Abstract
Borderline personality disorder (BPD) confers risk for cardiovascular disease (CVD). The present study used the interpersonal perspective to investigate potential mechanisms underlying this association. In two undergraduate samples (N = 293; N = 188) in Study 1, we replicated and extended research by demonstrating that BPD features were associated with hostile and somewhat submissive interpersonal behavior. Further, BPD features were associated with low social support and high levels of interpersonal conflict, two well-established risk factors for CVD. Also, hostile-submissive behavior contributed to the association of BPD features with low social support. In Study 2, we examined associations of BPD features with blood pressure (BP) responses to two interpersonal stressors implicated in models of the effects of stress on CVD, specifically by using laboratory tasks involving interpersonal conflict and evaluative threat in a third undergraduate sample (N = 143). BPD features predicted elevated BP reactivity to conflict but not evaluative threat, and such heightened reactivity previously has been found to predict the development of CVD. The interpersonal perspective may be useful for investigating mechanisms linking BPD to CVD risk, and processes that undermine otherwise protective social support or heighten exposure and reactivity to interpersonal conflict may be relevant in this regard.
Keywords: borderline personality disorder, psychosocial risk, cardiovascular disease, interpersonal perspective, social-evaluative threat, psychopathology
1. Introduction
Personality traits such as negative affectivity and antagonism predict the development of cardiovascular disease (CVD) (Chida & Steptoe, 2009; Smith, Baron, & Grove, 2014; Smith, Glazer, Ruiz, & Gallo, 2004; Suls & Bunde, 2005). Most research examines normal personality, but personality disorders also predict health outcomes, including CVD (Björkenstam, Björkenstam, Holm, Gerdin, & Ekselius, 2015; El-Gabalawy, Katz, & Sareen, 2010; Grant et al., 2008, Quirk et al., 2014). Current models emphasize continuity between normal personality and personality pathology (Widiger, 2011), suggesting that personality disorders are best understood as extremes of social and emotional tendencies rather than discrete classes (Samuel, Carroll, Rounsaville, & Ball, 2013). Thus, personality risk factors for CVD could be conceptualized along a continuum, with perhaps the greatest risk being associated with personality disorders.
Some evidence suggests that borderline personality disorder (BPD) is a risk factor for physical illness, including CVD (El-Gabalawy et al., 2010; Lee et al., 2010; Moran et al., 2007). BPD is a severe and pervasive disorder marked by multiple problematic characteristics, several of which could contribute to elevated risk for CVD. For example, borderline personality features such as impulsivity predict obesity (Powers & Oltmanns, 2013), a well-established risk factor for CVD (Bastien, Poirier, Lemieux, & Després, 2014). However, despite the growing interest in the health consequences of BPD, possible psychosocial mechanisms in the association of BPD with CVD are not well-studied.
In models of psychosocial risk for CVD, individual-level characteristics such as personality traits and disorders are believed to influence pathophysiology through recurrent stress processes, specifically through 1) heightened exposure to stressors (e.g., interpersonal conflict) and reduced levels of protective experiences and resources (e.g., social support), 2) excessive psychophysiological reactivity to stressors and reduced physiologic benefit from protective experiences when they do occur, 3) delayed physiologic recovery from episodes of stress, and 4) poor restoration of physiological functioning (Williams, Smith, Gunn, & Uchino, 2010). Notably, BPD has been linked with heightened stress exposure and reduced levels of protective factors, in the form of related interpersonal difficulties (Ross & Babcock, 2009; Whisman & Schonbrun, 2009). Further, BPD is associated with difficulties regulating intense negative emotions (Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2006) and, although findings are somewhat mixed, research suggests BPD may also be related to heightened physiological reactivity to stressors (Austin & Porges, 2007; Cavazzi & Becerra, 2014; Ebner-Priemer et al., 2007). Finally, poor sleep quality is common among individuals with BPD (Grove, Smith, Crowell, & Ellis, in press; Selby, 2013), and disruption of this key restorative process increases risk for CVD (King et al., 2008).
1.1. The Interpersonal Perspective on Psychosocial Risk for Cardiovascular Disease
The interpersonal perspective in personality, clinical and social psychology (Horowitz & Strack, 2011; Pincus & Ansell, 2013) provides an integrative framework for the study of psychosocial risk for CVD (Smith & Cundiff, 2011; Smith et al., 2004; 2014). In this model, aspects of the individual (e.g., trait negative emotionality) and the social environment (e.g., isolation, low support, interpersonal conflict) are not separate classes of influences on CVD, but instead are related through interpersonal processes that confer risk (Gallo & Smith, 1999). Specifically, in this view individuals influence – and are influenced by — their social contexts through transactional processes. An individual’s internal processes (e.g. affect, appraisals, motives) influence his or her overt interpersonal behavior (e.g. hostility, warmth), which in turn constrains the reactions of interaction partners. Over time, these responses from others tend to maintain the initial actor’s internal experience and overt behavior, and foster stable patterns of interpersonal experiences and relationships. In the case of personality risk factors for CVD (e.g., negative affectivity, antagonism), these transactional processes result in recurring patterns of adverse interpersonal experience (i.e., high conflict, low support) and physiological responses to those experiences that over time hasten the progression of CVD through the stress mechanisms described previously (Smith et al., 2010; 2014).
In interpersonal theory, these patterns are described in the interpersonal circumplex (IPC) (Horowitz et al., 2006; Pincus & Ansel, 2013, Wiggins, 1979), comprising two orthogonal dimensions of affiliation (e.g. warmth vs. hostility) and control (dominance vs. submissiveness). The IPC describes momentary behavior, but also more enduring characteristics, such as personality traits and aspects of social context (Gurtman, 1992). The complementarity principle –a central tenet of interpersonal theory –states that an individual’s interpersonal behavior invites responses from others that are similar in affiliation but opposite in control (Pincus & Ansell, 2013). Related research supports this prediction for affiliation (i.e., warmth evokes warmth in return; hostility evokes hostile responses), but dominant behavior is often met with dominance in return, rather than the predicted submissiveness (e.g., Cundiff, Smith, Butner, Critchfield, & Nealey-Moore, 2015). Thus, this framework provides a common description of risk factors that emphasize aspects of the individual (e.g., personality traits, emotional adjustment), the social context, and associations between these domains (Gallo & Smith, 1999; Smith et al., 2014).
Interpersonal traits or behavioral styles associated with psychosocial risk factors can be determined by their associations with IPC-based measures of personality (Gurtman, 1992), and the complementarity principle then provides a prediction regarding related interpersonal experiences. For example, psychosocial characteristics associated with a hostile interpersonal style would be expected to be associated with low levels of social support and high levels of conflict (Gallo & Smith, 1999; Gallo, Smith, & Ruiz, 2003). These recurring interpersonal processes, in turn, can influence CVD through stress responses (i.e. heightened exposure and reactivity, and impaired recovery and restoration) (Smith et al., 2014; 2004).
The interpersonal perspective is clearly applicable to examining BPD as a CVD risk factor. Individuals with BPD display several maladaptive internal processes, including negative affect, emotion dysregulation, appraisals of others as hostile, and poor inhibition of angry impulses (Gratz et al., 2006; Linehan, 1993; Sadikaj, Moskowitz, Russell, Zuroff, & Paris, 2013). These processes promote problematic overt interpersonal behavior common among these individuals, such as hostility towards others and conflict escalation (Crowell, Beauchaine, & Linehan, 2009; Gunderson, 2007). Through the transactional processes described previously, these patterns likely reduce social support and increase exposure to interpersonal conflict. The effects of these stress exposures may be particularly unhealthy if BPD is also associated with excessive physiological responses to such stressors, resulting in greater cumulative physiological activation.
The present studies are an initial attempt to apply this perspective on psychosocial risk for CVD to BPD. The objective of Study 1 was to replicate prior research using the IPC to describe the interpersonal style associated with BPD (e.g., Pincus & Wiggins, 1990; Wright et al., 2013), and to examine the relation between BPD features and interpersonal processes associated with CVD. That is, Study 1 examined exposure to interpersonal sources of risk (i.e., high conflict and low social support). In Study 2 we examined associations between BPD features and stress reactivity, specifically cardiovascular responses to social stressors. Notably, our samples are comprised of young adult undergraduate students, a population that is decades younger than the typical age for the clinical appearance of CVD. However, the atherosclerotic process underlying CVD begins as early as later childhood and adolescence (McGill, McMahon, & Gidding, 2008). Further, psychosocial risk factors and cardiovascular reactivity in young adulthood predict progression of this disease process and later manifestations of CVD (Chida & Steptoe, 2010; Smith & Cundiff, 2011). Thus, examination psychosocial and psychophysiological processes in this age range is relevant in efforts to explicate associations of BPD symptoms with CVD risk.
2. Study 1: Interpersonal Style and Consequences Related to BPD
In studies using IPC assessments of interpersonal style, BPD is generally associated with low warmth or high hostility, although results are somewhat inconsistent, perhaps due to variability across subtypes of individuals with BPD or instability in their interpersonal behavior (Hopwood et al., 2009; Russell, Moskowitz, Zuroff, Sookman, & Paris, 2007; Sadikaj et al., 2013; Wright et al., 2013; Wright et al., 2012). BPD is sometimes associated with a more submissive style (Russell et al., 2007), but findings regarding this IPC dimension are inconsistent. BPD is a highly heterogeneous diagnosis (American Psychiatric Associaion, 2013), and interpersonal behavior in BPD may be largely dependent on the constellation of symptoms for a given person (Wright et al., 2013). Further, mean-level estimates of interpersonal style might not be representative of the actual interpersonal behavior in this population (Hopwood et al., 2009). Nonetheless, interpersonal style can be useful for describing general patterns of behavior that in turn predict specific outcomes (Pincus & Ansel, 2013), such as stress exposure and CVD (Smith et al., 2004; 2014).
To our knowledge, few studies have examined interpersonal style as a mechanism linking BPD symptoms to social outcomes related to CVD risk, such as low support and high conflict. Hence, this study sought to determine the interpersonal style associated with two measures of BPD symptoms, and test this style as a mechanism linking BPD symptoms to lower social support and higher interpersonal conflict. We hypothesized that: a) BPD symptoms would relate to a hostile-submissive interpersonal style, b) that BPD symptoms would be associated with lower social support and higher interpersonal conflict, and c) that these latter associations would involve indirect effects of interpersonal style.
2.1 Method
2.1.1. Participants
Two samples of undergraduate students from a public university received course credit (Sample 1: N = 293, 65% Female; Sample 2: N = 188, 63% Female). Across both samples the mean age was approximately 23 years, and 70% of the participants identified as Caucasian, 11% Asian/Pacific Islander, and 7% Hispanic.
2.1.2. Measures and Procedures
Participants completed self-report measures in small groups in a computer lab, monitored by research assistants. Surveys included measures of BPD features, interpersonal style (Samples 1 and 2), and interpersonal outcomes (i.e., social support and interpersonal conflict) (Sample 1).
2.1.2.1. BPD Features
Both samples completed the Borderline Symptom List-23 (BSL-23; Bohus et al., 2008), a widely used self-report measure of symptoms experienced during the prior two-weeks. This measure displays adequate internal consistency (alphas ranging from .75 to .90). In addition, both samples completed the Five-Factor Borderline Inventory (FFBI; Mullins-Sweatt et al., 2012). This measure consists of twelve subscales for maladaptive traits related to BPD, such as anxiety, anger, despondency, self-disturbance, behavioral dysregulation, affect dysregulation, oppositional, rashness, manipulative, dissociative, distrusting, and fragility. This measure displays good psychometric properties, consistent with adequate internal consistency (most subscales > .65) and good convergent validity based on its association with established BPD scales (Mullins-Sweatt et al., 2012). The present study examined the interpersonal correlates of the total BPD symptom score on the FFBI as well as each of its 12 subscales.
2.1.2.2. Interpersonal Style
Both samples completed the Interpersonal Adjectives Scales (IAS-R; Wiggins et al., 1988), a 64-item measure that yields scores for the two IPC dimensions (affiliation and control) with good reliability of the circumplex structure and construct validity.
2.1.2.3. Interpersonal Outcomes
The Test for Negative Social Exchanges Scale (TENSE; Ruehlman & Karoly, 1991) measures the extent to which an individual experienced negative social interactions, such as conflict or rejection, over the prior month. The Interpersonal Support Evaluation List (ISEL; Cohen, Mermelstein, Kamarck, & Hoberman, 1985) is a 12-item, widely used measure of general social support. Both measures have good psychometric properties in studies of CVD risk (e.g., Smith, Ruiz, Cundiff, Baron, & Nealey-Moore, 2013).
2.1.3. Data Analytic Plan
To examine the interpersonal style associated with BPD, we regressed measures of BPD features on the two dimensions of the IPC. The multiple-R indicates the extent to which a characteristic is related to interpersonal behavior. The individual coefficients for affiliation and control can be used to describe that style. Specifically, the angular displacement of the target scale within the IPC (Warm pole = 0°; dominance = 90°; hostility = 180°; submissiveness = 270°) can be calculated (Gurtman, 1992). To examine pathways linking BPD features to interpersonal outcomes, we utilized SEM to test direct associations between BPD symptoms and interpersonal stress exposure (i.e. social support, conflict), and indirect effects of BPD symptoms predicting these variables through interpersonal style (i.e. dominance vs. submissiveness; warmth vs. hostility). Although conceptually related to meditational effects of interpersonal style in the association of BPD features with social support and conflict, the cross-sectional design severely limits conclusions regarding mediation, per se (Maxwell & Cole, 2007). Given the non-normality of the variables in the analysis, we used bootstrapping procedures to generate model estimates.
2.2. Results
2.2.1. Correlations among Study Variables
As seen in Table 1, the BPD symptom scales were highly correlated, and these convergent associations were significantly larger than correlations of the BPD symptoms scales with all other variables, sample 1: all Z(293) > 5.0, p<.001; sample 2: all Z(188) > 3.5, p<.001, supporting the convergent and discriminant validity of the BPD symptom scales. Also, as expected, both BPD symptom measures were positively associated with interpersonal conflict and inversely associated with social support.
Table 1.
Intercorrelations, means, and reliability of variables in Sample 1.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. BSL23 | - | |||||
| 2. FFBI total | .71** | - | ||||
| 3. IAS-Submissiveness | .22** | .15* | - | |||
| 4. IAS-Hostility | .14* | .33** | .11 | - | ||
| 5. TENSE | .35** | .44** | −.09 | .13* | - | |
| 6. ISEL | −.34** | −.43** | −.39** | −.31** | −.12* | - |
|
| ||||||
| Mean (SD) | .72 (.69) | 289.30 (80.14) | .39 (.55)a | .83 (.52)b | 36.80 (9.92) | 27.65 (6.83) |
| α | .94 | .97 | .91 | .91 | .87 | .97 |
p < .05,
< .01, two-tailed.
IAS Dom (inverse of submissiveness).
IAS Lov (inverse of hostility).
Note: BSL-23=Borderline Symptom List, FFBI=Five Factor Borderline Inventory, IAS=Interpersonal Adjectives Scale, TENSE=Test for Negative Social Exchanges, ISEL=Interpersonal Support Evaluation List.
2.2.2. BPD symptoms and Interpersonal Style
BPD symptoms were inversely related to both warmth and dominance, for both the BSL-23 and the FFBI (see Table 2). Angular displacements indicated that BSL-23 scores were associated with a hostile interpersonal style (Sample 1 = 200.6°, Sample 2 = 196.8°), albeit with a significant association with submissiveness. The angular displacement of the FFBI indicated a hostile-submissive style (Sample 1 = 240.4°, Sample 2 = 235.9°). Comparisons of the multiple R values suggested that FFBI had somewhat stronger interpersonal content than the BSL-23, although both were highly significant.
Table 2.
Intercorrelations, descriptives, and reliability of variables in Sample 2.
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. BSL-23 | - | |||
| 2. FFBI total | .68** | - | ||
| 3. IAS-Submissiveness | .18* | .31** | - | |
| 4. IAS-Hostility | .44** | .23** | .11 | - |
|
| ||||
| Mean (SD) | .74 (.69) | 285.93 (75.38) | .47 (.50)a | .81 (.49)b |
| α | .95 | .97 | .89 | .90 |
p < .05,
< .01, two-tailed.
IAS Dom (inverse of submissiveness).
IAS Lov (inverse of hostility).
Note: BSL-23=Borderline Symptom List, FFBI=Five Factor Borderline Inventory, IAS=Interpersonal Adjectives Scale
Additionally, multiple R values for each of the FFBI subscales revealed that all 12 factors of BPD were inversely related to warmth. However, there was variability with regard to the control dimension. Several features significantly related to submissiveness, but others were unrelated to this IPC dimension and both manipulativeness and oppositionality were positively related to both dominance and hostility (see Table 4).
Table 4.
Multiple squared R values for the 12 Five Factor Borderline Inventory subscales and the two domains of the IPC for Study 1.
| FFBI Subscale | Sample | M (SD) | α | R | R2 | F | Affiliation β | Control β |
|---|---|---|---|---|---|---|---|---|
| Anxious Uncertainty | 1 | 30.22 (9.42) | .87 | .25 | .06 | 9.82*** | −.08 | −.23*** |
| 2 | 29.44 (9.25) | .87 | .29 | .08 | 8.66*** | −.21** | −.18* | |
| Anger | 1 | 24.13 (8.89) | .87 | .29 | .08 | 12.80*** | −.29*** | .06 |
| 2 | 23.99 (8.42) | .87 | .40 | .16 | 18.21*** | −.41*** | .03 | |
| Affect Instability | 1 | 22.75 (9.40) | .91 | .27 | .08 | 11.69*** | −.20** | −.17** |
| 2 | 22.02 (8.85) | .91 | .40 | .16 | 17.94*** | −.34*** | −.19** | |
| Behavior Dysregulation | 1 | 23.99 (7.89) | .82 | .23 | .05 | 7.69** | −.22*** | −.03 |
| 2 | 23.93 (7.06) | .81 | .34 | .12 | 12.01*** | −.33*** | −.05 | |
| Despondency | 1 | 26.29 (10.24) | .91 | .35 | .13 | 20.60*** | −.18** | −.29** |
| 2 | 26.13 (9.11) | .86 | .39 | .15 | 16.97*** | −.24*** | −.29*** | |
| Dissociative Tendencies | 1 | 26.28 (8.17) | .83 | .31 | .09 | 15.14*** | −.26*** | −.14* |
| 2 | 26.31 (8.02) | .83 | .29 | .08 | 8.17*** | −.25*** | −.11 | |
| Distrust | 1 | 25.59 (8.92) | .86 | .34 | .11 | 18.58*** | −.32*** | −.07 |
| 2 | 25.61 (8.63) | .85 | .37 | .14 | 14.83*** | −.37*** | −.04 | |
| Fragility | 1 | 21.51 (7.87) | .82 | .28 | .08 | 11.97*** | −.14* | −.23*** |
| 2 | 20.31 (7.31) | .81 | .41 | .17 | 19.11*** | −.27*** | −.29*** | |
| Manipulative | 1 | 20.15 (7.49) | .83 | .44 | .20 | 35.13*** | −.43*** | .15* |
| 2 | 19.89 (7.18) | .83 | .53 | .29 | 36.99*** | −.53*** | .16* | |
| Oppositional | 1 | 20.69 (6.35) | .74 | .58 | .33 | 72.60*** | −.55*** | .25*** |
| 2 | 21.16 (6.49) | .75 | .59 | .35 | 48.67*** | −.58*** | .19** | |
| Rashness | 1 | 21.25 (8.28) | .86 | .21 | .05 | 6.79* | −.21*** | .06 |
| 2 | 21.78 (7.42) | .81 | .26 | .07 | 6.85** | −.26*** | .03 | |
| Self- Disturbance | 1 | 26.41 (10.11) | .90 | .42 | .18 | 30.79*** | −.24*** | −.32*** |
| 2 | 25.32 (9.94) | .90 | .45 | .20 | 22.93*** | −.26*** | −.34*** |
p < .05,
< .01,
< .001
2.2.3. Interpersonal pathways to stress exposure
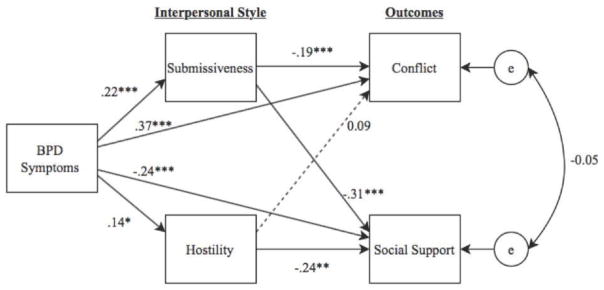
Using SEM, we tested the BSL-23 and the FFBI as predictors in separate models. Path analysis results were consistent across these measures. The BSL-23 model demonstrated a somewhat better fit and therefore is reported in detail (see Figure 1). Overall fit was acceptable, χ2 = 165.05, df = 10, p < .01; CFI = 0.99, TLI = 0.93; RMSEA = 0.06. In a significant direct effect (β;= −.24, SE = .06, p < .001), greater severity of BPD symptoms related to lower perceived social support. Further, the indirect effects of interpersonal behavior were significant in the relationship between BPD symptoms and low social support, for both submissiveness (point estimate = −.66, SE = .19, p = .001) and hostility (point estimate = −.33, SE = .16, p < .05).
Figure 1.
SEM model of associations between BPD, interpersonal style, and outcomes related to social stress exposure. Paths are denoted with standardized regression coefficients. Non-significant paths are represented by dotted lines. Coefficient signs were reversed for interpersonal style for clarity of interpretation. *p < .05, **p < .01, *** p < .001.
Similar SEM analyses with the TENSE indicated a direct effect in which higher BPD symptoms were associated with greater conflict (β = .37, SE = .05, p < .001). Further, there was a significant indirect effect for BPD via submissiveness (point estimate = −.60, SE = .19, p < .01), but in the opposite direction than predicted. That is, the submissive behavior related to BPD symptoms was inversely related to conflict. The effect involving the affiliation dimension in this association was not significant (point estimate = −.19, SE = .14, p = .18).
2.3. Discussion
As predicted, BPD features were generally associated with a hostile and submissive interpersonal style. However, further examination of the individual FFBI subscales revealed some variability in associations with the control dimension; across the various BPD component scales the associated interpersonal styles ranged from hostile submissiveness to hostile dominance. These findings provide additional evidence that interpersonal subtypes might exist in BPD (Wright et al., 2013), and indicate that our results linking overall BPD symptoms to submissiveness should be interpreted with caution. Future research should examine the extent to which such interpersonal subtypes of BPD might confer the greatest long-term risk for CVD and other chronic illnesses.
As predicted, BPD features were also associated with low levels of social support and high levels of interpersonal conflict, both of which are well-established risk factors for CVD. Further, hostile and submissive interpersonal behavior had significant indirect effects in the association between BPD symptoms and low social support. Hence, the results provide partial support for interpersonal models in which interpersonal style contributes to the association of individual-level CVD risk factors and risk factors traditionally seen as reflecting the social environment.
These findings involving BPD symptoms, interpersonal style, and low social support are not surprising, given that hostility is consistently associated with low support (Gallo & Smith, 1999; Smith et al., 2004). However, the lack of a similar role for hostile interpersonal style in the association between BPD features and conflict was unexpected, given that hostility in BPD has been consistently associated with negative social interactions (Russell et al., 2007; Sadikaj et al., 2013). Also surprising was the association between BPD features, submissive behavior, and lower conflict. Heightened sensitivity to rejection and criticism is linked with interpersonal dysfunction in BPD (Berenson, Downey, Rafaeli, Coifman, & Paquin, 2011; Gunderson, 2007). It is possible that submissive interpersonal behavior in BPD represents an effort to avoid rejection and criticism, which would otherwise be a source of conflict for these individuals (Chapman, Walters, & Gordon, 2014). Thus, individuals with elevated BPD features who are more successful in avoiding criticism and rejection through submissiveness may experience less interpersonal conflict, but perhaps at the cost of undermining potential social support. Additional research should examine interpersonal processes which might contribute to the association of BPD symptoms with heightened exposure to interpersonal conflict.
Overall, however, BPD symptoms appear to be associated with interpersonal processes and aspects of the social environment known to contribute to CVD risk (Smith et al., 2004; 2014). The general association of BPD symptoms with a hostile and to some extent submissive interpersonal style suggests a potentially important parallel with other well-established individual-level psychosocial risk factors for CVD, such as hostility, depression, anxiety, and pessimism (Gallo & Smith, 1998; Smith et al., 2010; Smith et al., 2013). This interpersonal style could represent a core element of vulnerability for several conceptually distinct psychosocial risk factors involving negative emotionality and problematic social behavior.
3. Study 2: BPD Features and Cardiovascular Reactivity to Social Stressors
Heightened cardiovascular reactivity (CVR; e.g., increases in blood pressure in response to stressors) and delayed recovery of these responses predict the development of CVD (Chida & Steptoe, 2010), and are hypothesized to contribute to the association of psychosocial risk factors with CVD. Hence, the association of BPD symptoms with these physiological responses is of considerable interest. In the interpersonal perspective, CVR in response to common social stressors is important in this regard (Smith et al., 2003; 2011).
Several social stressors may be particularly relevant in the association of BPD with CVR and ultimately CVD. Antagonistic or hostile interactions with others evoke substantial CVR (Gallo, Smith, & Kircher, 2000; Nealey-Moore et al., 2007; Smith et al., 2003, 2004), and individuals with high levels of BPD symptoms have greater exposure to such interpersonal stressors (Gunderson et al., 2011). However, the association between BPD features with CVR during controlled laboratory stressors involving interpersonal conflict has not been examined previously. Yet, prior work has indicated that several characteristics related to BPD (e.g., trait hostility, antagonism) are significant predictors for heightened subjective and physiological reactivity to conflict-related interpersonal stressors (Chu, Ma, Li, & Han, 2015; Smith & Gallo, 1999). Thus, we expect BPD symptoms to yield similar findings.
Social-evaluative threat (SET) may be another type of interpersonal stressor pertinent to BPD features. SETs occur when a valued aspect of the individual’s self-image or identity could be judged negatively, consistently evoking substantial physiological responses that relate to CVD (Dickerson & Kemeny, 2004; Smith & Jordan, 2015). BPD is associated with heightened sensitivity to real or imagined negative evaluations, rejection or abandonment (Berenson et al., , 2011). Thus, SET may also be important in understanding interpersonal risk for CVD associated with BPD. However, studies of the association of BPD with physiological responses to social-evaluative threat have been inconsistent to date (Chapman et al., 2014; Scott, Levy, & Granger, 2013). Further, no studies of this type have examined blood pressure reactivity, a particularly important response in the prediction of CVD (Chida & Steptoe, 2010).
In the current study, we conducted additional analyses of a prior study of social stress and physiological stress responses (Smith & Jordan, 2015). Specifically, we extend the prior report by testing associations of BPD features with systolic and diastolic blood pressure (SBP, DBP) responses to a laboratory task that presented two types of interpersonal stressors. The first involved social-evaluative threat. Participants in high threat conditions were told that raters would evaluate them on characteristics related to acceptance (e.g., likelihood of social inclusion) and/or status (e.g., competence). In the second stressor involving interpersonal conflict, all participants engaged in a role-played interpersonal exchange with a hostile partner.
As noted previously, our sample is comprised of undergraduates, who are decades younger than the usual age for the clinical emergence of CVD. However, early manifestations of the atherosclerosis underlying CVD often first appear in childhood and adolescence (McGill et al., 2008), and BP reactivity to stressors measured in young adulthood predicts progression of atherosclerosis and subsequent CVD (Chida & Steptoe, 2010). For example, BP responses of young adults to laboratory stress tasks predict atherosclerosis more than a decade following the initial assessment (Matthews, Zhu, Tucker, & Whooley, 2006). Thus, examining CVR in this age range is relevant in efforts to explicate associations of BPD symptoms with CVD risk.
Overall, we hypothesized that BPD symptoms would be positively associated with blood pressure responses to interpersonal stressors. Specifically, we predicted that BPD symptoms a) would be generally associated with greater CVR during the hostile interaction task (i.e., conflict stressor), and b) would moderate the effects on CVR of the experimental manipulation of social-evaluative threat, such that individuals endorsing higher levels of BPD symptoms would be more responsive to the threat manipulation. We examined both SBP and DBP reactivity, given that they are often influenced by distinct psychological processes. For example, DBP reactivity often reflects the experience of threat, whereas SBP reactivity often reflects challenge and task engagement (Seery, 2011). We examined these associations both while participants were silent and while speaking, to determine the possible contribution of speech artifacts. We also examined the association of BPD symptoms with self-reported affective responses during and after the tasks, and with self-reported rumination during recovery.
3.1. Method
3.1.1. Participants
The present sample included 143 undergraduates (74 females; 70% Caucasian; M age = 23.2 years, SD = 5.1) enrolled in the psychology subject pool at a public university. Participants were asked to refrain from caffeine consumption or nicotine use for 2 hours prior to the study. Further, participants taking medications that alter cardiac activity were excluded.
3.1.2. Materials
3.1.2.1. Self-reports
BPD symptoms were assessed using the BSL-23, described previously. State anger and anxiety were measured using 4-point Likert items from the Spielberger State Trait Anger and Anxiety Inventories (Spielberger, Jacobs, Russell, & Crane, 1983). Both measures display good internal consistency, each ranging from .75 to .90. State shame, or self-conscious emotions (SCE), was measured using a 10-item scale (4-point Likert) reflecting shame-like affect (Dickerson, Mycek, & Zaldivar, 2008) and has yielded adequate internal consistency (α ranging from .80 to .93). Rumination was assessed using 10 items (5-point Likert scale) from the Rumination-Reflection Questionnaire (RRQ; Trapnell & Campbell, 1999). The wording was altered to assess the degree to which individuals ruminated about the experimental task just completed (e.g. “My thoughts keep going back to the tasks”).
3.1.2.2. Cardiovascular response
A Dinamap Model 100 was used to measure systolic (SBP) and diastolic blood pressure (DBP). The Dinamap uses the occillometric method to calculate blood pressure. Average values for SBP and DBP were calculated for baseline, initial task, role play speaking, and role play listening periods. Specifically, three measures consisting of 90-second intervals near the end of the baseline period were averaged. One BP measurement was taken for each of the 90 second speaking and listening portions of the experimental task. Finally, three measurements were recorded and averaged during the post-task recovery period.
3.1.3. Design and Procedure
The design and procedure for this study are described in detail elsewhere (Smith & Jordan, 2015) and will be described briefly here. Participants were randomly assigned to one of four evaluative threat conditions. Hence, the design was a 2 (high vs. low Acceptance Threat) × 2 (high vs. low Status threat) × 2 (Gender) factorial. Prior to the experimental task, participants completed a pre-task questionnaire that assessed demographics and BPD symptoms.
3.1.3.1. Baseline period and initial experimental tasks
After a 10-minute baseline, pre-recorded audio instructions informed participants that the study concerned cardiovascular effects of social interaction, and they would provide verbal responses to social tasks. The initial task required them to respond to two different prompts about their personal qualities (e.g. long-term career interests). The participants were asked to speak for a full 90 seconds for each prompt while blood pressure was recorded for each 90-second speaking interval. The evaluative threat manipulation (described below) was delivered immediately after the basic task instructions.
3.1.3.2. Simulated interpersonal task and recovery period
Upon completion of the initial experimental tasks, a recording instructed the participants to imagine a situation in which they were involved in a minor car accident and required to interact with a passenger in the other car. The participants were asked to role-play this interaction by listening and responding to pre-recorded remarks by that passenger for two cycles, each consisting of two 90-second intervals of listening and then responding to the pre-recorded partner. A blood pressure reading was taken for each 90-second listening and speaking interval. The pre-recorded remarks of partner emphasized verbal content and vocal expression directed toward the participants that was hostile, abrasive, and accusatory. After the task, the participants again completed state-affect measures, about how they felt during the task. Cardiovascular measures were taken for five minutes during recovery, and then participants completed a final set of questionnaires about state affect and rumination.
3.1.3.3. Evaluative threat manipulation
Men and women were block-randomized to one of four conditions: (1) experimental control (i.e., low threat), (2) high Acceptance threat, (3) high Status threat, and (4) combination of high Status and Acceptance threat. For the three threat conditions, two confederates were placed in the experimental chamber with the participant during each of the experimental tasks. The confederates were instructed to make gestures of rating the participant at various times while the participant spoke (e.g. making markings on a paper). Participants in threat conditions were told that raters would use their task responses to rate them on qualities related to social acceptance (e.g. likeability, friendliness), status (e.g. intelligence, competency), or a combination of the two. Participants in the low threat condition were assured they would not be evaluated and no confederates were in the room.
3.2. Data Analysis
Reactivity of self-reported affect was calculated as task minus baseline change scores, whereas recovery was calculated as post-task minus baseline change scores. CVR and recovery was calculated similarly for SBP and DBP. The two BP readings for the initial experimental task were averaged. Further, the two listening intervals during the hostile interpersonal task were averaged to reflect overall CVR while listening, as were the two speaking intervals. Cardiovascular recovery is reported as the average SBP and DBP over this five-minute period.
Hierarchical linear regressions determined the extent to which BPD symptoms predicted changes in self-report affect and cardiovascular responses, and post-task rumination. For each regression, effect codes for the Acceptance Threat and Status Threat manipulations were first entered, followed by BSL-23 scores centered at their mean, with the final step consisting of BPD × threat condition product terms. These analyses allowed us to test the main and interactive effects of condition (i.e., high vs. low acceptance and/or status threat) and BPD symptoms in predicting BP and self-report affective reactivity to, and recovery from, the social stress task.
3.3. Results
3.3.1. Evaluative Threat Manipulation Check
Findings effects of the manipulations are reported in detail elsewhere (Smith & Jordan, 2015). Participants in high Acceptance Threat conditions reported significantly higher overall increases in self-report anger and anxiety. Participants in the high Status Threat conditions reported greater overall changes in SCE (self-conscious emotions). Finally, participants in threat conditions displayed greater overall SBP and DBP reactivity, relative to low threat controls.
3.3.2. Associations of Borderline Symptoms with Affect and Cardiovascular Responses
3.3.2.1. Self-Report Affect
BPD symptoms did not predict change in anger, anxiety, or SCE during the task. During recovery, BPD symptoms were associated with greater SCE or shame (β = .28, t(142)= 3.51, p = .001) and marginally associated with greater anxiety (β = .15, t(142)= 1.87, p = .06). In a significant BPD features × Acceptance Threat interaction on anger during recovery (β = .22, t(142)= 2.09, p = .03), BPD symptoms were marginally associated with anger in the high acceptance threat condition (β = .225, t(142) = 1.936, p = .055), but were not associated with anger in the low acceptance threat condition (β = −.053, t(142) = −.463, p = ns). Finally, BPD symptoms predicted greater rumination during recovery (β = .22, t(142)= 2.73, p < .01).
3.3.2.2. Cardiovascular Responses
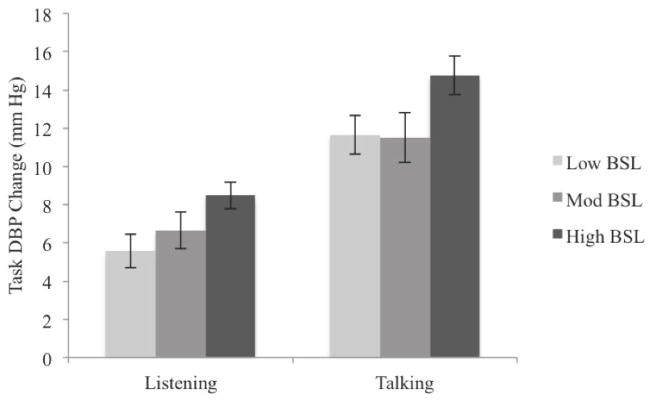
BPD symptoms did not predict CVR during the initial speaking tasks, either as a main effect or as an interaction with evaluative threat. During the hostile role-playing task, there were no significant effects on SBP involving BPD symptoms. However, in first-order effects BPD symptoms predicted DBP change while listening (β = .16, t(142)= 1.95, p = .05) and talking (β = .18, t(142)= 2.27, p = .03) to the hostile partner, independent of evaluative threat conditions, such that higher BSL scores were associated with larger DBP changes (see Figure 2). There were no significant effects for BPD symptoms on blood pressure responses during recovery.
Figure 2.
Means (and SEs) of DBP changes for the listening and talking portions of the social stressor task associated with low, moderate, and high BPD symptom scores.
3.4. Discussion
These findings provide partial support for the view that CVR to social stressors could contribute to associations of BPD with CVD risk, particularly social stressors involving interpersonal conflict. BPD symptoms predicted larger increases in DBP during the hostile interaction task, both while participants listened and spoke to the antagonistic and provoking interaction partner. The fact that this association was significant during both the speaking and listening periods suggests that it is not simply an artifact of differences in speech rate or volume associated with BPD features. These associations were not significant for SBP, however. This pattern may indicate that the association of BPD symptoms with CVR reflected a heightened threat response, as opposed to greater involvement or effort during the task (Seery, 2011). Thus, BPD features may be associated with appraising hostile interpersonal situations as more threatening. Notably, DBP reactivity in younger adults has been found to predict the subsequent development of CVD (Franklin, Wilkinson, & McEniery, 2012).
BPD symptom severity did not moderate the association between SET and CVR. These findings are consistent with prior studies of BPD and physiological responses to SET (Chapman et al., 2014; Nater et al., 2010; Scott et al., 2013). Hence, it may be that individuals with features or symptoms of BPD are more physiologically reactive to hostile interpersonal exchanges than to social-evaluative threats. Nonetheless, given the strong conceptual relevance of social-evaluative threats to BPD, additional research on this issue is necessary. For example, the threat of negative evaluations by close friends, family members, or intimate partners could evoke heightened physiological stress responses for individuals with elevated BPD symptoms.
Future social psychophysiological studies of BPD symptoms should replicate and extend the present findings, but also examine other interpersonal mechanisms. For example, trait hostility is associated with failure to benefit from social support with attenuated CVR in response to stressors (Holt-Lunstad, Smith, & Uchino, 2008; Kamarck, Manuck, & Jennings, 1990). Given the association of BPD features with a hostile interpersonal style and low levels of social support in Study 1, failure to benefit physiologically from albeit limited social support may be another mechanism linking BPD with CVD. Research on the physiologic mechanisms potentially involved in the association of BPD with CVD could also examine these effects with ambulatory methods, which have been informative in studies of BPD (Santangelo, Bohus, & Ebner-Priemer, 2014).
BPD symptoms were inconsistently related to state affect responses. This is somewhat surprising given that prior studies have found this association (Baer et al., 2012; Gratz et al., 2010). Although BPD is generally associated with heightened emotional reactivity, these findings vary across methods and outcomes (Ebner-Priemer et al., 2015). For example, BPD symptoms are associated with heightened emotional reactivity to abandonment and rejection (Chapman et al., 2014; Gratz, Dixon-Gordon, Breetz, & Tull, 2013), but not to generic stressors (Kuo, Neacsiu, Fitzpatrick, & MacDonald, 2014). Although clearly stressful (Smith & Jordan, 2015), the task used in the present study but might not be maximally relevant to BPD pathology. Again, results also might be different in the context of personal relationships.
Results for recovery following interpersonal stress were also somewhat inconsistent. There were no effects for BPD symptoms on BP responses during recovery, and BPD symptoms predicted shame during recovery, but not anxiety. The effect on recovery period shame is consistent with research indicating that shame-like emotions may be slower to return to baseline than other emotions in BPD (Gratz et al., 2010). BPD features were also related to rumination after the task. Rumination is a particularly prominent maladaptive cognitive correlate of BPD, which contributes to emotion dysregulation (see Baer et al., 2012 for review). The BPD × Acceptance Threat interaction on recovery period anger is consistent with the rage-rejection hypothesis (Berenson et al., 2011), such that BSL scores were positively associated with recovery period anger specifically under conditions of perceived threat to acceptance.
Overall, our findings suggest that BPD features are associated with heightened CVR during stressful interpersonal interactions marked by hostility and antagonism, which provides some support for interpersonal stress as a mechanism potentially linking BPD features to CV risk. Nonetheless, future research is warranted to confirm and extend these findings, particularly given the somewhat inconsistent results reported here.
4. General Discussion
Given recent evidence that individuals with BPD are at elevated risk for CVD (El-Gabalawy et al., 2010), the present studies examined associations of BPD features with interpersonal processes implicated in the development of this highly prevalent source of morbidity and mortality (Smith et al., 2004; 2014). In the first, BPD symptoms were associated with hostile-submissive interpersonal behavior, across two samples and two different well-validated measures of BPD. Furthermore, BPD symptoms predicted interpersonal risk factors for CVD, specifically lower levels of social support and greater levels of interpersonal conflict, consistent with a long line of research on BPD (Gunderson, 2007). In Study 2, BPD features predicted CVR in response to a social stressor. Specifically, BPD symptoms predicted DBP while participants listened and spoke during a simulated hostile social interaction. Heightened CVR in response to social stressors could contribute to the association of BPD with CVD (Chida & Steptoe, 2010). Thus, consistent with the interpersonal perspective on psychosocial risk for CVD (Smith et al., 2004; Smith & Cundiff, 2011), BPD features were associated with social risk factors and social psychophysiological mechanisms known to promote risk.
4.1. Limitations
There are important limitations of the present studies. The samples were predominately White undergraduates, and findings should be replicated with more diverse samples. Further, the majority of the participants were healthy young adults, much younger than the age of the typical onset of clinical CVD. Further, there is little normative information regarding the magnitude of CVR that confers heightened risk of CVD. However, it is important to note that variability in CVR within the range seen in the present study, when measured in young adulthood, predicts later development of CVD (Chida & Steptoe, 2010). Nonetheless, future research with older samples at greater risk for CVD is warranted.
It is also important to note that the test of the association of BPD features with CVR during interpersonal conflict did not involve an experimental manipulation of this feature of social context. Hence, the association of BPD symptoms with CVR during conflict could reflect other factors, such as the passage of time rather than conflict, per se. The stressor evoked substantial physiological and emotional responses (Smith & Jordan, 2015), but associations between BPD features with social support, conflict, and physiological responses should be replicated in more compelling contexts. For example, marital conflict predicts CVD, perhaps through the mechanisms of heightened physiological reactivity to this stressor (Robles & Kiecolt-Glaser, 2003; Smith et al., 2014), and BPD is also associated with greater levels of marital conflict and disruption (South, Turkheimer, & Oltmanns, 2008).
In addition, the present study did not include a clinical sample of individuals meeting criteria for BPD, nor did we oversample for participants reporting elevated BPD pathology. The mean scores on the BPD symptoms measures were within the normal range, as would be expected in these samples. To our knowledge, there is no official cutoff score indicating diagnosable BPD for either of the BPD measures used in this study. However, prior studies using the BSL on samples consisting of individuals meeting criteria for BPD have demonstrated mean scores of greater than 1.5 (see Bohus et al., 2008). By comparison, the mean scores for each of our samples was less than 1, and only a minority of participants in our samples scored within the range typical of individuals with BPD. Although there is evidence that BPD pathology is a dimensional construct (Widiger, 2011), effects could be different in individuals who are closer to the diagnostic threshold for BPD. Further, symptom measures by themselves are not sufficient for a BPD diagnosis.
Notably, interpersonal style in this study was conceptualized as trait-level interpersonal behavior. As such, our findings do not address the moment-to-moment fluctuations in interpersonal behavior, which is particularly relevant to BPD. Indeed, previous research has established that while interpersonal behavior in BPD appears to be, on average, related to hostility and perhaps submissiveness, there is substantial variability across situations that is highly dependent upon negative affect (Russell et al., 2007) and perception (Sadikaj et al., 2013). Further, recent studies have found significant heterogeneity with regard to interpersonal behavior in BPD, such that there may be distinct profiles of interpersonal behavior associated with BPD (Wright et al., 2013). More research is necessary to determine how moment-to-moment interpersonal behavior contributes to stress responses related to CVD.
The present study included multiple measures of BPD pathology, which is a significant strength. However, we did not include measures for other forms of psychopathology that both overlap with BPD and are associated with CVD risk. Hence, we cannot conclude that our findings are specific to BPD pathology. Future research should address this issue by including measures for other types of psychopathology related to BPD.
4.2. Future Directions
These limitations notwithstanding, the present studies provide preliminary support for the utility of the interpersonal perspective as a guide to needed research on mechanisms potentially contributing to associations of BPD features with CVD risk. In addition to addressing limitations described above, future research should examine further the associations of BPD with these interpersonal and social psychophysiological mechanisms. Evidence is mixed with regard to the relationship between BPD and reactivity to social stressors (Cavazzi & Becerra, 2014). The current study examined stressors involving SET and hostility, but individuals with BPD symptoms may react strongly to other social stressors. For instance, social exclusion (Williams & Jarvis, 2006) reliably evokes heightened negative affect in individuals with BPD symptoms relative to controls (Lazarus, Cheavens, Festa, & Rosenthal, 2014). Future studies might investigate CVR in BPD using such stressors or other laboratory tasks known to evoke reactivity in individuals with elevated BPD symptoms (e.g., family conflict; Crowell et al., 2013).
Future research should also examine interpersonal correlates of BPD related to CVD risk prospectively, and examine directly the transactional process hypothesized to link BPD with reduced social support and heightened conflict. Also, BPD is highly comorbid with depressive and anxiety disorders (Tomko, Trull, Wood, & Sher, 2014), which are also as associated with psychosocial stress and CV risk (Suls & Bunde, 2005). Thus, the extent to which BPD symptoms have a unique association with CVD and underlying mechanisms warrants additional research.
Finally, although we examined stress exposure, reactivity, and recovery as mechanisms potentially contributing to an association of BPD with CVD, we did not examine interpersonal processes in another core mechanism: restorative processes, especially sleep. Recent evidence suggests chronic sleep disturbance is a common problem associated with BPD (Grove et al., in press; Selby, 2013), and poor sleep quality is associated with a wide range of long-term health problems, including CVD (Williams et al., 2010). Further, poor sleep predicts–and is predicted by – daily interpersonal difficulties (Tavernier & Willoughby, 2014). Thus, BPD symptoms could influence CVD risk through reciprocal associations among sleep quality, exposure to interpersonal difficulties, and emotional and physiological responses.
5. Conclusion
Overall, BPD features may confer risk of CVD through recurring reciprocal processes in which these individuals experience greater interpersonal conflict and disruption and less connection and social support in their daily lives. They may also respond to such experiences with more frequent and severe psychophysiological responses that hasten the development and progression of CVD, and may fail to benefit physiologically from the support available to them, given that their social connections are often limited or troubled. Future studies could usefully extend the present findings by testing these interpersonal psychosomatic hypotheses. Such efforts could provide valuable information for prevention and management of CVD, and could help to limit the otherwise negative effects of BPD on health and well-being.
Table 3.
Multiple squared R values for composite scores of BPD symptoms and the two domains of the IPC for Study 1.
| Self-Report | M (SD) | α | R | R2 | F | β Affiliation | β Control |
|---|---|---|---|---|---|---|---|
| Sample 1 | df (2, 285) | ||||||
| BSL-23 | .72 (.69) | .94 | .25 | .06 | 9.50*** | −.12* | −.21*** |
| FFBI Composite | 289.30 (80.14) | .97 | .35 | .12 | 19.62*** | −.32*** | −.12* |
| Sample 2 | df (2, 185) | ||||||
| BSL-23 | .74 (.69) | .95 | .36 | .13 | 13.83*** | −.19** | −.28*** |
| FFBI Composite | 285.93 (75.38) | .97 | .46 | .21 | 24.80*** | −.43*** | −.13* |
p < .05,
< .01,
< .001.
Note: BSL-23=Borderline Symptom List-23, FFBI=Five Factor Borderline Inventory.
Highlights.
BPD associated with social factors linked with CVD (e.g., social support).
Hostile-submissive behavior contributed to link between BPD and social support.
BPD predicted elevated blood pressure responses to lab stressor involving conflict.
BPD did not predict blood pressure response to stressor involving evaluative threat.
BPD predicted shame during recovery from laboratory stress task.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jeremy L. Grove, University of Utah
Timothy W. Smith, University of Utah
Sheila E. Crowell, University of Utah
Paula G. Williams, University of Utah
Kevin D. Jordan, Indiana State University
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, D.C: 2013. [Google Scholar]
- Baer RA, Peters JR, Eisenlohr-Moul TA, Geiger PJ, Sauer SE. Emotion-related cognitive processes in borderline personality disorder: A review of the empirical literature. Clinical Psychology Review. 2012;32(5):359–369. doi: 10.1016/j.cpr.2012.03.002. [DOI] [PubMed] [Google Scholar]
- Bastien M, Poirier P, Lemieux I, Després JP. Overview of epidemiology and contribution of obesity to cardiovascular disease. Progress in Cardiovascular Diseases. 2014;56(4):369–381. doi: 10.1016/j.pcad.2013.10.016. [DOI] [PubMed] [Google Scholar]
- Berenson KR, Downey G, Rafaeli E, Coifman KG, Paquin NL. The rejection – rage contingency in borderline personality disorder. Journal of Abnormal Psychology. 2011;120(3):681. doi: 10.1037/a0023335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Björkenstam E, Björkenstam C, Holm H, Gerdin B, Ekselius L. Excess cause-specific mortality in in-patient-treated individuals with personality disorder: 25-year nationwide population-based study. The British Journal of Psychiatry. 2015;207(4):339–345. doi: 10.1192/bjp.bp.114.149583. [DOI] [PubMed] [Google Scholar]
- Bohus M, Kleindienst N, Limberger MF, Stieglitz RD, Domsalla M, Chapman AL, … Wolf M. The short version of the borderline symptom list (BSL-23): Development and initial data on psychometric properties. Psychopathology. 2008;42(1):32–39. doi: 10.1159/000173701. [DOI] [PubMed] [Google Scholar]
- Cavazzi T, Becerra R. Psychophysiological Research of Borderline Personality Disorder: Review and Implications for Biosocial Theory. Europe’s Journal of Psychology. 2014;10(1):185–203. [Google Scholar]
- Chapman AL, Walters KN, Gordon KLD. Emotional reactivity to social rejection and negative evaluation among persons with borderline personality features. Journal of Personality Disorders. 2014;28(5):720–733. doi: 10.1521/pedi_2012_26_068. [DOI] [PubMed] [Google Scholar]
- Cheng JT, Tracy JL, Foulsham T, Kingstone A, Henrich J. Two ways to the top: Evidence that dominance and prestige are distinct yet viable avenues to social rank and influence. Journal of Personality and Social Psychology. 2013;104(1):103. doi: 10.1037/a0030398. [DOI] [PubMed] [Google Scholar]
- Chida Y, Steptoe A. The association of anger and hostility with future coronary heart disease: A meta-analytic review of prospective evidence. Journal of the American College of Cardiology. 2009;53(11):936–946. doi: 10.1016/j.jacc.2008.11.044. [DOI] [PubMed] [Google Scholar]
- Chida Y, Steptoe A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status a meta-analysis of prospective evidence. Hypertension. 2010;55(4):1026–1032. doi: 10.1161/HYPERTENSIONAHA.109.146621. [DOI] [PubMed] [Google Scholar]
- Chu X, Ma Z, Li Y, Han J. Agreeableness, Extraversion, Stressor and Physiological Stress Response. International Journal of Social Science Studies. 2015;3(4):79–86. [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Social support: Theory, research and applications. Springer; 1985. Measuring the functional components of social support; pp. 73–94. [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan MM. A biosocial developmental model of borderline personality: Elaborating and extending linehan’s theory. Psychological Bulletin. 2009;135(3):495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cundiff JM, Smith TW, Butner J, Critchfield KL, Nealey-Moore J. Affiliation and control in marital interaction: Interpersonal complementarity is present but is not associated with affect or relationship quality. Personality and Social Psychology Bulletin. 2015;41(1):35–51. doi: 10.1177/0146167214557002. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychological Bulletin. 2004;130(3):355–391. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Mycek PJ, Zaldivar F. Negative social evaluation, but not mere social presence, elicits cortisol responses to a laboratory stressor task. Health Psychology. 2008;27(1):116–121. doi: 10.1037/0278-6133.27.1.116. [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Houben M, Santangelo P, Kleindienst N, Tuerlinckx F, Oravecz Z, … Kuppens P. Unraveling affective dysregulation in borderline personality disorder: A theoretical model and empirical evidence. Journal of Abnormal Psychology. 2015;124(1):186–198. doi: 10.1037/abn0000021. [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Welch SS, Grossman P, Reisch T, Linehan MM, Bohus M. Psychophysiological ambulatory assessment of affective dysregulation in borderline personality disorder. Psychiatry Research. 2007;150(3):265–275. doi: 10.1016/j.psychres.2006.04.014. [DOI] [PubMed] [Google Scholar]
- El-Gabalawy R, Katz LY, Sareen J. Comorbidity and associated severity of borderline personality disorder and physical health conditions in a nationally representative sample. Psychosomatic Medicine. 2010;72(7):641–647. doi: 10.1097/PSY.0b013e3181e10c7b. [DOI] [PubMed] [Google Scholar]
- Franklin SS, Wilkinson IB, McEniery CM. Unusual hypertensive phenotypes What is their significance? Hypertension. 2012;59(2):173–178. doi: 10.1161/HYPERTENSIONAHA.111.182956. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Smith TW. Construct validation of health-relevant personality traits: Interpersonal circumplex and five-factor model analyses of the aggression questionnaire. International Journal of Behavioral Medicine. 1998;5:129–147. doi: 10.1207/s15327558ijbm0502_4. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Smith TW. Patterns of hostility and social support: Conceptualizing psychosocial risk factors as characteristics of the person and the environment. Journal of Research in Personality. 1999;33:281–310. [Google Scholar]
- Gallo LC, Smith TW, Kircher JC. Cardiovascular and electrodermal responses to support and provocation: Interpersonal methods in the study of psychophysiologic reactivity. Psychophysiology. 2000;37:289–301. [PubMed] [Google Scholar]
- Gallo LC, Smith TW, Ruiz JM. An interpersonal analysis of adult attachment style: Circumplex descriptions, recalled developmental experiences, self-represntations, and interpersonal functioning in adulthood. Journal of Personality. 2003;71:141–181. doi: 10.1111/1467-6494.7102003. [DOI] [PubMed] [Google Scholar]
- Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, … Malaspina D. Short sleep duration as a risk factor for hypertension analyses of the first national health and nutrition examination survey. Hypertension. 2006;47(5):833–839. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, … Pickering RP. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of clinical psychiatry. 2008;69(4):533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Dixon-Gordon KL, Breetz A, Tull M. A laboratory-based examination of responses to social rejection in borderline personality disorder: the mediating role of emotion dysregulation. Journal of Personality Disorders. 2013;27(2):157–171. doi: 10.1521/pedi.2013.27.2.157. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez C, Gunderson JG. An experimental investigation of emotion dysregulation in borderline personality disorder. Journal of Abnormal Psychology. 2006;115(4):850–855. doi: 10.1037/0021-843X.115.4.850. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez C, Gunderson JG. An experimental investigation of emotional reactivity and delayed emotional recovery in borderline personality disorder: The role of shame. Comprehensive Psychiatry. 2010;51(3):275–285. doi: 10.1016/j.comppsych.2009.08.005. [DOI] [PubMed] [Google Scholar]
- Grove JL, Smith TW, Crowell SE, Ellis JH. Preliminary evidence for emotion dysregulation as a mechanism underlying poor sleep quality in borderline personality disorder. Journal of Personality Disorders. doi: 10.1521/pedi_2016_30_261. (in press) [DOI] [PubMed] [Google Scholar]
- Gunderson JG. Disturbed relationships as a phenotype for borderline personality disorder. American Journal of Psychiatry. 2007;164:1637–1640. doi: 10.1176/appi.ajp.2007.07071125. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Stout RL, McGlashan TH, Shea MT, Morey LC, Grilo CM, … Skodol AE. Ten-year course of borderline personality disorder: Psychopathology and function from the collaborative longitudinal personality disorders study. Archives of General Psychiatry. 2011;68(8):827–837. doi: 10.1001/archgenpsychiatry.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurtman MB. Construct validity of interpersonal personality measures: The interpersonal circumplex as a nomological net. Journal of Personality and Social Psychology. 1992;63(1):105–118. [Google Scholar]
- Haukkala A, Konttinen H, Laatikainen T, Kawachi I, Uutela A. Hostility, anger control, and anger expression as predictors of cardiovascular disease. Psychosomatic Medicine. 2010;72(6):556–562. doi: 10.1097/PSY.0b013e3181dbab87. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TW, Uchino BN. Can hostility interfere with the health benefits of giving and receiving social support? The impact of cynical hostility on cardiovascular reactivity during social support interactions among friends. Annals of Behavioral Medicine. 2008;35:319–330. doi: 10.1007/s12160-008-9041-z. [DOI] [PubMed] [Google Scholar]
- Hopwood CJ, Newman DA, Donnellan MB, Markowitz JC, Grilo CM, Sanislow CA, … Gunderson JG. The stability of personality traits in individuals with borderline personality disorder. Journal of Abnormal Psychology. 2009;118(4):806–815. doi: 10.1037/a0016954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz LM, Strack S, editors. Handbook of interpersonal psychology. Hoboken, NJ: Wiley; 2011. [Google Scholar]
- Horowitz LM, Wilson KR, Turan B, Zolotsev P, Constantino MJ, Henderson L. How interpersonal motives clarify the meaning of interpersonal behavior: A revised circumplex model. Personality and Social Psychology Review. 2006;10(1):67–86. doi: 10.1207/s15327957pspr1001_4. [DOI] [PubMed] [Google Scholar]
- Kamarck TW, Manuck SB, Jennings JR. Social support reduces cardiovascular reactivity to psychological challenge: a laboratory model. Psychosomatic Medicine. 1990;52(1):42–58. doi: 10.1097/00006842-199001000-00004. [DOI] [PubMed] [Google Scholar]
- King CR, Knutson KL, Rathouz PJ, Sidney S, Liu K, Lauderdale DS. Short sleep duration and incident coronary artery calcification. JAMA. 2008;300(24):2859–2866. doi: 10.1001/jama.2008.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo JR, Neacsiu AD, Fitzpatrick S, MacDonald DE. A Methodological Examination of emotion inductions in borderline personality disorder: A comparison of standardized versus idiographic stimuli. Journal of Psychopathology and Behavioral Assessment. 2014;36(1):155–164. [Google Scholar]
- Lazarus SA, Cheavens JS, Festa F, Rosenthal MZ. Interpersonal functioning in borderline personality disorder: A systematic review of behavioral and laboratory-based assessments. Clinical Psychology Review. 2014;34(3):193–205. doi: 10.1016/j.cpr.2014.01.007. [DOI] [PubMed] [Google Scholar]
- Lee HB, Bienvenu OJ, Cho SJ, Ramsey CM, Bandeen-Roche K, Eaton WW, Nestadt G. Personality disorders and traits as predictors of incident cardiovascular disease: findings from the 23-year follow-up of the Baltimore ECA study. Psychosomatics. 2010;51(4):289–296. doi: 10.1176/appi.psy.51.4.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan M. Cognitive-behavioral treatment of borderline personality disorder. Guilford Press; 1993. [Google Scholar]
- Matthews KA, Zhu S, Tucker DC, Whooley MA. Blood pressure reactivity to psychological stress and coronary calcification in the Coronary Artery Risk Development in Young Adults Study. Hypertension. 2006;47(3):391–395. doi: 10.1161/01.HYP.0000200713.44895.38. [DOI] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA. Bias in cross–sectional analyses of longitudinal mediation. Psychological Methods. 2007;12:23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- McGill HC, McMahan A, Gidding SS. Preventing heart disease in the 21st century: Implications of the Pathobiological Determinants of Atherosclerosis in Youth (PADY) study. Circulation. 2008;117:1216–1227. doi: 10.1161/CIRCULATIONAHA.107.717033. [DOI] [PubMed] [Google Scholar]
- Moran P, Stewart R, Brugha T, Bebbington P, Bhugra D, Jenkins R, Coid JW. Personality disorder and cardiovascular disease: Results from a national household survey. Journal of Clinical Psychiatry. 2007;68(1):69–74. doi: 10.4088/jcp.v68n0109. [DOI] [PubMed] [Google Scholar]
- Mullins-Sweatt SN, Edmundson M, Sauer-Zavala S, Lynam DR, Miller JD, Widiger TA. Five-factor measure of borderline personality traits. Journal of Personality Assessment. 2012;94(5):475–487. doi: 10.1080/00223891.2012.672504. [DOI] [PubMed] [Google Scholar]
- Nater UM, Bohus M, Abbruzzese E, Ditzen B, Gaab J, Kleindienst N, … Ehlert U. Increased psychological and attenuated cortisol and alpha-amylase responses to acute psychosocial stress in female patients with borderline personality disorder. Psychoneuroendocrinology. 2010;35(10):1565–1572. doi: 10.1016/j.psyneuen.2010.06.002. [DOI] [PubMed] [Google Scholar]
- Nealey-Moore J, Smith TW, Uchino BN, Hawkins M, Olson-Cerny C. Cardiovascular reactivity during positive and negative marital interactions. Journal of Bheavioral Medicine. 2007;30:505–519. doi: 10.1007/s10865-007-9124-5. [DOI] [PubMed] [Google Scholar]
- Pincus A, Ansell E. Interpersonal theory of personality. Handbook of psychology: Personality and social psychology. 2013;5:141–159. [Google Scholar]
- Pincus AL, Wiggins JS. Interpersonal problems and conceptions of personality disorders. Journal of Personality Disorders. 1990;4(4):342–352. [Google Scholar]
- Radstaak M, Geurts SA, Brosschot JF, Cillessen AH, Kompier MA. The role of affect and rumination in cardiovascular recovery from stress. International Journal of Psychophysiology. 2011;81(3):237–244. doi: 10.1016/j.ijpsycho.2011.06.017. [DOI] [PubMed] [Google Scholar]
- Robles TF, Kiecolt-Glaser JK. The physiology of marriage: Pathways to health. Physiology & behavior. 2003;79(3):409–416. doi: 10.1016/s0031-9384(03)00160-4. [DOI] [PubMed] [Google Scholar]
- Rosenthal MZ, Gratz KL, Kosson DS, Cheavens JS, Lejuez C, Lynch TR. Borderline personality disorder and emotional responding: A review of the research literature. Clinical Psychology Review. 2008;28(1):75–91. doi: 10.1016/j.cpr.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Ross JM, Babcock JC. Proactive and reactive violence among intimate partner violent men diagnosed with antisocial and borderline personality disorder. Journal of Family Violence. 2009;24(8):607–617. [Google Scholar]
- Ruehlman LS, Karoly P. With a little flak from my friends: Development and preliminary validation of the test of negative social exchange (TENSE) Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3(1):97–104. [Google Scholar]
- Russell JJ, Moskowitz D, Zuroff DC, Sookman D, Paris J. Stability and variability of affective experience and interpersonal behavior in borderline personality disorder. Journal of Abnormal Psychology. 2007;116(3):578–588. doi: 10.1037/0021-843X.116.3.578. [DOI] [PubMed] [Google Scholar]
- Ryan K, Shean G. Patterns of interpersonal behaviors and borderline personality characteristics. Personality and Individual Differences. 2007;42(2):193–200. [Google Scholar]
- Sadikaj G, Moskowitz D, Russell JJ, Zuroff DC, Paris J. Quarrelsome behavior in borderline personality disorder: Influence of behavioral and affective reactivity to perceptions of others. Journal of Abnormal Psychology. 2013;122(1):195–207. doi: 10.1037/a0030871. [DOI] [PubMed] [Google Scholar]
- Samuel DB, Carroll KM, Rounsaville BJ, Ball SA. Personality disorders as maladaptive, extreme variants of normal personality: Borderline personality disorder and neuroticism in a substance using sample. Journal of Personality Disorders. 2013;27(5):625–635. doi: 10.1521/pedi.2013.27.5.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santangelo P, Bohus M, Ebner-Priemer UW. Ecological momentary assessment in borderline personality disorder: A review of recent findings and methodological challenges. Journal of Personality Disorders. 2014;28(4):555–576. doi: 10.1521/pedi_2012_26_067. [DOI] [PubMed] [Google Scholar]
- Scott LN, Levy KN, Granger DA. Biobehavioral reactivity to social evaluative stress in women with borderline personality disorder. Personality Disorders: Theory, Research, and Treatment. 2013;4(2):91–100. doi: 10.1037/a0030117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seery MD. Challenge or threat? Cardiovascular indexes of resilience and vulnerability to potential stress in humans. Neuroscience & Biobehavioral Reviews. 2011;35(7):1603–1610. doi: 10.1016/j.neubiorev.2011.03.003. [DOI] [PubMed] [Google Scholar]
- Selby EA. Chronic sleep disturbances and borderline personality disorder symptoms. Journal of Consulting and Clinical Psychology. 2013;81(5):941–947. doi: 10.1037/a0033201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selby EA, Joiner TE., Jr Emotional cascades as prospective predictors of dysregulated behaviors in borderline personality disorder. Personality Disorders: Theory, Research, and Treatment. 2013;4(2):168–174. doi: 10.1037/a0029933. [DOI] [PubMed] [Google Scholar]
- Smith TW, Baron CE, Grove JL. Personality, Emotional Adjustment, and Cardiovascular Risk: Marriage as a Mechanism. Journal of Personality. 2014;82(6):502–514. doi: 10.1111/jopy.12074. [DOI] [PubMed] [Google Scholar]
- Smith TW, Cundiff JM. An interpersonal perspective on risk for coronary heart disease. In: Horowitz LM, Strack S, editors. Handbook of Interpersonal Psychology: Theory, Research, Assessment, and Therapeutic Interventions. Hoeboken, NJ: Wiley; 2011. pp. 471–489. [Google Scholar]
- Smith TW, Gallo LG. Hostility and cardiovascular reactivity during marital interaction. Psychosomatic Medicine. 1999;61(4):436–445. doi: 10.1097/00006842-199907000-00005. [DOI] [PubMed] [Google Scholar]
- Smith TW, Glazer K, Ruiz JM, Gallo LC. Hostility, anger, aggressiveness, and coronary heart disease: An interpersonal perspective on personality, emotion, and health. Journal of Personality. 2004;72(6):1217–1270. doi: 10.1111/j.1467-6494.2004.00296.x. [DOI] [PubMed] [Google Scholar]
- Smith TW, Jordan KD. Interpersonal motives and social-evaluative threat: Effects of acceptance and status stressors on cardiovascular reactivity and salivary cortisol response. Psychophysiology. 2015;52:269–276. doi: 10.1111/psyp.12318. [DOI] [PubMed] [Google Scholar]
- Smith TW, Nealey JB, Kircher JC, Limon JP. Social determinants of cardiovascular reactivity: Effects of incentive to exert influence and evaluative threat. Psychophysiology. 1997;34(1):65–73. doi: 10.1111/j.1469-8986.1997.tb02417.x. [DOI] [PubMed] [Google Scholar]
- Smith TW, Ruiz JM, Cundiff JM, Baron KG, Nealey-Moore JB. Optimism and pessimism in social context: An interpersonal perspective on resilience and risk. Journal of Research in Personality. 2013;47(5):553–562. doi: 10.1016/j.jrp.2013.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TW, Uchino BN, Berg CA, Florsheim P. Marital discord and coronary artery disease: A comparison of behaviorally defined discrete groups. Journal of Consulting and Clinical psychology. 2012;80(1):87–92. doi: 10.1037/a0026561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South SC, Turkheimer E, Oltmanns TF. Personality disorder symptoms and marital functioning. Journal of Consulting and Clinical Psychology. 2008;76(5):769–780. doi: 10.1037/a0013346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD, Jacobs G, Russell S, Crane RS. Assessment of anger: The state-trait anger scale. Advances in Personality Assessment. 1983;2:159–187. [Google Scholar]
- Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: the problems and implications of overlapping affective dispositions. Psychological Bulletin. 2005;131(2):260–300. doi: 10.1037/0033-2909.131.2.260. [DOI] [PubMed] [Google Scholar]
- Tavernier R, Willoughby T. Bidirectional associations between sleep (quality and duration) and psychosocial functioning across the university years. Developmental Psychology. 2014;50(3):674–682. doi: 10.1037/a0034258. [DOI] [PubMed] [Google Scholar]
- Tomko RL, Trull TJ, Wood PK, Sher KJ. Characteristics of borderline personality disorder in a community sample: Comorbidity, treatment utilization, and general functioning. Journal of personality disorders. 2014;28(5):734–750. doi: 10.1521/pedi_2012_26_093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trapnell PD, Campbell JD. Private self-consciousness and the five-factor model of personality: Distinguishing rumination from reflection. Journal of Personality and Social Psychology. 1999;76(2):284–304. doi: 10.1037//0022-3514.76.2.284. [DOI] [PubMed] [Google Scholar]
- Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Uchino BN, Holt-Lunstad J, Bloor LE, Campo RA. Aging and cardiovascular reactivity to stress: longitudinal evidence for changes in stress reactivity. Psychology and Aging. 2005;20(1):134. doi: 10.1037/0882-7974.20.1.134. [DOI] [PubMed] [Google Scholar]
- Uchino BN, Smith TW, Holt-Lunstad JL, Campo R, Reblin M. Stress and illness. In: Cacioppo J, Tassinary L, Berntson G, editors. Handbook of Psychophysiology. 3. New York: Cambridge University Press; 2007. pp. 608–632. [Google Scholar]
- Whisman MA, Schonbrun YC. Social consequences of borderline personality disorder symptoms in a population-based survey: Marital distress, marital violence, and marital disruption. Journal of Personality Disorders. 2009;23(4):410–415. doi: 10.1521/pedi.2009.23.4.410. [DOI] [PubMed] [Google Scholar]
- Widiger TA. The DSM-5 dimensional model of personality disorder: Rationale and empirical support. Journal of Personality Disorders. 2011;25(2):222–234. doi: 10.1521/pedi.2011.25.2.222. [DOI] [PubMed] [Google Scholar]
- Wiggins JS. A psychological taxonomy of trait-descriptive terms: The interpersonal domain. Journal of Personality and Social Psychology. 1979;37(3):395. [Google Scholar]
- Wiggins JS, Broughton R. A geometric taxonomy of personality scales. European Journal of Personality. 1991;5(5):343–365. [Google Scholar]
- Wiggins JS, Trapnell P, Phillips N. Psychometric and geometric characteristics of the revised interpersonal adjective scales (IAS-R) Multivariate Behavioral Research. 1988;23(4):517–530. doi: 10.1207/s15327906mbr2304_8. [DOI] [PubMed] [Google Scholar]
- Williams PG, Cribbet MR, Rau HK, Gunn HE, Czajkowski LA. The effects of poor sleep on cognitive, affective, and physiological responses to a laboratory stressor. Annals of Behavioral Medicine. 2013;46(1):40–51. doi: 10.1007/s12160-013-9482-x. [DOI] [PubMed] [Google Scholar]
- Williams PG, Smith TW, Gunn HE, Uchino BN. Personality and Stress: individual differences in exposure, reactivity, recovery, and restoration. The Handbook of Stress Science: Biology, Psychology, and Health. 2010:231–245. [Google Scholar]
- Wright AG, Hallquist MN, Morse JQ, Scott LN, Stepp SD, Nolf KA, Pilkonis PA. Clarifying interpersonal heterogeneity in borderline personality disorder using latent mixture modeling. Journal of Personality Disorders. 2013;27(2):125–143. doi: 10.1521/pedi.2013.27.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AG, Pincus AL, Hopwood CJ, Thomas KM, Markon KE, Krueger RF. An interpersonal analysis of pathological personality traits in DSM–5. Assessment. 2012;19(3):263–275. doi: 10.1177/1073191112446657. [DOI] [PMC free article] [PubMed] [Google Scholar]