Abstract
Background
Controversial data on the effects of vitamins (V) and nutrients on the management of type 2 diabetes mellitus (T2DM) is available. Thus, it is aimed to clarify the role of vitamins and nutrients through an umbrella review regarding the available observational/ trials meta-analyses.
Methods
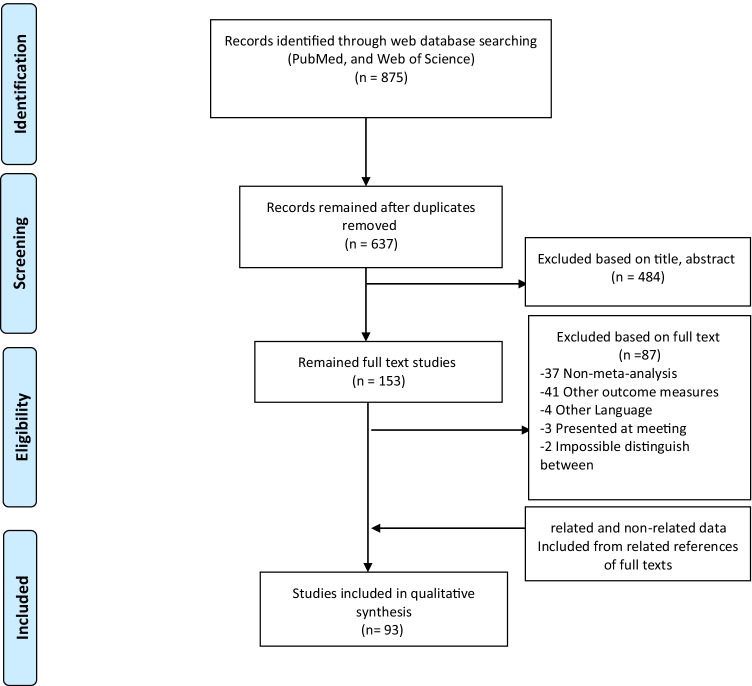
All meta-analyses of observational and clinical trials conducted on the impact of vitamins and nutrients in T2DM published until 5th June 2021 in PubMed or Web of Sciences were included in this review. Also, the meta-analysis on children, pregnant women, type 1 DM, or in vivo/in vitro studies was excluded. Search results were reported according to the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) flowchart.
Results
The overall of 93 papers (99 studies) consisting of 75 trials and 24 observational studies were included. Most studies were conducted on the effect of VD and alpha-lipoic acid (ALA) in both genders. Consumption of VD or its analogous; 20 IU/d to 450,000 IU/once for 3 weeks to 7 years showed to have a positive effect on the parameters of glucose hemostasis. Moreover, an inverse association was observed between VD level and T2DM risk. Daily consumption of 1200 mg VC for at least 12 weeks improved lipid profile and glucose hemostasis parameters. Furthermore, VB and medications for diabetic polyneuropathy (DPN) increased nerve conduction velocity. Vitamins K and E were showen to not have significant impact on T2DM. ALA had a beneficial effect on DPN symptoms after 2–4 weeks of intake of at least 300 mg/d. T2DM risk was reduced by doubling ALA intake. The effective daily doses of chromium, zinc and coenzyme Q10 on lipid profile and glucose hemostasis parameters were > 200 mg, < 25 mg, and < 200 mg, respectively.
Conclusion
This umbrella review suggests that dietary vitamins and nutrients can result in protective impacts the complications associated with T2DM. However, due to discrepancies between the results of the trials and observational studies is essential to conduct long-term high-qualified studies to prove the beneficial therapeutic effects of the vitamins and nutrients on T2DM and its complications.
Keywords: Antioxidants, Diabetes complications, Diabetes mellitus, Dietary supplements, Umbrella review
Background
Diabetes mellitus (DM) is a chronic multifactorial metabolic disorder with an increasing global prevalence, which is expected to rise from 537 million cases in 2021 to 783 million by 2045 [1]. It has been established that oxidative stress plays a crucial role in the pathogenesis of DM and its complications through cellular damage [2]. Under cellular damage condition, reactive oxygen species (ROS) are produced, which can be suppressed by the antioxidative defense system [3], and can be modified by enzymatic antioxidants such as glutathione peroxidase, or non-enzymatic antioxidants including vitamins and minerals [4].
Various studies have been conducted on patients with DM to investigate the effects of antioxidant vitamins on ROS. Also, numerous epidemiological studies showed significant negative associations between serum concentrations of these antioxidants and risk of diabetes and its complications [5, 6]. However, some findings are inconsistent, and the positive effects of antioxidants are far from exclusive [7, 8]. Consumption of vitamin D (VD) and its analogous improved glycemic status [9], however another meta-analysis study did not show the same beneficial impact [10]. Similarly, inconsistent results were reported in other meta-analysis studies of observational studies [11, 12], which assessed the effect of VD on the risk of type 2 diabetes mellitus (T2DM). The results of two meta-analyses of the trials conducted on vitamin C consumption were contradictory, too [13, 14]. A nearly 6 month trial with chromium, improved lipid profile and fasting blood sugar (FBS) [15, 16]. Still, another meta-analysis study showed that these factors were not improved after 7-month supplementation with chromium [17].
Meta-analysis studies earn the highest rank in the evidence-based approach [18]. Although several systematic reviews have been conducted on specific nutrients, an umbrella review of them can present an overview of the results and conclude the main findings. Therefore, we aimed to critically assess all available meta-analysis studies on the effects of the vitamins and nutrients for the management of DM, focusing on T2DM.
Material and methods
Data searches & study selection
All relevant meta-analyses of observational studies and clinical trials that had reviewed the effects of the most frequently studied antioxidants (vitamins A, B, C, D, E, K, and nutrients including alpha-lipoic acid (ALA), zinc, copper, selenium, chromium, and coenzyme Q10) on T2DM published until 5th June 2021 were included in this review. To obtain all relevant studies, PubMed and Web of Science databases were systematically searched using the following search terms: 'antioxidant', 'type 2 diabetes mellitus', 'vitamin', 'ascorbic', 'tocopherol', 'carotene', 'alpha-lipoic acid', 'retinol', 'zinc', 'copper', 'chromium', 'coenzyme Q10', and their equivalents, based on MeSH terms.
Eligibility criteria for inclusion were as follows.
Population: Any meta-analysis of observational studies and clinical trials on T2DM.
Intervention: Studies in which participants with T2DM received vitamins A, B, C, D, E, K, or nutrients including ALA, zinc, copper, selenium, chromium, and coenzyme Q10 at any concentration and for any duration.
Comparator: Any studies compared the above antioxidants with placebo or active control.
Outcomes: Any studies investigated any effect of the above antioxidants on risk, incidence, association, severity, or progression of T2DM and its complications
Meta-analyses conducted on children, pregnant women, or type 1 DM were excluded from this review. We used the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analysis) flowchart [19] to report our results. After excluding the duplicate publications, the titles and abstracts of the papers were examined. Moreover, hand searching was performed for full-text retrieval of the included studies' references. Two investigators performed all steps independently, and a third reviewer resolved any disagreement. Our search was limited to English language.
Data extraction and quality assessment
The following data were extracted; first author's name, year of publication, patients' characteristics (sample size, age, and sex), type of study and number of studies included in the meta-analysis, type of the antioxidant, dose, and duration of treatment, outcome measures, significant results, relative risk (RR) of diabetes, odds ratio (OR), effective dose, and quality assessment.
Results
Overall, 93 articles were included in the present umbrella review based on the PRISMA flowchart (Fig. 1). The details of the included meta-analysis studies are shown in Tables 1, 2, and 3.
Fig. 1.
Flow diagram of the study selection process
Table 1.
Characteristics of antioxidative vitamins’ effects on type 2 diabetes mellitus and its complications in meta-analysis of clinical trials
| Author | Type of antioxidant/ Control | meta-analyzed studies (n)/ Disorders | Participants | Intervention | Outcome measures | Significant results | Effective dose | Quality assessment | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size (n) | Age (yr) | Sex | Dose/ Frequency | Duration | |||||||
| Vitamin K | |||||||||||
| Shahdadian et al. 2018 [20] | VK alone or as multivitamin/ Placebo | 5/ Pre-diabetes, Healthy | 533 | 20–80 | Both | 500 µg/d- 90 mg/d | 1w-3 yr | FBS, FI, HOMA | NO | NA | Yes |
| Vitamin B | |||||||||||
| Sawangjit et al. 2020 [21] | Single Mecobalamin or combination with other treatments/ Placebo or active control | 15/ DPN | 1707 | 47–67 | Both | 0.5–2/d (varied mode: oral, IM, IV) | 2-24w | Pain (VAS, NRS), numbness, tingling weakness, tendon reflex, nerve conduction velocity (NCV) | ↑clinical therapeutic efficacy by alone or combination, ↑NCV by combination | No | Yes |
| Raval et al. 2015 [22] | Single or multiple VB derivatives/ Placebo or active control | 9/ T1DM, T2DM | 1354 | 30–75 | Both | varied: for single VB: 500 µg/d- 300 mg/d | 2-36 m | Kidney function, All-cause and Cardiovascular mortality, BP | NO | NA | Yes |
| Vitamin D | |||||||||||
| AlAnouti, et al. 2020 [23] | VD/Placebo | 4/ MetS | 303 | 40–65 | Both | Low dose: 2000 IU/d-20000 IU/w, High dose: 50,000 IU/w | 8w-1 yr | Lipid profiles, VD serum | ↑TGs by low dose and high dose VD | NO | Yes |
| Emadzadeh et al. 2020 [24] | VD-fortified food/Placebo, Ca | 11/T2DM, Healthy | 238 | 18–75 | Both | 100–28,000 IU/d | 8-24w | HbA1c, FBS, insulin, HOMA | ↓FBS, ↓Insulin, ↓HOMA | NO | Yes |
| Yammine et al. 2020 [25] | VD/ (before-after, or quasi-randomized controlled trial) | 4/DPN | 364 | 52.3–62 | Both | Varied, 2059/d-50000/w | 8–20 w | Serum VD, HbA1c, MPQ score | ↑serum VD, ↑MPQ score | NO | Yes |
| Zhang et al. 2020 [26] | VD2 and VD3/ Placebo | 8/ Pre-DM, VD deficiency, Obesity | 4896 | 46–62 | Both | Varied, 4000 IU/d-88865 IU/w | 6–60 m | New-onset T2DM, reversion prediabetes to normal | ↓risk T2DM, ↑reversion prediabetes to normo-glycemia | NO | Yes |
| Asbaghi et al. 2019 [5] | VD3-Co-Ca/ Placebo | 12/ T2DM, Healthy | 4395 | 24–72 | Both | 200–7142.8 IU/d | 8w-6.5 yr | FBS, HbA1c, HOMA, FI, Insulin sensitivity | Totally: ↓FBS, ↓HOMA, ↓FI, Subgroup analysis: ↓FBS by ≤ 12w treatment, ↓HOMA and ↓FI by each duration | ↓FBS, and ↓HbA1c, and ↓HOMA by high dose (Ca ≥ 1000 mg/d + VD ≥ 800 IU/d) | Yes |
| Gupta et al. 2019 [27] | VD and its analogues/ Placebo | 9/ T1DM, T2DM | 734 | Mean: 57 | Both | varied | 8w-6 m | UACR, UAER, 24 h-UP, UPCI, serum: Ca, Cr, PTH, 25-OHD, 1,25-OHD | NO | NA | Yes |
| Hu et al. 2019 [28] | VD3/ Placebo | 19/ Community population | 1374 | UN | UN | 2000 IU/d-300000 IU/ Once | 4w-12 m | FBS, HbA1c, HOMA, FI | Totally: NO, Subgroup analysis: ↓HbA1c, ↓HOMA, ↓FI in duration < 6 m | NO | Yes |
| Sahebi et al. 2019 [29] | VD fortified food/ Placebo, Ca or non-fortified | 37/ T1DM, T2DM, GDM | 1673 | UN | Both | UN | UN | FBS, HbA1c, HOMA, hs-CRP, serum VD | Totally: ↓serum VD in diabetics vs. healthy, Subgroup analysis: ↓FBS, ↓HbA1c, ↓HOMA | NO | Yes |
| Wang et al. 2019 [30] | Varied VD types/ Placebo, non-treatment | 20/ T1DN, T2DN | 1464 | 35–72 | UN | 10–7142.8 IU/d | 8w-6 m | FBS, HbA1c, renal function, inflammatory biomarkers | ↓24 h-UP, ↓UAER, ↓hs-CRP, ↓TNF-α, ↓IL-6 | No-difference between dose or treatment duration | Yes |
| He et al. 2018 [31] | VD/ Placebo, Non-VD | 23/ NGT, Pre-DM | UN | UN | UN | UN | UN | T2DM risk, FBS, HOMA, serum VD | Totally: NO, Subgroup analysis: RR in pre-DM: 0.84, ↓FBS in pre-DM or BMI < 25 or serum VDinsufficien,↓HOMA in sufficient serum VD, ↓T2DM risk in pre-DM or overweight | VD > 2000 IU/d for prevention T2DM | Yes |
| Li et al. 2018 [32] | VD3, VD2/ Placebo | 20/ Community population | 2703 | 48–67 | Both | VD3: 20 IU/d-300000 IU/Once, VD2:100000 IU/Once | 2-6 m | FBS, HbA1c, HOMA, FI, serum VD | Totally: ↑serum VD, ↓HOMA, Subgroup analysis: ↓FBS in Middle East, > 2000 IU/d, duration < 3 m, baseline VD serum < 50 nmol/L, ↓HbA1c in obese |
> 2000 IU/d |
Yes |
| Mansournia et al. 2018 [33] | VD3/ Placebo | 33/ T2DM, GDM, Diabetes complications (mostly T2DM) | 1053 | 20–75 | Both | 200 IU/d-300000 IU/once | 6w-12 m | Biomarkers of inflammation and oxidative stress | Totally: ↓hs-CRP, ↓MDA, ↓NO, ↑TAC, ↑GSH Subgroup analysis: ↓hs-CRP in T2DM, or complications | NO | Yes |
| Tabrizi et al., 2018 [34] | VD2, VD3/ Placebo |
22/ T2DM, PCOS, CKD, overweight, CVD, MetS (mostly T2DM) |
1799 | 27–89 | Both | Varied, 2000 IU/d, 40,000/w, 60,000/m, 300,000 once | 4–48 w | FMD, AI, PWV | ↑FMD | < 3000 IU/d for dysglicemics non-DM | Yes |
| Yu et al. 2018 [35] | VD/ varied (placebo, Ca, VK) | 13/ T2DM | 875 | 21–75 | Both | 20 IU/d-50000 IU/w | 8-52w |
FBS, HOMA, serum VD, hs-CRP, TNF-α, IL-6 |
Totally: ↓hs-CRP, ↓borderline TNF- α, Subgroup analysis: ↓hs-CRP by dose ≤ 4000 IU/d | ≤ 4000 IU/d | Yes |
| Krul-Poel et al. 2017 [36] | VD/ Placebo | 23/ T2DM | 1797 | 44–67 | Both | 400 IU/d-300000 IU/once | 4w-12 m | FBS, HbA1c | Totally: NO, Subgroup analysis: ↓FBS when HbA1c ≥ 8% | NO | Yes |
| Lee et al. 2017 [37] | VD formulations/ Placebo, non-VD | 22/ T2DM | 2747 | Mean: 48–70 | UN | 400 IU/d- 450,000 IU/ Once | 8w-6 yr | FBS, HbA1c | Totally: ↓HbA1c, Subgroup analysis: ↓HbA1c by dose ≤ 2000 IU/d, or duration ≤ 12w | ≤ 2000 IU/d | Yes |
| Mirhosseini et al. 2017 [38] | VD fortified food/Placebo | 24/ T2DM, obese diabetics | 1528 | 40–67 | Both | 400–8500 IU/d | 2 m-12 m | FBS, HbA1c, HOMA, serum VD | Totally: ↓FBS, ↓HbA1c, ↓HOMA, ↑serum VD after intake, Subgroup analysis: ↓HbA1c in non-obese, ↓HOMA in non-obese, ↓FBS &↓HOMA by serum VD ≥ 50 nmol/l | ≥ 4000 IU/d | Yes |
| de Paula et al. 2017 [39] | VD3, VD2/ Placebo or non-VD | 7/ T2DM | 542 | Mean: 50.7–66.8 | Both | D2:100,000 IU/Once, D3: 6250–50,000 IU/w | 3-4w | BP | ↓DBP | NO | Yes |
| Wu et al. 2017 [40] | VD formulations/ Placebo or non-VD | 26/ T2DM | 1877 | 42.4–67 | Both | 20 IU/d- 300,000 IU/ Once | 4-48w | FBS, HbA1c | Totally: ↓HbA1c, Subgroup analysis: ↓HbA1c in VD deficiency, ↓FBS in VD deficiency, ↓HbA1c in non-obese, ↓FBS by VD dose ≥ 1000 IU/d, ↓HbA1c by ≥ 12w treatment | ≥ 1000 IU/d | Yes |
| Jafari et al. 2016 [41] | VD supplement or food fortified/ Placebo | 17/ T2DM | 1365 | UN | UN | 20–7143 IU/d | 8–48 | Lipid profile | Totally: ↓lipid profile, Subgroup analysis: ↓TC by base serum VD ≥ 25 nmol/l, or food fortified, or VD dose ≤ 2000 IU/d, ↓TGs by food fortified, or VD dose ≤ 2000 IU/d, ↓LDL-C at base serum VD ≥ 50 nmol/l, or ≤ 12w treatment, ↓HDL-C by VD supplement, or base serum VD > 75 nmol/l, or ≤ 12w treatment | ≤ 2000 IU/d | Yes |
| Lee et al. 2016 [42] | VD2, VD3/ Placebo or non-VD | 15/ T2DM | 1134 | 21–75 | Both | D2: 100,000 IU/Once, D3:1000 IU/d-300000 IU/Once | 8w-12 m | BP | ↓DBP | NO | Yes |
| Poolsup et al. 2016 [9] | VD or VD analogues/ Placebo or Ca or non-treatment | 10/ Pre-DM | 1671 | 20–80 | Both | 400 IU/d-300000 IU/Once | 2 m-7 yr | FBS, HbA1c, 2 h-OGTT, HOMA | Totally: ↓FBS, ↓HbA1c, Subgroup analysis: ↓HOMA in base serum VD ≥ 50 nmol/l, ↓2 h-OGTT in base serum VD < 50 nmol/l | NO | Yes |
| Chokhandre et al. 2015 [43] | VD & its analogues/ Placebo | 6/ T2DN | 584 | UN | UN | 0.5 µg/d-50000 IU/w | 8-24w | UACR, albuminuria, eGFR, VD serum level, Ca, HbA1c | Significant improvement in kidney function | NO | Yes |
| Derakhshanian et al. 2015 [44] | VD derivatives/ Placebo | 4/ T2DN plus VD deficient | 219 | 57–60 | UN | 20–7142.8 IU/d | 6-24w | UACR | NO | NA | Yes |
| Seida et al. 2014 [8] | VD3/ Placebo or non-VD | 35/ T2DM, NGT, Pre-DM | 43,407 | 27–77 | Both |
125 IU/d-300000 IU/Once |
4w-3 yr | IR, Insulin secretion, HOMA, HbA1c | Totally: NO, Subgroup analysis: ↓FBS in non-DM | NA | Yes |
| Zhao et al. 2014 [45] | VD3/ Placebo, blank control | 20/ T2DN | 1497 | 35–75 | Both | UN | 4-48w | 24 h-UP, UACR, HbA1c, BP | ↓24 h-UP, ↓UACR | UN | Yes |
| George et al. 2012 [10] | VD3 or VD derivatives/ Placebo | 15/T2DM, NGT, IGT | 40,479 | 26–77 | Both | 0.25 µg/d-200000 IU/d | 7d-7 yr | FBS, HOMA, HbA1c | Totally: NO, Subgroup analysis: ↓FBS & ↓HOMA in DM or IGT | NO | Yes |
| Mitri et al. 2011 [46] | VD formulations/ Placebo | 11/ T2DM, Healthy | 41,070 | 18–79 | Both | 400–8571 IU/d | 8w-7 yr | FBS, HbA1c, HOMA | NO | NA | Yes |
| Vitamin C | |||||||||||
| Namkhah et al. 2021 [47] | VC/ Placebo | 15/ T2DM | 872 | 36–72 | Both | 200–3000 mg/d | 2-48w | Lipid profile | ↓ TGs, ↓TC | NO | Yes |
| Tareke et al. 2021 [13] | VC/ Placebo | 11/ T2DM | 606 | 37.8–60 | UN | 200–2000 mg/d | 4-52w | Lipid profile, FBS, HbA1c | ↓TGs, ↓FBS, ↓HbA1c | ≥ 1000 mg/d, > 12w, < 52.8 yr age for TGs, < 1000 mg/d, > 12w, < 52.8 yr age for LDL-C, each doses, w, age for FBS, HbA1C | Yes |
| Ashor et al. 2017 [14] | VC/ Placebo | 22/ T1DM, T2DM, Healthy | 937 | 22–60 | Both | 72–6000 mg/d | 1-120d | BG, Insulin serum, HbA1c | Totally: NO, Subgroup analysis: ↓BG in T2DM, ↓BG by > 30d VC, ↓insulin serum in T2DM, ↓insulin serum in fasting | NO | Yes |
| de Paula et al. 2017 [39] | VC/ Placebo | 2/ T2DM | 65 | 51.8–66.5 | Both | 500–1500 mg/d | 3-4w | BP | ↓DBP | NO | Yes |
| Khodaeian et al. 2015 [48] | VC/ Placebo | 3/ T2DM | 92 | 39–72 | Both | 200–1000 mg/d | 4-16w | HOMA | NO | NA | Yes |
| Tabatabaei-Malazy et al. 2014 [6] | VC/ Placebo | 4/ T2DM | 316 | 29–75 | Both | 200–1250 mg/d | 4w-3 m | FBS, FI, HbA1c, lipid profile, serum VC | ↓FBS, ↓HbA1c, ↓TC, ↓LDL-c | At least 1250 mg/d, and for 3 m | Yes |
| Vitamin E | |||||||||||
| Khodaeian et al. 2015 [48] | VE/ Placebo | 8/ T1DM, T2DM | 425 | 20–75 | Both | 150–800 mg/d | 4-27w | HOMA | NO | NA | Yes |
| Xu et al. 2014 [7] | VE/ Placebo or non-VE | 14/ T2DM | 714 | Mean age: 48.5–71.3 | Both | 200–1600 IU/d | 6-52w | FBS, FI, BS2hpp, HbA1c, BP, lipid profiles, HOMA | Totally: NO, Subgroup analysis: ↓HbA1c by dose > 400 mg/d, duration ≥ 12w, HbA1c < 8%, FBS < 8 mmol/l, normal baseline VE serum, ↓FBS in duration ≥ 12w,↓FI by dose > 400 mg/d, FBS ≥ 8 mmol/l | > 400 mg/d | Yes |
| Suksomboon et al. 2011 [49] | VE, tocotrienoles/ Placebo or non-treatment | 9/ T1DM, T2DM | 418 | 21–80 | UN | 6 mg/kg/d-1800 mg/d | 2-12 m | HbA1c | Totally: NO, Subgroup analysis: ↓HbA1c when HbA1c ≥ 8%, or low baseline VE serum | NA | Yes |
| Mixture antioxidants | |||||||||||
| Balbi et al. 2018 [50] | VB, VC, VD, VE, Mixture/ Placebo | 12/ T2DM | 1450 | 40–77 | Both | VB: 5 mg/d, VC:200–3000 mg/d, VD:500–200,000 IU/d, VE: 150–1200 mg/d, Mixture: varied | 4–24 w | FBS, HbA1c, oxidative/antioxidative biomarkers | Totally: ↓FBS, ↑GPx,↓MDA, ↓TBARS, ↑TAC, ↑SOD, Subgroup analysis: ↓FBS and ↓HbA1c by VE | NO | Yes |
| Bolignano et al. 2017 [51] | Alone or combination of VA, VC, VE, Sel, Zn/ placebo, or non-treatment | 14/ T1DN, T2DN | 4345 | 18.9–65.4 | Both | varied | 4w-4.5 yr | UAER, eGFR, serum Cr, percent of dialysis | Totally: ↓UAER, Subgroup analysis: ↓UAER by VE | NO | Yes |
| Kandhare et al. 2017 [52] | VC, VE, Turmeric, Green tea, pyridoxine/ Placebo, conventional treatment | 12/ T1DM, T2DM | 1461 | UN | Both | varied | 4-52w | BUN, eGFR, serum Cr, urine TGF-β, UACR | ↓BUN, ↓TGF-β, ↓eGFR | NO | Yes |
| Khodaeian et al. 2015 [48] | VE, VC, ALA, Zn, Chr/ placebo, sole intake vitamin or mineral | 5/ T2DM | 256 | 30–75 | Both | Varied | 6-24w | HOMA | NO | NA | Yes |
| Zheng et al., 2015 [53] | Breviscapine (B, a type flavonoid) + Mecobalamin (B12)/ Mecobalamin (M) | 17/ DPN | 1398 | 47–84 | Both |
B: 50–150 mg/d, M: 0.5–1.5 mg/d |
2-6w | MNCV, SNCV | ↑MNCV, ↑SNCV | NO | Yes |
| Montero et al. 2014 [54] | VE, VC/ Non-VE, Non-VC | 9/ T2DM | 296 | Mean: 47.9–64.2 | Both |
VC: 800-3000 mg/d VE: 537-811 mg/d |
2-52w | FMD | Totally: NO, Subgroup analysis: ↓FMD in non-obese T2DM | NA | Yes |
| Tabatabaei-Malazy et al. 2014 [6] | VE, EPA, Zn with-without VC/ Placebo | 3/ T2DM | 190 | 29–75 | Both | Varied | 4w-3 m | FBS, FI, HbA1c, lipid profile, serum VC | NO | NA | Yes |
| Akbar et al. 2011 [55] | VC, VE/ Placebo or without intervention | 14/ T1DM, T2DM | 562 | UN | UN |
VC:100 mg-2 g/Once, VE:100-1800 IU/varied |
VC:4–12 w, VE: 6–27 w | FBS, BS2hpp, HbA1c, FI | ↓HbA1c | NO | Yes |
Legend: Chr Chromium; VC Vitamin C; VE Vitamin E; T2DM Type 2 diabetes mellitus; Pre-DM Prediabetes; NIDDM Non-insulin dependent; W Week; FPG Fasting plasma glucose; HbA1c Glycosylated hemoglobin; TGs Triglycerides; NGT Normal glucose tolerance; IGT Impaired glucose tolerance; UN Unknown; m Month; FBS Fasting blood sugar; BS2hpp Blood sugar 2h post prandial; IS Insulin sensitivity; D Day; FI Fasting insulin; IU International unit; HOMA Homeostasis model assessment index; Yr Year; IR Insulin resistance; BP Blood pressure; NA Not applicable; CAD Coronary artery diseases; DBP Diastolic blood pressure; GPx Glutathione peroxidase, MDA Malondialdehyde; TBARS Thiobarbituric acid reactive substances; TAC Total antioxidant capacity; SOD Superoxide dismutase; Zn Zinc; ALA Alpha lipoic acid; Sel Selenium; LDL-C Low density lipoprotein cholesterol; CRP C-reactive protein; IL-6 Interleukin-6; VK vitamin K; EF Endothelial function; EPA Eicosapentaenoic acid; Ca Calcium; 2h-OGTT 2-h oral glucose tolerance test; GDM Gestational diabetes mellitus; UACR Urine albumin-to-creatinine ratio; UACR Urine albumin creatinine ratio; UAER Urinary albumin excretion rate, PTH Parathyroid hormone; UPCI Urine protein creatinine index; EF Endothelial function; DN Diabetic nephropathy; DPN Diabetic peripheral neuropathy; NCV Nerve conduction velocity; MPQ McGill Pain Questionnaire score, FMD Flow-mediated dilation; PWV Pulse wave velocity; AI Augmentation index; MNCV Motor nerve conduction velocity; SNCV sensory nerve conduction velocity
Table 2.
Characteristics of antioxidative micronutrients’ effects on type 2 diabetes mellitus and its complications in meta-analysis of clinical trials
| Author | Type of antioxidant/ Control | meta-analyzed studies (n)/ Disorders | Participants | Intervention | Outcome measures | Significant results | Effective dose | Quality assessment | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size (n) | Age (yr) | Sex | Dose/ Frequency | Duration | |||||||
| Chromium | |||||||||||
| Asbaghi et al. 2021 [15] | Chr/ Placebo | 24/ T2DM | 1418 | 35–73 | Both | 42–1000 µg/d | 6-25w | Lipid profiles | ↓TGs, ↓TC, ↑HDL-C | > 200 µg/d for TGs, TC, ≤ 200 µg/d for LDL-C | Yes |
| Zhao et al. 2021 [56] | Chr (Different formulations)/ Placebo | 10/ T2DM | 509 | 35–68 | Both | 42–1000 µg/d | 90–175 d | HbA1c, FBS, Lipid profile | ↓HbA1c | NO | Yes |
| Asbaghi et al. 2020 [57] | Chr/ Placebo | 23/ T2DM | 732 | 28–68 | Both | 50–1000 µg/d | 4-25w | FBS, Insulin, HbA1c, HOMA | ↓ FBS, ↓HbA1c, ↓HOMA, ↓Insulin | for all: > 200 and ≤ 200 mg/d | Yes |
| Yin et al. 2015 [58] | Chr (Different formulations)/ Placebo | 14/ T2DM | 875 | 30–83 | Both | 23.2–1000 µg/d | 8-24w | HbA1c, FBS | Subgroup analysis: ↓FBS | No | Yes |
| Suksomboon et al. 2014 [16] | Mono Chr or mixed with VC, VE, or biotin/ Placebo | 25/ T2DM, NIDDM, Healthy | 1641 | > 18–83 | Both | 1.28–1000 µg/d | 3–24 w | FPG, HbA1c, Lipid profile | ↓FPG, ↓HbA1c, ↓TGs | > 200 µg/d | Yes |
| Patal et al. 2010 [17] | Chr/ Placebo | 6/ T2DM | 671 | UN | UN | 200–1000 ug/d | 3-7 m | FBS, FI, HbA1c, 2hpp-Bs, lipid profile | Totally: NO, Subgroup analysis: ↓FBS, ↓HbA1c | NO | Yes |
| Balk et al. 2007 [59] | Chr (Different formulations)/ Placebo | 41/ T2DM, NGT, IGT | 1198 | UN | UN | 1.28–1000 µg/d | 3w-8 m | FBS, HbA1c, Bs2hpp, lipid profile, IS | In T2DM: ↓FBS ↓HbA1c | For FBS: 1000 µg/d, For HbA1c: 200 µg/d | Yes |
| Althuis et al. 2002 [60] | Chr (Different formulations)/ Placebo | 15/ T2DM, IGT, Healthy | 618 | 18–93 | Both | 10.8–1000 µg/d | 28d-16 m | FBS, Glucose at 120 min, HbA1c, FI, Insulin at 120 min | NO | NO | Yes |
| Zinc | |||||||||||
| Jayawardena et al. 2021 [61] | Zn with-without other micronutrients/ Placebo | 3/Pre-diabetes | 265 | UN | Both | 20–30 mg/d | 6-12 m | FBS, BS2hpp, HbA1c, HOMA, CRP, lipid profiles | ↓FBS, ↓BS2hpp, ↓TC, ↓HDL-C, ↓HOMA, ↑zinc serum | No | Yes |
| Pompano et al. 2021 [62] | Zn/ Placebo | 27/ T2DM, CVD, obese, healthy | 2016 | 20–70 | Both | 9.8–75 mg/d | 4-50w | FBS, HbA1c, HOMA, lipid profile | Low dose (< 25 mg/d): ↓FBS, ↓TC, ↓TGs, ↓LDL-C High dose (≥ 25 mg/d): ↓HbA1c, ↓HOMA | < 25 mg/d and ≥ 12 w | Yes |
| Asbaghi et al. 2020 [63] | Zn/ Placebo | 9/T2DM | 427 | 48–66 | Both | 30–660 mg/d | 6-52w | Lipid profiles | Totally: ↓TGs, ↓TC Subgroup analyses: ↓HDL-C | For TGs, LDL-C: < 100 mg/d, For TC, HDL-C each doses | Yes |
| Wang et al. 2019 [64] | Zn formulations/ Placebo | 32/ T2DM, Obese | 1700 | 18–75 | Both | 5-660 mg/d | 1-12 m | FBS, BS2hpp, HbA1c, FI, HOMA, hs-CRP | Totally: ↓FBS, ↓Bs2hpp, ↓FI, ↓HOMA, ↓HbA1c, ↓hs-CRP Subgroup analysis: ↓FBS in T2DM vs. others, ↓FBS by inorganic Zn vs. organic Zn | NO | Yes |
| Capdor et al. 2013 [65] | Zn formulations/ Placebo | 14/ T2DM, non-DM | 3978 | Infants-68 | Both | 3-240 mg/d | 1.4–390 w | FBS, HbA1c, Serum insulin, serum Zn | Totally: ↓FBS, ↓HbA1c, ↑serum Zn, Subgroup analysis: ↓FBS in T2DM and high risk for DM vs. healthy | NA | NO |
| Jayawardena et al. 2012 [66] | Zn formulation with-without other antioxidants/ Placebo | 25/ T1DM, T2DM | 1317 | Mean: 4.1–72.0 | UN | 7.5–660 mg/d | 3w-5 yr | FBS, BS2hpp, HbA1c, lipid profiles, BP | ↓FBS, ↓HbA1c, ↓TC, ↓LDL-C, ↓SBP, ↓DBP | NO | UN |
| Coenzyme Q10 | |||||||||||
| Dludla et al. 2020 [67] | CoQ10/ Placebo | 12/T2DM or MetS | 650 | 46 -63 | Both | 20–400 mg/d | 8-24w | FBS, insulin, HbA1c, Lipid profile, BMI | ↓LDL-C, ↓TC | No | Yes |
| Suksomboon et al. 2015 [68] | CoQ10 or CoQ10 + fenofibrate/ Placebo | 7/ DM | 356 | UN | UN | 100 mg/ twice daily or 200 mg/d | 3-6 m | FBS, HbA1c, lipid profile, BP | ↓TGs by CoQ10 or CoQ10 + Fenofibrate, ↓TC by CoQ10 + Fenofibrate | NA | Yes |
| Moradi et al. 2016 [69] | CoQ10/ UN | 14/ T2DM, non-DM | 920 | 35–70 | Both | 100–300 mg/d | 4-25w | FBS, HbA1c, FI | Totally: ↓FBS, Subgroup analysis: ↓FBS in duration < 20w, < 200 mg/d | < 200 mg/d | UN |
| Alpha lipoic acid | |||||||||||
| Ebada et al. 2019 [70] | ALA/Placebo | 10/ T1DM, T2DM | 553 | 46–72 | Both | 300–600 mg/d | 3-24w | HbA1c, FBS, Lipid profile, HOMA, GPx | ↑GPx | No | Yes |
| Rahimlou et al. 2019 [71] | ALA/ Placebo | 41/ T2DM, T1DM, Overweight, MetS, | 2564 | 15–74 | Both | 300–1200 mg/d | 2-192w | HbA1c, FBS, TNF-α, IL- 6, CRP, insulin, HOMA | ↓HbA1c, ↓FBS, ↓TNF-α, ↓IL-6, ↓CRP | < 600 and ≥ 600 mg/d for FBS, HbA1C, CRP, IL-6 | Yes |
| Akbari et al. 2018 [72] | ALA alone or plus nutrients/ Placebo | 24/ T2DM, non-DM | 1537 | 16–92 | UN | 200–1800 mg/d | 2-51w | FBS, FI, HbA1c, HOMA, lipid profile | Totally: ↓FBS, ↓FI, ↓HbA1c, ↓HOMA, ↓TGs, ↓TC, ↓LDL-C, Subgroup analysis: ↓FBS: in T2DM, by 600 mg/d, ↓FI: in non-DM, > 12w treatment, ↓HbA1c: by > 600 mg/d, > 12w treatment, by ALA with/ without nutrients, ↓HOMA: in T2DM, non-DM, by ≤ 600 mg/d, > 12w treatment, ↓TGs: in T2DM, by 600 mg/d, > 12w treatment, by combination, ↓TC: in T2DM, in non-DM, ≤ 600 mg/d, > 12w treatment, by sole ALA, ↓LDL-C: in T2DM, by 600 mg/d, < 8w treatment, by sole ALA | varied | Yes |
| Amato Nesbit et al. 2018 [73] | ALA/ Placebo | 6/ DPN | 1614 | UN | UN | 600–1800 mg/d | 3w-4 yr | DPN symptoms | ↓ Pain | NO | Yes |
| Wang et al. 2018 [74] | ALA + Epalrestat/ Epalrestat | 12/DPN | 813 | 40–87 | UN |
ALA:300 or 600 mg/d Epalrestat: 50 mg/tid |
14-28d | MNCV, SNCV, TSS, TCSS | Totally: effective, Subgroup analysis: After 14, 21, 28d by 300, or 600 mg ALA: ↑Median & peroneal MNCV, ↑median & peroneal SNCV, After 21d by 600 mg ALA: ↓TCSS, ↓TSS | 600 mg/dALA after 14d, 28d | Yes |
| Cakici et al. 2016 [75] | ALA/ Placebo | 6/ DPN (T1DM, T2DM) | 885 | 56–60 | UN | 100–1800 mg/d | 30 min IV-6 m oral | TSS | ↓TSS | 600 mg/d oral or IV | Yes |
| Snedecore et al. 2013 [76] | ALA, non-ALA/ Placebo, other treatments | 58/ painful DPN | 1183 | Mean: 53–71 | Both | Varied (ALA: 600–1800 mg/d) | 4-27w | Pain reduction | NO (for ALA) | NA | Yes |
| Han et al. 2012 [77] | ALA/ non-ALA | 15/ DPN | 1058 | Mean: 43.9–66.0 | UN | 300–600 mg/d | 14-28d | Efficacy treatment, MNCV, SNCV | ↑efficacy,↑MNCV, ↑SNCV | 300–600 mg/d for 2-4w | Yes |
| Mijnhout et al. 2012 [78] | ALA/ Placebo | 4/ DPN | 653 | 18–74 | UN | 100–1800 mg/d | 3-5w | TSS | ↓TSS | 600 mg/d for 3w | Yes |
| Ziegler et al. 2004 [79] | ALA/ Placebo | 4/ DPN | 1258 | 48–65 | Both | 600 mg/d IV | > 3w | TSS, NISLL | ↓TSS, ↓NISLL | 600 mg/d IV > 3w | Yes |
Legend: Chr Chromium; VC Vitamin C; VE Vitamin E; T2DM Type 2 diabetes mellitus; NIDDM Non-insulin dependent; W Week; FPG Fasting plasma glucose; HbA1c Glycosylated hemoglobin; TGs Triglycerides; NGT Normal glucose tolerance; IGT Impaired glucose tolerance; UN Unknown; m Month; FBS Fasting blood sugar; BS2hpp Blood sugar 2 h post prandial; IS Insulin sensitivity; D Day; FI Fasting insulin; IU International unit; HOMA Homeostasis model assessment index; Yr Year; IR Insulin resistance; CoQ10 Coenzyme Q10; BP Blood pressure; NA Not applicable; CAD Coronary artery diseases; DBP Diastolic blood pressure; GPx Glutathione peroxidase, MDA Malondialdehyde; TBARS Thiobarbituric acid reactive substances; TAC Total antioxidant capacity; SOD Superoxide dismutase; Zn Zinc; ALA Alpha lipoic acid; Sel Selenium; DPN Diabetic peripheral neuropathy; MNCV Motor nerve conduction velocity; SNCV Sensory nerve conduction velocity; TCSS Toronto clinical scoring system; TSS Total symptom score; LDL-C Low density lipoprotein cholesterol; CRP C-reactive protein; IL-6 Interleukin-6; NISLL Neuropathy impairment score lower limbs; GPx Glutathione peroxidase; TNF-α Tumor necrosis factor alpha.
Table 3.
Characteristics of antioxidants’ effects on risk of type 2 diabetes mellitus in meta-analysis of observational studies
| Author | Type of antioxidants | meta-analyzed studies (n)/ Population | Participants | Event (n) | Follow-up | Outcome measures | Significant results | Quality assessment/ adjusted | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Total population (n) | Age (yr) | Sex | ||||||||
| Vitamin D | ||||||||||
| Rafiq et al. 2021 [80] | Serum level VD | 40/ T2DM, non-DM | UN | > 18y | Both | UN | UN | Correlation between serum VD and Insulin Resistance | ↑insulin resistance with ↓ VD | Yes/ NO |
| Dai et al. 2019 [81] | Serum level VD | 7/ DF, DM | 1115 | Mean: 49.6–70.2 | Both | 40–289 | UN | Serum VD, Association of serum VD with DF | ↓Serum VD < 50 nmol/l in DF, and DM, ↑Risk DF (OR: 3.22 in VD < 25 nmol/l) | Yes/ NO |
| Zhang et al. 2019 [82] | Serum level VD | 13/ T2DM with—without DPN (case–control studies) | 2814 | 54- 66 | Both | UN | NA | correlation of VD and DPN in T2DM | ↓VD serum in DPNcompared to non-DPN, RR VD deficiency for DPN: 1.07 | Yes/NO |
| Rafiq et al. 2018 [11] | Serum level VD | 45/ T2DM, non-DM | UN | > 18 yr | Both | UN | UN | Correlation between serum VD and T2DM | ↑T2DM risk in diabetics and non-DM with hypo-D | Yes/ NO |
| Ekmekcioglu et al. 2017 [83] | Serum level VD | 28/ General population, Renal transplanted | 132,325 | UN | Both | UN | UN | Association of serum VD with T2DM | Dose–response U-Shape association, RR: 0.66 highest vs. lowest serum VD | UN/ Yes |
| Lucato et al. 2017 [84] | Serum level VD | 9/ Older population | 28,258 | 67.7 | Both | 2863 | 7.3 | Association of hypo-VD with T2DM | RR lower serum level vs. higher: 1.17 | Yes/ Yes |
| Luo et al. 2017 [85] | Serum level VD | 15/ T2DM with/without DR | 17,664 | > 18 yr | UN | 3455 | UN | Association serum VD with DR | OR VD deficiency with DR: 2.03, Pooled difference VD in DR vs. non-DR: -1.71 ng/ml | Yes/Yes |
| Qu et al. 2017 [86] | Serum level VD | 10/ T2DM | 1468 | UN | UN | NA | NA | Association serum VD with DPN | ↓Serum VD in Caucasian DPN vs. non-DPN, OR VD deficiency and DPN in Asian: 1.22 | Yes/ NO |
| Liang et al. 2016 [87] | Serum level VD | 11/ T1DM, T2DM | 6851 | 12–73 | Both | 2292 | NA | Association serum VD with DR | OR VD deficiency with DR in DM: 1.51, but in T2DM: 1.15 | UN/ Yes |
| Derakhshanian et al. 2015 [44] | Serum level VD | 6/ T1DM, T2DM | 3700 | 9–75 | UN | NA | NA | Association serum VD with DN | ↑Risk DN (OR: 1.80 in VD < 20 ng/ml or VD deficient) | Yes/ NO |
| Lv et al. 2015 [88] | Serum level VD | 6/ T2DM | 1484 | 54.6–63.3 | Both | NA | NA | Association VD deficiency with DPN | ↓VD serum in DPN, ↑Risk DPN with VD deficiency; OR: 2.88 | Yes/ Yes |
| Afzal et al. 2013 [89] | Serum level VD | 16/ General population | 9841 | 47–64 | Both | 810 | 29 yr | T2DM risk | ↑Odds ratio for T2DM: 1.50 for bottom vs. top quartile VD | Yes/ Yes |
| Khan et al. 2013 [12] | Serum level or dietary intake of VD | 14/ General population | 190,626 | 25–79 | Both | 9399 | 10 yr | T2DM risk | ↓19% risk T2DM (top 3rd vs. bottom 3rd) | Yes/ Yes |
| Song et al. 2013 [90] | Serum level VD | 21/ Population-based | 76,220 | 30–79 | Both | 4996 | 22 yr | T2DM risk | ↓Risk T2DM (RR:0.96 per 10 nmol/l increment in serum 25-OHD, RR: 0.62 highest vs. lowest serum 25-OHD) | UN/ Yes |
| Forouhi et al. 2012 [91] | Serum level VD | 11/ General population | 59,325 | 40–76 | Both | 3612 | 1.3–22 yr | T2DM risk | ↓VD in T2DM vs. non-DM, RR:0.59 highest vs. lowest level VD | Yes/ Yes |
| Mitri et al. 2011 [46] | Serum level VD, VD intake | 8/ General population | 238,423 | 30–75 | Both | 7915 | 1.3–22 yr | T2DM risk |
↓13% risk T2DM by VD intake > 500 IU/d vs. intake < 200 IU/d, ↓risk T2DM 43% highest serum level vs. lowest |
Yes/ Yes |
| Pittas et al. 2007 [92] | Serum level VD | 4/ General population | 8758 | > 20 | Both | UN | UN | Association with T2DM | OR: 0.36 highest vs. lowest serum VD in non-blacks | UN/ Yes |
| VD + Ca intake | 4/ General population | 203,402 | 39–55 | 9653 | OR: 0.82 highest vs. lowest by VD + Ca | |||||
| Alpha lipoic acid | ||||||||||
| Muley et al. 2014 [93] | ALA intake | 6/ General population | 153,751 | 35–75 | Both | NA | 4-16 yr | T2DM risk | ↓T2DM risk (RR: 0.90) by two fold increase intake ALA | Yes/ Yes |
| Selenium | ||||||||||
| Wang et al. 2016 [94] | Serum level of Sel | 5/ Community population | 13,460 | Mean: 45.2–77.7 | Both | NA | NA | OR association with T2DM | U shape association of serum Sel < 97.5, > 132.5 µg/L with T2DM | Yes/ NO |
| Copper | ||||||||||
| Qiu et al. 2017 [95] | Plasma and serum level of Cu | 15/T1DM, T2DM, Healthy | 1640 | 5–75 | Both | UN | UN | Determine level of Cu | ↑Cu in plasma and serum DM vs. healthy | Yes/ Yes |
| Zinc | ||||||||||
| Pearsey et al. 2020 [96] | Zinc-alpha2-glycoprotein (ZAG) | 3/ T2DM, PCOS, MetS, prediabetes | 3127 | 36–52 | Both | NA | NA | Relationship between ZAG, and FBS, BS2hpp, HbA1c, fasting insulin, HOMA | ↓ZAG in dysglycaemia compared to metabolically healthy obese | Yes/Yes |
| subgroup analysis: only sig. diff. for PCOS | ||||||||||
| Fernandez-Cao et al. 2019 [97] | Zn intake | 12/ Urban, Rural population | 405,466 | 18–84 | Both | 27,643 | 5–24 yr | T2DM risk | ↓13% or ↓41% T2DM risk by moderated high intake in general or in rural | Yes/ Yes |
| Zn serum level | 8/ General population | 10,151 | 40–92 | 3331 | 4.6–20 | ↑64% risk of T2DM by elevated serum Zn | ||||
| Fernandez-Cao et al. 2018 [98] | Zn intake | 6/ T2DM, Healthy | 685 | 25–72 | Both | NA | NA | Relationship with T2DM | ↓Zn intake in T2DM with complications | Yes/ Yes |
| Zn whole blood level | 5/T2DM, Healthy | 1416 | 25–75 | ↓Zn for each year T2DM: 732.6 + (-77.88)*duration of T2DM (yr) | ||||||
| Several antioxidants | ||||||||||
| Hamer et al. 2007 [99] | Highest intake of VE, VC, Flavonoids, Carotenoids, Lycopene/ lowest intake | 9/ General population | 139,793 | 18–74 | Both | 8813 | 13 yr | T2DM risk | ↓13% risk T2DM (mainly by VE) | Yes/ Yes |
Legend: T2DM Type 2 diabetes mellitus; MetS Metabolic syndrome; IR Insulin resistance; Sel Selenium, Zn Zinc; Cu Copper; DR Diabetic retinopathy; VC Vitamin C; VE Vitamin E; VD Vitamin D; UN Unknown; Yr Year; IR Insulin resistance; NA Not applicable; ALA Alpha lipoic acid; Sel Selenium; DPN Diabetic peripheral neuropathy; Ca Calcium; DF Diabetic foot; DN diabetic nephropathy; OR Odds ratio; RR Relative risk
Studies' characteristics
Most of the included studies were meta-analyses of clinical trials conducted on vitamins, antioxidative nutrients, and their combinations. Twenty-four meta-analyses were performed on observational studies investigating vitamins or antioxidative nutrients. Most of the included studies were shown on both genders. Most meta-analysis studies have compared the effects of vitamins and placebos on the prevention or progression of diabetes and its complications. Quality assessment or adjustments with age and sex were performed for nearly all the of included meta-analyses. Details of the included studies are described as follows.
Influence of vitamins on the prevention or progression of DM and its complications
Overall, 61 papers (65 meta-analyses) were included in this topic; 48 and 17 studies were clinical trials and observational studies, respectively. The most commonly studied antioxidant was VD, which was examined in 45 meta-analyses including 28 meta-analyses of clinical trials, and 17 meta-analyses of observational studies. These figures were followed by eight studies on combining vitamins or other nutrients, six studies on VC, three on VE, two on VB, and one on VK in the meta-analysis of clinical trials. No meta-analyses of clinical trials or observational studies were found on either VA or beta-carotene.
The main factors that were measured from the outcome of meta-analyses on VD trials were FBS as the glycemic index, followed by fasting insulin (FI), Homeostasis Model Assessment (HOMA) index [5, 8–10, 24–26, 28, 29, 31, 32, 38, 46], renal function [27, 30, 43–45], biomarkers of inflammation or oxidative stress [29, 30, 33, 35], flow-mediated dilation (FMD) [34], and lipid profile [23, 41]. VD supplementation was associated with significant improvements in FBS, HbA1c, HOMA index, inflammatory and oxidative stress biomarkers, but a substantial acceleration in FMD. However, the effect of VD consumption on renal function or lipid profile in patients with DM was inconsistent. Also, studies that had assessed the impact of VD intake on blood pressure (BP) [39, 42] showed a significant reduction in diastolic blood pressure (DBP). Overally, the dose of the VD taken varied from 20 IU/d to 450,000 IU/once, and VD was administered for 3 weeks to 7 years. Meta-analyses of observational studies on VD had assessed the association between serum levels of VD and the risk of T2DM [11, 12, 83, 84, 89–92], or its complications; insulin resistance [80], diabetic foot (DF) [81], diabetic retinopathy (DR) [85, 87], diabetic nephropathy (DN) [44], and diabetic polyneuropathy (DPN) [82, 86, 88]. All of the studies mentioned above reported significant associations between low serum levels of VD and the risk of T2DM and its complications.
The meta-analysis of clinical trials conducted on combinations of antioxidants had assessed their effects on FBS, HbA1c, FI, HOMA index, renal function, oxidative stress biomarkers, FMD, as well as the lipid profiles [50–52, 54, 55]. Significant improvements in all of the measured factors had been observed, excluding HOMA index [48], and lipid profiles [6]. The effect of VE on the improvement of FBS, HbA1c, and renal function was more significant than the other nutrients [50, 51]. A meta-analysis study of observational studies indicated that the highest intake of antioxidant mixtures, particularly VE vs. the lowest intake, reduced the risk of T2DM by 13% [99].
The outcome measures studied in meta-analyses of clinical trials on VC were FBS, HbA1c, FI, HOMA index, lipid profile, BP, and endothelial function (EF) [6, 13, 14, 39, 47, 48]. Significant reductions in FBS, HbA1c, FI, EF, DBP, total cholesterol (TC), and low-density lipoprotein cholesterol (LDL-C) were observed in these studies [6, 13, 14, 39]. FBS was significantly reduced when the patients were treated with VC for more than 30 days. The appropriate dose of VC for improving EF was significantly higher than 500 mg/d, and FBS, HbA1c, and lipid profiles were at least 1250 mg/d.
The meta-analysis of trials conducted on VE had assessed its effect on FBS, HbA1c, FI, HOMA index, BP, and lipid profiles [7, 48, 49]. A significant improvement in HbA1c and FI was observed for doses greater than 400 mg/d. A significant reduction in FBS was seen when patients were treated with VE for ≥ 12 weeks.
Although meta-analyses of clinical trials on multiple VK or VB derivatives did not recongnize any significant improvements in FBS, FI, HOMA index, renal function, and BP [20, 22], sole intake of mecobalamin or its combinations with other treatments or flavonoids has improved nerve conduction velocity [21, 53].
The influence of antioxidative nutrients on the prevention or progression of diabetes mellitus and its complications
Thirty-four papers (34 meta-analyses) were included in this review. Of these, 27 and 7 were meta-analyses of clinical trials and observational studies. The most commonly studied antioxidant was ALA, examined in 10 meta-analyses of clinical trials and one meta-analysis of observational studies. These figures were followed by eight studies on chromium (Cr), six studies on zinc (Zn), and three studies on coenzyme Q10 (CoQ10) in meta-analyses of clinical trials. One meta-analysis of observational studies was conducted on ALA, selenium, and copper (Cu) for each of these nutrients, and three meta-analyses were performed on Zn.
Nearly all meta-analysis studies of clinical trials on ALA [73–79] had been conducted on patients with DPN. ALA showed significant beneficial effects on DPN symptoms after 14, 21, or 28 days and doses of 300 mg/d and 600 mg/d. In addition, considerable improvements in FBS, FI, HbA1c, HOMA index, TC, triglycerides (TGs), and LDL-C by ALA was seen in patients with T2DM or non-diabetic subjects [71, 72]. Beneficial effects of ALA on inflammatory and antioxidative biomarkers were observed in two meta-analyses [70, 71]. A meta-analysis of an observational study on ALA indicated a significant reduction in T2DM risk by doubling its intake [93].
The main outcome measures in meta-analyses of trials conducted on the sole intake of Cr were FBS, HbA1c, FI, and lipid profiles [15–17, 56–60]; the HOMA index was the main outcome in studies on its combinations with vitamins [48, 57]. Cr supplementation was associated with a significantly reduction of FBS, HbA1c, and TGs. The appropriate dose of Cr intake for the significant decrease in HbA1c and TGs was ≥ 200 µg/d, but the significant reduction of FBS varied from > 200 to 1000 µg/d. Combining Cr with VC, VE, ALA, and Zn did not show any beneficial effects on the HOMA index.
In a meta-analysis of clinical trials that examined the effect of Zn [61–63, 65, 66, 74], significant reductions were observed in the serum levels of FBS, FI, HbA1c, HOMA index, TC, LDL-C, and high-sensitive C-reactive protein (hs-CRP). Meta-analyses by Capdor et al., 2013 and Jayawardena et al., 2021 reported a significant rise in serum levels of Zn after supplementation and subsequent significant reductions in FBS and HbA1c. In three meta-analyses of observational studies on Zn [96–98], a significantly low intake of Zn was observed in patients with T2DM complications, and the risk of T2DM was reduced by increasing the Zn intake. No significant improvements in FBS, FI, HbA1c, HOMA index, and lipid profile were observed upon combining Zn with other nutrients or vitamins [6, 48, 51]. However, a significant reduction in urinary albumin excretion rate (UAER) was reported in combinations of Zn with other antioxidative agents [51].
The effect of CoQ10 intake was assessed in three meta-analyses of clinical trials [67–69] through the measurement of FBS, HbA1c, FI, lipid profiles, and BP. CoQ10 supplementation improved FBS at doses lower than 200 mg/d or used for less than 20 weeks. In addition, it showed beneficial effects on TC and TGs levels when combined with fenofibrate.
A meta-analysis of observational studies on selenium [74] reported a significant U-shape association between serum levels of selenium (< 97.5 and > 132.5 µg/L) and T2DM risk. The combination of selenium and other antioxidants significantly reduced UAER [51]. The meta-analysis of observational studies [95] reported a significantly higher level of Cu in the serum and plasma of patients with DM compared with healthy individuals.
Discussion
Our study revealed that low serum levels of VD and high serum levels of Cu and Zn are associated with an increased risk of T2DM and its complications. Furthermore, supplementation of vitamins C, D, E, and nutrients Cr, Zn, CoQ10, and ALA can significantly impact FBS and glycemic control. Thus, it can result in beneficial impacts in patients with diabetes with/without presenting further complications.
The beneficial effects of VD in T2DM may be partly attributed to its direct and indirect beneficial impacts on insulin resistance and improvement of insulin function. Also, VD is associated to be beneficial for the systemic inflammation caused by increased insulin secretion through its specific receptors in pancreatic β-cells, reduced activity of NF-κB, and increased expression of calbindin against the apoptosis initiated by cytokines. The other uses of VD stem from its antioxidative effects, restricting oxidative biomarkers or elevating antioxidative biomarkers [92]. Furthermore, a link between VD level and the renin-angiotensin system, endothelial function, and blood pressure was indicated, all of which can be explained by the association between low levels of VD and the risk of T2DM and its complications [8, 36, 100]. However, most of the included meta-analyses recommended no effective VD dose to prevent or treat T2DM. A meta-analysis of 12 clinical trials on 4395 samples recommended a high daily dose of VD (≥ 800 IU/d) in combination with Ca ≥ 1000 mg/d for ≤ 12 weeks for the improvement of FBS, HbA1c, and the HOMA index [5]. However, numerous studies [37, 38, 40, 41] have recommended an effective dose for VD only –without Ca- ranging from ≥ 1000 to ≤ 4000 IU/d for ≤ 12 weeks to improve FBS, HbA1c, and HOMA index in those with deficient or sufficient VD levels. He et al. 2018 and Li et al. 2018, suggested concentration of > 2000 IU/d for < 3 months duration for the prevention of T2DM in pre-diabetics patients with insufficient serum levels of VD. The effective anti-inflammatory concentration of VD reported by Yu et al. 2018 was to be ≤ 4000 IU/d. In a meta-analysis, an improvement in lipid profiles was observed through the administration of an effective dose of ≤ 2000 IU/d for ≤ 12 weeks [41]. But another meta-analysis [23] reported a significant increase in TGs levels by intake of both low and high doses of VD (20,000 and 50,000 IU/week). In conclusion, the effect of VD supplements on lipid components and lipid profile differed based on the level of VD.
Non-enzymatic antioxidants such as vitamins C and E can scavenge ROS, protect against lipid peroxidation, inhibit protein kinase-C, decrease inflammatory activity, reverse β-cell apoptosis, and ameliorate insulin resistance [6, 48, 50]. The oxidative damage to cells and vessel walls [101] induced by thiobarbituric acid reactive substances (TBARS) and malondialdehyde (MDA) as end-products of lipid peroxidation, can be decreased by inhibiting the activity of free radicals or by reacting with free radicals after supplementation with antioxidant agents [2]. The recommended minimum effective dose of VC for improving FBS, HbA1c, and lipid profile was 1250 mg/d for 3 months [6, 13]. Supplementation of VE by doses higher than 400 mg/d for ≥ 12 weeks was effective for improving HbA1c in T2DM patients with poor glycemic control or normal baseline levels of VE [7].
The beneficial effects of VK on insulin sensitivity, glucose homeostasis, and risk of diabetes have been reported through decreasing the level of cytokines and inflammatory markers [102]. It has been postulated that vitamin K-dependent bone protein osteocalcin can influence insulin sensitivity by acting directly on pancreatic β-cells, increasing their proliferation and insulin secretion. However, we found no beneficial effects of VK on FBS, FI, HOMA index, and biomarkers of inflammation in our study [20].
VB and its derivatives showed anti-inflammatory effects and are also associated with reducing advanced glycation end (AGE) products and oxidative stress in renal cells [103, 104]. Those, as mentioned earlier, can result in a decreased incidence of albuminuria/proteinuria and prove effective in reducing kidney injury in diabetes. However, this effect was not confirmed by a meta-analysis of 9 clinical trials by VB and its derivatives on renal function [22]. The beneficial effects of single mecobalamin or its combinations with other medications have shown significant improvement in motor and sensory nerve conduction velocity of patients with DPN [21, 53].
Zn is an essential trace element that plays specific critical roles in the metabolism of carbohydrates via insulin synthesis, storage, crystallization, secretion by pancreatic β-cells, function, and translocation into the cells [105]. In addition, it demonstrated to have insulin-mimetic and anti-inflammatory activity; zinc suppresses nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) and protects against apoptosis of β-cells [97]. Although some studies have reported the beneficial effects of Zn supplementation on DN, DPN, peripheral insulin sensitivity, bio-inflammatory markers, DNA damage, and lipid peroxidation [106, 107], there is currently no evidence that supports the use of Zn supplements in the prevention of T2DM [108, 109]. The reason might be the failure of observational studies to differentiate between participants who received Zn alone and those used a combination of Zn with other nutrients [110, 111]. Thus, the interaction between these nutrients and Zn could have affected Zn intake and T2DM risk. Observational studies on the relationship between serum Zn levels and T2DM in Finnish men are contradictory [112] to the conclusions observed in Russian postmenopausal women [113]. The response mechanism against Zn excess in the serum/plasma (hyperzincuria) in diabetic patients [114] is consistent with the observed direct positive relationship between serum/plasma levels of Zn and T2DM. However, a significant linear negative association was reported between serum levels of Zn and the duration of diabetes [98].
Chromium is an essential element for the metabolism of carbohydrate and lipid, and its deficiency is associated with insulin resistance as well as diabetes [115]. It has been observed that Cr can increase the number of insulin receptors and insulin binding at its site of action. It can improve insulin sensitivity and decrease triglyceride levels via enhancing free fatty acid oxidation [94, 116]. However, its impact on glucose homeostasis parameters was controversial in our included meta-analyses. The suggested effective doses of Cr to improve FBS and HbA1c were 200–1000 µg/d and 200 µg/d, respectively [16, 57, 59]. Moreover, the recommended effective dose for improvement of TGs and TC was > 200 µg/d; however, to enhance the level of LDL-C, Cr was recommended at the concentration of < 200 µg/d [15]. Dietary Cr supplements are inexpensive and are safe even at high doses [117].
Inactivity of glycerol-3-phosphate dehydrogenase (G3PD), an electron transporter from the cytosol to the mitochondria, has been reported in diabetic patients. CoQ10 is a component of the mitochondrial respiratory chain that plays a key role in the electron transport chain in the absence of G3PD. In addition, it is a potent lipophilic antioxidant capable of regenerating and recycling other antioxidants such as tocopherol and ascorbates [118]. Although it has beneficial effects on insulin secretion and insulin sensitivity, the results of two meta-analyses were controversial regarding the impact of CoQ10 on glycemic control in diabetic patients [68, 69]. The observed mechanism of the beneficial effects of CoQ10 alone or in combination with fenofibrate on TGs [68] might be related to increased lipolysis of TGs [119].
ALA is commonly used to relieve neuropathic symptoms due to its beneficial effects on DPN via improved nerve blood flow and progress of nitric oxide-mediated endothelium-dependent vasodilation and anti-inflammatory anti-thrombotic activities [77]. Its appropriate dosage in most meta-analyses is usually recommended at 300–600 mg/d for 2–4 weeks [74, 75, 77–79]. The beneficial effects of ALA on the improvement of glycemic control of FBS, HbA1c, and lipid profiles, except for high-density lipoprotein cholesterol (HDL-C), might be related to elevated glutathione levels and the activity of antioxidant enzymes, the prevention of lipid peroxidation, suppression of NF-κB activity, and preservation of β-cell function via insulin sensitivity [120, 121]. Moreover, doubling ALA intake was negatively associated with the T2DM risk [93].
As one of the essential trace elements in maintaining human health, selenium is a crucial component of glutathione peroxidases (GPx). The overexpression of GPx in the islets of Langerhans can protect these cells from oxidative stress and improve their function [122]. Furthermore, a high concentration of selenium may interfere with insulin signaling. However, selenoproteins' anti-oxidative and anti-inflammatory effects have been previously proven [123, 124]. In several studies, lower selenium levels have been detected in patients with T2DM versus healthy individuals, which might be related to the inverse association between selenium and inflammation. Conversely, a higher selenium level in patients with T2DM than in healthy individuals has been reported elsewhere [125, 126], suggesting a U-Shape association between selenium and T2DM. This U-Shape association between selenium and T2DM was confirmed in a meta-analysis of five observational studies on selenium in 13,460 participants [94].
Although Cu is a key component of copper/zinc superoxide dismutase (Cu/Zn SOD) –a scavenger of free radicals- its antioxidative effect is usually known as a pro-oxidant [127]. Induction of oxidative stress and renal dysfunction in diabetic rats and raised lipid peroxidation in patients with T2DM after Cu supplementation [127] suggests that Cu does not protect against ROS. Moreover, higher concentrations of Cu can be replace with Zn and elevate the Cu-to-Zn ratio, resulting in impaired Zn metabolism, and inflammation and aggravation of oxidative stress, consequently [128, 129]. This evidence confirms Qiu et al., 2017 findings, which found higher serum levels of Cu in diabetic patients compared with healthy subjects.
Our study has particular strengths and limitations. The study's main strength is its review of systematic reviews and meta-analyses conducted on the most frequently studied antioxidants. The main limitation of the study is the controversy between the results of some meta-analyses due to differences in several parameters, including sample size, the subjects' health status, the quality score of studies, the supplemented dose, the methods used to measure vitamins/nutrients, not having evaluated the effect of confounding factors, and having not performed subgroup analysis, thereby leading to inconsistencies among the meta-analysis.
Conclusions
This review suggests that antioxidants may present some protective effects against T2DM and its complications and be helpful in the management of diabetes. However, due to the heterogeneity of results among the observational studies and clinical trials, caution should be taken in approving their beneficial effects on T2DM.
Abbreviations
- AGE
Advanced glycation end
- ALA
Alpha-lipoic acid
- BP
Blood pressure
- CoQ10
Coenzyme Q10
- Cr
Chromium
- Cu
Copper
- Cu/Zn SOD
Copper/zinc superoxide dismutase
- DBP
Diastolic blood pressure
- DF
Diabetic foot
- DM
Diabetes mellitus
- DN
Diabetic nephropathy
- DPN
Diabetic polyneuropathy
- DR
Diabetic retinopathy
- EF
Endothelial function
- FBS
Fasting blood sugar
- FI
Fasting insulin
- FMD
Flow-mediated dilation
- G3PD
Glycerol-3-phosphate dehydrogenase
- GPx
Glutathione peroxidases
- HDL-C
High-density lipoprotein cholesterol
- HOMA
Homeostasis Model Assessment
- hs-CRP
High-sensitive C-reactive protein
- LDL-C
Low-density lipoprotein cholesterol
- MDA
Malondialdehyde
- NF-κB
Nuclear factor kappa-light-chain-enhancer of activated B cells
- OR
Odds ratio
- PRISMA
Preferred Reporting Items for Systematic reviews and Meta-Analysis
- ROS
Reactive oxygen species
- RR
Relative risk
- T2DM
Type 2 diabetes mellitus
- TBARS
Thiobarbituric acid reactive substances
- TC
Total cholesterol
- TGs
Triglycerides
- UAER
Urinary albumin excretion rate
- VD
Vitamin D
- Zn
Zinc
Authors' Contributions
OTM and SN conceived and coordinated the study. OTM, SN, MA, and BL participated in the study's design. OTM, MP, and SHM extracted data from the published articles and drafted the manuscript. SN, MA, and BL helped to edit the manuscript draft. MP, OTM, and SN critically reviewed the manuscript and helped with quality assessment. All authors read and approved the final manuscript.
Funding
This study is an in-home study without any financial support.
Data Availability
Not applicable. All data analyzed in the current systematic reviews are extracted from published articles in PubMed, Web of Science, Scopus, and Cochrane Library databases.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing Interest
All authors declare that there are no conflicts of interest.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.IDF, 2021. IDF diabetes atlas, 10th edition 2021. Available at: https://diabetesatlas.org/atlas/tenth-edition. Accessed 19 June 2022.
- 2.Rahimi R, Nikfar S, Larijani B, Abdollahi M. A review on the role of antioxidants in the management of diabetes and its complications. Biomed Pharmacother. 2005;59:365–373. doi: 10.1016/j.biopha.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Ceriello A, Testa R, Genovese S. Clinical implications of oxidative stress and potential role of natural antioxidants in diabetic vascular complications. Nutr Metab Cardiovasc Dis. 2016;26(4):285–292. doi: 10.1016/j.numecd.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Tabatabaei-Malazy O, Khodaeian M, Bitarafan F, Larijani B, MAmoli M. Polymorphisms of antioxidant genes as a target for diabetes management. Int J Mol Cell Med. 2017;6(3):135–47. doi: 10.22088/acadpub.BUMS.6.3.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Asbaghi O, Khosroshahi MZ, Kashkooli S, Abbasnezhad A. Effect of calcium-vitamin D co-supplementation on insulin, insulin sensitivity, and glycemia: a systematic review and meta-analysis of randomized clinical trials. Horm Metab Res. 2019;51(5):288–295. doi: 10.1055/a-0887-0205. [DOI] [PubMed] [Google Scholar]
- 6.Tabatabaei-Malazy O, Nikfar S, Larijani B, Abdollahi M. Influence of ascorbic acid supplementation on type 2 diabetes mellitus in observational and randomized controlled trials; a systematic review with meta-analysis. J Pharm Pharm Sci. 2014;17:554–582. doi: 10.18433/J3ZG6R. [DOI] [PubMed] [Google Scholar]
- 7.Xu R, Zhang S, Tao A, Chen G, Zhang M. Influence of vitamin E supplementation on glycaemic control: a meta-analysis of randomised controlled trials. PLoS ONE. 2014;9:e95008. doi: 10.1371/journal.pone.0095008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seida JC, Mitri J, Colmers IN, Majumdar SR, Davidson MB, Edwards AL, et al. Clinical review: effect of vitamin D3 supplementation on improving glucose homeostasis and preventing diabetes: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2014;99(10):3551–3560. doi: 10.1210/jc.2014-2136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poolsup N, Suksomboon N, Plordplong N. Effect of vitamin D supplementation on insulin resistance and glycaemic control in prediabetes: a systematic review and meta-analysis. Diabet Med. 2016;33(3):290–299. doi: 10.1111/dme.12893. [DOI] [PubMed] [Google Scholar]
- 10.George PS, Pearson ER, Witham MD. Effect of vitamin D supplementation on glycaemic control and insulin resistance: a systematic review and meta-analysis. Diabet Med. 2012;29(8):e142–150. doi: 10.1111/j.1464-5491.2012.03672.x. [DOI] [PubMed] [Google Scholar]
- 11.Rafiq S, Jeppesen PB. Is hypovitaminosis D related to incidence of type 2 diabetes and high fasting glucose level in healthy subjects: a systematic review and meta-analysis of observational studies. Nutrients. 2018;10(1):pii:E59. doi: 10.3390/nu10010059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan H, Kunutsor S, Franco OH, Chowdhury R. Vitamin D, type 2 diabetes and other metabolic outcomes: a systematic review and meta-analysis of prospective studies. Proc Nutr Soc. 2013;72(1):89–97. doi: 10.1017/S0029665112002765. [DOI] [PubMed] [Google Scholar]
- 13.Tareke AA, Hadgu AA. The effect of vitamin C supplementation on lipid profile of type 2 diabetic patients: a systematic review and meta-analysis of clinical trials. Diabetol Metab Syndr. 2021;13(1):24. doi: 10.1186/s13098-021-00640-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ashor AW, Werner AD, Lara J, Willis ND, Mathers JC, Siervo M. Effects of vitamin C supplementation on glycaemic control: a systematic review and meta-analysis of randomised controlled trials. Eur J Clin Nutr. 2017;71(12):1371–1380. doi: 10.1038/ejcn.2017.24. [DOI] [PubMed] [Google Scholar]
- 15.Asbaghi O, Naeini F, Ashtary-Larky D, Moradi S, Zakeri N, Eslampour E, et al. Effects of chromium supplementation on lipid profile in patients with type 2 diabetes: A systematic review and dose-response meta-analysis of randomized controlled trials. J Trace Elem Med Biol. 2021;66:126741. doi: 10.1016/j.jtemb.2021.126741. [DOI] [PubMed] [Google Scholar]
- 16.Suksomboon N, Poolsup N, Yuwanakorn A. Systematic review and meta-analysis of the efficacy and safety of chromium supplementation in diabetes. J Clin PharmTher. 2014;39(3):292–306. doi: 10.1111/jcpt.12147. [DOI] [PubMed] [Google Scholar]
- 17.Patal PC, Cardino MT, Jimeno CA. A meta-analysis on the effect of chromium picolinate on glucose and lipid profiles among patients with type 2 diabetes mellitus. Philipp J Intern Med. 2010;48(1):32–37. [Google Scholar]
- 18.Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, et al., OCEBM Levels of Evidence Working Group. The Oxford levels of evidence2. Oxford Centre for Evidence-Based Medicine. 2019; Available at: http://www.cebm.net/index.aspx?o=5653. Last accessed: June 9, 2019
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviewsand Meta-analysis: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shahdadian F, Mohammadi H, Rouhani MH. Effect of vitamin K supplementation on glycemic control: a systematic review and meta-analysis of clinical trials. Horm Metab Res. 2018;50(3):227–235. doi: 10.1055/s-0044-100616. [DOI] [PubMed] [Google Scholar]
- 21.Sawangjit R, Thongphui S, Chaichompu W, Phumart P. Efficacy and safety of mecobalamin on peripheral neuropathy: a systematic review and meta-analysis of randomized controlled trials. J Altern Complement Med. 2020;26(12):1117–1129. doi: 10.1089/acm.2020.0068. [DOI] [PubMed] [Google Scholar]
- 22.Raval AD, Thakker D, Rangoonwala AN, Gor D, Walia R. Vitamin B and its derivatives for diabetic kidney disease. Cochrane Database Syst Rev. 2015;1:CD009403. doi: 10.1002/14651858.CD009403.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.AlAnouti F, Abboud M, Papandreou D, Mahboub N, Haidar S, Rizk R. Effects of vitamin D supplementation on lipid profile in adults with the metabolic syndrome: a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2020;12(11):3352. doi: 10.3390/nu12113352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Emadzadeh M, Sahebi R, Khedmatgozar H, Sadeghi R, Farjami M, Sharifan P, et al. A systematic review and meta-analysis of the effect of Vitamin D-fortified food on glycemic indices. BioFactors. 2020;46(4):502–513. doi: 10.1002/biof.1632. [DOI] [PubMed] [Google Scholar]
- 25.Yammine K, Wehbe R, Assi C. A systematic review on the efficacy of vitamin D supplementation on diabetic peripheral neuropathy. Clin Nutr. 2020;39(10):2970–2974. doi: 10.1016/j.clnu.2020.01.022. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Y, Tan H, Tang J, Li J, Chong W, Hai Y, et al. Effects of vitamin D supplementation on prevention of type 2 diabetes in patients with prediabetes: a systematic review and meta-analysis. Diabetes Care. 2020;43(7):1650–1658. doi: 10.2337/dc19-1708. [DOI] [PubMed] [Google Scholar]
- 27.Gupta S, Goyal P, Feinn RS, Mattana J. Role of vitamin D and its analogues in diabetic nephropathy: a meta-analysis. Am J Med Sci. 2019;357(3):223–229. doi: 10.1016/j.amjms.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 28.Hu Z, Chen J, Sun X, Wang L, Wang A. Efficacy of vitamin D supplementation on glycemic control in type 2 diabetes patients: a meta-analysis of interventional studies. Medicine (Baltimore) 2019;98(14):e14970. doi: 10.1097/MD.0000000000014970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sahebi R, Rezayi M, Emadzadeh M, Salehi M, Tayefi M, Parizadeh SM, et al. The effects of vitamin D supplementation on indices of glycemic control in Iranian diabetics: a systematic review and meta-analysis. Complement Ther Clin Pract. 2019;34:294–304. doi: 10.1016/j.ctcp.2018.12.009. [DOI] [PubMed] [Google Scholar]
- 30.Wang Y, Yang S, Zhou Q, Zhang H, Yi B. Effects of vitamin D supplementation on renal function, inflammation and glycemic control in patients with diabetic nephropathy: a systematic review and meta-analysis. Kidney Blood Press Res. 2019;44(1):72–87. doi: 10.1159/000498838. [DOI] [PubMed] [Google Scholar]
- 31.He S, Yu S, Zhou Z, Wang C, Wu Y, Li W. Effect of vitamin D supplementation on fasting plasma glucose, insulin resistance and prevention of type 2 diabetes mellitus in non-diabetics: a systematic review and meta-analysis. Biomed Rep. 2018;8(5):475–484. doi: 10.3892/br.2018.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li X, Liu Y, Zheng Y, Wang P, Zhang Y. The effect of vitamin D supplementation on glycemic control in type 2 diabetes patients: a systematic review and meta-analysis. Nutrients. 2018; 10(3). pii: E375. doi: 10.3390/nu10030375. [DOI] [PMC free article] [PubMed]
- 33.Mansournia MA, Ostadmohammadi V, Doosti-Irani A, Ghayour-Mobarhan M, Ferns G, Akbari H, et al. The effects of vitamin D supplementation on biomarkers of inflammation and oxidative stress in diabetic patients: a systematic review and meta-analysis of randomized controlled trials. Horm Metab Res. 2018;50(6):429–440. doi: 10.1055/a-0630-1303. [DOI] [PubMed] [Google Scholar]
- 34.Tabrizi R, Vakili S, Lankarani KB, Akbari M, Jamilian M, Mahdizadeh Z, et al. The effects of vitamin D supplementation on markers related to endothelial function among patients with metabolic syndrome and related disorders: a systematic review and meta-analysis of clinical trials. Horm Metab Res. 2018;50(8):587–596. doi: 10.1055/a-0651-4842. [DOI] [PubMed] [Google Scholar]
- 35.Yu Y, Tian L, Xiao Y, Huang G, Zhang M. Effect of vitamin D supplementation on some inflammatory biomarkers in type 2 diabetes mellitus subjects: a systematic review and meta-analysis of randomized controlled trials. Ann Nutr Metab. 2018;73(1):62–73. doi: 10.1159/000490358. [DOI] [PubMed] [Google Scholar]
- 36.Krul-Poel YH, Ter Wee MM, Lips P, Simsek S. Management of endocrine disease: The effect of vitamin D supplementation on glycaemic control in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Eur J Endocrinol. 2017;176(1):R1–R14. doi: 10.1530/EJE-16-0391. [DOI] [PubMed] [Google Scholar]
- 37.Lee CJ, Iyer G, Liu Y, Kalyani RR, Bamba N, Ligon CB, et al. The effect of vitamin D supplementation on glucose metabolism in type 2 diabetes mellitus: a systematic review and meta-analysis of intervention studies. J Diabetes Complications. 2017;31(7):1115–1126. doi: 10.1016/j.jdiacomp.2017.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mirhosseini N, Vatanparast H, Mazidi M, Kimball SM. The effect of improved serum 25-hydroxyvitamin D status on glycemic control in diabetic patients: a meta-analysis. J Clin Endocrinol Metab. 2017;102(9):3097–3110. doi: 10.1210/jc.2017-01024. [DOI] [PubMed] [Google Scholar]
- 39.de Paula TP, Kramer CK, Viana LV, Azevedo MJ. Effects of individual micronutrients on blood pressure in patients with type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. Sci Rep. 2017;7:40751. doi: 10.1038/srep40751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wu C, Qiu S, Zhu X, Li L. Vitamin D supplementation and glycemic control in type 2 diabetes patients: a systematic review and meta-analysis. Metabolism. 2017;73:67–76. doi: 10.1016/j.metabol.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 41.Jafari T, Fallah AA, Barani A. Effects of vitamin D on serum lipid profile in patients with type 2 diabetes: a meta-analysis of randomized controlled trials. ClinNutr. 2016;35(6):1259–1268. doi: 10.1016/j.clnu.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 42.Lee KJ, Lee YJ. Effects of vitamin D on blood pressure in patients with type 2 diabetes mellitus. Int J Clin Pharmacol Ther. 2016;54(4):233–242. doi: 10.5414/CP202493. [DOI] [PubMed] [Google Scholar]
- 43.Chokhandre MK, Mahmoud MI, Hakami T, Jafer M, Inamdar AS. Vitamin D & its analogues in type 2 diabetic nephropathy: a systematic review. J Diabetes Metab Disord. 2015;14:58. doi: 10.1186/s40200-015-0186-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Derakhshanian H, Shab-Bidar S, Speakman JR, Nadimi H, Djafarian K. Vitamin D and diabetic nephropathy: a systematic review and meta-analysis. Nutrition. 2015;31(10):1189–1194. doi: 10.1016/j.nut.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 45.Zhao J, Dong J, Wang H, Shang H, Zhang D, Liao L. Efficacy and safety of vitamin D3 in patients with diabetic nephropathy: a meta-analysis of randomized controlled trials. Chin Med J (Engl) 2014;127(15):2837–2843. [PubMed] [Google Scholar]
- 46.Mitri J, Muraru MD, Pittas AG. Vitamin D and type 2 diabetes: a systematic review. Eur J Clin Nutr. 2011;65(9):1005–1015. doi: 10.1038/ejcn.2011.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Namkhah Z, Ashtary-Larky D, Naeini F, Clark CCT, Asbaghi O. Does vitamin C supplementation exert profitable effects on serum lipid profile in patients with type 2 diabetes? A systematic review and dose-response meta-analysis. Pharmacol Res. 2021;169:105665. doi: 10.1016/j.phrs.2021.105665. [DOI] [PubMed] [Google Scholar]
- 48.Khodaeian M, Tabatabaei-Malazy O, Qorbani M, Farzadfar F, Amini P, et al. Effect of vitamins C and E on insulin resistance in diabetes: a meta-analysis study. Eur J Clin Invest. 2015;45(11):1161–1174. doi: 10.1111/eci.12534. [DOI] [PubMed] [Google Scholar]
- 49.Suksomboon N, Poolsup N, Sinprasert S. Effects of vitamin E supplementation on glycaemic control in type 2 diabetes: systematic review of randomized controlled trials. J Clin Pharm Ther. 2011;36(1):53–63. doi: 10.1111/j.1365-2710.2009.01154.x. [DOI] [PubMed] [Google Scholar]
- 50.Balbi ME, Tonin FS, Mendes AM, Borba HH, Wiens A, Fernandez-Llimos F, Pontarolo R. Antioxidant effects of vitamins in type 2 diabetes: a meta-analysis of randomized controlled trials. Diabetol Metab Syndr. 2018;10:18. doi: 10.1186/s13098-018-0318-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bolignano D, Cernaro V, Gembillo G, Baggetta R, Buemi M, D'Arrigo G. Antioxidant agents for delaying diabetic kidney disease progression: a systematic review and meta-analysis. PLoS ONE. 2017;12(6):e0178699. doi: 10.1371/journal.pone.0178699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kandhare AD, Mukherjee A, Bodhankar SL. Antioxidant for treatment of diabetic nephropathy: a systematic review and meta-analysis. Chem Biol Interact. 2017;278:212–221. doi: 10.1016/j.cbi.2017.10.031. [DOI] [PubMed] [Google Scholar]
- 53.Zheng C, Ou W, Shen H, Zhou Z, Wang J. Combined therapy of diabetic peripheral neuropathy with breviscapine and mecobalamin: a systematic review and a meta-analysis of Chinese studies. Biomed Res Int. 2015:680756. 10.1155/2015/680756. [DOI] [PMC free article] [PubMed]
- 54.Montero D, Walther G, Stehouwer CD, Houben AJ, Beckman JA, Vinet A. Effect of antioxidant vitamin supplementation on endothelial function in type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2014;15(2):107–116. doi: 10.1111/obr.12114. [DOI] [PubMed] [Google Scholar]
- 55.Akbar S, Bellary S, Griffiths HR. Dietary antioxidant interventions in type 2 diabetes patients: a meta-analysis. Br J Diabetes Vasc Dis. 2011;11(2):62–68. doi: 10.1177/1474651411407558. [DOI] [Google Scholar]
- 56.Zhao F, Pan D, Wang N, Xia H, Zhang H, Wang S, Sun G. Effect of chromium supplementation on blood glucose and lipid levels in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Biol Trace Elem Res. 2021 doi: 10.1007/s12011-021-02693-3. [DOI] [PubMed] [Google Scholar]
- 57.Asbaghi O, Fatemeh N, Mahnaz RK, Ehsan G, Elham E, Behzad N, et al. Effects of chromium supplementation on glycemic control in patients with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Pharmacol Res. 2020;161:105098. doi: 10.1016/j.phrs.2020.105098. [DOI] [PubMed] [Google Scholar]
- 58.Yin RV, Phung OJ. Effect of chromium supplementation on glycated hemoglobin and fasting plasma glucose in patients with diabetes mellitus. Nutr J. 2015;14:14. doi: 10.1186/1475-2891-14-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Balk EM, Tatsioni A, Lichtenstein AH, Lau J, Pittas AG. Effect of chromium supplementation on glucose metabolism and lipids: a systematic review of randomized controlled trials. Diabetes Care. 2007;30(8):2154–2163. doi: 10.2337/dc06-0996. [DOI] [PubMed] [Google Scholar]
- 60.Althuis MD, Jordan NE, Ludington EA, Wittes JT. Glucose and insulin responses to dietary chromium supplements: a meta-analysis. Am J Clin Nutr. 2002;76(1):148–155. doi: 10.1093/ajcn/76.1.148. [DOI] [PubMed] [Google Scholar]
- 61.Jayawardena R, Ranasinghe P, Kodithuwakku W, Dalpatadu C, Attia J. Zinc supplementation in pre-diabetes mellitus: a systematic review and meta-analysis. Minerva Endocrinol (Torino) 2021 doi: 10.23736/S2724-6507.21.03234-X. [DOI] [PubMed] [Google Scholar]
- 62.Pompano LM, Boy E. Effects of dose and duration of zinc interventions on risk factors for type 2 diabetes and cardiovascular disease: a systematic review and meta-analysis. Adv Nutr. 2021;12(1):141–160. doi: 10.1093/advances/nmaa087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Asbaghi O, Sadeghian M, Fouladvand F, Panahande B, Nasiri M, Khodadost M, et al. Effects of zinc supplementation on lipid profile in patients with type 2 diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis. 2020;30(8):1260–1271. doi: 10.1016/j.numecd.2020.03.021. [DOI] [PubMed] [Google Scholar]
- 64.Wang X, Wu W, Zheng W, Fang X, Chen L, Rink L, et al. Zinc supplementation improves glycemic control for diabetes prevention and management: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2019; pii: nqz041. 10.1093/ajcn/nqz041. [DOI] [PubMed]
- 65.Capdor J, Foster M, Petocz P, Samman S. Zinc and glycemic control: a meta-analysis of randomised placebo controlled supplementation trials in humans. J Trace Elem Med Biol. 2013;27(2):137–142. doi: 10.1016/j.jtemb.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 66.Jayawardena R, Ranasinghe P, Galappatthy P, Malkanthi R, Constantine G, Katulanda P. Effects of zinc supplementation on diabetes mellitus: a systematic review and meta-analysis. Diabetol Metab Syndr. 2012;4(1):13. doi: 10.1186/1758-5996-4-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dludla PV, Nyambuya TM, Orlando P, Silvestri S, Mxinwa V, Mokgalaboni K, et al. The impact of coenzyme Q10 on metabolic and cardiovascular disease profiles in diabetic patients: A systematic review and meta-analysis of randomized controlled trials. Endocrinol Diabetes Metab. 2020;3(2):e00118. doi: 10.1002/edm2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Suksomboon N, Poolsup N, Juanak N. Effects of coenzyme Q10 supplementation on metabolic profile in diabetes: a systematic review and meta-analysis. J Clin Pharm Ther. 2015;40(4):413–418. doi: 10.1111/jcpt.12280. [DOI] [PubMed] [Google Scholar]
- 69.Moradi M, Haghighatdoost F, Feizi A, Larijani B, Azadbakht L. Effect of coenzyme Q10 supplementation on diabetes biomarkers: a systematic review and meta-analysis of randomized controlled clinical trials. Arch Iran Med. 2016; 19(8):588-96. 0161908/AIM.0012 [PubMed]
- 70.Ebada MA, Fayed N, Fayed L, Alkanj S, Abdelkarim A, Farwati H, et al. Efficacy of Alpha-lipoic Acid in The Management of Diabetes Mellitus: A Systematic Review and Meta-analysis. Iran J Pharm Res. 2019;18(4):2144–2156. doi: 10.22037/ijpr.2019.1100842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rahimlou M, Asadi M, Banaei Jahromi N, Mansoori A. Alpha-lipoic acid (ALA) supplementation effect on glycemic and inflammatory biomarkers: A Systematic Review and meta- analysis. Clin Nutr ESPEN. 2019;32:16–28. doi: 10.1016/j.clnesp.2019.03.015. [DOI] [PubMed] [Google Scholar]
- 72.Akbari M, Ostadmohammadi V, Lankarani KB, Tabrizi R, Kolahdooz F, Khatibi SR, et al. The effects of alpha-lipoic acid supplementation on glucose control and lipid profiles among patients with metabolic diseases: A systematic review and meta-analysis of randomized controlled trials. Metabolism. 2018;87:56–69. doi: 10.1016/j.metabol.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 73.Amato Nesbit S, Sharma R, Waldfogel JM, Zhang A, Bennett WL, Yeh HC, et al. Non-pharmacologic treatments for symptoms of diabetic peripheral neuropathy: a systematic review. Curr Med Res Opin. 2018; 1–11. 10.1080/03007995.2018.1497958. [DOI] [PubMed]
- 74.Wang X, Lin H, Xu S, Jin Y, Zhang R. Alpha lipoic acid combined with epalrestat: a therapeutic option for patients with diabetic peripheral neuropathy. Drug Des Devel Ther. 2018;7(12):2827–2840. doi: 10.2147/DDDT.S168878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Çakici N, Fakkel TM, van Neck JW, Verhagen AP, Coert JH. Systematic review of treatments for diabetic peripheral neuropathy. Diabet Med. 2016;33(11):1466–1476. doi: 10.1111/dme.13083. [DOI] [PubMed] [Google Scholar]
- 76.Snedecor SJ, Sudharshan L, Cappelleri JC, Sadosky A, Mehta S, Botteman M. Systematic review and meta-analysis of pharmacological therapies for painful diabetic peripheral neuropathy. Pain Pract. 2014;14(2):167–184. doi: 10.1111/papr.12054. [DOI] [PubMed] [Google Scholar]
- 77.Han T, Bai J, Liu W, Hu Y. A systematic review and meta-analysis of α-lipoic acid in the treatment of diabetic peripheral neuropathy. Eur J Endocrinol. 2012;167(4):465–471. doi: 10.1530/EJE-12-0555. [DOI] [PubMed] [Google Scholar]
- 78.Mijnhout GS, Alkhalaf A, Kleefstra N, Bilo HJ. Alpha lipoic acid: a new treatment for neuropathic pain in patients with diabetes? Neth J Med. 2010;68(4):158–162. [PubMed] [Google Scholar]
- 79.Ziegler D, Nowak H, Kempler P, Vargha P, Low PA. Treatment of symptomatic diabetic polyneuropathy with the antioxidant alpha-lipoic acid: a meta-analysis. Diabet Med. 2004;21(2):114–121. doi: 10.1111/j.1464-5491.2004.01109.x. [DOI] [PubMed] [Google Scholar]
- 80.Rafiq S, Jeppesen PB. Insulin Resistance Is Inversely Associated with the Status of Vitamin D in Both Diabetic and Non-Diabetic Populations. Nutrients. 2021;13(6):1742. doi: 10.3390/nu13061742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dai J, Jiang C, Chen H, Chai Y. Vitamin D and diabetic foot ulcer: a systematic review and meta-analysis. Nutr Diabetes. 2019;9(1):8. doi: 10.1038/s41387-019-0078-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhang B, Zhao W, Tu J, Wang X, Hao Y, Wang H, et al. The relationship between serum 25-hydroxyvitamin D concentration and type 2 diabetic peripheral neuropathy: A systematic review and a meta-analysis. Medicine (Baltimore) 2019;98(48):e18118. doi: 10.1097/MD.0000000000018118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ekmekcioglu C, Haluza D, Kundi M. 25-hydroxyvitamin D status and risk for colorectal cancer and type 2 diabetes mellitus: a systematic review and meta-analysis of epidemiological studies. Int J Environ Res Public Health. 2017; 14(2). pii: E127. 10.3390/ijerph14020127. [DOI] [PMC free article] [PubMed]
- 84.Lucato P, Solmi M, Maggi S, Bertocco A, Bano G, Trevisan C, et al. Low vitamin D levels increase the risk of type 2 diabetes in older adults: a systematic review and meta-analysis. Maturitas. 2017;100:8–15. doi: 10.1016/j.maturitas.2017.02.016. [DOI] [PubMed] [Google Scholar]
- 85.Luo BA, Gao F, Qin LL. The association between vitamin D deficiency and diabetic retinopathy in type 2 diabetes: a meta-analysis of observational studies. Nutrients. 2017; 9(3). pii: E307. 10.3390/nu9030307. [DOI] [PMC free article] [PubMed]
- 86.Qu GB, Wang LL, Tang X, Wu W, Sun YH. The association between vitamin D level and diabetic peripheral neuropathy in patients with type 2 diabetes mellitus: an update systematic review and meta-analysis. J Clin Transl Endocrinol. 2017;9:25–31. doi: 10.1016/j.jcte.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Liang F, Wang K, Zhang H, Zhang J, Nie X, Zhang Zh, et al. Serum 25-hydroxyvitamin D levels and diabetic retinopathy: a systematic meta-analysis. Int J Clin Exp Pathol. 2016;9(12):12843–12848. [Google Scholar]
- 88.Lv WS, Zhao WJ, Gong SL, Fang DD, Wang B, Fu ZJ, et al. Serum 25-hydroxyvitamin D levels and peripheral neuropathy in patients with type 2 diabetes: a systematic review and meta-analysis. J Endocrinol Invest. 2015;38(5):513–518. doi: 10.1007/s40618-014-0210-6. [DOI] [PubMed] [Google Scholar]
- 89.Afzal S, Bojesen SE, Nordestgaard BG. Low 25-hydroxyvitamin D and risk of type 2 diabetes: a prospective cohort study and meta-analysis. Clin Chem. 2013;59(2):381–391. doi: 10.1373/clinchem.2012.193003. [DOI] [PubMed] [Google Scholar]
- 90.Song Y, Wang L, Pittas AG, Del Gobbo LC, Zhang C, Manson JE, et al. Blood 25-hydroxy vitamin D levels and incident type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2013;36(5):1422–1428. doi: 10.2337/dc12-0962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Forouhi NG, Ye Z, Rickard AP, Khaw KT, Luben R, Langenberg C, et al. Circulating 25-hydroxyvitamin D concentration and the risk of type 2 diabetes: results from the European Prospective Investigation into Cancer (EPIC)-Norfolk cohort and updated meta-analysis of prospective studies. Diabetologia. 2012;55(8):2173–2182. doi: 10.1007/s00125-012-2544-y. [DOI] [PubMed] [Google Scholar]
- 92.Pittas AG, Lau J, Hu FB, Dawson-Hughes B. The role of vitamin D and calcium in type 2 diabetes. a systematic review and meta-analysis. J Clin Endocrinol Metab. 2007;92(6):2017–29. doi: 10.1210/jc.2007-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Muley A, Muley P, Shah M. ALA, fatty fish or marine n-3 fatty acids for preventing DM?: a systematic review and meta-analysis. Curr Diabetes Rev. 2014;10(3):158–165. doi: 10.2174/1573399810666140515113137. [DOI] [PubMed] [Google Scholar]
- 94.Wang ZQ, Zhang XH, Russell JC, Hulver M, Cefalu WT. Chromium picolinate enhances skeletal muscle cellular insulin signaling in vivo in obese, insulin-resistant JCR: LA-cp rats. J Nutr. 2006;136:415–420. doi: 10.1093/jn/136.2.415. [DOI] [PubMed] [Google Scholar]
- 95.Qiu Q, Zhang F, Zhu W, Wu J, Liang M. Copper in diabetes mellitus: a meta-analysis and systematic review of plasma and serum studies. Biol Trace Elem Res. 2017;177(1):53–63. doi: 10.1007/s12011-016-0877-y. [DOI] [PubMed] [Google Scholar]
- 96.Pearsey HM, Henson J, Sargeant JA, Davies MJ, Khunti K, Suzuki T, et al. Zinc-alpha2-glycoprotein, dysglycaemia and insulin resistance: a systematic review and meta-analysis. Rev Endocr Metab Disord. 2020;21(4):569–575. doi: 10.1007/s11154-020-09553-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Fernández-Cao JC, Warthon-Medina M, H Moran V, Arija V, Doepking C, Serra-Majem L, et al. Zinc intake and status and risk of type 2 diabetes mellitus: a systematic review and meta-analysis. Nutrients. 2019;11(5).pii: E1027. 10.3390/nu11051027. [DOI] [PMC free article] [PubMed]
- 98.Fernández-Cao JC, Warthon-Medina M, Hall Moran V, Arija V, Doepking C, Lowe NM. Dietary zinc intake and whole blood zinc concentration in subjects with type 2 diabetes versus healthy subjects: a systematic review, meta-analysis and meta-regression. J Trace Elem Med Biol. 2018;49:241–251. doi: 10.1016/j.jtemb.2018.02.008. [DOI] [PubMed] [Google Scholar]
- 99.Hamer M, Chida Y. Intake of fruit, vegetables, and antioxidants and risk of type 2 diabetes: systematic review and meta-analysis. J Hypertens. 2007;25(12):2361–2369. doi: 10.1097/HJH.0b013e3282efc214. [DOI] [PubMed] [Google Scholar]
- 100.Beveridge LA, Struthers AD, Khan F, Jorde R, Scragg R, Macdonald HM, et al. D-PRESSURE Collaboration. Effect of vitamin D supplementation on blood pressure: a systematic review and meta-analysis incorporating individual patient data. JAMA Intern Med. 2015;175(5):745–54. doi: 10.1001/jamainternmed.2015.0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Mahreen R, Mohsin M, Nasreen Z, Siraj M, Ishaq M. Significantly increased levels of serum malonaldehyde in type 2 diabetics with myocardial infarction. Int J Diabetes Dev Ctries. 2010;30(1):49–51. doi: 10.4103/0973-3930.60006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ohsaki Y, Shirakawa H, Hiwatashi K, Furukawa Y, Mizutani T, Komai M. Vitamin K suppresses lipopolysaccharide-induced inflammation in the rat. Biosci Biotechnol Biochem. 2006;70:926–932. doi: 10.1271/bbb.70.926. [DOI] [PubMed] [Google Scholar]
- 103.Thornalley PJ. The potential role of thiamine (vitamin B1) in diabetic complications. Curr Diabetes Rev. 2005;1(3):287–298. doi: 10.2174/157339905774574383. [DOI] [PubMed] [Google Scholar]
- 104.Karachalias N, Babaei-Jadidi R, Ahmed N, Thornalley PJ. Accumulation of fructosyl-lysine and advanced glycation end products in the kidney, retina and peripheral nerve of streptozotocin-induced diabetic rats. Biochem Soc Trans. 2003;31(Pt 6):1423–1425. doi: 10.1042/bst0311423. [DOI] [PubMed] [Google Scholar]
- 105.Moore WT, Bowser SM, Fausnacht DW, Staley LL, Suh KS, Liu D. Beta cell function and the nutritional state: dietary factors that influence insulin secretion. Curr Diab Rep. 2015;15(10):76. doi: 10.1007/s11892-015-0650-1. [DOI] [PubMed] [Google Scholar]
- 106.Tang X, Shay NF. Zinc has an insulin-like effect on glucose transport mediated by phosphoinositol-3-kinase and Akt in 3 T3–L1 fibroblasts and adipocytes. J Nutr. 2001;131:1414–1420. doi: 10.1093/jn/131.5.1414. [DOI] [PubMed] [Google Scholar]
- 107.Prasad AS, Bao B, Beck FW, Kucuk O, Sarkar FH. Antioxidant effect of zinc in humans. Free Radic Biol Med. 2004;37:1182–1190. doi: 10.1016/j.freeradbiomed.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 108.El Dib R, Gameiro OL, Ogata MS, Módolo NS, Braz LG, Jorge EC, et al. Zinc supplementation for the prevention of type 2 diabetes mellitus in adults with insulin resistance. Cochrane. Database Syst Rev. 2015; 5: CD005525. 10.1002/14651858.CD005525.pub3. [DOI] [PMC free article] [PubMed]
- 109.Beletate V, El Dib RP, Atallah AN. Zinc supplementation for the prevention of type 2 diabetes mellitus. Cochrane Database Syst Rev. 1:CD005525.Review. Update in: Cochrane Database Syst Rev. 2007; 2015;5:CD005525. [DOI] [PubMed]
- 110.Drake I, Hindy G, Ericson U, Orho-Melander M. A prospective study of dietary and supplemental zinc intake and risk of type 2 diabetes depending on genetic variation in SLC30A8. Genes Nutr. 2017;12:30. doi: 10.1186/s12263-017-0586-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Song Y, Xu Q, Park Y, Hollenbeck A, Schatzkin A, Chen H. Multivitamins, individual vitamin and mineral supplements, and risk of diabetes among older U.S. adults. Diabetes Care. 2011;34(1):108–14. doi: 10.2337/dc10-1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yary T, Virtanen JK, Ruusunen A, Tuomainen TP, Voutilainen S. Serum zinc and risk of type 2 diabetes incidence in men: The Kuopio Ischaemic Heart Disease Risk Factor Study. J Trace Elem Med Biol. 2016;33:120–124. doi: 10.1016/j.jtemb.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 113.Skalnaya MG, Skalny AV, Yurasov VV, Demidov VA, Grabeklis AR, Radysh IV, et al. Serum trace elements and electrolytes are associated with fasting plasma glucose and HbA(1c) in postmenopausal women with type 2 diabetes mellitus. Biol Trace Elem Res. 2017;177(1):25–32. doi: 10.1007/s12011-016-0868-z. [DOI] [PubMed] [Google Scholar]
- 114.Liu B, Feng W, Wang J, Li Y, Han X, Hu H, Guo H, Zhang X, He M. Association of urinary metals levels with type 2 diabetes risk in coke oven workers. Environ Pollut. 2016;210:1–8. doi: 10.1016/j.envpol.2015.11.046. [DOI] [PubMed] [Google Scholar]
- 115.Vincent JB. Chromium: celebrating 50 years as an essential element? Dalton Trans. 2010;39:3787–3894. doi: 10.1039/b920480f. [DOI] [PubMed] [Google Scholar]
- 116.Chen G, Liu P, Pattar GR, Tackett L, Bhonagiri P, Strawbridge AB, Elmendorf JS. Chromium activates glucose transporter 4 traffi cking and enhances insulin-stimulated glucose transport in T3–L1 adipocytes via acholesterol-dependent mechanism. Mol Endocrinol. 2006;20:857–870. doi: 10.1210/me.2005-0255. [DOI] [PubMed] [Google Scholar]
- 117.Nielsen F. Controversial chromium: does the superstar mineral of the mountebanks receive appropriate attention from clinicians and nutritionists? Nutr Today. 1996;31:226–233. doi: 10.1097/00017285-199611000-00002. [DOI] [Google Scholar]
- 118.Bhagavan HN, Chopra RK. Coenzyme Q10: absorption, tissue uptake, metabolism and pharmacokinetics. Free Radic Res. 2006;40:445–453. doi: 10.1080/10715760600617843. [DOI] [PubMed] [Google Scholar]
- 119.Marcoff L, Thompson PD. The role of coenzymeQ10 in statin-associated myopathy: a systematic review. J Am Coll Cardiol. 2007;49:2231–2237. doi: 10.1016/j.jacc.2007.02.049. [DOI] [PubMed] [Google Scholar]
- 120.Stevens MJ, Obrosova I, Cao X, Van Huysen C, Greene DA. Effects of DL-alpha-lipoic acid on peripheral nerve conduction, blood flow, energy metabolism, and oxidative stress in experimental diabetic neuropathy. Diabetes. 2000;49:1006–1015. doi: 10.2337/diabetes.49.6.1006. [DOI] [PubMed] [Google Scholar]
- 121.Cummings BP, Stanhope KL, Graham JL, Evans JL, Baskin DG, Griffen SC, et al. Dietary fructose accelerates the development of diabetes in UCD-T2DM rats: amelioration by the antioxidant, alpha-lipoic acid. Am J Phys Regul Integr Comp Phys. 2010;298:R1343–1350. doi: 10.1152/ajpregu.00468.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Campbell SC, Aldibbiat A, Marriott CE, Landy C, Ali T, Ferris WF, et al. Selenium stimulates pancreatic beta-cell gene expression and enhances islet function. Febs Lett. 2008;582(15):2333–2337. doi: 10.1016/j.febslet.2008.05.038. [DOI] [PubMed] [Google Scholar]
- 123.Rayman MP, Stranges S. Epidemiology of selenium and type 2 diabetes: can we make sense of it? Free Radic Biol Med. 2013;65:1557–1564. doi: 10.1016/j.freeradbiomed.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 124.Rayman MP. Selenium and human health. Lancet. 2012;379(9822):1256–1268. doi: 10.1016/S0140-6736(11)61452-9. [DOI] [PubMed] [Google Scholar]
- 125.Laclaustra M, Navas-Acien A, Stranges S, Ordovas JM, Guallar E. Serum selenium concentrations and diabetes in U.S. Adults: national health and nutrition examination survey (NHANES) 2003–2004. Environ Health Perspect. 2009;117(9):1409–13. doi: 10.1289/ehp.0900704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Stranges S, Galletti F, Farinaro E, D'Elia L, Russo O, Iacone R, et al. Associations of selenium status with cardiometabolic risk factors: an 8-year follow-up analysis of the Olivetti heart study. Atherosclerosis. 2011;217(1):274–278. doi: 10.1016/j.atherosclerosis.2011.03.027. [DOI] [PubMed] [Google Scholar]
- 127.Galhardi CM, Diniz YS, Faine LA, Rodrigues HG, Burneiko RC, Ribas BO, et al. Toxicity of copper intake: lipid profile, oxidative stress and susceptibility to renal dysfunction. Food Chem Toxicol. 2004;42:2053–2060. doi: 10.1016/j.fct.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 128.Chasapis CT, Loutsidou AC, Spiliopoulou CA, Stefanidou ME. Zinc and human health: an update. Arch Toxicol. 2012;86:521–534. doi: 10.1007/s00204-011-0775-1. [DOI] [PubMed] [Google Scholar]
- 129.Formigari A, Gregianin E, Irato P. The effect of zinc and the role of p53 in copper-induced cellular stress responses. J Appl Toxicol. 2013;33:527–536. doi: 10.1002/jat.2854. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable. All data analyzed in the current systematic reviews are extracted from published articles in PubMed, Web of Science, Scopus, and Cochrane Library databases.