Abstract
Treatment resistant depression (TRD) is a complex condition associated with a great deal of disability and suffering. The relationship between TRD and psychological well-being (PWB) appears to be more complex than a simple antithesis. Transcranial magnetic stimulation (TMS) is a well-tolerated treatment for TRD. However successful, a drawback for TMS is that it has a lack of predictive biomarkers for treatment response. Our study focuses on the relationship between PWB and treatment resistant depression, and how PWB relates to TMS treatment response. We hypothesized that TMS treatment responders would have higher levels of PWB at baseline. In this study of 21 patients with TRD, we used the Ryff Scales of Psychological Well-Being and Patient Health Questionnaire-9 (PHQ-9). We found a significant relationship between environmental mastery, purpose in life, self-acceptance, and total PWB with baseline depression but no significant correlation between autonomy, personal growth, and positive relations with others and baseline PHQ-9 scores. No Ryff domain of PWB significantly predicted change in PHQ-9 score. Interestingly, however, we found that TMS responders had higher levels of autonomy (M(SD) = 62.10(10.46), p = 0.022) and personal growth (M(SD) = 65.00(11.04), p = 0.007) than non-responders at baseline. These specific aspects of well-being appear to be distinct from depression and particularly important in treatment response. This discovery suggests that assessing PWB might prove clinically useful when assessing future candidates for TMS treatment of TRD. Further research is necessary to evaluate the effects of TMS on PWB since these may be distinct from its effect on depression symptomology.
Keywords: Transcranial magnetic stimulation, Well-being, Depression
1. Introduction
Major depressive disorder (MDD) is a common psychiatric condition affecting 1-in-5 people at some point in their lifetime (Malhi and Mann, 2018). Globally, depressive disorders are one of the top 10 contributors to disease burden across the lifespan (GBD, 2019). The effects of long-term depression can be severe and include damaged relationships, occupational dysfunction, and suicide. Although advances in antidepressant medications have led to the development of more tolerable treatment options, approximately 20–30% of patients suffering from depression fail to respond to several antidepressant trials and are classified as “treatment resistant” (Cusin and Dougherty, 2012).
The National Institute of Mental Health defines treatment-resistant depression (TRD) as depression that does not improve after at least two antidepressant therapy trials. In the STAR*D trial, a large-scale multi-site clinical trial examining acute and long-term treatment outcomes for depression, 50% of patients with depression would meet criteria for TRD, with 1-in-3 subjects remaining resistant despite four unique treatment trials (Rush et al., 2006). In such cases, transcranial magnetic stimulation (TMS) may be used as an alternative treatment method. TMS is a noninvasive tool that serves to manipulate activity in specific neural circuits of the human brain (Paus and Barrett, 2004). TMS is a low risk, highly effective, and well tolerated treatment for MDD, approved by the FDA for adults who have had unsuccessful trials with antidepressants or psychotherapy (Cusin and Dougherty, 2012). Although TMS has proven efficacious for TRD patients, there remains a significant proportion of patients who fail to respond (Carpenter et al., 2012).
One drawback with TMS is the lack of predictive biomarkers of treatment response. Although not unique to TMS amongst the antidepressant treatments, this is especially problematic because of the time- and resource-intensive nature of TMS. The current well-established antidepressant treatment protocol requires patients to receive stimulation in the hospital five days per week for four to six weeks (Perera et al., 2016), necessitating frequent travel that can be logistically challenging and expensive. Small studies have identified various neurobiological, imaging-based, or electrophysiologic biomarkers of response, many of which fail to replicate or are yet to be prospectively validated (Kar, 2019; Cash et al., 2021). Methods or tests capable of identifying patients with a good chance of response are thus sorely needed. One area of study involves looking at baseline temperament and personality traits as predictors of treatment response (Siddiqi et al., 2016). Siddiqi et al. (2016) showed that patients who responded to TMS treatment had significantly higher levels of persistence at baseline compared to those who did not respond to treatment. In contrast, a study that investigated the Big Five personality traits suggested that none of the psychological measures they used were clinically meaningful predictors of rTMS treatment response in patients with MDD (Krepel et al., 2020). A study by Fitzgerald et al. (2016) found evidence for predictive utilities of psychological measures; however, they did not find it to be highly influential on rTMS response rates. Work in this area is nascent and remains open for exploration. The goal of this study was to investigate the relationship between psychological well-being (PWB) and difficult-to-treat depression (McAllister-Williams et al., 2020) in adults with MDD undergoing TMS.
Personality disposition has been implicated as a determinant of well-being levels (Costa Jr. et al., 1987) but, to our knowledge, no work to date has examined the relationship between PWB and treatment response in TMS. Like personality, research shows that PWB is an enduring, trait-like characteristic (Mann et al., 2021). While a singular definition of PWB remains elusive in the literature, PWB can be broadly conceptualized as optimal psychological functioning that is in line with a person’s true potential and values (Ryan and Huta, 2009). The Ryff scale (Ryff, 1989) and other contemporary investigations of PWB often operationalize well-being along six domains: autonomy, environmental mastery, personal growth, positive relations with others, purpose in life, and self-acceptance. A significant body of work has examined the correlates of PWB, showing that PWB is associated with improved physical and mental health outcomes (Keyes, 2005; Ryff et al., 2015; Lamers et al., 2015; Steptoe et al., 2015; Wood and Joseph, 2010).
Research shows an inverse relationship between depression and PWB (see Ruini and Cesetti, 2019 for review). Various studies support the dual continuum model of mental health which holds that mental health (i.e., emotional, psychological, and social well-being) and mental illness (i.e., major depression, anxiety, and other psychopathology) are two distinct but correlated unipolar dimensions of health (Keyes, 2005; Keyes et al., 2010). According to this model, PWB is not merely the absence of depression but rather a separate indicator of health (Fava et al., 1998; Keyes et al., 2010; Rafanelli et al., 2000; Ruini et al., 2003). Evidence suggests that PWB serves as a protective factor for mental health and that the absence of PWB may be a risk factor for developing depression (Keyes et al., 2010; Wood and Joseph, 2010).
To further elucidate the relationship between PWB and depression, in this study we examined how the Ryff scale’s various domains of psychological well-being — autonomy, environmental mastery, personal growth, positive relations with others, purpose in life, and self-acceptance — were associated with depression symptoms at baseline before treatment. Next, we investigated if baseline levels of well-being were related to TMS treatment response. We hypothesized that TMS responders would have higher levels of PWB at baseline, given the predictive value of PWB evidenced in the literature.
2. Methods
This study included 21 participants treated at the TMS clinic at University of Iowa Hospitals and Clinics. All subjects were assessed clinically for appropriateness of repetitive transcranial magnetic stimulation (rTMS) treatment. All subjects signed an informed consent document to allow for data collection while undergoing rTMS treatments.
2.1. Subjects
Subjects were recruited from the University of Iowa Interventional Psychiatry program. The study was approved by the Institutional Review Board at the university in accordance with the Declaration of Helsinki and was prospective and observational in nature, with subjects enrolled for additional testing while undergoing standard-of-care clinical transcranial magnetic stimulation for depressive symptoms (see Supplementary Fig. 1 for recruitment details). Subjects were eligible for inclusion if they had a DSM-V diagnosis of MDD, moderate or severe, without psychotic features, as determined by a clinical diagnostic exam performed by a psychiatrist specializing in the use of TMS. Treatment resistance was determined by history and review of medical records. All patients had at least two antidepressant medication trials with demonstrated inadequacy or intolerance. Subjects were excluded from participation if they had ferromagnetic material in the head or neck, history of seizure disorder, or depression attributable to a diagnosis other than MDD, as determined by the evaluating psychiatrist. All TMS treatments were performed with high frequency stimulation at the left dorsolateral prefrontal cortex for a six-week course of treatment, with five sessions per week, followed by a taper phase and thus averaging 34 treatments per subject. Some responders terminated treatment early if clinically indicated by the psychiatric treatment team. Treatment was conducted with a Magventure Figure8 Cool-B65 coil and a MagPro X100 stimulator (Alpharetta, GA). Treatment sessions consisted of either 10 Hz stimulation (3000 total pulses, 4 s train durations, 26 s intertrain interval) or intermittent theta burst stimulation (600 total pulses, 50 Hz triplets nested in 5 Hz carrier frequency, 2 s train duration, 8 s intertrain interval) based on the clinical decision of the psychiatrist and subject, delivered at 120% motor threshold as per standard treatment protocols. Twelve subjects received iTBS, eight subjects received 10 Hz, and one subject received 10 Hz until the 22nd treatment then switched to iTBS.
2.2. Instruments
2.2.1. PHQ-9
The 9-item Patient Health Questionnaire (PHQ-9) is a self-reported scale used to assess the presence and severity of depression. All participants completed this scale at their initial clinical evaluation and weekly throughout the duration of their rTMS course. A 50% or greater decrease in PHQ-9 score from the initial clinical evaluation to the six-week PHQ-9 score was used to indicate treatment response.
2.2.2. Ryff Scale of PWB
The Ryff Scale of Psychological Well-Being is a self-report scale used to assess six domains of PWB: autonomy, environmental mastery, personal growth, positive relations with others, purpose in life, and self- acceptance. Participants completed the 84-item Ryff scale at their initial visit. Each domain of the scale consists of 14 items and participants provide responses using a 6-point Likert-type scale with scores ranging from 14 to 84. Individual domain scores and a cumulative total well-being score were assessed and utilized in this analysis.
2.3. Statistical analyses
First, Pearson correlation coefficients were calculated to examine the relationship between the Ryff scale domains and baseline levels of depression. Then, participants were categorized into treatment responders or non-responders based on their change in score from the initial PHQ-9 total score to the final PHQ-9 total score in the acute treatment series. Percent change from PHQ-9 baseline score to PHQ-9 six-week score was calculated to determine treatment response. A 50% or greater decrease in PHQ-9 score defined treatment response, as per prior literature (Coley et al., 2019). Due to a small sample size, Welch Two Sample t-tests were performed to assess differences in demographics and baseline scores on Ryff scale domains between treatment responders and non-responders. A hierarchical regression analysis was performed to explore the relationship between each Ryff domain and percent change of the PHQ-9 score. No covariates were added to this analysis due to sample size and adjustments were made for multiple comparisons. A significance level of p < 0.05 was used for all two-sample t-test analyses and a significance level of p < 0.007 was used for the hierarchical regression analysis to correct for multiple comparisons. Statistical analyses were completed using RStudio Version 3.6.1.
3. Results
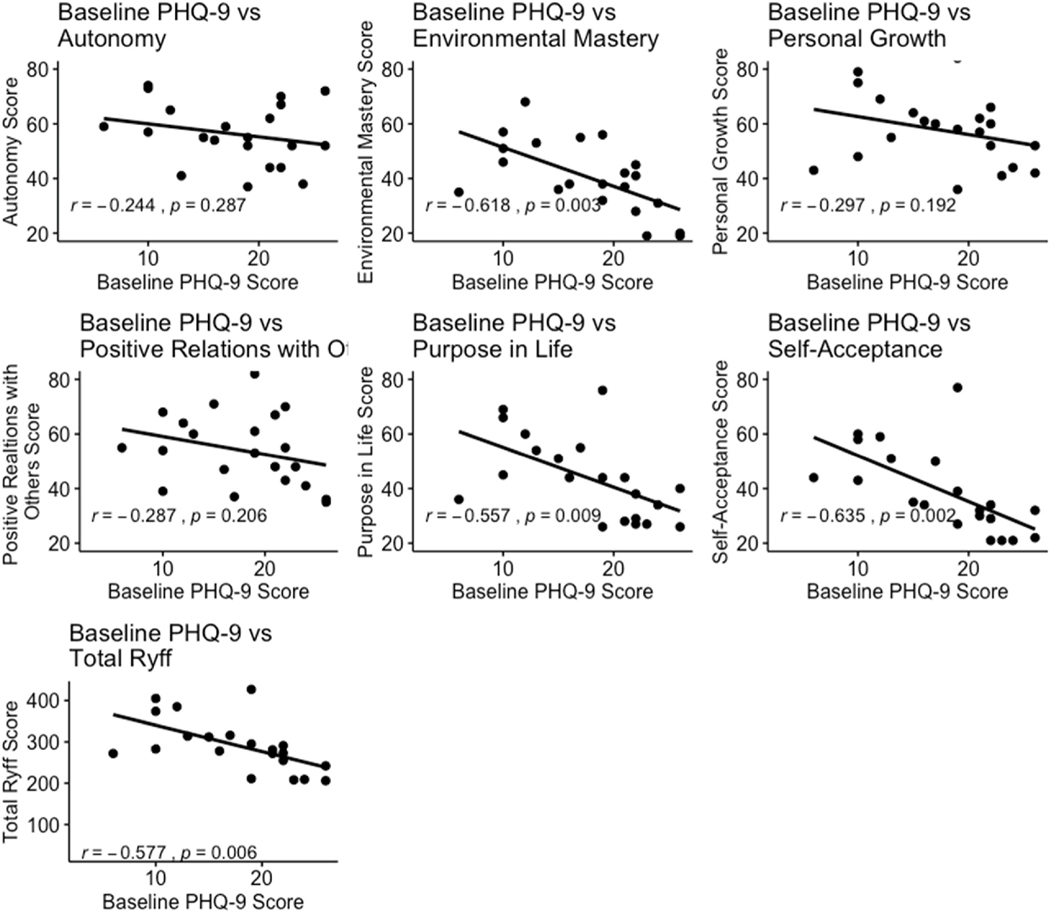
21 participants were eligible for inclusion in this analysis. Analyses showed that self-acceptance, environmental mastery, purpose in life, and total PWB were negatively correlated with baseline PHQ-9 score, illustrating an inverse relationship between well-being and depression (Fig. 1). Interestingly, autonomy, personal growth, and positive relations with others were not significantly related to baseline PHQ-9 score, indicating that these domains of well-being may be separate from depression.
Fig. 1.
Correlations between Ryff domain and baseline PHQ-9 score.
Table 1 describes baseline characteristics for each treatment group. No significant differences in age, sex, or initial PHQ-9 score were found between groups (see Supplementary Table 2 for group medication). A significant difference was observed between mean percent change in PHQ-9 score between groups, which was expected.
Table 1.
Sample characteristics by treatment response.
| Characteristic | Non-Responder (n = 11) |
Responder (n = 10) |
p |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
|
| |||
| Age (y) | 42.4 (16.6) | 52.6 (12.6) | 0.131 |
| Sex (%F) | 63.6% | 60.0% | 0.620 |
| Mean Initial PHQ-9 Score | 17.4 (6.4) | 18.2 (5.3) | 0.750 |
| Mean Percent Change in PHQ-9 Score | 13.7% (21.1) | 73.4% (12.6) | <0.001 |
Baseline scores on each Ryff scale domain and on total PWB were compared in responders (n = 10) vs. non-responders (n = 11) (Table 2). Significant differences between groups were found on measures of autonomy (p = 0.022) and personal growth (p = 0.007). Treatment responders were found to have higher baseline levels of autonomy and personal growth when compared to treatment non-responders.
Table 2.
Differences in baseline Ryff well-being domains by treatment response.
| Non-Responder (n = 11) |
Responder (n = 10) |
p | |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
|
| |||
| Autonomy | 51.0 (9.7) | 62.1 (10.5) | 0.022 |
| Environmental Mastery | 38.6 (14.6) | 42.2 (12.2) | 0.550 |
| Personal Growth | 50.7 (10.6) | 65.0 (11.0) | 0.007 |
| Positive Relations with Others | 50.6 (10.3) | 57.7 (15.5) | 0.242 |
| Purpose in Life | 38.6 (11.8) | 49.5 (16.9) | 0.107 |
| Self-Acceptance | 35.8 (12.1) | 42.5 (18.3) | 0.343 |
| Total Score | 265.4 (55.2) | 319.0 (62.9) | 0.051 |
A hierarchical regression analysis assessing Ryff domains on PHQ-9 score showed no significant results, although trends were identified as presented in the supplement (Supplementary Table 3). Please see supplementary material (Supplementary Tables 4 and 5) for additional analyses.
4. Discussion
In line with previous work, analyses showed that self-acceptance, environmental mastery, purpose in life, and total PWB were negatively correlated with baseline PHQ-9 score, illustrating an inverse relationship between well-being and depression. Interestingly, autonomy, personal growth, and positive relations with others were not significantly related to baseline PHQ-9 score, indicating that these domains of well-being may be separate from depression. Taken together, these initial results provide evidence in support of the dual-continuum hypothesis (Keyes, 2005; Trompetter et al., 2017; Westerhof and Keyes, 2010), illustrating the complex relationship between well-being and depression as overlapping and distinct constructs. PWB cannot simply be equated to lack of distress (Rafanelli et al., 2000) or absence of symptoms (Ruini et al., 2003) in mood and anxiety disorders and should be appropriately assessed in treatment protocols.
In comparisons of baseline well-being in responders vs. non-responders, significant differences emerged in the domains of autonomy and personal growth, such that autonomy and personal growth were higher in responders than in non-responders. Of note, autonomy and personal growth comprise two of the three aspects of well-being that were not correlated with baseline depression. This may indicate that these aspects of well-being, which are liksely distinct from depression, are particularly important in treatment response. This suggests that assessing PWB might provide added value to a psychiatric assessment when evaluating possible candidates for rTMS. Other studies have found that assessing positive PWB is crucial in contextualizing one’s depressive symptoms during a thorough psychiatric evaluation. Ruini et al. (2015) found that mood and anxiety disorders were associated with high levels of psychological distress and low levels of PWB, and evaluating these factors could assist with prognostication.
Furthermore, autonomy and personal growth might serve as useful behavioral treatment targets prior to and during an rTMS course. Although PWB therapy has not been combined with TMS to date, research on other forms of psychotherapy demonstrates a strong synergistic effect in combination with TMS and pharmacologic treatment for depression (Fava et al., 2004). For example, one study showed that response and remission rates in a patient population receiving rTMS and psychotherapy were higher than those published in other rTMS-only studies (Donse et al., 2018). Targeted PWB therapy may have similar positive effects for patients undergoing rTMS. Indeed, clinical intervention for depression is more effective when PWB is targeted along with targeting symptoms of depression (Moeenizadeh and Salagame, 2010), and identifying those patients with “deficiencies” in their PWB can allow providers to develop personalized treatment approaches to address them.
Evidence suggests that bolstering well-being metrics, such as autonomy and personal growth, may be an achievable goal. In a study that researched residual symptoms of affective disorders, researchers found that well-being therapy had a significant advantage in the reduction of residual symptoms (Fava et al., 1998). Positive psychology interventions can effectively increase PWB and aide in reducing depressive symptoms (Bolier et al., 2013). In a difficult-to-treat depression study, researchers claim that timely consideration of psychotherapy helps optimize results (McAllister-Williams et al., 2020). Thus, by coupling rTMS with well-being therapy, it may be possible to improve response to rTMS treatment, which could be an avenue for future research.
Our work suggests that knowledge about one’s PWB can inform thinking about likelihood of treatment response, and further exploration of this relationship is warranted. At a minimum, this argues for the inclusion of an assessment of PWB in standard psychiatric evaluations - a focus on illness and associated mood symptoms ignores important well-being aspects of a patient’s psychology and thus overall illness experience, such as behavioral strengths and mitigators of psychiatric illness. Despite these intriguing findings, our research found no Ryff domain of PWB significantly predictive of change in PHQ-9 score. Limitations of this study include a modest sample size. Future TMS studies with larger sample sizes, longitudinal follow-up to evaluate relapse rates, and measurement of post-treatment well-being scores could expand upon these findings.
5. Conclusion
Traits of autonomy and personal growth, two components of PWB, could play a significant role in antidepressant response to TMS treatment. Some components of well-being appear to be distinct from and unrelated to depression symptoms, suggesting the relationship between PWB and depression is more complex than purely being opposites along a continuum. Further research is needed to evaluate the effects of TMS on PWB, as these may be distinct from its effect on depression symptomology.
Supplementary Material
Acknowledgements
This research was supported in part by departmental funding from the Department of Psychiatry at the University of Iowa, Iowa City, IA, the INSPIRE Training Grant 5T32MH019113, and NIH-K23MH125145. As well as, the National Institutes of Health Predoctoral Training Grant (T32-GM108540) and the National Science Foundation Graduate Research Fellowship Program Grant (award number: 1546595).
Footnotes
Declaration of interest
None.
Declaration of competing interest
There are no conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2022.03.030.
References
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E, 2013. Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Publ. Health 13, 119. 10.1186/1471-2458-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter LL, Janicak PG, Aaronson ST, Boyadjis T, Brock DG, Cook IA, Dunner DL, Lanocha K, Solvason HB, Demitrack MA, 2012. Transcranial magnetic stimulation (TMS) for major depression: a multisite, naturalistic, observational study of acute treatment outcomes in clinical practice. Depress. Anxiety 29 (7), 587–596. 10.1002/da.21969. [DOI] [PubMed] [Google Scholar]
- Cash R, Cocchi L, Lv J, Fitzgerald PB, Zalesky A, 2021. Functional magnetic resonance imaging-guided personalization of transcranial magnetic stimulation treatment for depression. JAMA Psychiatr. 78 (3), 337–339. 10.1001/jamapsychiatry.2020.3794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coley R, Boggs J, Beck A, Hartzler A, Simon G, 2019. Defining success in measurement-based care for depression: a comparison of common metrics. Psychiatr. Serv. 71 (4), 312–318. 10.1176/appi.ps.201900295. [DOI] [PubMed] [Google Scholar]
- Cusin C, Dougherty DD, 2012. Somatic therapies for treatment-resistant depression: ECT, TMS, VNS, DBS. Biol mood anxiety disord. 10.1186/2F2045-5380-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fava GA, Rafanelli C, Cazzaro M, Conti S, Grandi S, 1998. Well-being therapy. A novel psychotherapeutic approach for residual symptoms of affective disorders. Psychol. Med. 28, 475–480. 10.1017/s0033291797006363, 02. [DOI] [PubMed] [Google Scholar]
- Fava GA, Ruini C, Rafanelli C, Finos L, Conti S, Grandi S, 2004. Six-year outcome of cognitive behavior therapy for prevention of recurrent depression. Am. J. Psychiatr. 161 (10), 1872–1876. 10.1176/ajp.161.10.1872, 2004. [DOI] [PubMed] [Google Scholar]
- Fitzgerald PB, Hoy KE, Anderson RJ, Daskalakis ZJ, 2016. A study of the pattern of response to rTMS treatment in depression. Depress. Anxiety 33 (8), 746–753. 10.1002/da.22503. [DOI] [PubMed] [Google Scholar]
- Kar SK, 2019. Predictors of response to repetitive transcranial magnetic stimulation in depression: a review of recent updates. Clinical psychopharmacology and neuroscience: the official scientific journal of the Korean College of Neuropsychopharmacology 17 (1), 25–33. 10.9758/cpn.2019.17.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes CL, 2005. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J. Consult. Clin. Psychol. 73 (3), 539. 10.1037/0022-006x.73.3.539. [DOI] [PubMed] [Google Scholar]
- Keyes CL, Dhingra SS, Simoes EJ, 2010. Change in level of positive mental health as a predictor of future risk of mental illness. AJPH (Am. J. Public Health) 100 (12), 2366–2371. 10.2105/2FAJPH.2010.192245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krepel N, Rush AJ, Iseger TA, Sack AT, Arns M, 2020. Can psychological features predict antidepressant response to rTMS? A discovery-replication approach. Psychol. Med. 50, 264–272. 10.1017/S0033291718004191, 2020. [DOI] [PubMed] [Google Scholar]
- Lamers SM, Westerhof GJ, Glas CA, Bohlmeijer ET, 2015. The bidirectional relation between positive mental health and psychopathology in a longitudinal representative panel study. J. Posit. Psychol. 10 (6), 553–560. 10.1080/17439760.2015.1015156. [DOI] [Google Scholar]
- Mann FD, DeYoung CG, Krueger RF, 2021. Patterns of cumulative continuity and maturity in personality and well-being: evidence from a large longitudinal sample of adults. Pers. Indiv. Differ. 169, 109737. 10.1016/j.paid.2019.109737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhi GS, Mann JJ, 2018. Depression. Lancet (London, England: ) 392 (10161), 2299–2312. 10.1016/S0140-6736(18)31948-2. [DOI] [PubMed] [Google Scholar]
- McAllister-Williams RH, Arango C, Blier P, Demyttenaere K, Falkai P, Gorwood P, Hopwood M, Javed A, Kasper S, Malhi GS, Soares JC, Vieta E, Young AH, Papadopoulos A, Rush AJ, 2020. The identification, assessment and management of difficult-to-treat depression: an international consensus statement. J. Affect. Disord. 267, 264–282. 10.1016/j.jad.2020.02.023. [DOI] [PubMed] [Google Scholar]
- Moeenizadeh M, Salagame KKK, 2010. The impact of well-being therapy on symptoms of depression. Int. J. Psychol. Stud. 2 (2), 223–230. 10.5539/ijps.v2n2p223, 2010. [DOI] [Google Scholar]
- Paus T, Barrett J, 2004. Transcranial magnetic stimulation (TMS) of the human frontal cortex: implications for repetitive TMS treatment of depression. J. Psychiatry Neurosci. 268–279. http://www.ncbi.nlm.nih.gov/pmc/articles/pmc446221/. [PMC free article] [PubMed] [Google Scholar]
- Perera T, George MS, Grammer G, Janicak PG, Pascual-Leone A, Wirecki TS, 2016. The clinical TMS society consensus review and treatment recommendations for TMS therapy for major depressive disorder. Brain stimulation 9 (3), 336–346. 10.1016/j.brs.2016.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rafanelli C, Park SK, Ruini C, Ottolini F, Cazzaro M, Fava GA, 2000. Rating well-being and distress. Stress Med. . [DOI] [Google Scholar]
- Ruini C, Ottolini F, Rafanelli C, Tossani E, Ryff CD, Fava GA, 2003. The relationship of PWB to distress and personality. Psychother. Psychosom. 72 (5), 268–275. 10.1159/000071898. [DOI] [PubMed] [Google Scholar]
- Ruini C, Albieri E, Vescovelli F, 2015. Well-being therapy: state of the art and clinical exemplifications. J. Contemp. Psychother. 45, 129–136. 10.1007/s10879-014-9290-z. [DOI] [Google Scholar]
- Ruini C, Cesetti G, 2019. Spotlight on eudaimonia and depression. A systematic review of the literature over the past 5 years. Psychol. Res. Behav. Manag. 12, 767–792. 10.2147/PRBM.S178255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, Niederehe G, Thase ME, Lavori PW, Lebowitz BD, McGrath PJ, Rosenbaum JF, Sackeim HA, Kupfer DJ, Luther J, Fava M, 2006. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am. J. Psychiatr. 163 (11), 1905–1917. 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Huta V, 2009. Wellness as Healthy Functioning or Wellness as Happiness: the Importance of Eudaimonic Thinking (response to the Kashdan et al. and Waterman discussion). J. Posit. Psychol. 4 (3), 202–204. 10.1080/17439760902844285. [DOI] [Google Scholar]
- Ryff CD, 1989. Happiness is everything, or is it? Explorations on the meaning of pyschological well-being. J. Pers. Soc. Psychol. 57 (6), 1069–1081. 10.1037/0022-3514.57.6.1069. [DOI] [Google Scholar]
- Ryff CD, Radler BT, Friedman EM, 2015. Persistent psychological well-being predicts improved self-rated health over 9–10 years: longitudinal evidence from MIDUS. Health Psychology Open. 10.1177/2F2055102915601582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqi SH, Chockalingam R, Cloninger CR, Lenze EJ, Cristancho P, 2016. Use of the temperament and character inventory to predict response to repetitive transcranial magnetic stimulation for major depression. J. Psychiatr. Pract. 22 (3), 193–202. 10.1097/pra.0000000000000150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Deaton A, Stone AA, 2015. Subjective wellbeing, health, and aging. Lancet 385 (9968), 640–648. 10.1016/S0140-6736(13)61489-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trompetter H, Lamers S, Westerhof GJ, Fledderus M, Bohlmeijer ET, 2017. Both positive mental health and psychopathology should Be monitored in psychotherapy: confirmation for the dual-factor model in acceptance and commitment therapy. Behav. Res. Ther. 91, 58–63. 10.1016/j.brat.2017.01.008. [DOI] [PubMed] [Google Scholar]
- Westerhof GJ, Keyes CLM, 2010. Mental illness and mental health: the two continua model across the lifespan. J. Adult Dev. 17 (2), 110–119. 10.1007/s10804-009-9082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood AM, Joseph S, 2010. The absence of positive psychological (eudemonic) well-being as a risk factor for depression: a ten-year cohort study. J. Affect. Disord. 122 (3), 213–217. 10.1016/j.jad.2009.06.032. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.