Abstract
Background/Aim: The Barthel index and Katz index are useful in assessing the physical function status of patients. We prospectively evaluated the relationship between the Barthel and Katz indices and postoperative complications in older patients undergoing gastrointestinal surgery.
Patients and Methods: We enrolled 250 patients aged ≥65 years who underwent gastrointestinal surgery between September 2018 and April 2020. Postoperative complications within 30 days after surgery were categorized using the Clavien-Dindo classification. The primary endpoint was the incidence of postoperative complications of Clavien-Dindo grade ≥II.
Results: Of the 250 patients (age, 74.1±6.2 years), 149 (59.6%) were male and 101 (40.4%) were female. The Barthel index was <100 in 49 patients (19.6%), and the Katz index was B-G in 23 patients (9.2%). Seventy-five patients (30%) developed postoperative complications of Clavien-Dindo grade ≥I, and 72 patients (28.8%) developed complications of Clavien-Dindo grade ≥II within 30 days after surgery. A Barthel index of <100 was more common in the group with complications, while the Katz index did not differ. A Barthel index of <100 was also a significant multivariate predictor of complications of Clavien-Dindo grade ≥II.
Conclusion: The Barthel index is a useful predictor of postoperative complications in older individuals undergoing gastrointestinal surgery.
Keywords: Outcome prediction, abdominal surgery, Barthel index, postoperative complication, comprehensive geriatric assessment
In recent years, population aging has been noted, both worldwide and in Japan. Approximately 36.01 million people in Japan were aged ≥65 years on March 1, 2018, which is 28.6% of the total population (http://www.stat.go.jp/ data/jinsui/index.html). The proportion of the population aged ≥65 years is expected to be just under 40% by 2050. With the population aging, the number of surgeries performed on older patients is also expected to increase, such as surgery for gastrointestinal cancer, which is the leading cause of death from malignancy. However, older individuals have impaired physiology and reserve; thus, postoperative complications may result in a severe and prolonged clinical course (1). Therefore, it is essential to conduct risk management from the preoperative stage.
The Eastern Cooperative Oncology Group-Performance Status, American Society of Anesthesiologists-Physical Status (ASA-PS), Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity (POSSUM), and Surgical Apgar Score are methods for multifaceted risk assessment. POSSUM is an evaluation method that was proposed by Copeland et al. in 1991, which calculates the postoperative complication and mortality rates using a predictive formula that combines physiological and operative severity scores (2,3). The Surgical Apgar Score evaluates the patient’s condition and blood loss immediately after surgery to predict the postoperative course (4,5). However, these indices are somewhat complicated because they require intraoperative and postoperative findings.
The Comprehensive Geriatric Assessment (CGA), which originated in the United Kingdom and was developed in the United States, is an assessment of the physical, psychological, and social aspects of older individuals. It is a simple and accurate assessment of functional impairment in older individuals. It is used to reduce mortality, shorten the length of hospital stay, and improve activities of daily living (ADL) (6,7). The Barthel index, which focuses on assessing physical function in the CGA, is helpful as a postoperative functional assessment in orthopedic surgery and as a predictor of postoperative complications in gastrointestinal surgery for certain diseases (8-11). The Katz index has fewer evaluation items than the Barthel index and evaluates six functions, namely bathing, dressing, toileting, transferring, continence, and feeding (12,13). However, to our best knowledge, no prospective studies have examined the usefulness of CGA in patients undergoing abdominal surgery. Therefore, we designed a prospective clinical trial to evaluate the relationship between the CGA and postoperative complications of gastrointestinal surgery using the Barthel index and the Katz index, which can be used to preoperatively assess ADLs. We hypothesized that these indices are helpful for assessing postoperative complications in patients undergoing abdominal surgery.
Patients and Methods
Patient enrollment and the CGA. This single-center prospective study enrolled patients aged ≥65 years who underwent surgery for gastrointestinal diseases at Tottori University Hospital between September 2018 and April 2020. Patients who met at least one of the following conditions were excluded: i) emergency surgery, ii) minor surgery (e.g. hernia, gallbladder stones, gallbladder polyps, appendicitis), and iii) unsuitable for this research, as determined by the principal investigator. Patients who consented to participate in this study were evaluated for their physical function before surgery using the Barthel and Katz indices, and the relationships of these indices with postoperative complications were prospectively investigated (14). Finally, 250 patients aged ≥65 years who underwent surgery for gastrointestinal diseases were statistically reviewed (Figure 1). The patients themselves (or their family members if the patients were unable) completed Barthel index and Katz index questionnaires. Postoperative complications were defined as events occurring within 30 days after surgery and were categorized using the Clavien-Dindo classification (CDc) (15,16).
Figure 1. Flow of patients through the study.
Data collection. Patients’ clinicopathological data were extracted from electronic medical records. Data for age, sex, body mass index, ASA-PS, preoperative blood test results (creatinine, albumin and C-reactive protein), medical history, type of surgery, operative time, the volume of blood loss, length of hospitalization after surgery, discharge destination, and postoperative complications classified using the CDc were prospectively obtained. The primary endpoint was the incidence of postoperative complications of grade II or above according to the CDc, and the secondary endpoints were the length of hospitalization after surgery and the discharge destination. The follow-up duration was calculated from the day of surgery to the day of discharge or death.
Statistical analysis. Continuous data are presented as the mean±standard deviation. For statistical analysis, a two-sided value of p<0.05 was considered statistically significant. All statistical analyses were performed using SPSS version 25 (IBM Corp., Armonk, NY, USA) and GraphPad Prism version 6.0 (GraphPad Software, San Diego, CA, USA). Pearson’s chi-square test was used to analyze categorical data, and Student’s t-test was used to evaluate continuous variables. Univariate and multivariate logistic regression analyses were used to identify preoperative clinical risk factors for CDc grade II or higher. Spearman’s rank correlation coefficient was used to examine the correlation between the Barthel index and the Katz index.
Ethics. All procedures in studies involving human participants were performed according to the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this study, the approval of the Ethics Committee of Tottori University Faculty of Medicine was obtained (Approval No. 18A077). This study did not contain any experiments or procedures involving animals. Written informed consent to participate in the study and consent to publish were obtained from each patient preoperatively.
Data availability. The dataset used and analyzed during the current study is available from the corresponding author on reasonable request.
Results
Patients’ characteristics. Patients’ characteristics are summarized in Table I. Of the 250 patients, 149 (59.6%) were male. The mean age of the patients was 74.1±6.2 years. There were 69 cases of upper gastrointestinal diseases, 86 cases of lower gastrointestinal diseases, 92 cases of hepatobiliary pancreatic disorders, and three cases of other conditions (lymph node biopsy for malignant lymphoma, hernioplasty for incisional hernia). The mean postoperative hospital stay was 18.5±20.0 days, and the discharge destination was home in 237 patients (94.8%), hospital transfer in 12 patients (4.8%), and death in one patient (0.4%). The Barthel index was <100 in 49 patients (19.6%), and the Katz index was B-G in 23 patients (9.2%).
Table I. Patients’ characteristics (n=250).
ASA-PS: American Society of Anesthesiologists-Physical Status; BMI: body mass index; CRP: C-reactive protein; SD: standard deviation.
Comparing patients with a Barthel index of 100 with those with a Barthel index of <100 (Table II), the latter were significantly older (73.7 vs. 78.8 years, p<0.001), were less frequently male (62.7% vs. 46.9%, p=0.044), had a higher ASA-PS (ASA-PS ≥3, 20.4% vs. 44.9%, p=0.002), and had a higher hospital transfer rate (2.0% vs. 16.3%, p<0.001). Preoperative blood tests showed that patients with a Barthel index of <100 had a significantly lower serum albumin concentration (4.0 vs. 3.7 mg/dl, p=0.003). The Katz index showed similar results (Table II). When comparing patients classified as Katz index A with those classified as Katz index B-G, the latter were significantly older, had a higher ASA-PS, and had a higher hospital transfer rate. Preoperative blood tests also showed that patients with Katz index B-G had a significantly lower serum albumin concentration.
Table II. Comparison of clinical factors by Barthel index and Katz index status.
ASA-PS: American Society of Anesthesiologists-Physical Status; BMI: body mass index; CRP: C-reactive protein; SD: standard deviation; n/a: not applicable.
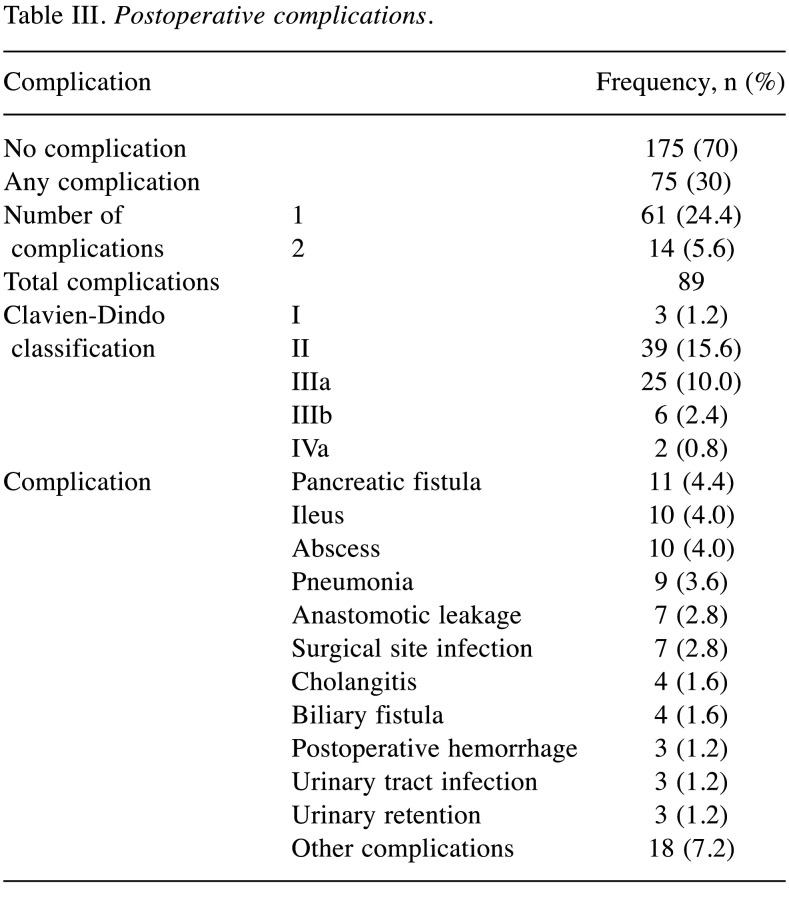
The breakdown of postoperative complications is shown in Table III. Of the 250 patients, 75 (30%) developed postoperative complications (CDc ≥I), and 72 patients (28.8%) developed complications of CDc grade ≥II within 30 days after surgery. The total number of complications is different from the number of patients who developed postoperative complications because some patients developed more than one complication. Fourteen patients developed two complications; therefore, the total number of complications was 89. In the CDc, the highest grade was II, with 39 complications, and 33 complications were grade III or above. There were no perioperative deaths (CDc grade V) within 30 days of surgery; however, one late perioperative death occurred on postoperative day 184, which was classed as CDc grade IIIb (anastomotic leakage). Pancreatic fistula was the most common complication (4.4%), followed by ileus and abscess (4.0%) and pneumonia (3.6%).
Table III. Postoperative complications.
Comparing the group with complications of CDc grade ≥II with the group without complications (CDc 0 or I), the group with complications had a higher proportion of male patients (53.9% vs. 73.6%), open surgery (38.2% vs. 63.9%), and hypertension (58.4% vs. 61.1%), as well as a lower serum albumin concentration (4.0 vs. 3.7 g/dl), a significantly longer operative time (315 vs. 444 min), a greater intraoperative blood loss (178 vs. 469 ml), and a longer hospital stay (12.4 vs. 33.9 days) (Table IV). Similarly, the transfer rate was higher (2.8% vs. 9.7%) and a low Barthel index (<100) was more common (7.3% vs. 31.9%) in the group with CDc grade ≥II complications. Conversely, the proportion of patients with a Katz index of B-G did not differ significantly between the groups with and without grade ≥II complications (7.3% vs. 13.9%).
Table IV. The relationships between complications and predictive factors.
ASA-PS: American Society of Anesthesiologists-Physical Status; BMI: body mass index; CRP: C-reactive protein; CDc: Clavien-Dindo classification of complications; SD: standard deviation; n/a: not applicable.
The Barthel index as a predictor of postoperative complications. Furthermore, to examine the clinical factors related to postoperative complications of CDc grade ≥II, we performed a logistic regression analysis (Table V). In the univariate analysis, male sex [odds ratio (OR)=2.38, p=0.005)], open surgery (OR=2.86, p<0.001), preoperative hypoalbuminemia (OR=0.44, p=0.014), a high preoperative CRP concentration (OR=1.07, p<0.001), a longer operative time (OR=1.01, p<0.001), greater blood loss (OR=1.00, p<0.001), and a Barthel index of <100 (OR=2.90, p=0.001) were significantly associated with the occurrence of complications of CDc grade ≥II. The multivariate analysis of variables with values of p<0.05 in the univariate analysis revealed that male sex (OR=2.281, p=0.021), a longer operative time (OR=1.004, p<0.001), and a Barthel index of <100 (OR=3.201, p=0.003) were significant independent predictors of complications graded as CDc II or more.
Table V. Univariate and multivariate analyses to predict postoperative complications.
ASA-PS: American Society of Anesthesiologists-Physical Status; BMI: body mass index; CRP: C-reactive protein; BMI, body mass index; CI: Confidence interval; OR: odds ratio.
Discussion
Our study used the Barthel and Katz indices to determine whether preoperative physical function assessment predicts postoperative complications in older individuals. The results showed that the Barthel index was an independent predictor of complications graded as CDc II or more. To the best of our knowledge, this is the first report to evaluate the usefulness of the Barthel index as a predictor of postoperative complications in a prospective cohort of older patients undergoing elective abdominal surgery.
Japan has one of the largest proportions of older people in the world. With population aging, the proportion of older patients requiring surgery is also expected to increase (17). Postoperative complications are a significant factor determining a prolonged hospital stay, higher medical costs, and a reduced quality of life, and understanding the risks is vital for patient management (18,19). A summary of nearly 4 million gastrointestinal surgery cases using the National Clinical Database in Japan reported that complications of CDc grade III or above occurred in 3.4-21.3% of cases (20). A slightly smaller multicenter study of nearly 400 non-cardiac surgery cases in patients aged >80 years found that complications occurred in 25% (21). Therefore, we believe that the rate of 13.2% for complications of CDc grade >III in this cohort was not high and that this study was performed at a safe institution.
In this cohort, the proportion of patients of male sex, with a low serum albumin concentration, and with a prolonged operative time, which are traditionally considered predictors of postoperative complications, was significantly higher in the group with complications of CDc grade ≥II (22,23). Various risk factors and predictors of postoperative complications in gastrointestinal surgical diseases have been reported (24,25). However, in this study, we found that male sex (OR=2.38, p=0.02), a long operative time (OR=1.004, p<0.001), and a low Barthel index (OR=3.2, p=0.003) were independent predictors in the multivariate analysis.
The Barthel index has also been reported as a risk factor for postoperative complications in retrospective reports (8-11), consistent with the present findings. However, the Katz index was not a significant indicator in the current analysis. The Katz and Barthel indices are both methods used to assess ADL. Both indices assess similar items, but there are some differences. The difference in the multivariate analysis results may be because the Katz index is based on six assessment items, while the Barthel index is based on 10. Moreover, the Barthel index focuses on more detailed assessment points.
Although no significance was shown for the Katz index in predicting postoperative complications in the logistic regression analysis, the two CGAs can be assessed using only questionnaires, which reduces the burden on patients. If a high postoperative complication rate can be predicted before surgery, it may be possible to prevent complications and provide early detection and treatment. When the Barthel index and the Katz index were examined in our dataset, there was indeed a significant correlation between these indices (r=−0.716, p<0.001; Figure 2).
Figure 2. Correlation between the Barthel index and the Katz index. There was a significant negative correlation between the Barthel and Katz indices (r=–0.716, p<0.001).

The findings of this study should be interpreted in light of some limitations. Firstly, the present study was conducted at a single institution, which may have resulted in bias in cases and surgical techniques. Secondly, information bias may have occurred because the patients or their family members answered a questionnaire to assess ADL. Further analysis in a multicenter setting is needed to confirm the results of this study.
Conclusion
In conclusion, this study provides new insights into the usefulness of the Barthel index as a predictor of postoperative complications in older individuals undergoing elective abdominal surgery. To the best of our knowledge, this is the first prospective study to confirm the usefulness of the Barthel index in a cohort of patients undergoing elective abdominal surgery. This result may facilitate the prevention and treatment of postoperative complications by understanding the functional status of patients before treatment.
Conflicts of Interest
The Authors declare that they have no conflicts of interest. The Authors declare that they have no financial ties to disclose.
Authors’ Contributions
Study conception and design: EU and TaH. Acquisition of data: TaH, MM, YM, TM, MY, NT and TS. Analysis and interpretation of data: EU, TaH, MM, YM, NT and TS. Drafting of the manuscript: EU and TaH. Critical revision of the article: ToH and YF.
Acknowledgements
The Authors thank Emily Woodhouse, Ph.D., from Edanz (https://jp.edanz.com/ac) for editing a draft of this article.
References
- 1.Hamel MB, Henderson WG, Khuri SF, Daley J. Surgical outcomes for patients aged 80 and older: morbidity and mortality from major noncardiac surgery. J Am Geriatr Soc. 2005;53(3):424–429. doi: 10.1111/j.1532-5415.2005.53159.x. [DOI] [PubMed] [Google Scholar]
- 2.Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg. 1991;78(3):355–360. doi: 10.1002/bjs.1800780327. [DOI] [PubMed] [Google Scholar]
- 3.Hu ZW, Xin RQ, Xia YJ, Jia GP, Chen XX, Wang S. Application of POSSUM and P-POSSUM in surgical risk assessment of elderly patients undergoing hepatobiliary and pancreatic surgery. Clin Interv Aging. 2020;15:1121–1128. doi: 10.2147/CIA.S258659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gawande AA, Kwaan MR, Regenbogen SE, Lipsitz SA, Zinner MJ. An Apgar score for surgery. J Am Coll Surg. 2007;204(2):201–208. doi: 10.1016/j.jamcollsurg.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 5.Regenbogen SE, Ehrenfeld JM, Lipsitz SR, Greenberg CC, Hutter MM, Gawande AA. Utility of the surgical apgar score: validation in 4119 patients. Arch Surg. 2009;144(1):30–6. doi: 10.1001/archsurg.2008.504. discussion 37. [DOI] [PubMed] [Google Scholar]
- 6.Parker SG, McCue P, Phelps K, McCleod A, Arora S, Nockels K, Kennedy S, Roberts H, Conroy S. What is Comprehensive Geriatric Assessment (CGA)? An umbrella review. Age Ageing. 2018;47(1):149–155. doi: 10.1093/ageing/afx166. [DOI] [PubMed] [Google Scholar]
- 7.Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, Conroy SP, Kircher T, Somme D, Saltvedt I, Wald H, O’Neill D, Robinson D, Shepperd S. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. 2017;9:CD006211. doi: 10.1002/14651858.CD006211.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gleich J, Pfeufer D, Keppler AM, Mehaffey S, Fürmetz J, Böcker W, Kammerlander C, Neuerburg C. Identification of hip fracture patients at risk for postoperative mobilisation complications via handgrip strength assessment. Arch Orthop Trauma Surg. 2022;142(6):997–1002. doi: 10.1007/s00402-021-03756-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burgos E, Gómez-Arnau JI, Díez R, Muñoz L, Fernández-Guisasola J, Garcia del Valle S. Predictive value of six risk scores for outcome after surgical repair of hip fracture in elderly patients. Acta Anaesthesiol Scand. 2008;52(1):125–131. doi: 10.1111/j.1399-6576.2007.01473.x. [DOI] [PubMed] [Google Scholar]
- 10.Scarpa M, Ruffolo C, Bassi D, Boetto R, D’Incà R, Buda A, Sturniolo GC, Angriman I. Intestinal surgery for Crohn’s disease: predictors of recovery, quality of life, and costs. J Gastrointest Surg. 2009;13(12):2128–2135. doi: 10.1007/s11605-009-1044-y. [DOI] [PubMed] [Google Scholar]
- 11.Mokutani Y, Mizushima T, Yamasaki M, Rakugi H, Doki Y, Mori M. Prediction of postoperative complications following elective surgery in elderly patients with colorectal cancer using the comprehensive geriatric assessment. Dig Surg. 2016;33(6):470–477. doi: 10.1159/000446709. [DOI] [PubMed] [Google Scholar]
- 12.Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983;31(12):721–727. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- 13.Wallace M, Shelkey M, Hartford Institute for Geriatric Nursing Katz Index of Independence in Activities of Daily Living (ADL) Urol Nurs. 2007;27(1):93–94. [PubMed] [Google Scholar]
- 14.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. the index of adl: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 15.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 17.Muramatsu N, Akiyama H. Japan: super-aging society preparing for the future. Gerontologist. 2011;51(4):425–432. doi: 10.1093/geront/gnr067. [DOI] [PubMed] [Google Scholar]
- 18.Maruyama H, Kusachi S, Yoshida H, Makino H, Nishimuta H, Niitsuma T. Association of respiratory tract infection after gastroenterological surgery with postoperative duration of hospitalization and medical expenses: Subanalysis of data from a multicenter study. J Nippon Med Sch. 2020;87(5):252–259. doi: 10.1272/jnms.JNMS.2020_87-501. [DOI] [PubMed] [Google Scholar]
- 19.Kurita N, Miyata H, Gotoh M, Shimada M, Imura S, Kimura W, Tomita N, Baba H, Kitagawa Y, Sugihara K, Mori M. Risk model for distal gastrectomy when treating gastric cancer on the basis of data from 33,917 Japanese patients collected using a nationwide web-based data entry system. Ann Surg. 2015;262(2):295–303. doi: 10.1097/SLA.0000000000001127. [DOI] [PubMed] [Google Scholar]
- 20.Hasegawa H, Takahashi A, Kakeji Y, Ueno H, Eguchi S, Endo I, Sasaki A, Takiguchi S, Takeuchi H, Hashimoto M, Horiguchi A, Masaki T, Marubashi S, Yoshida K, Konno H, Gotoh M, Miyata H, Seto Y. Surgical outcomes of gastroenterological surgery in Japan: Report of the National Clinical Database 2011-2017. Ann Gastroenterol Surg. 2019;3(4):426–450. doi: 10.1002/ags3.12258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu LL, Leung JM. Predicting adverse postoperative outcomes in patients aged 80 years or older. J Am Geriatr Soc. 2000;48(4):405–412. doi: 10.1111/j.1532-5415.2000.tb04698.x. [DOI] [PubMed] [Google Scholar]
- 22.Matsuda A, Yamada M, Matsumoto S, Sakurazawa N, Yamada T, Matsutani T, Miyashita M, Uchida E. Lysophosphatidylcholine as a predictor of postoperative complications after colorectal cancer surgery. Surg Today. 2018;48(10):936–943. doi: 10.1007/s00595-018-1675-2. [DOI] [PubMed] [Google Scholar]
- 23.Yokozuka K, Tomita K, Nakagawa M, Koganezawa I, Ochiai S, Gunji T, Ozawa Y, Hikita K, Kobayashi T, Sano T, Tabuchi S, Chiba N, Hidaka E, Kawachi S. New risk factors of postoperative complications in elective gastrointestinal surgery of elderly patients: a prospective cohort study. BMC Surg. 2021;21(1):173. doi: 10.1186/s12893-021-01171-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kondo H, Hirano Y, Ishii T, Hara K, Obara N, Wang L, Asari M, Kato T, Yamaguchi S. E-PASS scoring system may be useful for prediction of postoperative complications in super elderly colorectal cancer surgery patients. J Anus Rectum Colon. 2020;4(3):137–144. doi: 10.23922/jarc.2020-017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kanda M. Preoperative predictors of postoperative complications after gastric cancer resection. Surg Today. 2020;50(1):3–11. doi: 10.1007/s00595-019-01877-8. [DOI] [PMC free article] [PubMed] [Google Scholar]