Abstract
The age-associated decrease in appetite and food intake is referred to as “anorexia of aging”. Older adults with anorexia show changes in the quantity/quality of energy supplied to the organism which eventually may cause a mismatch between ingested calories and physiological energy demands. Therefore, a state of malnutrition and impaired metabolism may ensue which renders older people more vulnerable to stressors and more prone to incur negative health outcomes. These latter cover a wide range of conditions including sarcopenia, low engagement in physical activity, and more severe consequences such as disability, loss of independence, hospitalization, nursing home placement, and mortality. Malnutrition has been recognized by the European Society of Clinical Nutrition (ESPEN) among the chief risk factors for the development of frailty. Frailty refers to a state of increased vulnerability to stressors stemming from reduced physiologic reserve, and according to ESPEN, is also nutrition-based. Alike frailty, anorexia is highly prevalent among older adults, and its multifactorial nature includes metabolic changes that develop in older age and possibly underly the condition. Circulating factors, including hormones (eg, cholecystokinin, ghrelin, leptin, and inflammatory and microbial mediators of gut dysbiosis), have been proposed as biomarkers for this condition to support early identification and develop personalized nutritional interventions. Additional studies are needed to untangle the interrelationship between gut microbiota and appetite regulation in older adults operating through brain–gut crosstalk. Furthermore, the contribution of the genetic background to appetite regulation and specific nutritional needs warrants investigation. Here, we provide an overview on anorexia of aging in the context of age-related metabolic changes. A special focus is placed on candidate biomarkers that may be used to assist in the early identification of anorexia of aging and in the development of personalized nutritional counseling.
Keywords: frailty, geroscience, inflammation, muscle, nutrition, sarcopenia
Introduction
Decreased appetite and reduced food intake are commonly observed in older adults. The term “anorexia of aging” has been introduced to refer to this phenomenon that renders older people more vulnerable to stressors and more prone to incur negative health outcomes (eg, poor quality of life, reduced survival).1,2
The age-associated decrease in food intake results in changes in the quantity/quality of energy supplied to the organism that may ultimately cause a mismatch between ingested calories and physiological energy demands. Therefore, a state of malnutrition and impaired metabolism may ensue with several negative health-related consequences. These cover a wide range of conditions spanning from declines in muscle mass/strength and low engagement in physical activity to more severe consequences, such as disability, loss of independence, hospitalization, nursing home placement, and mortality, with an overall increase in healthcare burden.3–5
The European Society of Clinical Nutrition (ESPEN) has recognized malnutrition among the chief risk factors for the development of frailty, a state of increased vulnerability to stressors stemming from reduced physiologic reserve,6 thus making this condition also nutrition-based.7,8
Considering the high prevalence of anorexia in frail older adults and its multifactorial nature, we will frame anorexia of aging in the context of metabolic changes occurring in older age and possibly underlying this condition. A special focus will be placed on candidate biomarkers that may help support early identification of anorexia of aging and develop personalized nutritional counseling.
Anorexia of Aging: Prevalence, Causes, and Risk Factors
The prevalence of anorexia in older adults is rated at about 20% and varies according to setting, gender, and comorbidities.9 A higher prevalence of anorexia is observed among people older than 65 living in long-term institutions, hospitalized, or suffering from neurological disorders and/or inflammatory conditions.5,10 Anorexia has a multifactorial etiology encompassing both age-associated changes in peripheral and central physiological processes and the co-occurrence of pathological conditions.2,5,11 Declines in sight, smell, and taste occurring during aging are only a few of the age-related changes implicated in the development of anorexia.12 Factors related to poor oral health such as inadequate dentition, poor fitting dentures, inflammatory diseases of the oral cavity, and difficulties in chewing and swallowing limit food choices and contribute to reducing food intake in older adults.2 Socioeconomic factors (eg, living alone, low-income status) and the associated downside of reduced psychological well-being may also contribute to the development of anorexia of aging. However, recent evidence suggests that malnutrition in older adults is not necessarily dependent on socioeconomic factors.13 Psychological factors (ie, depression) negatively impact the quality and quantity of food being consumed.14 The Avoidant Restrictive Food Intake Disorder (ARFID) has been reported among older people and associated with avoidance of specific foods for different reasons (eg, fear of choking).14
As a whole, these factors are crucial for the assessment and management of anorexia of aging. However, endocrine, metabolic, and nutritional changes that accompany aging have emerged as relevant factors that may allow a better framing of anorexia in the context of age-associated metabolic milieu and will be discussed in more detail in the next sections.
Metabolic Changes of Anorexia of Aging: A Role for Cholecystokinin, Ghrelin, Leptin, and Gut Dysbiosis
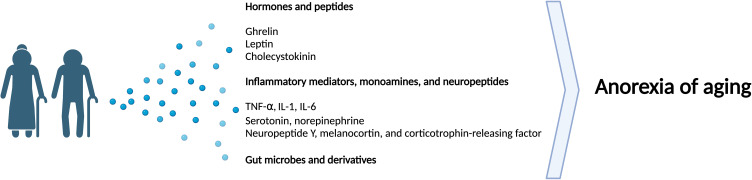
Modifications occurring at the gastric level during aging lead to altered regulation of appetite-related signaling.15 The physiology of the gastrointestinal tract becomes compromised with age, with a decrease in muscular tone and motility as well as reduced activity of visceral neurons and altered distension of the stomach (ie, fundus and antrum). The delay in gastric emptying observed in older people may explain longer-lasting satiety, which in turn contributes to reduced appetite.15 The reduced digestive ability of the stomach may further aggravate the lack of appetite and reduced food intake in older persons. As part of the changes occurring in the gastrointestinal system during aging, hormonal alterations have been observed and likely modulate the function and activity of brain circuits that regulate appetite/satiety (Figure 1).2,5,11 Among the age-associated hormonal perturbations are those related to the circulating levels of several gastrointestinal mediators including cholecystokinin (CCK), peptide tyrosine (PYY), glucagon-like peptide 1 (GLP1), gastric inhibitory polypeptide (GIP), and ghrelin.
Figure 1.
Schematic representation of major biological factors involved in anorexia of aging. Created with BioRender.com, accessed on 11 November 2022.
Abbreviations: IL, interleukin; TNF-α, tumor necrosis factor alpha.
Studies have reported a significant increase in circulating levels of CCK in older adults.16,17 CCK, also called pancreozymin, is an appetite-regulating peptide hormone that stimulates digestion of fat and proteins and regulates satiety. CCK is produced by the enteroendocrine cells of the first segment of the small intestine following the transit of lipids and proteins into the stomach. CCK is considered to be a major player in appetite loss in aging. In particular, a study investigating the effects of infusion of exogenous CCK in young and old individuals indicated that CCK induced a greater satiety effect in older than younger adults.16 Older people also showed higher endogenous levels of CCK during fasting and following low-calorie meals. Despite high levels of CCK, older adults retain sensitivity to the satietogenic effects of CCK, thus indicating that higher CCK activity may compromise appetite in older adults.16 In light of these observations, CCK antagonists have been proposed as therapeutic strategies that may help improve appetite in anorexia of aging.16
Reduced secretion of the orexigenic hormone ghrelin by the enteroendocrine cells of the gastrointestinal mucosa may also have an impact on dietary habits and behaviors of older adults. Ghrelin is secreted by the stomach, and its synthesis and release are triggered by fasting. Ghrelin release is under the control of ghrelin O-acyltransferase (GOAT) that acts on pro-opiomelanocortin neurons and the agouti-related protein neurons/neuropeptide Y-containing cell bodies of the hypothalamic arcuate nucleus. Albeit plasma concentrations of total ghrelin and acyl-ghrelin do not show variations with aging,18 positive effects of the non-peptide, orally active ghrelin agonist anamorelin on appetite stimulation and body composition have been described.19 Mitigation of lack of appetite and muscle loss have also been reported in tumor-bearing mice via the same signaling pathway.20 Results of anamorelin administration to cancer patients with cachexia are mixed.21,22 The possibility to exploit ghrelin agonists as a therapeutic strategy in anorexic older adults warrants further investigation.
The release of ghrelin is negatively modulated by circulating levels of leptin and insulin which may be higher in older adults due to central and peripheral resistance to these hormones.2,5,11,23 Leptin is a hormone released by adipose cells and enterocytes of the small intestine that can signal at the level of central nervous system. Leptin is a marker of energy storage, and high circulating levels of this mediator indicate overt adiposity. Leptin signaling is involved in long-term control of food intake.24 Older adults show higher circulating levels of leptin during fasting compared with younger people and no changes in serum levels of this mediator in post-prandial conditions.25 Although young and old participants were not matched by body mass index (BMI), BMI values were not significantly different between age groups.25 Moreover, while hunger feeling was inhibited after the prandial period in older adults, ghrelin levels remained unchanged.25 A recent study on the effects of short-term administration of the recombinant leptin analogue metreleptin in patients with anorexia nervosa indicated that this molecule was able to favor weight gain and increase appetite, possibly through amelioration of cognitive and emotional symptoms.26 Additional studies are needed to confirm this finding and explore whether the potential benefits of therapeutics based on leptin analogues can also be obtained in anorexia of aging.
Among the so-called hallmarks of aging, chronic low-grade inflammation involving high levels of pro-inflammatory interleukins (ILs) (ie, IL-1 and IL-6) and tumor necrosis factor alpha (TNF-α), is a major determinant. These mediators of inflamm-aging have been implicated in appetite reduction via regulatory pathways operating both at central and peripheral levels.27,28 Their involvement in the reduction of gastric emptying and intestinal motility while conveying anorexigenic signals at the level of the hypothalamic neurons and other orexigenic brain areas has been reported.27–29 Therefore, dysregulation in IL-1, IL-6, and TNF-α signaling can be considered a promoter of nutritional disarrangements and, ultimately, anorexia of aging (Figure 1).29 An association between poor appetite and reduced food intake with inflammation has also been documented in hospitalized older adults, indicating that inflammation may be a relevant mediator in the development of malnutrition in this setting.30 More recently, the growth and differentiation factor 15 (GDF15), a cytokine member of the transforming growth factor beta family, has been associated with anorexia, weight loss, and reduced survival in cancer patients and tumor-bearing rodents.31 Circulating levels of GDF15 increase during aging, which has been linked with reduced physical performance and physical frailty.32 Whether these associations are, at least partly, mediated by the anorexic effect of GDF15 needs to be established. Other mediators such as monoamines (ie, serotonin and norepinephrine), neuropeptides (ie, neuropeptide Y, melanocortin, and corticotropin-releasing factor) have also been included among the central regulators of appetite.33,34 Perturbations in circulating levels of these mediators during aging may contribute to anorexia.33,34
Alterations in gut microbiota have gained increasing attention as per their implication in age-related appetite dysregulation (Figure 1).35 Gut microbes influence a large set of body activities (eg, host–gut functions, endocrine and immune system) via gut–brain crosstalk.36,37 Among the major changes observed in gut microbiota during aging are the shift in taxonomic composition and decrease in microbial richness and diversity which have been associated with frailty and malnutrition.38–41 Variations in gut microbiome composition have also been associated with appetite status in older adults living in the community.42 Associations between alterations in gut microbiota and poor appetite have also been reported in people with eating disorders (ie, anorexia nervosa, bulimia) or cancer,43,44 and bacterial products have been attributed relevant roles in modulating satiety via the activation of arcuate pro-opiomelanocortin neurons.45,46 Metabolic fluctuations over the 24 hours that are observed in physiological systems and thus under the control of intracellular circadian clocks have been reported to be altered during aging and should be taken into account while studying anorexia of aging.47,48 For instance, circadian dysfunction of leptin has been linked to leptin resistance,49 a possible contributor to anorexia of aging.
The modulation of low-grade inflammation has been indicated as a therapeutic target to improve nutritional disarrangements in older people. Although more conclusive studies are needed, a set of nutraceuticals including omega-3 fatty acids and vitamins (ie, vitamin B12 and D) have been tested for their potential to attenuate inflammation.5 Results from a systematic review and meta-analysis have indicated that, more than one specific compound, the Mediterranean dietary patterns, which include foods rich in fat and dense in nutrients administered in a moderate volume, is associated with lower inflammation in older adults and contributes to healthy aging.50,51
Additional studies also evaluating the interrelationship between gut microbiome and appetite in older adults likely acting through brain–gut axis are needed. As a new frontier in the evaluation of these changes, the advent of next-generation sequencing approach enabling the identification of the genetic profile of individuals and how this may contribute/relate to nutritional needs (ie, nutrigenomics) holds promise for the field.
Biomarkers of Anorexia of Aging: Differences and Similarities with Other Age-Associated Conditions
Aging is a major risk factor for the development of multiple diseases, which may have a direct or indirect impact on nutritional status. Indeed, chronic and acute disease conditions (eg, acute and chronic inflammatory conditions, hyperthyroidism, chronic obstructive pulmonary disease, cancer, heart failure, gastrointestinal diseases with or without malabsorption) may induce nutritional disarrangements that may lead to appetite suppression, inflammatory load, malabsorption and micro- and macronutrient deficiencies, and/or increase in body energy needs.2,52
The co-existence of several disease conditions in older people requires consumption of multiple medications that may have negative effects on appetite, food intake, and nutritional status.53 For instance, cancer chemotherapy agents are well-documented inducers of lack of appetite, nausea, and vomiting. Also, therapeutics for rheumatoid arthritis (ie, penicillamine) decrease gastrointestinal tract absorption and zinc bioavailability and cause dysgeusia. Antacids, including aluminum hydroxide and calcium carbonate, may lead to gastrointestinal problems in older persons. Mobility limitations also impact food consumption through interfering with independent grocery activities, cooking, and eating.3,54 Hearing and vision impairments may further reduce the functional abilities of older people55 and, therefore, impinge on their nutritional status.56,57 However, data on the relationship between sensory impairments and anorexia of aging are not conclusive and the subject needs to be further explored.58
As previously mentioned, frailty has been linked to anorexia of aging. Frailty develops independent of chronological aging or specific diseases and can culminate into negative health-related events.59 Conceptualizations of frailty continue to emerge.60 However, its theoretical framework has been developed mainly based on two seminal models. The first, by Fried et al,61 is built on five pre-defined elements: 1) unintentional weight loss; 2) dynapenia; 3) fatigue; 4) poor mobility; and 5) inactive lifestyle.The second, by Rockwood et al,62 is based on the deficit accumulation paradigm and, in its original formulation, includes 70 items. Regardless of the assessment tool, clinical manifestations of frailty arise from multi-system dysregulations.6 In particular, stress-response and metabolic signaling are progressively lost in efficiency as we age63 and, passed a specific threshold, can compromise resilience and impair function.6 The unintentional weight loss that marks frailty is also a feature of anorexia of aging and the two conditions largely overlap. For instance, frailty was observed in over 20% community-dwelling older adults with anorexia, while only 8.4% of the older people without anorexia were frail.8 In another study, the association between frailty and malnutrition was explored in community-dwelling older people from the Singapore Longitudinal Aging Study 1.64 Prefrailty or frailty was associated with malnutrition in 23% of the participants. Notably, frail participants with malnutrition had higher rates of disability, poor quality of life, and mortality compared with those without nutritional problems.64 Finally, anorexia of aging has also been associated with sarcopenia in old community-dwellers.65
A set of cellular processes originally introduced as pillars of aging (ie, genomic and epigenetic instability, telomere attrition, altered nutrient sensing, loss of proteostasis, mitochondrial dysfunction, cellular senescence, decreased stemness, and altered intercellular signaling) are now recognized as mechanisms contributing to the pathophysiology of frailty and sarcopenia.63 Efforts have been made towards the incorporation of as many markers as possible pertaining to these processes in complex statistical models that may help identify pathways involved in the pathophysiology of frailty and sarcopenia.66,67 With a similar intent, a recent systematic review and meta-analysis on shared biomarkers between frailty and sarcopenia in older adults was performed.68 As a result of this analysis, biomarkers belonging to inflammatory, metabolic, hematologic pathways were retrieved as the most relevant mediators associated with frailty and sarcopenia that may explain their clinical overlap.68
The early identification of older adults at risk of or with malnutrition is crucial to mitigate the impact nutritional deficits on health status and quality of life. The analysis of metabolic mediators associated with anorexia of aging through comprehensive approaches like those tested in other geriatric conditions (ie, frailty and sarcopenia) may provide great support.
Conclusion
Anorexia is a highly prevalent condition among older adults, and its multifactorial etiology includes a set of metabolic changes that accompany the aging process. Circulating mediators, such as cholecystokinin, ghrelin, leptin, and inflammatory and microbial mediators of gut dysbiosis, have been proposed as biomarkers for the condition and may help identify anorexia of aging at an early stage and develop personalized nutritional counseling. Studies investigating the interrelationship between gut microbiota and appetite regulation in older adults as well as establishing whether the genetic background may influence the nutritional needs are highly sought after.
Acknowledgments
This work was supported by the Università Cattolica del Sacro Cuore [D1.2020 and D1.2022], the Italian Ministry of Health [Ricerca Corrente 2022], and the nonprofit research foundation “Centro Studi Achille e Linda Lorenzon” [N/A].
Disclosure
R.C. reports personal fees from Abbott, personal fees from Nutricia, outside the submitted work. E.M. has received consulting honoraria from Abbott, Nestlè and Pfizer. The other authors report no conflicts of interest in this work.
References
- 1.Landi F, Calvani R, Tosato M, et al. Anorexia of aging: risk factors, consequences, and potential treatments. Nutrients. 2016;8(2):69. doi: 10.3390/nu8020069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landi F, Picca A, Calvani R, Marzetti E. Anorexia of Aging. Clin Geriatr Med. 2017;33(3):315–323. doi: 10.1016/j.cger.2017.02.004 [DOI] [PubMed] [Google Scholar]
- 3.Landi F, Russo A, Liperoti R, et al. Anorexia, physical function, and incident disability among the frail elderly population: results from the ilSIRENTE study. J Am Med Dir Assoc. 2010;11(4):268–274. doi: 10.1016/j.jamda.2009.12.088 [DOI] [PubMed] [Google Scholar]
- 4.Kiesswetter E, Pohlhausen S, Uhlig K, et al. Malnutrition is related to functional impairment in older adults receiving home care. J Nutr Health Aging. 2013;17(4):345–350. doi: 10.1007/s12603-012-0409-1 [DOI] [PubMed] [Google Scholar]
- 5.Dent E, Hoogendijk EO, Wright ORL. New insights into the anorexia of ageing. Curr Opin Clin Nutr Metab Care. 2018;22(1):1. doi: 10.1097/MCO.0000000000000525 [DOI] [PubMed] [Google Scholar]
- 6.Fried LP, Cohen AA, Xue Q-L, Walston J, Bandeen-Roche K, Varadhan R. The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat Aging. 2021;1(1):36–46. doi: 10.1038/S43587-020-00017-Z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cederholm T, Barazzoni R, Austin P, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr. 2017;36(1):49–64. doi: 10.1016/j.clnu.2016.09.004 [DOI] [PubMed] [Google Scholar]
- 8.Tsutsumimoto K, Doi T, Makizako H, et al. Aging-related anorexia and its association with disability and frailty. J Cachexia Sarcopenia Muscle. 2018;9(5):834–843. doi: 10.1002/JCSM.12330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Donini LM, Poggiogalle E, Piredda M, et al. Anorexia and eating patterns in the elderly. PLoS One. 2013;8(5):e63539. doi: 10.1371/journal.pone.0063539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prell T, Perner C. Disease specific aspects of malnutrition in neurogeriatric patients. Front Aging Neurosci. 2018;10:80. doi: 10.3389/fnagi.2018.00080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wysokiński A, Sobów T, Kłoszewska I, Kostka T. Mechanisms of the anorexia of aging—a review. Age. 2015;37(4):9821. doi: 10.1007/s11357-015-9821-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanford AM. Anorexia of aging and its role for frailty. Curr Opin Clin Nutr Metab Care. 2017;20(1):54–60. doi: 10.1097/MCO.0000000000000336 [DOI] [PubMed] [Google Scholar]
- 13.Hoogendijk EO, Flores Ruano T, Martínez-Reig M, et al. Socioeconomic position and malnutrition among older adults: results from the FRADEA study. J Nutr Health Aging. 2018;22(9):1086–1091. doi: 10.1007/s12603-018-1061-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dent E. Anorexia of aging and avoidant/restrictive food intake disorder. J Am Med Dir Assoc. 2017;18(5):449–450. doi: 10.1016/j.jamda.2017.01.020 [DOI] [PubMed] [Google Scholar]
- 15.Sturm K, Parker B, Wishart J, et al. Energy intake and appetite are related to antral area in healthy young and older subjects. Am J Clin Nutr. 2004;80(3):656–667. doi: 10.1093/ajcn/80.3.656 [DOI] [PubMed] [Google Scholar]
- 16.MacIntosh CG, Morley JE, Wishart J, et al. Effect of exogenous cholecystokinin (CCK)-8 on food intake and plasma CCK, leptin, and insulin concentrations in older and young adults: evidence for increased CCK activity as a cause of the anorexia of aging. J Clin Endocrinol Metab. 2001;86(12):5830–5837. doi: 10.1210/JCEM.86.12.8107 [DOI] [PubMed] [Google Scholar]
- 17.Sturm K, MacIntosh CG, Parker BA, Wishart J, Horowitz M, Chapman IM. Appetite, food intake, and plasma concentrations of cholecystokinin, ghrelin, and other gastrointestinal hormones in undernourished older women and well-nourished young and older women. J Clin Endocrinol Metab. 2003;88(8):3747–3755. doi: 10.1210/JC.2002-021656 [DOI] [PubMed] [Google Scholar]
- 18.Hickson M, Moss C, Dhillo WS, Bottin J, Frost G. Increased peptide YY blood concentrations, not decreased acyl-ghrelin, are associated with reduced hunger and food intake in healthy older women: preliminary evidence. Appetite. 2016;105:320–327. doi: 10.1016/J.APPET.2016.06.002 [DOI] [PubMed] [Google Scholar]
- 19.Howick K, Griffin BT, Cryan JF, Schellekens H. From belly to brain: targeting the ghrelin receptor in appetite and food intake regulation. Int J Mol Sci. 2017;18(2):273. doi: 10.3390/IJMS18020273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miyake M, Hori S, Itami Y, et al. Supplementary oral anamorelin mitigates anorexia and skeletal muscle atrophy induced by gemcitabine plus cisplatin systemic chemotherapy in a mouse model. Cancers. 2020;12(7):1–17. doi: 10.3390/CANCERS12071942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Temel JS, Abernethy AP, Currow DC, et al. Anamorelin in patients with non-small-cell lung cancer and cachexia (ROMANA 1 and ROMANA 2): results from two randomised, double-blind, phase 3 trials. Lancet Oncol. 2016;17(4):519–531. doi: 10.1016/S1470-2045(15)00558-6 [DOI] [PubMed] [Google Scholar]
- 22.Fonseca GWPD, von Haehling S. An overview of anamorelin as a treatment option for cancer-associated anorexia and cachexia. Expert Opin Pharmacother. 2021;22(7):889–895. doi: 10.1080/14656566.2021.1873954 [DOI] [PubMed] [Google Scholar]
- 23.Soenen S, Chapman IM. Body weight, anorexia, and undernutrition in older people. J Am Med Dir Assoc. 2013;14(9):642–648. doi: 10.1016/j.jamda.2013.02.004 [DOI] [PubMed] [Google Scholar]
- 24.Di Francesco V, Fantin F, Omizzolo F, et al. The anorexia of aging. Dig Dis. 2007;25(2):129–137. doi: 10.1159/000099477 [DOI] [PubMed] [Google Scholar]
- 25.Di Francesco V, Zamboni M, Zoico E, et al. Unbalanced serum leptin and ghrelin dynamics prolong postprandial satiety and inhibit hunger in healthy elderly: another reason for the “anorexia of aging.”. Am J Clin Nutr. 2006;83(5):1149–1152. doi: 10.1093/AJCN/83.5.1149 [DOI] [PubMed] [Google Scholar]
- 26.Milos G, Antel J, Kaufmann LK, et al. Short-term metreleptin treatment of patients with anorexia nervosa: rapid on-set of beneficial cognitive, emotional, and behavioral effects. Transl Psychiatry. 2020;10(1):303. doi: 10.1038/S41398-020-00977-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yeh -S-S, Blackwood K, Schuster MW. The cytokine basis of cachexia and its treatment: are they ready for prime time? J Am Med Dir Assoc. 2008;9(4):219–236. doi: 10.1016/j.jamda.2008.01.003 [DOI] [PubMed] [Google Scholar]
- 28.Laviano A, Meguid MM, Inui A, Muscaritoli M, Rossi-Fanelli F. Therapy insight: cancer anorexia–cachexia syndrome—when all you can eat is yourself. Nat Clin Pract Oncol. 2005;2(3):158–165. doi: 10.1038/ncponc0112 [DOI] [PubMed] [Google Scholar]
- 29.Molfino A, Rossi-Fanelli F, Laviano A. The interaction between pro-inflammatory cytokines and the nervous system. Nat Rev Cancer. 2009;9(3):224. doi: 10.1038/NRC2507-C1 [DOI] [PubMed] [Google Scholar]
- 30.Sieske L, Janssen G, Babel N, Westhoff TH, Wirth R, Pourhassan M. Inflammation, appetite and food intake in older hospitalized patients. Nutrients. 2019;11(9):1986. doi: 10.3390/NU11091986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Breit SN, Brown DA, Tsai VWW. The GDF15-GFRAL pathway in health and metabolic disease: friend or foe? Annu Rev Physiol. 2021;83:127–151. doi: 10.1146/ANNUREV-PHYSIOL-022020-045449 [DOI] [PubMed] [Google Scholar]
- 32.Semba RD, Gonzalez-Freire M, Tanaka T, et al. Elevated plasma growth and differentiation factor 15 is associated with slower gait speed and lower physical performance in healthy community-dwelling adults. J Gerontol a Biol Sci Med Sci. 2020;75(1):175–180. doi: 10.1093/gerona/glz071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morley JE. Peptides and aging: their role in anorexia and memory. Peptides. 2015;72:112–118. doi: 10.1016/j.peptides.2015.04.007 [DOI] [PubMed] [Google Scholar]
- 34.Morley JE. Anorexia of ageing: a key component in the pathogenesis of both sarcopenia and cachexia. J Cachexia Sarcopenia Muscle. 2017;8(4):523–526. doi: 10.1002/jcsm.12192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Salazar N, Valdés-Varela L, González S, Gueimonde M, de Los Reyes-Gavilán CG. Nutrition and the gut microbiome in the elderly. Gut Microbes. 2017;8(2):82–97. doi: 10.1080/19490976.2016.1256525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Postler TS, Ghosh S. Understanding the holobiont: how microbial metabolites affect human health and shape the immune system. Cell Metab. 2017;26(1):110–130. doi: 10.1016/j.cmet.2017.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Calvani R, Picca A, Lo monaco MR, Landi F, Bernabei R, Marzetti E. Of microbes and minds: a narrative review on the second brain aging. Front Med. 2018;5:53. doi: 10.3389/fmed.2018.00053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haran JP, Bucci V, Dutta P, Ward D, McCormick B. The nursing home elder microbiome stability and associations with age, frailty, nutrition and physical location. J Med Microbiol. 2018;67(1):40–51. doi: 10.1099/jmm.0.000640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jackson M, Jeffery IB, Beaumont M, et al. Signatures of early frailty in the gut microbiota. Genome Med. 2016;8(1):8. doi: 10.1186/s13073-016-0262-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Picca A, Ponziani FR, Calvani R, et al. Gut microbial, inflammatory and metabolic signatures in older people with physical frailty and sarcopenia: results from the BIOSPHERE study. Nutrients. 2019;12(1):65. doi: 10.3390/nu12010065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Picca A, Fanelli F, Calvani R, et al. Gut dysbiosis and muscle aging: searching for novel targets against sarcopenia. Mediators Inflamm. 2018;2018:1–15. doi: 10.1155/2018/7026198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cox NJ, Bowyer RCE, Ni Lochlainn M, Wells PM, Roberts HC, Steves CJ. The composition of the gut microbiome differs among community dwelling older people with good and poor appetite. J Cachexia Sarcopenia Muscle. 2021;12(2):368–377. doi: 10.1002/JCSM.12683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Molfino A, Amabile MI, Imbimbo G, et al. Plasma enterobacterial ClpB levels and ClpB- and α-MSH-reactive immunoglobulins in lung cancer patients with and without anorexia. Nutrition. 2020;78:110952. doi: 10.1016/J.NUT.2020.110952 [DOI] [PubMed] [Google Scholar]
- 44.Breton J, Legrand R, Akkermann K, et al. Elevated plasma concentrations of bacterial ClpB protein in patients with eating disorders. Int J Eat Disord. 2016;49(8):805–808. doi: 10.1002/EAT.22531 [DOI] [PubMed] [Google Scholar]
- 45.Fetissov SO. Role of the gut microbiota in host appetite control: bacterial growth to animal feeding behaviour. Nat Rev Endocrinol. 2017;13(1):11–25. doi: 10.1038/NRENDO.2016.150 [DOI] [PubMed] [Google Scholar]
- 46.Breton J, Tennoune N, Lucas N, et al. Gut commensal E. coli proteins activate host satiety pathways following nutrient-induced bacterial growth. Cell Metab. 2016;23(2):324–334. doi: 10.1016/J.CMET.2015.10.017 [DOI] [PubMed] [Google Scholar]
- 47.Chaudhari A, Gupta R, Makwana K, Kondratov R. Circadian clocks, diets and aging. Nutr Heal Aging. 2017;4:101–112. doi: 10.3233/NHA-160006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hood S, Amir S. The aging clock: circadian rhythms and later life. J Clin Invest. 2017;127(2):437–446. doi: 10.1172/JCI90328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kettner NM, Mayo SA, Hua J, Lee C, Moore DD, Fu L. Circadian dysfunction induces leptin resistance in mice. Cell Metab. 2015;22(3):448–459. doi: 10.1016/j.cmet.2015.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wu PY, Chen KM, Tsai WC. The Mediterranean dietary pattern and inflammation in older adults: a systematic review and meta-analysis. Adv Nutr. 2021;12(2):363–373. doi: 10.1093/ADVANCES/NMAA116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Coelho-Júnior HJ, Trichopoulou A, Panza F. Cross-sectional and longitudinal associations between adherence to Mediterranean diet with physical performance and cognitive function in older adults: a systematic review and meta-analysis. Ageing Res Rev. 2021;70:101395. doi: 10.1016/J.ARR.2021.101395 [DOI] [PubMed] [Google Scholar]
- 52.Morley JE. Pathophysiology of the anorexia of aging. Curr Opin Clin Nutr Metab Care. 2013;16(1):27–32. doi: 10.1097/MCO.0b013e328359efd7 [DOI] [PubMed] [Google Scholar]
- 53.Fávaro-Moreira NC, Krausch-Hofmann S, Matthys C, et al. Risk factors for malnutrition in older adults: a systematic review of the literature based on longitudinal data. Adv Nutr. 2016;7(3):507–522. doi: 10.3945/an.115.011254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Landi F, Lattanzio F, Dell’Aquila G, et al. Prevalence and potentially reversible factors associated with anorexia among older nursing home residents: results from the ULISSE project. J Am Med Dir Assoc. 2013;14(2):119–124. doi: 10.1016/j.jamda.2012.10.02255 [DOI] [PubMed] [Google Scholar]
- 55.Zhao Y, Ding Q, Lin T, et al. Combined vision and hearing impairment is associated with frailty in older adults: results from the West China Health and Aging Trend study. Clin Interv Aging. 2022;17:675–683. doi: 10.2147/CIA.S362191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Muurinen SM, Soini HH, Suominen MH, Saarela RKT, Savikko NM, Pitkälä KH. Vision impairment and nutritional status among older assisted living residents. Arch Gerontol Geriatr. 2014;58(3):384–387. doi: 10.1016/J.ARCHGER.2013.12.002 [DOI] [PubMed] [Google Scholar]
- 57.O’Keeffe M, Kelly M, O’Herlihy E, et al. Potentially modifiable determinants of malnutrition in older adults: a systematic review. Clin Nutr. 2019;38(6):2477–2498. doi: 10.1016/J.CLNU.2018.12.007 [DOI] [PubMed] [Google Scholar]
- 58.Mathieu ME, Reid RER, King NA. Sensory profile of adults with reduced food intake and the potential roles of nutrition and physical activity interventions. Adv Nutr. 2019;10(6):1120–1125. doi: 10.1093/ADVANCES/NMZ044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cesari M, Calvani R, Marzetti E. Frailty in older persons. Clin Geriatr Med. 2017;33(3):293–303. doi: 10.1016/J.CGER.2017.02.002 [DOI] [PubMed] [Google Scholar]
- 60.Morley JE, Vellas B, Abellan van Kan G, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–397. doi: 10.1016/J.JAMDA.2013.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. Journals Gerontol Ser a Biol Sci Med Sci. 2001;56(3):M146–M157. doi: 10.1093/gerona/56.3.M146 [DOI] [PubMed] [Google Scholar]
- 62.Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62(7):722–727. doi: 10.1093/gerona/62.7.722 [DOI] [PubMed] [Google Scholar]
- 63.Guerville F, De Souto Barreto P, Ader I, et al. Revisiting the hallmarks of aging to identify markers of biological age. J Prev Alzheimers Dis. 2020;7(1):56–64. doi: 10.14283/JPAD.2019.50 [DOI] [PubMed] [Google Scholar]
- 64.Wei K, Nyunt MSZ, Gao Q, Wee SL, Yap KB, Ng TP. Association of frailty and malnutrition with long-term functional and mortality outcomes among community-dwelling older adults: results from the Singapore Longitudinal Aging Study 1. JAMA Netw open. 2018;1(3):e180650. doi: 10.1001/JAMANETWORKOPEN.2018.0650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Landi F, Liperoti R, Russo A, et al. Association of anorexia with sarcopenia in a community-dwelling elderly population: results from the ilSIRENTE study. Eur J Nutr. 2013;52(3):1261–1268. doi: 10.1007/S00394-012-0437-Y [DOI] [PubMed] [Google Scholar]
- 66.Rodriguez-Mañas L, Araujo de Carvalho I, Bhasin S, et al. ICFSR task force perspective on biomarkers for sarcopenia and frailty. J Frailty Aging. 2020;9(1):4–8. doi: 10.14283/jfa.2019.32 [DOI] [PubMed] [Google Scholar]
- 67.Gomez-Cabrero D, Walter S, Abugessaisa I, et al. A robust machine learning framework to identify signatures for frailty: a nested case-control study in four aging European cohorts. GeroScience. 2021;43(3):1317–1329. doi: 10.1007/S11357-021-00334-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Picca A, Coelho-Junior HJ, Calvani R, Marzetti E, Vetrano DL. Biomarkers shared by frailty and sarcopenia in older adults: a systematic review and meta-analysis. Ageing Res Rev. 2022;73:101530. doi: 10.1016/J.ARR.2021.101530 [DOI] [PubMed] [Google Scholar]