Abstract
Background
This overview summarizes the best available systematic review (SR) evidence on the health effects of Tai Chi.
Methods
Nine databases (PubMed, Cochrane Library, EMBASE, Medline, Web of Science, China National Knowledge Infrastructure (CNKI), Chinese Scientific Journal Database (VIP), Sino-Med, and Wanfang Database) were searched for SRs of controlled clinical trials of Tai Chi interventions published between Jan 2010 and Dec 2020 in any language. Effect estimates were extracted from the most recent, comprehensive, highest-quality SR for each population, condition, and outcome. SR quality was appraised with AMSTAR 2 and overall certainty of effect estimates with the GRADE method.
Results
Of the 210 included SRs, 193 only included randomized controlled trials, one only included non-randomized studies of interventions, and 16 included both. Common conditions were neurological (18.6%), falls/balance (14.7%), cardiovascular (14.7%), musculoskeletal (11.0%), cancer (7.1%), and diabetes mellitus (6.7%). Except for stroke, no evidence for disease prevention was found; however, multiple proxy-outcomes/risks factors were evaluated. One hundred and fourteen effect estimates were extracted from 37 SRs (2 high, 6 moderate, 18 low, and 11 critically low quality), representing 59,306 adults. Compared to active and/or inactive controls, 66 of the 114 effect estimates reported clinically important benefits from Tai Chi, 53 reported an equivalent or marginal benefit, and 6 an equivalent risk of adverse events. Eight of the 114 effect estimates (7.0%) were rated as high, 43 (37.7%) moderate, 36 (31.6%) low, and 27 (23.7%) very low certainty evidence due to concerns with risk of bias (92/114, 80.7%), imprecision (43/114, 37.7%), inconsistency (37/114, 32.5%), and publication bias (3/114, 2.6%). SR quality was often limited by the search strategies, language bias, inadequate consideration of clinical, methodological, and statistical heterogeneity, poor reporting standards, and/or no registered SR protocol.
Conclusions
The findings suggest Tai Chi has multidimensional effects, including physical, psychological and quality of life benefits for a wide range of conditions, as well as multimorbidity. Clinically important benefits were most consistently reported for Parkinson’s disease, falls risk, knee osteoarthritis, low back pain, cerebrovascular, and cardiovascular diseases including hypertension. For most conditions, higher-quality SRs with rigorous primary studies are required.
Systematic review registration
PROSPERO CRD42021225708.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13643-022-02100-5.
Keywords: Tai Chi, Overview, Systematic review, Treatment, Prevention, Rehabilitation
Background
Tai Chi is a traditional exercise, martial art, and mind–body practice that is practiced by people of different ages and health statuses. Also known as Tai Chi Chuan/Quan or Taiji, Tai Chi originated in China in the seventeenth century A.D. [1]. The practice is low to moderate intensity with repetitive, flowing, meditative movements that aim to cultivate and maintain health and wellbeing [2]. There are five major traditional styles of Tai Chi, namely Chen, Yang, Wu, Wu/Hao, and Sun styles, along with numerous newer styles, hybrids, and extensions. Tai Chi integrates the essence of Chinese folk and military martial arts, with traditional Chinese medicine theories [3, 4]. The core components of Tai Chi are traditionally described as including sequenced movements, meditative and visualization techniques, and deep, abdominal breathing [3]. In China, Tai Chi is widely taught in high schools and higher education-related organizations [5].
Interest in evaluating the effects of Tai Chi in both healthy populations and people with a wide range of diseases, conditions, and symptoms has steadily increased globally [6, 7]. A bibliometric analysis of clinical studies of Tai Chi published between 1958 and 2013 identified 507 studies, of which 43 (8.3%) were systematic reviews (SRs) of randomized controlled trials (RCTs) and/or non-randomized studies of interventions (NRSIs) [6]. The 2010 to 2020 update identified 987 studies, of which 157 (15.9%) were SRs [7].
Given the large number of SRs of Tai Chi, SRs of SRs (henceforth referred to as overviews) are increasingly being conducted. Some have evaluated multiple interventions for a single condition [8–16], whilst others have focused only on Tai Chi interventions for either a single condition [17–22] or multiple conditions [23–27]. Limitations of the overviews evaluating only Tai Chi interventions [17–27] were the potential for language bias [17, 18, 22, 23, 25–27], reporting bias in which the most favourable results were emphasized [23, 27], and reporting multiple estimates of effects/results for the same or similar outcome and population, with limited or no discussion about conflicting results or overlapping of the primary studies [18–25, 27].
As such, this overview aims to systematically identify and appraise the best available SR evidence reported in the most recent, comprehensive, and/or highest-quality SRs, on the safety and effectiveness of Tai Chi for health promotion and managing disease.
Methods
The methods were guided by the Cochrane Handbook for Systematic Reviews of Interventions [28], in particular Chapter V: Overview of Reviews [29], the Joanna Briggs Institute Manual for Evidence Synthesis: Chapter 10 Umbrella Review [30], the GRADE (Grading of Recommendations, Assessment, Development and Evaluations) Handbook [31], and the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 statement [32]. The PRISMA 2020 checklist is presented in Additional file 1.
Protocol and registration
A protocol was registered prior to data extraction at the International Prospective Register for Systematic Reviews (PROSPERO) (CRD42021225708). Deviations from the protocol prior to formal screening and data extraction were as follows: only partial blinding of the reviewers to the results when selecting SRs and outcomes, including important secondary outcomes of a SR, reporting more than three outcomes for some populations; and including SRs of NRSIs.
Populations
All populations were included, regardless of health status, setting, location, and country.
Interventions
All exercise programs described as Tai Chi were included. No limitations were applied to Tai Chi styles (such as Chen, Yang, Wu, Wu/Hao, and Sun style) or forms (such as 6-form, 24-form, 54-form, and 83-form Tai Chi). Exercise programs that combined Tai Chi with other interventions such as Qigong, meditation, or conventional exercise were only included if the reviewers clarified that Tai Chi was the core component. A SR that evaluated Tai Chi and other interventions (e.g. any form of exercise) was excluded if the effects of Tai Chi was not analysed in a separate analysis.
Comparisons
Any type of control was included, for example, no intervention, waitlist control, usual care, and active control. When the data was available, the pooled effects according to control group categories were extracted to reduce clinical and methodological diversity. Comparisons also include a co-intervention if applied in all arms.
Outcomes
Any outcome was eligible for inclusion. However, as much as possible, the number of outcomes extracted per population/comparison group was limited to three. These were selected to reflect the SR’s primary/main outcome(s), outcomes that align with the reasons why people use Tai Chi and what matters to them, the validity/reliability of the measurement tool, and directness of the outcome measure to health status (e.g. clinical outcomes in preference to risk factors). Core outcome sets and other resources such as those published on the Core Outcome Measures in Effectiveness Trials (COMET) Initiative database [33] were used to inform these decisions. Two senior reviewers (GYY, JH) jointly made these decisions. When estimates of effect were reported for multiple timepoints, the timepoints with the most RCTs was selected. Additional timepoints were only selected if the studies were not included in the first estimate.
Study designs
All SRs of interventions, with or without a meta-analysis of RCTs, quasi-RCTs, and other NRSIs (e.g. cohort studies, case–control studies, controlled before-and-after studies, interrupted-time-series studies, case series and case reports), were included. Whilst SRs of RCTs were likely to provide the most reliable evidence for most estimates of effect, SRs of NRSIs were also included (post protocol, pre-data extraction) in the circumstance when this was the best available evidence.
Literature search
The search strategy built upon a bibliometric analysis of Tai Chi intervention studies published between 1st January 2010 and 31st January 2020 [7]. The search was updated for the purpose of this overview (1st January to 12th December 2020) using the same search terms and databases—PubMed, Cochrane Library, EMBASE, Medline, Web of Science, China National Knowledge Infrastructure (CNKI), Chinese Scientific Journal Database (VIP), Sino-Med, and Wanfang Database (Additional file 2). The search strategies were developed and refined by the team of experts who conducted an earlier bibliometric analysis [6]. Tai Chi search terms include “Taiji”, “Tai Ji”, “Tai-ji”, “Tai Chi”, “Tai Chi Chuan”, “Tai Chi Quan”, or “Taijiquan”. Limitation to language and publication status was not applied. Grey literature was included. Database searches were augmented with bibliography searches of other recently published SRs of SRs [8–27].
Study selection
The search results from English databases were exported into EndNote (version X9), and those from Chinese databases into NoteExpress (version 3.2). Duplicates were removed before study selection. Following calibration exercises, reviewers (GYY, JH, WLH, HZ) worked in pairs to independently screen the title/abstracts and full texts. Two reviewers (GYY, JH) rescreened the full texts of the 157 SRs (106 published in English, 41 published in Chinese) that were identified in the 2020 bibliometric analysis [7]. Final decisions were made by consensus and involved other reviewers when necessary.
To minimize overlap of primary studies, one SR for each population, condition, or outcome (PCO) was then selected for the final evidence synthesis. A staged approach was applied to selecting this subset of SRs with the aim of identifying the most recent, comprehensive, and highest-quality SR for each PCO. First, SRs with a meta-analysis of RCTs were grouped according to their PCO, from which the publication date and number of RCTs were compared. When multiple SRs were published within 4–5 years of each other and/or the number of RCTs were similar, a single reviewer (GYY, JH) extracted further data about the number of databases searched, any language restrictions, the primary/main outcomes, and the number of RCTs and overlapping RCTs per meta-analysis. An informal appraisal of the SR quality using AMSTAR 2 [34] was also done. Finally, SRs without a meta-analysis were then screened, and SRs that included a meta-analysis of NRSIs were rescreened to ensure there were no missing PCO.
Data collection
A pre-defined data extraction form that was an extension of the bibliometric analysis extraction form was designed and piloted by two reviewers (GYY, JH). Data extraction was staged for pragmatic reasons and to partially blind the investigators when selecting the SRs and PCO. For all included SRs, information about the characteristics of the studies (i.e. citation details, authors, study design, number of RCTs and NRSIs, participants characteristics, and types of outcomes) were extracted. For the subset of SRs selected for the final evidence synthesis (and those when SR selection could not be made based on the preliminary data extraction), additional information about the search strategy, study characteristics of included studies, and the SR quality was also extracted. For each estimate of effect that was selected for the final evidence synthesis, additional information about the participants, settings, estimates of effect, statistical heterogeneity, subgroup and sensitivity analysis, and publication bias was then extracted. Estimates of effect were not extracted for the SRs with no meta-analysis as this would require extracting data from the original publications of the primary studies, nor for a meta-analysis that did not meet the criteria outlined in item 11 of AMSTAR 2. Following calibration exercises, five reviewers (GYY, WLH, FLB, HZ, JH) extracted data into Research Electronic Data Capture (REDCap) [35] that was verified by two senior reviewers (GYY, JH). Final decisions were made by consensus with the review team.
Quality assessment
Only the subset of SRs included in the final evidence synthesis were formally assessed for quality using AMSTAR 2 (A MeaSurement Tool to Assess systematic Reviews, improved version) critical appraisal tool and rated as high, moderate, low, or critically low quality [34]. Items 2, 4, 9, 11, 13, and 15 were deemed critical. Item 7, which requires the list of the excluded articles with the rationale is reported, was introduced to AMSTAR 2 in late 2017. A similar reporting requirement was introduced to the revised PRISMA 2020 statement published in early 2021 [32]. Consequently, for the purpose of this review item 7 was deemed non-critical. Additionally, SRs published before 2019 were not downrated for item 7 if they met the accepted reporting standards for excluded articles as per PRISMA 2009 [36]. For all other items, the AMSTAR 2 guidance was followed. A sensitivity analysis was conducted to compare this modified AMSTAR 2 rating for item 7 with the original guidance.
GRADE guidelines [31] and GRADEpro GDT software [37] were used to rate the overall certainty (quality) of the evidence for the extracted effect estimates. Due to pragmatic constraints, assessments of the risk of bias of the primary studies, heterogeneity, and publication bias relied upon the assessments reported in the SR. However, the results of any sensitivity analyses were extracted and considered. Given the large number of SRs, evaluating a wide range of populations and outcomes, a pragmatic approach similar to that used by Pollock et al. [38] was applied where specific thresholds, ranges, and criteria were established and piloted to optimize consistency and transparency across all the ratings. The details of the rubric used to inform the GRADE assessments are reported in Supplementary File 6 and summarized below.
For the risk of bias (RoB) assessments, randomization/selection bias, assessor blinding, and missing data were deemed the most important categories. This decision reflected the need to select domains assessed by the RoB assessment tools used in the SRs and that it is not possible to blind Tai Chi study participants. For there to be no serious concerns with RoB, at least 75% of the included RCTs in the SR had a low RoB in each of these three categories.
Inconsistency was investigated when the I2 test for statistical heterogeneity was ≥ 75%. This involved inspecting the Forest plot for overlapping 95% confidence intervals (CI) and direction of effects, and the findings from any subgroup or sensitivity analysis reported in the SR. In a post hoc sensitivity analysis, inconsistency was investigated if the I2 test was ≥ 30% or τ2 test p ≥ 0.1.
Since all participants, interventions, and outcomes were directly relevant to the research question, all estimates of effect were automatically rated as having no serious concerns with indirectness.
Assessments of imprecision were according to whether the optimum information size was likely to be met, the width of the 95% CI, and whether important benefits and/or harms could be excluded. Due to pragmatic constraints, unless reported otherwise in the SR, thresholds were set for optimum information sizes [31, 38]. In a post hoc sensitivity analysis, the threshold for the optimum information size for continuous data was increased from 200 [38] to 400 [31]. For standardized mean differences (SMD), the minimal clinically important difference (MCID) for important benefit was set at 0.5 that is considered to be a moderate effect size, and a large effect size was set at 0.8 [39]. For mean differences (MD), the MCID for important benefit was based on studies involving similar populations [40–59]. For relative risks (RR), the cut-off for important benefits was set at < 0.75 or > 1.25. For risk differences (RD), the cut-off for important harm was set at ± 0.1 for non-serious AEs and ± 0.01 for serious AEs.
Publication bias was only considered when at least ten RCTs were in the meta-analysis. In instances when the SR did not report on the publication bias for an effect estimates yet assessed it for another, the findings from that assessment were applied. If there was no information, at least half of the studies had to have a sample size larger than 100 for there to be no serious concerns about publication bias.
Following calibration exercises, the AMSTAR 2 assessments were independently made by two reviewers in pairs (GYY, JH, FLB) and the GRADE certainty assessments were made by one of these reviewers and verified by a second reviewer. Final decisions were made by consensus with the team.
Synthesis of results
The results are narrated and presented in tables, including a summary of findings table for all estimates of effect. Dichotomous data are presented as RR or RD and number needed to treat (NNT), with 95% confidence intervals (CIs). When available, rates are presented as the number of participants. Continuous data are presented as weighted MD or SMD, with 95% CIs. No further meta-analysis, network analysis, or re-analysis of the results was conducted.
Results
Search results
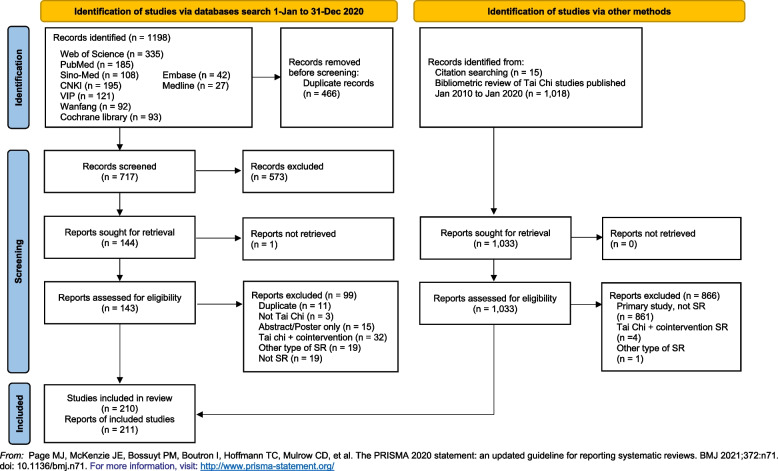
The literature searches identified 210 eligible SRs (211 articles) of Tai Chi (Fig. 1). The citations with the reason for excluding 100 full-text articles are listed in Additional file 3.
Fig. 1.
PRISMA flow diagram
Study selection for evidence synthesis
From the 210 SRs of Tai Chi, 47 SRs [60–106] were selected for the final evidence synthesis and 114 estimates of effect, representing 59,306 adult participants in RCTs, were extracted from 37 SRs [61, 62, 64, 66–68, 70, 71, 73–75, 77, 79–88, 90–94, 96–98, 100–106]. Estimates of effects were not extracted, and the GRADE certainty of the evidence was not appraised for four SRs with unreliable meta-analyses [65, 76, 78, 99] and six SRs with no meta-analysis [60, 63, 69, 72, 89, 95]. No results were extracted from, nor was the AMSTAR-2 quality formally appraised or reported for 163 SRs (164 articles) because for 79 SRs, a far more recent SR, typically with more primary studies, was identified; for 46 SRs (47 articles) following further consideration, a SR of higher quality and/or with more primary studies in the meta-analysis for the PCO was selected; and for 38 of the SRs that did not conduct a meta-analysis, the PCO were reported by a SR with a meta-analysis. When the analysis of this overview has been finalised, we found an erratum for an included SR with a meta-analysis on fear of falling was published on 3rd September 2022 [107], which corrects the error that led a misinterpretation of their methodology and findings because a meta-regression was performed with the SMD as the dependent variable. As a result, the comparison we included from this SR was Tai Chi with and without supervision by a Tai Chi instructor, which is not eligible for inclusion. The SR was still included as the corrections did not alter the overall assessment of the certainty of the evidence for that outcome. The citations and reasons for excluding the 163 potentially eligible SRs from the evidence synthesis are reported in Additional file 4.
Characteristics of studies
Since 2010, the number of SRs published each year in English and Chinese databases rose exponentially (Table 1). Most were SRs with a meta-analysis of RCTs (78.6%, 165/210) and were published in English (73.8%, 155/210) or Chinese (25.7%, 54/210). The first author of 139 (66.2%) SRs was from a university/institution located in mainland China, Hong Kong, or Taiwan. The median number of participants per SR was 750, ranging from 42 to 9263. Only 18 (8.6%) SRs included studies in which at least some of the study participants were under 25 years of age. Multiple outcomes measuring the effects of Tai Chi in a wide range of populations were evaluated. The most common conditions and their associated risks factors were for cardio/cerebrovascular diseases and falls. One SR specifically evaluated the risk of adverse events.
Table 1.
Characteristics of systematic reviews of Tai Chi interventions
| Number of systematic reviews (SRs) | 210 |
| Meta-analysis | 165 |
| Narrative analysis only | 45 |
| Studies included in SRs | 210 |
| RCTs only | 193 |
| NRSIs only | 1 |
| Both RCTs and NRSIs | 16 |
| RCTs per SR: Median (range) | 9 (1–77) |
| NRSIs per SR: Median (range) | 4 (1–18) |
| Participants per SR: Median (range) | 750 (42–9263) |
| Publication year | |
| 2010–2012 | 20 |
| 2013–2014 | 33 |
| 2015–2016 | 37 |
| 2017–2018 | 54 |
| 2019–2020 | 66 |
| Publication language | |
| English | 155 |
| Chinese | 54 |
| Korean | 1 |
| Country / region of first author | |
| China, Hong Kong, Taiwan | 139 |
| United States of America, Canada, Brazil | 35 |
| Western Europe | 19 |
| South Korea, Singapore, Thailand | 10 |
| Australia, New Zealand | 6 |
| Funding | |
| Government / national grants | 84 |
| University | 15 |
| Charity | 3 |
| No information | 108 |
| Disease / condition | |
| Healthy adolescents/ adults | 8 |
| Multiple chronic diseases | 9 |
| Falls, balance, other falls risk factors | 32 |
| Hypertension | 15 |
| Cancer (breast cancer n = 8) | 15 |
| Diabetes mellitus | 14 |
| Cognitive impairment | 13 |
| Parkinson’s disease | 13 |
| Chronic obstructive pulmonary disease | 13 |
| Cerebrovascular disease (stroke) | 11 |
| Mental health | 11 |
| Ischaemic heart disease | 10 |
| Osteoarthritis (knee n = 5) | 10 |
| Osteoporosis / osteopenia | 8 |
| Heart failure | 6 |
| Sleep disorders / quality | 6 |
| 3 SRs each for: Low back pain, chronic pain | |
| 2 SRs each for: Multiple sclerosis, rheumatoid arthritis | |
| 1 SR each for: Hyperlipidaemia, fatigue, fibromyalgia, frailty, immunity/HIV infection, adverse effects | |
RCT randomized controlled trial, NRSI non-randomized studies of interventions, QoL quality of life
Table 2 summarizes the characteristics of the 47 SRs (41 SRs with meta-analysis and 6 SRs without meta-analysis) included in the final evidence synthesis. Of note, only two SRs included adolescents [95, 100] and 40 included older adults (≥ 60 years). Almost all study participants were living in independently in the community. Most SRs included participants from both Asian and non-Asian countries. Only two SRs were limited to Chinese participants only [103, 104].
Table 2.
Characteristics of systematic reviews included in the evidence synthesis
| Review ID | Populations (no.) Conditions |
Main outcomes * (Other outcomes) |
Tai Chi (TC) minutes/session, frequency/week, follow-up Comparisons |
Search date No. databases No. studies (Languages) |
Funding | SR analysis AMSTAR 2 quality rating |
|---|---|---|---|---|---|---|
| Buto 2020 [60] | Older adults (n = 2063; TC = 1728) Prefrail and frail | Functional capacity, QoL |
20–60 min 1–5 times/week, 15–96 weeks TC vs Ucare, HEd, PT, Ex, other |
Sep 2019 6 databases (Eng.) 15 RCTs (Tai Chi: 9 RCTs) (Eng. Chin.) |
Uni |
No meta-analysis Moderate (†Low) |
| Cheng 2019 [61] |
Adults (n = 657) Fibromyalgia |
Fibromyalgia impact (fatigue, pain, sleep quality, depression, QoL) |
55–120 min 1–3 times/week, 10–24 weeks TC vs Ucare, Ex |
May 2019 3 databases (Eng.) 6 RCTs (Eng.) |
Uni |
Meta-analysis Low (†Critically low) |
| Choo 2020 [62] |
Older adults (n = 869) Chronic diseases |
NI (QoL, mental health, physical function, AE) |
40–90 min 1–4 times/week, 10–24 weeks TC vs noRx, Ucare, HEd, Pharm, Ex, other, waitlist |
NI 7 databases (Eng. Chin.) 13 RCTs (Eng. Chin.) |
NI | Meta-analysis Critically low |
| Cocchiara 2020 [63] |
Adults (n = 467) Workplace wellness of healthcare workers |
NI (work-related stress, physical and mental health, improvement in attention and/or productivity) |
8–12 weeks NI |
Mar, 2019 4 databases (Eng.) 1 SR, 3 RCTs, 1 NRSI, 1 case report (Eng.) |
NI |
No meta-analysis Critically low |
| Cui 2019 [64] |
Adults, older adults (n = 1794) Healthy, chronic diseases |
Serious and non-serious adverse events |
30–60 min 1–5 times/week, 12–48 weeks TC vs active or inactive intervention |
Feb 2016 3 databases (Eng.) 24 RCTs (Eng.) |
Gov | Meta-analysis Critically low |
| Dong 2020 [65] |
Adults, older adults (n = 1608) with or without hypertension |
Systolic and diastolic BP |
30–120 min 1–7 times/week, 8–24 weeks TC vs noRx, Ex |
Jan 2019 6 databases (Eng. Chin.), 24 RCTs (Eng. Chin.) |
Gov | Meta-analysis Critically low |
| Gu 2017 [66] |
Adults, older adults (n = 918) Chronic heart failure |
6MWD, QoL (B-type natriuretic peptide, LVEF, BP, VO2peak) |
15–60 min 2–7 times/week, 4–24 weeks TC vs Ucare, Ex, Pharm |
Jun 2016 6 databases (Eng. Chin.) 13 RCTs (Eng. Chin.) |
Gov |
Meta-analysis Low (†Critically low) |
| Guo 2020 [67] |
Adults, older adults (n = 1508) COPD |
Lung function tests (6MWD, QoL) |
30–60 min 2–5 times/week, 8–48 weeks TC vs noRx, Ex |
Aug 2018 9 databases (Eng. Chin.) 16 RCTs (Eng. Chin.) |
Gov | Meta-analysis Low |
| Hall 2017 [68] |
Adults, older adults (n = 1012) Musculoskeletal chronic pain |
Pain (disability, stiffness, QoL) |
40–60 min 2 times/week, 6–20 weeks TC vs Ucare, HEd, waitlist |
Nov 2015 7 databases (Eng.) 15 RCTs (Eng.) |
NI |
Meta-analysis Low (†Critically low) |
| Ho 2013 [69] | Adolescents, adults, older adults (n = 939) Healthy, HIV | NI (any symptoms of infections, biomedical indicators of immunity) |
30–60 min 1–5 times/week, 5–576 weeks TC vs Ucare, HEd, Ex, waitlist |
Jan 2011 14 databases (Eng. Chin.) 7 RCTs, 9 NRSIs (Eng. Chin.) |
NI |
No meta-analysis Low (†Critically low) |
| Hu 2020 [70] |
Older adults (n = 986) Knee osteoarthritis |
Pain, stiffness, physical function, mental health, self-efficacy, AE |
30–60 min 1–4 times/week, 5–52 weeks TC vs noRx, Ucare, HEd, PT, waitlist |
Jun 2020 9 databases (Eng. Chin.) 16 RCTs (Eng. Chin.) |
No |
Meta-analysis Low (†Critically low) |
| Huang 2017 [73] |
Older adults (n = 3824) Chronic diseases |
No. of people who fell (falls incidence) |
1–5 times/week, 16–96 weeks TC vs noRx, PT, Ex, waitlist |
Feb 2016 3 databases (Eng.) 18 RCTs (Eng. Chin.) |
Gov |
Meta-analysis Low (†Critically low) |
| Huang 2019 [72] |
Adults, older adults (n = 132) Vestibular balance disorders |
Balance, gait, neuromuscular function, trunk stability (symptom severity/relief/impact, AE) |
45–90 min 1–5 times/week, 3–18 weeks TC vs noRx, vestibular training/education, Ex; TC individualized vs TC standardized |
Dec 2016 4 (English) 3 RCTs, I NRSI (English) |
NI |
No meta-analysis Low (†Critically low) |
| Huang 2020 [71] |
Adults, older adults (n = 3842) Falls |
Falls rate (Balance—single leg standing, Berg balance scale, time-up-and-go) |
30–90 min 1–7 times/week, 8–48 weeks TC vs ADL, PT, HEd, Ex, other |
Aug 2019 6 databases (Eng. Chin.) 20 RCTs (Eng. Chin.) |
Gov | Meta-analysis Critically low |
| Jiang 2018 [74] |
Older adults (n = 290) Stable angina |
NI (VO2max, maximum heart rate) |
12–48 weeks TC vs noRx, Ex |
1999–2015 10 databases (Eng. Chin.) 5 RCTs (Eng. Chin.) |
NI |
Meta-analysis Low (†Critically low) |
| Kruisbrink 2020 [75] |
Older adults (NI) Falls |
Fear of falling |
30–60 min 2–7 times/week, 8–24 weeks TC vs noRx, Ucare |
Jul 2005–Jul 2019 5 databases (Eng.) 62 RCTs / 38 Tai Chi (Eng.) |
Uni |
Meta-analysis Low (†Critically low) |
| Liu F 2020 [76] |
Adults (n = 772; TC = 179) Substance abuse disorders |
Depression, anxiety (AE) |
45–60 min 3–4 times/week, 45–60 weeks TC vs usual care |
Jan 2019 (English Chinese) 1 RCT, 6 NRSIs (English, Chinese) | Uni |
Meta-analysis Critically low |
| Liu LZ 2020 [77] |
Adults, older adults (n = 1268) Breast cancer |
Fatigue, sleep quality, QoL |
30–120 min 2–3 times/week, 10–24 weeks TC vs Ucare, Psych, sham QiGongEx; TC + Rehab vs Dance + Rehab |
Jun 2019 8 databases (Eng. Chin.) 16 RCTs (Eng. Chin.) |
n.f.p | Meta-analysis Critically low |
| Liu WJ 2020 [78] |
Older adults (n = 798) Osteoarthritis |
NI (Pain, stiffness & function, time-up-and-go, 6MWD, other) |
8–48 weeks TC vs Ucare, HEd, other |
Jan 2019 6 databases (Eng. Chin.) 15 RCTs (Eng. Chin.) |
NI | Meta-analysis Critically low |
| Luo 2020 [79] |
Female adults (n = 885) Breast cancer |
Quality of life (fatigue, BMI, laboratory blood tests) |
20–120 min 3–7 times/week, 12–24 weeks TC vs Psych; TC + Ucare vs Ucare; TC + Rehab vs Rehab |
Feb 2020 11 databases (Eng. Chin. Japanese Korean Tai) 15 RCTs (Eng. Chin.) |
Gov |
Meta-analysis Moderate (†Low) |
| Lyu 2018 [81] |
Adults, older adults (n = 1293) Stroke survivors |
NI (ADL, motor function, balance, mental health, AE) |
20–48 weeks TC vs Rehab |
Oct 2017 7 databases (Eng. Chin.) 21 RCTs (Eng. Chin.) |
Gov |
Meta-analysis Moderate (†Low) |
| Lyu 2020 [80] |
Adults, older adults (n = 723) Stroke survivors |
NI (mental health, sleep quality, cognitive impairment) |
6–48 weeks TC vs Ucare, Rehab; TC + Rehab vs Rehab |
Jul 2020 7 databases (Eng. Chin.) 11 RCTs (Eng. Chin.) |
Gov |
Meta-analysis Moderate (†Low) |
| Mudano 2019 [82] |
Adults, older adults (n = 345) Rheumatoid arthritis |
NI (pain, disease activity, physical function, AE) |
7–60 min 1–2 times/week, 8–12 weeks TC vs Ucare, HEd, Ex; TC + HEd + other vs TCM; TC + HEd class vs HEd brochure |
Sep 2018 5 databases (Eng.) 2 RCTs, 5 NRSIs (Eng. Chin.) |
NI | Meta-analysis High |
| Ni 2019 [83] |
Adults, older adults (n = 1410) Cancer |
QoL (limb function, fatigue, sleep quality, laboratory blood tests, AE) |
20–60 min 3–5 times/week, 12–24 weeks TC vs Ucare, Rehab, HEd, Psych, Ex, sham Qigong |
Apr 2018 7 databases (Eng. Chin.) 22 RCTs (Eng. Chin.) |
Gov |
Meta-analysis Low (†Critically low) |
| Pan 2016 [84] |
Adults, older adults (n = 445) Hyperlipidaemia |
Lipid measures—cholesterol, triglycerides, LDL-C, HDL-C (AE) |
40–60 min 3–7 times/week, 12–48 weeks TC vs Ucare, Ex, waitlist |
Jun 2015 6 databases (Eng. Chin.) 6 RCTs (Eng.) |
NI |
Meta-analysis Low (†Critically low) |
| Qin 2019 [85] |
Adults, older adults (n = 959) Back pain |
Pain, disability (AE) |
40–60 min 1–6 times/week, 2–28 weeks TC vs noRx; TC + HEd vs HEd; TC + massage vs massage; TC + PT vs PT |
Mar 2019 6 databases (Eng. Chin.) 10 RCTs (Eng. Chin.) |
NI |
Meta-analysis Low (†Critically low) |
| Si 2020 [86] |
Adults, older adults (n = 1858) Healthy, chronic diseases |
Sleep quality assessed with Pittsburgh Sleep Quality Index (AE) |
5–120 min 1–5 times/week, 8–36 weeks TC vs noEx, ADL, HEd, Psych, Ex, Rehab, other, waitlist, sham Qigong |
Aug 2019 6 databases (Eng. Chin.) 25 RCTs (Eng. Chin.) |
Gov |
Meta-analysis Low (†Critically low) |
| Song 2018 [87] |
Adults, older adults (n = 373) Cancer |
Cancer related fatigue |
30–60 min 2–7 times/week, 4–12 weeks TC vs Ucare, HEd, Psych, Ex, sham Qigong |
Apr 2017 9 databases (Eng. Chin.) 6 RCTs (Eng. Chin.) |
Gov |
Meta-analysis Low (†Critically low) |
| Su 2020 [88] |
Adults, older adults (n = 762) Healthy, osteoarthritis |
Knee strength |
2–7 times/week, 12–72 weeks TC vs noEx, ADL, HEd, Ex |
NI 7 databases (Eng. Chin.) 12 RCTs (Eng. Chin.) |
Gov | Meta-analysis Critically low |
| Taylor 2017 [89] |
Adults (n = 193) Multiple sclerosis |
Balance, gait, flexibility, strength, fatigue, QoL, symptoms, perception of disease, mood (AE) |
40–90 min TC vs noRx, Ucare, TC + meditation |
Aug 2016 12 databases (Eng.) 3 RCTs, 5 NRSIs (Eng.) |
NI |
No meta-analysis Low (†Critically low) |
| Taylor-Piliae 2020 [90] |
Adults, older adults (n = 1853) Hypertension, chronic heart failure |
Quality of life, mental health (AE) |
30 min, 6–52 weeks TC vs noRx, Ucare, PT, Rehab, Ex TC + HEd vs noRx; TC + Rehab vs Rehab; TC + Ex vs Ex |
Jul 2009–Jul 2019 10 databases (Eng.) 13 RCTs, 2 NRSIs (Eng.) |
No | Meta-analysis Critically low |
| Wang 2010 [93] |
Adults, older adults (n = 3817) Healthy, chronic diseases, depression, frail |
NI (Stress, anxiety, depression, self-esteem, mood, AE) |
30–120 min 1–4 times/week, 10–24 weeks TC vs ADL, HEd, Ex, Psych, waitlist |
Mar 2009 11 databases (Eng. Chin.) 17 RCTs, 7 CCS, 16 CS (Eng.) |
NI | Meta-analysis Critically low |
| Wang 2017 [92] |
Adults, older adults (n = 344) Females, perimenopause |
QoL, 8 domains assessed by SF-36 (BMD) |
30–90 min 3–7 times/week, 20–36 weeks TC vs Ucare, placebo |
Jan 2014 4 databases (Eng. Chin.) 5 RCTs (Eng. Chin.) |
Gov | Meta-analysis Critically low |
| Wang 2020 [91] |
Older adults (n = 1170) Healthy, chronic diseases |
Quality of life |
15–90 min 2–5 times/week, 4–24 weeks TC vs Ucare, ADL, Ex |
Dec 2019 6 databases (Eng. Chin.) 10 RCTs (Eng. Chin.) |
NI | Meta-analysis Critically low |
| Wayne 2014 [94] |
Older adults (n = 2553) Cognitive impairment |
Global cognitive function, executive function (other cognitive tests, AE) |
20–60 min 1–4 times/week, 10–48 weeks TC vs noRx, HEd, Ex |
Mar 2013 4 databases (Eng.) 11 RCTs, 5 NRSIs, 4 CS (Eng.) |
NI | Meta-analysis Critically low |
| Webster 2016 [95] | Adolescents (n = 9263) | Physical flexibility, depression, anxiety, interpersonal (other physical/mental health) | NI |
Feb 2013 11 (Eng. Chin.) 12RCTs, 18NRSIs, 19CS (Eng. Chin.) |
NI |
No meta-analysis Critically low |
| Wu 2020 [96] |
Adults, older adults (n = 615) Myocardial infarction |
6-min walk distance, left ventricular ejection fraction (AE) |
5–60 min 3–5 times/week, 12–44 weeks TC + HEd + Pharm vs HEd + Pharm; TC + HEd + Ex vs HEd + ADL; TC + HEd + Ex vs HEd + Ex; TC + Ex + Rehab vs + Ex + Rehab |
Jan 1976–May 2019 6 databases (Eng. Chin.) 7 RCTs (Chin.) |
NI |
Meta-analysis Low (†Critically low) |
| Xiang 2017 [97] |
Adults, older adults (n = 689) Fatigue no serious ailment, chronic disease |
Fatigue (vitality, depression, sleep, AE) |
40–60 min 1–7 times/week, 12–24 weeks TC vs noRx, Ucare, HEd, Ex, other, sham Qigong |
Apr 2016 7 databases (Eng. Chin.) 10 RCTs (Eng. Chin.) |
Gov |
Meta-analysis Moderate (†Low) |
| Yin 2014 [98] | Adults, older adults (n = 2765 TC = 1435) Anxiety, depression and/or chronic diseases | Depression, anxiety (AE) |
30–120 min 1–5 times/week, 4–48 weeks TC vs noRx, Ex, sham/other |
April 2013 (English) 25 RCTs (English) |
NI |
Meta-analysis Low |
| Yu 2019 [99] |
University students (n = 325) Depression or symptoms |
Depression |
60 min 2–3 times/week, 7–18 weeks TC vs noRx, Ex |
Oct 2016 8 databases (Eng. Chin.) 12 RCTs (Eng. Chin.) |
Gov |
Meta-analysis Critically low |
| Yu 2018 [100] |
Older adults (n = 556) Parkinson’s disease |
Motor manifestations, balance, walking ability, QoL |
45–60 min 2–10 times/week, 4–24 weeks TC vs noRx, Ex; TC + Ucare vs Ucare; TC + Ucare vs Ex + Ucare |
Dec 2018 6 (English Chinese) 7 RCTs (English, Chinese, Korean) |
Gov | Meta-analysis Critically low |
| Zhang 2019 [101] |
Adults, older adults (n = 857) Osteoporosis, or osteopenia |
Osteoporosis-related fractures (BMD, pain, QoL, biochemical markers) |
30–120 min 1–6 times/week, 16–48 weeks TC vs noRx, Ucare; TC + Ucare vs Ucare |
Sep 2017 7 databases (Eng. Chin.) 15 RCTs (Eng. Chin.) |
NI |
Meta-analysis Moderate (†Low) |
| Zhang 2020 [102] |
Older adults (n = 1068) Mild cognitive impairment |
Global cognitive function assessed by MMSE (delayed recall test, digit span test) |
5–50 min 3–4 times/week, 12–52 weeks TC vs Ucare, ADL, HEd, Psych, Ex |
Feb 2020 9 databases (Eng. Chin.) 7 RCTs (Eng.) |
NI |
Meta-analysis Low (†Critically low) |
| Zheng 2015 [103] |
Adults, older adults (n = 2393) Stroke (prevention) |
Incidence of fatal & nonfatal stroke (stroke risk factors (body weight, BP, lipids, glucose), AE) |
30–120 min 3–21 times/week, 4–96 weeks TC vs noRx; TC + Ucare vs Ucare |
Oct 2013 6 databases (Eng. Chin.) 23 RCTs, 11 NRSIs, 2 CS (Chin.) |
NI |
Meta-analysis Low (†Critically low) |
| Zheng 2016 [104] |
Adults, older adults (n = 483) Schizophrenia, in hospital or other residential care |
Positive and negative symptoms assessed by PANSS (social, cognitive, behavioural, stress, discontinuation rate, AE) |
45–60 min 2–7 times/week, 12–24 weeks TC + (Pharm + / − Ucare) vs Pharm + (noEx, Ucare, HEd, Ex, or waitlist) |
Aug 2016 9 databases (Eng. Chin.) 6 RCTs (Eng. Chin.) |
Uni |
Meta-analysis Moderate (†Low) |
| Zhong 2020 [105] |
Adults, older adults (n = 2937) Essential hypertension |
Systolic and diastolic BP (AE) |
30–120 min 3–14 times/week, 6–240 weeks TC vs noRx, HEd, Ex, other activities; TC + HEd vs HEd; TC + Pharm vs Pharm; TC + HEd vs Pharm + HEd; TC + HEd + Pharm vs Ex + HEd + Pharm; TC + HEd vs Qigong + HEd |
Jan 2020 9 databases (Eng. Chin.) 28 RCTs (Eng. Chin.) |
Gov | Meta-analysis High |
| Zhou 2019 [106] |
Adults, older adults (n = 1235) Type 2 diabetes |
Fasting glucose, glycosylated haemoglobin (HbA1c), fasting insulin, insulin resistance, BMI, BP |
15–120 min 2–14 times/week, 4–24 weeks TC vs Ucare, Ucare + TCM, HEd, sham exercise |
Mar 2018 7 databases (Eng. Chin.) 23 RCTs (Eng. Chin.) |
NI | Meta-analysis Critically low |
NI no information, Age groups adolescents 10–18 years, adults 25–59 years, older adults ≥ 60 years, AE adverse effects, 6MWD 6-min walk distance/test, BMD bone mineral density, BMI body mass index, BP blood pressure, COPD chronic obstructive pulmonary disease, HDL-C high-density lipoprotein cholesterol, LDL-C low-density lipoprotein cholesterol, LVEF cardiac left ventricular ejection fraction, MMSE Mini-Mental State Examination, PANSS positive and negative syndrome scale, QoL quality of life, ADL routine activities of daily living/ routine lifestyle, Ex exercise (any type, including stretching), HEd health education or other educational interventions, noRx no treatment, control, Pharm pharmaceutical drugs / medication, Psych psychological interventions, counselling, support, PT physical therapy/physiotherapy, Rehab rehabilitation programs, TC Tai Chi intervention, TCM traditional Chinese herbal medicine, Ucare usual care, conventional treatment, standard medical care
*reported as NI if no clear statement about primary outcome(s) of interest
Sensitivity analysis shows different rating
For AMSTAR-2 quality rating refer to Additional File 5
Quality of studies
According to AMSTAR 2 quality rating, two (4%) of the 47 SRs were rated as ‘High’ [82, 105], seven (15%) as ‘Moderate’ [60, 79–81, 97, 101, 104], 20 (43%) as ‘Low’ [61, 66–70, 72–75, 83–87, 89, 96, 98, 102, 103], and 18 (38%) as ‘Critically low’ [62–65, 71, 76–78, 88, 90–95, 99, 100, 106] (Table 2, Table 3, and Additional file 5). Notably, only four SRs (9%) clearly stated a rationale for the study design inclusion/exclusion criteria (item 3), five (11%) reported the funding details of the included studies (item 10); five (11%) listed the articles excluded at full-text screening (item 10); and 17 (40%) had registered or published a protocol (item 2). Other common deficiencies were not adequately considering and/or discussing how the risk of bias of individual studies might impact the results (items 12), and/or not adequately considering or examining statistical, methodological, or clinical heterogeneity (items 13). Six SRs used the PEDro Scale [107] and another six, Jadad, and whilst both are well regarded risk of bias assessment tools, they do not ask about selective reporting bias that is a requirement for full marks for item 9. However, even if full marks were awarded, a sensitivity analysis confirmed this would not have changed their overall ratings. In contrast, a sensitivity analysis found that if item 7 was added to the critical item list and no concessions for SRs published before 2019 was applied, then despite having met the 2009 PRISMA reporting standards for excluded articles [108], only five (11%) of the systematic reviews would have met the criteria. Consequently, an additional seven SRs would be downrated from moderate to low quality [60, 79–81, 97, 101, 104] and 18 from low to critically low quality [61, 66, 68–70, 72–75, 83–87, 89, 96, 102, 103] (Additional file 5).
Table 3.
Summary of findings of the health effects of Tai Chi
| Study ID | Populations; settings; countries | |||
|---|---|---|---|---|
|
AMSTAR-2 SR quality |
Outcome, subgroup population (no. studies: no. overlapping studies) |
Intervention vs Comparisons (no. participants) |
Estimate of effect* (95% CI) Effect size |
GRADE certainty |
| Adverse events (AE) | ||||
| Adults, older adults; healthy, obesity, cancer, myocardial infarction, chronic heart failure, osteoarthritis, type 2 diabetes mellitus, chronic pulmonary disease; in community settings; China, South Korea, Australia, USA, Brazil, Israel, France, Italy, Turkey | ||||
|
Cui 2019 [64] Critically low |
Serious AE (15 RCTs) | TC (n = 476) vs physically active interventions (n = 489) |
RD 0.0 (− 0.02 to 0.02) Equivalent risk |
LOW dd |
| Non-serious AE (15 RCTs) | TC (n = 476) vs physically active interventions (n = 489) |
RD 0.01 (− 0.01 to 0.03) Equivalent risk |
MODERATE d |
|
| TC related AE (15 RCTs) | TC (n = 476) vs physically active interventions (n = 489) |
RD 0.0 (− 0.01 to 0.02) Equivalent risk |
MODERATE d |
|
| Serious AE (9 RCTs) | TC (n = 421) vs physically inactive interventions (n = 408) |
RD − 0.03 (− 0.06 to 0.00) Equivalent risk |
MODERATE d |
|
| Non-serious AE (9 RCTs) | TC (n = 421) vs physically inactive interventions (n = 408) |
RD 0.03 (− 0.00 to 0.07) Equivalent risk |
MODERATE d |
|
| TC related AE (9 RCTs) | TC (n = 421) vs physically inactive interventions (n = 408) |
RD 0.0 (− 0.01 to 0.02) Equivalent risk |
MODERATE d |
|
| General health and quality of Life | ||||
| Older adults, with or without chronic diseases (also see cancer, cardiovascular diseases, diabetes, chronic obstructive pulmonary disease, Parkinson’s disease, perimenopause) | ||||
| Older adults; healthy, low bone mass, chronic obstructive pulmonary disease, chronic heart failure & depression, benign prostate hyperplasia, total knee arthroplasty, highly maladjusted institutionalized; in community settings, intermediate care rehabilitation unit, long-term care institution; China, Hong Kong, South Korea, USA, Spain, Germany, Iran | ||||
|
Wang 2020 [91] Critically low |
QoL—overall (6 RCTs) | TC (n = 277) vs Ucare, Ex (n = 275) |
SMD 1.23 (0.56 to 1.89) Large effect |
LOW a, b |
| Older adults; with chronic disease—osteopenia, osteoporosis, osteoarthritis, stroke, hypertension, Parkinson’s disease, diabetes; in community settings; China, South Korea, USA, Australia, Turkey | ||||
|
Choo 2020 [62] Critically low |
QoL—physical (6 RCTs: 1 RCT Taylor-Piliae 2020 [90], 1 RCT Wang 2017 [92]) | TC (n = 257) vs noRx, ADL, Ucare, HEd, attention control, waitlist (n = 238) |
SMD 0.46 (0.13 to 0.80) Small to moderate effect |
MODERATE a |
| QoL—mental health (6 RCTs: 1 RCT Wang 2017 [92]) | TC (n = 257) vs noRx, ADL, Ucare, HEd, attention control, waitlist (n = 238) |
SMD 0.21 (0.03 to 0.39) Small effect |
MODERATE a |
|
| Perimenopause | ||||
| Female adults and older adults; perimenopause, with or without low bone mineral density; in community settings; China, USA | ||||
|
Wang 2017 [92] Critically low |
QoL—physical function SF-36 (4 RCTs) | TC + / − placebo capsule (n = 154) vs Ucare, ADL, placebo capsule (n = 160) |
MD − 1.8 points (− 5.2 to 1.6) Equivalent effect, MCID − 2 points [50] |
LOW a, d |
| QoL—bodily pain SF-36 (3 RCTs) | TC + / − placebo capsule (n = 112) vs usual care, ADL, placebo capsule (n = 118) |
MD − 3.6 points (− 6.6 to − 0.6) Moderate effect, MCID − 3 points [50] |
MODERATE a (†LOW) |
|
| QoL—general health SF-36 (3 RCTs) | TC + / − placebo capsule (n = 112) vs ADL, placebo capsule (n = 118) |
MD − 5.1 points (− 7.6 to − 2.6) Large effect, MCID − 2 points [50] |
MODERATE a (†LOW) |
|
| QoL—vitality SF-36 (3 RCTs) | TC + / − placebo capsule (n = 112) vs ADL, placebo capsule (n = 118) |
MD − 5.7 points (− 8.5 to − 2.8) Large effect, MCID − 2 points [50] |
MODERATE a (†LOW) |
|
| QoL—mental health SF-36 (4 RCTs) | TC + / − placebo capsule (n = 154) vs Ucare, ADL, placebo capsule (n = 160) |
MD − 2.5 (− 4.8 to − 0.2) Small effect, MCID − 3 points [50] |
MODERATE a (†LOW) |
|
| QoL—social function SF-36 (3 RCTs) | TC + / − placebo capsule (n = 112) vs ADL, placebo capsule (n = 118) |
MD − 2.2 points (− 5.0 to 0.6) Equivalent effect, MCID − 3 points [50] |
LOW a, d |
|
| Cancer | ||||
| Adults, older adults; cancer; in community settings; China, USA | ||||
|
Ni 2019 [83] Low (†Critically low) |
QoL—physical, breast cancer or female (9 RCTs) | TC (n = 331) vs Ucare, Rehab, HEd, Psych, Ex, sham Qigong (n = 348) |
SMD 0.34 (0.09 to 0.59) Small effect |
LOW aa |
| QoL—psychological, breast cancer or female (9 RCTs) | TC (n = 333) vs Ucare, Rehab, HEd, Psych, Ex, sham Qigong (n = 348) |
SMD 0.60 (0.12 to 1.08) Moderate effect |
VERY LOW aa, b |
|
| QoL—social relationship, breast cancer or female (8 RCTs) | TC (n = 292) vs Ucare, Rehab, HEd, Psych, Ex, sham Qigong (n = 303) |
SMD 0.26 (0.25 to 0.77) Small effect |
VERY LOW aa, b |
|
| Sleep quality, breast or lung cancer (3 RCTs: 2 RCTs Si 2020 [86]) | TC (n = 106) vs Ucare, Psych, sham Qigong (n = 112) |
SMD 0.26 (− 0.02 to 0.53) Equivalent effect |
VERY LOW aa, b, d |
|
| Adults, older adults; lung cancer, prostate cancer; in community settings; China | ||||
|
Song 2018 [87] Low (†Critically low) |
Fatigue < 8 weeks, lung cancer (2 RCTs) | TC (n = 77) vs Ucare, Ex (n = 74) |
SMD − 0.5 (− 0.83 to − 0.18) Moderate effect |
VERY LOW aa, d |
| Fatigue < 8 weeks, prostate cancer (1 RCT) | TC (n = 21) vs Ex (n = 45) |
SMD 0.01 (− 0.51 to 0.52) favours control Equivalent effect |
VERY LOW aa, dd |
|
| Adults, older adults; Breast cancer; in community settings; China, Thailand, USA | ||||
|
Liu LZ 2020 [77] Critically low |
Fatigue 3 months (2 RCTs) | TC + Ucare, Rehab (n = 60) vs Ucare, Rehab (n = 56) |
SMD − 0.91 (− 1.30 to − 0.53) Large effect |
LOW a, d |
| Fatigue 3 months (2 RCTs) | TC (n = 85) vs Psych, sham Qigong (n = 89) |
MD − 0.46 points (− 1.09 to 0.17) Equivalent effect, MCID unknown |
LOW a, d |
|
| Fatigue 6 months (2 RCTs) | TC (n = 80) vs Psych, sham Qigong (n = 83) |
MD − 0.16 (− 0.98 to 0.67) Equivalent effect, MCID unknown |
LOW a, d |
|
| Female adults; breast cancer; in community settings; China, Thailand, USA | ||||
|
Luo 2020 [79] Moderate(†Low) |
Pain, 3 weeks (2 RCTs) | TC (n = 110) vs Rehab (n = 109) |
SMD 0.25 (− 0.02 to 0.51) Equivalent effect |
LOW a, d |
| Pain, 3 months (4 RCTs) | TC (n = 169) vs Ucare, Rehab (n = 168) |
SMD 0.30 (0.08 to 0.51) Small effect |
MODERATE a (†LOW) |
|
| Cardiovascular, diabetes, and risk factors | ||||
| Chronic heart failure | ||||
| Adults, older adults; chronic heart failure, left ventricular ejection fraction (LVEF) ≤ 45%; in community settings; China, USA, UK, Italy | ||||
|
Gu 2017 [66] Low (†Critically low) |
6-min walk test—6-MWT (10 RCTs) | TC (n = 344) vs Ucare, HEd, Ex (n = 379) |
MD 51 m (30.49 to 71.5) Moderate effect, MCID 36 m [57] |
VERY LOW aa, b |
|
Left ventricular ejection fraction—LVEF (7 RCTs) |
TC (n = 283) vs Ucare, HEd, Ex (n = 306) |
MD 7.7% (3.6 to 11.9) Moderate effect, MCID 3.2% [53] |
VERY LOW aa, b |
|
| QoL: Minnesota Living with Heart Failure Questionnaire—MLHFQ (8 RCTs) | TC (n = 280) vs Ucare, HEd, Ex (n = 318) |
MD − 10.4 points (− 14.4 to − 6.3) Moderate effect, MCID − 8 to − 19 [46] |
VERY LOW aa, b |
|
| Adults, older adults; chronic heart failure; in community settings; USA | ||||
|
Taylor-Piliae 2020 [90] Critically low |
Psychological distress, chronic heart failure (2 RCTs) | TC (n = 58) vs HEd, Ex (n = 58) |
SMD − 0.58 (− 0.95 to − 0.22) Moderate effect |
MODERATE d |
| Ischaemic heart disease | ||||
| Older adults; stable angina; in community settings; China, Brazil | ||||
|
Jiang 2018 [74] Low(†Critically low) |
VO2max (4 RCTs) | TC (n = 148) vs noRx, Ex (n = 88) |
SMD 2.2 (0.81 to 3.63) Large effect |
VERY LOW aa, b |
| Adults, older adults; myocardial infarction; in community settings; China | ||||
|
Wu 2020 [96] Low (†Critically low) |
6-min walk time—6MWT (5 RCTs) | TC (n = 234) vs Ucare, HEd, Ex (n = 231) |
SMD 1.3 (0.50 to 2.11) Large effect |
LOW a, b |
| Left ventricular ejection fraction—LVEF (5 RCTs) | TC (n = 234) vs Ucare, HEd, Ex (n = 231) |
SMD 1.0 (0.43 to 1.57) Large effect |
LOW a, b |
|
| Hyperlipidaemia | ||||
| Adults, older adults; hyperlipidemia, type 2 diabetes mellitus, hypertension, obesity; in community settings; China, Hong Kong, Taiwan, Australia | ||||
|
Pan 2016 [84] Low (†Critically low) |
Total cholesterol (6 RCTs) | TC (n = 220) vs Ucare, Ex, waitlist (n = 225) |
MD − 7.7 mg/dL (− 17.3 to 1.4) Equivalent effect, MCID 20 mg/dL (10% reduction from 200 mg/dL) |
VERY LOW a, b, d |
| Triglycerides (6 RCTs) | TC (n = 220) vs Ucare, Ex, waitlist (n = 225) |
MD − 16.8 mg/dL (− 31.3 to − 2.4) Moderate effect, MCID 15 mg/dL (10% reduction from 150 mg/dL) |
MODERATE a |
|
| High-density lipoprotein cholesterol—HDL-C (5 RCTs) | TC (n = 192) vs Ucare, Ex (n = 200) |
MD 0.46 mg/dL (− 0.71 to 1.64) Equivalenteffect, MCID 4 mg/dL (10% increase from 40 mg/dL) |
MODERATE a (†LOW) |
|
| Low-density lipoprotein cholesterol—LDL-C (4 RCTs) | TC (n = 136) vs Ucare, Ex (n = 152) |
MD − 1.61 mg/dL (− 16.25 to 13.02) Equivalent effect, MCIS − 10 mg/dL (10% reduction from 100 mg/dL) |
VERY LOW a, bb, d |
|
| Essential hypertension | ||||
| Adults, older adults; essential hypertension; in community settings; China, Taiwan | ||||
|
Zhong 2020 [105] High |
Systolic blood pressure (9 RCTs) | TC (n = 456) vs noRx, HEd (n = 458) |
MD − 14.8 (− 19.6 to − 10.0) Large effect, MCID − 10 mmHg |
LOW a, b |
| Diastolic blood pressure (9 RCTs) | TC (n = 456) vs noRx, HEd (n = 458) |
MD − 7.0 (− 9.1 to − 5.0) Large effect, MCID − 5 mmHg |
MODERATE a |
|
| Systolic blood pressure (15 RCTs) | TC (n = 406) vs Pharm (n = 348) |
MD − 9.1 (− 14.0 to − 4.1) Moderate effect, MCID − 10 mmHg |
LOW a, b |
|
| Diastolic blood pressure (15 RCTs) | TC (n = 406) vs Pharm (n = 348) |
MD − 5.6 (− 14.0 to − 4.1) Moderate effect, MCID − 5 mmHg |
LOW a, b |
|
| Systolic blood pressure (5 RCTs) | TC (n = 123) vs Ex (n = 123) |
MD − 7.9 (− 14.2 to − 1.7) Small effect, MCID − 10 mmHg |
LOW a, b (†VERY LOW) |
|
| Diastolic blood pressure (5 RCTs) | TC (n = 123) vs Ex (n = 123) |
MD − 3.9 (− 6.5 to − 1.2) Small effect, MCID − 5 mmHg |
MODERATE a (†LOW) |
|
| Adults, older adults; hypertension; in community settings; China, Hong Kong, USA | ||||
|
Taylor-Piliae 2020 [90] Critically low |
QoL—mental health (3 RCTs) | TC (n = 311) vs Ucare (n = 311) |
SMD 0.13 (NI) p = 0.13 Equivalent effect |
MODERATE d |
| QoL—physical (3 RCTs) | TC (n = 311) vs Ucare (n = 311) |
SMD 0.47 (NI) p < 0.001 Small effect |
HIGH | |
| Diabetes mellitus | ||||
| Adults, older adults; type 2 diabetes mellitus; in community settings; China, South Korea, Thailand, Australia | ||||
|
Zhou 2019 [106] Critically low |
Glycosylated haemoglobin—HbA1c % (14 RCTs) | TC (n = 466) vs Ucare, Ucare + TCM, HEd, sham exercise (n = 395) |
MD − 0.88% (− 1.45 to − 0.31) Small effect, MCID 1% [56] |
LOW a, b |
| Systolic blood pressure—SBP (5 RCTs) | TC (n = 151) vs Ucare, ADL, noEx (n = 139) |
MD − 10.0 mmHg (− 15.8 to − 4.3) Moderate effect, MCID 10 mmHg |
MODERATE a (†LOW) |
|
| Diastolic blood pressure—DBP (5 RCTs) | TC (n = 151) vs Ucare, ADL, noEx (n = 139) |
MD − 4.9 mmHg (− 8.2 to − 1.5) Moderate effect, MCID 5 mmHg |
MODERATE a (†LOW) |
|
| QoL physical function – SF36 (5 RCTs) | TC (n = 151) vs Ucare, ADL, noEx (n = 139) |
MD 7.1 (0.79 to 13.4) Large effect, MCID 3 points [50] |
LOW a, b (†VERY LOW) |
|
| QoL bodily pain – SF36 (5 RCTs) | TC (n = 151) vs Ucare, ADL, noEx (n = 139) |
MD 4.3 (0.8 to 7.8) Moderate effect, MCID 3 points [50] |
MODERATE a (†LOW) |
|
| Chronic obstructive pulmonary disease | ||||
| Adults, older adults; chronic obstructive pulmonary disease; in community settings; China, Hong Kong, USA | ||||
|
Guo 2020 [67] Low |
Forced expiratory volume in 1 s—FEV1, ≤ 3 months (3 RCTs) | TC (n = 111) vs noEx (n = 108) |
MD 0.13L (0.06 to 0.20) Moderate effect, MCID 0.1L [43] |
MODERATE a (†LOW) |
| FEV1, ≤ 3 months (5 RCTs) | TC (n = 272) vs Ex + /or breathing Ex (n = 275) |
MD 0.06L (− 0.01 to 0.14) Equivalent effect, MCID 0.1L [43] |
LOW a, d |
|
| 6-min walk time—6MWT, ≤ 3 months (6 RCTs) | TC (n = 182) vs noEx (n = 181) |
MD 24.3 m (6.3 to 42.3) |
LOW a, b (†VERY LOW) |
|
| 6MWT, ≤ 3 months (6 RCTs) | TC (n = 308) vs Ex + /or breathing Ex (n = 313) |
MD 7.5 m (2.1 to 12.3) |
MODERATE a |
|
| QoL—St George Respiratory Questionnaire—SGRQ, ≤ 3 months (3 RCTs) | TC (n = 129) vs noEx (n = 128) |
MD − 8.7 points (− 14.6 to − 2.7) |
MODERATE a (†LOW) |
|
| QoL—SGRQ, ≤ 3 months (4 RCTs) | TC (n = 260) v Ex + /or breathing Ex (n = 265) |
MD − 1.9 points (− 4.6 to 0.7) |
MODERATE a |
|
| Cognitive function and impairment | ||||
| Older adults; no cognitive impairment; in in community settings; China, Hong Kong, Japan, France | ||||
|
Wayne 2014 [94] Critically low |
Executive function (4 RCTs) | TC (n = 151) vs noEx (n = 270) |
SMD 0.90 (0.03 to 1.78) Large effect |
MODERATE b |
| Executive function (2 RCTs) | TC (n = 67) vs Ex (n = 69) |
SMD 0.51 (0.17 to 0.85) Moderate effect |
MODERATE d |
|
| Older adults; Mild cognitive impairment; in community settings; China, Thailand, USA, France | ||||
|
Zhang 2020 [102] Low (†Critically low) |
Global cognitive function—Mini-Mental State Examination—MMSE (5 RCTs) | TC (n = 325) vs Cognition-action, Ucare, HEd, Ex, other activities (n = 460) |
MD 0.29 points (− 0.61 to 0.74) Equivalent effect, MCID 1 point [41] |
HIGH |
| Memory—Delayed Recall Test (4 RCTs) | TC (n = 297) vs ADL, HEd, Ex (n = 429) |
MD 0.37 points (0.13 to 0.61) A positive effect, MCID unknown |
HIGH | |
| Performance—Digit Span Test (4 RCTs) | TC (n = 297) vs ADL, HEd, Ex (n = 429) |
MD 0.03 point (− 0.16 to 0.22) Equivalent effect, MCID unknown |
HIGH | |
| Fatigue, fibromyalgia, and sleep quality | ||||
| Fatigue, any cause | ||||
| Adults, older adults; fatigue without serious ailments, cancer, multiple sclerosis, chronic obstructive pulmonary disease, insomnia, rheumatoid arthritis; in community settings; China, Hong Kong, USA, Spain, Germany | ||||
|
Xiang 2017 [97] Moderate (†Low) |
Fatigue (10 RCTs) | TC (n = 356) vs noRx, Ucare, HEd, Ex, sham Qigong (n = 333) |
SMD − 0.45 (− 0.70 to − 0.20) Small effect |
MODERATE a |
| Vitality (4 RCTs) | TC (n = 115) vs noRx, HEd, Ex (n = 333) |
SMD 0.63 (0.20 to 1.07) Moderate effect |
LOW aa |
|
| Depression (7 RCTs) | TC (n = 216) vs noRx, Ucare, HEd, Ex, other control (n = 199) |
SMD − 0.58 (− 1.04 to − 0.11) Moderate effect |
VERY LOW aa, b |
|
| Fibromyalgia | ||||
| Adults; fibromyalgia; in community settings; USA, South Korea, UK, Italy | ||||
|
Cheng 2019 [61] Low (†Critically low) |
QoL—Fibromyalgia impact questionnaire—FIQ 12–16 weeks (4 RCTs) | TC (n = 158) vs Ucare (n = 149) |
SMD − 0.61 (− 0.90 to − 0.31) Moderate effect |
MODERATE a (†LOW) |
| QoL—FIQ 24–32 weeks (2 RCTs) | TC (n = 82) vs Ucare (n = 78) |
SMD − 0.49 (− 1.56 to 0.58) Equivalent effect |
VERY LOW a, b, dd |
|
| Pain (3 RCTs) | TC (n = 100) vs noRx, Ucare, HEd, Ex (n = 90) |
SMD − 0.88 (− 1.58 to − 0.18) Large effect |
VERY LOW a, b, d |
|
| Sleep quality | ||||
| Adults, older adults; healthy, stroke, fibromyalgia, cancer, arthritis, depression, chronic kidney disease, heart disease; in community settings; China, Japan, Vietnam, USA, Italy, Iran | ||||
|
Si 2020 [86] Low (†Critically low) |
Pittsburgh Sleep Quality Index, healthy (10 RCTs) | TC (n = 426) vs noRx, Ex, HEd (n = 401) |
SMD − 0.68 (− 1.06 to − 0.31) Moderate effect |
LOW a, b |
| Pittsburgh Sleep Quality Index, chronic disease (15 RCTs) | TC (n = 543) vs Ucare, Hed, Psych, Rehab, sham Qigong, acupuncture, waitlist (n = 564) |
SMD − 0.39 (− 0.74 to − 0.05) Small effect |
LOW a, b |
|
| Mental health | ||||
| Depression, anxiety, stress, mood for general populations (also see chronic heart failure, stroke, knee osteoarthritis, fatigue) | ||||
| Adults, older adults; depression and/or chronic diseases; Asian, North American and European countries | ||||
|
Yin 2014 [98] Low |
Depression (25 RCTs: 1RCT Lyu 2020 [80], 1 RCT Hu 2020 [70]) |
TC vs noRx, Ex, sham/other (total sample < 1435) |
SMD 0.36 (0.19 to 0.53) Small effect |
HIGH |
| Anxiety (11 RCTs) |
TC vs noRx (total sample < 1435) |
SMD 0.34 (0.02 to 0.66) Small effect |
MODERATE b |
|
| Adults, older adults; healthy, osteoarthritis, rheumatoid arthritis, fibromyalgia, HIV infection, depression, frail; in community settings; China, USA, Australia, UK, Germany, France | ||||
|
Wang 2010 [93] Critically low |
Stress (4 RCTs) |
TC vs ADL, Psych, waitlist (total sample n = 308) |
SMD 0.97 (0.06 to 1.87) Large effect |
VERY LOW aa, bb |
| Mood / affect (2 RCTs) |
TC vs ADL, Psych, waitlist (total sample n = 191) |
SMD 0.25 (− 0.04 to 0.53) Equivalent effect |
VERY LOW aa, d |
|
| Schizophrenia | ||||
| Adults, older adults; schizophrenia; in hospital, long-stay care, halfway house service; China | ||||
|
Zheng 2016 [104] Moderate (†Low) |
Negative symptoms—Positive and Negative Syndrome Scale—PANSS (6 RCTs) | TC + Ucare (n = 200) vs Ucare + / − Pharm, HEd, Ex, noEx, waitlist (n = 251) |
SMD − 0.87 (− 1.51 to − 0.24) Large effect |
LOW a, b |
| Positive symptoms—PANSS (5 RCTs) | TC + Ucare (n = 170) vs Ucare + / − Pharm, HEd, Ex, noEx, waitlist (n = 221) |
SMD − 0.09 (− 0.44 to 0.26) Equivalent effect |
MODERATE a (†LOW) |
|
| Discontinuation rate (4 RCTs) | TC + Ucare (n = 170) vs Ucare + / − Pharm, HEd, Ex, noEx, waitlist (n = 221) |
RR 0.06 (0.23 to 1.40) 3 fewer per 100 adults |
VERY LOW a, dd |
|
| Musculoskeletal conditions and pain | ||||
| Osteoarthritis | ||||
| Older adults; knee osteoarthritis; in community settings; China, South Korea, USA | ||||
|
Hu 2020 [70] Low (†Critically low) |
WOMAC pain (14 RCTs) | TC (n = 455) vs Ucare, noEx, HEd, PT (n = 422) |
SMD − 0.69 (− 0.95 to − 0.44) Moderate effect |
MODERATE a |
| WOMAC stiffness (12 RCTs) | TC (n = 396) vs Ucare, noEx, HEd, PT (n = 373) |
SMD − 0.65 (− 0.98 to − 0.33) Moderate effect |
LOW a, b |
|
| WOMAC physical function (13 RCTs) | TC (n = 437) vs Ucare, noEx, HEd, PT (n = 407) |
SMD − 0.92 (− 1.16 to − 0.69) Large effect |
MODERATE a |
|
| Depression (3 RCTs: 1 RCT in Yin 2014 [98]) | TC (n = 167) vs Ucare, noEx, HEd, PT (n = 152) |
SMD − 0.46 (− 0.68, − 0.24) Small effect |
MODERATE a |
|
| Arthritis self-efficacy scale (4 RCTs) | TC (n = 185) vs Ucare, noEx, HEd, PT (n = 167) |
SMD 0.27 (0.06 to 0.48) Small effect |
MODERATE a (†LOW) |
|
| Adults, older adults; healthy, osteoarthritis; in in community settings | ||||
|
Su 2020 [88] Critically low |
Knee extensor muscle strength, females (60°/s) (2 RCTs) | TC (n = 40) vs noRx, Ex, Pharm, HEd (n = 45) |
MD 17.5 (− 12.0 to 47.0) Equivalent effect, MCID unknown |
VERY LOW a, b, dd |
| Knee flexor muscle strength, females (60°/s) (2 RCTs) | TC (n = 40) vs noRx, Ex, Pharm, HEd (n = 45) |
MD 22.1 (1.1 to 43.2) Positive effect, MCID unknown |
VERY LOW a, dd (†LOW) |
|
| Knee flexor muscle strength one maximum strength—1-RM (2 RCTs) | TC (n = 57) vs noRx, HEd (n = 57) |
MD 3.3 (2.1 to 4.4) Positive effect, MCID unknown |
LOW a, d |
|
|
Knee extensor muscle strength 1-RM (4 RCTs) |
TC (n = 114) vs noRx, HEd, Ex (n = 112) |
SMD 0.90 (0.34 to 1.45) Large effect |
MODERATE a (†LOW) |
|
| Rheumatoid arthritis | ||||
| Adults, older adults; rheumatoid arthritis; in community settings; China, South Korea, USA | ||||
|
Mudano 2019 [82] High |
Pain, visual analogue scale, 12 weeks (2 RCTs) | TC (n = 42) vs noEx, Ex (n = 39) |
SMD − 0.95 (− 1.41 to − 0.49) Large effect |
VERY LOW aa, dd |
| Disease activity, DAS-28-ESR, 12 weeks (1 RCT) | TC (n = 29) vs HEd (n = 14) |
MD − 0.40 points (− 1.10 to 0.30) Equivalent effect, MCID − 1.17 points [58] |
VERY LOW aa, dd |
|
| Function, Health Assessment Questionnaire – HAQ, 12 weeks (2 RCTs) | TC (n = 39) vs Hed, Ex (n = 24) |
MD − 0.33 points (− 0.79 to 0.12) Equivalent effect, MCID − 0.38 points [58] |
VERY LOW aa, b, dd |
|
| Low back pain | ||||
| Adults, older adults; Low back pain; in community settings; China, Australia | ||||
|
Qin 2019 [85] Low (†Critically low) |
Pain VAS 1–10 scale (3 RCTs) | TC (n = 123) vs ADL, waitlist (n = 120) |
MD − 1.2 points (− 2.3 to − 1.1) Moderate effect, MCID − 1.2 |
LOW a, b (†VERY LOW) |
| Pain VAS 1–10 scale (5 RCTs) | TC + Ucare (n = 363) vs Ucare (n = 268) |
MD − 1.1 (− 1.3 to − 0.9) Moderate effect, MCID − 1.2 |
MODERATE a |
|
| Headache | ||||
| Adults, older adults; chronic pain from tension headaches; in community settings; USA | ||||
|
Hall 2017 [68] Low (†Critically low) |
Pain SF-36 15 weeks (1 RCT) | TC (n = 13) vs waitlist (n = 17) |
SMD − 1.85 (− 2.73 to − 0.97) Large effect |
VERY LOW aa, dd |
| Osteoporosis, osteopenia | ||||
| Adults, older adults; osteoporosis, osteopenia; in community settings; NI countries | ||||
|
Zhang 2019 [101] Moderate (†Low) |
Spine Bone mineral density—BMD (6 RCTs) | TC (n = 128) vs noRx (n = 119) |
MD 0.04 g/cm2 (0.02 to 0.06) Small effect, MCID ~ 0.05 g/cm2 [54] |
MODERATE a (†LOW) |
| Femur BMD (3 RCTs) | TC (n = 85) vs noRx (n = 83) |
MD 0.04 g/cm2 (0.01 to 0.06) Small effect, MCID ~ 0.05 g/cm2 [54] |
LOW a, d |
|
| Spine BMD (2 RCTs) | TC (n = 52) vs Ucare (n = 55) |
MD 0.16 g/cm2 (0.09 to 0.23) Large effect, MCID ~ 0.05 g/cm2 [54] |
LOW a, d |
|
| Femur BMD (2 RCTs) | TC (n = 52) vs Ucare (n = 55) |
MD 0.16 g/cm2 (0.04 to 0.29) Large effect, MCID ~ 0.05 g/cm2 [54] |
VERY LOW a, b, d |
|
| Stroke, Parkinson’s disease, and falls | ||||
| Stroke | ||||
| Adults, older adults; healthy, type 2 diabetes mellitus, hyperlipidaemia; in community settings; China | ||||
|
Zheng 2015 [103] Low (†Critically low) |
Incidence of nonfatal stroke over 1–2 years (2 RCTs) | TC + Ucare (n = 62) vs Ucare (n = 58) |
RR 0.11 (0.01 to 0.85) 89% reduced risk |
LOW a, d |
|
Incidence of fatal stroke over 1–2 years (2 RCTs) |
TC + Ucare (n = 62) vs Ucare (n = 58) |
RR 0.33 (0.05 to 2.05) 77% reduced risk |
LOW a, d (†VERY LOW) |
|
| Adults, older adults; stroke survivors; in community settings; NI countries | ||||
|
Lyu 2018[81] Moderate (†Low) |
Berg Balance Scale—BBS (2 RCTs) | TC (n = 75) vs Rehab (n = 75) |
MD 5.2 points (3.4 to 7.1) Moderate effect, MCID 4.3 to 7.3 points [47] |
LOW a, d |
|
Fugl-Meyer Assessment FMA—all four limbs (2 RCTs) |
TC + Rehab (n = 51) vs Rehab (n = 49) |
MD 4.5 points (1.9 to 7.1) A positive effect, MCID unknown |
LOW a, d |
|
| FMA—upper extremity (2 RCTs) | TC + Rehab (n = 56) vs Rehab (n = 51) |
MD 8.3 points (4.7 to 11.8) Large effect, MCID 5.3 points [51] |
LOW a, d |
|
| FMA—lower extremity (3 RCTs) | TC + Rehab (n = 85) vs Rehab (n = 81) |
MD 2.8 points (0.95 to 4.56) Small effect, MCID 6 points [52] |
VERY LOW a, b, d |
|
| Timed up and go—TUG (4 RCTs) | TC + Rehab (n = 100) vs Rehab (n = 96) |
MD 2.6 s (1.8 to 3.4) Small effect, MCID 8 s [47] |
LOW a, d |
|
|
Activities of daily living—Barthel Index (2 RCTs) |
TC (n = 81) vs Rehab (n = 85) |
MD 9.9 points (6.8 to 13.0) Large effect, MCID 6.8 points [44] |
LOW a, d |
|
| Adults, older adults; stroke survivors; in community settings; China, South Korea, Japan, USA, Israel | ||||
|
Lyu 2020 [80] Moderate (†Low) |
Depression (6 RCTs) | TC (n = 278) vs Rehab (n = 280) |
SMD 0.36 (0.10 to 0.61) Small effect |
LOW aa |
| Parkinson’s disease | ||||
| Older adults; Parkinson’s disease; in community settings; NI countries | ||||
|
Yu 2018 [100] Critically low |
Unified Parkinson’s Disease Rating III: Motor (8 RCTs) | TC (n = 204) vs noRx, Ucare, Pharm, Ex (n = 262) |
MD − 3.7 points (− 5.7 to − 1.7) Moderate effect, MCID − 3.3 points [48] |
MODERATE b |
| Timed up and go—TUG (7 RCTs) | TC (n = 188) vs noRx, Ucare, Pharm, Ex (n = 251) |
SMD − 0.50 (− 0.88 to − 0.11) Moderate effect |
HIGH | |
| Berg balance scale—BBS (6 RCTs) | TC (n = 144) vs noRx, Ucare, Pharm, Ex (n = 145) |
SMD 0.85 (0.44 to 1.27) Large effect |
HIGH (†MODERATE) |
|
| QoL – Parkinson’s Disease Questionnaire—PDQ-39, PDQ-8 (3 RCTs) | TC (n = 104) vs noRx, Ucare, Pharm, Ex (n = 159) |
SMD − 0.75 (− 1.45 to − 0.04) Moderate effect |
HIGH (†MODERATE) |
|
| Falls and risk factors | ||||
| Older adults; with or without a history of falling, stroke, Parkinson’s disease, females with osteopenia; in hospital, in community settings; China, Taiwan, USA, Canada, Australia, New Zealand, Netherlands | ||||
|
Huang 2017 [73] Low (†Critically low) |
Rate of people who fell (no. of fallers) (16 RCTs) | TC (n = 1889) vs ADL, noRx, PT, Ex (n = 1650) |
RR 0.80 (0.72 to 0.88) 20% reduced risk, 9 fewer per 100 |
MODERATE e |
| Incidence of falls (no. falls) (15 RCTs) | TC (n = 1512) vs ADL, noRx, PT, Ex (n = 1542) |
RR 0.69 (0.60 to 0.80) 31% reduced risk |
MODERATE e |
|
| Older adults; in hospital, nursing home, in community settings; China, USA, Canada, Australia, New Zealand, UK, Netherlands | ||||
|
Huang 2020 [71] Critically low |
Balance – Single Leg Stance (SLS) (8 RCTs) | TC (n = 417) vs ADL, Ex, other activities (n = 419) |
MD 5.8 s (0.62 to 10.90) Small effect, MCID 41 s [45] |
VERY LOW a, bb |
| Berg balance scale—BBS (4 RCTs) | TC (n = 412) vs ADL, Ex (n = 400) |
MD 1.0 points (0.2 to 1.9) Small effect, MCID 4 points [42] |
MODERATE a |
|
| Timed up and go—TUG (6 RCTs) | TC (n = 190) vs ADL, Ex (n = 178) |
MD − 0.71 s (− 0.88 to − 0.54) Probably small effect, MCID unknown |
MODERATE a (†LOW) |
|
| Older adults; with or without a history of falling; in community settings; USA, Canada, China, Vietnam, Iran | ||||
|
Kruisbrink 2020 [75] Low (†Critically low) |
Fear of falling (6 RCTs) | §TC with an instructor vs TC with no information about instructor (NI sample size) |
SMD.B − 1.05 (− 1.60 to − 0.50) Large effect |
VERY LOW aa, b, e |
§Erratum published 3 Sept. 2022 confirming control group was also TC. CI confidence interval, RD risk difference, MD mean difference, MID minimally important difference, SMD standardized mean difference, SMD.B: regression co-efficient for standardised mean difference, RR relative risk, RCT randomized controlled trial, QoL quality of life, ADL routine activities of daily living/ routine lifestyle, Ex exercise (any type, including stretching), HEd health/lifestyle/other education, noRx no treatment, control, Pharm pharmaceutical drugs / medication, Psych psychological interventions, counselling, support, PT physical therapy/physiotherapy, Rehab rehabilitation programs, TC Tai Chi intervention, TCM traditional Chinese herbal medicine, Ucare usual care, conventional treatment, standard medical care, MCID minimal clinically important difference, for SMD ≥ 0.50 is a moderate effect and SMD ≥ 0.80 large effect, a serious risk of bias, aa very serious risk of bias, b serious inconsistency between studies, bb very serious inconsistency between studies, c serious indirectness of evidence, cc very serious indirectness of evidence, d serious imprecision of effect, dd very serious imprecision of effect, e serious publication bias, ee very serious publication bias
*Estimate of effect favours Tai Chi unless stated otherwise
†Sensitivity analysis suggests a different rating.
For AMSTAR-2 refer to Additional File 5. For GRADE certainty refer to Additional File 6
GRADE evidence certainty
Of the 114 estimates of effect that were extracted, only eight (7.0%) were graded as high certainty evidence; 43 (37.7%) moderate, 36 (31.6%) low, and 27 (23.7%) very low. Serious or very serious concerns with the risk of bias of the individual RCTs was the predominant issue that negatively impacted 92 (80.7%) of the extracted effect estimates. Imprecision in effect estimates was the next most common issue (43 effect estimates, 37.7%) that was a function of the small number of studies in the meta-analysis and/or their small sample sizes. Thirty-seven (32.5%) effect estimates were graded down for inconsistency. Whilst all the meta-analyses had at least one RCT with a small sample size, only three instances of publication bias were identified. However, if the thresholds and criteria from the post hoc sensitivity analyses were applied, then 31 (25.8%) estimates would be further downrated due to serious or very serious concerns with imprecision, and 6 (5.0%) estimates would be rated up from very serious to serious concerns. In this instance, only 6 (5.0%) would be graded as high certainty evidence; 28 (23.3%) moderate, 53 (44.2%) low, and 33 (27.5%) very low. Details of the GRADE certainty assessments can be found in Additional file 6.
Summary of the effects of Tai Chi
Table 3 presents the Summary of Findings of 114 estimates of effect and the GRADE certainty of the evidence of Tai Chi SRs according to population, outcome, and comparison that were extracted from 37 SRs with a meta-analysis. Of the 108 estimates of effect reported for Tai Chi treatment outcomes, 107 favoured Tai Chi. However, 21 estimates were not significant and are interpreted as equivalent to the comparison groups. This included the one estimate that favoured the comparison groups.
Adverse events
Cui et al. [64] evaluated the overall safety of Tai Chi. No significant differences were found in the risk of serious, non-serious, or intervention-related adverse events (AEs) from Tai Chi compared to both physically active and inactive interventions in healthy adults and people with chronic diseases (low to moderate certainty). The most common AEs were non-serious AEs, such as musculoskeletal aches and pains. Serious AEs were found in studies involving patients with heart failure, including death, hospitalized, and worsening heart failure or its co-morbidities. The reviewers reported that no serious AEs were determined to be attributable to Tai Chi or control conditions. The reviewers noted that an important limitation of the evidence was ongoing underreporting of AEs in many RCTs and only a few used an AE monitoring protocol.
Twenty of the other SRs included in the evidence synthesis also reported AEs (Table 2). Of which, 18 reported no AEs [62, 70, 72, 76, 81, 83, 84, 86, 89, 90, 93, 94, 96–98, 103, 104] and two reported mild, transient musculoskeletal AEs [82, 85].
General health, quality of life, and wellbeing
Whilst most SRs were for adults and older adults with chronic diseases, a SR with no meta-analysis reported various physical and psychological benefits of Tai Chi for students in higher education [95]. Another SR with no meta-analysis reported improved workplace productivity/motivation and work-related stress for healthcare workers [63].
Health-related quality of life (QoL) outcomes were frequently evaluated for adults and older adults, most of whom had one or more chronic diseases. The results from the meta-analyses of QoL outcomes for single conditions are presented in their respective sections below. Disease-specific QoL outcomes are reported for chronic heart failure [66], chronic obstructive pulmonary disease [67], fibromyalgia [61], and Parkinson’s disease [100], and generic QoL outcomes for cancer [83], hypertension [90], and type 2 diabetes mellitus [106]. Other related outcomes are reported for stroke (activities of daily living) [81], rheumatoid arthritis (functional status), and knee osteoarthritis (self-efficacy) [70].
Three additional SRs representing QoL outcomes for other populations were also selected. For women in the perimenopausal life stage, there was moderate certainty evidence of a clinically important effect for some of the Short Form Health Survey 36-item (SF-36) QoL domains (general health, vitality, bodily pain, and mental health) and low certainty evidence of equivalence to other control groups for the physical and social function QoL domains [92]. For older adults with or without chronic diseases, there were clinically important improvements in overall QoL that was measured using various generic and disease-specific QoL tools (low certainty) [91]. For those with chronic diseases, there were small improvements in both the physical and mental health SF-36/SF-12 QoL domains (moderate certainty) [62]. For the physical QoL domain, two RCTs overlapped with other reported effect estimates, one for hypertension (high certainty, small effect) [90] and one for perimenopause (low certainty, equivalent effect) [92], and for the mental health domain, one RCT overlapped with the perimenopause effect estimate (moderate certainty, small effect) [92].
Cancer
The effects of Tai Chi on QoL, pain, fatigue, and sleep were commonly appraised, particularly for breast cancer survivors. Four SRs were selected [77, 79, 83, 87]; however, none of the SRs were comprehensive and all of them had missed numerous eligible RCTs. Most of the effects from Tai Chi were either small or equivalent to the comparison groups, or there was very low certainty evidence.
For female cancer survivors, the evidence was more mixed. There was low certainty evidence of small improvements in the QoL physical domain [83]. However, the effects of Tai Chi were unclear for both psychological and social QoL domains due to very low certainty evidence [83]. For breast cancer survivors only, there were clinically important improvement in fatigue at 3 months when Tai Chi was added to usual care or rehabilitation (low certainty) [77], yet no difference at 3 or 6 months compared to psychological interventions or sham Qigong (low certainty evidence) [77]. Similarly, compared to usual care or rehabilitation, there were small improvements in pain at 3 months (moderate certainty), yet no difference at 3 weeks compared to rehabilitation only (low certainty) [79].
Cardiovascular diseases, diabetes, and risk factors
For adults and older adults post myocardial infarction, clinically important improvements in VO2-max were found (low certainty) [96], but the effects were unclear for older adults with stable angina due to very low certainty evidence [74]. For those with chronic heart failure, the effects of Tai Chi on left ventricular ejection fraction (LVEF), distance they could walk in 6 min, and disease-specific QoL were also unclear due to very low certainty evidence [66]. However, there was moderate certainty of clinically important improvements in psychological distress for people with chronic heart failure [90].
Clinically important reductions in both systolic and diastolic blood pressure were found for people with essential hypertension (moderate to low certainty) [102] and diabetes mellitus (moderate certainty) [106]. There was probably no effect for normotensive adults; however, the estimates are not reported because some RCTs were excluded from the final the meta-analyses and no sensitivity analysis was reported [65]. The antihypertensive effects for people with essential hypertension were greatest when Tai Chi was compared to no intervention or health education (moderate to low certainty, large effect), followed by anti-hypertensive medication (low certainty, moderate effect), and then other exercise interventions (moderate to low certainty, small effect) [102]. Compared to usual care, the effects of Tai Chi on psychological QoL were equivalent (moderate certainty) and there were small improvements in physical QoL (high certainty) [90].
The effects of Tai Chi were mixed for people with hyperlipidemia. Only moderate reductions in triglyceride levels were found (moderate certainty), and there was probably no difference between Tai Chi and usual care or other types of exercise on total cholesterol, high-density lipoprotein cholesterol, or low-density lipoprotein cholesterol (low to very low certainty) [84].
For people with type 2 diabetes mellitus, improvements in glycemic control were small and unlikely to be clinically important (moderate certainty) [106]. However, there were clinically important improvements in the QoL domains of pain and physical function (moderate certainty) [106].
Chronic obstructive pulmonary disease
When Tai Chi was compared to no exercise controls for people with chronic obstructive pulmonary disease, there were clinically important improvements in both lung function and disease-specific QoL (moderate certainty); however, the improvement in the distance walked in 6 min was unlikely to be clinically important (low certainty) [67]. Tai Chi was unlikely to be any more effective than other types of exercise (moderate to low certainty) [67].
Cognitive function and impairment
Clinically important effects on the executive function of people with no cognitive impairment were found when Tai Chi was compared to no exercise and exercise (moderate certainty) [94]. For people with mild cognitive impairment, only the delayed recall test improved (high certainty) [102]. There were no differences between the Tai Chi and control groups’ mini-mental state examination (MMSE) (high certainty) and digit span tests (moderate certainty) [102].
Fatigue, sleep quality, and fibromyalgia
For adults suffering from fatigue, with or without any serious ailments or chronic diseases, there were clinically important improvements in vitality (low certainty) and small improvements in fatigue (moderate certainty) [97].
For healthy adults, there were moderate improvements in sleep quality (low certainty) and small improvements for adults with chronic diseases (low certainty) [86]. Two of the three RCTs in the meta-analysis of sleep quality for cancer survivors (very low certainty, equivalent effect) [83] overlapped with the this larger meta-analysis of 15 RCTs for adults with chronic diseases [86].
For adults with fibromyalgia, there were clinically important improvements in activities of daily living after 12 to 16 weeks when Tai Chi was compared to usual care (moderate certainty); however, at 24 to 32 weeks, the effects were unclear due to very low certainty evidence [61]. Whether Tai Chi reduced the pain from fibromyalgia was also unclear due to very low certainty evidence [61].
Immunity
One SR with no meta-analysis reported improvements in cell-mediated immunity (including in people with HIV infections) and antibody levels (including in older adults) [69]. However, none of the studies included in the SR evaluated whether these improvements translated into direct clinical outcomes such as preventing or recovering from infections.
Mental health
Except for schizophrenia and university students with symptoms of depression, the SRs pooled the results of studies of participants who had mental health problems such as depression with studies of participants who had other health conditions in which mental health problems are a common comorbidity.
For adults and older adults with chronic diseases, including those suffering from depression, a 2014 SR reported small improvements in depression outcomes (high quality) and anxiety outcomes (moderate quality) and both estimates of effect were stable after adjusting for participants’ severity of baseline symptoms, health status, age, and ethnicity, and whether depression or anxiety was the primary outcome of the RCT [98]. The findings were congruent with more recent SRs that reported depression outcomes for stroke survivors (low certainty, small effect, one overlapping RCT) [80], fatigue from any cause (very low certainty, moderate effect, no overlapping RCTs) [97], knee osteoarthritis (moderate certainty, small effect, one overlapping RCT) [40] and older adults (moderate certainty, small effect, three overlapping RCTs) [62], and also psychological distress associated with chronic heart failure (moderate certainty, moderate effect, no overlapping RCTs) [90]. However, in another SR with no overlapping RCTs, due to very low certainty evidence, it was unclear if stress or mood outcomes improved in those with chronic diseases [93].
Improvements in depression outcomes were found when university students with depression or depressive symptoms used Tai Chi compared to no intervention or other exercise; however, the effect estimate was not extracted due to a probable data transformation error [99].
Clinically important improvements in negative symptoms (low certainty), but not positive symptoms (moderate certainty) of schizophrenia, were found when Tai Chi was added to usual care; however, it was unclear if discontinuation rates were lower (very low certainty) [104].
Multiple sclerosis
A SR with no meta-analysis reported positive improvements in fatigue, as well as balance, gait, flexibility, depression, and quality of life in adults with multiple sclerosis [89]. However, despite this positive trend, in a subgroup analysis of fatigue for any condition, the findings from two RCTs (one overlapping) were not significant (SMD − 0.77, 95% CI − 1.76 to 0.22) [97].
Musculoskeletal conditions and pain
Most of the SRs and their included primary studies were for older adults with knee osteoarthritis. There were clinically important improvements in pain (moderate certainty), stiffness (low certainty), physical function (moderate certainty), and depression outcomes (moderate certainty), as well as small improvements in self-efficacy (moderate certainty) [70]. Similar findings were also reported in the most recent SR for any type of osteoarthritis [78]. However, the effect estimates were not extracted due probable data transformation errors and/or extensive overlap with the meta-analyses reported for knee osteoarthritis.
The effects of Tai Chi on knee flexor and extensor muscle strength were also evaluated in adults with or without osteoarthritis. The effects favoured Tai Chi, especially when Tai Chi was only compared to non-exercise controls (low or moderate certainty) [88].
For people with rheumatoid arthritis, whilst the results were promising, there was only very low certainty evidence about the effects of Tai Chi on pain, disease activity, and function [82].
The findings were mixed for people with osteoporosis or osteopenia. Compared to usual care, there were clinically important improvements in spine bone mineral density (BMD) (low certainty) and possibly femur BMD (very low certainty) [101]. Compared to no-treatment controls, the improvements in spine BMD (moderate certainty) and femur BMD (low certainty) were small and probably clinically unimportant [101].
Regarding pain outcomes, there were clinically important improvements in bodily pain for perimenopausal females with or without osteopenia/osteoporosis (moderate certainty) [92] and low back pain when compared to usual care (moderate certainty) or inactive controls (low certainty) [85]. However, due to very low certainty evidence, it was unclear if Tai Chi reduced pain caused by tension headaches [68]. No SRs were identified that synthesized results for neck or shoulder pain.
Stroke, Parkinson’s disease, and falls
There was low certainty evidence of a 77% reduced risk of fatal stroke and an 89% reduction in the risk of nonfatal stroke over 1 to 2 years, in healthy older adults and people with diabetes and/or hyperlipidemia [103]. For stroke survivors, the addition of Tai Chi to their rehabilitation program resulted in clinically important improvements in upper limb function (low certainty) and balance (low certainty). The effects on lower limb function were unclear due to very low certainty evidence and there were only small improvements in timed up-and-go tests (low certainty) [81]. Compared to rehabilitation, there was low certainty evidence of improvements in disease-specific activities of daily living [81] and depression outcomes [80]. However, the improvements in depression were small and unlikely to be clinically important.
Clinically important improvements in the overall motor function of people with Parkinson’s disease (moderate certainty), balance (high certainty), and timed up-and-go tests (high certainty), as well as their disease-specific QoL (high certainty), were found [100].
Falls prevention and associated risk factors such as balance, mobility, and fear of falling were commonly reviewed. Tai Chi was found to reduce the risk of falling by at least 20% (NNT: 11) for older adults with or without a history of falling, including adults with Parkinson’s disease and stroke survivors (moderate certainty) [73]. Subgroup analysis suggested there might be a dose-relationship between the number of times Tai Chi was practiced per week and falls risk, but the findings were not statistically significant [73]. Falls risk factors also improved for older adults; however, the effects were unlikely to be clinically important (moderate or very low certainty) [71]. Mixed findings for falls risk factors in prefrail and frail older adults were also reported in a SR with no meta-analysis [60]. It was unclear if Tai Chi reduced the fear of falling due to very low certainty evidence [75].
Vestibular disorders
A SR with no meta-analysis of Tai Chi for vestibular rehabilitation reported improvements in dynamic balance, gait, and postural performance [72].
Discussion
This critical overview comprehensively identified SRs of Tai Chi published in English, Chinese, and Korean languages that evaluated the effectiveness and safety of Tai Chi for health promotion, and disease prevention and management. Tai Chi was found to be generally safe, even for frail older adults; however, mild, transient discomfort during the first few weeks was reported by some participants. Clinically important benefits were most consistently reported for Parkinson’s disease, falls risk, knee osteoarthritis, low back pain, cardiovascular diseases including hypertension, and stroke.
Despite the large number of SRs, there were gaps in the available SR evidence. For the most part, the conditions most commonly evaluated by SRs generally matched those most commonly evaluated by primary studies. However, based on the bibliometric analyses of studies evaluating Tai Chi interventions [6, 7], the following had sufficient RCTs and were yet to be systematically reviewed. These were for people with depression, anxiety, drug dependency, musculoskeletal conditions of the hip, neck or shoulder, sarcopenia/frailty, diabetic neuropathy, or dysmenorrhea. Other evidence gaps included a paucity of SRs examining effects of Tai Chi for disease prevention. Except for stroke prevention, only indirect disease prevention outcomes (i.e. risk factors) such as hypertension, hyperlipidemia, HbA1c, falls prevention, balance, mobility, bone mineral density, and executive cognitive function were identified. Finally, whilst some SRs included healthy participants, with the exception of executive cognitive function [94], only a few evaluated the effects of Tai Chi for health promotion, quality of life, and wellbeing in healthy participants [63, 95]. This is despite an astounding number of RCTs, well over 100 [6, 7], evaluating these outcomes in healthy population groups.
It is noteworthy that a rapid search of PubMed, Embase, Cochrane Library, and CNKI databases for SRs published between 1 January 2021 and 5 June 2022 identified 38 potentially eligible SRs. Therefore, some of the identified gaps in the evidence may have been addressed and there may be higher quality, more comprehensive SRs than those included in this synthesis. Given this rapidly growing evidence base, an update of this overview is warranted.
Limitations of the evidence
Rather than relying on the conclusions in the SRs, we appraised the evidence for the included estimates of effects. Notably, the GRADE certainty of the evidence for just over half of the estimates of effect was rated as low or very low. This was despite making a number concessions according to a pragmatic algorithm developed by Pollock et al. [38] when grading over 100 estimates for a Cochrane overview. Like Pollock et al. [38], the risk of bias for blinding focused on the study investigators rather than participants; the cut-off for the optimum information size for continuous outcomes was set at ≥ 200 participants, rather than the 400 tentatively recommended by GRADE [31]; and the cut-off for the I2 statistic when rating statistical heterogeneity was set at ≤ 75%. Additionally, although only a few instances of publication bias were identified, small sample sizes in many studies often reduced the imprecision of the estimates. Larger, higher-quality studies are therefore required to confirm many of the findings reported in this overview.
Limitations with the overall quality of the available SRs were another major concern. The majority of SRs were rated as low or critically low quality according to AMSTAR 2. Some of this reflected avoidable deficiencies in reporting. However, there were also numerous methodological deficiencies. Notably, many results were potentially conflated by pooling Tai Chi interventions of different intensity, frequency, and duration; comparison groups, regardless of whether they were likely to be an active or inactive control; and populations who may vary in their baseline severity, risk, prognosis, or clinical responsiveness. The impact of these decisions was often not appropriately investigated with subgroup or sensitivity analyses, or meta-regression. This may have exacerbated statistical heterogeneity and/or led to an over or underestimation of the effect sizes of Tai Chi. It also limited the ability to assess dose effects and determine how often and for how long Tai Chi needs to be practiced.
Issues with comprehensiveness and missing RCTs were another concern. Notably, during the final selection process, it became apparent that meeting the requirements for a comprehensive literature search strategy (item 4) and the overall AMSTAR 2 rating was no guarantee that all eligible primary studies were identified. For example, neither the high-quality Cochrane review of exercise interventions for falls [109, 110] nor its moderate quality 2020 update [111] was selected as they missed more of the eligible Tai Chi studies, partly due to not searching Chinese language databases. However, even when both English and Chinese language databases were searched, issues with missed studies were also identified in SRs for cancer, Parkinson’s disease, cardio/cerebrovascular diseases, and diabetes. It is highly recommended that reviewers pay greater attention to searching the reference lists not only of the included studies but also published SRs, consulting content experts in the field, and including experienced research librarians if possible to help optimize search strategies [112]. Further, considering Tai Chi originated in China and over half of the primary clinical studies have been published in Chinese [6, 7], it is difficult to justify not searching the major Chinese databases [112].
Strengths and limitations of this overview
Strengths of this overview include the comprehensive literature search, transparent study selection, prioritizing the outcomes, low overlap of primary studies, and independent rating of the GRADE certainty of the evidence for each estimate of effect. In addition, we developed a pragmatic GRADE certainty rubric to facilitate a transparent and consistent rating process. However, by not evaluating the primary studies, variations among the interventions, and setting thresholds for some decisions, important nuances may have been overlooked that could have justified upgrading or downgrading the evidence [113]. For instance, the post hoc sensitivity analyses applied more rigorous criteria that led to the evidence certainty for 31 of the 120 estimates being downgraded one level. Yet this approach was still blunt, as it did not allow for instances when there are borderline concerns across a few domains that when combined may justify rating down one level rather than two. Indeed, there were numerous instances when the same evidence was given a different GRADE certainty rating by other reviewers [13, 19, 23, 27]. Therefore, whilst the findings provide a general overview of Tai Chi effectiveness and the evidence gaps, an appraisal of the primary studies, involvement of stakeholders, and consideration of context and expert consensus may still be required before making any critical decisions for Tai Chi clinical guidelines or policies [113].
Substantially more SRs were identified than equivalent reviews [23, 26, 27]. This was despite restricting our search to publications from 2010. There were no language limitations, and the major English and Chinese databases were searched. Nevertheless, some SRs are likely to have been missed, including SRs only indexed in databases of another language such as Korean, Japanese, or Thai.
Due to the large number of SRs, most of which were screened using a partially blinded process to help reduce the risk of selective reporting bias, it is possible that some populations and outcomes were also missed. However, we are confident that we have reported the important outcomes also highlighted in other SRs of SRs [8–27].
Efforts were made to minimize overlapping among the selected SRs, yet there were still a few instances of overlap (e.g. quality of life, mobility, mental health, and sleep) in which one or two RCTs were included in more than one of the reported estimates of effect. This may have biased results for the same outcome, either positively or negatively. However, unlike similar overviews of Tai Chi [23, 27], these limitations were offset in this overview by not reporting every estimate of effect for every SR and reporting the certainty of the evidence in the main summary of findings table irrespective of the effect size or statistical significance.
Finally, there was the potential for bias to be introduced during the selection and assessment processes, as three of the reviewers (GYY, JL, and PMW) were Tai Chi investigators (see “Competing interests” section). However, only GYY was directly involved in the screening, selection, and appraisal processes and was yet to publish a SR before the completion of this overview. Of the 210 included SRs, four were authored by reviewers of this overview [94, 114–116] and only one was selected in the final synthesis [94]. The SR was included despite being published in 2014 and rated as critically low quality because it was the only SR to meta-analyses cognitive performance outcomes for the healthy older adult population group.
Conclusions
This overview comprehensively identified and critically appraised the most recent, best available SR evidence. Tai Chi was found to be generally safe and can be practiced at various levels of intensity by healthy adults, frail older adults, and people with chronic diseases. There was some evidence of beneficial physical, psychological, and quality of life outcomes from Tai Chi for a wide range of conditions. Given its multisystem effects, Tai Chi might be a suitable choice for those seeking a single intervention to help with numerous problems and symptoms.
However, the certainty in the evidence was often limited by the quality of the primary studies and their systematic reviews, clinical, methodological and statistical heterogeneity, and small sample sizes. Further research, including implementation and cost-effective research is warranted to support patient decisions, clinical practice, and policies.
Supplementary Information
Additional file 1. PRISMA 2020 checklist.
Additional file 2. Database search results.
Additional file 3. Full-text articles excluded from updated 2020 search with reason for exclusion.
Additional file 4. Systematic review (SRs) with a meta-analysis of Tai Chi randomized controlled trials not selected for the evidence synthesis.
Additional file 5. AMSTAR 2 quality rating of systematic reviews.
Additional file 6. GRADE appraisal of the certainty of the evidence.
Acknowledgements
The authors thank the following co-investigators/authors of the 2010-2020 bibliometric analysis: Zahra Ayati, Alan Bensoussan, Dennis Chang, Yan-Jun Cheng, Ning Dai, Carolyn Ee, Ming-Xian Jia, Hosen Kiat, Angelo Sabag, Min Wen, Chen-Hao Zhang, Li-Ning Zhang, Xiao-Wen Zhang, and Xian Zhou.
Abbreviations
- RCTs
Randomized controlled trial
- NRSIs
Non-randomized studies of interventions
- SRs
Systematic reviews
- PROSPERO
International Prospective Register for Systematic Reviews
- COMET
Core Outcome Measures in Effectiveness Trials
- CNKI
China National Knowledge Infrastructure
- VIP
Chinese Scientific Journal Database
- REDCap
Research Electronic Data Capture
- AMSTAR
A MeaSurement Tool to Assess systematic Reviews
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- GRADE
Grading of Recommendations, Assessment, Development and Evaluation
- PCO
Population, condition and outcome
- RR
Risk ratio
- RD
Risk difference
- NNT
Number needed to treat
- CI
Confidence interval
- MD
Mean difference
- SMD
Standardized mean difference
- MCID
Minimal clinically important difference
- NI
No information
- AE
Adverse effects
- 6MWD
6-Min walk distance/test
- BMD
Bone mineral density
- BMI
Body mass index
- BP
Blood pressure
- MS
Multiple sclerosis
- COPD
Chronic obstructive pulmonary disease
- HDL-C
High-density lipoprotein cholesterol
- LDL-C
Low-density lipoprotein cholesterol
- LVEF
Cardiac left ventricular ejection fraction
- MMSE
Mini-mental state examination
- PANSS
Positive and negative syndrome scale
- QoL
Quality of life
- ADL
Routine activities of daily living/ routine lifestyle
- Ex
Exercise (any type, including stretching)
- HEd
Health education or other educational interventions
- noRx
No treatment, control
- Pharm
Pharmaceutical drugs / medication
- Psych
Psychological interventions, counselling, support
- PT
Physical therapy/physiotherapy
- Rehab
Rehabilitation programs
- TC
Tai Chi intervention
- TCM
Traditional Chinese herbal medicine
- Ucare
Usual care, conventional treatment, standard medical care
- TC
Tai Chi
- PROMs
Patient-reported outcome measures
- TUG
Timed Up-and-Go
- MMSE
Mini-mental state examination
Authors’ contributions
GYY and JH contributed to conceptualization, methodology, investigation, formal analysis, project administration, validation, visualization, writing—original draft preparation and writing—review and editing. FLB, WLH, and HZ contributed to investigation, validation, and writing—review and editing. PW and JPL contributed to writing—review and editing. All authors read and approved the final manuscript.
Funding
This study was not supported by specific funding. PW was supported by National Institutes of Health grant K24AT009282. The funding sources had no role in the study design data collection, analysis, interpretation, or report writing.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and its additional files.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
GYY is an academic researcher at NICM Health Research Institute. As a medical research institute, NICM Health Research Institute receives research grants and donations from foundations, universities, government agencies, individuals, and industry. Sponsors and donors provide untied funding for work to advance the vision and mission of the Institute. This review was not undertaken as part of a contractual relationship with any donor or sponsor.
GYY is an academic researcher with interest in traditional, complementary, and integrative medicine. She has spoken at research workshops, seminars, and conferences for which registration and travel has been paid by the organizers.
JH is the director and beneficial share holder of Health Research Group and an academic general practitioner with a clinical interest in integrative medicine. JH has received payment for providing expert advice about traditional, complementary, and integrative medicine, including nutraceuticals, to industry, government bodies and non-government organizations, and spoken at workshops, seminars and conferences for which registration, travel and/or accommodation has been paid for by the organizers.
FLB, WLH, and HZ have no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
PW is the founder and sole owner of the Tree of Life Tai Chi Center. PW’s interests were reviewed and managed by the Brigham and Women’s Hospital and Partner’s HealthCare in accordance with their policies of conflict of interest. PW was supported by National Institutes of Health grant K24AT009282.
JPL is an academic researcher with interest in traditional, complementary, and integrative medicine. He has spoken at research workshops, seminars, and conferences for which registration and travel has been paid by the organizers.
Reviewers JH, WLH, FLB, and HZ were not Tai Chi investigators and were yet to publish a SR evaluating a Tai Chi intervention. JH directed the selection process of the SRs for the final synthesis and was involved in all aspects of rating both the quality of the SRs and the GRADE certainty in the evidence. Of the other four reviewers (GYY, WLH, FLB, and HZ) who were involved in screening, selecting, extracting data, and appraising the SRs and evidence certainty, only GYY was a Tai Chi investigator. GYY had conducted and published RCTs evaluating Tai Chi interventions but was yet to publish a SR evaluating a Tai Chi intervention before the completion of this overview.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Guo-Yan Yang and Jennifer Hunter equally contributed to this work.
Contributor Information
Guo-Yan Yang, Email: e.yang@westernsydney.edu.au.
Jennifer Hunter, Email: drjenniferhunter@healthresearchgroup.com.au.
Fan-Long Bu, Email: bufanlong@bucm.edu.cn.
Wen-Li Hao, Email: haowenli-1981@163.com.
Han Zhang, Email: zhpowder@126.com.
Peter M. Wayne, Email: pwayne@bwh.harvard.edu
Jian-Ping Liu, Email: Liujp@bucm.edu.cn.
References
- 1.Tang H, Gu L. Study on Tai Chi. Beijing: People’s Sport Publishing House of China; 2012. The history and development of Tai Chi. [Google Scholar]
- 2.Wayne PM, Manor B, Novak V, Costa MD, Hausdorff JM, Goldberger AL, Ahn AC, Yeh GY, Peng CK, Lough M, et al. A systems biology approach to studying Tai Chi, physiological complexity and healthy aging: design and rationale of a pragmatic randomized controlled trial. Contemp Clin Trials. 2013;34(1):21–34. doi: 10.1016/j.cct.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gu L, Shen J. Chen style Tai Chi. Beijing: People’s Sports Publishing House of China; 2007. [Google Scholar]
- 4.Wayne PM, Kaptchuk TJ. Challenges inherent to t’ai chi research: part II-defining the intervention and optimal study design. J Altern Complement Med. 2008;14(2):191–7. [DOI] [PubMed]
- 5.Yang JY. A practical exploration on the reform of Taijiquan elective courses in universities based on the Chinese health physical education curriculum model. J Phys Educ. 2020;06:111–117. [Google Scholar]
- 6.Yang GY, Wang LQ, Ren J, Zhang Y, Li ML, Zhu YT, Luo J, Cheng YJ, Li WY, Wayne PM, et al. Evidence base of clinical studies on Tai Chi: a bibliometric analysis. PLoS ONE. 2015;10(3):e0120655. doi: 10.1371/journal.pone.0120655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang G, Sabag A, Hao W, Zhang L, Jia M, Dai N, Zhang H, Ayati Z, Cheng Y, Zhang CH, et al. Tai Chi for health and well-being: a bibliometric analysis of published clinical studies between 2010 and 2020. Complement Ther Med. 2021;60:102748. doi: 10.1016/j.ctim.2021.102748. [DOI] [PubMed] [Google Scholar]
- 8.Lauche R, Cramer H, Häuser W, Dobos G, Langhorst J. A systematic overview of reviews for complementary and alternative therapies in the treatment of the fibromyalgia syndrome. Evid Based Complement Alternat Med. 2015;2015:610615. doi: 10.1155/2015/610615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;1(1):CD011279. doi: 10.1002/14651858.CD011279.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Husebø AML, Husebø TL. Quality of life and breast cancer: how can mind-body exercise therapies help? An overview study. Sports (Basel) 2017;5(4):79. doi: 10.3390/sports5040079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferreira RM, Duarte JA, Gonçalves RS. Non-pharmacological and non-surgical interventions to manage patients with knee osteoarthritis: an umbrella review. Acta Reumatol Port. 2018;43(3):182–200. [PubMed] [Google Scholar]
- 12.García-Rudolph A, Sánchez-Pinsach D, Salleras EO, Tormos JM. Subacute stroke physical rehabilitation evidence in activities of daily living outcomes: a systematic review of meta-analyses of randomized controlled trials. Medicine (Baltimore) 2019;98(8):e14501. doi: 10.1097/MD.0000000000014501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McLaughlin EC, El-Kotob R, Chaput JP, Janssen I, Kho ME, Poitras VJ, Ross R, Ross-White A, Saunders TJ, Sherrington C, et al. Balance and functional training and health in adults: an overview of systematic reviews. Appl Physiol Nutr Metab. 2020;45(10):S180–S196. doi: 10.1139/apnm-2020-0279. [DOI] [PubMed] [Google Scholar]
- 14.Wu SYF, Brown T, Yu ML. Older adults’ psychosocial responses to a fear of falling: a scoping review to inform occupational therapy practice. Occup Ther Ment Health. 2020;36(3):207–43.
- 15.Zhang Y, Yao F, Kuang X, Li L, Huang L, Zhou Q, Peng J, Chang Q. How can alternative exercise traditions help against the background of the COVID-19 in cancer care? An overview of systematic reviews. Cancer Manag Res. 2020;12:12927–12944. doi: 10.2147/CMAR.S282491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amatya B, Khan F, Lew TE, Dickinson M. Rehabilitation in patients with lymphoma: an overview of systematic reviews. J Rehabil Med. 2021;53(3):jrm00163. doi: 10.2340/16501977-2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kedzior KK, Kaplan I. Tai Chi and Parkinson’s disease (PD): a systematic overview of the scientific quality of the past systematic reviews. Complement Ther Med. 2019;46:144–52. [DOI] [PubMed]
- 18.Reid KF, Bannuru RR, Wang C, Mori DL, Niles BL. The effects of Tai Chi mind-body approach on the mechanisms of gulf war illness: an umbrella review. Integr Med Res. 2019;8(3):167–172. doi: 10.1016/j.imr.2019.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhong D, Xiao Q, Xiao X, Li Y, Ye J, Xia L, Zhang C, Li J, Zheng H, Jin R. Tai Chi for improving balance and reducing falls: an overview of 14 systematic reviews. Ann Phys Rehabil Med. 2020;63(6):505–517. doi: 10.1016/j.rehab.2019.1012.1008. [DOI] [PubMed] [Google Scholar]
- 20.Huang J, Liu H, Chen J, Cai X, Huang Y. The effectiveness of Tai Chi in patients with breast cancer: an overview of systematic reviews and meta-analyses. J Pain Symptom Manage. 2021;61(5):1052–1059. doi: 10.1016/j.jpainsymman.2020.10.007. [DOI] [PubMed] [Google Scholar]
- 21.Huang J, Qin X, Shen M, Xu Y, Huang Y. The effects of Tai Chi exercise among adults with chronic heart failure: an overview of systematic review and meta-analysis. Front Cardiovasc Med. 2021;8:589267. doi: 10.3389/fcvm.2021.589267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Imoto AM, Amorim FF, Palma H, Lombardi Júnior I, Salomon AL, Peccin MS, Silva H, Franco ESB, Göttems L, Santana LA. Evidence for the efficacy of Tai Chi for treating rheumatoid arthritis: an overview of systematic reviews. Sao Paulo Med J. 2021;139(2):91–97. doi: 10.1590/1516-3180.2020.0346.r1.18112020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Easwaran K, Gopalasingam Y, Green DD, Lach V, Melnyk JA, Wan C, Bartlett DJ. Effectiveness of Tai Chi for health promotion for adults with health conditions: a scoping review of Meta-analyses. Disabil Rehabil. 2021;43(21):2978–2989. doi: 10.1080/09638288.2020.1725916. [DOI] [PubMed] [Google Scholar]
- 24.Lee MS, Ernst E. Systematic reviews of t’ai chi: an overview. Br J Sports Med. 2012;46(10):713–8. [DOI] [PubMed]
- 25.Solloway MR, Taylor SL, Shekelle PG, Miake-Lye IM, Beroes JM, Shanman RM, Hempel S. An evidence map of the effect of Tai Chi on health outcomes. Syst Rev. 2016;5(1):126. doi: 10.1186/s13643-016-0300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang F-C, Desai AB, Esfahani P, Sokolovskaya TV, Bartlett DJ. Effectiveness of Tai Chi for health promotion of older adults: a scoping review of meta-analyses. Am J Lifestyle Med. 2021:15598276211001291. Epub 2020. [DOI] [PMC free article] [PubMed]
- 27.Zou L, Xiao T, Cao C, Smith L, Imm K, Grabovac I, Waldhoer T, Zhang Y, Yeung A, Demurtas J, et al. Tai Chi for chronic illness management: synthesizing current evidence from meta-analyses of randomized controlled trials. Am J Med. 2021;134(2):194–205.e12. doi: 10.1016/j.amjmed.2020.08.015. [DOI] [PubMed] [Google Scholar]
- 28.Cochrane handbook for systematic reviews of interventions. Version 6.0 [www.training.cochrane.org/handbook]
- 29.Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overview of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, editors. Cochrane handbook for systematic reviews of interventions Version 60. Welch VA: Cochrane; 2020. [Google Scholar]
- 30.JBI Manual for Evidence Synthesis [https://synthesismanual.jbi.global. 10.46658/JBIMES-20-01]
- 31.Schünemann H, Brożek J, Guyatt G, Oxman A. Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach. Updated October 2013. In.: The GRADE Working Group. 2013.
- 32.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Core outcome measures in effectiveness trials (COMET) [https://www.comet-initiative.org/]
- 34.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed]
- 36.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65–94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 37.GRADEpro Guideline Development Tool [Software] [gradepro.org]
- 38.Pollock A, Farmer SE, Brady MC, Langhorne P, Mead GE, Mehrholz J, van Wijck F, Wiffen PJ. An algorithm was developed to assign GRADE levels of evidence to comparisons within systematic reviews. J Clin Epidemiol. 2016;70:106–110. doi: 10.1016/j.jclinepi.2015.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cohen J. Statistical power analysis for the behavioral sciences. Academic press; 2013.
- 40.Alma HJ, de Jong C, Jelusic D, Wittmann M, Schuler M, Sanderman R, Schultz K, Kocks J, van der Molen T. Thresholds for clinically important deterioration versus improvement in COPD health status: results from a randomised controlled trial in pulmonary rehabilitation and an observational study during routine clinical practice. BMJ Open. 2019;9(6):e025776. doi: 10.1136/bmjopen-2018-025776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Andrews JS, Desai U, Kirson NY, Zichlin ML, Ball DE, Matthews BR. Disease severity and minimal clinically important differences in clinical outcome assessments for Alzheimer’s disease clinical trials. Alzheimers Dement (N Y). 2019;5:354–63. [DOI] [PMC free article] [PubMed]
- 42.Donoghue D, Stokes EK. How much change is true change? The minimum detectable change of the Berg Balance Scale in elderly people. J Rehabil Med. 2009;41(5):343–346. doi: 10.2340/16501977-0337. [DOI] [PubMed] [Google Scholar]
- 43.Donohue JF. Minimal clinically important differences in COPD lung function. COPD. 2005;2(1):111–124. doi: 10.1081/COPD-200053377. [DOI] [PubMed] [Google Scholar]
- 44.Ghandehari K, Ghandehari K, Saffarian-Toosi G, Masoudinezhad S, Yazdani S, Nooraddin A, Ebrahimzadeh S, Ahmadi F, Abrishamchi F. Comparative interrater reliability of Asian Stroke Disability Scale, modified Rankin Scale and Barthel Index in patients with brain infarction. ARYA Atheroscler. 2012;8(3):153–157. [PMC free article] [PubMed] [Google Scholar]
- 45.Goldberg A, Casby A, Wasielewski M. Minimum detectable change for single-leg-stance-time in older adults. Gait Posture. 2011;33(4):737–739. doi: 10.1016/j.gaitpost.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 46.Gonzalez-Saenz de Tejada M, Bilbao A, Ansola L, Quirós R, García-Perez L, Navarro G, Escobar A. Responsiveness and minimal clinically important difference of the Minnesota living with heart failure questionnaire. Health Qual Life Outcomes. 2019;17(1):36. doi: 10.1186/s12955-019-1104-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hiengkaew V, Jitaree K, Chaiyawat P. Minimal detectable changes of the Berg Balance Scale, Fugl-Meyer Assessment Scale, Timed “Up & Go” Test, gait speeds, and 2-minute walk test in individuals with chronic stroke with different degrees of ankle plantarflexor tone. Arch Phys Med Rehabil. 2012;93(7):1201–8. [DOI] [PubMed]
- 48.Horváth K, Aschermann Z, Ács P, Deli G, Janszky J, Komoly S, Balázs É, Takács K, Karádi K, Kovács N. Minimal clinically important difference on the Motor Examination part of MDS-UPDRS. Parkinsonism Relat Disord. 2015;21(12):1421–1426. doi: 10.1016/j.parkreldis.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 49.Jones PW, Quirk FH, Baveystock CM. The St George’s Respiratory Questionnaire. Respir Med. 1991;85 Suppl B:25–31. [DOI] [PubMed]
- 50.Maruish ME, Maruish M, Kosinski MJ, Bjorner JB, Gandek B, Turner-Bowker DM, Ware JE. User’s manual for the SF-36v2 survey. 3. Lincoln, Rhode Island: Quality Metric Incorporated; 2011. [Google Scholar]
- 51.Page SJ, Fulk GD, Boyne P. Clinically important differences for the upper-extremity Fugl-Meyer Scale in people with minimal to moderate impairment due to chronic stroke. Phys Ther. 2012;92(6):791–798. doi: 10.2522/ptj.20110009. [DOI] [PubMed] [Google Scholar]
- 52.Pandian S, Arya KN, Kumar D. Minimal clinically important difference of the lower-extremity fugl-meyer assessment in chronic-stroke. Top Stroke Rehabil. 2016;23(4):233–239. doi: 10.1179/1945511915Y.0000000003. [DOI] [PubMed] [Google Scholar]
- 53.Phelan D, Thavendiranathan P, Collier P, Marwick TH. Aldosterone antagonists improve ejection fraction and functional capacity independently of functional class: a meta-analysis of randomised controlled trials. Heart. 2012;98(23):1693–1700. doi: 10.1136/heartjnl-2012-302178. [DOI] [PubMed] [Google Scholar]
- 54.Phillips PJ, Phillipov G. Bone mineral density - frequently asked questions. Aust Fam Physician. 2006;35(5):341–344. [PubMed] [Google Scholar]
- 55.Polkey MI, Spruit MA, Edwards LD, Watkins ML, Pinto-Plata V, Vestbo J, Calverley PM, Tal-Singer R, Agustí A, Bakke PS, et al. Six-minute-walk test in chronic obstructive pulmonary disease: minimal clinically important difference for death or hospitalization. Am J Respir Crit Care Med. 2013;187(4):382–386. doi: 10.1164/rccm.201209-1596OC. [DOI] [PubMed] [Google Scholar]
- 56.Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Täger T, Hanholz W, Cebola R, Fröhlich H, Franke J, Doesch A, Katus HA, Wians FH, Jr, Frankenstein L. Minimal important difference for 6-minute walk test distances among patients with chronic heart failure. Int J Cardiol. 2014;176(1):94–98. doi: 10.1016/j.ijcard.2014.06.035. [DOI] [PubMed] [Google Scholar]
- 58.Ward MM, Guthrie LC, Alba MI. Clinically important changes in individual and composite measures of rheumatoid arthritis activity: thresholds applicable in clinical trials. Ann Rheum Dis. 2015;74(9):1691–1696. doi: 10.1136/annrheumdis-2013-205079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wise RA, Brown CD. Minimal clinically important differences in the six-minute walk test and the incremental shuttle walking test. COPD. 2005;2(1):125–129. doi: 10.1081/COPD-200050527. [DOI] [PubMed] [Google Scholar]
- 60.Buto MSD, de Oliveira MPB, Carvalho C, Vassimon-Barroso V, Takahashi ACD. Effect of complementary therapies on functional capacity and quality of life among prefrail and frail older adults: a systematic review of randomized controlled trials. Arch Gerontol Geriatr. 2020;91:104236. doi: 10.1016/j.archger.2020.104236. [DOI] [PubMed] [Google Scholar]
- 61.Cheng CA, Chiu YW, Wu DA, Kuan YC, Chen SN, Tam KW. Effectiveness of Tai Chi on fibromyalgia patients: a meta-analysis of randomized controlled trials. Complement Ther Med. 2019;46:1–8. doi: 10.1016/j.ctim.2019.07.007. [DOI] [PubMed] [Google Scholar]
- 62.Choo YT, Jiang Y, Hong J, Wang W. Effectiveness of Tai Chi on quality of life, depressive symptoms and physical function among community-dwelling older adults with chronic disease: a systematic review and meta-analysis. Int J Nurs Stud. 2020;111:103737. doi: 10.1016/j.ijnurstu.2020.103737. [DOI] [PubMed] [Google Scholar]
- 63.Cocchiara RA, Dorelli B, Gholamalishahi S, Longo W, Musumeci E, Mannocci A, La Torre G. Tai Chi and workplace wellness for health care workers: a systematic review. Int J Environ Res Public Health. 2020;17(1):343. doi: 10.3390/ijerph17010343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cui H, Wang QY, Pedersen M, Wang Q, Lv SJ, James D, Larkey L. The safety of tai chi: a meta-analysis of adverse events in randomized controlled trials. Contemp Clin Trials. 2019;82:85–92. doi: 10.1016/j.cct.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 65.Dong XS, Ding M, Yi XR. Meta-analysis of randomized controlled trials of the effects of Tai Chi on blood pressure. Evid Based Complement Alternat Med. 2020;2020:8503047. doi: 10.1155/2020/8503047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gu Q, Wu SJ, Zheng Y, Zhang Y, Liu C, Hou JC, Zhang K, Fang XM. Tai Chi exercise for patients with chronic heart failure: a meta-analysis of randomized controlled trials. Am J Phys Med Rehabil. 2017;96(10):706–716. doi: 10.1097/PHM.0000000000000723. [DOI] [PubMed] [Google Scholar]
- 67.Guo CY, Xiang GL, Xie L, Liu ZL, Zhang XM, Wu QH, Li SQ, Wu Y. Effects of Tai Chi training on the physical and mental health status in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Thorac Dis. 2020;12(3):504–521. doi: 10.21037/jtd.2020.01.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hall A, Copsey B, Richmond H, Thompson J, Ferreira M, Latimer J, Maher CG. Effectiveness of Tai Chi for chronic musculoskeletal pain conditions: updated systematic review and meta-analysis. Phys Ther. 2017;97(2):227–238. doi: 10.2522/ptj.20160246. [DOI] [PubMed] [Google Scholar]
- 69.Ho RTH, Wang CW, Ng SM, Ho AHY, Ziea ETC, Wong VT, Chan CLW. The effect of t’ai chi exercise on immunity and infections: a systematic review of controlled trials. J Altern Complement Med. 2013;19(5):389–96. [DOI] [PubMed]
- 70.Hu L, Wang Y, Liu X, Ji X, Ma Y, Man S, Hu Z, Cheng J, Huang F. Tai Chi exercise can ameliorate physical and mental health of patients with knee osteoarthritis: systematic review and meta-analysis. Clin Rehabil. 2021;35(1):64–79. doi: 10.1177/0269215520954343. [DOI] [PubMed] [Google Scholar]
- 71.Huang Y, Jin R, Zhong D, Li J, Li Y, Shi L. The influence of Tai Chi on the fall and balance function of middle-aged and the elderly: a meta-analysis [Chinese] Chin J Evid Based Med. 2020;20(3):281–288. [Google Scholar]
- 72.Huang HW, Nicholson N, Thomas S. Impact of Tai Chi exercise on balance disorders: a systematic review. Am J Audiol. 2019;28(2):391–404. doi: 10.1044/2018_AJA-18-0115. [DOI] [PubMed] [Google Scholar]
- 73.Huang ZG, Feng YH, Li YH, Lv CS. Systematic review and meta-analysis: Tai Chi for preventing falls in older adults. BMJ Open. 2017;7(2):e013661. doi: 10.1136/bmjopen-2016-013661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jiang H. Effects of Tai Chi on cardiopulmonary function and quality of life in patients with stable angina pectoris [Chinese] 2018. [Google Scholar]
- 75.Kruisbrink M, Delbaere K, Kempen GIJM, Crutzen R, Ambergen T, Cheung K-L, Kendrick D, Iliffe S, Zijlstra GAR. Intervention characteristics associated with a reduction in fear of falling among community-dwelling older people: a systematic review and meta-analysis of randomized controlled trials. Gerontologist. 2021;61(6):e269–e282. doi: 10.1093/geront/gnaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liu F, Cui JB, Liu X, Chen KW, Chen XR, Li R. The effect of tai chi and Qigong exercise on depression and anxiety of individuals with substance use disorders: a systematic review and meta-analysis. BMC Complement Med Ther. 2020;20(1):161. doi: 10.1186/s12906-020-02967-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liu LZ, Tan HJ, Yu SG, Yin HY, Baxter GD. The effectiveness of tai chi in breast cancer patients: a systematic review and meta-analysis. Complement Ther Clin Pract. 2020;38:101078. doi: 10.1016/j.ctcp.2019.101078. [DOI] [PubMed] [Google Scholar]
- 78.Liu W, Hao J. Tai Chi exercise for pain, stiffness and function in patients with osteoarthritis: a systematic review and meta-analysis [Chinese] Chin J Gerontol. 2020;40(16):3471–3475. [Google Scholar]
- 79.Luo XC, Liu J, Fu J, Yin HY, Shen L, Liu ML, Lan L, Ying J, Qiao XL, Tang CZ, et al. Effect of Tai Chi Chuan in breast cancer patients: a systematic review and meta-analysis. Front Oncol. 2020;10:607. doi: 10.3389/fonc.2020.00607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lyu D, Wang J, Yang F, Zhang Y, Zhang W, Liu H, Lyu X, Fang B. Effect of Tai Chi on post-stroke non-motor disorders: a systematic review and meta-analysis of randomized controlled trials. Clin Rehabil. 2021;35(1):26–38. doi: 10.1177/0269215520951020. [DOI] [PubMed] [Google Scholar]
- 81.Lyu DY, Lyu XX, Zhang Y, Ren Y, Yang F, Zhou L, Zou YH, Li ZH. Tai Chi for stroke rehabilitation: a systematic review and meta-analysis of randomized controlled trials. Front Physiol. 2018;9:983. doi: 10.3389/fphys.2018.00983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mudano AS, Tugwell P, Wells GA, Singh JA. Tai Chi for rheumatoid arthritis. Cochrane Database Syst Rev. 2019;9(9):CD004849. doi: 10.1002/14651858.CD004849.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ni XS, Chan RJ, Yates P, Hu WY, Huang XH, Lou Y. The effects of Tai Chi on quality of life of cancer survivors: a systematic review and meta-analysis. Support Care Cancer. 2019;27(10):3701–3716. doi: 10.1007/s00520-019-04911-0. [DOI] [PubMed] [Google Scholar]
- 84.Pan XH, Mahemuti A, Zhang XH, Wang YP, Hu P, Jiang JB, Xiang MX, Liu G, Wang JA. Effect of Tai Chi exercise on blood lipid profiles: a meta-analysis of randomized controlled trials. J Zhejiang Univ Sci B. 2016;17(8):640–648. doi: 10.1631/jzus.B1600052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Qin J, Zhang Y, Wu L, He Z, Huang J, Tao J, Chen L, Enix D. Effect of Tai Chi alone or as additional therapy on low back pain: systematic review and meta-analysis of randomized controlled trials. Medicine (United States) 2019;98(37):e17099. doi: 10.1097/MD.0000000000017099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Si YH, Wang CY, Yin H, Zheng JH, Guo Y, Xu GH, Ma Y. Tai Chi Chuan for subjective sleep quality: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. 2020;2020:4710527. doi: 10.1155/2020/4710527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Song SJ, Yu JH, Ruan Y, Liu X, Xiu LJ, Yue XQ. Ameliorative effects of Tai Chi on cancer-related fatigue: a meta-analysis of randomized controlled trials. Support Care Cancer. 2018;26(7):2091–2102. doi: 10.1007/s00520-018-4136-y. [DOI] [PubMed] [Google Scholar]
- 88.Su Z, Jiang J. Tai Chi for improving knee muscle strength: a meta-analysis [Chinese] Chinese J Rehab Med. 2020;35(4):475–481. [Google Scholar]
- 89.Taylor E, Taylor-Piliae RE. The effects of Tai Chi on physical and psychosocial function among persons with multiple sclerosis: a systematic review. Complement Ther Med. 2017;31:100–108. doi: 10.1016/j.ctim.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 90.Taylor-Piliae RE, Finley BA. Tai Chi exercise for psychological well-being among adults with cardiovascular disease: a systematic review and meta-analysis. Eur J Cardiovasc Nurs. 2020;19(7):580–591. doi: 10.1177/1474515120926068. [DOI] [PubMed] [Google Scholar]
- 91.Wang D, Wang PC, Lan K, Zhang YC, Pan YL. Effectiveness of Tai chi exercise on overall quality of life and its physical and psychological components among older adults: a systematic review and meta-analysis. Braz J Med Biol Res. 2020;53(10):e10196. doi: 10.1590/1414-431x202010196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang Y, Shan WC, Li Q, Yang N, Shan WY. Tai Chi exercise for the quality of life in a perimenopausal women organization: a systematic review. Worldviews Evid Based Nurs. 2017;14(4):294–305. doi: 10.1111/wvn.12234. [DOI] [PubMed] [Google Scholar]
- 93.Wang C, Bannuru R, Ramel J, Kupelnick B, Scott T, Schmid CH. Tai Chi on psychological well-being: systematic review and meta-analysis. BMC Complement Altern Med. 2010;10:23. doi: 10.1186/1472-6882-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wayne PM, Walsh JN, Taylor-Piliae RE, Wells RE, Papp KV, Donovan NJ, Yeh GY. Effect of tai chi on cognitive performance in older adults: systematic review and meta-analysis. J Am Geriatr Soc. 2014;62(1):25–39. doi: 10.1111/jgs.12611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Webster CS, Luo AY, Krageloh C, Moir F, Henning M. A systematic review of the health benefits of Tai Chi for students in higher education. Preventive medicine reports. 2016;3:103–112. doi: 10.1016/j.pmedr.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wu B, Ding Y, Zhong B, Jin X, Cao Y, Xu D. Intervention treatment for myocardial infarction with Tai Chi: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2020;101(12):2206–2218. doi: 10.1016/j.apmr.2020.02.012. [DOI] [PubMed] [Google Scholar]
- 97.Xiang Y, Lu LM, Chen XK, Wen ZH. Does Tai Chi relieve fatigue? A systematic review and meta-analysis of randomized controlled trials. Plos One. 2017;12(4):e0174872. doi: 10.1371/journal.pone.0174872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yin JC, Dishman RK. The effect of Tai Chi and Qigong practice on depression and anxiety symptoms: a systematic review and meta-regression analysis of randomized controlled trials. Ment Health Phys Act. 2014;7(3):135–146. doi: 10.1016/j.mhpa.2014.08.001. [DOI] [Google Scholar]
- 99.Yu Q, Li LG, Li EY. A meta-analysis of Tai Chi training for depressive mood in university students. J Int Psychiatry. 2019;46(3):409–412. [Google Scholar]
- 100.Yu F, Zhong Q, Tong Q, Tao Z. Impact of Tai Chi on mild to moderate Parkinson’s disease: a meta-analysis [Chinese]. Chin J Rehab Med. 2018;33(8):959–65.
- 101.Zhang YL, Chai Y, Pan XJ, Shen H, Wei X, Xie YM. Tai chi for treating osteopenia and primary osteoporosis: a meta-analysis and trial sequential analysis. Clin Interv Aging. 2019;14:91–104. doi: 10.2147/CIA.S187588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhang Q, Song H, Cao R, Sun X, Jin Y. Effects of Tai Chi on cognitive function for aged with mild cognitive impairment: a Meta-analysis [Chinese] Chin Nurs Manag. 2020;20(6):865–871. [Google Scholar]
- 103.Zheng GH, Huang MM, Liu FW, Li SZ, Tao J, Chen LD. Tai Chi Chuan for the primary prevention of stroke in middle-aged and elderly adults: a systematic review. Evid Based Complement Alternat Med. 2015;2015:742152. doi: 10.1155/2015/742152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zheng W, Li Q, Lin J, Xiang Y, Guo T, Chen Q, Cai D, Xiang Y. Tai Chi for schizophrenia: a systematic review. Shanghai Arch Psychiatry. 2016;28(4):185–194. doi: 10.11919/j.issn.1002-0829.216051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhong D, Li J, Yang H, Li Y, Huang Y, Xiao Q, Liu T, Jin R. Tai Chi for essential hypertension: a systematic review of randomized controlled trials. Curr Hypertens Rep. 2020;22(3):25. doi: 10.1007/s11906-020-1031-y. [DOI] [PubMed] [Google Scholar]
- 106.Zhou Z, Zhou R, Li K, Zhu Y, Zhang Z, Luo Y, Luan R. Effects of tai chi on physiology, balance and quality of life in patients with type 2 diabetes: a systematic review and meta-analysis. J Rehabil Med. 2019;51(6):405–417. doi: 10.2340/16501977-2555. [DOI] [PubMed] [Google Scholar]
- 107.de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55(2):129–133. doi: 10.1016/S0004-9514(09)70043-1. [DOI] [PubMed] [Google Scholar]
- 108.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sherrington C, Fairhall N, Wallbank G, Tiedemann A, Michaleff ZA, Howard K, Clemson L, Hopewell S, Lamb S. Exercise for preventing falls in older people living in the community: an abridged Cochrane systematic review. Br J Sports Med. 2020;54(15):885–891. doi: 10.1136/bjsports-2019-101512. [DOI] [PubMed] [Google Scholar]
- 110.Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, Clemson L, Hopewell S, Lamb SE. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1(1):CD012424. doi: 10.1002/14651858.CD012424.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sherrington C, Fairhall N, Kwok W, Wallbank G, Tiedemann A, Michaleff ZA, Ng C, Bauman A. Evidence on physical activity and falls prevention for people aged 65+ years: systematic review to inform the WHO guidelines on physical activity and sedentary behaviour. Int J Behav Nutr Phys Act. 2020;17(1):144. doi: 10.1186/s12966-020-01041-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hunter J, Arentz S, Goldenberg J, Yang G, Beardsley J, Lee MS, Myers SP. Choose your shortcuts wisely: COVID-19 rapid reviews of traditional, complementary and integrative medicine. Integr Med Res. 2020;9(3):100484. doi: 10.1016/j.imr.2020.100484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Liu JP. GRADE Methods in traditional medicine. Integr Med Res. 2022;11(2):100836. doi: 10.1016/j.imr.2022.100836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wayne PM, Berkowitz DL, Litrownik DE, Buring JE, Yeh GY. What do we really know about the safety of tai chi?: A systematic review of adverse event reports in randomized trials. Arch Phys Med Rehabil. 2014;95(12):2470–2483. doi: 10.1016/j.apmr.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wayne PM, Krebs DE, Wolf SL, Gill-Body KM, Scarborough DM, McGibbon CA, Kaptchuk TJ, Parker SW. Can Tai Chi improve vestibulopathic postural control? Arch Phys Med Rehabil. 2014;85(1):142–152. doi: 10.1016/S0003-9993(03)00652-X. [DOI] [PubMed] [Google Scholar]
- 116.Wayne PM, Lee MS, Novakowski J, Osypiuk K, Ligibel J, Carlson LE, Song R. Tai Chi and Qigong for cancer-related symptoms and quality of life: a systematic review and meta-analysis. J Cancer Surviv. 2018;12(2):256–267. doi: 10.1007/s11764-017-0665-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. PRISMA 2020 checklist.
Additional file 2. Database search results.
Additional file 3. Full-text articles excluded from updated 2020 search with reason for exclusion.
Additional file 4. Systematic review (SRs) with a meta-analysis of Tai Chi randomized controlled trials not selected for the evidence synthesis.
Additional file 5. AMSTAR 2 quality rating of systematic reviews.
Additional file 6. GRADE appraisal of the certainty of the evidence.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article and its additional files.