Abstract
This scoping review identified observational studies of adults that utilized accelerometry to assess physical activity and sedentary behavior. Key elements on accelerometry data collection were abstracted to describe current practices and completeness of reporting. We searched three databases (PubMed, Web of Science, and SPORTDiscus) on June 1, 2021 for articles published up to that date. We included studies of non-institutionalized adults with an analytic sample size of at least 500. The search returned 5686 unique records. After reviewing 1027 full-text publications, we identified and abstracted accelerometry characteristics on 155 unique observational studies (154 cross-sectional/cohort studies and 1 case control study). The countries with the highest number of studies included the United States, the United Kingdom, and Japan. Fewer studies were identified from the continent of Africa. Five of these studies were distributed donor studies, where participants connected their devices to an application and voluntarily shared data with researchers. Data collection occurred between 1999 to 2019. Most studies used one accelerometer (94.2%), but 8 studies (5.2%) used 2 accelerometers and 1 study (0.6%) used 4 accelerometers. Accelerometers were more commonly worn on the hip (48.4%) as compared to the wrist (22.3%), thigh (5.4%), other locations (14.9%), or not reported (9.0%). Overall, 12.7% of the accelerometers collected raw accelerations and 44.6% were worn for 24 hours/day throughout the collection period. The review identified 155 observational studies of adults that collected accelerometry, utilizing a wide range of accelerometer data processing methods. Researchers inconsistently reported key aspects of the process from collection to analysis, which needs addressing to support accurate comparisons across studies.
Introduction
“Accelerometry” refers to device-based motion sensors that provide detailed movement information by capturing changes in a person’s gravitational acceleration in space [1]. The first accelerometers, developed in the 1920’s, weighed about one pound and measured the vibration of aircraft and large structures such as bridges [2]. In the 1950’s, accelerometers measured gait velocity [3], and by the 1970’s their potential for measurement of human movement was recognized [4]. Researchers began adopting accelerometry as an indicator of physical activity in the 1980’s, and Troiano et al. [5] estimated that they have been used in epidemiologic studies for research and surveillance since the mid-1990’s. A number of technologic advances in accelerometry sensors occurred since the 1990’s, including increased storage, longer battery life, wider acceleration range, waterproofing, and smaller size [1, 5]. These technologic advances, along with the relative improvement in cost and validity over time of the device to represent physical activity and sedentary behavior, contributed to subsequent rise in the application of the device by researchers.
The use of accelerometry to measure physical activity and sedentary behavior (together referred to as “physical behavior”) was a significant milestone in the field. Accelerometers enabled measurement of detailed components of the behaviors in conditions where self-reports were not possible (i.e., young age, cognitive impairment, assessment of light physical activity, or bouts of physical activity) and allowed for both cross-language and cross-population comparisons. Entire networks, such as the International Physical Activity and the Environment Network (IPEN; https://www.ipenproject.org/) and the Prospective Physical Activity, Sitting, and Sleep consortium (ProPASS; https://www.propassconsortium.org/), facilitate harmonization of accelerometer methods and data analysis between global research endeavors. However, not enough effort has been dedicated to fully understanding where and how physical behavior research using accelerometers is happening. Systematically cataloging these studies and their reporting methods has the potential to increase global collaborations and harmonization efforts.
While the use of accelerometry expanded over the last four decades, reporting in scientific studies on key aspects of the devices and decisions made in processing the data remains inconsistent. Calls for improvement in reporting date back to at least 2004, at an international meeting focused on accelerometry measurement for physical activity. The conference recommended that researchers state their decision rules for collecting, processing, and analyzing the data, and that they work towards developing common practices and guidance [6, 7]. More complete reporting of accelerometry methods is necessary in order to compare across studies, and promote standardized decision rules to facilitate future harmonization with studies using these devices, such as in meta analyses [8–10]. Several seminal papers on best practices using accelerometry in population-based research provide guidance on key accelerometry information to report, such as the number of participants enrolled and accelerometry wear and nonwear definitions [11, 12]. It is not known how well studies follow these accelerometry reporting guidelines.
To address these issues, we conducted a scoping review to identify and describe observational studies that utilized accelerometry to assess physical activity and sedentary behavior. From the studies found, we abstracted key study information and then applied an accelerometry reporting tool to describe the completeness of describing key information [13]. This work was done in order to describe the current state of the science and reporting practices for accelerometry, and to identify and facilitate future global collaborations and harmonization across studies.
Materials and methods
Search methods
The systematic review protocol was developed in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) statement [14]. The PRISMA Scoping Review checklist [15] can be found in S1 File. Since this review focused on accelerometry measurement and was a scoping rather than systematic review [16], it did not fit the current criteria to register with PROSPERO [17]. We searched three databases (PubMed, Web of Science, and SPORTDiscus) on June 1, 2021 for articles published up to that date, with the search strategy detailed in S2 File. After removing duplicate citations, two authors independently screened all titles/abstracts and full-text articles for inclusion using Covidence systematic review software (www.covidence.org; Veritas Health Innovation, Melbourne, Australia) with discrepancies resolved by consensus.
Inclusion and exclusion criteria
Inclusion criteria included observational studies, including surveillance studies, with analytical sample sizes of at least 500 community-dwelling adults 18 years and older who wore an accelerometer for the purposes of collecting physical activity and sedentary behavior. We included studies that used accelerometry to collect physical activity (including steps) or sedentary behavior, regardless of whether raw or proprietary-based metrics were used. Studies needed to be described in full-length peer-reviewed papers in English. If there was more than one publication identifying a single study that met our criteria for inclusion, then we included one publication to represent the study, using the study that provided the most information we were abstracting. If needed, we sought missing information from other publications captured by the search.
In cases in which a protocol was referenced in the main paper, information was also abstracted from the protocol. We reviewed all publications identified for each study to determine the best source paper. For example, we identified 29 papers that published on the United Kingdom Biobank Study, but only one was included in the sample. Several publications identified in our search included data from multiple studies in a single publication; as long as the unique study met inclusion criteria, they were retained. Surveillance studies that recruited a unique set of participants for each wave were included as separate studies. For example, NHANES 2003–2004 [18] and NHANES 2005–2006 [19] were counted as separate studies. For cohort studies with multiple waves of accelerometer data collection, we did not count multiple waves as separate studies.
We excluded publications in the grey literature, abstracts, dissertations, and conference proceedings. We excluded studies of hospitalized or institutionalized adults, or samples that gave consent by proxy, as well as studies of youth (children or adolescents <18 years of age). We excluded intervention studies (i.e., randomized trials, quasi-experimental trials), unless there was a new consent process that enrolled participants into an observational study. We excluded studies that used spring-levered pedometers, but included pedometers that used accelerometry, as further distinguished elsewhere [20]. Studies that collected accelerometry, but did not report on physical behaviors, were excluded. For example, Scarlett et al. [21] collected accelerometry data but only used it to describe sleep, and was therefore excluded. If a publication met multiple exclusion criteria, it was excluded in the priority order in which they appear in Fig 1.
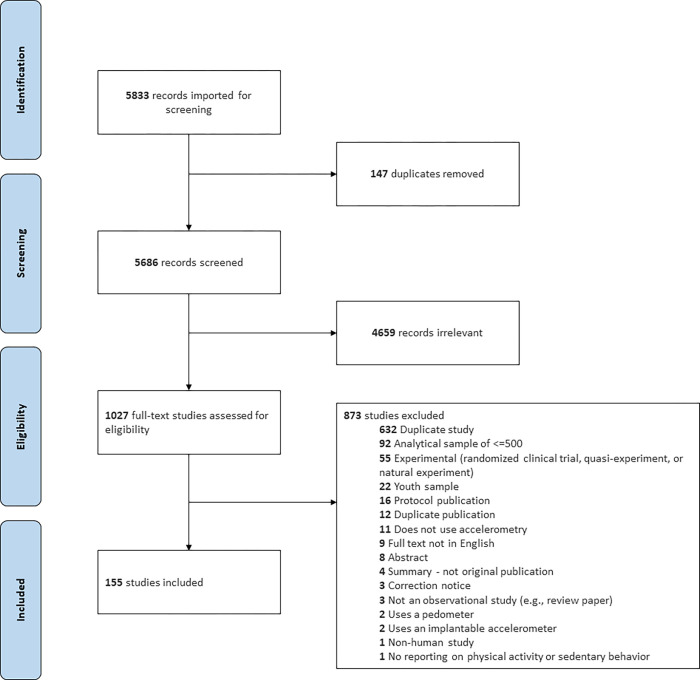
Fig 1. PRISMA chart displaying the identification, screening, eligibility and inclusion for each study reviewed.
In total, 155 studies were included from 154 publications. One publication included two studies (Dutch Longitudinal Internet Studies for Social Sciences and Understanding America Study) that were not mentioned in other identified publications.
Abstraction
Using Covidence software, one rater abstracted the information and a second rater checked the abstraction, with discrepancies resolved by consensus. The abstraction tool included the following domains: study information (e.g., study design, gender, country, years of accelerometry collection, population-based sampling, sample weights used, logbook kept, number of accelerometers worn, analytic sample size), brand and settings (e.g., sampling frequency, epoch length), method of distribution, and method of return. If years of accelerometry collection was missing, we made an attempt to contact the authors for the information. We counted a study as using population-based sampling if the sampling frame was clearly defined and allowed for inference to an underlying reference population. If the geography that the sample came from was well defined, regardless of how small it was, we counted it. Sampling from schools or clinics was not included unless all schools or clinics from a defined geographic area were part of the sampling frame. We identified a data collection protocol as being a “distributed donor” if participants connected their own commercial devices that contained an accelerometer (e.g., Fitbit) to an application to share their data with researchers.
We also collected accelerometer wear (e.g., days of data collection, days required, wear protocol, diary used), nonwear (e.g., criteria to define nonwear, adherent days of wear for analysis, adherent time of wear for analysis, weekend wear), placement, and attachment. For nonwear algorithms, when the Choi algorithm was referenced [22], we assumed that nonwear was defined as > = 90 consecutive minutes of zero counts, with a movement window of up to 2 minutes and an upstream and downstream window of 30 minutes. Similarly, when the NHANES algorithm was referenced [23], we assumed that nonwear was defined by an interval of > = 60 consecutive minutes of zero counts with a movement window up to 2 minutes between 0–100 counts/minute. When abstracting analytic sample size, in cases where multiple accelerometers were worn, we reported on the largest sample size for one accelerometer.
A random sample of 49 studies was selected for further contact using two attempts with at least two different people associated with the study. Studies were selected with probability proportional to the number of publications identified from the search that belonged to the study and stratified by region. For these 49 studies, an intake sheet was created with abstracted information about accelerometry from all publications and the study website. In total, 26 responded by reviewing, correcting, or completing missing accelerometry information.
When assessing the completeness of reporting, we applied the accelerometry reporting tool developed by Montoye et al. [13] to the data we extracted from the published papers. Specifically for the scoring of the tool, we did not include supplemental information obtained through study contact with 26 studies. The reporting tool included 12 items: 7 questions on accelerometer information, 4 questions on data processing and interpretation, and 1 question on protocol non-compliance which we modified for our purposes (S3 File).
Analysis
Analyses were conducted by study (n = 155) and by accelerometer (n = 166), as some studies had participants wear multiple accelerometers, and sometimes multiple brands. These two datasets are publicly accessible elsewhere [24]. In this review, percentages were reported for categorical variables and means with standard deviations were reported for continuous variables. These analyses were conducted in SAS (Cary, North Carolina). We created a map to indicate location using the rworldmap package in R [25, 26].
Results
Study selection
A total of 5686 records were screened with 1027 full-text studies assessed for eligibility. Among those, 873 were excluded, resulting in a final list of 155 unique observational studies of adults using accelerometry to measure physical activity or sedentary behavior (Fig 1) [27–175]. Four publications referred to more than one included study [52, 53, 110, 164]. Most of the 873 studies were excluded because they represented a publication from a study we already included (n = 632), but other common reasons included an analytic sample size of less than 500 (n = 92), experimental study design (n = 53), or a youth sample less than 18 years without at least 500 adults (n = 22). Other reasons can be found in Fig 1.
Study description
From 155 included observational studies, all were cross-sectional or cohort except for 1 case control study. Five (3.2%) studies, all published in 2020–2021, utilized a distributed donor protocol, whereby participants in the study remotely connected their personal device with an accelerometer to an application to share accelerometer data with researchers (Table 1). Overall, 8.4% of the studies enrolled females only, while 2.6% enrolled males only.
Table 1. Description of observational studies of adults collecting accelerometry (n = 155).
| Overall | ||
|---|---|---|
| Description | % | n |
| Starting year of data collection: | ||
| 1999–2004 | 5.2 | 8 |
| 2005–2009 | 30.3 | 47 |
| 2010–2014 | 40.0 | 62 |
| 2015–2021 | 24.5 | 38 |
| Distributed donor protocol: | ||
| Yes | 3.2 | 5 |
| No | 96.8 | 150 |
| Gender: | ||
| Male | 2.6 | 4 |
| Female | 8.4 | 13 |
| Male and Female | 89.0 | 138 |
| Population based: | ||
| Yes | 51.0 | 79 |
| No or not indicated | 49.0 | 76 |
| Sample weights used: | ||
| Yes | 12.9 | 20 |
| No or not indicated | 87.1 | 135 |
| Analytic sample size*: | ||
| 500–700 | 24.5 | 38 |
| 701–1000 | 22.6 | 35 |
| 1001–2250 | 27.1 | 42 |
| > 2250 | 25.8 | 40 |
| Log book kept: | ||
| Yes | 29.7 | 46 |
| No or not indicated | 70.3 | 109 |
| Number of accelerometers worn: | ||
| 1 | 94.2 | 146 |
| 2 | 5.2 | 8 |
| 3 | 0.0 | 0 |
| 4 | 0.6 | 1 |
*In a few cases, the analytic sample size may include youths less than 18 years of age.
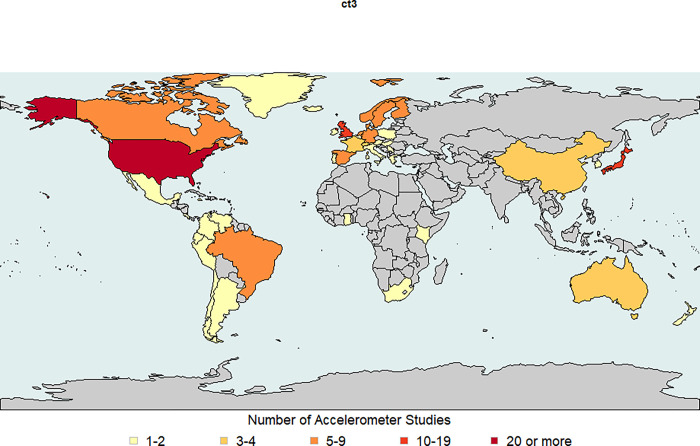
Accelerometry collection occurred in 31 countries, in addition to 7 studies that collected in more than one country (S4 File). Fig 2 displays the country where participants lived, revealing a high number of studies in Japan (n = 16), the United Kingdom (including England, Scotland, Wales, and Northern Ireland) (n = 16), and the United States (n = 43). The continents of Africa, Asia (with the exception of Japan), and Australia had much lower representation.
Fig 2. World map displaying the frequency of accelerometry studies found by country (n = 150).
This map does not include the 5 distributed donor studies. England, Scotland, Wales, and Northern Ireland were mapped as the United Kingdom. Republished from [26] under a CC BY license, with permission from Dr. Andy South, original copyright 2011.
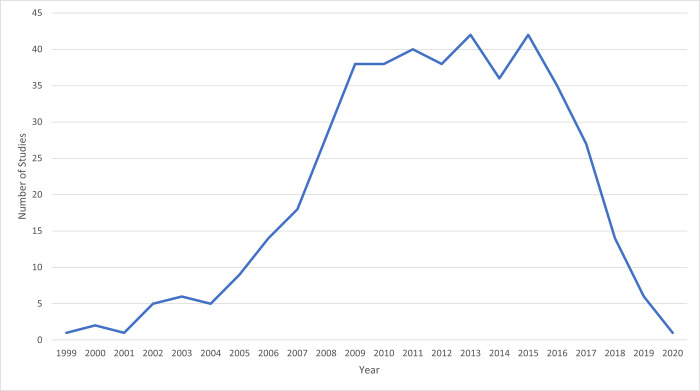
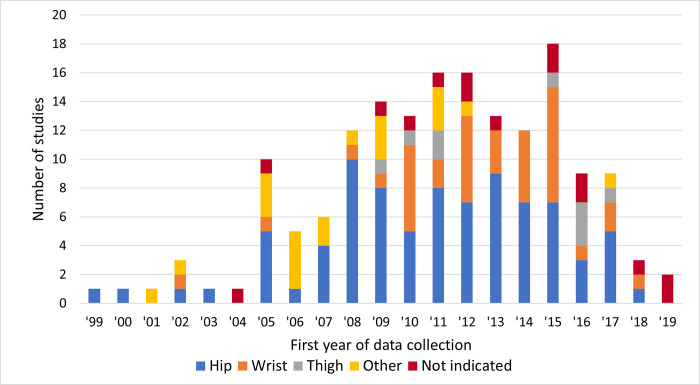
The earliest study year with accelerometry data collection was 1999, [175] with a noticeable rise in usage from 2004 to 2009 (Fig 3). The declining data collection in 2018 to 2020 is attributable to the time it takes to collect, process, analyze, and publish results in relation to our search date.
Fig 3. Number of studies collecting data by year (n = 155).
Note that if a study collects accelerometry over multiple years, then it is included on the graph in each of those years.
Approximately half (51.0%) of the studies used population-based sampling (Table 1). However, only 12.9% used sample weights. Two studies did not meet our definition of population-based, but did create sampling weights for their study [63, 143]. In terms of sampling, the majority of studies enrolled community dwelling adults, but 13 studies selected participants based on the following health conditions: first bariatric surgery (n = 1) [114], females experiencing infertility (n = 1) [128], fibromyalgia (n = 1) [27], survivors of acute lymphoblastic leukemia (n = 1) [97], and pregnancy (n = 2) [54, 134], and postmenopause (n = 1) [120]. In addition, several studies selected participants with or at risk for knee osteoarthritis (n = 2) [63, 172], and diabetes or specific blood glucose levels (n = 4) [40, 86, 89, 117]. Analytic sample sizes ranged from 512 to 8,203,261, with a median of 1095 (interquartile range 703 to 2325) and mean 55,580.
Almost one-third (29.7%) of studies asked participants to keep a logbook of accelerometer wear time, nonwear time, and/or sleep time (Table 1). A few studies also specified a protocol to capture workday activities (n = 5) [84, 107, 108, 119, 162], bicycling (n = 3) [63, 110], swimming/water activities (n = 2) [32, 63], and outdoor activities (n = 1) [141]. Most studies required wear of one accelerometer (94.2%); however, 8 studies (5.2%) asked participants to wear two accelerometers at the same time and 1 study (0.6%) asked participants to wear four accelerometers at the same time.
Accelerometer characteristics
Table 2 displays the accelerometer characteristics based on the total number of accelerometers worn [147 studies with one accelerometer] + (8*2) [8 studies with 2 accelerometers] + (1*4) [one study with 4 accelerometers] = 166). Overall, studies used 25 different brands of accelerometers, with the most popular including the ActiGraph (46.4%), Actical (8.4%), and GENEACtiv (7.8%). Most studies did not report on sampling frequency, but among those that did the most common setting was 30 Hz, ranging from 5 Hz to 100 Hz. The epoch length ranged from 1 second to 5 minutes, with 21 accelerometers capturing raw data that was used in the publication.
Table 2. Description of accelerometers used by observational studies of adults (n = 166).
| Overall | ||
|---|---|---|
| Description | % | n |
| Accelerometer Brand and Settings | ||
| Brand of accelerometer: | ||
| Actiband | 0.6 | 1 |
| Actibelt | 0.6 | 1 |
| Actical | 8.4 | 14 |
| ActiGraph (includes Computer Science Application, Inc.) | 46.4 | 77 |
| ActiHeart | 4.8 | 8 |
| ActivPAL | 3.6 | 6 |
| Actiwatch Spectrum | 1.8 | 3 |
| Ambulator | 0.6 | 1 |
| Axivity | 1.8 | 3 |
| Bong II | 0.6 | 1 |
| Fitbit | 4.2 | 7 |
| GENEActiv | 7.8 | 13 |
| Hookie | 1.8 | 3 |
| Kao | 0.6 | 1 |
| Lifecorder | 3.0 | 5 |
| Omron Active style Pro | 4.2 | 7 |
| Orthocare Stepwatch | 1.2 | 2 |
| Panasonic Actimarker | 0.6 | 1 |
| Polar | 1.2 | 2 |
| RT3 | 0.6 | 1 |
| SenseWear | 2.4 | 4 |
| StepWatch | 0.6 | 1 |
| UKK | 1.2 | 2 |
| Withings | 0.6 | 1 |
| X15-1c | 0.6 | 1 |
| Sampling frequency in Hz: | ||
| 5 | 2.4 | 4 |
| 20 | 1.8 | 3 |
| 30 | 15.7 | 26 |
| 32 | 6.6 | 11 |
| 50 | 3.0 | 5 |
| 60 | 1.8 | 3 |
| 80 | 0.6 | 1 |
| 85.7 | 3.0 | 5 |
| 100 | 6.7 | 11 |
| Not indicated or not a choice | 58.4 | 97 |
| Epoch length: | ||
| 1 second | 5.4 | 9 |
| 4 seconds | 1.2 | 2 |
| 5 seconds | 3.6 | 6 |
| 6 seconds | 0.6 | 1 |
| 10 seconds | 3.6 | 6 |
| 15 seconds | 3.0 | 5 |
| 30 seconds | 6.6 | 11 |
| 1 minute | 41.6 | 69 |
| 2 minutes | 0.6 | 1 |
| 5 minutes | 0.6 | 1 |
| Raw and raw with epochs of 1 to 60 seconds | 12.7 | 21 |
| Not indicated or not a choice | 20.5 | 34 |
| Accelerometer Distribution and Return: | ||
| Method of accelerometer distribution: | ||
| In-person | 43.4 | 72 |
| 17.5 | 29 | |
| Mailed or in-person | 1.8 | 3 |
| Not applicable (e.g., distributed cohort) | 3.0 | 5 |
| Not indicated | 34.3 | 57 |
| Method of accelerometer return: | ||
| In-person | 16.9 | 28 |
| 30.7 | 51 | |
| Device not asked to be returned | 0.6 | 1 |
| Not applicable (e.g., distributed cohort) | 3.0 | 5 |
| Not indicated | 48.8 | 81 |
| Accelerometer Wear | ||
| Days of data collection: | ||
| 1 day | 0.6 | 1 |
| 2 days | 1.2 | 2 |
| 3 days | 1.2 | 2 |
| 4 days | 4.2 | 7 |
| 5 days | 2.4 | 4 |
| 6 days | 1.2 | 2 |
| 7 days | 62.0 | 103 |
| 4 to 7 days variable by participant | 1.8 | 3 |
| 8 days | 6.6 | 11 |
| 9 to 14 day range | 9.6 | 16 |
| Other | 5.4 | 9 |
| Not indicated | 3.6 | 6 |
| Wear protocol: | ||
| Wake only | 45.2 | 75 |
| 24 hours (including sleep) | 44.6 | 74 |
| Not indicated | 10.2 | 17 |
| Accelerometer Non-wear | ||
| Weekend wear required to be adherent: | ||
| Yes | 11.4 | 19 |
| No/Not indicated | 88.6 | 147 |
| Number of adherent days of wear to be used in the analysis: | ||
| 1 day | 6.6 | 11 |
| 2 days | 5.4 | 9 |
| 3 days | 13.9 | 23 |
| 4 days | 38.0 | 63 |
| 5 days | 9.6 | 16 |
| 6 days | 0.6 | 1 |
| 7 days | 5.4 | 9 |
| Other | 3.6 | 6 |
| Not indicated | 16.9 | 28 |
| Number of minutes/day of wear to be an adherent day: | ||
| 480 minutes (8 hours) | 4.2 | 7 |
| 600 minutes (10 hours) | 59.0 | 98 |
| 800 minutes (12 hours) | 0.6 | 1 |
| 840 minutes (14 hours) | 0.6 | 1 |
| 960 minutes (16 hours) | 3.0 | 5 |
| 1080 minutes (18 hours) | 0.6 | 1 |
| 1200 minutes (20 hours) | 1.2 | 2 |
| 1440 minutes (24 hours) | 2.4 | 4 |
| Other | 8.4 | 14 |
| Not indicated | 19.9 | 33 |
Note: Eight studies used 2 accelerometers, and one study used 4 accelerometers; therefore, the sample size was n = 166 for this table. We selected a sample of studies and n = 29 responded to check their entries and fill in missing information when possible. Therefore, the "not indicated" category is reduced when the study provided missing information from the selected study.
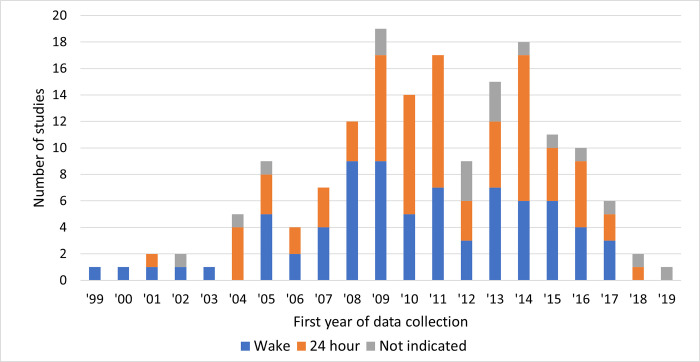
Accelerometer distribution was more frequently in-person (n = 71) rather than mailed (n = 29) (Table 2). In contrast, mail (n = 51) was the more common return method over in-person (n = 28). The most common number of days of data collection was 7 days (n = 103), although 32 accelerometers collected 8 or more days of wear. Four accelerometer protocols specified weekend days of wear. For the accelerometry wear protocols, 75 required wake only and 74 required continuous wear including sleep. When exploring by the first year of data collection (Fig 4), we found a larger proportion of studies using a 24-hour protocol compared to a wake only protocol starting in 2010 and following for most years.
Fig 4. Wear protocol by first year of data collection, graphed at the accelerometer level (n = 166).
The studies applied a wide variety of algorithms to remove nonwear time. Most of them were based on consecutive zeros, and many algorithms accounted for a short interruption period (S5 File). For 20 accelerometers, nonwear was identified using raw data. Uniquely, we found a few studies used a capacitive sensor (n = 1) [124], galvanic heat sensor (n = 1) [94], heart rate (n = 1) [160], or a logbook (n = 2) [76, 88] to distinguish wear from nonwear periods. The number of required adherent days (regardless of the physical activity or sedentary behavior metric) ranged from 1 to 7 days, with the most common of 4 days used (n = 64) (Table 2). The number of hours to wear an accelerometer to be defined as an adherent day was most often specified for at least 10 hours/day of wear (n = 98). A few studies described individually calibrating the accelerometer using a step test (n = 4 on the whole sample [50, 86, 160] or a subsample [55]) or a treadmill test (n = 1) [173].
The most common accelerometer placement was the hip or waist (n = 82), followed by the wrist (n = 37) and the thigh (n = 9) (Table 3). When exploring by the first year of data collection (Fig 5), hip remained most common by year but wrist collection increased starting around 2010 (with 4 studies collecting wrist data prior to that year). For the hip placement, accelerometer protocols specified wearing it on the right side (n = 47), either side (n = 7), left side (n = 4), dominant side (n = 2), nondominant side (n = 3), on lower back (n = 1), or not indicated (n = 18). For the wrist placement, accelerometer protocols specified nondominant side (n = 29), dominant side (n = 1), nondominant side (n = 1), right side (n = 1), or not indicated (n = 5). For the thigh placement, accelerometer protocols specified right side (n = 5), dominant side (n = 1), or not indicated (n = 3).
Table 3. Description of accelerometer placement and attachment method used by observational studies of adults (n = 166).
| Overall | ||
|---|---|---|
| Description | % | n |
| Placement location: | ||
| Hip/waist | 48.4 | 82 |
| Wrist | 22.3 | 37 |
| Thigh | 5.4 | 9 |
| Chest | 4.8 | 8 |
| Back | 3.0 | 5 |
| Tricep | 1.8 | 3 |
| Ankle | 1.2 | 2 |
| Arm | 1.2 | 2 |
| Hip or lower back | 0.6 | 1 |
| Waist or elsewhere to be clipped on clothing | 0.6 | 1 |
| Wrist or clipped onto belt or clothing | 0.6 | 1 |
| Not indicated | 9.0 | 15 |
| Placement Side: | ||
| Right | 33.7 | 56 |
| Left | 2.4 | 4 |
| Either side | 4.2 | 7 |
| Non-dominant | 19.9 | 33 |
| Dominant | 3.0 | 5 |
| Lower back | 3.0 | 5 |
| Upper back | 0.6 | 1 |
| Not indicated | 33.1 | 55 |
| Attachment method: | ||
| Adhesive | 6.0 | 10 |
| Adhesive, medical grade | 0.6 | 1 |
| Band | 7.8 | 13 |
| Belt | 27.7 | 46 |
| Clip | 1.2 | 2 |
| Electrode | 3.6 | 6 |
| Strap | 0.6 | 1 |
| Tape | 0.6 | 1 |
| Wristband | 4.2 | 7 |
| Other | 1.2 | 2 |
| Not indicated | 46.4 | 77 |
Note: Eight studies used 2 accelerometers, and one study used 4 accelerometers; therefore, the sample size was n = 166 for this table. We selected a sample of studies and n = 29 responded to check their entries and fill in missing information when possible. Therefore, the "not indicated" category is reduced when the study provided missing information from the selected study.
Fig 5. Accelerometer wear location by first year of data collection, graphed at the accelerometer level (n = 166).
Completeness of reporting accelerometry information
Using 12 items, we evaluated the completeness of reporting on the accelerometer (Table 4). The report is at the accelerometer level (n = 166), rather than the study level (n = 155), since some completeness of reporting differed by accelerometer even within the same publication. Overall, 9.6% reported all 12 items, 15.7% reported 11 items, and 22.4% reported 10 items. The overall mean reporting score was 9.5 (SD 1.9) items reported. The items reported less often included accelerometer return method (41.6%), number of accelerometers distributed (50.0%), and distribution method for sending out accelerometers (57.8%).
Table 4. Accelerometry reporting using a tool from Montoye et al. [13] (n = 166).
| Overall | ||
|---|---|---|
| Reporting | % | n |
| Brand of accelerometer used: | ||
| yes | 100 | 166 |
| Model of accelerometer used: | ||
| yes | 73.5 | 122 |
| Epoch length used: | ||
| yes | 78.3 | 130 |
| Accelerometer placement: | ||
| Yes both location and side | 63.9 | 106 |
| Yes but either location or side only | 24.9 | 43 |
| No | 10.2 | 17 |
| Sample size of accelerometers distributed: | ||
| yes | 50.0 | 83 |
| Accelerometer distribution method out: | ||
| yes | 57.8 | 96 |
| Accelerometer distribution method return: | ||
| yes | 41.6 | 69 |
| Accelerometer distribution method: | ||
| Yes out and return | 38.0 | 63 |
| Yes but either out or return only | 24.1 | 40 |
| No | 34.9 | 58 |
| Not applicable | 3.0 | 5 |
| Days of data collection: | ||
| yes | 96.4 | 160 |
| Criteria for non-wear: | ||
| yes | 68.7 | 114 |
| Number adherent days: | ||
| yes | 83.7 | 139 |
| Time to be considered adherent day: | ||
| yes | 77.1 | 128 |
| How meaning was derived: | ||
| yes | 99.4 | 165 |
| Sample size not meeting wear time criteria: | ||
| yes | 72.9 | 121 |
Note: Eight studies used 2 accelerometers, and one study used 4 accelerometers; therefore, the sample size was n = 166 for this table. Since we collected information from 29 studies about their missing information, the missingness in the prior tables will not match the missingness presented in this table.
The percent indicates that the item was reported, such that the higher the percent the more complete the reporting.
S4 File provides examples of responses to the questions.
Discussion
Despite widespread use of accelerometry in epidemiological research, a comprehensive list of observational studies leveraging accelerometry to assess physical activity and sedentary behavior did not exist. This scoping review filled this gap by describing the use of accelerometry in 155 observational studies. We documented a growth in the use of accelerometry over time from 1999 to 2019. A marked increase in accelerometry data collection, starting around 2004 to 2009, is congruent with the number of citations in the literature. From 1981 to 1996, fewer than 10 publications per year mentioned physical activity/exercise and accelerometry [176]. This citation index increased to almost 90 per year in 2003–2004 and to more than 600 per year in 2012–2013 [5]. In our review, 20 studies reported collecting accelerometry from more than one time period, offering a glimpse into the prospects of future studies that can potentially account for changes in physical activity and sedentary behavior over time, a limitation of most current studies of accelerometry in association with a health outcome.
We identified 5 studies using distributed donor data, all published since 2020 [65, 131, 153–155]. We expected a rise in this type of study, given the ubiquity of activity trackers in the general population [177], people’s willingness to share their data [178], and the wide-ranging type and amount of granular data collected. It would be important to identify best practices for this study type, given the differences in the way participants might wear the activity tracker without researcher instruction. Researchers should also consider the selectivity in the data collected, because those who own activity trackers tend to be more active, better educated, and younger than those who do not [179]. Among those who own activity trackers, willingness to donate data is related to physical activity and trust in health care providers [178].
Our review identified many areas of the world without accelerometer-based epidemiologic studies, such as large regions on the continents of Africa, Asia, and South America. This finding is consistent with the Global Observatory for Physical Activity Country Cards and Almanac that documented unequal distribution of research productivity by region [180, 181]. These authors point out that in the future, focusing on the global equity of research conducted and the public health impact it makes can contribute to improved physical activity around the world. Lack of physical activity is a worldwide concern, as an estimated 27.5% of adults do not engage in at least 150 minutes/week of moderate intensity, at least 75 minutes/week of vigorous intensity, or an equivalent combination of the two [182]. Moreover, a recent review indicated a decline in physical activity from 1995 to 2017 based on wearable devices collected in 8 countries [183].
Our review collected wear location and attachment method used across studies. As indicated by Fig 5, the use of wrist placement is likely increasing due to its greater comfort and lower intrusion, making it easier to wear for a 24-hour protocol. The 24-hour protocol can provide information on sleep, in addition to physical activity and sedentary behavior, to create a 24-hour activity cycle [184]. For wrist placement, the decision to wear the device on the dominant versus the non-dominant hand will impact results, since there is more hand movement on the dominant side that impacts the estimate of sedentary behavior [1, 185, 186]. In our review, most studies that reported on the wrist location used the nondominant side. For hip placement, wearing on the right or left hip may not make much difference [187]. In our review, most studies that reported on the hip location used the right side.
As documented in the 2004 international conference on accelerometry [6], researchers called for device-based companies to provide access to the raw accelerometer signal in order to move away from proprietary-based algorithms that only provided count-based data. Since that time, several accelerometers offered access to the raw signal. This review identified 21 studies that collected raw data. This shift in the field is promising since it facilitates harmonization across device types. Our abstraction tool included a section on machine learning approaches [188], but we did not identify any studies we abstracted using this approach. As data processing improves and algorithms become more widely available, we anticipate that more studies will use the raw signal to identify posture, some types of activities, and finer-grained patterns of physical activity and sedentary behavior.
While approximately half (n = 79) of the studies in the review utilized population-based sampling, only 20 studies used sample weights. When studies do not use these weights, their results may not reflect the characteristics of the population. Stamatakis et al. [189] points out that most observational studies are not representative of the general population due to low response rates. The use of sampling weights helps correct for differential selection probabilities, nonresponse, and other mismatches between the sample and the reference population. When response rates are low, adjustments to the sample weights can be made to reduce the potential for bias due to non-participation, including adjusting for differential nonresponse at the levels of selection and calibration to the census of the underlying geographic area based on sociodemographic characteristics (i.e., age, gender, race/ethnicity). For example, the United Kingdom Biobank Study achieved a 5.5% response rate, and further investigation indicated the presence of bias due to nonresponse [190].
In our review, the completeness of reporting of accelerometer procedures varied across studies. The overall mean reporting score was 9.5, indicating that of 12 key items to report on accelerometry, on average two to three were missing. The completeness of reporting was generally higher than the review that documented reporting from intervention studies [13]. In applying this reporting form, we found in some cases the questions were not relevant for a certain accelerometers, such as specification of epoch length. As more raw data are being used, the reporting tools will need to be updated to reflect these developments.
To our knowledge, this scoping review is the first to systematically identify and describe observational studies of adults with accelerometry measures. However, the scoping review has several limitations that should be acknowledged. First, we generally abstracted one publication per study, so it is possible that missing abstracted fields for a study could be available in other publications. There was a large range of publications for some studies. For example, for the NHANES 2005–2006 wave, the number of publications we collected was 199. Metrics may be differentially reported or more complete in other publications from the same study.
Second, we captured studies with an analytic sample size for accelerometry measurement of at least 500. This designation is somewhat arbitrary and excluded epidemiologic studies with smaller samples. Third, we included only studied published in English, thereby possibly undercounting studies published in other languages. This may also lead to underrepresentation on the map displaying study location. Fourth, although important we did not capture data availability, as this was inconsistently reported particularly in early publications when it often was not a required component of journal articles. Finally, we included studies that used step counting devices that relied on an accelerometer only, and not an older spring-levered configuration. However, we did not specifically search on the term “pedometer”, so studies that focused on step counting using an accelerometer but referred to only as a “pedometer” may have been missed.
Conclusions
The first peer-reviewed publication in the field of physical activity and public health was published in 1953 by Morris et al. [191] comparing London transport drivers to conductors on incidence of coronary heart disease [192]. The first epidemiologic study of adults (with a sample size of at least 500) that used an accelerometer was published 46 years later, in 1999 [175]. Since 1999, the uptake of the accelerometer into epidemiologic research has been remarkable, as documented by our review.
The database of studies resulting from the review can be useful in identifying potential studies for harmonization and meta analyses using similar protocols and devices [24]. Future efforts could link both health outcomes and data availability to the studies to facilitate research across studies. Our review results indicate the inconsistencies in reporting, supported by prior studies [13, 185], and a wide range of decisions applied to manage and use the data for analysis. The use of a checklist that is completed with journal submission would facilitate more complete reporting. Access to raw accelerometry is becoming more common, and it would benefit the field to create a consensus approach for reporting a set of standardized metrics in order to evaluate key accelerometer decisions, replicate the analysis, and promote harmonization across studies. This review identified regions in the world without any epidemiologic studies of accelerometry.
Supporting information
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
The authors thank Drs. Robert Furberg and Gabriel Madson for their help on this project.
Data Availability
The dataset is available in a public repository: Accelerometer level dataset: https://doi.org/10.15139/S3/8GPGJZ Cohort level dataset: https://doi.org/10.15139/S3/ZYVHUO.
Funding Statement
The project was supported by the National Center for Advancing Translational Sciences, National Institutes of Health grant #UL1TR002489 (https://tracs.unc.edu/). Carmen Cuthbertson and Kennedy Peter were supported by the National Heart, Lung, and Blood Institute National Research Service Award (T32-HL007055; https://www.nhlbi.nih.gov/grants-and-training). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders did not have a role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Gao Z, Liu W, McDonough DJ, Zeng N, Lee JE. The Dilemma of Analyzing Physical Activity and Sedentary Behavior with Wrist Accelerometer Data: Challenges and Opportunities. J Clin Med. 2021;10(24). doi: 10.3390/jcm10245951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walter P. The history of the accelerometer: 1920s-1996—prologue and epilogue, 2006. Sound and Vibration. 2007;41(1):84–92. [Google Scholar]
- 3.Saunders JB, Inman VT, Eberhart HD. The major determinants in normal and pathological gait. J Bone Joint Surg Am. 1953;35-A(3):543–58. [PubMed] [Google Scholar]
- 4.Morris JR. Accelerometry—a technique for the measurement of human body movements. J Biomech. 1973;6(6):729–36. doi: 10.1016/0021-9290(73)90029-8 [DOI] [PubMed] [Google Scholar]
- 5.Troiano RP, McClain JJ, Brychta RJ, Chen KY. Evolution of accelerometer methods for physical activity research. Br J Sports Med. 2014;48(13):1019–23. doi: 10.1136/bjsports-2014-093546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ward D, Evenson K, Vaughn A, Rodgers A, Troiano R. Accelerometer use in physical activity: best practices and research recommendations. Med Sci Sports Exerc. 2005;37(11 Suppl):S582–S8. doi: 10.1249/01.mss.0000185292.71933.91 [DOI] [PubMed] [Google Scholar]
- 7.Trost S, McIver K, Pate R. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(11 Suppl):S531–S43. doi: 10.1249/01.mss.0000185657.86065.98 [DOI] [PubMed] [Google Scholar]
- 8.Wijndaele K, Westgate K, Stephens SK, Blair SN, Bull FC, Chastin SF, et al. Utilization and harmonization of adult accelerometry data: Review and expert consensus. Med Sci Sports Exerc. 2015;47(10):2129–39. doi: 10.1249/MSS.0000000000000661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Hees VT, Thaler-Kall K, Wolf KH, Brond JC, Bonomi A, Schulze M, et al. Challenges and Opportunities for Harmonizing Research Methodology: Raw Accelerometry. Methods Inf Med. 2016;55(6):525–32. doi: 10.3414/ME15-05-0013 [DOI] [PubMed] [Google Scholar]
- 10.Albrecht BM, Flasskamp FT, Koster A, Eskofier BM, Bammann K. Cross-sectional survey on researchers’ experience in using accelerometers in health-related studies. BMJ open sport & exercise medicine. 2022;8(2):e001286. doi: 10.1136/bmjsem-2021-001286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matthews CE, Hagstromer M, Pober DM, Bowles HR. Best practices for using physical activity monitors in population-based research. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S68–76. doi: 10.1249/MSS.0b013e3182399e5b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tudor-Locke C, Mire EF, Dentro KN, Barreira TV, Schuna JM, Zhao P Jr., et al. A model for presenting accelerometer paradata in large studies: ISCOLE. The international journal of behavioral nutrition and physical activity. 2015;12:52. doi: 10.1186/s12966-015-0213-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Montoye AHK, Moore RW, Bowles HR, Korycinski R, Pfeiffer KA. Reporting accelerometer methods in physical activity intervention studies: a systematic review and recommendations for authors. Br J Sports Med. 2018;52(23):1507–16. doi: 10.1136/bjsports-2015-095947 [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic reviews. 2015;4:1. doi: 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 16.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Booth A, Clarke M, Dooley G, Ghersi D, Moher D, Petticrew M, et al. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Systematic reviews. 2012;1:2. doi: 10.1186/2046-4053-1-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Center for Health Statistics. 2003–2004 National Health and Nutrition Examination Survey (NHANES): Survey brochures and consent documents. Accessed October 30, 2015 at http://www.cdc.gov/nchs/nhanes/nhanes2003-2004/brochures03_04.htm 2015 [
- 19.National Center for Health Statistics. 2005–2006 National Health and Nutrition Examination Survey (NHANES): Survey brochures and consent documents. Accessed October 30, 2015 at http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/brochures05_06.htm 2015 [
- 20.Bassett DR, Toth LP Jr., LaMunion SR, Crouter SE. Step Counting: A Review of Measurement Considerations and Health-Related Applications. Sports medicine (Auckland, NZ. 2017;47(7):1303–15. doi: 10.1007/s40279-016-0663-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scarlett S, Nolan H, Kenny RA, O’Connell MD. Objective Sleep Duration in Older Adults: Results From The Irish Longitudinal Study on Ageing. J Am Geriatr Soc. 2020;68(1):120–8. doi: 10.1111/jgs.16177 [DOI] [PubMed] [Google Scholar]
- 22.Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011;43(2):357–64. doi: 10.1249/MSS.0b013e3181ed61a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Troiano R, Berrigan D, Dodd K, Masse L, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. doi: 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- 24.Evenson K, Scherer E, Cuthbertson C, Peter K, Madson G, Eckman S. Dataset of worldwide observational studies of adults with accelerometry measured physical activity and sedentary behavior. Data in Brief. 2022:under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing. Accessed at http://www.R-project.org/ Vienna, Austria2014 [ [Google Scholar]
- 26.South A. Rworldmap: A new R package for mapping global data. The R Journal. 2011;3(1):35–43. Accessed at http://journal.r-project.org/archive/2011-1/RJournal_-1_South.pdf. [Google Scholar]
- 27.Acosta-Manzano PS-J, Estevez-Lopez V., Alvarez-Gallardo F., Soriano-Maldonado I. C., Borges-Cosic A., Gavilan-Carrera M., et al. Do women with fibromyalgia present higher cardiovascular disease risk profile than healthy women? The al-Ãndalus project. Clin Exp Rheumatol. 2017;35(3):S61–S7. [PubMed] [Google Scholar]
- 28.Acs PV, Rocha R., Doczi P., Raposa T., Baumann B. L., Ostojic P., S. et al. Criterion validity and reliability of the International Physical Activity Questionnaire—Hungarian short form against the RM42 accelerometer. BMC Public Health. 2021;21(SUPPL 1):10. doi: 10.1186/s12889-021-10372-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aebi NJB-I, Schaffner B., Caviezel E., Imboden S., Probst-Hensch M., N. Patterns of cross-sectional and predictive physical activity in Swiss adults aged 52+: results from the SAPALDIA cohort. Swiss Med Wkly. 2020;150:w20266. doi: 10.4414/smw.2020.20266 [DOI] [PubMed] [Google Scholar]
- 30.Alessa HBC, Hankinson Andrea K., Barnett Susan E., Rood Junaidah B., Jennifer Matthews, Rimm Charles E., et al. Objective Measures of Physical Activity and Cardiometabolic and Endocrine Biomarkers. Medicine & Science in Sports & Exercise. 2017;49(9):1817–25. doi: 10.1249/MSS.0000000000001287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amagasa SI S. Ukawa S. Sasaki S. Nakamura K. Yoshimura A. Tanaka A. et al. Are Japanese women less physically active than men? Findings from the DOSANCO Health Study. J Epidemiol. 2020;31(10):530–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arnardottir NYK A. Van Domelen D. R. Brychta R. J. Caserotti P. Eiriksdottir G. Sverrisdottir J. E. et al. Objective measurements of daily physical activity patterns and sedentary behaviour in older adults: Age, Gene/Environment Susceptibility-Reykjavik Study. Age Ageing. 2013;42(2):222–9. doi: 10.1093/ageing/afs160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Asai YO K. Oume M. Ogura M. Takeuchi K. Yamagami Y. Tai Y. et al. Farming habit, light exposure, physical activity, and depressive symptoms. A cross-sectional study of the HEIJO-KYO cohort. J Affect Disord. 2018;241:235–40. doi: 10.1016/j.jad.2018.08.003 [DOI] [PubMed] [Google Scholar]
- 34.Balkau BM, L.Oppert J. M. Nolan J. Golay A. Porcellati F. Laakso M.et al. Physical activity and insulin sensitivity: the RISC study. Diabetes. 2008;57(10):2613–8. doi: 10.2337/db07-1605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bassett JKS, Hodge Christopher T. V., Mahmood Allison M., Shahid Csizmadi, Ilona Owen, Neville et al. Calibration of the Active Australia questionnaire and application to a logistic regression model. Journal of Science & Medicine in Sport. 2021;24(5):474–80. doi: 10.1016/j.jsams.2020.11.007 [DOI] [PubMed] [Google Scholar]
- 36.Bernard PH-M, G.Atoui S. Moullec G. Daily Objective Physical Activity and Sedentary Time in Adults with COPD Using Spirometry Data from Canadian Measures Health Survey. Can Respir J. 2018;2018(2018:9107435). doi: 10.1155/2018/9107435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berntsen SR K. R, Morkrid K. Sletner L. Birkeland K. I. Jenum A. K. Objectively recorded physical activity in early pregnancy: A multiethnic population-based study. Scandinavian Journal of Medicine & Science in Sports. 2014;24(3):594–601. doi: 10.1111/sms.12034 [DOI] [PubMed] [Google Scholar]
- 38.Bielemann RML A. Z, Bertoldi A. D. Tomasi E. Demarco F. F. Gonzalez M. C.et al. Objectively Measured Physical Activity Reduces the Risk of Mortality among Brazilian Older Adults. J Am Geriatr Soc. 2020;68(1):137–46. doi: 10.1111/jgs.16180 [DOI] [PubMed] [Google Scholar]
- 39.Bonn SER, Matthews Eric B., Troiano Charles E., Bowles Richard P., Rood Heather R., Jennifer Barnett, et al. Associations of Sedentary Time with Energy Expenditure and Anthropometric Measures. Medicine & Science in Sports & Exercise. 2018;50(12):2575–83. doi: 10.1249/MSS.0000000000001729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Braver NRd F, Wagtendonk A. J. Kok J. G. Harms P. P. Brug J. Beulens J. W. J.et al. Neighborhood walkability, physical activity and changes in glycemic markers in people with type 2 diabetes: The Hoorn Diabetes Care System cohort. Health Place. 2021;69(May):102560. [DOI] [PubMed] [Google Scholar]
- 41.Bringolf-Isler BS, Kayser C, Suggs B, Probst-Hensch L. S, N. Objectively measured physical activity in population-representative parent-child pairs: parental modelling matters and is context-specific. BMC Public Health. 2018;18(1):1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buman MPH E. B. Haskell W. L.Pruitt L.Conway T. L.Cain K. L.Sallis J. et al. Objective Light-Intensity Physical Activity Associations With Rated Health in Older Adults. Am J Epidemiol. 2010;172(10):1155–65. doi: 10.1093/aje/kwq249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burchartz AM K. Anedda B.Niessner C.Oriwol D.Schmidt S.Woll A. Measurement of physical activity and sedentary behavior by accelerometry among a nationwide sample of the KiGGS and MoMo study: a study protocol. JMIR Res Protoc. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Buszkiewicz JR, Gupta C.R, Ko S., Mou L. K., Moudon J., Hurvitz A.V. P. et al. A cross-sectional analysis of physical activity and weight misreporting in diverse populations: The Seattle Obesity Study III. Obes Sci Pract. 2020;6(6):615–27. doi: 10.1002/osp4.449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cabanas-Sanchez VE-C, I. Migueles J. H.Banegas J. R.Graciani A.Rodriguez-Artalejo F.Martinez-Gomez D. Twenty four-hour activity cycle in older adults using wrist-worn accelerometers: The seniors-ENRICA-2 study. Scandinavian Journal of Medicine & Science in Sports. 2020;30(4):700–8. doi: 10.1111/sms.13612 [DOI] [PubMed] [Google Scholar]
- 46.Cawthon PMB T. L. Cauley J. A. Ensrud K. E. Dam T. T. Harrison S. L. Peters K. W. et al. Objective assessment of activity, energy expenditure, and functional limitations in older men: the Osteoporotic Fractures in Men study. J Gerontol A Biol Sci Med Sci. 2013;68(12):1518–24. doi: 10.1093/gerona/glt054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cepeda MK C. M. van Rooij F. J. A. Tiemeier H. Guxens M. Franco O. H. Schoufour J. D. Seasonality of physical activity, sedentary behavior, and sleep in a middle-aged and elderly population: The Rotterdam study. Maturitas. 2018;110:41–50. [DOI] [PubMed] [Google Scholar]
- 48.Chen TK H. Honda T.Hata J.Yoshida D.Mukai N.Shibata M. et al. Patterns and Levels of Sedentary Behavior and Physical Activity in a General Japanese Population: The Hisayama Study. J Epidemiol. 2018;28(5):260–5. doi: 10.2188/jea.JE20170012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen TN, KenjiHaeuchi YukaChen, SanmeiHonda TakanoriKumaga Shuzo i. Associations of Sedentary Time and Breaks in Sedentary Time With Disability in Instrumental Activities of Daily Living in Community-Dwelling Older Adults. Journal of Physical Activity & Health. 2016;13(3):303–9. doi: 10.1123/jpah.2015-0090 [DOI] [PubMed] [Google Scholar]
- 50.Christensen DLF-J D. Boit M. K.Mwaniki D. L.Kilonzo B.Tetens I.Kiplamai F. K. et al. Cardiorespiratory fitness and physical activity in Luo, Kamba, and Maasai of rural Kenya. American Journal of Human Biology. 2012;24(6):723–9. doi: 10.1002/ajhb.22303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chu AHYvD R. M. Biddle S. J. H.Tan C. S.Koh D.Muller-Riemenschneider F. Self-reported domain-specific and accelerometer-based physical activity and sedentary behaviour in relation to psychological distress among an urban Asian population. International Journal of Behavioral Nutrition and Physical Activity. 2018;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Clarke JC R. Janssen I. Tremblay M. S. Accelerometer-measured moderate-to-vigorous physical activity of Canadian adults, 2007 to 2017. Health Rep. 2019;30(8):3–10. doi: 10.25318/82-003-x201900800001-eng [DOI] [PubMed] [Google Scholar]
- 53.da Silva ICMvH V. T. Ramires V. V.Knuth A. G.Bielemann R. M.Ekelund U.Brage S. et al. Physical activity levels in three Brazilian birth cohorts as assessed with raw triaxial wrist accelerometry. Int J Epidemiol. 2014;43(6):1959–68. doi: 10.1093/ije/dyu203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.da Silva SGE K. R. da Silva I. C. M.Mendes M. A.Domingues M. R.da Silveira M. F.Wehrmeister F. C. et al. Correlates of accelerometer-assessed physical activity in pregnancy-The 2015 Pelotas (Brazil) Birth Cohort Study. Scand J Med Sci Sports. 2018;28(8):1934–45. doi: 10.1111/sms.13083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dahl-Petersen IKB P. Brage S.Jorgensen M. E. Physical activity energy expenditure is associated with 2-h insulin independently of obesity among Inuit in Greenland. Diabetes Res Clin Pract. 2013;102(3):242–9. doi: 10.1016/j.diabres.2013.10.004 [DOI] [PubMed] [Google Scholar]
- 56.Dallal CMB L. A. Matthews C. E.Pfeiffer R. M.Hartman T. J.Lissowska J.Falk R. T. et al. Association of Active and Sedentary Behaviors with Postmenopausal Estrogen Metabolism. Med Sci Sports Exerc. 2016;48(3):439–48. doi: 10.1249/MSS.0000000000000790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.de Groot RL J. Brug J.Lagerberg J. W.de Korte, D.Hoekstra T.de Kort, Wlamvan den Hurk K. Lifestyle behaviours are not associated with haemolysis: results from Donor InSight. Blood Transfusion. 2020;18(2):86–95. doi: 10.2450/2019.0151-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.de la Chica JAG-T S.Garcia-Ruiz J. M. Garcia-Lunar I.Oliva B.Fernandez-Alvira J. M.Lopez-Melgar B. et al. Association Between Left Ventricular Noncompaction and Vigorous Physical Activity. J Am Coll Cardiol. 2020;76(15):1723–33. doi: 10.1016/j.jacc.2020.08.030 [DOI] [PubMed] [Google Scholar]
- 59.de Sousa TLWO, TlvdSperandio E. F.Arantes R. L.Gagliardi A. R. D.Romiti M.da Silva R. P. et al. Dose-response relationship between very vigorous physical activity and cardiovascular health assessed by heart rate variability in adults: Cross-sectional results from the EPIMOV study. PLoS One. 2019;14(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.del Pozo-Cruz BM A. Martin-Garcia M.Marin-Puyalto J.Garcia-Garcia F. J.Rodriguez-Manas L.Guadalupe-Grau A. et al. Frailty is associated with objectively assessed sedentary behaviour patterns in older adults: Evidence from the Toledo Study for Healthy Aging (TSHA). PLoS One. 2017;12(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Doherty AJ D. Hammerla N.Plotz T.Olivier P.Granat M. H.White T. et al. Large Scale Population Assessment of Physical Activity Using Wrist Worn Accelerometers: The UK Biobank Study. PLoS One. 2017;12(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dohrn I-M, Paul A.Winkler, ElisabethWelmer Anna-Karin. Device-measured sedentary behavior and physical activity in older adults differ by demographic and health-related factors. European Reviews of Aging & Physical Activity. 2020;17(1):1–11. doi: 10.1186/s11556-020-00241-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dunlop DDS J. Semanik P. A.Chang R. W.Sharma L.Bathon J. M.Eaton C. B. et al. Objective Physical Activity Measurement in the Osteoarthritis Initiative Are Guidelines Being Met? Arthritis Rheum. 2011;63(11):3372–82. doi: 10.1002/art.30562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ekblom-Bak EO G. Ekblom O.Ekblom B.Bergstrom G.Borjesson M. The Daily Movement Pattern and Fulfilment of Physical Activity Recommendations in Swedish Middle-Aged Adults: The SCAPIS Pilot Study. PLoS One. 2015;10(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.El Fatouhi DD L. Goetzinger C.Malisoux L.Affret A.Campo D.Fagherazzi G. Associations of Physical Activity Level and Variability With 6-Month Weight Change Among 26,935 Users of Connected Devices: Observational Real-Life Study. JMIR Mhealth Uhealth. 2021;9(4):e25385. doi: 10.2196/25385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Elhakeem AC R. Whincup P.Brage S.Kuh.Hardy R. Physical Activity, Sedentary Time, and Cardiovascular Disease Biomarkers at Age 60 to 64 Years. J Am Heart Assoc. 2018;7(16):e007459. doi: 10.1161/JAHA.117.007459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Elhakeem AH K. Deere K. C.Hartley A.Clark E. M.Moss C.Edwards M. H. et al. Associations of lifetime walking and weight bearing exercise with accelerometer-measured high impact physical activity in later life. Prev Med Rep. 2017;8:183–9. doi: 10.1016/j.pmedr.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Elhakeem AH J. Tobias J. H.Lawlor D. A. Physical Activity Throughout Adolescence and Peak Hip Strength in Young Adults. JAMA Netw Open. 2020;3(8):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Eriksson UA D. Sundquist K. Availability of exercise facilities and physical activity in 2,037 adults: cross-sectional results from the Swedish neighborhood and physical activity (SNAP) study. BMC Public Health. 2012;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Evenson KRM, Kimberly B.Fang WenScanlin, Kathleen Physical Activity and Sedentary Behavior Among Adults 60 Years and Older: New York City Residents Compared With a National Sample. Journal of Aging & Physical Activity. 2014;22(4):499–507. doi: 10.1123/japa.2012-0345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Evenson KRS-A, DanielaYu DengMarshall, Isasi Simon J, Carmen R.Esliger, Dale W.et al. Accelerometer Adherence and Performance in a Cohort Study of US Hispanic Adults. Medicine & Science in Sports & Exercise. 2015;47(4):725–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fernberg UF M. Hurtig-Wennlöf A. Higher Total Physical Activity is Associated with Lower Arterial Stiffness in Swedish, Young Adults: The Cross-Sectional Lifestyle, Biomarkers, and Atherosclerosis Study. Vasc Health Risk Manag. 2021;17:175–85. doi: 10.2147/VHRM.S283211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ferrari GLDK I. Fisberg.Gomez G.Rigotti A.Sanabria L. Y. C.Garcia M. C. Y.et al. Association of moderate-to-vigorous physical activity with neck circumference in eight Latin American countries. BMC Public Health. 2019;19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Foong YCA D. Winzenberg T.Otahal P.Scott D.Jones G. The association between physical activity and reduced body fat lessens with age—Results from a cross-sectional study in community-dwelling older adults. Exp Gerontol. 2014;55:107–12. doi: 10.1016/j.exger.2014.04.006 [DOI] [PubMed] [Google Scholar]
- 75.Forsyth AO J. M. Lee B.Schmitz K. H. The built environment, walking, and physical activity: Is the environment more important to some people than others? Transportation Research Part D-Transport and Environment. 2009;14(1):42–9. [Google Scholar]
- 76.Fraysse FG A. C. Muller J.Wake M.Olds T. Physical activity and sedentary activity: population epidemiology and concordance in Australian children aged 11–12 years and their parents. BMJ Open. 2019;9(Suppl 3):136–46. doi: 10.1136/bmjopen-2018-023194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gallo LCC J. A. Sotres-Alvarez D.Sallis J. F.Jankowska M. M.Roesch S. C.Gonzalez F.et al. The Hispanic Community Health Study/Study of Latinos Community and Surrounding Areas Study: sample, design, and procedures. Ann Epidemiol. 2019;30:57–65. doi: 10.1016/j.annepidem.2018.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.García-Ortiz LR-R J. I. Schmidt-Trucksäss A.Puigdomenech-Puig E.Martínez-Vizcaíno V.Fernández-Alonso C.Rubio-Galan J.et al. Relationship between objectively measured physical activity and cardiovascular aging in the general population—the EVIDENT trial. Atherosclerosis. 2014;233(2):434–40. doi: 10.1016/j.atherosclerosis.2014.01.021 [DOI] [PubMed] [Google Scholar]
- 79.Gibbs BBG K. P. Reis J. P.Jakicic J. M.Carnethon M. R.Sternfeld B. Cross-sectional and Longitudinal Associations Between Objectively Measured Sedentary Time and Metabolic Disease: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Diabetes Care. 2015;38(10):1835–43. doi: 10.2337/dc15-0226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Glazer NLL, AsyaEsliger, Blease Dale W, Susan J.Freedson, Massaro Patty S, Joseph M.Murabito, Joanne M.et al. Sustained and Shorter Bouts of Physical Activity Are Related to Cardiovascular Health. Medicine & Science in Sports & Exercise. 2013;45(1):109–15. doi: 10.1249/MSS.0b013e31826beae5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gubelmann CH R. Haba-Rubio J.Vollenweider P.Marques-Vidal. Physical activity is associated with higher sleep efficiency in the general population: the CoLaus study. Sleep. 2018;41(7). [DOI] [PubMed] [Google Scholar]
- 82.Gudnadottir UC-B L. Spicer A.Gorzelitz J.Malecki K. The relationship between occupational physical activity and self-reported vs measured total physical activity. Prev Med Rep. 2019;15:100908. doi: 10.1016/j.pmedr.2019.100908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.HAGSTRÖMER M OJA P, SJÖSTRÖM M. Physical Activity and Inactivity in an Adult Population Assessed by Accelerometry. Medicine & Science in Sports & Exercise. 2007;39(9):1502–8. [DOI] [PubMed] [Google Scholar]
- 84.Halonen JIP A. Pentti J.Kallio M.Koskela S.Kivimaki M.Kawachi I.et al. Cross-sectional associations of neighbourhood socioeconomic disadvantage and greenness with accelerometer-measured leisure-time physical activity in a cohort of ageing workers. BMJ Open. 2020;10(8):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hamer MS, Chastin E., Pearson S., Brown N., Gilbert M., Sullivan E. A. Feasibility of Measuring Sedentary Time Using Data From a Thigh-Worn Accelerometer The 1970 British Cohort Study. Am J Epidemiol. 2020;189(9):963–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hansen ALSC B. Helge J. W.Johansen N. B.Gram B.Christiansen J. S.Brage S.et al. Combined Heart Rate- and Accelerometer-Assessed Physical Activity Energy Expenditure and Associations With Glucose Homeostasis Markers in a Population at High Risk of Developing Diabetes The ADDITION-PRO study. Diabetes Care. 2013;36(10):3062–9. doi: 10.2337/dc12-2671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hansen BHK E. Dyrstad S. M.Holme I.Anderssen S. A. Accelerometer-Determined Physical Activity in Adults and Older People. Med Sci Sports Exerc. 2012;44(2):266–72. doi: 10.1249/MSS.0b013e31822cb354 [DOI] [PubMed] [Google Scholar]
- 88.Hashimoto YM K. Sawada S. S.Gando Y.Kawakami R.Sloan R. A.Kinugawa C.et al. Association between objectively measured physical activity and body mass index with low back pain: a large-scale cross-sectional study of Japanese men. BMC Public Health. 2018;18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Henson JR Baldry A. V., Brady E., Davies E. M., Edwardson M. J. Yates C. L. T. et al.Codec, Investigators. Physical behaviors and chronotype in people with type 2 diabetes. BMJ Open Diabetes Res Care. 2020;8(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hermsen SM J. Kerkhof P.Wiekens C.De Groot M. Determinants for Sustained Use of an Activity Tracker: Observational Study. JMIR Mhealth Uhealth. 2017;5(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hesketh KRG L. Ekelund U.McMinn A. M.Godfrey M.Inskip H. M.Cooper C.et al. Activity levels in mothers and their preschool children. Pediatrics. 2014;133(4):e973–80. doi: 10.1542/peds.2013-3153 [DOI] [PubMed] [Google Scholar]
- 92.Hetherington-Rauth MM J. P. Judice P. B.Ara I.Rosa G. B.Correia I. R.Manas A. et al. Physical activity moderates the effect of sedentary time on an older adult’s physical independence. J Am Geriatr Soc. 2021;69:1964–70. doi: 10.1111/jgs.17141 [DOI] [PubMed] [Google Scholar]
- 93.Hinckson EC E. Mavoa S.Smith M.Badland H.Witten K.Kearns R. et al. What are the associations between neighbourhood walkability and sedentary time in New Zealand adults? The URBAN cross-sectional study. BMJ Open. 2017;7(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ho ECH L. Dale W.Waite L.Huisingh-Scheetz M. Social capital predicts accelerometry-measured physical activity among older adults in the US: a cross-sectional study in the National Social Life, Health, and Aging Project. BMC Public Health. 2018;18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Honda TC S. M. Kishimoto H.Narazaki K.Kumagai S. Identifying associations between sedentary time and cardio-metabolic risk factors in working adults using objective and subjective measures: a cross-sectional analysis. BMC Public Health. 2014;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Howard VJR J. DavidMosher AleenaHutto, BrentStewart Margaret S.Colabianchi Natalie et al. Obtaining Accelerometer Data in a National Cohort of Black and White Adults. Medicine & Science in Sports & Exercise. 2015;47(7):1531–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Howell CRW C. L. Ehrhardt M. J.Partin R. E.Kaste S. C.Lanctot J. Q.Pui C. H.et al. Clinical Impact of Sedentary Behaviors in Adult Survivors of Acute Lymphoblastic Leukemia: A Report From the St. Jude Lifetime Cohort Study. Cancer. 2018;124(5):1036–43. doi: 10.1002/cncr.31162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Husu PS J. Vaha-Ypya H.Sievanen H.Tokola K.Valkeinen H.Maki-Opas T. et al. Objectively measured sedentary behavior and physical activity in a sample of Finnish adults: a cross-sectional study. BMC Public Health. 2016;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Immerwahr S, Wyker B, Bartley K, Eisenhower D. Physical Activity and Transit Survey Device Follow-up Study: Methodology Report. Accessed February 15, 2022. at https://www1.nyc.gov/assets/doh/downloads/pdf/episrv/PAT-device-methodology.pdf. The New York City Department of Health and Mental Hygiene; 2012. [Google Scholar]
- 100.Inoue SO Y. Odagiri Y.Takamiya T.Kamada.Okada S.Tudor-Locke C. et al. Characteristics of accelerometry respondents to a mail-based surveillance study. J Epidemiol. 2010;20(6):446–52. doi: 10.2188/jea.je20100062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jago RS S. J. Wood L.Pool L.Zahra J.Thompson J. L.Lawlor D. A. Associations between objectively assessed child and parental physical activity: a cross-sectional study of families with 5–6 year old children. BMC Public Health. 2014;14:655. doi: 10.1186/1471-2458-14-655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Jankowska MMS D. D. Natarajan L.Martinez E.Anderson C. A. M.Sallis J. F.Matthews S. A.Crist K.D illon L.Johnson E.Barrera-Ng A.Full K.et al. Protocol for a cross sectional study of cancer risk, environmental exposures and lifestyle behaviors in a diverse community sample: the Community of Mine study. BMC Public Health. 2019;19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Jantunen HW N. Salonen M. K.Perala M. M.Osmond C.Kautiainen H.Simonen M. et al. Objectively measured physical activity and physical performance in old age. Age Ageing. 2017;46(2):232–7. doi: 10.1093/ageing/afw194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jefferis BJI S. Kendrick D.Kerse N.Trost S.Lennon L. T.Ash S. et al. How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC Geriatr. 2014;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jefferis BJS C. Lee I. M.Choi M.Amuzu A.Gutierrez C.Casas J. P. et al. Adherence to physical activity guidelines in older adults, using objectively measured physical activity in a population-based study. BMC Public Health. 2014;14:382. doi: 10.1186/1471-2458-14-382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Johansson JN A. Nordstrom P. Objectively measured physical activity is associated with parameters of bone in 70-year-old men and women. Bone. 2015;81:72–9. doi: 10.1016/j.bone.2015.07.001 [DOI] [PubMed] [Google Scholar]
- 107.Johansson MSK M. Schnohr P.Marott J. L.Prescott E. I. B.Sogaard K.Holtermann. Time spent cycling, walking, running, standing and sedentary: a cross-sectional analysis of accelerometer-data from 1670 adults in the Copenhagen City Heart Study Physical behaviours among 1670 Copenhageners. BMC Public Health. 2019;19(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Jørgensen MBG N. Korshøj M.Lagersted-Olsen.Villumsen M.Mortensen O. S.Skotte J. et al. The DPhacto cohort: An overview of technically measured physical activity at work and leisure in blue-collar sectors for practitioners and researchers. Appl Ergon. 2019;77:29–39. doi: 10.1016/j.apergo.2019.01.003 [DOI] [PubMed] [Google Scholar]
- 109.Jung SL S. Lee S.Bae S.Imaoka.Harada K.Shimada H. Relationship between physical activity levels and depressive symptoms in community-dwelling older Japanese adults. Geriatr Gerontol Int. 2018;18(3):421–7. doi: 10.1111/ggi.13195 [DOI] [PubMed] [Google Scholar]
- 110.Kapteyn AB J. Hamer M.Smith J. P.Steptoe A.van Soest A.Koster A. et al. What they say and what they do: comparing physical activity across the USA, England and the Netherlands. J Epidemiol Community Health. 2018;72(6):471–6. doi: 10.1136/jech-2017-209703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Keadle SKS E. J. Freedson P. S.Lee I. M. Impact of accelerometer data processing decisions on the sample size, wear time and physical activity level of a large cohort study. BMC Public Health. 2014;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Keevil VLC, Andrew J M. Wijndaele, KatrienRobert Luben, Wareham, Nicholas J.Brage Soren et al. Objective Sedentary Time, Moderate-to- Vigorous Physical Activity, and Physical Capability in a British Cohort. Medicine & Science in Sports & Exercise. 2016;48(3):421–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kim YB R. D. Lee D. C.Welk G. J. Associations of movement behaviors and body mass index: comparison between a report-based and monitor-based method using Compositional Data Analysis. International Journal of Obesity. 2021;45(1):266–75. doi: 10.1038/s41366-020-0638-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.King WCC J. Y. Courcoulas A. P.Mitchell J. E.Wolfe B. M.Patterson E. J.Inabnet W. B.et al. Objectively-measured sedentary time and cardiometabolic health in adults with severe obesity. Prev Med. 2016;84:12–8. doi: 10.1016/j.ypmed.2015.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kiselev JN T. Spira D.Buchmann N.Steinhagen-Thiessen E.Lederer C.Daumer M.et al. Long-term gait measurements in daily life: Results from the Berlin Aging Study II (BASE-II). PLoS One. 2019;14(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kitano NK Y. Jindo T.Tsunoda K.Arao T. Compositional data analysis of 24-hour movement behaviors and mental health in workers. Prev Med Rep. 2020;20:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Koivula RWA-P N. Giordano G. N.White T.Adamski J.Bell J. D.Beulens J.et al.Imi Direct, Consortium. The role of physical activity in metabolic homeostasis before and after the onset of type 2 diabetes: an IMI DIRECT study. Diabetologia. 2020;63(4):744–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Koohsari MJS A. Ishii K.Kurosawa S.Yasunaga A.Hanibuchi T.Nakaya T.et al. Built environment correlates of objectively-measured sedentary behaviours in densely-populated areas. Health Place. 2020;66(): 102447. doi: 10.1016/j.healthplace.2020.102447 [DOI] [PubMed] [Google Scholar]
- 119.Laakkonen EKK J. Aukee P.Hakonen H.Kujala U. M.Lowe D. A.Kovanen V.et al. Female reproductive factors are associated with objectively measured physical activity in middle-aged women. PLoS One. 2017;12(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.LaCroix AZR-S E. Buchner D.Evenson K R Di C. Z.Lee I. M.Marshall. et al. The Objective Physical Activity and Cardiovascular Disease Health in Older Women (OPACH) Study. BMC Public Health. 2017;17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lakoski SGK, Julia. Ethnic Differences in Physical Activity and Metabolic Risk: The Dallas Heart Study. Medicine & Science in Sports & Exercise. 2014;46(6):1124–32. [DOI] [PubMed] [Google Scholar]
- 122.Lee PHY Y. Y. McDowell I.Leung G. M.Lam T. H. A cluster analysis of patterns of objectively measured physical activity in Hong Kong. Public Health Nutr. 2013;16(8):1436–44. doi: 10.1017/S1368980012003631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lee SWS J. S. Song B. M.Lee H. J.Bae H. Y.Park J. H.Choi H. R. et al. Comparison of self-reported and accelerometer-assessed measurements of physical activity according to socio-demographic characteristics in Korean adults. Epidemiol Health. 2018;40:e2018060. doi: 10.4178/epih.e2018060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lo Cascio CMQ M. Hoffman E. A.Bertoni A. G.Aaron C. P.Schwartz J. E.Avdalovic M. V. et al. Percent Emphysema and Daily Motor Activity Levels in the General Population: Multi-Ethnic Study of Atherosclerosis. Chest. 2017;151(5):1039–50. doi: 10.1016/j.chest.2016.11.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lu ZL F. M. H. Leung J. C. S.Kwok T. C. Y. The U-shaped relationship between levels of bouted activity and fall incidence in community-dwelling older adults: a prospective cohort study. J Gerontol A Biol Sci Med Sci. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Luke AB P. Plange-Rhule J.Forrester T. E.Lambert E. V.Schoeller D. A.Dugas L. R. et al. A mixed ecologic-cohort comparison of physical activity & weight among young adults from five populations of African origin. BMC Public Health. 2014;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Ma YQY B. Fan S. H.Luo Y. Z.Wen X. Association between Air Quality and Sedentary Time in 3270 Chinese Adults: Application of a Novel Technology for Posture Determination. J Clin Med. 2018;7(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mumford SLJ E. Kim K.Ahmad M.Salmon S.Summers K.Chaney K. et al. A Prospective Cohort Study to Evaluate the Impact of Diet, Exercise, and Lifestyle on Fertility (IDEAL): Design and Baseline Characteristics. Am J Epidemiol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Murayama HA S. Inoue S.Fujiwara T.Shobugawa Y. Sekentei and objectively-measured physical activity among older Japanese people: a cross-sectional analysis from the NEIGE study. BMC Public Health. 2019;19(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Nagai KT K. Kusunoki H.Wada Y.Tsuji S.Ito M.Sano K. et al. Isotemporal substitution of sedentary time with physical activity and its associations with frailty status. Clinical Interventions in Aging. 2018;13:1831–6. doi: 10.2147/CIA.S175666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Natarajan AP A. Emir-Faronas H.Natarajan P. Heart rate variability with photoplethysmography in 8 million individuals: a cross-sectional study. Lancet Digital Health. 2020;2(12):E650–E7. doi: 10.1016/S2589-7500(20)30246-6 [DOI] [PubMed] [Google Scholar]
- 132.Niemela MK M. Farrahi V.Kiviniemi A.Leinonen A. M.Ahola R.Puukka K. et al. Intensity and temporal patterns of physical activity and cardiovascular disease risk in midlife. Prev Med. 2019;124:33–41. doi: 10.1016/j.ypmed.2019.04.023 [DOI] [PubMed] [Google Scholar]
- 133.Nishida YH Y. Taguchi N.Hara M.Nakamura K.Nanri H.Imaizumi T. et al. Objectively measured physical activity and inflammatory cytokine levels in middle-aged Japanese people. Prev Med. 2014;64:81–7. doi: 10.1016/j.ypmed.2014.04.004 [DOI] [PubMed] [Google Scholar]
- 134.Nygaard IEW A. Bardsley T.Egger M. J.Shaw J. M. Early postpartum physical activity and pelvic floor support and symptoms 1 year postpartum. Am J Obstet Gynecol. 2021;224(2):193. doi: 10.1016/j.ajog.2020.08.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Okely JAC I. Shaw R. J.Chastin S. F.Dall P. M.Deary I. J.Der G. et al. Positive and negative well-being and objectively measured sedentary behaviour in older adults: evidence from three cohorts. BMC Geriatr. 2019;19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Osuka YY N. Kim M.Seino S.Nemoto M.Jung S.Okubo Y. et al. Association between habitual light-intensity physical activity and lower-extremity performance: A cross-sectional study of community-dwelling older Japanese adults. Geriatr Gerontol Int. 2015;15(3):268–75. doi: 10.1111/ggi.12268 [DOI] [PubMed] [Google Scholar]
- 137.Park SP S. Y. Oh G.Yoon E. J.Oh I. H. Association between Reallocation Behaviors and Subjective Health and Stress in South Korean Adults: An Isotemporal Substitution Model. Int J Environ Res Public Health. 2020;17(7). doi: 10.3390/ijerph17072488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Peters TMM S. C. Xiang Y. B.Yang G.Shu X. O.Ekelund U.Ji B. et al. E.Leitzmann, M. F. Accelerometer-measured physical activity in Chinese adults. Am J Prev Med. 2010;38(6):583–91. doi: 10.1016/j.amepre.2010.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Petersen TLB J. C. Kristensen P. L.Aadland E.Grøntved A.Jepsen R. Resemblance in accelerometer-assessed physical activity in families with children: the Lolland-Falster Health Study. Int J Behav Nutr Phys Act. 2020;17(1):161. doi: 10.1186/s12966-020-01067-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ramires VVW F. C. Bohm A. W.Galliano L.Ekelund U.Brage S.da Silva I. C. M. Physical activity levels objectively measured among older adults: a population-based study in a Southern city of Brazil. International Journal of Behavioral Nutrition and Physical Activity. 2017;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Rapp KK J. Benzinger P.Franke S.Denkinger M. D.Peter R.Acti F. E. et al. Physical performance and daily walking duration: associations in 1271 women and men aged 65–90 years. Aging Clin Exp Res. 2012;24(5):455–60. doi: 10.3275/8264 [DOI] [PubMed] [Google Scholar]
- 142.Rees-Punia E, Charles E.Evans, Ellen M.Keadle, Sarah K.Anderson Rebecca L.Gay Jennifer L. et al. Demographic-specific Validity of the Cancer Prevention Study-3 Sedentary Time Survey. Medicine & Science in Sports & Exercise. 2019;51(1):41–8. doi: 10.1249/MSS.0000000000001743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Rosenberg DW R. Greenwood-Hickman M. A.Bellettiere J.Xiang Y. H.Richmire K.Higgins M. et al. Device-assessed physical activity and sedentary behavior in a community-based cohort of older adults. BMC Public Health. 2020;20(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Roth MAM, Jennifer S. Who Provides Accelerometry Data? Correlates of Adherence to Wearing an Accelerometry Motion Sensor: The 2008 Health Survey for England. Journal of Physical Activity & Health. 2013;10(1):70–8. doi: 10.1123/jpah.10.1.70 [DOI] [PubMed] [Google Scholar]
- 145.Sabia SC P. van Hees V. T.Bell J. A.Elbaz A.Kivimaki M.Singh-Manoux A. Physical Activity and Adiposity Markers at Older Ages: Accelerometer Vs Questionnaire Data. J Am Med Dir Assoc. 2015;16(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Saelens BEM A. V. Kang B.Hurvitz P. M.Zhou C. Relation Between Higher Physical Activity and Public Transit Use. American Journal of Public Health. 2014;104(5):854–9. doi: 10.2105/AJPH.2013.301696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Sagelv EHE U. Pedersen S.Brage S.Hansen B. H.Johansson J.Grimsgaard S. et al. Physical activity levels in adults and elderly from triaxial and uniaxial accelerometry. The Tromso Study. PLoS One. 2019;14(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sallis JFS B. E. Frank L. D.Conway T. L.Slymen D. J.Cain K. L.Chapman J. E. et al. Neighborhood built environment and income: Examining multiple health outcomes. Social Science & Medicine. 2009;68(7):1285–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Salvo DT C. Villa U.Rivera J. A.Sarmiento O. L.Reis R. S.Pratt M. Accelerometer-based physical activity levels among Mexican adults and their relation with sociodemographic characteristics and BMI: a cross-sectional study. International Journal of Behavioral Nutrition and Physical Activity. 2015;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Santos DAJ P. B. Magalhães J. P.Correia I. R.Silva A. M.Baptista F.Sardinha L. B. Patterns of accelerometer-derived sedentary time across the lifespan. J Sports Sci. 2018;36(24):2809–17. doi: 10.1080/02640414.2018.1474537 [DOI] [PubMed] [Google Scholar]
- 151.Savin KLP S. R. Clark T. L.Bravin J. I.Roesch S. C.Sotres-Alvarez D.Mossavar-Rahmani Y. et al. Relationships of Sleep Duration, Midpoint, and Variability with Physical Activity in the HCHS/SOL Sueno Ancillary Study. Behav Sleep Med. 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Schrack JAK P. L. Wanigatunga A. A.Di J. R.Simonsick E. M.Spira A. P.Ferrucci L. et al. Active-to-Sedentary Behavior Transitions, Fatigability, and Physical Functioning in Older Adults. Journals of Gerontology Series a-Biological Sciences and Medical Sciences. 2019;74(4):560–7. doi: 10.1093/gerona/gly243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Semaan SD T. A. Tison G. H.Nah G.Vittinghoff E.Pletcher M. J.Olgin J. E. et al. Physical activity and atrial fibrillation: Data from wearable fitness trackers. Heart Rhythm. 2020;17(5 Pt B):842–6. doi: 10.1016/j.hrthm.2020.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Shapiro AB B. Landes S.Kammann P.De Fer B. B.Lee W. N.Lange R. A novel digital approach to describe real world outcomes among patients with constipation. Npj Digital Medicine. 2021;4(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Shapiro AM N. Clay I.Bradshaw B.Ramirez E.Min J.Trister A. et al. Characterizing COVID-19 and Influenza Illnesses in the Real World via Person-Generated Health Data. Patterns (N Y). 2021;2(1):100188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Sohail SY L. Bennett D. A.Buchman A. S.Lim A. S. Irregular 24-hour activity rhythms and the metabolic syndrome in older adults. Chronobiol Int. 2015;32(6):802–13. doi: 10.3109/07420528.2015.1041597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Solbraa AK, Sigmund AlfredHolme, Ingar MortenKolle, Elin Hansen, Bjørge HermanAshe, Maureen C. The built environment correlates of objectively measured physical activity in Norwegian adults: A cross-sectional study. Journal of Sport & Health Science. 2018;7(1):19–26. doi: 10.1016/j.jshs.2017.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Spartano NLD S. Himali J. J.Dukes K. A.Murabito J. M.Vasan R. S.Beiser A. S. et al. Accelerometer-determined physical activity and cognitive function in middle-aged and older adults from two generations of the Framingham Heart Study. Alzheimers Dement (N Y). 2019;5:618–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Stappers NEHVK D. H. H. De Vries N. K.Kremers S. P. J. Do Physical Activity Friendly Neighborhoods Affect Community Members Equally? A Cross-Sectional Study. Int J Environ Res Public Health. 2018;15(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Steene-Johannessen JA S. A. van der Ploeg H. P.Hendriksen I. J.Donnelly A. E.Brage S.Ekelund U. Are Self-report Measures Able to Define Individuals as Physically Active or Inactive? Med Sci Sports Exerc. 2016;48(2):235–44. doi: 10.1249/MSS.0000000000000760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Stenback VM S. J. Leppaluoto J.Gagnon D. D.Makela K. A.Jokelainen J.Keinanen-Kiukaanniemi S. et al. Association of Physical Activity With Telomere Length Among Elderly Adults—The Oulu Cohort 1945. Front Physiol. 2019;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Straker LMH G. L. Mountain J.Howie E. K.White E.McArdle N.Eastwood P. R. Rationale, design and methods for the 22 year follow-up of the Western Australian Pregnancy Cohort (Raine) Study. BMC Public Health. 2015;15:663. doi: 10.1186/s12889-015-1944-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Tranah GJB T. Ancoli-Israel S.Paudel M. L.Ensrud K. E.Cauley J. A.Redline S. et al. Circadian activity rhythms and mortality: the study of osteoporotic fractures. J Am Geriatr Soc. 2010;58(2):282–91. doi: 10.1111/j.1532-5415.2009.02674.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Troiano RPB D. Dodd K. W.Masse L. C.Tilert T.McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. doi: 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- 165.van Ballegooijen AJvdP, Hidde P.Visser Marjolein. Daily sedentary time and physical activity as assessed by accelerometry and their correlates in older adults. European Reviews of Aging & Physical Activity. 2019;16(1):N.PAG-N.PAG. doi: 10.1186/s11556-019-0210-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.van der Berg JDS C. D. A.Bosma H.van der Velde, JhpmWillems P. J. B.Savelberg HhcmSchram, M. T.Sep S. J. S.et al. Associations of total amount and patterns of sedentary behaviour with type 2 diabetes and the metabolic syndrome: The Maastricht Study. Diabetologia. 2016;59(4):709–18. doi: 10.1007/s00125-015-3861-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Van Dyck D, GreetDeforche BenedicteGiles-Corti, BillieSallis JamesOwen, NevilleBourdeaudhuij Ilse. Environmental and Psychosocial Correlates of Accelerometer-Assessed and Self-Reported Physical Activity in Belgian Adults. International Journal of Behavioral Medicine. 2011;18(3):235–45. doi: 10.1007/s12529-010-9127-4 [DOI] [PubMed] [Google Scholar]
- 168.Waller KV-Y H. Tormakangas T.Hautasaari P.Lindgren N.Iso-Markku P.Heikkila K et al. Long-term leisure-time physical activity and other health habits as predictors of objectively monitored late-life physical activity—A 40-year twin study. Sci Rep. 2018;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Wang CL O. Hachen D. S. Using Fitbit data to examine factors that affect daily activity levels of college students. PLoS One. 2021;16(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Watanabe DY T. Watanabe Y.Yamada Y.Kimura M.Kyoto-Kameoka Study, Grp. Objectively Measured Daily Step Counts and Prevalence of Frailty in 3,616 Older Adults. J Am Geriatr Soc. 2020;68(10):2310–8. doi: 10.1111/jgs.16655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Wennman HP A. Rissanen H.Valkeinen H.Partonen T.Maki-Opas T.Borodulin K. Gender, age and socioeconomic variation in 24-hour physical activity by wrist-worn accelerometers: the FinHealth 2017 Survey. Sci Rep. 2019;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.White DKT-L C. Felson D. T.Gross K. D.Niu J. B.Nevitt M.Lewis C. E. et al. Do radiographic disease and pain account for why people with or at high risk of knee osteoarthritis do not meet physical activity guidelines? Arthritis Rheum. 2013;65(1):139–47. doi: 10.1002/art.37748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.White TW K. Wareham N. J.Brage S. Estimation of Physical Activity Energy Expenditure during Free-Living from Wrist Accelerometry in UK Adults. PLoS One. 2016;11(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Witham MDD P. T. Vadiveloo T.Sniehotta F. F.Crombie I. K.Feng Z. Q.McMurdo M. E. T. Association of Day Length and Weather Conditions with Physical Activity Levels in Older Community Dwelling People. PLoS One. 2014;9(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Yoshioka MA M. Yahiro T.Higuchi H.Higaki Y.St-Amand J.Miyazaki H.et al. Long-period accelerometer monitoring shows the role of physical activity in overweight and obesity. International Journal of Obesity. 2005;29(5):502–8. doi: 10.1038/sj.ijo.0802891 [DOI] [PubMed] [Google Scholar]
- 176.Troiano R. A timely meeting: Objective measurement of physical activity. Med Sci Sports Exerc. 2005;37(11 supplement):S487–S9. doi: 10.1249/01.mss.0000185473.32846.c3 [DOI] [PubMed] [Google Scholar]
- 177.Shin G, Jarrahi MH, Fei Y, Karami A, Gafinowitz N, Byun A, et al. Wearable activity trackers, accuracy, adoption, acceptance and health impact: A systematic literature review. J Biomed Inform. 2019;93:103153. doi: 10.1016/j.jbi.2019.103153 [DOI] [PubMed] [Google Scholar]
- 178.Rising CJ, Gaysynsky A, Blake KD, Jensen RE, Oh A. Willingness to Share Data From Wearable Health and Activity Trackers: Analysis of the 2019 Health Information National Trends Survey Data. JMIR mHealth and uHealth. 2021;9(12):e29190. doi: 10.2196/29190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Omura JD, Carlson SA, Paul P, Watson KB, Fulton JE. National physical activity surveillance: Users of wearable activity monitors as a potential data source. Prev Med Rep. 2016;5:124–6. doi: 10.1016/j.pmedr.2016.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Ramirez Varela A, Cruz GIN, Hallal P, Blumenberg C, da Silva SG, Salvo D, et al. Global, regional, and national trends and patterns in physical activity research since 1950: a systematic review. The international journal of behavioral nutrition and physical activity. 2021;18(1):5. doi: 10.1186/s12966-020-01071-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Ramirez Varela A, Pratt M. The GoPA! Second Set of Country Cards Informing Decision Making for a Silent Pandemic. Journal of physical activity & health. 2021;18(3):245–6. doi: 10.1123/jpah.2020-0873 [DOI] [PubMed] [Google Scholar]
- 182.Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. The Lancet Global health. 2018;6(10):e1077–e86. [DOI] [PubMed] [Google Scholar]
- 183.Conger SA, Toth LP, Cretsinger C, Raustorp A, Mitas J, Inoue S, et al. Time Trends in Physical Activity Using Wearable Devices: A Systematic Review and Meta-analysis of Studies from 1995 to 2017. Med Sci Sports Exerc. 2022;54(2):288–98. doi: 10.1249/MSS.0000000000002794 [DOI] [PubMed] [Google Scholar]
- 184.Rosenberger ME, Fulton JE, Buman MP, Troiano RP, Grandner MA, Buchner DM, et al. The 24-Hour Activity Cycle: A New Paradigm for Physical Activity. Med Sci Sports Exerc. 2019;51(3):454–64. doi: 10.1249/MSS.0000000000001811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Migueles JH, Cadenas-Sanchez C, Ekelund U, Delisle Nystrom C, Mora-Gonzalez J, Lof M, et al. Accelerometer Data Collection and Processing Criteria to Assess Physical Activity and Other Outcomes: A Systematic Review and Practical Considerations. Sports medicine (Auckland, NZ. 2017;47(9):1821–45. doi: 10.1007/s40279-017-0716-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Migueles JH, Cadenas-Sanchez C, Rowlands AV, Henriksson P, Shiroma EJ, Acosta FM, et al. Comparability of accelerometer signal aggregation metrics across placements and dominant wrist cut points for the assessment of physical activity in adults. Sci Rep. 2019;9(1):18235. doi: 10.1038/s41598-019-54267-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Aadland E, Ylvisaker E. Reliability of the Actigraph GT3X+ Accelerometer in Adults under Free-Living Conditions. PLoS One. 2015;10(8):e0134606. doi: 10.1371/journal.pone.0134606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Farrahi V, Niemela M, Kangas M, Korpelainen R, Jamsa T. Calibration and validation of accelerometer-based activity monitors: A systematic review of machine-learning approaches. Gait & posture. 2019;68:285–99. doi: 10.1016/j.gaitpost.2018.12.003 [DOI] [PubMed] [Google Scholar]
- 189.Stamatakis E, Owen KB, Shepherd L, Drayton B, Hamer M, Bauman AE. Is Cohort Representativeness Passe? Poststratified Associations of Lifestyle Risk Factors with Mortality in the UK Biobank. Epidemiology. 2021;32(2):179–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, et al. Comparison of Sociodemographic and Health-Related Characteristics of UK Biobank Participants With Those of the General Population. Am J Epidemiol. 2017;186(9):1026–34. doi: 10.1093/aje/kwx246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Morris J, Heady J, Raffle P, Roberts C, Parks J. Coronary heart disease and physical activity of work. Lancet. 1953;Nov 21, 1953:1053–7, 111–120. [DOI] [PubMed] [Google Scholar]
- 192.Varela AR, Pratt M, Harris J, Lecy J, Salvo D, Brownson RC, et al. Mapping the historical development of physical activity and health research: A structured literature review and citation network analysis. Prev sMed. 2018;111:466–72. doi: 10.1016/j.ypmed.2017.10.020 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
The dataset is available in a public repository: Accelerometer level dataset: https://doi.org/10.15139/S3/8GPGJZ Cohort level dataset: https://doi.org/10.15139/S3/ZYVHUO.