Abstract
Introduction
Intrapartum-related events account for nearly 700,000 neonatal deaths globally yearly. Endotracheal intubation is a cornerstone in preventing many of these deaths, but it is a difficult skill to acquire. Previous studies have described intubation performances in high-income countries, but data from low- and middle-income countries are lacking. We aimed to assess the performance of delivery room intubation in a lower middle-income country.
Methods
This prospective observational study was conducted at the Phu San Hanoi Hospital, Vietnam, from September 2020 to January 2021. Video cameras were positioned above the resuscitation tables and data were extracted using adopted software (NeoTapAS). All neonates requiring positive pressure ventilation were included. Our main variables of interest were time to first intubation attempt, first intubation attempt duration, and successful first intubation attempt.
Results
18,107 neonates were born during the five months. Of these, 75 (0.4%) received positive pressure ventilation, and 36 (0.2%) required endotracheal intubation of whom 24 were captured on video. The median time to the first intubation attempt was 252 seconds (range 91–771 seconds), the median first attempt duration was 49 seconds (range 10–105 seconds), and the first attempt success rate was 75%.
Conclusion
Incidences of positive pressure ventilation and endotracheal intubation were low in comparison to global estimates. Three out of four intubations were successful at the first attempt and the procedural duration was often longer than recommended. Future studies should focus on how to achieve and maintain intubation skills and could include considering alternative devices for airway management at birth.
Keywords: Birth asphyxia, Endotracheal intubation (ETI), Neonatal resuscitation, Intrapartum-related events, Positive pressure ventilation (PPV), Vietnam
Abbreviations: ETI, Endotracheal tube intubation; FMV, Face mask ventilation; ILCOR, International Liaison Committee on Resuscitation; PPV, Positive pressure ventilation
Introduction
Intrapartum-related events (birth asphyxia) account for nearly 700,000 neonatal deaths globally yearly. This makes up approximately-one-quarter of the neonates that die during their first month of life1, 2. For the affected but surviving neonate, the development of hypoxic-ischemic encephalopathy is a strong predictor of long-term neurological impairment. Current knowledge of intrapartum-related events in Vietnam is limited. As the country has improved its economy and implemented many humanitarian initiatives in recent years, it is often seen as a role model among middle-income countries. However, substantial under-reporting of neonatal mortality has been reported, and geographical and socioeconomic disparities exist3, 4. Phu San Hanoi Hospital is the largest obstetric hospital in Hanoi and is considered one of Vietnam’s best public hospitals. Our research team has previously reported a low rate of intrapartum-related events at Phu San Hanoi Hospital compared to global figures. In November 2019 the overall positive pressure ventilation (PPV) rate at birth was 0.6%, the incidence of hypoxic-ischemic encephalopathy was 0.15%, the stillbirth rate was 1.0%, and no term live-born neonates died due to an intrapartum-related event5, 6.
Effective PPV is a cornerstone in neonatal resuscitation and may reduce brain injury in the asphyxiated neonate. PPV is most often administered via face mask and, in the case of face mask ventilation (FMV) failure, via endotracheal intubation (ETI). According to best practice, FMV should be initiated within 60 seconds after birth in a neonate with apnea/gasping or a heart rate < 100 beats per minute, and ETI should be considered if FMV remains ineffective despite corrective measures (adjusting face Mask, Reposition head, Suction, Open mouth, increase ventilation Pressure, and artificial Airway, e.g. ETI/supraglottic airway, summarized in the popular acronym MRSOPA). Neonatal deterioration has previously been defined as a fall in SpO2, heart rate, or both, by > 10% compared to the value just before the ETI attempt7. To minimize PPV interruption, and to prevent neonatal deterioration during the ETI attempt, the duration of each attempt should not exceed 30 seconds Wyckoff et al., 2020; Madar et al., 2021; Aziz et al., 2020; 1428, 9, 10. Findings from studies conducted in high-income countries show that ETI is a technically difficult skill to acquire, and it has previously been questioned whether current best practice is achievable7, 11, 12, 13. Data on ETI practice in low- and middle-income countries are lacking. We used video cameras to record the resuscitative procedures in a lower middle-income country14 delivery room. Information from this study could raise awareness of ETI performance, and how it compares to current guidelines.
Methods
This prospective observational study was conducted at the Phu San Hanoi Hospital, the largest obstetric hospital in northern Vietnam, from September 2020 to January 2021. All neonates that received PPV in the delivery room were included in the study.
Study setting
At the Phu San Hanoi Hospital, approximately 40,000 deliveries take place every year. The delivery wards are equipped with paper-printed cardiotocography, heaters, wall-mounted suction devices, oxygen blenders, bag valve masks and ETI equipment. Cole uncuffed endotracheal tubes and Miller straight blade laryngoscopes are used. The route for intubation is orotracheal. Neither pre-interventional oxygen nor premedication are routinely used in the delivery room (although some preterm neonates receive oxygen via face mask ventilation as part of the initial resuscitative attempt). Pulse oximeters exist but are not routinely used. The wards lack T-piece resuscitators, CPAP, supraglottic airways and video laryngoscopy. There are ten neonatal resuscitation tables located in dedicated delivery rooms. Midwives attend all the stages of labor. Before each birth, the obstetrician examines the mother, to evaluate the risk and indication for the mode of delivery. The hospital’s overall c-section rate is above 50%, of which approximately half are emergency c-sections. The most common indications for emergency c-section include previous c-section in labor, livable multiple pregnancies in labor, abnormal presentation, failure to progress, fetal distress, indeterminate fetal heart rate tracing, and suspected macrosomia. The Phu San Hanoi Hospital is situated next to Vietnam National Children’s Hospital. The sickest neonates at the Phu San Hanoi neonatal unit (including the neonates who require cooling) are transferred to the National Children’s Hospital.
Resuscitating team and guidelines
The neonatal resuscitation team is called when a newborn neonate is anticipated to be, or is, distressed at birth. The team comprises two midwives and one neonatology junior doctor with a variable experience in neonatal intensive care and ETI. The team can be expanded to include a larger neonatal team including an anesthetist. All staff who attend deliveries complete an in-house resuscitation training program based on the UK Resuscitation Council guidelines15.
Data collection
Eligible study participants were identified by implementing a three-step approach;1 all doctors at the Phu San Hanoi neonatal unit received information about the study and were requested to inform the research team (date, time and resuscitation table) in the event of administered PPV at birth;2 every weekday, two research team members screened the neonatal unit for eligible participants (at the Phu San Hanoi Hospital, PPV at birth is a neonatal unit admission indication);3 video cameras were positioned above six of the ten resuscitation tables (chosen based on highest usage) and data were recorded around the clock. A trained research assistant reviewed the video recordings and extracted all relevant episodes.
We analyzed all extracted episodes and identified whether, and when, ETI was attempted. Data on the resuscitative procedures were extracted from the video recordings using the adopted software NeoTapAS (Version 1.6.2., Tap4life, Stockholm, Sweden) and R16, 17. To facilitate heart rate monitoring, NeoBeat (Laerdal Global Health, Stavanger, Norway), a reusable dry-electrode ECG that takes seconds to put on the neonate’s abdomen was introduced18. Our main variables of interest were time to first ETI attempt (seconds), first ETI attempt duration (seconds), and successful first ETI attempt (yes/no). The duration of an intubation attempt was defined as the time elapsed from the introduction of the laryngoscope blade into the mouth to its removal (if failed), or to the first ventilated breath (if successful). We determined success according to the resuscitating doctor’s evaluation in the clinical improvement (heart rate and color). Deep suction was defined as an estimated depth > 4 cm. Vigorous stimulation was defined as noticeably vigorous stimulation on the newborn’s back or stimulation of any other body part. Ventilation and chest compression rates were defined as the mean of three representative rates during the first minute (each rate was established by tapping on NeoTapAS’ touchscreen at the same rate as was visualized on the video recording).
Case report forms focusing on maternal and neonatal demographics, hypoxic-ischemic encephalopathy evaluation (according to the Sarnat scoring system at 6 and 12 hours, and 1, 2, 3 and 7 days of life), clinical management, and outcomes, were filled out for all neonates19. Study participants were followed until their discharge (including participants that transferred to the National Children’s Hospital). We did not have any polyclinical follow up for the neonates that were discharged prior to day 7 of life. Data were subsequently transferred from the case report forms into an electronic database (RedCap, Vanderbilt, USA) by a trained research assistant20.
Statistical analyses
Variables were reported as frequencies and percentages for categorical data, and medians with interquartile ranges (IQR) for continuous data. To facilitate comparison with previous studies we also provided continuous data as means with standard deviations. Data analysis was performed using STATA version 16.1 (StataCorp LCC, Texas, USA).
Ethical considerations and consent
The study was approved by the Vietnamese and Swedish Institutional Review Boards (details in the Ethical Approvals section). Ethical aspects of video recording for data documentation during neonatal resuscitation have previously been thoroughly discussed21. Only the neonate and the gloved hands of the resuscitating staff were visible on the muted video recordings. All staff involved in neonatal resuscitation received at least one information session prior to study commencement and the staff could opt not to participate in the study at any time. We adopted a two-tier procedure for parental consent: i) posters were put up in all relevant hospital wards, during which stage parents of both eligible and non-eligible neonates had the opportunity to actively opt out; ii) the parents of eligible neonates were approached for a deferred consent before reviewing the video of their resuscitated newborn neonate. Standard care was given to the resuscitated neonates, the only difference was the use of NeoBeat.
Results
Study cohort and demographics
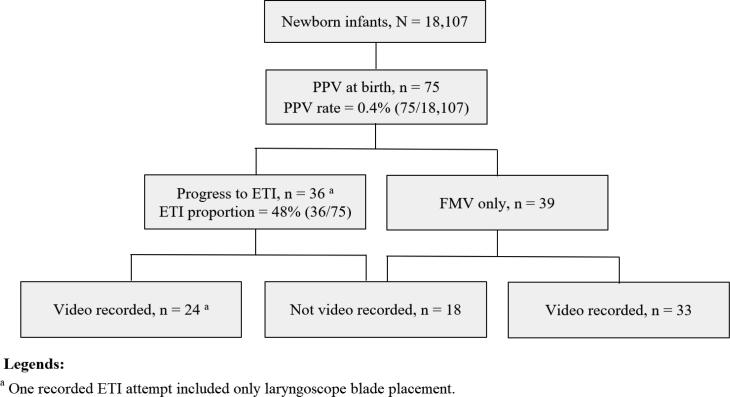
During the five study months, a total of 18,107 neonates were born at Phu San Hanoi Hospital. The three-step system for identifying eligible study participants was congruent. Consent was given to all eligible neonates. The entire cohort is presented in Fig. 1. The overall PPV rate at birth was 0.4% (n = 75), and of these 48% (n = 36) required ETI. The demographics of the included neonates are presented in Table 1.
Fig. 1.
Flowchart over neonates born between 2020.09.01 and 2021.01.31, and required PPV at birth.
Table 1.
Demographics of the study-included neonates (N = 75).
| Total (N = 75) | Video recorded (n = 57) | Video recorded ETI (n = 24) | |
|---|---|---|---|
| N (%) / median (IQR) | N (%) / median (IQR) | N (%) / median (IQR) | |
| General | |||
| Female | 27 a (36) | 21b (37) | 12 (50) |
| Multiple births | 8 (11) | 8 (14) | 2 (8) |
| Gestational age (weeks) | |||
| <28 | 10 (13) | 10 (18) | 3 (13) |
| 28–32 | 15 (20) | 13 (23) | 9 (38) |
| 32–37 | 19 (25) | 11 (19) | 5 (21) |
| >37 | 31 (41) | 23 (40) | 7 (29) |
| Birth weight | |||
| <1,000 grams | 9 (12) | 8 (14) | 1 (4) |
| 1,000–1,499 grams | 18 (24) | 16 (28) | 10 (42) |
| 1,500–2,500 grams | 14 (19) | 9 (16) | 5 (21) |
| >2,500 grams | 34 (45) | 24 (42) | 8 (33) |
| Mode of deliveryb | |||
| Spontaneous vaginal delivery | 30 (40) | 27 (47) | 11 (46) |
| Elective c-section | 11 (15) | 8 (14) | 1 (4) |
| Emergency c-section | 33 (44) | 22 (39) | 12 (50) |
| Maternal factors | |||
| Age (years) | 31 (27–34) | 30 (26–33) | 32 (28–34) |
| Primipara | 32 (43) | 27 (47) | 9 (38) |
| Previous preterm births b | 3 (4) | 1 (2) | 1 (4) |
| Previous miscarriage/stillbirth b | 12 (16) | 8 (14) | 5 (21) |
| Perinatal factors | |||
| Stained/foul-smelling meconium | 1 (1) | 1 (2) | 1 (4) |
| PROM b | 8 (11) | 6 (11) | 4 (17) |
| PPROM | 4 (5) | 3 (5) | 2 (8) |
| Prolonged PROM (>18 hrs) | 2 (3) | 2 (4) | 1 (4) |
| Intrapartum infection | 3 (4) | 3 (5) | 2 (8) |
| GBS positiv b | 1 (1) | 0 (0) | 0 (0) |
| Preeclampsia | 4 (5) | 2 (4) | 1 (4) |
| Placenta praevia | 8 (11) | 6 (11) | 3 (13) |
| Placenta abruption | 1 (1) | 1 (2) | 0 (0) |
| Apgar | |||
| Apgar score at 1 min | 4 (3–6) | 4 (3–5) | 3 (2–4) |
| Apgar score at 5 min | 6 (5–7) | 6 (5–8) | 5 (4–5) |
Gender is missing for two subjects.
Missing for one subject.
Video recorded study participants
A total of 57 neonates who received PPV were captured on a video camera (Table 2). Of the video recorded neonates, 24 required ETI, and neonatology junior doctors carried out at least 22 of these (data on staff members who delivered PPV were missing for two neonates). The endotracheal tube placement was confirmed by auscultation within 15 seconds for three (13%) neonates. Data on heart rate changes during the first ETI attempts were available for nine neonates, of whom four had a heart rate reduction exceeding 10% (Table 3 and Supplementary information 1).
Table 2.
Resuscitative measures for the video recorded neonates (N = 57).
| N (%) / median (IQR) | min–max | |
|---|---|---|
| Stimulation, N = 57 | ||
| Total stimulation time (sec) | 26 (8–56) | 0–267 |
| Number of stimulation episodes | 11 (4–18) | 0–69 |
| Number of vigorous stimulation episodes a | 0 (0–1) | 0–13 |
| Suction, N = 57 | ||
| Total suction time (sec) | 24 (11–43) | 0–104 |
| Number of suction episodes | 1 (1–3) | 0–10 |
| Number of deep suction episodes b | 1 (0–3) | 0–8 |
| Number of suction episodes via the endotracheal tube | 0 (0–0) | 0–1 |
| Initiation of positive pressure ventilation (PPV), N = 57 | ||
| Time to initiation of PPV (sec)c | 30 (15–60) | 2–385 |
| Duration of PPV before first interruption (sec) | 9 (2–21) | 0–195 |
| Ventilation rate (breaths per minute) d | 72 (57–95) | 30–158 |
| Face mask ventilation (FMV, only), N = 33 | ||
| Total duration of FMV without pauses (sec) | 69 (40–111) | 8–228 |
| Total duration of FMV included pauses (sec) | 98 (49–247) | 8–538 |
| Endotracheal intubation (ETI), N = 24 | ||
| Duration of FMV prior to successful ETI, without pauses (sec) | 94 (68–141) | 0–404 |
| Duration of FMV prior to successful ETI, included pauses (sec) | 205 (117–344) | 0–805 |
| Surfactant administered | 1 (4) | - |
| Measuring exhaled CO2 | 0 (0) | - |
| Lung auscultation ≤ 15 seconds after tube placement | 3 (13) | - |
| Circulation, N = 57 | ||
| Heart auscultation within one minute c | 17 (30) | - |
| Adrenaline administered e | 1 (2) | - |
| Chest compressions administered f | 9 (6) | - |
| Chest compression rate (beats per minute) g | 276 (195–304) | 144–323 |
Stimulation of the back that was noticeably vigorous or stimulation to any other part of the neonate than the back.
Estimated > four centimeter depth, and include all suctions via the endotracheal tube.
Time is counted from arrival at the resuscitation table.
The mean of three representative rates during the first minute of PPV. The mean of two or one representative rate is used for four observations due to the short total ventilation time. One observation has no recorded rate due to the ventilation bag being held outside of the camera view.
Intracardiac injection.
Three observations in FMV group and six observations in ETI group.
The mean of three representative rates during the first minute of chest compressions. For one observation, the mean of two representative rates is used due to the short total chest compression time.
Table 3.
Changes in heart rate during the first ETI attempt, for neonates where NeoBeat was used and displaying a visible heart rate on its monitor (N = 9).
| Heart reate (bpm) |
|||
|---|---|---|---|
| ETI attempt | Immediately preceding attempt | Lowest during attempt | Reduction from baseline (%) |
| 1 | 183 | 175 | 4 |
| 2 | 175 | 83 | 53 |
| 3 | 156 | 138 | 12 |
| 4 | 185 | 181 | 2 |
| 5 | 154 | 144 | 6 |
| 6 | 52 | 50 | 4 |
| 7 | 157 | 116 | 26 |
| 8 | 126 | 110 | 13 |
| 9 | 77 | 70 | 9 |
Endotracheal intubation details of video recorded study participants
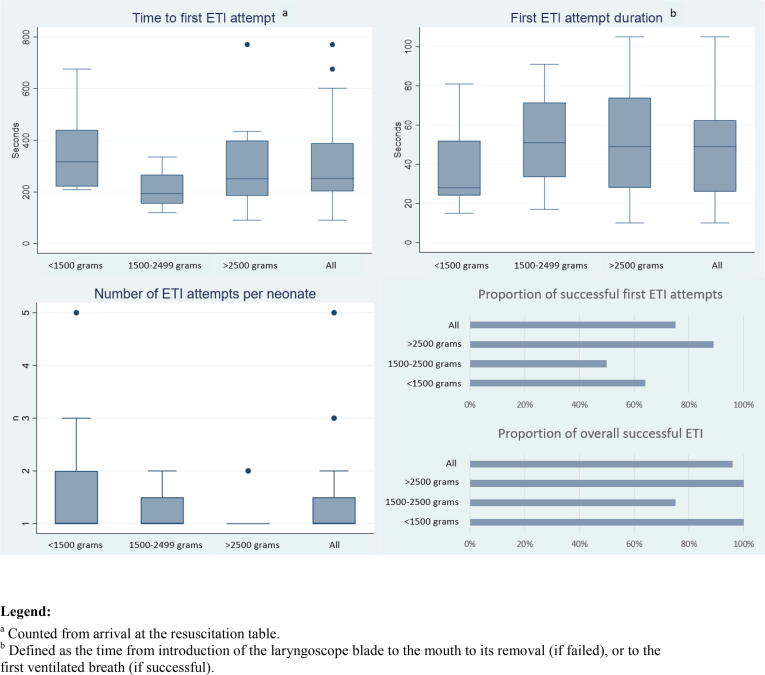
The postnatal time to the first ETI attempt ranged between 91 and 771 seconds (median = 252 seconds, IQR = 203–390 seconds; mean = 311 seconds, standard deviation = 174 seconds). The success rate for the first attempt was 75% (n = 18), and the maximum number of attempts was five. ETI failed in one neonate, but this neonate did not receive a real attempt to place an endotracheal tube, only a laryngoscope. A sensitivity analysis with this neonate removed showed no relevant changes to the results (Supplementary information 2). The initial ETI attempt durations ranged from 10 to 105 seconds (median = 49 seconds, IQR = 26–63; mean = 47 seconds, standard deviation = 26 seconds). Timings and success rates were stratified according to birth weight groups for the neonates that required ETI (Fig. 2 and Supplementary information 3).
Fig. 2.
Endotracheal intubation (ETI) details for the video recorded neonates (N = 24), arranged into birth weight categories (<1500 grams, n = 11; 1500–2499 grams, n = 4; >2500 grams, n = 9).
Clinical outcome
The clinical outcomes for all neonates (n = 75) are presented in Table 4. The mortality rate was 15% (n = 11), and 30% (n = 22) received a hypoxic-ischemic encephalopathy diagnosis (24 to 40 weeks gestation). No ETI-related complications (noxious autonomic reflex, local bleeding, vocal cord injury, tissue perforation, pneumothorax, subglottic stenos, post-extubation laryngeal edema and/or stridor) were observed.
Table 4.
Neurological outcome and clinical management (neurological, respiratory, admission duration and mortality) at NICU (N = 75).
| N (%)/median (IQR) | |
|---|---|
| Neurological outcome | |
| Apgar < 7 at 5 min | 44 (59) |
| pH < 7,00 or BE < −16 within one hour from birth a | 6 (10) |
| Hypoxic ischemic encephalopathy b,c | 22 (30) |
| Mild | 11 (15) |
| Moderate | 9 (12) |
| Severe | 2 (3) |
| Seizure c,d | 2 (3) |
| Intraventricular hemorrhage c | 6 (8) |
| Neurological managementc | |
| Anticonvulsant | 3 (4) |
| Cooling | 5 (7) |
| Respiratory managementc | |
| Surfactant | 13 (17) |
| O2 | 43 (57) |
| CPAP | 24 (32) |
| Mechanical ventilation e | 43 (57) |
| Mechanical ventilation duration (days) f | 4 (2–8) |
| Dischargec | |
| Duration of NICU admission (days) | 8 (4–29) |
| Mortality prior to discharge | 11 (15) |
Missing for 17 subjects.
Diagnosed according to Sarnat scoring system. 16 of these neonates had an apgar score < 7 at 5 min.
Missing for one subject.
EEG verified.
20 of these neonates received ETI during resuscitation at the delivery unit.
Missing for 5 subjects.
Discussion
In this study, 0.2% of neonates were intubated at birth. ETI was first attempted between 91 and 771 seconds (median 252 seconds; mean = 311 seconds), counted from the time that the neonate was placed on the resuscitation table. The initial ETI attempt durations ranged from 10 to 105 seconds (median 49 seconds; mean = 47 seconds) which means that most were outside the recommendations for best practice. The success rate of the first ETI attempt was 75%. Our study adds the perspective of ETI performance in a lower middle-income country under fast economic growth14.
Our findings are consistent with previous studies that have used video recordings to assess neonatal ETI during emergency conditions4, 9. An Australian study reported that the time to first ETI was between 86 and 699 seconds (mean 253 seconds, counted from birth), the success rate was 62% for all ETI attempts, and the duration ranged from 8 to 70 seconds per successful attempt. The duration range was not reported for the failed attempts but the mean duration was comparable in successful and combined successful/failed attempts (31and 33seconds)7. In accordance with this, an Irish study that included 203 patients and 455 ETI attempts, found a success rate of 44% for all ETI attempts and an attempt duration that ranged from 5 to 180 seconds. No statistically significant difference between successful and failed attempts was observed, and none of the recorded patient factors (including weight, gestational age, or several previous ETI attempts) were associated with success rates13. Similarly, an American study found that the mean ETI attempt duration for successful intubations was 27 seconds compared to 30 seconds for failed attempts, the difference was not statistically significant12. Finally, a study conducted in four neonatal units in the UK found that 52% of the initial ETI attempts in the delivery room were successful. The authors did not report on ETI duration11. All the above studies showed that greater clinical experience is associated with greater success rates and shorter duration of attempts7, 11, 12, 13. As neonatology junior doctors (i.e. lesser clinical experience) performed the ETIs for at least 22 of the 24 neonates, the successful intubation rate registered in our study should be considered high when compared to previous reports. However, we report a longer first ETI attempt mean duration than both the Australian and American studies7, 11, 12, 13. The reason for this might partly be because most ETI attempts were performed by neonatology junior doctors, and partly due to the lack of a working routine for timing the ETI attempts. The first ETI attempt median duration of 49 seconds, longer than the recommended standard of 30 seconds, together with other observations, such as the lack of a routine to confirm the endotracheal tube placement and the high chest compression rate, indicate the need for additional training. Nevertheless, intubation skills remain an important challenge for healthcare givers also in the delivery wards of high-income countries. A publication bias may exist, as we suspect that only high-performing hospitals dare to report real numbers. We recommend future studies with a larger sample size, analytical design, and multi-centered nature for valid evidence generation in the field. It is also important to conduct studies assessing the most effective training for achieving and maintaining ETI skills among caregivers involved in neonatal resuscitation. Finally, we should consider alternative devices for airway management at birth.
It is possible that using an artificial airway that requires less skill, such as the supraglottic airway, would lead to one or more of the following: a shorter time before the initial attempt to establish a patent artificial airway, a higher success rate, a shorter attempt duration22. The International Liaison Committee on Resuscitation (ILCOR) guidelines stated in 2020 that the supraglottic airway can be used as an alternative to ETI10. In the event of a global shift in clinical practice towards the use of supraglottic airway, the most benefit will likely be seen in low- and middle-income countries, where staff with the highly specialized skills necessary for ETI are often lacking23. To date, no approved supraglottic airways exist for neonates with a birth weight < 1,500 grams9, 10. We report a birth weight < 1,500 grams in 46% of the video recorded neonates who required ETI. Despite the small size and bearing in mind the descriptive nature of the study, our data suggest that low birth weight neonates may also have a higher number of attempts (up to five attempts for one neonate). An American retrospective chart review of resuscitated neonates with a birth weight < 1,000 grams showed the importance of fewer ETI attempts when they reported that death or neurodevelopmental impairment at 18 to 22 months of age occurred in 29% of neonates with a successful first ETI attempt, compared to 53% of neonates that required multiple attempts26. An Iranian study found that repeated ETI was a contributing factor to ETI-associated short-term complications including trauma to the larynx and vocal cords25. We did not find any ETI-associated complications in our study. In our study, 56% of neonates who received ETI and 59% of neonates who received FMV alone, subsequently required mechanical ventilation. The neonates that require an endotracheal tube for subsequent respiratory support, will likely benefit from placing this during less stressful conditions24.
We report a mortality rate of 15%, but we have not differentiated between the causes, nor have we reported on the stillbirth rate (Supplementary information 4). It is difficult to find comparative mortality rates among this neonatal subgroup, but a study conducted in rural Tanzania found an early mortality rate (≤7 days of life) of 23% among neonates that received PPV and subsequently were admitted to the neonatal unit25. A review that looked at the outcomes of 579 neonates (across 16 studies) who had received cardiopulmonary resuscitation for at least 10 minutes at birth (on the indications of bradycardia, asystole or pulseless electrical activity) found overall mortality at follow-up of 41%. Individual studies ranged from 2% to 100%, with a follow-up period that ranged from hospital discharge to 12 years of age26.
Finally, this study confirms remarkably low PPV and ETI incidences at birth in this setting (0.4% and 0.2%). This is consistent with data previously reported from the Phu San Hanoi Hospital by our research team (0.6% and 0.2%)6. The expected PPV incidence is 3–6% and ETI incidence is 1–2%8, 27. We have previously discussed some possible explanations for our findings, including a high c-section rate (over 50% of all births, approximately half of which are emergency c-sections) and few instrumental deliveries6. Nonetheless, it is truly difficult to interpret our findings. Future studies should focus on describing perinatal care in more detail to fully understand the clinical situation at the Phu San Hanoi Hospital, and to identify some possible key success factors.
Limitations
Phu San Hanoi Hospital may not mirror a typical lower middle-income country delivery room. However, this resource heterogeneity is a known phenomenon within developing countries29. Although our research team had previous experience in using video recording for data documentation during neonatal resuscitation28, it is possible that the resuscitating staff acted differently due to awareness of video cameras and the change in routine using NeoBeat. We tried to address this through information sessions and an induction period (approximately-one week) during which no video recordings were included in the study. The video recordings did not capture the events between birth and the moment that the neonate was placed on the resuscitation table. Meanwhile this affected (increased) the time to PPV initiation and first ETI attempt, the duration of the first ETI attempt, and the success status were unaffected. When defining failed ETI attempt duration, the time from laryngoscope blade removal to subsequent first ventilated breath (via face mask) was excluded. If prolonged, this time might have worsened the hypoxic state. We consider NeoTapAS to be a reliable assessment tool, but only one person (a senior pediatric trainee) reviewed the video recordings. This might have affected the more subjective variables, such as the depth of suctioning, the vigor of stimulation and, rarely, the differentiation between PPV interruption and slow ventilation rate. It is unlikely to have affected the objective timings of laryngoscope blade placement and removal, or the first ventilated breath through the endotracheal tube. One major limitation is that the endotracheal tube position was not confirmed with a chest X-ray. Considering the lack of CO2 devices, and a low rate of lung-auscultation post ETI placement, the success rate could be lower than what we report. However, based on the video recordings we have no reason to believe that any endotracheal tube was incorrectly positioned. Finally, the limited sample size precluded further investigations and subgroup comparisons.
Conclusions
In accordance with previous studies conducted in high-income countries, our findings from a lower middle-income country showed that ETI attempts were often unsuccessful during neonatal resuscitation in the delivery room, and their duration was frequently longer than best practice guidelines. Future studies should focus on assessing the most effective training for achieving and maintaining ETI skills among caregivers involved in neonatal resuscitation and could consider alternative devices for airway management at birth.
Authors' contributions
TD conceived and developed the study, coordinated the project, developed the case report forms, held information sessions, extracted data from video recordings, analysed the data and created the tables and illustrations, and wrote the manuscript.
HLN developed the study, developed the case report forms, held information sessions, and collected data from the study including patient charts.
HTN developed the study, developed the case report forms, held information sessions, and collected data from the study including patient charts.
XAB installed video cameras, managed technical issues, and collected video recordings.
PTTP conceived and developed the study, held information sessions, and managed the project and resources.
TN conceived and developed the study, held information sessions, communicated with ethical boards in Vietnam, and managed the project and resources.
DH programmed IT software to facilitate data transfer from NeoTapAS into STATA.
FC developed the study and was responsible for scientific validation.
DT conceived and developed the study, and was responsible for the acquisition of financial support, and scientific validation.
SMH conceived and developed the study, developed the case report forms, and was responsible for the supervision, acquisition of financial support, and scientific validation.
MB conceived the study and was responsible for the supervision, acquisition of financial support, and scientific validation.
LO conceived and developed the study, helped to develop the case report forms, held information sessions, installed video cameras, managed technical issues, managed the project and resources, communicated with ethical boards in Vietnam, supervised, and was responsible for scientific validation.
HV conceived and developed the study, held information sessions, managed the project and resources, and was responsible for supervision.
ADN was responsible for project management and resources, and the acquisition of financial support.
TA conceived and developed the study, and was responsible for the supervision, acquisition of financial support, and scientific validation.
NJ conceived and developed the study, and was responsible for the supervision, acquisition of financial support, and scientific validation.
All authors read and approved the final manuscript.
Funding
The above study is part of a larger project that has received a Swedish Research Council (Vetenskapsrådet, VR) grant (2018-02770). No funding or benefits were received from any commercial sectors for this study. The Swedish Research Council has no direct role in any technical or intellectual aspect of this work.
Ethical approvals
The study was approved by the Vietnamese Institutional Review Board in Human Research Dinh Tien Hoang Institute of Medicine (IRB-2002) on the 2020-03-26. The data analysis took place in Sweden and was approved by the Swedish Ethical Review Authority (Dnr 2021-00064) on the 2021-03-05.
Availability of data and materials
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the lack of its specification within the ethical application and approval.
Data collection tools
NeoTapAS: https://tap4life.org/neotapas-advances-support/.
RStudio: https://www.rstudio.com/.
NeoBeat: https://laerdal.com/se/products/technology/simulation-technology/neobeat/.
Acknowledgments
Acknowledgements
The authors thank the following individuals for their contributions. Hang T. T. Tran for the help to fill in the case report forms for the neonates that transferred from Phu San Hanoi Hospital to the Vietnam National Children’s Hospital. Tung Thanh Truong for technical support, extracting and cutting the video-recorded data; Phuong Phung and Phan Nguyen for inserting the hard copy data into RedCap.
Conflict of interests
The authors declare that they have no conflict of interest. SMH, NJP and TA are co-founders of the non-profit organization Tap4Life (www.tap4life.org), which produced the free-of-charge application NeoTapAS. The authors do not receive any salary from Tap4Life.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2022.100338.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Liu L., Oza S., Hogan D., Chu Y., Perin J., Zhu J., et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388:3027–3035. doi: 10.1016/S0140-6736(16)31593-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United Nation's Inter-agency Group for Child Mortality. Levels & Trends in Child Mortality 2019 [Available from: https://www.unicef.org/media/60561/file/UN-IGME-child-mortality-report-2019.pdf.
- 3.Målqvist M. Neonatal mortality: an invisible and marginalised trauma. Glob Health Action. 2011;4 doi: 10.3402/gha.v4i0.5724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trevisanuto D., Marchetto L., Arnolda G., Chien T.D., Lincetto O., Cavallin F., et al. Neonatal resuscitation in Vietnam: a national survey of a middle-income country. Acta Paediatr. 2015;104:e255–e262. doi: 10.1111/apa.12925. [DOI] [PubMed] [Google Scholar]
- 5.Ersdal H.L., Eilevstjønn J., Linde J.E., Yeconia A., Mduma E.R., Kidanto H., et al. Fresh stillborn and severely asphyxiated neonates share a common hypoxic-ischemic pathway. Int J Gynaecol Obstet. 2018;141:171–180. doi: 10.1002/ijgo.12430. [DOI] [PubMed] [Google Scholar]
- 6.Dempsey T.N., Nguyen H.L., Nguyen H.T., et al. Incidence of intrapartum-related events at the largest obstetric hospital in Hanoi, Vietnam: A retrospective study. Children. 2022;9 doi: 10.3390/children9030321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O'Donnell C.P., Kamlin C.O., Davis P.G., Morley C.J. Endotracheal intubation attempts during neonatal resuscitation: success rates, duration, and adverse effects. Pediatrics. 2006;117:e16–e21. doi: 10.1542/peds.2005-0901. [DOI] [PubMed] [Google Scholar]
- 8.Wyckoff M.H., Wyllie J., Aziz K., de Almeida M.F., Fabres J.W., Fawke J., et al. Neonatal life support 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020;156:A156–A187. doi: 10.1016/j.resuscitation.2020.09.015. [DOI] [PubMed] [Google Scholar]
- 9.Madar J., Roehr C.C., Ainsworth S., Ersdal H., Morley C., Rüdiger M., et al. European resuscitation council guidelines 2021: Newborn resuscitation and support of transition of infants at birth. Resuscitation. 2021;161:291–326. doi: 10.1016/j.resuscitation.2021.02.014. [DOI] [PubMed] [Google Scholar]
- 10.Aziz K., Lee H.C., Escobedo M.B., Hoover A.V., Kamath-Rayne B.D., Kapadia V.S., et al. Part 5: Neonatal resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S524–S550. doi: 10.1161/CIR.0000000000000902. [DOI] [PubMed] [Google Scholar]
- 11.Edwards G., Belkhatir K., Brunton A., Abernethy C., Conetta H., O'Shea J.E. Neonatal intubation success rates: four UK units. Arch Dis Child Fetal Neonatal Ed. 2020;105:684. doi: 10.1136/archdischild-2020-319111. [DOI] [PubMed] [Google Scholar]
- 12.Lane B., Finer N., Rich W. Duration of intubation attempts during neonatal resuscitation. J Pediatr. 2004;145:67–70. doi: 10.1016/j.jpeds.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 13.Haubner L.Y., Barry J.S., Johnston L.C., Soghier L., Tatum P.M., Kessler D., et al. Neonatal intubation performance: room for improvement in tertiary neonatal intensive care units. Resuscitation. 2013;84:1359–1364. doi: 10.1016/j.resuscitation.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 14.Bank TW. [Available from: https://www.worldbank.org/en/home.
- 15.Hampshire JFJWJMSARTRCNWJCVMALS. Newborn resuscitation and support of transition of infants at birth Guidelines.: Resuscitation Council UK.; 2021 [Available from: https://www.resus.org.uk/library/2021-resuscitation-guidelines/newborn-resuscitation-and-support-transition-infants-birth.
- 16.Team. R. RStudio: Integrated Development for R. RStudio, PBC, Boston, MA URL. 2021. [Available from: http://www.rstudio.com/.
- 17.Helldén D., Myrnerts Höök S., Pejovic N.J., McLellan D., Lubulwa C., Tylleskär T., et al. Neonatal resuscitation practices in Uganda: a video observational study. BMJ Paediatr Open. 2021;5:e001092. doi: 10.1136/bmjpo-2021-001092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.NeoBeat: Laerdal; [Available from: https://laerdal.com/se/products/technology/simulation-technology/neobeat/.
- 19.Mrelashvili A., Russ J.B., Ferriero D.M., Wusthoff C.J. The Sarnat score for neonatal encephalopathy: looking back and moving forward. Pediatr Res. 2020;88:824–825. doi: 10.1038/s41390-020-01143-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garcia K.K.S., Abrahão A.A. Research development using REDCap software. Healthc Inform Res. 2021;27:341–349. doi: 10.4258/hir.2021.27.4.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O'Donnell C.P., Kamlin C.O., Davis P.G., Morley C.J. Ethical and legal aspects of video recording neonatal resuscitation. Arch Dis Child Fetal Neonatal Ed. 2008;93:F82–F84. doi: 10.1136/adc.2007.118505. [DOI] [PubMed] [Google Scholar]
- 22.Wanous A.A., Wey A., Rudser K.D., Roberts K.D. Feasibility of laryngeal mask airway device placement in neonates. Neonatology. 2017;111:222–227. doi: 10.1159/000450691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bansal S.C., Caoci S., Dempsey E., Trevisanuto D., Roehr C.C. The laryngeal mask airway and its use in neonatal resuscitation: A critical review of where we are in 2017/2018. Neonatology. 2018;113:152–161. doi: 10.1159/000481979. [DOI] [PubMed] [Google Scholar]
- 24.Khatami S.F., Parvaresh P., Behjati S. Common complications of endotracheal intubation in newborns. Irananian J Neonatol. 2011;2:12–17. [Google Scholar]
- 25.Moshiro R., Perlman J.M., Kidanto H., Kvaløy J.T., Mdoe P., Ersdal H.L. Predictors of death including quality of positive pressure ventilation during newborn resuscitation and the relationship to outcome at seven days in a rural Tanzanian hospital. PLoS One. 2018;13:e0202641. doi: 10.1371/journal.pone.0202641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Foglia E.E., Weiner G., de Almeida M.F.B., Wyllie J., Wyckoff M.H., Rabi Y., et al. Duration of resuscitation at birth, mortality, and neurodevelopment: A systematic review. Pediatrics. 2020;146 doi: 10.1542/peds.2020-1449. [DOI] [PubMed] [Google Scholar]
- 27.Lee A.C., Cousens S., Wall S.N., Niermeyer S., Darmstadt G.L., Carlo W.A., et al. Neonatal resuscitation and immediate newborn assessment and stimulation for the prevention of neonatal deaths: a systematic review, meta-analysis and Delphi estimation of mortality effect. BMC Public Health. 2011;11:S12. doi: 10.1186/1471-2458-11-S3-S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pejovic N.J., Myrnerts Höök S., Byamugisha J., Alfvén T., Lubulwa C., Cavallin F., et al. A Randomized trial of laryngeal mask airway in neonatal resuscitation. N Engl J Med. 2020;383:2138–2147. doi: 10.1056/NEJMoa2005333. [DOI] [PubMed] [Google Scholar]
- 29.van Zyl C., Badenhorst M., Hanekom S., Heine M. Unravelling 'low-resource settings': a systematic scoping review with qualitative content analysis. BMJ Glob Health. 2021;6 doi: 10.1136/bmjgh-2021-005190. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the lack of its specification within the ethical application and approval.