Abstract
Background
Despite growing emphasis on empathic care, numerous studies demonstrate diminishing empathy in medical students. Involving patient educators in medical curricula may be a solution. Therefore, we conducted a systematic review to evaluate patient-involved interventions that promote empathy among medical students.
Method
A literature search of MEDLINE, Embase, PsycINFO, and ERIC databases was performed using the keywords “empathy,” “medical student,” and their synonyms. Results were independently screened in duplicate. Conflicts were resolved by group consensus. All English studies describing interventions that promote empathy in medical students engaging patient educators were included. Relevant data was extracted and summarized.
Results
1467 studies were screened. 14 studies were included, of which 10 were pilot studies. Studies included patient involved interventions such as storytelling (5/14), shadowing patients (3/14), recorded videos (3/14), or combinations of methods (3/14). Qualitative measurements of empathy included written feedback and group discussions. Quantitative measurements included validated scales measuring empathy. All studies demonstrated increase in empathy among medical students. Participants reported satisfaction with training and patients reported being proud of giving back by training future physicians.
Conclusion
Interventions engaging patient educators were shown to have a positive impact on medical student empathy. Furthermore, patient-led education was shown to increase medical student understanding of subject and knowledge retention while empowering patients. Further implementation of patient-involved education is an important step forward in patient-partnered care and may identify additional advantages of patient engagement in medical education.
Abstract
Contexte
Malgré l’importance grandissante accordée à l’empathie dans les soins de santé, de nombreuses études démontrent une diminution de l’empathie chez les étudiants en médecine. La participation de patients éducateurs dans les programmes d’études médicales pourrait être une solution. Nous avons donc réalisé une revue systématique pour évaluer les interventions qui visent à promouvoir l’empathie chez les étudiants et qui font participer des patients.
Méthode
Nous avons effectué une recherche dans les bases de données MEDLINE, Embase, PsycINFO et ERIC en utilisant les mots-clés «empathie», «étudiant en médecine» et leurs synonymes. Les résultats ont été examinés de manière indépendante et en double. Les conflits ont été résolus par consensus de groupe. Toutes les études en anglais décrivant des interventions visant à promouvoir l’empathie chez les étudiants en médecine avec la participation de patients éducateurs ont été incluses. Les données pertinentes ont été extraites et résumées.
Résultats
Des 1467 études examinées, 14 ont été incluses, dont 10 études pilotes. Les interventions avec des patients mentionnées dans les études comprenaient des récits (5/14), l’observation des patients (3/14), des vidéos enregistrées (3/14) ou des combinaisons de méthodes (3/14). Les mesures qualitatives de l’empathie comprenaient des commentaires écrits et des discussions de groupe. Les mesures quantitatives étaient des échelles validées mesurant l’empathie. Toutes les études indiquent une augmentation de l’empathie chez les étudiants en médecine. Les participants se disent satisfaits de la formation et les patients déclarent être fiers de redonner aux soignants en contribuant à former les futurs médecins.
Conclusion
Les interventions faisant appel à des patients éducateurs ont eu un effet positif sur le développement de l’empathie des étudiants en médecine. En outre, il a été démontré que la participation de patients dans la formation augmentait la compréhension du sujet et la rétention des connaissances par les étudiants en médecine tout en responsabilisant les patients. La généralisation de l’intervention des patients dans l’éducation constitue une avancée importante dans les soins en partenariat avec le patient et pourrait révéler d’autres avantages de la participation des patients dans l’éducation médicale.
Introduction
Empathy, or a physician’s ability to understand a patient’s unique situation and emotions, to communicate their understanding back to the patient to determine accuracy, and to act in an altruistic manner according to the patient’s values, beliefs, and priorities, is a critical component of care.1 Patients cared for by empathetic physicians are more likely to be satisfied with their care, to trust their physicians, to adhere to treatment plans, and to have better outcomes.2,3 Additionally, developing and nurturing physician empathy has beneficial effects not only for strengthening the doctor-patient relationship but also for fostering patient and physician well-being. Not only are patients less stressed, depressed, and aggressive when healthcare providers empathize with them, but empathy also decreases physician burnout, lowers malpractice rates, and enhances overall physician wellness.4–6
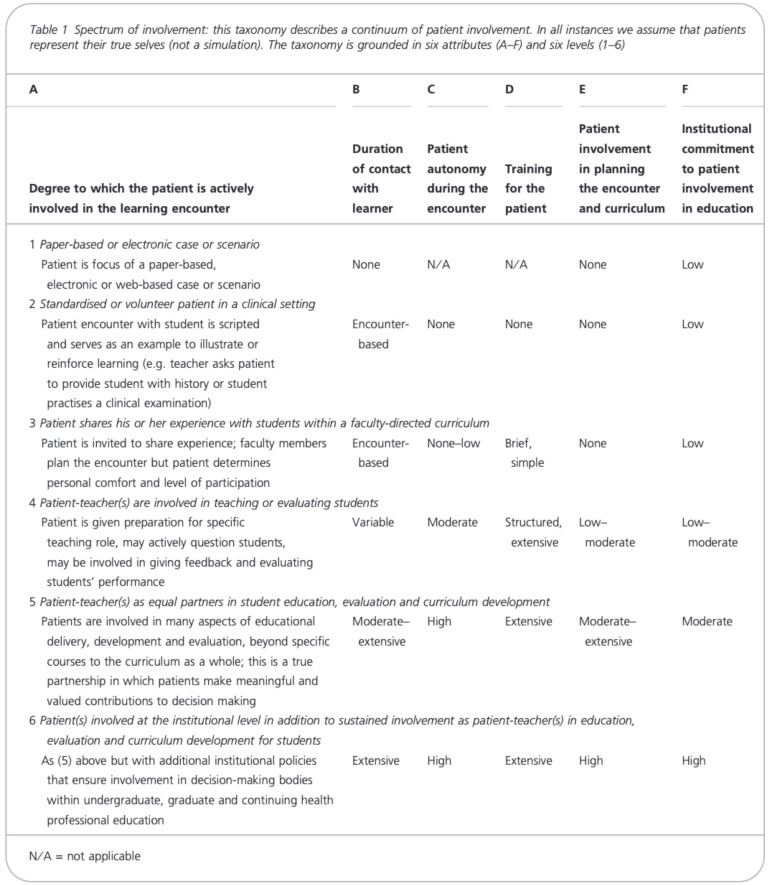
Recent studies, however, suggest that empathy declines as trainees progress along the medical education continuum for reasons including long working hours, reduced quality of life, decreased time spent with patients, understaffed work environments, increased workload, and heightened pressure to meet targets.7–12 An array of methods have been used to stem this decline, including those involving patients teaching empathy to learners.13,14 Since patient involvement in medical education may range from their passive involvement as a subject of examination during clinical encounters to their active facilitation of learning,15 Towle and colleagues developed a taxonomy of engagement based on the depth of involvement of the patient in the process of creating and administrating educational initiatives.16
Although neither the level of patient engagement nor outcomes of patient teaching sessions have been robustly synthesized, the benefits of patient-led empathy interventions seem promising. For instance, understanding empathy from the patient point of view appears to impart valuable learning for medical students.16 Moreover, increased exposure to patients outside of the clinical setting may shift students’ focus from the biomedical to the humanistic during care encounters, thus enhancing medical student empathy, confidence, and insight into various aspects of disease.17 However, despite calls for their greater inclusion in medical education, patients largely remain an untapped resource in undergraduate training.16,18 Myriad factors, including concerns about feasibility, safety, and credibility, seem to impede formal, systematic, and meaningful patient engagement in medical education.15,16,19–21 Since sound evidence could shift perceptions and spark the curricular innovations required for greater patient involvement, we conducted a systematic review of the literature to examine and evaluate patient-led interventions aimed at boosting medical students’ empathy.
Method
Search strategy
This systematic review followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines.22 A comprehensive literature search of four bibliographic databases including MEDLINE, Embase, PsycINFO, and ERIC was performed from inception to April 2020 using the keywords “empathy,” “medical student,” and any of their synonyms. No search restrictions were applied. The search strategy was developed with help from the institution’s research librarian (Appendix A).
Eligibility
Studies that described an original educational intervention that aimed to improve empathy in medical students using current or former patients as educators were included. Studies that did not incorporate patients as active participants in teaching empathy were excluded. Active participation in this study was defined according to Towle and colleagues classification.16 Their classification is based on the duration of the encounter, the patient’s autonomy, their involvement in curriculum planning, and the degree of institutional commitment to including patients in education (Appendix B). To ensure we captured initiatives with active patient participation, Towle’s Level three (patients share their experiences) was the minimum required for inclusion. Any type of peer-reviewed studies except review articles, editorials or letters, and conference abstracts were included.
Study selection and data extraction
All search results were exported to Covidence (Veritas Health Innovation, Melbourne, Australia) for screening. Articles were divided among the authors (MB, AL, IK, EMA, MY) so that each article was independently screened in duplicate by title and abstract for potentially eligible papers. These articles underwent further full-text screening in duplicate. Any conflicts were resolved by consensus or by a third author (KAL) when disagreement persisted.
Data from the included studies were subsequently extracted by two authors, in a similar form to the screening process, using the standardized form in Covidence. This included study characteristics (publication year, study design, country of study), number and type of participants, details regarding the intervention (mode of patient involvement, level of interaction with students, duration of intervention), and the study findings (quantitative or qualitative measures, measurement tools used, and impact on empathy).
Summary of results
Extracted data were summarized in tabular or diagrammatic form along with a narrative summary. The settings, populations, and study designs for each article, along with the interventions’ teaching content and reported findings were summarized. A meta-analysis and formal assessment of methodological quality were not performed due to the anticipated heterogeneity of methodology and outcomes among the included studies. Procedures were reviewed by the expert statisticians at the Ottawa Methods Centre to ensure conformity with systemic review standards.
Results
The literature search yielded 2237 studies of which 770 duplicates were removed, resulting in 1467 papers screened by title and abstract. Seventy articles were appropriate for further full-text screening, resulting in 14 studies that met eligibility (Figure 1). A summary of each study’s interventions can be found in Table 1, and summaries of the measurement methods and results of each study can be seen in Table 2.
Figure 1.
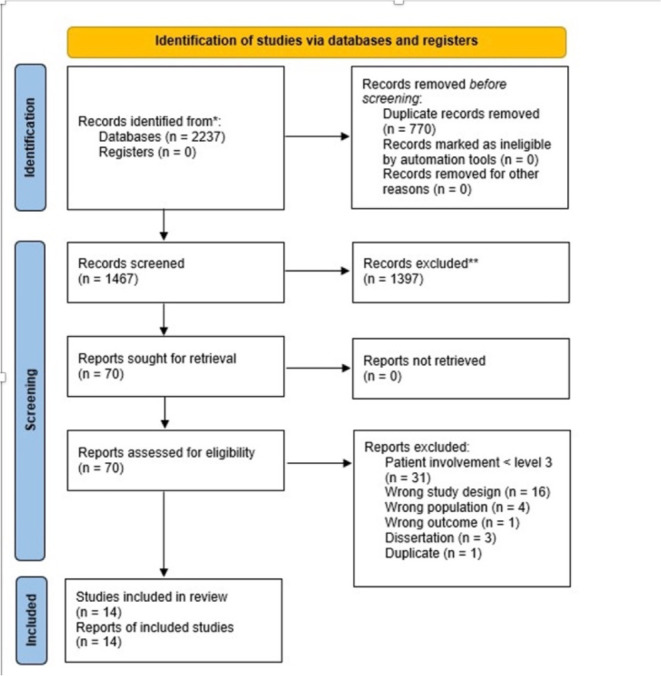
PRIMSA 2020 flow diagram for the number of articles included in the literature search and screening
Table 1.
Summary of interventions based on type of patient involvement.
| Type of Intervention | Paper | Summary of Intervention |
|---|---|---|
| Direct | Chandrasekar18 | Storytelling workshop: medical students interviewed patient families and created a video of the family’s experience |
| Cumberland21 | Medical students were paired with patients with Parkinson’s disease. | |
| Morhardt30 | Buddy program: pairing medical students with a patient diagnosed with Dementia with monthly program meetings | |
| Shuja23 | Home visits: medical students visiting patients with various disabilities within their home environment | |
| Player24 | Patients, who were homeless and had tri-morbidity (physical health, mental health, and substance abuse), shared their narratives with medical students as part of the “humanising medicine” lecture. | |
| Hennrikus29 | Patient spoke to medical students about their medical experience and medical students wrote about their reflections. | |
| Hendriksz28 | Medical students participated in sessions where patients shared their medical experiences. | |
| Chretien27 | Medical students took part in a narrative medicine curriculum that involved an introduction session, a patient storytelling activity, and a group reflection session. | |
| Luchetti19 | Medical students took part in the “Geriatrics and Gerontology” course that involved in person activities and didactic classes. | |
| Bramstedt22 | A small number of medical students interviewed patients, while the rest of the medical students observed the telemedicine session. | |
| Direct and Indirect | Shapiro31 | Medical students took part in the Human Kindness curriculum that included both lectures and patient interactions. |
| Indirect | Kieran Sweeney, Paul Baker20 | Medical students watched videos of patients sharing their experiences on navigating the healthcare system and interacting with the healthcare team. |
| Chen26 | Medical students played an interactive video game called “That Dragon, Cancer” in which the players take the roles of the parents of a terminally ill child. | |
| Singh25 | Medical students took part in simulations that involved case discussions and videos of patients who had hospital acquired infections. |
Table 2.
Summary of measurement type, measurement used, and results of each study.
| Author(s) | Type of measurement | Measurement used to assess empathy | Results of changes in empathy |
|---|---|---|---|
| Chandrasekar H. et al (2018)18 | Qualitative | Focus groups were conducted to assess whether students found that the workshop enhanced their learning. | Increased student insights into patients’ home lives. Students explained that narratives enabled greater understanding of nonphysician partners within the health care system. One student stated, “It broadly opened up my considering of patients’ lives after leaving the hospital and ways that their specific disease can continue to have an impact on all the different aspects of their life outside of just the symptoms that we might try to manage.” |
| Lucchetti A. et al (2019)19 | Quantitative | Modified Maxwell–Sullivan Attitudes Scale measured empathy and attitudes towards the elderly. | Statistically significant increase in attitudes measured by UCLA-GAS(r = 0.55-0.81, P < 0.001) and empathy towards geriatrics patients measured by the Modified Maxwell-Sullivan Attitudes Scale (r = 0.51, P < 0.001). However, there were other components of the curriculum that did not include patients. |
| Kieran Sweeney, Paul Baker (2018)20 | Quantitative and qualitative | Patient Practitioner Orientation Scale was used to measure patient-centered attitude. Post-session feedback forms were used to assess the behavioural changes students made when interacting with patients. | 21 students (54%) demonstrated an increase in patient-centred attitudes, whereas 13 students (33%) demonstrated no change, and five students (13%) demonstrated a decreased score. The mean pre-session score was 78.8, whereas the mean post-session score was 82.0. Students reported that the session had given them insight into the patient experience and felt an emphasis on the value of relational care. |
| Cumberland et al. (2019)21 | Quantitative and qualitative | Paper-based surveys (pre/post), Parkinson Attitude Scale and focus groups with students and patients were used to assess knowledge and empathy. | PD knowledge scores significantly increased with large effect size (pre-test mean = 14.77, [SD = 2.57]; post-test mean = 19.69 [SD = 2.06], Cohen’s d= 1.64). Significant change in Parkinson Attitude Scale score (p-value < 0.05) with small effect size: M= 53.66 at baseline and 55.49 at end of program with Cohen's d = 0.37. Survey results show that 91% students would recommend the program to others, and 82% would participate again. Focus group results showed that students saw their buddy as a human being and not just a patient, and that there was rise in empathy. |
| Darby Morhardt (2006)30 | Quantitative and qualitative | Pre- and post-tests were administered for knowledge of dementia. After each visit, the students were asked to write a summary of their buddy visit experience in a journal. Diagnosed individuals and their family members were asked to evaluate the program by completing a questionnaire. | Pre to post knowledge/attitude test scores improved on average (however the article did not include data to back up this claim as the authors decided that it was outside the scope of the article) Student reflections demonstrated growth in basic knowledge regarding Alzheimer’s disease and related dementias, and in empathy and compassion for persons with dementia as seen in excerpts of their written reflections. |
| Bramstedt et al. (2014)22 | Qualitative | Interviewers submitted narrative responses to 2 open-ended questions about their experience. Observing students completed an anonymous 10 question online survey. | All interview panelist students submitted overwhelmingly positive narrative responses to 2 open-ended questions about their experience. Indirect arm: 12/15 agreed that the session improved their understanding of the psychosocial burdens of dialysis, quality of life, and human suffering, and improved their empathy toward patients; 12/15 “Strongly agreed” or “Agreed” that the session encouraged reflective thinking and was an aid to improving their communication skills. |
| Shuja et al. (2014)23 | Qualitative | In-depth interviews and focus group discussions were conducted to examine student emotions, feelings, and experiences when interacting with people with disabilities. | Good feedback from all students on the effect of the visits on their compassion and empathy. Major themes reflective of the personal narratives were PWDs and their sufferings, putting yourself in other's shoes and working for PWDs. The positive responses from the students revealed that this exercise made them feel the actual pain & sufferings of others. |
| Shapiro et al. (2019)31 | Quantitative and qualitative | The Jefferson Scale for Empathy (JSE) specific for medical students was used to measure empathy. To assess the curriculum, individual medical student evaluations of each session were done. Narrative comments were also solicited and recorded. | In the pilot year, there were no significant intragroup differences pre-post HK curriculum (P = 0.451). Upon re-evaluation of second-year students in the pilot group in the latter part of their 3rd year, they did not show the characteristic “dip” in empathy documented in the literature (JSE post-HK curriculum MS2 = 114.8 standard deviation (SD) =12.7; JSE MS3 = 115.8, SD = 10.7). In the implementation year, with a revamped curriculum, scores improved significantly pre-post HK curriculum (P = 0.012 for MS1, P = 0.004 for MS2). Positive narrative entries noted the importance of incorporating clinical scenarios. Negative comments expressed doubts about being taught kindness and questioned the value of the empathetic video experience. |
| Player et al. (2019)24 | Qualitative | Anonymous questionnaires which were co-designed by expert patients and lecturers were completed by students evaluating changes in empathy and response to the lectures. The questionnaires included free text narrative responses. | Students reported through the questionnaires that the sessions led to a rich learning experience about compassionate care, understanding the complexities and struggles of marginalised groups and giving back. Subthemes included humanity, empathy and listening and holistic care. |
| Hennrikus, et al. (2018)29 | Qualitative | Written student illness scripts which included free response sections addressing humanism and health systems as well as end of the course student feedback were evaluated using a thematic analysis approach. | Qualitative results revealed 7 main themes among the students’ responses: patients make the basic science relevant, empathy and awareness, patient resilience, the doctor-patient relationship, cost of care, barriers to care, and support systems. |
| Hendriksz (2016)28 | Quantitative | Anonymous electronic surveys were used to assess perceptions on the effectiveness of the sessions. | Increased empathy in responses (F-score=41, P = 0.005). 89% agreed that the sessions increased their empathy. 71% agreed that the sessions achieved the objective of increased empathy. |
| Singh et al. (2017)25 | Quantitative & qualitative | The Toronto empathy questionnaire (TEQ) and an anonymous semi-structure feedback questionnaire were used to measure empathy and perceptions on the interventions. | Improved empathy scores measured by the Toronto Empathy Questionnaire after intervention in both groups compared to control (p = 0.011 for CDG & p = 0.046 for VSG). All students in the CDG and 88.5% in VSG felt that the session helped them assess the impact of healthcare-associated infections on patients' emotional, financial and social life and this helped them understand the difficulties faced by a patient and their relatives due to non-compliance to certain protocols. Most students (95.8%) thought the case discussion provided them an opportunity to explore their thoughts and emotions about patient suffering, which was felt by 80.8% of students in the VSG group. |
| Chen, et al. (2018)26 | Quantitative | The first 5 questions of Jefferson Scales of Physician Empathy (JSPE) with additional feedback questions were used to evaluate empathy as well as their perspective on the use of video games to teach empathy. | Improved average empathy scores on first 5 questions of JSPE compared to before playing the game (5.7738 vs 6.2322, p = <0.0001). Most students found video games to be a better and more interesting medium to teach empathy than didactic learning with 31% saying that learning empathy through a video game was more effective than through didactic learning and 64% saying that they preferred the video game format. |
| Chretien, et al. (2015)27 | Qualitative | Illness narratives and feedback from a writing prompt were used to evaluate students' learning and perspective on patient experience as well as group discussion sessions. | Students felt the activity was meaningful and rewarding, allowed them to see patients as patients more than an illness. Students also reported that their patient relationships felt enriched. Students brought out the following themes: patients are more than their disease, be open to opportunities to slow down and listen, stories give new insights into patients, 4) stories can affect patient care, and patients as individuals. |
Among the 14 included studies, 10 were pilot studies that have not yet been replicated or formally implemented into curricula.23–32 Only one of these papers repeated their study across more than one cohort,29 and only the paper by Singh et al. included a randomized control trial (RCT).30 The remaining four studies consisted of three that tested established curricula with patient teachers and one study that presented data for both the piloting phase and follow-up period.33–36 Most studies (n = 8) were published in 2018-2019. Studies were most frequently from the United States of America (n = 9; 64%) and the United Kingdom (n = 2; 14%).
Learners included students from all years of their undergraduate medical training, but studies most commonly involved third-year students (Figure 2). The role of the students varied across studies and included attending courses created by faculty (n = 8; 30%), interviewing patients or shadowing patients (n = 4; 15%), and participating in home visits (n = 1; 4%). In the study conducted by Hennrikus et al., 300 first year medical students attended lectures given by patients who shared a narrative experience of living with the disease that was taught during that week of class.34 In another study by Chretien, et al., 31 third year medical students attended focus groups where patients told stories of their illness experiences followed by group reflection sessions.32
Figure 2.
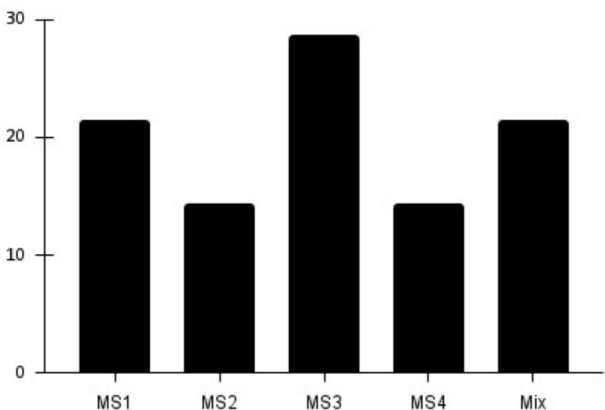
Total number of medical students assessed by interventions across all studies based on year of undergraduate medical training
The degree of patient involvement in the interventions varied among the studies. Patients were most frequently included as part of Level Three of Towle’s classification where they shared their experience with students within a faculty-directed curriculum.16 Among the studies with a Level three classification, the majority were direct interventions such as storytelling sessions, live sessions where patients would share their stories of lived experience with a disease to students,24,29,32–34 or patient shadowing where students accompanied and spent time with patients during their life at home or in the hospital to experience the effects of daily living with an illness.26,28,35 Other Level three studies used indirect interventions, such as students watching video interviews prepared by patients who shared their stories of living with disease.25,27,30,36 Three studies were able to achieve higher levels of involvement with Shapiro et al. and Player et al. having patients taking on a more autonomous teaching role (Towle level Four) as expert educators giving presentations and lectures to students, and with Chen et al. having a patient’s family create the intervention itself, a video game about the patient’s whole experience of life with their illness played by the medical students (Towle level five).29,31,36 Intervention duration varied among the studies, ranging from 60-minutes27 to two years.33,34
Methods to measure the effect on student empathy were heterogenous across studies. Empathy was most frequently assessed using transcriptions of student feedback (n = 8; 57%),25,27–29,32,34–36 and group discussion (n = 4; 15%).23,26,28,32 Quantitative measures included validated scores such as the Toronto Empathy Questionnaire,30 Modified Maxwell–Sullivan Attitudes Scale,24 and the Jefferson Scale of Physician Empathy-Student (JSPE-S).31,36
Outcomes
All studies demonstrated improved empathy post-intervention. Specifically, students responded that the intervention improved their understanding of patient’s emotions,23,28,29,32–34 increased appreciation for a holistic, biopsychosocial approach to patient care,26–29,32 improved their understanding of under-represented patient populations,24,28,35 and enhanced their communication skills.26,27 Quantitative findings showed significant increases in empathy scores compared to pre-intervention or to the control group.30,31,36 Attitude scores towards patients also showed significant increase post intervention.24,26,35
Student empathy was not the only positive result from these interventions. Medical knowledge and ability to retain information increased with patient involvement during teaching.24,30,33,34 This was shown specifically by Hennrikus et al. and Singh et al. who observed a significant increase in knowledge scores post intervention compared to pre-test and control group respectively.30,34 Although only a handful of studies directly evaluated student satisfaction with the sessions, most students reported sessions were interesting,30 enjoyable, rewarding, meaningful,32 fun and engaging.27 Additionally, most students reported that they would both participate again and recommend the program to others.26 Students did not seem to prefer one intervention over another, although their preferences were not explicitly explored. However, students provided feedback suggesting that interventions should be planned around their schedules,23,26,33,35 more clinically relevant,36 and include more interactive time with patients.32,33,36
Patient story-telling sessions were not only beneficial for students. Patients leading sessions reported “feeling like they are giving back,” “being proud of being an expert in this particular field,”26,29 and proud to impart influential learning for future physicians.23 Cumberland et al. reported that 86% of their patients would recommend the experience and 65% would participate in future interventions.26 Findings reported by Gordon and colleagues’ also suggested that patients both gained confidence in their knowledge of their diseases, and derived satisfaction from sharing their experiences and knowledge with future physicians.37
Discussion
The recency of the studies we reviewed suggests a heightened interest in, not only more meaningfully including patients as teachers in undergraduate medical education, but also evidencing the value of the learning patients impart. Although research in this area remains woefully limited, all included papers demonstrated positive outcomes across various training years, institutions, and various levels of patient engagement. Specifically, the papers that used RCTs,30 replications,29,33–35 or follow up data report that effects of patient-involved interventions were positive,36 significantly better than control, and had long-lasting benefits for students. Furthermore, the qualitative data unanimously suggest that students find patient-led teaching not only enjoyable but also valuable for generating the knowledge and skillset required for empathetic and competent patient centered care.23,25–30,32,34,35 By systematically examining and synthesizing this literature, our review provides compelling evidence to support the feasibility, credibility, and learning value of patient-led teaching38—not only for fostering empathy37,39 but also for enhancing students’ knowledge of certain diseases, such as dementia and Parkinson’s,26,35 improving basic science learning science concepts,41 and developing clinical skills including CanMEDS roles such as communicator, professional, and manager.14
The studies assessing interventions on third year MS are particularly striking. Medical students’ empathy appears to start declining once they begin interacting with patients in clinical learning environments3,40 yet, the studies we reviewed suggest that patient-led interactions had the opposite effect, boosting empathy and other aspects of learning.23,27,28 The learning environment may partly explain this disconnect. Time pressures and assessment worries are ubiquitous in clinical learning environments. Students’ negative coping mechanisms, along with a hidden curriculum that prioritizes biomedical knowledge over patients’ lived expertise, may affect empathy.41,42 Having protected time and space to engage with patients—and supportive role-models who value patient expertise—in a setting where clerkship students can safely talk about and process the stresses of patient care may not only attenuate this decline,43 but also facilitate learning in multiple domains.
Students also find non-traditional teaching approaches valuable, although it is unclear if the type of patient-led intervention affects empathy or learning gains.44 Indeed, according to Dale et al., students normally retain more information from real-life experiences compared to indirect ones such as watching videos,45 yet both direct and indirect patient involvement resulted in statistically significant improvement in medical student empathy.25,26,30,35 The one paper in our sample that included both direct and indirect patient involvement did not compare the results of the two modes of patient interactions.36 Nevertheless, future studies can experiment with both direct and indirect interactions to shed light on the affordances and limitations of each approach, including whether learning value depends on context, type of students, or comfort of the patients. However, curriculum designers should be mindful that patients derived greater benefit from their active engagement in teaching. Indeed, patient-authors in Gordon and colleagues’ paper reported that their involvement at higher levels of Towle’s taxonomy made them feel like partners in education, rather than ‘a live body to be poked and prodded.’37
Implications
Implementing teaching opportunities that are valuable for both students and patients requires a dedicated team of stakeholders to innovate. For instance, in June 2021, our institution established a Patient Partnership Working Group consisting of patient or caregiver representatives, medical students, and MD and PhD faculty who collaborated to generate best practices for overhauling the curriculum at the University of Ottawa to centre patient expertise. Additionally, the authors of this article co-founded MedReal—a medical student interest group aimed at patient engagement in medical learning. Through this platform, patients are invited on a monthly basis to share their stories, train medical students in the basics of empathy and communication and initiate valuable discussions of the important role of patients in medical education.
Through these initiatives, we have compiled key learning points and recommendations to guide future research and implementation of patient-led initiatives:
Although direct comparison of the results was not possible, both direct and indirect patient interactions were shown by multiple studies to be effective. If both modes are possible, we recommend combining these methods to provide various opportunities for patient engagement and decreasing possible inhibitory factors to patient involvement (e.g. travel distance, scheduling difficulties, etc.).
We recommend follow-up of the student participants as they continue their medical education to observe whether the effects of the initiative are long lasting.
We recommend performing these initiatives across cohort levels (MS1-4). This may help shed a light on key time points when such initiatives may have the most amount of benefit.
We also recommend the combined use of qualitative and quantitative methods not only to attain a baseline measure of empathy and track changes throughout the initiative, but also to understand personal perspectives, improve the design and support the implementation. Furthermore, tools that incorporate patient feedback will not only increase the level of patient engagement in the initiative but will also provide valuable feedback that can corroborate the results of other tools and increase their validity in clinical settings.
As mentioned above, incorporating patients in the design and implementation of initiatives can have a positive effect for both patients and learners. This is important due to the issue caused by the lack of an explicit definition for medical empathy. Without such a definition that can be precisely measured, a new initiative may be susceptible to focusing on aspects that are not essential from a patient’s perspective. Therefore, including patients in both the design and the evaluation is essential.
Limitations
Our review only focused on peer-reviewed, primary research written in English. Although the evidence for patient-led interventions is compelling, the lack of a reliable quantitative measure for empathy, RCTs, and follow-up or replication studies limits the generalizability of results. These limitations have been previously reported.39 Furthermore, effect size and risk of bias analysis could not be statistically measured because most papers used a different form of evidence to assess effect on empathy. Only one study evaluated long-term outcomes through a follow-up measurement three years later and, hence, it cannot be statistically confirmed that increased empathy is long-lasting.36 Additionally, the effect of student performance following these interventions on patient outcomes was not assessed. Perceptions matter, however, and the qualitative data reported in many studies is valuable not only for exploring the influence of patient-led teaching on a complex and abstract topic like empathy, but also for ascertaining constructive feedback from students to improve future sessions, and for understanding how meaningful engagement in medical education benefits patients.
Conclusion
Although more research is warranted, the studies we systematically reviewed reporting both the value and learning impact of patient-led interventions are not only compelling, but also resonate with our experiences partnering with patients at our institution.27,30,32 However, while patient storytellers, patient representatives, and patients involved in the included research studies are eager to participate in medical education, the hidden curriculum remains a seemingly impenetrable roadblock to their meaningful engagement. We remind clinician teachers that medicine promises a patient centered approach to both teaching and care; fulfilling this promise depends, not only on appreciating the value of patient-led teaching, but also on strategizing opportunities to meaningfully engage patients in teaching the skills trainees require for competent, 21st century practice.
Acknowledgements
We would like to thank Sarah Visintini for her help in developing the final search strategy for this study. We would also like to thank Dr. Tim Ramsay and the Ottawa Methods Centre for their assistance with the data analysis of this project.
Appendices
Appendix A
Appendix B. MEDLINE Literature Search Strategy
| Search Terms | Number of Results | |
|---|---|---|
| 1 | Empathy/ | 18676 |
| 2 | (empathy or empathetic or empathi?e).mp. | 26309 |
| 3 | 1 or 2 | 26309 |
| 4 | Schools, Medical/ | 25445 |
| 5 | Students, Medical/ | 33421 |
| 6 | Education, Medical, Undergraduate/ | 23783 |
| 7 | (medical school? or medical student? or undergraduate medical education).mp. | 65055 |
| 8 | 4 or 5 or 6 or 7 | 97873 |
| 9 | exp Teaching/ | 84820 |
| 10 | Education/ or exp Curriculum/ | 103715 |
| 11 | (education* or curriculum? or training? or teaching? or learning? or intervention?).mp. | 2354275 |
| 12 | 9 or 10 or 11 | 2356247 |
| 13 | 3 and 8 and 12 | 1209 |
Conflicts of Interest
The authors have no conflicts of interest to disclose.
Funding
None.
Authorship
Boshra and Lee co-first authors to this work. I Kim, E Malek-Adamian, and M Yau are co-second authors.
References
- 1.Mercer SW, Reynolds WJ. Empathy and quality of care. Br J Gen Pract. 2002;52(Suppl):S9- [PMC free article] [PubMed] [Google Scholar]
- 2.Riess H. The Science of Empathy. J Patient Exp. 2017;4(2):74- 10.1177/2374373517699267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shapiro J. Walking a mile in their patients’ shoes: empathy and othering in medical students’ education. Philos Ethics Humanit Med. 2008. Mar 12;3: https://pubmed.ncbi.nlm.nih.gov/18336719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182– 10.1097/ACM.0b013e3181b17e55 [DOI] [PubMed] [Google Scholar]
- 5.Neumann M, Edelhäuser F, Tauschel D, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86(8):996–10 10.1097/ACM.0b013e318221e615 [DOI] [PubMed] [Google Scholar]
- 6.Ferreira-Valente A, Monteiro JS, Barbosa RM, Salgueira A, Costa P, Costa MJ. Clarifying changes in student empathy throughout medical school: a scoping review. Advances. 2017;22(5):1293-3 10.1007/s10459-016-9704-7 [DOI] [PubMed] [Google Scholar]
- 7.Kerasidou A, Horn R. Making space for empathy: supporting doctors in the emotional labour of clinical care. BMC Med Ethics. 2016;17(1) 10.1186/s12910-016-0091-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kerasidou A. Empathy and efficiency in healthcare at times of austerity. Heal Care Anal. 2019;27(3):171– 10.1007/s10728-019-00373-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riess H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27(10):1280-12 10.1007/s11606-012-2063-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moudatsou M, Stavropoulou A, Philalithis A, Koukouli S. The Role of Empathy in Health and Social Care Professionals. Healthcare (Basel). 2020;8(1):Published 2020 Jan 10.3390/healthcare8010026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brunero S, Lamont S, Coates M. A review of empathy education in nursing. Nurs Inq. 2010. Mar 1;17(1):65– 10.1111/j.1440-1800.2009.00482.x [DOI] [PubMed] [Google Scholar]
- 12.Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009. Sep 23;302(12):1284– 10.1001/jama.2009.1384 [DOI] [PubMed] [Google Scholar]
- 13.Brennan TA, Leape LL, Laird NM, et al. incidence of adverse events and negligence in hospitalized patients. N Engl J Med. 1991. Feb 7;324(6):370– 10.1056/NEJM199102073240604 [DOI] [PubMed] [Google Scholar]
- 14.Spencer J, Blackmore D, Heard S, et al. Patient-oriented learning: a review of the role of the patient in the education of medical students. Med Educ. 2000;34(10):851– 10.1046/j.1365-2923.2000.00779.x [DOI] [PubMed] [Google Scholar]
- 15.Dijk SW, Duijzer EJ, Wienold M. Role of active patient involvement in undergraduate medical education: a systematic review. BMJ Open. 2020;10(7):e372 10.1136/bmjopen-2020-037217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Towle A, Bainbridge L, Godolphin W, Katz A, Kline C, Lown B, et al. Active patient involvement in the education of health professionals. Med Educ. 2010;44(1):64– 10.1111/j.1365-2923.2009.03530.x [DOI] [PubMed] [Google Scholar]
- 17.Dornan T, Littlewood S, Margolis SA, Scherpbier A, Spencer J, Ypinazar V. How can experience in clinical and community settings contribute to early medical education? A BEME systematic review. Med Teach. 2006;28(1):3– 10.1080/01421590500410971 [DOI] [PubMed] [Google Scholar]
- 18.Chandrasekar H, Harte S, Sherman J, Park KT, Lee HC. Gaining perspectives on patient and family disease experiences by storytelling. Acad Pediatr. 2018;18(4):475– 10.1016/j.acap.2018.01.014 [DOI] [PubMed] [Google Scholar]
- 19.Lucchetti ALG, Duarte BSVF, de Assis T V, Laurindo BO, Lucchetti G. Is it possible to teach Geriatric Medicine in a stimulating way? Measuring the effect of active learning activities in Brazilian medical students. Australas J Ageing. 2019;38(2):e58– 10.1111/ajag.12626 [DOI] [PubMed] [Google Scholar]
- 20.Sweeney K, Baker P. Promoting empathy using video-based teaching. Clin Teach. 2018;15(4):336– 10.1111/tct.12693 [DOI] [PubMed] [Google Scholar]
- 21.Cumberland D, Sawning S, Church-Nally M, et al. Experiential learning: transforming theory into practice through the Parkinson’s Disease buddy program. Teach Learn Med. 2019;31(4): 453-465, 10.1080/10401334.2019.1580583 [DOI] [PubMed] [Google Scholar]
- 22.Bramstedt KA, Prang M, Dave S, Shin PNH, Savy A, Fatica RA. Telemedicine as an ethics teaching tool for medical students within the nephrology curriculum. Prog Transplant. 2014;24(3):294– 10.7182/pit2014289 [DOI] [PubMed] [Google Scholar]
- 23.Shuja F, Ansari S, Babar T, et al. Empathy building in undergraduate medical students through an interaction with persons with disabilities in their natural home environment a descriptive qualitative study. Rawal Med J. 2014;39(2):208– [Google Scholar]
- 24.Player E, Gure-Klinke H, North S, et al. Humanising medicine: teaching on tri-morbidity using expert patient narratives in medical education. Educ Prim Care. 2019;30(6):368– 10.1080/14739879.2019.1670097 [DOI] [PubMed] [Google Scholar]
- 25.Singh SP, Modi CM, Patel CP, Pathak AG. Low-fidelity simulation to enhance understanding of infection control among undergraduate medical students. Natl Med J India. 2017;30(4):2 10.4103/0970-258X.218677 [DOI] [PubMed] [Google Scholar]
- 26.Chen A, Hanna JJ, Manohar A, Tobia A. Teaching empathy: The implementation of a video game into a psychiatry clerkship curriculum. Acad Psychiatry. 2018;42(3):362– 10.1007/s40596-017-0862-6 [DOI] [PubMed] [Google Scholar]
- 27.Chretien KC, Swenson R, Yoon B, et al. Tell me your story: a pilot narrative medicine curriculum during the medicine clerkship. J Gen Intern Med. 2015;30(7):1025– 10.1007/s11606-015-3211-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hendriksz T. Using patient perspective sessions to increase empathy and recall in preclinical medical students. J Am Osteopat Assoc. 2016;116(10):662– 10.7556/jaoa.2016.130 [DOI] [PubMed] [Google Scholar]
- 29.Hennrikus EF, Skolka MP, Hennrikus N. Applying metacognition through patient encounters and illness scripts to create a conceptual framework for basic science integration, storage, and retrieval. J Med Educ Curric Dev. 2018;5:23821205187777 10.1177/2382120518777770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morhardt, D. (2006). Educating medical students on Alzheimer's disease and related disorders: an overview of the Northwestern University Buddy Program. Dementia. 448-4 10.1177/147130120600500311 [DOI] [Google Scholar]
- 31.Shapiro J, Youm J, Kheriaty A, Pham T, Chen Y, Clayma R. The human kindness curriculum: an innovative preclinical initiative to highlight kindness and empathy in medicine. Educ Health (Abingdon). 2019;32(2):53– 10.4103/efh.EfH_133_18 [DOI] [PubMed] [Google Scholar]
- 32.Gordon M, Gupta S, Thornton D, Reid M, Mallen E, Melling A. Patient/service user involvement in medical education: a best evidence medical education (BEME) systematic review: BEME Guide No. Med Teach. 2020;42(1):4– 10.1080/0142159X.2019.1652731 [DOI] [PubMed] [Google Scholar]
- 33.Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. Teaching empathy to medical students: an updated, systematic review. Acad Med. 2013;88(8):1171– 10.1097/ACM.0b013e318299f3e3 [DOI] [PubMed] [Google Scholar]
- 34.Morhardt, D. (2018), P3-642: The Buddy Program Increases Medical Student Knowledge, Empathy And Attitudes Toward Persons Living With Dementia. Alzheimer's & Dementia, 14: P1379 P13 10.1016/j.jalz.2018.06.2009 [DOI] [Google Scholar]
- 35.Karazivan P, Dumez V, Flora L, et al. The patient-as-partner approach in health care: a conceptual framework for a necessary transition. Acad Med. 2015. Apr 1;90(4):437- 10.1097/ACM.0000000000000603 [DOI] [PubMed] [Google Scholar]
- 36.Chen DCR, Kirshenbaum DS, Yan J, Kirshenbaum E, Aseltine RH. Characterizing changes in student empathy throughout medical school. Med Teach. 2012;34(4):305– 10.3109/0142159X.2012.644600 [DOI] [PubMed] [Google Scholar]
- 37.Werner ER, Korsch BM. The vulnerability of the medical student: Posthumous presentation of LL Stephens’ ideas. Pediatrics. 1976;57(3):321– 10.1542/peds.57.3.321 [DOI] [PubMed] [Google Scholar]
- 38.West CP, Shanafelt TD. The influence of personal and environmental factors on professionalism in medical education. BMC Med Educ. 2007;7(1):1– 10.1186/1472-6920-7-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosenthal S, Howard B, Schlussel YRet al. Humanism at heart: preserving empathy in third-year medical students. Acad Med. 2011;86(3):350– 10.1097/ACM.0b013e318209897f [DOI] [PubMed] [Google Scholar]
- 40.Dale, E. (1969). Audio-Visual Methods in Teaching (3rd ed., p. 108). Holt, Rinehart & Winston, New York: Dryden Press. [Google Scholar]
- 41.Gruppen LD, Branch VK, Laing TJ. The use of trained patient educators with rheumatoid arthritis to teach medical students. Arthritis Rheum Off J Am Coll Rheumatol. 1996;9(4):302– [DOI] [PubMed] [Google Scholar]
- 42.Oswald A, Czupryn J, Wiseman J, Snell L. Patient-centred education: what do students think? Med Educ. 2014;48(2):170– 10.1111/medu.12287 [DOI] [PubMed] [Google Scholar]
- 43.Bombeke K, Van Roosbroeck S, De Winter B, et al. Medical students trained in communication skills show a decline in patient-centred attitudes: an observational study comparing two cohorts during clinical clerkships. Patient Educ Couns. 2011;84(3):310– 10.1016/j.pec.2011.03.007 [DOI] [PubMed] [Google Scholar]
- 44.Mercer SW, Maxwell M, Heaney D, Watt G. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam Pract. 2004;21(6):699–7 10.1093/fampra/cmh621 [DOI] [PubMed] [Google Scholar]