Abstract
Natural hazards (NHs) associated with climate change have been increasing in frequency and intensity. These acute events impact humans both directly and through their effects on social and environmental determinants of health. Rather than relying on a fully reactive incident response disposition, it is crucial to ramp up preparedness initiatives for worsening case scenarios. In this perspective, we review the landscape of NH effects for human health and explore the potential of health informatics to address associated challenges, specifically from a preparedness angle. We outline important components in a health informatics agenda for hazard preparedness involving hazard-disease associations, social determinants of health, and hazard forecasting models, and call for novel methods to integrate them toward projecting healthcare needs in the wake of a hazard. We describe potential gaps and barriers in implementing these components and propose some high-level ideas to address them.
Keywords: climate change, hazard preparedness, health informatics, social determinants of health
INTRODUCTION
Natural hazards (NHs) pose a seasonal destructive threat to populations globally.1,2 Climate change has strong linkages to the increasing frequency and intensity of NHs.3 Since the 1960s, the annual average deaths from NHs dropped drastically,1 heightening focus on those living with comorbidities and mental trauma, difficulties thriving, and ultimately unready for another disaster. Marginalized and vulnerable populations, seen as having unmet social needs and intersectional experience with inequities, bear a disproportionate burden recovering from NHs.4 Yet capture and coverage of patient-level social determinants of health (SDoH) have lagged.5–8 With the increasing frequency of NHs disrupting communities, health informatics innovations are needed to support planning and adapting to NHs.
Climate changes in local environments can be separated into two general groups of phenomena: (1) changes that create conditions for more frequent and intense acute NHs and (2) gradual “slow-burn” changes that destabilize weather and land pattern (eg, glacial melt, sea-level rise, chronic aerosol exposures). While health effects of floods and coastal surges have been well-documented,9–11 climate change and compounded disasters may reveal previously under-reported effects. Forecasted heatwaves contribute to wildfire risks and long-term consequences of drought, food shortages, and worker safety risks.12–14 Poor mental health status spikes dramatically with disasters, adding mental trauma and suicide risks even among those indirectly affected.13 The Coronavirus Disease 2019 (COVID-19) pandemic reminded the world that prolonged occupational stress leads to burn-out and capacity shortage.15 Despite known effects of NHs (Table 1), health systems need a holistic data-driven approach to recognize pattern changes from climate change and impacts on SDoH and research information needs to empower policy and preparedness actions.
Table 1.
Known impacts of climate change on natural hazards associated with health effects
| Natural hazard | Impact of climate change on natural hazards | Health effects | Vulnerable or underserved populations at risk |
|---|---|---|---|
| Heat and heat waves |
|
||
| Hurricanes and floods |
|
||
| Wildfires | The population exposed to wildfire smoke has increased dramatically in the last 20 years.31 Parts of the world are projected to see a rise in area burned due to wildfire by 40%–100%.12,32 |
|
SDoH: social determinants of health.
Observational systems deployed in the ocean and land and satellite remote sensing systems inform early warning systems and evacuation to safety.16,17 Such systems generate high volumes of high-resolution data, requiring analytic tools like artificial intelligence (AI) to extract research insights. Yet, communities experiencing the intersection of multiple health inequities and social needs often bear a disproportionate burden recovering from disasters.18 Further improvements are needed to capture knowledge about SDoH and design strategies for resilience for those most vulnerable.7,19
In this perspective article, we focus on acute NHs (Table 1) that exacerbate the deterioration of SDoHs and present what biomedical/health informatics should support to integrate research capacities into preparedness.
TOWARD AN INFORMATICS AGENDA: GAPS, BARRIERS, AND RECOMMENDATIONS
From a preparedness perspective, the central need in the wake of an NH is the ability to send early warning messages and appropriately allocate first-response resources (eg, provider support, medications, debris removal). NHs are stochastic and forecasting healthcare utilization is highly complex owing to local environments and community structures. Traditional forecasting systems are agnostic of the local burden of disease and social needs in the communities. We posit that any such comprehensive forecasting system must comprise the following components:
C1. Localized syndromic surveillance models for NHs.
C2. Regular updates to SdoH and associated geographical distributions of vulnerable/underserved populations.
C3. High-resolution spatiotemporal models to predict NHs in the future.
C4. Methods to integrate syndromic surveillance models, demographic distributions, and NH prediction models.
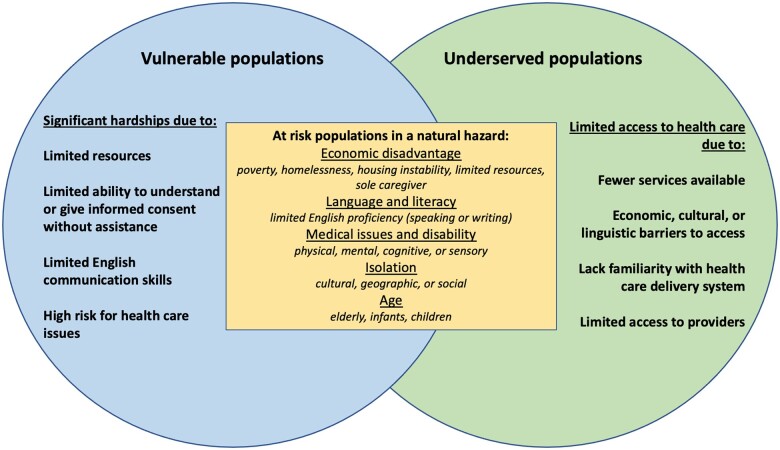
Before we elaborate on these components, we note that vulnerability can be defined differently depending on the context of the hazard of concern.42–45 For the purposes of this perspective, we rely on definitions of vulnerable and underserved populations by CDC and CMS to highlight groups most broadly at-risk to NHs (Figure 1). We acknowledge that marginalized communities often experience multiple health inequities—such as discrimination and barriers to basic resources—and historical underrepresentation within biomedical research. Highlighting notable gaps in research and data infrastructure, we propose high-level ideas to address barriers as a long-term call-to-action for the informatics community.
Figure 1.
At-risk populations in a natural hazard are populations at greater risk of negative health outcomes due to disparities in social determinants of health and/or physical health compared to the majority who are facing the same natural disaster.44 Adapted from: PUBLIC HEALTH WORKBOOK—To Define, Locate, and Reach Special, Vulnerable, and At-risk Populations in an Emergency46 and “Serving Vulnerable and Underserved Populations.” U.S. Centers for Medicare & Medicaid Services, Department of Health and Human Services.47
C1. Localized syndromic surveillance models for NHs
Healthcare resource allocation directly depends on the types of conditions that will see a major uptick. Therefore, it is imperative to build models that capture distributions of conditions in the wake of an NH by type. Retrospective case studies and survey-based estimates document salient trends from specific NHs by type (Table 1). As NHs reach greater intensity and duration, it is not apparent how historical syndromic patterns observed during prior events may under-extrapolate disease burden into new geographic settings for future projections. Expert intuitions may not capture all second-order effects of burden (eg, drug overdose deaths reached a record high in the United States during the COVID-19 pandemic48 despite having no direct relationship to COVID-19).
A comprehensive database of various NHs and associated distributions of conditions across time post-NH, ranging from a week to several months, is needed. Recent data sets provide the spatial-temporal information about NH-affected zones.1,49 What remains missing is health outcomes data combined with individual- and community-level SDoH. As of now, the US National Centers for Environmental Information tracks deaths and injuries from NHs and the National Syndromic Surveillance Program (NSSP) collects chief complaint data from nearly 6000 healthcare facilities and emergency departments.50 However, NSSP only constitutes 1/7th of US outpatient clinics;51 a collaboration between local healthcare facilities and state health information exchange may provide a fuller snapshot, although the roughly 10% of Americans without interactions with healthcare systems may be under-represented. Augmenting traditional surveillance data with social media platform may mitigate this representation issue.52,53 Social media usage and preferences vary between demographics, so it is crucial to consider the platforms’ diversity and representativeness. For example, in the United States, 46% of Hispanic Americans and only 16% of white Americans use WhatsApp54; Facebook, Twitter, and Instagram are amenable to crisis informatics research55 and connectivity cold-spot detection56 across demographics. This syndromic distribution database should be retrospectively collected for previous NHs and mined in real time to build a rich up-to-date resource for new NHs.
C2. Regular updates to SDoH and associated geographical distributions of vulnerable/underserved populations
Information collected from C1 may not be sufficient to extrapolate disease patterns beyond the location and population characteristics at the time. As such, it is important to gather appropriate snapshots of population characteristics. Different metrics have been adapted to use static representations of spatial risks,4,57 compute composite indices,58 and identify vulnerable population areas. This supports a known emergency response use case: identifying geographic areas with high concentrations of vulnerable/underserved people for triage.42,59 Unfortunately, census-based population estimates gathered every 10 years become less accurate as time progresses.60,61 Thus, there needs to be a focus on regular capture of changes in measures of SdoH in a population.
Regular, explicit updates of SDoH attributes are becoming more practical, and integration of SDoH data into clinical records is progressing.62–64 SDOH data from a population should ideally be captured at a rate sufficient to prepare for predictable NH periods, such as seasonal risks which might occur annually. Leveraging EMRs and HL7-FHIR infrastructure, public health surveillance can track SDoH variations across visits and healthcare facilities, which can then be aggregated for community-level measures. However, EMR-based coding of SDoH needs data quality and process improvement.65,66 Tools (eg, for clinical note processing) and vocabulary are needed to screen for discrimination by gender identity, employment and occupation status, and education opportunities. With appropriate incentives in-place,67 the data collection strategy would inform healthcare stakeholders with fresh snapshots of the patient population vulnerabilities, driving policy changes to promote disaster resilience.
C3. High-resolution spatiotemporal models to predict NHs in the future
C1 addresses the disease burden of NHs, but it lacks the capability to predict healthcare utilization events. Modeling NH risk is central to leveraging the other components to estimate future healthcare utilization. Recent disaster datasets provide spatial information and damage assessments of past NHs.1,49 While this is useful for follow-up inquiries for affected areas, it does not help with extending predictions to new areas. A full discussion of methods that forecast NHs is out-of-the-scope for this article but a recent survey by Ward et al2 highlights different approaches taken in this area. Recently, AI methods have been proposed to predict storm duration, severe wind, and severe hail in the near term.68 Deep neural networks have seen a major resurgence in unstructured data analysis and the same appears to hold true for weather forecasting.69 Jacques-Dumas et al70 use a convolutional neural network with transfer learning to predict extreme long-lasting heat waves with a 15-day lead time. Using the famous U-net convolutional architecture for image segmentation, Weyn et al71 generate 6-week subseasonal forecasts in 3 min, demonstrating NH prediction with a 4-day forecast for hurricane Irma, retrospectively. This work has been improved to model more variables and at 8 times higher resolution using the vision transformer architecture as the backbone.72 Application of the latest AI advances for NH prediction is still nascent and there is a serious call to create new benchmarks to rigorously test methods in this area.73
C4. Methods to integrate syndromic surveillance models, demographic distributions, and NH prediction models
If we know the risk of a particular NH occurring in an area (C3), based on the prior syndromic distribution for that NH (C1) and the current vulnerable demographic snapshot of that area (C2), healthcare utilization in the wake of that NH can be projected, analogous to the COVID-19 SEIR models.74 This involves developing novel methods to integrate different models and distributions (C1–C3) to map to utilization across disaster management phases. We posit that extra resource needs can be directly tied to uptick in diseases and hence we set out to model the distribution of diseases in a particular location at a given time of the year. Future distributions of diseases estimated from the combination of C1, C2, and C3 will enable local facilities to associate upticks in diseases with potential extra resources needed. Estimating model uncertainty arising out of the three component estimates will be challenging. In complex systems involving multiple interacting variables each carrying noise, uncertainty snowballs and lead to unreliable projections (eg, overshooting utilization leads to resource wastage). These aspects of uncertainty and complexity are the two main pillars identified from a consensus study of digital technologies and environmental sciences.75 In terms of specific methods, computer vision, causal inference, uncertainty quantification, transfer learning, and time series analysis have been put forward by AI scientists76 to handle climate change in general; these methods are pertinent in the context of joint modeling needed to integrate C1–C3.
CONCLUDING REMARKS
In this perspective, we reviewed climate change-induced NHs and associated disease burden. Subsequently, we identified gaps and barriers in appropriate resource allocation in the wake of such NHs and presented essential components central to an informatics strategy in mitigating adverse human health impacts. We conclude with some important considerations surrounding cost burden, interoperability, and privacy.
We note that federal and state health agencies may have to incur a major cost burden to materialize a resource planning system that aligns with our agenda. There is a value conflict between health system profit margins, adequate staffing, and organizational investment into disaster risk reduction for climate change response. However, the significant financial burden of handling climate and sensitive health outcomes during future climate crises may dwarf the upfront costs.77 Since climate crises disproportionately affect marginalized and vulnerable populations, there is merit in gauging the economic tradeoff of addressing the health harms in relation to the costs of inaction disproportionately felt by marginalized groups.78
This perspective has an implicit focus on the USA. However, the ongoing COVID-19 pandemic has demonstrated that international data sharing and collaboration are essential for rapid advances. As pointed out by a recent G7 health ministers' communique,2 striving toward standards for data sharing is essential while complying with international patient privacy regulations. Federated machine learning79 approaches ought to be considered to minimize concerns of data sharing and privacy breaches. Within the United States, at best the area deprivation index describes vulnerability as fine as the census block-group scale.80 Inadvertent private health information disclosures can occur if SDoH data are captured at the block-group scale. Although AI methods are bound to play a crucial operational role, unscrupulous use of AI algorithmic decision-making may exacerbate disparities.81,82 Deliberate considerations of the use of particular AI methods83 should be a top priority to avoid detrimental outcomes in mitigating the effects of climate change on human health.
FUNDING
This work was supported by US National Center for Advancing Translational Sciences Grants UL1TR001998 and U24TR002306 (including the supplement U24TR002306-04S3). The Office of Data Science Strategy, US NIH, provided funding for AYL as a Data and Technology Advancement (DATA) National Service Scholar. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
AUTHOR CONTRIBUTIONS
JP initiated the work and wrote the first draft of the paper with NOR contributing substantially with literature review, tables, and figures. RK conceived the perspective, including the high-level agenda proposed, and coordinated the writing efforts. All remaining authors contributed equally to the content, drafting, and revision and are hence listed in the alphabetical order.
ACKNOWLEDGEMENT
The authors especially thank technical advisor Bev Corwin, who provided editorial feedback for this article.
Conflict of interest statement
None declared.
Contributor Information
Jimmy Phuong, University of Washington, School of Medicine, Research Information Technologies, Seattle, Washington, USA; University of Washington, Harborview Injury Prevention and Research Center, Seattle, Washington, USA.
Naomi O Riches, University of Utah School of Medicine, Obstetrics and Gynecology Research Network, Salt Lake City, Utah, USA.
Luca Calzoni, National Institute on Minority Health and Health Disparities (NIMHD), National Institutes of Health, Bethesda, Maryland, USA; Department of Biomedical Informatics, University of Pittsburgh, Pittsburgh, Pennsylvania, USA.
Gora Datta, Department of Civil & Environmental Engineering, University of California at Berkeley, Berkeley, California, USA.
Deborah Duran, National Institute on Minority Health and Health Disparities (NIMHD), National Institutes of Health, Bethesda, Maryland, USA.
Asiyah Yu Lin, National Human Genome Research Institute (NHGRI), National Institutes of Health, Bethesda, Maryland, USA.
Ramesh P Singh, School of Life and Earth Sciences, Schmid College of Science and Technology, Chapman University, Orange, California, USA.
Anthony E Solomonides, Department of Communication Design, NorthShore University Health System, Outcomes Research Network, Research Institute, Evanston, Illinois, USA.
Noreen Y Whysel, New York City College of Technology, CUNY, Brooklyn, New York, USA.
Ramakanth Kavuluru, Division of Biomedical Informatics, Department of Internal Medicine, University of Kentucky, Lexington, Kentucky, USA.
Data Availability
No new data were generated or analyzed in support of this research.
REFERENCES
- 1. Shen G, Hwang SN.. Spatial–Temporal snapshots of global natural disaster impacts Revealed from EM-DAT for 1900-2015. Geomat Nat Hazards Risk. 2019; 10 (1): 912–34. [Google Scholar]
- 2. Ward PJ, Blauhut V, Bloemendaal N, et al. Natural hazard risk assessments at the global scale. Nat Hazards Earth Syst Sci. 2020; 20 (4): 1069–96. [Google Scholar]
- 3. United Nations. Climate and Weather Related Disasters Surge Five-Fold over 50 Years, But Early Warnings Save Lives—WMO Report. UN News; 2021. https://news.un.org/en/story/2021/09/1098662. Accessed April 17, 2022.
- 4. US EPA. EPA Report Shows Disproportionate Impacts of Climate Change on Socially Vulnerable Populations in the United States; 2021. https://www.epa.gov/newsreleases/epa-report-shows-disproportionate-impacts-climate-change-socially-vulnerable. Accessed April 3, 2022.
- 5. Hatef E, Rouhizadeh M, Tia I, et al. Assessing the availability of data on social and behavioral determinants in structured and unstructured electronic health records: a retrospective analysis of a multilevel health care system. JMIR Med Inform. 2019; 7 (3): e13802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Truong HP, Luke AA, Hammond G, et al. Utilization of social determinants of health ICD-10 z-codes among hospitalized patients in the United States, 2016–2017. Med Care. 2020; 58 (12): 1037–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Moscrop A, Ziebland S, Bloch G, et al. If social determinants of health are so important, shouldn’t we ask patients about them? BMJ. 2020; 371: m4150. [DOI] [PubMed] [Google Scholar]
- 8. Baker C, Chinaka O, Stewart EC.. The time is now: why we must identify and address health disparities in sport and recreation injury. Inj Epidemiol. 2021; 8 (1): 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lane K, Charles-Guzman K, Wheeler K, et al. Health effects of coastal storms and flooding in urban areas: a review and vulnerability assessment. J Environ Public Health. 2013; 2013: e913064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lowe D, Ebi KL, Forsberg B.. Factors increasing vulnerability to health effects before, during and after floods. Int J Environ Res Public Health. 2013; 10 (12): 7015–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alderman K, Turner LR, Tong S.. Floods and human health: a systematic review. Environ Int. 2012; 47: 37–47. [DOI] [PubMed] [Google Scholar]
- 12. Sun Q, Miao C, Hanel M, et al. Global heat stress on health, wildfires, and agricultural crops under different levels of climate warming. Environ Int. 2019; 128: 125–36. [DOI] [PubMed] [Google Scholar]
- 13. Palinkas LA, Wong M.. Global climate change and mental health. Curr Opin Psychol. 2020; 32: 12–6. [DOI] [PubMed] [Google Scholar]
- 14. Varghese BM, Hansen A, Bi P, et al. Are workers at risk of occupational injuries due to heat exposure? A comprehensive literature review. Saf Sci. 2018; 110: 380–92. [Google Scholar]
- 15. Dang A, Thakker R, Li S, et al. Hospitalizations and mortality from non-SARS-CoV-2 causes among medicare beneficiaries at US hospitals during the SARS-CoV-2 pandemic. JAMA Netw Open. 2022; 5 (3): e221754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Leaning J, Guha-Sapir D.. Natural disasters, armed conflict, and public health. N Engl J Med. 2013; 369 (19): 1836–42. [DOI] [PubMed] [Google Scholar]
- 17. Singh RP. Reflections on the 1900 Galveston Hurricane, Hurricane Harvey, and the Increase in Extreme Weather Events. From The Prow; 2017.https://fromtheprow.agu.org/reflections-1900-galveston-hurricane-hurricane-harvey-increase-extreme-weather-events/. Accessed April 13, 2022.
- 18. Aitsi-Selmi A, Egawa S, Sasaki H, et al. The Sendai Framework for disaster risk reduction: renewing the global commitment to people’s resilience, health, and well-being. Int J Disaster Risk Sci. 2015; 6 (2): 164–76. [Google Scholar]
- 19. Braveman P, Gottlieb L.. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014; 129 (suppl 2): 19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. US EPA. Climate Change Indicators: Heat-Related Deaths; 2016. https://www.epa.gov/climate-indicators/climate-change-indicators-heat-related-deaths. Accessed April 4, 2022.
- 21. US EPA. Climate Change Indicators: Heat Waves; 2021.https://www.epa.gov/climate-indicators/climate-change-indicators-heat-waves. Accessed April 5, 2022.
- 22. Arbuthnott KG, Hajat S.. The health effects of hotter summers and heat waves in the population of the United Kingdom: a review of the evidence. Environ Health. 2017; 16 (Suppl 1): 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jung J, Uejio CK, Kintziger KW, et al. Heat illness data strengthens vulnerability maps. BMC Public Health. 2021; 21 (1): 1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Li M, Gu S, Bi P, et al. Heat waves and morbidity: current knowledge and further direction-a comprehensive literature review. Int J Environ Res Public Health. 2015; 12 (5): 5256–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schwartz J. Who is sensitive to extremes of temperature?: A case-only analysis. Epidemiology. 2005; 16 (1): 67–72. [DOI] [PubMed] [Google Scholar]
- 26. O'Neill MS, Zanobetti A, Schwartz J.. Modifiers of the temperature and mortality association in seven US cities. Am J Epidemiol. 2003; 157 (12): 1074–82. [DOI] [PubMed] [Google Scholar]
- 27. Ting M, Kossin JP, Camargo SJ, Li C.. Past and future hurricane intensity change along the U.S. East Coast. Sci Rep. 2019; 9 (1): 7795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wing OEJ, Lehman W, Bates PD, et al. Inequitable patterns of US flood risk in the Anthropocene. Nat Clim Chang. 2022; 12 (2): 156–62. [Google Scholar]
- 29. Waddell SL, Jayaweera DT, Mirsaeidi M, et al. Perspectives on the health effects of hurricanes: a review and challenges. Int J Environ Res Public Health. 2021; 18 (5): 2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lindell MK, Prater CS.. Assessing community impacts of natural disasters. Nat Hazards Rev. 2003; 4 (4): 176–85. [Google Scholar]
- 31. Xu R, Yu P, Abramson MJ, et al. Wildfires, global climate change, and human health. N Engl J Med. 2020; 383 (22): 2173–81. [DOI] [PubMed] [Google Scholar]
- 32. Turco M, Rosa-Cánovas JJ, Bedia J, et al. Exacerbated fires in Mediterranean Europe due to anthropogenic warming projected with non-stationary climate-fire models. Nat Commun. 2018; 9 (1): 3821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Augusto S, Ratola N, Tarín-Carrasco P, et al. Population exposure to particulate-matter and related mortality due to the Portuguese wildfires in October 2017 driven by storm Ophelia. Environ Int. 2020; 144: 106056. [DOI] [PubMed] [Google Scholar]
- 34. DeFlorio-Barker S, Crooks J, Reyes J, et al. Cardiopulmonary effects of fine particulate matter exposure among older adults, during wildfire and non-wildfire periods, in the United States 2008-2010. Environ Health Perspect. 2019; 127 (3): 37006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Liu JC, Wilson A, Mickley LJ, et al. Wildfire-specific fine particulate matter and risk of hospital admissions in urban and rural counties. Epidemiology. 2017; 28 (1): 77–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wen B, Wu Y, Xu R, et al. Excess emergency department visits for cardiovascular and respiratory diseases during the 2019–20 bushfire period in Australia: a two-stage interrupted time-series analysis. Sci Total Environ. 2022; 809: 152226. [DOI] [PubMed] [Google Scholar]
- 37. Abdo M, Ward I, O’Dell K, et al. Impact of wildfire smoke on adverse pregnancy outcomes in Colorado, 2007–2015. Int J Environ Res Public health. 2019; 16 (19): 3720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Heft-Neal S, Driscoll A, Yang W, et al. Associations between wildfire smoke exposure during pregnancy and risk of preterm birth in California. Environ Res. 2022; 203: 111872. [DOI] [PubMed] [Google Scholar]
- 39. Reid CE, Brauer M, Johnston FH, et al. Critical review of health impacts of wildfire smoke exposure. Environ Health Perspect. 2016; 124 (9): 1334–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Grant E, Runkle JD.. Long-term health effects of wildfire exposure: a scoping review. J Clim Change Health. 2022; 6: 100110. [Google Scholar]
- 41. Cascio WE. Wildland fire smoke and human health. Sci Total Environ. 2018; 624: 586–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Balbus JM, Malina C.. Identifying vulnerable subpopulations for climate change health effects in the United States. J Occup Environ Med. 2009; 51 (1): 33–7. [DOI] [PubMed] [Google Scholar]
- 43. Tomio J, Sato H.. Emergency and disaster preparedness for chronically ill patients: a review of recommendations. Open Access Emerg Med. 2014; 6: 69–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Rukmana D. Vulnerable populations In: Michalos AC, ed. Encyclopedia of Quality of Life and Well-Being Research. Dordrecht: Springer Netherlands; 2014. 6989–92. doi: 10.1007/978-94-007-0753-5_3184. [DOI] [Google Scholar]
- 45. Butler DC, Petterson S, Phillips RL, et al. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res. 2013; 48 (2 Pt 1): 539–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Centers for Disease Control and Prevention (U.S). Office of Public Health Preparedness and Response, ed. Public Health Workbook to Define, Locate and Reach Special, Vulnerable, and At-Risk Populations in an Emergency. United States; 2010. https://emergency.cdc.gov/workbook/pdf/ph_workbookfinal.pdf. Accessed September 7, 2022.
- 47. Centers for Medicare & Medicaid Services. Serving Vulnerable and Underserved Populations. 2022. https://marketplace.cms.gov/technical-assistance-resources/training-materials/vulnerable-and-underserved-populations.pdf. Accessed April 13, 2022.
- 48. CDC. Drug Overdose Deaths in the U.S. Top 100,000 Annually; 2021. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm. Accessed April 17, 2022.
- 49. Rosvold EL, Buhaug H.. GDIS, a global dataset of geocoded disaster locations. Sci Data. 2021; 8 (1): 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. CDC. National Syndromic Surveillance Program (NSSP); 2021. https://www.cdc.gov/nssp/overview.html. Accessed April 17, 2022.
- 51.CBRE: Outpatient Centers on the Rise as Average Asking Rent for U.S. Medical Office Buildings Reaches Record High. https://www.cbre.com/press-releases/2018-medical-office-building-report. accessed April 17, 2022.
- 52. Finch KC, Snook KR, Duke CH, et al. Public health implications of social media use during natural disasters, environmental disasters, and other environmental concerns. Nat Hazards. 2016; 83 (1): 729–60. [Google Scholar]
- 53. Muniz-Rodriguez K, Ofori SK, Bayliss LC, et al. Social media use in emergency response to natural disasters: a systematic review with a public health perspective. Disaster Med Public Health Prep. 2020; 14 (1): 139–49. [DOI] [PubMed] [Google Scholar]
- 54. Auxier B, Anderson M. Social Media Use in 2021. Pew Research Center: Internet, Science & Tech2021.https://www.pewresearch.org/internet/2021/04/07/social-media-use-in-2021/ (accessed 12 Jul 2022).
- 55. Pine KH, Lee M, Whitman SA, et al. Making Sense of Risk Information amidst Uncertainty: Individuals’ Perceived Risks Associated with the COVID-19 Pandemic. In: Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems. New York, NY: Association for Computing Machinery; 2021: 1–15. doi: 10.1145/3411764.3445051 [DOI]
- 56. Maas P, Iyer S, Gros A, et al. Facebook Disaster Maps: Aggregate Insights for Crisis Response & Recovery. Spain: Universitat Politecnica de Valencia; 2019. http://inis.iaea.org/search/search.aspx?orig_q=RN:52117277
- 57. Benz SA, Burney JA.. Widespread race and class disparities in surface urban heat extremes across the United States. Earths Future. 2021; 9: e2021EF002016. [Google Scholar]
- 58. Cutter SL. The landscape of disaster resilience indicators in the USA. Nat Hazards. 2016; 80 (2): 741–58. [Google Scholar]
- 59. Phuong J, Bandaragoda CJ, Haldar S, et al. Information needs and priority use cases of population health researchers to improve preparedness for future hurricanes and floods. J Am Med Inform Assoc. 2021; 28 (2): 249–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Spielman SE, Tuccillo J, Folch DC, et al. Evaluating social vulnerability indicators: criteria and their application to the Social Vulnerability Index. Nat Hazards. 2020; 100 (1): 417–36. [Google Scholar]
- 61. Acosta RJ, Kishore N, Irizarry RA, et al. Quantifying the dynamics of migration after Hurricane Maria in Puerto Rico. Proc Natl Acad Sci U S A. 2020; 117 (51): 32772–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Phuong J, Riches NO, Madlock-Brown C, et al. Social determinants of health factors for gene–environment COVID-19 research: challenges and opportunities. Adv Genet. 2022; 3 (2): 2100056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Phuong J, Hong S, Palchuk MB, et al. Advancing interoperability of patient-level social determinants of health data to support COVID-19 research. AMIA Annu Symp Proc. 2022; 2022: 396–405. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9285174/. Accessed August 19, 2022. [PMC free article] [PubMed] [Google Scholar]
- 64. Holcomb J, Oliveira LC, Highfield L, et al. Predicting health-related social needs in Medicaid and Medicare populations using machine learning. Sci Rep. 2022; 12 (1): 4554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Cottrell EK, Dambrun K, Cowburn S, et al. Variation in electronic health record documentation of social determinants of health across a national network of community health centers. Am J Prev Med. 2019; 57 (6 Suppl 1): S65–S73. [DOI] [PubMed] [Google Scholar]
- 66. Cook LA, Sachs J, Weiskopf NG.. The quality of social determinants data in the electronic health record: a systematic review. J Am Med Inform Assoc. 2021; 29 (1): 187–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Palacio AM, Suarez M, del Toro Y, et al. Integrating social determinants of health into the electronic health records of a large health system: a qualitative perspective. Perspect Health Inf Manage. 2018; 1–19. [Google Scholar]
- 68. McGovern A, Elmore KL, Gagne DJ, et al. Using artificial intelligence to improve real-time decision-making for high-impact weather. Bull Am Meteorol Soc. 2017; 98 (10): 2073–90. [Google Scholar]
- 69. LeCun Y, Bengio Y, Hinton G.. Deep learning. Nature. 2015; 521 (7553): 436–44. [DOI] [PubMed] [Google Scholar]
- 70. Jacques-Dumas V, Ragone F, Borgnat P, et al. Deep learning-based extreme heatwave forecast. Front Clim. 2022; 4: 789641. https://www.frontiersin.org/articles/10.3389/fclim.2022.789641. Accessed Jul 12, 2022. [Google Scholar]
- 71. Weyn JA, Durran DR, Caruana R, et al. Sub-seasonal forecasting with a large ensemble of deep-learning weather prediction models. J Adv Model Earth Syst. 2021; 13 (7): e2021MS002502. [Google Scholar]
- 72. Pathak J, Subramanian S, Harrington P, et al. FourCastNet: A Global Data-Driven High-Resolution Weather Model using Adaptive Fourier Neural Operators; 2022. doi: 10.48550/arXiv.2202.11214. [DOI]
- 73. Dueben P, Schultz MG, Chantry M, et al. Challenges and benchmark datasets for machine learning in the atmospheric sciences: definition, status and outlook. Artif Intell Earth Syst. 2022; 1: 1–29. [Google Scholar]
- 74. Feng S, Feng Z, Ling C, et al. Prediction of the COVID-19 epidemic trends based on SEIR and AI models. PLoS One. 2021; 16 (1): e0245101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Blair GS, Bassett R, Bastin L, et al. The role of digital technologies in responding to the grand challenges of the natural environment: the Windermere Accord. Patterns. 2021; 2 (1): 100156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Rolnick D, Donti PL, Kaack LH, et al. Tackling climate change with machine learning. ACM Comput Surv. 2023; 55 (2): 1–96. [Google Scholar]
- 77. Limaye VS, Max W, Constible J, et al. Estimating the health-related costs of 10 climate-sensitive U.S. events during 2012. Geohealth. 2019; 3 (9): 245–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Limaye VS, Max W, Constible J, et al. Estimating the costs of inaction and the economic benefits of addressing the health harms of climate change. Health Aff. 2020; 39 (12): 2098–104. [DOI] [PubMed] [Google Scholar]
- 79. Rieke N, Hancox J, Li W, et al. The future of digital health with federated learning. NPJ Digit Med. 2020; 3: 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Kolak M, Bhatt J, Park YH, et al. Quantification of neighborhood-level social determinants of health in the continental United States. JAMA Netw Open. 2020; 3 (1): e1919928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Obermeyer Z, Powers B, Vogeli C, et al. Dissecting racial bias in an algorithm used to manage the health of populations. Science. 2019; 366 (6464): 447–53. [DOI] [PubMed] [Google Scholar]
- 82. Fiscella K, Franks P, Gold MR, et al. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. J Am Med Assoc. 2000; 283 (19): 2579–84. [DOI] [PubMed] [Google Scholar]
- 83. Solomonides AE, Koski E, Atabaki SM, et al. Defining AMIA’s artificial intelligence principles. J Am Med Inform Assoc. 2022; 29 (4): 585–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or analyzed in support of this research.