Abstract
Patent foramen ovale (PFO) is implicated in the pathogenesis of a number of medical conditions but to date only one official position paper related to left circulation thromboembolism has been published. This interdisciplinary paper, prepared with the involvement of eight European scientific societies, reviews the available evidence and proposes a rationale for decision making for other PFO-related clinical conditions. In order to guarantee a strict evidence-based process, we used a modified grading of recommendations, assessment, development, and evaluation (GRADE) methodology. A critical qualitative and quantitative evaluation of diagnostic and therapeutic procedures was performed, including assessment of the risk/benefit ratio. The level of evidence and the strength of the position statements were weighed and graded according to predefined scales. Despite being based on limited and observational or low-certainty randomised data, a number of position statements were made to frame PFO management in different clinical settings, along with suggestions for new research avenues. This interdisciplinary position paper, recognising the low or very low certainty of existing evidence, provides the first approach to several PFO-related clinical scenarios beyond left circulation thromboembolism and strongly stresses the need for fresh high-quality evidence on these topics.
Introduction
Patent foramen ovale (PFO) is implicated in the pathogenesis of a number of medical conditions. However, the high prevalence of a PFO in the normal population (20-30%) implies that PFO can often be an incidental finding rather than a causative one. To help clinicians with decision making, the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Scientific Documents and Initiatives Committee invited eight European scientific societies and international experts to develop interdisciplinary position statements on the management of PFO, based on systematic assessments of the literature.
A previous position paper has been published addressing issues related to cryptogenic thromboembolism1,2. The present paper reports the approach to patients with PFO and decompression sickness, desaturation syndromes, migraine, and other clinical presentations.
Methods
To guarantee a strictly evidence-based process, position statements were developed using modified grading of recommendations assessment, development, and evaluation (GRADE) methodology (http://gdt.guidelinedevelopment.org/app/handbook/handbook.html), and by answering population-intervention-comparator-outcome (PICO) questions and non-PICO questions. A detailed review of the methodology employed can be found in Supplementary Appendix 1 and in an appendix of the previously published first part of this position paper1. Systematic reviews and statistical analysis were performed by a dedicated evidence synthesis team. A detailed insight and discussion of each section and the most important paragraphs can be found in Supplementary Appendix 2.
DECOMPRESSION SICKNESS
Decompression sickness (DCS) is a complex condition triggered by the trapping of gas emboli in vessels and tissues, which can result in a wide range of acute clinical scenarios, from mild to severe, with possible persistent disability or death. DCS occurs when a person moves from a higher pressure to a lower pressure area, such as a rapid ascent at high altitude or a rapid ascent from depth (compressed air work or diving).
A PFO can allow paradoxical embolisation of venous gaseous emboli (VGE) when there is a rise in right heart pressures due to pulmonary gas embolism or physical exercise; however, in large PFOs with spontaneous right-to-left (R-T-L) shunts, paradoxical VGE can also occur without other provocation3,4. Mild embolism may cause subclinical lesions, with still unknown late consequences5,6,7,8,9.
The risk of DCS from diving is difficult to estimate, but an incidence up to approximately 1.5% has been reported10. In divers, the association between PFO and DCS is supported by retrospective case-controlled epidemiological studies, mechanistic studies and association studies. In our meta-analysis of four correlation studies comparing the prevalence of R-T-L shunts in patients with and without DCS, we found an odds ratio (OR) of 5.63 (95% CI: 3.14-10.09) for R-T-L shunts in patients with DCS11,12,13,14 (Supplementary Figure 1).
The occurrence of altitude DCS is lower and is decreasing over time. High-altitude military pilots with long flights in a hypobaric environment (i.e., U2 plane pilots) may have short-term and long-term complications15,16,17 but there are no studies published about correlation with cardiac defects. Therefore, the role of PFO in individual cases of altitude DCS can remain elusive6,7,18,19.
IS IT CLINICALLY POSSIBLE TO ESTIMATE THE PROBABILITY OF A CAUSAL RELATIONSHIP BETWEEN A PFO AND DECOMPRESSION SICKNESS?
Determination of a causal role of PFO in DCS is difficult and should take into account that systematic and prospective evaluations of PFO-associated DCS are lacking; considerations can only be based on case reports, retrospective and mechanistic studies. Therefore, an individual assessment is mandatory. PFO-related DCS can produce earlier and more abundant VGE arterialisation but its role should be weighed against other individual factors that affect VGE production and trapping (dive/flight characteristics, physiological characteristics of tissues and factors that influence the threshold of “VGE tolerance”). Therefore, a technical analysis of the pre-decompression and decompression phase characteristics of each particular case is necessary20. In professional divers suffering from PFO-associated DCS, PFO size has been found to be a predictor of recurrence21,22. The main characteristics which can be considered are summarised in Supplementary Table 1, with position statements in Supplementary Table 2.
DIAGNOSTIC WORKUP
Patients with a history of DCS should have a thorough workup to identify factors that may have led to the occurrence of DCS. DCS has multiple and non-specific clinical manifestations (Supplementary Table 3)23; there are no imaging or laboratory test patterns which are unequivocal for DCS. Therefore, the diagnosis of DCS should be made by an experienced hyperbaric or aerospace physician according to the characteristics of the exposure, symptoms and the absence of other causes. VGE detected by echocardiography in patients with suspected DCS reinforces the diagnosis24.
High-resolution computerised tomography (CT) scanning and pulmonary function testing with bronchial provocation testing can exclude alveolar barotrauma but should not delay prompt recompression treatment of DCS.
When the diagnosis of DCS is unlikely, it may be unnecessary to begin secondary prevention workup even if a PFO is known to be present. In cases of DCS where no obvious risk factors for DCS can be identified or in activities with a high but non-modifiable risk of DCS, PFO screening should be considered part of the diagnostic workup.
PFO screening should be carried out at experienced sites, employing the previously published diagnostic approach1,2 to minimise false-negative tests, which could increase DCS risk during subsequent activities due to a false sense of security25,26.
When a clear, modifiable cause can be identified (e.g., diving outside acceptable decompression limits), or when more than two risk factors known to increase the risk for DCS are present (e.g., dehydration; heavy exercise at depth or at height; diving while cold near the end of the dive causing peripheral vasoconstriction; alcohol consumption), screening for PFO is not generally recommended27.
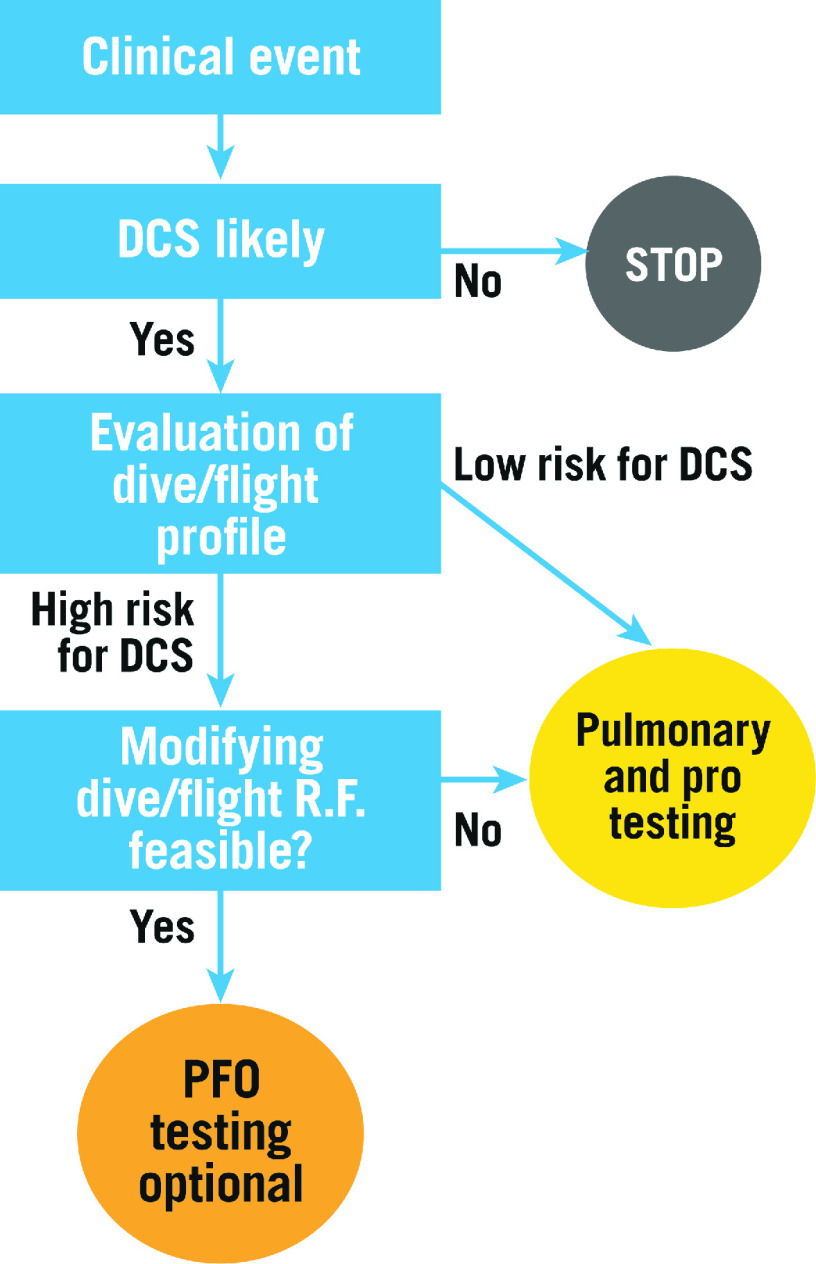
Figure 1 displays the recommended stepwise approach to DCS.
Figure 1.
Flow chart depicting strategy for investigation after DCS. R.F.: risk factors
SECONDARY PREVENTION
There are no published randomised studies comparing PFO closure to behavioural prevention of DCS. Moreover, limited observational evidence in divers is available and no data are available for aircrews. However, on any occasion, inhibiting the production of VGE has the potential to prevent further DCS, irrespective of the presence of a PFO28,29. This can be achieved by: a) modifying the individual’s lifestyle and personal physiologic characteristics (smoking and alcohol consumption, body weight, ensuring adequate hydration pre and post dive); b) avoiding those technical dive or flight factors that have caused abnormal VGE production; and c) reducing the inert gas saturation of tissues before decompression by breathing high concentrations of oxygen before the ascent (Supplementary Table 4).
Nonetheless, there are certain categories of aircrew or diver for whom performing conservative flights or dives is not a realistic option27,30. In these people, PFO closure may be proposed based on observational data suggesting that PFO closure is associated with reduced DCS incidence in divers5 and prevents arterialisation of VGE31,32,33. However, since recurrent DCS has also been observed after PFO closure in some studies, it should be remembered that diving may be a cause of DCS even without a PFO33,34,35. Current recommendations are that diving should be resumed only in the presence of a sealed PFO30,36. In the absence of complete closure post procedure, divers should not be allowed to return to “unrestricted” diving and should only make low-risk dives.
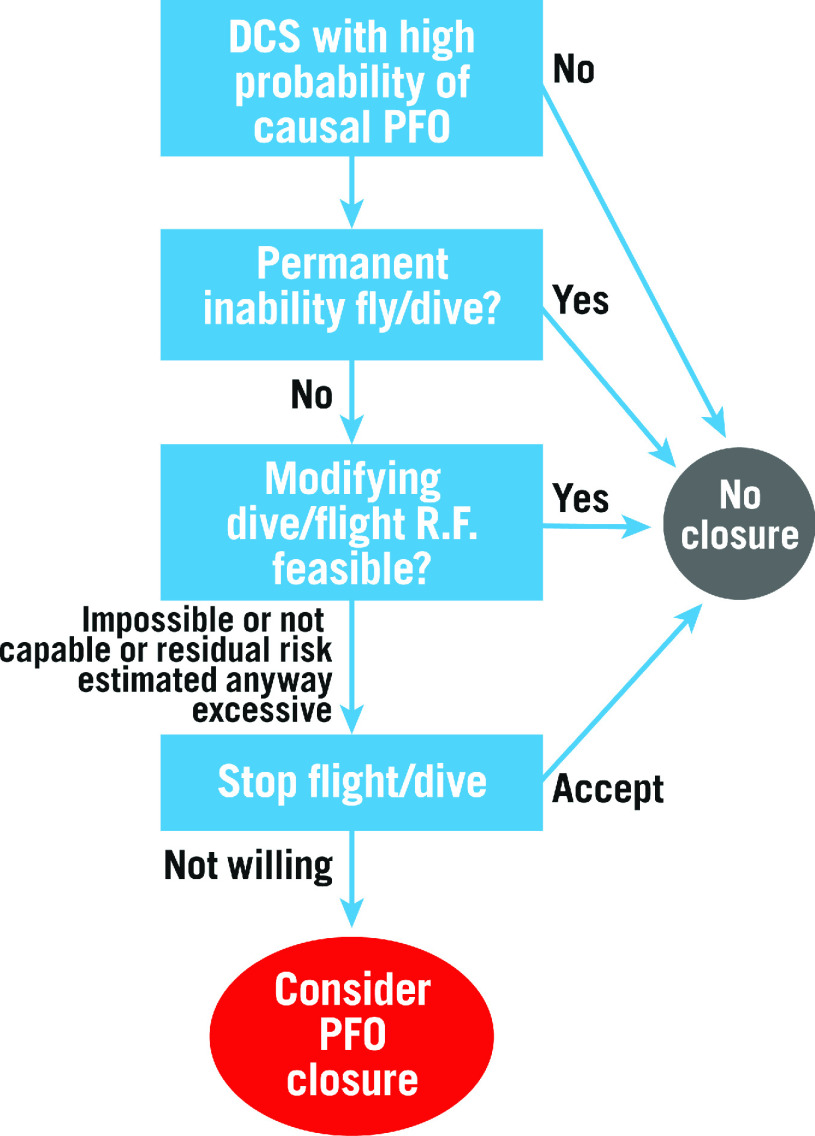
Figure 2 displays the treatment algorithm developed by this task force; Supplementary Table 2 displays the position statements.
Figure 2.
Flow chart for therapeutic decision making for DCS. R.F.: risk factors
IS A PRIMARY SCREENING OR PREVENTION ADVISED?
No evidence-based statements can be formulated regarding PFO closure as primary prevention of DCS.
General lifestyle and behavioural changes and technical procedure adherence are usually indicated in both divers and flying crews.
Based on the mismatch between the high prevalence of PFO and low incidence of DCS, it is suggested that primary screening for PFO should not be carried out on a routine basis in either divers or conventional altitude pilots30,36,37,38.
However, in professional divers, primary screening for PFO can be foreseen in accurately selected cases with high-risk work activity, in order to evaluate the possibility of a primary percutaneous closure. On the same basis, primary screening for PFO could be carried out in select military pilots performing intensive very high-altitude flight activities16,17. However, primary PFO closure in pilots should be weighed against the possibility of disqualification from flight activity.
When a PFO is an incidental finding in pilots or divers with no history of DCS, no restriction in conventional altitude flights is required, while recreational divers should be counselled by an experienced diving physician either to stop diving, or to undertake only low-risk profile dives. PFO closure indications should always be considered in conjunction with an experienced diving or aerospace physician.
PRACTICAL SUMMARY 1: DECOMPRESSION SICKNESS
WHAT TO DO
PFO screening in DCS cases with no obvious risk factors or with high but non-modifiable risk for DCS
After a DCS, primarily prevent bubbles with behavioural and technical (B&T) changes
If B&T changes are not possible or not effective, PFO closure can be proposed with shared decision making underscoring the lack of evidence
Resume unrestricted activity only after confirmed PFO sealing post intervention
WHAT NOT TO DO
Primary PFO screening
Deny conventional flight or diving after incidental finding of PFO
High-risk recreational dives after incidental finding of PFO
Propose PFO closure if B&T changes can be made and are effective
MIGRAINE
Migraine is a common disorder which affects approximately 12% of the general population (4-9% of men and 15-17% of women between 20 and 64 years of age39) and is often disabling40. It is estimated that 1-4% of the population meet the criteria for chronic migraine41,42. In the general population, it is estimated that the prevalence of migraine with aura ranges from 1 to 4% in men and 3 to 10% in women43.
Position statements are summarised in Supplementary Table 5.
IS PFO ASSOCIATED WITH MIGRAINE? WHAT ARE THE UNDERLYING MECHANISMS?
The association between PFO and migraine has been suggested by a higher prevalence of PFO in those with migraine, especially among those with aura, than in the general population44,45,46,47,48,49,50,51 and by the finding of incidental improvement in migraine in patients who have undergone percutaneous closure of the PFO for other reasons52,53. Moreover, the high prevalence of migraine attacks in some disorders wherein atrial or pulmonary shunts exist54,55 would suggest a pathogenic role of R-T-L shunts.
However, the association between migraine and PFOs varies considerably across heterogeneous populations46,56,57,58,59,60.
The most plausible electrophysiological substrate of headaches and aura symptoms is cortical spreading depression (CSD)61,62 which, in this case, would be triggered by paradoxical cerebral thromboemboli45,47,49,61,63,64,65,66,67 and/or the direct passage of metabolites into the systemic circulation, also possibly caused by the release of active metabolites from platelets activated by shear stress in the PFO, resulting in irritation of the trigeminal nerve and the brain’s vascular network67,68.
IS IT CLINICALLY POSSIBLE TO ESTIMATE THE PROBABILITY OF A CAUSAL RELATIONSHIP BETWEEN A PFO AND MIGRAINE?
In some retrospective and prospective observational studies, a higher prevalence of an atrial septal aneurysm (ASA)69 and larger PFO sizes in subjects with migraine with aura has been reported60,70. Also, the number of bubbles crossing the PFO, as detected by contrast transcranial Doppler (cTCD), has been found to correlate with the severity and frequency of attacks among migraineurs with aura in other studies45,56. However, the results of other studies do not support an association between the frequency of migraine attacks and PFO characteristics56,57,58.
In patients with previous stroke, an association between PFO and migraine has been reported47, and percutaneous closure has been shown to be more effective at reducing the frequency and severity of migraine attacks than in patients without cerebrovascular disease71,72.
Older age seems to be associated with an absence of any relationship between PFO and migraine59,60.
TREATMENT
To date, three randomised studies73,74,75 and three meta-analyses72,76,77 have addressed the issue of percutaneous closure as therapy for migraine. We performed an updated meta-analysis of randomised and observational studies to support the position statements in this document.
Observational studies yielded a statistically significant improvement in migraine, albeit with marked inconsistency between studies, whereas individual randomised clinical trials (RCTs) and their meta-analyses failed to demonstrate any statistically significant difference in primary outcomes, responder rates or complete migraine resolution. On the other hand, a meta-analysis of secondary endpoints revealed a statistically significant reduction in migraine attack frequency and duration. Also, subgroups of patients with aura and patients with cerebrovascular disease experienced statistically significant improvement in migraine with PFO closure, when compared to medical therapy (Supplementary Figure 2-Supplementary Figure 4).
One thing to be considered is that, according to GRADE methodology, the certainty of effects was judged severely, implying that a number of limitations need to be addressed in future studies (Supplementary Table 6). Moreover, it is possible that the neutral primary results of PFO closure studies may be due to the inclusion of patients without a causative PFO2. Additionally, the choice of migraine study endpoints is problematic, being largely arbitrary78. Therefore, further RCTs are necessary to obtain satisfactory certitude of effects.
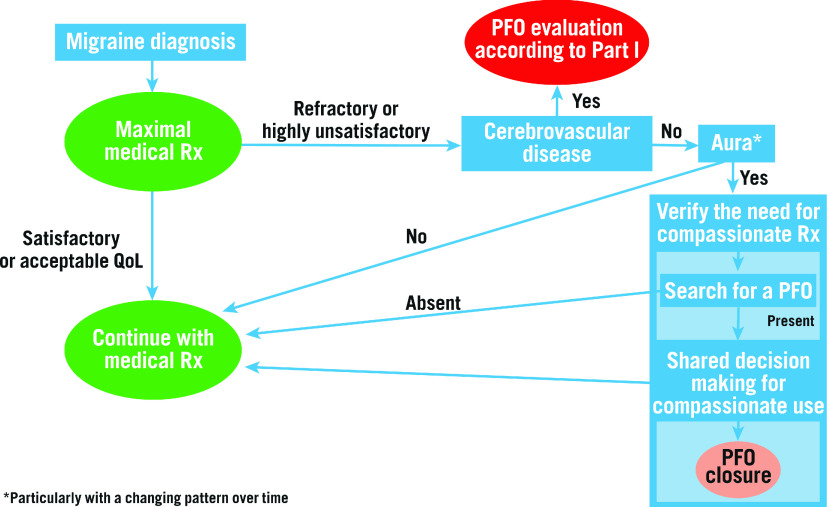
Supplementary Table 7 shows the GRADE table for the treatment of migraine and Figure 3 summarises the proposed treatment algorithm, according to the statements.
Figure 3.
Algorithm for the management of PFO-associated migraine. Rx: therapy
Detailed answers to the PICO question and the detailed characteristics of the considered studies are displayed in Supplementary Table 8 and Supplementary Table 9.
PRACTICAL SUMMARY 2: MIGRAINE
WHAT TO DO
Treat migraine with conventional therapies
Consider PFO closure only in clinical trials or for compassionate use in migraine with aura
WHAT NOT TO DO
Consider PFO closure as part of a routine treatment algorithm
ARTERIAL DEOXYGENATION SYNDROMES
Arterial hypoxaemia is a decrease in the content of oxygen in the blood (SaO2 or SpO2 <90% or PaO2 <60 mmHg), with or without cyanosis. Its main symptoms are exertional and/or resting dyspnoea.
PFO has been associated with several arterial deoxygenation syndromes. Up to 30% of patients with a PFO were discovered to have clinically significant arterial deoxygenation during effort in one study79. To date, only a few studies have been published on this topic. These are summarised in Supplementary Table 10.
CAN PFO BE ASSOCIATED WITH ARTERIAL HYPOXAEMIA? WHAT ARE THE UNDERLYING MECHANISMS?
Several case reports and some experimental and clinical studies have demonstrated that a shunt through a PFO has the potential to cause arterial deoxygenation by mixing venous and arterial blood. In most cases, the PFO shunt only aggravates pre-existing causes of hypoxaemia.
All the causes that elevate pressure in the right heart chambers, such as pulmonary hypertension, can also increase minor shunts. However, several anatomical conditions may also cause a significant shunt, even in the presence of normal mean right atrial pressure (Supplementary Table 10).
DIAGNOSTIC WORKUP
Prior to considering a PFO, an in-depth interdisciplinary diagnostic workup, specific for each clinical syndrome, should be performed to assess the contribution of different potential causes of hypoxaemia, and the pre-test probability of a PFO role in each syndrome should be considered (Supplementary Table 10). The evaluation should be performed and discussed at least by a cardiologist and a pulmonologist.
Every situation in which the baseline condition does not fully explain symptoms and/or the hypoxaemia indicates a need to consider assessing a possible contribution of the PFO.
The diagnostic workup for PFO was published in the first part of this paper1.
In the infrequent case of platypnoea-orthodeoxia syndrome (POS), the most common cause is a PFO80; however, other cardiac and non-cardiac conditions should be ruled out with appropriate tests. A bubble test should be obtained during cardiac imaging with the patient in both a supine and an upright position. The presence of a persistent prominent Eustachian valve may lead to diversion of blood flow from the inferior vena cava towards a PFO. This effect could be exacerbated by atrial deformities and may also lead to a false-negative result during contrast-enhanced transthoracic echocardiography (c-TTE) or contrast transoesophageal echocardiography (c-TOE) via the antecubital vein. A femoral vein contrast injection may be considered in case of high suspicion for POS, prominent Eustachian valve and negative contrast exams.
In obstructive sleep apnoea syndrome (OSAS), it is important to assess the number and severity of episodes of desaturation on therapy to evaluate the possible role of PFO in clinical findings.
Exercise hypoxaemia is significant when there is an SaO2 or SpO2 drop ≥8% from baseline, or to a level <90%.
In all syndromes, a lower-than-expected or absent increase in SaO2 or SpO2 with FiO2 1.0 suggests a significant intracardiac shunt.
Whenever possible, an invasive evaluation of pulmonary pressure to rule out severe pulmonary hypertension and SaO2 measurements (in the left atrium and each pulmonary vein) should be performed to document a step-down in SaO2 while excluding pulmonary abnormalities (pulmonary embolism or intrapulmonary shunts). Moreover, during catheterisation, an occlusion test can demonstrate increased systemic saturation.
IS IT CLINICALLY POSSIBLE TO ESTIMATE THE PROBABILITY OF A CAUSAL RELATIONSHIP BETWEEN A PFO AND HYPOXAEMIA?
Evaluating the role of a PFO in hypoxaemia is difficult and should encompass all the patient’s clinical, imaging and functional data.
In the few available observational studies that have been published, larger and more durably open PFO were the characteristics which correlated more frequently with hypoxaemia in different clinical syndromes.
Invasive measurement of intracardiac arterial oxygen saturation is a key tool for decision making. However, one must consider interference of the catheter in PFO shunting, as well as the difficulty of extrapolating the clinical impact of lab measurements in syndromes in which the opening of a PFO is intermittent.
TREATMENT
Treatment is based on severity of symptoms and the pathogenic role of PFO on shunting. Patients with chronic severe pulmonary hypertension should be excluded from interventional treatment.
No randomised trials have been performed addressing percutaneous closure of PFO in desaturation syndromes.
We performed a meta-analysis of observational before and after closure studies which reported SaO2 or SpO2 for two disparate hypoxaemia syndromes – POS and exertional desaturation. We found a statistically significant increase in SaO2 or SpO2 in both clinical conditions after PFO closure: in exercise desaturation 9.8% (95% CI: 7.1-12.5%) with a severe heterogeneity among studies (I2]: 79%) and in POS 9.6% (95% CI: 5.7-13.5%) also with a severe heterogeneity among studies (I2]: 82%) (Supplementary Figure 5).
In POS due to PFO and OSAS, the evidence for percutaneous closure is based on case reports, case series and small registries. The studies on POS revealed stable relief of symptoms up to five years with improved standing arterial oxygen saturation in all patients who did not have other dominating causes of hypoxaemia81,82,83,84,85. In OSAS, one case-control observational study on 40 patients showed a statistically significant improvement in left ventricular diastolic function, in indices of apnoea and desaturation episodes and a reduction in systemic arterial pressure86.
Only preliminary reports with good results are available for exertional desaturation and high-altitude pulmonary oedema (HAPO), whereas no data are available regarding PFO closure in chronic obstructive pulmonary disease (COPD) patients.
Taken together, these data show that percutaneous closure of PFO has the potential to impact on arterial oxygen saturation and improve symptoms in select patients with an arterial hypoxaemia syndrome. Randomised studies are required to demonstrate effectiveness and safety in these contexts. Position statements are listed in Supplementary Table 11.
PRACTICAL SUMMARY 3: ARTERIAL DEOXYGENATION SYNDROMES
WHAT TO DO
Individually assess and weigh the role of all factors involved in the desaturation syndrome
Whenever possible obtain invasive evidence of the PFO role
Where appropriate, propose PFO closure with shared decision making underscoring the lack of evidence
WHAT NOT TO DO
Routinely close PFO
Close a PFO in the presence of severe chronic pulmonary hypertension
Close a PFO without clear evidence of a crucial role in desaturation
SELECT HIGH-RISK CLINICAL CONDITIONS
PREGNANCY, DELIVERY AND THE PUERPERIUM
Pregnant women are at an increased risk of ischaemic and haemorrhagic stroke and venous thromboembolism compared to non-pregnant women, and PFO-related strokes do happen during pregnancy and the puerperium87,88. However, to date, no large studies have addressed the question of whether PFO is a risk factor for stroke and systemic thrombotic embolisation under such conditions. Specific characteristics of PFO-associated stroke seem to emerge from an analysis of the available reports, but the evidence consists mainly of small case series, so no conclusions can be drawn87. Moreover, no studies have been published testing different preventive approaches for PFO-related stroke. Relevant position statements are listed in Supplementary Table 12.
PREOPERATIVE EVALUATION IN NON-CARDIAC SURGERY
Perioperative stroke, with an incidence ranging from 0.2% to 9.7%, is a serious complication of surgical procedures, with significant consequences in terms of morbidity, duration of hospitalisation and mortality89,90,91.
The incidence of PFO-related stroke during and after surgery and anaesthesia may potentially be increased by haemodynamic changes, hypercoagulability, and the formation of venous thrombosis.
A recent large retrospective study involving 150,198 adult patients who underwent non-cardiac surgery and were extubated after the operation showed a statistically significant increased risk of perioperative ischaemic stroke in patients with a PFO (3.5% vs 0.5%)92. The incidence of stroke in patients with PFO was more significantly increased in otherwise low-risk stroke patients. Moreover, PFO was associated with larger strokes and with more severe neurological deficits and was linked to an increased risk of other systemic embolic complications.
However, there are neither prospective studies addressing these issues, nor RCTs assessing the effectiveness of pharmacotherapy or interventional procedures at decreasing risk.
Relevant position statements are listed in Supplementary Table 12.
NEUROSURGERY IN THE SITTING POSITION
During neurosurgery, after venous incision, a venous air embolism with severe immediate or delayed cardiopulmonary and cerebral complications can potentially occur93,94,95,96,97,98. This occurs more frequently when patients are in a sitting position (up to 50-79% of cases). Adoption of this position has declined considerably99,100,101, also because of other complications102. Notwithstanding this, many surgical teams still place patients in a sitting position as a first choice to approach posterior fossa or dorsally located parietal lesions93,103,104, because of the position’s advantages for surgeons105,106,107,108,109,110,111. In patients with PFO, this results in paradoxical air embolism in up to 14% of the cases112,113,114,115. For this reason, a prone position is usually considered mandatory in safety data116,117. However, paradoxical air embolism can also happen when the patient is prone93.
Diagnostic workup
The diagnostic workup to detect a PFO is described in part I of this document1,2.
Prevention and treatment
Position statements are summarised in Supplementary Table 13.
PERIOPERATIVE MONITORING
During the procedure, patients can be monitored using transoesophageal echocardiography (TOE) and/or transcranial Doppler (TCD). Additionally, end tidal CO2 detects clinically significant venous air emboli118,119. Capnography is a readily available diagnostic tool, with moderate sensitivity and specificity for diagnosing air emboli. An alternative method is to measure expired nitrogen120.
PFO CLOSURE
Since perioperative monitoring can make a timely diagnosis but cannot stop ongoing embolism, preoperative PFO closure has been proposed and presented in extremely limited preliminary reports with good results for the ensuing neurosurgical operation in the sitting position93,121,122.
However, to date, no clinical studies have been published, and questions about the timing of surgery post intervention remain unanswered, especially regarding effective sealing of the defect, the endothelialisation of the device, and the duration of antiplatelet therapy123.
Limitations
This position paper must not be read as a guideline. Indeed, when approaching the statements of this document, one should consider that the included conditions are often uncommon, their pathophysiology still incompletely known, and high-quality data regarding their management are still lacking. The ensuing result is an amount of sparse data with low or very low certainty of evidence. This, of course, has made it impossible to express conclusive focused indications but – since the patients suffering from these syndromes need treatment – has stimulated scientific societies to come together to express shared position statements in order to help approach these conditions rationally according to the available literature.
Conclusion
PFO comes into play in several pathogenic conditions, interacting with other causative processes in disparate dynamic networks. As a result, the heterogeneity of patients is high and evidence, where available, is weak. Therefore, therapeutic solutions often remain empiric, and will probably remain so for a long time due to the low number of patients with similar characteristics, which precludes adequately powered studies. Therefore, beyond the guidelines paradigm which cannot be applied in this context at the moment, this interdisciplinary position paper, based on a comprehensive and strict evaluation of the available data, may be useful for physicians to follow as a broad clinical approach. Nonetheless, based on the published research, we strongly underscore the need for new observational and randomised studies in order to allow the expression of conclusive indications for these poorly focused, and yet clinically relevant, syndromes.
Guest editor
This paper was guest edited by Franz-Josef Neumann, MD; Department of Cardiology and Angiology II, University Heart Center Freiburg - Bad Krozingen, Bad Krozingen, Germany.
Supplementary data
. Methods.
. Detailed evaluation of specific issues.
. Meta-analysis of studies comparing the prevalence of R-T-L shunting in patients with and without DCS.
. Meta-analysis of observational and randomised trials regarding the incidence of persistent migraine comparing closure versus non-closure of PFO in studies with two cohorts.
. Meta-analysis of observational and randomised trials regarding the incidence of persistent migraine comparing closure versus non-closure of PFO in studies with two cohorts, by aura status.
. Meta-analysis of observational trials assessing persistence of migraine before and after PFO closure, by aura status.
. Meta-analysis of studies on PFO closure in desaturation syndromes. Improvement in blood oxygen saturation after PFO closure.
. PRISMA diagram of decompression sickness studies in recreational divers.
. PRISMA diagram of decompression sickness studies in professional divers.
. PRISMA diagram of decompression sickness studies in desaturation syndromes.
. PRISMA diagram of migraine studies.
. Characteristics for the evaluation of a probable causal link between a PFO and DCS.
. Summary of statements on DCS and PFO.
. Classification of DCS.
. Primary measures for secondary prevention of DCS.
. Summary of statements on migraine and PFO.
. GRADE evaluation of certitude of effects- studies on PFO closure for migraine prevention.
. Summary of PICO question on migraine treatment.
. Detailed PICO question for therapy of migraine.
. Characteristics of the studies on PFO closure for migraine.
. Diseases in which PFO can contribute to arterial hypoxaemia and its clinical consequences.
. Summary of statements on arterial deoxygenation and PFO.
. Position statements on pregnancy and the pre-operative management of patients.
. Position statements on neurosurgery in the sitting position.
. GRADE evaluation of certitude of effects - DCS.
. Studies on DCS in recreational divers.
. Studies on DCS in professional divers.
. GRADE evaluation of certitude of effects - desaturation syndromes.
Acknowledgments
Conflict of interest statement
R. Byrne reports personal fees from B. Braun Melsungen AG and from Biotronik, and grants from CeloNova Biosciences, outside the submitted work. B. Dalvi reports other financial activities from Abbott, outside the submitted work. D. Dudek reports grants and personal fees from Abbott, outside the submitted work. D. Hildick-Smith reports personal fees from Abbott, Gore, Occlutech, and Holistick, outside the submitted work. S.E. Kasner reports grants from W.L. Gore, during the conduct of the study, personal fees from Bristol-Myers Squibb and from Boehringer Ingelheim, and grants and personal fees from Medtronic and Bayer, outside the submitted work. J.L. Mas reports personal fees from Abbott, during the conduct of the study. B. Meier reports personal fees from Abbott, outside the submitted work. E.M. Onorato reports personal fees from Occlutech, outside the submitted work. P. Scacciatella reports grants from Abbott Medical and Gore Medical, outside the submitted work. H. Sievert reports reimbursement for clinical trials from 4tech Cardio, Abbott, Ablative Solutions, Ancora Heart, Append Medical, Axon, Bavaria Medizin Technologie GmbH, Bioventrix, Boston Scientific, Carag, Cardiac Dimensions, Cardiac Success, Cardimed, CeloNova, Comed B.V., Contego, CVRx, Dinova, Edwards, Endologix, Endomatic, Hemoteq, Hangzhou Nuomao Medtech, Holistick Medical, K2, Lifetech, Maquet Getinge Group, Medtronic, Mokita, Occlutech, Recor, Renal Guard, Terumo, Trisol, Vascular Dynamics, Vectorious Medtech, Venus, Venock, and Vivasure Medical, outside the submitted work. G. Tarantini reports personal fees from Abbott and Vascular Innovations, during the conduct of the study. J. Thomson reports personal fees from Gore Medical, outside the submitted work. T. Toni reports personal fees from Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Medtronic, and Pfizer, outside the submitted work. The chairman of the Task Force and all the other authors declare no conflicts of interest for this work. The Guest Editor has no conflicts of interest to declare.
Abbreviations
- B&T
behavioural and technical
- c-TCD
contrast-enhanced transcranial Doppler
- c-TOE
contrast transoesophageal echocardiography
- c-TTE
contrast-enhanced transthoracic echocardiography
- CO2
carbon dioxide
- COPD
chronic obstructive pulmonary disease
- CSD
cortical spreading depression
- CT
computerised tomography
- DCS
decompression sickness
- EAPCI
European Association of Percutaneous Cardiovascular Interventions
- FiO2
fraction of inspired oxygen
- GRADE
grading of recommendations assessment, development, and evaluation
- HAPO
high-altitude pulmonary oedema
- MRI
magnetic resonance imaging
- NYHA
New York Heart Association
- OSAS
obstructive sleep apnoea syndrome
- PaO2
partial pressure of oxygen in the blood
- PFO
patent foramen ovale
- PICO
population-intervention-comparator-outcome
- POS
platypnoea-orthodeoxia syndrome
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- R-T-L
right-to-left
- RCT(s)
randomised clinical trial(s)
- SaO2
oxygen haemoglobin saturation
- SMD
standardised mean difference
- SpO2
peripheral capillary oxygen saturation
- TCD
transcranial Doppler
- TOE
transoesophageal echocardiography
- VGE
venous gaseous emboli
Contributor Information
Christian Pristipino, S. Filippo Neri Hospital ASL Roma 1, Rome, Italy.
Peter Germonpré, Military Hospital, Brussels, Belgium.
Danilo Toni, Hospital Policlinico Umberto I, Sapienza University, Rome, Italy.
Horst Sievert, CardioVascular Center Frankfurt (CVC Frankfurt), Frankfurt, Germany; Anglia Ruskin University, Chelmsford, United Kingdom; University California San Francisco (UCSF), San Francisco, CA, USA.
Bernhard Meier, University Hospital, Bern, Switzerland.
Fabrizio D'Ascenzo, Città della Salute e della Scienza Hospital, University of Turin, Turin, Italy.
Sergio Berti, Heart Hospital, Massa, Italy.
Eustaquio Onorato, Centro Cardiologico Monzino, IRCCS, Milan, Italy.
Francesco Bedogni, IRCCS Policlinico San Donato, San Donato Milanese, Milan, Italy.
Jean-Louis Mas, Hôpital Sainte-Anne, Université Paris Descartes, Paris, France.
Paolo Scacciatella, U. Parini Hospital, Aosta, Italy.
David Hildick-Smith, Sussex Cardiac Centre, Brighton and Sussex University Hospitals, Brighton, United Kingdom.
Fiorenzo Gaita, Città della Salute e della Scienza Hospital, University of Turin, Turin, Italy.
Paul Kyrle, Medical University, Vienna, Austria.
John Thomson, Leeds General Infirmary, Leeds, United Kingdom.
Geneviève Derumeaux, Hôpital Henri Mondor, Faculté de Médecine de Créteil, Créteil, France.
Dirk Sibbing, Privatklinik Lauterbacher Mühle am Ostersee, Iffeldorf and Ludwig-Maximilians-Universität (LMU) München, Munich, Germany.
Massimo Chessa, IRCCS Policlinico San Donato, San Donato Milanese, Milan, Italy.
Marius Hornung, CardioVascular Center Frankfurt (CVC Frankfurt), Frankfurt, Germany.
Jose Zamorano, University Hospital Ramón y Cajal, Madrid, Spain.
Dariusz Dudek, Jagiellonian University Medical College, Krakow, Poland; Maria Cecilia Hospital, GVM Care & Research, Cotignola (RA), Italy.
References
- Pristipino C, Sievert H, D’Ascenzo F, Mas JL, Meier B, Scacciatella P, Hildick-Smith D, Gaita F, Toni D, Kyrle P, Thomson J, Derumeaux G, Onorato E, Sibbing D, Germonpre P, Berti S, Chessa M, Bedogni F, Dudek D, Hornung M, Zamorano J Joint Task Force of the European Association of Percutaneous Cardiovascular Interventions (EAPCI), European Stroke Organisation (ESO), European Heart Rhythm Association (EHRA), European Association for Cardiovascular Imaging (EACVI), Association for European Paediatric and Congenital Cardiology (AEPC), ESC Working group on GUCH, ESC Working group on Thrombosis, European Haematological Society (EHA), European Underwater and Baromedical Society (EUBS) European position paper on the management of patients with patent foramen ovale. General approach and left circulation thromboembolism. EuroIntervention. 2019;14:1389–402. doi: 10.4244/EIJ-D-18-00622. [DOI] [PubMed] [Google Scholar]
- Pristipino C, Sievert H, D’Ascenzo F, Louis Mas J, Meier B, Scacciatella P, Hildick-Smith D, Gaita F, Toni D, Kyrle P, Thomson J, Derumeaux G, Onorato E, Sibbing D, Germonpre P, Berti S, Chessa M, Bedogni F, Dudek D, Hornung M, Zamorano J International Experts. European position paper on the management of patients with patent foramen ovale. General approach and left circulation thromboembolism. Eur Heart J. 2019;40:3182–95. doi: 10.1093/eurheartj/ehy649. [DOI] [PubMed] [Google Scholar]
- Wilmshurst PT. The role of persistent foramen ovale and other shunts in decompression illness. Diving Hyperb Med. 2015;45:98–104. [PubMed] [Google Scholar]
- Cambier BA, Missault LH, Kockx MM, Vandenbogaerde JF, Alexander JP, Taeymans YM, Van Cauwelaert PA, Brutsaert DL. Influence of the breathing mode on the time course and amplitude of the cyclic inter-atrial pressure reversal in postoperative coronary bypass surgery patients. Eur Heart J. 1993;14:920–4. doi: 10.1093/eurheartj/14.7.920. [DOI] [PubMed] [Google Scholar]
- Billinger M, Zbinden R, Mordasini R, Windecker S, Schwerzmann M, Meier B, Seiler C. Patent foramen ovale closure in recreational divers: effect on decompression illness and ischaemic brain lesions during long-term follow-up. Heart. 2011;97:1932–7. doi: 10.1136/heartjnl-2011-300436. [DOI] [PubMed] [Google Scholar]
- McGuire S, Sherman P, Profenna L, Grogan P, Sladky J, Brown A, Robinson A, Rowland L, Hong E, Patel B, Tate D, Kawano ES, Fox P, Kochunov P. White matter hyperintensities on MRI in high-altitude U-2 pilots. Neurology. 2013;81:729–35. doi: 10.1212/WNL.0b013e3182a1ab12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire SA, Sherman PM, Wijtenburg SA, Rowland LM, Grogan PM, Sladky JH, Robinson AY, Kochunov PV. White matter hyperintensities and hypobaric exposure. Ann Neurol. 2014;76:719–26. doi: 10.1002/ana.24264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erdem I, Yildiz S, Uzun G, Sonmez G, Senol MG, Mutluoglu M, Mutlu H, Oner B. Cerebral white-matter lesions in asymptomatic military divers. Aviat Space Environ Med. 2009;80:2–4. doi: 10.3357/ASEM.2234.2009. [DOI] [PubMed] [Google Scholar]
- Gempp E, Sbardella F, Stephant E, Constantin P, De Maistre S, Louge P, Blatteau JE. Brain MRI signal abnormalities and right-to-left shunting in asymptomatic military divers. Aviat Space Environ Med. 2010;81:1008–12. doi: 10.3357/ASEM.2786.2010. [DOI] [PubMed] [Google Scholar]
- Balestra C. Dive Computer Use in Recreational Diving: Insights from the DAN-DSL Database. In: Blogg SL, Lang MA, Møllerløkken A, editors. Proc. Valid. Dive Comput. Work., Gdansk, Poland. Trondheim, Norway: Akademika Publishing; 2012. pp. 99–102. [Google Scholar]
- Cantais E, Louge P, Suppini A, Foster PP, Palmier B. Right-to -left shunt and risk of decompression illness with cochleovestibular and cerebral symptoms in divers: case control study in 101 consecutive dive accidents. Crit Care Med. 2003;31:84–8. doi: 10.1097/00003246-200301000-00013. [DOI] [PubMed] [Google Scholar]
- Germonpre P, Dendale P, Unger P, Balestra C. Patent foramen ovale and decompression sickness in sports divers. J Appl Physiol. 1998;84:1622–6. doi: 10.1152/jappl.1998.84.5.1622. [DOI] [PubMed] [Google Scholar]
- Moon RE, Camporesi EM, Kisslo JA. Patent foramen ovale and decompression sickness in divers. Lancet. 1989;1:513–4. doi: 10.1016/S0140-6736(89)90064-0. [DOI] [PubMed] [Google Scholar]
- Wilmshurst PT, Pearson MJ, Walsh KP, Morrison WL, Bryson P. Relationship between right-to-left shunts and cutaneous decompression illness. Clin Sci. 2001;100:539–42. doi: 10.1042/cs1000539. [DOI] [PubMed] [Google Scholar]
- Bendrick GA, Ainscough MJ, Pilmanis AA, Bisson RU. Prevalence of decompression sickness among U-2 pilots. Aviat Space Environ Med. 1996;67:199–206. [PubMed] [Google Scholar]
- Hundemer GL, Jersey SL, Stuart RP, Butler WP, Pilmanis AA. Altitude decompression sickness incidence among U-2 pilots: 1994-2010. Aviat Space Environ Med. 2012;83:968–74. doi: 10.3357/ASEM.3201.2012. [DOI] [PubMed] [Google Scholar]
- Jersey SL, Hundemer GL, Stuart RP, West KN, Michaelson RS, Pilmanis AA. Neurological altitude decompression sickness among U-2 pilots: 2002-2009. Aviat Space Environ Med. 2011;82:673–82. doi: 10.3357/ASEM.2851.2011. [DOI] [PubMed] [Google Scholar]
- McGuire SA, Tate DF, Wood J, Sladky JH, McDonald K, Sherman PM, Kawano ES, Rowland LM, Patel B, Wright SN, Hong E, Rasmussen J, Willis AM, Kochunov PV. Lower neurocognitive function in U-2 pilots: Relationship to white matter hyperintensities. Neurology. 2014;83:638–45. doi: 10.1212/WNL.0000000000000694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire SA, Boone GR, Sherman PM, Tate DF, Wood JD, Patel B, Eskandar G, Wijtenburg SA, Rowland LM, Clarke GD, Grogan PM, Sladky JH, Kochunov PV. White Matter Integrity in High-Altitude Pilots Exposed to Hypobaria. Aerosp Med Hum Perform. 2016;87:983–8. doi: 10.3357/AMHP.4585.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson G, Ebersole D, Covington D, Denoble PJ. The effectiveness of risk mitigation interventions in divers with persistent (patent) foramen ovale. Diving Hyperb Med. 2019;49:80–7. doi: 10.28920/dhm49.2.80-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gempp E, Louge P, Blatteau JE, Hugon M. Risks factors for recurrent neurological decompression sickness in recreational divers: a case-control study. J Sports Med Phys Fitness. 2012;52:530–6. [PubMed] [Google Scholar]
- Cartoni D, De Castro S, Valente G, Costanzo C, Pelliccia A, Beni S, Di Angelantonio E, Papetti F, Serdoz LV, Fedele F. Identification of professional scuba divers with patent foramen ovale at risk for decompression illness. Am J Cardiol. 2004;94:270–3. doi: 10.1016/j.amjcard.2004.03.084. [DOI] [PubMed] [Google Scholar]
- Germonpre P, Balestra C, Obeid G, Caers D. Cutis Marmorata skin decompression sickness is a manifestation of brainstem bubble embolization, not of local skin bubbles. Med Hypotheses. 2015;85:863–9. doi: 10.1016/j.mehy.2015.09.022. [DOI] [PubMed] [Google Scholar]
- Eftedal OS, Lydersen S, Brubakk AO. The relationship between venous gas bubbles and adverse effects of decompression after air dives. Undersea Hyperb Med. 2007;34:99–105. [PubMed] [Google Scholar]
- Johansson MC, Eriksson P, Guron CW, Dellborg M. Pitfalls in diagnosing PFO: Characteristics of false-negative contrast injections during transesophageal echocardiography in patients with patent foramen ovales. J Am Soc Echocardiogr. 2010;23:1136–42. doi: 10.1016/j.echo.2010.08.004. [DOI] [PubMed] [Google Scholar]
- Germonpre P. Patent foramen ovale and diving. Cardiol Clin. 2005;23:97–104. doi: 10.1016/j.ccl.2004.10.005. [DOI] [PubMed] [Google Scholar]
- Sykes O, Clark JE. Patent foramen ovale and scuba diving: a practical guide for physicians on when to refer for screening. Extrem Physiol Med. 2013;2:10. doi: 10.1186/2046-7648-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klingmann C, Rathmann N, Hausmann D, Bruckner T, Kern R. Lower risk of decompression sickness after recommendation of conservative decompression practices in divers with and without vascular right-to-left shunt. Diving Hyperb Med. 2012;42:146–50. [PubMed] [Google Scholar]
- Honěk J, Šrámek M, Šefc L, Januška J, Fiedler J, Horváth M, Tomek A, Novotný Š, Honěk T, Veselka J. Effect of conservative dive profiles on the occurrence of venous and arterial bubbles in divers with a patent foramen ovale: a pilot study. Int J Cardiol. 2014;176:1001–2. doi: 10.1016/j.ijcard.2014.04.218. [DOI] [PubMed] [Google Scholar]
- Smart D, Mitchell S, Wilmshurst P, Turner M, Banham N. Joint position statement on persistent foramen ovale (PFO) and diving: South pacific Underwater Medicine Society (SPUMS) and the United Kingdom Sports Diving Medical Committee (UKSDMC). Diving Hyperb Med. 2015;45:129–31. [PubMed] [Google Scholar]
- Honěk J, Šrámek M, Šefc L, Januška J, Fiedler J, Horváth M, Tomek A, Novotný Š, Honěk T, Veselka J. Effect of catheter-based patent foramen ovale closure on the occurrence of arterial bubbles in scuba divers. JACC Cardiovasc Interv. 2014;7:403–8. doi: 10.1016/j.jcin.2013.12.199. [DOI] [PubMed] [Google Scholar]
- Walsh KP, Wilmshurst PT, Morrison WL. Transcatheter closure of patent foramen ovale using the Amplatzer septal occluder to prevent recurrence of neurological decompression illness in divers. Heart. 1999;81:257–61. doi: 10.1136/hrt.81.3.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearman A, Bugeja L, Nelson M, Szantho GV, Turner M. An audit of persistent foramen ovale closure in 105 divers. Diving Hyperb Med. 2015;45:94–7. [PubMed] [Google Scholar]
- EEde MV. Recurrent cutaneous decompression illness after PFO device implantation: a case report. Undersea Hyperb Med. 2016;43:841–5. [PubMed] [Google Scholar]
- Vanden Eede M, Van Berendoncks A, De Wolfe D, De Maeyer C, Vanden Eede H, Germonpre P. Percutaneous closure of patent foramen ovale for the secondary prevention of decompression illness in sports divers: mind the gap. Undersea Hyperb Med. 2019;46:625–32. [PubMed] [Google Scholar]
- Moon R, Bove, Mitchell . PFO Statement. In: Denoble PJ, Holm JR, editors. Patent Foramen Ovale Fitness to Dive Consensus. Workshop Proceedings. Durham, NC, USA: Divers Alert Network; 2015. pp. 156–60. [Google Scholar]
- Laden G, Colvin A. Incidence of decompression sickness arising from air diving operations. Undersea Hyperb Med. 1998;25:237–9. [PubMed] [Google Scholar]
- Glen SK, Georgiadis D, Grosset DG, Douglas JD, Lees KR. Transcranial Doppler ultrasound in commercial air divers: a field study including cases with right-to-left shunting. Undersea Hyperb Med. 1995;22:129–35. [PubMed] [Google Scholar]
- Stewart WF, Roy J, Lipton RB. Migraine prevalence, socioeconomic status, and social causation. Neurology. 2013;81:948–55. doi: 10.1212/WNL.0b013e3182a43b32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD 2016 Headache Collaborators. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:954–76. doi: 10.1016/S1474-4422(18)30322-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buse DC, Manack AN, Fanning KM, Serrano D, Reed ML, Turkel CC, Lipton RB. Chronic migraine prevalence, disability, and sociodemographic factors: results from the American Migraine Prevalence and Prevention Study. Headache. 2012;52:1456–70. doi: 10.1111/j.1526-4610.2012.02223.x. [DOI] [PubMed] [Google Scholar]
- Natoli JL, Manack A, Dean B, Butler Q, Turkel CC, Stovner L, Lipton RB. Global prevalence of chronic migraine: a systematic review. Cephalalgia. 2010;30:599–609. doi: 10.1111/j.1468-2982.2009.01941.x. [DOI] [PubMed] [Google Scholar]
- Manzoni GC, Torelli P. Epidemiology of migraine. J Headache Pain. 2003;4:s18–22. doi: 10.1007/s101940300003. [DOI] [Google Scholar]
- Ries S, Steinke W, Neff W, Schindlmayr C, Meairs S, Hennerici M. Ischemia-induced migraine from paradoxical cardioembolic stroke. Eur Neurol. 1996;36:76–8. doi: 10.1159/000117212. [DOI] [PubMed] [Google Scholar]
- Del Sette M, Angeli S, Leandri M, Ferriero G, Bruzzone GL, Finocchi C, Gandolfo C. Migraine with aura and right-to-left shunt on transcranial Doppler: a case-control study. Cerebrovasc Dis. 1998;8:327–30. doi: 10.1159/000015875. [DOI] [PubMed] [Google Scholar]
- Khessali H, Mojadidi MK, Gevorgyan R, Levinson R, Tobis J. The effect of patent foramen ovale closure on visual aura without headache or typical aura with migraine headache. JACC Cardiovasc Interv. 2012;5:682–7. doi: 10.1016/j.jcin.2012.03.013. [DOI] [PubMed] [Google Scholar]
- West BH, Noureddin N, Mamzhi Y, Low CG, Coluzzi AC, Shih EJ, Gevorgyan Fleming R, Saver JL, Liebeskind DS, Charles A, Tobis JM. Frequency of Patent Foramen Ovale and Migraine in Patients With Cryptogenic Stroke. Stroke. 2018;49:1123–8. doi: 10.1161/STROKEAHA.117.020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwerzmann M, Meier B. Impact of percutaneous patent foramen ovale closure on migraine course. Interv Cardiol. 2010;2:177–88. doi: 10.2217/ica.10.6. [DOI] [Google Scholar]
- Anzola GP, Magoni M, Guindani M, Rozzini L, Dalla Volta G. Potential source of cerebral embolism in migraine with aura: a transcranial Doppler study. Neurology. 1999;52:1622–5. doi: 10.1212/WNL.52.8.1622. [DOI] [PubMed] [Google Scholar]
- Tariq N, Tepper SJ, Kriegler JS. Patent Foramen Ovale and Migraine: Closing the Debate-A Review. Headache. 2016;56:462–78. doi: 10.1111/head.12779. [DOI] [PubMed] [Google Scholar]
- Takagi H, Umemoto T ALICE (All-Literature Investigation of Cardiovascular Evidence) Group. A meta-analysis of case-control studies of the association of migraine and patent foramen ovale. J Cardiol. 2016;67:493–503. doi: 10.1016/j.jjcc.2015.09.016. [DOI] [PubMed] [Google Scholar]
- Wilmshurst PT, Nightingale S, Walsh KP, Morrison WL. Effect on migraine of closure of cardiac right-to-left shunts to prevent recurrence of decompression illness or stroke or for haemodynamic reasons. Lancet. 2000;356:1648–51. doi: 10.1016/S0140-6736(00)03160-3. [DOI] [PubMed] [Google Scholar]
- Kanwar SM, Noheria A, DeSimone CV, Rabinstein AA, Asirvatham SJ. Coincidental Impact of Transcatheter Patent Foramen Ovale Closure on Migraine with and without Aura — A Comprehensive Meta-Analysis. Clin Trials Regul Sci Cardiol. 2016;15:7–13. doi: 10.1016/j.ctrsc.2016.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele JG, Nath PU, Burn J, Porteous ME. An association between migrainous aura and hereditary haemorrhagic telangiectasia. Headache. 1993;33:145–8. doi: 10.1111/j.1526-4610.1993.hed3303145.x. [DOI] [PubMed] [Google Scholar]
- Angeli S, Carrera P, Del Sette M, Assini A, Grandis M, Biancolini D, Ferrari M, Gandolfo C. Very high prevalence of right-to-left shunt on transcranial Doppler in an Italian family with cerebral autosomal dominant angiopathy with subcortical infarcts and leukoencephalopathy. Eur Neurol. 2001;46:198–201. doi: 10.1159/000050804. [DOI] [PubMed] [Google Scholar]
- Kahya Eren N, Bülbül NG, Yakar Tülüce S, Nazlı C, Beckmann Y. To Be or Not to Be Patent: The Relationship Between Migraine and Patent Foramen Ovale. Headache. 2015;55:934–42. doi: 10.1111/head.12618. [DOI] [PubMed] [Google Scholar]
- Dalla Volta G, Guindani M, Zavarise P, Griffini S, Pezzini A, Padovani A. Prevalence of patent foramen ovale in a large series of patients with migraine with aura, migraine without aura and cluster headache, and relationship with clinical phenotype. J Headache Pain. 2005;6:328–30. doi: 10.1007/s10194-005-0223-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg P, Servoss SJ, Wu JC, Bajwa ZH, Selim MH, Dineen A, Kuntz RE, Cook EF, Mauri L. Lack of association between migraine headache and patent foramen ovale: results of a case-control study. Circulation. 2010;121:1406–12. doi: 10.1161/CIRCULATIONAHA.109.895110. [DOI] [PubMed] [Google Scholar]
- Rundek T, Elkind MSV, Di Tullio MR, Carrera E, Jin Z, Sacco RL, Homma S. Patent foramen ovale and migraine: a cross-sectional study from the Northern Manhattan Study (NOMAS). Circulation. 2008;118:1419–24. doi: 10.1161/CIRCULATIONAHA.108.771303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Küper M, Rabe K, Holle D, Savidou I, Dommes P, Frings M, Diener HC, Katsarava Z. Prevalence of cardiac right left shunts in migraine: a population-based case-control study. Neurol Sci. 2013;34:205–8. doi: 10.1007/s10072-012-0986-0. [DOI] [PubMed] [Google Scholar]
- Sevgi EB, Erdener SE, Demirci M, Topcuoglu MA, Dalkara T. Paradoxical air microembolism induces cerebral bioelectrical abnormalities and occasionally headache in patent foramen ovale patients with migraine. J Am Heart Assoc. 2012;1:e001735. doi: 10.1161/JAHA.112.001735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finocchi C, Del Sette M. Migraine with aura and patent foramen ovale: myth or reality? Neurol Sci. 2015;36 Suppl 1:61–6. doi: 10.1007/s10072-015-2163-8. [DOI] [PubMed] [Google Scholar]
- Sharma A, Gheewala N, Silver P. Role of patent foramen ovale in migraine etiology and treatment: a review. Echocardiography. 2011;28:913–7. doi: 10.1111/j.1540-8175.2011.01460.x. [DOI] [PubMed] [Google Scholar]
- Dinia L, Roccatagliata L, Bonzano L, Finocchi C, Del Sette M. Diffusion MRI during migraine with aura attack associated with diagnostic microbubbles injection in subjects with large PFO. Headache. 2007;47:1455–6. doi: 10.1111/j.1526-4610.2007.00948.x. [DOI] [PubMed] [Google Scholar]
- Caputi L, Usai S, Carriero MR, Grazzi L, D’Amico D, Falcone C, Anzola GP, Del Sette M, Parati E, Bussone G. Microembolic air load during contrast-transcranial doppler: a trigger for migraine with aura? Headache. 2010;50:1320–7. doi: 10.1111/j.1526-4610.2010.01621.x. [DOI] [PubMed] [Google Scholar]
- Rigatelli G, Cardaioli P, Dell’avvocata F, Giordan M, Braggion G, Chinaglia M, Roncon L. Transcatheter patent foramen ovale closure is effective in reducing migraine independently from specific interatrial septum anatomy and closure devices design. Cardiovasc Revasc Med. 2010;11:29–33. doi: 10.1016/j.carrev.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Zeller JA, Frahm K, Baron R, Stingele R, Deuschl G. Platelet-leukocyte interaction and platelet activation in migraine: a link to ischemic stroke? J Neurol Neurosurg Psychiatry. 2004;75:984–7. doi: 10.1136/jnnp.2003.019638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilmshurst PT, Nightingale S, Walsh KP, Morrison WL. Clopidogrel reduces migraine with aura after transcatheter closure of persistent foramen ovale and atrial septal defects. Heart. 2005;91:1173–5. doi: 10.1136/hrt.2004.047746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snijder RJ, Luermans JG, de Heij AH, Thijs V, Schonewille WJ, Van De Bruaene A, Swaans MJ, Budts WI, Post MC. Patent Foramen Ovale With Atrial Septal Aneurysm Is Strongly Associated With Migraine With Aura: A Large Observational Study. J Am Heart Assoc. 2016;5:e003771. doi: 10.1161/JAHA.116.003771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadrameli SS, Gadhia RR, Kabir R, Volpi JJ. Patent Foramen Ovale in Cryptogenic Stroke and Migraine with Aura: Does Size Matter? Cureus. 2018;10:e3213. doi: 10.7759/cureus.3213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigna C, Marchese N, Inchingolo V, Giannatempo GM, Pacilli MA, Di Viesti P, Impagliatelli M, Natali R, Russo A, Fanelli R, Loperfido F. Improvement of migraine after patent foramen ovale percutaneous closure in patients with subclinical brain lesions: a case-control study. JACC Cardiovasc Interv. 2009;2:107–13. doi: 10.1016/j.jcin.2008.10.011. [DOI] [PubMed] [Google Scholar]
- Butera G, Biondi-Zoccai GG, Carminati M, Caputi L, Usai S, Bussone G, Meola G, Delogu AB, Sheiban I, Sangiorgi G. Systematic review and meta-analysis of currently available clinical evidence on migraine and patent foramen ovale percutaneous closure: much ado about nothing? Catheter Cardiovasc Interv. 2010;75:494–504. doi: 10.1002/ccd.22232. [DOI] [PubMed] [Google Scholar]
- Dowson A, Mullen MJ, Peatfield R, Muir K, Khan AA, Wells C, Lipscombe SL, Rees T, De Giovanni JV, Morrison WL, Hildick-Smith D, Elrington G, Hillis WS, Malik IS, Rickards A. Migraine Intervention With STARFlex Technology (MIST) trial: a prospective, multicenter, double-blind, sham-controlled trial to evaluate the effectiveness of patent foramen ovale closure with STARFlex septal repair implant to resolve refractory migraine headache. Circulation. 2008;117:1397–404. doi: 10.1161/CIRCULATIONAHA.107.727271. [DOI] [PubMed] [Google Scholar]
- Mattle HP, Evers S, Hildick-Smith D, Becker WJ, Baumgartner H, Chataway J, Gawel M, Göbel H, Heinze A, Horlick E, Malik I, Ray S, Zermansky A, Findling O, Windecker S, Meier B. Percutaneous closure of patent foramen ovale in migraine with aura, a randomized controlled trial. Eur Heart J. 2016;37:2029–36. doi: 10.1093/eurheartj/ehw027. [DOI] [PubMed] [Google Scholar]
- Tobis JM, Charles A, Silberstein SD, Sorensen S, Maini B, Horwitz PA, Gurley JC. Percutaneous Closure of Patent Foramen Ovale in Patients With Migraine. J Am Coll Cardiol. 2017;70:2766–74. doi: 10.1016/j.jacc.2017.09.1105. [DOI] [PubMed] [Google Scholar]
- Shi YJ, Lv J, Han XT, Luo GG. Migraine and percutaneous patent foramen ovale closure: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2017;17:203. doi: 10.1186/s12872-017-0644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbadawi A, Barssoum K, Abuzaid AS, Rezq A, Biniwale N, Alotaki E, Mohamed AH, Vuyyala S, Ogunbayo GO, Saad M. Meta-analysis of randomized trials on percutaneous patent foramen ovale closure for prevention of migraine. Acta Cardiol. 2019;74:124–9. doi: 10.1080/00015385.2018.1475027. [DOI] [PubMed] [Google Scholar]
- Meier B, Nietlispach F. Fallacies of Evidence-Based Medicine in Cardiovascular Medicine. Am J Cardiol. 2019;123:690–4. doi: 10.1016/j.amjcard.2018.11.004. [DOI] [PubMed] [Google Scholar]
- Devendra GP, Rane AA, Krasuski RA. Provoked exercise desaturation in patent foramen ovale and impact of percutaneous closure. JACC Cardiovasc Interv. 2012;5:416–9. doi: 10.1016/j.jcin.2012.01.011. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Palkar A, Talwar A. The multiple dimensions of Platypnea-Orthodeoxia syndrome: A review. Respir Med. 2017;129:31–8. doi: 10.1016/j.rmed.2017.05.016. [DOI] [PubMed] [Google Scholar]
- Landzberg MJ, Sloss LJ, Faherty CE, Morrison BJ, Bittl JA, Bridges ND, Casale PN, Keane JF, Lock JE. Orthodeoxia-platypnea due to intracardiac shunting--relief with transcatheter double umbrella closure. Cathet Cardiovasc Diagn. 1995;36:247–50. doi: 10.1002/ccd.1810360312. [DOI] [PubMed] [Google Scholar]
- Blanche C, Noble S, Roffi M, Testuz A, Müller H, Meyer P, Bonvini JM, Bonvini RF. Platypnea-orthodeoxia syndrome in the elderly treated by percutaneous patent foramen ovale closure: a case series and literature review. Eur J Intern Med. 2013;24:813–7. doi: 10.1016/j.ejim.2013.08.698. [DOI] [PubMed] [Google Scholar]
- Mojadidi MK, Gevorgyan R, Noureddin N, Tobis JM. The effect of patent foramen ovale closure in patients with platypnea-orthodeoxia syndrome. Catheter Cardiovasc Interv. 2015;86:701–7. doi: 10.1002/ccd.25953. [DOI] [PubMed] [Google Scholar]
- Guerin P, Lambert V, Godart F, Legendre A, Petit J, Bourlon F, De Geeter B, Petit A, Monrozier B, Rossignol AM, Jimenez M, Crochet D, Choussat A, Rey C, Losay J. Transcatheter closure of patent foramen ovale in patients with platypnea-orthodeoxia: results of a multicentric French registry. Cardiovasc Intervent Radiol. 2005;28:164–8. doi: 10.1007/s00270-004-0035-3. [DOI] [PubMed] [Google Scholar]
- Shah AH, Osten M, Leventhal A, Bach Y, Yoo D, Mansour D, Benson L, Wilson WM, Horlick E. Percutaneous Intervention to Treat Platypnea-Orthodeoxia Syndrome: The Toronto Experience. JACC Cardiovasc Interv. 2016;9:1928–38. doi: 10.1016/j.jcin.2016.07.003. [DOI] [PubMed] [Google Scholar]
- Rimoldi SF, Ott S, Rexhaj E, de Marchi SF, Allemann Y, Gugger M, Scherrer U, Seiler C. Patent Foramen Ovale Closure in Obstructive Sleep Apnea Improves Blood Pressure and Cardiovascular Function. Hypertension. 2015;66:1050–7. doi: 10.1161/HYPERTENSIONAHA.115.06303. [DOI] [PubMed] [Google Scholar]
- Chen L, Deng W, Palacios I, Inglessis-Azuaje I, McMullin D, Zhou D, Lo EH, Buonanno F, Ning M. Patent foramen ovale (PFO), stroke and pregnancy. J Investig Med. 2016;64:992–1000. doi: 10.1136/jim-2016-000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovsepian DA, Sriram N, Kamel H, Fink ME, Navi BB. Acute cerebrovascular disease occurring after hospital discharge for labor and delivery. Stroke. 2014;45:1947–50. doi: 10.1161/STROKEAHA.114.005129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selim M. Perioperative Stroke. N Engl J Med. 2007;356:706–13. doi: 10.1056/NEJMra062668. [DOI] [PubMed] [Google Scholar]
- Mrkobrada M, Hill MD, Chan MTV, Sigamani A, Cowan D, Kurz A, Sessler DI, Jacka M, Graham M, Dasgupta M, Dunlop V, Emery DJ, Gulka I, Guyatt G, Heels-Ansdell D, Murkin J, Pettit S, Sahlas DJ, Sharma M, Sharma M, Srinathan S, St John P, Tsai S, Gelb AW, O’Donnell M, Siu D, Chiu PWY, Sharath V, George A, Devereaux PJ. Covert stroke after non-cardiac surgery: a prospective cohort study. Br J Anaesth. 2016;117:191–7. doi: 10.1093/bja/aew179. [DOI] [PubMed] [Google Scholar]
- Mashour GA, Shanks AM, Kheterpal S. Perioperative Stroke and Associated Mortality after Noncardiac, Nonneurologic Surgery. Anesthesiology. 2011;114:1289–96. doi: 10.1097/ALN.0b013e318216e7f4. [DOI] [PubMed] [Google Scholar]
- Ng PY, Ng AK-Y, Subramaniam B, Burns SM, Herisson F, Timm FP, Cand Med, Rudolph MI, Cand Med, Scheffenbichler F, Cand Med, Friedrich S, Cand Med, Houle TT, Bhatt DL, Eikermann M. Association of Preoperatively Diagnosed Patent Foramen Ovale With Perioperative Ischemic Stroke. JAMA. 2018;319:452–62. doi: 10.1001/jama.2017.21899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fathi AR, Eshtehardi P, Meier B. Patent foramen ovale and neurosurgery in sitting position: a systematic review. Br J Anaesth. 2009;102:588–96. doi: 10.1093/bja/aep063. [DOI] [PubMed] [Google Scholar]
- Rath GP, Bithal PK, Chaturvedi A, Dash HH. Complications related to positioning in posterior fossa craniectomy. J Clin Neurosci. 2007;14:520–5. doi: 10.1016/j.jocn.2006.02.010. [DOI] [PubMed] [Google Scholar]
- Barlow J. An Account of the Removal of a Tumour situated on the Cheek. Med Chir Trans. 1831;16:19–35. doi: 10.1177/09595287310160P103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giraldo M, Lopera LM, Arango M. Venous air embolism in neurosurgery. Colomb J Anesthesiol. 2015;43:40–4. [Google Scholar]
- Leslie K, Hui R, Kaye AH. Venous air embolism and the sitting position: A case series. J Clin Neurosci. 2006;13:419–22. doi: 10.1016/j.jocn.2005.08.007. [DOI] [PubMed] [Google Scholar]
- Hindman BJ, Palecek JP, Posner KL, Traynelis VC, Lee LA, Sawin PD, Tredway TL, Todd MM, Domino KB. Cervical spinal cord, root, and bony spine injuries: a closed claims analysis. Anesthesiology. 2011;114:782–95. doi: 10.1097/ALN.0b013e3182104859. [DOI] [PubMed] [Google Scholar]
- Di Lorenzo N, Caruso R, Floris R, Guerrisi V, Bozzao L, Fortuna A. Pneumocephalus and tension pneumocephalus after posterior fossa surgery in the sitting position: a prospective study. Acta Neurochir (Wien) 1986;83:112–5. doi: 10.1007/BF01402388. [DOI] [PubMed] [Google Scholar]
- Drummond JC, Shapiro . Cerebral physiology. In: Miller RD, editor. Anesthesia. 3rd ed. Edinburgh, UK: Churchill Livingstone; 1990. pp. 621–58. [Google Scholar]
- Elton RJ, Howell RS. The sitting position in neurosurgical anaesthesia: a survey of British practice in 1991. Br J Anaesth. 1994;73:247–8. doi: 10.1093/bja/73.2.247. [DOI] [PubMed] [Google Scholar]
- Dalrymple DG, MacGowan SW, MacLeod GF. Cardiorespiratory effects of the sitting position in neurosurgery. Br J Anaesth. 1979;51:1079–82. doi: 10.1093/bja/51.11.1079. [DOI] [PubMed] [Google Scholar]
- Voorhies RM, Fraser RA, Van Poznak A. Prevention of air embolism with positive end expiratory pressure. Neurosurgery. 1983;12:503–6. doi: 10.1227/00006123-198305000-00004. [DOI] [PubMed] [Google Scholar]
- Papadopoulos G, Kuhly P, Brock M, Rudolph KH, Link J, Eyrich K. Venous and paradoxical air embolism in the sitting position. A prospective study with transoesophageal echocardiography. Acta Neurochir (Wien) 1994;126:140–3. doi: 10.1007/BF01476424. [DOI] [PubMed] [Google Scholar]
- Leonard IE, Cunningham AJ. The sitting position in neurosurgery--not yet obsolete! Br J Anaesth. 2002;88:1–3. doi: 10.1093/bja/88.1.1. [DOI] [PubMed] [Google Scholar]
- Porter JM, Pidgeon C, Cunningham AJ. The sitting position in neurosurgery: a critical appraisal. Br J Anaesth. 1999;82:117–28. doi: 10.1093/bja/82.1.117. [DOI] [PubMed] [Google Scholar]
- Feigl GC, Decker K, Wurms M, Krischek B, Ritz R, Unertl K, Tatagiba M. Neurosurgical procedures in the semisitting position: evaluation of the risk of paradoxical venous air embolism in patients with a patent foramen ovale. World Neurosurg. 2014;81:159–64. doi: 10.1016/j.wneu.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Ammirati M, Lamki TT, Shaw AB, Forde B, Nakano I, Mani M. A streamlined protocol for the use of the semi-sitting position in neurosurgery: a report on 48 consecutive procedures. J Clin Neurosci. 2013;20:32–4. doi: 10.1016/j.jocn.2012.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orliaguet GA, Hanafi M, Meyer PG, Blanot S, Jarreau MM, Bresson D, Zerah M, Carli PA. Is the sitting or the prone position best for surgery for posterior fossa tumours in children? Paediatr Anaesth. 2001;11:541–7. doi: 10.1046/j.1460-9592.2001.00733.x. [DOI] [PubMed] [Google Scholar]
- Williams EL, Hart WM Jr, Tempelhoff R. Postoperative ischemic optic neuropathy. Anesth Analg. 1995;80:1018–29. doi: 10.1097/00000539-199505000-00029. [DOI] [PubMed] [Google Scholar]
- Bhardwaj A, Long DM, Ducker TB, Toung TJ. Neurologic deficits after cervical laminectomy in the prone position. J Neurosurg Anesthesiol. 2001;13:314–9. doi: 10.1097/00008506-200110000-00006. [DOI] [PubMed] [Google Scholar]
- Furuya H, Suzuki T, Okumura F, Kishi Y, Uefuji T. Detection of air embolism by transesophageal echocardiography. Anesthesiology. 1983;58:124–9. doi: 10.1097/00000542-198302000-00004. [DOI] [PubMed] [Google Scholar]
- Garachemani A, Eshtehardi P, Meier B. Paradoxical emboli through the patent foramen ovale as the suspected cause of myocardial and renal infarction in a 48-year-old woman. Catheter Cardiovasc Interv. 2007;70:1010–2. doi: 10.1002/ccd.21214. [DOI] [PubMed] [Google Scholar]
- Loscalzo J. Paradoxical embolism: clinical presentation, diagnostic strategies, and therapeutic options. Am Heart J. 1986;112:141–5. doi: 10.1016/0002-8703(86)90692-7. [DOI] [PubMed] [Google Scholar]
- Windecker S, Wahl A, Chatterjee T, Garachemani A, Eberli FR, Seiler C, Meier B. Percutaneous closure of patent foramen ovale in patients with paradoxical embolism: long-term risk of recurrent thromboembolic events. Circulation. 2000;101:893–8. doi: 10.1161/01.CIR.101.8.893. [DOI] [PubMed] [Google Scholar]
- Alam S, Hossain A, Amin R, Wakil A, Islam K, Chowdhury R. The Sitting Position in Neurosurgery: A Clinical Study in 30 Cases. Bangladesh Journal of Neuroscience. 2012;28:45–51. doi: 10.3329/bjn.v28i1.17192. [DOI] [Google Scholar]
- Himes BT, Mallory GW, Abcejo AS, Pasternak J, Atkinson JLD, Meyer FB, Marsh WR, Link MJ, Clarke MJ, Perkins W, Van Gompel JJ. Contemporary analysis of the intraoperative and perioperative complications of neurosurgical procedures performed in the sitting position. J Neurosurg. 2017;127:182–8. doi: 10.3171/2016.5.JNS152328. [DOI] [PubMed] [Google Scholar]
- Pandia MP, Bithal PK, Dash HH, Chaturvedi A. Comparative incidence of cardiovascular changes during venous air embolism as detected by transesophageal echocardiography alone or in combination with end tidal carbon dioxide tension monitoring. J Clin Neurosci. 2011;18:1206–9. doi: 10.1016/j.jocn.2011.01.023. [DOI] [PubMed] [Google Scholar]
- Vinay B, Sriganesh K, Gopala Krishna KN. An abrupt reduction in end-tidal carbon-dioxide during neurosurgery is not always due to venous air embolism: a capnograph artefact. J Clin Monit Comput. 2014;28:217–9. doi: 10.1007/s10877-013-9505-y. [DOI] [PubMed] [Google Scholar]
- Kumar R, Goyal V, Chauhan RS. Venous air embolism during microelectrode recording in deep brain stimulation surgery in an awake supine patient. Br J Neurosurg. 2009;23:446–8. doi: 10.1080/02688690902775538. [DOI] [PubMed] [Google Scholar]
- Zanchetta M, Onorato E, Rigatelli G, Pedon L, Zennaro M, Maiolino P. Can posterior fossa lesions be a place for preventive patent foramen ovale transcatheter closure? J Invasive Cardiol. 2004;16:346–50. [PubMed] [Google Scholar]
- Laban JT, Rasul FT, Brecker SJD, Marsh HT, Martin AJ. Patent foramen ovale closure prior to surgery in the sitting position. Br J Neurosurg. 2014;28:421–2. doi: 10.3109/02688697.2013.865709. [DOI] [PubMed] [Google Scholar]
- Carroll JD. PFO and Various Types of Surgery. In: Amin Z, Tobis JM, Sievert H, Carroll JD, editors. Patent Foramen Ovale. London: Springer-Verlag; 2015. p. 123. [Google Scholar]
- Ljubkovic M, Marinovic J, Obad A, Breskovic T, Gaustad SE, Dujic Z. High incidence of venous and arterial gas emboli at rest after trimix diving without protocol violations. J Appl Physiol. 2010;109:1670–4. doi: 10.1152/japplphysiol.01369.2009. [DOI] [PubMed] [Google Scholar]
- Ljubkovic M, Dujic Z, Møllerløkken A, Bakovic D, Obad A, Breskovic T, Brubakk AO. Venous and arterial bubbles at rest after no-decompression air dives. Med Sci Sports Exerc. 2011;43:990–5. doi: 10.1249/MSS.0b013e31820618d3. [DOI] [PubMed] [Google Scholar]
- Vann RD, Butler FK, Mitchell SJ, Moon RE. Decompression illness. Lancet. 2011;377:153–64. doi: 10.1016/S0140-6736(10)61085-9. [DOI] [PubMed] [Google Scholar]
- Madden D, Lozo M, Dujic Z, Ljubkovic M. Exercise after SCUBA diving increases the incidence of arterial gas embolism. J Appl Physiol (1985) 2013;115:716–22. doi: 10.1152/japplphysiol.00029.2013. [DOI] [PubMed] [Google Scholar]
- Arieli R, Marmur A. Ex vivo bubble production from ovine large blood vessels: size on detachment and evidence of “active spots”. Respir Physiol Neurobiol. 2014;200:110–7. doi: 10.1016/j.resp.2014.05.014. [DOI] [PubMed] [Google Scholar]
- Buttolph TB, Dick EJ, Toner CB, Broome JR, Williams R, Kang YH, Wilt NL. Cutaneous lesions in swine after decompression: histopathology and ultrastructure. Undersea Hyperb Med. 1998;25:115–21. [PubMed] [Google Scholar]
- Muth CM, Shank ES. Gas embolism. N Engl J Med. 2000;342:476–82. doi: 10.1056/NEJM200002173420706. [DOI] [PubMed] [Google Scholar]
- Bove AA. Risk of decompression sickness with patent foramen ovale. Undersea Hyperb Med. 1998;25:175–8. [PubMed] [Google Scholar]
- Files DS, Webb JT, Pilmanis AA. Depressurization in military aircraft: rates, rapidity, and health effects for 1055 incidents. Aviat Space Environ Med. 2005;76:523–9. [PubMed] [Google Scholar]
- Morgagni F, Autore A, Landolfi A, Torchia F, Ciniglio Appiani G. Altitude chamber related adverse effects among 1241 airmen. Aviat Space Environ Med. 2010;81:873–7. doi: 10.3357/ASEM.2625.2010. [DOI] [PubMed] [Google Scholar]
- Ohrui N, Takeuchi A, Tong A, Ohuchi M, Iwata M, Sonoda H, Yamasaki S, Akasaki S, Hakamata N, Ohashi K, Nakamura A. Physiological incidents during 39 years of hypobaric chamber training in Japan. Aviat Space Environ Med. 2002;73:395–8. [PubMed] [Google Scholar]
- Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984;59:17–20. doi: 10.1016/S0025-6196(12)60336-X. [DOI] [PubMed] [Google Scholar]
- Wilmshurst PT, Byrne JC, Webb-Peploe MM. Relation between intertrial shunts and decompression sickness in divers. Lancet. 1989;2:1302–6. doi: 10.1016/S0140-6736(89)91911-9. [DOI] [PubMed] [Google Scholar]
- Guenzani S, Mereu D, Messersmith M, Olivari D, Arena M, Spanò A. Inner-ear decompression sickness in nine trimix recreational divers. Diving Hyperb Med. 2016;46:111–6. [PubMed] [Google Scholar]
- Ignatescu M, Bryson P, Klingmann C. Susceptibility of the inner ear structure to shunt-related decompression sickness. Aviat Space Environ Med. 2012;83:1145–51. doi: 10.3357/ASEM.3326.2012. [DOI] [PubMed] [Google Scholar]
- Kemper TC, Rienks R, van Ooij PJ, van Hulst RA. Cutis marmorata in decompression illness may be cerebrally mediated: a novel hypothesis on the aetiology of cutis marmorata. Diving Hyperb Med. 2015;45:84–8. [PubMed] [Google Scholar]
- Kang KW, Kim JT, Choi WH, Park WJ, Shin YH, Choi KH. Patent foramen ovale and asymptomatic brain lesions in military fighter pilots. Clin Neurol Neurosurg. 2014;125:9–14. doi: 10.1016/j.clineuro.2014.07.011. [DOI] [PubMed] [Google Scholar]
- Weber F, Goriup A. Prevalence of right-to-left shunts in active fighter pilots. Aviat Space Environ Med. 2007;78:135–6. [PubMed] [Google Scholar]
- Ries S, Knauth M, Kern R, Klingmann C, Daffertshofer M, Sartor K, Hennerici M. Arterial gas embolism after decompression: correlation with right-to-left shunting. Neurology. 1999;52:401–4. doi: 10.1212/WNL.52.2.401. [DOI] [PubMed] [Google Scholar]
- Gerriets T, Tetzlaff K, Liceni T, Schäfer C, Rosengarten B, Kopiske G, Algermissen C, Struck N, Kaps M. Arteriovenous bubbles following cold water sport dives: relation to right-to-left shunting. Neurology. 2000;55:1741–3. doi: 10.1212/WNL.55.11.1741. [DOI] [PubMed] [Google Scholar]
- Torti SR, Billinger M, Schwerzmann M, Vogel R, Zbinden R, Windecker S, Seiler C. Risk of decompression illness among 230 divers in relation to the presence and size of patent foramen ovale. Eur Heart J. 2004;25:1014–20. doi: 10.1016/j.ehj.2004.04.028. [DOI] [PubMed] [Google Scholar]
- Liou K, Wolfers D, Turner R, Bennett M, Allan R, Jepson N, Cranney G. Patent Foramen Ovale Influences the Presentation of Decompression Illness in SCUBA Divers. Heart Lung Circ. 2015;24:26–31. doi: 10.1016/j.hlc.2014.07.057. [DOI] [PubMed] [Google Scholar]
- Wilmshurst PT, Morrison WL, Walsh KP, Pearson MJ, Nightingale S. Comparison of the size of persistent foramen ovale and atrial septal defects in divers with shunt-related decompression illness and in the general population. Diving Hyperb Med. 2015;45:89–93. [PubMed] [Google Scholar]
- Germonpre P, Balestra C. Risk of decompression illness among 230 divers in relation to the presence and size of patent foramen ovale. Eur Heart J. 2004;25:2173–4. doi: 10.1016/j.ehj.2004.07.042. [DOI] [PubMed] [Google Scholar]
- Germonpre P, Hastir F, Dendale P, Marroni A, Nguyen AF, Balestra C. Evidence for increasing patency of the foramen ovale in divers. Am J Cardiol. 2005;95:912–5. doi: 10.1016/j.amjcard.2004.12.026. [DOI] [PubMed] [Google Scholar]
- Vik A, Jenssen BM, Brubakk AO. Arterial gas bubbles after decompression in pigs with patent foramen ovale. Undersea Hyperb Med. 1993;20:121–31. [PubMed] [Google Scholar]
- Balestra C, Germonpre P, Marroni A. Intrathoracic pressure changes after Valsalva strain and other maneuvers: implications for divers with patent foramen ovale. Undersea Hyperb Med. 1998;25:171–4. [PubMed] [Google Scholar]
- Knauth M, Ries S, Pohimann S, Kerby T, Forsting M, Daffertshofer M, Hennerici M, Sartor K. Cohort study of multiple brain lesions in sport divers: role of a patent foramen ovale. BMJ. 1997;314:701–5. doi: 10.1136/bmj.314.7082.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch AE, Kampen J, Tetzlaff K, Reuter M, McCormack P, Schnoor PW, Struck N, Heine L, Prytulla I, Rieckert H. Incidence of abnormal cerebral findings in the MRI of clinically healthy divers: role of a patent foramen ovale. Undersea Hyperb Med. 2004;31:261–8. [PubMed] [Google Scholar]
- Balestra C, Marroni A, Farkas B, Peetrons P, Vanderschueren F, Duboc E, Snoeck T, Germonpre P. The Fractal Approach as a tool to understand asymptomatic Brain Hyperintense MRI Signals. Fractals. 2004;12:67–72. doi: 10.1142/S0218348X0400232X. [DOI] [Google Scholar]
- Balestra C, Germonpre P. Correlation between Patent Foramen Ovale, Cerebral "Lesions" and Neuropsychometric Testing in Experienced Sports Divers: Does Diving Damage the Brain? Front Psychol. 2016;7:696. doi: 10.3389/fpsyg.2016.00696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tetzlaff K, Reuter M, Leplow B, Heller M, Bettinghausen E. Risk factors for pulmonary barotrauma in divers. Chest. 1997;112:654–9. doi: 10.1378/chest.112.3.654. [DOI] [PubMed] [Google Scholar]
- Germonpre P, Balestra C, Pieters T. Influence of scuba diving on asymptomatic isolated pulmonary bullae. Diving Hyperb Med. 2008;38:206–11. [PubMed] [Google Scholar]
- Wilmshurst P, Bryson P. Relationship between the clinical features of neurological decompression illness and its causes. Clin Sci (Lond) 2000;99:65–75. doi: 10.1042/cs0990065. [DOI] [PubMed] [Google Scholar]
- Bason R, Yacavone DW. Loss of cabin pressurization in U.S. Naval aircraft: 1969-90. Aviat Space Environ Med. 1992;63:341–5. [PubMed] [Google Scholar]
- Benton PJ, Woodfine JD, Westwood PR. Arterial gas embolism following a 1-meter ascent during helicopter escape training: a case report. Aviat Space Environ Med. 1996;67:63–4. [PubMed] [Google Scholar]
- British Thoracic Society Fitness to Dive Group, Subgroup of the British Thoracic Society Standards of Care Committee. British Thoracic Society guidelines on respiratory aspects of fitness for diving. Thorax. 2003;58:3–13. doi: 10.1136/thorax.58.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss LD, Van Meter KW. Cerebral air embolism in asthmatic scuba divers in a swimming pool. Chest. 1995;107:1653–4. doi: 10.1378/chest.107.6.1653. [DOI] [PubMed] [Google Scholar]
- Reuter M, Tetzlaff K, Warninghoff V, Steffens JC, Bettinghausen E, Heller M. Computed tomography of the chest in diving-related pulmonary barotrauma. Br J Radiol. 1997;70:440–5. doi: 10.1259/bjr.70.833.9227223. [DOI] [PubMed] [Google Scholar]
- Bhindi R, Ruparelia N, Newton J, Testa L, Ormerod OJ. Acute worsening in migraine symptoms following PFO closure: a matter of fact? Int J Cardiol. 2010;144:299–300. doi: 10.1016/j.ijcard.2009.02.027. [DOI] [PubMed] [Google Scholar]
- Yankovsky AE, Kuritzky A. Transformation into daily migraine with aura following transcutaneous atrial septal defect closure. Headache. 2003;43:496–8. doi: 10.1046/j.1526-4610.2003.03096.x. [DOI] [PubMed] [Google Scholar]
- Wilmshurst PT. Migraine with aura and persistent foramen ovale. Eye. 2018;32:184–8. doi: 10.1038/eye.2017.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyer C. Migraine doctor is suspended for serious breach of professional standards. BMJ. 2015;350:h982. doi: 10.1136/bmj.h982. [DOI] [PubMed] [Google Scholar]
- Mojadidi MK, Ruiz JC, Chertoff J, Zaman MO, Elgendy IY, Mahmoud AN, Al-Ani M, Elgendy AY, Patel NK, Shantha G, Tobis JM, Meier B. Patent Foramen Ovale and Hypoxemia. Cardiol Rev. 2019;27:34–40. doi: 10.1097/CRD.0000000000000205. [DOI] [PubMed] [Google Scholar]
- Mojadidi MK, Bokhoor PI, Gevorgyan R, Noureddin N, MacLellan WC, Wen E, Aysola R, Tobis JM. Sleep apnea in patients with and without a right-to-left shunt. J Clin Sleep Med. 2015;11:1299–304. doi: 10.5664/jcsm.5190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanoudy H, Soliman A, Raggi P, Liu JW, Russell DC, Jarmukli NF. Prevalence of patent foramen ovale and its contribution to hypoxemia in patients with obstructive sleep apnea. Chest. 1998;113:91–6. doi: 10.1378/chest.113.1.91. [DOI] [PubMed] [Google Scholar]
- Shaikh ZF, Jaye J, Ward N, Malhotra A, De Villa M, Polkey MI, Mullen MJ, Morrell MJ. Patent foramen ovale in severe obstructive sleep apnea: clinical features and effects of closure. Chest. 2013;143:56–63. doi: 10.1378/chest.12-0334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soliman A, Shanoudy H, Liu J, Russell DC, Jarmukli NF. Increased prevalence of patent foramen ovale in patients with severe chronic obstructive pulmonary disease. J Am Soc Echocardiogr. 1999;12:99–105. doi: 10.1016/S0894-7317(99)70121-5. [DOI] [PubMed] [Google Scholar]
- Shaikh ZF, Kelly JL, Shrikrishna D, De Villa M, Mullen MJ, Hopkinson NS, Morrell MJ, Polkey MI. Patent foramen ovale is not associated with hypoxemia in severe chronic obstructive pulmonary disease and does not impair exercise performance. Am J Respir Crit Care Med. 2014;189:540–7. doi: 10.1164/rccm.201309-1618OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martolini D, Tanner R, Davey C, Patel M, Elia D, Purcell H, Palange P, Hopkinson NS, Polkey MI. Significance of Patent Foramen Ovale in Patients with GOLD Stage II Chronic Obstructive Pulmonary Disease (COPD). Chronic Obstr Pulm Dis. 2014;1:185–92. doi: 10.15326/jcopdf.1.2.2013.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacievliyagil SS, Gunen H, Kosar FM, Sahin I, Kilic T. Prevalence and clinical significance of a patent foramen ovale in patients with chronic obstructive pulmonary disease. Respir Med. 2006;100:903–10. doi: 10.1016/j.rmed.2005.08.015. [DOI] [PubMed] [Google Scholar]
- Levine BD, Grayburn PA, Voyles WF, Greene ER, Roach RC, Hackett PH. Intracardiac shunting across a patent foramen ovale may exacerbate hypoxemia in high-altitude pulmonary edema. Ann Intern Med. 1991;114:569–70. doi: 10.7326/0003-4819-114-7-569. [DOI] [PubMed] [Google Scholar]
- Allemann Y, Hutter D, Lipp E, Sartori C, Duplain H, Egli M, Cook S, Scherrer U, Seiler C. Patent foramen ovale and high-altitude pulmonary edema. JAMA. 2006;296:2954–8. doi: 10.1001/jama.296.24.2954. [DOI] [PubMed] [Google Scholar]
- Das BB, Wolfe RR, Chan KC, Larsen GL, Reeves JT, Ivy D. High-altitude pulmonary edema in children with underlying cardiopulmonary disorders and pulmonary hypertension living at altitude. Arch Pediatr Adolesc Med. 2004;158:1170–6. doi: 10.1001/archpedi.158.12.1170. [DOI] [PubMed] [Google Scholar]
- Godart F, Rey C, Prat A, Vincentelli A, Chmaït A, Francart C, Porte H. Atrial right-to-left shunting causing severe hypoxaemia despite normal right-sided pressures. Report of 11 consecutive cases corrected by percutaneous closure. Eur Heart J. 2000;21:483–9. doi: 10.1053/euhj.1999.1944. [DOI] [PubMed] [Google Scholar]
- Altman M, Robin E. Platypnea (diffuse zone I phenomenon?). N Engl J Med. 1969;281:1347–8. doi: 10.1056/NEJM196912112812408. [DOI] [PubMed] [Google Scholar]
- Cheng TO. Platypnea-orthodeoxia syndrome: etiology, differential diagnosis, and management. Catheter Cardiovasc Interv. 1999;47:64–6. doi: 10.1002/(SICI)1522-726X(199905)47:1<64::AID-CCD15>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- Chen GP, Goldberg SL, Gill EA. Patent foramen ovale and the platypnea-orthodeoxia syndrome. Cardiol Clin. 2005;23:85–9. doi: 10.1016/j.ccl.2004.10.003. [DOI] [PubMed] [Google Scholar]
- Sorrentino M, Resnekov L. Patent foramen ovale associated with platypnea and orthodeoxia. Chest. 1991;100:1157–8. doi: 10.1378/chest.100.4.1157. [DOI] [PubMed] [Google Scholar]
- Toffart AC, Bouvaist H, Feral V, Blin D, Pison C. Hypoxemia-orthodeoxia related to patent foramen ovale without pulmonary hypertension. Heart Lung. 2008;37:385–9. doi: 10.1016/j.hrtlng.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Ghamande S, Ramsey R, Rhodes JF, Stoller JK. Right hemidiaphragmatic elevation with a right-to-left interatrial shunt through a patent foramen ovale: a case report and literature review. Chest. 2001;120:2094–6. doi: 10.1378/chest.120.6.2094. [DOI] [PubMed] [Google Scholar]
- Sanikommu V, Lasorda D, Poornima I. Anatomical factors triggering platypnea-orthodeoxia in adults. Clin Cardiol. 2009;32:E55–7. doi: 10.1002/clc.20461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begin R. Platypnea after pneumonectomy. N Engl J Med. 1975;293:342–3. doi: 10.1056/NEJM197508142930707. [DOI] [PubMed] [Google Scholar]
- Dlabal PW, Stutts BS, Jenkins DW, Harkleroad LE, Stanford WT. Cyanosis following right pneumonectomy: importance of patent foramen ovale. Chest. 1982;81:370–2. doi: 10.1378/chest.81.3.370. [DOI] [PubMed] [Google Scholar]
- Bhattacharya K, Birla R, Northridge D, Zamvar V. Platypnea-orthodeoxia syndrome: a rare complication after right pneumonectomy. Ann Thorac Surg. 2009;88:2018–9. doi: 10.1016/j.athoracsur.2009.01.047. [DOI] [PubMed] [Google Scholar]
- Bertaux G, Eicher JC, Petit A, Dobšák P, Wolf JE. Anotomic interaction between the aortic root and the atrial septum: a prospective echocardiographic study. J Am Soc Echocardiogr. 2007;20:409–14. doi: 10.1016/j.echo.2006.09.008. [DOI] [PubMed] [Google Scholar]
- Faller M, Kessler R, Chaouat A, Ehrhart M, Petit H, Weitzenblum E. Platypnea-orthodeoxia syndrome related to an aortic aneurysm combined with an aneurysm of the atrial septum. Chest. 2000;118:553–7. doi: 10.1378/chest.118.2.553. [DOI] [PubMed] [Google Scholar]
- Gonzalez JM, Johnson FR, Runken MC, Poulos CM. Evaluating migraineurs’ preferences for migraine treatment outcomes using a choice experiment. Headache. 2013;53:1635–50. doi: 10.1111/head.12142. [DOI] [PubMed] [Google Scholar]
- Mitsikostas DD, Belesioti I, Arvaniti C, Mitropoulou E, Deligianni C, Kasioti E, Constantinidis T, Dermitzakis M, Vikelis M Hellenic Headache Society. Patients’ preferences for headache acute and preventive treatment. J Headache Pain. 2017;18:102. doi: 10.1186/s10194-017-0813-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peres M, Silberstein S, Moreira F, Corchs F, Vieira D, Abraham N. Patients’ preference for migraine preventive therapy. Headache. 2007;47:540–5. doi: 10.1111/j.1526-4610.2007.00757.x. [DOI] [PubMed] [Google Scholar]
- Malik SN, Hopkins M, Young WB, Silberstein SD. Acute migraine treatment: patterns of use and satisfaction in a clinical population. Headache. 2006;46:773–80. doi: 10.1111/j.1526-4610.2006.00437.x. [DOI] [PubMed] [Google Scholar]
- Cowan R, Cohen JM, Rosenman E, Iyer R. Physician and patient preferences for dosing options in migraine prevention. J Headache Pain. 2019;20:50. doi: 10.1186/s10194-019-0998-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anzola GP, Frisoni GB, Morandi E, Casilli F, Onorato E. Shunt-associated migraine responds favorably to atrial septal repair: a case-control study. Stroke. 2006;37:430–4. doi: 10.1161/01.STR.0000199082.07317.43. [DOI] [PubMed] [Google Scholar]
- Araszkiewicz A, Grygier M, Iwańczyk S, Trojnarska O, Lesiak M, Grajek S. Long-term follow-up after percutaneous closure of patent foramen ovale with Amplatzer PFO Occluder: a single center experience. Postepy Kardiol Interwencyjnej. 2016;12:49–54. doi: 10.5114/pwki.2016.56949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azarbal B, Tobis J, Suh W, Chan V, Dao C, Gaster R. Association of interatrial shunts and migraine headaches: impact of transcatheter closure. J Am Coll Cardiol. 2005;45:489–92. doi: 10.1016/j.jacc.2004.09.075. [DOI] [PubMed] [Google Scholar]
- Biasco L, Infantino V, Orzan F, Vicentini S, Rovera C, Longo G, Chinaglia A, Belli R, Allais G, Gaita F. Impact of transcatheter closure of patent foramen ovale in the evolution of migraine and role of residual shunt. J Cardiol. 2014;64:390–4. doi: 10.1016/j.jjcc.2014.02.023. [DOI] [PubMed] [Google Scholar]
- Dubiel M, Bruch L, Schmehl I, Liebner M, Winkelmann A, Stretz A, Grad MO, Kleber FX. Migraine headache relief after percutaneous transcatheter closure of interatrial communications. J Interv Cardiol. 2008;21:32–7. doi: 10.1111/j.1540-8183.2007.00316.x. [DOI] [PubMed] [Google Scholar]
- Giardini A, Donti A, Formigari R, Salomone L, Prandstraller D, Bonvicini M, Palareti G, Guidetti D, Gaddi O, Picchio FM. Transcatheter patent foramen ovale closure mitigates aura migraine headaches abolishing spontaneous right-to-left shunting. Am Heart J. 2006;151:922.e1–5. doi: 10.1016/j.ahj.2005.09.019. [DOI] [PubMed] [Google Scholar]
- Jesurum JT, Fuller CJ, Kim CJ, Krabill KA, Spencer MP, Olsen JV, Likosky WH, Reisman M. Frequency of migraine headache relief following patent foramen ovale "closure" despite residual right-to-left shunt. Am J Cardiol. 2008;102:916–20. doi: 10.1016/j.amjcard.2008.05.035. [DOI] [PubMed] [Google Scholar]
- Kimmelstiel C, Gange C, Thaler D. Is patent foramen ovale closure effective in reducing migraine symptoms? A controlled study. Catheter Cardiovasc Interv. 2007;69:740–6. doi: 10.1002/ccd.21025. [DOI] [PubMed] [Google Scholar]
- Luermans JG, Post MC, Temmerman F, Thijs V, Schonewille WJ, Plokker HW, Suttorp MJ, Budts WI. Closure of a patent foramen ovale is associated with a decrease in prevalence of migraine: a prospective observational study. Acta Cardiol. 2008;63:571–7. doi: 10.2143/AC.63.5.2033223. [DOI] [PubMed] [Google Scholar]
- Milev I, Zafirovska P, Zimbakov Z, Idrizi S, Ampova-Sokolov V, Gorgieva E, Ilievska L, Tosheski G, Hristov N, Georgievska-Ismail L, Anguseva T, Mitrev Z. Transcatheter closure of patent foramen ovale: A single center experience. Open Access Maced J Med Sci. 2016;4:613–8. doi: 10.3889/oamjms.2016.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morandi E, Anzola GP, Casilli F, Onorato E. Migraine: traditional or "innovative" treatment? A preliminary case-control study. Pediatr Cardiol. 2005;26:231–3. doi: 10.1007/s00246-005-1006-4. [DOI] [PubMed] [Google Scholar]
- Post MC, Thijs V, Herroelen L, Budts WI. Closure of a patent foramen ovale is associated with a decrease in prevalence of migraine. Neurology. 2004;62:1439–40. doi: 10.1212/01.WNL.0000120756.25236.37. [DOI] [PubMed] [Google Scholar]
- Reisman M, Christofferson RD, Jesurum J, Olsen JV, Spencer MP, Krabill KA, Diehl L, Aurora S, Gray WA. Migraine headache relief after transcatheter closure of patent foramen ovale. J Am Coll Cardiol. 2005;45:493–5. doi: 10.1016/j.jacc.2004.10.055. [DOI] [PubMed] [Google Scholar]
- Rigatelli G, Dell’avvocata F, Ronco F, Cardaioli P, Giordan M, Braggion G, Aggio S, Chinaglia M, Rigatelli G, Chen JP. Primary transcatheter patent foramen ovale closure is effective in improving migraine in patients with high-risk anatomic and functional characteristics for paradoxical embolism. JACC Cardiovasc Interv. 2010;3:282–7. doi: 10.1016/j.jcin.2009.11.019. [DOI] [PubMed] [Google Scholar]
- Schwerzmann M, Wiher S, Nedeltchev K, Mattle HP, Wahl A, Seiler C, Meier B, Windecker S. Percutaneous closure of patent foramen ovale reduces the frequency of migraine attacks. Neurology. 2004;62:1399–401. doi: 10.1212/01.WNL.0000120677.64217.A9. [DOI] [PubMed] [Google Scholar]
- Trabattoni D, Fabbiocchi F, Montorsi P, Galli S, Teruzzi G, Grancini L, Gatto P, Bartorelli AL. Sustained long-term benefit of patent foramen ovale closure on migraine. Catheter Cardiovasc Interv. 2011;77:570–4. doi: 10.1002/ccd.22826. [DOI] [PubMed] [Google Scholar]
- Wahl A, Praz F, Findling O, Nedeltchev K, Schwerzmann M, Tai T, Windecker S, Mattle HP, Mejer B. Percutaneous closure of patent foramen ovale for migraine headaches refractory to medical treatment. Catheter Cardiovasc Interv. 2009;74:124–9. doi: 10.1002/ccd.21921. [DOI] [PubMed] [Google Scholar]
- Kheiri B, Abdalla A, Osman M, Ahmed S, Hassan M, Bachuwa G. Patent foramen ovale closure versus medical therapy after cryptogenic stroke: An updated meta-analysis of all randomized clinical trials. Cardiol J. 2018 doi: 10.5603/CJ.a2018.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billinger M, Schwerzmann M, Rutishauser W, Wahl A, Windecker S, Meier B, Seiler C. Patent foramen ovale screening by ear oximetry in divers. Am J Cardiol. 2013;111:286–90. doi: 10.1016/j.amjcard.2012.09.030. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
. Methods.
. Detailed evaluation of specific issues.
. Meta-analysis of studies comparing the prevalence of R-T-L shunting in patients with and without DCS.
. Meta-analysis of observational and randomised trials regarding the incidence of persistent migraine comparing closure versus non-closure of PFO in studies with two cohorts.
. Meta-analysis of observational and randomised trials regarding the incidence of persistent migraine comparing closure versus non-closure of PFO in studies with two cohorts, by aura status.
. Meta-analysis of observational trials assessing persistence of migraine before and after PFO closure, by aura status.
. Meta-analysis of studies on PFO closure in desaturation syndromes. Improvement in blood oxygen saturation after PFO closure.
. PRISMA diagram of decompression sickness studies in recreational divers.
. PRISMA diagram of decompression sickness studies in professional divers.
. PRISMA diagram of decompression sickness studies in desaturation syndromes.
. PRISMA diagram of migraine studies.
. Characteristics for the evaluation of a probable causal link between a PFO and DCS.
. Summary of statements on DCS and PFO.
. Classification of DCS.
. Primary measures for secondary prevention of DCS.
. Summary of statements on migraine and PFO.
. GRADE evaluation of certitude of effects- studies on PFO closure for migraine prevention.
. Summary of PICO question on migraine treatment.
. Detailed PICO question for therapy of migraine.
. Characteristics of the studies on PFO closure for migraine.
. Diseases in which PFO can contribute to arterial hypoxaemia and its clinical consequences.
. Summary of statements on arterial deoxygenation and PFO.
. Position statements on pregnancy and the pre-operative management of patients.
. Position statements on neurosurgery in the sitting position.
. GRADE evaluation of certitude of effects - DCS.
. Studies on DCS in recreational divers.
. Studies on DCS in professional divers.
. GRADE evaluation of certitude of effects - desaturation syndromes.