Background:
To conduct a systematic review of the efficacy of Chinese herbal bath therapy on children with Atopic dermatitis.
Methods:
We searched Chinese databases (CNKI, VIP, and Wanfang) and English databases (PubMed, Embase, Web of science, Cochrane library) for studies from the establishment of the database to September 2022. The included literature was randomized control studies investigating the treatment of Atopic dermatitis in children by Chinese herbal bath therapy. The outcomes included the cure rate, scoring atopic dermatitis (SCORAD) index, adverse reactions and recurrence rate. RevMan 5.4 was used to analyze the extracted data.
Results:
A total of 8 related studies were included containing 854 cases. The meta-analysis showed that Chinese herbal bath therapy group was superior to control group in terms of cure rate, SCORAD index, adverse reactions and recurrence rate in children with Atopic dermatitis [RR = 1.11, 95%(1.02, 1.21), P = .01; SMD = –0.77, 95%(-0.99, -0.55), P < .00001; RR = 0.44, 95%CI(0.28,0.67), P = .0002; RR = 0.25, 95%CI(0.10, 0.59), P = .0002].
Conclusion:
The present study shows that Chinese herbal bath therapy is an effective treatment for children with Atopic dermatitis in China.
Keywords: atopic dermatitis, children, Chinese herbal bath therapy, meta-analysis
1. Introduction
Atopic dermatitis (AD) is a chronic inflammatory skin disease characterized by intense itching and recurrent eczema-like lesions. Since the 1970s, the incidence of AD in industrialized countries has increased by 2 to 3 times, affecting about 15% to 20% of children and 1% to 3% of adults, becoming 1 of the most common skin diseases in children.[1–3] AD onset is the most common to 3 and 6 months of age, with approximately 60% of patients developing the eruption in the first year of life and 90% by 5 years of age.[4] Twenty percent of children who develop AD before the age of 2 will have persistent symptoms; 17% of people have intermittent symptoms by age 7, and only 16.8% of AD patients develop after puberty.[5] The etiology and pathogenesis of atopic dermatitis have not been clarified, but current studies have shown that they are closely related to family genetics, environmental factors, modern lifestyles, environmental exposure and psychological factors.[6] The symptoms of itching and sleep disorders caused by recurrent episodes of AD seriously affect the growth and development of the child, while affecting the quality of daily life and causing other psychosocial problems.[7,8] It also brings a heavy financial burden on the families and societies.[3] Therefore, there is an urgent need to conduct research evaluations to find more effective treatment strategies for AD in children.
According to the guidelines of care for the management of atopic dermatitis developed by the American Academy of Dermatology in 2014, the treatment of AD usually includes 5 parts: topical therapy, phototherapy, systemic medication, prevention of disease onset, and adjuvant therapy.[5,9–11] Pharmacotherapy is still the first choice in the current treatment plan, such as glucocorticoids, antihistamines, immunosuppressants, et cetera. However, none of these drugs can completely cure AD. Moreover, long-term use of these drugs will have greater side effects and high recurrence rates, which are unacceptable to patients.[12] As a result, many researchers are looking for other effective treatments from complementary and alternative medicine therapies.
Chinese herbal bath therapy is an important part of traditional Chinese medicine and has a long history as a traditional diagnosis/treatment method of complementary and alternative medicine therapy. According to the theory of traditional Chinese medicine, Chinese herbal bath therapy can achieve a satisfactory effect by penetrating the drugs with warm effect into the skin, meridian points and blood vessels. At the same time, it can play an important role in regulating the function of the internal organs and helping to correct and dispel evil. Modern medical research has found that Chinese herbal solutions can not only play antibacterial and anti-inflammatory effects directly on the surface of the body, but also can be absorbed by sweat glands, mucous membranes, capillaries, et cetera to produce local or systemic therapeutic effects.[13,14] In addition, the nerve endings receptors under the skin can reflexively regulate the functioning of nerves, body fluids and circulation after being stimulated by Chinese herbal liquids, thereby improving the body’s disease resistance and repair ability.[15] In recent years, Chinese herbal bath therapy has been widely used in the treatment of children’s atopic dermatitis. By combining traditional Chinese medicine decoction with bathing, the drug plays a role in reducing inflammation, improving microcirculation, and promoting the resolution of skin lesions by acting on the skin, and achieving a relatively satisfactory effect.[16,17]
Previous studies have shown that Chinese herbal bath therapy has a good therapeutic effect on AD. From the perspective of safety and comfort, it is more suitable for children than other treatment methods.[18–20] However, there are no systematic review studies specifically for the treatment of AD in children with Chinese herbal bath therapy. Therefore, we conducted systematic reviews and meta-analyses of Chinese herbal bath therapy for the treatment of AD in children to evaluate its efficacy and safety. Our goal is to fill this research gap by seeking the latest evidence available to researchers, physicians and patients.
2. Methods
2.1. Ethics statement
Our study protocol has been registered in the PROSPERO and the registration number is CRD42022359138. As all analyses in our article were based on previously published studies, no ethical approval or patient consent was required.
2.2. Literature search
The Cochrane and grading of recommendations, assessment, development and evaluation approaches[21,22]were used to guide the conduct of this review. This review was prospectively registered (PROSPERO CRD42022359138). This study was reported in accordance to Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. Scientific databases (PubMed, Embase, Web of Science, Cochrane library, VIP, CNKI, Wanfang) were comprehensively searched to identify relevant literature without language restriction. Relevant keywords, medical terms and titles include Dermatitis, Atopic, children, bath, hydrotherapy, and randomized controlled trials. The search results included original research papers published in online journals. Specific search method, Appendix 1, Supplemental Digital Content, http://links.lww.com/MD/H990.
2.3. Inclusion and exclusion criteria
According to the aims of the study, the inclusion criteria were as follows: the included population should meet the diagnostic criteria for AD[5]; age < 18 years old; Chinese herbal bath therapy intervention is the main therapeutic approach; randomized controlled trials; complete original data.
Exclusion criteria were as follows: conference abstracts and systematic reviews; repeated publications; animal experiments or non-clinical experiments; articles with unreasonable experimental design; full text was not available.
2.4. Data selection and data extraction
First, all literature was screened using End-Note 9.0 software according to the preset inclusion/exclusion criteria, and any duplicated literature from different databases was removed. Then, any obviously irrelevant literature was excluded based on the title and abstract. Finally, the full text of all remaining literature was read intensively, and those papers conforming to the requirements were included (Fig. 1). The data were extracted independently by 2 investigators; a cross-check was made. Any disagreement was settled through discussion or the arbitration of a third investigator.
Figure 1.
PRISMA flow diagram.
The following data were extracted from each eligible study: first author, year, study types, country, number of participants, age, gender, course, intervention, period of treatment, follow-up time, cure rate, scoring atopic dermatitis (SCORAD) index, adverse reactions and recurrence rate.
2.5. Risk of bias assessment
The Cochrane Risk of Bias tool[23] was applied to assess the quality of the included randomized controlled trial (RCTs), including sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other potential threats to validity. Studies were rated on each variable as low risk, high risk, or unclear risk of bias. If a study received “high risk” judgment in any 1 domain, it would be classified as “high risk of bias.” Two independent assessors conducted quality assessment, and any disagreement was settled by reaching a consensus or consulting a third researcher.
2.6. Statistical analysis
RevMan 5.4 supplied by the Cochrane net was used in this meta-analysis. The pooled enumeration data was expressed as relative risk (RR) and 95% confidence interval (CI). The pooled continuous variables were expressed as mean standard deviation (MD) and 95% CI Operation. P < .05 was used as the standard to determine the difference to be statistically significant. Q test (P value) and chi-square test (I2) were used to determine the heterogeneity. If the test results indicated that there was no significant heterogeneity (P ≥ .1, I2 < 50%), the fixed-effects model was used for analysis. When there is statistical heterogeneity between studies (P < .1, I2 > 50%), a random effect model is used, and a sensitivity analysis is performed to exclude studies that can cause heterogeneity, and then a meta-analysis is performed. When the included literature > 10, a funnel plot was used to test for publication bias.
3. Results
3.1. Literature search and screening
A total of 1076 articles were initially retrieved, and 761 articles were selected after removing duplicated publication. A total of 176 articles were removed by reading the title and abstract. After reading the full text, 12 articles were removed due to incomplete results, unavailable data, and low quality of the literature, and 8 articles were finally involved in this analysis[24–31] with a total of 854 patients. The flow chart of literature search is shown in Figure 1.
The trial group was treated with Chinese herbal bath, which contained a total of 28 kinds of Chinese herbal medicines, and each prescription ranged from 4 to 14 kinds. The Chinese herbal medicines and functions commonly used in the 8 Chinese herbal baths are shown in Table 1. Nine kinds of Chinese herbal medicines (Phellodendri Amurensis Cortex, Portulaca oleracea, Millettia dielsiana, Rhubarb, Salviae Miltiorrhizae, Akebiae Caulis, Herba Agastaches, Clove, Honeysuckle Flower) claimed anti-inflammatory effects. Nine kinds of traditional Chinese medicine (LargeheadAtractylodesRhizome, Poria, Chinese Angelica, Radix Paeoniae Rubra, Divaricate Saposhniovia, Schizonepetae Herba, CoixSeed, Licorice, Clematidis Radix Et Rhizoma) claimed an efficacy of regulating immunity. Seven kinds of Chinese herbal medicines (Cortex Dictamni, Sophora flavescens, Common Cnidium Fruit, Sessile Stemona Root, Glabrous Greenbrier Rhizome, Fructus Tribuli, Aluminum potassium sulfate) claimed an efficacy of relieving itch. Three kinds of Chinese herbal medicines (Kochiae Fructus, Sanguisorbae Radix, Artemisiae Argyi Folium) claimed an efficacy of anti-allergy. The treatment duration in Chinese herbal bath therapy is 10 to 15 minutes each time, 1 to 2 times a day. The control group mostly used Tacrolimus ointment, Hydrocortisone butyrate cream or Fluticasone propionate cream for topical treatment 1 to 2 times a day. Both groups were treated for 2 to 4 weeks.
Table 1.
Chinese herbs and efficacy according to the frequency of usage.
| English name | Latin name | Chinese Pinyin name | Frequency of usage |
|---|---|---|---|
| Anti-inflammatory | |||
| Phellodendri Amurensis Cortex | Phellodendron amurense Rupr | Huangbo | 7 |
| Portulaca oleracea | Portulaca oleracea L | Machixian | 6 |
| Millettia dielsiana | Kadsura interior | Jixueteng | 4 |
| Rhubarb | Rheum officinale | Dahuang | 3 |
| Salviae Miltiorrhizae | Salvia miltiorrhiza Bunge | Danshen | 3 |
| Honeysuckle Flower | Lonicera japonica Thunb | Jinyinhua | 2 |
| Akebiae Caulis | Akebiae Caulis | Mutong | 1 |
| Herba Agastaches | Agastacherugosa | Huoxiang | 1 |
| Clove | Syzygium aromaticum | Dingxiang | 1 |
| Regulating immunity | |||
| LargeheadAtractylodesRhizome | Atractylodes macrocephala | Baizhu | 3 |
| Poria | Poria | Fuling | 3 |
| Chinese Angelica | Angelicae Sinensis Radix | Danggui | 3 |
| Radix Paeoniae Rubra | Radix Paeoniae Rubra | Chishao | 2 |
| Divaricate Saposhniovia | Saposhnikovia divaricata | Fangfeng | 2 |
| Schizonepetae Herba | FineleafSchizonepetaHerb | Jingjie | 2 |
| CoixSeed | Semen Coicis | Yiyiren | 1 |
| Licorice | Glycyrrhiza uralensis Fisch | Gancao | 1 |
| Clematidis Radix Et Rhizoma | Clematidis Radix et Rhizoma | Weilingxian | 1 |
| Relieving itch | |||
| Cortex Dictamni | Cortex Dictamni | Baixianpi | 4 |
| Sophora flavescens | Sophora flavescens | Kushen | 4 |
| Common Cnidium Fruit | Cnidium monnieri Cuss | Shechuangzi | 2 |
| Sessile Stemona Root | Stemona japonica | Baibu | 1 |
| Glabrous Greenbrier Rhizome | Smilax glabra | Tufuling | 1 |
| Fructus Tribuli | Tribulus terrestris L | Jili | 1 |
| Aluminum potassium sulfate | Alumen | Kufan | 1 |
| Anti-allergy | |||
| Kochiae Fructus | Kochia scoparia | Difuzi | 3 |
| Sanguisorbae Radix | Sanguisorba officinalis L | Diyu | 1 |
| Artemisiae Argyi Folium | Artemisia argyi | Aiye | 1 |
3.2. Basic characteristics and quality evaluation of the included literature
The 8 studies included in this analysis were all randomized controlled studies published in Chinese. A total of 854 subjects were included, among which 415 subjects were in the experimental group and 439 in the control group. The detailed characteristics of the literature are shown in Table 2. The plot for risk of bias is shown in Figure 2.
Table 2.
Basic information of the included literature.
| Number | Year | Author | Study Types | Country | Cases | Ages(mean ± sd) | Gender (Male/female) |
Course | Intervention | Period of treatment | Follow-up time | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T | C | T | C | T | C | T | C | T | C | |||||||
| 1 | 2019 | Li Pengying[24] | RCT | China | 35 | 35 | 6.6 ± 1.1 yr | 6.4 ± 1.3 yr | 22/13 | 20/15 | 1.6 ± 0.3 yr | 1.4 ± 0.5 yr | Chinese herbal bath based on treatment of the control group | external application of 0.03% Tacrolimus ointment | 4 w |
- |
| 2 | 2017 | Xu Jianqing[25] | RCT | China | 53 | 54 | 6.5 ± 2.3 yr | 7.1 ± 1.9 yr | 38/15 | 35/19 | 0.9 ± 0.3 yr | 0.8 ± 0.2 yr | Chinese herbal bath based on treatment of the control group | external application of Hydrocortisone butyrate cream | 2 mon |
- |
| 3 | 2012 | Yang Lijun[26] | RCT | China | 60 | 60 | 1.2 ± 0.09 yr | 1.1 ± 0.1 yr | 31/29 | 30/30 | 17 ± 0.45 d | 18 ± 0.39 d | Chinese herbal bath | external application of Hydrocortisone butyrate cream | 3d, 15d | |
| 4 | 2016 | Huang Wenhui[27] | RCT | China | 34/34 | 34 | 6.3 ± 2.2/6.5 ± 2 yr | 6.6 ± 2.3 yr | 19/1518/16 | 20/14 | - | - | Chinese herbal bath based on treatment of the control group | external application of 0.05% Desonide ointment or Tacrolimus ointment | 3 w |
3 mon |
| 5 | 2021 | Huang Wenxin[28] | RCT | China | 30 | 38 | 10.6 ± 2.51 yr | 9.33 ± 2.8 yr | 18/12 | 23/15 | - | - | Chinese herbal bath based on treatment of the control group | external application of Tacrolimus ointment | 2‐3 mon |
|
| 6 | 2013 | Han Haijun[29] | RCT | China | 22 | 23 | 10 ± 2.56 yr | 9.61 ± 2.64 yr | 12/10 | 13/10 | - | - | Chinese herbal bath based on treatment of the control group | external application of Tacrolimus ointment | 4 w |
3 mon |
| 7 | 2021 | Chen Hanqiang[30] | RCT | China | 31 | 31 | 15.89 ± 2.1 yr | 16.12 ± 2.05 yr | 21/10 | 20/11 | - | - | Chinese herbal bath | external application of Fluticasone propionate cream | 4 w |
- |
| 8 | 2020 | Zhu Jie[31] | RCT | China | 140 | 140 | 5.95 ± 0.75 yr | 5.44 ± 0.62 yr | 94/46 | 96/44 | 11.87 ± 1.75 mon | 11.41 ± 0.69 mon | Chinese herbal bath based on treatment of the control group | external application of Hydrocortisone butyrate ointment and mustela stelatopia emollient cream | 2 w |
- |
RCT = randomized controlled trial.
Figure 2.
Risk of bias summary and graph.
3.3. Meta-analysis results
3.3.1. Cure rate.
There were 8 studies[24–31] mentioning the cure rate of the 2 groups which was presented as dichotomous variables. The random-effects model (I2 = 63%, P = .009) was used to pool the effect size. The pooled results showed that the difference between the 2 groups was statistically significant [RR = 1.11, 95%CI (1.02, 1.21), P = .01] (Fig. 3A). However, the heterogeneity between groups was obvious for the effective meta-analysis. We correspondingly excluded individual documents 1 by 1 for a sensitivity analysis. The results showed that the heterogeneity was significantly reduced (P = .07, I2 = 48%) while Huang Wenhui’s literature was deleted. Though, this paper was stripped out when analyzing efficiency and the fixed-effects model was used to pool the effect size. Finally, the results of the meta-analysis were not affected [RR = 1.14, 95% (1.04, 1.24), P = .004] (Fig. 3B). The meta-analysis results presented that the effect of Chinese herbal bath therapy was significantly superior to the control group in AD. Since the number of documents is < 10, we did not make funnel charts for analysis.
Figure 3.
Forest plot and sensitivity analysis of meta-analysis on Cure rate.
3.3.2. Severity scoring of AD.
A total of 6 papers[24,25,27–29,31] reported improvements in AD severity score. Five of the studies evaluated AD severity by SCORAD index, involving a total of 632 samples, of which 311 were in the trial group and 321 in the control group. One study[27] evaluated the severity of AD by eczema area and severity index score, involving a total of 102 samples, of which 68 were in the trial group and 34 in the control group. Because there was only 1 document using eczema area and severity index as the evaluation indicator, the data were insufficient, so only 5 articles with SCORAD index as criteria were meta-analyzed. The random-effects model (I2 = 31%, P = .21) was used to pool the effect size. The pooled results showed that the difference between the 2 groups was statistically significant [SMD = -0.77, 95%CI(-0.99, -0.55), P < .00001] (Fig. 4). The meta-analysis results presented that the effect of Chinese herbal bath therapy was significantly superior to that of the control group in improving SCORAD index.
Figure 4.
Forest plot of meta-analysis on SCORAD index. SCORAD = scoring atopic dermatitis.
3.3.3. Adverse reactions.
In the included articles, 5 studies[24,27–30] mentioned the occurrence of adverse reactions, which reported the number of adverse reactions and specific symptoms of adverse reactions in the trial and control groups, such as burning sensation, mild tingling, papules and dry skin. All literature reported on the incidence of adverse reactions was expressed as dichotomous variables. The fixed-effects model (I2 = 33%, P = .20) was used to pool the effect size. The pooled results showed that the difference between the 2 groups was statistically significant [RR = 0.44, 95%CI(0.28,0.67), P = .0002] (Fig. 5). The meta-analysis results presented that the effect of Chinese herbal bath therapy was significantly superior to that of the control group in adverse reactions.
Figure 5.
Forest plot of meta-analysis on adverse reactions.
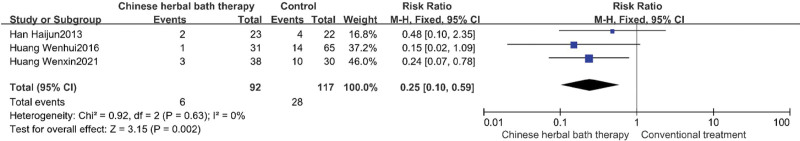
3.3.4. Recurrence rate.
A total of 3 studies[27–29] reported recurrence rates as an outcome indicator. All literature reported on the recurrence was expressed as dichotomous variables. The fixed-effects model (I2 = 0%, P = .63) was used to pool the effect size. The pooled results showed that the difference between the 2 groups was statistically significant [RR = 0.25, 95%CI(0.10,0.59), P = .0002] (Fig. 6). The meta-analysis results presented that the effect of Chinese herbal bath therapy was significantly superior to that of the control group in recurrence rate.
Figure 6.
Forest plot of meta-analysis on recurrence rate.
4. Discussion
This first systemic review and meta-analysis of 8 RCTs in 854 individuals indicate that Chinese herbal bath therapy has greater beneficial effects than control group treatment for AD in children. Overall, Chinese herbal bath therapy appears to be safe and effective for children who suffer with AD.
The etiology and pathogenesis of atopic dermatitis are complex and have not been fully elucidated but are closely related to various factors such as genetics, immunity, environment, and infection. Pharmacological treatment of AD includes systemic drugs (antihistamines and anti-inflammatory mediators, anti-infective drugs, glucocorticoids, immunosuppressants, traditional Chinese medicine, etc.) and topical drugs (moisturizers, glucocorticoids, calcineurin inhibitors, antimicrobial preparations, antipruritics, etc.), the main purpose is to reduce recurrence and relieve clinical symptoms such as pruritus. Some of these treatments have the disadvantages of high side effects, slow onset, and high price, such as long-term topical glucocorticoid preparations that can lead to local skin atrophy and telangiectasia.[32,33] Due to the risk of long-term medication coupled with the recurrence of the disease, the patient’s compliance and confidence in curing the disease is greatly reduced. At present, although the mechanism of action of Chinese herbal bath therapy in the treatment of AD has not been elucidated, it has the characteristics of hyperthermia and medicinal therapy, which can accelerate blood circulation by dilating capillaries, thereby promoting the transcutaneous absorption of drugs directly on the site of the lesion and giving full play to the therapeutic role.[14] Most of the Chinese herbal medicines selected in Chinese herbal bath have anti-inflammatory, anti-allergic and immunomodulatory effects, and work synergistically through multiple targets and multiple pathways. Studies have confirmed that Chinese medicine can play a therapeutic role by acting on immune response, skin barrier function, neuro-endocrine-immune system, microbial flora, et cetera.[34–36]
This article systematically reviews the clinical efficacy and safety of Chinese herbal bath therapy in the treatment of AD in children. Eight studies were selected to evaluate the clinical efficacy from multiple perspectives, such as cure rate, recurrence rate, incidence of adverse reactions, and AD severity score (SCORAD). The results showed that the effective rate of Chinese herb bath therapy was higher than that of conventional treatment. While performing the efficiency analysis, there was significant heterogeneity between studies. Therefore, the method of excluding documents 1 by 1 was adopted to perform a sensitivity analysis, and homogeneity between studies was significantly increased while removing the research of Huang Wenhui. At this time, the cure rate of the Chinese herb bath group was still significantly higher than that of the control group. The reason this article affects homogeneity may be that this study had 2 control groups with different treatment and 2 sets of data were merged together after we re-read Huang Wenhui’s research. In addition, the SCORAD index, recurrence rate and incidence of adverse reactions of Chinese herb bath therapy group are significantly lower than control group. According to the available evidence, Chinese herbal bath therapy can significantly improve the symptoms of skin lesions, itching and other symptoms, reduce the number of AD attacks, and can avoid the side effects of oral drugs on the body to a certain extent.[37] However, in most studies, the intervention of experimental group was Chinese herbal bath therapy based on conventional treatment. Therefore, the available evidence suggests that Chinese herbal bath can only be used as an adjunct therapy, and cannot yet be used as a monotherapy for AD.
It is important to note that our study still had certain limitations: The included literature was of low quality; the generation of random allocation sequences and the concealment of randomization protocols were not reported in some studies; the conditions of dropout and withdrawal from the study were not described in detail; These studies were short-term, whose treatment did not exceed 8 weeks; therefore, longer duration of follow-ups is needed in the future research; The publication bias, which was caused by all the studies being published in China, may exaggerate the efficacy of Chinese herbal bath therapy to some extent; The included RCTs were all single-center studies, and the sample size of the experimental studies was relatively small, which made the research results lack reliability; There were some discrepancies in the interventions of the control groups in the trials. Consequently, the efficacy of Chinese herbal bath therapy for AD needs to be further confirmed by more well-designed, large-scale clinical trials.
5. Conclusion
The present study shows that Chinese herbal bath therapy is an effective treatment for children with AD in China, especially in relieving clinical symptoms and reducing recurrence. Due to the limitations of the study, further research should be conducted in the future with rigorous design, large sample size, sham/placebo control or blank/waiting control, and accurate report to support the evidence of Chinese herbal bath therapy of AD in children.
Author contributions
Methodology: Zheng Guo, Yiming Hou, Guangxia Pan.
Supervision: Zheng Guo, Youpeng Wang.
Writing – original draft: Zheng Guo, Yongjun Li.
Writing – review & editing: Zheng Guo, Yongjun Li, Yuan Liang, Xiuying Si, Yijie Wang, Qihui Hu.
Supplementary Material
Abbreviations:
- AD =
- atopic dermatitis
- RCT =
- randomized controlled trial
- SCORAD =
- scoring atopic dermatitis
Supplemental Digital Content is available for this article.
The authors have no funding and conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
How to cite this article: Guo Z, Li Y, Hou Y, Wang Y, Liang Y, Si X, Pan G, Wang Y, Hu Q. Chinese herbal bath therapy for the treatment of Atopic dermatitis in children: A meta-analysis and systematic review. Medicine 2022;101:47(e31923).
Contributor Information
Yongjun Li, Email: 1531323122@qq.com.
Youpeng Wang, Email: 2351098552@qq.com.
Yuan Liang, Email: 1045193695@qq.com.
Xiuying Si, Email: 1720603344@qq.com.
Guangxia Pan, Email: 109825848@qq.com.
Yijie Wang, Email: 2351098552@qq.com.
Qihui Hu, Email: 871945176@qq.com.
References
- [1].Bieber T. Atopic dermatitis. N Engl J Med. 2008;358:1483–94. [DOI] [PubMed] [Google Scholar]
- [2].Berke R, Singh A, Guralnick M. Atopic dermatitis: an overview. Am Fam Physician. 2012;86:35–42. [PubMed] [Google Scholar]
- [3].Drucker AM, Wang AR, Li WQ, et al. The burden of atopic dermatitis: summary of a report for the National Eczema Association. J Invest Dermatol. 2017;137:26–30. [DOI] [PubMed] [Google Scholar]
- [4].Hanifin JM, Reed ML. A population-based survey of eczema prevalence in the United States. Dermatitis. 2007;18:82–91. [DOI] [PubMed] [Google Scholar]
- [5].Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70:338–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Megna M, Napolitano M, Patruno C, et al. Systemic treatment of adult atopic dermatitis: a review. Dermatol Ther (Heidelb). 2017;7:1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Brunello L. Atopic dermatitis. Nat Rev Dis Primers. 2018;4:2. [DOI] [PubMed] [Google Scholar]
- [8].Silverberg JI. Associations between atopic dermatitis and other disorders. F1000Res. 2018;7:303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Eichenfield LF, Tom WL, Berger TG, et al. Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies. J Am Acad Dermatol. 2014;71:116–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Sidbury R, Davis DM, Cohen DE, et al. Guidelines of care for the management of atopic dermatitis: section 3. Management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. 2014;71:327–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Sidbury R, Tom WL, Bergman JN, et al. Guidelines of care for the management of atopic dermatitis: section 4. Prevention of disease flares and use of adjunctive therapies and approaches. J Am Acad Dermatol. 2014;71:1218–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Drucker AM, Eyerich K, de Bruin-Weller MS, et al. Use of systemic corticosteroids for atopic dermatitis: international Eczema Council consensus statement. Br J Dermatol. 2018;178:768–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Chen B, Zhan H, Chung M, et al. Chinese herbal bath therapy for the treatment of knee osteoarthritis: meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. 2015;2015:949172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Lee JH, Seo EK, Shim JS, et al. The effects of aroma massage and foot bath on psychophysiological response in stroke patients. J Phys Ther Sci. 2017;29:1292–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Hu Y, li Y, Long Y, et al. Research progression of Chinese herbal bath therapy. Shi Zhen Guo Yi Guo Yai. 2021;32:1201–4. [Google Scholar]
- [16].Gu S, Yang AW, Xue CC, et al. Chinese herbal medicine for atopic eczema. Cochrane Database Syst Rev. 2013;9:CD008642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Gu SX, Zhang AL, Coyle ME, et al. Chinese herbal medicine for atopic eczema: an overview of clinical evidence. J Dermatolog Treat. 2017;28:246–50. [DOI] [PubMed] [Google Scholar]
- [18].Lin Y, Chen CD, Chen SH, et al. Efficacy and safety of anti-inflammatory moisturizing lotion on atopic dermatitis. Zhong Guo Shi Yan Fang Ji Xue Za Zhi. 2014;20:220–4. [Google Scholar]
- [19].Yang LJ, Han YT, Zhang XY. Effects on CD4+ CD25+ Treg cells of peripheral blood in children with atopic dermatitis by treatment of medicated bath. Si Chuan Yi Xue. 2010;31:783–4. [Google Scholar]
- [20].Lin HE, Li ZY, Peng J, et al. New progress in the treatment of atopic dermatitis with traditional Chinese medicine. Liao Ning Zhong Yi Yao Da Xue Xue Bao. 2019;21:29–32. [Google Scholar]
- [21].Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10:ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Li PY, Zhang GR, Liu HX. Effect of Chinese medicine bath combined with tacrolimus ointment on treating children with atopic dermatitis. Da Yi Sheng. 2019;4:89–90. [Google Scholar]
- [25].Xu JQ, Chen S. Clinical observation of integrative traditional Chinese and Western medicine in the treatment of atopic dermatitis in children with damp and hot pooled knots. Bei Fang Yao Xue. 2017;14:9–10. [Google Scholar]
- [26].Yang LJ, Zhang XY, Li YX, et al. Observation on the efficacy of traditional Chinese medicine bath treatment in 110 cases of pediatric atopic dermatitis and discussion on the theory of traditional Chinese and Western medicine. Zhong Guo Mei Rong Yi Xue. 2012;21:215. [Google Scholar]
- [27].Huang WH, Wang CM. Curative effect of TCM medicated bath combined with tacrolimus onmoderate to severe atopic dermatitis in children and influence on serum LTB4 on LTC4. Zhong Hua Quan Ke Yi Xue. 2016;14:604–6. [Google Scholar]
- [28].Huang WX. Efficacy of traditional Chinese medicine bath combined with tacrolimus ointment in the treatment of atopic dermatitis in children. Shi Yong Zhong Yi Yao Za Zhi. 2021;37:1688–9. [Google Scholar]
- [29].Han HJ, Guo F, Liu HX. Efficacy and safety observation of Chinese Medicine bath joint tacrolimus ointment for the treatment of children with atopic dermatitis. Zhong Guo Zhong Xi Yi Jie He Pi Fu Xing Bing Xue Za Zhi. 2013;12:164–6. [Google Scholar]
- [30].Chen HQ. Clinical observation of the curative effect of traditional Chinese medicine Zhiyang powder external lotion on atopic dermatitis. Zhong Yi Lin Chuang Yan Jiu. 2021;13:78–80. [Google Scholar]
- [31].Zhu J, Chen J. Zhiyang powder external lotion on atopic dermatiti. Xin Zhong Yi. 2020;52:85–7. [Google Scholar]
- [32].Furue M, Terao H, Rikihisa W, et al. Clinical dose and adverse effects of topical steroids in daily management of atopic dermatitis. Br J Dermatol. 2003;148:128–33. [DOI] [PubMed] [Google Scholar]
- [33].Morley KW, Dinulos JG. Update on topical glucocorticoid use in children. Curr Opin Pediatr. 2012;24:121–8. [DOI] [PubMed] [Google Scholar]
- [34].Xu XJ, Banerjee P, Rustin MH, et al. Modulation by Chinese herbal therapy of immune mechanisms in the skin of patients with atopic eczema. Br J Dermatol. 1997;136:54–9. [PubMed] [Google Scholar]
- [35].Xu Y, Chen S, Zhang L, et al. The anti-inflammatory and anti-pruritus mechanisms of Huanglian Jiedu decoction in the treatment of atopic dermatitis. Front Pharmacol. 2021;12:735295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Fan HJ, Xie ZP, Lu ZW, et al. Anti-inflammatory and immune response regulation of Si-Ni-San in 2,4-dinitrochlorobenzene-induced atopic dermatitis-like skin dysfunction. J Ethnopharmacol. 2018;222:1–10. [DOI] [PubMed] [Google Scholar]
- [37].Chen HY, Lin YH, Wu JC, et al. Use of traditional Chinese medicine reduces exposure to corticosteroid among atopic dermatitis children: a 1-year follow-up cohort study. J Ethnopharmacol. 2015;159:189-96. [DOI] [PubMed] [Google Scholar]