Abstract
Extracellular Vesicles (EVs) are circulating particles surrounded by a plasma membrane carrying a cargo consisting of proteins, lipids, RNAs, and DNA fragments, stemming from the cells from which they originated. EV factors (i.e., miRNAs) play relevant roles in intercellular crosstalk, both locally and systemically. As EVs increasingly gained attention as potential carriers for targeted genes, the study of EV effects on the host immune response became more relevant. It has been demonstrated that EVs regulate the host immune response, executing both pro- and anti-inflammatory functions. It is also known that physical exercise triggers anti-inflammatory effects. This review underlines the role of circulating EVs as players in the anti-inflammatory events associated with the regulation of the host’s immune response to physical exercise.
Keywords: extracellular vesicles, inflammation, physical exercise
1. Introduction
Over the last decade, it has emerged that physical inactivity and sedentary behavior lead to the development of an inflammatory state linked to the onset of several clinical conditions [1,2,3,4]. It is already known that inflammation is aetiologically associated with the pathogenesis of neurological, pulmonary, and cardiovascular diseases (CVD), cancer, and depression [1,5,6,7,8], and a chronic low-grade inflammatory state has been considered a risk predictor factor for some of them [9]. Such an inflammatory state is characterized by high levels of different circulating inflammation markers, such as C-reactive protein (CRP), tumor necrosis factor (TNF), and interleukin-6 (IL-6). Notably, the inactivity induces visceral fat accumulation, triggering the infiltration of the adipose tissue of pro-inflammatory immune cells, further inducing the increased release of adipokines, and the development of a low-grade systemic inflammatory state [7]. The latter, in turn, has been associated with insulin resistance development, tumor growth, neurodegeneration, and atherosclerosis [4,6]. Exercise has anti-inflammatory effects, and, for this reason, regular physical activity may be protective against the development of chronic diseases [1,6,7,8].
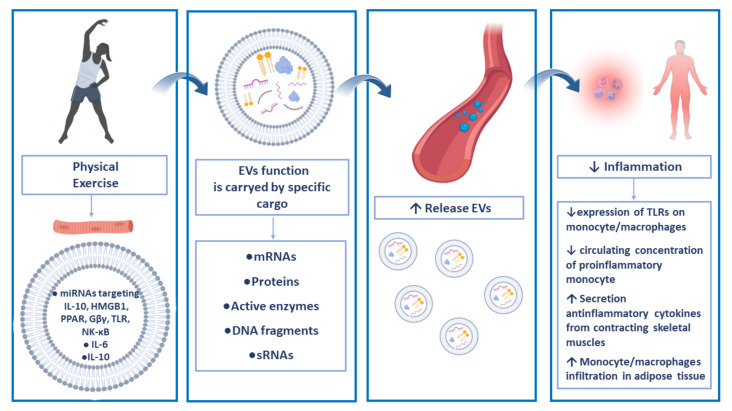
Three different possible mechanisms have been proposed to explain the anti-inflammatory effects of physical exercise: reduction in visceral fat mass; increased secretion of anti-inflammatory cytokines from contracting skeletal muscles [10,11]; and reduced expression of Toll-like receptors (TLRs) on monocytes and macrophages [12] with the subsequent inhibition of downstream responses, such as the expression of major histocompatibility complex (MHC) and co-stimulatory molecules and the production of pro-inflammatory cytokines [13]. In addition, studies on animal models have underlined that the anti-inflammatory effects induced by physical exercise also rely on other mechanisms, such as the inhibition of monocyte and macrophage infiltration into the adipose tissue and the phenotypic switching of macrophages within the adipose tissue [14]. Although these types of data are difficult to be confirmed in humans, the analysis of human peripheral blood following exercise has shown a decrease in the circulating concentrations of pro-inflammatory monocytes and an increase in the circulating frequencies of regulatory T cells, which have been demonstrated to be involved in the anti-inflammatory effects triggered by physical exercise [15].
In this context, the role of the intercellular crosstalk must be underlined, given that it is a relevant process for the spread of the cell signals to neighboring and/or distant target cells for the regulation of many functions, such as those linked to the immune system, metabolism, survival, repair/regeneration of damaged tissues, and homeostasis maintenance [16]. Intercellular crosstalk is realized by several forms of cell-to-cell communication. Cross-communication among cells may require direct contact with communicating cells (i.e., throughout the gap junctions or tunneling nanotubes). Furthermore, often the intercellular crosstalk is realized by the release from a donor cell of soluble factors (i.e., growth factors, hormones) that act as paracrine or endocrine signals on a recipient cell [16]. More recently, intercellular communication has been associated with the release and the specific loading of extracellular vesicles, small particles secreted in the extracellular milieu theoretically from all cell types [17].
The positive benefits of exercise are believed to be, at least in part, mediated by intercellular crosstalk. The study of EVs in such a context is particularly challenging and, in this review, we analyzed the potential of EVs in the mechanisms by which physical exercise exerts its anti-inflammatory role.
2. Extracellular Vesicle-Mediated Intercellular Crosstalk
“Extracellular vesicles” (EVs) is the “umbrella term” including different subtypes of membrane-surrounded particles released in the extracellular milieu by all cell types [18,19]. EV release occurs both in a constitutive and regulated manner; it is induced by Ca2+ signaling in response to different stimuli, such as ATP, neurotransmitters, depolarization, thrombin receptor activation, lipopolysaccharides, or cell stress [20,21,22,23,24,25,26].
EVs have been involved in intercellular communication, given that upon their release, they are able to pass through biological barriers and therefore can interact with their target cells over long distances [27,28,29]. It is also known that EVs exert their function throughout specific cargoes, consisting of biologically active molecules, such as active enzymes (i.e., the chaperone Hsp70), DNA fragments, mitochondria-derived vesicles, mtDNA, mRNAs, and small RNAs, that they horizontally transfer to target cells [30,31]. Therefore, EVs are specifically loaded to exert their functions on target cells. According to their diameters and the biogenesis mechanisms, EVs have been traditionally classified into apoptotic bodies (larger than 1000 nm), microvesicles released by shedding from the plasma membranes (50–1000 nm), and exosomes (around 100 nm) secreted from multivesicular endosomes [19,32]. Such a classification has been recently revised by the International Society of Extracellular Vesicles (ISEV), establishing the need to use the term EVs for all vesicle subtypes, given that they are overlapping in size and the previously used nomenclature caused confusion [33]. Therefore, the ISEV recommends identifying as small EVs, those smaller than 200 nm, and as large EVs, those with diameters larger than 200 nm [33]. Notably, it has been demonstrated that all body fluids contain mixtures of different EV phenotypes [34,35,36,37,38,39]. It is also known that EVs carry patterns of specific biomolecules related to the phenotypes and the actual status of their parental cells. For these reasons, by studying their phenotypes, it is possible to define their origins [33,37,40,41]. For example, platelet-, endothelial-, and leukocyte-derived EVs can be identified and counted from whole peripheral blood samples [34,37]. Furthermore, circulating EVs, reflecting the physiological and pathophysiological condition of the body, have been identified as reliable biomarkers for liquid biopsy purposes [42,43,44]. Peripheral EV concentrations, as well as their cargo composition, are characterized by a profound inter-subject variability, indicating that their release is a highly dynamic process [45].
For these reasons, EVs, with their specific cargoes, are emerging as comprehensive signaling entities mediating adaptive responses over large distances with widespread implications in physiological and pathophysiological events in vivo [39,46,47]. In other words, EVs modulate the functions of target cells by delivering specific cargoes that play a relevant role in intercellular signals [46]. In general, the EV crosstalk has been involved in many different homeostatic processes, such as cell metabolism, maturation, and regeneration events, modulation of the immune system as well as in the activation of blood clotting, and more generally in the processes associated with the dynamic adaptation of cells and tissues to environmental changes [48,49,50,51,52,53,54].
Notably, the EV-mediated immune system modulation is carried out by EVs stemming from immune cells and non-immune cells (mesenchymal stem cells and tumor cells) and may impact both on innate and adaptive immunity [55]. Many reports have demonstrated that lymphocytes, macrophages, dendritic cells (DCs), and natural killer cells (NKs) release EVs with the characteristics of their parental cells [56]. EVs derived from T regulatory (Treg) cells display immunosuppressive effects, given that they carry miRNAs with pro-apoptotic and anti-proliferative functions [57,58]. Therefore, Treg-derived EVs carry miRNA Let-7d and suppress interferon-γ (IFN-γ) release and T helper 1 proliferation [59]. Furthermore, EVs stemming from Tregs and expressing CD73 suppress T cell responses and cytokine production [60]. EVs released by CD4+ lymphocytes in general enhance B lymphocyte responses [61], while EVs stemming from CD8+ T cells are related to their parental subtype and its activation status. EVs derived from exhausted CD8+ T cells impair the proliferation, cell activity, and cytokine production of non-exhausted CD8+ lymphocytes, regulating gene expression and metabolic processes [62]. It has been also demonstrated that EVs are more efficient than soluble peptides in transferring antigens between Antigen presenting cells (APCs). Activated macrophages, in fact, release EVs carrying microbial antigens and pathogen-associated patterns that promote macrophage-induced inflammatory responses [63]. Cytotoxic T Lymphocytes (CTLs), NK, and dendritic cells kill their target cells through the release of EVs expressing CD95L [64,65,66]. Macrophages and DCs release EVs carrying enzymes able to synthesize leukotrienes C4 and B4, which mediate pro-inflammatory effects at the inflammation sites [67]. EVs have been implicated in the events regulating the pathogenesis of inflammatory and autoimmune diseases [68,69,70]. The intercellular crosstalk among non-immune and immune cells via EVs has been the focus of more recent scientific research, studying the role exerted by stem cell-derived and tumor-derived EVs on the host immune system. It has been demonstrated that stem cells, and in particular mesenchymal stem cells (MSCs), which roles in regenerative medicine and as immunosuppressive agents are well-established, release EVs. MSC-derived EVs have been demonstrated to produce immunosuppressive effects, throughout the transfer of their cargoes to target cells [71,72,73]. Moreover, mitochondria delivered by EVs participate in immune regulation and exert immunoregulatory effects [74]. On the other hand, it has been shown that tumor-derived EVs may stimulate or suppress the immune system. Given that EVs are enriched in specific tumor antigens, they may stimulate antitumor responses [75,76,77]. However, substantial evidence demonstrates that EVs suppress antigen-specific and non-specific immune responses. Tumor-derived EVs suppress the expression of CD3 ζ-chain, NK cytotoxicity, and CD8+ T cell functions [78]. Tumor-derived EVs also affect APC functions, favoring the generation of myeloid-suppressor cells (MDSCs), which in turn induce the regulatory activity of regulatory T cells, in inhibiting antitumor responses [79,80,81,82]. Furthermore, tumor-derived EVs can directly enhance Treg functions [83]. Moreover, it has been largely demonstrated that many other cell types (platelets, skeletal muscle cells, endothelial cells) release EVs carrying pro-inflammatory or anti-inflammatory cytokines, thus participating in the EV-mediated intercellular exchange of inflammatory or anti-inflammatory factors [34,39,55,84].
3. Extracellular Vesicles and Physical Exercise
Physical exercise produces immediate changes in several physiological parameters, such as heart rate, blood pressure, respiration, lactate levels, and circulating cell-free DNA, triggering acute responses. Furthermore, regular exercise initiates beneficial long-term adaptation processes involving muscle metabolism, cardiovascular system responses, and immune modulatory effects [4,85,86,87].
In such a context, EVs are merging as signaling entities that can contribute to mediating adaptive responses to physical exercise, possibly because they are implicated in the disposal of cellular waste produced under stress conditions, helping the body to maintain homeostasis, and participating in the immune modulation processes, tissue repair, angiogenesis, and cardio protection [88].
It has been demonstrated that the levels of small EVs increased in response to cycling exercise, dropping during the early recovery phase [89,90]. Acute bouts of exercise or short-term training produced an increase in small EV release, even in aged people [91,92,93]. It was also shown that exercise can increase the levels of EVs in diabetic mice after aerobic exercise [94].
Furthermore, the EVs released after exercise are enriched in specific markers, such as Programmed cell death 6-interacting protein (Alix), CD81, Annexin A11 (ANAX11), Alpha-actin-4 (ACTN4), and Disintegrin and metalloproteinase domain-containing protein 12 (ADAM12). These EVs have a specific tropism for the liver. Different proteins, and some novel myokines, were modulated in EVs after exercise [95], where myokines are molecules released by skeletal muscle cells and play crucial roles in reducing inflammation and carrying positive effects on lipid and glucose metabolism [96,97,98].
Therefore, exercise produces an increase in peripheral blood EV concentration related to the physiological activation state of the body. However, it is difficult to state the origin of the EVs released by the exercise, even if it may be speculated that, according to published data, the major contributing compartments to the release of EVs after exercise are muscle tissue and cardiomyocytes, endothelial and immune system cells, and platelets [90,95,99,100,101,102,103,104,105,106,107].
In cell culture experiments, cardiomyocytes increased EV release under hypoxia [108,109,110]. Therefore, part of the EVs found after exercise could be related to the reduction in the oxygen supply at the tissue level.
Muscle-derived EVs are released into the bloodstream in response to exercise and exert both paracrine and endocrine functions [111,112]. It is known that a total of ∼5% of the circulating small EVs stem from skeletal muscle [110,112], and these data are sustained by the fact that skeletal muscle cells release higher numbers of EVs than adipocytes [112]. Furthermore, using reporter mice, it was demonstrated that skeletal muscle EVs are released directly into circulation [112]. Those EVs seemed to be released upon aerobic exercise rather than by resistance exercise [113]. The release of muscle-derived EVs into circulation after exercise has been largely demonstrated by the increase in muscle- specific miRNAs in EVs [110,114]. Muscle-derived EVs participate in the systemic antioxidant defense [115]. Skeletal muscle-derived EVs exert their functions at long distances, passing across the biological barriers, given that, after their intraperitoneal injection in mice, they have been found within many different cell compartments, such as skeletal muscle, brain, liver, heart, lungs, gastrointestinal tract, spleen, kidney, and pancreas cells [116]. Additionally, it appears that skeletal muscle EVs contribute to the crossover effects of unilateral exercise [117]. Twenty-four hours after the injection of green fluorescent protein-labeled skeletal muscle EVs into the right tibialis anterior of mice, fluorescence was detected in the right quadriceps and the left tibialis anterior [116]. It was largely demonstrated, both in humans and in animal models, that aerobic physical exercise exerts beneficial effects on adipose tissue and, in general, on whole-body metabolism. In detail, both acute and chronic exercise increase catecholamine sensitivity. A single bout of resistance exercise increases adipocyte lipolysis and muscle fatty acid oxidation and such lipolytic response was impaired in obese men [118]. In response to mechanical overload, skeletal muscle cells release EVs carrying miR-1. Those EVs act on epidydimal white adipose tissue, where miR-1 promotes adrenergic signaling and lipolysis [114], and, based on these results, a clinical trial has been set up (NCT04500769).
However, capillarization is a fundamental process that influences exercise resistance, performance, muscle mass preservation, and muscle insulin response. Many factors may negatively or positively impact on skeletal capillarization. Among them, vascular endothelial growth factor (VEGF), produced by different cell subtypes, stimulates the formation of blood vessels, playing a crucial role in skeletal muscle capillarization. Of note, VEGF was not detected in EVs stemming from skeletal muscle cells, moreover, EVs cannot induce any VEGFR2 phosphorylation in recipient endothelial cells. Conversely, skeletal muscle-derived EVs induce the increase in the pro-inflammatory cytokine interleukin-8 (IL8) and of Angptl4 (Angiopoietin-like 4) without affecting Ang2/Ang1 (angiopoietin 2/angiopoietin 1), Mcp1 (monocyte chemoattractant protein 1), VEGF, and BDNF (brain-derived neurotrophic factor) mRNA expression [119]. These data suggest that skeletal muscle-derived EVs activate an angiogenetic modulating mechanism independent from VEGF-signaling. This mechanism may be instead attributed to the production of reactive oxygen species (ROS) and to the activation of nuclear factor-κB (NF-κB) signaling in endothelial cells. The characterization of miRNAs carried by skeletal muscle-derived EVs has revealed that they are muscle-specific (miR-133a and miR-206) and related to pro-angiogenic processes (miR-15, miR-16, miR-126, miR-130a, miR-210, miR-221, miR-222, miR-378, miR-503, and let7f). Those miRNAs can be transferred to endothelial cells, inducing the overexpression of miR130a with the consequent downregulation of anti-angiogenic targets, such as mesenchyme homeobox 2 (Gax). Furthermore, an increased EV production was demonstrated in oxidative more than in glycolytic muscles and this evidence was consistent with a greater capillarization of oxidative muscles [119]. As stated, together with EVs of muscle origins, endothelial-derived EVs are also released under moderate endurance exercise [99]. It is known that exercise promotes angiogenesis through the upregulation of liver-derived EVs carrying miR-122-5p, which enhances fatty acid utilization by targeting 1-acyl-sn-glycerol-3-phosphate acyltransferase alpha (AGPAT1) in endothelial cells, highlighting its therapeutic potential in tissue repair [120].
Furthermore, platelets contribute to the release of EVs after training, given that it was demonstrated that platelet-derived EVs, associated with pro-coagulant and regenerating functions, increased when subjects underwent strenuous exercises [99,101,104,105,106,107].
4. Anti-Inflammatory Roles of Exercise-Related EVs
The anti-inflammatory effects elicited by EVs have been largely demonstrated [121,122,123,124]. The EV contribution to exercise-induced improvements in systemic inflammation was also analyzed, and muscle and peripheral blood cells have been implicated in such a mechanism (Figure 1). Muscle-derived EVs improve inflammatory signaling and increase endothelial cell proliferation, migration, and tube formation through the activation of the NF-κB pathway [119]. Sullivan and collaborators demonstrated that obesity alters skeletal muscle-derived EV miRNAs, affecting mRNA targets belonging to the growth pathways (cardiac hypertrophy, Wnt/β-catenin, Phosphoinositide 3-kinases/RAC-alpha serine/threonine-protein kinase, PI3K/AKT, Insulin-like growth factor 1, IGF-1, and Phosphatase and tensin homolog, PTEN) and inflammation signaling (Pigment endothelium-derived factor, PEDF, death receptor, and Gαi). In addition, one week of concurrent aerobic and resistance exercise training altered skeletal muscle-derived small EV miRNAs targeting mRNA related to inflammation (Interleukin-10, IL-6, role of macrophages, Toll-like receptor, HMGB1, and NF-κB), growth (cardiac hypertrophy and Gβγ), and metabolism (Peroxisome proliferator-activated receptor, PPAR), indicating an overall reduction in inflammation. In particular, the activation of PPAR signaling increases lipid metabolism, exercise tolerance, and mitochondrial biogenesis via peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC1-α). Skeletal muscle Wnt3a, Wnt5a, and Wnt7a, and IGF-1 mRNAs are all reduced in obese subjects; moreover, one week of concurrent exercise training reduces, in skeletal muscle cells, mRNA expression levels of Jun, Fos, and IL-8 by approximately 25%, 65%, and 50%, respectively, in both lean and obese individuals [125]. Exercise training also induces the release and the loading of EVs acting as anti-inflammatory agents on skeletal muscles. Contracting muscles may directly release IL-6. It has been demonstrated that exercise-induced muscle-derived IL-6 exerts anti-inflammatory effects, inhibiting TNF-α, IL-10, and IL-1β activities, and protecting against TNF-induced insulin resistance [96,126,127]. The regulation of IL-6 by physical exercise has been widely investigated in the last years and IL-6 was found to be the main cytokine involved in exercise physiology. IL-6 levels rise to 100-fold (especially during intense and prolonged exercise) after physical activity, but they drop rapidly during the following rest period [128], and IL-6 has been defined as a myokine (a cytokine secreted from active skeletal muscle) [96]. The IL-6 produced by physical exercise therefore appears to have a purely anti-inflammatory role. This role seems to be mediated through the induction of IL-1Ra and IL-10 as well [128]. EVs released after exercise also carry meteorin-like protein [129], a molecule able to stimulate the release of many anti-inflammatory cytokines [130].
Figure 1.
Physical exercise and anti-inflammatory effects of EVs. Physical exercise induces the release of EVs of different origins. It has been demonstrated that exercise training induces the secretion of EVs stemming from skeletal muscle cells that carry anti-inflammatory signaling molecules (miRNAs and cytokines). Once released, (leukocyte-, muscle-, and platelet-derived EVs) EVs act locally and systemically reaching target tissues throughout blood circulation. EVs produced by physical exercise therefore act as anti-inflammatory agents.
In animal models undergoing aerobic, acrobatic, resistance, or the combination of previous exercise typologies, the cargo analysis of the EVs released after the training was carried out, demonstrating that aerobic exercise produced an increase in brain-derived neurotrophic factor (BDNF) and Interleukin- 1β (IL-1β) in aged rats, while acrobatic and combined exercises decreased the IL-1β content within EVs from adult rats. For these reasons, it has been hypothesized that the aforementioned changes may be associated with the previously observed reduction in mortality rate and improvement in memory performance [131].
It is also known that altogether EVs released after exercise, carrying IL-10 and the other anti-inflammatory cytokines, produce systemic effects, and exert their beneficial actions on the brain, directly regulating central inflammation, therefore protecting against inflammation-dependent neurological diseases [132,133].
5. Conclusions
This review underlines the role of circulating EVs as players in the anti-inflammatory events associated with the regulation of the host immune response to physical exercise. Many large epidemiological studies have demonstrated that physical inactivity is related to the occurrence of cardiovascular diseases (CVD), the leading cause of death in modern societies. For these reasons, studying the mechanisms related to such a phenomenon may suggest new strategies to improve the effects of exercise on inflammation processes implicated in the development of CVD and other chronic pathologies. In this context, EVs may play a central role and, even if more studies are needed to better identify the specific EV cargo modifications triggered by physical exercise, EVs are promising systemic carriers of anti-inflammatory messages.
Author Contributions
Conceptualization, P.S. and P.L.; investigation, G.C., D.D.B., and S.V.; resources, P.S.; writing—original draft preparation, G.C.; writing—review and editing, P.S., B.C., and P.L.; visualization, D.D.B.; supervision, B.C. and P.L.; project administration, P.L.; funding acquisition, P.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rook G.A.W., Dalgleish A. Infection, immunoregulation, and cancer. Immunol. Rev. 2011;240:141–159. doi: 10.1111/j.1600-065X.2010.00987.x. [DOI] [PubMed] [Google Scholar]
- 2.Pedersen B.K., Saltin B. Evidence for prescribing exercise as therapy in chronic disease. Scand. J. Med. Sci. Sports. 2006;16((Suppl. 1)):3–63. doi: 10.1111/j.1600-0838.2006.00520.x. [DOI] [PubMed] [Google Scholar]
- 3.Warren T.Y., Barry V., Hooker S.P., Sui X., Church T.S., Blair S.N. Sedentary behaviors increase risk of cardiovascular disease mortality in men. Med. Sci. Sports Exerc. 2010;42:879–885. doi: 10.1249/MSS.0b013e3181c3aa7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walsh N.P., Gleeson M., Shephard R.J., Gleeson M., Woods J.A., Bishop N.C., Fleshner M., Green C., Pedersen B.K., Hoffman-Goetz L., et al. Position statement. Part one: Immune function and exercise. Exerc. Immunol. Rev. 2011;17:6–63. [PubMed] [Google Scholar]
- 5.Hotamisligil G.S. Inflammation and metabolic disorders. Nature. 2006;444:860–867. doi: 10.1038/nature05485. [DOI] [PubMed] [Google Scholar]
- 6.Matulewicz N., Karczewska-Kupczewska M. Insulin resistance and chronic inflammation. Postepy Hig. Med. Dosw. 2016;70:1245–1258. [PubMed] [Google Scholar]
- 7.Ouchi N., Parker J.L., Lugus J.J., Walsh K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol. 2011;11:85–97. doi: 10.1038/nri2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leonard B.E. Inflammation, depression and dementia: Are they connected? Neurochem. Res. 2007;32:1749–1756. doi: 10.1007/s11064-007-9385-y. [DOI] [PubMed] [Google Scholar]
- 9.Pradhan A.D., Manson J.E., Rifai N., Buring J.E., Ridker P.M. C-reactive protein, interleukin 6, and risk of developing type 2 diabetes mellitus. JAMA. 2001;286:327–334. doi: 10.1001/jama.286.3.327. [DOI] [PubMed] [Google Scholar]
- 10.Petersen A.M.W., Pedersen B.K. The anti-inflammatory effect of exercise. J. Appl. Physiol. 2005;98:1154–1162. doi: 10.1152/japplphysiol.00164.2004. [DOI] [PubMed] [Google Scholar]
- 11.Pedersen B.K., Febbraio M.A. Muscle as an endocrine organ: Focus on muscle-derived interleukin-6. Physiol. Rev. 2008;88:1379–1406. doi: 10.1152/physrev.90100.2007. [DOI] [PubMed] [Google Scholar]
- 12.Flynn M.G., McFarlin B.K. Toll-like receptor 4: Link to the anti-inflammatory effects of exercise? Exerc. Sport Sci. Rev. 2006;34:176–181. doi: 10.1249/01.jes.0000240027.22749.14. [DOI] [PubMed] [Google Scholar]
- 13.Gleeson M., McFarlin B., Flynn M. Exercise and Toll-like receptors. Exerc. Immunol. Rev. 2006;12:34–53. [PubMed] [Google Scholar]
- 14.Kawanishi N., Yano H., Yokogawa Y., Suzuki K. Exercise training inhibits inflammation in adipose tissue via both suppression of macrophage infiltration and acceleration of phenotypic switching from M1 to M2 macrophages in high-fat-diet-induced obese mice. Exerc. Immunol. Rev. 2010;16:105–118. [PubMed] [Google Scholar]
- 15.Timmerman K.L., Flynn M.G., Coen P.M., Markofski M.M., Pence B.D. Exercise training-induced lowering of inflammatory (CD14+CD16+) monocytes: A role in the anti-inflammatory influence of exercise? J. Leukoc. Biol. 2008;84:1271–1278. doi: 10.1189/jlb.0408244. [DOI] [PubMed] [Google Scholar]
- 16.Plotnikov E.Y., Silachev D.N., Popkov V.A., Zorova L.D., Pevzner I.B., Zorov S.D., Jankauskas S.S., Babenko V.A., Sukhikh G.T., Zorov D.B. Intercellular Signalling Cross-Talk: To Kill, To Heal and To Rejuvenate. Heart. Lung Circ. 2017;26:648–659. doi: 10.1016/j.hlc.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Li Y., Yin P., Guo Z., Lv H., Deng Y., Chen M., Gu Y., Tang P., Zhang L. Bone-Derived Extracellular Vesicles: Novel Players of Interorgan Crosstalk. Front. Endocrinol. 2019;10:846. doi: 10.3389/fendo.2019.00846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raposo G., Stoorvogel W. Extracellular vesicles: Exosomes, microvesicles, and friends. J. Cell Biol. 2013;200:373–383. doi: 10.1083/jcb.201211138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Colombo M., Raposo G., Théry C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu. Rev. Cell Dev. Biol. 2014;30:255–289. doi: 10.1146/annurev-cellbio-101512-122326. [DOI] [PubMed] [Google Scholar]
- 20.Savina A., Furlán M., Vidal M., Colombo M.I. Exosome release is regulated by a calcium-dependent mechanism in K562 cells. J. Biol. Chem. 2003;278:20083–20090. doi: 10.1074/jbc.M301642200. [DOI] [PubMed] [Google Scholar]
- 21.Wilson H.L., Francis S.E., Dower S.K., Crossman D.C. Secretion of intracellular IL-1 receptor antagonist (type 1) is dependent on P2X7 receptor activation. J. Immunol. 2004;173:1202–1208. doi: 10.4049/jimmunol.173.2.1202. [DOI] [PubMed] [Google Scholar]
- 22.Lachenal G., Pernet-Gallay K., Chivet M., Hemming F.J., Belly A., Bodon G., Blot B., Haase G., Goldberg Y., Sadoul R. Release of exosomes from differentiated neurons and its regulation by synaptic glutamatergic activity. Mol. Cell. Neurosci. 2011;46:409–418. doi: 10.1016/j.mcn.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Obregon C., Rothen-Rutishauser B., Gitahi S.K., Gehr P., Nicod L.P. Exovesicles from human activated dendritic cells fuse with resting dendritic cells, allowing them to present alloantigens. Am. J. Pathol. 2006;169:2127–2136. doi: 10.2353/ajpath.2006.060453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nolte-’t Hoen E.N.M., van der Vlist E.J., de Boer-Brouwer M., Arkesteijn G.J.A., Stoorvogel W., Wauben M.H.M. Dynamics of dendritic cell-derived vesicles: High-resolution flow cytometric analysis of extracellular vesicle quantity and quality. J. Leukoc. Biol. 2013;93:395–402. doi: 10.1189/jlb.0911480. [DOI] [PubMed] [Google Scholar]
- 25.Eldh M., Ekström K., Valadi H., Sjöstrand M., Olsson B., Jernås M., Lötvall J. Exosomes communicate protective messages during oxidative stress; possible role of exosomal shuttle RNA. PLoS ONE. 2010;5:e15353. doi: 10.1371/journal.pone.0015353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heijnen H.F., Schiel A.E., Fijnheer R., Geuze H.J., Sixma J.J. Activated platelets release two types of membrane vesicles: Microvesicles by surface shedding and exosomes derived from exocytosis of multivesicular bodies and alpha-granules. Blood. 1999;94:3791–3799. doi: 10.1182/blood.V94.11.3791. [DOI] [PubMed] [Google Scholar]
- 27.Simeone P., Bologna G., Lanuti P., Pierdomenico L., Guagnano M.T., Pieragostino D., Del Boccio P., Vergara D., Marchisio M., Miscia S., et al. Extracellular Vesicles as Signaling Mediators and Disease Biomarkers across Biological Barriers. Int. J. Mol. Sci. 2020;21:2514. doi: 10.3390/ijms21072514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Canonico B., Luchetti F., Arcangeletti M., Guescini M., Degli Esposti M., Papa S. Flow cytometric analyses disclose intercellular communications in FasL-stimulated T cells: Results and trouble shooting. Cytometry. A. 2012;81:5–8. doi: 10.1002/cyto.a.21151. [DOI] [PubMed] [Google Scholar]
- 29.Luchetti F., Canonico B., Arcangeletti M., Guescini M., Cesarini E., Stocchi V., Degli Esposti M., Papa S. Fas signalling promotes intercellular communication in T cells. PLoS ONE. 2012;7:e35766. doi: 10.1371/journal.pone.0035766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Picca A., Guerra F., Calvani R., Bucci C., Lo Monaco M., Bentivoglio A., Coelho-Júnior H., Landi F., Bernabei R., Marzetti E. Mitochondrial Dysfunction and Aging: Insights from the Analysis of Extracellular Vesicles. Int. J. Mol. Sci. 2019;20:805. doi: 10.3390/ijms20040805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lazo S., Noren Hooten N., Green J., Eitan E., Mode N.A., Liu Q., Zonderman A.B., Ezike N., Mattson M.P., Ghosh P., et al. Mitochondrial DNA in extracellular vesicles declines with age. Aging Cell. 2021;20:e13283. doi: 10.1111/acel.13283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cocucci E., Meldolesi J. Ectosomes and exosomes: Shedding the confusion between extracellular vesicles. Trends Cell Biol. 2015;25:364–372. doi: 10.1016/j.tcb.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 33.Théry C., Witwer K.W., Aikawa E., Alcaraz M.J., Anderson J.D., Andriantsitohaina R., Antoniou A., Arab T., Archer F., Atkin-Smith G.K., et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): A position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles. 2018;7:1535750. doi: 10.1080/20013078.2018.1535750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Falasca K., Lanuti P., Ucciferri C., Pieragostino D., Cufaro M.C., Bologna G., Federici L., Miscia S., Pontolillo M., Auricchio A., et al. Circulating extracellular vesicles as new inflammation marker in HIV infection. AIDS. 2021;35:595–604. doi: 10.1097/QAD.0000000000002794. [DOI] [PubMed] [Google Scholar]
- 35.Rossi C., Cicalini I., Cufaro M.C., Agnifili L., Mastropasqua L., Lanuti P., Marchisio M., De Laurenzi V., Del Boccio P., Pieragostino D. Multi-Omics Approach for Studying Tears in Treatment-Naïve Glaucoma Patients. Int. J. Mol. Sci. 2019;20:4029. doi: 10.3390/ijms20164029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brocco D., Lanuti P., Pieragostino D., Cufaro M.C., Simeone P., Bologna G., Di Marino P., De Tursi M., Grassadonia A., Irtelli L., et al. Phenotypic and Proteomic Analysis Identifies Hallmarks of Blood Circulating Extracellular Vesicles in NSCLC Responders to Immune Checkpoint Inhibitors. Cancers. 2021;13:585. doi: 10.3390/cancers13040585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marchisio M., Simeone P., Bologna G., Ercolino E., Pierdomenico L., Pieragostino D., Ventrella A., Antonini F., Del Zotto G., Vergara D., et al. Flow Cytometry Analysis of Circulating Extracellular Vesicle Subtypes from Fresh Peripheral Blood Samples. Int. J. Mol. Sci. 2020;22:48. doi: 10.3390/ijms22010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pieragostino D., Lanzini M., Cicalini I., Cufaro M.C., Damiani V., Mastropasqua L., De Laurenzi V., Nubile M., Lanuti P., Bologna G., et al. Tear proteomics reveals the molecular basis of the efficacy of human recombinant nerve growth factor treatment for Neurotrophic Keratopathy. Sci. Rep. 2022;12:1229. doi: 10.1038/s41598-022-05229-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pieragostino D., Lanuti P., Cicalini I., Cufaro M.C., Ciccocioppo F., Ronci M., Simeone P., Onofrj M., van der Pol E., Fontana A., et al. Proteomics characterization of extracellular vesicles sorted by flow cytometry reveals a disease-specific molecular cross-talk from cerebrospinal fluid and tears in multiple sclerosis. J. Proteomics. 2019;204:103403. doi: 10.1016/j.jprot.2019.103403. [DOI] [PubMed] [Google Scholar]
- 40.Brocco D., Lanuti P., Simeone P., Bologna G., Pieragostino D., Cufaro M.C., Graziano V., Peri M., Di Marino P., De Tursi M., et al. Circulating Cancer Stem Cell-Derived Extracellular Vesicles as a Novel Biomarker for Clinical Outcome Evaluation. J. Oncol. 2019;2019:5879616. doi: 10.1155/2019/5879616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Simeone P., Celia C., Bologna G., Ercolino E., Pierdomenico L., Cilurzo F., Grande R., Diomede F., Vespa S., Canonico B., et al. Diameters and Fluorescence Calibration for Extracellular Vesicle Analyses by Flow Cytometry. Int. J. Mol. Sci. 2020;21:7885. doi: 10.3390/ijms21217885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buca D., D’Antonio F., Buca D., Di Sebastiano F., Simeone P., Di Girolamo R., Bologna G., Vespa S., Catitti G., Liberati M., et al. Extracellular Vesicles in pregnancy: Their potential role as a liquid biopsy. J. Reprod. Immunol. 2022;154:103734. doi: 10.1016/j.jri.2022.103734. [DOI] [PubMed] [Google Scholar]
- 43.Vaidyanathan R., Soon R.H., Zhang P., Jiang K., Lim C.T. Cancer diagnosis: From tumor to liquid biopsy and beyond. Lab Chip. 2018;19:11–34. doi: 10.1039/C8LC00684A. [DOI] [PubMed] [Google Scholar]
- 44.Lucidi A., Buca D., Ronsini C., Tinari S., Bologna G., Buca D., Leombroni M., Liberati M., D’Antonio F., Scambia G., et al. Role of Extracellular Vesicles in Epithelial Ovarian Cancer: A Systematic Review. Int. J. Mol. Sci. 2020;21:8762. doi: 10.3390/ijms21228762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bastos-Amador P., Royo F., Gonzalez E., Conde-Vancells J., Palomo-Diez L., Borras F.E., Falcon-Perez J.M. Proteomic analysis of microvesicles from plasma of healthy donors reveals high individual variability. J. Proteomics. 2012;75:3574–3584. doi: 10.1016/j.jprot.2012.03.054. [DOI] [PubMed] [Google Scholar]
- 46.Yáñez-Mó M., Siljander P.R.-M., Andreu Z., Zavec A.B., Borràs F.E., Buzas E.I., Buzas K., Casal E., Cappello F., Carvalho J., et al. Biological properties of extracellular vesicles and their physiological functions. J. Extracell. Vesicles. 2015;4:27066. doi: 10.3402/jev.v4.27066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pieragostino D., Cicalini I., Lanuti P., Ercolino E., di Ioia M., Zucchelli M., Zappacosta R., Miscia S., Marchisio M., Sacchetta P., et al. Enhanced release of acid sphingomyelinase-enriched exosomes generates a lipidomics signature in CSF of Multiple Sclerosis patients. Sci. Rep. 2018;8:3071. doi: 10.1038/s41598-018-21497-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Isaac R., Reis F.C.G., Ying W., Olefsky J.M. Exosomes as mediators of intercellular crosstalk in metabolism. Cell Metab. 2021;33:1744–1762. doi: 10.1016/j.cmet.2021.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rautiainen S., Laaksonen T., Koivuniemi R. Angiogenic Effects and Crosstalk of Adipose-Derived Mesenchymal Stem/Stromal Cells and Their Extracellular Vesicles with Endothelial Cells. Int. J. Mol. Sci. 2021;22:890. doi: 10.3390/ijms221910890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Krämer-Albers E.-M., Hill A.F. Extracellular vesicles: Interneural shuttles of complex messages. Curr. Opin. Neurobiol. 2016;39:101–107. doi: 10.1016/j.conb.2016.04.016. [DOI] [PubMed] [Google Scholar]
- 51.Karasu E., Eisenhardt S.U., Harant J., Huber-Lang M. Extracellular Vesicles: Packages Sent With Complement. Front. Immunol. 2018;9:721. doi: 10.3389/fimmu.2018.00721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li C.-J., Fang Q.-H., Liu M.-L., Lin J.-N. Current understanding of the role of Adipose-derived Extracellular Vesicles in Metabolic Homeostasis and Diseases: Communication from the distance between cells/tissues. Theranostics. 2020;10:7422–7435. doi: 10.7150/thno.42167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Grieco G.E., Fignani D., Formichi C., Nigi L., Licata G., Maccora C., Brusco N., Sebastiani G., Dotta F. Extracellular Vesicles in Immune System Regulation and Type 1 Diabetes: Cell-to-Cell Communication Mediators, Disease Biomarkers, and Promising Therapeutic Tools. Front. Immunol. 2021;12:682948. doi: 10.3389/fimmu.2021.682948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grande R., Dovizio M., Marcone S., Szklanna P.B., Bruno A., Ebhardt H.A., Cassidy H., Ní Áinle F., Caprodossi A., Lanuti P., et al. Platelet-Derived Microparticles From Obese Individuals: Characterization of Number, Size, Proteomics, and Crosstalk With Cancer and Endothelial Cells. Front. Pharmacol. 2019;10:7. doi: 10.3389/fphar.2019.00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Buzas E.I., The roles of extracellular vesicles in the immune system Nat. Rev. Immunol. 2022. [(accessed on 24 October 2022)]. Available online: https://www.webofscience.com/wos/woscc/full-record/WOS:000836097900001. [DOI] [PMC free article] [PubMed]
- 56.Yang P., Peng Y., Feng Y., Xu Z., Feng P., Cao J., Chen Y., Chen X., Cao X., Yang Y., et al. Immune Cell-Derived Extracellular Vesicles—New Strategies in Cancer Immunotherapy. Front. Immunol. 2021;12:771551. doi: 10.3389/fimmu.2021.771551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liu Y., Gu Y., Cao X. The exosomes in tumor immunity. Oncoimmunology. 2015;4:e1027472. doi: 10.1080/2162402X.2015.1027472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yu X., Huang C., Song B., Xiao Y., Fang M., Feng J., Wang P. CD4+CD25+ regulatory T cells-derived exosomes prolonged kidney allograft survival in a rat model. Cell. Immunol. 2013;285:62–68. doi: 10.1016/j.cellimm.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 59.Okoye I.S., Coomes S.M., Pelly V.S., Czieso S., Papayannopoulos V., Tolmachova T., Seabra M.C., Wilson M.S. MicroRNA-containing T-regulatory-cell-derived exosomes suppress pathogenic T helper 1 cells. Immunity. 2014;41:89–103. doi: 10.1016/j.immuni.2014.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xie F., Zhou X., Fang M., Li H., Su P., Tu Y., Zhang L., Zhou F. Extracellular Vesicles in Cancer Immune Microenvironment and Cancer Immunotherapy. Adv. Sci. (Weinheim, Baden-Wurttemberg, Ger. 2019;6:1901779. doi: 10.1002/advs.201901779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lu J., Wu J., Xie F., Tian J., Tang X., Guo H., Ma J., Xu P., Mao L., Xu H., et al. CD4+ T Cell-Released Extracellular Vesicles Potentiate the Efficacy of the HBsAg Vaccine by Enhancing B Cell Responses. Adv. Sci. 2019;6:1802219. doi: 10.1002/advs.201802219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang X., Shen H., He Q., Tian W., Xia A., Lu X.-J. Exosomes derived from exhausted CD8+ T cells impaired the anticancer function of normal CD8+ T cells. J. Med. Genet. 2019;56:29–31. doi: 10.1136/jmedgenet-2018-105439. [DOI] [PubMed] [Google Scholar]
- 63.Bhatnagar S., Shinagawa K., Castellino F.J., Schorey J.S. Exosomes released from macrophages infected with intracellular pathogens stimulate a proinflammatory response in vitro and in vivo. Blood. 2007;110:3234–3244. doi: 10.1182/blood-2007-03-079152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Monleón I., Martínez-Lorenzo M.J., Monteagudo L., Lasierra P., Taulés M., Iturralde M., Piñeiro A., Larrad L., Alava M.A., Naval J., et al. Differential secretion of Fas ligand- or APO2 ligand/TNF-related apoptosis-inducing ligand-carrying microvesicles during activation-induced death of human T cells. J. Immunol. 2001;167:6736–6744. doi: 10.4049/jimmunol.167.12.6736. [DOI] [PubMed] [Google Scholar]
- 65.Zuccato E., Blott E.J., Holt O., Sigismund S., Shaw M., Bossi G., Griffiths G.M. Sorting of Fas ligand to secretory lysosomes is regulated by mono-ubiquitylation and phosphorylation. J. Cell Sci. 2007;120:191–199. doi: 10.1242/jcs.03315. [DOI] [PubMed] [Google Scholar]
- 66.Munich S., Sobo-Vujanovic A., Buchser W.J., Beer-Stolz D., Vujanovic N.L. Dendritic cell exosomes directly kill tumor cells and activate natural killer cells via TNF superfamily ligands. Oncoimmunology. 2012;1:1074–1083. doi: 10.4161/onci.20897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Esser J., Gehrmann U., D’Alexandri F.L., Hidalgo-Estévez A.M., Wheelock C.E., Scheynius A., Gabrielsson S., Rådmark O. Exosomes from human macrophages and dendritic cells contain enzymes for leukotriene biosynthesis and promote granulocyte migration. J. Allergy Clin. Immunol. 2010;126:1032–1040. doi: 10.1016/j.jaci.2010.06.039. [DOI] [PubMed] [Google Scholar]
- 68.Zhang H.-G., Liu C., Su K., Su K., Yu S., Zhang L., Zhang S., Wang J., Cao X., Grizzle W., et al. A membrane form of TNF-alpha presented by exosomes delays T cell activation-induced cell death. J. Immunol. 2006;176:7385–7393. doi: 10.4049/jimmunol.176.12.7385. [DOI] [PubMed] [Google Scholar]
- 69.Skriner K., Adolph K., Jungblut P.R., Burmester G.R. Association of citrullinated proteins with synovial exosomes. Arthritis Rheum. 2006;54:3809–3814. doi: 10.1002/art.22276. [DOI] [PubMed] [Google Scholar]
- 70.Anderson H.C., Mulhall D., Garimella R. Role of extracellular membrane vesicles in the pathogenesis of various diseases, including cancer, renal diseases, atherosclerosis, and arthritis. Lab. Investig. 2010;90:1549–1557. doi: 10.1038/labinvest.2010.152. [DOI] [PubMed] [Google Scholar]
- 71.Cantaluppi V., Gatti S., Medica D., Figliolini F., Bruno S., Deregibus M.C., Sordi A., Biancone L., Tetta C., Camussi G. Microvesicles derived from endothelial progenitor cells protect the kidney from ischemia-reperfusion injury by microRNA-dependent reprogramming of resident renal cells. Kidney Int. 2012;82:412–427. doi: 10.1038/ki.2012.105. [DOI] [PubMed] [Google Scholar]
- 72.Arslan F., Lai R.C., Smeets M.B., Akeroyd L., Choo A., Aguor E.N.E., Timmers L., van Rijen H.V., Doevendans P.A., Pasterkamp G., et al. Mesenchymal stem cell-derived exosomes increase ATP levels, decrease oxidative stress and activate PI3K/Akt pathway to enhance myocardial viability and prevent adverse remodeling after myocardial ischemia/reperfusion injury. Stem Cell Res. 2013;10:301–312. doi: 10.1016/j.scr.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 73.Hu S., Xing H., Zhang J., Zhu Z., Yin Y., Zhang N., Qi Y. Mesenchymal Stem Cell-Derived Extracellular Vesicles: Immunomodulatory Effects and Potential Applications in Intervertebral Disc Degeneration. Stem Cells Int. 2022;2022:7538025. doi: 10.1155/2022/7538025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.She Z., Xie M., Hun M., Abdirahman A.S., Li C., Wu F., Luo S., Wan W., Wen C., Tian J. Immunoregulatory Effects of Mitochondria Transferred by Extracellular Vesicles. Front. Immunol. 2020;11:628576. doi: 10.3389/fimmu.2020.628576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wolfers J., Lozier A., Raposo G., Regnault A., Théry C., Masurier C., Flament C., Pouzieux S., Faure F., Tursz T., et al. Tumor-derived exosomes are a source of shared tumor rejection antigens for CTL cross-priming. Nat. Med. 2001;7:297–303. doi: 10.1038/85438. [DOI] [PubMed] [Google Scholar]
- 76.Andre F., Schartz N.E.C., Movassagh M., Flament C., Pautier P., Morice P., Pomel C., Lhomme C., Escudier B., Le Chevalier T., et al. Malignant effusions and immunogenic tumour-derived exosomes. Lancet (London, England) 2002;360:295–305. doi: 10.1016/S0140-6736(02)09552-1. [DOI] [PubMed] [Google Scholar]
- 77.Alpegiani M., Bedeschi A., Zarini F., Della Bruna C., Jabes D., Perrone E., Franceschi G. Synthesis and biological properties of FCE 25199, a new oral penem. J. Antibiot. 1992;45:797–801. doi: 10.7164/antibiotics.45.797. [DOI] [PubMed] [Google Scholar]
- 78.Taylor D.D., Gerçel-Taylor C., Lyons K.S., Stanson J., Whiteside T.L. T-cell apoptosis and suppression of T-cell receptor/CD3-zeta by Fas ligand-containing membrane vesicles shed from ovarian tumors. Clin. Cancer Res. 2003;9:5113–5119. [PubMed] [Google Scholar]
- 79.Valenti R., Huber V., Filipazzi P., Pilla L., Sovena G., Villa A., Corbelli A., Fais S., Parmiani G., Rivoltini L. Human tumor-released microvesicles promote the differentiation of myeloid cells with transforming growth factor-beta-mediated suppressive activity on T lymphocytes. Cancer Res. 2006;66:9290–9298. doi: 10.1158/0008-5472.CAN-06-1819. [DOI] [PubMed] [Google Scholar]
- 80.Xiang X., Liu Y., Zhuang X., Zhang S., Michalek S., Taylor D.D., Grizzle W., Zhang H.-G. TLR2-mediated expansion of MDSCs is dependent on the source of tumor exosomes. Am. J. Pathol. 2010;177:1606–1610. doi: 10.2353/ajpath.2010.100245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chalmin F., Ladoire S., Mignot G., Vincent J., Bruchard M., Remy-Martin J.-P., Boireau W., Rouleau A., Simon B., Lanneau D., et al. Membrane-associated Hsp72 from tumor-derived exosomes mediates STAT3-dependent immunosuppressive function of mouse and human myeloid-derived suppressor cells. J. Clin. Investig. 2010;120:457–471. doi: 10.1172/JCI40483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Liu Y., Xiang X., Zhuang X., Zhang S., Liu C., Cheng Z., Michalek S., Grizzle W., Zhang H.-G. Contribution of MyD88 to the tumor exosome-mediated induction of myeloid derived suppressor cells. Am. J. Pathol. 2010;176:2490–2499. doi: 10.2353/ajpath.2010.090777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Guo D., Chen Y., Wang S., Yu L., Shen Y., Zhong H., Yang Y. Exosomes from heat-stressed tumour cells inhibit tumour growth by converting regulatory T cells to Th17 cells via IL-6. Immunology. 2018;154:132–143. doi: 10.1111/imm.12874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hussain M.T., Iqbal A.J., Norling L.V. The Role and Impact of Extracellular Vesicles in the Modulation and Delivery of Cytokines during Autoimmunity. Int. J. Mol. Sci. 2020;21:7096. doi: 10.3390/ijms21197096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Egan B., Zierath J.R. Exercise metabolism and the molecular regulation of skeletal muscle adaptation. Cell Metab. 2013;17:162–184. doi: 10.1016/j.cmet.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 86.Walsh N.P., Gleeson M., Pyne D.B., Nieman D.C., Dhabhar F.S., Shephard R.J., Oliver S.J., Bermon S., Kajeniene A. Position statement. Part two: Maintaining immune health. Exerc. Immunol. Rev. 2011;17:64–103. [PubMed] [Google Scholar]
- 87.Breitbach S., Tug S., Simon P. Circulating cell-free DNA: An up-coming molecular marker in exercise physiology. Sports Med. 2012;42:565–586. doi: 10.2165/11631380-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 88.Kyu H.H., Bachman V.F., Alexander L.T., Mumford J.E., Afshin A., Estep K., Veerman J.L., Delwiche K., Iannarone M.L., Moyer M.L., et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: Systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ. 2016;354:i3857. doi: 10.1136/bmj.i3857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Brahmer A., Neuberger E., Esch-Heisser L., Haller N., Jorgensen M.M., Baek R., Möbius W., Simon P., Krämer-Albers E.-M. Platelets, endothelial cells and leukocytes contribute to the exercise-triggered release of extracellular vesicles into the circulation. J. Extracell. Vesicles. 2019;8:1615820. doi: 10.1080/20013078.2019.1615820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Frühbeis C., Helmig S., Tug S., Simon P., Krämer-Albers E.-M. Physical exercise induces rapid release of small extracellular vesicles into the circulation. J. Extracell. Vesicles. 2015;4:28239. doi: 10.3402/jev.v4.28239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Oliveira G.P., Porto W.F., Palu C.C., Pereira L.M., Petriz B., Almeida J.A., Viana J., Filho N.N.A., Franco O.L., Pereira R.W. Effects of Acute Aerobic Exercise on Rats Serum Extracellular Vesicles Diameter, Concentration and Small RNAs Content. Front. Physiol. 2018;9:532. doi: 10.3389/fphys.2018.00532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bertoldi K., Cechinel L.R., Schallenberger B., Corssac G.B., Davies S., Guerreiro I.C.K., Belló-Klein A., Araujo A.S.R., Siqueira I.R. Circulating extracellular vesicles in the aging process: Impact of aerobic exercise. Mol. Cell. Biochem. 2018;440:115–125. doi: 10.1007/s11010-017-3160-4. [DOI] [PubMed] [Google Scholar]
- 93.Bei Y., Xu T., Lv D., Yu P., Xu J., Che L., Das A., Tigges J., Toxavidis V., Ghiran I., et al. Exercise-induced circulating extracellular vesicles protect against cardiac ischemia-reperfusion injury. Basic Res. Cardiol. 2017;112:38. doi: 10.1007/s00395-017-0628-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lässer C., Eldh M., Lötvall J. Isolation and characterization of RNA-containing exosomes. J. Vis. Exp. 2012;59:e3037. doi: 10.3791/3037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Whitham M., Parker B.L., Friedrichsen M., Hingst J.R., Hjorth M., Hughes W.E., Egan C.L., Cron L., Watt K.I., Kuchel R.P., et al. Extracellular Vesicles Provide a Means for Tissue Crosstalk during Exercise. Cell Metab. 2018;27:237–251. doi: 10.1016/j.cmet.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 96.Febbraio M.A., Pedersen B.K. Contraction-induced myokine production and release: Is skeletal muscle an endocrine organ? Exerc. Sport Sci. Rev. 2005;33:114–119. doi: 10.1097/00003677-200507000-00003. [DOI] [PubMed] [Google Scholar]
- 97.Eckardt K., Görgens S.W., Raschke S., Eckel J. Myokines in insulin resistance and type 2 diabetes. Diabetologia. 2014;57:1087–1099. doi: 10.1007/s00125-014-3224-x. [DOI] [PubMed] [Google Scholar]
- 98.O’Leary M.F., Wallace G.R., Bennett A.J., Tsintzas K., Jones S.W. IL-15 promotes human myogenesis and mitigates the detrimental effects of TNFα on myotube development. Sci. Rep. 2017;7:12997. doi: 10.1038/s41598-017-13479-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sossdorf M., Otto G.P., Claus R.A., Gabriel H.H.W., Lösche W. Cell-derived microparticles promote coagulation after moderate exercise. Med. Sci. Sports Exerc. 2011;43:1169–1176. doi: 10.1249/MSS.0b013e3182068645. [DOI] [PubMed] [Google Scholar]
- 100.Laterza O.F., Lim L., Garrett-Engele P.W., Vlasakova K., Muniappa N., Tanaka W.K., Johnson J.M., Sina J.F., Fare T.L., Sistare F.D., et al. Plasma MicroRNAs as sensitive and specific biomarkers of tissue injury. Clin. Chem. 2009;55:1977–1983. doi: 10.1373/clinchem.2009.131797. [DOI] [PubMed] [Google Scholar]
- 101.Maruyama K., Kadono T., Morishita E. Plasma levels of platelet-derived microparticles are increased after anaerobic exercise in healthy subjects. J. Atheroscler. Thromb. 2012;19:585–587. doi: 10.5551/jat.11791. [DOI] [PubMed] [Google Scholar]
- 102.Lundberg T.R., Fernandez-Gonzalo R., Tesch P.A., Rullman E., Gustafsson T. Aerobic exercise augments muscle transcriptome profile of resistance exercise. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2016;310:R1279-87. doi: 10.1152/ajpregu.00035.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mach N., Plancade S., Pacholewska A., Lecardonnel J., Rivière J., Moroldo M., Vaiman A., Morgenthaler C., Beinat M., Nevot A., et al. Integrated mRNA and miRNA expression profiling in blood reveals candidate biomarkers associated with endurance exercise in the horse. Sci. Rep. 2016;6:22932. doi: 10.1038/srep22932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chen Y.-W., Chen Y.-C., Wang J.-S. Absolute hypoxic exercise training enhances in vitro thrombin generation by increasing procoagulant platelet-derived microparticles under high shear stress in sedentary men. Clin. Sci. 2013;124:639–649. doi: 10.1042/CS20120540. [DOI] [PubMed] [Google Scholar]
- 105.Chen Y.-W., Chen J.-K., Wang J.-S. Strenuous exercise promotes shear-induced thrombin generation by increasing the shedding of procoagulant microparticles from platelets. Thromb. Haemost. 2010;104:293–301. doi: 10.1160/TH09-09-0633. [DOI] [PubMed] [Google Scholar]
- 106.Chaar V., Romana M., Tripette J., Broquere C., Huisse M.-G., Hue O., Hardy-Dessources M.-D., Connes P. Effect of strenuous physical exercise on circulating cell-derived microparticles. Clin. Hemorheol. Microcirc. 2011;47:15–25. doi: 10.3233/CH-2010-1361. [DOI] [PubMed] [Google Scholar]
- 107.Sossdorf M., Otto G.P., Claus R.A., Gabriel H.H., Lösche W. Release of pro-coagulant microparticles after moderate endurance exercise. Platelets. 2010;21:389–391. doi: 10.3109/09537101003698564. [DOI] [PubMed] [Google Scholar]
- 108.MacPherson R.E.K., Baumeister P., Peppler W.T., Wright D.C., Little J.P. Reduced cortical BACE1 content with one bout of exercise is accompanied by declines in AMPK, Akt, and MAPK signaling in obese, glucose-intolerant mice. J. Appl. Physiol. 2015;119:1097–1104. doi: 10.1152/japplphysiol.00299.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mi Y., Guo N., He T., Ji J., Li Z., Huang P. miR-410 enhanced hESC-derived pancreatic endoderm transplant to alleviate gestational diabetes mellitus. J. Mol. Endocrinol. 2015;55:219–229. doi: 10.1530/JME-15-0100. [DOI] [PubMed] [Google Scholar]
- 110.Guescini M., Canonico B., Lucertini F., Maggio S., Annibalini G., Barbieri E., Luchetti F., Papa S., Stocchi V. Muscle Releases Alpha-Sarcoglycan Positive Extracellular Vesicles Carrying miRNAs in the Bloodstream. PLoS ONE. 2015;10:e0125094. doi: 10.1371/journal.pone.0125094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Rome S., Forterre A., Mizgier M.L., Bouzakri K. Skeletal Muscle-Released Extracellular Vesicles: State of the Art. Front. Physiol. 2019;10:929. doi: 10.3389/fphys.2019.00929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Estrada A.L., Valenti Z.J., Hehn G., Amorese A.J., Williams N.S., Balestrieri N.P., Deighan C., Allen C.P., Spangenburg E.E., Kruh-Garcia N.A., et al. Extracellular vesicle secretion is tissue-dependent ex vivo and skeletal muscle myofiber extracellular vesicles reach the circulation in vivo. Am. J. Physiol. Cell Physiol. 2022;322:C246–C259. doi: 10.1152/ajpcell.00580.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Vanderboom P.M., Dasari S., Ruegsegger G.N., Pataky M.W., Lucien F., Heppelmann C.J., Lanza I.R., Nair K.S. A size-exclusion-based approach for purifying extracellular vesicles from human plasma. Cell Rep. Methods. 2021;1:100055. doi: 10.1016/j.crmeth.2021.100055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Vechetti I.J., Peck B.D., Wen Y., Walton R.G., Valentino T.R., Alimov A.P., Dungan C.M., Van Pelt D.W., von Walden F., Alkner B., et al. Mechanical overload-induced muscle-derived extracellular vesicles promote adipose tissue lipolysis. FASEB J. 2021;35:e21644. doi: 10.1096/fj.202100242R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Gao L., Wang H.-J., Tian C., Zucker I.H. Skeletal Muscle Nrf2 Contributes to Exercise-Evoked Systemic Antioxidant Defense Via Extracellular Vesicular Communication. Exerc. Sport Sci. Rev. 2021;49:213–222. doi: 10.1249/JES.0000000000000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jalabert A., Vial G., Guay C., Wiklander O.P.B., Nordin J.Z., Aswad H., Forterre A., Meugnier E., Pesenti S., Regazzi R., et al. Exosome-like vesicles released from lipid-induced insulin-resistant muscles modulate gene expression and proliferation of beta recipient cells in mice. Diabetologia. 2016;59:1049–1058. doi: 10.1007/s00125-016-3882-y. [DOI] [PubMed] [Google Scholar]
- 117.Pietrangelo T., Bondi D., Kinel E., Verratti V. The Bottom-Up Rise Strength Transfer in Elderly After Endurance and Resistance Training: The BURST. Front. Physiol. 2018;9:1944. doi: 10.3389/fphys.2018.01944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bittel A.J., Bittel D.C., Mittendorfer B., Patterson B.W., Okunade A.L., Yoshino J., Porter L.C., Abumrad N.A., Reeds D.N., Cade W.T. A single bout of resistance exercise improves postprandial lipid metabolism in overweight/obese men with prediabetes. Diabetologia. 2020;63:611–623. doi: 10.1007/s00125-019-05070-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Nie Y., Sato Y., Garner R.T., Kargl C., Wang C., Kuang S., Gilpin C.J., Gavin T.P. Skeletal muscle-derived exosomes regulate endothelial cell functions via reactive oxygen species-activated nuclear factor-κB signalling. Exp. Physiol. 2019;104:1262–1273. doi: 10.1113/EP087396. [DOI] [PubMed] [Google Scholar]
- 120.Lou J., Wu J., Feng M., Dang X., Wu G., Yang H., Wang Y., Li J., Zhao Y., Shi C., et al. Exercise promotes angiogenesis by enhancing endothelial cell fatty acid utilization via liver-derived extracellular vesicle miR-122-5p. J. Sport Health Sci. 2022;11:495–508. doi: 10.1016/j.jshs.2021.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Rhys H.I., Dell’Accio F., Pitzalis C., Moore A., Norling L.V., Perretti M. Neutrophil Microvesicles from Healthy Control and Rheumatoid Arthritis Patients Prevent the Inflammatory Activation of Macrophages. EBioMedicine. 2018;29:60–69. doi: 10.1016/j.ebiom.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Headland S.E., Jones H.R., Norling L.V., Kim A., Souza P.R., Corsiero E., Gil C.D., Nerviani A., Dell’Accio F., Pitzalis C., et al. Neutrophil-derived microvesicles enter cartilage and protect the joint in inflammatory arthritis. Sci. Transl. Med. 2015;7:315ra190. doi: 10.1126/scitranslmed.aac5608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lai N., Wu D., Liang T., Pan P., Yuan G., Li X., Li H., Shen H., Wang Z., Chen G. Systemic exosomal miR-193b-3p delivery attenuates neuroinflammation in early brain injury after subarachnoid hemorrhage in mice. J. Neuroinflamm. 2020;17:74. doi: 10.1186/s12974-020-01745-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Luo P., Jiang C., Ji P., Wang M., Xu J. Exosomes of stem cells from human exfoliated deciduous teeth as an anti-inflammatory agent in temporomandibular joint chondrocytes via miR-100-5p/mTOR. Stem Cell Res. Ther. 2019;10:216. doi: 10.1186/s13287-019-1341-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Sullivan B.P., Nie Y., Evans S., Kargl C.K., Hettinger Z.R., Garner R.T., Hubal M.J., Kuang S., Stout J., Gavin T.P. Obesity and exercise training alter inflammatory pathway skeletal muscle small extracellular vesicle microRNAs. Exp. Physiol. 2022;107:462–475. doi: 10.1113/EP090062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Festa A., D’Agostino R., Howard G., Mykkänen L., Tracy R.P., Haffner S.M. Chronic subclinical inflammation as part of the insulin resistance syndrome: The Insulin Resistance Atherosclerosis Study (IRAS) Circulation. 2000;102:42–47. doi: 10.1161/01.CIR.102.1.42. [DOI] [PubMed] [Google Scholar]
- 127.Pedersen B.K., Fischer C.P. Beneficial health effects of exercise—The role of IL-6 as a myokine. Trends Pharmacol. Sci. 2007;28:152–156. doi: 10.1016/j.tips.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 128.Docherty S., Harley R., McAuley J.J., Crowe L.A.N., Pedret C., Kirwan P.D., Siebert S., Millar N.L. The effect of exercise on cytokines: Implications for musculoskeletal health: A narrative review. BMC Sport. Sci. Med. Rehabil. 2022;14:5. doi: 10.1186/s13102-022-00397-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Safdar A., Saleem A., Tarnopolsky M.A. The potential of endurance exercise-derived exosomes to treat metabolic diseases. Nat. Rev. Endocrinol. 2016;12:504–517. doi: 10.1038/nrendo.2016.76. [DOI] [PubMed] [Google Scholar]
- 130.Rao R.R., Long J.Z., White J.P., Svensson K.J., Lou J., Lokurkar I., Jedrychowski M.P., Ruas J.L., Wrann C.D., Lo J.C., et al. Meteorin-like is a hormone that regulates immune-adipose interactions to increase beige fat thermogenesis. Cell. 2014;157:1279–1291. doi: 10.1016/j.cell.2014.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Barcellos N., Cechinel L.R., de Meireles L.C.F., Lovatel G.A., Bruch G.E., Carregal V.M., Massensini A.R., Dalla Costa T., Pereira L.O., Siqueira I.R. Effects of exercise modalities on BDNF and IL-1β content in circulating total extracellular vesicles and particles obtained from aged rats. Exp. Gerontol. 2020;142:111124. doi: 10.1016/j.exger.2020.111124. [DOI] [PubMed] [Google Scholar]
- 132.Kinney J.W., Bemiller S.M., Murtishaw A.S., Leisgang A.M., Salazar A.M., Lamb B.T. Inflammation as a central mechanism in Alzheimer’s disease. Alzheimer’s Dement. 2018;4:575–590. doi: 10.1016/j.trci.2018.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wood H. Dementia: Peripheral inflammation could be a prodromal indicator of dementia. Nat. Rev. Neurol. 2018;14:127. doi: 10.1038/nrneurol.2018.8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.