., Holler E. HERG-2 positive breast cancer targeting and treatment by a peptide-conjugated mini nanodrug. Nanomedicine. 2017;13:631–639. doi: 10.1016/j.nano.2016.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Chen B., Dai W., He B., Zhang H., Wang X., Wang Y., Zhang Q. Current multistage drug delivery systems based on the tumor microenviron ment. Theranostics. 2017;7:538–558. doi: 10.7150/thno.16684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Praveen K., Das S., Dhaware V., Pandey B., Mondal B., Gupta S.S. pH-responsive ‘supra-amphiphilic’ nanoparticles based on homoarginine polypeptides. ACS Appl. Bio Mater. 2019;2:4162–4172. doi: 10.1021/acsabm.9b00432. [DOI] [PubMed] [Google Scholar]
- 108.Sonawane S.J., Kalhapure R.S., Govender T. Hydazone linkages in pH responsive drug delivery systems. Eur. J. Pharm. Sci. 2017;1:45–65. doi: 10.1016/j.ejps.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 109.Liu B., Thayumanavan S. Substituent effects on the pH sensitivity of acetals and ketals and their correlation with encapsulation stability in polymeric nanogels. J. Am. Chem. Soc. 2017;139:2306–2317. doi: 10.1021/jacs.6b11181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kalia J., Raines R.T. Hydrolytic stability of hydrazones and oximes. Angew. Chem. Int. Ed. 2008;47:7523–7526. doi: 10.1002/anie.200802651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Murphy G., Nagase H. Reappraising metalloproteinases in rheumatoid arthritis and osteoarthritis: Destruction or repair? Nat. Clin. Pract. Rheumatol. 2008;4:128–135. doi: 10.1038/ncprheum0727. [DOI] [PubMed] [Google Scholar]
- 112.de la Rica R., Aili D., Stevens M.M. Enzyme-responsive nanoparticles for drug release and diagnostics. Adv. Drug Deliv. Rev. 2012;64:967–978. doi: 10.1016/j.addr.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 113.Heeswijk W.A.R., Hoes C.J.T., Stoffer T., Eenink M.J.D., Potman W., Feijen J. The synthesis and characterization of polypeptide-adriamycin conjugates and its complexes with adriamycin. Part I. J. Control. Release. 1985;1:301–315. doi: 10.1016/0168-3659(85)90006-9. [DOI] [Google Scholar]
- 114.Mahmood U., Tung C.H., Bogdanov A., Weissleder R. Near-infrared optical imaging of protease activity for tumor detection. Radiology. 1999;213:866–870. doi: 10.1148/radiology.213.3.r99dc14866. [DOI] [PubMed] [Google Scholar]
- 115.Weissleder R., Tung C.H., Mahmood U., Bogdanov A. In vivo imaging of tumors with protease-activated near-infrared fluorescent probes. Nat. Biotechnol. 1999;17:375–378. doi: 10.1038/7933. [DOI] [PubMed] [Google Scholar]
- 116.Tung C.H., Mahmood U., Bredow S., Weissleder R. In vivo imaging of proteolytic enzyme activity using a novel molecular reporter. Cancer Res. 2000;60:4953–4958. [PubMed] [Google Scholar]
- 117.Klahan B., Seidi F., Crespy D. Oligo(thioether-ester)s blocks in polyurethanes for slowly releasing active payloads. Macromol. Chem. Phys. 2018;219:1800392. doi: 10.1002/macp.201800392. [DOI] [Google Scholar]
- 118.Tsuchikama K., An Z. Antibody-drug conjugates: Recent advances in conjugation and linker chemistries. Protein Cell. 2018;9:33–46. doi: 10.1007/s13238-016-0323-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wu G., Fang Y.Z., Yang S., Lupton J.R., Turner N.D. Glutathionemetabolism and its implications for health. J. Nutr. 2004;134:489–492. doi: 10.1093/jn/134.3.489. [DOI] [PubMed] [Google Scholar]
- 120.Taresco V., Alexander C., Singh N., Pearce A.K. Stimuli-responsive prodrug chemistries for drug delivery. Adv. Ther. 2018;1:1800030. doi: 10.1002/adtp.201800030. [DOI] [Google Scholar]
- 121.Yue D., Cheng G., He Y., Nie Y., Jiang Q., Cai X., Gu Z. Influence of reduction-senitive diselenide bonds and isulfide bonds on oligoethylenimine conjugates for gene delivery. J. Mater. Chem. 2014;2:7210–7221. doi: 10.1039/c4tb00757c. [DOI] [PubMed] [Google Scholar]
- 122.Mochida Y., Cabral H., Kataoka K. Polymeric micelles for targeted tumor therapy of Platinum anti-cancer drugs. Expert Opin. Drug Deliv. 2017;14:1423–1438. doi: 10.1080/17425247.2017.1307338. [DOI] [PubMed] [Google Scholar]
- 123.Zagorodko O., Arroyo-Crespo J.J., Nebot V.J., Vincent M.J. Polypeptide-based conjugates as therapeutics: Opportunities and challenges. Macromol. Biosci. 2017;17:1600316. doi: 10.1002/mabi.201600316. [DOI] [PubMed] [Google Scholar]
- 124.Ha J.H., Lee D.Y., Lee S.H., Yun C.O., Kim Y.C. Development of apoptsis-inducing polypeptide via simultaneous mitochondrial via membranę disruption and Ca2+ delivery. Biomaterials. 2019;197:51–59. doi: 10.1016/j.biomaterials.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 125.Chia-Hung C., Min-Liang K., Jen-Ling W., Wei-Chuan L., Li-Ching C., Leong-Perng C., Johnson L. CCM-AMI, a polyethylene glycol micelle with amifostine, as an acute radiation syndrome protectant in C57BL/6 Mice. Health Phys. 2015;109:242–248. doi: 10.1097/HP.0000000000000326. [DOI] [PubMed] [Google Scholar]
- 126.Wang C.H., Cheng C.Y., Chen C.H., Liao W.C. Chelating complex micelles for delivering cytoprotectant amifostine and its application in radiation protection. J. Pharmacovigil. 2018;6:3. [Google Scholar]
- 127.Bargh J.D., Isidro-Llobet A., Parker J.S., Spring D.R. Cleavable linkers in antibody-drug conjugates. Chem. Soc. Rev. 2019;48:4361. doi: 10.1039/C8CS00676H. [DOI] [PubMed] [Google Scholar]
- 128.Vrettos E.I., Mező G., Tzakos A.G. On the design principles of peptide-drug conjugates for targeted drug delivery to the malignant tumor site. Beilstein J. Org. Chem. 2018;14:930. doi: 10.3762/bjoc.14.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Walsh S.J., Bargh J.D., Dannheim F.M., Hanby A.R., Seki H., Counsell A.J., Ou X., Fowler E., Ashman N., Takada Y., et al. Site-selective modification strategies in antibody–drug conjugates. Chem. Soc. Rev. 2021;50:1305. doi: 10.1039/D0CS00310G. [DOI] [PubMed] [Google Scholar]
- 130.Bargh J.D., Walsh S.J., Isido-Llobet A., Omarjee S., Caroll J.S., Spring D.R. Sulfatase-cleavable linkers for antibody-drug conjugates. Chem. Sci. 2020;11:2375–2380. doi: 10.1039/C9SC06410A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lu J., Jiang F., Lu A., Zhang G. Linkers Having a Crucial Role in Antibody-Drug Conjugates. Int. J. Mol. Sci. 2016;17:561. doi: 10.3390/ijms17040561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Majumdar S., Siahaan T.J. Peptide-mediated targeted drug delivery. Med. Res. Rev. 2012;32:637. doi: 10.1002/med.20225. [DOI] [PubMed] [Google Scholar]
- 133.Staben L.R., Koenig S.G., Lehar S.M., Vandlen R., Zhang D., Chuh J., Yu S.F., Ng C., Guo J., Liu Y., et al. Targeted drug delivery through the traceless release of tertiary and heteroaryl amines from antibody-drug conjugates. Nat. Chem. 2016;8:1112. doi: 10.1038/nchem.2635. [DOI] [PubMed] [Google Scholar]
- 134.Anami Y., Yamazaki C.M., Xiong W., Gui X., Zhang N., An Z., Tsuchikama K. Glutamic acid–valine–citrulline linkers ensure stability and efficacy of antibody–drug conjugates in mice. Nat. Commun. 2018;9:2512. doi: 10.1038/s41467-018-04982-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Jeffrey S.C., Andreyka J.B., Bernhardt S.X., Kissler K.M., Kline T., Lenox J.S., Moser R.F., Nguyen M.T., Okeley N.M., Stone I.J., et al. Development and properties of beta-glucuronide linkers for monoclonal antibody-drug conjugates. Bioconjug. Chem. 2006;17:831. doi: 10.1021/bc0600214. [DOI] [PubMed] [Google Scholar]
- 136.Su Z., Xiao D., Xie F., Liu L., Wang Y., Fan S., Zhou X., Li S. Antibody-drug conjugates: Recent advances in linker chemistry. Acta Pharm. Sin. B. 2021;11:3889–3907. doi: 10.1016/j.apsb.2021.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Patel M.S., Nemeria N.S., Furey W., Jordan F. The pyruvate dehydrogenase complexes: Structure-based function and regulation. J. Biol. Chem. 2014;289:16615. doi: 10.1074/jbc.R114.563148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yin H., Zhang Q., Yang J., Wang H., Xu J., Zheng J. IRGD as a tumor-penetrating peptide for cancer therapy (Review) Mol. Med. Rep. 2017;15:2925–2930. doi: 10.3892/mmr.2017.6419. [DOI] [PubMed] [Google Scholar]
- 139.Ndagi U., Mhlongo N., Soliman M.E. Metal complexes in cancer therapy—An update from drug design perspective. Drug Des. Devel. Ther. 2017;11:599. doi: 10.2147/DDDT.S119488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hilchie A.L., Hoskin D.W. Power Coombs MR. Anti-cancer Activities of Natural and Synthetic Peptides. Adv. Exp. Med. Biol. 2019;1117:131. doi: 10.1007/978-981-13-3588-4_9. [DOI] [PubMed] [Google Scholar]
- 141.Glassman P.M., Muzykantov V.R. Pharmacokinetic and Pharmacodynamic Properties of Drug Delivery Systems. J. Pharmacol. Exp. Ther. 2019;370:570. doi: 10.1124/jpet.119.257113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Wang Y., Zhang X., Wan K., Zhou N., Wei G., Su Z. Supramolecular peptide nano-assemblies for cancer diagnosis and therapy: From molecular design to material synthesis and function-specific applications. J. Nanobiotechnol. 2021;19:253. doi: 10.1186/s12951-021-00999-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Gokhale A.S., Satyanarayanajois S. Peptides and peptidomimetics as immunomodulators. Immunotherapy. 2014;6:755. doi: 10.2217/imt.14.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Liu M., Fang X., Yang Y., Wang C. Peptide-Enabled Targeted Delivery Systems for Therapeutic Applications. Front. Bioeng. Biotechnol. 2021;9:701504. doi: 10.3389/fbioe.2021.701504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Akhtar M.J., Ahamed M., Alhadlaq H.A., Alrokayan S.A., Kumar S. Targeted anti-cancer therapy: Overexpressed receptors and nanotechnology. Clin. Chim. Acta. 2014;436:787. doi: 10.1016/j.cca.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 146.Mckertish C.M., Kayser V. Advances and Limitations of Antibody Drug Conjugates for Cancer. Biomedicines. 2021;9:872. doi: 10.3390/biomedicines9080872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Lucas A.T., Moody A., Schorzman A.N., Zamboni W.C. Importance and Considerations of Antibody Engineering in Antibody-Drug Conjugates Development from a Clinical Pharmacologist’s Perspective. Antibodies. 2021;10:30. doi: 10.3390/antib10030030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Worm D.J., Els-Heindl S., Beck-Sickinger A.G. Targeting of peptide-binding receptors on cancer cells with peptide-drug conjugates. Pept. Sci. 2020;112:e24171. doi: 10.1002/pep2.24171. [DOI] [Google Scholar]
- 149.Morales-Cruz M., Delgado Y., Castillo B., Figueroa C.M., Molina A.M., Torres A., Millian M., Griebenow K. Smart Targeting to Improve Cancer Therapeutics. Drug Des. Devel. Ther. 2019;13:3753. doi: 10.2147/DDDT.S219489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Kalimuthu K., Lubin B.C., Bazylevich A., Gellerman G., Shpilberg O., Luboshits G., Firer M.A. Gold nanoparticles stabilize peptide-drug-conjugates for sustained targeted drug delivery to cancer cells. J. Nanobiotechnol. 2018;16:34. doi: 10.1186/s12951-018-0362-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Lelle M., Frick S.U., Steinbrink K., Peneva K. Novel cleavable cel-penetrating peptide-drug conjugates: Synthesis and characteization. J. Pept. Sci. 2014;20:323–333. doi: 10.1002/psc.2617. [DOI] [PubMed] [Google Scholar]
- 152.Kaloyanova S., Lelle M., Mullen K., Peneva K. Branched cel-penetrating peptide drug conjugates for overcoming drug resistance. Eur. J. Cancer. 2014;50:S207–S208. doi: 10.1016/S0959-8049(14)50755-1. [DOI] [Google Scholar]
- 153.Hingorani D.V., Allevato M.M., Camargo M.F., Lesperance J., Quaraishi M.A., Aguilera J., Franiak-Pietryga I., Scanderberg D.J., Wang Z., Molinolo A.A., et al. Monomethyl auristatin antibody and peptide drug conjugates for trimodal cancer chemo-radio-immunotherapy. Nat. Commun. 2022;13:3869. doi: 10.1038/s41467-022-31601-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Apostolopoulos V., Stojanovska L., Gargosky S.E. MUC1 (CD227): A multi-tasked molecule. Cell. Mol. Life Sci. 2015;72:4475–4500. doi: 10.1007/s00018-015-2014-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Apostolopoulos V., Pietersz G.A., McKenzie I.F. MUC1 and breast cancer. Curr. Opin. Mol. Ther. 1999;1:98–103. [PubMed] [Google Scholar]
- 156.Apostolopoulos V., McKenzie I.F.C. Cellular mucins: Targets for immunotherapy. Crit. Rev. Immunol. 2017;37:421–437. doi: 10.1615/CritRevImmunol.v37.i2-6.110. [DOI] [PubMed] [Google Scholar]
- 157.Swaan P.W. Recent advances in intestinal macromolecular drug delivery via receptor-mediated transport pathways. Pharmaceut. Res. 1998;15:826–834. doi: 10.1023/A:1011908128045. [DOI] [PubMed] [Google Scholar]
- 158.Wang C.K., Nelepcu I., Hui D., Oo H.Z., Truong S., Zhao S., Tahiry Z., Esfandnia S., Ghaidi F., Adomat H., et al. Internalization and trafficking of CSPG-bound recombinant VAR2CSA lectins in cancer cells. Sci. Rep. 2022;12:3075. doi: 10.1038/s41598-022-07025-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Diez-Torrubia A., Cabrera S., de Castro S., Garcia-Aparicio C., Mulder G., De Meester I., Camarasa M.J., Balzarini J., Velazquez S. Novel water-soluble prodrugs of acyclovir cleavable by the dipeptidyl-peptidase IV (DPP IV/CD26) enzyme. Eur. J. Med. Chem. 2013;70:456. doi: 10.1016/j.ejmech.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 160.Liu N., Zhang Y., Lei Y., Wang R., Zhan M., Liu J., Zhou Y.A.Y., Zhan J., Yin F., Li Z. Design and evaluation of a novel peptide-drug conjugate covalently targeting SARS-CoV-2 papain-like protease. J. Med. Chem. 2022;65:876–884. doi: 10.1021/acs.jmedchem.1c02022. [DOI] [PubMed] [Google Scholar]
- 161.Baranyai Z., Kratky M., Vosatka R., Szabo E., Senoner Z., David S., Stolarikova J., Vinsova J., Bosze S. In vitro biological evaluation of new antimycobacterial salicylanilide-tuftsin conjugates. Eur. J. Med. Chem. 2017;133:152. doi: 10.1016/j.ejmech.2017.03.047. [DOI] [PubMed] [Google Scholar]
- 162.Long Y., Sun J., Song T.Z., Liu T., Tang F., Zhang X., Ding L., Miao Y., Weiliang Z., Xiaoyan P., et al. CoVac501, a self-adjuvanting peptide vaccine conjugated with TLR7 agonists, against SARS-CoV-2 induces protective immunity. Cell Discov. 2022;8:1. doi: 10.1038/s41421-021-00370-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Ferreira S.Z., Carneiro H.C., Lara H.A., Alves R.B., Resende J.M., Oliveira H.M., Silva L.M., Santos D.A., Freitas R.P. Synthesis of a new peptide-coumarin conjugate: A potential agent against cryptococcosis. ACS Med. Chem. Lett. 2015;6:271. doi: 10.1021/ml500393q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Wilkinson B.L., Day S., Malins L.R., Apostolopoulos V., Payne R.I. Self-adjuvanting multicomponent cancer candidates combining Per-glycosylated MUC1 glycopeptides and the toll-like receptor 2 agonist Pam3CysSer. Angew. Chem. Int. Ed. 2011;50:1635–1639. doi: 10.1002/anie.201006115. [DOI] [PubMed] [Google Scholar]
- 165.Shokri B., Zarghi A., Shahhoseini S., Mohammadi R., Kobarfard F. Design, synthesis and biological evaluation of peptide-NSAID conjugates for targeted cancer therapy. Arch. Pharm. 2019;352:e1800379. doi: 10.1002/ardp.201800379. [DOI] [PubMed] [Google Scholar]
- 166.Schieb H., Weidlich S., Schlechtingen G., Linning P., Jennings G., Gruner M., Wiltfang J., Klafki H.W., Knolker H.J. Structural design, solid-phase synthesis and activity of membrane-anchored ß-secretase inhibitors on Aß generation from wild-type and Swedish-mutant APP. Chem. Eur. J. 2010;16:14412. doi: 10.1002/chem.201002878. [DOI] [PubMed] [Google Scholar]
- 167.Tang Q., Cao B., Wu H., Cheng G. Cholesterol-peptide hybrids to form liposome-like vesicles for gene delivery. PLoS ONE. 2013;8:e54460. doi: 10.1371/journal.pone.0054460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Yi Y., Sanchez L., Gao Y., Yu Y. Janus particles for biological imaging and sensing. Analyst. 2016;141:3526. doi: 10.1039/C6AN00325G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Marriott B. Highlights of Prescribing Information. Regulatory Education for Industry. [(accessed on 3 November 2015)];2015 Available online: www.fda.gov.
- 170.Wang Z., Liang C., Shi F., He T., Gong C., Wang L., Yang Z. Cancer vaccines using supramolecular hydrogels of NSAID-modified peptides as adjuvants abolish tumorigenesis. Nanoscale. 2017;9:14058–14064. doi: 10.1039/C7NR04990K. [DOI] [PubMed] [Google Scholar]
- 171.Mohammadi R., Shokri B., Shamshirian D., Zarghi A., Shahhosseini S. Synthesis and biological evaluation of RGD conjugated with Ketoprofen/Naproxen and radiolabeled with [99mTc] via N4(GGAG) for αVβ3 integrin-targeted drug delivery. DARU. J. Pharm. Sci. 2020;28:87–96. doi: 10.1007/s40199-019-00318-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Park J.Y., Shin Y., Won W.R., Lim C., Kim J.C., Kang K., Husni P., Lee E.S., Youn Y.S., Oh K.T. Development of AE147 Peptide-Conjugated Nanocarriers for Targeting uPAR-Overexpressing Cancer Cells. Int. J. Nanomed. 2021;16:5437. doi: 10.2147/IJN.S315619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Szabo I., Bosze S., Orban E., Sipos E., Halmos G., Kovacs M., Mezo G. Comparative in vitro biological evaluation of daunorubicin containing GnRH-I and GnRH-II conjugates developed for tumor targeting. J. Pept. Sci. 2015;21:426. doi: 10.1002/psc.2775. [DOI] [PubMed] [Google Scholar]
- 174.Cheng H., Zhu J.Y., Xu X.D., Qiu W.X., Lei Q., Han K., Cheng Y.J., Zhang X.Z. Activable cell-penetrating peptide conjugated prodrug for tumor targeted drug delivery. ACS Appl. Mater. Interfaces. 2015;7:16061. doi: 10.1021/acsami.5b04517. [DOI] [PubMed] [Google Scholar]
- 175.Bera S., Zhanel G.G., Schweizer F. Synthesis and antibacterial activity of amphiphilic lysine-ligated neomycin B conjugates. Carbohydr. Res. 2011;346:560. doi: 10.1016/j.carres.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 176.Brezden A., Mohamed M.F., Nepal M., Harwood J.S., Kuriakose J., Seleem M.N., Chmielewski J. Dual Targeting of Intracellular Pathogenic Bacteria with a Cleavable Conjugate of Kanamycin and an Antibacterial Cell-Penetrating Peptide. J. Am. Chem. Soc. 2016;138:10945. doi: 10.1021/jacs.6b04831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Horváti K., Bacsa B., Szabó N., Fodor K., Balka G., Rusvai M., Kiss E., Mezo G., Grolmusz V., Vertessy B., et al. Antimycobacterial activity of peptide conjugate of pyridopyrimidine derivative against Mycobacterium tuberculosis in a series sssof in vitro and in vivo models. Tuberculosis. 2015;95:S207. doi: 10.1016/j.tube.2015.02.026. [DOI] [PubMed] [Google Scholar]
- 178.Pérez B.C., Teixeira C., Figueiras M., Gut J., Rosenthal P.J., Gomes J.R.B., Gomes P. Novel cinnamic acid/4-aminoquinoline conjugates bearing non-proteinogenic amino acids: Towards the development of potential dual action antimalarials. Eur. J. Med. Chem. 2012;54:887. doi: 10.1016/j.ejmech.2012.05.022. [DOI] [PubMed] [Google Scholar]
- 179.Mura F., Zuniga-Nunez D., Mallet J.M., Lavielle S., Matton P., Barrias P., Fuentealba D., Aspee A. A microenvironment-sensitive coumarin-labeled pepotde for the assessment of lipid-peptide interactions. Dye. Pigment. 2020;176:108234. doi: 10.1016/j.dyepig.2020.108234. [DOI] [Google Scholar]
- 180.Hilchie A.L., Vale R., Zemlak T.S., Hoskin D.W. Generation of a hematologic malignancy-selective membranolytic peptide from the antimicrobial core (RRWQWR) of bovine lactoferricin. Exp. Mol. Pathol. 2013;95:192. doi: 10.1016/j.yexmp.2013.07.006. [DOI] [PubMed] [Google Scholar]
- 181.Gao G., Wang Y., Hua H., Li D., Tang C. Marine Antitumor Peptide Dolastatin 10: Biological Activity, Structural Modification and Synthetic Chemistry. Mar. Drugs. 2021;19:363. doi: 10.3390/md19070363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Um W., Park J., Ko H., Lim S., Yoon H.Y., Shim M.K., Lee S., Ko Y.J., Kim M.J., Park J.H., et al. Visible light-induced apoptosis activatable nanoparticles of photosensitizer-DEVD-anticancer drug conjugate for targeted cancer therapy. Biomaterials. 2019;224:119494. doi: 10.1016/j.biomaterials.2019.119494. [DOI] [PubMed] [Google Scholar]
- 183.Huang Y., Li X., Sha H., Zhang L., Bian X., Han X., Liu B. Tumor-penetrating peptide fused to a pro-apoptotic peptide facilitates effective gastric cancer therapy. Oncol. Rep. 2017;37:2063. doi: 10.3892/or.2017.5440. [DOI] [PubMed] [Google Scholar]
- 184.Redko B., Tuchinsky H., Segal T., Tobi D., Luboshits G., Ashur-Fabian O., Pinhasov A., Gerlitz G., Gellerman G. Toward the development of a novel non-RG cyclic peptide drug conjugate for treatment of human metastatic melanoma. Oncotarget. 2017;8:757–768. doi: 10.18632/oncotarget.12748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Brunetti J., Pillozzi S., Falciani C., Depau L., Tenori E., Scali S., Lozzi L., Pini A., Arcangeli A., Menichetti S., et al. Tumor-selective peptide-carrier delivery of Paclitaxel increases in vivo activity of the drug. Sci. Rep. 2015;5:17736. doi: 10.1038/srep17736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Salem A.F., Wang S., Billet S., Chen J.-F., Udompholkul P., Gambini L., Baggio C., Tseng H.-R., Posadas E.M., Bhowmick N.A., et al. Reduction of Circulating Cancer Cells and Metastases in Breast-Cancer Models by a Potent EphA2-Agonistic Peptide-drug Conjugate. J. Med. Chem. 2018;61:2052. doi: 10.1021/acs.jmedchem.7b01837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Kuol N., Yan X., Barriga V., Karakkat J., Vassilaros S., Fyssas I., Tsimpanis A., Fraser S., Nurgali K., Apostolopoulos V. Pilot Study: Immune Checkpoints Polymorphisms in Greek Primary Breast Cancer Patients. Biomedicines. 2022;10:1827. doi: 10.3390/biomedicines10081827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Barriga V., Kuol K., Apostolopoulos V. The complex interaction between the tumor micro-environment and immune checkpoints in breast cancer. Cancers. 2019;11:1205. doi: 10.3390/cancers11081205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Kuol N., Stojanovska L., Nurgali K., Apostolopoulos V. PD-1/PD-L1 in disease. Immunotherapy. 2018;10:149–160. doi: 10.2217/imt-2017-0120. [DOI] [PubMed] [Google Scholar]
- 190.Kuol N., Stojanovska L., Nurgali K., Apostolopoulos V. The mechanisms tumor cells utilize to evade the host`s immune system. Maturitas. 2017;105:8–15. doi: 10.1016/j.maturitas.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 191.Xia H., Gu G., Hu Q., Liu Z., Jiang M., Kang T., Miao D., Song Q., Yao L., Tu Y., et al. Activatable cell penetrating peptide-conjugated nanoparticles with enhanced permeability for site-specific targeting delivery of anticancer drug. Bioconjug. Chem. 2013;20:419–430. doi: 10.1021/bc300520t. [DOI] [PubMed] [Google Scholar]
- 192.Zhu W., Bai Y., Zhang N., Yan J., Chen J., He Z., Sun Q., Pu Y., He B., Ye X. A tumor extracellular pH-sensitive PD-L1 binding peptide nanoparticle for chemo-immunotherapy of cancer. J. Mater. Chem. B. 2021;9:4201. doi: 10.1039/D1TB00537E. [DOI] [PubMed] [Google Scholar]
- 193.Liu M., Wang H., Liu L., Wang B., Sun G. Melittin-MIL-2 fusion protein as a candidate for cancer immunotherapy. J. Transl. Med. 2016;14:155. doi: 10.1186/s12967-016-0910-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Li M., Li M., Yang Y., Liu Y., Xie H., Yu Q., Tian L., Tang X., Ren K., Li J., et al. Remodeling tumor immune microenvironment via targeted blockade of PI3K-gamma and CSF-1/CSF-1R pathways in tumor associated macrophages for pancreatic cancer therapy. J. Control. Release. 2020;321:23. doi: 10.1016/j.jconrel.2020.02.011. [DOI] [PubMed] [Google Scholar]
- 195.Park C.C., Ali S., Janoff A.S., Meers P. Triggerable liposomal fusion by enzyme cleavage of a novel-lipid conjugate. Biochim. Biophys. Acta. 1998;1372:13–27. doi: 10.1016/s0005-2736(98)00041-8. [DOI] [PubMed] [Google Scholar]
- 196.Baines I.C., Colas P. Peptide aptamers as guides for small molecule drug discovery. Drug Discov. Today. 2006;11:334–341. doi: 10.1016/j.drudis.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 197.Hassanzadeganroudsari M., Soltani M., Heydarinasab A., Apostolopoulos V., Akbarzadehkhiyavi A., Nurgali K. Targeted nano-drug delivery system for glioblastoma therapy: In vitro and in vivo study. J. Drug Deliv. Sci. Technol. 2020;60:102039. doi: 10.1016/j.jddst.2020.102039. [DOI] [Google Scholar]
- 198.Maraming P., Daduang J., Yong Kah J.C. Conjugation with gold nanoparticles improves the stability of the KT2 peptide and maintains its anti-cancer properties. RSC Adv. 2022;12:319. doi: 10.1039/D1RA05980G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Park J., Choi Y., Chang H., Um W., Ryu J.H., Kwon I.C. Alliance with EPR Effect: Combined Strategies to Improve the EPR Effect in the Tumor Microenvironment. Theranostics. 2019;9:8073. doi: 10.7150/thno.37198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Jiang Z., Guan J., Qian J., Zhan C. Peptide ligand-mediated targeted drug delivery of nanomedicines. Biomater. Sci. 2019;7:461. doi: 10.1039/C8BM01340C. [DOI] [PubMed] [Google Scholar]
- 201.Caldwell C., Jr., Johnson C.E., Balaji V.N., Balaji G.A., Hammer R.D., Kannan R. Identification and Validation of a PD-L1 Binding Peptide for Determination of PDL1 Expression in Tumors. Sci. Rep. 2017;7:13682. doi: 10.1038/s41598-017-10946-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Lee S., Trinh T.H., Yoo M., Shin J., Lee H., Kim J., Hwang E., Lim Y.-B., Ryou C. Self-Assembling Peptides and Their Application in the Treatment of Diseases. Int. J. Mol. Sci. 2019;20:5850. doi: 10.3390/ijms20235850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Zhang L., Giraudo E., Hoffman J.A., Hanahan D., Ruoslahti E. Lymphatic zip codes in premalignant lesions and tumors. Cancer Res. 2006;66:5696–5706. doi: 10.1158/0008-5472.CAN-05-3876. [DOI] [PubMed] [Google Scholar]
- 204.Ferro-Flores G., Ramirez F.d.M., Melendez-Alafort L., Santos-Cuevas C.L. Peptides for in vitro target-specific cancer imaging. Med. Chem. 2010;10:87–97. doi: 10.2174/138955710791112596. [DOI] [PubMed] [Google Scholar]
- 205.Haubner R., Beer A., Wang H., Chen X. Positron emission tomography tracers for imaging angiogenesis. Eur. J. Nucl. Med. Mol. Imaging. 2010;37:86–103. doi: 10.1007/s00259-010-1503-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Kuil J., Velders A.H., van Leeuwen F.W.B. Multimodal tumor-targeting peptides functionalized with both a radio- and a fluorescent label. Bioconjug. Chem. 2010;21:1709–1719. doi: 10.1021/bc100276j. [DOI] [PubMed] [Google Scholar]
- 207.Mudd G.E., Brown A., Chen J., van Rietschoten K., Teufel D.P., Pavan S., Lani R., Huxley P., Bennett G.S. Identification and optimization of EphA2-selective bicycles for the delivery of cytotoxic payloads. J. Med. Chem. 2020;63:4107. doi: 10.1021/acs.jmedchem.9b02129. [DOI] [PubMed] [Google Scholar]
- 208.Sapra R., Verma R.P., Maurya G.P., Dhawan S., Babu J., Haridas V. Designer peptide and protein dendrimers: A cross-sectional analysis. Chem. Rev. 2019;119:11391. doi: 10.1021/acs.chemrev.9b00153. [DOI] [PubMed] [Google Scholar]
- 209.Li N., Li N., Yi Q., Luo K., Guo C., Pan D., Gu Z. Amphiphilic peptide dendritic copolymer-doxorubicin nanoscale conjugate self-assembled to enzyme-responsive anti-cancer agent. Biomaterials. 2014;35:9529. doi: 10.1016/j.biomaterials.2014.07.059. [DOI] [PubMed] [Google Scholar]
- 210.Carvalho M.R., Carvalho C.R., Maia F.R., Caballero D., Kundu S.C., Reis R.L., Oliveira J.M. Peptide-Modified Dendrimer Nanoparticles for Targeted Therapy of Colorectal Cancer. Adv. Ther. 2019;2:1900132. doi: 10.1002/adtp.201900132. [DOI] [Google Scholar]
- 211.Cooper B.M., Iegre J., O’Donovan D.H., Halvarsson M.O., Spring D.R. Peptides as a platform for targeted therapeutics for cancer: Peptide-drug conjugates. Chem. Soc. Rev. 2021;50:1480. doi: 10.1039/D0CS00556H. [DOI] [PubMed] [Google Scholar]
- 212.Brooks N.A., Pouniotis D.S., Sheng K.C., Apostolopoulos V., Pietersz G.A. A membrane penetrating multiple antigen peptide (MAP) incorporating ovalbumin CD8 epitope induces potent immune responses in mice. Biochim. Biophys. Acta Biomembr. 2010;12:2286–2295. doi: 10.1016/j.bbamem.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 213.Sheng K.C., Kalkanidis M., Pouniotis D.S., Esparon S., Tang C.K., Apostolopoulos V., Pietersz G.A. Delivery of antigen using a novel mannosylated dendrimer potentiates immunogenicity in vitro and in vivo. Eur. J. Immunol. 2008;38:424–436. doi: 10.1002/eji.200737578. [DOI] [PubMed] [Google Scholar]
- 214.Pouniotis D.S., Apostolopoulos V., Pietersz G.A. Penetration tandemly linked to a CTL peptide induces anti-tumour T-cell responses via a cross-presentation pathway. Immunology. 2005;117:329–339. doi: 10.1111/j.1365-2567.2005.02304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Apostolopoulos V., Pounotis D.S., van Maanen P.J., Andriessen R.W., Lodding J., Xing P.X., McKenzie I.F.C., Loveland B.E., Pietersz G.A. Delivery of tumor associated antigens to antigen presenting cells using penetratin induces potent immune responses. Vaccine. 2006;12:3191–3202. doi: 10.1016/j.vaccine.2006.01.032. [DOI] [PubMed] [Google Scholar]
- 216.Brooks N.A., Pouniotis D.S., Tang C.K., Apostolopoulos V., Pietersz G.A. Cell-penetrating peptides: Application in vaccine delivery. Biochim. Biophys. Acta Rev. Cancer. 2020;1805:25–34. doi: 10.1016/j.bbcan.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 217.Pouniotis D.S., Esparon S., Apostolopoulos V., Pietersz G.A. Whole protein and defined CD8+ and CD4+ peptides linked to penetratin targets both MHC class I and II antigen presentation pathways. Immunol. Cell Biol. 2011;89:904–913. doi: 10.1038/icb.2011.13. [DOI] [PubMed] [Google Scholar]
- 218.Pouniotis D., Tang C.K., Apostolopoulos V., Pietersz G. Vaccine delivery by penetratin: Mechanism of antigen presentation by dendritic cells. Immunol. Res. 2016;64:887–900. doi: 10.1007/s12026-016-8799-5. [DOI] [PubMed] [Google Scholar]
- 219.Hao M., Zhang L., Chen P. Membrane Internalization Mechanisms and Design Strategies of Arginine-Rich Cell-Penetrating Peptides. Int. J. Mol. Sci. 2022;23:9038. doi: 10.3390/ijms23169038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Del Genio V., Falanga A., Allard-Vannier E., Hervé-Aubert K., Leone M., Bellavita R., Uzbekov R., Chourpa I., Galdiero S. Design and Validation of Nanofibers Made of Self-Assembled Peptides to Become Multifunctional Stimuli-Sensitive Nanovectors of Anticancer Drug Doxorubicin. Pharmaceutics. 2022;14:1544. doi: 10.3390/pharmaceutics14081544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Miller D.S., Scambia G., Bondarenko I., Westermann A.M., Oaknin A., Oza A.M., Lisyanskaya A.S., Vergote I., Wenham R.M., Temkin S.M., et al. ZoptEC: Phase III randomized controlled study comparing zoptarelin with doxorubicin as second line therapy for locally advanced, recurrent, or metastatic endometrial cancer ( NCT01767155) J. Clin. Oncol. 2018;36:5503. doi: 10.1200/JCO.2018.36.15_suppl.5503. [DOI] [Google Scholar]
- 222.Engel J.B., Tinneberg H.R., Rick F.G., Berkes E., Schally A.V. Targeting of peptide cytotoxins to LHRH receptors for treatment of cancer. Curr. Drug Targets. 2016;17:488. doi: 10.2174/138945011705160303154717. [DOI] [PubMed] [Google Scholar]
- 223.Langer C.J., O’Byrne K.J., Socinski M.A., Mikhailov S.M., Lesniewski-Kmak K., Smakal M., Ciuleanu T.E., Orlov S.V., Dediu M., Heigener D., et al. Phase III trial comparing paclitaxel poliglumex (CT-2103, PPX) in combination with carboplatin versus standard paclitaxel and carboplatin in the treatment of PS 2 patients with chemotherapy-naïve advanced non-small cell lung cancer. J. Thorac. Oncol. 2018;3:623. doi: 10.1097/JTO.0b013e3181753b4b. [DOI] [PubMed] [Google Scholar]
- 224.Graybill W.S., Coleman R.L. Vintafolide: A novel targeted agent for epithelial ovarian cancer. Future Oncol. 2014;10:541. doi: 10.2217/fon.14.8. [DOI] [PubMed] [Google Scholar]
- 225.Balogh B., Ivanczi M., Nizami B., Beke-Somfai T., Mandity I.M. ConjuPeptDB: A database of peptide-drug conjugates. Nucl. Ac. Res. 2021;49:1. doi: 10.1093/nar/gkaa950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Therapeutics, Programs. [(accessed on 14 May 2020)]. Available online: https://www.bicycletherapeutics.com/programs/#bicycle-conjugates.
- 227.Fang Y., Wang H. Molecular Engineering of Peptide-drug Conjugates for Therapeutics. Pharmaceutics. 2022;14:212. doi: 10.3390/pharmaceutics14010212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Xu L., Xu S., Xiang T., Liu H., Chen L., Jiang B., Yao J., Zhu H., Hu R., Chen Z. Multifunctional building elemenst for the construction of peptide drug conjugates. Eng. Regen. 2022;3:92–109. [Google Scholar]
- 229.Fu C., Yu L., Miao Y., Liu X., Yu Z., Wei M. Peptide-drug conjugates (PDCs). A novel trend of research and development on targeted therapy, hype or hope? Acta Pharm. Sin. B. 2022 doi: 10.1016/j.apsb.2022.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.