Abstract
Background and Aims
Parent–child interaction therapy (PCIT) is an evidence-based behavioral parent training program designed for preschool-age children that emphasizes supporting parent–child interaction patterns to improve child behavior and enhance the quality of parent–child relationships. PCIT has been deemed efficacious in treating children with disruptive behavior disorders, and recent studies have shown promising results utilizing aspects of PCIT with children with autism spectrum disorder (ASD), but none of these studies applied the entire PCIT intervention per manual protocol. The present study is the first to test the efficacy of PCIT, without modification, with families of preschool-age children with ASD without comorbid behavioral difficulties.
Methods
This study employed a single-subject multiple-probe design to evaluate the efficacy of PCIT with four families with children with ASD between the ages of 2 and 4 years old (M = 40 months) over a 4-month period.
Results
PCIT was effective in increasing positive parenting behavior, decreasing negative parenting behavior, and increasing child compliance to parental commands. Parents reported greater confidence in parenting abilities post-treatment and significant improvement in the core areas of autism symptomatology. Parents endorsed significant improvement in aspects of the parent–child relationship, such as attachment and involvement.
Conclusions
Parents of children with ASD demonstrated more positive and effective parenting behavior and reported enhancements in the parent–child relationship after participating in PCIT. Children were more compliant to parental commands and exhibited improvements in social and behavioral functioning. Increases in positive parenting behaviors and child compliance to parental requests were maintained 1 month after treatment and outside the clinic setting during generalization sessions. Parents of children with ASD reported a high degree of satisfaction with PCIT.
Implications
The present study provides initial evidence of the efficacy of utilizing PCIT with families of preschool-age children with ASD and supports the continued investigation of the efficacy of PCIT with this population.
Keywords: PCIT, autism, intervention, parenting skills, compliance
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by persistent differences in social communication and interaction along with restricted, repetitive patterns of behavior, interests, or activities (American Psychiatric Association, 2013). Intervention literature for children with ASD consistently states that parents should play a collaborative and active role in the design and implementation of their child's intervention services (e.g., Karst & Van Hecke, 2012; Klinger et al., 2013). The success of interventions that utilize parents either as co-therapists or primary therapists for their children with autism has been documented (Bearss et al., 2015; Burrell & Borrego, 2012).
Parent-implemented interventions (PIIs) meet evidence-based practice (EBP) standards for various age groups and outcomes (Steinbrenner et al., 2020). For preschoolers, PIIs meet EBP standards to communication, adaptive behavior, challenging behavior, joint attention, play, and social outcomes. In addition to improving child functioning, PIIs have been shown to improve the parent–child relationship and parent functioning (Burrell & Borrego, 2012). Parental involvement in the treatment of children with ASD, whether direct or indirect, has resulted in enhanced sibling, marital, and parent–child relationships. In the few studies that have assessed parent outcomes after intervention, parents of children with ASD have demonstrated improved parenting self-efficacy (PSE), increased ASD knowledge, and lowered levels of depression and stress (Karst & Van Hecke, 2012). Research using parents as intervention providers across clinical populations has documented increased parental self-efficacy and competence, generalization to other family members, and longer maintenance of treatment gains (Bearss et al., 2015). In sum, effective parenting interventions result in larger child, parent, and family benefits.
Parent–child interaction therapy
Parent–child interaction therapy (PCIT) is an evidence-based behavioral parent training program designed for preschool-age children that emphasizes supporting parent–child interaction patterns to improve child behavior and enhance the quality of parent–child relationships (McNeil & Hembree-Kigin, 2010). During PCIT, parents are taught specific skills to establish a secure, nurturing relationship with their child while simultaneously increasing their child's prosocial behavior and decreasing their child's negative behavior. Key features of PCIT include direct coaching of parent–child interactions, using data to guide treatment, specialized space and equipment, positive and nonjudgmental philosophy, targeting a range of behavioral problems, and addressing patterns of interaction rather than discrete behaviors (McNeil & Hembree-Kigin, 2010).
The efficacy of PCIT in treating children who present with disruptive behavior has been documented in various studies (e.g., Bagner & Eyberg, 2007; Funderburk et al., 1998). Several efficacy studies have documented improvements in children's home and school behavior problems, as well as improvements in parents' interactional style after participating in PCIT (Eisenstadt et al., 1993). Parents have reported more confidence in the ability to manage their child's behavior, less personal distress, improvement in psychological well-being, and satisfaction with the process and result of PCIT (Eyberg & Robinson, 1982). Furthermore, the effects of PCIT have been shown to be stable across time (Boggs et al., 2005). PCIT has garnered empirical support for treating a variety of child clinical concerns, such as anxiety and intellectual disability, among others (Cooley et al., 2014).
Applying PCIT to ASD
PCIT has recently been evaluated for ASD. PCIT shares several similarities to treatments for ASD, such as importance of family involvement across settings, one-on-one parent–child interaction following the child's lead, utilizing positive social reinforcement to increase prosocial behaviors, and child compliance training (Masse et al., 2016). Differential reinforcement, naturalistic environment, modeling, and parent implementation have been identified as EBPs in ASD (Wong et al., 2013), and all are components of the child-directed interaction (CDI) phase of PCIT (Ginn et al., 2015).
Solomon et al. (2008) implemented PCIT with families of 5- to 12-year-old males with ASD and significant behavior problems and found reduced problem behavior, reduced atypical behavior, and increased child adaptability. Parental stress was not reduced by PCIT, and parents continued to self-report stress scores in the clinical range post-treatment (Solomon et al., 2008). Of note, parents demonstrated significant increases in positive affect and shared parent–child positive affect after participating in PCIT.
After Solomon et al.'s (2008) work, seven published reports have indicated support for the value of PCIT for families of children with ASD (see Table 1 for a synopsis). Ginn et al. (2015) found that mothers of children with ASD acquired positive parenting skills that reduced children's disruptive behavior after participating in CDI training alone. Masse et al. (2016) conducted the full PCIT protocol in the home setting with children diagnosed with ASD and comorbid behavioral difficulties and reported increased child compliance, acquisition of positive parenting behaviors, and reduction in parent-reported child behavioral functioning. Most of the studies included children with ASD who were also experiencing comorbid behavioral difficulties. All of the previously published studies with ASD modified the PCIT protocol in some manner, such as reducing amount of time spent in time out, ignoring circumscribed interests, and including visual supports and social stories. A review of the research showed that Masse et al. (2016) followed the standardized PCIT protocol the closest of any other published study, with the only exception being that sessions were held in the home rather than the clinic.
Table 1.
Published PCIT and ASD research studies.
| Author | Year | Design | Participants | Modifications |
|---|---|---|---|---|
| Masse, McNeil, Wagner, and Quetsch | 2016 | Single-subject research design (non-concurrent multiple baseline) | 3 children between 2 and 7 years of age diagnosed with ASD and compliance issues | Home setting |
| Armstrong, DeLoatche, Preece, and Agazzi | 2015 | Case study | 5-year-old girl with comorbid ASD, ID, and epilepsy | Addition of visual supports and a social story |
| Ginn, Clionsky, Eyberg, Warner-Metzger, and Abner | 2015 | Randomized controlled trial | 30 mother–child dyads, children 3–7 years of age with ASD | Child-directed interaction phase only |
| Lesack, Bears, Celano, and Sharp | 2014 | Case study | 5-year-old boy with ASD, DD, and compliance difficulties | Both phases modified; CDI: reflection procedure, PDI: teaching of commands; time out length reduced, holding chair |
| Agazzi, Tan, and Tan | 2013 | Case study | 7-year-old boy with comorbid ASD and behavioral difficulties | Within PDI such as order and deletion of planned ignoring |
| Armstrong and Kimonis | 2013 | Case study | 5-year-old boy with comorbid ASD and severe behavioral problems | Adaptations to ensure appropriateness and generalizability |
| Hatamzadeh, Pouretemad, and Hassanabadi | 2010 | Single-subject research design (A–B) | 4 boys 4–7 years of age with high functioning autism and clinically significant behavioral problems | Not reported, ECBI not given at every session |
| Solomon, Ono, Timmer, and Goodlin-Jones | 2008 | Wait-list control group design | 19 boys 5–12 years of age with ASD and clinically significant behavioral problems | Prohibited mention of circumscribed interests, redirect interactions if controlling, praise initiation of social interaction |
Note. PCIT = parent–child interaction therapy; ASD = autism spectrum disorder; CDI = child-directed interaction; PDI = parent-directed interaction; ECBI = Eyberg Child Behavior Inventory; ID = intellectual disability; DD = developmental delay.
Purpose of the study
The present study provides an important contribution to the field as it evaluates whether PCIT can be an effective intervention for families of children with ASD when conducted per manualized procedures. PCIT has been deemed efficacious in treating children with disruptive behavior disorders, and recent studies have shown promising results utilizing aspects of PCIT with children with ASD (see Table 1), but none of these studies applied the entire PCIT intervention per manual protocol. Therefore, this study is the first to test the efficacy of PCIT, without modification, with families of preschool-age children with ASD without comorbid behavioral difficulties. Unlike previous research, the present study is unique in that PCIT was implemented according to the current treatment manual protocol at the time of the study (Eyberg & Child Study Lab, 1999) without modification, and the age of child participants was within the range (2–6 years of age) for which PCIT has been deemed efficacious (Eyberg, 2005), with the only participant characteristic that differed from traditional PCIT efficacy research being the child diagnosis, that is, ASD instead of oppositional defiant disorder (ODD), conduct disorder (CD), or attention-deficit hyperactivity disorder (ADHD). Furthermore, routine PCIT measures were supplemented in the current research with standardized measures designed to assess ASD characteristics according to published recommendations (Smith et al., 2007). The inclusion of standardized autism measures enhances the importance of the study as it allows examination of the effect of PCIT on specific autism symptomatology and parenting behaviors that have not been examined in other studies applying aspects of PCIT to children with ASD.
The research questions and hypotheses are as follows:
What effect will PCIT have on parental competence? Parents are predicted to exhibit more positive and effective parenting behavior after participating in PCIT, as well as self-report greater confidence in parenting abilities.
What impact will PCIT have on the parent–child relationship? PCIT is hypothesized to improve the relationship between children with ASDs and their parents as evidenced by increased attachment, emotional availability, and favorable attitudes toward family functioning.
Will PCIT affect child functioning? PCIT is predicted to improve compliance to parental commands, as well as decrease disruptive behavior and increase prosocial behavior, in children with ASDs in this study.
Methods
Participants
Four families of children with ASD participated in the study (see Table 2). All parents were mothers; two of the children were female and two were male. All participants were White. At study entry, children ranged in age from 2 years, 8 months to 4 years, 1 month (M = 3 years, 4 months), and parental age ranged from 34 to 38 years (M = 36.25). Two children met criteria for autistic disorder, and two children met criteria for pervasive developmental disorder-not otherwise specified (PDD-NOS) according to DSM-IV TR (American Psychiatric Association, 2000). Inclusion criteria were as follows: (a) child between the ages of 2 and 6 with an ASD diagnosis, confirmed using diagnostic measures prior to study enrollment, (b) score of 80 or higher on a standardized intelligence measure administered within the past year, (c) minimum score of 85 on either the Peabody Picture Vocabulary Test—Fourth Edition (PPVT-IV; average range: 85–115) or a recently administered equivalent measure, (d) caregiver willing to participate in treatment alongside their child, and (e) reliable transportation to attend weekly sessions. Families were recruited through a university-based training clinic, community groups with special interest in ASD, and area occupational therapists and speech and language pathologists. This study was approved by the University's Institutional Review Board (IRB). Written parental consent for the child's participation and informed consent for parental participation in the study were obtained from participants. Families did not receive compensation for participation in the study.
Table 2.
Participant descriptions.
| Participant | Age | Gender/ethnicity | Parent involved | Receptive vocabulary | Entry autism information |
|---|---|---|---|---|---|
| Elise | 3:5 | Female/White | Mother | PPVT-IV: | ADOS |
| 34 | 85 | classification: | |||
| White | Low | Autistic range | |||
| Married | Average | CARS: 25 Non- | |||
| Range | autistic range | ||||
| PDDBI Autism | |||||
| Composite: 40 | |||||
| Dx: Autism | |||||
| Peyton | 3:1 | Female/White | Mother | PPVT-IV: | ADOS |
| 37 | 102 | classification: | |||
| White | Average | Autistic range | |||
| Married | Range | CARS: 40 | |||
| Severe range | |||||
| PDDBI Autism | |||||
| Composite: 67 | |||||
| Dx: Autism | |||||
| Charles | 4:1 | Male/White | Mother | PPVT-IV: | ADOS |
| 36 | 115 | classification: | |||
| White | High | Autistic range | |||
| Married | Average | CARS: 28.5 Non- | |||
| Range | autistic range | ||||
| PDDBI Autism | |||||
| Composite: 41 | |||||
| Dx: PDD-NOS | |||||
| Thomas | 2:8 | Male/White | Mother | PPVT-IV: | ADOS |
| 38 | Unscorable | classification: | |||
| White | Autism spectrum | ||||
| Married | range | ||||
| CARS: Non- | |||||
| autistic range | |||||
| PDDBI Autism | |||||
| Composite: 67 | |||||
| Dx: PDD-NOS |
Note. PPVT-IV = peabody picture vocabulary test—fourth edition; ADOS = autism diagnostic observation schedule; CARS = childhood autism rating scale; PDDBI = pervasive developmental disorders behavior inventory; PDD-NOS = pervasive developmental disorder-not otherwise specified.
Procedure
The research was conducted at a university-based training clinic located in the Southeastern United States. All intervention sessions occurred in a 10 × 7 foot room equipped with one 3 × 5 rectangular table, three chairs, two to three sets of toys, and a one-way observation mirror. Sessions were videotaped from behind the observation mirror for behavioral coding and fidelity/reliability coding. Generalization sessions took place in a snack bar on the first floor of the building, in hallways and stairwells throughout the building, on campus buses operated by the university transit system, the crosswalk, and the parking lot.
A single-subject, multiple-probe research design across families was implemented. This design type is advantageous because it allows developmental maturation and exposure to treatment settings to be controlled, as well as enables the researcher to measure several target behaviors simultaneously while assessing the efficacy of the intervention (Gast & Ledford, 2014).
Per design requirements, the length of the pre-treatment probe condition was staggered across families (Gast & Ledford, 2014). Parent skills were monitored to determine the start of intervention for each family. Stability in the frequency of parent skills was the primary criterion for entry into intervention while continued movement in a non-therapeutic direction was the secondary criterion. If data had not yet stabilized for a family during baseline, but the number of inappropriate parenting skills was either increasing or maintaining at a high level, then the secondary criterion was satisfied and families entered intervention.
Data were obtained for all four families during pre-treatment probe (A), both phases of treatment (B and C), post-treatment (PT), and follow-up (FU) approximately 1 month after treatment ended. PCIT includes two distinct phases of treatment: child-directed interaction (CDI) and parent-directed interaction (PDI). The Dyadic Parent–Child Interaction Coding System-III (DPICS-III) was the dependent measure utilized to determine when families could move from the CDI phase (B) to the PDI phase (C) of treatment, as well as to determine when families could end the PDI phase of treatment and enter post-treatment assessment. Per the PCIT protocol, in order for a family to exit the CDI phase and enter the PDI phase, 10 labeled praise (LP) statements, 10 reflection (RF) statements, and 10 behavior description (BD) statements had to occur during the 5-min CDI coding session. As the RF category requires the parent to reflect a child's vocalization and children with ASD often have delayed expressive language skills, it was anticipated that a child might not verbalize at least 10 statements during a 5-min session, thus preventing the family from moving into the second phase of the treatment. PCIT policy recommends that alternate decision criteria be employed when a child speaks less than 10 words during the 5-min CDI coding segment. The alternate criteria state that a parent must reflect a minimum of 80% of the words spoken by the child if there are less than 10 opportunities to reflect. Alternate decision criteria of 10 LP, 10 BD, and RF 80% of child's intelligible words spoken during the session were employed for Family 4 only. Per the PCIT protocol, families remained in the PDI phase (C) of treatment until the child complied to 75% of parental commands and parents had 100% correct follow-through on commands during the 5-min PDI coding segment at the beginning of the session.
Treatment
The primary investigator was certified in PCIT and served as the therapist for all sessions. Sessions were videotaped for subsequent reliability and fidelity analysis. PCIT was implemented according to manualized procedures (Eyberg & Child Study Lab, 1999; www.pcit.org). At the beginning of each session, an Eyberg Child Behavior Inventory (ECBI) and the DPICS-III coding segment were conducted. DPICS-III coding decisions were based on operational definitions and decision criteria delineated in the DPICS-III Manual (Eyberg et al., 2005). Graduation from the PCIT program involved meeting individual CDI and PDI mastery requirements (see below), along with an ECBI score of 114 or less.
Child-directed interaction phase
Within the CDI phase, parents are taught to follow the child's lead and utilize “PRIDE” skills in practicing differential social attention. PRIDE skills include: Praising the child's behavior, Reflecting the child's statements, Imitating and Describing the child's play, and using Enthusiasm (Eyberg & Child Study Lab, 1999). During CDI, parents practice following the child's play by using non-directive attending skills, that is, “Do Skills” such as praising the child (labeled praise/unlabeled praise). Parents are taught to change their child's behavior by utilizing the “Do skills” when the child is engaged in appropriate play and by ignoring inappropriate behaviors. Parents are taught to avoid using questions (QU), commands (CO), and criticisms (negative talk [NT]; i.e., “Don’t Skills”). During CDI coaching sessions, therapists coach parents in their use of “Do” skills from the observation room through a bug-in-the-ear device while the parent is playing with her child.
Parent-directed interaction phase
During the PDI phase of treatment, parents are taught to use effective commands and specific consequences for compliance and noncompliance. The first session of PDI is an individual didactic session which teaches the parent the skills and principles of PDI, such as consistency, predictability, and follow-through. Direct, positively stated, specific, and developmentally appropriate commands are recommended as well as only giving commands when necessary. After practicing following-through on effective commands during the coaching session with the therapist, parents are asked to practice PDI skills at home in brief 5-min practice sessions after the daily CDI play session. After the parent becomes more confident with the PDI skills, the parent is instructed to use PDI at home when it is important that the child obey a specific command. In later sessions of PDI, parents are taught variations of the PDI procedure to deal with aggressive behavior and public misbehavior.
Treatment fidelity and generalization
Fifty percent of session tapes from each family were randomly selected and checked for integrity by another investigator using the PCIT manual checklists. The accuracy rate with the treatment protocol was 99.3%. Per the PCIT protocol, coaching outside the clinic is conducted to promote the generalization of learned skills to new situations. Once families approached mastery, portions of each session were conducted outside the clinic to establish generalization. Parents were coached in these settings, such as during a campus bus ride, to increase their confidence in implementing PCIT in public places and to demonstrate consistency of expectations across settings. Generalization sessions were individualized according to family problem areas. For example, during a generalization session for a child often noncompliant when getting into his car seat, the therapist coached the parent during the walk to the car and the seatbelt buckling process. Generalization data are presented as child compliance to parental commands (see Figure 2).
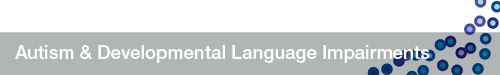
Figure 2.
Percentage of beta compliance (BCCP) during parent-led play (PLP). BCCP is the number of times the child complied with parental commands divided by the total number of commands delivered by the parent during the PLP Dyadic Parent–Child Interaction Coding System-III (DPICS-III) coding segments.
Measures
Pre-treatment: Autism diagnostic observation schedule
All participants were administered the Autism Diagnostic Observation Schedule (ADOS; current version at the time of the study) to assess social interaction, communication, play, and imaginative use of materials prior to inclusion in this study (Lord et al., 2000). As one participant had completed an ADOS within the past 6 months, the information from the previous administration was utilized to describe the participant.
Demographic information questionnaire
This questionnaire was created by the researcher to elicit demographic information, such as age, gender, and income, necessary to describe the sample for journal publications.
Peabody picture vocabulary test—fourth edition
The PPVT-IV is a measure of single-word receptive vocabulary for individuals aged 2.5–90+ years (Dunn & Dunn, 2007). The PPVT-IV Form A was used to ensure the child had an adequate level of receptive vocabulary to benefit from the intervention. Internal consistency (Mα coefficient = .97 for Form A), test–retest (4-week interval, Mr = .92 across age groups), and alternate form (Mr = .88 across age groups) reliabilities are satisfactory.
Childhood autism rating scale
The Childhood Autism Rating Scale (CARS) was employed in this study to provide information about the severity of autistic symptoms experienced by the participants (Schopler et al., 1988). Test authors report that the CARS total score correlates r = .84 with clinical ratings made during the same diagnostic sessions and r = .80 with independent clinical assessments made by child psychologists (Schopler et al., 1988).
The pervasive developmental disorders behavior inventory
The Pervasive Developmental Disorders Behavior Inventory (PDDBI) was developed to evaluate changes in functioning in individuals with autism over time and was designed to document treatment outcomes in various domains of functioning (Cohen & Sudhalter, 2005; Cohen et al., 2003). Cohen (2003) reported adequate criterion-related validity of the PDDBI with the CARS (r = .53) and the Autism Diagnostic Interview-Revised. The PDDBI was included in this research to provide additional participant descriptive information, as well as to evaluate the impact of PCIT on child functioning.
Parenting practices questionnaire)
The Parenting Practices Questionnaire (PPQ) is a 34-item questionnaire completed by parents to evaluate parenting practices. The PPQ was included in this study to assess mothers' use of parenting practices. Strayhorn and Weidman (1988) reported a 6-month interval test–retest reliability coefficient of .79.
Parenting relationship questionnaire-Preschool Version
The Parenting Relationship Questionnaire-Preschool Version (PRQ-P) assesses the parent's perspective of the parent–child relationship (Kamphaus & Reynolds, 2006). The PRQ is a self-report measure that provides information regarding constructs, such as attachment, parenting style, involvement, and parenting confidence. Adequate median internal consistency values are demonstrated across norm groups (r = .82 to .87).
Assessment: Treatment
Per manualized procedures (Eyberg & Child Study Lab, 1999), the following measures were administered during every session. During the probe condition, these measures are intended to establish a stable baseline against which to evaluate treatment effects. The DPICS-III was used to assess mastery of therapeutic goals required to move from CDI to PDI and to graduate from treatment.
Dyadic parent–child interaction coding system-III)
The DPICS-III (Eyberg et al., 2005) behavioral coding system was employed across all conditions of the study to measure the quality of parent–child interactions. The DPICS-III, the current version at the time of the study, is a free operant event recording system where the observer obtains a frequency count for each category of child and parent verbalizations. Data are presented as a number of occurrences. Every verbalization emitted by the parent and child during the observation session is recorded. The DPICS-III provides an observational measure of parent–child behaviors during three 5-min standard situations that vary in the degree of required parental control (i.e., child-led play, parent-led play, and clean-up). Identical categories (verbalizations, vocalizations, and physical behaviors) are coded for parent and child verbalizations. Sequences of behavior, such as compliance to commands, are also coded during the interaction. Definitions of each coding category are operationalized in the DPICS-III manual (Eyberg et al., 2005). The frequency of “Do” (LP, BD, RF) and “Don’t” (QU, CO, NT) skills, as well as compliance (i.e., percentage of times a child complies with parent requests), was compared to both baseline and previous sessions.
DPICS-III interrater reliability
Two research assistants were trained on DPICS-III coding to 80% agreement with a criterion tape before coding mother-child interactions. Reliability data were collected for one-third of each family's sessions. Interrater reliability was calculated using a total agreement method (Gast & Ledford, 2014). For each DPICS-III behavioral category, the percentage agreement was averaged across 14 sessions. Average percentage agreement between the primary investigator and the reliability coders was 81%. Agreement between the two reliability coders was 83%. “A frequently cited minimum for IOA (Interobserver Agreement) is 80% agreement” (Gast, 2010, p. 161). Both total agreement calculations fell within the recommended 80% or higher standard for IOA.
Eyberg child behavior inventory
The ECBI is a 36-item parent-report measure that assesses conduct problems for children aged 2–16 years (Eyberg & Pincus, 1999). The scale measures both the frequency of the child's disruptive behavior (Intensity Scale) and how problematic the behavior is for the parent (Problem Scale). Internal consistency coefficients of r = .98 were reported for both scales of the ECBI (Robinson et al., 1980).
Assessment: Post-treatment
The post-treatment assessment involved two sessions with 15-min DPICS-III observations (5 min of child-led play, 5 min of parent-led play, and 5 min of clean-up) and the completion of post-treatment measures. The same measures completed during the baseline probe session were administered after PCIT completion in order to enable pre- and post-treatment score comparison. In order to assess maintenance, an additional DPICS-III coding session was conducted approximately 1 month after treatment completion.
Therapy attitude inventory
The Therapy Attitude Inventory (TAI) was administered post-treatment to assess parental satisfaction with the process and outcome of therapy (Eyberg, 1993). The TAI consists of 10 multiple-choice questions regarding the perceived impact of the intervention on the quality of the parent–child interaction, the child's behavior, the parent's confidence in discipline skills, and overall family adjustment. Test–retest reliability over a 4-month period (r = .85) and sensitivity to treatment change are established (Brestan et al., 1999).
Results
Visual analysis of graphically displayed data was utilized to determine treatment efficacy (Gast & Ledford, 2014). Data from two measures, DPICS-III and ECBI, were collected at every observation point, displayed graphically (see Figures 1–3), and examined using common visual analysis procedures. In order to gain additional information regarding treatment, several measures were administered at pretest and posttest and were analyzed with paired-samples t tests.
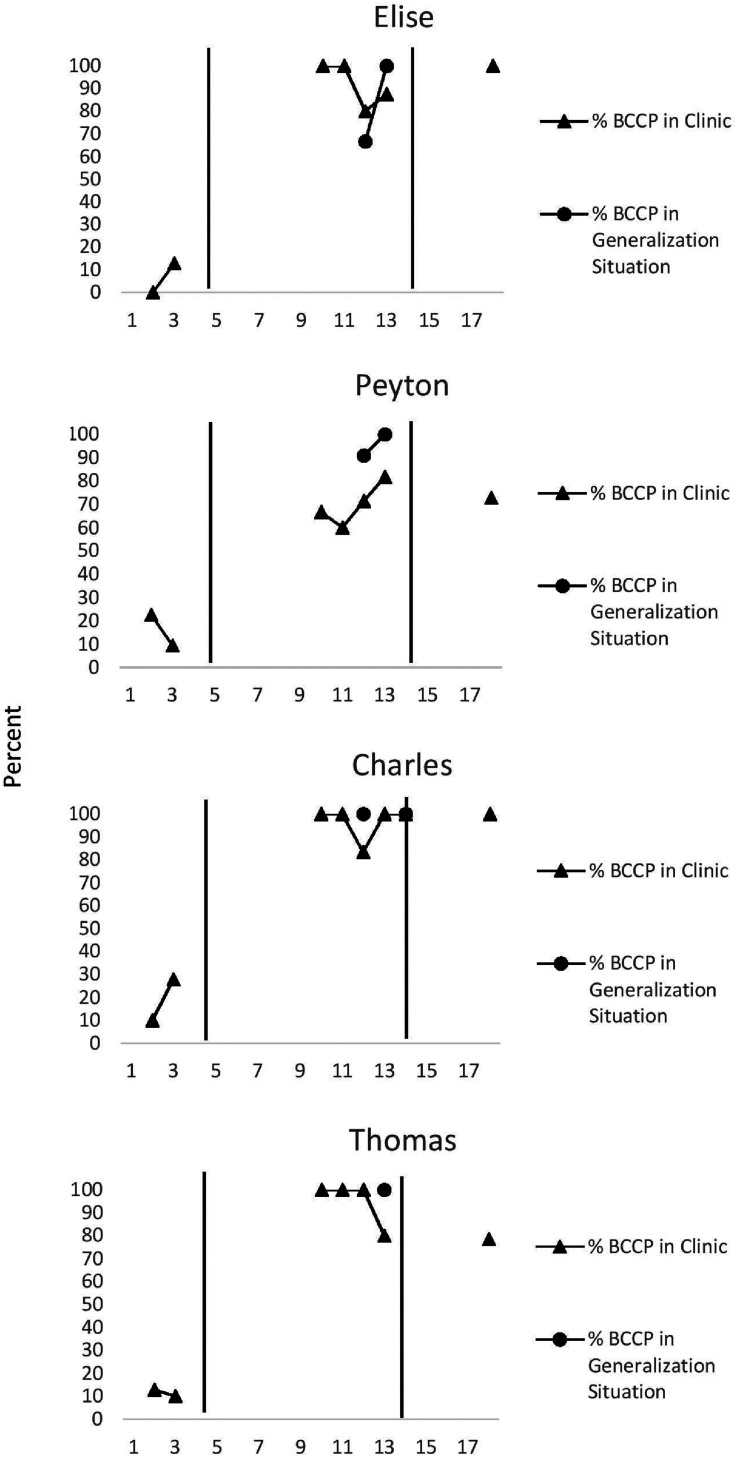
Figure 1.
Mother “Do” and Don’t” skills. The number of DPICS-III “Do” (LP + RF + BD) and “Don’t” (NT + CO + QU) skills demonstrated by four mothers during the CDI coding segment across phases of PCIT. Note. DPICS-III = Dyadic Parent–Child Interaction Coding System-III; LP = labeled praise; RF = reflection; BD = behavior description; NT = negative talk; CO = commands; QU = questions; CDI = child-directed interaction; PCIT = parent–child interaction therapy.
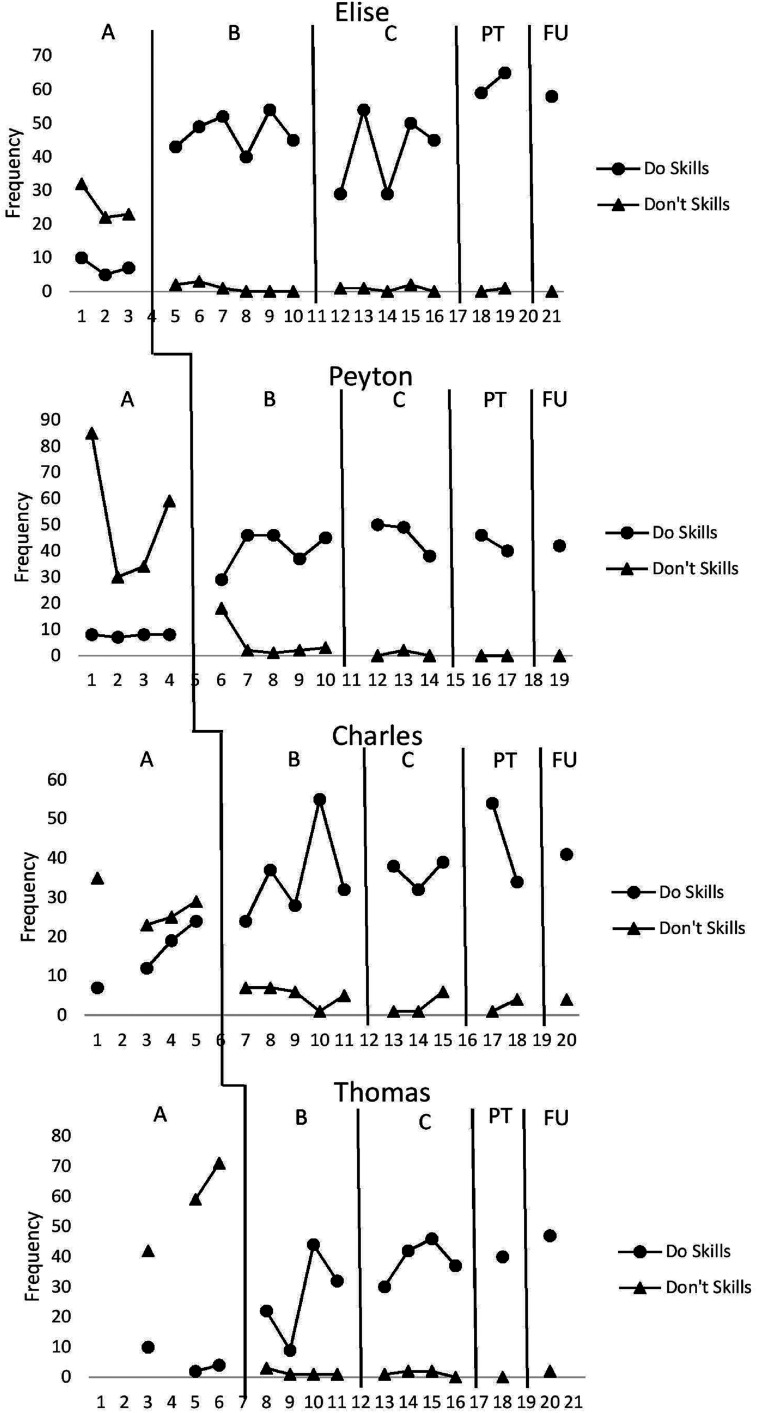
Figure 3.
Eyberg Child Behavior Inventory (ECBI) scores. Problem and intensity scores across all phases of parent–child interaction therapy (PCIT).
Parent functioning: Parenting competence
The data presented in Figure 1 demonstrate that the introduction of PCIT to families in this study effected a positive change in the number of “Do” and “Don’t” parenting skills employed. Intersubject replication was demonstrated as all four families maintained an increase in positive parenting skills post-treatment and at 1-month follow-up.
“Do skills” (labeled praise + behavior description + reflection)
Families 2, 3, and 4 evidenced a therapeutic, accelerating trend in the number of “Do skills” parents employed upon introduction of CDI. The average percentage of overlap in “Do skills” between baseline and CDI for all families was 11.25%. All four families experienced a positive relative level change in the direction of the intervention objective. Three of the four families demonstrated a dramatic absolute level change in the number of “Do skills” exhibited during the first intervention coding session when compared to the last session of the baseline condition. Upon introduction of PDI, three families maintained an accelerating or zero-celerating trend in the number of “Do skills” demonstrated. Despite Family 2's contra-therapeutic trend change after PDI introduction, trend change from post-treatment to 1-month follow-up was positive and therapeutic. Families 2 and 3 evidenced a positive absolute level change with the introduction of PDI. Families 1 and 4 experienced a negative absolute level change when PDI was introduced, but exhibited both a positive absolute level change post-assessment and greater “Do skills” median values post-treatment than baseline (62 vs. 7; 40 vs. 4).
“Don’t skills” (commands + questions + negative talk)
All four parents exhibited a positive change in the number of “Don’t skills” after the introduction of the intervention across all four families. All families demonstrated a positive absolute and relative level change in the number of “Don’t skills” after CDI was introduced. Percentage of overlap between baseline and CDI intervention was 0% for all families in the study. Trend either remained stable or changed from variable to stable, when CDI was introduced. Families 1, 2, and 3 continued the therapeutic trend direction demonstrated in baseline and Family 4's trend level changed from contra-therapeutic to therapeutic. The number of “Don’t skills” exhibited by the parents continued to decrease in the intended direction after the introduction of PDI, post-assessment, and at follow-up.
Parenting practices questionnaire
SPSS data analysis revealed significant pre-post intervention differences for the PPQ, a measure that assesses parenting practices associated with child behavior problems (t(3) = 4.48, p = .021). This finding suggests that parents reported a decreased use of ineffective parenting practices after participating in PCIT.
Child functioning: Compliance
The data presented in Figure 2 show a positive change in child compliance after the introduction of the intervention. An abrupt, positive change in level was replicated across all four families after PCIT was introduced. The magnitude of this abrupt level change in child compliance is further reflected in the 0% overlap in compliance between the probe and intervention condition in all four families. Increased compliance was maintained at the 1-month follow-up data point. Families 1 and 3 achieved 100% beta compliance to parental commands at follow-up, while Families 2 and 4 demonstrated 72.73% and 78.57% compliance at follow-up, an improvement from median probe compliance of 16.05% and 7.31%, respectively.
Compliance generalization data are also presented in Figure 2. A DPICS-III coding session was conducted post-treatment during a campus bus ride to assess each family's ability to transfer skills learned and demonstrated in the clinic to real-life situations. Child compliance to parental commands successfully generalized to the campus bus ride in all four families as each child demonstrated 100% beta compliance to parental commands. Per the PCIT protocol (Eyberg & Child Study Lab, 1999), compliance data were collected in a high-demand, cleanup situation during two probe and two post-treatment sessions. Mean beta compliance improved dramatically from probe condition to post-PCIT. Average cleanup compliance during probe condition of 16.25% and 17.13%, respectively, for Families 1 and 2 increased to 100% average cleanup compliance post-PCIT (Family 3: 50%–95.84%; Family 4: 9.02%–66.67%). These data implicate that demonstrated in-session PCIT skills also generalized to higher-demand situations both within and outside the clinic.
Child functioning: Externalizing behaviors
The ECBI was included in this study to be consistent with the PCIT protocol (Eyberg & Child Study Lab, 1999) and to monitor any changes in externalizing behaviors throughout the intervention. As traditional PCIT research includes participants with externalizing disorders, an ECBI score within the clinical range during pre-assessment is a prerequisite for participation in the program, and an ECBI score within the normal range is included in program graduation criteria. The current study did not include comorbid externalizing problems as an entry requirement; consequently, none of the participants scored within the clinical range on the ECBI during the probe condition. Figure 3 presents ECBI Intensity and Problem scale scores. Through visual analysis of ECBI data, the author can conclusively state that the externalizing behavior of participants, as measured by the ECBI, did not worsen during PCIT. ECBI score trend was either zero-celerating or decelerating throughout the intervention for all families. The ECBI scores for all families remained subclinical throughout the intervention, and ECBI Intensity and Problem scores for all families were lower at post-treatment than pre-treatment.
Child functioning: Autism symptomatology
One composite and five domains on the PDDBI demonstrated statistically significant improvement after completion of PCIT. Parents reported statistically significant post-intervention changes on the Expressive Social Communication Abilities Composite (EXSCA/C; t(3) = 8.22, p = .004) which contains the Social Approach Behaviors domain (SOCAPP; t(3) = 4.92, p = .016) and the Expressive Language domain (EXPRESS; t(3) = 3.43, p = .042) which both showed statistically significant change post-intervention. The SOCAPP domain assesses social communication skills that are generally difficult for children with autism, such as visual social approach behaviors, positive affect behaviors, gestural approach behaviors, responsiveness to social inhibition cues, social play behaviors, imaginative play behaviors, empathy behaviors, social interaction behaviors, and social imitative behaviors. The EXPRESS domain assesses the child's ability to speak sounds associated with the English language and use words and sentences that demonstrate competence with grammar and the pragmatic aspects of communication.
Parental report of Semantic/Pragmatic Problems (SEMPP), or the degree of difficulty children with autism have in using spoken language to communicate meaning and sustain a conversation, significantly decreased after participation in PCIT (t(3) = 3.44, p = .041). Statistically significant differences were also reported by the parent post-PCIT in the Specific Fears domain (FEARS; t(3) = 3.25, p = .048) and the Learning, Memory, and Receptive Language domain (LMRL; t(3) = 3.39, p = .043). The FEARS domain measures behaviors that communicate anxieties and fears associated with withdrawal from social stimuli, such as sadness or anxiety when in a new situation or away from a caregiver or auditory withdrawal behaviors. While pre-post intervention changes on the Autism Composite (AUTISM) were not statistically significant, the AUTISM mean declined by 1 SD after the completion of PCIT suggesting parents reported less severity in overall behaviors associated with autism after receiving the intervention.
Parent–child relationship
Significant differences between pre- and post-treatment scores were found on four of the five PRQ-P scales, indicating PCIT had a positive effect on parental perception of the parent–child relationship. On the Attachment (AT) scale, which measures the affective, cognitive, and behavioral relationship between parent and child, mothers reported a stronger bond with their respective child after PCIT (t(3) = 3.6, p = .036). Pre- and post-treatment differences on the Discipline (DP) scale indicated that parents reported a greater tendency to consistently apply consequences to their child's misbehavior and greater support of the establishment and adherence of rules post-PCIT (t(3) = 3.4, p = .042). Parents reported significantly greater involvement with their children after participating in PCIT on the Involvement scale (IN; (t(3) = 5.2, p = .014) along with greater feelings of comfort, control, and confidence when making parenting decisions, as evidenced by their scores on the Parent Confidence scale (PC; t(3) = 5.4, p = .013).
Consumer satisfaction
The TAI was administered to all families post-treatment. TAI scores ranged from 46 to 49 out of a possible score of 50 (M = 47.75, Mdn = 48) indicating families were highly satisfied with treatment.
Discussion
This study provides support for the use of PCIT with preschool children with ASD without comorbid externalizing disorders. Post-treatment, parents demonstrated more positive and effective parenting behavior and reported enhancements in the parent–child relationship. Children were more compliant to parental commands and exhibited improvements in social and behavioral functioning after participating in PCIT. Increases in positive parenting behaviors and child compliance to parental requests were maintained 1 month after treatment and outside the clinic setting during generalization sessions. Furthermore, parents of children with ASD reported a high degree of satisfaction with PCIT.
Parent functioning
The hypothesis that parents would demonstrate more positive and effective parenting behavior after participating in PCIT was supported. Parents demonstrated and reported more effective parenting practices after participating in PCIT. They employed a greater number of positive parenting skills (i.e., “Do skills”) upon introduction of PCIT and maintained this increase in positive parenting skills throughout the intervention and 1 month after treatment. Furthermore, parents demonstrated an immediate reduction in the utilization of negative parenting practices (i.e., “Don’t skills”) upon introduction of PCIT. The decrease in negative parenting practice continued throughout the intervention and was maintained post-treatment and at 1-month follow-up. These findings support the premise that parent training techniques developed for mothers of children with other clinical disorders can be effective in teaching parents of children with ASD.
Support for the hypothesis that parents would report greater competence and confidence in their parenting ability was demonstrated. Parents reported significant improvement post-intervention in utilizing effective parenting practices associated with child behavior problems on the PPQ and reported significantly more confidence in their ability to parent on the PRQ-P post-intervention.
Child functioning
The hypothesis that after PCIT, child compliance would improve was supported. An immediate, abrupt positive level change in beta compliance on the DPICS-III was demonstrated across all four families with the introduction of PDI. Improved beta compliance was maintained at 1-month follow-up and in settings outside the clinic. All children demonstrated 100% beta compliance during generalization data collection. Furthermore, improved compliance was demonstrated post-treatment during high-demand cleanup sessions in the clinic.
Unlike most participants in PCIT efficacy studies for externalizing disorders, disruptive behavior was not the most relevant treatment target area for the families that participated in this study. Clinically significant scores on the ECBI were not required for participation in treatment, and participants in this study did not have comorbid externalizing problems. The ECBI was included as a measure of child behavior to be consistent with the PCIT protocol and to monitor behavioral changes throughout the intervention. Recall that this study is the first to examine PCIT in the ASD population without comorbid externalizing disorders. Encouraging support was found for the hypothesis that PCIT would reduce disruptive child behavior in children with ASD and without comorbid behavioral disorders, as all families maintained a decelerating or zero-celerating trend on the ECBI throughout treatment.
Support for the hypothesis that PCIT would increase child prosocial behavior was confirmed. Parents reported significant improvement in child social approach behaviors and receptive-expressive language communication skills on the PDDBI post-treatment. While hypotheses did not include predictions in other specific areas of ASD-related symptomatology, improvement on PDDBI scales and composites post-treatment provides initial evidence that PCIT may impact ASD symptoms. Parents endorsed statistically significant post-PCIT improvement on social communication skills, including positive affect behaviors, gestural approach behaviors, responsiveness to social inhibition cues, social play behaviors, imaginative play behaviors, empathy behaviors, and social imitative behaviors. Parents also reported statistically significant reductions in withdrawal behaviors and anxiety and fears associated with withdrawal from social stimuli on the PDDBI. Statistically significant improvement post-PCIT was also reported on the PDDBI in the child's pragmatic aspects of expressive communication, such as the ability to speak sounds in the English language, ability to comprehend spoken language, ability to respond to the interests of others, and ability to sustain a conversation. While not statistically significant, the post-treatment group mean on the AUTISM decreased by more than 1 SD from the pre-treatment mean, indicating parents perceived less severity in overall behaviors associated with ASD post-PCIT. As the PDDBI has demonstrated adequate reliability and validity, is designed to account for developmental changes in the child due to time and maturity (Cohen & Sudhalter, 2005) and was sensitive to the effects of treatment in the current study, the authors recommend inclusion of the PDDBI in future PCIT research with families of children with ASD.
Parent–child relationship
The hypothesis that PCIT would result in more favorable attitudes toward family functioning and improve the relationship between parent and child by demonstrating increased attachment, closeness, involvement, and understanding of the child was supported. The PRQ-P was included in this study as the primary outcome variable to measure parental perception of the parent–child relationship. Significant pre-post differences were obtained on four of the five PRQ-P scales: AT, DP, IN, and PC. Significant increases on the AT scale are reflective of a stronger parent–child bond after PCIT and increased understanding of child. Greater empathy and closeness with the child are also indicated on the AT scale. Improvement on the IN scale indicates increased time parent and child spend participating together in common activities and increased parental knowledge of child activities after participating in PCIT. Current study results warrant inclusion of the PRQ-P in future PCIT efficacy studies with ASD populations and further study of the utility of additional measures that may add greater depth to the examination of the effect of PCIT on the parent–child relationship.
Implications
The current research takes a well-established efficacious treatment for families of children with disruptive behavior disorders and applies it to families of children with ASD. This research study contributes to the growing body of literature that documents the utility and benefit of applying PCIT to children with ASD by demonstrating that PCIT without modifications to the treatment protocol can be effective for this population. This is the only published study to examine the effects of PCIT conducted in the exact manner as delineated in the manual without any modifications to the treatment protocol specific to ASD and with participants who do not have comorbid externalizing disorders. Furthermore, by including measures specific to autism symptomatology, such as the PDDBI, this research was able to document how participation in PCIT can directly impact specific symptoms of ASD, such as social communication and interaction. Based on their utility in capturing changes in the current study, the authors recommend that future trials of PCIT with families of children with ASD include the PDDBI as a measure of change in autism symptomatology and the PRQ-P as a measure of aspects of the parent–child relationship. PSE (caregiver's belief in their ability to effectively parent their child) can be affected in parents with children with ASD due to deficits in reciprocal social communication, but a few research studies have demonstrated that PSE can be improved with brief, targeted interventions with this population (Karst & Van Hecke, 2012). The current study demonstrated that participating parents increased their PSE after participating in PCIT through significant changes on the PPQ (parents self-reported a decrease in their use of ineffective parenting practices) and significant increases on the PRQ PC scale (increased belief that they can effectively parent their child). These findings indicate an additional benefit of PCIT for families with ASD could be increased PSE. As PSE is a relatively new area of research in the ASD population, additional research investigating the contribution of PCIT in increasing PSE in parents of children with autism could be a promising contribution to the field.
The current research has several notable limitations. In addition to small sample size, the participants in this study lacked diversity and were not fully representative of the population of families with children with ASD. All participants were White and all caregivers were female. Individuals with comorbid externalizing disorders were not recruited for this research. As PCIT was designed to treat families of children with disruptive behavior disorders, and subsequent efficacy trials with new populations have included comorbid diagnosis with externalizing disorders, perhaps the inclusion of comorbid diagnoses would have changed the results of this study. Most of the published studies applying PCIT to the ASD population retained comorbid clinical levels of externalizing behavior in the inclusion criteria.
Future directions
As there is a growing body of research applying PCIT to families of children with ASD with success, further replication of this line of research by additional investigators is recommended to determine what modifications, if any, could be beneficial when conducting PCIT with children with ASD. While the current study demonstrated that PCIT conducted without modification to the treatment protocol was effective with children with ASD, functioning and presentation vary greatly among the population. For instance, further research may show that the number of reflections should consistently be changed from the standard 10 to a specific percentage of child utterances when a child's expressive language level does not allow for 10 utterances within the 5-min coding period. Additional research can also confirm the inclusion of autism-specific measures into the PCIT assessment protocol. The current study demonstrated increased child compliance, improved child social and communication functioning, increased positive parenting behaviors, and decreased negative parenting behaviors without any necessary modifications to PCIT, however, the population in this study did not reflect the entire range of functioning exhibited by individuals with ASD, and modifications may be necessary for children with different profiles. A short-term research goal should be to develop a manual that standardizes the assessment and application of PCIT to families of children with ASD, yet allows for individualization by incorporating decision rules to modify the intervention plan. For example, clinicians might need specific guidance when working with a child with ASD on how to handle repetitive behaviors and speech or circumscribed interests within the context of PCIT. Published case studies utilizing PCIT with children with ASD have reported modifications to the standardized PCIT protocol to meet the unique needs and profiles of the children served by the intervention (e.g., Agazzi et al., 2013). According to Eyberg (2005), the developer of PCIT, tailoring is defined as changing the delivery style or focus of essential elements during intervention in order to meet the needs of the family. Adaptation refers to changing an existing treatment model so it may be used with a specific population or within a specific situation. With the exception of the current study, which followed the PCIT protocol without modification, all of the previously published efficacy studies of PCIT with children with ASD changed the PCIT protocol in one or more ways. The creation of a manual that delineates acceptable variations in delivering PCIT with families of ASD based on participant characteristics or participant response to the intervention would be optimal. The principle of “constrained flexibility” addresses the need to balance uniformity with the need for individualization and maintains that limited variation in intervention is acceptable provided suggested alternate courses of action are delineated in the manual (Smith et al., 2007). Due to the heterogeneous presentation across individuals with ASD, any intervention manual must allow for “constrained flexibility” so clinicians can meet the individual needs of participants with ASD while still employing evidence-based techniques.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Sarah F. Vess https://orcid.org/0000-0002-2221-8938
Contributor Information
Sarah F. Vess, Developmental Behavioral Pediatrics, Brenner Children's Hospital, Wake Forest School of Medicine Winston Salem, NC, USA
Jonathan M. Campbell, Department of Psychology, Western Carolina University, Cullowhee, NC, USA
References
- Agazzi H., Tan R., Tan S. (2013). A case study of parent-child interaction therapy for the treatment of autism spectrum disorder. Clinical Case Studies, 12(6), 428–442. 10.1177/1534650113500067 [DOI] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders: Fourth Edition Text Revision. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders: Fifth Edition (DSM-5). [Google Scholar]
- Armstrong K., DeLoatche K. J., Preece K. K., Agazzi H. (2015). Combining parent-child interaction therapy and visual supports for the treatment of challenging behavior in a child with autism and intellectual disabilities and comorbid epilepsy. Clinical Case Studies, 14(1), 3–14. 10.1177/1534650114531451 [DOI] [Google Scholar]
- Armstrong K., Kimonis E. R. (2013). Parent-child interaction therapy for the treatment of Asperger’s disorder in early childhood: A case study. Clinical Case Studies, 12(1), 60–72. 10.1177/1534650112463429 [DOI] [Google Scholar]
- Bagner D. M., Eyberg S. M. (2007). Parent-child interaction therapy for disruptive behavior in children with mental retardation: A randomized controlled trial. Journal of Clinical Child and Adolescent Psychology, 36(3), 418–429. 10.1080/15374410701448448 [DOI] [PubMed] [Google Scholar]
- Bearss K., Burrell L. S., Stewart L., Scahill L. (2015). Parent training in autism spectrum disorder: What’s in a name? Clinical Child Family Psychology Review, 18(2), 170–182. 10.1007/s10567-015-0179-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boggs S. R., Eyberg S. M., Edwards D. L., Rayfield A., Jacobs J., Bagner D., Hood K. K. (2005). Outcomes of parent-child interaction therapy: A comparison of treatment completers and study dropouts one to three years later. Child & Family Behavior Therapy, 26(4), 1–22. 10.1300/J019v26n04_01 [DOI] [Google Scholar]
- Brestan E. V., Jacobs J. E., Rayfield A. R., Eyberg S. M. (1999). A consumer satisfaction measure for parent-child treatments and its relationship to measures of child behavior change. Behavior Therapy, 30(1), 17–30. 10.1016/S0005-7894(99)80043-4 [DOI] [Google Scholar]
- Burrell T. L., Borrego J., Jr. (2012). Parents’ involvement in ASD treatment: What is their role? Cognitive and Behavioral Practice, 19(3), 423–432. 10.1016/j.cbpra.2011.04.003 [DOI] [Google Scholar]
- Cohen I. L. (2003). Criterion-related validity of the PDD Behavior Inventory. Journal of Autism and Developmental Disorders, 33(1), 47–53. 10.1023/A:1022278420716 [DOI] [PubMed] [Google Scholar]
- Cohen I. L., Schmidt-Lackner S., Romanczyk R., Sudhalter V. (2003). The PDD Behavior Inventory: A rating scale for assessing response to intervention in children with pervasive developmental disorder. Journal of Autism and Developmental Disorders, 33(1), 31–35. 10.1023/A:1022226403878 [DOI] [PubMed] [Google Scholar]
- Cohen I. L., Sudhalter V. (2005). The PDD Behavior Inventory (PDDBI) professional manual. Psychological Assessment Resources. [Google Scholar]
- Cooley M. E., Veldorale-Griffin A., Petren R., Mullis A. K. (2014). Parent-child interaction therapy: A meta-analysis of child behavior outcomes and parent stress. Journal of Family Social Work, 17(3), 191–208. 10.1080/10522158.2014.888696 [DOI] [Google Scholar]
- Dunn L. M., Dunn D. M. (2007). Peabody Picture Vocabulary Test—Fourth Edition. Pearson Assessments. [Google Scholar]
- Eisenstadt T. H., Eyberg S., McNeil C. B., Newcomb K., Funderburk B. (1993). Parent-child interaction therapy with behavior problem children: Relative effectiveness of two stages and overall treatment outcome. Journal of Clinical Child Psychology, 22(1), 42–51. 10.1207/s15374424jccp2201_4 [DOI] [Google Scholar]
- Eyberg S. M. (1993). Consumer satisfaction measures for assessing parent training programs. In Vandecreek L., Knapp S., Jackson T. L. (Eds.), Innovations in clinical practice: A sourcebook Vol. 12, pp.377–382. Professional Resource Press. [Google Scholar]
- Eyberg S. M. (2005). Tailoring and adapting parent-child interaction therapy to new populations. Education and Treatment of Children, 28(2), 197–201. [Google Scholar]
- Eyberg S. M., Funderburk B. W., Hembree-Kigin T. L., McNeil C. B., Querido J. G., Hood K. K. (2001). Parent-child interaction therapy with behavior problem children: One and two-year maintenance of treatment effects in the family. Child and Family Behavior Therapy, 23(4), 1–20. 10.1300/J019v23n04_01 [DOI] [Google Scholar]
- Eyberg S. M., & Child Study Lab. (1999). Parent-child interaction therapy: Procedures manual [Unpublished manuscript]. University of Florida. [Google Scholar]
- Eyberg S. M., McDiarmid-Nelson M., Duke M., Boggs S. R. (2005). Manual for the Dyadic Parent-Child Interaction Coding System—Third Edition [Unpublished manuscript]. University of Florida. [Google Scholar]
- Eyberg S. M., Pincus D. (1999). Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Inventory: Professional manual. Psychological Assessment Resources. [Google Scholar]
- Eyberg S. M., Robinson E. A. (1982). Parent-child interaction therapy: Effects on family functioning. Journal of Clinical Child Psychology, 11(2), 130–137. 10.1080/15374418209533076 [DOI] [Google Scholar]
- Funderburk B., Eyberg S. M., Newcomb K., McNeil C., Hembree-Kigin T., Capage L. (1998). Parent-child interaction therapy with behavior problem children: Maintenance of treatment effects in the school setting. Child and Family Behavior Therapy, 20(2), 17–38. 10.1300/J019v20n02_02 [DOI] [Google Scholar]
- Gast D. L. (2010). Single case research methodology: Applications in special education and behavioral sciences (1st ed.). Routledge. [Google Scholar]
- Gast D. L., Ledford J. R. (2014). Single case research methodology: Applications in special education and behavioral sciences (2nd ed.). Routledge. [Google Scholar]
- Ginn N. C., Clionsky L. N., Eyberg S. M., Warner-Metzger C., Abner J. (2015). Child-directed interaction training for young children with autism spectrum disorders: Parent and child outcomes. Journal of Clinical Child & Adolescent Psychology, 46(1), 1–9. 10.1080/15374416.2015.1015135 [DOI] [PubMed] [Google Scholar]
- Hatamzadeh A., Pouretemad H., Hassanabadi H. (2010). The effectiveness of parent-child interaction therapy for children with high functioning autism. Procedia Social and Behavioral Sciences, 5, 994–997. 10.1016/j.sbspro.2010.07.224 [DOI] [Google Scholar]
- Kamphaus R. W., Reynolds C. R. (2006). Parenting Relationship Questionnaire (PRQ) manual. Pearson Assessments. [Google Scholar]
- Karst J. S., Van Hecke A. (2012). Parent and family impact of autism spectrum disorders: A review and proposed model for intervention evaluation. Clinical Child and Family Psychology Review, 15(3), 247–277. 10.1007/s10567-012-0119-6 [DOI] [PubMed] [Google Scholar]
- Klinger L. G., Ence W., Meyer A. (2013). Caregiver-mediated approaches to managing challenging behaviors in children with autism spectrum disorder. Dialogues in Clinical Neuroscience, 15(2), 225–233. 10.31887/DCNS.2013.15.2/lklinger [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesack R., Bearss K., Celano M., Sharp W. G. (2014). Parent-child interaction therapy and autism spectrum disorder: Adaptations with a child with severe developmental delays. Clinical Practice in Pediatric Psychology, 2(1), 68–82. 10.1037/cpp0000047 [DOI] [Google Scholar]
- Lord C., Rutter M., DiLavore P., Risi S. (2000). Autism Diagnostic Observation Schedule (ADOS) manual. Western Psychological Services. [Google Scholar]
- Masse J. J., McNeil C. B., Wagner S., Quetsch L. B. (2016). Examining the efficacy of parent-child interaction therapy with children on the autism spectrum. Journal of Child and Family Studies, 25(8), 2508–2525. 10.1007/s10826-016-0424-7 [DOI] [Google Scholar]
- McNeil C. B., Hembree-Kigin T. L. (2010). Parent-child interaction therapy. Springer. [Google Scholar]
- Robinson E. A., Eyberg S. M., Ross A. W. (1980). The standardization of an inventory of child conduct problem behaviors. Journal of Clinical Child Psychology, 9(1), 22–28. 10.1080/15374418009532938 [DOI] [Google Scholar]
- Schopler E., Reichler R. J., Renner B. (1988). The Childhood Autism Rating Scale (CARS). Western Psychological Services. [Google Scholar]
- Smith T., Scahill L., Dawson G., Guthrie D., Lord C., Odom S., Rogers S., Wagner A. (2007). Designing research studies on psychosocial interventions in autism. Journal of Autism and Developmental Disorders, 37(2), 354–366. 10.1007/s10803-006-0173-3 [DOI] [PubMed] [Google Scholar]
- Solomon M., Ono M., Timmer S., Goodlin-Jones B. (2008). The effectiveness of parent-child interaction therapy for families of children on the autism spectrum. Journal of Autism and Developmental Disorders, 38(9), 1767–1776. 10.1007/s10803-008-0567-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinbrenner J. R., Hume K., Odom S. L., Morin K. L., Nowell S. W., Tomaszewski B., Szendrey S., McIntyre N. S., Yucesoy-Ozkan S., Savage M. N. (2020). Evidence-based practices for children, youth, and young adults with autism. The University of North Carolina at Chapel Hill, Frank Porter Graham Child Development Institute, National Clearinghouse on Autism Evidence and Practice Review Team.
- Strayhorn J. M., Weidman C. S. (1988). A parenting practices scale and its relation to child and parent mental health. Journal of the American Academy of Child and Adolescent Psychiatry, 27(5), 613–618. 10.1097/00004583-198809000-00016 [DOI] [PubMed] [Google Scholar]
- Wong C., Odom S. L., Hume K., Cox A. W., Fettig A., Kucharczyk S., Brock M. E., Plavnick J. B., Fleury V. P., Schultz T. R. (2013). Evidence-based practices for children, youth, and young adults with autism spectrum disorder. The University of North Carolina, Frank Porter Graham Child Development Institute, Autism Evidence-Based Practice Review Group. [DOI] [PubMed]