Abstract
Background
Adverse childhood experiences (ACEs) are common and linked to negative health outcomes. Previous studies have found associations between ACEs and binge-eating disorder (BED), though they have mainly focused on adults and use cross-sectional data. The objective of this study was to examine the associations between ACEs and BED in a large, national cohort of 9–14-year-old early adolescents in the US.
Methods
We analyzed prospective cohort data from the Adolescent Brain Cognitive Development (ABCD) Study (N = 10,145, 2016–2020). Logistic regression analyses were used to determine the associations between self-reported ACEs and BED based on the Kiddie Schedule for Affective Disorders and Schizophrenia at two-year follow-up, adjusting for sex, race/ethnicity, baseline household income, parental education, site, and baseline binge-eating disorder.
Results
In the sample, (49% female, 46% racial/ethnic minority), 82.8% of adolescents reported at least one ACE and 1.2% had a diagnosis of BED at two-year follow-up. The mean number of ACEs was higher in those with a diagnosis of BED compared to those without (2.6 ± 0.14 vs 1.7 ± 0.02). The association between number of ACEs and BED in general had a dose–response relationship. One ACE (adjusted odds ratio [aOR] 3.48, 95% confidence interval [CI] 1.11–10.89), two ACEs (aOR 3.88, 95% CI 1.28–11.74), and three or more ACEs (aOR 8.94, 95% CI 3.01–26.54) were all associated with higher odds of BED at two-year follow-up. When stratified by types of ACEs, history of household mental illness (aOR 2.18, 95% 1.31–3.63), household violence (aOR 2.43, 95% CI 1.42–4.15), and criminal household member (aOR 2.14, 95% CI 1.23–3.73) were most associated with BED at two-year follow-up.
Conclusions
Children and adolescents who have experienced ACEs, particularly household challenges, have higher odds of developing BED. Clinicians may consider screening for ACEs and providing trauma-focused care when evaluating patients for BED.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40337-022-00682-y.
Keywords: Adolescent health, Adverse childhood experiences (ACEs), Binge-eating disorder
Plain English summary
Adverse childhood experiences (ACEs) are common among adolescents and a significant public health concern given their associations with various health outcomes later in life. The current study examined the associations between ACEs and binge-eating disorder (BED) among early adolescents using a large, national sample in the United States. Participants with three or more ACEs had nearly nine times higher odds of developing BED at two-year follow-up. Of the different types of ACEs, household mental illness, household violence, and having a criminal household member were most strongly associated with BED. Screening for ACEs when evaluating adolescents for BED should be considered, and clinicians should provide trauma-informed care for adolescents with BED.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40337-022-00682-y.
Background
Adverse childhood experiences (ACEs), defined as potentially traumatic abuse, neglect, and household challenges during childhood and adolescence, can have detrimental effects on health and wellbeing [1]. The prevalence of ACEs is high, with the Centers for Disease Control and Prevention (CDC) reporting nearly 61% of adults having experienced at least one type of ACE before age 18, and one in six adults having experienced four or more types of ACEs [2, 3]. Accumulating ACEs has been particularly linked to deleterious medical, mental health, and social outcomes [4, 5]. Given the high prevalence and ongoing public health burden of ACEs, additional studies and interventions are necessary to both elucidate and reduce their impact, as proposed by the American Academy of Pediatrics [6, 7].
A growing body of research has described relationships between ACEs and eating disorders (EDs). EDs, which include but are not limited to diagnoses such as anorexia nervosa, bulimia nervosa, and binge-eating disorder (BED), are complex psychiatric conditions associated with significant distress, medical comorbidities, and high mortality rates [8–10]. Previous studies have demonstrated associations between childhood trauma and EDs and disordered eating behaviors in adulthood [11–15]. For example, a national survey of adult men and women found higher rates of post-traumatic stress disorder (PTSD), sub-threshold PTSD, and exposure to any type of trauma among those with EDs, particularly BED [15]. In one cross-sectional, nationally representative sample of U.S. young adults (mean age 22 years), those with multi-type childhood maltreatment, reported a two-fold increase in the odds of binge-eating symptoms [13]. Another cross-sectional study using a clinical sample of adult patients receiving eating disorder treatment reported higher levels of ACEs among all patients with eating disorders, and those with BED had even higher levels of ACEs compared to those with anorexia nervosa, restricting subtype [16].
Despite bourgeoning research describing the relationship between ACEs and EDs, several important gaps remain. Because EDs typically develop between late adolescence and young adulthood, prior research has mainly focused adults and young adults [17, 18]. Recent studies have demonstrated BED, the most common eating disorder characterized by frequent episodes of food overconsumption, loss of control feelings of shame, and marked distress with episodes [19], often first presents in middle childhood and early adolescence [20]. Middle childhood and early adolescence are critical periods of psychosocial development vulnerable to the establish of health-related behaviors [21, 22]. Thus, early prevention and detection of BED in the early adolescent time period is crucial. Meta-analyses have found an overall estimated prevalence of 1.3% BED and 3.0% subclinical BED in children and adolescents [23]. Given links between BED and health outcomes such as obesity and depression [24, 25], both prevalent and high incidence conditions during adolescence [26, 27], further investigation is critical to understanding how binge-eating disorder develops in children.
The objective of this study was to determine the associations between number of ACEs and BED in a population-based, demographically diverse cohort of 9–14 year-old early adolescents and to determine which types of ACEs (i.e., abuse, neglect, household challenges) were most strongly associated with BED given the little research on individual ACEs and BED. We hypothesized that a greater number of ACEs would be associated with greater odds of BED in early adolescence.
Methods
Study population
We analyzed prospective data from the Adolescent Brain Cognitive Development (ABCD) Study, a longitudinal study of brain development and health across adolescence in 11,875 children recruited from 21 sites around the U.S. To recruit a sample representative of U.S. diversity, the ABCD study implemented epidemiologically-informed strategies largely through school systems and considering sociodemographic factors. Additional details are described elsewhere [28]. Data analyzed are from the ABCD 4.0 release for the baseline (2016–2018, 9–10-years-old) and two-year-follow-up (2018–2020, 10–14 years-old) assessments. Participants with missing data for ACEs during the study or BED at baseline and two-year follow-up were excluded, yielding the total sample of 10,145. We used Gaussian normal regression imputation to impute missing data for participants with missing confounder data. Centralized institutional review board (IRB) approval was obtained from the University of California, San Diego. Study sites obtained approval from their respective IRBs, caregivers provided written informed consent, and each child provided written assent. Data used in this study were obtained from the ABCD Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA).
Exposure: ACE score
ACE score was determined through parent and adolescent responses in the baseline (2016–2018), one-year follow-up (2017–2019), and the first half of two-year follow-up (2018–2019) surveys. The ABCD study assesses nine out of ten ACEs reflecting the items in the original CDC-Kaiser ACE study [4]; emotional abuse was not included as it was not evaluated in the ABCD study. A “yes” response to any of the following nine ACEs at any time point was counted as one point: physical abuse, sexual abuse, household violence, household mental illness, substance abuse in the household, divorce/separation, criminal household member, emotional neglect, and physical neglect. These points were totaled to yield an ACE score. Further details regarding the coding of ACE variables are presented in Additional file 1: Table 1. Previous literature has demonstrated increased deleterious outcomes with accumulated ACEs [4, 5].
Outcome: binge-eating disorder
BED was assessed at the two-year follow-up through the Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS-5), a computerized tool for categorizing child and adolescent mental health concerns based on the DSM-5 [19, 29]. Parents/caregivers completed all modules of the KSADS-5 to frequency, duration, characteristics of their child’s binge eating as well as associated distress. Using the KSADS-5 computerized scoring system, responses to the interview questions were extrapolated into their respective diagnosis from reported symptoms corresponding to the DSM-5 [19].
Confounders
We selected potential sociodemographic confounders for the association between screen time and behavioral disorders based on previous literature and theory [30]. Age (years), sex (female, male), race/ethnicity (White, Latino/Hispanic, Black, Asian, Native American, other), household income (U.S. dollars, six categories: Less than $25,000, $25,000 through $49,999, $50,000 through $74,999, $75,000 through $99,999, $100,000 through $199,999, $200,000 and greater), and highest parent education (high school or less vs. college or more) were based on baseline parents’ self-report. ABCD Study site was included as a confounder to adjust for potential regional variation. Diagnosis of binge-eating disorder at baseline was further included as a confounder.
Statistical analysis
Multiple logistic regression analyses were conducted in 2022 using Stata 15.1 (StataCorp, College Station, TX) to estimate associations between ACEs (exposure variable) and BED at two-year-follow-up (outcome variable), adjusting for confounders listed above. ACEs were analyzed as a cumulative score and individually in separate models. Propensity weights were applied to yield representative estimates based on the American Community Survey from the US Census [31]. Given previously studied relationships between trauma, BED, and other psychiatric disorders [15, 32, 33], additional sensitivity analyses were performed adjusting for baseline major depressive disorder, generalized anxiety disorder, and PTSD, with all findings unchanged.
Results
The descriptive characteristics of the 10,145 participants are shown in Table 1. The analytic sample was approximately matched by sex (49% female) and was racially and ethnically diverse (46% non-White). Four out of five participants reported a history of at least one ACE, and 9.71% reported four or more ACEs. The prevalence of BED at two-year follow-up was 1.16%.
Table 1.
Sociodemographic, adverse childhood experiences, and binge-eating disorder of 10,145 adolescent brain cognitive development (ABCD) study participants
| Sociodemographic characteristics (baseline) | Mean (SD)/% |
|---|---|
| Age (years) | 9.9 (0.6) |
| Sex, n (%) | |
| Female | 48.90 |
| Male | 51.10 |
| Race/ethnicity (%) | |
| White | 54.00 |
| Latino/Hispanic | 19.80 |
| Black | 16.10 |
| Asian | 5.40 |
| Native American | 3.20 |
| Other | 1.50 |
| Household income (%) | |
| Less than $25,000 | 16.20 |
| $25,000 through $49,999 | 20.50 |
| $50,000 through $74,999 | 18.30 |
| $75,000 through $99,999 | 16.50 |
| $100,000 through $199,999 | 21.80 |
| $200,000 and greater | 6.80 |
| Parent with college education or more (%) | 81.60 |
| Number of ACEs* | |
| 0 | 17.20 |
| 1 | 31.20 |
| 2 | 26.40 |
| 3 + | 25.21 |
| ACE subtype present | |
| Physical abuse | 1.07 |
| Sexual abuse | 1.22 |
| Emotional neglect | 1.57 |
| Physical neglect | 7.19 |
| Household substance use | 40.77 |
| Household divorce or separation | 17.24 |
| Household mental illness | 31.85 |
| Household violence | 55.59 |
| Criminal household member | 15.32 |
| Binge-eating disorder (baseline) | 0.57 |
| Binge-eating disorder (two-year follow-up) | 1.16 |
Propensity weights were applied to yield nationally representative estimates based on the American Community Survey from the US Census. SD = standard deviation
ACEs = Adverse Childhood Experiences
Figure 1 shows the mean number of ACEs in participants with and without a diagnosis of BED (2.6 ± 0.14 vs 1.7 ± 0.02). Adjusted logistic regression models examining the associations between ACE score and BED at two-year follow-up are presented in Table 2. One ACE (adjusted odds ratio [aOR] 3.48, 95% confidence interval [CI] 1.11–10.89), two ACEs (aOR 3.88, 95% CI 1.28–11.74), and three or more ACEs (aOR 8.94, 95% CI 3.01–26.54) were all associated with higher odds of BED at two-year follow-up. When stratified by types of ACEs, history of household mental illness (aOR 2.18, 95% 1.31–3.63), household violence (aOR 2.43, 95% CI 1.42–4.15), and criminal household member (aOR 2.14, 95% CI 1.23–3.73) were most associated with BED at two-year follow-up.
Fig. 1.
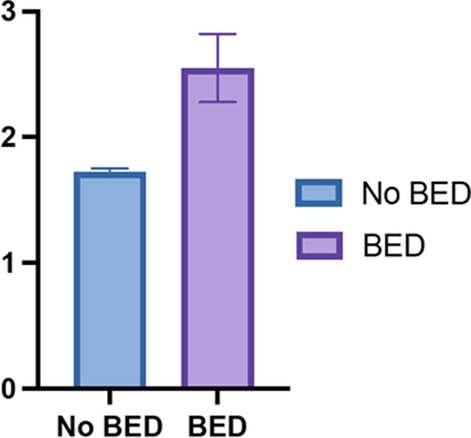
Mean number of ACEs among participants with and without BED
Table 2.
Associations between adverse childhood experiences (ACEs) and binge-eating disorder (BED) at two-year follow-up in the Adolescent Brain Cognitive Development Study
| BED | ||
|---|---|---|
| Adjusteda | ||
| OR (95% CI) | p | |
| Number of ACEs | ||
| 0 | REF | |
| 1 | 3.48 (1.11–10.89) | 0.032 |
| 2 | 3.88 (1.28–11.76) | 0.016 |
| 3 + | 8.94 (3.01–26.54) | < 0.001 |
| ACE subtypes | ||
| Physical abuse | 0.16 (0.01–2.37) | 0.181 |
| Sexual abuse | 0.94 (0.11–8.15) | 0.953 |
| Emotional neglect | 0.82 (0.16–4.30) | 0.811 |
| Physical neglect | 1.78 (0.84–3.79) | 0.135 |
| Household substance use | 1.16 (0.74–1.84) | 0.516 |
| Household divorce or separation | 0.92 (0.48–1.73) | 0.790 |
| Household mental illness | 2.18 (1.31–3.63) | 0.003 |
| Household violence | 2.43 (1.42–4.15) | 0.001 |
| Criminal household member | 2.14 (1.23–3.73) | 0.007 |
Bold indicates p < 0.05
aCovariates: race/ethnicity, sex, household income, parent education, site, and baseline BED
Discussion
In this population-based, demographically diverse sample of 10,145 9–14 year-old early adolescents in the US, the current study found that a greater number of ACEs was associated with BED in a dose-dependent manner, even after adjusting for confounders, including baseline BED. This finding confirms our hypothesis. The specific types of ACEs most strongly associated with BED at two-year follow-up were history of household mental illness, household violence, and a criminal household member.
These findings are congruent with prior research examining the relationship between ACEs and BED. However, whereas previous evidence has been confined to mostly cross-sectional clinical samples of adults receiving eating disorder treatment [11–13, 16], this study adds to the existing literature by: 1) using a large, national prospective cohort design with two-year-follow-up, 2) incorporating DSM-5 diagnosis of BED in children and adolescents, an important developmental period when long-term health behaviors are established, and 3) examining the specific types of ACEs most strongly associated with BED.
ACEs have been previously linked to several negative emotional, cognitive, and behavioral outcomes, which may help elucidate the mechanisms through which increased ACE score predisposes children and adolescents to develop BED [34]. For example, previous studies have found associations between higher levels of ACEs and negative urgency, which involves acting impulsively in times of extreme distress, alongside diminished inhibitory control [35]. Psychological models aiming to elucidate the pathways driving binge-eating behaviors describe how low self-esteem, negative affect, and difficulty with emotional regulation play a major role in their development [36], all of which have been demonstrated as psychological sequelae of ACEs [37–39]. Trauma may also have impacts on reward and inhibitory control networks [40], which has been implicated in pre-adolescent BED and in adult binge-type eating disorders [41, 42]. In a national sample of adult women, disinhibition was high in those with binge-type eating disorders, but even greater in those with comorbid PTSD, implicating the additional role of trauma on impulsivity [42]. Dissociation and depressive features associated with ACEs may further exacerbate the frequency and duration of binge-eating episodes and lead to the feelings of distress required for the diagnosis of BED [43–45]. Of note, in sensitivity analyses adjusting for baseline diagnosis of major depressive disorder, generalized anxiety disorder, and PTSD, the associations between higher number of ACEs with BED as well as specific ACE types with BED, remained unchanged.
The current study found that reported household mental illness, household violence, and having a criminal household member were all associated with BED in early adolescence. It is unclear why these specific ACEs appear to have a stronger association with BED than others. Prior studies have also attempted to examine whether certain ACEs serve as risk factors for specific eating disorders, but have reported mixed findings[11–14, 16, 46]. For instance, while some studies have found associations between different forms of childhood abuse with BED [16], others have focused on the role of neglect, such as childhood food neglect and emotional neglect [46]. The findings in the present study may reflect differences in prevalence of ACEs in different samples and different age groups. The inconsistent results underscore the need for further investigation into the role that specific ACEs may have in the development of BED.
Interestingly, household mental illness, household violence, and having a criminal household member all fall into the household dysfunction category of ACEs. This relationship may indicate a unique association between the role of the household unit and the development of binge-eating symptoms and subsequently, BED. In a community-based, case–control study of young adults with BED compared to healthy controls, parental depression was a major risk factor for BED [47]. The presence of familial and household relationships represents a central component for the emotional and developmental wellbeing of adolescents [48]. Higher familial functioning and parental support, which may not always be possible in situations involving household violence and criminal household members, have been shown to be protective of disordered eating behaviors [49]. Thus, strained relationships with family in the setting of household dysfunction may predispose individuals to BED.
Despite the strengths of the study, which include utilizing a large, diverse, and national cohort and a prospective study design, important limitations must be noted. First, although covariates were based on prior literature and theory, residual confounding remains possible. Second, given the observational study design, we cannot establish causality. Additionally, the ABCD study did not assess the severity of ACEs and also did not include questions about emotional abuse; thus, we were only able to examine nine out of the original ten ACEs that have been previously categorized [2, 4]. Furthermore, the evaluation of ACEs only determined exposure to different types of trauma, rather than the number of actual traumatic occurrences, which can be an important source of variance. This study also did not investigate recently expanded ACEs [50], which include living in foster homes, bullying, and experiencing racism. Finally, measures of BED were based on parent self-report, which may be subject to reporting bias. Although parent and child reports of binge eating have previously been shown to have low concordance [51, 52], parents are especially important reporters for EDs in this age range [53], since young children may have less insight regarding their eating behaviors [54].
Conclusion
ACEs remain a high-priority public health issue in the US. The Healthy People 2030 initiative recently added new objectives to reduce the prevalence of ACEs in young adults. Addressing the burden of ACEs and EDs such as BED is critical given the high prevalence of ACEs and the negative outcomes associated with EDs. Although there is limited evidence that universal screening of ACEs improves the identification of childhood adversity [6], clinicians may consider ACEs in those at risk for EDs. The findings from the current study highlight the need to consider ACEs and provide trauma-focused care when evaluating and treating children and adolescents with BED, which may improve the outcomes and lived experiences of those affected [55].
Supplementary Information
Additional file 1: Supplemental Table 1: Adverse Childhood Experiences (ACEs) Scale from the ABCD study.
Acknowledgements
The ABCD Study was supported by the National Institutes of Health and additional federal partners under award numbers U01DA041022, U01DA041025, U01DA041028, U01DA041048, U01DA041089, U01DA041093, U01DA041106, U01DA041117, U01DA041120, U01DA041134, U01DA041148, U01DA041156, U01DA041174, U24DA041123, and U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners/. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/principal-investigators.html. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in the analysis or writing of this report.
Abbreviations
- ABCD
Adolescent brain cognitive development study
- ACEs
Adverse childhood experiences
- EDs
Eating disorders
- BED
Binge-eating disorder
- CDC
Centers for Disease Control and Prevention
- PTSD
Post-traumatic stress disorder
- IRB
Institutional review board
- KSADS-5
Kiddie schedule for affective disorders and schizophrenia
Author contributions
JC conducted the analysis, drafted the manuscript, and edited the manuscript. JR cleaned the data, drafted parts of the manuscript, and provided critical revision of the manuscript. KG, AT, DJ, and SM provided critical revision of the manuscript. KW and AR conducted the literature review and provided critical revision of the manuscript. JN conceptualized the study, provided critical revision of the manuscript, and provided supervision. All authors approve the final manuscript.
Funding
J.M.N. was funded by the American Heart Association Career Development Award (CDA34760281), the National Institutes of Health (K08HL159350), and the Doris Duke Charitable Foundation (2022056). S.B.M. was supported by the National Institutes of Health (K23 MH115184). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Availability of data and materials
Data used in the preparation of this article were obtained from the ABCD Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA).
Declarations
Ethics approval and consent to participate
Centralized institutional review board (IRB) approval was obtained from the University of California, San Diego. Study sites obtained approval from their respective IRBs, caregivers provided written informed consent, and each child provided written assent.
Consent for publication
Not applicable.
Competing interests
The authors have no conflict to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bellis MA, Hughes K, Ford K, Ramos Rodriguez G, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Heal. 2019;4. [DOI] [PMC free article] [PubMed]
- 2.Preventing Adverse Childhood Experiences (ACEs): Leveraging the best available evidence. National center for injury prevention and control, centers for disease control and prevention. 2019.
- 3.Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of adverse childhood experiences from the 2011–2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatr. 2018;172. [DOI] [PMC free article] [PubMed]
- 4.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am J Prev Med. 2019;56. [DOI] [PubMed]
- 5.Testa A, Jackson DB. Adverse childhood experiences and food insecurity in adulthood: evidence from the national longitudinal study of adolescent to adult health. J Adolesc Heal. 2020;67. [DOI] [PubMed]
- 6.Loveday S, Hall T, Constable L, Paton K, Sanci L, Goldfeld S, et al. Screening for adverse childhood experiences in children: a systematic review. Pediatrics. 2022. [DOI] [PMC free article] [PubMed]
- 7.Jee SH, Steen M, Raynor J. Teaching interventions for adverse childhood experiences (ACEs): a systematic review. 2021.
- 8.O’Brien KM, Whelan DR, Sandler DP, Hall JE, Weinberg CR. Predictors and long-term health outcomes of eating disorders. PLoS One. 2017;12. [DOI] [PMC free article] [PubMed]
- 9.Santomauro DF, Melen S, Mitchison D, Vos T, Whiteford H, Ferrari AJ. The hidden burden of eating disorders: an extension of estimates from the Global Burden of Disease Study 2019. The Lancet Psychiatry. 2021;8. [DOI] [PMC free article] [PubMed]
- 10.van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiat. 2020. [DOI] [PMC free article] [PubMed]
- 11.Guillaume S, Jaussent I, Maimoun L, Ryst A, Seneque M, Villain L, et al. Associations between adverse childhood experiences and clinical characteristics of eating disorders. Sci Rep. 2016;6. [DOI] [PMC free article] [PubMed]
- 12.Caslini M, Bartoli F, Crocamo C, Dakanalis A, Clerici M, Carrà G. Disentangling the association between child abuse and eating disorders: a systematic review and meta-analysis. Psychosom. Med. 2016. [DOI] [PubMed]
- 13.Hazzard VM, Bauer KW, Mukherjee B, Miller AL, Sonneville KR. Associations between childhood maltreatment latent classes and eating disorder symptoms in a nationally representative sample of young adults in the United States. Child Abus Negl. 2019;98. [DOI] [PMC free article] [PubMed]
- 14.Ziobrowski HN, Buka SL, Austin SB, Duncan AE, Simone M, Sullivan AJ, et al. Child and adolescent maltreatment patterns and risk of eating disorder behaviors developing in young adulthood. Child Abus Negl. 2021;120. [DOI] [PMC free article] [PubMed]
- 15.Mitchell KS, Mazzeo SE, Schlesinger MR, Brewerton TD, Smith BN. Comorbidity of partial and subthreshold ptsd among men and women with eating disorders in the national comorbidity survey-replication study. Int J Eat Disord 2012. [DOI] [PMC free article] [PubMed]
- 16.Rienecke RD, Johnson C, Mehler PS, Le Grange D, Manwaring J, Duffy A, et al. Adverse childhood experiences among a treatment-seeking sample of adults with eating disorders. Eur Eat Disord Rev. 2022;30. [DOI] [PubMed]
- 17.Volpe U, Tortorella A, Manchia M, Monteleone AM, Albert U, Monteleone P. Eating disorders: what age at onset? Psychiatry Res 2016;238. [DOI] [PubMed]
- 18.Udo T, Grilo CM. Prevalence and correlates of DSM-5–defined eating disorders in a nationally representative sample of U.S. Adults Biol Psychiatry. 2018;84. [DOI] [PMC free article] [PubMed]
- 19.Sarmiento C, Lau C. Diagnostic and statistical manual of mental disorders, 5th Ed.: DSM‐5. Wiley Encycl Personal Individ Differ. 2020.
- 20.Murray SB, Ganson KT, Chu J, Jann K, Nagata JM. The prevalence of preadolescent eating disorders in the United States. J Adolesc Heal. 2022;70. [DOI] [PubMed]
- 21.Dorn LD, Hostinar CE, Susman EJ, Pervanidou P. Conceptualizing puberty as a window of opportunity for impacting health and well-being across the life span. J Res Adolesc. 2019;29. [DOI] [PubMed]
- 22.Dahl RE, Allen NB, Wilbrecht L, Suleiman AB. Importance of investing in adolescence from a developmental science perspective. Nature. 2018. [DOI] [PubMed]
- 23.Kjeldbjerg ML, Clausen L. Prevalence of binge-eating disorder among children and adolescents: a systematic review and meta-analysis. Eur Child Adolesc Psychiatry. 2021. [DOI] [PubMed]
- 24.de Zwaan M. Binge eating disorder and obesity. Int J Obes. 2001;25. [DOI] [PubMed]
- 25.Araujo DMR, Santos GFDS, Nardi AE. Binge eating disorder and depression: a systematic review. World J Biol Psychiatry. 2010. [DOI] [PubMed]
- 26.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Brief. 2017; [PubMed]
- 27.Ghandour RM, Sherman LJ, Vladutiu CJ, Ali MM, Lynch SE, Bitsko RH, et al. Prevalence and treatment of depression, anxiety, and conduct problems in US children. J Pediatr. 2019;206. [DOI] [PMC free article] [PubMed]
- 28.Garavan H, Bartsch H, Conway K, Decastro A, Goldstein RZ, Heeringa S, et al. Recruiting the ABCD sample: design considerations and procedures. Dev Cogn Neurosci. 2018;32. [DOI] [PMC free article] [PubMed]
- 29.Townsend L, Kobak K, Kearney C, Milham M, Andreotti C, Escalera J, et al. Development of three web-based computerized versions of the kiddie schedule for affective disorders and schizophrenia child psychiatric diagnostic interview: preliminary validity data. J Am Acad Child Adolesc Psychiatry. 2020;59. [DOI] [PubMed]
- 30.Willoughby T, Adachi PJC, Good M. A longitudinal study of the association between violent video game play and aggression among adolescents. Dev Psychol. 2012;48. [DOI] [PubMed]
- 31.Heeringa SG, Berglund PA. A guide for population-based analysis of the adolescent brain cognitive development (ABCD) study baseline data. bioRxiv. 2020.
- 32.Convertino AD, Blashill AJ. Psychiatric comorbidity of eating disorders in children between the ages of 9 and 10. J Child Psychol Psychiatry Allied Discip. 2022;63. [DOI] [PubMed]
- 33.Merrick MT, Ports KA, Ford DC, Afifi TO, Gershoff ET, Grogan-Kaylor A. Unpacking the impact of adverse childhood experiences on adult mental health. Child Abus Negl. 2017;69. [DOI] [PMC free article] [PubMed]
- 34.Herzog JI, Schmahl C. Adverse childhood experiences and the consequences on neurobiological, psychosocial, and somatic conditions across the lifespan. Front. Psychiatry. 2018. [DOI] [PMC free article] [PubMed]
- 35.Shin SH, McDonald SE, Conley D. Profiles of adverse childhood experiences and impulsivity. Child Abus Negl. 2018;85. [DOI] [PMC free article] [PubMed]
- 36.Burton AL, Abbott MJ. Processes and pathways to binge eating: Development of an integrated cognitive and behavioural model of binge eating. J Eat Disord. 2019;7. [DOI] [PMC free article] [PubMed]
- 37.Rudenstine S, Espinosa A, McGee AB, Routhier E. Adverse childhood events, adult distress, and the role of emotion regulation. Traumatology (Tallahass Fla). 2019;25.
- 38.Kim Y, Lee H, Park A. Patterns of adverse childhood experiences and depressive symptoms: self-esteem as a mediating mechanism. Soc Psychiatry Psychiatr Epidemiol. 2022;57. [DOI] [PMC free article] [PubMed]
- 39.Von CE, Sinnott C, Dahly D. Kearney PM. Perceived social support as a potential protective factor. BMJ Open: Adverse childhood experiences (ACEs) and later-life depression; 2017. p. 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Seidemann R, Duek O, Jia R, Levy I, Harpaz-Rotem I. The reward system and post-traumatic stress disorder: does trauma affect the way we interact with positive stimuli? Chronic Stress. 2021. [DOI] [PMC free article] [PubMed]
- 41.Murray SB, Alba C, Duval CJ, Nagata JM, Cabeen RP, Lee DJ, et al. Aberrant functional connectivity between reward and inhibitory control networks in pre-adolescent binge eating disorder. Psychol Med. 2022; [DOI] [PubMed]
- 42.Brewerton TD, Cotton BD, Kilpatrick DG. Sensation seeking, binge-type eating disorders, victimization, and PTSD in the National Women’s Study. Eat Behav. 2018;30. [DOI] [PubMed]
- 43.Wagner-Skacel J, Riedl D, Kampling H, Lampe A. Mentalization and dissociation after adverse childhood experiences. Sci Rep. Nature Research; 2022;12. [DOI] [PMC free article] [PubMed]
- 44.Palmisano GL, Innamorati M, Vanderlinden J. Life adverse experiences in relation with obesity and binge eating disorder: A systematic review. J Behav Addict 2016. [DOI] [PMC free article] [PubMed]
- 45.Palmisano GL, Innamorati M, Sarracino D, Bosco A, Pergola F, Scaltrito D, et al. Trauma and dissociation in obese patients with and without binge eating disorder: a case–control study. Cogent Psychol. 2018;5.
- 46.Amianto F, Spalatro AV, Rainis M, Andriulli C, Lavagnino L, Abbate-Daga G, et al. Childhood emotional abuse and neglect in obese patients with and without binge eating disorder: Personality and psychopathology correlates in adulthood. Psychiatry Res. 2018;269. [DOI] [PubMed]
- 47.Fairburn CG, Doll HA, Welch SL, Hay PJ, Davies BA, O’Connor ME. Risk factors for binge eating disorder: A community-based, case-control study. Arch Gen Psychiatry. 1998;55. [DOI] [PubMed]
- 48.Guevara RM, Moral-García JE, Urchaga JD, López-García S. Relevant factors in adolescent well-being: family and parental relationships. Int J Environ Res Public Health. 2021;18. [DOI] [PMC free article] [PubMed]
- 49.Berge JM, Wall M, Larson N, Eisenberg ME, Loth KA, Neumark-Sztainer D. The unique and additive associations of family functioning and parenting practices with disordered eating behaviors in diverse adolescents. J Behav Med. 2014;37. [DOI] [PMC free article] [PubMed]
- 50.Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, et al. Adverse childhood experiences: expanding the concept of adversity. Am J Prev Med. 2015;49. [DOI] [PubMed]
- 51.Bartholdy S, Allen K, Hodsoll J, O’Daly OG, Campbell IC, Banaschewski T, et al. Identifying disordered eating behaviours in adolescents: how do parent and adolescent reports differ by sex and age? Eur Child Adolesc Psychiatry. 2017;26. [DOI] [PMC free article] [PubMed]
- 52.Tanofsky-Kraff M, Yanovski SZ, Yanovski JA. Comparison of child interview and parent reports of children’s eating disordered behaviors. Eat Behav. 2005;6. [DOI] [PMC free article] [PubMed]
- 53.Barch DM, Albaugh MD, Avenevoli S, Chang L, Clark DB, Glantz MD, et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: Rationale and description. Dev Cogn Neurosci 2018. [DOI] [PMC free article] [PubMed]
- 54.Braet C, Soetens B, Moens E, Mels S, Goossens L, Van Vlierberghe L. Are two informants better than one? Parent-child agreement on the eating styles of children who are overweight. Eur Eat Disord Rev. 2007;15. [DOI] [PubMed]
- 55.Brewerton TD, Alexander J, Schaefer J. Trauma-informed care and practice for eating disorders: personal and professional perspectives of lived experiences. Eat Weight Disord. 2019;24. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplemental Table 1: Adverse Childhood Experiences (ACEs) Scale from the ABCD study.
Data Availability Statement
Data used in the preparation of this article were obtained from the ABCD Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA).


