Supplemental digital content is available in the text.
Key Words: Simulation-based learning, allied health, professional placements
Summary Statement
Emerging literature continues to demonstrate the use of innovative practices such as simulated-based learning experiences to prepare students for professional placements. This scoping review aimed to provide a broad overview of how simulated-based learning experiences have been implemented within or immediately before the professional practice placements of entry-level allied health programs. Four databases (MEDLINE, EMCARE, CINAHL, and Scopus) were searched up to August 2020. Kirkpatrick's evaluation framework was used to categorize outcomes, and the Simulation-Based Research Extension for the CONSORT statement was used to appraise the quality of simulation reporting. The search revealed 6584 unique abstracts with 321 full-text articles reviewed. Forty-eight studies met the inclusion criteria. This review has shown a clear trend toward using simulation within or immediately before the professional practice placements of allied health programs. Using Kirkpatrick's evaluation framework, most studies reported on student reaction (level 1) and learning (level 2) obtained during the simulation experience. There was limited evidence showing how the benefits gained in simulation translated to the clinical environment (level 3) or impacted the organization (level 4). Further research is required to review the optimal proximity of simulation to allied health professional placements and how gains are obtained from simulation transition to the clinical environment. In addition, more consistent reporting of simulation methodologies and evaluation methods are needed to strengthen the evidence base.
Professional placements are an essential component of university-based allied health programs designed to prepare students for clinical practice.1 Mandated by professional accreditation bodies, placements provide opportunities to develop competent health professionals.1,2 However, clinical environments can be challenging for students as they navigate the complexities of real-world settings and transition from classroom theory to practice.3,4 Health professions such as physiotherapy, occupational therapy, medicine, and nursing have endeavored to overcome these challenges by incorporating simulated-based learning experiences (SBLEs) into the entry-level curriculum.5–10 The versatility of SBLEs allows them to meet the educational needs of a range of allied health professions. Encompassing various technologies and modalities,11 SBLEs have been commonly reported to increase confidence,12–15 improve communication skills,16–18 develop reasoning and critical thinking,19–21 and facilitate readiness for professional placement.12,21–23 To guide student learning and outcomes, learning theories can provide a framework for designing and implementing SBLEs.24,25 Common theories identified within SBLE literature include behaviorism, social learning theory, and constructivism.25–27 However, this area is often poorly reported in the literature, and there is no consensus on which model best fits.24,25
The use of SBLEs as an educational tool in preparation or substitution for clinical hours in the medicine and nursing professions has been well reviewed.5,28–31 Within allied health professional placements, simulation has been used as a partial substitute for traditional placements within the physiotherapy and occupational therapy professions.8–10,32 Audiology and speech pathology disciplines have used SBLEs to compliment placement with activities focusing on developing communication and counseling skills.14,33–35 Pharmacy programs have used simulation to examine the development of communication skills and technical skills such as taking blood pressure and reducing errors in medication dispensing.18,36
To ensure the provision of quality education, educational initiatives should be evaluated.37 Kirkpatrick's evaluation framework38 is a 4-level model to determine the efficacy of a particular educational intervention. Level 1 (reaction) evaluates participant perceptions or satisfaction with the training program. Level 2 (learning) examines changes in attitudes, knowledge, or skills during the training program. Level 3 (behavior) relates to the learning application and how behavior has changed because of the training program. Level 4 (results) examines the impact of the training program on the organization.38 Previous research using this framework39–42 has demonstrated the strength of SBLEs on immediate student outcomes, for example, satisfaction (level 1) and development of skills and knowledge (level 2). However, within the existing allied health literature, there is limited research beyond the immediate outcomes (levels 1 and 2) to demonstrate transferability or value of SBLEs within the clinical setting (levels 3 and 4).
No known reviews have examined and mapped the current use of SBLEs in university-based, entry-level allied health programs' professional placements. The purposes of this scoping review were to examine the use of SBLEs within or immediately before the professional practice placements of entry-level allied health programs and to explore the range of reported outcomes.
METHODS
Arksey and O'Malley's methodological framework guided this scoping review.43 The 5 stages guiding the review included identifying the research question; identifying relevant studies; selecting studies; charting the data; and collating, summarizing, and reporting the results. A scoping review was chosen for this study to allow a broader investigation of the literature and to map the body of knowledge that existed succinctly.43 This review is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews.44 A protocol was registered with Open Science Framework and is available at https://osf.io/zpc4u/.45
The review questions were designed to examine the breadth of the literature. This scoping review aimed to examine the following:
How do entry-level allied health programs incorporate SBLEs within or immediately before their professional placements?
Using Kirkpatrick's evaluation framework,38 what levels of outcomes are used to evaluate SBLEs within or immediately before entry-level allied health professional placements?
What are the reported barriers and enablers to implementing SBLEs within or immediately before entry-level allied health programs?
Participants
The authors (K.S., L.M.W., C.J.) were considered experienced with simulation activities and determined the scope and definition of activities of the included studies. Studies were required to include undergraduate or postgraduate students enrolled in a university-based allied health program participating in SBLEs within or immediately before their professional placement. There is no standard definition within the literature of allied health or allied health professions. For this review, allied health professionals were considered tertiary qualified health professionals eligible for membership of their professional association or national board who provide therapeutic or diagnostic services to restore and maintain optimal function.46 This included arts therapy, audiology, child life therapy (formerly play therapy), counseling, dietetics and nutrition, diversional therapy, exercise physiology, genetic counseling, music therapy, nuclear medicine, occupational therapy, orthoptics, orthotics and prosthetics, pharmacy, physiotherapy, podiatry, psychology, radiation therapy, radiography, sexual assault, social work, speech pathology, and welfare.47 Studies incorporating interprofessional student groups were included and provided data specific to allied health students, which could be extracted.
Intervention
Simulated-based learning experiences are structured activities that replicate actual or potential clinical situations for educational purposes.11 As this review focused on SBLEs being incorporated into placement, studies were included if they used SBLEs immediately before or within the professional placement or were used as part of or as a substitution for placement weeks. In addition, all simulation modalities were included, as were studies that evaluated and reported at least 1 measurable outcome.
Learning outcomes of the simulation programs were reviewed against Kirkpatrick's evaluation framework.38 Although the model cannot be used to determine the quality of individual studies, it provides a framework for examining the types of learning outcomes described in the literature.26,41,42
No set criteria were identified for the comparison of interventions to allow for the broadest possible search return. Studies were excluded if students completed simulation activities as part of their university studies not immediately before or within the professional placement or if articles reported on simulation pedagogy or design without measuring outcomes.
Search Strategy
A comprehensive literature search of 4 online databases was conducted (MEDLINE, EMCARE, CINAHL, Scopus) for articles published in peer review literature, including any date up to August 18, 2020. The search strategy and results are presented in Table 1 and Figure 1 (see Table, Supplementary Digital Content 1, http://links.lww.com/SIH/A766, for the complete search strategies for each database).
TABLE 1.
Search Strategy
| Main Concepts | |||
|---|---|---|---|
| Simulation | Placement | Allied Health | |
| Search terms | Computer Simulation/ or High-Fidelity Simulation Training/ or Patient Simulation Simulation Training/ simulat* adj3 learning* Manikins/ Virtual Reality/ Video Games/ simulation* or “human simulation*” or “simulated patient*” or “standardi?ed patient*” or manikin* or mannikin* or mannequin* or “augmented realit*” or gam* or “virtual realit*” or “task trainer*” or “computer adj3 simulat*” |
Preceptorship/ “Internship and Residency”/ Professional Practice/ Clinical Clerkship/ Problem-Based Learning/ “practice education” or fieldwork or “field work” or “clinical placement*” or “clinical education” or “clinical practice” or “clinical training” or “student placement*” or “student supervision” or “work based learning” or “work integrated learning” or WIL or practicum* or preceptorship* or “clinical clerkship*” or “experiential learning” or “placement environment*” or “clinical learning environment*” or internship* or placement* |
Schools, Health Occupations/ or Allied Health Personnel/ or Health Personnel Allied Health Occupations/ or Health Occupations Art Therapy/ Dance Therapy/ Music Therapy/ Audiology/ Play Therapy/ Counseling/ Genetic Counseling/ Dietetics/ Nuclear Medicine/ Occupational Therapy/ Orthoptics/ Schools, Pharmacy/ or Education, Pharmacy/ or Pharmacy/ of Students, Pharmacy/ or Pharmacy Residencies/ Podiatry/ Psychology/ Radiography/ Social Work/ Speech-Language Pathology/ Radiotherapy/ Physical Therapists/ orthoptic* or orthotic* or prosthetic* or “child life therap*” or “diversional therap*” or “exercise physiolog*” or physiotherap* or “occupational therap*” or dietetic* or “speech adj2 patholog*” or “speech adj2 therap*” or psycholog* or podiatr* or “physical therap*” or “social work*” or “radiation therap*” or “sexual assault” or welfare or “art therap*” or “dance therap*” or “music therap*” or audiolog* or “play therap*” or counsel* or pharmac* or radiograph* or “allied health” |
FIGURE 1.
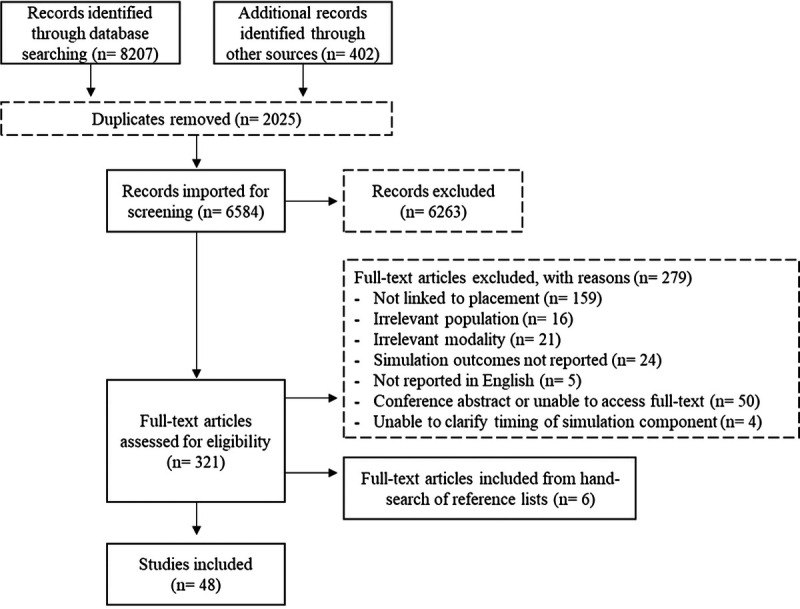
Search results with study selection and inclusion process.
To ensure all sources were explored, Google Scholar was searched using the same search terms and included any date up to December 1, 2020. Three simulation-specific journals (Simulation in Healthcare, Advances in Simulation, BMJ Simulation and Technology Enhanced Learning) were also searched for associated articles through the on-site search engine on December 7, 2020. References of the included articles were hand searched for any relevant literature not already identified.
Article Selection
Titles and abstracts were each screened by 2 reviewers for eligibility. Full-text articles requiring further review were obtained. If insufficient or unclear data were documented in the article, the authors were contacted via e-mail to clarify details or obtain data. Articles were excluded if insufficient data were available to complete the data extraction table. All full-text articles retrieved were read in full and independently appraised by 2 reviewers and assessed against the inclusion criteria. Any conflicts were resolved through discussion with a third reviewer. Ineligible articles were excluded, and reasons for these exclusions were noted.
Data Extraction and Synthesis
One author (K.S.) extracted data from all studies based on study aims, participant data, outcome measures, key results, limitations, simulation design, and identified barriers and enablers to implementation. A second reviewer charted the data for a random sample of 15 studies to check for consistency and accuracy of extraction. Any discrepancies were resolved through discussion with a third reviewer. The study outcome measures were categorized according to the 4 levels of the Kirkpatrick's evaluation framework.38
To critique the literature on simulation, data were charted according to the reporting guidelines for health care simulation research, which are extensions to the CONSORT and STROBE statements by Cheng et al.48 The reporting guidelines focus on contextual elements of the study design, such as type of simulator and simulation environment, participants' orientation, description of the scenario, and any feedback or debriefing that occurred.48 To collate data for this review, a purpose-designed tool was developed identifying the elements of the Simulation-Based Research Extensions for the CONSORT statement.48 Based on the assumption that all data should be reported, only data presented within the articles were used for appraising simulation reporting quality.
RESULTS
The search strategy identified 8207 citations from online peer-reviewed databases. An additional 402 results were identified from Google Scholar. After the removal of duplicates, 6584 were screened based on title and abstract. Title and abstract screening located 321 articles for full-text review. Nine studies reported insufficient details to determine eligibility based on simulation timing in relation to the placement program. Those authors were contacted via e-mail to request additional information. This was provided for 5 of the studies. The remaining 4 were not. Six additional studies were retrieved from hand searching of reference lists. After full-text review, 48 studies8–10,13,14,18,22,49–89 were included for data synthesis (see Table, Supplementary Digital Content 2, http://links.lww.com/SIH/A767, for simulation experiences integrated into the placement of allied health programs: descriptions by study).
Description of Included Studies
Of the 48 included studies, the year of publication ranged from 1996 to 2020, with 43 (90%) published from 2010 onward. Among the articles included, 27 were conducted in Australia,8–10,14,18,50–52,55,56,59–62,64,66–68,71,72,75,82,84,85,87–89 16 in the United States,13,22,49,54,57,63,70,73,74,76,77,79–81,83,86 4 conducted in the UK,58,65,69,78 and 1 in United Arab Emirates.53
Eight allied health professions were represented throughout the articles. The main disciplines represented included physiotherapy (n = 15),8,10,50,51,61–63,70,79–81,84,85,87,88 pharmacy (n = 9),18,49,54–56,68,77,82,86 radiography (n = 6),53,65–67,69,78 speech pathology (n = 6),14,59,60,71,75,82 and dietetics (n = 5).13,22,57,71,83 Five studies presented findings from interprofessional simulation activities.57,71,73,82,88 Using SBLEs to substitute placement hours was reported by 18 studies,8–10,18,50,51,55,56,59,61–63,65,73–75,86,87 whereas 16 studies implemented SBLEs immediately before professional placement52,57,58,64,66–68,70,77–81,84,85,88 and 13 studies used simulation as an additional component during a professional placement.13,14,22,49,53,54,60,69,72,76,82,83,89 One study included participants across different stages of placement (before placement, during placement, and during curriculum) completing one simulation activity.71
The 48 studies described 43 different simulation programs. The length of the program varied from a single 30-minute interaction to 18 days. Participant numbers ranged from 6 to 394, with mandatory SBLE participation reported in 33 studies8,9,13,14,18,22,49,50,54,55,57,59–61,63–66,68,70–77,81,83–86,89 compared with 15 studies reporting voluntary participation.10,51–53,56,58,62,67,69,78–80,82,87,88 Five different types of simulation modalities were identified including simulated patients (n = 40),8–10,13,14,18,22,50–52,54–57,59–65,68,70,71,73–82,84–89 high-fidelity simulation (n = 10),10,54,57,59,73,79–82,86 computer/online simulation (n = 11),49,53,58,65–67,69,72,75,83,89 and prerecorded simulation (n = 3).52,71,88 Sixteen studies included a hybrid of simulation modalities,10,52,54,57,59,65,71,73,75,79–82,86,88,89 commonly incorporating simulated patients and high-fidelity simulation.
Only 10 studies reported on a learning theory in the development and implementation of the SBLEs,18,53,69,70,73,75,76,80,81,86 with Bandura's Social Learning Theory most commonly reported (n = 5).18,53,73,80,81 There was also variability in the context of the SBLEs reported across all studies. The hospital setting was the most commonly used setting for SBLE (n = 20),8,10,49–51,57,59,61,62,69,76,79–81,83–88 3 studies reported using both hospital and ambulatory care scenarios,55,56,68,90 and 2 reported SBLE within the ambulatory care setting.63,74 A number of studies (n = 17) only reported on the scenario (eg, type 2 diabetes, pediatrics, or orthopedics), which could be applicable within a hospital or ambulatory care setting,9,13,14,18,53,58,60,65,67,70–73,75,78,82,89 and 6 studies did not provide sufficient details of the setting or scenario.22,52,54,64,66,77
The use of actors or community members as simulated patients was the most commonly reported (n = 30).8–10,14,18,22,50,52,55,56,59–65,68,70,71,74,75,78,82,84–89 In 4 studies, the role of patient was played by a student (same discipline/different year n = 1,64 different discipline n = 313,22,57). In addition, 6 studies also reported the use of students within the same discipline cohort portraying additional roles within the simulation including a family member, allied health professional, physician, or therapist assistant.63,76,77,79–81
Overall, studies sought to provide evidence that SBLEs could be used to substitute placement hours and were equivalent to a professional placement experience. The study aims were focused across 4 key areas: (i) development of skills, knowledge, or competency, commonly communication and interpersonal skills; (ii) student confidence or self-efficacy in terms of communication, readiness for placement, or anxiety; (iii) attitudes or perceptions of students, patient, or facilitators; and (iv) a description of the simulation program.
Data were collected at various stages before, during, and after SBLE. Twenty-four studies did not include a comparison group13,14,18,22,52–57,60–62,64,67–69,71–73,77,82,88,89 with 1 study reporting that their ethics committee provided advice not to include a comparison group because of the overwhelming evidence for the benefit of simulation in that program.22 Nineteen studies compared SBLEs with usual placement or university practices,8–10,50,51,59,63,65,66,70,74,76,78–81,84,86,87 3 compared with other activities such as different delivery modes,49,58,83 1 compared the type of placement locations (university-based simulation clinic vs. nursing home),75 and 1 compared the timing of the simulation in the placement structure.85
Program Outcomes According to Kirkpatrick's Framework
Thirty-seven studies reported level 1 outcomes related to student reaction,9,10,13,14,18,22,49,50,52,53,55,56,58,60–64,66–73,75–78,80,81,83,85,86,88,89 captured by experience and satisfaction with the simulation program or emotional responses to participation in SBLEs (stress and anxiety; Table 2). Student learning (level 2) outcomes were described in 37 studies,8–10,14,18,22,49,50,52,54–58,60,63–69,71–73,75–78,80–82,85–89 with self-reported confidence the most common (n = 21).8–10,14,22,50,54,57,58,60,64,65,67,68,72,75,77,80,85–87 Fourteen studies reported level 3 outcomes related to student behavior within the clinical environment,8–10,50,51,59,65,70,74,79,83–85,87 and only 3 studies reported outcomes related to level 4, the organization (university or health care setting).10,51,77
TABLE 2.
Simulation Program Outcomes
| Author (Year) | Profession | Simulation Intervention | Attitudes/Satisfaction With Simulation | Knowledge Development | Skill Development | Change in Confidence | Readiness for Professional Role | Interprofessional Collaboration | Emotional Response | Competency Assessment | Kirkpatrick's Hierarchy |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Preplacement | |||||||||||
| Brown and Williams52 (2009)* | Occupational therapy | Prerecorded SBLE + sim patients | ✓ | ✓ | ✓ | 1, 2 | |||||
| Gibbs et al57 (2015) | Dietetics and nursing | High-fidelity SBLE + sim patients | ✓ | ✓ | ✓ | 2 | |||||
| Green and Appleyard58 (2011) | Radiation therapy | Computer SBLE | ✓ | ✓ | ✓ | 1, 2 | |||||
| Kelly et al64 (2020) | Radiation therapy | Sim patients | ✓ | ✓ | ✓ | 1, 2 | |||||
| Lee et al66 (2020) | Radiography | Computer SBLE | ✓ | ✓ | 1, 2 | ||||||
| Liley et al67 (2018) | Radiography | Computer SBLE | ✓ | ✓ | ✓ | ✓ | 1, 2 | ||||
| Lucas et al (2019)68 | Pharmacy | Sim patients | ✓ | ✓ | 1, 2 | ||||||
| Miller et al70 (2017) | Physiotherapy | Sim patients | ✓ | ✓ | 1, 3 | ||||||
| Sando et al77 (2013) | Pharmacy | Sim patients | ✓ | ✓ | ✓ | 1, 2, 4 | |||||
| Shiner78 (2019) | Radiography | Sim patients | ✓ | ✓ | 1, 2 | ||||||
| Silberman et al79 (2016)† | Physiotherapy | High-fidelity SBLE | ✓ | ✓ | 1, 2 | ||||||
| Silberman et al80 (2016)† | Physiotherapy | High-fidelity SBLE | ✓ | 3 | |||||||
| Silberman et al81 (2013) | Physiotherapy | High-fidelity SBLE | ✓ | ✓ | 1, 2 | ||||||
| Tuttle and Horan84 (2019) | Physiotherapy | Sim patients | ✓ | 3 | |||||||
| Tuttle and Biolocerkowski85 (2017) | Physiotherapy | Sim patients | ✓ | ✓ | ✓ | 1, 2, 3 | |||||
| Williams et al88 (2010)* | Occupational therapy and physiotherapy | Prerecorded SBLE + sim patients | ✓ | ✓ | ✓ | 1, 2 | |||||
| Preplacement and during placement | |||||||||||
| Mills et al71 (2020) | Occupational therapy, speech pathology and dietetics | Prerecorded SBLE + sim patients | ✓ | ✓ | 1, 2 | ||||||
| During placement | |||||||||||
| Al-Dahir et al49 (2014) | Pharmacy | Computer SBLE | ✓ | ✓ | 1, 2 | ||||||
| Elshami and Abuzaid53 (2017) | Radiography | Computer SBLE | ✓ | 1 | |||||||
| Eng et al54 (2014) | Pharmacy | High-fidelity SBLE + sim patients | ✓ | ✓ | ✓ | 2 | |||||
| Farahat et al22 (2015) | Dietetics | Sim patients | ✓ | ✓ | ✓ | ✓ | ✓ | 1, 2 | |||
| Henry et al13 (2009) | Dietetics | Sim patients | ✓ | 1 | |||||||
| Hill et al60 (2013) | Speech pathology | Sim patients | ✓ | ✓ | ✓ | ✓ | 1, 2 | ||||
| Messer and Griffiths69 (2007) | Radiography | Computer high-fidelity SBLE | ✓ | ✓ | 1,2 | ||||||
| Opie and Elsner72 (2010) | Radiation therapy | High-fidelity SBLE | ✓ | ✓ | ✓ | 1, 2 | |||||
| Reed76 (2014) | Occupational therapy | Sim patients | ✓ | ✓ | 1, 2 | ||||||
| Shorland et al14 (2018) | Speech pathology | Sim patients | ✓ | ✓ | ✓ | 1, 2 | |||||
| Taylor et al82 (2017) | Speech pathology, pharmacy and medicine | High-fidelity SBLE + sim patients | ✓ | ✓ | 2 | ||||||
| Turner et al83 (2000) | Dietetics | Computer SBLE | ✓ | ✓ | 1, 3 | ||||||
| Wilson et al89 (2010) | Audiology | Computer SBLE + sim patients | ✓ | ✓ | ✓ | 1, 2 | |||||
| Substitute placement hours | |||||||||||
| Barker et al18 (2018)‡ | Pharmacy | Sim patients | ✓ | ✓ | ✓ | 1, 2 | |||||
| Blackford et al50 (2015)§ | Physiotherapy | Sim patients | ✓ | ✓ | ✓ | ✓ | 1, 2, 3 | ||||
| Blackford et al51 (2020)§ | Physiotherapy | Sim patients | ✓ | ✓ | ✓ | 3, 4 | |||||
| Blackstock et al10 (2013) | Physiotherapy | High-fidelity SBLE + sim patients | ✓ | ✓ | ✓ | ✓ | 1, 2, 3, 4 | ||||
| Fejzic and Barker55 (2016)‡ | Pharmacy | Sim patients | ✓ | ✓ | 1, 2 | ||||||
| Fejzic and Barker56 (2015)‡ | Pharmacy | Sim patients | ✓ | ✓ | ✓ | 1, 2 | |||||
| Hill et al59 (2020) | Speech pathology | Sim patients | ✓ | 3 | |||||||
| Imms et al9 (2018) | Occupational therapy | Sim patients | ✓ | ✓ | ✓ | ✓ | 1, 2, 3 | ||||
| Johnston et al61 (2018) | Physiotherapy | Sim patients | ✓ | 1 | |||||||
| Judd et al62 (2016) | Physiotherapy | Sim patients | ✓ | 1 | |||||||
| Kelly et al63 (1996) | Physiotherapy | Sim patients | ✓ | ✓ | ✓ | 1, 2 | |||||
| Ketterer et al65 (2020) | Radiography | High-fidelity SBLE + sim patients | ✓ | ✓ | 2, 3 | ||||||
| Pfaff73 (2014) | Radiologic technology | High-fidelity SBLE + sim patients | ✓ | ✓ | ✓ | 1, 2 | |||||
| Phillips et al74 (2018) | Social work | Sim patients | ✓ | 3 | |||||||
| Quail et al75 (2016) | Speech pathology | Computer SBLE and sim patients | ✓ | ✓ | ✓ | ✓ | ✓ | 1, 2 | |||
| Vyas et al86 (2010) | Pharmacy | High-fidelity SBLE + sim patients | ✓ | ✓ | ✓ | ✓ | 1, 2 | ||||
| Watson et al87 (2012) | Physiotherapy | Sim patients | ✓ | ✓ | 2, 3 | ||||||
| Wright et al8 (2018) | Physiotherapy | Sim patients | ✓ | ✓ | 2, 3 | ||||||
*Related studies.
†Related studies.
‡Related studies.
§Related studies.
Most studies explored outcomes from the student perspective (n = 44),8–10,13,14,18,22,49,50,52–58,60–73,75–83,85–89 21 studies included outcomes from clinical educators,8–10,50,51,54,57,59,63,65,70,72,74,77,79,83–87,89 5 studies incorporated reflections of simulation facilitators,8,18,55,57,77 and 1 study included the patient perspective.10 The use of validated tools to measure outcomes was reported in 19 studies,8–10,18,50,57,59,62,65,70,71,73–76,79,84,85,87 with the physiotherapy specific placement evaluation tool, Assessment of Physiotherapy Practice,91 the most reported (n = 6).8,10,50,84,85,87 Purpose developed tools were described in 42 studies, with 11 adapted from profession-specific competency tools to meet the simulation learning objectives18,22,50,51,54,56,59,70,74,77,79 and 14 adapted from previous studies.8,14,18,52–54,60,62,66,67,75,81,83,89
Simulation Reporting Appraisal
Key simulation characteristics are reported in Table 3, based on Cheng et al.48 Of the 30 items outlined in the reporting guidelines, studies reported between 2 and 21 items. Twelve studies reported on providing orientation of SBLEs for participants,13,14,22,49,57,58,63,66,67,73,76,77 with an additional 11 partially reporting details.18,54,61,69,75,80,83–85,87,89 The location used for the simulation event was described in 25 studies,8,10,14,22,49,50,52,53,57,59,61–63,67,69,70,72,75–77,81,84,86,87,89 with an additional 7 partially reporting details.9,13,65,66,68,73,74 Description of equipment was well documented in 4 of the 10 studies using high-fidelity simulation54,73,81,86 and 9 of the 11 studies using computer/online simulation.49,53,58,66,67,69,72,83,89 The description of the simulation scenario was the most commonly reported item (n = 45).8–10,13,14,18,22,49,50,52–63,65,67–89
TABLE 3.
Reporting of Simulation Design
| Author (Year) | Orientation | Environment | Event | Design | Feedback | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SBLE | Environment | Location | Equipment | External Stimuli | Description | Learning Obj | Participants | Use of Props | Facilitator Characteristics | Pilot Testing | Sim Patients | Duration | Timing | Frequency/Repetitions | Clinical Variations | Ix Adaptability | Range of Difficulty | Non-SBLE Activities | Assessment | Integration | Duration | Source | Facilitator Present | Facilitator Characteristics | Content | Structure or Models | Timing | Video Recording | Scripted Debrief | ||
| Sim patients | |||||||||||||||||||||||||||||||
| Barker18 (2018) | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||
| Blackford50 (2015) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | P | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | P | ✓ | ✓ | P | |||||||||||||
| Blackford51 (2020) | ✓ | ✓ | |||||||||||||||||||||||||||||
| Farahat22 (2015) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||||||
| Fejzic55 (2016) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||
| Fejzic56 (2015) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | P | |||||||||||||||
| Henry13 (2009) | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | P | ✓ | |||||||||||||||||
| Hill60 (2013) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||||||||||||||
| Imms9 (2018) | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | P | ✓ | ✓ | ||||||||||||||||||
| Johnston61 (2018) | P | ✓ | ✓ | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||||||
| Judd62 (2016) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||||||||||||||
| Kelly63 (1996) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | P | ✓ | ✓ | ||||||||||||
| Kelly64 (2020) | ✓ | ✓ | ✓ | ✓ | |||||||||||||||||||||||||||
| Lucas68 (2019) | P | ✓ | P | ✓ | P | ||||||||||||||||||||||||||
| Miller70 (2017) | ✓ | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | P | ✓ | ✓ | ✓ | P | ||||||||||||
| Phillips74 (2018) | P | ✓ | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||||||
| Reed76 (2014) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||||||
| Sando77 (2013) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||
| Shiner78 (2019) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||||||||
| Shorland14 (2018) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||
| Tuttle84 (2019) | P | ✓ | P | ✓ | P | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | P | |||||||||||
| Tuttle85 (2017) | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||||
| Watson87 (2012) | P | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||||
| Wright8 (2018) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||
| Hybrid: sim patients + high-fidelity SBLE | |||||||||||||||||||||||||||||||
| Blackstock10 (2013) | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||||
| Eng54 (2014) | P | ✓ | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | P | P | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||
| Gibbs57 (2015) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||
| Hill59 (2020) | ✓ | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | P | ||||||||||||||
| Pfaff73 (2014) | ✓ | P | ✓ | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||
| Silberman79 (2016) | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||
| Silberman80 (2016) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||
| Silberman81 (2013) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||||
| Taylor82 (2017) | P | ✓ | P | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||||||
| Vyas86 (2010) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||
| Hybrid: sim patients + prerecorded SBLE | |||||||||||||||||||||||||||||||
| Brown52 (2009) | ✓ | P | ✓ | ✓ | P | ✓ | ✓ | ✓ | Stated no debriefing occurred | ||||||||||||||||||||||
| Mills71 (2020) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||||||||||||||
| Williams88 (2010) | ✓ | ✓ | P | ✓ | ✓ | ✓ | ✓ | P | ✓ | Stated no debriefing occurred | |||||||||||||||||||||
| Computer SBLE | |||||||||||||||||||||||||||||||
| Al-Dahir49 (2014) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | :P | - | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | P | P | ✓ | ||||||||||||||
| Elshami53 (2017) | ✓ | ✓ | ✓ | P | ✓ | ✓ | ✓ | - | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||||||||
| Green58 (2011) | ✓ | ✓ | P | ✓ | P | - | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||||||||||
| Lee66 (2020) | ✓ | P | ✓ | ✓ | ✓ | - | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | P | ✓ | |||||||||||||||
| Liley67 (2018) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | - | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||||||
| Messer69 (2007) | P | ✓ | ✓ | ✓ | P | ✓ | - | ✓ | ✓ | ✓ | ✓ | P | |||||||||||||||||||
| Opie72 (2010) | ✓ | ✓ | ✓ | ✓ | P | - | P | ✓ | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||
| Turner83 (2000) | P | ✓ | P | ✓ | ✓ | ✓ | - | ✓ | ✓ | ✓ | ✓ | ✓ | P | ||||||||||||||||||
| Hybrid: sim patients and computer SBLE | |||||||||||||||||||||||||||||||
| Ketterer65 (2020) | P | P | ✓ | P | ✓ | ✓ | ✓ | P | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||||||
| Quail75 (2016) | P | P | ✓ | ✓ | P | ✓ | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||
| Wilson89 (2010) | P | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | P | P | ✓ | P | ✓ | ✓ | |||||||||||||
*Related studies.
†Related studies.
‡Related studies.
§Related studies.
P, partial reporting or inadequate detail provided.
Feedback was provided to students mostly in group formats immediately after the simulation events and was commonly provided by instructors or clinical educators (n = 23),8,10,14,18,22,50,54,56,57,59,60,63,70,73–75,77,81,84–87,89 simulated patients (n = 16),8,10,13,14,18,22,50,55,56,59–61,70,84,85,87 and peers (n = 8).50,59,70,73,75,77,85,89 Communication, interpersonal skills, and performance were identified as common focus areas for feedback. The use of a formal simulation feedback model (Promoting Excellence in Reflective Learning in Simulation92) was only reported in 1 study.78 An additional 10 studies reported on structuring debriefing sessions using concepts from previous studies or purpose developed checklists based on competency outcomes.18,55–57,70,79–81,84,85
Implementation of Simulation
Short-term funding was provided for 20 studies reporting 17 programs, with 12 awarded external funding (Australian Research Council Linkage Grant,87 Health Workforce Australia,8,55,56 Commonwealth or State Department of Health,9,52,66,67,85,88 Health Education and Training Institute,61 Carolina Healthcare Foundation73) and 9 studies receiving internal university grants.13,22,50,51,63,65,66,75,89
Most studies acknowledged the barriers and enabling factors pertinent for all organizations in implementing such programs. A compilation of the key themes can be seen in Table 4.
TABLE 4.
Identified Barriers and Enablers to Implementing Simulation-Based Learning Experiences
| Barriers | Facilitators |
|---|---|
| –Specificity of SBLE activities not applicable across all placement locations (eg, acute hospital vs private practice) –Variability in student experiences with sim patient dependent on student data gathering –Educators are often not included in the design and implementation –No consideration of student learning styles –Inconsistent provision of feedback dependent on SBLE modality (eg, sim patient SBLE more feedback vs. self-directed computer/prerecorded SBLE) –Impact of technology on learning experiences ○ Equitable access to the internet ○ Software updates –Faculty input to develop sessions ○ Time ○ Experience –Availability of suitable resources, including rooms and equipment –Placement scheduling –Extensive initial financial input for setting up rooms and equipment, training staff and sim patients, development of scenarios –Student anxiety and stress |
–The flexibility of computer and prerecorded SBLE to be scheduled in placements –External and internal funding opportunities –Availability of dedicated SBLE rooms and equipment –Financial benefits once initial outlay invested –Ability to demonstrate rare and complex clinical cases in a safe environment |
DISCUSSION
This is the first known scoping review to synthesize simulation activities incorporated immediately before or within professional placements, focusing on allied health professions and assessing against a structured framework.38,48 The review included 48 studies describing 43 different simulation experiences integrated into the placement components of entry-level allied health professional programs. Simulation programs were valuable to student learning regardless of where and how they were integrated into the professional placement. However, there was considerable variability in the implementation. Most studies also did not acknowledge the reasons related to the timing of SBLEs to placement or the chosen length of the model.
With the expansion of SBLEs, commonly due to increasing student numbers and limited professional placement capacity,10,41,93–95 it is crucial to evaluate the impact on the student and practice to ensure that students are meeting competency requirements without compromising learning opportunities.96
Using Kirkpatrick's hierarchy of evaluation,38 most studies were focused on evaluating level 1 reaction and level 2 learning. Most commonly, this includes evaluating participant satisfaction and self-reported increases in confidence and knowledge, consistent with studies in medicine and nursing.42,97 Although this evaluation method may not provide evidence to suggest immediate learning occurred, it is an essential component of evaluation that can influence the design and implementation of future simulation experiences.42 Studies categorized into level 2 were only related to changes in learning and behaviors in the simulated setting. Most studies focused on developing communication and interpersonal skills, particularly with the use of simulated patients. Because of the link between professional competency and skills required, each simulation program was conducted in a context specific to the allied health profession. For example, a simulation activity related to the specific skill set of using a computed tomography scanner66 cannot be compared with a board game used to undertake a medication reconciliation.77 This variability in simulated programs, which has also been demonstrated within medical specialities,5,6,23,31,97 can impact the generalizability of the results to other professions. It is also important to acknowledge that although these skills seem to achieve the desired learning outcomes in the simulation environment, they do not necessarily demonstrate the ability to transfer the learning to actual practice. The experience of working in a clinical setting is vastly different from the practice of simulation in a safe environment where the experience can be paused, discussed, and reattempted.98 While learning outcomes can be achieved in the simulation environment, it is essential to consider how students respond and adapt when confronted with workplace environments and practices.
Studies exploring simulation application in the clinical environment (level 3) and relevance to the organization (level 4) were limited. Weller et al93 acknowledged the difficulties associated with conducting higher-level evaluations of SBLEs within the medical profession, which has applicability across all health programs. The limited transferability of simulation programs between contexts and the commonly embedded nature of simulation activities into the curriculum makes it hard to isolate learning outcomes.93 Of the studies that evaluated competency in clinical practice,9,10,50,59,65,74,85,87 just more than half found that there was no significant difference in attainment of competency for those who participated in a simulation program compared with those who did not. Student assessments used to assess competence were completed as part of usual practice by the clinical educator at the end of the placement. Placement durations ranged from 5 weeks to a semester in length. Of the studies that found a difference in competency between intervention groups, 2 favorably identified that the simulation group scored higher on competency ratings.8,84 One study found no difference in clinical competency skills between groups, but the control group performed more favorably on professionalism.50 It was reported that training in competency assessments was provided to educators to support the reliability of the tools. However, the educator's interpretation of the evaluation tools and the ability of the tools to accurately measure a meaningful change in clinical performance was commonly identified as a limitation.
Although educators and patients were used to rate student learning, there was no evaluation of the impact of simulation on educator workload or real-patient outcomes. One study investigating physiotherapy educator perspectives found that clinical educators were not aware of the content covered in the SBLEs and tried to compensate for the time students spent away from the clinical environment.51 Although educators saw simulation as a positive concept, overall, they felt that it should not replace clinical time.51 This suggests that greater stakeholder involvement may aid the implementation of SBLEs.
With the increasing popularity of SBLEs for student education, the importance of quality and consistent reporting has been emphasized.99 It has been acknowledged in the literature that simulation research is often poorly reported.48,99 This is consistent with the findings of our review with variability in the reporting of simulation activities identified and most studies poorly reported. Studies commonly described the basic implementation of the SBLEs but failed to include adequate details on methodology and feedback methods. The lack of homogeneity and ability to compare studies makes it problematic to determine the impact of simulation in this area thoroughly. However, it is acknowledged that more than half of the studies included in this review were published before the publication of the Simulation-Based Research Extension for the CONSORT statement48 used to appraise the quality of simulation reporting.
While simulation is a valuable component of the student learning experience, facilitators and funders need to understand the barriers and enablers to implement simulation programs. Most studies indirectly acknowledged barriers and enablers for implementing SBLEs, which were not unique to the allied health professions.93,100 However, few studies addressed the sustainability of programs in the future. With environments constrained by resource availability, facilitators need to take a planned and collaborative approach to develop SBLEs with key consideration to curriculum integration, infrastructure, and staff training.93,101,102
Limitations and Future Research
The purpose of this review was to map the current use of SBLEs within the allied health professions. As such, it offers a broad overview of how SBLEs are being implemented into allied health placements. However, it does not examine the specific outcomes of SBLE or allow for assessment or appraisal of the quality of evidence in the studies. This can limit the ability to generalize findings.
The heterogeneity of the studies was evident, reducing the ability to compare data. This was impacted by including all types of simulation modalities, the variability of tools used for data collection, and the lack of validated tools to measure learning outcomes. In addition, small sample sizes affect the generalizability of the results. Poor reporting of the SBLEs and study methodology made it difficult to assess against the inclusion/exclusion criteria. Although attempts were made to contact authors to obtain details, some studies may have inadvertently been excluded because of a lack of clarity around the timing of SBLEs in relation to professional placement.
It is acknowledged the importance of underpinning learning theories in the design and implementation of SBLEs.25 As this article aimed to map the current use of SBLEs within the allied health professions, the authors made the pragmatic choice to not comprehensively review the link between learning theories and SBLE within allied health programs. However, it is recommended that as SBLEs within allied health programs continue to evolve, more facilitators understand how learning theories can be used to provide a framework for guide student learning outcomes.
Future research should ensure systematic reporting of SBLEs as outlined by Cheng et al48 to ensure a more consistent and meaningful interpretation of learning outcomes.99 Further research could also consider investigating the effects of simulation programs concerning level 3 and level 4 of the Kirkpatrick's evaluation hierarchy.38 This would allow understanding of the transferability of the simulation programs into the clinical environment and the program's value over other educational-based approaches to organizations.
CONCLUSIONS
This review has shown a clear trend toward using simulation in allied health professions as preparation for placement or replacing placement hours. Simulation activities were shown to support students' learning, particularly the development of confidence to perform activities specific to communication and interpersonal skills. There was limited evidence of how this was transferred to the clinical environment. Studies examining clinical competence related to placement outcomes found no difference in the ability to meet competencies between groups who participated in SBLEs and those who did not. This indicates that simulation can substitute for professional placement time without impacting students' ability to meet competencies. However, a model of SBLE, which is used as an adjunct educational tool to a professional placement, could still benefit to ease the increasing demands on clinical placement environments.
Further research is required to determine the optimal proximity of simulation to or within the placement and whether gains obtained from participation in simulation experiences can transition to the clinical environment. Future research requires consistent reporting of simulation methodologies and evaluation methods to strengthen the simulation evidence base.
Supplementary Material
ACKNOWLEDGMENT
The authors thank Julia Fluit for her assistance with data charting and Lucy Kocanda, Lisa Urquhart, Elesa Crowley, Sonja Littlejohns, Rebecca Wolfgang, Jamie Marjoribanks, Alina Roper, and Rachel Urquhart for their assistance with reviewing abstracts and full-text articles. The authors also thank medical librarian Debbie Booth for helping initiate the search strategy.
Footnotes
The authors declare no conflict of interest.
K.S. undertook this research as a partial requirement for the degree of PhD (nutrition and dietetics), the University of Newcastle, Australia. Funding for a research assistant (J Fluit) was supported by the Research Higher Degree funds.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.simulationinhealthcare.com).
Contributor Information
Kelly Squires, Email: kelly.squires@newcastle.edu.au.
Susan Heaney, Email: susan.heaney@newcastle.edu.au.
Lesley MacDonald-Wicks, Email: lesley.wicks@newcastle.edu.au.
Catherine Johnston, Email: cath.johnston@newcastle.edu.au.
REFERENCES
- 1.Maidment J. Getting ready for placement. In: Stagnitti K, Schoo A, Welch D, eds. Clinical and Fieldwork Placement in the Health Professions. South Melbourne, Victoria: Oxford University Press; 2010. [Google Scholar]
- 2.Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge, United Kingdom: Cambridge University Press; 1991. [Google Scholar]
- 3.Graj E, Sheen J, Dudley A, Sutherland-Smith W. Adverse health events associated with clinical placement: a systematic review. Nurse Educ Today 2019;76:178–190. [DOI] [PubMed] [Google Scholar]
- 4.Kilminster S, Zukas M, Quinton N, Roberts T. Preparedness is not enough: understanding transitions as critically intensive learning periods. Med Educ 2011;45(10):1006–1015. [DOI] [PubMed] [Google Scholar]
- 5.McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med 2011;86(6):706–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kneebone RL, Scott W, Darzi A, Horrocks M. Simulation and clinical practice: strengthening the relationship. Med Educ 2004;38(10):1095–1102. [DOI] [PubMed] [Google Scholar]
- 7.Norman J. Systematic review of the literature on simulation in nursing education. ABNF J 2012;23(2):24–28. [PubMed] [Google Scholar]
- 8.Wright A Moss P Dennis DM, et al. The influence of a full-time, immersive simulation-based clinical placement on physiotherapy student confidence during the transition to clinical practice. Adv Simul 2018;3(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Imms C Froude E Chu EMY, et al. Simulated versus traditional occupational therapy placements: a randomised controlled trial. Aust Occup Ther J 2018;65(6):556–564. [DOI] [PubMed] [Google Scholar]
- 10.Blackstock FC Watson KM Morris NR, et al. Simulation can contribute a part of cardiorespiratory physiotherapy clinical education: two randomized trials. Simul Healthc 2013;8(1):32–42. [DOI] [PubMed] [Google Scholar]
- 11.Lopreiato JO. Healthcare Simulation Dictionary. Rockville, MD: Agency for Healthcare Research and Quality; October 2016. AHRQ Publication No. 16(7)-0043; 2016. [Google Scholar]
- 12.Todd JD, McCarroll CS, Nucci AM. High-fidelity patient simulation increases dietetic students' self-efficacy prior to clinical supervised practice: a preliminary study. J Nutr Educ Behav 2016;48(8):563–7.e1. [DOI] [PubMed] [Google Scholar]
- 13.Henry BW, Duellman MC, Smith TJ. Nutrition-based standardised patient sessions increased counseling awareness and confidence among dietetic interns. Top Clin Nutr 2009;24(1):25–34. [Google Scholar]
- 14.Shorland J, Morris C, Stephens D. Simulation speaks for itself: building speechlanguage pathology students' confidence through high quality simulation within a workplace clinical placement. Focus Health Prof Educ 2018;2:53. [Google Scholar]
- 15.Baillie L, Curzio J. Students' and facilitators' perceptions of simulation in practice learning. Nurse Educ Pract 2009;9(5):297–306. [DOI] [PubMed] [Google Scholar]
- 16.Halkett GKB, McKay J, Shaw T. Improving students' confidence levels in communicating with patients and introducing students to the importance of history taking. Radiography 2011;17(1):55–60. [Google Scholar]
- 17.Gibson SJ, Davidson ZE. An observational study investigating the impact of simulated patients in teaching communication skills in preclinical dietetic students. J Hum Nutr Diet 2016;29(4):529–536. [DOI] [PubMed] [Google Scholar]
- 18.Barker M, Fejzic J, Mak AS. Simulated learning for generic communication competency development: a case study of Australian postgraduate pharmacy students. Higher Educ Res Dev 2018;37(6):1109–1123. [Google Scholar]
- 19.Raidl MA, Wood OB, Lehman JD, Evers WD. Computer-assisted instruction improves clinical reasoning skills of dietetics students. J Am Diet Assoc 1995;95(8):868–873. [DOI] [PubMed] [Google Scholar]
- 20.Mok HT, So CF, Chung JWY. Effectiveness of high-fidelity patient simulation in teaching clinical reasoning skills. Clin Simul Nurs 2016;12(10):453–467. [Google Scholar]
- 21.Miles A, Friary P, Jackson B, Sekula J, Braakhuis A. Simulation-based dysphagia training: teaching interprofessional clinical reasoning in a hospital environment. Dysphagia 2016;31(3):407–415. [DOI] [PubMed] [Google Scholar]
- 22.Farahat E, Rice G, Daher N, Heine N, Schneider L, Connell B. Objective Structured Clinical Examination (OSCE) improves perceived readiness for clinical placement in nutrition and dietetic students. J Allied Health 2015;44(4):208–214. [PubMed] [Google Scholar]
- 23.Harper M, EalesReynolds L, Markham C. Transforming simulation in clinical education: is pre-placement hybrid learning valuable to healthcare students. J Contemp Med Educ 2013;1:1. [Google Scholar]
- 24.Bearman M, Nestel D, McNaughton N. Theories informing healthcare simulation practice. In: Nestel D, Kelly M, Jolly B, Watson M, eds. Healthcare Simulation Education: Evidence, Theory and Practice. West Sussex, United Kingdom: John Wiley & Sons Ltd; 2018:7–15. [Google Scholar]
- 25.O'Shea MC, Palermo C, Rogers GD, Cardell E, Williams LT. It is time to link theory to practice in simulation-based learning: lessons from learning theories. J Acad Nutr Diet 2021;S2212-2672(21):00411–00411. [DOI] [PubMed] [Google Scholar]
- 26.Rutherford-Hemming T. Simulation methodology in nursing education and adult learning theory. Adult Learn 2012;23(3):129–137. [Google Scholar]
- 27.Erlam G, Smythe L, Wright-St Clair V. Simulation is not a pedagogy. Open J Nurs 2017;7:779–787. [Google Scholar]
- 28.Larue C, Pepin J, Allard E. Simulation in preparation or substitution for clinical placement: a systematic review of the literature. J Nurs Educ Pract 2015;5. [Google Scholar]
- 29.Roberts E, Kaak V, Rolley J. Simulation to replace clinical hours in nursing: a meta-narrative review. Clin Simul Nurs 2019;37:5–13. [Google Scholar]
- 30.Bogossian FE Cant RP Ballard EL, et al. Locating “gold standard” evidence for simulation as a substitute for clinical practice in prelicensure health professional education: a systematic review. J Clin Nurs 2019;28(21–22):3759–3775. [DOI] [PubMed] [Google Scholar]
- 31.Giblett N, Rathore R, Carruthers D. Simulating the surgical patient pathway for undergraduates. J Surg Educ 2017;74(2):271–276. [DOI] [PubMed] [Google Scholar]
- 32.Chu EMY, Sheppard L, Guinea S, Imms C. Placement replacement: a conceptual framework for designing simulated clinical placement in occupational therapy. Nurs Health Sci 2019;21(1):4–13. [DOI] [PubMed] [Google Scholar]
- 33.Hill AE, Davidson BJ, McAllister S, Wright J, Theodoros DG. Assessment of student competency in a simulated speech-language pathology clinical placement. Int J Speech Lang Pathol 2014;16(5):464–475. [DOI] [PubMed] [Google Scholar]
- 34.Dzulkarnain AA, Wan Mhd Pandi WM, Rahmat S, Zakaria N. Simulated learning environment (SLE) in audiology education: a systematic review. Int J Audiol 2015;54(12):881–888. [DOI] [PubMed] [Google Scholar]
- 35.MacBean N, Theodoros D, Davidson B, Hill AE. Simulated learning environments in speech-language pathology: an Australian response. Int J Speech Lang Pathol 2013;15(3):345–357. [DOI] [PubMed] [Google Scholar]
- 36.Seybert AL. Patient simulation in pharmacy education. Am J Pharm Educ 2011;75(9):187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marks-Maran D. Educational research methods for researching innovations in teaching, learning and assessment: the nursing lecturer as researcher. Nurse Educ Pract 2015;15(6):472–479. [DOI] [PubMed] [Google Scholar]
- 38.Kirkpatrick J, Kirkpatrick WK. Kirkpatrick's Four Levels of Training Evaluation [electronic resource]. Alexandria, VA: ATD Press; 2016. [Google Scholar]
- 39.Hakimi M, Kheirkhah M, Abolghasemi J, Hakimi R, Farshad F. The effect of competency-based education in obstetric emergencies on midwifery students in clinical skill lab, based on Kirkpatrick evaluation model: a randomised controlled trial. bioRxiv 2019;695791. [Google Scholar]
- 40.Oh J, Kim SJ, Kim S, Vasuki R. Evaluation of the effects of flipped learning of a nursing informatics course. J Nurs Educ 2017;56(8):477–483. [DOI] [PubMed] [Google Scholar]
- 41.Rutherford-Hemming T, Nye C, Coram C. Using simulation for clinical practice hours in nurse practitioner education in the United States: a systematic review. Nurse Educ Today 2016;37:128–135. [DOI] [PubMed] [Google Scholar]
- 42.Johnston S, Coyer FM, Nash R. Kirkpatrick's evaluation of simulation and debriefing in health care education: a systematic review. J Nurs Educ 2018;57(7):393–398. [DOI] [PubMed] [Google Scholar]
- 43.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8(1):19–32. [Google Scholar]
- 44.Tricco AC Lillie E Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169(7):467–473. [DOI] [PubMed] [Google Scholar]
- 45.Squires K, Brown L, MacDonald-Wicks L, Johnston C. Mapping the outcomes of simulated learning experiences incorporated into placement components of university-based allied health programs: a scoping review protocol. Available at: https://osf.io/zpc4u/. Accessed June 24. 2019. [DOI] [PMC free article] [PubMed]
- 46.Allied Health Professions Australia . What is allied health? 2017. Available at: https://ahpa.com.au/what-is-allied-health/. Accessed January 23 2020.
- 47.Allied health professions Australia . Allied health professions. 2017. Available at: https://ahpa.com.au/allied-health-professions/. Accessed January 23 2020.
- 48.Cheng A Kessler D Mackinnon R, et al. Reporting guidelines for health care simulation research: extensions to the CONSORT and STROBE statements. Adv Simul (Lond) 2016;1:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Al-Dahir S, Bryant K, Kennedy KB, Robinson DS. Online virtual-patient cases versus traditional problem-based learning in advanced pharmacy practice experiences. Am J Pharm Educ 2014;78(4):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Blackford J, McAllister L, Alison J. Simulated learning in the clinical education of novice physiotherapy students. Int J Pract Based Learn Health Soc Care 2015;3(1):77–93. [Google Scholar]
- 51.Blackford J, Alison J, McAllister L, Nisbet G. The clinical educators' experience of replacing physiotherapy student clinical education time with simulation. Int J Pract Based Learn Health Soc Care 2020;8(1):60–72. [Google Scholar]
- 52.Brown T, Williams B. The use of DVD simulation as an interprofessional education tool with undergraduate occupational therapy students. Br J Occup Ther 2009;72(6):266–274. [Google Scholar]
- 53.Elshami W, Abuzaid M. Transforming magnetic resonance imaging education through simulation-based training. J Med Imaging Radiat Sci 2017;48(2):151–158. [DOI] [PubMed] [Google Scholar]
- 54.Eng AJ Namba JM Box KW, et al. High-fidelity simulation training in advanced resuscitation for pharmacy residents. Am J Pharm Educ 2014;78(3):59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fejzic J, Barker M, Hills R, Priddle A. Communication capacity building through pharmacy practice simulation. Am J Pharm Educ 2016;80(2):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fejzic J, Barker M. Implementing simulated learning modules to improve students' pharmacy practice skills and professionalism. Pharm Pract (Granada) 2015;13(3):583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gibbs H, George K, Barkley R, Meyer M. Using multiple-patient simulations to facilitate interprofessional communication between dietetic and nursing students and improve nutrition care process skills. Top Clin Nutr 2015;30(3):230–238. [Google Scholar]
- 58.Green D, Appleyard R. The influence of VERT™ characteristics on the development of skills in skin apposition techniques. Radiography 2011;17(3):178–182. [Google Scholar]
- 59.Hill AE Ward E Heard R, et al. Simulation can replace part of speech-language pathology placement time: a randomised controlled trial. Int J Speech Lang Pathol 2020;23:92–102. [DOI] [PubMed] [Google Scholar]
- 60.Hill AE, Davidson BJ, Theodoros DG. Speech-language pathology students' perceptions of a standardised patient clinic. J Allied Health 2013;42(2):84–91. [PubMed] [Google Scholar]
- 61.Johnston CLP, Wilson JCB, Wakely LP, Walmsley SP, Newstead CJB. Simulation as a component of introductory physiotherapy clinical placements. N Z J Physiother 2018;46(3):95–104. [Google Scholar]
- 62.Judd BK, Alison JA, Waters D, Gordon CJ. Comparison of psychophysiological stress in physiotherapy students undertaking simulation and hospital-based clinical education. Simul Healthc 2016;11(4):271–277. [DOI] [PubMed] [Google Scholar]
- 63.Kelly DG, Brown DS, Perritt L, Gardner DL. A descriptive study comparing achievement of clinical education objectives and clinical performance between students participating in traditional and mock clinics. J Phys Ther Educ 1996;10(1):26–31. [Google Scholar]
- 64.Kelly T, Surjan Y, Rinks M, Warren-Forward H. Effect of communication skills training on radiation therapy student's confidence and interactions during their first clinical placement. Radiography (Lond) 2021;27:59–66. [DOI] [PubMed] [Google Scholar]
- 65.Ketterer SJ Callender J Warren M, et al. Simulated versus traditional therapeutic radiography placements: a randomised controlled trial. Radiography (Lond) 2020;26(2):140–146. [DOI] [PubMed] [Google Scholar]
- 66.Lee K, Baird M, Lewis S, McInerney J, Dimmock M. Computed tomography learning via high-fidelity simulation for undergraduate radiography students. Radiography (Lond) 2020;26(1):49–56. [DOI] [PubMed] [Google Scholar]
- 67.Liley T, Ryan E, Lee K, Dimmock M, Robinson J, Lewis SJ. Student perceptions of remote access simulated learning in computed tomography. Interact Learn Environ 2018;1–11. [Google Scholar]
- 68.Lucas C, Williams K, Bajorek B. Virtual pharmacy programs to prepare pharmacy students for community and hospital placements. Am J Pharm Educ 2019;83(10):7011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Messer S, Griffiths M. An online clinical governance learning package for student radiographers. Radiography 2007;13(2):95–102. [Google Scholar]
- 70.Miller AH, Tomlinson S, Tomlinson JD, Readinger J. Addition of a patient examination module to address student preparedness for the first full-time clinical experience. J Phys Ther Educ 2017;31(2). [Google Scholar]
- 71.Mills B Hansen S Nang C, et al. A pilot evaluation of simulation-based interprofessional education for occupational therapy, speech pathology and dietetic students: improvements in attitudes and confidence. J Interprof Care 2020;34(4):472–480. [DOI] [PubMed] [Google Scholar]
- 72.Opie C, Elsner K. Using simulations to train students in treatment planning. Radiat Ther 2010;19(1):18–26. [Google Scholar]
- 73.Pfaff MA. Learning together: the image gently interprofessional simulation for nursing and allied health students. Teach Learn Nurs 2014;9(3):108–114. [Google Scholar]
- 74.Phillips ES Wood GJ Yoo J, et al. A virtual field practicum: building core competencies prior to agency placement. J Soc Work Educ 2018;54(4):620–640. [Google Scholar]
- 75.Quail M, Brundage SB, Spitalnick J, Allen PJ, Beilby J. Student self-reported communication skills, knowledge and confidence across standardised patient, virtual and traditional clinical learning environments. BMC Med Educ 2016;16(1):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Reed HE. An Examination of Critical Thinking Skills in Traditional and Simulated Environments for Occupational Therapy Students [Ed.D.]. Ann Arbor, MI: San Diego State University; 2014. [Google Scholar]
- 77.Sando KR, Elliott J, Stanton ML, Doty R. An educational tool for teaching medication history taking to pharmacy students. Am J Pharm Educ 2013;77(5):105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shiner N. Can simulation impact on first year diagnostic radiography students' emotional preparedness to encounter open wounds on their first clinical placement: a pilot study. Radiography 2019;25(4):294–300. [DOI] [PubMed] [Google Scholar]
- 79.Silberman NJ, Litwin B, Panzarella KJ, Fernandez-Fernandez A. Student clinical performance in acute care enhanced through simulation training. J Acute Care Phys Ther 2016;7(1):25–36. [Google Scholar]
- 80.Silberman NJ, Litwin B, Panzarella KJ, Fernandez-Fernandez A. High fidelity human simulation improves physical therapist student self-efficacy for acute care clinical practice. J Phys Ther Educ 2016;30(1):14–24. [Google Scholar]
- 81.Silberman NJ, Panzarella KJ, Melzer BA. Using human simulation to prepare physical therapy students for acute care clinical practice. J Allied Health 2013;42(1):25–32. [PubMed] [Google Scholar]
- 82.Taylor S, Fatima Y, Lakshman N, Roberts H. Simulated interprofessional learning activities for rural health care services: perceptions of health care students. J Multidiscip Healthc 2017;10:235–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Turner RE, Evers WD, Wood OB, Lehman JD, Peck LW. Computer-based simulations enhance clinical experience of dietetics interns. J Am Diet Assoc 2000;100(2):183–190. [DOI] [PubMed] [Google Scholar]
- 84.Tuttle N, Horan SA. The effect of replacing 1 week of content teaching with an intensive simulation-based learning activity on physiotherapy student clinical placement performance. Adv Simul 2019;4(suppl 1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tuttle N, Bialocerkowski A. Developing student skills to actively engage in feedback conversations: a pilot study. Int J Allied Health Sci Pract 2017;15(4). DOI 10.46743/1540-580X/2017.1681. [DOI] [Google Scholar]
- 86.Vyas D, Wombwell E, Russell E, Caligiuri F. High-fidelity patient simulation series to supplement introductory pharmacy practice experiences. Am J Pharm Educ 2010;74(9):169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Watson K Wright A Morris N, et al. Can simulation replace part of clinical time? Two parallel randomised controlled trials. Med Educ 2012;46(7):657–667. [DOI] [PubMed] [Google Scholar]
- 88.Williams B, Brown T, Scholes R, French J, Archer F. Can interdisciplinary clinical DVD simulations transform clinical fieldwork education for paramedic, occupational therapy, physiotherapy, and nursing students? J Allied Health 2010;39(1):3–10. [PubMed] [Google Scholar]
- 89.Wilson WJ, Hill A, Hughes J, Sher A, Laplante-Levesque A. Student audiologists' impressions of a simulation training program. Austr N Z J Audiol 2010;32(1):19–30. [Google Scholar]
- 90.Manchester school of pharmacy to house “virtual hospital ward”. Pharm J 2002;269(7213):272. [Google Scholar]
- 91.Dalton M, Davidson M, Keating J. The assessment of physiotherapy practice (APP) is a valid measure of professional competence of physiotherapy students: a cross-sectional study with Rasch analysis. J Physiother 2011;57(4):239–246. [DOI] [PubMed] [Google Scholar]
- 92.Eppich W, Cheng A. Promoting Excellence and Reflective Learning in Simulation (PEARLS): development and rationale for a blended approach to health care simulation debriefing. Simul Healthc 2015;10(2):106–115. [DOI] [PubMed] [Google Scholar]
- 93.Weller JM, Nestel D, Marshall SD, Brooks PM, Conn JJ. Simulation in clinical teaching and learning. Med J Aust 2012;196(9):594. [DOI] [PubMed] [Google Scholar]
- 94.Sheepway L, Lincoln M, Togher L. An international study of clinical education practices in speech-language pathology. Int J Speech Lang Pathol 2011;13(2):174–185. [DOI] [PubMed] [Google Scholar]
- 95.Gustafsson L, Brown T, McKinstry C, Caine A-M. Practice education: a snapshot from Australian university programmes. Aust Occup Ther J 2017;64(2):159–169. [DOI] [PubMed] [Google Scholar]
- 96.Voelker R. Medical simulation gets real. JAMA 2009;302(20):2190–2192. [DOI] [PubMed] [Google Scholar]
- 97.McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation-based medical education research: 2003–2009. Med Educ 2010;44(1):50–63. [DOI] [PubMed] [Google Scholar]
- 98.Kaplonyi J Bowles K-A Nestel D, et al. Understanding the impact of simulated patients on health care learners' communication skills: a systematic review. Med Educ 2017;51(12):1209–1219. [DOI] [PubMed] [Google Scholar]
- 99.Sevdalis N, Nestel D, Kardong-Edgren S, Gaba DM. A joint leap into a future of high-quality simulation research-standardizing the reporting of simulation science. Adv Simul (Lond) 2016;1:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nestel D, Kelly M, Jolly B, Watson M. Healthcare Simulation Education : Evidence, Theory and Practice. New York, United Kingdom: John Wiley & Sons, Incorporated; 2017;3–4. [Google Scholar]
- 101.Nestel D, Brazil V, Hay M. You can't put a value on that… Or can you? Economic evaluation in simulation-based medical education. Med Educ 2018;52(2):139–141. [DOI] [PubMed] [Google Scholar]
- 102.Motola I, Devine LA, Chung HS, Sullivan JE, Issenberg SB. Simulation in healthcare education: a best evidence practical guide. AMEE Guide No. 82. Med Teach 2013;35(10):e1511–e1530. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


