Abstract
While many case studies have described the implementation of self-scheduling tools, which allow patients to schedule visits and imaging studies asynchronously online, none have explored the impact of self-scheduling on equitable access to care.1 Using an electronic health record patient portal, University of California San Francisco deployed a self-scheduling tool that allowed patients to self-schedule diagnostic imaging studies. We analyzed electronic health record data for the imaging modalities with the option to be self-scheduled from January 1, 2021 to September 1, 2021. We used descriptive statistics to compare demographic characteristics and created a multivariable logistic regression model to identify predictors of patient self-scheduling utilization. Among all active patient portal users, Latinx, Black/African American, and non-English speaking patients were less likely to self-schedule studies. Patients with Medi-Cal, California’s Medicaid program, and Medicare insurance were also less likely to self-schedule when compared with commercially insured patients. Efforts to facilitate use of patient portal-based applications are necessary to increase equitability and decrease disparities in access.
Keywords: medical informatics applications, telehealth, eHealth, mobile Health, patient web portal
INTRODUCTION
Healthcare organizations have invested heavily in electronic health record (EHR) systems and patient portals, enabling new means of patient interaction and patient-centered care delivery.2,3 Through portals, patients communicate asynchronously with their care team about prior or upcoming visits, symptoms, test results, and medications.4 Patient portal messaging allows enhanced chronic disease self-management through improved care coordination.5 Ninety percent of all healthcare systems offer patient portals and in 2020, almost 40% of adults in the United States reported accessing their online medical record portal at least once in the prior year.3,6 The uptake of these portals, however, has not been evenly distributed across demographic groups, with older adults and those from minority backgrounds being less likely to enroll in patient portals.7–9 Barriers to using digital tools include limited internet access, low computer skills, and strong habits associated with face-to-face or phone scheduling.10 These barriers disproportionately impact certain racial, ethnic, and socioeconomic groups. Data on machine learning and online EHR-based portals have highlighted the potential for bias, suggesting that evaluations of new digital tools must include their impact on equity, disparity, and access.11,12
Self-scheduling tools are patient portal applications that allow patients to schedule visits and imaging studies asynchronously online or via an app.13 While many case studies have described the implementation of self-scheduling tools, few have quantified the disparities in patients’ use of these tools and completion of recommended studies.1,14 One systematic review found that web-based appointment systems showed positive impact on process metrics including no-show rates, staff labor, waiting times, and improved satisfaction.15,16 To our knowledge, none explore the impact of self-scheduling on equitable access to care.
Using an EHR-based patient portal, University of California San Francisco (UCSF) deployed a self-scheduling tool that allows patients to self-schedule imaging studies. The objective of this study was to understand the impact of a patient portal-based self-scheduling application for imaging studies on patient access and disparities.
MATERIALS AND METHODS
Setting
UCSF Health is a large academic medical center with approximately 45 000 hospital admissions and 2.1 million outpatient visits annually.
Tool
Since 2012 UCSF has used Epic (Epic Systems, Verona WI) as its EHR vendor. Among adult patients who receive ambulatory care at UCSF, 89% of patients are enrolled in their patient portal. In May 2020, UCSF implemented Epic’s patient portal-based self-scheduling tool through its patient portal, MyChart, enabling all UCSF ambulatory patients to self-schedule diagnostic imaging studies. Traditionally, patients could only schedule diagnostic imaging studies by calling the radiology department or walking into a radiology location during business hours. Self-scheduling was implemented in waves beginning in May 2020. By January 2021, self-scheduling had been implemented for all CT, MRI, DEXA, Mammography, and a subset of MRI and US studies. The self-scheduling tool was only available in English. An electronic self-scheduling ticket is generated that specifies the type of test, location, and date range for the test when a clinician orders an imaging study. Patients receive an email notification directing them to the patient portal where they can use the self-scheduling ticket to select from available dates, times, and locations to schedule the imaging study.
Data
Data were queried from the EHR and included the modality by which the test was scheduled (eg, self-scheduling ticket) and patient demographic information for all diagnostic imaging tests completed at UCSF Health between January 1, 2021 and September 1, 2021. The study period was chosen because self-scheduling for the imaging modalities included in this study had been implemented by January 2021. X-rays were excluded from this study because the majority of X-rays are completed via walk-in, and the data do not allow us to identify the small subset of scheduled X-rays. We therefore excluded X-rays from this study. Self-scheduling was only available to patients enrolled in MyChart. The study was approved by the UCSF Institutional Review and Ethics Board (21-35559).
Statistical analysis
We used descriptive statistics to compare the demographic characteristics of individuals who utilized the diagnostic imaging self-scheduling tool versus the traditional method of scheduling (mainly by phone). We substratified those who scheduled studies traditionally by portal and nonportal users. We used a chi-squared test to compare categorical variables and a t-test for continuous variables.
We created multivariable logistic regression model to identify predictors of patient self-scheduling utilization. Features of this model included imaging type, gender, age, race/ethnicity, marital status, language, and payor. Patients self-reported their race/ethnicity and gender. Significance level of <0.01 was used for the purposes of this study. All analyses were performed using R 3.5.
RESULTS
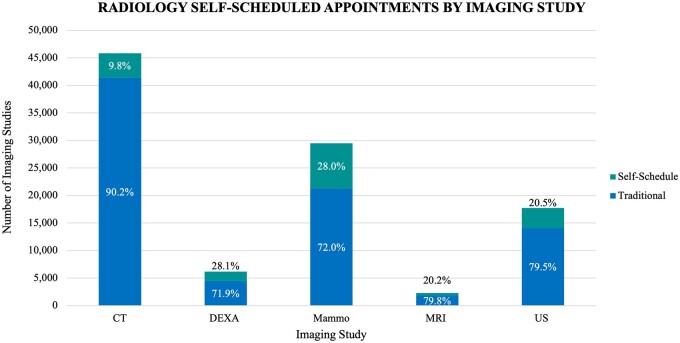
Between January 1, 2021 and September 1, 2021, 18 552 diagnostic imaging studies were scheduled using the self-scheduling tool in the patient portal. All differences except for patient age and nonbinary gender were statistically significant. Of these imaging studies, 44.5% (8247) were mammograms, 24.1% (4469) were CT scans, 19.6% (3643) were ultrasound studies, 9.3% (1731) were DEXA scans, and 2.5% (462) were MRI studies (Table 1). Over the same period, among patients who had access to the UCSF patient portal, 82 964 diagnostic imaging studies were scheduled via traditional methods (by phone, in-person). Of these imaging studies, 49.8% (41 356) were CT scans, 25.6% (21 248) were mammograms, and 17.0% (14 096) were US (Table 1). Of the imaging modalities, DEXA (28.1%) and Mammography (28.0%) had the highest rates of self-scheduling (Figure 1).
Table 1.
Comparing characteristics of patients who schedule imaging studies via self-schedule versus traditional modalities (eg, phone, in-person)
| All studies | All studies | ||||
|---|---|---|---|---|---|
| Portal and nonportal users |
Portal users only |
||||
| Traditional | Absolute percent difference |(traditional—self-schedule)| | Traditional | Self-schedule | Absolute percent difference |(traditional—self-schedule)| | |
| N | 95 712 | 82 964 | 18 552 | ||
| Imaging type | |||||
| CT | 45 512 (48.0%) | 24.0% | 41 356 (50.0%) | 4469 (24.0%) | 26.0% |
| DEXA | 5286 (5.5%) | 4.0% | 4437 (5.3%) | 1731 (9.3%) | 4.0% |
| Mammography | 25 274 (26.0%) | 18.0% | 21 248 (26.0%) | 8247 (44.0%) | 18.0% |
| MRI | 2069 (2.2%) | 0.3% | 1827 (2.2%) | 462 (2.5%) | 0.3% |
| US | 17 571 (18.0%) | 2.0% | 14 096 (17.0%) | 3643 (20.0%) | 0.3% |
| Race/ethnicity | |||||
| White or Caucasian | 50 823 (53.0%) | 4.0% | 45 609 (55.0%) | 10 490 (57.0%) | 2.0% |
| Asian | 20 052 (21.0%) | 2.0% | 17 818 (21.0%) | 4209 (23.0%) | 2.0% |
| Latinx | 11 441 (12.0%) | 3.2% | 9458 (11.0%) | 1639 (8.8%) | 2.2% |
| Black or African American | 5287 (5.5%) | 1.0% | 4076 (4.9%) | 857 (4.6%) | 0.3% |
| Multirace/ethnicity | 2126 (2.2%) | 0.2% | 1951 (2.4%) | 450 (2.4%) | 0.0% |
| Native Hawaiian or other Pacific Islander | 611 (0.6%) | 0.1% | 416 (0.5%) | 86 (0.5%) | 0.0% |
| American Indian or Alaska Native | 269 (0.3%) | 0.1% | 227 (0.3%) | 40 (0.2%) | 0.1% |
| Other | 2982 (3.1%) | 0.3% | 2334 (2.8%) | 520 (2.8%) | 0.0% |
| Unknown/declined | 2121 (2.2%) | 0.8% | 1075 (1.3%) | 261 (1.4%) | 0.1% |
| Gender | |||||
| Woman | 65 561 (68.0%) | 10.0% | 56 671 (68.0%) | 14 480 (78.0%) | 10.0% |
| Man | 30 062 (31.0%) | 9.0% | 26 211 (32.0%) | 4054 (22.0%) | 10.0% |
| Nonbinary | 8 (<0.1%) | 0.0% | 8 (<0.1%) | 5 (<0.1%) | 0.0% |
| Unknown | 81 (<0.1%) | 0.0% | 74 (<0.1%) | 13 (<0.1%) | 0.0% |
| Patient age | 58 (45,70) | 58 (45, 70) | 59 (49, 69) | ||
| Marital status | |||||
| Partnered | 54 731 (57.0%) | 4.0% | 49 902 (60.0%) | 11 366 (61.0%) | 1.0% |
| Single | 37 128 (39.0%) | 3.0% | 31 008 (37.0%) | 6720 (36.0%) | 1.0% |
| Unknown/declined | 3853 (4.0%) | 1.5% | 2054 (2.5%) | 466 (2.5%) | 0.0% |
| Language | |||||
| English | 85 701 (90.0%) | 5.0% | 75 846 (91.0%) | 17 539 (95.0%) | 5.0% |
| Other | 10 011 (10.0%) | 4.5% | 7118 (8.6%) | 1013 (5.5%) | 5.1% |
| Health insurance | |||||
| Commercial | 34 024 (36.0%) | 7.0% | 29 729 (36.0%) | 7976 (43.0%) | 7.0% |
| Medi-Cal/CC | 13 139 (14.0%) | 4.0% | 10 774 (13.0%) | 1935 (10.0%) | 3.0% |
| Medicare | 36 241 (38.0%) | 8.0% | 31 757 (38.0%) | 5657 (30.0%) | 8.0% |
| Other | 10 718 (11.0%) | 4.0% | 9573 (12.0%) | 2815 (15.0%) | 3.0% |
| Self-Pay | 1590 (1.7%) | 0.8% | 1131 (1.4%) | 169 (0.9%) | 0.5% |
Figure 1.
Radiology self-scheduled appointments by imaging study.
Among all active patient portal users, a higher proportion of patients who identified as Asian used the self-scheduling tool (23.0% vs 21.0%, P < .01). Patients who identified as Latinx were less likely to use the self-scheduling tool (8.8% vs 11.0%). This difference was slightly larger (8.8% vs 12.0%) when nonportal users were included. Patients identifying as women were more likely to use the self-scheduling tool (78.0% vs 68.0%, P < .01). A higher proportion of patients who self-scheduled were commercially insured (43.0% vs 36.0%, P < .01), and a lower proportion of patients who self-scheduled were insured by the state Medicaid program (10.0% vs 13.0%, P < .01) and Medicare (30.0% vs 38.0%, P < .01). When all active-patient portal users and nonportal users were included, there was a slightly larger difference among patients who self-scheduled studies and those who scheduled traditionally compared to when only portal users were included for both Black or African American and Latinx patients. In a secondary analysis, non-English speaking Latinx patients accounted for 2756 (24.0%) of the studies scheduled traditionally by Latinx patients and 123 (7.5%) of the studies self-scheduled online. Among all English-speaking patients, Latinx patients accounted for 7663 (10.0%) of studies scheduled traditionally and 1516 (8.6%) self-scheduled online.
In our multivariate model, the type of imaging study ordered was the primary predictor of whether the study would be self-scheduled. DEXA (OR 3.6, 95% confidence interval [CI] 3.4–3.8) and mammography (OR 3.5, CI 3.3–3.6) had the highest likelihood of self-scheduling. Latinx patients (OR 0.9, 95% CI 0.8–0.9), Black/African American patients (OR 0.9, 95% CI 0.8–1.0), and those whose primary language was not English (OR 0.7, 95% CI 0.7–0.8) had lower likelihoods of self-scheduling. Patients with Medi-Cal, Medicare, and self-pay patients were less likely to self-schedule when compared to commercially insured patients (Table 2). Interaction terms between age and insurance, age and imaging modality, and gender and imaging modality were added as a sensitivity analysis. While statistically significant, the terms had very low effect sizes and were excluded from the model.
Table 2.
Predictors of self-scheduling: multivariate regression model
| Odds ratio | 95% confidence interval | P-value | |
|---|---|---|---|
| Imaging modality (compared to CT) | |||
| DEXA | 3.6 | 3.4–3.8 | <.01 |
| Mammography | 3.5 | 3.3–3.6 | <.01 |
| MRI | 2.4 | 2.1–2.6 | <.01 |
| US | 2.4 | 2.3–2.6 | <.01 |
| Gender (compared to woman) | |||
| Man | 1.0 | 1.0–1.1 | .06 |
| Nonbinary | 3.5 | 1.0–10.9 | .04 |
| Unknown | 0.8 | 0.4–1.4 | .50 |
| Age (per year) | 1.0 | 1.0–1.0 | .54 |
| Race/ethnicity (compared to White) | |||
| Asian | 1.0 | 1.0–1.1 | .59 |
| Latinx | 0.9 | 0.8–0.9 | <.01 |
| Black or African American | 0.9 | 0.8–1.0 | <.01 |
| Multirace/ethnicity | 1.0 | 0.9–1.1 | .84 |
| Native Hawaiian or other pacific Islander | 0.8 | 0.7–1.1 | .15 |
| American Indian or Alaska Native | 0.9 | 0.6–1.3 | .61 |
| Other | 0.9 | 0.8–1.0 | .05 |
| Unknown/declined | 0.9 | 0.8–1.1 | .31 |
| Marital status (compared to partnered) | |||
| Single | 1.0 | 1.0–1.1 | .97 |
| Unknown | 0.9 | 0.8–1.0 | .81 |
| Language (compared to English) | |||
| Other | 0.7 | 0.7–0.8 | <.01 |
| Health insurance (compared to commercial) | |||
| Medi-Cal/CC | 0.9 | 0.8–0.9 | <.01 |
| Medicare | 0.7 | 0.7–0.7 | <.01 |
| Other | 1.1 | 1.0–1.1 | <.01 |
| Self-Pay | 0.7 | 0.6–0.8 | <.01 |
P values <.01 are considered significant and shaded in green.
DISCUSSION
Patient portal-based self-scheduling applications are an effective tool for patients who have access to and feel comfortable using online patient portals by allowing them to expeditiously schedule studies while decreasing the need for staff scheduler time.16,17 Our study found significant demographic differences among patients who self-scheduled and those who scheduled imaging studies through traditional phone and in-person methods. When all portal and nonportal users were included, the differences widened for certain demographic groups. Patients identifying as Asian and women were more likely to self-schedule while Latinx patients were less likely to self-schedule studies. In a multivariate model, primary language, self-reported ethnicity, and imaging study type were found to be significant predictors of self-scheduling. Our self-scheduling tool was only offered in English, which may account for the finding that non-English speaking patients were less likely to self-schedule imaging studies. DEXA and mammography studies were associated with highest likelihood of self-scheduling, which may be because patients schedule these tests several weeks and months in advance. Furthermore, a higher proportion of patients with Medicaid are from lower income and minority backgrounds while Medicare patients are more likely to be older adults.18 These patients were less likely to self-schedule compared to patients with commercial insurance, which may highlight the persistence of disparities even among patients who are considered to be active in their patient portal.
These data on the impact of a patient portal-based self-scheduling tool mirror studies in the literature on disparities in patient portal enrollment.7 Studies show that patients from racial or ethnic minority backgrounds, older adult patients, patient with low health literacy, and those experiencing lower socioeconomic status, chronic illness, or disability use patient portals less often.12 Given patient portals are increasingly used to seek advice and access care, differential use may exacerbate health inequities. While several studies outline the disparities in patient portal use, few have studied the additive impact of digital tools embedded within the electronic patient portal. This study demonstrates that disparities in use of a self-scheduling tool persisted even among patients who are considered enrolled in a patient portal. Ongoing systematic efforts to facilitate patient use of patient portal-based applications beyond enrollment will be necessary to ensure equitable access. Furthermore, health systems must invest in multilingual tools to facilitate access for patients with limited English proficiency.
Without concerted efforts to ensure equitable access to online patient portals beyond enrollment, digital tools such as self-scheduling applications have the potential to perpetuate disparities and may have tangible implications for the completion rates of imaging studies. These include screening studies like mammography, which may facilitate early detection of malignancy, and ultimately impact health outcomes. In areas where resources are scarce, such as access to coronavirus disease 2019 testing, vaccines, or urgent care visits, differential portal use may limit some patients’ access to life-saving testing or treatments. The data on interventions to address patient portal-based disparities are somewhat limited, but one review found evidence for using technical training and targeted assistance programs for patients.19 Another study corroborated that one-on-one patient training was associated with higher rates of patient portal use, but clinicians reported a lack of workflows to support portal use in routine practice.12
Limitations and future work
The self-scheduling tool was implemented in waves beginning May 2020 to April 2022. Our dataset included all imaging studies from January 2021 to September 2021, which may not have captured the impact of the tool at its steady state of utilization for all imaging modalities. Early adopters may represent a more technically savvy population which may not reflect the demographics of the population that uses to the tool after more widespread adoption. The number of self-scheduled studies relative to all imaging studies ordered was small, which limits our ability to draw broad-based conclusions about the effects of the tool on population health. In addition, the dataset lacks information about whether a healthcare proxy or family member helped patients schedule the study within the patient portal and lacks other metrics of patient portal use beyond self-scheduling of imaging studies. We also recognize that the demographic data labels in this dataset fail to capture the complexity of individuals’ identities and lived experiences. Further research is needed to understand the impact of digital tools embedded within online patient portal on health disparities, and to evaluate approaches to ensure equitable uptake of these tools.
CONCLUSIONS
In conclusion, studies have demonstrated that patient portals have the potential to improve patient engagement and outcomes but may also exacerbate health disparities. Our study adds to the literature by demonstrating disparate use of an online patient portal-based self-scheduling tool among individuals enrolled in their patient portal. Moving forward, health systems should focus on improving patient engagement with patient portals and digital tools by addressing underlying barriers, investing in multilingual tools, and continuously monitoring the impact of these tools on health disparities.
FUNDING
This work was supported by the Agency for Healthcare Research and Quality (K12HS026383), and the National Center for Advancing Translational Sciences (KL2TR001870).
AUTHOR CONTRIBUTIONS
All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the work to take public responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the manuscript. Furthermore, each author certifies that this material or similar material has not been and will not be submitted to or published in any other publication. Conception and Design of the study: SG, MK, WB, and AO. Acquisition of data: LP. Analysis and/or interpretation of data: LP, AO, and SG. Drafting the manuscript: SG. Revising the manuscript critically for important intellectual content: MM, TJ, AO, WB, MK, and SG.
CONFLICT OF INTEREST STATEMENT
None declared.
Contributor Information
Smitha Ganeshan, Center for Digital Health Innovation, University of California, San Francisco, San Francisco, California, USA; Department of Medicine, School of Medicine, University of California, San Francisco, San Francisco, California, USA.
Logan Pierce, Center for Digital Health Innovation, University of California, San Francisco, San Francisco, California, USA; Department of Medicine, School of Medicine, University of California, San Francisco, San Francisco, California, USA.
Michelle Mourad, Center for Digital Health Innovation, University of California, San Francisco, San Francisco, California, USA; Department of Medicine, School of Medicine, University of California, San Francisco, San Francisco, California, USA.
Timothy J Judson, Center for Digital Health Innovation, University of California, San Francisco, San Francisco, California, USA; Department of Medicine, School of Medicine, University of California, San Francisco, San Francisco, California, USA.
Marc D Kohli, Department of Radiology and Biomedical Imaging, School of Medicine, University of California, San Francisco, San Francisco, California, USA.
Anobel Y Odisho, Center for Digital Health Innovation, University of California, San Francisco, San Francisco, California, USA; Department of Urology, School of Medicine, University of California, San Francisco, San Francisco, California, USA.
William Brown, III, Center for Digital Health Innovation, University of California, San Francisco, San Francisco, California, USA; Department of Medicine, School of Medicine, University of California, San Francisco, San Francisco, California, USA; Bakar Computational Health Sciences Institute, University of California, San Francisco, San Francisco, California, USA.
DATA AVAILABILITY STATEMENT
Data cannot be shared publicly due to ethical/privacy reasons because the study used an identified patient dataset. The data will be shared on reasonable request to the corresponding author.
REFERENCES
- 1. Paré G, Trudel M-C, Forget P.. Adoption, use, and impact of e-booking in private medical practices: mixed-methods evaluation of a two-year showcase project in Canada. JMIR Med Inform 2014; 2 (2): e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.MGMA Stat: Most Practices Offer a Patient Portal. 2018. https://www.mgma.com/news-insights/quality-patient-experience/mgma-stat-most-practices-offer-a-patient-portal Accessed October 25, 2021.
- 3. Health Information Technology. HHS Should Assess the Effectiveness of Its Efforts to Enhance Patient Access to and Use of Electronic Health Information | U.S. GAO. https://www.gao.gov/products/gao-17-305 Accessed October 25, 2021.
- 4. Antonio MG, Petrovskaya O, Lau F.. The state of evidence in patient portals: umbrella review. J Med Internet Res 2020; 22 (11): e23851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hefner JL, MacEwan SR, Biltz A, Sieck CJ.. Patient portal messaging for care coordination: a qualitative study of perspectives of experienced users with chronic conditions. BMC Fam Pract 2019; 20 (1): 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hong YA, Jiang S, Liu PL. Use of patient portals of electronic health records remains low from 2014 to 2018: results from a national survey and policy implications. Am J Health Promot 2020; 34 (6): 677–80. [DOI] [PubMed]
- 7. Anthony DL, Campos-Castillo C, Lim PS.. Who isn’t using patient portals and why? Evidence and implications from a national sample of US adults. Health Aff (Millwood) 2018; 37 (12): 1948–54. [DOI] [PubMed] [Google Scholar]
- 8. Tuot DS, Leeds K, Murphy EJ, et al. Facilitators and barriers to implementing electronic referral and/or consultation systems: a qualitative study of 16 health organizations. BMC Health Serv Res 2015; 15 (1): 568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Denizard-Thompson NM, Feiereisel KB, Stevens SF, Miller DP, Wofford JL.. The digital divide at an urban community health center: implications for quality improvement and health care access. J Community Health 2011; 36 (3): 456–60. [DOI] [PubMed] [Google Scholar]
- 10. Zhang X, Yu P, Yan J. Patients’ adoption of the e-appointment scheduling service: a case study in primary healthcare. Stud Health Technol Inform2014; 204: 176–181. [PubMed] [Google Scholar]
- 11. Obermeyer Z, Powers B, Vogeli C, Mullainathan S.. Dissecting racial bias in an algorithm used to manage the health of populations. Science 2019; 366 (6464): 447–53. [DOI] [PubMed] [Google Scholar]
- 12. Lyles CR, Nelson EC, Frampton S, Dykes PC, Cemballi AG, Sarkar U.. Using electronic health record portals to improve patient engagement: research priorities and best practices. Ann Intern Med 2020; 172 (11 Suppl): S123–S129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Judson TJ, Odisho AY, Neinstein AB, et al. Rapid design and implementation of an integrated patient self-triage and self-scheduling tool for COVID-19. J Am Med Inform Assoc 2020; 27 (6): 860–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cao W, Wan Y, Tu H, et al. A web-based appointment system to reduce waiting for outpatients: a retrospective study. BMC Health Serv Res 2011; 11 (1): 318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhao P, Yoo I, Lavoie J, Lavoie BJ, Simoes E.. Web-based medical appointment systems: a systematic review. J Med Internet Res 2017; 19 (4): e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. North F, Nelson EM, Majerus RJ, Buss RJ, Thompson MC, Crum BA.. Impact of web-based self-scheduling on finalization of well-child appointments in a primary care setting: retrospective comparison study. JMIR Med Inform 2021; 9 (3): e23450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Han H-R, Gleason KT, Sun C-A, et al. Using patient portals to improve patient outcomes: systematic review. JMIR Hum Factors 2019; 6 (4): e15038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Guth M, Artiga S.. Medicaid and Racial Health Equity. San Francisco, CA: Kaiser Family Foundation; 2022. [Google Scholar]
- 19. Grossman LV, Masterson Creber RM, Benda NC, Wright D, Vawdrey DK, Ancker JS.. Interventions to increase patient portal use in vulnerable populations: a systematic review. J Am Med Inform Assoc 2019; 26 (8–9): 855–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data cannot be shared publicly due to ethical/privacy reasons because the study used an identified patient dataset. The data will be shared on reasonable request to the corresponding author.