Abstract
Transverse vaginal septum is a congenital anomaly in which a membrane obstructs the vagina. This can be partial or complete in type. Although rare, it presents peculiar challenges in symptomatology, diagnosis, and ultimate management. To our knowledge, we are the first to report a shortest vaginoplasty-conception interval following successful repair of previously failed repair of partial transverse vaginal septum.
A 28-year-old Nigerian married nulliparous lady who presented to us with history of inability of penile–vaginal penetration with the presence of normal menstrual flow after two previous failed attempts at repair. She had a vaginoplasty with placement of a vaginal mold to prevent stenosis. She was subsequently able to have successful sexual intercourse and achieved pregnancy after 2 months, without recurrence of vaginal stenosis.
When transverse vaginal septum is encountered in a married nullipara, a thorough clinical evaluation of the viability and feasibility of a vaginoplasty should be made during the first surgery. If repeated failed repair occurs, as in our case, we recommend meticulous and experienced surgical attention from the outset. The originality in this report lies in the very short period between repair and successful conception. Thus, we obtained satisfactory short-term clinical outcome of successful conception at the 2 months follow-up.
Keywords: Mullerian anomaly, pregnancy, vaginoplasty, vaginal septum, vaginal stenosis
Introduction
Transverse vaginal septum is a rare congenital abnormality in which an obstructing membrane bridges the vagina. It is said to be a mullerian anomaly, resulting from the failure of fusion and recanalization of the urogenital sinus and the mullerian ducts.1 The incidence is between 1/2100 and 1/7200.2 The obstructing septum is usually about 1–2 cm thick and may be complete or incomplete.3
The presentation depends on whether the septum is perforate or imperforate in type. Patients with imperforate septum may present with primary amenorrhea, cyclical pelvic pain, inability to consummate marriage with sexual intercourse, and primary infertility if left untreated; while those with perforate septum present more with difficulty with intercourse and primary infertility if left untreated.1 This, of course, is with the attendant psychological trauma from personality complexes to marital misunderstanding. Also, those with perforate septum presents peculiar diagnostic challenge as they may be asymptomatic, or presenting with dyspareunia or infertility.4 The diagnosis is made from a careful clinical history and perineal examination, while the membrane thickness and depth is further characterized with the use of ultrasound and magnetic resonance imaging.5 The treatment is surgical, which can be achieved via the vaginal, laparoscopic, or an abdominoperineal approach with a possible risk of stenosis after treatment, particularly in post-pubertal patients.6,7 We report a first case of a shortest vaginoplasty-conception interval following successful repair of partial vaginal septum after two-failed repair attempts. The learning points are that lessons learnt from the wrong doings or mishaps of the previous failed septum repairs, which included the meticulous postoperative care with serial dilatation and early resumption of coitus to enhance the successful repair and earlier conception. These lessons ultimately led to success we recorded since we avoided repeating the mistakes of others in the past.
Case presentation
The patient is a 28-year-old woman married for 6 months, who presented with complaint of inability of penile–vaginal penetration during sexual intercourse. Patient has not achieved coitarche prior to marriage. She has normal regular menstrual cycle with moderate flow. She had hysteroscopy 6 months prior to presentation. She also had vaginoplasty procedures twice in two different private hospitals, with no improvement. The initial diagnosis of partial transverse vaginal septum was made following her marital union, when she was 26 years old. The first failed repair was at the time the patient was 26 years and the second failed attempt was when she was 27 years old. The two attempted repairs were via vaginal routes. The two procedures were said to have failed because there were no scheduled postoperative vaginal dilatations after discharge from the hospital. There was no other associated congenital anomaly, and there was no family history of similar problem. Her past medical and psychosocial history was unremarkable.
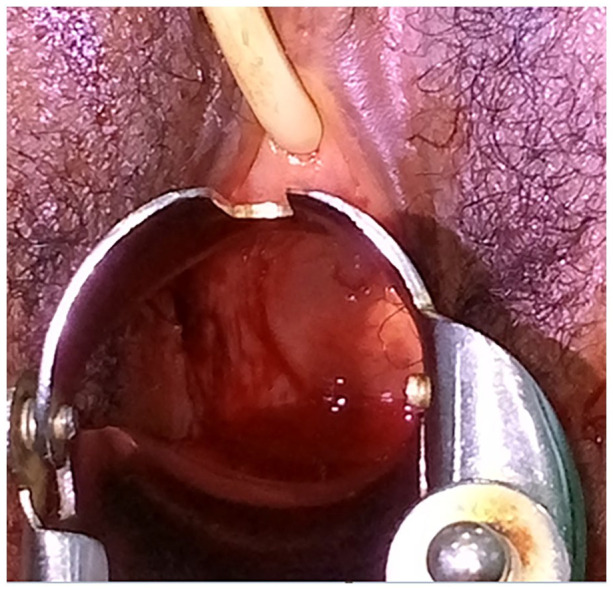
Physical examination (Figure 1) revealed a lady with normal facie and body build. She had normal secondary sexual characteristics, with no breast masses. Perineal examination revealed well-developed external genitalia. Vaginal examination revealed a shallow vagina, about 1 cm deep to the hymen, with a spanning septum which has a pinhole at the 12 O’clock position.
Figure 1.

The transverse vaginal septum.
Except for the findings in the vagina, the ultrasound (perineal, transrectal, or abdominopelvic) showed normal findings. There was no hematocolpos or hydrocolpos.
Patient eventually had a vaginoplasty under spinal anesthesia after obtaining a written informed consent for surgery. Patient was catheterized per urethra for easy identification of the urethra while a pre-procedure rectal examination was done. Thereafter, a transverse incision was made with number 10 blade at the mid-plane of the septum, which was extended upward by both sharp and blunt dissection with guidance of urinary catheter anteriorly and a finger along anterior wall of the rectum. Eventually, the proximal aspect of the septum was reached, and the septum was carefully excised, creating a continuity with the rest of the vaginal tract (Figure 2). There were some difficulties in tissue dissections during the surgery due to the two previous failed surgical procedures. Serial vaginal dilators were used to widen the vagina to accommodate a regular penile shaft.
Figure 2.
After resection of vaginal septum.
An improvised vaginal mold (Figure 3) was constructed with the barrel of a 50-ml syringe wrapped with a sterile guaze, following which a male condom was worn over it and then a sufratulle vaseline gauze was circumferentially applied around the gauzed syringe barrel. The mold was gently inserted into the vagina wall as far reaching as possible (Figure 4). The essence of the vaginal mold was to prevent possible vaginal stenosis during healing.
Figure 3.

The improvised vaginal mold.
Figure 4.

In situ improvised vaginal mold.
She was maintained on rectal diclofenac and oral antibiotics while the mold was changed after 72 h. The mold was eventually removed on the 5th day postoperation. The patient was counseled to maintain regular coitus alongside use of vaginal dilators of size 17 mm/18 mm to obviate occurrence of gynetresia. She was discharged and presented 2 months after the procedure with symptoms suggestive of pregnancy. Bedside ultrasound confirmed an intrauterine fetus at 6 weeks plus 5 days gestation. She was counseled on findings and was transferred to the obstetric clinic. Following this, the patient delivered a healthy female baby with birth weight of 3.0 kg through cesarean section at term. There was no birth defect or birth anomaly on the baby.
Discussion
Transverse vaginal septum is a rare type of Mullerian anomaly. The sinovaginal bulbs from the urogenital sinus meet the Müllerian tubercle on the caudal end of the Müllerian ducts to form the vaginal plate, which is then canalized to form the lower part of the vagina by the fifth month of pregnancy.8,9 But when there is a failure in the canalization of the vaginal plate at the point or in the fusion of the urogenital sinus to the Müllerian duct, a transverse vaginal septa results.1,10
This lesion can occur in isolation or in association with other congenital anomalies particularly those of the genitourinary and anorectal regions such as vesicovaginal fistula, hypoplastic kidney, hydronephrosis, bicornuate uterus, persistent cloaca, and Hirschsprung disease.11 Other rarer associations include musculoskeletal defects, coarctation of the aorta and atrial septal defect.12 The etiology as with other congenital anomalies remains unknown; however, it has been associated with maternal use of Thalidomide and Stilbesterol, while it has also been associated with autosomal recessive transmission.3,13
The symptomatology differs based on whether the septum is perforate or imperforate. In imperforate septum, there is pooling of menstrual blood above the septum and patients present with primary amenorrhea, cyclical pelvic pain, dyspareunia, and dysmenorrhea around the age of menarche. The diagnosis is usually late, more in the adolescents. An incomplete septum which is initially asymptomatic, is usually discovered after adolescence when patient presents with infertility or dyspareunia since secretions and menstrual blood flow from vagina through the small opening.14
Careful clinical history and perineal examination is important in diagnosis, though the condition can still be missed if the septum occurs in mid or high location. Where it is visible in the lower vagina, it must be differentiated from imperforate hymen, which transilluminates.9,15 Magnetic resonance imaging has been reported as the gold standard in the diagnosis of transverse vaginal septum, though in resource-poor settings, clinical assessment and ultrasound may suffice due their cost effectiveness.16 Ultrasound demonstrates the septum as well as any associated hematocolpos.
The thickness and the location of transverse vaginal septum/septa is/are important factor(s) that determine the surgical management.6 Low thin septae and thin perforate septae are less complex and can be resected vaginally with a low complication rate while the high, thick ones will benefit more from an abdominoperineal approach because of the risk of injury to adjacent cervix if approached solely from the vagina.6 Some researchers have also reported great success with laparoscopic approach and this finds particular importance in cultures where the preservation of the hymen is revered.5
Different techniques have been described for the low thin septum. Apart from the simple excision of the septum, which is the commonest approach, (a technique used for our patient), the septum can also be managed with a cruciate incision, then closed transversely (the Grünberger method) or a Z plasty can be used.1 The “pull through and push through” techniques described by Van Bijsterveldt and group with other modifications have also been shown to offer good outcome, especially in thick septum with its attendant common association with stenosis.17
The major post-management challenge remains the possible development of vaginal stenosis. Many methods have been used to prevent this complication. Manual stretching of the excised septal area has been described, as well as the use of vaginal dilators, dilatation balloon and other improvised materials (as used in our patient).3 Some scholars have also described the use of a cut gut segment to bridge the vaginal gap, and skin grafts as well as amniotic membrane-coated vaginal mold have all been tried.6,18 The aim is to encourage healing by epitheliosis rather than by fibrosis, which will lead to gynetresia. In our index patient, we improvised with the barrel of a 50-ml syringe, wrapped with cotton gauze and enveloped with a male condom and then wrapped with sufratulle gauze, which gave a very favorable outcome.
Regardless of etiology, this complication could be prevented by performing a meticulous surgery without sequelae. However, if it occurs, a meticulous post-surgical care and follow-up should be made so that the success of the repair of the septum can be ensured during the first surgery. This could avoid a subsequent complication and a multiple repeat operation, as was encountered in our case.19,20
To the best of our knowledge, we have not found any report in the literature of a shortest vaginoplasty-conception interval following successful repair of partial transverse vaginal septum, after multiple failed repair attempts. In a previous case report by Sohail et al. on successful pregnancy following after transverse vaginal septum resection, the conception occurred 7 months following repair, and coitus was said to have resumed 3 months after surgery.18
Conclusion
Transverse vaginal septum though a rare pathology is associated with physical and psychosocial effects. Adequate diagnosis and early treatment can restore patient’s self-confidence. The major aims of management are to restore the quality of life, restore marital harmony, and even lead to a successful vaginal delivery of a healthy neonate. It is imperative to ensure a free stenotic healing outcome but a re-epithelization of the vaginal mucosa. Thus, we obtained satisfactory short-term clinical outcome of successful conception at the 2-month follow-up. The originality in this report lies in the very short period between repair and successful conception.
As in our case, the obstructive vaginal anomalies such as transverse vaginal septum may infrequently present in infancy or childhood with hydrocolpos and/or hydrometra. They typically go unrecognized until presentation with amenorrhea, coital difficulty, or infertility in puberty. Our patient subsequently had elective cesarean section so as to avoid obstetrics complications like obstructed labor and laceration of vagina.
Acknowledgments
The authors would like to thank the Department of Obstetrics and Gynecology at Nnamdi Azikiwe University Teaching Hospital, Nnewi, Nigeria, and staff of Rembo Specialist Hospital, Nnewi, Nigeria.
Footnotes
Author contributions: G.U.E., E.C.I., and O.A.O. conceived, supervised the study, and performed the surgery. E.P.I., C.N.I., and T.O.C. analyzed data. C.C.O., K.C.O., and B.C.O. wrote the manuscript. E.P.I. and G.U.E. made manuscript revisions. All authors reviewed the results and approved of the final version of the manuscript.
Consent for publication: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed consent: A written informed consent was obtained from the patient to allow the reporting of this case as well as the use of her intraoperative picture.
ORCID iDs: George Uchenna Eleje  https://orcid.org/0000-0002-0390-2152
https://orcid.org/0000-0002-0390-2152
Boniface Chukwuneme Okpala  https://orcid.org/0000-0003-1693-373X
https://orcid.org/0000-0003-1693-373X
References
- 1. Bello S, Au M, Ja G, et al. Management and outcome of transverse vaginal septum in a Nigerian tertiary health institution. Sch Int J Obstet Gynec 2021; 4(7): 291–296. [Google Scholar]
- 2. Kamal EM, Lakhdar A, Baidada A. Management of a transverse vaginal septum complicated with hematocolpos in an adolescent girl: case report. Int J Surg Case Rep 2020; 77: 748–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Adejumo R, Akande TS, Aminu YK, et al. Management of transverse septum in a low resource setting: a case report 2020; 4(104): 1–4. [Google Scholar]
- 4. Esteban R, Losa J, Celis F, et al. The McKusick-Kaufman syndrome: a report of 5 new cases, including a male. An Esp. Pediatr 1996; 44(5): 493–495. [PubMed] [Google Scholar]
- 5. Scutiero G, Greco P, Iannone P, et al. Management of transverse vaginal septum by vaginoscopic resection: hymen conservative technique. Rev Bras Ginecol Obstet 2018; 40(10): 642–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Williams CE, Nakhal RS, Hall- Craggs MA, et al. Transverse vaginal septae: management and long-term outcomes. BJOG 2014; 121: 1653–1659. [DOI] [PubMed] [Google Scholar]
- 7. Rock JA. Surgery for anomalies of the müllerian ducts. In: JA En Rock, JD Thompson. (eds) Telinde’s operative gynecology. 8th ed. Philadelphia, PA: Lippincott-Raven, 1997, pp. 687–729. [Google Scholar]
- 8. Coskun A, Okur N, Ozdemir O, et al. Uterus didelphys with an obstructed unilateral vagina by a transverse vaginal septum associated with ipsilateral renal agenesis, duplication of inferior vena cava, high-riding aortic bifurcation, and intestinal malrotation: a case report. Fertil Steril 2008; 90(05): 2006.e9–2006.e11. [DOI] [PubMed] [Google Scholar]
- 9. Gray SW, Skandalakis JE, Broecker BH. Female reproductive system. In: JE Skandalakis, SW Gray. (eds) Embryology for surgeons. 2nd ed. Baltimore, MD: Lippincott Williams & Wilkins, 1994; 816–847. [Google Scholar]
- 10. Moore KL, Persaud TVN. The developing human: clinically oriented embryology. 7th ed. Philadelphia, PA: WB Saunders, 2003. [Google Scholar]
- 11. Ameh EA, Mshelbwala PM, Ameh N. Congenital vaginal obstruction in neonates and infants: recognition and management. J Pediatr Adolesc Gynecol 2011; 24(2): 74–78. [DOI] [PubMed] [Google Scholar]
- 12. Rock JA, Zacur HA, Dlugi AM, et al. Pregnancy success following surgical correction of imperforate hymen and complete transverse vaginal septum. Obstet Gynecol 1982; 59(4): 448–451. [PubMed] [Google Scholar]
- 13. Deligeoroglou E, Iavazzo C, Sofoudis C, et al. Management of hematocolpos in adolescents with transverse vaginal septum. Arch Gynecol Obstet 2012; 285(04): 1083–1087. [DOI] [PubMed] [Google Scholar]
- 14. Sasikala R, Priyadharshini M, Poomalar GK. Perforated transverse vaginal septum: a rare case report. Int J Reprod Contracept Obstet Gynecol 2015; 4(4): 1217–1219. [Google Scholar]
- 15. Walker DK, Salibian RA, Salibian AD, et al. Overlooked disease of the vagina: a directed anatomic-pathologic approach for imaging assessment. Radiographics 2011; 31(6): 1583–1598. [DOI] [PubMed] [Google Scholar]
- 16. Burgis J. Obstructive mullerian anomalies: case report, diagnosis, and management. Am J Obstet Gynecol 2001; 185(2): 338–344. [DOI] [PubMed] [Google Scholar]
- 17. van Bijsterveldt C, Willemsen W. Treatment of patients with a congenital transversal vaginal septum or a partial aplasia of the vagina. The vaginal pull-through versus the push-through technique. J Pediatr Adolesc Gynecol 2009; 22(3): 157–161. [DOI] [PubMed] [Google Scholar]
- 18. Sohail R, Malik A, Ashraf A, et al. Successful pregnancy outcome after septum resection and use of amnion graft in patient with high transverse vaginal septum. BMJ Case Rep 2019; 12: e228769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Eleje GU, Udigwe GO, Obiagwu HI, et al. Perforated transverse vagina septum associated with primary infertility: diagnostic and management challenges in a low-income setting. JMCRR 2020; 3(12): 792–796. [Google Scholar]
- 20. Mentessidou A, Mirilas P. Surgical disorders in pediatric and adolescent gynecology: vaginal and uterine anomalies. Int J Gynaecol Obstet. Epub ahead of print 26 July 2022. DOI: 10.1002/ijgo.14362. [DOI] [PubMed] [Google Scholar]


