Abstract
Periodontitis is an inflammatory disease that is characterized by progressive destruction of the periodontium and causes tooth loss in adults. Periodontitis is known to be associated with dysbiosis of the oral microflora, which is often linked to various diseases. However, the complexity of plaque microbial communities of periodontitis, antibiotic resistance, and enhanced virulence make this disease difficult to treat. In this study, using metagenomic shotgun sequencing, we investigated the etiology, antibiotic resistance genes (ARGs), and virulence genes (VirGs) of periodontitis. We revealed a significant shift in the composition of oral microbiota as well as several functional pathways that were represented significantly more abundantly in periodontitis patients than in controls. In addition, we observed several positively selected ARGs and VirGs with the Ka/Ks ratio > 1 by analyzing our data and a previous periodontitis dataset, indicating that ARGs and VirGs in oral microbiota may be subjected to positive selection. Moreover, 5 of 12 positively selected ARGs and VirGs in periodontitis patients were found in the genomes of respiratory tract pathogens. Of note, 91.8% of the background VirGs with at least one non-synonymous single-nucleotide polymorphism for natural selection were also from respiratory tract pathogens. These observations suggest a potential association between periodontitis and respiratory infection at the gene level. Our study enriches the knowledge of pathogens and functional pathways as well as the positive selection of antibiotic resistance and pathogen virulence in periodontitis patients, and provides evidence at the gene level for an association between periodontitis and respiratory infection.
Keywords: Periodontitis, Metagenomic sequencing, Antibiotic resistance gene, Virulence gene, Respiratory infection
Introduction
Periodontitis is an inflammatory disease of the periodontium which is characterized by progressive destruction of the periodontium, and causes tooth loss in adults [1]. It is one of the most well-characterized human diseases associated with dysbiosis of the oral microflora [2], [3]. The inflammatory infiltration induced by the microbes often destroys the supportive tissue, leading to alveolar bone loss before developing into an irreversible situation [4], [5]. A number of systemic diseases have been reported to be associated with periodontitis, such as atherosclerotic vascular disease, cardiovascular disease, rheumatoid arthritis, and diabetes [6], [7]. Moreover, periodontitis pathogens of the oral cavity as well as respiratory pathogens have been found to access the respiratory tract and induce respiratory infection [8], [9], [10].
Among the factors contributing to the periodontitis, virulence factors of the oral microbiota have been a critical and important issue, influencing the onset of the disease. A set of key virulence factors produced by Porphyromonas gingivalis, a well-established oral keystone pathogen, have been discovered and determined for the role of pathogenesis, such as Lys- and Arg-proteases, lipoprotein, and atypical lipopolysaccharide [11]. Bacterial sialidases have been considered as virulence factors in oral pathogens like Tannerella forsythia [12], [13]. In addition, functional studies showed that the activation of the metalloproteases, peptidases, and proteins involved in iron metabolism in oral pathogens might be linked to the potential association with periodontal disease [2], [14].
Antibiotic resistance, described as “bacteria changing in ways that reduce or eliminate the effectiveness of antibiotics”, is another impediment to treatment [15]. When drug-sensitive pathogens are eliminated, drug-resistant pathogens are left to be selected [16]. Bacteria often acquire resistance by random mutations in functional genes or by horizontal gene transfer (HGT). The exchange of genes via HGT is common among bacteria and can facilitate the spread of drug resistance [15]. Considering that the evolutionary dynamics of drug resistance is usually derived from the increasing overuse of antibiotics [17], the empirical and broad use of antibiotics resulting from the lack of clarification of periodontal disease pathogens may increase the risk of antibiotic resistance problems in periodontitis [18]. Subgingival periodontal pathogens from chronic periodontitis patients were found to be resistant to at least one of the commonly used antibiotics, and several strains from the “red complex” have already developed resistance to various antibiotics [19], [20]. Therefore, it is necessary to gain more insights into drug-resistance genes and associated pathways involved in periodontitis.
In this study, we explored the differences in composition and functional pathways of oral microbiota between patients with periodontitis and individuals with a healthy periodontium using metagenomic shotgun sequencing. We also investigated the potential bacteria, virulence genes (VirGs), and antibiotic resistance genes (ARGs) associated with periodontitis. Our results contribute to enriching our understanding of the bacterial ecology of periodontitis and reveal a potential association between periodontitis and respiratory infections.
Results
Metagenomic sequencing and data quality control
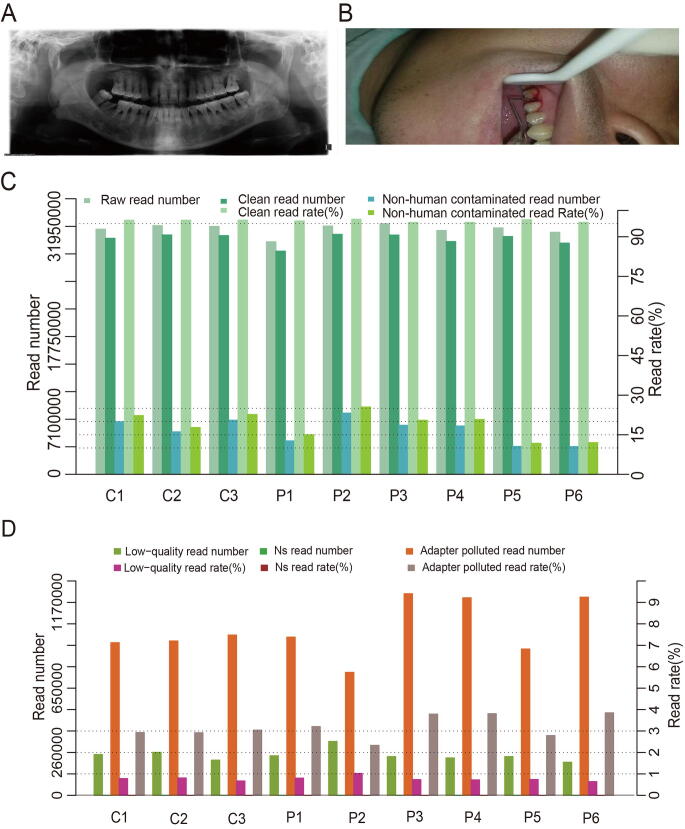
A total of 30 patients with periodontitis and 15 healthy individuals were recruited with detailed clinical information including age, sex, diagnosis, tooth number, dental history, and treatment history (Table S1). In addition, periodontitis participants showed obvious bone loss and bleeding through clinical examination (Figure S1A and B). Due to the insufficient amount of DNA extracted from each dental plaque sample, every five samples were pooled together, and six periodontitis specimens (P1, P2, P3, P4, P5, and P6) and three controls (C1, C2, and C3) were ultimately obtained. Sequencing of the six periodontitis specimens and three controls generated 2.38–2.68 gigabases (Gb) of raw sequencing data consisting of 30–32 million paired-end (PE) reads per sample (Table S2). After data processing, 2.30–2.50 Gb of clean high-quality data were retained, consisting of 29–31 million PE reads for each sample. The clean read rate for each sample ranged from 95% to 97% (Figure S1C), and the clean Q30 base rate ranged from 92% to 93%. The low-quality read rate, NS read (read with “N” or “.” bases that couldn’t be assign a specific base by the basecaller tool) rate, and adapter read rate were as low as expected (Figure S1D; Table S2). Alignment against hg19 revealed that the human sequence read rate ranged from 74% to 88% for all specimens (Figure S1C). After removal of human sequence contamination, we retained approximately 3.58–7.89 million reads for all samples for subsequent analyses (Table S2).
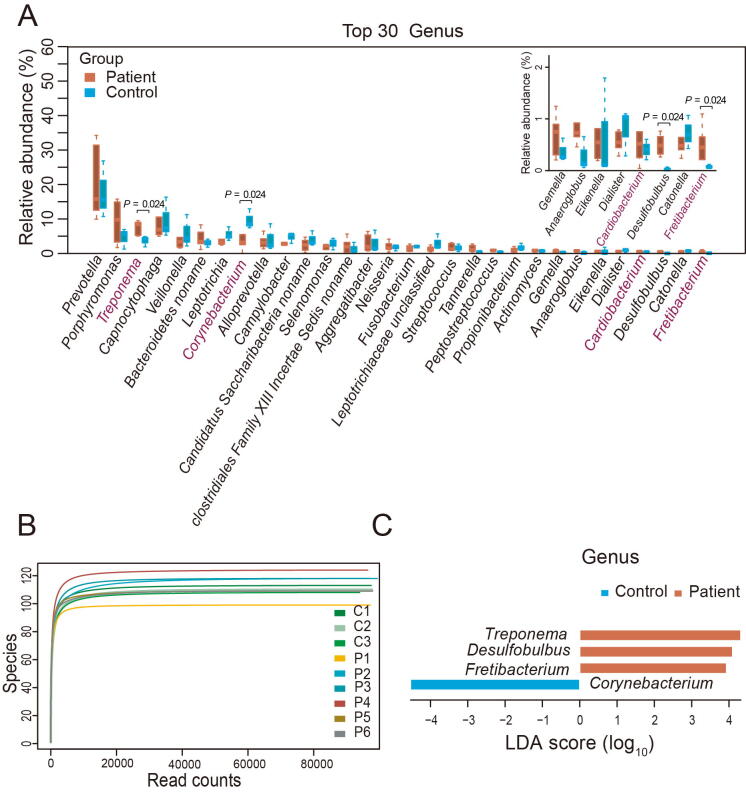
Significant differences in the composition and diversity of oral microbiota between periodontal patients and controls
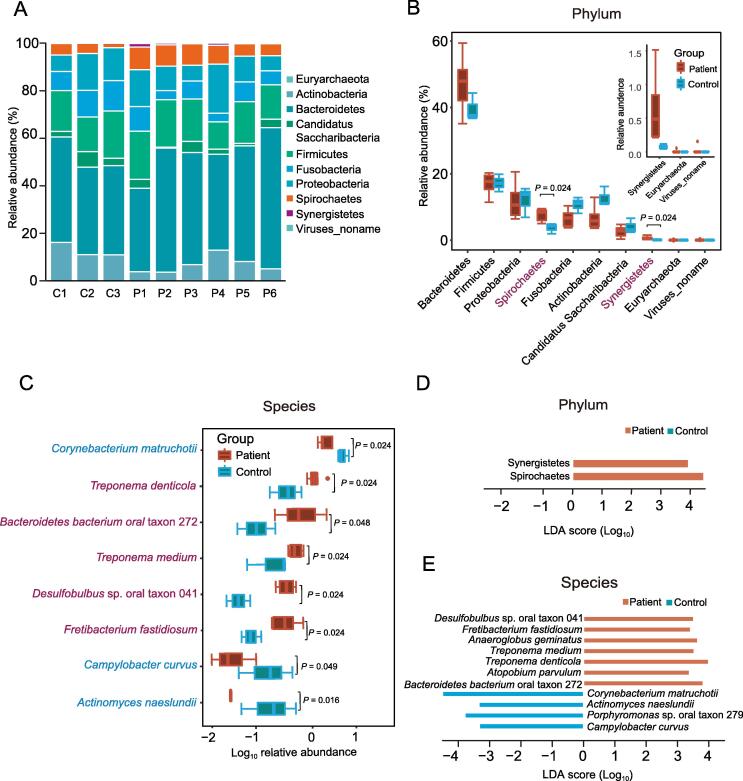
To explore the taxonomic composition, we applied MetaPhlAn2 [21] to analyze the abundance information of each sample in each taxonomy hierarchy. At the kingdom level, the analysis revealed that almost all the reads were aligned to Bacteria, with only 0.16% reads aligned to Viruses and 0.06% reads aligned to Archaea (Table S3). At the phylum level, there were ten phyla aligned, among which Bacteroidetes was the most dominant bacterial phylum (Figure 1A). Both Synergistetes (Wilcoxon rank sum test, P = 0.024) and Spirochaetes (Wilcoxon rank sum test, P = 0.024) were significantly enriched in periodontal patients over controls (Figure 1B; Table S4). At the genus level, 69 genera were aligned, with 89%–97% of reads in all samples aligned to the top 30 genera. Among these genera, Prevotella was the most dominant genus in both the periodontal patients and controls. In addition, Treponema, Desulfobulbus, and Fretibacterium were significantly enriched in periodontal patients, and Corynebacterium was significantly enriched in controls (Wilcoxon rank sum test, P < 0.05; Figure S2A; Table S5). At the species level, rarefaction curves indicated that sequence data could be sufficient to identify the majority of species (Figure S2B) and the read alignment identified a total of 168 species, among which there were five species enriched in periodontal patients, and three species enriched in controls (Wilcoxon rank sum test, P < 0.05; Figure 1C; Table S6).
Figure 1.
The shift in oral microbiota composition at the phylum and species levels
A. Composition of oral microbiota at the phylum level in each sample. P1–P6, six periodontitis specimens; C1–C3, three control specimens. For both periodontitis and control samples, every five samples were pooled together as one specimen. B. Comparison of relative aboundance of each phylum between periodontitis and control samples. The significantly abundant phyla in periodontitis samples are marked with red. The three small boxplots in the boxplot-in-boxplot indicate a zooming state for their corresponding boxplots in a vertical direction in the main boxplot. C. Eight species with significant differences in relative aboundance between periodontitis and control samples. The significantly abundant species in periodontitis and control samples are marked in red and light blue, respectivley. D. LEfSe analysis at the phylum level. E. LEfSe analysis at the species level. LDA, linear discriminant analysis; LEfSe, linear discriminant analysis effect size.
Further linear discriminant analysis (LDA) effect size (LEfSe) analysis at the phylum level revealed LDA scores of Synergistetes and Spirochaetes greater than 3 in periodontal patients (Figure 1D). At the genus level, LEfSe analysis showed that Treponema, Desulfobulbus, and Fretibacterium in periodontal patients and Corynebacterium in controls had an LDA score passing the cutoff threshold of 3 (Figure S2C). At the species level, Treponema denticola, Treponema medium, Fretibacterium fastidiosum, Desulfobulbus sp. oral taxon 041, Bacteroidetes bacterium oral taxon 272, Anaeroglobus geminatus, and Atopobium parvulum in periodontitis patients, as well as Corynebacterium matruchotii, Actinomyces naeslundii, Porphyromonas sp. oral taxon 279, and Campylobacter curvus in controls, passed the LDA cutoff threshold of 3 (Figure 1E).
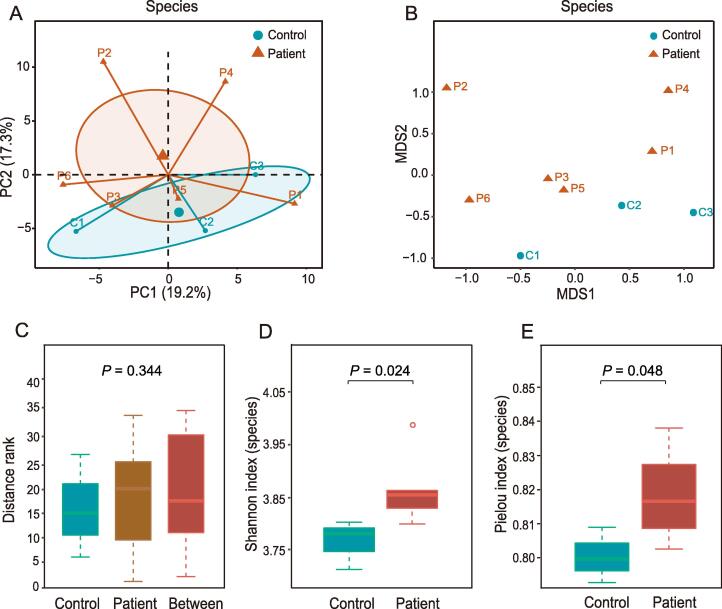
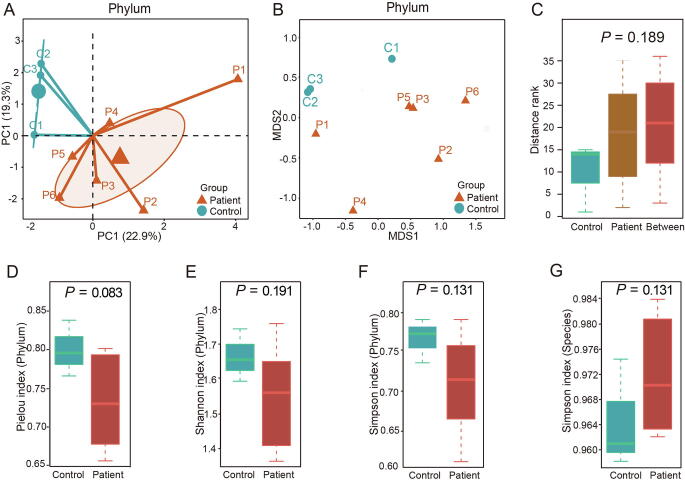
For beta diversity, principal component analysis (PCA) and non-metric multidimensional scaling (NMDS) analysis were performed at the phylum and species levels (Figure S3A and B, Figure 2A and B). Both PCA and NMDS showed distinct distribution of distance between periodontitis patients and controls, although there was no significant difference. Similar observation was shown up in the analysis of similarities (ANOSIM) of the NMDS results at the phylum and species levels (Figure S3C, Figure 2C). For alpha diversity at the phylum level, Pielou index, Shannon index, and Simpson index tended to be higher in controls than in periodontitis patients but without statistical significance (Figure S3D–F). At the species level, periodontitis patients showed higher Shannon index (P = 0.024) and Pielou index (P = 0.048) than controls (Figure 2D and E). The Simpson index at the species level also tended to be higher in periodontitis patients, although not significantly (Figure S3G).
Figure 2.
Alpha diversity and beta diversity at the species level
A. PCA of all samples at the species level. B. NMDS analysis of all samples at the species level. C. ANOSIM of NMDS results at the species level. D. and E. Shannon index (D) and Pielou index (E) of the alpha diversity at the species level. The two indexes were significantly higher in periodontitis patients than in controls. PCA, principal component analysis; NMDS, non-metric multidimensional scaling; ANOSIM, analysis of similarities.
Functional annotations associated with drug resistance and virulence were significantly enriched in periodontitis
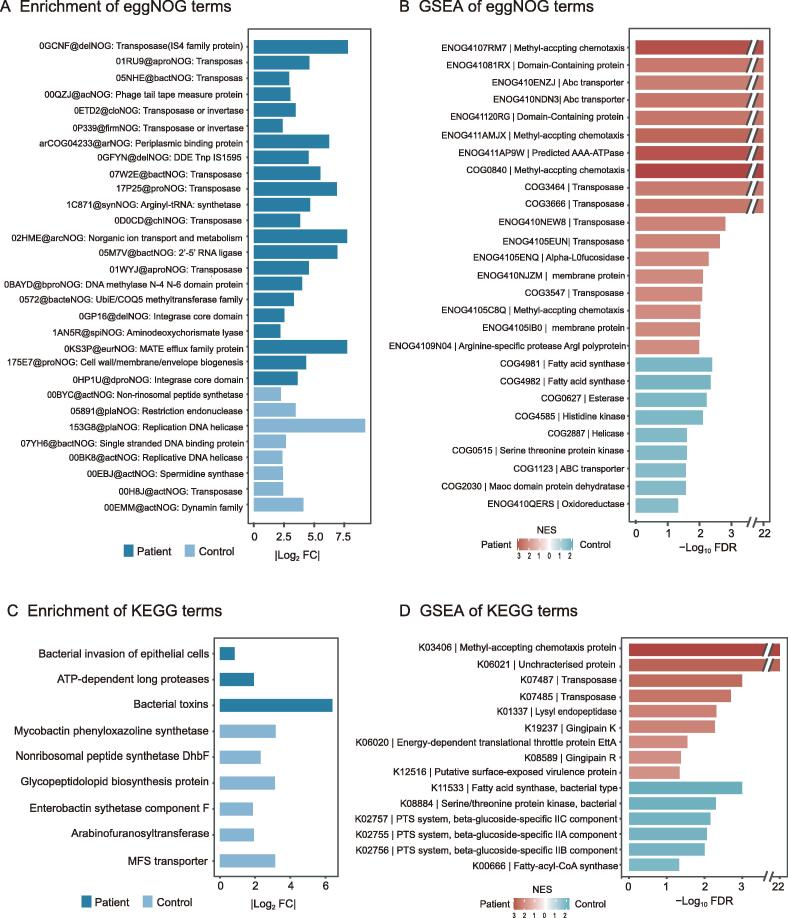
To determine the differential functions of microbial taxa between periodontitis patients and controls, we performed several functional predictions including evolutionary genealogy of genes: Non-supervised Orthologous Groups (eggNOG) annotations, Gene Ontology (GO) analysis, and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis, as well as the corresponding gene set enrichment analysis (GSEA). According to the annotations with a false discovery rate (FDR) < 0.05 after applying DESeq2 with reads per kb (RPK) values, we found 22 eggNOG terms significantly enriched in periodontitis patients, among which there were ten terms associated with transposase that might function as resistance against many different antibiotics. Several eggNOG terms functioning in strengthening physical defenses were also up-regulated in periodontitis, including the multidrug and toxin compound extrusion (MATE) efflux family protein, the ATP-binding cassette (ABC) superfamily transporter extruding multidrug and toxic compounds, and cell wall/membrane/envelope biogenesis [22] (Figure 3A; Table S7). GSEA of eggNOG terms revealed several significantly enriched terms [FDR < 0.05, normalized enrichment score (NES) > 1] in periodontitis patients. Several transposase terms and ABC-transporter terms were still significantly enriched in periodontitis patients, indicating their important roles in periodontitis. Several terms involved in the synthesis of fatty acids were found to be significantly enriched in controls, such as fatty acid synthase, esterase, MaoC domain protein dehydratase, and oxidoreductase (Figure 3B; Table S8).
Figure 3.
Significant differences between periodontitis and control samples in various functional annotations
A. Significantly enriched eggNOG terms in periodontitis samples or control samples with FDR < 0.05 and |Log2 FC| > 0.7. B. GSEA of eggNOG terms with NES > 1 and FDR < 0.05 in periodontitis patients and controls. C. Significantly enriched KEGG terms in periodontitis samples or control samples (FDR < 0.1, |Log2 FC| > 0.7). D. GSEA of KEGG terms with NES > 1 and FDR < 0.05 in periodontitis patients and controls. eggNOG, evolutionary genealogy of genes: Non-supervised Orthologous Groups; FDR, false discovery rate; FC, fold change; GSEA, gene set enrichment analysis; NES, normalized enrichment score; KEGG, Kyoto Encyclopedia of Genes and Genomes.
The GO enrichment analysis showed that there were 39 GO terms down-regulated in periodontitis patients (Table S7). GSEA of GO terms revealed no significantly enriched terms in periodontitis patients but found 75 GO terms significantly enriched in controls, including synthesis of fatty acids, cell cycle processes, membrane assembly as well as several other GO terms which may all contribute to the maintenance of health status (Table S8). There were three KEGG pathways significantly up-regulated (FDR < 0.1, Log2 FC > 0.7) in periodontitis patients, including bacterial invasion of epithelial cells, ATP-dependent long proteases, and bacterial toxins (Figure 3C; Table S7). GSEA of KEGG terms revealed several significantly enriched proteins in periodontitis patients identical to those identified by GSEA of eggNOG terms, such as methyl-accepting chemotaxis protein (MCP), transposase, and unique virulence proteins. In controls, GSEA of KEGG terms revealed only one significantly enriched KEGG term (fatty acid synthase, bacteria type) consistent with the that identified by GSEA for eggNOG terms (Figure 3D; Table S8).
ARG and virulence annotation revealed convergent enrichment in several genes in periodontitis from a significantly different gene context
To investigate the abundances of each gene family in the oral microbiota from periodontitis patients and controls, we used the HUMAnN2 to annotate all sequencing reads and found 196 gene families significantly abundant in periodontitis patients. Several genes encoding various functional types of proteins, including resistance proteins, transposons, transposases or transporters, were annotated (Table S7). For example, A3CPG0 was annotated as an ABC-type bacitracin resistance protein with the taxon assigned to Streptococcus sanguinis. F2KUK8 was the conjugative transposon protein (TraA) encoded in Prevotella denticola. F5RK90 was a transposase from Centipeda periodontii. C8PRE7 and C9LSP5 were two flagellar FlbD family proteins encoded in Treponema vincentii ATCC 35580 and Selenomonas sputigena ATCC 35185, respectively, both of which function in the invasion of pathogens. Most of the other genes encode proteins associated with translation, such as 30S and 50S ribosomal proteins and transcriptional regulators (Table S7).
To further explore the potential ARGs from the oral microbiota, we used DeepARG tool to annotate the reads [23], and found that there were 30 ARG biomarkers with LDA score > 2 in periodontitis patients using LEfSe analysis (Table S9). For VirGs, after sequence alignment and annotation, LEfSe analysis revealed 10 VirG biomarkers with LDA score > 2 in periodontitis (Table S9).
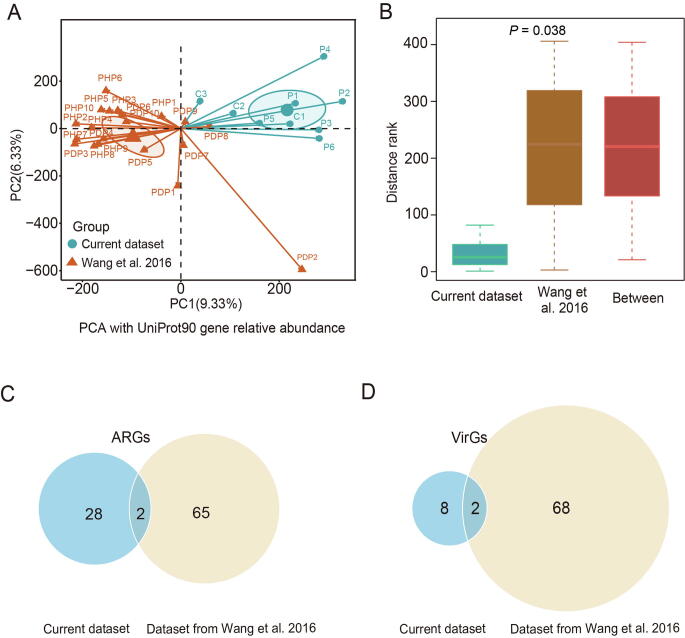
To eliminate sample bias, we analyzed the metagenomic data for dental plaques of periodontal health (PHP) and disease (PDP) from a previous study by Wang et al. [24] as a comparison. After removal of human DNA contamination, we found that there was no significant difference of non-human sequence rate either in periodontitis patient samples (Wilcoxon rank sum test, P = 0.559) or controls (Wilcoxon rank sum test, P = 0.161) between current dataset and the dataset from Wang et al. [24] (Table S10). The PCA and ANOSIM using the relative abundance of genes aligned by HUMAnN2 showed a significant difference between the two studies. This difference might be due to several factors including the difference in the regions where participants resided or technical bias for library construction and sequencing between two datasets, even though the same analytical methods were used (P = 0.038, Figure S4A and B). After ARG annotation, LEfSe analysis revealed 67 ARG biomarkers with LDA score > 2 in periodontitis samples from the previous study (Table S11). For VirGs, LEfSe analysis revealed 70 VirG biomarkers with LDA score > 2 in periodontitis samples from the previous study (Table S11). In addition, comparative analysis indicated that there were two identical ARGs as well as two identical VirGs between our dataset and the dataset from the previous study (Figure S4C and D).
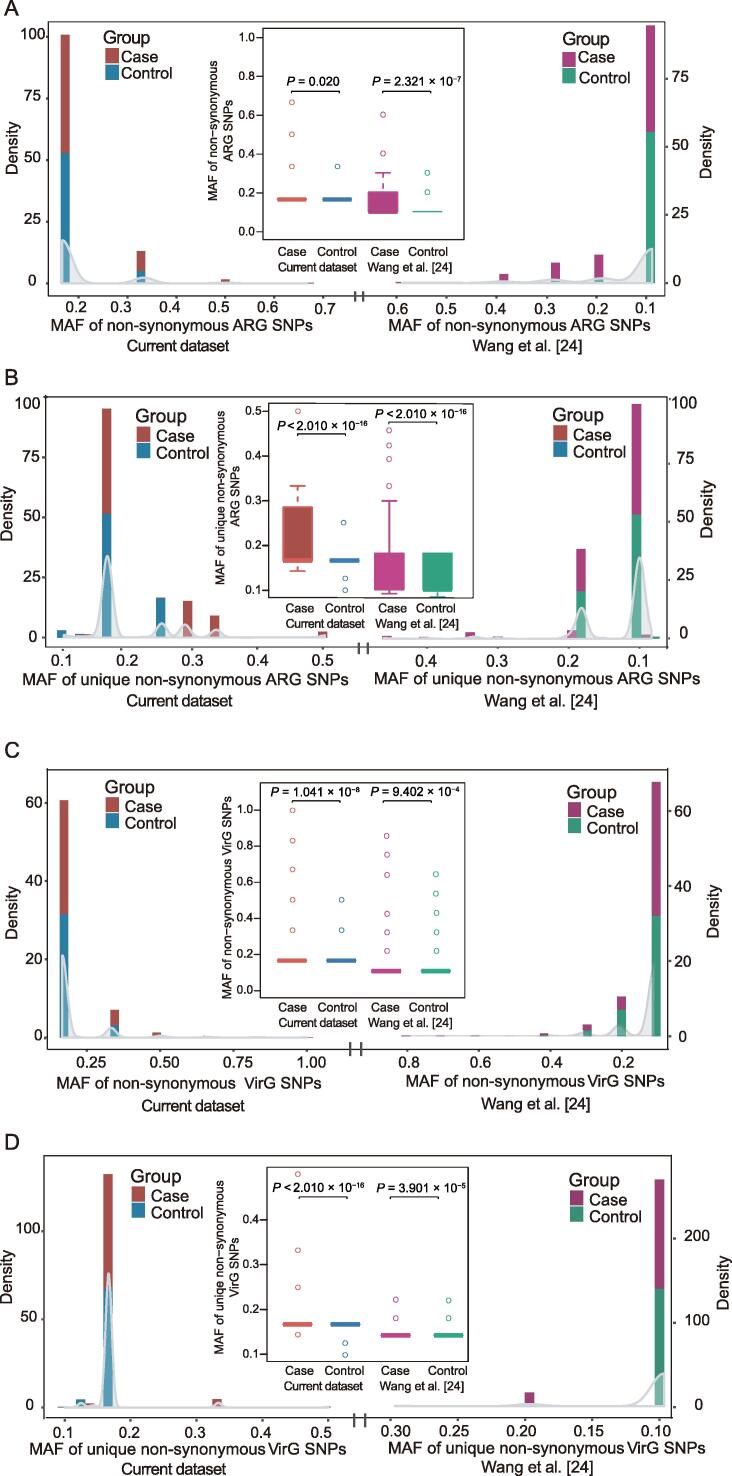
Minor allele frequency of non-synonymous single-nucleotide polymorphisms in ARGs and VirGs were significantly higher in periodontitis
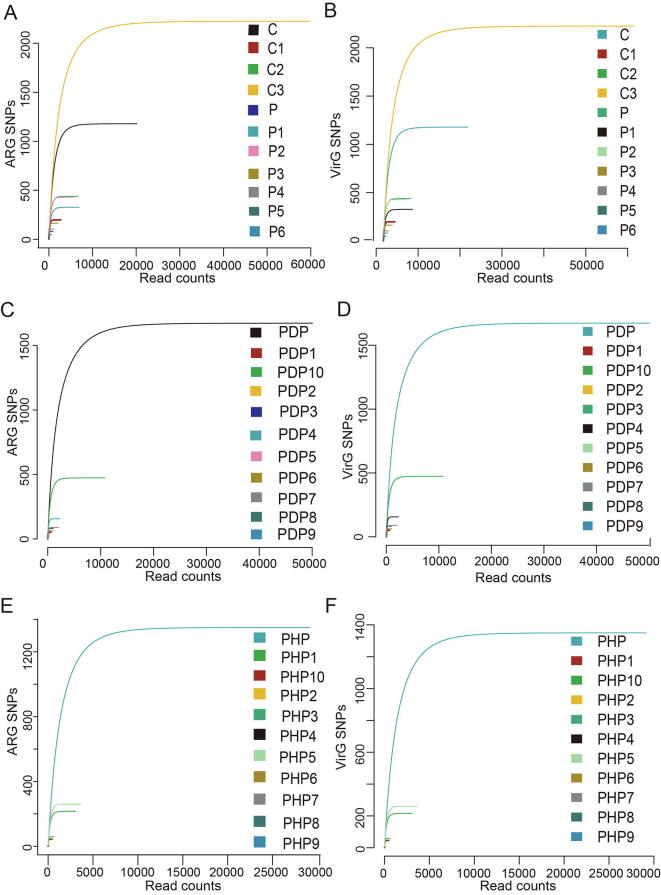
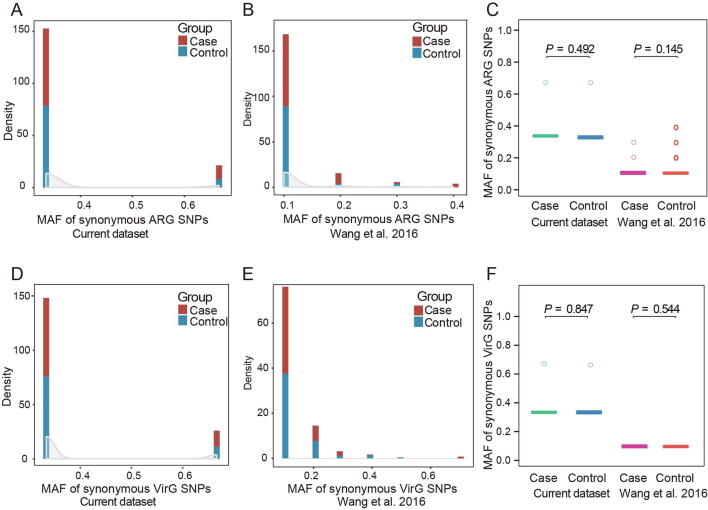
After single-nucleotide polymorphism (SNP) calling in ARGs from each sample by BCFtools and VarScan, we calculated the minor allele frequency (MAF) of non-synonymous SNPs and unique non-synonymous SNPs, as well as synonymous SNPs, in ARGs and VirGs between periodontitis patients and controls from current dataset and the dataset from Wang and colleagues [24]. The rarefaction curve of SNPs in ARGs and VirGs showed that SNP number was sufficient for analysis of all samples (Figure S5). We found that the MAF of non-synonymous SNPs in ARGs was significantly higher in periodontitis patients than in controls in current dataset. The same difference was also observed in the dataset from Wang et al. [24] (Figure 4A). For unique non-synonymous ARG SNPs, similar results were also obtained in both datasets (Figure 4B). However, there was no significant difference for the MAF of synonymous SNPs in ARGs between periodontitis patients and controls in both datasets (Figure S6A–C). These findings indicated that ARGs in periodontitis patients may suffer more selection pressure than those in controls. Similarly, we also calculated the MAF of non-synonymous and unique non-synonymous SNPs in VirGs in periodontitis patients and controls from both datasets. There was a significant difference in the MAF of non-synonymous (Figure 4C) and unique non-synonymous VirG SNPs (Figure 4D) between periodontitis patients and controls, while there was no significant difference in the MAF of synonymous VirG SNPs between periodontitis patients and controls in either dataset (Figure S6D–F). The MAF of SNPs in VirGs indicated that VirGs may also be subject to more positive selection in periodontitis patients than those in controls.
Figure 4.
Comparison of non-synonymous SNPs in ARGs and VirGs between periodontitis and control samples from both datasets
A. Distribution of the MAF of non-synonymous SNPs in ARGs from both the current study and a study by Wang and colleagues [24]. Comparison of the MAF of non-synonymous SNPs in ARGs between periodontitis and control samples in both datasets. B. Distribution of the MAF of unique non-synonymous SNPs in ARGs from both the current study and a study by Wang and colleagues [24]. Comparison of the MAF of unique non-synonymous SNPs in ARGs between periodontitis and control samples in both datasets. C. Distribution of the MAF of non-synonymous SNPs in VirGs from both the current study and a study by Wang and colleagues [24]. Comparison of the MAF of non-synonymous SNPs in VirGs between periodontitis and control samples in both datasets. D. Distribution of the MAF of unique non-synonymous SNPs in VirGs from both the current study and a study by Wang and colleagues [24]. Comparison of the MAF of unique non-synonymous SNPs in VirGs between periodontitis and control samples in both datasets. All P values were calculated using Wilcoxon rank sum test. SNP, single-nucleotide polymorphism; ARG, antibiotic resistance gene; VirG, virulence gene; MAF, minor allele frequency.
Several ARGs and all VirGs with Ka/Ks > 1 in periodontitis were frequent from respiratory infection pathogens
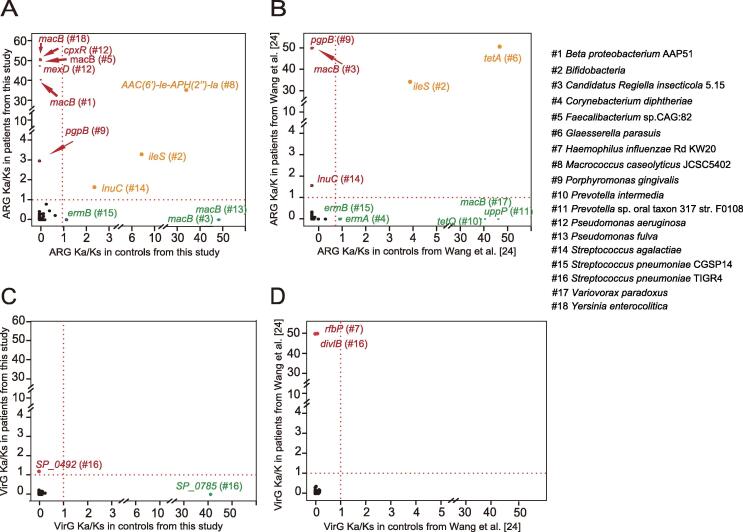
Given that Ka and Ks represent the number of substitutions per non-synonymous and synonymous site, respectively, the Ka/Ks ratio is often used for the estimation of evolutionary rates [25], [26]. The Ka/Ks > 1 and Ka/Ks < 1 indicate positive selection and negative selection, respectively [25], [26]. To identify positively selected ARGs, Ka/Ks was calculated for each ARG. In our dataset, there were six ARGs with Ka/Ks > 1 in periodontitis patients and Ka/Ks < 1 in controls, including macB (Yersinia enterocolitica, Faecalibacterium sp. CAG:82, and beta proteobacterium AAP51), mexD and cpxR (Pseudomonas aeruginosa), and pgpB (Porphyromonas gingivalis) (Figure 5A; Table S12). These genes were considered positively selected only in periodontitis patients and negatively selected only in controls in the current dataset. In the dataset from Wang and colleagues [24], pgpB from Porphyromonas gingivalis, macB from Candidatus Regiella insecticola, and lnuC from Streptococcus agalactiae all had Ka/Ks > 1 in periodontitis patients and Ka/Ks < 1 in controls. However, macB from Candidatus Regiella insecticola was found to be positively selected in our controls, but negatively selected in our periodontitis patients (Figure 5A). In the meantime, lnuC from Streptococcus agalactiae was positively selected both in our periodontitis patients and controls (Figure 5A and B). The ileS gene from Bifidobacteria was positively selected in both periodontitis patients and controls from both datasets, indicating a strong evolutionary dynamic (Figure 5A and B).
Figure 5.
Ka/Ks ratios of ARGs and VirGs in periodontitis and control samples from both datasets
A. Ka/Ks ratios of ARGs in periodontitis and control samples from current dataset. B. Ka/Ks ratios of ARGs in periodontitis and control samples from Wang and colleagues [24]. C. Ka/Ks ratios of VirGs in periodontitis and control samples from current dataset. D. Ka/Ks ratios of VirGs in periodontitis and control samples from Wang and colleagues [24]. Genes are marked in red if their Ka/Ks ratios are higher than 1 in periodontitis samples and lower than 1 in control samples. Genes are marked in green if their Ka/Ks ratios are higher than 1 in control samples and lower than 1 in periodontitis samples. Genes are colored in orange if their Ka/Ks ratios are higher than 1 in both periodontitis and control samples.
Besides ARGs, a total of 181 VirGs with at least one non-synonymous SNP were identified, highlighting the evolutionary potential in VirGs in both studies. Notably, 145 of these VirGs from pathogens were reported to be associated with respiratory infection (Table S13). We found a total of three VirGs positively selected only in periodontitis patients and negatively selected only in controls from both datasets (Figure 5C and D; Table S13). One gene from current dataset was SP_0492, which encodes a conserved protein in Streptococcus pneumoniae TIGR4 (Figure 5C). The other two genes from the previous study [24] were divIB, encoding a cell division protein in Streptococcus pneumoniae TIGR4, and rfbP, encoding an undecaprenyl-phosphate galactose phosphotransferase involved in the biosynthesis of bacterial lipopolysaccharides in Haemophilus influenzae Rd KW20 (Figure 5D). Notably, all pathogens in which these VirGs were positively selected were associated with respiratory infection (Table S13).
Discussion
Increased epidemiologic evidence supported the associations between periodontitis and systemic diseases, such as respiratory disease. Dysbiosis of the oral microflora easily leads to translocation of bacteria and bacterial metabolites to the airway, increasing risk of respiratory infection. In this study, we found a set of significantly abundant bacteria as well as functional pathways in periodontitis patients based on metagenomic sequencing data from six periodontitis plaque specimens and three healthy periodontal plaque specimens. Through investigating potential bacteria, ARGs, and VirGs associated with periodontitis, we found several positively selected genes encoding virulence proteins and antibiotic resistance proteins encoded by respiratory disease-associated pathogens from both our dataset and the study by Wang and colleagues [24]. These findings indicate a potential association between periodontitis and respiratory infection.
Both Wilcoxon rank rum test and LEfSe analysis showed that two phyla and five species had significantly increased abundance in periodontitis patients than in controls. Spirochaetes is one of the two phyla significantly increased in patients, whose accumulation in subgingival plaques appears to be a marker of the clinical severity of periodontal disease [27], comprising up to 50% of the polymicrobial population in subgingival plaques in periodontitis, and < 1% in healthy periodontium [28]. Among members of Spirochaetes, Treponema is the only genus that appears in the human mouth [29] which was also significantly enriched in our patients. Among species of Treponema, Treponema denticola and Treponema medium were significantly enriched in our patients, and both were reported to be periodontitis pathogens [30]. Treponema denticola is an important pathogen associated with periodontitis, as it not only destroys host tissue but also co-aggregates with Porphyromonas gingivalis, Fusobacterium nucleatum, and Tannerella forsythia to form the ‘red complex’ [31], [32]. Synergistetes is another significantly enriched phylum playing a role in increasing pocket depth, inflammation, anaerobiosis, and gingival tissue destruction [33]. Species members Fretibacterium fastidiosum, Desulfobulbus sp. oral taxon 041, and Bacteroidetes bacterium oral taxon 272, which were significantly enriched in our periodontitis patients, have been reported to be significantly associated with periodontitis [33], [34], [35].
Several eggNOG terms associated with drug-resistance and bacteria virulence were found to be significantly enriched in periodontitis patients. Transposase, the most frequently abundant term of functional eggNOG terms, often harbors resistance genes against many different antibiotics. Most DNA transposons confer resistance to all major antibiotic classes against bacteria, and transpositions of these transposons are major drivers of resistance spreading [36]. The significantly over-abundant cell wall/membrane/envelope biogenesis and MATE efflux family proteins in patients together facilitate drug effluxion and induce drug resistance [37], [38]. Active efflux could reduce the intracellular accumulation of antimicrobials, which is a major mechanism of antimicrobial resistance in pathogenic organisms [38]. It is crucially important to maintain an effective barrier around the organism for active efflux systems to reduce the influx of antimicrobials into the cell [37]. GSEA showed the enrichment for MCP and gingipain R in patients and genes associated with the synthesis of fatty acids in controls. MCPs, which are enriched in periodontitis patients, comprise a family of bacterial receptors that accept diverse environmental signals such as those from attractants and repellents and mediate the approach or escape through alteration of swimming behavior [39]. Gingipains are trypsin-like cysteine proteinases produced by Porphyromonas gingivalis, one of the most prominent virulence factors in periodontal disease. Gingipains not only deal with cell surface proteins when contact but also degrade components of the cell-to-cell contacts and cause detachment of epithelial cells from the connective tissue of the gingiva [40]. Several genes associated with the synthesis of fatty acids, such as those encoding fatty acid synthase, esterase, and MaoC domain protein dehydratase, were found to be enriched in controls, and some kinds of fatty acids have been reported to be of benefit for oral health and play a positive role in periodontitis treatment [41].
We called SNPs and compared the MAF of non-synonymous and unique non-synonymous SNPs in ARGs between periodontitis patients and controls in both studies, showing that ARGs may suffer much more selection pressure in periodontitis patients compared with controls, which is similar to the findings by Zhao and colleagues [42]. Besides ARGs, we also found similar trends in VirGs, indicating that VirGs may also be under more selection pressure in periodontitis patients compared with controls. In fact, inclusion criteria for subjects in our study were similar to the previous study by Wang et al. [24], including without systemic diseases and prosthetic dental appliances. In addition, all subjects had never received professional periodontal therapy or antibiotic treatment within 3 months prior the study. Considering that the periodontitis and control subjects in the same study were all local residents and shared similar climate and environmental conditions without distinct dietary habits, the selection pressure may be associated with the interaction between pathogenesis and treatment.
The Ka/Ks ratio is commonly used in understanding the evolutionary dynamic of protein-coding sequences across closely related and yet divergent species [26], [43]. Several ARGs were found with Ka/Ks > 1 in periodontitis patients and Ka/Ks < 1 in controls. Proteins encoded by cpxR in Pseudomonas aeruginosa activate the expression of the MexAB-OprM efflux pump and enhance drug resistance [44]. pgpB, encoding lipid A 4′-phosphatase in Porphyromonas gingivalis ATCC 33277, confers resistance to polymyxin B by making lipid A lose a negative charge from the lipid A 4′-phosphate [45]. It is noted that Porphyromonas gingivalis is one of the most import periodontitis pathogen and lipid A is one of the key virulence factors in Porphyromonas gingivalis invasion. pgpB was the only ARG existing in periodontitis-associated pathogens with Ka/Ks > 1 in periodontitis patients and Ka/Ks < 1 in controls; this gene was identical in both the study by Wang et al. [24] and our data. Interestingly, Porphyromonas gingivalis could also cause pneumonia [10], and polymyxin B resisted by pgbB has already been widely used in pneumonia treatment [46]. It was supposed that selection pressure of pgpB is likely to be associated with both periodontitis and pneumonia.
None of the Ka values of the virulence proteins in periodontitis pathogens were found to be higher than the Ks values in both datasets. However, three VirGs in respiratory tract pathogens were found to have Ka/Ks > 1 in periodontitis patients and Ka/Ks < 1 in controls, two of which were from Streptococcus pneumoniae TIGR4 and one was involved in the biosynthesis of bacterial lipopolysaccharides in Haemophilus influenzae Rd KW20. When focusing on the background VirGs with at least one non-synonymous SNP, these three VirGs were positively selected. It was noted that nearly all (91.8%) of the background VirGs with at least one non-synonymous SNP for natural selection were from respiratory tract pathogens. The evolutionary background of VirGs in periodontitis may suggest a possible association with respiratory infection.
Multiple epidemiological studies have reported an association between periodontal inflammation and respiratory infection [47], [48]. Poor oral hygiene and periodontal disease may facilitate the colonization of potential respiratory pathogens (PRPs) [49], especially on the surface of dental plaques. Once the host’s defense is compromised, PRPs can access the respiratory tract by oropharyngeal secretions or inhalation, and then overwhelm the host’s immune system [9]. Some pathogens associated with periodontitis, such as Porphyromonas gingivalis and Treponema denticola, are also reported to cause pneumonia [10]. In our study, it may be hypothesized that although the pathogens associated with respiratory infection were not significantly dominant in periodontitis, some of the virulence proteins or the antibiotic resistance proteins of these pathogens were significantly abundant and putatively positively selected; therefore, these pathogens could have been ready to access and invade the respiratory tract. It is likely that there could be an interaction between respiratory disease and periodontitis at the gene level.
Conclusion
Although the oral microbial profile of periodontitis is still unclear, the present study provides several points of clarification. Apart from increased abundance of pathogens and community diversity consistent with previous studies, we found a new pathogen and several abundant functional pathways that differed between periodontitis patients and healthy controls. We also found that ARGs as well as VirGs may also be subject to positive selection. Several identical significantly abundant and positively selected ARGs and VirGs were identified in respiratory disease-associated pathogens in the two different datasets. These genes could not only serve as targets for further studies but may also offer clues for studying the association between respiratory disease and periodontitis. Our findings may enrich the knowledge of pathogens, drug resistance, and functional pathways in the oral microbiota of periodontitis and shed lights on the association of periodontitis with respiratory disease. However, animal model or deep functional assays should be carried out to explore the functional mechanisms of pathogens in periodontitis and the association between periodontal inflammation and systemic diseases in the future.
Materials and methods
Sample and data collection
A total of 30 periodontitis patients and 15 periodontal healthy individuals were recruited based on the defined standard description in a previous study [50]. Participants were all previously un-treated for periodontitis. Periodontal health was defined as having a probing depth and attachment loss < 2 mm. Participants with any other dental or medical history other than chronic periodontitis, prosthetic dental appliances, antibiotic treatment within the previous 3 months, diabetes, hypertension or hepatitis were excluded. Clinical details for each participant, including age, sex, diagnosis, tooth number, sample location, periodontal probing depth (mm), clinical attachment loss (mm), dental history, smoking, alcohol consumption, hypertension, diabetes, hepatitis, and treatment history are provided in the Table S1. The periodontist performed a full-mouth examination and took dental plaque samples from the tooth with the poorest condition, excluding third molars.
For each individual, dental plaques were collected from 3 to 4 sites (buccal surface, lingual surface, and supragingival sites) by a periodontist and pooled together as one sample. Dental plaques were collected using a sterilized inoculating-loop-like device to increase accumulation and to avoid gingival bleeding. Each plaque sample was placed in a sterilized 1.5-ml centrifuge tube containing 50 μl of phosphate buffer solution (PBS; pH = 8.0) and stored at −80 °C until use. All specimens were collected in a sterilized operating room with strict aseptic operation.
Previous raw sequencing data for dental plaques (PHP1-10 and PDP1-10) from the study by Wang et al. [24] were downloaded from the Sequence Read Archive database (SRA: SRP033553, https://www.ncbi.nlm.nih.gov/sra). The ARGs and VirGs were analyzed with SRA toolkit (v2.10.0) with the “prefetch” command. The “fastq-dump” command was used to obtain the FASTQ files from the downloaded SRA file.
Specimen processing and metagenomic sequencing
Metagenomic DNA was isolated from the 45 specimens individually using a QIAamp DNA Mini Kit (Catalog No. 51306, Qiagen, Hilden, Germany). The quality and quantity of isolated DNA were measured using a Qubit Fluorometer, a NanoDrop 2000 spectrophotometer (ND2000CLAPTOP, ThermoFisher Scientific, Waltham, MA), and agarose gel electrophoresis. For each specimen, 0.5 μg of purified metagenomic DNA was sheared into fragments of ∼ 180 bp in length, which then were end-polished, A-tailed, and ligated with the full-length adaptor for library construction using TruSeq DNA Library Preparation Kit (v2) according to a standard protocol provided by Illumina, Inc. (Catalog No. FC-121-2002, Illumina, San Diego, CA). After further PCR amplification, the PCR products were purified using the AMPure XP system (Catalog No. A63880, Beckman Coulter, Brea, CA). Finally, the libraries were analyzed for size distribution with the Agilent2100 bioanalyzer (Catalog No. G2939BA, Agilent Technologies, Palo Alto, CA) and quantified using real-time PCR before high-throughput sequencing on an Illumina HiSeq 2500.
Read filtering and merging
First, the quality control, cutoff of the adapter, and removal of the low-quality reads were performed as described previously [51]. Second, filtered high-quality PE reads were aligned to human genome assembly (hg19) using Bowtie2 (v2.3.4) to remove human contamination, and further visualized through Splicing Viewer [52]. Finally, the nonhuman PE reads were merged using FLASH (v1.2.11) with overlapping lengths ranging from 6 bp to 40 bp and mismatch threshold set to 0.15. These filtering and merging steps were processed for the current dataset and the dataset from Wang and colleagues [24].
Taxonomic classification, construction of a nonredundant reference gene set, and functional annotation
MetaPhlAnv2 [21] was used to process the taxonomic profiles, and the Wilcoxon rank sum test was used to determine the differential abundance of microbial taxa between periodontitis patients and controls. Based on the abundance profiles at the phylum and species levels, the beta diversity was estimated by PCA and NMDS analysis, and the alpha diversity was measured using the Shannon index, Simpson index, and Pielou index. LEfSe [53] analysis was performed to obtain taxonomic biomarkers. To obtain a nonredundant reference gene set, all FASTA files were integrated, and then MEGAHIT (v1.1.3) was used to assemble these reads into contigs, in which only contigs with a length of 500 bp or more were retained. A set of proteins predicted by MetaGeneMark (v3.8) was input into CD-HIT (v4.6.2) to obtain the nonredundant reference protein sequence set, and a nonredundant nucleotide reference gene set was also obtained from the predicted nucleotide sequences according to the gene number. Reads were aligned to the nonredundant nucleotide gene set using Bowtie2, and the gene RPK value was calculated.
eggNOG-mapper (v1.0.3) [54] was used to map the correlated protein sequences of all predicted genes to annotation databases, such as KEGG, eggNOG, and GO. The RPK value of each annotation was obtained by summing the RPK values of genes with the same annotation, and DESeq2 was used to obtain the significant functional annotations. GSEA was performed using GSEA (v3.0) with RPK values in genes from both patients and controls as well as genes included in KEGG terms, GO terms, and eggNOG terms.
ARG and VirG annotation
The abundance of each gene family in the oral microbiota was analyzed by HUMAnN2 (v0.11.1) [55] in RPK units. The significantly enriched gene families were obtained using DESeq2. DeepARG [23] was used to annotate all ARG reads in each sample in our data and the data from the study by Wang and colleagues [24]. The DIAMOND cutoff was set to 50% for the threshold of sequence matching ratio as well as 60% for similarity and 1.00 × 10−7 for the e-value as recommended by ARGs-OAP [56]. The relative abundance of each ARG was calculated as described previously [57]; LEfSe [53] analysis was used to obtain the ARG biomarkers. Virulence protein sequences were downloaded from PATRIC (ftp://ftp.patricbrc.org/specialty_genes/referenceDBs/PATRIC_VF.faa) [58], Victors (http://www.phidias.us/victors/downloads/gen_downloads_protein.php) [59], and the virulence factor database (http://www.mgc.ac.cn/VFs/download.htm) [60]. A nonredundant reference virulence sequence was finally obtained after using CD-HIT. All reads in each sample in our data and the data from the study by Wang et al. [24] were annotated using the same method and cutoff values as those in the ARG annotation.
Reference ARG and VirG nucleotide sequence construction, SNP calling, and positively selected gene detection
The reference ARG protein sequences processed in DeepARG were used to construct a custom database. Among a total of 14,974 nonredundant ARG proteins, there were 10,619 protein sequences from UniProt90 (https://ftp.uniprot.org/pub/databases/uniprot/previous_releases/release-2018_11/), 2152 from the Comprehensive Antibiotic Research Database (https://card.mcmaster.ca/download, CARD Data for October 2018 release), and 2203 from the Antibiotic Resistance Genes Database (ftp://ftp.cbcb.umd.edu/pub/data/ARDB/ardbAnno1.0.tar.gz). Almost all correlated nucleotide sequences were downloaded from the official website. To ensure the accuracy, the downloaded nucleotide sequences were aligned against the reference protein sequences using BLASTX, and the matched nucleotide sequence segment in the best hit in each blast was considered as the correlating reference nucleotide sequence.
The FASTA files of each sample were aligned to the constructed reference nucleotide sequences using BWA-mem (v0.7.17). SAMtools (v1.9), BCFtools (v1.9), and VarScan (v2.4.3) were used to call SNPs, and VCFtools (v0.1.16) was used to filter the low-quality SNPs from each sample [61]. SNPs called by BCFtools were combined with those called by VarScan. According to the Bacterial and Plant Plastid Code, the amino acid encoded by an altered codon was compared with that encoded by a reference codon to determine whether the SNP was a synonymous or non-synonymous SNP. The SNP rarefaction curve was plotted using the R package “Vegan”, and the Ka/Ks ratio was calculated using the KaKs calculator after producing the axt file [42].
The nonredundant reference virulence protein sequences were aligned to the NT database (https://www.ncbi.nlm.nih.gov/genbank/, Release 228) using TBLASTN. The aligned nucleic acid sequence with the best hit score was considered as the corresponding nucleic acid sequence. The subsequent SNP calling and annotation methods were similar to those used in the calling and annotation of ARG SNPs.
Ethical statement
This study was approved by the Ethics Committee of the First Affiliated Hospital of Wenzhou Medical University, China, and written informed consent was received from all participants before their enrolment.
Data availability
The raw sequence data reported in this study have been deposited in the Genome Sequence Archive [62] at the National Genomics Data Center, Beijing Institute of Genomics, Chinese Academy of Sciences / China National Center for Bioinformation (GSA: CRA003553) and are publicly accessible at https://ngdc.cncb.ac.cn/gsa.
CRediT author statement
Zhenwei Liu: Formal analysis, Visualization, Writing - original draft, Writing - review & editing. Tao Zhang: Methodology, Formal analysis, Visualization, Writing - original draft. Keke Wu: Software, Data curation, Visualization, Writing - original draft. Zhongshan Li: Formal analysis, Data curation. Xiaomin Chen: Investigation, Resources. Shan Jiang: Formal analysis, Validation. Lifeng Du: Data curation, Resources. Saisai Lu: Investigation, Validation. Chongxiang Lin: Resources, Data curation. Jinyu Wu: Conceptualization, Writing - original draft, Writing - review & editing, Supervision. Xiaobing Wang: Conceptualization, Writing - original draft, Writing - review & editing, Supervision, Funding acquisition. All authors have read and approved the final manuscript.
Competing interests
The authors have declared no competing interests.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (Grant No. 81700062), the Wenzhou Medical University Key Program Cultivation Project, China (Grant No. KYYW202005), the Science and Technology Project of Zhejiang Provincial Health Commission, China (Grant No. 2019RC050), and the Science and Technology Project of Wenzhou, China (Grant No. Y20160028). We thank Helen Jeays, BDSc AE, from Liwen Bianji, Edanz Editing China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript. We also thank Jianmin Wu for providing insightful comments and suggestions on this manuscript.
Handled by Fangqing Zhao
Footnotes
Peer review under responsibility of Beijing Institute of Genomics, Chinese Academy of Sciences / China National Center for Bioinformation and Genetics Society of China.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.gpb.2021.07.001.
Contributor Information
Jinyu Wu, Email: iamwujy@wmu.edu.cn.
Xiaobing Wang, Email: wangxiaobing@wzhospital.cn.
Supplementary material
The following are the Supplementary data to this article:
Supplementary Figure S1.
Clinical evidence and quality controls of raw and clean reads A. X ray film of one patient with obvious bone loss. B. Photo of a patient with bleeding on probing. C. Clean, raw, and uncontaminated read numbers as well as the clean read rate and non-human contaminated read rate of our data. D. Read number and rates of NS reads (reads with N bases), low-quality reads, and polluted adapter reads in the current dataset.
Supplementary Figure S2.
The shift of oral microbiota between periodontitis and control samples at the genus level A. The difference in relative abundance of each genus between periodontitis and control samples among the top 30 genera. The significantly differential relative abundance for genera was marked by red (Wilcoxon rank sum test). B. Rarefaction curve at the species level. C. Genus biomarkers in periodontitis and control samples were depicted by LEfSe analysis (LDA > 3).
Supplementary Figure S3.
Beta diversity and alpha diversity at the phylum or species level A. PCA analysis at the phylum level. B. The NMDS analysis at the phylum level. C. The ANOSIM of NMDS analysis at the phylum level. D. Pielou index at the phylum level between periodontitis and control samples. E. Shannon index at the phylum level between periodontitis and control samples. F. Simpson index at the phylum level between periodontitis and control samples. G. Simpson index at the species level between periodontitis and control samples. All P values were calculated by Wilcoxon rank sum test. PCA, Principal component analysis; NMDS, non-metric multidimensional scaling; ANOSIM, analysis of similarities.
Supplementary Figure S4.
Comparison of the relative abundance of UniProt90 genes between the both datasets A. PCA analysis between two datasets. B. The NMDS analysis of all samples using UniProt90 gene relative abundance from both datasets. C. Intersections between ARGs in our patient samples and Wang’s patient samples. D. Intersections between VirGs in our patient samples and Wang’s patient samples. ARGs, antibiotic resistance genes; VirGs, virulence genes.
Supplementary Figure S5.
Rarefaction curve of SNPs in ARGs and VirGs from both datasets Rarefaction curve of SNPs in ARGs (A) and VirGs (B) from the current dataset. Rarefaction curve of SNPs in ARGs (C) and VirGs (D) of periodontitis patients from Wang et al. 2016. Rarefaction curve of SNPs in ARGs (E) and VirGs (F) of controls from Wang et al. 2016. SNPs, single-nucleotide polymorphisms. SNPs, single-nucleotide polymorphisms.
Supplementary Figure S6.
Comparison of synonymous SNPs in ARGs and VirGs between periodontitis and control samples from both datasets Distribution of MAF of SNPs in ARGs from both the current study (A) and a previous study (B). C. Comparison of the MAF of synonymous SNPs in ARGs between periodontitis patients and controls in both datasets. Distribution of the MAF of synonymous SNPs in VirGs both the current study (D) and a previous study (E). F. Comparison of the MAF of synonymous SNPs in VirGs between periodontitis patients and controls in both datasets. All P values were calculated by Wilcoxon rank sum test. MAF, minor allele frequency.
Detailed clinical information for all participants
Quality control of our sequenced data
Relative abundance of kingdom level in the current samples
Relative abundance of phylum level in the current samples
Relative abundance of genus level in the current samples
Relative abundance of species level in the current samples
The differential function of microbial taxa between periodontitis patients and controls
The GSEA analysis in KEGG, GO, and EggNOG terms
LEfSe analysis of ARGs and VirGs in the current dataset
Quality control of dataset by Wang et al. 2016
LEfSe analysis of ARGs and VirGs in the dataset by Wang et al. 2016
The Ka/Ks value of each ARG in both datasets
The Ka/Ks value of each VirG in both datasets
References
- 1.Kononen E., Gursoy M., Gursoy U.K. Periodontitis: a multifaceted disease of tooth-supporting tissues. J Clin Med. 2019;8:1135. doi: 10.3390/jcm8081135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Curtis M.A., Diaz P.I., Van Dyke T.E. The role of the microbiota in periodontal disease. Periodontol. 2020;83:14–25. doi: 10.1111/prd.12296. [DOI] [PubMed] [Google Scholar]
- 3.Minty M., Canceil T., Serino M., Burcelin R., Tercé F., Blasco-Baque V. Oral microbiota-induced periodontitis: a new risk factor of metabolic diseases. Rev Endocr Metab Disord. 2019;20:449–459. doi: 10.1007/s11154-019-09526-8. [DOI] [PubMed] [Google Scholar]
- 4.Zhang S., Yu N., Arce R.M. Periodontal inflammation: integrating genes and dysbiosis. Periodontol. 2020;82:129–142. doi: 10.1111/prd.12267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loos B.G., Van Dyke T.E. The role of inflammation and genetics in periodontal disease. Periodontol. 2020;83:26–39. doi: 10.1111/prd.12297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liccardo D., Cannavo A., Spagnuolo G., Ferrara N., Cittadini A., Rengo C., et al. Periodontal disease: a risk factor for diabetes and cardiovascular disease. Int J Mol Sci. 2019;20:1414. doi: 10.3390/ijms20061414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Molon R.S., Rossa C., Jr., Thurlings R.M., Cirelli J.A., Koenders M.I. Linkage of periodontitis and rheumatoid arthritis: current evidence and potential biological interactions. Int J Mol Sci. 2019;20:4541. doi: 10.3390/ijms20184541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mammen M.J., Scannapieco F.A., Sethi S. Oral-lung microbiome interactions in lung diseases. Periodontol. 2020;83:234–241. doi: 10.1111/prd.12301. [DOI] [PubMed] [Google Scholar]
- 9.Bansal M., Khatri M., Taneja V. Potential role of periodontal infection in respiratory diseases - a review. J Med Life. 2013;6:244–248. [PMC free article] [PubMed] [Google Scholar]
- 10.Kimizuka R., Kato T., Ishihara K., Okuda K. Mixed infections with Porphyromonas gingivalis and Treponema denticola cause excessive inflammatory responses in a mouse pneumonia model compared with monoinfections. Microbes Infect. 2003;5:1357–1362. doi: 10.1016/j.micinf.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 11.Costalonga M., Herzberg M.C. The oral microbiome and the immunobiology of periodontal disease and caries. Immunol Lett. 2014;162:22–38. doi: 10.1016/j.imlet.2014.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roy S., Douglas C.W.I., Stafford G.P. A novel sialic acid utilization and uptake system in the periodontal pathogen Tannerella forsythia. J Bacteriol. 2010;192:2285–2293. doi: 10.1128/JB.00079-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sudhakara P., Sellamuthu I., Aruni A.W. Bacterial sialoglycosidases in virulence and pathogenesis. Pathogens. 2019;8:39. doi: 10.3390/pathogens8010039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Solbiati J., Frias-Lopez J. Metatranscriptome of the oral microbiome in health and disease. J Dent Res. 2018;97:492–500. doi: 10.1177/0022034518761644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Read A.F., Woods R.J. Antibiotic resistance management. Evol Med Public Health. 2014;2014:147. doi: 10.1093/emph/eou024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ventola C.L. The antibiotic resistance crisis: part 1: causes and threats. P T. 2015;40:277–283. [PMC free article] [PubMed] [Google Scholar]
- 17.zur Wiesch P.A., Kouyos R., Engelstädter J., Regoes R.R., Bonhoeffer S. Population biological principles of drug-resistance evolution in infectious diseases. Lancet Infect Dis. 2011;11:236–247. doi: 10.1016/S1473-3099(10)70264-4. [DOI] [PubMed] [Google Scholar]
- 18.Rams T.E., Degener J.E., van Winkelhoff A.J. Antibiotic resistance in human chronic periodontitis microbiota. J Periodontol. 2014;85:160–169. doi: 10.1902/jop.2013.130142. [DOI] [PubMed] [Google Scholar]
- 19.Ardila C.M., Granada M.I., Guzman I.C. Antibiotic resistance of subgingival species in chronic periodontitis patients. J Periodontal Res. 2010;45:557–563. doi: 10.1111/j.1600-0765.2010.01274.x. [DOI] [PubMed] [Google Scholar]
- 20.van Winkelhoff A.J., Herrera D., Oteo A., Sanz M. Antimicrobial profiles of periodontal pathogens isolated from periodontitis patients in the Netherlands and Spain. J Clin Periodontol. 2005;32:893–898. doi: 10.1111/j.1600-051X.2005.00782.x. [DOI] [PubMed] [Google Scholar]
- 21.Truong D.T., Franzosa E.A., Tickle T.L., Scholz M., Weingart G., Pasolli E., et al. Metaphlan2 for enhanced metagenomic taxonomic profiling. Nat Methods. 2015;12:902–903. doi: 10.1038/nmeth.3589. [DOI] [PubMed] [Google Scholar]
- 22.Nikaido H. Multiple antibiotic resistance and efflux. Curr Opin Microbiol. 1998;1:516–523. doi: 10.1016/s1369-5274(98)80083-0. [DOI] [PubMed] [Google Scholar]
- 23.Arango-Argoty G., Garner E., Pruden A., Heath L.S., Vikesland P., Zhang L. Deeparg: a deep learning approach for predicting antibiotic resistance genes from metagenomic data. Microbiome. 2018;6:23. doi: 10.1186/s40168-018-0401-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J., Gao Y., Zhao F. Phage-bacteria interaction network in human oral microbiome. Environ Microbiol. 2016;18:2143–2158. doi: 10.1111/1462-2920.12923. [DOI] [PubMed] [Google Scholar]
- 25.Liu G., Wu J., Yang H., Bao Q. Codon usage patterns in Corynebacterium glutamicum: mutational bias, natural selection and amino acid conservation. Comp Funct Genomics. 2010;2010:343569. doi: 10.1155/2010/343569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang Z., Li J., Zhao X.Q., Wang J., Wong G.S., Yu J. KaKs_Calculator: calculating Ka and Ks through model selection and model averaging. Genomics Proteomics Bioinformatics. 2006;4:259–263. doi: 10.1016/S1672-0229(07)60007-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Loesche W.J. The role of spirochetes in periodontal disease. Adv Dent Res. 1988;2:275–283. doi: 10.1177/08959374880020021201. [DOI] [PubMed] [Google Scholar]
- 28.Chan E.C., McLaughlin R. Taxonomy and virulence of oral spirochetes. Oral Microbiol Immunol. 2000;15:1–9. doi: 10.1034/j.1399-302x.2000.150101.x. [DOI] [PubMed] [Google Scholar]
- 29.Dewhirst F.E., Chen T., Izard J., Paster B.J., Tanner A.C., Yu W.H., et al. The human oral microbiome. J Bacteriol. 2010;192:5002–5017. doi: 10.1128/JB.00542-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Belda-Ferre P., Alcaraz L.D., Cabrera-Rubio R., Romero H., Simón-Soro A., Pignatelli M., et al. The oral metagenome in health and disease. ISME J. 2012;6:46–56. doi: 10.1038/ismej.2011.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ikegami A., Honma K., Sharma A., Kuramitsu H.K. Multiple functions of the leucine-rich repeat protein lrra of Treponema denticola. Infect Immun. 2004;72:4619–4627. doi: 10.1128/IAI.72.8.4619-4627.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosen G., Genzler T., Sela M.N. Coaggregation of Treponema denticola with Porphyromonas gingivalis and Fusobacterium nucleatum is mediated by the major outer sheath protein of Treponema denticola. FEMS Microbiol Lett. 2008;289:59–66. doi: 10.1111/j.1574-6968.2008.01373.x. [DOI] [PubMed] [Google Scholar]
- 33.You M., Mo S., Watt R.M., Leung W.K. Prevalence and diversity of Synergistetes taxa in periodontal health and disease. J Periodontal Res. 2013;48:159–168. doi: 10.1111/j.1600-0765.2012.01516.x. [DOI] [PubMed] [Google Scholar]
- 34.Gao W., Chan Y., You M., Lacap-Bugler D.C., Leung W.K., Watt R.M. In-depth snapshot of the equine subgingival microbiome. Microb Pathog. 2016;94:76–89. doi: 10.1016/j.micpath.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 35.Cao Y., Qiao M., Tian Z., Yu Y., Xu B., Lao W., et al. Comparative analyses of subgingival microbiome in chronic periodontitis patients with and without IgA nephropathy by high throughput 16S rRNA sequencing. Cell Physiol Biochem. 2018;47:774–783. doi: 10.1159/000490029. [DOI] [PubMed] [Google Scholar]
- 36.Rubio-Cosials A., Schulz E.C., Lambertsen L., Smyshlyaev G., Rojas-Cordova C., Forslund K., et al. Transposase-DNA complex structures reveal mechanisms for conjugative transposition of antibiotic resistance. Cell. 2018;173 doi: 10.1016/j.cell.2018.02.032. 208–20.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nikaido H. Preventing drug access to targets: cell surface permeability barriers and active efflux in bacteria. Semin Cell Dev Biol. 2001;12:215–223. doi: 10.1006/scdb.2000.0247. [DOI] [PubMed] [Google Scholar]
- 38.Borges-Walmsley M.I., Walmsley A.R. The structure and function of drug pumps. Trends Microbiol. 2001;9:71–79. doi: 10.1016/s0966-842x(00)01920-x. [DOI] [PubMed] [Google Scholar]
- 39.Derr P., Boder E., Goulian M. Changing the specificity of a bacterial chemoreceptor. J Mol Biol. 2006;355:923–932. doi: 10.1016/j.jmb.2005.11.025. [DOI] [PubMed] [Google Scholar]
- 40.Nakayama M., Ohara N. Molecular mechanisms of Porphyromonas gingivalis-host cell interaction on periodontal diseases. Jpn Dent Sci Rev. 2017;53:134–140. doi: 10.1016/j.jdsr.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sommakia S., Baker O.J. Regulation of inflammation by lipid mediators in oral diseases. Oral Dis. 2017;23:576–597. doi: 10.1111/odi.12544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhao F., Bai J., Wu J., Liu J., Zhou M., Xia S., et al. Sequencing and genetic variation of multidrug resistance plasmids in Klebsiella pneumoniae. PLoS One. 2010;5:e10141. doi: 10.1371/journal.pone.0010141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yu T., Li J., Yang Y., Qi L., Chen B., Zhao F., et al. Codon usage patterns and adaptive evolution of marine unicellular cyanobacteria Synechococcus and Prochlorococcus. Mol Phylogenet Evol. 2012;62:206–213. doi: 10.1016/j.ympev.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 44.Tian Z.X., Yi X.X., Cho A., O’Gara F., Wang Y.P., Parsek M.R. CpxR activates MexAB-oprm efflux pump expression and enhances antibiotic resistance in both laboratory and clinical nalB-type isolates of Pseudomonas aeruginosa. PLoS Pathog. 2016;12:e1005932. doi: 10.1371/journal.ppat.1005932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Coats S.R., To T.T., Jain S., Braham P.H., Darveau R.P. Porphyromonas gingivalis resistance to polymyxin b is determined by the lipid a 4′-phosphatase, PGN_0524. Int J Oral Sci. 2009;1:126–135. doi: 10.4248/IJOS.09062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Palmer L.B. Aerosolized antibiotics in the intensive care unit. Clin Chest Med. 2011;32:559–574. doi: 10.1016/j.ccm.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 47.Laurence B., Mould-Millman N.K., Scannapieco F.A., Abron A. Hospital admissions for pneumonia more likely with concomitant dental infections. Clin Oral Invest. 2015;19:1261–1268. doi: 10.1007/s00784-014-1342-y. [DOI] [PubMed] [Google Scholar]
- 48.Sjogren P., Nilsson E., Forsell M., Johansson O., Hoogstraate J. A systematic review of the preventive effect of oral hygiene on pneumonia and respiratory tract infection in elderly people in hospitals and nursing homes: effect estimates and methodological quality of randomized controlled trials. J Am Geriatr Soc. 2008;56:2124–2130. doi: 10.1111/j.1532-5415.2008.01926.x. [DOI] [PubMed] [Google Scholar]
- 49.Scannapieco F.A., Mylotte J.M. Relationships between periodontal disease and bacterial pneumonia. J Periodontol. 1996;67:1114–1122. doi: 10.1902/jop.1996.67.10s.1114. [DOI] [PubMed] [Google Scholar]
- 50.Wang J., Qi J., Zhao H., He S., Zhang Y., Wei S., et al. Metagenomic sequencing reveals microbiota and its functional potential associated with periodontal disease. Sci Rep. 2013;3:1843. doi: 10.1038/srep01843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang T., Liu Q., Li X., Wang X., Li J., Zhu X., et al. RRBS-Analyser: a comprehensive web server for reduced representation bisulfite sequencing data analysis. Hum Mutat. 2013;34:1606–1610. doi: 10.1002/humu.22444. [DOI] [PubMed] [Google Scholar]
- 52.Liu Q., Chen C., Shen E., Zhao F., Sun Z., Wu J. Detection, annotation and visualization of alternative splicing from RNA-Seq data with SplicingViewer. Genomics. 2012;99:178–182. doi: 10.1016/j.ygeno.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 53.Segata N., Izard J., Waldron L., Gevers D., Miropolsky L., Garrett W.S., et al. Metagenomic biomarker discovery and explanation. Genome Biol. 2011;12:R60. doi: 10.1186/gb-2011-12-6-r60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huerta-Cepas J., Forslund K., Coelho L.P., Szklarczyk D., Jensen L.J., von Mering C., et al. Fast genome-wide functional annotation through orthology assignment by eggNOG-Mapper. Mol Biol Evol. 2017;34:2115–2122. doi: 10.1093/molbev/msx148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Franzosa E.A., McIver L.J., Rahnavard G., Thompson L.R., Schirmer M., Weingart G., et al. Species-level functional profiling of metagenomes and metatranscriptomes. Nat Methods. 2018;15:962–968. doi: 10.1038/s41592-018-0176-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yang Y., Jiang X., Chai B., Ma L., Li B., Zhang A., et al. ARGs-OAP: online analysis pipeline for antibiotic resistance genes detection from metagenomic data using an integrated structured ARG-database. Bioinformatics. 2016;32:2346–2351. doi: 10.1093/bioinformatics/btw136. [DOI] [PubMed] [Google Scholar]
- 57.Hu Y., Yang X., Qin J., Lu N., Cheng G., Wu N., et al. Metagenome-wide analysis of antibiotic resistance genes in a large cohort of human gut microbiota. Nat Commun. 2013;4:2151. doi: 10.1038/ncomms3151. [DOI] [PubMed] [Google Scholar]
- 58.Driscoll T., Gabbard J.L., Mao C., Dalay O., Shukla M., Freifeld C.C., et al. Integration and visualization of host-pathogen data related to infectious diseases. Bioinformatics. 2011;27:2279–2287. doi: 10.1093/bioinformatics/btr391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sayers S., Li L., Ong E., Deng S., Fu G., Lin Y., et al. A web-based knowledge base of virulence factors in human and animal pathogens. Nucleic Acids Res. 2019;47:D693–D700. doi: 10.1093/nar/gky999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu B, Zheng D, Jin Q, Chen L, Yang J. VFDB 2019: a comparative pathogenomic platform with an interactive web interface. Nucleic Acids Res 2019;47:D687–92. [DOI] [PMC free article] [PubMed]
- 61.Chen Y., Li Z., Hu S., Zhang J., Wu J., Shao N., et al. Gut metagenomes of type 2 diabetic patients have characteristic single-nucleotide polymorphism distribution in Bacteroides coprocola. Microbiome. 2017;5:15. doi: 10.1186/s40168-017-0232-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chen T., Chen X., Zhang S., Zhu J., Tang B., Wang A., et al. The Genome Sequence Archive Family: toward explosive data growth and diverse data types. Genomics Proteomics Bioinformatics. 2021;19:578–583. doi: 10.1016/j.gpb.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Detailed clinical information for all participants
Quality control of our sequenced data
Relative abundance of kingdom level in the current samples
Relative abundance of phylum level in the current samples
Relative abundance of genus level in the current samples
Relative abundance of species level in the current samples
The differential function of microbial taxa between periodontitis patients and controls
The GSEA analysis in KEGG, GO, and EggNOG terms
LEfSe analysis of ARGs and VirGs in the current dataset
Quality control of dataset by Wang et al. 2016
LEfSe analysis of ARGs and VirGs in the dataset by Wang et al. 2016
The Ka/Ks value of each ARG in both datasets
The Ka/Ks value of each VirG in both datasets
Data Availability Statement
The raw sequence data reported in this study have been deposited in the Genome Sequence Archive [62] at the National Genomics Data Center, Beijing Institute of Genomics, Chinese Academy of Sciences / China National Center for Bioinformation (GSA: CRA003553) and are publicly accessible at https://ngdc.cncb.ac.cn/gsa.