Abstract
Background
Sleep is essential for recovery from illness. As a result, researchers have shown a growing interest in the sleep of hospitalized patients. Although many studies have been conducted over the past years, an up to date systematic review of the results is missing.
Objective
The objective of this systematic review was to assess sleep quality and quantity of hospitalized patients and sleep disturbing factors.
Methods
A systematic literature search was conducted within four scientific databases. The search focused on synonyms of 'sleep’ and 'hospitalization’. Papers written in English or Dutch from inception to April 25th,2022 were included for hospitalized patients >1 year of age. Papers exclusively reporting about patients receiving palliative, obstetric or psychiatric care were excluded, as well as patients in rehabilitation and intensive care settings, and long-term hospitalized geriatric patients. This review was performed in accordance with the PRISMA guidelines.
Results
Out of 542 full text studies assessed for eligibility, 203 were included, describing sleep quality and/or quantity of 17,964 patients. The median sample size of the studies was 51 patients (IQR 67, range 6–1472). An exploratory meta-analysis of the Total Sleep Time showed an average of 7.2 h (95%-CI 4.3, 10.2) in hospitalized children, 5.7 h (95%-CI 4.8, 6.7) in adults and 5.8 h (95%-CI 5.3, 6.4) in older patients (>60y). In addition, a meta-analysis of the Wake After Sleep Onset (WASO) showed a combined high average of 1.8 h (95%-CI 0.7, 2.9). Overall sleep quality was poor, also due to nocturnal awakenings. The most frequently cited external factors for poor sleep were noise and number of patients in the room. Among the variety of internal/disease-related factors, pain and anxiety were most frequently mentioned to be associated with poor sleep.
Conclusion
Of all studies, 76% reported poor sleep quality and insufficient sleep duration in hospitalized patients. Children sleep on average 0.7–3.8 h less in the hospital than recommended. Hospitalized adults sleep 1.3–3.2 h less than recommended for healthy people. This underscores the need for interventions to improve sleep during hospitalization to support recovery.
Keywords: Hospitalized patient, Sleep quality, Sleep epidemiology, meta-Analysis
Highlights
-
•
An overview of the magnitude of sleep deprivation in hospitalized patients.
-
•
A meta-analysis of studies reporting on some of the main sleep outcomes.
-
•
An overview of internal and external factors affecting sleep in hospitalized patients.
-
•
Guidance for potential interventions to improve sleep during clinical admission.
-
•
Uncovers a knowledge gap regarding the sleep quality of hospitalized children and daytime sleep of hospitalized adults.
1. Introduction
Sleep is an essential daily requirement for the development and maintenance of physical and psychological health [1]. Among the important functions of sleep are memory processing and consolidation, cellular repair, brain development and hormonal regulation [[2], [3], [4], [5], [6]]. Good sleep quality consists of a sufficient amount of sleep, uninterrupted sleep, age-appropriate naps and a sleep schedule that fits with one's natural biological rhythms [7]. Sleep satisfaction – one's subjective perception of the quality of sleep – is also important, since people with a high sleep satisfaction have a better quality of life [8]. The most common short-term consequences of insufficient sleep are daytime sleepiness, reduced alertness, poor emotion regulation, increased pain perception, memory loss and difficulties with decision-making [[9], [10], [11], [12], [13]]. It is also associated with an increased risk of fall incidents and delirium [14]. Long-term health consequences of sleep disturbances include anxiety, hypertension, cardiovascular disease, weight-related issues, dyslipidemia, and type 2 diabetes mellitus [1,15,16].
Hospitalized patients are at risk for sleep disturbances caused by disease-related factors (e.g. pain, discomfort, co-morbidities, medications), environmental factors (e.g. care-related routines, noise and light), psychological factors (e.g. anxiety or fatigue) and social factors (e.g. changed parenting strategies for hospitalized children, loss of autonomy and familiar bedtime routines) [[17], [18], [19], [20]]. There is evidence that hospitalization is a risk indication for insomnia that may remain for months or years after discharge [21,22]. In addition, sleep deprivation may contribute to impaired recovery, prolonged length of stay, reduced subjective well-being, and poor patient perception of hospitalized care [23]. The growing evidence for the importance of sleep in physical and mental health and recovery, has stimulated research into this topic. However, an overview of all findings is still missing today. Therefore, the aim of this study was to systematically review all studies that describe the quality and quantity of sleep in hospitalized pediatric and adult patients, and to perform meta-analyses where possible.
2. Method
This systematic review was performed according to the Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines [24]. This review has been registered on PROSPERO (international prospective register of systematic reviews), with registration number CRD42022300723. Where possible, a meta-analysis was performed.
2.1. Search strategy
A systematic search was performed on November 2nd, 2021 (by PB and GLB) using the databases MEDLINE (OVID), Embase.com, Clarivate Analytics/Web of Science Core Collection and PsycINFO. An updated search followed on April 25th, 2022. The search included keywords and free text terms for (synonyms of) 'sleep’ combined with (synonyms of) 'hospitalization’. A full overview of the search strategy can be found in the supplementary information of this paper. No limitations on date or language were applied in the search.
2.2. Inclusion/exclusion criteria
The inclusion criteria were: 1) patients of one year and older 2) assessment of sleep and report on at least one sleep outcome variable (see paragraph “main outcomes”) 3) hospitalization for at least one night, and 4) written in Dutch or English. Excluded were studies: 1) related to specific diagnosed sleep conditions, 2) related to specific sleep-inducing medications, 3) conducted in Intensive Care Units, 4) exclusively reporting about patients receiving palliative care, obstetric care, or psychiatric care 5) including solely patients in sleep-laboratories, 6) in rehabilitation settings, 7) containing long-term hospitalized geriatric patients (e.g. patients in nursing homes) 8) were systematic reviews or conference abstracts, 8) or non peer-reviewed studies from Embase or Web of Science.
2.3. Main outcomes
The phenomena of interest before data analysis took place were: total sleep time (TST), sleep duration, time in bed, wake-up time, sleep efficiency (SE), sleep onset latency (SOL), wake after sleep onset (WASO), nighttime awakenings, total daily sleep time, daytime sleep time, Pittsburgh Sleep Quality Index (PSQI) scores, Richards-Campbell Sleep Questionnaire (RCSQ) scores. Sleep outcomes were added when additional relevant outcomes arose from the data during data analysis, and if they were used more often. Table 1 shows an overview of all definitions/explanations, as well as all extra sleep outcomes added in this review. For interventional studies, only data from the control group were used, as the aim of this review is to describe sleep unaffected by interventions.
Table 1.
Definitions or explanations of all sleep parameters used to describe sleep quality. Items in italic style represent sleep outcomes added during data analysis.
| Sleep parameter | Definition/Explanation |
|---|---|
| Total sleep time (TST) | Total minutes of night-time sleep (“Time in bed” minus “wake after sleep onset” minus “sleep onset latency” OR “sleep duration” – “wake after sleep onset”) |
| Sleep duration | Total amount of time between sleep onset and offset (“time in bed” minus “sleep onset latency”) |
| Time in bed | Total number of minutes in bed during the night; The time between Bedtime and wake-up time. |
| Bedtime | Time of going to bed |
| Wake-up time | Time of waking |
| Wake after sleep onset (WASO) | Total number of minutes spent awake after sleep onset during the sleep period at night |
| Sleep efficiency (SE) | Number of minutes of actual sleep (TST) during the night divided by the number of minutes in bed, multiplied by 100 |
| Sleep onset latency (SOL) | Duration between bedtime and sleep onset |
| Nighttime Awakenings | Total number of wake episodes between bedtime and wake time. |
| Total daily sleep time | Total minutes of sleep in a 24h period |
| Daytime Sleep time | Number of minutes sleep during daytime |
| Pittsburgh Sleep Quality Index (PSQI) [229] | 19 self-rated questions (and 5 questions rated by the bed partner or roommate) which assesses sleep behavior from the previous month. PSQI has 7 subcategories, which sums up to a score between 0 and 21: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, daytime dysfunctions, sleep disturbances, sleep medication). A total score ≥ 5 is considered poor quality. |
| Richards-Campbell Sleep Questionnaire (RCSQ) [244] | 5 self-rated questions which assess sleep quality of the previous night, rated on a 100 mm Visual Analogue Scale (VAS). Questions are about awakenings, sleep quality, sleep latency, sleep depth, and returning to sleep. The average of all questions is considered the RCSQ total score. A total score ≤ 50 is considered poor sleep quality. |
| Verran Snyder-Halpern Sleep scale (VSH) [247] | Originally an 8-item VAS tool to capture sleep latency, fragmentation, length and depth, but often the extended 15-item version is used which sums scores to calculate sleep quality in three domains: sleep effectiveness (5 questions, sums up to scores between 0 and 500), sleep disturbance (7 questions, sums up to scores between 0 and 700) and supplemental sleep (4 questions, sums up to scores between 0 and 400). For disturbance and supplementation, higher scores indicate worse sleep quality, whereas for effectiveness, higher scores indicate better sleep quality. |
| Insomnia Severity Index (ISI) [248] | 7 self-rated questions, using a 5-point Likert scale, to assess the severity of sleep-onset, sleep-maintenance, and early awakenings, as well as the satisfaction with current sleep patterns, interference with daytime functioning, noticeability of impairment to others and level of distress. Assesses the last 2 weeks. Total scores range from 0 to 28, with scores of 0–7, 8–14, 15–21 and 22–28 deemed indicative of no clinically significant insomnia, subthreshold insomnia, moderate insomnia and severe insomnia, respectively. |
| Epworth Sleepiness Scale (ESS) [249] | 8 self-report items to evaluate the general sleepiness state within a day, using a 4-point Likert type scale. Total scores range from 0 to 24, where 0–5 indicates enough sleep, 6–10 indicates slight drowsiness, 11–15 indicates average drowsiness and >15 indicates severe drowsiness. |
| St. Mary Hospital Sleep Questionnaire [250] | 11 self-reported items to assess sleep pattern disorders, using a 3-point Likert type scale. Total scores range from 11 to 44, where scores of 11–21 indicate slight sleep disorders, 22–32 indicate average disorders and 33–44 indicate severe sleep disorders. |
| PROMIS Sleep disturbance [251] | 8- or 4-items questionnaire to assess sleep quality of the previous night, rated on a five-point scale. A standardized T-score can be calculated from the total score, to allow for comparison to a reference population. A patient with a T-score of 60 has a sleep quality that is worse than approximately 84% of persons in the reference population. |
| Karolinska Sleepiness scale [252] | Nine-point Likert scale assessing the patient's subjective sleepiness over the past 10 min, ranging from 1 = very alert to 9 = very sleepy. |
2.4. Meta-analysis
Performing a meta-analysis on all data was not feasible, due to the heterogeneity of the data and the different ways of annotating results. A series of random effects exploratory meta-analyses was conducted on the PSQI Total score (45 out of 65 possible papers were included), RCSQ Total Score (18 out of 24), TST (42 out of 60), sleep duration (18 out of 29), SE (37 out of 54) and WASO (17 out of 22) [25]. Only studies reporting means with standard deviations were included in the meta-analysis; as a result, median (IQR) were excluded (since normal distribution of the data could not be guaranteed). The tables containing data of all studies (medians (IQR), means (SD) etc.) are published separately [26]. Out of 203 included studies, 110 studies were included in one or more of the meta-analyses. A wide variety of outcome measures have been used in the different articles. To improve readability, only the most frequently reported outcomes are shown in the figures of this manuscript. The results of all papers including those that used less common outcome measures can be found in the separately published dataset.
The I2 index was used to measure the potential heterogeneity present between the point estimates. I2 is a ratio of variation among point estimates, and its values lie on a scale from 0 to 100. Large I2 values suggest that the point estimates are not drawn from the same population.
2.5. Study selection and data extraction
Following the initial database search a total of 12,861 papers were identified after deduplication. All titles and abstracts were screened independently for eligibility by two researchers (PB and EE). In case of disagreement, consensus was obtained by involving a third team member. After identifying all eligible papers, one reviewer (PB or EE) collected all the data using a structured form, while a second reviewer (PB, EE or WL) assured quality by validating the extracted data. Disagreements were resolved through discussion.
2.6. Quality assessment
A quality assessment was independently performed by two researchers (PB, EE, WL) on all included papers using the Study Quality Assessment Tool created by NHLBI for Controlled Trials and observational studies [27]. Each paper was assessed using the standardized criteria. Each criterion was rated yes, no, not reported or not applicable. A total score was determined by evaluating the number of positive ratings out of applicable criteria. A paper with a score above 65% was considered of ‘good quality’, studies with a score between 35% and 65% were considered of ‘fair’ quality and studies with a score below 35% were considered ‘poor’ quality. The quality assessment has been used primarily to determine if studies included are consistent with the standard quality appraisal. Yet, no papers were excluded based upon this assessment.
3. Results
3.1. Selection and quality assessment
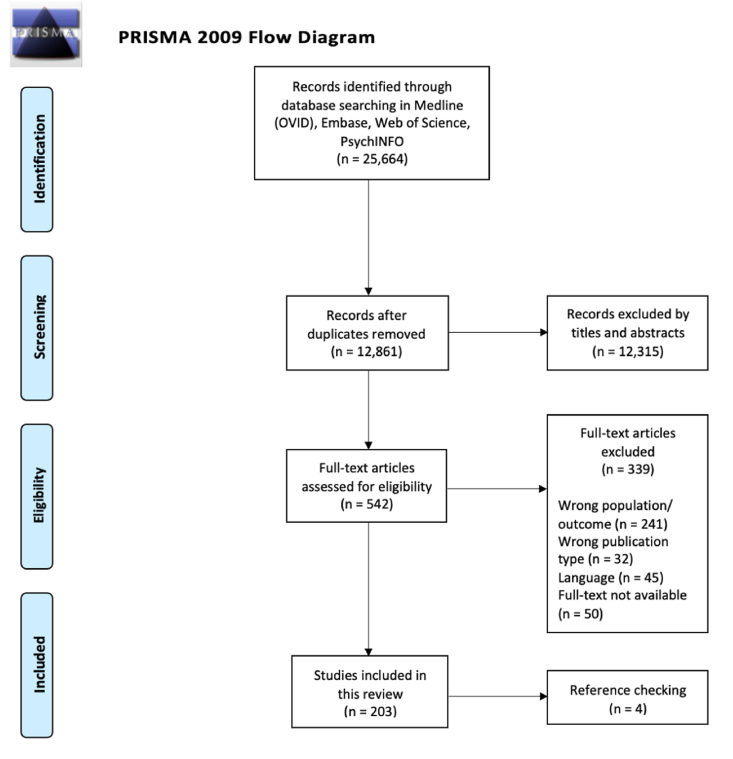
In Fig. 1, a PRISMA flow chart describes the selection of studies. Out of 542 potentially eligible studies, 202 were included. A total of 17,964 patients were described in these studies. The median sample size was 51 patients (IQR 67, range 6–1472). Eighty-four studies were of good quality [[28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104], [105], [106], [107], [108], [109], [110]], 100 studies were considered to be of fair quality [[111], [112], [113], [114], [115], [116], [117], [118], [119], [120], [121], [122], [123], [124], [125], [126], [127], [128], [129], [130], [131], [132], [133], [134], [135], [136], [137], [138], [139], [140], [141], [142], [143], [144], [145], [146], [147], [148], [149], [150], [151], [152], [153], [154], [155], [156], [157], [158], [159], [160], [161], [162], [163], [164], [165], [166], [167], [168], [169], [170], [171], [172], [173], [174], [175], [176], [177], [178], [179], [180], [181], [182], [183], [184], [185], [186], [187], [188], [189], [190], [191], [192], [193], [194], [195], [196], [197], [198], [199], [200], [201], [202], [203], [204], [205], [206], [207], [208], [209], [210], [211]], and 18 of poor quality [13,[212], [213], [214], [215], [216], [217], [218], [219], [220], [221], [222], [223], [224], [225], [226], [227], [228]]. A variety of tools have been used to assess sleep, which are displayed in Table 2. Among the included studies 30 studies were conducted on children, and the remaining on adults/elderly. Ninety papers included patients admitted to a medical ward, 56 to a chirurgical 39 to an oncology, 28 to a cardiology, 11 to a neurology, 2 to a geriatric ward and 4 to an emergency department. Also, 143 studies were observational, whereas 65 were interventional studies.
Fig. 1.
PRISMA flow diagram of study selection.
Table 2.
Ways of assessing sleep in hospitalized patients including the number of papers using the assessment.
| Type of measurements | Type of assessment |
|---|---|
| Objective measurements | Wrist actigraphy (50 studies) [30,32,35,[37], [38], [39], [40],43,[49], [50], [51], [52], [53],55,57,60,65,66,70,72,[74], [75], [76],82,83,97,101,105,106,110,[114], [115], [116],127,144,145,149,[151], [152], [153],157,161,162,166,172,174,175,183,188,191,253,254], video recordings (1 study) [126], polysomnography (10 studies) [45,56,67,115,125,131,132,143,169,176], silent observations with a 5 or 10-min interval (3 studies) [138,223,255], sleep diaries (34 studies) [13,36,38,43,47,49,50,54,55,57,65,66,70,72,74,79,80,84,98,101,105,121,127,133,136,151,[162], [163], [164],166,175,183,191,253], activity sensors (2 studies) [128,133], Fitbit (2 studies) [31,141], hourly patient sleep log [123], vitalog [147] |
| Subjective measurements | Interviews (6 studies) [20,113,163,213,256,257], numeric rating scales (3 studies) [58,59,258], |
| Sleep in a Children's Hospital Survey (4 studies) [29,66,77,127], Children's Sleep Habit Questionnaire (CSHQ) (4 studies) [20,66,74,77], Patient Sleep Questionnaire + Brief Infant Sleep Questionnaire (1 study) [42], Spence Children's Anxiety Scale and Post-Hospital Behavior Questionnaire (1 study) [66], Potential Hospital Sleep Disruption and Noises Questionnaire [259], Pediatric Sleep Questionnaire [133], Pediatric Quality of Life Inventory [254], Selfmade/unpublished/unvalidated (22 studies) [28,54,66,69,113,117,122,125,137,156,171,177,178,180,204,212,214,216,223,224,260,261], Verran and Snyder-Halpern (VSH) (13 studies) [44,46,75,92,120,142,144,162,170,176,204,211,215], Insomnia Severity Index (ISI) (5 studies) [34,71,109,118,139], Epworth Sleepiness scale (ESS) (9 studies) [85,104,134,136,139,145,166,183,219], PROMIS Sleep disturbance (6 studies) [78,80,89,104,134,160], Sint Mary Hospital Sleep Questionnaire (SMHSQ) (9 studies) [64,91,102,124,190,197,199,219,262], Karolinska sleepiness scale (7 studies) [30,36,60,101,110,183,188], Karolinska Sleep Quality Log (3 studies) [30,110,166], Visual Analogue scale (13 studies) [13,36,58,59,122,132,161,180,183,207,210,216,222], Pittsburgh Sleep Quality Index (PSQI) scores (65 studies) [[33], [34], [35],41,60,61,67,68,73,76,82,[84], [85], [86],88,90,95,[98], [99], [100],103,112,119,121,129,130,139,140,145,146,148,154,158,163,165,168,173,[181], [182], [183], [184], [185], [186], [187], [188], [189],[193], [194], [195],202,203,205,206,208,217,223,[225], [226], [227], [228],[263], [264], [265]], Richards-Campbell Sleep Questionnaire (RCSQ) scores (26 studies) [31,[62], [63], [64],79,82,87,93,94,96,107,108,128,135,149,150,153,155,159,192,198,200,201,207,209,220,221], Quality of Life Questionnaire – Core 30 [53], Edmonton Symptom Assessment Scale [222], Leeds Sleep Evaluation questionnaire [158] |
3.2. Sleep quantity
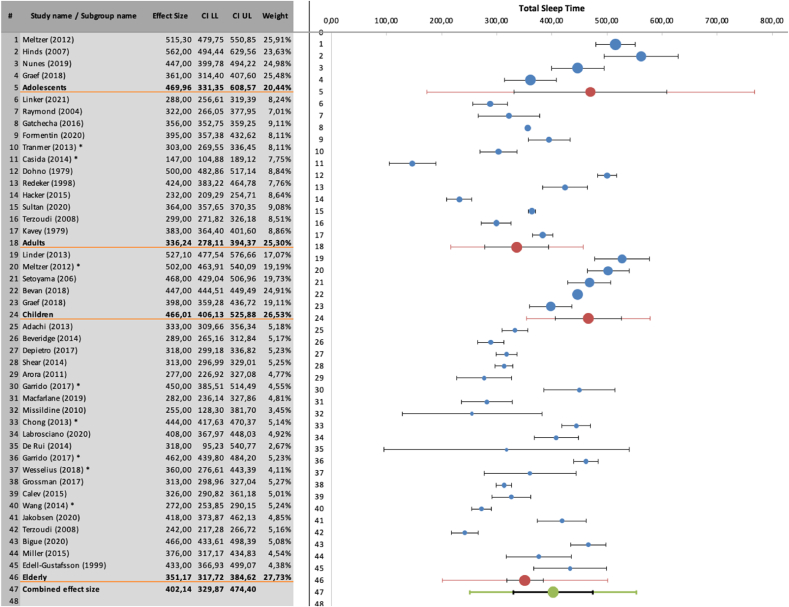
A combination of different quantitative sleep variables enables a comprehensive description of sleep. Most studies (76%, 80/106) reported that sleep duration was shorter during hospitalization [13,29,30,[32], [33], [34],[37], [38], [39], [40],[42], [43], [44], [45],[49], [50], [51], [52], [53], [54], [55], [56], [57],60,63,[65], [66], [67],70,72,[76], [77], [78], [79], [80],82,83,97,98,101,102,105, 110,111,[113], [114], [115],117,[122], [123], [124], [125], [126], [127], 131,133,134,136,138,141,[143], [144], [145],147,149,[151], [152], [153],156,157,[161], [162], [163], [164],166,[168], [169], [170], [171], [172],174,175,177, 183,188,191,208,212,221,223,224], as compared to National Sleep Foundation (NSF) recommendations. A subgroup meta-analysis of the TST showed an average sleep of 7.8 h (95%-CI 6.8, 8.8) in hospitalized children, 7.8h (95%-CI 6.0, 10.1) in adolescents, 5.6h (95%-CI 4.6, 6.5) in adults and 5.9 h (95%-CI 5.2, 6.4) in elderly patients (>60y), see Fig. 2. The total sample included 2539 observations; the main analysis of TST indicated a significant amount of heterogeneity (τ2 = 47,001), most of which was true heterogeneity, not sampling error (I2 = 99%). Twenty out of 22 studies (90%) comparing TST or sleep duration during hospitalization with sleep at home, age-specific norms or healthy volunteers reported TST/sleep duration to be significantly lower during hospitalization [29,30,38,44,54,67,72,80,105,111,113,114,117,120,127,133,134,156,174,213,216]. Similarly, a meta-analysis in patients >18y showed an average sleep duration of 6.6h (95%-CI 6.4, 6.9), see supplement.
Fig. 2.
Subgroup meta-analysis for Total sleep time (children, adolescents, adults, elderly), shown in minutes. Recommended sleep duration in children (6-12y) is between 540 and 660 min, in adolescents (13-18y) 480 and 600 min, in adults (18-60y) 420 and 540 min..
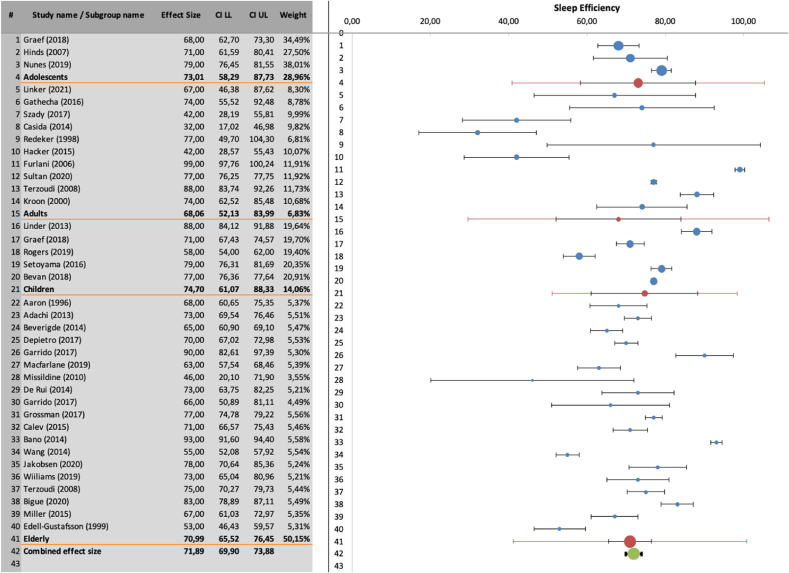
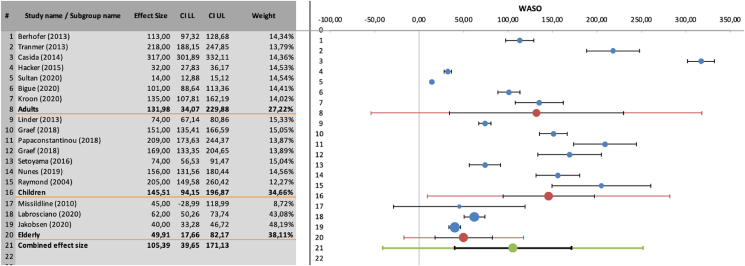
SE was also reported to be lower in-hospital compared to home [38,72,111,114]. The meta-analysis showed an average of 71.9% (95%-CI 66.9, 73.9), with no differences between hospitalized children, adolescents, adults, and older adults (>60y) (Fig. 3). The main analysis of SE indicated a significant amount of heterogeneity (τ2 = 105), most of which was true heterogeneity, not sampling error (I2 = 98%). Compared to home, more awakenings [29,67,80,113,116,117,127,216], longer sleep onset latency (SOL) [47,72,81,113,173] and longer WASO have been reported [67]. A meta-analysis of the WASO showed an average of 105 min (95%-CI 39, 171), again with a significant amount of heterogeneity (Fig. 4). Studies using wrist actigraphy or polysomnography, reported up to averages of 41 awakenings per night [35,45,51,55,60,66,70,72,75,77,83,105,115,124,125,127,141,143,145,152,153,161,162,172,183]. Findings about bedtime and wake up time in hospital are inconclusive; while some studies report earlier bedtimes and wakeup times compared to home [47,72,113], others report delayed ones [29,105,117]. Only 12 studies assessed daytime sleep duration [32,47,51,65,66,72,78,97,113,131,161,214]. Half of which assessed children <18 years old. Mean total daytime sleep duration in children ranged from 39 to 221 min. Studies in adults reported mean daytime sleep duration between 55 and 90 min.
Fig. 3.
Subgroup meta-analysis for Sleep efficiency (children, adolescents, adults, elderly), shown in percentages.
Fig. 4.
Meta-analysis of Wake after sleep onset, shown in minutes.
Some studies have reported that sleep gradually improves over the course of hospitalization hospital length of stay [47,53,61,62,68,132,135,140,143,151,166,173], while others did not find any significant improvement over time [40,41,45,64,65,80,89,128,129,147,175,215].
3.3. Sleep quality
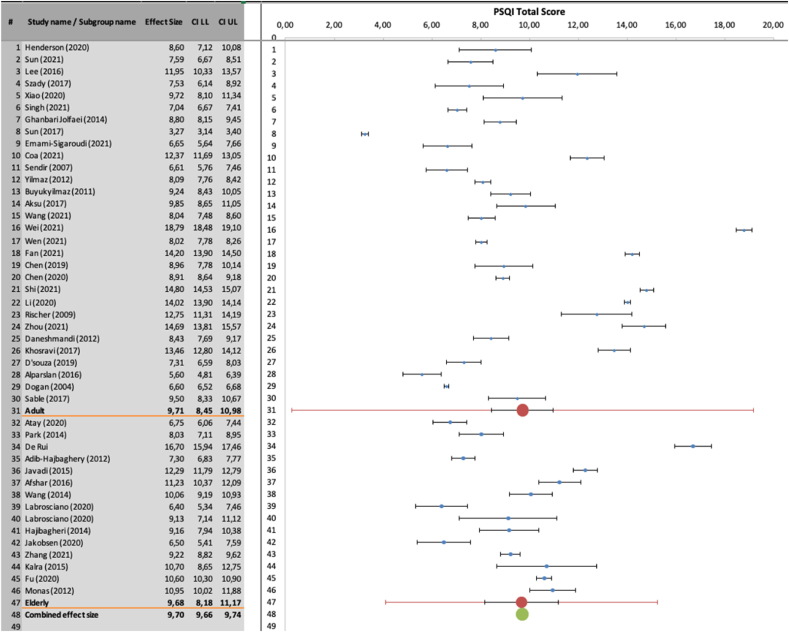
An overview and explanation of all sleep questionnaires used is presented in Table 1, Table 2. All but one (60/61) studies reporting on total PSQI showed a total score greater than 5, which distinguishes good sleepers from bad sleepers, with higher scores indicating worse sleep [229]. Scores ranged from 3.27 to 18.79 [33,34,41,61,73,[84], [85], [86],88,90,95,[98], [99], [100],103,112,119,129,130,139,140,145,146,148, 154,158,163,165,168,173,181,[183], [184], [185], [186], [187], [188], [189],[193], [194], [195], 202,203,205,206,208,217,[225], [226], [227], [228]]. A meta-analysis of the PSQI total score showed a mean of 9.70 (95%-CI 9.66, 9.74), with no difference between younger adults (18-60y) and older adults (Fig. 5). Subgroup analysis showed that oncology patients had the worst PSQI total scores (12.80 (95%-CI 10.08, 15.52)), compared to mean scores of 10.00 (95%-CI 8.36, 11.64), 8.44 (95%-CI 6.74, 10.14) and 8.42 (95%-CI 8.42, 10.10) in cardiology, medical and surgical patients, respectively. The main analysis of PSQI Total score indicated a significant amount of heterogeneity (τ2 = 19), most of which was true heterogeneity, not sampling error (I2 = 99%). From the seven available subscores, sleep duration and sleep latency were the biggest contributers to the total score.
Fig. 5.
Subgroup meta-analysis of Pittsburgh Sleep Questionnaire Index (adults, elderly). Total score between 0 and 21, with a score ≥ 5 considered to be poor quality.
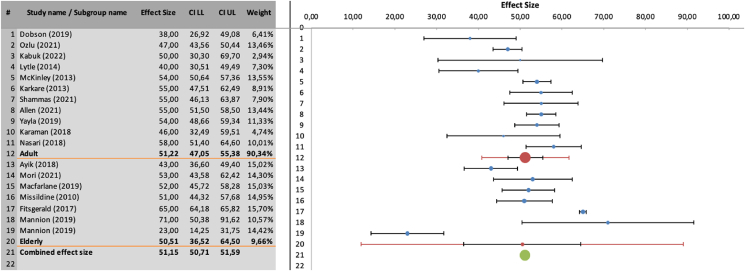
RCSQ scores revealed a similar trend, where all but one (25/26 studies) showed average total scores below 70, indicating poor sleep [31,[62], [63], [64],79,87,93,94,96,107,108,128,135,149,150,153,155,159,192,198,200,201,209,220]. A meta-analysis of the RSCQ total score revealed a mean of 50.4 (95%-CI 45.4, 55.5), with no difference between younger and older adults (Fig. 6). Studies using the Verran and Snyder-Halpern Sleep Scale (VSH) also showed low levels of sleep quality [44,46,142,162,176,204,211,215]. Compared to US non-hospitalized adults [46], inpatients seem to have worse scores in all scales.
Fig. 6.
Subgroup analysis of Richard-Campbell Sleep Questionnaire (adults, elderly). Total score ranging from 0 to 100 with a score ≤ 50 considered to be poor sleep quality.
3.4. Associations/correlations with sleep
Many associations and/or correlations with (poor) sleep have been described (Fig. 7). Two of the most frequently cited external factors are noise [29,52,61,71,73,74,77,106,111,112,122,139,146,155,158,164,174,180,214,215,218] and the number of patients in the room [38,[43], [44], [45],55,62,71,73,74,140,180]. A variety of internal/disease-related factors have been reported to be associated with poor sleep as well, with pain [13,28,29,52,53,58,68,73,106,112,119,122,134,139,140,151,161,165,168,170,180,201,215], and anxiety/fear [62,64,71,72,77,86,113,135,146,180,215,230] being most frequently reported to be associated with poor sleep quality. Please see the supplemental information for an overview of all associations found, which also includes studies that did not find correlations.
Fig. 7.
Overview of items associated with inpatient sleep, where dotted lines are positive correlations. The bigger the balloon, the more frequently the association has been reported.
4. Discussion
To the best of our knowledge, this systematic review with meta-analysis is the most extensive and complete overview of sleep measurements in normal care inpatients to date. It provides an overview of the magnitude and causes of the sleep problems in the hospital population for various medical specialties and age groups. In addition, it provides a clear picture of the current state of literature, the knowledge gaps and challenges for future sleep research in the hospital setting.
Overall, this review provides solid evidence that patient's sleep is impacted negatively during hospitalization. Of all included studies that report on sleep duration/TST, 76% (80/106) found a sleep quantity less than the recommended average for healthy people by the National Sleep Foundation (NSF) [231]. Of these, 37 studies (46%) reported adults sleeping even less than 6 h, which is considered unhealthy sleep as per NSF recommendations. To specify, meta-analysis showed a large sleep deficit of 0.7–3.8 h in hospitalized children and 1.3–3.2 h in adult inpatients. In addition, patients experience many (up to 42 per night) nocturnal awakenings and a high average WASO of 122 min, often caused by external and potentially avoidable sleep disturbances. The high WASO could account for a low SE. Yet the average SE in hospitalized children (71%–91%) was comparable to SE in healthy populations (76%–82%) [232].
Impaired sleep during admission probably results from factors related to hospitalization, e.g. environmental, disease or treatment-related factors. However, studies also suggest that suboptimal sleep during hospitalization is associated with poor sleeping prior to admission [44,47,54,223]. This indicates that poorer sleep during hospitalization might partly result from overall bad sleep hygiene or from imminent disease or underlying (chronic) condition. It underlines the importance of the use of control data in future research (e.g. include questions about sleep prior to hospitalization/onset of disease). Many sleep disrupters in the hospital seem to be related to external factors, with noise being the most frequently reported cause. Also, sleep in hospitalized patients may be substantially affected by (nocturnal) care related, but potentially redundant, interventions (e.g. vital signs check-ups). Hospitals are therefore advised to take a critical look at the design of both the care processes and in-patient ward structure. Optimizing individualized patient care could play a key role in optimizing patients' sleep; is bad sleep due to a room close to the nurse desk or does a patient share a room with a restless fellow patient? Are the nightly checkups necessary for this specific patient? Can vital check-ups, iv fluid changes and medication rounds be postponed to the day shift instead of the night shift? Or can vital signs be monitored remotely (and automatically with silent alarms) limiting the need of interventions in the room? Etc. Sleep disturbances are also related to emotions like depression and anxiety. While it will be difficult to completely rule out such feelings, it could help when healthcare professionals pay attention to both the medical as well as the psychological state of their patients during hospital stay.
More research is warranted to understand the exact influence of hospital setting, healthcare professionals' behavior and disease on patient's sleep. In addition to the need for extra research, healthcare professionals can already play a key role in sleep promotion with relatively simple and cheap interventions. Previous research highlighted the lack of awareness among healthcare professionals of the importance of sleep for general health and physical recovery, however [233]. Therefore, education for health care professionals about the importance of sleep and factors affecting patient's sleep quality for (better recovery to) optimal health seems important.
Studies investigating sleep of hospitalized children are sparse; only 30 out of the 205 included studies investigated the sleep of hospitalized children. Some of these studies did not find a difference in total sleep time among various ages, which could suggest that sleep of younger children is more affected in the hospital compared to older children. On the other hand, many studies did not stratify for age which hampers to infer robust conclusions. Not only sleep duration is decreasing over the years [234,235], a recent study among healthy subjects also showed a shorter SOL, a decreased WASO, and (hence) an increased SE in older children compared to young ones [232]. It is therefore recommended that future research should stratify for age (e.g. toddlers, school aged children and adolescents).
Sleep measurements varied among the studies, hampering firm conclusions on sleep during hospitalization. Using wrist actigraphy only, has its limitations since it is accurate in estimating wake and sleep patterns, but is limited in its ability to measure sleep latency, and therefore may overestimate sleep efficiency [236]. In addition, actigraphy only measures sleep quantity, and therefore does not tell anything about (subjective) sleep quality. Furthermore, standardized sleep actigraphy requires a minimum of five days to gather reliable data [237], while patients in acute care settings are often admitted for shorter time periods. Other studies used (only) sleep diaries which are found to be an accurate way of measuring total time in bed and SOL. However, patients (and parents rooming in) are less accurate in assessing TST and number of nocturnal awakenings [238]. Therefore, it is recommended to combine wrist actigraphy with sleep diaries. Only 12 studies assessed daytime sleep time using actigraphy and diaries. Subjective daytime sleep time was also assessed as a sub score in the St Mary's Hospital Sleep questionnaire (8 studies), and 12 studies appraised daytime sleepiness (using the Epworth Sleepiness Scale [ESS] or Karolinska Sleepiness Scale [KSS]). It is plausible that bedridden sick patients spent many hours sleeping during the day. Physical inactivity and daytime naps potentially negatively influence sleep pressure and sleep quality at night [64]. In addition, taking a nap is (often) part of young children's normal sleep-rhythm. It is therefore worth considering measuring 24-h sleep in inpatients, rather than focusing solely on nighttime sleep. Therefore, future research could focus on a reliable way to measure daytime sleep in bedridden hospitalized patients. Is actigraphy specific enough, are sleep diaries reliable for afternoon naps and is the ESS reliable in sick patients?
Moreover, even when sleep quantity is considered adequate, sleep quality can still be impaired. Some studies even conclude that sleep quality is superior to quantity regarding prevention of sleep-related negative health outcomes [239]. Therefore, it is essential to combine subjective (sleep questionnaires) and objective sleep measures (like wrist actigraphy and sleep diaries) for a comprehensive overview of all aspects of sleep. While many papers investigating inpatient sleep in adult populations include both objective as well as subjective measures for sleep behavior, most sleep research in hospitalized children does not [[240], [241], [242]].
Although subjective sleep quality is often assessed in the adult population, due to the many different questionnaires that have been used, it is difficult to compare results. Apparently, there is no consensus on which questionnaire is best to assess sleep quality of hospitalized patients. The most frequently used questionnaire is the PSQI [229]. The PSQI assesses sleep behavior from the previous month, and it has been validated in many populations, both healthy as well as with/during diseases [243]. The median length of stay in inpatients in an hospital is two to three days, resulting in the need to adapt the PSQI to match the timelines in hospital. In addition, the 5 questions rated by the bedpartner/roommate have often been omitted when assessing inpatient sleep. Making changes into validated questionnaires not only affects the validity of the tool, but it also makes it difficult to compare results. Another questionnaire commonly used to assess sleep quality is the RCSQ [244]. It takes approximately 2 min to complete, and it has been largely used in critical care settings. It is one of the few questionnaires that assess last-night sleep and can be used in the hospital setting without textual adjustments. The Verran Snyder-Halpern Sleep scale is another frequently used tool, but originally validated to measure sleep in healthy adults. As shown in Table 2, other questionnaires have been used as well to evaluate sleep quality. It goes beyond the scope of this paper to discuss all in detail. Above illustrates however, the need for the development/validation of questionnaires that fit the hospital setting, i.e. that are easy to use (especially for children, older or seriously ill patients), evaluate the intended sleep period (e.g. one night instead of a week or month) and that is validated for the population that is to be investigated. Reaching consensus on which questionnaire is best to use, would better allow inter-study comparison of results.
This review showed that the studies assessing the sleep of hospitalized patients often consist of small sample sizes, use modified or non-validated questionnaires, or suffer from overall poor quality. However, this is mostly an expression of the complexity of doing research in this field. As stated earlier, there is a need for validated questionnaires that fit the hospital setting. In addition, quality assessment tools often require studies to assess patients for consecutive nights, which may not be desirable because short stay patients will be missed. Nevertheless, in some respects, the reporting of much sleep research is indeed deficient, such as the reporting of a sample size justification and the duration of daytime sleep. The development of symptoms over time substantially affects sleep. Often sleep increases with an increasing length of stay, as symptoms disappear with adequate treatment and patients get used to the hospital environment [62,68,165]. Yet, studies rarely report how many nights patients had spent in the hospital at the time of assessment. Also, information about the many potential confounders (e.g. use of sleep medication) and about pre-existing sleep disorders is often missing. These are crucial for interpreting the results.
The strength of this review is its comprehensiveness. It includes 203 articles, whereas previously published reviews often include no more than 50 due to restriction in study type or specific patient group [245]. A recently published scoping review on the sleep of hospitalized children focused only on sleep duration [246]. Therefore, we feel that this is the first review that provides a complete overview of all existing sleep parameters – both qualitative (subjective) as well as quantitative. However, this review also comes with some limitations. First, it was limited by the overall quality and heterogeneity of the included studies., Yet as nearly all studies conclude that patients suffer from poor sleep quality and quantity during hospitalization, this appears a message to be taken seriously. Secondly, the language was restricted to English and Dutch. Thirdly, we included an overview of sleep promoting and disturbing factors, showing the frequency with which certain associations have been reported in the literature. However, the frequency of reporting does not necessarily say something about the impact of the association. Fourth, our study does not include the full range of hospitalized patients. For instance, patients admitted to the ICU have been excluded, since several recent reviews on this subpopulation have been published and sleep in the often heavily sedated ICU population cannot be compared with that of non-ICU patients. .In addition, infants have been excluded as well, since – at that age – children still have an unstable circadian rhythm.
5. Conclusion
Sleep quantity and quality are insufficient in hospitalized patients. Sleep duration was 1–4 h shortened in hospitalized patients compared to home. Moreover, almost all studies reported poor sleep quality. Understanding determinants, including patient factors (e.g., disease related factors and psychological factors), sociocultural and environmental factors, associated with quality of sleep in hospitalized patients is mandatory. Subsequently interventions may be devised and assessed, aiming to optimize sleep quality to enhance recovery from conditions that require clinical admission.
Funding
None.
CRediT authorship contribution statement
Pia Burger: Conceptualization, Methodology, Formal analysis, Investigation, Writing – original draft, Visualization, Data curation, Project administration, Validation. Eva S. Van den Ende: Methodology, Data curation, Investigation, Formal analysis, Writing – review & editing, Validation, Visualization. Wen Lukman: Investigation, Data curation, Validation, Writing – review & editing. George L. Burchell: Investigation, Writing – review & editing. Lindsay M.H. Steur: Writing – review & editing. Hanneke Merten: Writing – review & editing. Prabath W.B. Nanayakkara: Writing – review & editing. Reinoud J.B.J. Gemke: Conceptualization, Writing – review & editing, Validation, Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sleepx.2022.100059.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Alvarez G.G., An T. The impact of daily sleep duration on health: a review of the literature. Prog Cardiovasc Nurs. 2004;19:56–59. doi: 10.1111/j.0889-7204.2004.02422.x. [DOI] [PubMed] [Google Scholar]
- 2.Leproult R., Van Couter E. Role of sleep and sleep loss in hormonal release and metabolism. Endocr Dev. 2010;17:11–21. doi: 10.1159/000262524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kopasz M., Loessl B., Hornyak M. Sleep and memory in healthy children and adolescents - a critical review. Sleep Med Rev. 2010;14:167–177. doi: 10.1016/j.smrv.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 4.Tononi G., Cirelli C. Sleep function and synaptic homeostasis. Sleep Med Rev. 2006;10(1):49–62. doi: 10.1016/j.smrv.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 5.Dinges D.F. The state of sleep deprivation: from functional biology to functional consequences. Sleep Med Rev. 2006;10(5):303–305. doi: 10.1016/j.smrv.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 6.Stickgold R., Walker M.P. Sleep-dependent memory consolidation and reconsolidating. Sleep Med. 2007;8(4):331–343. doi: 10.1016/j.sleep.2007.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Breus M. Good, sound sleep for your child. https://www.webmd.com/children/features/good-sound-sleep-for-children#1 [Available from:
- 8.Blackwell C.A.-O., Hartstein L.E., Elliott A.J., Forrest C.B., Ganiban J., Hunt K.J., et al. How sleep quality influences children's life satisfaction. 2020. Better sleep, better life? pp. 1573–2649. [Electronic))] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sadeh A. Consequences of sleep loss or sleep disruption in children. Sleep Medicine Clinics. 2007;2(3):513–520. [Google Scholar]
- 10.Aydin A., Selvi Y., Fau - Besiroglu L., Besiroglu L., Fau - Boysan M., Boysan M., Fau - Atli A., Atli A Fau - Ozdemir O., Ozdemir O Fau - Kilic S., et al. 2013. Mood and metabolic consequences of sleep deprivation as a potential endophenotype' in bipolar disorder; pp. 1573–2517. (Electronic)) [DOI] [PubMed] [Google Scholar]
- 11.Patrick Y., Lee A., Raha O., Pillai K., Gupta S., Sethi S., et al. 2017. Effects of sleep deprivation on cognitive and physical performance in university students; pp. 1446–9235. (Print)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cullen T.A.-O., Thomas G.A.-O., Wadley A.A.-O., Myers T.A.-O. 2019. The effects of a single night of complete and partial sleep deprivation on physical and cognitive performance: a Bayesian analysis. 1466-447X (Electronic)) [DOI] [PubMed] [Google Scholar]
- 13.Raymond I., Nielsen T.A., Lavigne G., Manzini C., Choinière M. Quality of sleep and its daily relationship to pain intensity in hospitalized adult burn patients. Pain. 2001;92(3):381–388. doi: 10.1016/S0304-3959(01)00282-2. [DOI] [PubMed] [Google Scholar]
- 14.Wu L., Sun D. 2017. Sleep duration and falls: a systemic review and meta-analysis of observational studies; pp. 1365–2869. (Electronic)) [DOI] [PubMed] [Google Scholar]
- 15.Medic G., Wille M., Hemels M.E. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep. 2017;9:151–161. doi: 10.2147/NSS.S134864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chorney D.B., Detweiler M.F., Morris T.L., Kuhn B.R. The interplay of sleep disturbance, anxiety and depression in children. J. Paediatr. Psychol. 2008;33(4):339–348. doi: 10.1093/jpepsy/jsm105. [DOI] [PubMed] [Google Scholar]
- 17.Webster R., Thomson D.R. Sleep in hospital. J Adv Nurs. 1986;11:447–457. doi: 10.1111/j.1365-2648.1986.tb01272.x. [DOI] [PubMed] [Google Scholar]
- 18.Morawska A., Calam R., Fraser J. Parenting interventions for childhood chronic illness: a review and recommendations for intervention design and delivery. J Child Health Care. 2014;19(1):5–17. doi: 10.1177/1367493513496664. [DOI] [PubMed] [Google Scholar]
- 19.Oliveira L., Gomes C., Bacelar Nicolau L., Ferreira L., Ferreira R. Environment in pediatric wards: light, sound, and temperature. Sleep Med. 2015;16(9):1041–1048. doi: 10.1016/j.sleep.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 20.Stickland A., Clayton E., Sankey R., Hill C.M. A qualitative study of sleep quality in children and their resident parents when in hospital. Arch Dis Child. 2016;101(6):546–551. doi: 10.1136/archdischild-2015-309458. [DOI] [PubMed] [Google Scholar]
- 21.Griffiths M.F., Peerson A. 2005. Risk factors for chronic insomnia following hospitalization. (0309-2402 (Print)) [DOI] [PubMed] [Google Scholar]
- 22.Smith M.T., Klick B., Kozachik S., Edwards R.E., Holavanahalli R., Wiechman S., et al. Sleep onset insomnia symptoms during hospitalization for major burn injury predict chronic pain. Pain. 2008;138(3):497–506. doi: 10.1016/j.pain.2008.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morse A.M., Bender E. 2019. Sleep in hospitalized patients; pp. 2624–5175. (Electronic)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.PRISMA 2009. http://prisma-statement.org/PRISMAStatement/ [Checklist and Flow Diagram]. Available from:
- 25.Suurmond RA-O, van Rhee HA-O, Hak TA-O. Introduction, comparison, and validation of Meta-Essentials: a free and simple tool for meta-analysis. (1759-2887 (Electronic)). [DOI] [PMC free article] [PubMed]
- 26.Burger P., Van den Ende E., Lukman W., Burchell G.L., Steur L.M.H., Merten H., et al. Sleep in hospitalized pediatric and adult patients – data from a systematic review. Mendeley Data, V1. 2022 doi: 10.17632/xtvpxg4m8c.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.NLHBI https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools Study quality assessment tools]. Available from:
- 28.Accardi-Ravid M.C., Dyer J.R., Sharar S.R., Wiechman S., Jensen M.P., Hoffman H.G., et al. The nature of trauma pain and its association with catastrophizing and sleep. Int J Behav Med. 2018;25(6):698–705. doi: 10.1007/s12529-018-9751-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meltzer L.J., Davis K.F., Mindell J.A. Patient and parent sleep in a children's hospital. Pediatr Nurs. 2012;38(2):64–71. ; quiz 2. [PubMed] [Google Scholar]
- 30.Adachi M., Staisiunas P.G., Knutson K.L., Beveridge C., Meltzer D.O., Arora V.M. Perceived control and sleep in hospitalized older adults: a sound hypothesis? J Hosp Med. 2013;8(4):184–190. doi: 10.1002/jhm.2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Allen R.W., Burney C.P., Davis A., Henkin J., Kelly J., Judd B.G., et al. Deep sleep and beeps: sleep quality improvement Project in general surgery patients. J Am Coll Surg. 2021;232(6):882–888. doi: 10.1016/j.jamcollsurg.2021.02.010. [DOI] [PubMed] [Google Scholar]
- 32.Amofah H.A., Brostrom A., Fridlund B., Bjorvatn B., Haaverstad R., Hufthammer K.O., et al. Sleep in octogenarians during the postoperative phase after transcatheter or surgical aortic valve replacement. Eur J Cardiovasc Nurs : J. Work. Group on Cardiovasc. Nursing of the Europ. Soc. Cardiol. 2016;15(2):168–177. doi: 10.1177/1474515115620992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Atay S., Sayilan A.A. Pre-transurethral prostate resection anxiety on postoperative pain and sleep quality: a correlational study. Int. J. urol. nurs. 2021;15(2):70–76. [Google Scholar]
- 34.Azizoglu Sen I., Ozsurekci C., Balci C., Caliskan H., Esme M., Unsal P., et al. Sleep quality and sleep-disturbing factors of geriatric inpatients. Europ geriatr med. 2021;12(1):133–141. doi: 10.1007/s41999-020-00400-4. [DOI] [PubMed] [Google Scholar]
- 35.Bakken L.N., Lee K.A., Kim H.S., Finset A., Lerdal A. Sleep-wake patterns during the acute phase after first-ever stroke. Stroke Res Treat. 2011;2011 doi: 10.4061/2011/936298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bano M., Chiaromanni F., Corrias M., Turco M., De Rui M., Amodio P., et al. The influence of environmental factors on sleep quality in hospitalized medical patients. Front Neurol. 2014;5:267. doi: 10.3389/fneur.2014.00267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bernhofer E.I., Higgins P.A., Daly B.J., Burant C.J., Hornick T.R. Hospital lighting and its association with sleep, mood and pain in medical inpatients. J Adv Nurs. 2014;70(5):1164–1173. doi: 10.1111/jan.12282. [DOI] [PubMed] [Google Scholar]
- 38.Bevan R., Grantham-Hill S., Bowen R., Clayton E., Grice H., Venditti H.C., et al. Sleep quality and noise: comparisons between hospital and home settings. Arch Dis Child. 2019;104(2):147–151. doi: 10.1136/archdischild-2018-315168. [DOI] [PubMed] [Google Scholar]
- 39.Beveridge C., Knutson K., Spampinato L., Flores A., Meltzer D.O., Van Cauter E., et al. Daytime physical activity and sleep in hospitalized older adults: association with demographic characteristics and disease severity. J Am Geriatr Soc. 2015;63(7):1391–1400. doi: 10.1111/jgs.13520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Casida J.M., Davis J.E., Shpakoff L., Yarandi H. An exploratory study of the patients' sleep patterns and inflammatory response following cardiopulmonary bypass (CPB) J Clin Nurs. 2014;23(15):2332–2342. doi: 10.1111/jocn.12515. [DOI] [PubMed] [Google Scholar]
- 41.Cici R., Özkan M. Determination of sleep quality of hospitalized patients in a neurosurgery clinic. J Tur Sleep Med. 2020;7(3):189–194. [Google Scholar]
- 42.Cook D.J., Arora V.M., Chamberlain M., Anderson S., Peirce L., Erondu A., et al. Improving hospitalized children's sleep by reducing excessive overnight blood pressure monitoring. Pediatrics. 2020;146(3) doi: 10.1542/peds.2019-2217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.DePietro R.H., Knutson K.L., Spampinato L., Anderson S.L., Meltzer D.O., Van Cauter E., et al. Association between inpatient sleep loss and hyperglycemia of hospitalization. Diabetes Care. 2017;40(2):188–193. doi: 10.2337/dc16-1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dobing S., Frolova N., McAlister F., Ringrose J. Sleep quality and factors influencing self-reported sleep duration and quality in the general internal medicine inpatient population. PLoS One. 2016;11(6) doi: 10.1371/journal.pone.0156735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dohno S., Paskewitz D.A., Lynch J.J., Gimbel K.S., Thomas S.A. Some aspects of sleep disturbance in coronary patients. Percept Mot Skills. 1979;48(1):199–205. doi: 10.2466/pms.1979.48.1.199. [DOI] [PubMed] [Google Scholar]
- 46.Frighetto L., Marra C Fau - Bandali S., Bandali S Fau - Wilbur K., Wilbur K., Fau - Naumann T., Naumann T., Fau - Jewesson P., Jewesson P. 2004. An assessment of quality of sleep and the use of drugs with sedating properties in hospitalized adult patients; pp. 1477–7525. (Electronic)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Farias-Fernandez M., Rendon-Macias M.E., Iglesias-Leboreiro J., Bernardez-Zapata I., Gordillo-Rodriguez L. Effects of hospitalization on children's sleep pattern irrespective of sleep problems history. Efectos de la hospitalizacion en el patron del sueno en ninos independientemente de antecedentes de problemas del sueno. 2021;78(4):279–286. doi: 10.24875/BMHIM.20000277. [DOI] [PubMed] [Google Scholar]
- 48.Furlani R., Ceolim M.F. Sleep quality of women with gynecological and breast cancer. Rev Latino-Am Enferm. 2006;14(6):872–878. doi: 10.1590/s0104-11692006000600007. [DOI] [PubMed] [Google Scholar]
- 49.Gathecha E., Rios R., Buenaver L.F., Landis R., Howell E., Wright S. Pilot study aiming to support sleep quality and duration during hospitalizations. J Hosp Med. 2016;11(7):467–472. doi: 10.1002/jhm.2578. [DOI] [PubMed] [Google Scholar]
- 50.Hinds P.S., Hockenberry M., Rai S.N., Zhang L., Razzouk B.I., Cremer L., et al. Clinical field testing of an enhanced-activity intervention in hospitalized children with cancer. J Pain Symptom Manag. 2007;33(6):686–697. doi: 10.1016/j.jpainsymman.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 51.Graef D.M., Crabtree V.M., Srivastava D.K., Li C., Pritchard M., Hinds P.S., et al. Sleep and mood during hospitalization for high-dose chemotherapy and hematopoietic rescue in pediatric medulloblastoma. Psycho Oncol. 2018;27(7):1847–1853. doi: 10.1002/pon.4737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grossman M.N., Anderson S.L., Worku A., Marsack W., Desai N., Tuvilleja A., et al. Awakenings? Patient and hospital staff perceptions of nighttime disruptions and their effect on patient sleep. J Clin Sleep Med : JCSM : off publica Am Acad Sleep Med. 2017;13(2):301–306. doi: 10.5664/jcsm.6468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hacker E.D., Kapella M.C., Park C., Ferrans C.E., Larson J.L. Sleep patterns during hospitalization following hematopoietic stem cell transplantation. Oncol Nurs Forum. 2015;42(4):371–379. doi: 10.1188/15.ONF.371-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Herbert A.R., de Lima J., Fitzgerald D.A., Seton C., Waters K.A., Collins J.J. Exploratory study of sleeping patterns in children admitted to hospital. J Paediatr Child Health. 2014;50(8):632–638. doi: 10.1111/jpc.12617. [DOI] [PubMed] [Google Scholar]
- 55.Hinds P.S., Hockenberry M., Rai S.N., Zhang L., Razzouk B.I., McCarthy K., et al. Nocturnal awakenings, sleep environment interruptions, and fatigue in hospitalized children with cancer. Oncol Nurs Forum. 2007;34(2):393–402. doi: 10.1188/07.ONF.393-402. [DOI] [PubMed] [Google Scholar]
- 56.Ibala R., Mekonnen J., Gitlin J., Hahm E.Y., Ethridge B.R., Colon K.M., et al. A polysomnography study examining the association between sleep and postoperative delirium in older hospitalized cardiac surgical patients. J sleep rees. 2021;30(5) doi: 10.1111/jsr.13322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ida M., Onodera H., Yamauchi M., Kawaguchi M. Preoperative sleep disruption and postoperative functional disability in lung surgery patients: a prospective observational study. J Anesth. 2019;33(4):501–508. doi: 10.1007/s00540-019-02656-y. [DOI] [PubMed] [Google Scholar]
- 58.Jacob E., Miaskowski C., Savedra M., Beyer J.E., Treadwell M., Styles L. Changes in sleep, food intake, and activity levels during acute painful episodes in children with sickle cell disease. J Pediatr Nurs. 2006;21(1):23–34. doi: 10.1016/j.pedn.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 59.Jacob E., Hesselgrave J., Sambuco G., Hockenberry M. Variations in pain, sleep, and activity during hospitalization in children with cancer. J Pediatr Oncol Nurs. 2007;24(4):208–219. doi: 10.1177/1043454207299875. [DOI] [PubMed] [Google Scholar]
- 60.Jakobsen G., Engstrom M., Thronaes M., Lohre E.T., Kaasa S., Fayers P., et al. Sleep quality in hospitalized patients with advanced cancer: an observational study using self-reports of sleep and actigraphy. Support Care Cancer : off. J. Multinatl. Assoc. Supp. Care Cancer. 2020;28(4):2015–2023. doi: 10.1007/s00520-019-04998-5. [DOI] [PubMed] [Google Scholar]
- 61.Javadi N., Darvishpour A., Mehrdad N., Lakeh N.M. Survey of sleep status and its related factors among hospitalized patients with heart failure. J. Tehran Heart Center. 2015;10(1):9–17. [PMC free article] [PubMed] [Google Scholar]
- 62.Jensen P.S., Specht K., Mainz H. Sleep quality among orthopaedic patients in Denmark - a nationwide cross-sectional study. Int J orthop trauma nurs. 2021;40 doi: 10.1016/j.ijotn.2020.100812. [DOI] [PubMed] [Google Scholar]
- 63.Karaman Ozlu Z., Sahin Altun O., Olcun Z., Kaya M., Yurttas A. Examination of the relationship between elective surgical patients' methods for coping with stress and sleeping status the night before an operation. J PeriAnesthesia Nurs : off j Am Soc PeriAnesth Nurses. 2018;33(6):855–864. doi: 10.1016/j.jopan.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 64.Karkare K., Sinha S., Taly A.B., Rao S. Prevalence and profile of sleep disturbances in Guillain-Barre Syndrome: a prospective questionnaire-based study during 10 days of hospitalization. Acta Neurol Scand. 2013;127(2):116–123. doi: 10.1111/j.1600-0404.2012.01688.x. [DOI] [PubMed] [Google Scholar]
- 65.Kessler R., Knutson K.L., Mokhlesi B., Anderson S.L., Shah M., Meltzer D.O., et al. Sleep and activity patterns in older patients discharged from the hospital. Sleep. 2019;42(11) doi: 10.1093/sleep/zsz153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Papaconstantinou E.A., Hodnett E., Stremler R. A behavioral-educational intervention to promote pediatric sleep during hospitalization: a pilot randomized controlled trial. Behav Sleep Med. 2018;16(4):356–370. doi: 10.1080/15402002.2016.1228639. [DOI] [PubMed] [Google Scholar]
- 67.Krenk L., Jennum P., Kehlet H. Sleep disturbances after fast-track hip and knee arthroplasty. Br J Anaesth. 2012;109(5):769–775. doi: 10.1093/bja/aes252. [DOI] [PubMed] [Google Scholar]
- 68.Kulpatcharapong S., Chewcharat P., Ruxrungtham K., Gonlachanvit S., Patcharatrakul T., Chaitusaney B., et al. Sleep quality of hospitalized patients, contributing factors, and prevalence of associated disorders. Sleep disorders. 2020;2020 doi: 10.1155/2020/8518396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Raymond I., Nielsen T.A., Lavigne G., Choiniere M. Incorporation of pain in dreams of hospitalized burn victims. Sleep. 2002;25(7):765–770. doi: 10.1093/sleep/25.7.765. [DOI] [PubMed] [Google Scholar]
- 70.Rogers V.E., Zhu S., Ancoli-Israel S., Liu L., Mandrell B.N., Hinds P.S. A pilot randomized controlled trial to improve sleep and fatigue in children with central nervous system tumors hospitalized for high-dose chemotherapy. Pediatr Blood Cancer. 2019;66(8) doi: 10.1002/pbc.27814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sakr N., Hallit S., Mattar H. Incidence of and factors associated with new-onset insomnia among Lebanese hospitalised patients: a single-centre study. Sultan Qaboos Univ med J. 2021;21(2):e210–e220. doi: 10.18295/squmj.2021.21.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Setoyama A., Ikeda M., Kamibeppu K. Objective assessment of sleep status and its correlates in hospitalized children with cancer: exploratory study. Pediatr Int. 2016;58(9):842–849. doi: 10.1111/ped.12927. [DOI] [PubMed] [Google Scholar]
- 73.Singh S., Sharma S., Bishnoi S., Saini S., Jose S., Sharma R., et al. Sleep and Vigilance; 2021. Sleep quality index and factors influencing sleep of patients in tertiary care hospital: a cross-sectional study. [Google Scholar]
- 74.Stremler R., Micsinszki S., Adams S., Parshuram C., Pullenayegum E., Weiss S.K. 2021. Objective sleep characteristics and factors associated with sleep duration and waking during pediatric hospitalization; pp. 2574–3805. (Electronic)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Suh M., Choi-Kwon S., Kim J.S. Sleep disturbances after cerebral infarction: role of depression and fatigue. J Stroke Cerebrovasc Dis : off J Natl Stroke Assoc. 2014;23(7):1949–1955. doi: 10.1016/j.jstrokecerebrovasdis.2014.01.029. [DOI] [PubMed] [Google Scholar]
- 76.Sultan A., Pati A.K., Choudhary V., Parganiha A. Repeated chemotherapy cycles produced progressively worse and enduring impairments in the sleep-wake profile of hospitalized breast cancer patients. Biol Rhythm Res. 2020;51(8):1166–1181. [Google Scholar]
- 77.Traube C., Rosenberg L., Thau F., Gerber L.M., Mauer E.A., Seghini T., et al. Sleep in hospitalized children with cancer: a cross-sectional study. Hosp Pediatr. 2020;10(11):969–976. doi: 10.1542/hpeds.2020-0101. [DOI] [PubMed] [Google Scholar]
- 78.van den Ende E.S., van Veldhuizen K.D.I., Toussaint B., Merten H., van de Ven P.M., Kok N.A., et al. Hospitalized COVID-19 patients were five times more likely to suffer from total sleep deprivation compared to non-COVID-19 patients; an observational comparative study. Front Neurosci. 2021;15 doi: 10.3389/fnins.2021.680932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.van den Ende E.S., Burger P., Keesenberg M., Merten H., Gemke R.J.B.J., Nanayakkara P.W.B. Patient-nurse agreement on inpatient sleep and sleep disturbing factors. Sleep Med X. 2022;4 doi: 10.1016/j.sleepx.2022.100047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wesselius H.M., van den Ende E.S., Alsma J., ter Maaten J.C., Schuit S.C.E., Stassen P.M., et al. Quality and quantity of sleep and factors associated with sleep disturbance in hospitalized patients. JAMA Intern Med. 2018;178(9):1201–1208. doi: 10.1001/jamainternmed.2018.2669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.White M.A., Wear E., Stephenson G. A computer-compatible method for observing falling asleep behavior of hospitalized children. Res Nurs Health. 1983;6(4):191–198. doi: 10.1002/nur.4770060407. [DOI] [PubMed] [Google Scholar]
- 82.Wilcox M.E., Rubenfeld G.D., Walczak K.D., Black S.E., McAndrews M.P., Lim A.S. Actigraphic measures of sleep on the wards after ICU discharge. J Crit Care. 2019;54:163–169. doi: 10.1016/j.jcrc.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 83.Williams E.T., Buchanan D.T., Buysse D.J., Thompson H.J. Injury, sleep, and functional outcome in hospital patients with traumatic brain injury. J Neurosci Nurs : J Am Assoc Neurosci Nurses. 2019;51(3):134–141. doi: 10.1097/JNN.0000000000000441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Afshar P.F., Zahednezhad H., Khamesloo M.A., Gheshlagh R.G., Fathi R. Effect of white noise on the sleep of elderly patients hospitalized in coronary care units. Salmand-Iranian J ageing. 2016;11(1):44–50. [Google Scholar]
- 85.Aksu N.T., Erdogan A., Ozgur N. Effects of progressive muscle relaxation training on sleep and quality of life in patients with pulmonary resection. Sleep & breathing = Schlaf & Atmung. 2018;22(3):695–702. doi: 10.1007/s11325-017-1614-2. [DOI] [PubMed] [Google Scholar]
- 86.Seid Tegegne S., Fenta Alemnew E. Postoperative poor sleep quality and its associated factors among adult patients: a multicenter cross-sectional study. Ann med surg (2012) 2022;74 doi: 10.1016/j.amsu.2022.103273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ayik C., Ozden D. The effects of preoperative aromatherapy massage on anxiety and sleep quality of colorectal surgery patients: a randomized controlled study. Compl Ther Med. 2018;36:93–99. doi: 10.1016/j.ctim.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 88.Blackburn L., Achor S., Allen B., Bauchmire N., Dunnington D., Klisovic R., et al. The effect of aromatherapy on insomnia and other common symptoms among patients with acute leukemia. Oncol Nurs Forum. 2017;44(4):E185–E193. doi: 10.1188/17.ONF.E185-E193. [DOI] [PubMed] [Google Scholar]
- 89.Bryant A.L., Deal A.M., Battaglini C.L., Phillips B., Pergolotti M., Coffman E., et al. The effects of exercise on patient-reported outcomes and performance-based physical function in adults with acute leukemia undergoing induction therapy: exercise and quality of life in acute leukemia (EQUAL) Integr Cancer Ther. 2018;17(2):263–270. doi: 10.1177/1534735417699881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cao M. Fine nursing model combined with psychological intervention on patients after eyeball enucleation due to ocular trauma. Am J Tourism Res. 2021;13(6):7071–7076. [PMC free article] [PubMed] [Google Scholar]
- 91.Ramezani Kermani A., Aghebati N., Mohajer S., Ghavami V. Effect of guided imagery along with breathing relaxation on sleep quality of the elderly patients under abdominal surgery: a randomized clinical trial. Holist Nurs Pract. 2020;34(6):334–344. doi: 10.1097/HNP.0000000000000415. [DOI] [PubMed] [Google Scholar]
- 92.Khoddam H., Maddah S.A., Rezvani Khorshidi S., Zaman Kamkar M., Modanloo M. The effects of earplugs and eye masks on sleep quality of patients admitted to coronary care units: a randomised clinical trial. J Sleep Res. 2022;31(2) doi: 10.1111/jsr.13473. [DOI] [PubMed] [Google Scholar]
- 93.Leong R.W., Davies L.J., Fook-Chong S., Ng S.Y., Lee Y.L. Effect of the use of earplugs and eye masks on the quality of sleep after major abdominal surgery: a randomised controlled trial. Anaesthesia. 2021;76(11):1482–1491. doi: 10.1111/anae.15468. [DOI] [PubMed] [Google Scholar]
- 94.Lytle J., Mwatha C., Davis K.K. Effect of lavender aromatherapy on vital signs and perceived quality of sleep in the intermediate care unit: a pilot study. Am J Crit Care : an off publ Am Assoc Critical-Care Nurses. 2014;23(1):24–29. doi: 10.4037/ajcc2014958. [DOI] [PubMed] [Google Scholar]
- 95.Ou Y.Y., Liu S., Zhang J.L., Yuan H.Z., Zheng Y.H. Effects of whole-course standardized nursing and humanistic care on the sleep condition and quality of life of elderly patients undergoing hysterectomy for cervical cancer. Eur J Gynaecol Oncol. 2021;42(1):154–160. [Google Scholar]
- 96.Shammas R.L., Marks C.E., Broadwater G., Le E., Glener A.D., Sergesketter A.R., et al. The effect of lavender oil on perioperative pain, anxiety, depression, and sleep after microvascular breast reconstruction: a prospective, single-blinded, randomized, controlled trial. J Reconstr Microsurg. 2021;37(6):530–540. doi: 10.1055/s-0041-1724465. [DOI] [PubMed] [Google Scholar]
- 97.Wakamura T., Tokura H. Influence of bright light during daytime on sleep parameters in hospitalized elderly patients. J Physiol Anthropol Appl Hum Sci. 2001;20(6):345–351. doi: 10.2114/jpa.20.345. [DOI] [PubMed] [Google Scholar]
- 98.Wang L.-N., Tao H., Zhao Y., Zhou Y.-Q., Jiang X.-R. Optimal timing for initiation of biofeedback-assisted relaxation training in hospitalized coronary heart disease patients with sleep disturbances. J Cardiovasc Nurs. 2014;29(4):367–376. doi: 10.1097/JCN.0b013e318297c41b. [DOI] [PubMed] [Google Scholar]
- 99.Wen Y., Ma J., Jiang X., Gao G., Xie H., Lu P. Influencing factors of holistic nursing intervention under a social medical model on the psychology and quality of life of patients with advanced gastric cancer. Am J Tourism Res. 2021;13(4):3369–3379. [PMC free article] [PubMed] [Google Scholar]
- 100.Zhang P., Zhang Y., Han X., Zhang X., Zhu X., Li T. Effect of individualized psychological intervention on negative emotion and sleep quality of patients after bladder cancer surgery: a randomized controlled trial. Transl Androl Urol. 2021;10(7):3021–3029. doi: 10.21037/tau-21-534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Formentin C., Carraro S., Turco M., Zarantonello L., Angeli P., Montagnese S. Effect of morning light glasses and night short-wavelength filter glasses on sleep-wake rhythmicity in medical inpatients. Front Physiol. 2020;11:5. doi: 10.3389/fphys.2020.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ghorbani A., Hajizadeh F., Sheykhi M.R., Mohammad Poor Asl A. The effects of deep-breathing exercises on postoperative sleep duration and quality in patients undergoing coronary artery bypass graft (CABG): a randomized clinical trial. J Caring Sci. 2019;8(4):219–224. doi: 10.15171/jcs.2019.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Dai W.-S., Xie W.-P., Liu J.-F., Chen Q., Cao H. The effects of eye masks on post-operative sleep quality and pain in school-age children with CHD. Cardiol Young. 2021:1–5. doi: 10.1017/S1047951121004480. [DOI] [PubMed] [Google Scholar]
- 104.Farrehi P.M., Clore K.R., Scott J.R., Vanini G., Clauw D.J. Efficacy of sleep tool education during hospitalization: a randomized controlled trial. Am J Med. 2016;129(12):1329. doi: 10.1016/j.amjmed.2016.08.001. e9-.e17. [DOI] [PubMed] [Google Scholar]
- 105.Linder L.A., Christian B.J. Nighttime sleep characteristics of hospitalized school-age children with cancer. J Spec Pediatr Nurs (JSPN) 2013;18(1):13–24. doi: 10.1111/jspn.12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Linder L.A., Christian B.J. Nighttime sleep disruptions, the hospital care environment, and symptoms in elementary school-age children with cancer. Oncol Nurs Forum. 2012;39(6):553–561. doi: 10.1188/12.ONF.553-561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.McKinley S., Fien M., Elliott R., Elliott D. Sleep and psychological health during early recovery from critical illness: an observational study. J Psychosom Res. 2013;75(6):539–545. doi: 10.1016/j.jpsychores.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 108.FitzGerald J.M., O'Regan N., Adamis D., Timmons S., Dunne C.P., Trzepacz P.T., et al. Sleep-wake cycle disturbances in elderly acute general medical inpatients: longitudinal relationship to delirium and dementia. Alzheimer's Dementia. 2017;7:61–68. doi: 10.1016/j.dadm.2016.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chakrabarti S. Mental health in hospitalised COVID 19 patients in quarantine during second wave in a south Indian private teaching hospital. J Multidiscip Healthc. 2021;14:2777–2789. doi: 10.2147/JMDH.S330812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Calev H., Spampinato L.M., Press V.G., Meltzer D.O., Arora V.M. Prevalence of impaired memory in hospitalized adults and associations with in-hospital sleep loss. J Hosp Med. 2015;10(7):439–445. doi: 10.1002/jhm.2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Aaron J.N., Carlisle C.C., Carskadon M.A., Meyer T.J., Hill N.S., Millman R.P. Environmental noise as a cause of sleep disruption in an intermediate respiratory care unit. Sleep. 1996;19(9):707–710. doi: 10.1093/sleep/19.9.707. [DOI] [PubMed] [Google Scholar]
- 112.Adib-Hajbaghery M., Izadi-Avanji F., Akbari H. Quality of sleep and its related risk factors in hospitalized older patients in Kashan's Hospitals, Iran 2009. Iran J Nurs Midwifery Res. 2012;17(6):414–420. [PMC free article] [PubMed] [Google Scholar]
- 113.Akgul E.A., Sari H.Y. Sleep characteristics of pediatric burn patients. J Pediatr Res. 2019;6(2):128–134. [Google Scholar]
- 114.Arora V.M., Chang K.L., Fazal A.Z., Staisiunas P.G., Meltzer D.O., Zee P.C., et al. Objective sleep duration and quality in hospitalized older adults: associations with blood pressure and mood. J Am Geriatr Soc. 2011;59(11):2185–2186. doi: 10.1111/j.1532-5415.2011.03644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bigue J.L., Duclos C., Dumont M., Paquet J., Blais H., Menon D.K., et al. Validity of actigraphy for nighttime sleep monitoring in hospitalized patients with traumatic injuries. J Clin Sleep Med : JCSM : off publica Am Acad Sleep Med. 2020;16(2):185–192. doi: 10.5664/jcsm.8162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bisgaard T., Kjaersgaard M., Bernhard A., Kehlet H., Rosenberg J. Computerized monitoring of physical activity and sleep in postoperative abdominal surgery patients. J Clin Monit Comput. 1999;15(1):1–8. doi: 10.1023/a:1009930026753. [DOI] [PubMed] [Google Scholar]
- 117.Bisogni S., Chiarini I., Giusti F., Ciofi D., Poggi G.M., Festini F. Impact of hospitalization on the sleep patterns of newborns, infants and toddlers admitted to a pediatric ward: a cross-sectional study. Minerva Pediatr. 2015;67(3):209–217. [PubMed] [Google Scholar]
- 118.Boonstra L., Harden K., Jarvis S., Palmer S., Kavanaugh-Carveth P., Barnett J., et al. Sleep disturbance in hospitalized recipients of stem cell transplantation. Clin J Oncol Nurs. 2011;15(3):271–276. doi: 10.1188/11.CJON.271-276. [DOI] [PubMed] [Google Scholar]
- 119.Buyukyilmaz F.E., Sendir M., Acaroglu R. Evaluation of night-time pain characteristics and quality of sleep in postoperative Turkish orthopedic patients. Clin Nurs Res. 2011;20(3):326–342. doi: 10.1177/1054773811406110. [DOI] [PubMed] [Google Scholar]
- 120.Casida J.M., Davis J.E., Zalewski A., Yang J.J. Night-time care routine interaction and sleep disruption in adult cardiac surgery. J Clin Nurs. 2018;27(7):e1377–e1384. doi: 10.1111/jocn.14262. [DOI] [PubMed] [Google Scholar]
- 121.Chang W.-P., Lin C.-C. Correlation between rest-activity rhythm and survival in cancer patients experiencing pain. Chronobiol Int. 2014;31(8):926–934. doi: 10.3109/07420528.2014.931412. [DOI] [PubMed] [Google Scholar]
- 122.Chauny J.-M., Paquet J., Carrier J., Lavigne G., Marquis M., Cournoyer A., et al. Subjective sleep quality and its etiology in the emergency department. CJEM. 2019;21(2):249–252. doi: 10.1017/cem.2018.394. [DOI] [PubMed] [Google Scholar]
- 123.Chong M.S., Tan K.T., Tay L., Wong Y.M., Ancoli-Israel S. Bright light therapy as part of a multicomponent management program improves sleep and functional outcomes in delirious older hospitalized adults. Clin Interv Aging. 2013;8:565–572. doi: 10.2147/CIA.S44926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Clarke L.L., Wilson S., Kirwan J.R. Using actigraphy to measure sleep patterns in rheumatoid arthritis: a pilot study in patients taking night-time prednisone. Muscoskel Care. 2013;11(3):179–185. doi: 10.1002/msc.1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Cone L., Gottschlich M.M., Khoury J., Simakajornboon N., Kagan R.J. The effect of healing touch on sleep patterns of pediatric burn patients: a prospective pilot study. J Sleep Disor: Treat Care 3: 2. of. 2014;6:2. [Google Scholar]
- 126.Cowherd E.L., Sutton A.G., Vincent J.O., Humphries M.S., Ritter V., Fine J., et al. Timing and duration of sleep in hospitalized children: an observational study. Hosp Pediatr. 2019;9(5):333–339. doi: 10.1542/hpeds.2018-0236. [DOI] [PubMed] [Google Scholar]
- 127.Crawford S., Utt A., Beebe C., Armbruster R., Fisher A., Olney A., et al. Quality of sleep in a pediatric hospital: a descriptive study based on an assessment of interruptions, perceptions, and the environment. J Nurs Adm. 2019;49(5):273–279. doi: 10.1097/NNA.0000000000000750. [DOI] [PubMed] [Google Scholar]
- 128.Dobson L., Stutzman S.E., Hicks A.D., Olson D.M. Sleep hygiene in patients with chronic respiratory disease. Nursing. 2019;49(2):64–69. doi: 10.1097/01.NURSE.0000549722.07316.42. [DOI] [PubMed] [Google Scholar]
- 129.Dogan O., Ertekin S., Dogan S. Sleep quality in hospitalized patients. J Clin Nurs. 2005;14(1):107–113. doi: 10.1111/j.1365-2702.2004.01011.x. [DOI] [PubMed] [Google Scholar]
- 130.D'Souza O.L., Alvares I.T.R., Baliga M.S. Factors affecting quality of sleep in hospitalized patients: a cross-sectional survey in a tertiary care hospital. Indian J Med Specialities. 2019;10(4):201–206. [Google Scholar]
- 131.Edéll-Gustafsson U.M., Hetta J.E., Arén C.B. Sleep and quality of life assessment in patients undergoing coronary artery bypass grafting. J Adv Nurs. 1999;29(5):1213–1220. doi: 10.1046/j.1365-2648.1999.01006.x. [DOI] [PubMed] [Google Scholar]
- 132.Ekkernkamp E., Storre J.H., Windisch W., Dreher M. Impact of intelligent volume-assured pressure support on sleep quality in stable hypercapnic chronic obstructive pulmonary disease patients: a randomized, crossover study. Respirat int rev thoracic diseases. 2014;88(4):270–276. doi: 10.1159/000364946. [DOI] [PubMed] [Google Scholar]
- 133.Erondu A.I., Orlov N.M., Peirce L.B., Anderson S.L., Chamberlain M., Hopkins K., et al. Characterizing pediatric inpatient sleep duration and disruptions. Sleep Med. 2019;57:87–91. doi: 10.1016/j.sleep.2019.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Foo C.T., O'Driscoll D.M., Ogeil R.P., Lubman D., Young A.C. Sleep & breathing = Schlaf & Atmung; 2021. Barriers to sleep in acute hospital settings. [DOI] [PubMed] [Google Scholar]
- 135.Gao J., Li Y., Sun Y., Hu W., Liu Y., An D., et al. The study of sleep disorder factors in patients with Guillain-Barre syndrome. Int J Neurosci. 2016;126(10):893–898. doi: 10.3109/00207454.2015.1080699. [DOI] [PubMed] [Google Scholar]
- 136.Garrido M., Saccardo D., De Rui M., Vettore E., Verardo A., Carraro P., et al. Abnormalities in the 24-hour rhythm of skin temperature in cirrhosis: sleep-wake and general clinical implications. Liver Int : off J Int Assoc Study of the Liver. 2017;37(12):1833–1842. doi: 10.1111/liv.13525. [DOI] [PubMed] [Google Scholar]
- 137.Gulam S., Xyrichis A., Lee G.A. Still too noisy - an audit of sleep quality in trauma and orthopaedic patients. Int emerg nursing. 2020;49 doi: 10.1016/j.ienj.2019.100812. [DOI] [PubMed] [Google Scholar]
- 138.Hagemann V. Night sleep of children in a hospital. Part I: sleep duration. Matern Child Nurs J. 1981;10(1):1–13. [PubMed] [Google Scholar]
- 139.Henderson D., Moore V., MacMorran K., Castellini J., Hay K., Keegan V., et al. A cohort study of sleep quality in adult patients with acute pulmonary exacerbations of cystic fibrosis. Intern Med J. 2020;52(1):63–68. doi: 10.1111/imj.15082. [DOI] [PubMed] [Google Scholar]
- 140.Ghanbari Jolfaei A., Makvandi A., Pazouki A. Quality of sleep for hospitalized patients in Rasoul-Akram hospital. Med J Islam Repub Iran. 2014;28:73. [PMC free article] [PubMed] [Google Scholar]
- 141.Jurdi N.E., Nock N., Fu P., Cao S., Cotton J.M., Ali N., et al. Physical activity and sleep measures using a fitness tracking device during hematopoietic cell transplantation: a pilot study. Transpl cellular therapy. 2021;27(6) doi: 10.1016/j.jtct.2021.02.015. 502.e1-.e6. [DOI] [PubMed] [Google Scholar]
- 142.Kamkar M.Z., Khorshidi S.R., Maddah S.M.A., Emami Zeydi A., Modanloo M. A cross-sectional study examining the correlation between nocturnal melatonin level and sleep quality in patients admitted to the cardiac care unit. Open access Maced j med sci. 2018;6(12):2342–2347. doi: 10.3889/oamjms.2018.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kavey N.B., Ahshuler K.Z. Sleep in herniorrhaphy patients. Am J Surg. 1979;138(5):683–687. doi: 10.1016/0002-9610(79)90348-9. [DOI] [PubMed] [Google Scholar]
- 144.Kroon K., West S. 'Appears to have slept well': assessing sleep in an acute care setting. Contemp Nurse. 2000;9(3):284–294. doi: 10.5172/conu.2000.9.3-4.284. [DOI] [PubMed] [Google Scholar]
- 145.Labrosciano C., Tavella R., Reynolds A., Air T., Beltrame J.F., Ranasinghe I., et al. The association between sleep duration and quality with readmissions: an exploratory pilot-study among cardiology inpatients. Clocks & sleep. 2020;2(2):120–142. doi: 10.3390/clockssleep2020011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Lei Z., Qiongjing Y., Qiuli W., Sabrina K., Xiaojing L., Changli W. Sleep quality and sleep disturbing factors of inpatients in a Chinese general hospital. J Clin Nurs. 2009;18(17):2521–2529. doi: 10.1111/j.1365-2702.2009.02846.x. [DOI] [PubMed] [Google Scholar]
- 147.Linker C.-M., Strasburg S., Welsner M., Dietz-Terjung S., Brato S., Geldmacher J., et al. Sleep assessment in cystic fibrosis patients using a minimal-impact biomotion system. Sleep Med. 2021;83:21–25. doi: 10.1016/j.sleep.2021.04.019. [DOI] [PubMed] [Google Scholar]
- 148.Lorenzoni G., Azzolina D., Fraccaro C., Zoccarato C., Minto C., Iliceto S., et al. Sleep quality in patients undergoing transcatheter aortic valve implantation (TAVI) Int J Environ Res Publ Health. 2021;18(16) doi: 10.3390/ijerph18168889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Macfarlane M., Rajapakse S., Loughran S. What prevents patients sleeping on an acute medical ward? An actigraphy and qualitative sleep study. Sleep health. 2019;5(6):666–669. doi: 10.1016/j.sleh.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 150.Mannion H., Molloy D.W., O'Caoimh R. Sleep disturbance in older patients in the emergency department: prevalence, predictors and associated outcomes. Int J Environ Res Publ Health. 2019;16(19) doi: 10.3390/ijerph16193577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Miller A., Roth T., Roehrs T., Yaremchuk K. Correlation between sleep disruption on postoperative pain. Otolaryngol head and neck surg : off j Am Acad Otolaryngol-Head and Neck Surg. 2015;152(5):964–968. doi: 10.1177/0194599815572127. [DOI] [PubMed] [Google Scholar]
- 152.Missildine K. Sleep and the sleep environment of older adults in acute care settings. J Gerontol Nurs. 2008;34(6):15–21. doi: 10.3928/00989134-20080601-06. [DOI] [PubMed] [Google Scholar]
- 153.Missildine K., Bergstrom N., Meininger J., Richards K., Foreman M.D. Sleep in hospitalized elders: a pilot study. Geriatr Nurs. 2010;31(4):263–271. doi: 10.1016/j.gerinurse.2010.02.013. [DOI] [PubMed] [Google Scholar]
- 154.Monas L., Csorba S., Kovalyo M., Zeligman R., Dror Y.F., Musgrave C.F. The relationship of sleep disturbance and symptom severity, symptom interference, and hospitalization among Israeli inpatients with cancer. Oncol Nurs Forum. 2012;39(4):E361–E372. doi: 10.1188/12.ONF.E361-E372. [DOI] [PubMed] [Google Scholar]
- 155.Mori C., Boss K., Indermuhle P., Stahl E., Chiu S.-H., Shanks L. Is it noise? Factors linked with sleep interruption in hospitalized patients. Clinic nurse special CNS. 2021;35(4):199–207. doi: 10.1097/NUR.0000000000000606. [DOI] [PubMed] [Google Scholar]
- 156.Mouch C.A., Baskin A.S., Yearling R., Miller J., Dossett L.A. Sleep patterns and quality among inpatients recovering from elective surgery: a mixed-method study. J Surg Res. 2020;254:268–274. doi: 10.1016/j.jss.2020.04.032. [DOI] [PubMed] [Google Scholar]
- 157.Nunes M.D.R., Nascimento L.C., Fernandes A.M., Batalha L., De Campos C., Gonçalves A., et al. Pain, sleep patterns and health-related quality of life in paediatric patients with cancer. Eur J Cancer Care. 2019;28(4) doi: 10.1111/ecc.13029. [DOI] [PubMed] [Google Scholar]
- 158.Park M.J., Yoo J.H., Cho B.W., Kim K.T., Jeong W.-C., Ha M. Noise in hospital rooms and sleep disturbance in hospitalized medical patients. Environ health and toxicol. 2014;29 doi: 10.5620/eht.2014.29.e2014006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Prendiville R., Umana E., Avalos G., McNicholl B. No rest for the weary: a cross-sectional study comparing patients' sleep in the emergency department to those on the ward. Emerg Med J : EMJ. 2020;37(1):42–44. doi: 10.1136/emermed-2017-207371. [DOI] [PubMed] [Google Scholar]
- 160.Rawal S., Kwan J.L., Razak F., Detsky A.S., Guo Y., Lapointe-Shaw L., et al. Association of the trauma of hospitalization with 30-day readmission or emergency department visit. JAMA Intern Med. 2019;179(1):38–45. doi: 10.1001/jamainternmed.2018.5100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Raymond I., Ancoli-Israel S., Choiniere M. Sleep disturbances, pain and analgesia in adults hospitalized for burn injuries. Sleep Med. 2004;5(6):551–559. doi: 10.1016/j.sleep.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 162.Redeker N.S., Tamburri L., Howland C.L. Prehospital correlates of sleep in patients hospitalized with cardiac disease. Res Nurs Health. 1998;21(1):27–37. doi: 10.1002/(sici)1098-240x(199802)21:1<27::aid-nur4>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 163.Rischer J., Scherwath A., Zander A.R., Koch U., Schulz-Kindermann F. Sleep disturbances and emotional distress in the acute course of hematopoietic stem cell transplantation. Bone Marrow Transplant. 2009;44(2):121–128. doi: 10.1038/bmt.2008.430. [DOI] [PubMed] [Google Scholar]
- 164.Sampath R., Nayak R., Gladston S., Ebenezer K., Mudd S.S., Peck J., et al. Sleep disturbance and psychological distress among hospitalized children in India: parental perceptions on pediatric inpatient experiences. J Spec Pediatr Nurs (JSPN) : J Spec Pediatr Nurs (JSPN) 2021 doi: 10.1111/jspn.12361. [DOI] [PubMed] [Google Scholar]
- 165.Sendir M., Acaroglu R., Kaya H., Erol S., Akkaya Y. Evaluation of quality of sleep and effecting factors in hospitalized neurosurgical patients. Neurosciences. 2007;12(3):226–231. [PubMed] [Google Scholar]
- 166.Shear T.C., Balachandran J.S., Mokhlesi B., Spampinato L.M., Knutson K.L., Meltzer D.O., et al. Risk of sleep apnea in hospitalized older patients. J Clin Sleep Med : JCSM : off publica Am Acad Sleep Med. 2014;10(10):1061–1066. doi: 10.5664/jcsm.4098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Sun H., Li Y., Liu K., Xin D., Chen H., Niu X., et al. Effect of perioperative nursing for artificial knee replacement on patients with osteosarcoma of the distal femur. Am J Tourism Res. 2021;13(9):10356–10362. [PMC free article] [PubMed] [Google Scholar]
- 168.Szady P., Baczyk G., Kozlowska K. Fatigue and sleep quality in rheumatoid arthritis patients during hospital admission. Reumatologia. 2017;55(2):65–72. doi: 10.5114/reum.2017.67600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Terzoudi A., Vorvolakos T., Heliopoulos I., Livaditis M., Vadikolias K., Piperidou H. Sleep architecture in stroke and relation to outcome. Eur Neurol. 2009;61(1):16–22. doi: 10.1159/000165344. [DOI] [PubMed] [Google Scholar]
- 170.Tranmer J.E., Minard J., Fox L.A., Rebelo L. The sleep experience of medical and surgical patients. Clin Nurs Res. 2003;12(2):159–173. doi: 10.1177/1054773803012002004. [DOI] [PubMed] [Google Scholar]
- 171.White M.A., Williams P.D., Alexander D.J., Powell-Cope G.M., Conlon M. Sleep onset latency and distress in hospitalized children. Nurs Res. 1990;39(3):134–139. [PubMed] [Google Scholar]
- 172.Yang C.-F.J., Aibel K., Meyerhoff R., Wang F., Harpole D., Abernethy A.P., et al. Actigraphy assessment of sleep quality among patients with acute myeloid leukaemia during induction chemotherapy. BMJ Support Palliat Care. 2018;8(3):274–277. doi: 10.1136/bmjspcare-2018-001509. [DOI] [PubMed] [Google Scholar]
- 173.Yilmaz M., Sayin Y., Gurler H. Sleep quality of hospitalized patients in surgical units. Nurs Forum. 2012;47(3):183–192. doi: 10.1111/j.1744-6198.2012.00268.x. [DOI] [PubMed] [Google Scholar]
- 174.Yoder J.C., Staisiunas P.G., Meltzer D.O., Knutson K.L., Arora V.M. Noise and sleep among adult medical inpatients: far from a quiet night. Arch Intern Med. 2012;172(1):68–70. doi: 10.1001/archinternmed.2011.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Stewart N.H., Walters R.W., Mokhlesi B., Lauderdale D.S., Arora V.M. Sleep in hospitalized patients with chronic obstructive pulmonary disease: an observational study. J Clin Sleep Med : JCSM : off publica Am Acad Sleep Med. 2020;16(10):1693–1699. doi: 10.5664/jcsm.8646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Aalami H., Moghadam H.M., Moghaddam M.B., Bazeli J. Effect of hybrid aromatherapy on sleep quality of patients with acute coronary syndrome admitted to cardiac care unit. World family med. 2018;16(1):268–275. [Google Scholar]
- 177.Albala L., Bober T., Hale G., Warfield B., Collins M.L., Merritt Z., et al. Effect on nurse and patient experience: overnight use of blue-depleted illumination. BMJ open quality. 2019;8(3) doi: 10.1136/bmjoq-2019-000692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Aldemir K., Sayilan A.A. Effect of a mobilization program administered after open cholecystectomy on sleep duration and several other clinical variables. Cukurova med J. 2020;45(2):613–620. [Google Scholar]
- 179.Babaii A., Adib-Hajbaghery M., Hajibagheri A. Effect of using eye mask on sleep quality in cardiac patients: a randomized controlled trial. Nursing and midwifery stud. 2015;4(4) doi: 10.17795/nmsjournal28332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Cabrera Jaime S., Martinez C., Gonzalo Bachiller V., Zarza Arnau N., Martin Maldonado L., Belen Manrique Palles A., et al. Participatory action research intervention for improving sleep in inpatients with cancer. J Clin Nurs. 2022 doi: 10.1111/jocn.16279. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 181.Chang M., Wang H., Niu T. Influence of psychological nursing on negative emotion and sleep quality of glaucoma trabeculectomy patients. Am J Tourism Res. 2021;13(7):8415–8420. [PMC free article] [PubMed] [Google Scholar]
- 182.Chen S. Research on the improvement of complications and adverse emotions of cervical cancer patients by humanistic care and psychological nursing. Int J Clin Exp Med. 2020;13(10):7303–7312. [Google Scholar]
- 183.De Rui M., Middleton B., Sticca A., Gatta A., Amodio P., Skene D.J., et al. Sleep and circadian rhythms in hospitalized patients with decompensated cirrhosis: effect of light therapy. Neurochem Res. 2015;40(2):284–292. doi: 10.1007/s11064-014-1414-z. [DOI] [PubMed] [Google Scholar]
- 184.Daneshmandi M., Neiseh F., SadeghiShermeh M., Ebadi A. Effect of eye mask on sleep quality in patients with acute coronary syndrome. J Caring Sci. 2012;1(3):135–143. doi: 10.5681/jcs.2012.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Emami-Sigaroudi A., Salari A., Nourisaeed A., Ahmadnia Z., Ashouri A., Modallalkar S.S., et al. Comparison between the effect of aromatherapy with lavender and damask rose on sleep quality in patients undergoing coronary artery bypass graft surgery: a randomized clinical trial. ARYA atherosclerosis. 2021;17(1):1–9. doi: 10.22122/arya.v17i0.2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Fan L., Lei F., Zhu Z., Hu C., Ye L., Wang N. Nursing intervention using a whole-process escort playing a relative role combined with mind mapping in patients undergoing breast cancer surgery: a randomized trial. Ann Palliat Med. 2021;10(12):12047–12054. doi: 10.21037/apm-21-915. [DOI] [PubMed] [Google Scholar]
- 187.Fu Y., Lu H., Shaomin W. Effect of integrated nursing care in treatment of lung cancer patients. Int J Clin Exp Med. 2020;13(4):2766–2773. [Google Scholar]
- 188.Gimenez M.C., Geerdinck L.M., Versteylen M., Leffers P., Meekes G.J.B.M., Herremans H., et al. Patient room lighting influences on sleep, appraisal and mood in hospitalized people. J sleep rees. 2017;26(2):236–246. doi: 10.1111/jsr.12470. [DOI] [PubMed] [Google Scholar]
- 189.Hajibagheri A., Babaii A., Adib-Hajbaghery M. Effect of Rosa damascene aromatherapy on sleep quality in cardiac patients: a randomized controlled trial. Compl Ther Clin Pract. 2014;20(3):159–163. doi: 10.1016/j.ctcp.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 190.Harorani M., Davodabady F., Masmouei B., Barati N. The effect of progressive muscle relaxation on anxiety and sleep quality in burn patients: a randomized clinical trial. Burns : j Int Soc Burn Injuries. 2020;46(5):1107–1113. doi: 10.1016/j.burns.2019.11.021. [DOI] [PubMed] [Google Scholar]
- 191.Jacobs S., Mowbray C., Cates L.M., Baylor A., Gable C., Skora E., et al. Pilot study of massage to improve sleep and fatigue in hospitalized adolescents with cancer. Pediatr Blood Cancer. 2016;63(5):880–886. doi: 10.1002/pbc.25902. [DOI] [PubMed] [Google Scholar]
- 192.Kabuk A., Sendir M., Filinte G. The effect of reflexology massage and passive music therapy intervention before burn dressing on pain, anxiety level and sleep quality. Burns : j Int Soc Burn Injuries. 2021;48(7):1743–1752. doi: 10.1016/j.burns.2021.10.012. [DOI] [PubMed] [Google Scholar]
- 193.Neeru, Khakha D.C., Satapathy S., Dey A.B. Impact of Jacobson Progressive Muscle Relaxation (JPMR) and deep breathing exercises on anxiety, psychological distress and quality of sleep of hospitalized older adults. J Psychosoc Res. 2015;10(2):211–223. [Google Scholar]
- 194.Khosravi A., Bolourchifard F., Ikhani M., Pourhoseingholi M.A. The effect of massage therapy on sleep quality in cardiac care unit patients. Biosci Biotech Res commun. 2017;10(4):645–651. [Google Scholar]
- 195.Lee J.H., Shin J.S., Yoo H.K., Lee J., Lee Y.J., Kim M.R., et al. Short-term effects of a functional cervical pillow on inpatients with neck discomfort: a randomized controlled trial. Int J Clin Exp Med. 2016;9(6):11397–11408. [Google Scholar]
- 196.Li J., Yuan Q., Chen L. Original article effects of psychological nursing on mood, psychology, sleep and quality of life of patients with cervical cancer after neoadjuvant chemotherapy. Int J Clin Exp Med. 2020;13(4):2823–2831. [Google Scholar]
- 197.Moeini M., Khadibi M., Bekhradi R., Mahmoudian S.A., Nazari F. Effect of aromatherapy on the quality of sleep in ischemic heart disease patients hospitalized in intensive care units of heart hospitals of the Isfahan University of Medical Sciences. Iran J Nurs Midwifery Res. 2010;15(4):234–239. [PMC free article] [PubMed] [Google Scholar]
- 198.Nasari M., Ghezeljeh T.N., Haghani H. Effects of nature sounds on sleep quality among patients hospitalized in coronary care units: a randomized controlled clinical trial. Nurs midwifery stud. 2018;7(1):18–23. [Google Scholar]
- 199.Otaghi M., Qavam S., Norozi S., Borji M., Moradi M. Investigating the effect of lavender essential oil on sleep quality in patients candidates for angiography. Biomed Pharmacol J. 2017;10(1):473–478. [Google Scholar]
- 200.Ozlu I., Ozturk Z., Karaman Ozlu Z., Tekin E., Gur A. The effects of progressive muscle relaxation exercises on the anxiety and sleep quality of patients with COVID-19: a randomized controlled study. Psychiatr Care. 2021;57(4):1791–1797. doi: 10.1111/ppc.12750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Ritmala-Castren M., Salantera S., Holm A., Heino M., Lundgren-Laine H., Koivunen M. Sleep improvement intervention and its effect on patients' sleep on the ward. J Clin Nurs. 2021 doi: 10.1111/jocn.15906. Epub 2021 Jun 10. [DOI] [PubMed] [Google Scholar]
- 202.Sable A., Sivabalan T., Shetti A.N. Effectiveness of back massage on sleep pattern among patients with congestive cardiac failure. Iran J Nurs Midwifery Res. 2017;22(5):359–362. doi: 10.4103/ijnmr.IJNMR_142_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Shi X., Ma L., Hao J., Yan W. Regulatory effects of comprehensive psychological intervention on adverse emotions and immune status of cervical cancer patients during the perioperative period. Am J Tourism Res. 2021;13(6):6362–6371. [PMC free article] [PubMed] [Google Scholar]
- 204.Smith M.C., Kemp J., Hemphill L., Vojir C.P. Outcomes of therapeutic massage for hospitalized cancer patients. J Nurs Scholarsh : an off pub Sigma Theta Tau Int Honor Soc Nursing. 2002;34(3):257–262. doi: 10.1111/j.1547-5069.2002.00257.x. [DOI] [PubMed] [Google Scholar]
- 205.Sun H., Liu H., Li J., Wang X. The patterns of graded psychological nursing care for patients after cardiothoracic surgeries. Iran J Public Health. 2017;46(7):899–905. [PMC free article] [PubMed] [Google Scholar]
- 206.Sun L., Yi B., Pan X., Wu L., Shang Z., Jia Y., et al. PTSD symptoms and sleep quality of COVID-19 patients during hospitalization: an observational study from two centers. Nat Sci Sleep. 2021;13:1519–1531. doi: 10.2147/NSS.S317618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Sweity S., Finlay A., Lees C., Monk A., Sherpa T., Wade D. SleepSure: a pilot randomized-controlled trial to assess the effects of eye masks and earplugs on the quality of sleep for patients in hospital. Clin Rehabil. 2019;33(2):253–261. doi: 10.1177/0269215518806041. [DOI] [PubMed] [Google Scholar]
- 208.Wang S., Tian H., Xue R. Using psychological interventions in the nursing care of rectal cancer patients. Am J Tourism Res. 2021;13(6):7282–7287. [PMC free article] [PubMed] [Google Scholar]
- 209.Yayla A., Ozer N. Effects of early mobilization protocol performed after cardiac surgery on patient care outcomes. Int J Nurs Pract. 2019;25(6) doi: 10.1111/ijn.12784. [DOI] [PubMed] [Google Scholar]
- 210.Manuel A.R., Ribeiro A.F., Completo S., Silva S., L’oureiro H.C. Sleep friendly ward: a pilot Project in a level II hospital. Port J pediatr. 2021:52. [Google Scholar]
- 211.Lima R.O., Landim M.B.P., de França Ferreira L.G., Pinto J.G.M., de Moura N.R.V., Barbosa M.F.L. Subjective sleep pattern in hospitalized patients. Sleep Sci. 2022;15:120–127. doi: 10.5935/1984-0063.20220010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Cilingir D., Hintistan S., Ergene O. Factors affecting the sleep status of surgical and medical patients at a University Hospital of Turkey. JPMA J Pakist Med Assoc. 2016;66(12):1535–1540. [PubMed] [Google Scholar]
- 213.Delaney L.J., Currie M.J., Huang H.C.C., Lopez V., Van Haren F. "They can rest at home": an observational study of patients' quality of sleep in an Australian hospital. BMC Health Serv Res. 2018;18(1):524. doi: 10.1186/s12913-018-3201-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Pimentel-Souza F., Carvalho J.C., Siqueira A.L. Noise and the quality of sleep in two hospitals in the city of Belo Horizonte, Brazil. Brazil j med biol res Revista brasileira de pesquisas médicas e biológicas/Sociedade Brasileira de Biofísica [et al] 1996;29(4):515–520. [PubMed] [Google Scholar]
- 215.Simpson T., Lee E.R., Cameron C. Relationships among sleep dimensions and factors that impair sleep after cardiac surgery. Res Nurs Health. 1996;19(3):213–223. doi: 10.1002/(SICI)1098-240X(199606)19:3<213::AID-NUR5>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 216.Yinnon A.M., Ilan Y., Tadmor B., Altarescu G., Hershko C. Quality of sleep in the medical department. Br J Clin Pract. 1992;46(2):88–91. [PubMed] [Google Scholar]
- 217.Alparslan G.B., Orsal Ö., Unsal A. Assessment of sleep quality and effects of relaxation exercise on sleep quality in patients hospitalized in internal medicine services in a university hospital: the effect of relaxation exercises in patients hospitalized. Holist Nurs Pract. 2016;30(3):155–165. doi: 10.1097/HNP.0000000000000147. [DOI] [PubMed] [Google Scholar]
- 218.Antonio C.K. Improving quiet at night on a telemetry unit: introducing a holistic sleep menu intervention. Am J Nurs. 2020;120(10):58–64. doi: 10.1097/01.NAJ.0000718660.44502.86. [DOI] [PubMed] [Google Scholar]
- 219.Borji M., Otaghi M., Salimi E., Sanei P. Investigating the effect of performing the quiet time protocol on the sleep quality of cardiac patients. Biomed Res. 2017;28(16):7076–7080. [Google Scholar]
- 220.Herscher M., Mikhaylov D., Barazani S., Sastow D., Yeo I., Dunn A.S., et al. A sleep hygiene intervention to improve sleep quality for hospitalized patients. Joint Comm J Qual Patient Saf. 2021;47(6):343–346. doi: 10.1016/j.jcjq.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 221.Lareau R., Benson L., Watcharotone K., Manguba G. Examining the feasibility of implementing specific nursing interventions to promote sleep in hospitalized elderly patients. Geriatr Nurs. 2008;29(3):197–206. doi: 10.1016/j.gerinurse.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 222.Lopez G., Christie A.J., Powers-James C., Bae M.S., Dibaj S.S., Gomez T., et al. The effects of inpatient music therapy on self-reported symptoms at an academic cancer center: a preliminary report. Support Care Cancer. 2019;27(11):4207–4212. doi: 10.1007/s00520-019-04713-4. [DOI] [PubMed] [Google Scholar]
- 223.Norton C., Flood D., Brittin A., Miles J. Improving sleep for patients in acute hospitals. Nurs Stand : 1987) 2015;29(28):35–42. doi: 10.7748/ns.29.28.35.e8947. [DOI] [PubMed] [Google Scholar]
- 224.Thomas K.P., Salas R.E., Gamaldo C., Chik Y., Huffman L., Rasquinha R., et al. Sleep rounds: a multidisciplinary approach to optimize sleep quality and satisfaction in hospitalized patients. J Hosp Med. 2012;7(6):508–512. doi: 10.1002/jhm.1934. [DOI] [PubMed] [Google Scholar]
- 225.Wei R., Chen Y. Factors influencing mental resilience and the applied value of modified cognitive behavioral intervention in patients with spinal metastases. Int J Clin Exp Med. 2021;14(2):1264–1273. [Google Scholar]
- 226.Xiao C.-X., Lin Y.-J., Lin R.-Q., Liu A.-N., Zhong G.-Q., Lan C.-F. Effects of progressive muscle relaxation training on negative emotions and sleep quality in COVID-19 patients: a clinical observational study. Medicine. 2020;99(47) doi: 10.1097/MD.0000000000023185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Zhang G., Wang H., Zhang X., Feng X., Sun Y., Lou C. Observation of quality of life and negative emotions of patients with cervical cancer after neoadjuvant chemotherapy in early psychological nursing. Int J Clin Exp Med. 2019;12(3):2784–2791. [Google Scholar]
- 228.Zhou J., Xu H., Jiang M., Cao H., Jiang L., Xu T., et al. Effect of PDCA-based nursing management model on the quality of life and complications of patients with acute leukemia undergoing chemotherapy. Am J Tourism Res. 2021;13(4):3246–3253. [PMC free article] [PubMed] [Google Scholar]
- 229.Buysse D.J., Reynolds Cf, Fau - Monk T.H., Monk Th, Fau - Berman S.R., Berman Sr Fau - Kupfer D.J., Kupfer D.J. 1989. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. (0165-1781 (Print)) [DOI] [PubMed] [Google Scholar]
- 230.Aktas Y.Y., Yilmaz E.B. The association of pain, anxiety, depression, and sleep patterns in postoperative Turkish patients. Kuwait Medical Journal. 2017;49(4):306–312. [Google Scholar]
- 231.Ohayon M., Wickwire E.M., Hirshkowitz M., Albert S.M., Avidan A., Daly F.J., et al. 2017. National Sleep Foundation's sleep quality recommendations: first report; pp. 2352–7226. (Electronic)) [DOI] [PubMed] [Google Scholar]
- 232.Rensen N.A.-O., Steur L.A.-O.X., Wijnen N., van Someren E.A.-O., Kaspers G.A.-O., van Litsenburg R.A.-O. 2020. Actigraphic estimates of sleep and the sleep-wake rhythm, and 6-sulfatoxymelatonin levels in healthy Dutch children; pp. 1525–6073. (Electronic)) [DOI] [PubMed] [Google Scholar]
- 233.Chaput J.-P., Dutil C. Lack of sleep as a contributor to obesity in adolescents: impacts on eating and activity behaviors. Int J Behav Nutr Phys Activ. 2016;13(1):103. doi: 10.1186/s12966-016-0428-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. (2352-7226 (Electronic)). [DOI] [PubMed]
- 235.Kocevska DA-O, Lysen TA-OX, Dotinga A, Koopman-Verhoeff ME, Luijk MA-O, Antypa N, et al. Sleep characteristics across the lifespan in 1.1 million people from The Netherlands, United Kingdom and United States: a systematic review and meta-analysis. LID - 10.1038/s41562-020-00965-x [doi]. (2397-3374 [Electronic))]. [DOI] [PubMed]
- 236.Pollak CP, Tryon Ww, Fau - Nagaraja H, Nagaraja H, Fau - Dzwonczyk R, Dzwonczyk R. How accurately does wrist actigraphy identify the states of sleep and wakefulness? (0161-8105 (Print)). [DOI] [PubMed]
- 237.Acebo C, Sadeh A Fau - Seifer R, Seifer R, Fau - Tzischinsky O, Tzischinsky O Fau - Wolfson AR, Wolfson Ar Fau - Hafer A, Hafer A Fau - Carskadon MA, et al. Estimating sleep patterns with activity monitoring in children and adolescents: how many nights are necessary for reliable measures? (0161-8105 (Print)). [DOI] [PubMed]
- 238.Sadeh A. Evaluating night wakings in sleep-disturbed infants: a methodological study of parental reports and actigraphy. (0161-8105 (Print)). [DOI] [PubMed]
- 239.INVALID CITATION !!! (235-237).
- 240.Seow L.A.-O., Tan X.W., Chong S.A., Vaingankar J.A., Abdin E., Shafie S., et al. 2016. Independent and combined associations of sleep duration and sleep quality with common physical and mental disorders: results from a multi-ethnic population-based study; pp. 1932–6203. (Electronic)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Lao X.Q., Liu X., Deng H.B., Chan T.C., Ho K.F., Wang F., et al. 2018. Sleep quality, sleep duration, and the risk of coronary heart disease: a prospective cohort study with 60,586 adults; pp. 1550–9397. (Electronic)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Moore P.J., Adler Ne Fau - Williams D.R., Williams Dr, Fau - Jackson J.S., Jackson J.S. 2002. Socioeconomic status and health: the role of sleep. (0033-3174 (Print)) [DOI] [PubMed] [Google Scholar]
- 243.Mollayeva T., Thurairajah P., Burton K., Mollayeva S., Shapiro C.M., Colantonio A. 2016. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis; pp. 1532–2955. (Electronic)) [DOI] [PubMed] [Google Scholar]
- 244.Richards K.C., O'Sullivan Ps Fau - Phillips R.L., Phillips R.L. 2000. Measurement of sleep in critically ill patients; pp. 1061–3749. (Print)) [PubMed] [Google Scholar]
- 245.INVALID CITATION !!! (242, 243).
- 246.Hybschmann J., Topperzer M.K., Gjærde L.K., Born P., Mathiasen R., Sehested A.M., et al. Sleep in hospitalized children and adolescents: a scoping review. Sleep Med Rev. 2021 doi: 10.1016/j.smrv.2021.101496. [DOI] [PubMed] [Google Scholar]
- 247.Snyder-Halpern R Fau - Verran J.A., Verran J.A. 1987. Instrumentation to describe subjective sleep characteristics in healthy subjects. (0160-6891 (Print)) [DOI] [PubMed] [Google Scholar]
- 248.Bastien C.H., Vallières A., Morin C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 249.Johns M.W. 1991. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. (0161-8105 (Print)) [DOI] [PubMed] [Google Scholar]
- 250.Ellis B.W., Johns M.W., Lancaster R., Raptopoulos P., Angelopoulos N., Priest R.G. The St. Mary's Hospital sleep questionnaire: a study of reliability. Sleep. 1981;4(1):93–97. doi: 10.1093/sleep/4.1.93. [DOI] [PubMed] [Google Scholar]
- 251.Yu L., Buysse Dj, Fau - Germain A., Germain A Fau - Moul D.E., Moul De Fau - Stover A., Stover A Fau - Dodds N.E., Dodds Ne Fau - Johnston K.L., et al. 2011. Development of short forms from the PROMIS™ sleep disturbance and Sleep-Related Impairment item banks; pp. 1540–2010. (Electronic)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Akerstedt T., Gillberg M. 1990. Subjective and objective sleepiness in the active individual. (0020-7454 (Print)) [DOI] [PubMed] [Google Scholar]
- 253.Linder L.A., Christian B.J. Nighttime sleep characteristics of hospitalized school-age children with cancer. J Spec Pediatr Nurs (JSPN) 2013;18(1):13–24. doi: 10.1111/jspn.12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Nunes M.D.R., Nascimento L.C., Fernandes A.M., Batalha L., De Campos C., Gonçalves A., et al. Pain, sleep patterns and health-related quality of life in paediatric patients with cancer. Eur J Cancer Care. 2019;28(4):1–10. doi: 10.1111/ecc.13029. [DOI] [PubMed] [Google Scholar]
- 255.Hagemann V. Night sleep of children in a hospital. Part II: sleep disruption. Matern Child Nurs J. 1981;10(2):127–142. [PubMed] [Google Scholar]
- 256.Lundgren J., Norell-Clarke A., Hellstrom I., Angelhoff C. vol. 6. Sage Open Nursing; 2020. (Adolescents' experiences of staying overnight at family-centered pediatric wards). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Ackerman S.L., Lown E.A., Dvorak C.C., Dunn E.A., Abrams D.I., Horn B.N., et al. Massage for children undergoing hematopoietic cell transplantation: a qualitative report. Evid Based Complement Alternat Med. 2012;2012 doi: 10.1155/2012/792042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Anggerainy S.W., Wanda D., Nurhaeni N. Music therapy and story telling: nursing interventions to improve sleep in hospitalized children. Compr Child Adolesc Nurs. 2019;42:82–89. doi: 10.1080/24694193.2019.1578299. [DOI] [PubMed] [Google Scholar]
- 259.Peirce L.B., Orlov N.M., Erondu A.I., Anderson S.L., Chamberlain M., Gozal D., et al. Caregiver and staff perceptions of disruptions to pediatric inpatient sleep. J Clin Sleep Med. 2018;14(11):1895–1902. doi: 10.5664/jcsm.7488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Grandsire C. La qualité du sommeil de l'enfant hospitalisé. Soins - Pediatr Pueric. 1999;(190):20–21. 3. [PubMed] [Google Scholar]
- 261.Mozer C.L., Bhagat P.H., Seward S.A., Mason N.R., Anderson S.L., Byron M., et al. Optimizing oral medication schedules for inpatient sleep: a quality improvement intervention. Hosp Pediatr. 2021;11(4):327–333. doi: 10.1542/hpeds.2020-002261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Talebi Ghadicolaei H., Heydary Gorji M.A., Bagheri B., Yazdani Charati J., Hadinejad Z. The effect of warm footbath on the quality of sleep on patients with acute coronary syndrome in cardiac care unit. J Caring Sci. 2019;8(3):137–142. doi: 10.15171/jcs.2019.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Chen S.-C., Yeh M.-L., Chang H.-J., Lin M.-F. Music, heart rate variability, and symptom clusters: a comparative study. Support Care Cancer : off. J. Multinatl. Assoc. Supp. Care Cancer. 2020;28(1):351–360. doi: 10.1007/s00520-019-04817-x. [DOI] [PubMed] [Google Scholar]
- 264.Kalra R., Natu M.V., Deswal R.S., Agarwal A.K. Dream features in psychiatric patients on multiple psychoactive drugs. Hum Psychopharmacol. 2000;15(7):525–528. doi: 10.1002/1099-1077(200010)15:7<525::AID-HUP215>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 265.Sun H., Li Y., Liu K.M., Xin D.S., Chen H.W., Niu X.M., et al. Effect of perioperative nursing for artificial knee replacement on patients with osteosarcoma of the distal femur. Am J Tourism Res. 2021;13(9):10356–10362. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.