Abstract
Background
Photodynamic therapy (PDT) is a noninvasive treatment for patients with superficial basal-cell carcinoma (sBCC). The efficacy of PDT may vary with different photosensitizers and treatment schedules.
Objective
Our objective was to evaluate whether fractionated 5-aminolevulinic acid 20% (ALA)-PDT is superior to conventional two-stage methyl aminolevulinate (MAL)-PDT for sBCC.
Methods
We present the 5 years results of a single-blind, randomized, multicenter trial. 162 patients with a histologically confirmed primary sBCC were randomized to fractionated ALA-PDT or MAL-PDT.
Results
The 5-year tumor-free survival rate was 70.7% (95% CI 58.2–80.1%) for ALA-PDT and 76.5% (95% CI 64.4–85.0%) for MAL-PDT. In the first 3 years, there was no significant difference in risk of treatment failure (HR = 1.53, p = 0.283), but in the long-term, the risk of recurrence was significantly lower following MAL-PDT compared to ALA-PDT (HR = 0.125, p = 0.049). As judged by patients, the esthetic result was good-excellent in 96.8% (61/63) and 94.4% (56/59) of patients treated with ALA-PDT and MAL-PDT, respectively (p = 0.631).
Conclusion
The long-term efficacy is significantly higher for conventional two-stage MAL-PDT than for fractionated ALA-PDT, whereas there was no significant difference in esthetic outcome between the treatments at 5 years after treatment. These results indicate that fractionated ALA-PDT offers no benefit over conventional two-stage MAL-PDT.
Keywords: Superficial basal-cell carcinoma, Photodynamic therapy, Tumor-free survival, Cosmetic result, Long-term analysis, Light fractionation
Introduction
Noninvasive treatments are increasingly used to treat superficial basal-cell carcinomas (sBCC) [1, 2]. Photodynamic therapy (PDT) is an option for patients who do not opt for surgery or are not able to apply cream, and leads to excellent cosmetic results [3, 4, 5]. However, in a trial comparing treatments of patients with sBCC with imiquimod, 5-fluorouracil, or PDT, methyl aminolevulinate (MAL)-PDT was the least effective treatment option. Therefore, optimization of PDT is needed [6, 7].
Several studies showed that the efficacy of 5-aminolevulinic acid (ALA)-PDT was optimal using fractionated illuminations with a 2-hour dark period in between and a low fluence rate during the first illumination followed by a high fluence rate during the second illumination [8, 9, 10, 11, 12]. In a previous paper, we reported on the results of a randomized trial with head-to-head comparison of ALA-PDT and MAL-PDT in patients with sBCC. The 1-year probability of remaining free from treatment failure was 92.3% after fractionated ALA-PDT versus 83.4% after MAL-PDT (p = 0.091) [13]. The aim of the current study was to compare the 5-year efficacy of treatment with MAL-PDT versus fractionated ALA-PDT.
Methods
Patients participating in the randomized trial were treated between September 2013 and May 2015 and were recruited in three hospitals in the Netherlands. The study protocol and exact treatment schemes were described in detail by Kessels et al. [13]. All tumors were histologically confirmed sBCC which was defined as an epidermal tumor existing of small, discrete islands of basaloid cells with peripheral palisading and stromal retraction, presenting intermittently along the basal layer of the epidermis [14].
In the ALA group, 5-ALA 20% ointment was applied; after a 4-hour coverage, the tumor was illuminated with a light-emitting diode light source using a wavelength of ∼630 nm ± 5 nm and a fluence of 20 J cm−2 for 4 min at an irradiance of 50 mW cm−2. The area was covered for 2 h and illuminated again with a fluence of 80 J cm−2 for 18 min. In the MAL-PDT group, Metvix® ointment was applied, covered for 3 h, and illuminated with either Aktilite or Omnilux with a fluence of 37 J cm−2 at an irradiance of 75 mW cm−2 for 7 min. This regimen was repeated after 1 week (conventional two-stage regimen).
The outcome of primary interest in this follow-up study was the 5-year probability of remaining free from histologically confirmed recurrent BCC. The esthetic result at 5 years post-treatment measured on a 4-point scale (excellent, good, fair, poor) was also evaluated by both patient and physician. For this study, a follow-up visit was planned at 60 months after treatment. The site of the treated sBCC was evaluated by one investigator (L.C.J.v.D.) who was blinded to treatment assignment.
The study was approved by the ethics board of the EMC Rotterdam and was performed in accordance with the Declaration of Helsinki. The trial was registered at clinicaltrials.gov (NCT01491711).
Statistical Analysis
Kaplan-Meier survival analyses were performed to estimate the 5-year cumulative probability of remaining free from treatment failure. The Cox proportional hazards assumption was tested on the basis of Schoenfeld residuals. If the proportional hazard assumption does not hold, hazard ratios are not constant over time. Consequently, period-specific hazard ratios and corresponding p values have to be calculated with Cox regression analysis with time-varying covariates using an interaction term for treatment and time.
Percentages of patients with good-excellent esthetic results were compared using the χ2 test. p values ≤0.05 were considered to indicate significance. All data were analyzed using SPSS version 23.0 (IBM, Armonk, NY, USA), openepi.com or Stata version 14.0 (Stata Corp, College Station, TX, USA).
Results
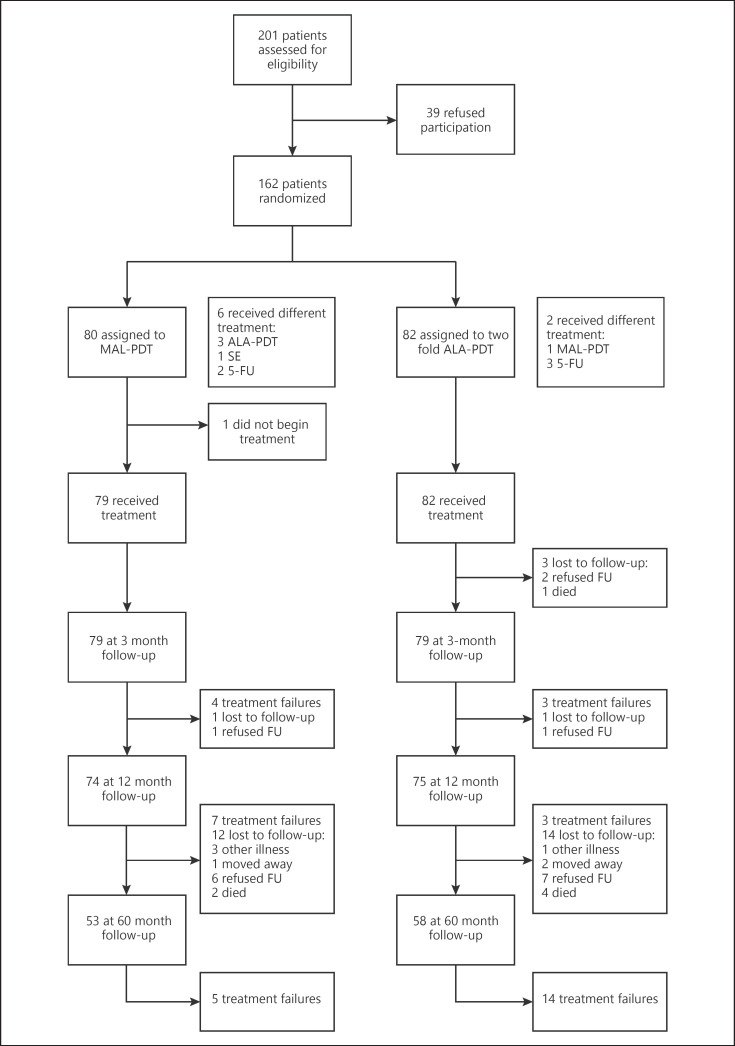
Figure 1 shows the patient flow until 5 years of follow-up. Thirty-one patients were lost to follow-up (19.3%) of whom 13 were treated with MAL-PDT and 18 with ALA-PDT. In 20 patients who consulted their dermatologist before the planned study visit at 60 months, a recurrent BCC was diagnosed between 12 and 60 months.
Fig. 1.
Patient flowchart. ALA, aminolevulinic acid; MAL, methyl aminolevulinate; PDT, photodynamic therapy; 5-FU, 5-fluorouracil; SE, surgical excision; FU, follow-up.
Comparison of baseline characteristics between the randomized groups (Table 1) shows that there were minor imbalances in the distribution of the study center and tumor location [13]. According to the intention-to-treat analysis, at 5-year follow-up, 20 treatment failures had occurred after treatment with ALA-PDT of which 14 were diagnosed after the first year of follow-up. Following MAL-PDT, 16 treatment failures were observed; 5 were diagnosed after 1 year.
Table 1.
Baseline characteristics of participants with sBCC
| MAL-PDT (N = 80) | Fractionated ALA-PDT (N = 82) | |
|---|---|---|
| Mean age, years (range) | 63.6 (28–83) | 65.9 (38–85) |
| Sex, N (%) | ||
| Male | 35 (44) | 40 (49) |
| Female | 45 (56) | 42 (51) |
| Study center, N (%) | ||
| MUMC+ | 27 (34) | 35 (43) |
| EMC | 34 (43) | 26 (32) |
| VCMC | 19 (24) | 21 (26) |
| Tumor location, N (%) | ||
| Head/neck | 1 (1) | 7 (8) |
| Trunk | 58 (73) | 45 (55) |
| Upper extremities | 7 (9) | 16 (20) |
| Lower extremities | 14 (18) | 14 (17) |
| Mean tumor size, mm (±SD) | 11.2 (±7.1) | 10.8 (±5.3) |
MAL, methyl aminolevulinate; PDT, photodynamic therapy; ALA, aminolevulinic acid; MUMC+, Maastricht University Medical center+; EMC, Erasmus Medical Centre; VCMC, VieCuri Medical Center.
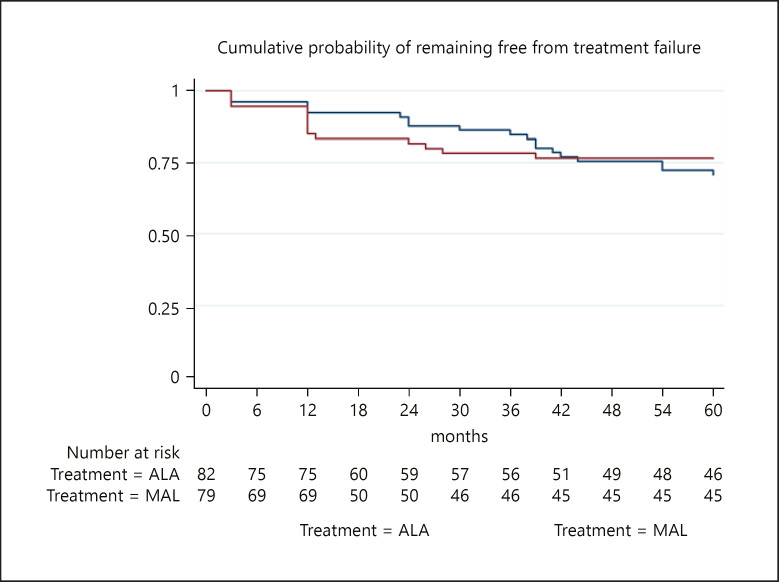
The survival curves (Fig. 2) show that in the first years of follow-up, the cumulative probability of tumor-free survival was higher for ALA-PDT than for MAL-PDT, but at 5 years, the cumulative probability was 76.5% (95% confidence interval [CI] 64.4–85.0%) in the MAL-PDT group and 70.7% (95% CI 58.2–80.1%) in the ALA-PDT group (Table 2). The survival curves intersect at around 3 years post-treatment, and the proportional hazard assumption did not hold (p = 0.006). Therefore, period-specific HRs for treatment failure with p values were calculated for the first 3 years and last 2 years of follow-up. Within the first period, the HR (for MAL-PDT vs. ALA-PDT) was 1.53 (95% CI: 0.70–3.33, p = 0.283). Within the second period, the HR was 0.123 (95% CI: 0.016–0.987, p = 0.049), indicating a significantly lower risk of treatment failure in the MAL-PDT group later during follow-up. A per protocol analysis gave similar results.
Fig. 2.
Cumulative probability of tumor-free survival 5 years after treatment with MAL-PDT and fractionated ALA-PDT for sBCC. Intention-to-treat analysis. ALA, aminolevulinic acid; MAL, methyl aminolevulinate.
Table 2.
Cumulative probability of tumor-free survival at 1 and 5 years after treatment with MAL-PDT or fractionated ALA-PDT for sBCC
| MAL-PDT |
ALA-PDT |
|||
|---|---|---|---|---|
| ITT% (95% CI) | PP% (95% CI) | ITT% (95% CI) | PP% (95% CI) | |
| 1 year | 83.4% (73.1–90.0) | 83.4% (73.1–90.0) | 92.3% (83.7–96.5) | 91.9% (82.9–96.3) |
| 5 years | 76.5% (64.4–85.0) | 76.9% (64.9–85.2) | 70.7% (58.2–80.1) | 69.8% (57.1–79.4) |
ALA, aminolevulinic acid; MAL, methyl aminolevulinate; PDT, photodynamic therapy; ITT, intention to treat; PP, per protocol; CI, confidence interval.
The esthetic result 5 years after treatment as judged by patients was good-excellent in 96.8% (61/63) following ALA-PDT and 94.4% (56/59) after MAL-PDT (p = 0.631). According to the judgment of the physician (L.C.J. v. D.), the esthetic result was good-excellent in 73.1% (46/63) after ALA-PDT and 83.1% (49/59) following MAL-PDT (p = 0.191). In an additional analysis which was restricted to patients without treatment failure, 100% of the patients scored the cosmetic results as good-excellent in both the MAL-PDT and ALA-PDT group.
Discussion
The results of this randomized trial do not support the hypothesis that fractionated ALA-PDT is more effective than conventional two-stage MAL-PDT. In the last 2-year period, the risk of treatment failure in the MAL-PDT group was significantly lower than in the ALA-PDT group.
A former randomized trial by Jansen et al. [6] comparing three noninvasive therapies for sBCC showed less favorable results for conventional two-stage MAL-PDT. The 5-year probability of recurrence-free survival after MAL-PDT was only 62.7% compared to 76.5% in this study. An explanation may be that in the study by Jansen et al. [6], sBCCs were more frequently (12%) located in the head and neck area than in this study (1.3%). Prior research showed that recurrences in the head and neck area following noninvasive treatment are more often of a mixed or nonsuperficial subtype and thus more susceptible to misclassification and consequently, undertreatment [15, 16, 17, 18]. Between-study differences in characteristics of study populations are the reason that it is important to perform head-to-head comparisons of therapies.
We described in our previous publication that treatment with ALA-PDT led to more side effects and pain/burning sensation during treatment [13]. Advantages of ALA-cream are that, in The Netherlands, it is cheaper than MAL-cream (Metvix; Galderma) and has to be applied only once. It could be advantageous for patients with decreased mobility because only one hospital visit is needed. However, these advantages do not seem to outweigh the disadvantages.
A limitation of this study was that due to the COVID pandemic, 9 patients (6 with ALA-PDT and 3 with MAL-PDT) had their final follow-up visit later than planned. However, this limitation had no impact on the results because none of these patients had a recurrence.
Conclusion
This study shows that the long-term efficacy is significantly higher for conventional two-stage MAL-PDT than for fractionated ALA-PDT, whereas there was no statistically significant difference in the esthetic outcome between conventional two-stage MAL-PDT or fractionated ALA-PDT.
Key Message
Long-term efficacy of methyl aminolevulinate photodynamic therapy (PDT) for superficial basal-cell carcinoma is significantly higher compared to fractionated 5-aminolevulinic acid-PDT.
Statement of Ethics
The study was approved by the institutional review board of the Erasmus Medical Center, Rotterdam. The trial was registered at clinicaltrials.gov (NCT01491711).
Conflict of Interest Statement
There were no conflicts of interest for any of the authors.
Funding Sources
This study was funded by a grant from the Health Foundation Limburg, the Netherlands. The funding source was not involved in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Author Contributions
Conceptualization (ideas; formulation or evolution of overarching research goals and aims): N.W.J.K.-S., P.J.N., J.P.H.M.K., K.M., E.R.M.d.H., M.H.R., and H.K. Data curation (management activities to annotate [produce metadata], scrub data and maintain research data [including software code, where it is necessary for interpreting the data itself] for initial use and later reuse): J.P.H.M.K. Formal analysis (application of statistical, mathematical, computational, or other formal techniques to analyze or synthesize study data): L.C.J.v.D. and P.J.N. Funding acquisition (acquisition of the financial support for the project leading to this publication): J.P.H.M.K., N.W.J.K.-S., and M.H.R. Investigation (conducting a research and investigation process, specifically performing the experiments, or data/evidence collection): L.C.J.v.D., J.P.H.M.K., and H.K. Methodology (development or design of methodology; creation of models): J.P.H.M.K., M.H.R., H.K., and P.J.N. Project administration (management and coordination responsibility for the research activity planning and execution): L.C.J.v.D., J.P.H.M.K., and H.K. Resources (provision of study materials, reagents, materials, patients, laboratory samples, animals, instrumentation, computing resources, or other analysis tools): M.J.M.d.R., N.W.J.K.-S., and E.R.M.d.H. Supervision (oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team): N.W.J.K.-S, E.R.M.d.H., K.M., P.J.N., and M.J.M.d.R. Validation (verification, whether as a part of the activity or separate, of the overall replication/reproducibility of results/experiments and other research outputs): L.C.J.v.D. and P.J.N. Visualization (preparation, creation, and/or presentation of the published work, specifically visualization/data presentation): L.C.J.v.D. and P.J.N. Writing − original draft preparation (creation and/or presentation of the published work, specifically writing the initial draft [including substantive translation]): L.C.J.v.D. Writing − review and editing (preparation, creation, and/or presentation of the published work by those from the original research group, specifically critical review, commentary, or revision − including pre- or post-publication stages): P.J.N., J.P.H.M.K., H.K., E.R.M.d.H., N.W.J.K.-S., K.M., M.J.M.d.R., and M.H.R.
Data Availability Statement
The data that support the findings of this study are not publicly available because these documents contain information that could compromise the privacy of research participants but are available from L.C.J.v.D. or N.W.J.K.-S. upon reasonable request.
Acknowledgments
We would like to thank all the patients who participated in follow-up and the nurses from all the hospitals for performing PDT treatments and planning.
Funding Statement
This study was funded by a grant from the Health Foundation Limburg, the Netherlands. The funding source was not involved in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
References
- 1.Peris K, Fargnoli MC, Garbe C, Kaufmann R, Bastholt L, Seguin NB, et al. Diagnosis and treatment of basal cell carcinoma: European consensus-based interdisciplinary guidelines. Eur J Cancer. 2019;118:10–34. doi: 10.1016/j.ejca.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 2.Work Group; Invited Reviewers. Kim JYS, Kozlow JH, Mittal B, Moyer J, Olencki T, et al. Guidelines of care for the management of basal cell carcinoma. J Am Acad Dermatol. 2018;78((3)):540–559. doi: 10.1016/j.jaad.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Jansen MHE, Koekelkoren FHJ, Nelemans PJ, Arits AHMM, Roozeboom MH, Kelleners-Smeets NWJ, et al. Comparison of long-term cosmetic outcomes for different treatments of superficial basal cell carcinoma. J Am Acad Dermatol. 2018;79((5)):961–964. doi: 10.1016/j.jaad.2018.04.053. [DOI] [PubMed] [Google Scholar]
- 4.Cosgarea R, Susan M, Crisan M, Senila S. Photodynamic therapy using topical 5-aminolaevulinic acid vs. surgery for basal cell carcinoma. J Eur Acad Dermatol Venereol. 2013;27((8)):980–984. doi: 10.1111/j.1468-3083.2012.04619.x. [DOI] [PubMed] [Google Scholar]
- 5.Morton CA, Szeimies RM, Basset-Séguin N, Calzavara-Pinton PG, Gilaberte Y, Haedersdal M, et al. European Dermatology Forum guidelines on topical photodynamic therapy 2019 part 2: emerging indications − field cancerization, photorejuvenation and inflammatory/infective dermatoses. J Eur Acad Dermatol Venereol. 2020;34((1)):17–29. doi: 10.1111/jdv.16044. [DOI] [PubMed] [Google Scholar]
- 6.Jansen MHE, Mosterd K, Arits AHMM, Roozeboom MH, Sommer A, Essers BAB, et al. Five-year results of a randomized controlled trial comparing effectiveness of photodynamic therapy, topical imiquimod, and topical 5-fluorouracil in patients with superficial basal cell carcinoma. J Invest Dermatol. 2018;138((3)):527–533. doi: 10.1016/j.jid.2017.09.033. [DOI] [PubMed] [Google Scholar]
- 7.Arits AH, Spoorenberg E, Mosterd K, Nelemans P, Kelleners-Smeets NW, Essers BA. Cost-effectiveness of topical imiquimod and fluorouracil vs. photodynamic therapy for treatment of superficial basal-cell carcinoma. Br J Dermatol. 2014;171((6)):1501–1507. doi: 10.1111/bjd.13066. [DOI] [PubMed] [Google Scholar]
- 8.de Bruijn HS, van der Veen N, Robinson DJ, Star WM. Improvement of systemic 5-aminolevulinic acid-based photodynamic therapy in vivo using light fractionation with a 75-minute interval. Cancer Res. 1999;59((4)):901–904. [PubMed] [Google Scholar]
- 9.van der Veen N, Hebeda KM, de Bruijn HS, Star WM. Photodynamic effectiveness and vasoconstriction in hairless mouse skin after topical 5-aminolevulinic acid and single- or two-fold illumination. Photochem Photobiol. 1999;70((6)):921–929. [PubMed] [Google Scholar]
- 10.Robinson DJ, de Bruijn HS, de Wolf WJ, Sterenborg HJ, Star WM. Topical 5-aminolevulinic acid-photodynamic therapy of hairless mouse skin using two-fold illumination schemes: PpIX fluorescence kinetics, photobleaching and biological effect. Photochem Photobiol. 2000;72((6)):794–802. doi: 10.1562/0031-8655(2000)072<0794:TAAPTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Star WM, Veen AJ, Robinson DJ, Munte K, de Haas ERM, Sterenborg HJCM. Topical 5-aminolevulinic acid mediated photodynamic therapy of superficial basal cell carcinoma using two light fractions with a two-hour interval: long-term follow-up. Acta Derm Venereol. 2006;86((5)):412–417. doi: 10.2340/00015555-0129. [DOI] [PubMed] [Google Scholar]
- 12.de Vijlder HC, Sterenborg HJ, Neumann HA, Robinson DJ, de Haas ER. Light fractionation significantly improves the response of superficial basal cell carcinoma to aminolaevulinic acid photodynamic therapy: five-year follow-up of a randomized, prospective trial. Acta Derm Venereol. 2012;92((6)):641–647. doi: 10.2340/00015555-1448. [DOI] [PubMed] [Google Scholar]
- 13.Kessels J, Kreukels H, Nelemans PJ, Roozeboom MH, van Pelt H, Mosterd K, et al. Treatment of superficial basal cell carcinoma by topical photodynamic therapy with fractionated 5-aminolaevulinic acid 20% vs. two-stage topical methyl aminolaevulinate: results of a randomized controlled trial. Br J Dermatol. 2018;178((5)):1056–1063. doi: 10.1111/bjd.15967. [DOI] [PubMed] [Google Scholar]
- 14.Barnhill RL, Crowson A, Magro CM, Piepkorn MW, Kutzner H, Desman GT. Barnhill's dermatopathology. 4th ed. Europe: McGraw-Hill Education; 2020. Available from: https://dermatology.mhmedical.com/content.aspx?bookid=2802§ionid=238125243 (accessed May 2, 2022) [Google Scholar]
- 15.Fiechter S, Skaria A, Nievergelt H, Anex R, Borradori L, Parmentier L. Facial basal cell carcinomas recurring after photodynamic therapy: a retrospective analysis of histological subtypes. Dermatology. 2012;224((4)):346–351. doi: 10.1159/000339335. [DOI] [PubMed] [Google Scholar]
- 16.Skaria AM. Facial basal cell carcinomas recurring after imiquimod therapy. Dermatology. 2013;226((1)):13–14. doi: 10.1159/000345763. [DOI] [PubMed] [Google Scholar]
- 17.van Delft LCJ, Nelemans PJ, Jansen MHE, Arits AHMM, Roozeboom MH, Hamid MA, et al. Histologic subtype of treatment failures after noninvasive therapy for superficial basal cell carcinoma: an observational study. J Am Acad Dermatol. 2019;80((4)):1022–1028. doi: 10.1016/j.jaad.2018.12.028. [DOI] [PubMed] [Google Scholar]
- 18.Devine C, Srinivasan B, Sayan A, Ilankovan V. Epidemiology of basal cell carcinoma: a 10-year comparative study. Br J Oral Maxillofac Surg. 2018;56((2)):101–106. doi: 10.1016/j.bjoms.2017.11.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are not publicly available because these documents contain information that could compromise the privacy of research participants but are available from L.C.J.v.D. or N.W.J.K.-S. upon reasonable request.