Abstract
Objective:
Caregivers of children with rare diseases often consider caregiving to be a rewarding experience, despite high levels of burden. The present study examined associations between caregiver stress and positive aspects of caregiving (PAC); investigated associations between interpersonal coping strategies and PAC; and determined whether coping strategies moderated associations between stressors and PAC.
Design:
Survey data came from a study on caregivers across different caregiving conditions, including caregivers of children diagnosed with inherited metabolic conditions (n=167), undiagnosed diseases (n=23), and caregivers of typically-developing children (n=74).
Main Outcome Measures:
Positive Aspects of Caregiving (PAC) scale.
Results:
Results from generalized linear models indicated that perceived burden was not associated with PAC. Venting was negatively associated with PAC (b=−0.09, p=.03), whereas emotional support was associated with increased PAC for caregivers of children with undiagnosed conditions (b=0.15, p=.02). Care needs were associated with greater PAC among caregivers engaged in high levels of emotional support coping (b=0.10, p=.01) and venting (b=0.09, p=.03).
Conclusion:
These findings illuminate important differences in PAC based on the caregiving condition, and aspects of the caregiver stress process model that might be universal to caregivers. Results inform stress process theory and highlight the potential of support-based interventions for promoting PAC.
Keywords: caregiving, positive aspects of caregiving, caregiver burden, coping, rare disease
Informal caregiving is a chronic stressor that puts caregivers at increased risk for poor health and well-being (McConkie-Rosell et al., 2018; Raina et al., 2005). Despite caregiving-related stress and burdens, caregivers also report positive experiences that result from their caregiving roles. Positive aspects of caregiving (PAC) have been conceptualized in a variety of ways across studies, primarily involving care of older adults. Domains of PAC include feelings of accomplishment (e.g., gains, satisfaction, esteem), relationship quality with care recipient and other family (e.g., feeling appreciated), and meaning-making (Carbonneau et al., 2010; Tarlow et al., 2004). PAC has been associated with better self-rated health and psychological well-being, as well as continued involvement with caregiving (Bermejo-Toro et al., 2020; Cohen et al., 2002). Given the importance of positive aspects on caregiver well-being, it is critical to identify facets of the caregiving experience that promote or diminish PAC. This study aims to disentangle the links between caregiver burden, coping strategies, and PAC.
We apply the caregiver stress process model to unique caregiving conditions that vary by the care recipient’s health condition. Specifically, this study includes caregivers of children with rare inherited metabolic conditions and undiagnosed diseases. We also include caregivers of typically-developing children to assess whether differences can be observed in the experience of PAC by caregiving condition. Caring for a child with a rare disease poses unique challenges to caregivers. In addition to the physical, emotional, and financial demands of caregiving, caregivers of children with rare disease often encounter a scarcity of resources and information about the disease and experience a significant decline in free time while meeting the child’s medical and behavioral needs (McConkie-Rosell et al., 2018; Pelentsov et al., 2015). Families of children with rare disease, particularly those that are undiagnosed, endure long periods of uncertainty as medical professionals explore treatment options (Cardinali et al., 2019; Lewis et al., 2010). Consequently, caregivers of children with rare disease experience high levels of stress, burden, depression, and anxiety, though some also adapt successfully to caregiving as they gain experience with and knowledge about the disease and its management and develop adaptive coping strategies (Carpenter et al., 2018; Senger et al., 2016).
Theoretical Frameworks
The caregiver stress process model describes how caregiving stress and coping impacts caregiver well-being (Pearlin et al., 1990). Caregiving stress is shaped by caregiving context, sociodemographic characteristics of caregivers, and caregiving resources (Supplemental Figure 1). Primary caregiving stressors stem directly from providing care, including perceived caregiver burden and the care needs of the care recipient. Secondary stressors refer to processes that result from primary stressors. These include role strains, such as family conflict, and intrapsychic strains, such as loss of self. Intrapsychic strains also encompass dimensions of self-concept and psychological states that can arise in the absence of or despite primary stressors (e.g., esteem and mastery). We conceptualize PAC as an intrapsychic gain that results from caregiving.
Finally, coping strategies used by caregivers can have both direct and indirect effects on caregiver well-being (Pruchno & Resch, 1989). The main effects model posits that the association between coping strategies and caregiving outcomes, such as PAC, is independent of caregiver stress. The moderation model of coping suggests that coping strategies vary in their impact depending on caregiving stress level (Morimoto et al., 2019). Guided by the stress-buffering model of social support (Cohen & McKay, 1984), we focus on coping strategies with an interpersonal component, including use of emotional support, instrumental support, and venting. We assess the direct effect of coping strategies on PAC, as well as the moderating effect of coping on the link between primary stressors and PAC.
Primary Caregiving Stressors
Among the most widely recognized primary stressors of caregiving are care needs of the care recipient and perceived caregiving burden. Care needs are conceptualized using activities of daily living (ADLs) and typically correspond to amount and difficulty of caregiving (Pearlin et al., 1990). Perceived burden encompasses the subjective evaluations about caregiving load as identified by the caregiver. According to the caregiver stress process model, primary stressors are associated with lower intrapsychic gains. However, studies that have examined this link yield inconsistent findings. A systematic review on PAC in caregivers of people with dementia reported most findings identified a negative association between burden and PAC (Quinn & Toms, 2019). Similarly, among caregivers of cancer patients, greater perceived and objective burden was associated with lower PAC (Cassidy, 2013). Although these findings primarily emerged from adult caregiving samples, some studies examine this association in caregivers of chronically ill children. Research on Chinese caregivers of children with pediatric glaucoma found a negative relationship between PAC and perceived caregiver burden, particularly the emotional aspects, such as negative feelings about caregiving (Zhu et al., 2019).
Other studies point to a positive association or no association between caregiving burden and PAC. Magliano et al. (2014) found that among caregivers of children with muscular dystrophy, those whose care recipients presented more challenges, dependency, and longer duration of illness reported higher PAC. Similarly, Pendergrass and colleagues (2019) found that caregivers of older adults who reported greater subjective burden and spent more time with caregiving tasks also reported greater positive benefits of caregiving. These studies provide evidence that more burdensome caregiving experiences might be associated with higher PAC. In contrast, Fekete et al. (2017) found weak correlations between measures of perceived burden, ADLs, and PAC, but noted that lower PAC and higher subjective burden were both strongly associated with poorer health outcomes. Although the literature is inconclusive with few studies considering pediatric care contexts, the stress process model posits that higher perceived burden and greater care needs would be associated with lower PAC.
Coping Strategies
The caregiver stress process model posits a positive association between coping strategies, particularly the availability of social resources, and intrapsychic gains. For example, caregivers of children with muscular dystrophy who had more social contacts and connections reported higher perceived PAC (Magliano et al., 2014). Research on caregivers of patients with dementia indicates that perceptions of social support quality are linked to higher ratings of PAC (Lee & Choi, 2013). Here we consider coping strategies that harness caregivers’ interpersonal resources, including use of emotional support, instrumental support, and venting (Carver, 1997; Cooper et al., 2008). Emotional support seeking is an emotion-focused strategy that involves receiving understanding and comfort from others. Instrumental support seeking is a problem-focused strategy that involves getting help and advice from other people. And venting is a dysfunctional strategy that comprises expressing negative feelings. Each of these can also be conceptualized as relationship-focused, or interpersonal, depending on the goal and social context (Kramer, 1993; Stephenson et al., 2016).
In a study of caregivers of pediatric cancer survivors, caregiving benefits were positively associated with available emotional resources (Willard et al., 2016). Similarly, family members’ instrumental support contributions, such as help with chores, collaboration and participation in care, have been tied to feelings of positivity around caregiving experiences (Chen & Greenberg, 2004; Mosher et al., 2017; Parveen & Morrison, 2012). Other studies have found no association or a negative association between support experiences of PAC. For example, among parents of children with type 1 diabetes, increased social support seeking as a coping strategy was associated with lower caregiver motivation, an important dimension of PAC (Grover et al., 2016). Parveen and Morrison (2012) found that, in contrast to instrumental support, total support and satisfaction with social support were not associated with caregiver gains. Though empirical evidence is mixed, based on the model, we hypothesize that instrumental and emotional support coping are associated with greater PAC.
Previous findings on venting as a coping strategy are similarly mixed. Caregivers may feel that venting to friends and family is helpful for providing catharsis and managing their caregiving responsibilities (Dickson et al., 2012; Markoulakis et al., 2012). But there is a large body of literature identifying venting as an unproductive coping strategy that increases feelings of burden (Carver et al., 1989; Thomas et al., 2014; Wrosch et al., 2011). Although there is limited work assessing the direct link between venting and PAC, there is evidence that venting is negatively associated with PAC in caregivers of older adult relatives (López et al., 2005). Indeed, theories of coping indicate that venting is a dysfunctional and maladaptive strategy in most circumstances (Stephenson et al., 2016). Thus, we hypothesize that coping through venting is associated with lower PAC.
The caregiver stress process model also posits that caregivers’ coping strategies can moderate the association between primary stressors and intrapsychic strains, buffering the negative impact of stress. Although coping strategies operate through a variety of mechanisms, we test the stress-buffering hypothesis given our focus on coping strategies that rely on caregivers’ social resources (Cohen & McKay, 1984). Studies on the indirect effects of social support on caregiver well-being appear inconclusive, with some studies suggesting a buffering effect. Thus, we make no specific predictions, but rather explore whether caregivers’ use of coping strategies buffers, strengthens, or has no effect the predicted negative impact of primary stressors on PAC.
Present Study
Previous research indicates that primary stressors, caregiving gains, and coping strategies are fundamental to caregivers’ experience and have important implications for caregiver well-being. Further research is needed to fully understand their relationship, especially across different caregiving conditions. Here, we aim to fill this gap by exploring these features of the stress process model among rare disease caregivers, an especially vulnerable group of informal caregivers, as well as caregivers of typically-developing children.
Specifically, we (1) evaluate the association between primary stressors (i.e., perceived burden and care needs) and PAC; (2) examine the association between coping strategies (i.e., emotional support, instrumental support, and venting) and PAC; and (3) explore whether associations between primary stressors and PAC are moderated by coping strategies. Further, to examine the novel contexts of caregivers of relatives with rare, inherited disease compared to those caring for a typically-developing child, we test whether each of these associations varies across caregiving conditions.
Materials and Methods
Sample & Procedures
Data came from Inherited Diseases, Caregiving, and Social Networks Project. The first participants from each family (i.e., index participants) were recruited through ongoing studies of rare, inherited and undiagnosed diseases at the National Institutes of Health. Participants were matched to healthy volunteers based on age (±1 year) of the care recipient and gender of the caregiver. Additional eligibility criteria for this “typically-developing” control group were that care recipients not be diagnosed with a chronic health condition or disease requiring daily care. Index participants referred members of the care recipient’s caregiving network into study. Participants were contacted and consented over the phone. All procedures were approved by the IRB (Protocol 12-HG-0022). Participants completed a survey and interview about their caregiving experiences, including caregiving roles and expectations, coping strategies, and well-being. Our analytic sample included 214 parents and other primary caregivers of care recipients under 21 years of age across 146 families. In this study, “primary caregiver” refers to any participant who was considered by themselves or by another participant to be a primary caregiver.
Measures
Positive Aspects of Caregiving.
The Positive Aspects of Caregiving (PAC) scale measures positive dimensions of a caregiver’s mental and affective state in relation to the caregiving experience, including self-affirmation (e.g., “made me feel needed”) and outlook on life (e.g., “enabled me to appreciate life more) (Tarlow et al., 2004). Participants rated the extent to which they agreed with each of nine items (α = .89) on a 5-point Likert scale (agree/disagree). Mean scores were used as a continuous outcome measure.
Primary caregiving stressors.
The primary caregiving stressors assessed included care needs of the care recipient and perceived caregiver burden. The Pediatric ADL of the Children’s Habilitation Assessment Tool (Maine DHHS & Children’s Behavioral Health Services, 2011) measures the extent to which participants supported the child/relative in caregiving-related activities, such as eating/feeding, dressing, and social skills. Participants rated the frequency with which the care recipient required assistance or displayed certain behaviors on a scale from 0 (never) to 4 (all the time). Ratings from the 15 items were averaged for a total score of care needs, with higher scores indicating greater care needs. The Zarit Burden Interview measured perceived caregiving burden (Bédard et al., 2001) using 12 items on 4-point scale ranging from 1 (not at all) to 4 (very much) (α = .90). All items were averaged for a total score with higher scores reflecting greater perceived burden.
Coping strategies.
We measured use of interpersonal coping strategies with the Brief COPE. The Brief COPE is comprised of 28 items that fall into 14 subscales (Carver, 1997). Respondents indicated the extent to which they used different strategies on a 4-point scale from 1 (I haven’t been doing this at all) to 4 (I’ve been doing this a lot). Items for each subscale were summed to create a total score ranging from 2 to 8. We consider the subscales for emotional support (2 items, r = .62), instrumental support (2 items, r = .71), and venting (2 items, r = .56).
Caregiving condition.
Caregiving condition refers to the health condition of the care recipient, whether the care recipient was typically-developing or affected by an inherited metabolic condition or undiagnosed disease.
Covariates.
Sociodemographic information, including caregiver age and sex, was collected in the survey. We also accounted for caregivers’ depressive symptomology, measured by the CES-D.
Analysis Strategy
First, we reported descriptive statistics and calculated correlation coefficients for study measures. A series of hierarchical models were estimated to address each research question. The number of participants per family ranged from one to five, with 125 participants belonging to a family from which two or more caregivers participated in the study. Generalized estimating equations (GEE) with exchangeable covariances were fitted to account for clustering of participants within families. Model 1 included care needs and caregiving burden to assess the main effects of primary caregiving stressors on PAC. Then we modeled the interaction between each of these primary stressors and caregiving condition separately, with caregivers of typically-developing children serving as the reference group, to assess whether the association between care needs or caregiver burden and PAC varied by caregiving condition. In Model 2, we added interpersonal coping mechanisms (emotional support, instrumental support, and venting) to assess the main effects of coping on PAC. Next, we modeled the interaction between each of these coping strategies and caregiving condition separately to assess whether the direct effect of coping on PAC varied by condition. The final set of models (Models 3a through 3c) assessed the moderating effect of coping strategies on the link between primary caregiving stressors and PAC. We separately estimated the interaction between primary stressors with emotional support, instrumental support, and venting due to better model fit, as indicated by Quasi information criterion, and to better isolate these associations. Significant interactions were interpreted by plotting and using simple slopes analysis (Preacher et al., 2006). All continuous variables were grand mean-centered. All models controlled for caregiver sex (1 = male), age (years), and depressive symptomology. Analyses described above were conducted in R version 4.0.2 (R Core Team, 2018) using gee (Carey et al., 2018) and tables were created using the package sjPlot (Lüdecke, 2020). The data that support the findings of this study are available on request.
Results
Descriptive Statistics
Participants included 214 caregivers of children with inherited metabolic conditions (60.7%), undiagnosed diseases (10.3%), and typically-developing children (34.5%) (Table 1). Most caregivers were mothers (55.6%) and fathers (34.6%). Other primary caregivers included grandparents, aunts, and uncles. Caregivers ranged from age 23 to 72 years old (M = 40.2). Bivariate correlations are presented in Table 2. PAC was negatively correlated with depressive symptoms (r = −0.26, p < 0.01), venting (r = −0.20, p < 0.01), and perceived burden (r = −0.26, p < 0.01). PAC was not significantly correlated with care needs, emotional support coping, or instrumental support coping.
Table 1.
Sample characteristics and descriptives by caregiving condition, M (SD) or n (%) (N = 214).
| Typically Developing (n = 62) | Inherited Metabolic Conditions (n = 130) | Undiagnosed Diseases (n = 22) | Total (N = 214) | |
|---|---|---|---|---|
|
| ||||
| Participant Age | 40.7 (±8.09) | 40.7 (±8.89) | 35.9 (±6.14) | 40.2 (±8.51) |
| Care Recipient Age | 7.73 (±4.18) | 8.12 (±5.64) | 5.55 (±3.02) | 7.74 (±5.07) |
| Participant female | 38 (61.3%) | 83 (63.8%) | 13 (59.1%) | 134 (62.6%) |
| Care Recipient female | 36 (58.1%) | 44 (33.8%) | 8 (36.4%) | 88 (41.1%) |
| Education | ||||
| Less than HS | 0 (0%) | 0 (0%) | 2 (9.1%) | 2 (1.4%) |
| HS Diploma/GED | 4 (6.4%) | 16 (12.3%) | 1 (4.5%) | 21 (9.8%) |
| Some College | 10 (16.1%) | 34 (26.1%) | 6 (27.2%) | 50 (23.4%) |
| Bachelor’s Degree | 18 (29.0%) | 51 (39.2%) | 8 (36.4%) | 77 (36.0%) |
| Post-Graduate Degree | 29 (46.8%) | 25 (19.2%) | 5 (22.7%) | 59 (27.6%) |
| Married / Cohabitating | 48 (77.4%) | 115 (88.5%) | 20 (90.9%) | 183 (85.5%) |
| Race | ||||
| American Indian / Alaska Native | 0 (0%) | 1 (0.8%) | 0 (0%) | 1 (0.5%) |
| Asian | 9 (14.5%) | 4 (3.1%) | 0 (0%) | 13 (6.1%) |
| Black or African American | 10 (16.1%) | 3 (2.3%) | 0 (0%) | 13 (6.1%) |
| Native Hawaiian /Pacific Islander | 1 (1.6%) | 0 (0%) | 0 (0%) | 1 (0.5%) |
| White | 35 (56.5%) | 110 (84.6%) | 22 (100%) | 167 (78.0%) |
| Other | 6 (9.7%) | 10 (7.7%) | 0 (0%) | 16 (7.5%) |
| Hispanic or Latino | 4 (6.5%) | 10 (7.7%) | 0 (0%) | 14 (6.5%) |
| Relationship to Care Recipient | ||||
| Father | 22 (35.5%) | 43 (33.1%) | 9 (40.9%) | 74 (34.6%) |
| Mother | 33 (53.2%) | 74 (56.9%) | 12 (54.5%) | 119 (55.6%) |
| Others (e.g., grandparents, uncles, aunts, family friend) | 7 (11.3%) | 13 (10.0%) | 1 (4.5%) | 21 (9.8%) |
| Positive Aspects of Caregiving | 4.41 (± 0.72) | 4.02 (± 0.72) | 3.77 (± 0.70) | 4.11 (± 0.74) |
| Perceived Burden | 0.98 (± 0.63) | 1.49 (± 0.81) | 1.77 (± 0.59) | 1.37 (± 0.78) |
| Care needs | 1.04 (± 0.90) | 1.91 (± 1.07) | 1.85 (± 0.93) | 1.65 (± 1.08) |
| Coping | ||||
| Emotional Support | 4.56 (± 1.82) | 4.75 (± 1.80) | 4.91 (± 1.57) | 4.71 (± 1.78) |
| Instrumental Support | 4.32 (± 1.91) | 4.42 (± 1.71) | 4.41 (± 1.56) | 4.39 (± 1.75) |
| Venting | 3.35 (± 1.49) | 3.65 (± 1.63) | 3.95 (± 1.29) | 3.60 (± 1.56) |
Notes. M = mean.
SD = standard deviation.
Table 2.
Bivariate correlations among main variables of interest (N = 214)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
|
| ||||||
| 1. Positive Aspects of Caregiving | ||||||
| 2. Care needs | −.12 | |||||
| [−.25, .00] | ||||||
| 3. Perceived burden | −.26** | .59** | ||||
| [−.37, −.13] | [.51, .67] | |||||
| 4. Depressive symptoms | −.26** | .33** | .59** | |||
| [−.38, −.14] | [.21, .44] | [.52, .68] | ||||
| 5. Emotional Support Coping | .02 | .04 | .06 | −.04 | ||
| [−.10, .15] | [−.09, .16] | [−.06, .19] | [−.16, .09] | |||
| 6. Instrumental Support Coping | .03 | .05 | .14* | .05 | .70** | |
| [−.10, .16] | [−.08, .17] | [−.01, .27] | [−.08, .18] | [.63, .76] | ||
| 7. Venting | −.20** | .32** | .49** | .29** | .40** | .42** |
| [−.33, −.07] | [.19, .43] | [.38, .58] | [.16, .40] | [.28, .50] | [.30, .53] | |
Notes. Values in square brackets indicate the 95% confidence interval for each correlation.
p < .05.
p < .01.
Stress, Coping, and PAC
Results of GEE models testing the associations between primary stressors, coping, and PAC are presented in Table 3. A covariates-only model revealed that caregivers of children with inherited metabolic conditions (b = −0.33, p = .006) and undiagnosed diseases (b = −0.48, p = .01) reported significantly lower PAC compared to caregivers of typically-developing children. Neither perceived burden nor care needs were significantly associated with PAC (Table 3, Model 1). There were no significant interactions with caregiving condition for either of care needs or perceived burden, indicating that these primary stressors were not associated with PAC across any caregiving conditions (Supplemental Table 1).
Table 3.
Positive aspects of caregiving as a function of primary stressors and use of coping strategies (n = 214)
| Model 1 | Model 2 | Model 3a | Model 3b | Model 3c | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictors | b | SE | b | SE | b | SE | b | SE | b | SE |
|
| ||||||||||
| (Intercept) | 4.36*** | 0.11 | 4.37*** | 0.10 | 4.37*** | 0.10 | 4.37*** | 0.10 | 4.37*** | 0.11 |
| Inherited Metabolic Conditions | −0.33** | 0.12 | −0.35** | 0.12 | −0.36** | 0.12 | −0.36** | 0.12 | −0.35** | 0.12 |
| Undiagnosed Diseases | −0.48** | 0.18 | −0.49** | 0.18 | −0.53** | 0.18 | −0.49** | 0.17 | −0.50** | 0.18 |
| Participant Male | 0.00 | 0.09 | −0.01 | 0.09 | 0.00 | 0.08 | −0.00 | 0.09 | −0.01 | 0.08 |
| Participant Age (years) | −0.00 | 0.01 | −0.00 | 0.01 | 0.00 | 0.01 | −0.00 | 0.01 | 0.00 | 0.01 |
| Depressive symptoms | −0.20 | 0.13 | −0.19 | 0.12 | −0.16 | 0.12 | −0.18 | 0.12 | −0.17 | 0.12 |
| Perceived burden | −0.13 | 0.09 | −0.07 | 0.09 | −0.07 | 0.09 | −0.07 | 0.10 | −0.06 | 0.10 |
| x Emotional support | −0.04 | 0.04 | ||||||||
| x Instrumental support | 0.00 | 0.04 | ||||||||
| x Venting | −0.06 | 0.05 | ||||||||
| Care needs | 0.06 | 0.06 | 0.07 | 0.06 | 0.09 | 0.06 | 0.08 | 0.06 | 0.07 | 0.06 |
| x Emotional support | 0.10* | 0.04 | ||||||||
| x Instrumental support | 0.05 | 0.04 | ||||||||
| x Venting | 0.09* | 0.04 | ||||||||
| Emotional support | 0.00 | 0.04 | 0.01 | 0.04 | 0.01 | 0.04 | 0.00 | 0.04 | ||
| Instrumental support | 0.04 | 0.03 | 0.04 | 0.04 | 0.04 | 0.04 | 0.04 | 0.03 | ||
| Venting | −0.09* | 0.04 | −0.11* | 0.04 | −0.10* | 0.04 | −0.09 | 0.05 | ||
Notes.
p < .05;
p < .01;
p < .001.
b = unstandardized estimate.
SE = standard error.
The next model assessed the association of coping strategies with PAC (Table 3, Model 2). Emotional support coping was not significantly associated with PAC. However, a significant interaction emerged indicating that emotional support coping was more strongly associated with higher PAC among caregivers of children with undiagnosed disease (b = 0.15, p = .02) compared to caregivers of typically-developing children (Supplemental Table 1). Coping with instrumental support was not associated with PAC across any caregiving conditions. Coping through venting was negatively associated with PAC (b = −.09, p = .03), and this association did not vary by caregiving condition.
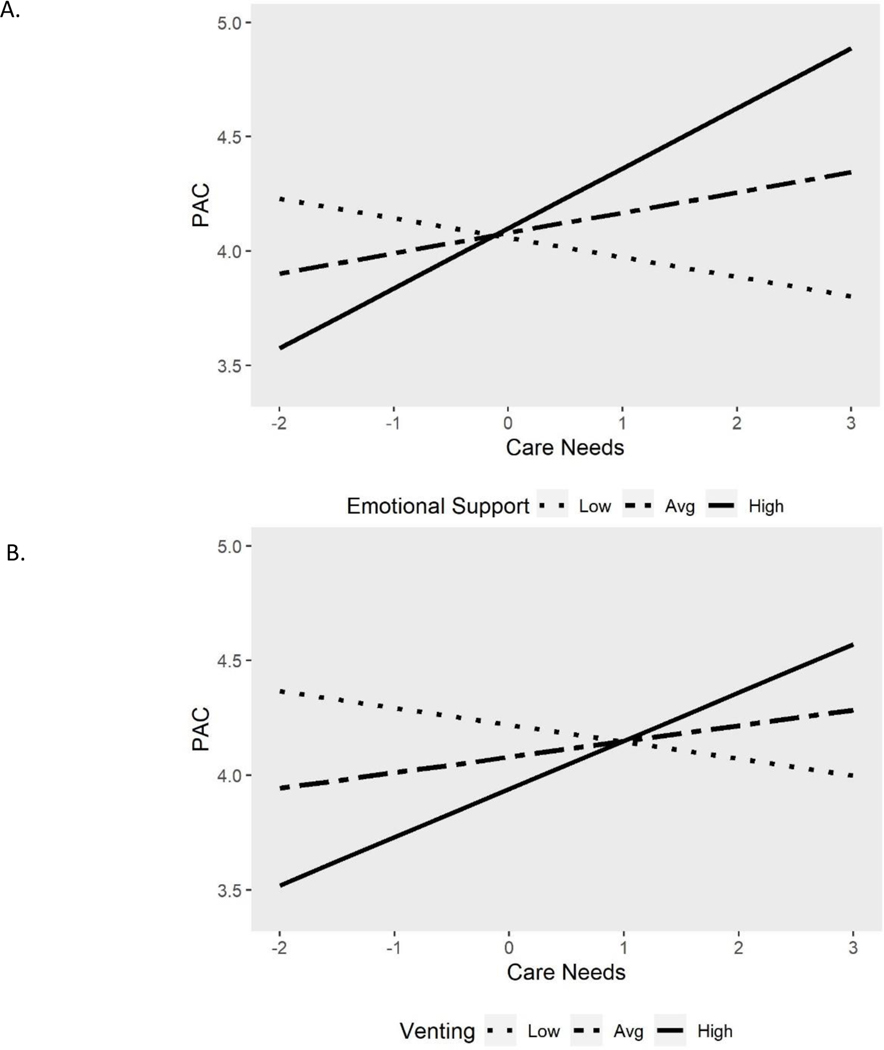
Finally, we assessed the moderating effect of coping strategies on the association between primary stressors and PAC (Table 3, Models 3a-3c). None of the coping strategies moderated the association between perceived burden and PAC. The association between care needs and PAC was significantly moderated by emotional support coping (b = 0.10, p = .01) and venting (b = 0.09, p = .03) (Figure 1). Care needs were associated with greater PAC among caregivers whose use of emotional support and venting as coping strategies was above average. These associations remained consistent across caregiving conditions, though the results of these three-way interaction models should be interpreted with caution given the sample size (Supplemental Table 2).
Figure 1.
Predicted levels of positive aspects of caregiving (PAC) as a function of affected relatives’ care needs at varying levels of caregivers’ use of emotional support (A) and use of venting (B).
Notes. Low and high refer to 1.5 standard deviations below and above the mean, respectively. Simple slopes for emotional support— low: b = −.09, CI [−.23, .06]; average: b = .09, CI [−.03, .21]; high: b = .26, CI [ .05, .48]. Simple slopes for venting low: b = −.07, CI [−.22, .07]; average: b = .07, CI [ −.05, .18]; high: b = .21, CI [.01, .41]. PAC ranges from 1 to 5.
Discussion
Positive aspects of caregiving (PAC) promote caregiver health and well-being and is understudied in the caregiving literature. Guided by the caregiving stress process model and the stress buffering hypothesis, we examined if primary caregiving stressors and coping strategies were associated with PAC and whether these associations differed based on caregiving condition. Additionally, this study investigated whether caregivers’ use of interpersonal coping strategies moderated the association between caregiving stress and PAC.
Our results indicate that primary caregiving stressors, including perceived burden or care needs of the care recipient, were not directly associated with PAC. These null findings are a departure from previous studies that have identified links between caregivers’ perceived burden and endorsement of PAC among caregivers of older adults (Carbonneau et al., 2010). Further, we did not find evidence that care needs were associated with PAC in either direction, a finding inconsistent with previous literature (Magliano et al., 2014; Pendergrass et al., 2019; Quinn and Toms, 2019). Although numerous studies indicate that greater caregiving burden and responsibilities lead to reduced caregiver well-being, our findings show that this effect is not likely attributed to diminished PAC among caregivers of typically-developing children or those with rare disease. Inconsistent findings may indicate non-linear associations such that PAC would be highest under moderate amounts of caregiving burden (Cassidy, 2013). Importantly, even after accounting for care needs and perceived burden, caregivers of children with rare disease reported significantly lower PAC than caregivers of typically-developing children. This suggests that the disparity in PAC across these different caregiving conditions does not stem from primary caregiving stress, but stress originating elsewhere.
Regarding the direct effect of coping strategies on PAC, our results indicated that caregivers’ use of instrumental support was not associated with PAC. We found that emotional support was more strongly associated with PAC for caregivers of children with undiagnosed diseases compared to caregivers of typically-developing children. Social support, especially being able to communicate with others, has been identified by rare disease caregivers as important for maintaining a positive outlook on the caregiving situation (Pelentsov et al., 2015). The uncertainty of undiagnosed conditions leaves caregivers of children with undiagnosed diseases exceptionally vulnerable to the detrimental consequences of caregiving (Yanes et al., 2017). We show that, for this subgroup of caregivers of children with rare disease, emotional support coping is an adaptive coping strategy for promoting PAC. Several existing studies have noted that use of interpersonal coping strategies was related to greater experiences of PAC (Chen and Greenberg, 2004; Willard et al., 2016; Magliano et al. 2014); thus, more research is needed on the relationship between interpersonal dimensions of coping and PAC across different caregiving conditions.
The negative association between venting and PAC was consistent with literature and with the stress process model, suggesting that venting operates differently than other interpersonal coping strategies as a dysfunctional coping strategy. Venting fails to promote caregivers’ ability to manage the stressor, but rather, discussing unpleasant feelings reinforces those feelings (Thomas et al., 2014; Wrosch et al., 2011). Venting involves the expression of negative feelings, but this form of coping does not necessarily elicit supportive reactions, such as help towards a solution or feedback that emphasizes positive experiences. In contrast, venting that is met with help or understanding then becomes instrumental or emotional support. Though caregivers may perceive venting as a viable coping strategy offering emotional release, findings from the present study suggest expressing negative feelings hinders caregivers’ ability to experience PAC.
Upon examination of the moderation model of coping, we found that among caregivers who engage greater levels of coping through either emotional support or venting, there is a strong positive association between care needs and PAC. This pattern provides evidence for buffering effects of emotional support and venting against caregiving stress. Studies suggest that more time spent caregiving and day-to-day challenges associated with care may provide caregivers with more opportunities to experience the kind of benefits associated with PAC (Magliano et al., 2014; Parveen & Morrison, 2012; Pendergrass et al., 2019). These opportunities may be made salient through use of interpersonal coping strategies. Caregivers who do not have as many care responsibilities may not have the same opportunities to find positive aspects in their caregiving role. Our findings suggest that caregivers may be most predisposed to positive caregiving experiences despite high care needs when they leverage certain coping strategies.
Implications
Findings from the present study have implications for both theory and practice. This application showcased the universality of the stress process across different caregiving conditions, including rare disease and typically-developing. In general, associations between primary stressors, coping, and PAC did not vary across the caregiving conditions that we examined. This is important when developing interventions and policies designed to support informal caregivers in terms of identifying how and when to tailor to specific contexts. It should be noted, however, that caregivers of children with rare disease consistently reported lower PAC relative to caregivers of typically-developing relatives, even after accounting for caregiving stress and coping. Thus, there are other factors that are contributing to caregivers’ evaluations of their caregiving experience that need to be identified. These may include stressors indirectly related to providing care, such as strained relationships, financial burdens, or difficulties navigating the healthcare system (Carpenter et al., 2018; Pelentsov et al., 2015; Yanes et al., 2017).
Our findings also highlighted the importance of examining different dimensions of caregiving stress and coping. For example, distinguishing between care needs and perceived burden allowed us to isolate the associations of each with PAC. Further, caregivers’ use of interpersonal coping strategies may also shape the way they appraise caregiving stressors and experience PAC, as evidenced by the moderating effects of emotional support coping and venting. Our findings on venting, in particular, pose important considerations for caregiver health. Providers should be mindful that venting may be less adaptive than other coping strategies as it reinforces caregivers’ negative feelings. However, our findings indicate that there is value in venting of emotions. Interventions that facilitate and provide structure to conversations about caregivers’ complex emotions, like support groups (Fidika et al., 2013), may allow for harnessing of the cathartic aspects of venting while minimizing the maladaptive effects.
Although this study provides evidence for some associations between coping strategies and PAC, the null findings suggest that PAC is an independent construct with the potential to promote caregiver health and well-being without being directly tied to caregivers’ evaluations of stress or use of coping strategies. One study found that mothers’ successful adaptation to caregiving over time was predicted by resilience and positive impact, rather than children’s care needs and caregiver burden (Peay et al., 2016). In addition to social support, Cassidy (2013) found that resilience, optimism, and self-efficacy were positively associated with benefit finding. Strengths-based interventions are likely to be more effective for supporting caregiver well-being than those focused on reducing burden.
Limitations and Future Directions
Due to the present study’s cross-sectional nature, we cannot make claims about the directionality of these associations. Longitudinal data would allow us to determine changes in PAC as caregivers adjust to their caregiver role and, for caregivers of relatives with rare disease, gain more knowledge of and experience with managing the illness. Parveen and Morrison (2012) demonstrated that caregiver gains remained stable over several months, but changes in other aspects of the experience, such as instrumental support, were predictive of caregiver gains. This may be especially relevant for rare disease caregivers and over longer periods of time. Longitudinal caregiving studies will better enable us to identify the contexts in which different coping strategies are most adaptive, given that most coping strategies do not follow a “one size fits all” model (Stephenson et al., 2016). Studying informal caregiving over time would also provide greater understanding of how aspects of the caregiving experience, both positive and negative, change with age and life stage.
It is also important to consider the specific measures that are used to describe the caregiving experience. Much of the inconclusiveness of the literature can be attributed to the variety of ways different constructs, like stress and support, are measured. For example, Parveen and Morrison (2012) found that it was time spent caregiving, rather than caregiving tasks, that were predictive of caregiving gains over time. The present study’s measure of care needs captured both time and number of tasks in the total score. By disentangling these distinct components of care needs to more precisely identify the sources of caregiving stress.
Additional limitations concern the generalizability of these findings. It is important to consider potential group differences in the experience of PAC. Roth and colleagues (2015) reported scale differences in PAC by race among dementia caregivers, with African American and Hispanic caregivers reporting greater PAC, and gender, with male caregivers reporting greater PAC. Although gender was accounted for in the analyses, the majority of our sample was comprised of white caregivers, so future research should include greater racial and ethnic diversity. Similarly, the limited sample size, particularly of caregivers of children with undiagnosed diseases, affects the extent to which we can conduct comparative analyses. However, by definition, rare diseases are not prevalent and families affected by them are not well represented in the caregiving literature (National Alliance for Caregiving, 2018). The present study is noteworthy in shedding light on the caregiving process among this population and highlighting areas for further inquiry.
Conclusions
Substantial research on caregiving of older adults underscores the role of PAC in caregiver well-being (Carbonneau et al., 2010), but PAC remains understudied, especially among caregivers of relatives with rare disease. The findings of this study reveal how components of the caregiving stress process are interconnected in a heterogeneous sample of caregivers, demonstrating the universality of this model. This study underscores the importance of considering multiple aspects of the caregiving experience, such as care needs of the care recipient, as most coping strategies are seldom globally adaptive (Stephenson et al., 2016). Our results also suggest that interventions that encourage use and availability of emotional support or those that elicit support from venting promote PAC, particularly for the most burdened caregivers. Overall, this study provides a foundation for more nuanced investigations of PAC in caregivers of children with chronic illnesses ultimately aimed at enhancing the health and well-being of these caregivers and their families.
Supplementary Material
Funding:
This research was supported by funding from the Intramural Research Program of the National Human Genome Research Institute (Grant ZIAHG20335)
Footnotes
Author details: JM was responsible for study design, interpretation of results, and drafting of manuscript. SS and HD were responsible for data management, data analysis, and drafting of manuscript. MG and MAG were responsible for data management and drafting of manuscript. LK provided supervision and edited the manuscript.
Disclosure statement: No conflicts of interest to report.
Data availability statement:
Data are available upon reasonable request to the authors.
References
- Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, & O’donnell M (2001). The Zarit Burden Interview: A new short version and screening version. Gerontologist. 10.1093/geront/41.5.652 [DOI] [PubMed] [Google Scholar]
- Bermejo-Toro L, Sánchez-Izquierdo M, Calvete E, & Roldán MA (2020). Quality of life, psychological well-being, and resilience in caregivers of people with acquired brain injury (ABI). Brain Injury, 34(4), 480–488. 10.1080/02699052.2020.1725127 [DOI] [PubMed] [Google Scholar]
- Carbonneau H, Caron C, & Desrosiers J (2010). Development of a conceptual framework of positive aspects of caregiving in dementia. Dementia, 9(3), 327–353. 10.1177/1471301210375316 [DOI] [Google Scholar]
- Cardinali P, Migliorini L, & Rania N (2019). The caregiving experiences of fathers and mothers of children with rare diseases in Italy: Challenges and social support perceptions. Frontiers in Psychology, 10(JULY), 1–14. 10.3389/fpsyg.2019.01780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter K, Wittkowski A, Hare DJ, Medford E, Rust S, Jones SA, & Smith DM (2018). Parenting a child with Phenylketonuria (PKU): An Interpretative Phenomenological Analysis (IPA) of the experience of parents. Journal of Genetic Counseling, 27(5), 1074–1086. 10.1007/s10897-018-0227-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS (1997). You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine. 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, & Weintraub JK (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56(2), 267–283. 10.1037/0022-3514.56.2.267 [DOI] [PubMed] [Google Scholar]
- Cassidy T (2013). Benefit finding through caring: The cancer caregiver experience. Psychology and Health, 28(3), 250–266. 10.1080/08870446.2012.717623 [DOI] [PubMed] [Google Scholar]
- Chen F, & Greenberg JS (2004). A positive aspect of caregiving: The influence of social support on caregiving gains for family members of relatives with schizophrenia. Community Mental Health Journal, 40(5), 423–435. 10.1023/B:COMH.0000040656.89143.82 [DOI] [PubMed] [Google Scholar]
- Cohen CA, Colantonio A, & Vernich L (2002). Positive aspects of caregiving: Rounding out the caregiver experience. International Journal of Geriatric Psychiatry, 17(2), 184–188. 10.1002/gps.561 [DOI] [PubMed] [Google Scholar]
- Cohen S, & McKay G (1984). Social support, stress, and the buffering hypothesis: A theoretical analysis. In Handbook of psychology and health (Vol. 4, Issues 5–6, pp. 253–267). 10.1387/ijdb.082595mg [DOI] [Google Scholar]
- Cooper C, Katona C, & Livingston G (2008). Validity and reliability of the brief cope in carers of people with dementia: The LASER-AD study. Journal of Nervous and Mental Disease, 196(11), 838–843. 10.1097/NMD.0b013e31818b504c [DOI] [PubMed] [Google Scholar]
- Dickson A, O’Brien G, Ward R, Flowers P, Allan D, & O’Carroll R (2012). Adjustment and coping in spousal caregivers following a traumatic spinal cord injury: An interpretative phenomenological analysis. Journal of Health Psychology, 17(2), 247–257. 10.1177/1359105311411115 [DOI] [PubMed] [Google Scholar]
- Fekete C, Tough H, Siegrist J, & Brinkhof MWG (2017). Health impact of objective burden, subjective burden and positive aspects of caregiving: an observational study among caregivers in Switzerland. BMJ Open, 7(12), e017369. 10.1136/bmjopen-2017-017369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fidika A, Salewski C, & Goldbeck L (2013). Quality of life among parents of children with phenylketonuria (PKU). Health and Quality of Life Outcomes, 11(1), 1–9. 10.1186/1477-7525-11-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover S, Bhadada S, Kate N, Sarkar S, Bhansali A, Avasthi A, Sharma S, & Goel R (2016). Coping and caregiving experience of parents of children and adolescents with type-1 diabetes: An exploratory study. Perspectives in Clinical Research, 7(1), 32. 10.4103/2229-3485.173776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer BJ (1993). Expanding the conceptualization of caregiver coping: The importance of relationship-focused coping strategies. Family Relations, 42(4), 383–391. http://www.jstor.org/stable/585338?seq=1#page_scan_tab_contents [Google Scholar]
- Lee Y, & Choi S (2013). Korean American dementia caregivers’ attitudes toward caregiving: The role of social network versus satisfaction with social support. Journal of Applied Gerontology, 32(4), 422–442. 10.1177/0733464811431163 [DOI] [PubMed] [Google Scholar]
- Lewis C, Skirton H, & Jones R (2010). Living without a diagnosis: The parental experience. Genetic Testing and Molecular Biomarkers, 14(6), 807–815. 10.1089/gtmb.2010.0061 [DOI] [PubMed] [Google Scholar]
- López J, López-Arrieta J, & Crespo M (2005). Factors associated with the positive impact of caring for elderly and dependent relatives. Archives of Gerontology and Geriatrics, 41(1), 81–94. 10.1016/j.archger.2004.12.001 [DOI] [PubMed] [Google Scholar]
- Magliano L, Patalano M, Sagliocchi A, Scutifero M, Zaccaro A, D’Angelo MG, Civati F, Brighina E, Vita G, Vita GL, Messina S, Sframeli M, Pane M, Lombardo ME, Scalise R, D’Amico A, Colia G, Catteruccia M, Balottin U, … Politano L (2014). “I have got something positive out of this situation”: Psychological benefits of caregiving in relatives of young people with muscular dystrophy. Journal of Neurology, 261(1), 188–195. 10.1007/s00415-013-7176-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maine DHHS, & Children’s Behavioral Health Services. (2011). Children’s Habilitation Assessment Tool (CHAT). [Google Scholar]
- Markoulakis R, Fletcher P, & Bryden P (2012). Seeing the glass half full: Benefits to the lived experiences of female primary caregivers of children with autism. Clinical Nurse Specialist. 10.1097/NUR.0b013e31823bfb0f [DOI] [PubMed] [Google Scholar]
- McConkie-Rosell A, Hooper SR, Pena LDM, Schoch K, Spillmann RC, Jiang YH, Cope H, Palmer C, & Shashi V (2018). Psychosocial profiles of parents of children with undiagnosed diseases: Managing well or just managing? Journal of Genetic Counseling, 27(4), 935–946. 10.1007/s10897-017-0193-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morimoto H, Furuta N, Kono M, & Kabeya M (2019). Stress-buffering Effect of Coping Strategies on Interrole Conflict among Family Caregivers of People with Dementia. Clinical Gerontologist, 42(1), 34–46. 10.1080/07317115.2017.1368764 [DOI] [PubMed] [Google Scholar]
- Mosher CE, Adams RN, Helft PR, O’Neil BH, Shahda S, Rattray NA, & Champion VL (2017). Positive changes among patients with advanced colorectal cancer and their family caregivers: a qualitative analysis. Psychology and Health, 32(1), 94–109. 10.1080/08870446.2016.1247839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance for Caregiving. (2018). Rare disease caregiving in America (Issue February). 10.1097/01.cot.0000471986.11116.76 [DOI]
- Parveen S, & Morrison V (2012). Predicting caregiver gains: A longitudinal study. British Journal of Health Psychology, 17(4), 711–723. 10.1111/j.2044-8287.2012.02067.x [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, & Skaff MM (1990). Caregiving and the stress process: An overview of concepts and their measures. Gerontologist, 30(5), 583–594. 10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Peay HL, Meiser B, Kinnett K, Furlong P, Porter K, & Tibben A (2016). Mothers’ psychological adaptation to Duchenne/Becker muscular dystrophy. European Journal of Human Genetics, 24(5), 633–637. 10.1038/ejhg.2015.189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelentsov LJ, Laws TA, & Esterman AJ (2015). The supportive care needs of parents caring for a child with a rare disease: A scoping review. Disability and Health Journal, 8(4), 475–491. 10.1016/j.dhjo.2015.03.009 [DOI] [PubMed] [Google Scholar]
- Pendergrass A, Mittelman M, Graessel E, Özbe D, & Karg N (2019). Predictors of the personal benefits and positive aspects of informal caregiving. Aging & Mental Health, 23(11), 1533–1538. 10.1080/13607863.2018.1501662 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31(4), 437–448. 10.3102/10769986031004437 [DOI] [Google Scholar]
- Pruchno RA, & Resch NL (1989). Mental health of caregiving spouses: coping as mediator, moderator, or main effect? Psychology and Aging, 4(4), 454–463. 10.1037/0882-7974.4.4.454 [DOI] [PubMed] [Google Scholar]
- Quinn C, & Toms G (2019). Influence of positive aspects of dementia caregiving on caregivers’ well-being: A systematic review. The Gerontologist, 59(5), e584–e596. 10.1093/geront/gny168 [DOI] [PubMed] [Google Scholar]
- Raina P, O’Donnell M, Rosenbaum P, Brehaut J, Walter SD, Russell D, Swinton M, Zhu B, & Wood E (2005). The health and well-being of caregivers of children with cerebral palsy. Pediatrics, 115(6). 10.1542/peds.2004-1689 [DOI] [PubMed] [Google Scholar]
- Roth DL, Dilworth-Anderson P, Huang J, Gross AL, & Gitlin LN (2015). Positive aspects of family caregiving for dementia: Differential item functioning by race. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 70(6), 813–819. 10.1093/geronb/gbv034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senger BA, Ward LD, Barbosa-Leiker C, & Bindler RC (2016). The parent experience of caring for a child with mitochondrial disease. Journal of Pediatric Nursing, 31(1), 32–41. 10.1016/j.pedn.2015.08.007 [DOI] [PubMed] [Google Scholar]
- Stephenson E, King DB, & DeLongis A (2016). Coping Process. In Stress: Concepts, Cognition, Emotion, and Behavior (pp. 359–364). Elsevier. 10.1016/B978-0-12-800951-2.00045-5 [DOI] [Google Scholar]
- Tarlow BJ, Wisniewski SR, Belle SH, Rubert M, Ory MG, & Gallagher-Thompson D (2004). Positive aspects of caregiving: Contributions of the REACH project to the development of new measures for Alzheimer’s caregiving. Research on Aging, 26(4), 429–453. 10.1177/0164027504264493 [DOI] [Google Scholar]
- Thomas PT, Rajaram P, & Nalini A (2014). Psychosocial challenges in family caregiving with children suffering from Duchenne Muscular Dystrophy. Health & Social Work, 39(3), 144–152. 10.1093/hsw/hlu027 [DOI] [PubMed] [Google Scholar]
- Wrosch C, Amir E, & Miller GE (2011). Goal adjustment capacities, coping, and subjective well-being: The sample case of caregiving for a family member with mental illness. Journal of Personality and Social Psychology, 100(5), 934–946. 10.1037/a0022873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanes T, Humphreys L, McInerney-Leo A, & Biesecker B (2017). Factors associated with parental adaptation to children with an undiagnosed medical condition. Journal of Genetic Counseling, 26(4), 829–840. 10.1007/s10897-016-0060-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, Gao J, Li X, Yang Q, Lian Y, Xiao H, & Huang W (2019). Burden, positive aspects, and predictive variables of caregiving: A study of caregivers of patients with pediatric glaucoma. Journal of Ophthalmology, 2019, 1–7. 10.1155/2019/6980208 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request to the authors.