Abstract
Background: Knee osteoarthritis (OA) is a common musculoskeletal disorder that is associated with balance impairment. Recent studies have used balance exercises for improvement of balance and functional performance among knee OA patients. The purpose of this study was analyzing the effects of balance training in patients with knee OA.
Methods: This review included clinical trials in which the effect of balance training on functional measures was assessed compared to other physiotherapy interventions or control groups in patients with knee OA. To this aim, Electronic databases (PubMed, SCOPUS, EMBASE, PEDro, CINAHL, and WOS) were searched from 1 January 1990 to 30 June 2021. Two independent reviewers selected the studies, extracted the data, and assessed the quality of the studies.
Results: Fifteen articles of clinical trials were eligible to include in this review. Most studies used patient-reported outcome measures, and some studies used performance-based functional outcome measures for the evaluation of functional outcomes. The findings of studies showed that physical function in knee OA patients could have clinical improvements significantly after receiving balance training. However, studies assessing the effect of balance training on muscle strength of the quadriceps and the hamstring had conflicting results. Also, the finding of studies showed that more significant improvement in postural stability and balance in the balance training group rather than the control group.
Conclusion: The results of the current systematic review demonstrate balance exercises significantly improve balance and functionality in knee OA patients. However, the effect of balance training on muscle strength was not clearly revealed due to few studies.
Keywords: Balance Training, Knee Osteoarthritis, Functional Measures, Balance, Muscle Strength, Range of Motion
Introduction
↑What is “already known” in this topic:
People with knee OA often experience increased balance impairment due to a possible decrease in muscle strength and joint position sense. Recent studies have shown that balance training improves patients' balance and functional performance. However, there is controversy on the effect of balance training on functional measures in these patients.
→What this article adds:
The results of this study showed that a rehabilitation program with an emphasis on balance exercises significantly improves balance and functionality in knee OA patients. However, the current evidence may be confirmed or discarded by further research with carefully adopted study designs.
Knee osteoarthritis (OA) is a common disabling condition that is known as the main cause of disability among the elderly in developed countries (1). People with knee OA often experience increased balance impairment due to a possible decrease in m uscle strength and joint position sense (2). Such physical impairments lead to decreased functional activities such as diminished ability to walk and increased risk of falling in knee OA patients compared with healthy peers (3-5). In addition, falling in the elderly with knee OA may lead to fear of movement, serious injuries and even death, which could impose enormous financial costs on the health system (6). Therefore, treatment programs that reduce the risk of falling by improving balance impairments are essential to achieving optimal results of rehabilitation programs (7).
In previous studies, the benefits of routine physiotherapy exercises such as range of motion, stretching, strengthening, and endurance training exercises on reducing pain and improving patients' functional performance have been identified (8-10). Recent works, however, have used exercises that intensify the sensory systems to improve balance and reported improved patients' balance and functional performance. These studies compared the experimental groups (i.e., with balance exercises) for several weeks and the control groups (i.e., with no particular emphasis on balance training) (3,11-14). Overall, the results have shown that rehabilitation programs for patients with knee OA, including balance exercises or programs emphasizing the sensory-motor system training, will improve functional performance and specific balance outcomes. While these findings have important clinical applications for the development of an effective rehabilitation program for knee OA patients, the considerable differences in the methodological designs of these studies have made the comprehensive interpretation complicated.
The main differences identified in the methodological designs include the type of outcome measures, statistical design, and duration of the exercise program (3,11-14). A new meta-analysis study has examined the effect of proprioception training on pain, joint stiffness, and functional outcomes in knee OA patients (15), but so far, no systematic review has been conducted on the effect of balance training in subjects with knee OA. Therefore, there is a clear need for a systematic review to assess the effect of balance exercises among patients suffering from knee OA to make a clinical comparison and critical evaluation of these studies. Hence, the purposes of this systematic review are; (1) to systematically and critically evaluate the studies that assessed the effects of balance training compared to the control group on patient-reported and performance-based functional outcomes in knee OA patients, and (2) to systematically and critically examine the studies which measured the effect of balance training on outcomes of pain, quadriceps and hamstring muscle strength, postural stability and balance disturbance, knee range of motion in patients with knee OA compared to control group.
Methods
This systematic review process followed the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement (16). The protocol of this systematic review has been registered in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42021250302).
Eligibility criteria
Clinical trials with a concurrent comparison group(s) in which the effect of balance training or sensorimotor training or neuromuscular training was compared to other physiotherapy interventions and placebo or control group in patients with knee OA were eligible to be included in the review. Our review also included studies addressing knee OA patients aged equal to or more than 50 years, with a history of chronic knee OA and OA grade 3 or lower according to the Kellgren and Lawrence plain radiograph classification. The studies that examined patients with rheumatologic disease (i.e., RA), intra-articular knee joint fractures, and those who underwent total knee arthroplasty, were excluded.
Moreover, studies in which the following validated outcome measures were used for the assessment of functional outcomes were also considered: Western Ontario and McMaster Universities Arthritis Index (WOMAC), Knee injury and osteoarthritis outcome score (KOOS), International Knee Documentation Committee [IKDC] Knee Forms, Tegner activity scale, and Short Form-36 Health Survey. Also included in the review were studies assessing function based on tests such as the timed get-up-and-go, timed stair ascent, Berg Balance Scale, walking-speed timed test [WST], get-up-and-go [GUAG] test, chair stand test, or the sixty-meter walk test in knee OA were also considered.
Outcomes of pain, quadriceps, and hamstring muscle strength, postural stability and balance disturbance (Biodex stability system, force plate, etc.), and knee range of motion were also included as secondary outcomes.
Results obtained from theses/dissertations, conference proceedings, abstracts, narrative reviews, case reports, book chapters, and websites were excluded.
Information Sources and Search Strategy
Our review included studies published in English from 1 January 1990 to 30 June 2021. The search was conducted on the following databases: PubMed/MEDLINE, Scopus, Embase, Physiotherapy Evidence Database (PEDro), Web of Science (WOS), CINAHL, Cochrane Central Register of Controlled Clinical Trials (CENTRAL). Unpublished and gray literature was sought in ProQuest, Google Scholar, and World Wide Science. In order to find more related works, the reference lists of selected studies were reviewed.
Study selection
A quantitative data extraction form was developed by two reviewers based on eligible studies. The data extraction was performed independently by the two reviewers (KHK, FR), and a third reviewer (NP) was invited for discussion in case of any disagreements between the two reviewers.
The extracted data included the first author’s name, publication date, study design, sample size, length of follow-up, demographic information of samples (age, gender and body mass index [BMI] or body weight), intervention and comparator details (sample size for each treatment group, blinding, type, frequency and duration of the exercise programs, withdrawals and drop-outs), the outcome measures, and the conclusions.
Assessment of methodological quality
Two reviewers (NP, NM) independently assessed methodological quality based on PEDro scale, which is a standardized critical appraisal instrument. Disagreements were resolved either by discussion or by inviting a third reviewer (MJSH).
PEDro includes 11 appraisal items that are exclusively designed for assessing the quality of RCTs. Answers to each item include yes or no. Items 2-9 of this scale are dedicated to the internal validity of the study, while sufficient statistical information to enable appropriate interpretation of the results is evaluated in items 10 and 11 (17). Since Item 1 addresses the external validity (i.e., ‘generalizability’ or ‘applicability’) of the trial, it is not included in the total PEDro score. Studies obtaining scores more than 6 on this scale are regarded as ‘high quality’, those with a score of 4 or 5 as ‘fair quality’, and studies below 3 as ‘poor quality’ (18).
Data synthesis
In the first stage, PEDro scale was used for a critical appraisal of the methodological quality of the studies included (Table 1). The next stage involved a descriptive review of studies using balance training, perturbation/agility training, or sensorimotor training in patients with knee OA (Table 2). To this aim, two reviewers (KHK and FR) independently analyzed all data extracted from the studies. A third reviewer (NP) was invited to resolve any disagreements.
Table 1. PEDro Scale for quality assessment of included studies .
| Study | Dıracoglu | Tsauo | Chaipinyo | Fitzgerald | Rogers | Rogers | Apparao | Ghosh | Takacs | Jahantigh | Gomiero | Pazit | Bhaskar | Jahanjoo | Elsheikh |
| PEDro criteria | 2005 | 2008 | 2009 | 2011 | 2011 | 2012 | 2015 | 2015 | 2017 | 2018 | 2018 | 2018 | 2019 | 2019 | 2020 |
| Eligibility criteria | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Random allocation | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Concealed allocation | No | No | Yes | Yes | No | No | No | No | Yes | No | Yes | Yes | No | No | No |
| Baseline comparability | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Yes |
| blinding of all subjects | No | No | Yes | No | No | Yes | No | No | No | Yes | No | No | No | No | No |
| blinding of all therapists | No | No | No | No | No | No | No | No | No | No | No | Yes | No | No | No |
| blinding of all assessors | Yes | Yes | Yes | Yes | No | No | No | No | Yes | No | Yes | No | No | Yes | No |
| Adequate follow-up (C85 %) | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Intention-to-treat analysis | No | Yes | No | Yes | No | Yes | No | No | Yes | No | Yes | Yes | No | No | No |
| Between-group analysis | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Point estimates and variability | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Total score | 7 | 7 | 8 | 8 | 5 | 7 | 5 | 1 | 8 | 5 | 8 | 8 | 4 | 6 | 5 |
Table 2. Summary of included studies .
| Study (Author, year) |
Sample size (n) | Participant characteristics Gender (m/f), Age (years) |
Study design | Intervention, Control | Dose | Evaluated outcomes | Follow-up periods (Weeks) |
Main conclusion | |
| Elsheikh 2020 |
60Mild or moderate knee OA |
50-70 y Strength exercise group: m/f: 9/21 25.367±1.45 y Biodex stability system exercise and strength exercise group: m/f: 8/22 24.967±1.65 y |
Randomized trials | Strength exercise group(Group I) Biodex stability system exercise and strength exercise group(Group II) |
12 weeks, three session a week balance training protocol consisted of: Postural Stability Training, Limit of Stability Training, Weight Shift Training, Maze Control Training, The Random Control Training, Percent Weight-Bearing Training for 20 min. Strength and stretch protocol: Leg raise, Hamstring stretch, Half-squat, One-leg dip and leg stretch With a 2.5 kg up to 5 kg and10 repetitions. |
Pain by VAS, Tenderness by Ritchie's scale, morning stiffness, range of motion, physical performance by chair stand test, functional assessment by WOMAC, assessment of postural stability and balance disturbance by postural stability test- fall risk test- limits of stability test |
6 and 12 weeks | Combined therapy of strength exercises rehabilitation program and training program of balance by Biodex stability system have more potential effects in treatment of mild and moderate knee OA greater than strength exercises rehabilitation program only. |
|
| Jahanjoo 2019 |
60 Mild or moderate knee OA |
50-70 y Routine Physical therapy group: m/f: 5/25 55.57 ± 1.6 y Balance training group: m/f: 8/22 57.53 ± 0.8 y |
Single blind RCT | Balance training group Routine Physical therapy group |
5 weeks, twice a week one-hour treatment with routine physical therapy: 20 min hot pack, 10 min US 1MHz,1.5 w/cm2 20 min TENS 60-100 HZ, 60 msec pulse duration and 10 min quadriceps setting exercise. 1-hour Balance training: postural stability, limits of stability and weight shift using the Biodex Balance System-after 0.5 hour break of routine physical therapy. |
Pain by VAS, , Knee pain, stiffness and functional disability level by WOMAC, Functional status by Lequesne questionnaire, Mobility via Time Up and Go, and Fall risk by Biodex Balance System |
- |
The combination of balance training and physical therapy yielded more pain relief and development of functional abilities in patients with knee OA. |
|
| Bhaskar 2019 |
30 knee OA With Grade 3 Kellageren and Lawernce Scale |
50-65 y Control group: m/f: 8/7 55.87 ± 2.10 y Perturbation group: m/f: 8/7 55.53 ± 2.59 y |
RCT | Control group, Perturbation training group | 14 sessions Conventional exercises: 10 min US, 2 sets with 10 repetitions Knee flexion and extension, Quadriceps and Hamstring strength, SLR, Stretching exercise Perturbation exercises: 2-3 sets, 1 min each Rocker board (A/P, M/L), Roller board bilaterally (A/P, M/L, diagonal, rotational), 2-3 sets, 30 sec-1min Roller board (A/P, M/L, diagonal, rotational). |
Balance by Time Up and Go, Function by Functional reach test score | - | Perturbation training given with conventional treatment was found to provide a significantly better effect in improving the function of the lower extremity in OA knee subjects. |
|
| Jahantigh 2018 |
26 Female with Grade 1-4 knee OA according to Kellageren and Lawernce Scale |
Balance exercise group: 49.20 ± 8.80 y Control group: 51.93 ± 6.64 y |
Single-blind RCT | Balance exercise group Electrotherapy and strength exercise Control group |
3 weeks, 5 times a week (Balance exercises: 2 min single leg standing, stepping in forward, backward, and sides with 30 repetitions, 20 min Strength exercise: 3 sets with 10 repetitions, Electrotherapy: 25 min TENS 100 HZ and US 1MHZ, 0.8 W/cm2) |
Knee instability via a questionnaire, and knee pain by VAS. |
- | The balance exercises resulted in improvement in self-reported knee joint instability score compared to control group. |
|
| Gomiero 2018 |
64 Knee OA With Grade < 4 Kellageren and Lawernce Scale |
Sensory-motor training group: m/f: 2/30 61.6 ± 6.8 y Resistance training group: m/f: 1/31 61.8 ± 6.4 y |
Single blind RCT |
Sensory-motor training group and Resistance training group No Control group |
16 weeks, twice a week. Sensory-motor training: walking in different directions following verbal commands, crossing steps while walking; crossing steps while walking backwards, walking on several types of surfaces, maintaining posture during use of a balance board; and using a mini-trampoline to expose individuals to potentially destabilizing loads. Resistance exercises: quadriceps and hamstring strengthening exercises using ankle weights, isometric exercises for the quadriceps muscle (hip flexion with leg extended). |
Primary: Pain with VAS, Mobility by Time up and Go, and QOL by SF-36. Secondary: Isometric quadriceps femoris force by dynamometer, Balance via Tinetti balance scale, and Functional capacity by WOMAC questionnaire. |
- | Resistance training and sensory motor training for the lower limbs among patients with knee osteoarthritis appeared to present similar effects on pain and function. |
|
| Pazit 2018 |
28 Knee OA | 60-90 y Control group: m/f: 4/5 70.44 ± 7.83 y High speed resistance training group: m/f: 5/4 67.78 ± 6.28 y High speed resistance training plus balance exercises group: m/f: 4/6 65.10 ± 4.77 y |
Pilot RCT | Control group, High speed resistance training, High speed resistance training plus balance exercises |
8 weeks, twice a week High speed resistance exercises: leg press, sit to stand, squat, step-up, calf raises lunges, going up stairs (7-10 repetitions), Balance exercises: Walking forward and backward, single leg standing, single leg tapping, side stepping and backward walking. |
Primary: Feasibility and safety by adherence, drop-out rate, adverse events, pain during and post-exercise. Secondary: strength by The 30s chair stand test, Physical function by Time Up and Go, pain by numerical rating scale and WOMAC, balance by The Four Square Step Test, muscle power by The Timed Stair Climb Test, Postural sway by Swaymeter, Knee proprioception by legs positions matching with closed eye, executive function with cognitive tests-Trail Making Test, Digit Span from The Wechsler Adult Intelligence Scale-III, Stroop Color and Word Test Victoria Version, Physical activity level by Incidental and Planned Exercise Questionnaire, Fear of fall by Falls Efficacy Scale & QOL. |
- | Both exercise groups were feasible and safe and improved physical function and strengthwith overall pain reduction. |
|
| Takacs 2017 |
40 knee OA With Grade ≥ 2 Kellageren and Lawernce Scale |
50-80 y Partially-supervised Exercise group: m/f: 1/19 66.1 ± 8.7 y Control group: m/f: 7/13 67.1 ± 5.4 y |
Single-blind RCT | Partially-supervised Exercise group No intervention Control group |
10 weeks, 4 times a week, 2 – 3 sets of 8 – 12 repetitions dynamic balance control, eccentric lower limb muscle strength, and core stability |
Primary: Dynamic balance using Community balance and mobility scale, and physical function by WOMAC. Secondary: Knee pain using numerical rating scale, fear of movement by Brief Fear of Movement Scale, and muscle strength by isokinetic dynamometer. |
- | A ten-week dynamic balance training program for people with knee OA significantly improved self-reported knee pain, physical function, and fear of movement. | |
| Ghosh 2015 |
30 moderates to severe OA | 50-65 years | Randomized comparative study | Group A: balancing exercises Group B: strengthening exercises. Both groups received TENS. |
4 days a week for 4 weeks. Balance exercises: One-leg balance (Open and closed eyes)-30 sec with 10 sec rest and 3 times repetitions Cross-body leg swing-15 times repetitions Tendem-walking Rocker board-5 to 30 min per day Strength exercise: Quadriceps setting-10 sec, 10 times repetitions SLR- 10 sec, 10 times repetitions Hamstring setting- 10 sec, 10 times repetitions Quadriceps strengthening with weight cuff on the chair- 5 to 10 sec, 5 to 10 times repetitions Mini-squat- 10 times repetitions. |
Pain by VAS, Function by WOMAC | - | The results showed balancing exercise is more effective than strengthening exercise to improve the functional ability of people with knee OA. |
|
| Apparo 2015 |
60 knee OA | 50-70 years Group A (Functional task exercise): m/f: 13/17 57.07± 4.56 y Group B (Agility and perturbation training): m/f: 19/11 57.50± 5.57 y |
Randomized trials | Group A: functional task exercises Group B: agility and perturbation training |
4 weeks Functional task exercises: Unilateral balance, Squat with arms forward, Lateral squats, Forward or backward leans, Squat with diagonal reach, Walk around obstacle, Rotation Lunges, Lunge and chop, Stair climbing Agility and perturbation training: Side stepping, Lateral cross over steps, Front and back cross over steps during forward ambulation, Shuttle walking, Multiple change in direction during walking on therapist command, Double leg foam balance activity, Tilt board balance training, Roller board. |
Pain intensity by VAS, Function by WOMAC scale | - | None of the groups are superior to each other. No significant difference showed between functional task exercises and perturbation training in people with osteoarthritis of knee. | |
| Rogers 2012 |
43 knee OA | ≥ 50 years m/f: 13/20 kinesthesia, balance and agility (KBA)Group: 70.7 ± 10.7 y Group Resistance training (RT): 70.8 ± 6.5 y Group KBA + RT: 68.8 ± 10.1 y Control Group: 71.2 ± 10.9 y |
Single-blind, block randomized placebo controlled clinical trial |
Group one: KBA Group two: RT Group three: KBA + RT Group four: control. |
8-weeks, 3 times per week 30-40 min KBA exercises-15 t0 75 steps/ 30 sec, 3 times repetitions: Wedding and Backward wedding march, High knees march, Side stepping, Semi-Tandem and Tandem walk, Cross-over walk, Modified grapevine, Toe and Heel walk, Static and Dynamic balance RT- 15 repetitions: Ankle dorsiflex and plantar flex, Knee flex and ext, Hip Abd, Add, Internal and external rotation with Thera band in sitting position and Hip hyper-ext in standing position. |
WOMAC Index of Pain, Stiffness, and Physical Function (PF), community activity level, exercise self-efficacy, self-report knee stability, and 15m get up & go walk (GUG) |
- | The results demonstrated KBA, RT, or a combination of the two administered as home exercise programs were effective in reducing symptoms and improving the quality of life among people with knee OA. |
|
| Rogers 2011 |
20 knee OA | Kinesthesia, balance and agility (KBA): m/f: 2/6 69.29 ± 11.36 y Strength training (ST): m/f: 2/10 72.4 ± 11.02 y |
Randomized trial | Group I: KBA Group II: ST |
8 weeks, 3-days per week, 30 min KBA exercises-15 to 75 steps/ 30 sec, 3 times repetitions: Wedding and Backward wedding march, High knees march, Side stepping, Semi-Tandem and Tandem walk, Cross-over walk, Modified grapevine, Toe and Heel walk, Static and Dynamic balance ST- 15 repetitions: Ankle dorsiflex and plantar flex, Knee flex and ext, Hip Abd, Add, Internal and external rotation with Thera band in sitting position and Hip hyper-ext in standing position |
the Human Activity Profile (HAP), the Self-Efficacy for Exercise (SEE) scale, WOMAC, timed 15-meter Get Up & Go (GUG) walk, timed 10-stair climb, and timed 10-stair descent | - | Both interventions were effective to improve function and knee stability among people with symptomatic knee OA. | |
| Fitzgerald 2011 |
183 Knee OA With Grade ≥ 2 Kellageren and Lawernce Scale |
≥ 50 years m/f: 61/122 Agility and perturbation training with standard exercise therapy group: 63.3 ± 8.9 y m/f: 31/60 Standard exercise therapy group: 64.6 ± 8.4 y m/f: 30/62 |
Single-blinded randomized controlled trial | One group: Agility and perturbation training with standard exercise therapy Other group: only the standard exercise program |
12 supervised sessions of their respective program, 6- to 8weeks, a walking program of at least 30 minutes per day at least 3 days a week for the home program. Standard exercises: Quadriceps femoris, hamstring, and calf muscle stretching and Quadriceps setting, SLR, pronehip extensions, seated isometric knee extensions, single-leg leg presses, Standing hamstring curls, and Standing heel raises, Long-sitting knee flexion and extension range of motion, and treadmill walking Agility training: Side stepping, Lateral stepping combined with forward and backward crossover steps, front crossover steps, back crossover steps, shuttle walking and Forward and Backward, right and left lateral steps, diagonally backward and forward during walking. |
Self-reported knee pain and function, self-reported knee instability, a performance-based measure of function, and global rating of change. |
baseline and at 2, 6, and 12 months |
Both intervention groups demonstrated improvement in self-reported function and the global rating of change. Adding agility and perturbation training to standard exercise therapy had no more effects in this sample of individuals with knee OA. |
|
| Chaipinyo 2009 |
48 knee OA | ≥ 50 years Balance training Group: 62 ± 6 y m/f: 9/15 Strength Group: 70 ± 6 y m/f: 2/22 |
Randomized trial with concealed allocation and assessor blinding |
Two groups received home-based exercise programs: one group performed balance training and the other performed strength training. |
5 days/week for 4 weeks Balance training: Stepping forward and backward with left and right leg 30 times, Bilateral mini squat 10 times, Stepping sideward to the left and right 30 times Strength training: isometric knee extension in sitting- 5 sec hold, 10 times repetitions. |
Pain by KOOS, knee flexor and extensor strength by isokinetic dynamometer, and mobility by Get up and Go, walking up 11 stairs, and walking down 11 stairs |
- | There was no difference in pain between home-based strength training and home-based balance training in patients with knee osteoarthritis. |
|
| Tasauo 2008 |
29 knee OA with grade 2-3 Kellageren and Lawernce Scale |
Training group: 61.7± 6.6 y m/f: 1/ 14 Control group: 60.1 ± 6.7 y m/f: 4/10 |
Randomized, single-blind, controlled trial | Training group: Sensory motor training + Routine physical therapy Control group: Routine physical therapy |
Three times per week for eight weeks. Sensorimotor training program using a sling suspension system Routine physical therapy program was: thermotherapy, interferential therapy and instructions for exercise at home. Straight leg raising, short arc extension exercise, and walking for 30 min. |
Active joint repositioning, functional testings (60-m straight walking, figure-of-eight walking, and climbing up and down stairs), and self-reported function with the WOMAC |
- | A sensorimotor training using a sling suspension system improved the patients’ proprioception in the knee joints and their self-reported function. these exercises may use as an exercise program for patients with knee osteoarthritis. |
|
| Diracoglu 2005 |
60 Female with grade 1-2 Kellageren and Lawernce Scale |
35-65 y | Randomized study | Kinesthesia group Strengthening group |
3 days a week for 8 weeks. Kinesthesia and balance exercises Modified Romberg exercise, Retrowalking, Walking on heels and toes, Walking with eyes closed, Standing on one extremity for 30 sec, Leaning forward, backward, and to the sides on one extremity Sitting down and standing up from a high chair slowly. Exercise with “rocker-bottom” balance board, Sitting down and standing up from a low chair slowly, Plyometric exercise, Walking slowly& quickly, wide circle, Walking slowly& quickly, narrow circle, Exercise with “BAPS board”, Minitrampoline exercise, Plyometric exercise, Carioca crossover maneuver. Strength exercises:(without & with resistance) 5-min fixed bike exercise without resistance, Range-of-motion and active stretching exercises applied to hamstring and quadriceps muscles, Quadriceps& Hamstring isometric strengthening exercise (6 sec, 8 repetitions), ,Short-arc terminal extension exercise, Isometric exercise for the Hip abductor& adductor muscles. |
WOMAC, SF-36 Form, times for performing activities of daily living, isokinetic quadriceps muscle strength, and proprioceptive sensation levels. |
- | Kinesthesia and balance exercises had additional positive effects in knee OA. These exercises could be able to increase the functional capacities of patients. |
Abbreviations
y: year, QOL: Quality of life, EuroQol 5-D: Euro quality of life 5-dimension questionnaire, WOMAC: Western Ontario and McMaster Universities osteoarthritis, mCTSIB: modified Clinical test of sensory interaction and balance, A/P: Anterior/ Posterior, M/L: Medial/ Lateral, US: Ultrasound, TENS: Transcutaneous electrical nerve stimulation, Sec: Second, msec: milliseconds, Min: Minute, ADL: Activity daily living, ADLS: Activities of daily living scale, Abd: abduction, Add: Adduction, Flex: flexion, Ext: Extension.
The overall quality of the evidence for each outcome was summarized by the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach was used to summarize (19). This is done based on the five following domains: (1) risk of bias: which is related to the presence of limitations within the studies; (2) heterogeneity: which is about the inconsistency of results; (3) indirectness: which refers to how indirect the evidence is; (4) imprecision: which deals with imprecise effect estimates; and (5) risk of publication bias. Based on these domains, the quality of evidence is graded as high, moderate, low, or very low. If there are serious or very serious limitations, the evidence can also be downgraded from “high quality” by one or two levels, respectively, based on assessments of these domains.
Results
Identification of studies
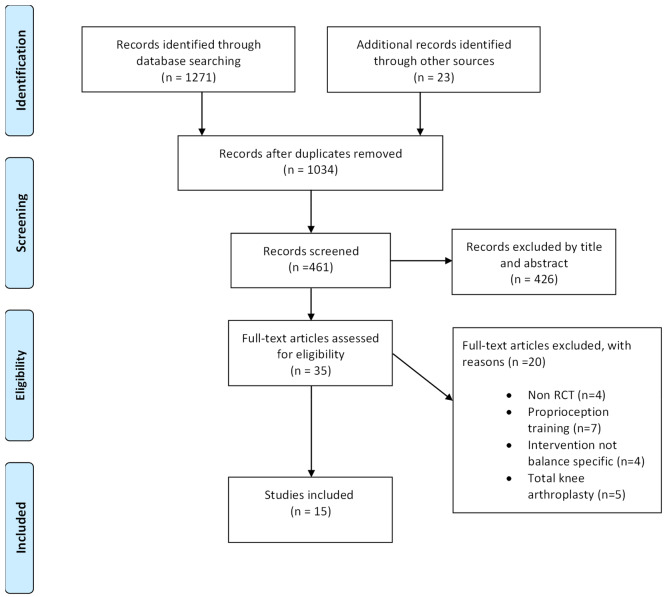
Upon completion of our database search, a total of 1271 studies were obtained, of which 1034 remained after duplicate studies were excluded (Fig. 1). Screening for titles and abstracts was done for 461 studies according to eligibility criteria, and 35 studies were considered for full-text review. Twenty articles were excluded since they did not meet the eligibility criteria. Finally, fifteen articles remained for the final review.
Fig. 1.
PRISMA flow diagram of search strategy
Risk of bias within studies
Table 1 provides a summary of the quality assessment of the studies included in this review. The risk of bias in the articles included, according to the PEDRO checklist, was moderate to low. Only one study (20) has a high risk of bias. The absence of blinding of patients and/or therapists was the highest risk of bias within studies.
Participants and designs of the interventions
Of the 862 participants with a mean age of 60.76 years which included, 411 participants received balance exercise training or sensorimotor or perturbation training. Interventions of control groups contained strengthening exercise (13,14,20-26) or routine physiotherapy (3,27-29) or no specific training (30).
Interventions were identical in intervention and control groups, but the intervention group involved balance training (13,20,21,24-26,28,30), sensorimotor (23,29), perturbation (3,27,31), or balance training using Biodex stability system (22,28).
The periods of experimental interventions ranged from 2 to 12 weeks. The training frequencies range from two to five sessions per week with a mean of three sessions/week and a total of 10–40 training sessions. The duration of a single training session lasted between 10 and60 min. The follow-up period of included articles was 2-12 weeks, except for the study of Fitzgerald et al. 2011 (32), which reported 12 months.
Outcome measures
Most studies used patient-reported outcome measures for the evaluation of functional outcomes, including WOMAC, KOOS, and SF-36 (3,13,20-26,28-31).Some studies used performance-based functional outcome measures such as the Timed Up and Go test (TUG), Get Up and Go test (GUG), functional reach test, stair climb test, 30s chair stand test, and 10 or 60m walking (3,13,21-29).There are few studies that have measured quadriceps and hamstring muscle strength and used sophisticated equipment (Biodex stability system, sway-meter) for measuring postural sway and fall risk score (14,22,24,28).
Effects following balance training
Primary outcomes
The results of most included studies showed that the implementation of balance training or sensorimotor or perturbation training improved self-reported functionality or performance-based functional outcomes in knee OA patients, although they did not have superiority over to control group (3,14,21,23-26,29,31). However, some studies showed experimental group attained superior improvement in comparison with the control group (13,20,22,27,28,30).
The improvements in self-reported physical function reported in these studies were ranging from 8.5% to 34%, which showed that they are larger than the change of 21% considered as minimum clinically important improvement (33). According to the findings of these studies, patients with knee OA can experience clinically significant improvements in their physical function by doing balance training.
Secondary outcomes
The studies examining pain in knee OA patients following balance training have used various outcome measures such as the visual analogue scale, Numbering rating scale, and pain subscale of the WOMAC questionnaire. However, irrespective of a large variety in outcome measures of pain, it could be found that there is a significant improvement in pain intensity in the balance training group that did not have superiority over to control group (3,21-23,25,26,30).
There are few studies that have measured quadriceps and hamstring muscle strength in knee OA patients following balance training (13,21,23,30). In Chaipinyo’s study, in which home-based balance training was given for four weeks, no difference was found in muscle strength of patients with knee OA who had home-based strength training and those who had home-based balance training (21).
The results of Takacs et al.’s study showed that no within- or between-group differences were observed for muscle strength. In this study, the experimental group received ten weeks (four times per week) of dynamic balance training, and the control group received no intervention (30). In contrast, Diracoglu et al.’s study demonstrated that the addition of kinesthesia and balance exercises (i.e., retro-walking, walking on toes, leaning to the sides, doing balance board, mini-trampoline, and plyometric exercises, etc.) to strengthening exercises compared to only the strengthening exercises could result in significantly greater improvements in isokinetic muscle strength at high angular velocities (p<0.05) (13). Also, the results of Gomiero et al.’ s study revealed that as far as the outcome of isometric strength is concerned, 16 weeks following treatment, a greater improvement was observed in the sensorimotor training group compared to the resistance training group (MD 6.5; 95% CI 0.13 to 12.87; d = 0.55, i.e., a medium effect) (23).
There are three studies that evaluated measurement of postural stability and balance disturbance in knee OA patients following balance training (22,24,28). The results of these studies showed more significant improvement in postural stability and balance in the balance training group rather than the control group (22,24,28).
Finally, only one study analyzed the impact of balance exercises on knee range of motion (22). There were also further improvements in the experimental group compared to the control group.
The details of the included articles are shown in Table 2.
Quality of Evidence
The GRADE approach was used to assess the quality of evidence for the outcome measures (Table 3). As far as the functional outcome (Patient-reported and performance-based functional measures) was concerned, very low-quality evidence (downgraded because of inconsistency, imprecision, and publication bias) was observed, showing that at the short-term follow-up, balance training contributed to improved function in patients with knee OA.
Table 3. Grades of Recommendation, Assessment, Development, and Evaluation quality of evidence and strength of recommendation for the primary and secondary outcomes .
| Outcomes | Within Study limitation | Inconsistency | indirectness | imprecision | Publication bias | GRADE quality |
| Patient reported functional measures | No serious | serious | No serious | serious | serious | ⊕⊝⊝⊝ (very low grade) |
| Performance based functional measures | No serious | serious | No serious | serious | serious | ⊕⊝⊝⊝ (very low grade) |
| pain | No serious | No serious | No serious | serious | No serious | ⊕⊕⊕⊝ (moderate grade) |
| Quadriceps and hamstring strength | No serious | serious | No serious | serious | No serious | ⊕⊕⊝⊝ (low grade) |
| Postural stability and balance disturbance | No serious | No serious | No serious | serious | No serious | ⊕⊕⊕⊝ (moderate grade) |
| Range of motion | serious | No serious | No serious | serious | No serious | ⊕⊕⊝⊝ (low grade) |
With respect to pain and postural stability, there was moderate-quality evidence (downgraded due to imprecision) demonstrating that balance training could reduce pain and improve postural stability in patients with knee OA at the short-term follow-up. In addition, there was a low grade of evidence (downgraded because of inconsistency and imprecision) indicating that balance training could improve quadriceps and hamstring strength and knee ROM in knee OA patients at the short-term follow-up.
Discussion
The primary aim of the present systematic review was to evaluate studies assessing the effects of balance training compared to the control group on patient-reported and performance-based functional outcomes in knee OA patients. This review also aimed to investigate studies measuring the effect of balance training on outcomes of pain, quadriceps and hamstring muscle strength, postural stability and balance disturbance, and knee range of motion in patients suffering from knee OA compared to the control group.
The effect of balance training on functional outcomes was reported in 13 out of 15 included studies using different patient-reported and performance-based outcomes. These studies used WOMAC (3,13,20,22-26,28-31) and one study used KOOS (21) as an outcome measure to evaluate the effectiveness of balance training on function in knee OA patients, while others used different functional tests as outcome measures such as Timed Up and Go test (TUG) (23,27,28),Get Up and Go test (GUG) (13,22,24-26), functional reach test (27), stair climb test, 30s chair stand test (22,24) and 10 stairs climbing time (13,24),10-m walking time (13), 60-m straight walking, figure-of-eight walking, and climbing up and down stairs (29),walking along a level unobstructed corridor for 15 meters, rising from a chair and walking 15 meters [Get up and Go], walking up 11 stairs, and walking down 11 stairs (21) for examining the effect of balance training on functional outcomes in patients with knee OA.
Due to the heterogeneity of outcome measures in the studies included, it was not possible to perform a meta-analysis. On the other hand, given that the 24-item WOMAC questionnaire consisted of three subscales for assessing knee pain (5 items), joint stiffness (2 items), and physical function (17 items) (34); in some included studies, only a Total WOMAC score was reported, but the score of physical function subscale of WOMAC was not separately reported. Therefore, we did not have access to scores of physical functions in many included articles to conduct a quantitative data synthesis.
Of course, regardless of different outcome measures for assessing function, it could be concluded that although implementing of balance training led to improvement in functional outcomes in knee OA patients, it had no significant difference compared with the control group (strengthening training or routine physiotherapy) in most studies (3,14,21,23-26,28,29). In another word, it seems both interventions result in improving function among patients with knee OA. According to these studies, isometric exercises and strengthening the muscles of the quadriceps and hamstring may explain the functional improvement observed in the con trol group. Only 5 articles included, it was seen a greater improvement in functional outcomes rather than control group following balance training in knee OA patients (13,20,22,27,30). One possible reason may be that the total volume of exercises in these studies was greater than in other included studies. For example, in Elsheikh et al. study, exercises were repeated 3 times weekly for 12 weeks (22). Also, exercises in Diracoglu et al.’ s study were done 3 days a week for 8 weeks (13), and in Takacs et al.’ s study, knee OA patients were trained for 4 times per week for 10 weeks (30).
On the whole, based on previous reviews (15,35) and the results of the present study, balance training seems to have a positive effect on patients with knee OA. Therefore, based on current evidence, clinicians are recommended to continue to prescribe balance training as part of the rehabilitation program. However, future studies need to investigate the greater volume of balance training and a longer period of follow-up.
The current systematic review showed controversy in the results of studies that examined the impact of balance training on quadriceps and hamstring muscle strengths in patients suffering from knee OA. According to our results, implementing balance training alone may not improve muscle strength; therefore, these exercises are suggested to be included besides the strengthening training in the rehabilitation program of knee OA patients.
This study could provide clinically significant information as it concluded that exercises focusing on balance and sensorimotor training could be a suitable supplement to physiotherapy care. This is particularly true if these exercises are aimed at gaining a clinical effect on functional and balance outcomes.
Strengths and limitations
Strength of the current review was that since all studies included in this review were randomized trials, the level of evidence is ensured. Furthermore, most of the articles included had an acceptable internal validity. However, we could not conduct a meta-analysis because of the diversity in the assessment measures of outcomes, the different scoring of these outcome measures, and the limited number of studies for some of the outcome measures.
The designs of the studies had different outcomes and limited follow-up assessments. In addition, many studies didn’t account for data needed to calculate Standardized Mean Difference (SMD). Therefore, it is recommended that future studies report pre and post-means and standard deviations for the intended balance and functional outcomes. Since few studies reported the effects on muscle strength, postural stability, and range of motion, these results need to be interpreted cautiously.
Conclusion
According to the results of the current systematic review, balance and functionality in knee OA patients can be significantly improved by adopting a rehabilitation program with an emphasis on balance exercises. Thus, clinicians should consider implementing balance training as a suitable addition to routine physiotherapy in knee OA patients. Also, based on the results of the current review, the effect of balance training on muscle strength and knee range of motion was not intensely revealed due to few studies. It would be suggested to conduct further research keeping a homogenous pattern of balance training with an excellent method design to confirm or discard the current evidence.
Acknowledgments
The authors would like to express their gratitude to Ahvaz Jundishapur University of Medical Sciences for supporting this research financially (IR.AJUMS.REC.1399.594).
Ethical Approval
This study was approved by the Research Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (IR.AJUMS.REC.1399.594)
Conflict of Interests
The authors declare that they have no competing interests.
Cite this article as: Pirayeh N, Kazemi K, Rahimi F, Mostafaee N, Shaterzadeh-Yazdi MJ. The Effect of Balance Training on Functional Outcomes in Patients with Knee Osteoarthritis: A Systematic Review. Med J Islam Repub Iran. 2022 (17 Sep);36:107. https://doi.org/10.47176/mjiri.36.107
References
- 1.Litwic A EM, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185–99. doi: 10.1093/bmb/lds038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hinman RS BK, Metcalf BR, Crossley KM. Balance impairments in individuals with symptomatic knee osteoarthritis: a comparison with matched controls using clinical tests. Rheumatology. 2002;41(12):1388–94. doi: 10.1093/rheumatology/41.12.1388. [DOI] [PubMed] [Google Scholar]
- 3.Fitzgerald GK, Piva SR, Gil AB, Wisniewski SR, Oddis CV, Irrgang JJ. Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial. Phys Ther. 2011;91(4):452–69. doi: 10.2522/ptj.20100188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lyytinen T LT, Bragge T, Hakkarainen M, Karjalainen PA, Arokoski JP. Postural control and thigh muscle activity in men with knee osteoarthritis. J Electromyogr Kinesiol. 2010;20(6):1066–74. doi: 10.1016/j.jelekin.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Schmitt LC FG, Reisman AS, Rudolph KS. Instability, laxity, and physical function in patients with medial knee osteoarthritis. Phys Ther. 2008;88(12):1506–16. doi: 10.2522/ptj.20060223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ng CT, Tan MP. Osteoarthritis and falls in the older person. Age Ageing. 2013;42(5):561–6. doi: 10.1093/ageing/aft070. [DOI] [PubMed] [Google Scholar]
- 7.Tasci Bozbas G SO, Aydemir AH. Primary knee osteoarthritis increases the risk of falling. J Back Musculoskelet Rehabil. 2017;30:785–9. doi: 10.3233/BMR-150413. [DOI] [PubMed] [Google Scholar]
- 8.Golightly YM AK, Caine DJ. A comprehensive review of the effectiveness of different exercise programs for patients with osteoarthritis. Physician Sportsmed. 2012;40(4):52–65. doi: 10.3810/psm.2012.11.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iwamoto J SY, Takeda T, Matsumoto H. Effectiveness of exercise for osteoarthritis of the knee: A review of the literature. World J Orthop. 2011;2(5):37–42. doi: 10.5312/wjo.v2.i5.37. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 10. Li Y, Su Y, Chen S, Zhang Y, Zhang Z, Liu C, et al. The effects of resistance exercise in patients with knee osteoarthritis: a systematic review and meta-analysis. Clin Rehabil. 2016 Oct;30(10):947-959. [DOI] [PubMed]
- 11.Ahmed A. Effect of sensorimotor training on balance in elderly patients with knee osteoarthritis. J Adv Res. 2011;2(4):305–11. [Google Scholar]
- 12.Chhabr HK, Sathya P. Effect of conventional exercises with balance training &only conventional exercises in patients with osteoarthritis of knee. Int J Innov Res Sci Eng. 2015;4(7):5048–56. [Google Scholar]
- 13.Diracoglu D, Aydin R, Baskent A, Celik A. Effects of kinesthesia and balance exercises in knee osteoarthritis. J Clin Rheumatol. 2005;11(6):303–10. doi: 10.1097/01.rhu.0000191213.37853.3d. [DOI] [PubMed] [Google Scholar]
- 14.Jahantigh Akbari N, Mohammadi M, Nouraisarjou S. The Effect of Balance Exercises on Knee Instability and Pain Intensity in Patients with Knee Osteoarthritis:A Randomized Clinical Trial. J Med Dent Sci. 2018;6(2):74–82. [Google Scholar]
- 15.Jeong HS, Lee SC, Jee H, Song JB, Chang HS, Lee SY. Proprioceptive training and outcomes of patients with knee osteoarthritis: a meta-analysis of randomized controlled trials. J Athl Train. 2019;54(4):418–28. doi: 10.4085/1062-6050-329-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–21. [PubMed] [Google Scholar]
- 18. Cashin AG, McAuley JH. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J Physiother 2019;66(1). [DOI] [PubMed]
- 19.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical research ed) 2008;336(7650):924–6. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghosh PK, Ray D, Chatterjee B, Acharya S, Adhikary S, De A. Comparative study of the effectiveness between balancing exercises and strengthening exercises with common use of TENS to improve functional ability in Osteoarthritis involving knee joint. Int Arch Integrat Med. 2015;2(10):1–17. [Google Scholar]
- 21.Chaipinyo K, Karoonsupcharoen O. No difference between home-based strength training and home-based balance training on pain in patients with knee osteoarthritis: a randomised trial. J Physiother. 2009;55(1):25–30. doi: 10.1016/s0004-9514(09)70057-1. [DOI] [PubMed] [Google Scholar]
- 22. Elsheikh MMA, El-Hawa MAA, El-saadany HM, Elsergany MAES. The Effect of Balance Training in Knee Osteoarthritis. Adv Med Sci. 2020:246-55.
- 23.Gomiero AB, Kayo A, Abraão M, Peccin MS, Grande AJ, Trevisani VF. Sensory-motor training versus resistance training among patients with knee osteoarthritis: randomized single-blind controlled trial. Sao Paulo Med J. 2017;136:44–50. doi: 10.1590/1516-3180.2017.0174100917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pazit L, Jeremy D, Nancy B, Michael B, George E, Hill KD. Safety and feasibility of high speed resistance training with and without balance exercises for knee osteoarthritis: A pilot randomised controlled trial. Phys Ther Sport. 2018;34:154–63. doi: 10.1016/j.ptsp.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 25.Rogers MW, Tamulevicius N, Coetsee MF, Curry BF, Semple SJ. Knee osteoarthritis and the efficacy of kinesthesia, balance & agility exercise training: a pilot study. Int J Exerc Sci. 2011;4(2):124. [PMC free article] [PubMed] [Google Scholar]
- 26.Rogers MW, Tamulevicius N, Semple SJ, Krkeljas Z. Efficacy of home-based kinesthesia, balance & agility exercise training among persons with symptomatic knee osteoarthritis. J Sports Sci Med. 2012;11(4):751. [PMC free article] [PubMed] [Google Scholar]
- 27. Bhaskar B, Jimshad T, Solomen S. Efficacy Of Perturbation Training In Improving Balance And Function In The Management Of Knee Osteoarthritis. Int J Physiother 2019;6(4).
- 28.Jahanjoo F, Eftekharsadat B, Bihamta A, Babaei-Ghazani A. Efficacy of balance training in combination with physical therapy in rehabilitation of knee osteoarthritis: A randomized clinical trial. Crescent J Med Biol Sci. 2019;6(3):225–334. [Google Scholar]
- 29.Tsauo JY, Cheng PF, Yang RS. The effects of sensorimotor training on knee proprioception and function for patients with knee osteoarthritis: a preliminary report. Clin Rehabil. 2008;22(5):448–57. doi: 10.1177/0269215507084597. [DOI] [PubMed] [Google Scholar]
- 30.Takacs J, Krowchuk NM, Garland SJ, Carpenter MG, Hunt MA. Dynamic balance training improves physical function in individuals with knee osteoarthritis: a pilot randomized controlled trial. Arch Phys Med Rehabil. 2017;98(8):1586–93. doi: 10.1016/j.apmr.2017.01.029. [DOI] [PubMed] [Google Scholar]
- 31.Patchava Apparao C, Swamy G, Subramaniam S. Effectiveness of Functional Task Exercises versus Agility and Perturbation Training in Osteoarthritis Knee Subjects. Int J Health Sci. 2015;5(9):328–37. [Google Scholar]
- 32.Fitzgerald GK, Piva SR, Gil AB, Wisniewski SR, Oddis CV, Irrgang JJ. Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial. Phys Ther. 2011;91(4):452–69. doi: 10.2522/ptj.20100188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tubach F, Ravaud P, Baron G, Falissard B, Logeart I, Bellamy N, et al. Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: the minimal clinically important improvement. Ann Rheum Dis. 2005;64(1):29–33. doi: 10.1136/ard.2004.022905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Williams VJ, Piva SR, Irrgang JJ, Crossley C, Fitzgerald GK. Comparison of reliability and responsiveness of patient-reported clinical outcome measures in knee osteoarthritis rehabilitation. J Orthop Sports Phys Ther. 2012;42(8):716–23. doi: 10.2519/jospt.2012.4038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smith TO, King JJ, Hing CB. The effectiveness of proprioceptive-based exercise for osteoarthritis of the knee: a systematic review and meta-analysis. Rheumatol Int. 2012;32(11):3339–51. doi: 10.1007/s00296-012-2480-7. [DOI] [PubMed] [Google Scholar]