Abstract
Firefighters are occupationally exposed to an array of hazardous chemicals, and these exposures have been linked to the higher rates of some cancer in firefighters. However, additional research that characterizes firefighters’ exposure is needed to fully elucidate the impacts on health risks. In a pilot study, we used silicone wristbands to quantify off-duty and on-duty chemical exposures experienced by 20 firefighters in Durham, North Carolina. By using each firefighter’s off-duty wristband to represent individual baseline exposures, we assessed occupation-related exposures (i.e. on-duty exposures). We also investigated the influence of responding to a fire event while on-duty. In total, 134 chemicals were quantified using both GC-MS/MS and LC-MS/MS targeted methods. Seventy-one chemicals were detected in at least 50% of all silicone wristbands, including 7 PFAS, which to our knowledge, have not been reported on wristbands previously. Of these, phthalates were generally measured at the highest concentrations, followed by brominated flame retardants (BFRs) and organophosphate esters (OPEs). PFAS were measured at lower concentrations overall, but firefighter PFOS exposures while on-duty and responding to fires were 2.5 times higher than off-duty exposures. Exposure to polycyclic aromatic hydrocarbons (PAH), BFRs, and some OPEs were occupationally associated, with firefighters experiencing 0.5 to 8.5 times higher exposure while on-duty as compared to off-duty. PAH exposures were also higher for firefighters who respond to a fire than those who did not while on-duty. Additional research with a larger population of firefighters that builds upon this pilot investigation may further pinpoint exposure sources that may contribute to firefighters’ risk for cancer, such as those from firefighter gear or directly from fires. This research demonstrates the utility of using silicone wristbands to quantify occupational exposure in firefighters and the ability to disentangle exposures that may be specific to fire events as opposed to other sources that firefighters might experience.
Introduction
Firefighters are occupationally exposed to a complex mixture of potentially carcinogenic chemical exposures which has raised concerns regarding how these exposures may be related to their elevated risk of disease, and especially cancer. Firefighter occupational exposures were illuminated after the events of 9/11 in New York, New York, USA. Recent studies, including the World Trade Center Health Program1–3, have demonstrated that general cancer incidence is higher for first responders, particularly for prostate cancer, thyroid cancer, and leukemia.4 However, specific chemicals related to disease risk have not been fully investigated. To understand whether occupational exposure to hazardous chemicals is related to firefighter health and disease, data must be collected to characterize specific exposures to a wide range of chemicals.
There is no typical exposure for a firefighter, as exposures may differ depending on several factors. For example, exposures differ when responding to a municipal fire, wildfire, car fire, or a residential fire.5 Additionally, the types of exposures firefighters may experience is dependent on their role while responding to the fire event,6 the particular materials burning, or the fire station in which they reside while on-duty.5
Previous studies investigating firefighter chemical exposures have documented exposure to complex mixtures that include environmental phenols, phthalates, per- and polyfluoroalkyl substances (PFAS), and pesticides.6–9 Biomonitoring studies of firefighters have found differences in exposures as compared to the general population. For example, studies of firefighters in the United States have demonstrated elevated serum levels of some PFAS10 and elevated levels of polybrominated diphenyl ethers (PBDEs).11,12 Further, elevated urinary metabolites of polycyclic aromatic hydrocarbons (PAHs) in firefighters are higher than the general, non-smoking public.13 Exposure to organophosphate flame retardants have also been associated with responding to residential fires.12 However, measurements of exposure biomarkers are often limited by the temporality of sample collection due to differences in biological half-lives of many organic contaminants.
Silicone wristbands have successfully been used as personal passive sampling devices for measuring exposures to semi-volatile organic chemicals (SVOCs) in a wide range of settings. A small number of studies have investigated firefighter occupational exposure using silicone passive sampling devices.6,14,15 In particular, firefighter exposure has been investigated through silicone dog-tags worn by firefighters.6 Results of this work demonstrated elevated exposure to PAHs while working as a firefighter. However, investigations of firefighters’ exposures in a full, single on-duty work shift, as compared to a full off-duty shift are limited, as are investigations that drill down on differences in fire response versus no fire response while on-duty. This investigation fills that gap in the literature.
In this investigation, we conducted an exposure assessment with firefighters in Durham, North Carolina using silicone wristbands. Firefighters wore wristbands while on-duty and while off-duty and reported on daily activities (e.g., whether or not they responded to a fire event). A total of 134 chemicals across nine chemical classes were measured. Unlike previous studies, we evaluated wristbands using targeted methods of SVOC quantification across three exposure scenarios. These chemicals represent many SVOCs associated with health effects that are also found in consumer products or building materials that firefighters may encounter when responding to fires; PBDEs, PAHs, PFAS, pesticides, phthalates, and flame retardants are associated with health effects such as hormonal disruption, negative reproductive and developmental effects, respiratory symptoms, and diabetes.16–20 The primary objectives of this study were twofold: to determine if significant differences would be observed in chemical exposures off-duty as compared to on-duty, and if there would be significant differences in chemical exposures while responding to a fire versus not responding to a fire while on-duty.
Materials and Methods
Study Population
Firefighters were recruited to participate in this study from fire stations in Durham, North Carolina (NC) in 2019. Firefighters were asked to wear wristbands while on-duty and while off-duty and complete a corresponding survey for each period that they wore a wristband. In total, 43 firefighters from six different stations enrolled, and samples were collected between August 2019 and February 2020. Over this time, not all firefighters responded to a fire while on-duty. To support our study goals, we only analyzed wristbands for the 20 firefighters that completed at least one off-duty wristband and survey as well as one on-duty wristband while responding to a fire and completing a survey. Of these 20 firefighters, 11 were also able to complete an on-duty shift with no fire event and a survey. All wristbands included in this pilot study were from two different fire stations. Figure 1 presents an overview of the study design and summarizes the number of wristbands analyzed in this study among the various time periods (e.g. off-duty vs on-duty). All participants provided informed consent prior to participating and the study was approved by the Duke University Institutional Review Board.
Figure 1.
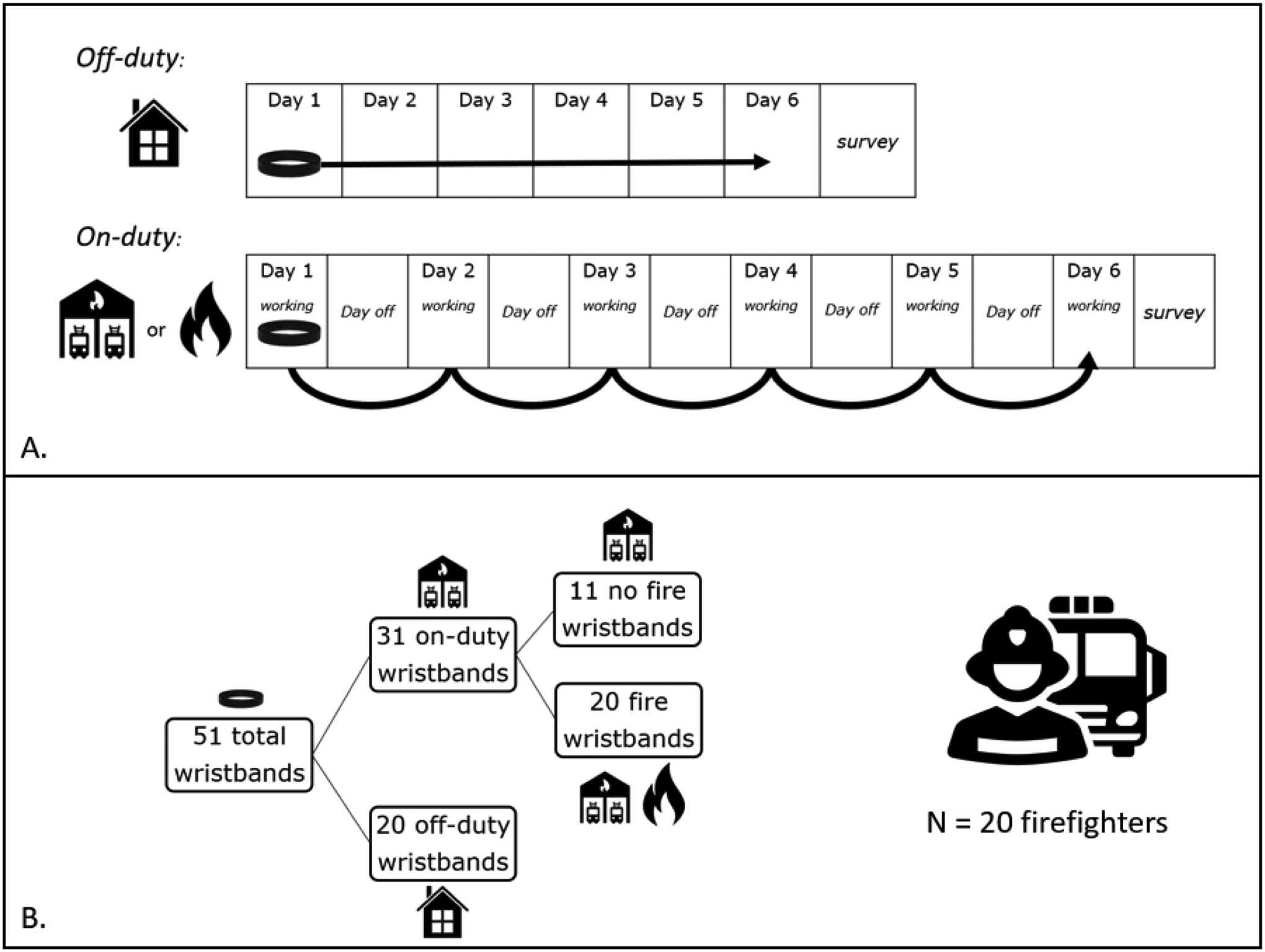
Pictorial description of wristband experimental design and breakdown across all firefighters: A. Description of how wristbands were worn to capture 6 days of “on-duty” and 6 days of “off-duty” exposures. On-duty wristbands were stored in closed containers during days off while on-duty. B. Breakdown of total wristbands (51) collected across all 20 firefighters.
Wristband Collection
Commercially available silicone wristbands (24hourwristbands.com, Houston, TX, USA) were pre-cleaned through two 12 hour Soxhlet extractions using first 1:1 ethyl acetate/hexane (v/v) and then 1:1 ethyl acetate/methanol (v/v).21 Wristbands were then dried in a vacuum oven at room temperature. When dried, cleaned wristbands were wrapped in precleaned aluminum foil (combusted at 450°C) and stored in airtight jars until distribution to study participants.
Firefighters were first asked to complete an intake survey to collect demographic information and other general information such as tenure at the Durham Fire Department, second job description, and housing age. Firefighters were asked to wear a silicone wristband for six consecutive days during different periods (Figure 1). On the first day of each period, firefighters were asked to wear a new, clean wristband. While on duty, firefighters wore wristbands whenever they were at the fire station or responding to calls. When leaving the station at the end of a shift, firefighters wrapped their silicone wristbands in clean aluminum foil (provided) and placed the wrapped wristband in a provided Ziplock bag and placed in the fire station freezer (approximately −20°C) until the next time they were working at the station. Importantly, our study design accounted for time away from the firehouse (e.g., days off) and wristbands were worn for the same amount of time during each period (Figure 1). A new wristband was used during each six-day shift until at least one wristband from each of the three study periods (off-duty, on-duty and responding to a fire, and on-duty without responding to a fire) was collected. Each firefighter was also asked to complete an electronic survey at the end of each work period to provide information on their work activities, behavioral habits, and personal care product use throughout the week that they wore each silicone wristband. After wearing the wristbands, firefighters were asked to again wrap the wristband in provided aluminum foil and enclose it in a plastic zip-top bag. Samples were then stored in the freezer at the fire house before being transported to the research lab at Duke University. Once in the laboratory, wristbands were stored at −20°C until analysis.
Wristband Extraction
Wristband extraction for SVOCs is described in detail elsewhere,22–24 but briefly, the mass of a small piece (~0.75 g) piece of each wristband was first recorded and then cut into three pieces and transferred to a glass centrifuge tube for extraction. Samples were spiked with isotopically labeled internal standards and extracted using 1:1 hexane:dichloromethane (Supplemental Information (SI) Table S1). Extracts were concentrated to 1.0 mL using a Thermo Scientific SpeedVac Concentrator, then purified using a packed glass column containing Florisil resin. Final extracts were concentrated to 1.0mL and transferred to auto sampler vials (ASV) for analysis by GC-MS. Samples were analyzed for a suite of compounds using a Q Exactive GC hybrid quadrupole-Orbitrap GC−MS/MS system (Thermo Scientific) in full scan electron ionization mode. These chemicals include: 11 PCBs, 31 OPEs, 10 phthalates and their alternatives, 12 pesticides, and 20 PAHs. PBDEs and brominated flame retardants (BFR) were quantified using a Q Exactive GC hybrid quadrupole-Orbitrap GC−MS/MS system (Thermo Scientific) operated in negative chemical ionization mode. These BFRs include 10 PBDEs and 3 novel BFRs. Full method details are available in the supporting information (SI Item S1).
Isotopically labelled recovery standards were spiked into each sample extract prior to MS analysis and were used to calculate recovery of the internal standards (SI Table S1). Overall, lab processing blanks (solvent only, n = 2) and field blanks (unworn wristbands, n =5) were analyzed alongside the wristband samples for quality assurance and control. All sample values were blank-subtracted by subtracting the average level measured in a field blank (if detected). Method detection limits (MDLs) were determined by calculating three times the standard deviation of the average field blank levels for wristband samples and then dividing by the mass of the wristband. If the analyte was not detected in a field blank, the MDL was determined using a signal to noise ratio of 10 on the instrument. Values that fell below the MDL were replaced by MDL divided by the square root of 2. To assess precision in measurements, 10 wristbands were randomly selected from this study. In these 10 wristbands, three pieces (~0.75 g each) were cut from different areas around the wristband and extracted using the methods described above. On average, the relative standard deviation of the three measurements within a wristband was 9% among all anlytes. More details are provided SI Item S2 and Figure S1.
PFAS were extracted from a separate piece of wristband (~1 g) using a different method, described in detail in the SI (SI Item S3, SI Table S2). Wristband pieces were weighed, cut into three pieces, and placed in glass test tubes. Samples were spiked with 20 ng of each internal standard (SI Table S1), extracted three times in 10 mL 0.1% NH4OH/methanol by ultrasonication for 15 min. Extracts were combined, concentrated to approximately 100 μL under N2, reconstituted in 300 μL 1:1 MeOH:water, spiked with 20 ng of a recovery standard (Perfluoro-n-[1,2-13C2]octanoic acid, Wellington Labs), transferred to 0.2 μM nylon Whatman UniPrep vials and filtered. Samples were analyzed by electrospray ionization LC/MS-MS as previously described.9,25 A full list of PFAS compounds evaluated is provided in SI Table S3. Further details regarding the analysis can be found in the Supplemental Information (SI Item S3, SI Table S3).
In addition, lab blanks (empty test tubes, n = 5) and field blanks (unworn, cleaned wristbands, n = 5) were analyzed alongside the wristband samples for quality assurance and control. Recoveries of all internal standards are available in SI Table S1.
Statistical Analysis
In total, 51 wristbands were analyzed, 20 of these were off-duty wristbands, 20 were on-duty with fire wristbands, and 11 were on-duty with no fire wristbands (Figure 1). All analyses were performed using SAS statistical software (version 9.4; SAS Institute Inc., Cary, NC) for analytes detected in >50% of all wristbands, per chemical. All results were assessed at α = 0.05 for significance.
Values were non-normally distributed, as confirmed by a Shapiro-Wilk test, and were therefore log10-transformed. Regression analyses were performed per chemical to investigate differences between wristbands worn during the three sampling periods. These analyses used generalize estimating equations (GEEs) to account for potential residual correlation arising from our repeated measured study design. We present exponentiated beta coefficients from regression analyses which represent the multiplicative change in the mass of each chemical measured in on-duty wristbands relative to the reference category of off-duty wristbands. Comparisons were also made between the different types of on-duty bands (fire vs no fire).
Results and Discussion
Demographic characteristics of the firefighters included in this study population are detailed in Table 1. Most participants identified as White (90%), and 75% of all participants identifying as men. Five women were included in our study, all of whom identified as White. Participating firefighters had a median age of 34 years, with a median tenure of 3–6 years working at their current firehouse.
Table 1.
Selected Characteristics of Participating Firefighters from Durham, NC (n = 20)
| Demographics | N | % | |
|---|---|---|---|
| Sex | M | 15 | 75% |
| F | 5 | 25% | |
| Age (y) | 20–29 | 4 | 20% |
| 30–39 | 10 | 50% | |
| 40–49 | 3 | 15% | |
| 50–59 | 3 | 15% | |
| Race/Ethnicity | White | 18 | 90% |
| Black | 1 | 5% | |
| No Answer | 1 | 5% | |
| Fire Events only (n = 20) | N | % | |
| Type of Firea | Structure | 22 | 81% |
| Residential | 17 | 63% | |
| Business | 5 | 19% | |
| Vehicle | 3 | 11% | |
| Other | 3 | 11% | |
| More than one type selected | 1 | 4% | |
| Type of PPEb worn | Bunker pants | 1 | 5% |
| Full turn-out gear with SCBA | 18 | 86% | |
| Duty uniform, helmet, gloves | 2 | 10% | |
| Time spent at Fire | < 30 minutes | 8 | 38% |
| ≥ 30 minutes | 13 | 62% | |
| Type of extinguisher used at Fire | None | 1 | 5% |
| Water | 16 | 76% | |
| Dry Chemical | 1 | 5% | |
| Water and Dry Chemical | 3 | 14% | |
| Fire events per wristband | 1 | 13 | 65% |
| 2 | 7 | 35% | |
n = 27, due to some wristbands experiencing two fire events in a single work period;
PPE = personal protective equipment
Details regarding survey results reported while on-duty or off-duty are also provided in Table 1. Firefighters mostly reported responding to structural fires during this study period, with 81% of all fires reported as structural (63% of which were residential and 19% were business structure fires). Most firefighters (62%) reported spending more than 30 minutes responding to a fire. Of the fires reported during this study period, firefighters reported using water to extinguish the fire more than 75% of the time. 86% of firefighters who responded to a fire while on duty reported using “full turn-out gear with a self-contained breathing apparatus (SCBA)” for personal protective equipment (PPE). Durham firefighter gear is standardized across the department. Of the 20 firefighters providing a wristband sample while on-duty and responding to a fire, 35% represented two fires in a single six-day shift, while the remaining 65% represented one fire in a single six-day shift.
Of the 134 targeted chemicals in our method, 71 were detected in more than 50% of wristbands. A detailed breakdown of detection frequencies and distribution information for each compound is included in supplemental material (SI Table S4). Phthalates were the most commonly detected compounds; all 10 phthalates targeted were detected on every wristband (Table 2). Similarly, phthalates were detected at the highest median concentrations on wristbands followed by BFRs and OPEs. PCBs were detected at the lowest median concentrations across all wristbands. Of the PCBs quantified in this study, only PCB11 and PCB28 were detected in greater than 50% of samples. Generally, detection frequencies were higher in the on-duty wristbands compared to the off-duty wristbands, particularly for BDEs, OPEs, and PAHs (Table 2). Detection frequencies were higher for phthalates in the off-duty wristbands, though only marginally. Additional details regarding each compound class and differences in firefighter exposures can be found below.
Table 2.
Detection and distribution across classes of compounds including the number of compounds in each class evaluated, median sum concentrations and detection frequencies for each type of wristband.
| Summed median concentration (ng/g)A | N compounds >50% DF | |||||||
|---|---|---|---|---|---|---|---|---|
| Class of Compounds | N compounds | Overall % of wristbands with DF >50% | Off-Duty WBs | On-Duty No Fire WBs | On-Duty Fire WBs | Off-Duty | On-Duty, No Fire | On-Duty, Fire |
| BFRs | 16 | 81% | 682.3 | 3,166 | 2,194 | 69% | 81% | 81% |
| OPEs | 36 | 64% | 55,600 | 58,620 | 57,940 | 58% | 64% | 64% |
| PAH | 25 | 52% | 164.8 | 219.4 | 373.7 | 28% | 44% | 64% |
| PCBs | 11 | 18% | 0.96 | 1.43 | 0.79 | 18% | 27% | 18% |
| Pesticides | 16 | 31% | 182.9 | 101.0 | 98.3 | 31% | 31% | 31% |
| Phthalates | 10 | 100% | 306,100 | 201,200 | 245,800 | 100% | 100% | 100% |
| PFAS | 18 | 39% | 39.35 | 39.35 | 37.07 | 39% | 39% | 39% |
Note that summed median concentrations include chemical-specific imputed values from measurements <MDL
PAHs
We quantified 25 PAHs in all wristbands, only two of which were not detected on any wristband (7,12-Dimethylbenz(a)anthracene and 3-Methylcholanthrene). Of the 23 detected PAHs, 13 were detected in at least 50% of samples overall. The highest median concentrations were observed for phenanthrene, pyrene, and fluoranthene. This differs slightly from a previous study measuring PAHs with silicone wristbands worn by Florida firefighters while on-duty, where the three highest concentrations were observed for phenanthrene, naphthalene, and fluorene.14 The detection frequencies of PAHs measured on wristbands were higher for wristbands worn on-duty as compared to off-duty. While only 7 of 25 PAHs assessed were detected in at least 50% of wristbands worn while off duty, 11 compounds were detected while on duty and 17 were detected while on-duty and responding to a fire. Similarly, median ∑PAHs were measured at lower levels on off-duty wristbands compared to on-duty wristbands, and median ∑PAH values were highest in the on-duty wristbands with fire (Table 2), a pattern that was generally consistent for individual PAHs as well (SI Table S4). This is likely a reflection of the fact that PAHs are associated with combustion reactions associated with fires.
Regression analyses were conducted to statistically evaluate differences in exposures related to firefighting. Figure 2 displays the multiplicative change in PAH concentrations in on-duty (with and without a fire event) compared to off-duty (reference value) wristbands. PAH concentrations were 1.7 to 8.5 times higher (acenaphthene and acenaphthylene, respectively) for on-duty while responding to a fire as compared to off-duty wristbands. PAH concentrations ranged from 0.5 to 2.7 times higher (for both acenaphthylene and phenanthrene, and indeno(1,2,3-cd)pyrene, respectively) on-duty without responding to a fire event. Taken together, these PAH results indicate higher levels of exposure while on-duty, which was confirmed by regression analyses similar to those described above, except using on-duty without a fire event wristbands as the referent group. PAH concentrations while on-duty with a fire were 0.6 to 5.1 times higher as compared to wristbands worn on-duty without a fire (SI Figure S2). This further suggest that these PAH exposures are associated with direct exposure to fires.
Figure 2.
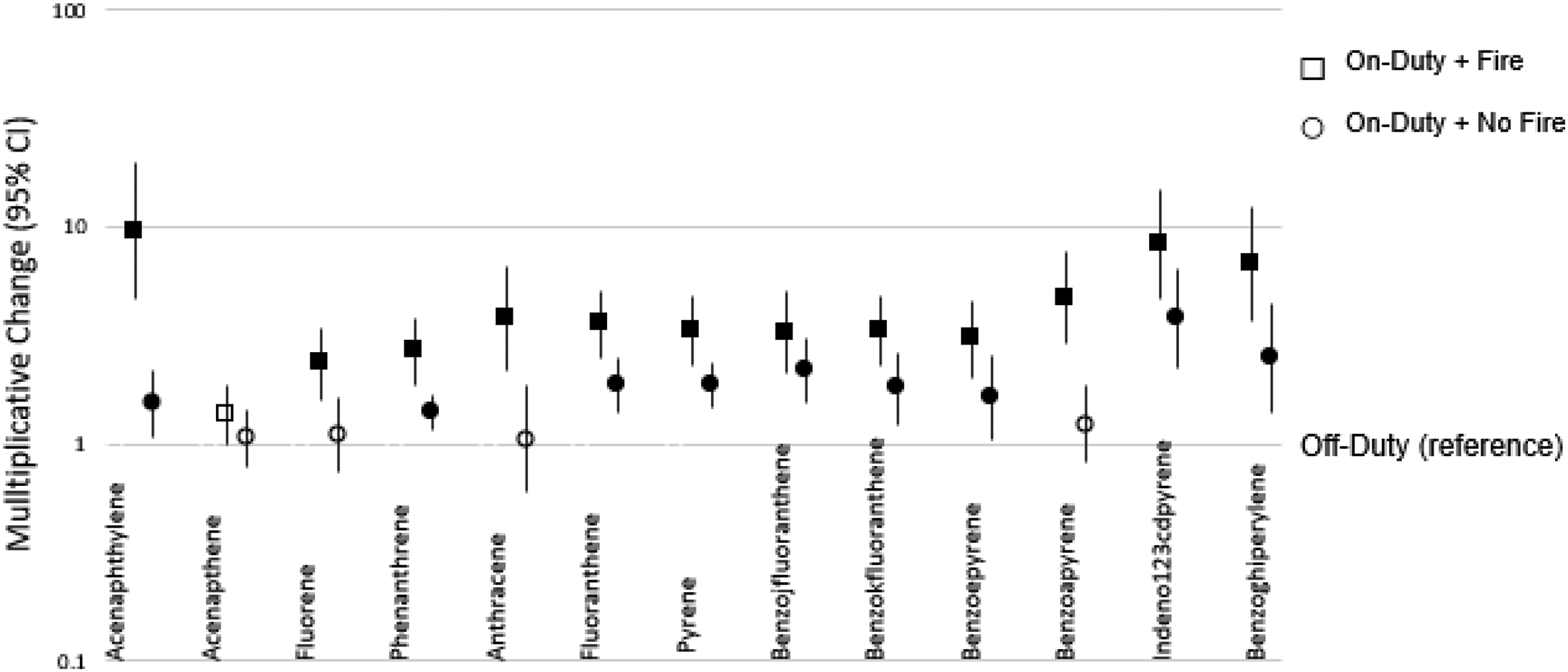
Multiplicative change (10β) in silicone wristband PAH measurements while on-duty (with fire event and without fire event) as compared to off-duty. Exponentiated beta coefficients from these regression analyses represent the multiplicative change in log10-transformed mass of chemical(s) found on on-duty wristbands relative to the reference category of off-duty wristbands. Filled shapes indicate p<0.05.
Few studies have quantified exposures experienced by firefighters using silicone passive samplers. Prior studies with municipal firefighters have deployed samplers for different lengths of time, ranging from 24 hours to 30 days and under different conditions.6,14,15,26 Study design differences make comparisons across studies difficult; while silicone uptake of SVOCs is thought to be linear over time, this is still under investigation.27 Furthermore, these investigations have not all specifically documented exposures to municipal firefighters in the United States, further complicating inter-study comparisons. For example, firefighters in the Dominican Republic had the highest levels of PAH concentrations on silicone wristbands worn while on-duty for phenanthrene, pyrene, and fluoranthene, though this study only required firefighters to wear the silicone wristband for 24h while working.15 Another investigation of firefighter exposure used a silicone passive sampler designed in the shape of a dog tag to capture exposure to PAHs, phthalates, and pesticides.6 One silicone dog tag was worn for 30 days while on-duty and another was worn for 30 days while off-duty. In these samples, 20 of the 21 measured PAHs were found in higher concentrations while on-duty as compared to off-duty.6,26 Our data displayed a similar trend, with PAHs detected more frequently and measured in higher concentrations while on-duty (with or without a fire response) as compared to off. In a follow-up study of PAH exposure from the same group of firefighters that stratified exposures based on call volume, duty shift, and other variables, differences observed between on-duty and off-duty PAH exposure remained, but were generally lower (i.e., on-duty median PAH concentrations were up to 170% of those measured on off-duty tags).28 In our study, PAH medians measured on-duty when responding to fire events were up to 1250% of off-duty medians, and on-duty with no fire medians were up to 580% of off-duty medians. Differences between studies may be due to differences in samples preparation and analysis. For example, we did not rinse wristbands with water before extraction. Some research groups rinse off wristbands prior to analysis which may remove chemicals associated with or sorbed to those particles. As a result, our methods may capture particle-bound PAHs and lead to a higher exposure estimate than studies that rinse off the wristbands.
BFRs
Of the 16 BFRs quantified, 13 were measured in >50% of samples overall. Median concentrations of EHTBB, BDE47 and BDE99 were numerically higher than other BFRs across all wristband types, similar to previous wristband exposure study in the general population.29 BFR exposures were generally higher on-duty versus off-duty and detection of BFRs varied across duty shifts. For example, two BFRs, BDE85 and BDE183, were both detected in 40% and 35%, respectively, of off-duty samples but 100% and 74% (respectively) of on-duty samples, suggesting that these BFRs are associated with an occupational exposure.
Multiplicative change plots comparing levels of BFRs measured on all three types of wristbands are shown in Figure 3. Associations suggests a general occupational exposure to BFRs that was independent of responding to a fire event. Compared to off-duty wristbands, multiplicative change values were very similar while on-duty, regardless of whether or not a firefighter responded to a fire event. The concentrations of BFRs while on-duty were 1 to 7 times higher (p < 0.05) than off-duty concentrations. In general, multiplicative change estimates for the older generation of BFRs, polybrominated diphenyl ethers (PBDEs), were higher when on-duty but not responding to a fire, although associations for on-duty with fire samples were very similar. BDE209 and DBDPE seemed to show an opposite pattern with slightly higher multiplicative change when on-duty with a fire event. This is interesting given that DBDPE is a primary replacement chemical for BDE-209. All together, these data suggest that BFR exposures may be occupational, though not associated with a fire event response, because these compounds are often associated with materials such as furniture, building materials, or even firefighter protective gear that may be present in firehouses, particularly if these materials were procured before the US phase out of the penta-BDE mixture in 2005.
Figure 3.
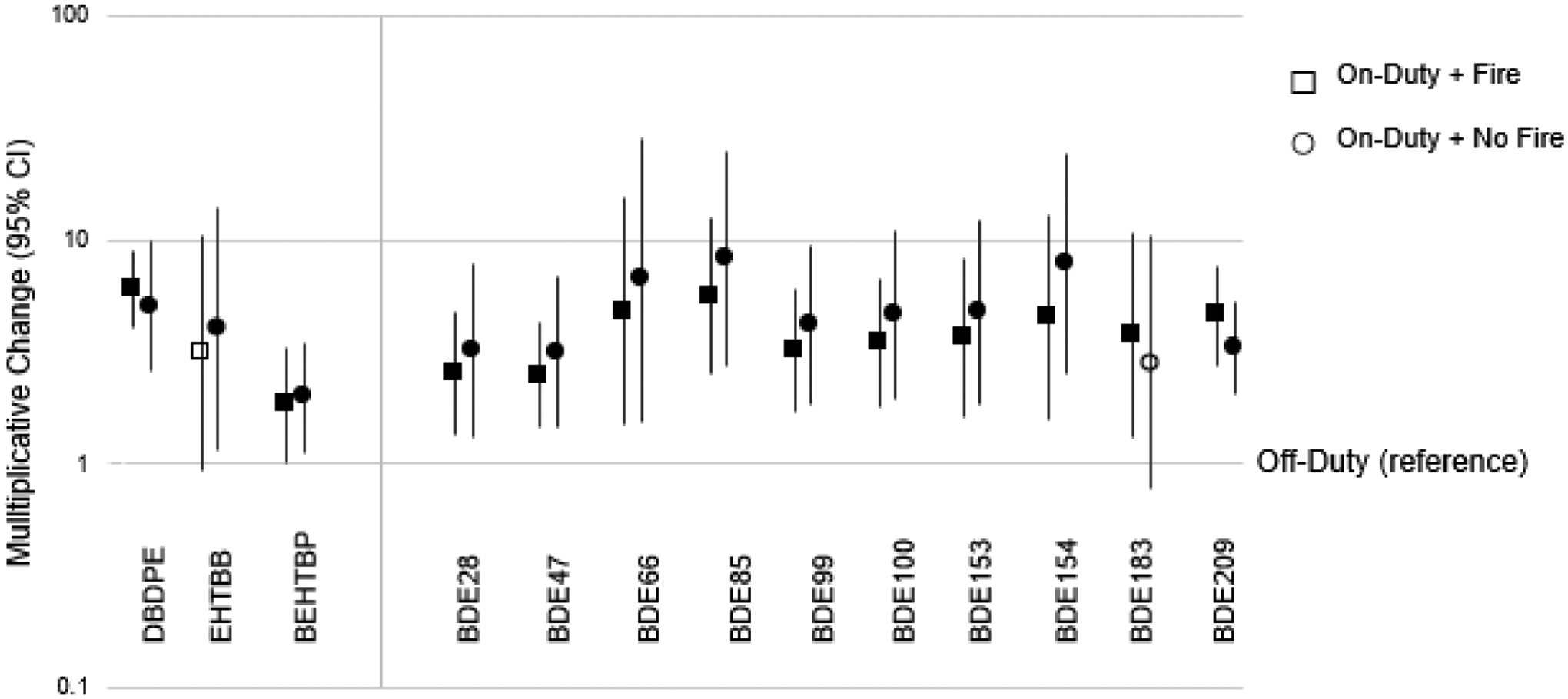
Multiplicative change (10β) in silicone wristband BFR measurements while on-duty (with fire event and without fire event) as compared to off-duty. Exponentiated beta coefficients from these regression analyses represent the multiplicative change in log10-transformed mass of chemical(s) found on on-duty wristbands relative to the reference category of off-duty wristbands. Filled shapes indicate p<0.05. Acronyms: DBDPE = decabromodiphenyl ethane; EHTBB = 2-ethyl-hexyl tetrabromobenzoate; BEHTBP = bis(2-ethylhexyl) tetrabromophthalate; BDE = brominated diphenylether.
Phthalates and phthalate alternatives
As shown in Table 2, the highest concentrations observed across all three types of wristbands were from DEHP, DEHT, and DINP, similar to other studies assessing phthalates on wristbands in non-occupational settings.24,30 On-duty measurements of DMP, DEP, and DBP were significantly lower (0.49 – 0.59 times, p<0.05; Figure 4) as compared to off-duty wristbands. These lower molecular weight phthalates are often used in personal care products or scented products,31–33 and therefore this difference likely suggests that higher exposure off-duty may be related to a general difference in behaviors and differences in use of personal care products between off-duty and on-duty periods. This implies that being a firefighter does not generally increase exposure to phthalates.
Figure 4.
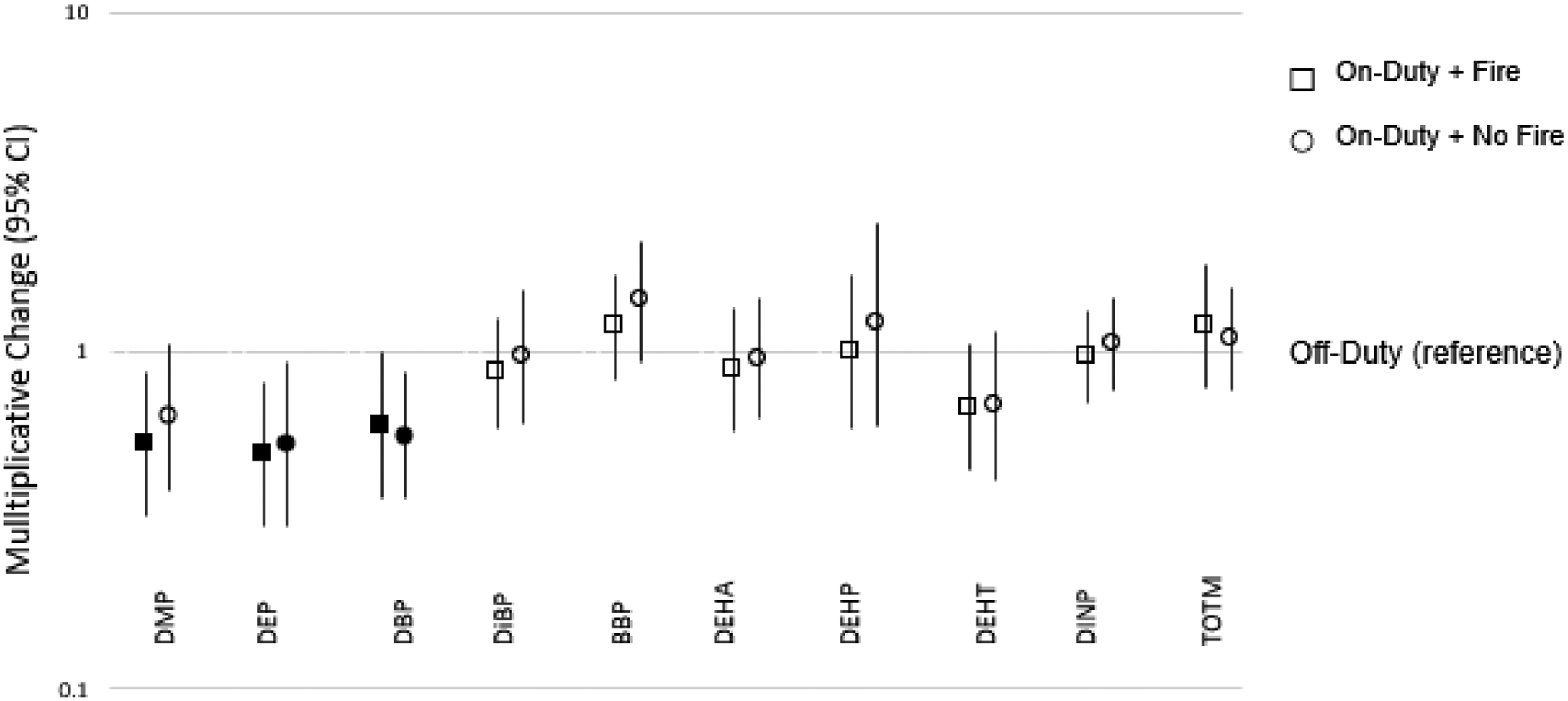
Multiplicative change (10β) in silicone wristband phthalate and non-phthalate plasticizer measurements while on-duty (with fire event and without fire event) as compared to off-duty. Exponentiated beta coefficients from these regression analyses represent the multiplicative change in log10-transformed mass of chemical(s) found on on-duty wristbands relative to the reference category of off-duty wristbands. Filled shapes indicate p<0.05. Acronyms: DMP = dimethyl phthalate; DEP = diethyl phthalate; DBP = dibutyl phthalate; DiBP = diisobutyl phthalate; BBP = benzyl butyl phthalate; DEHA = di-(2-ethylhexyl) adipate; DEHP = di(2-ethylhexyl)phthalate; DEHT = dioctyl terephthalate; DiNP = diisononyl phthalate; TOTM = trioctyltrimellitate.
In a previous study using silicone dog tags to monitor exposure to firefighters in Oregon, phthalates were observed at a higher median while on-duty than off-duty, with DEHP and DIBP measured at the highest levels while on-duty.26 Researchers noted that this may be due to the presence of phthalates in firefighter turnout gear.26,34,35 While we did not evaluate turn-out gear in our study, and cannot evaluate this hypothesis, we did collect information on personal care product use which may be related to exposure to some phthalates used in fragrances. In total 11 (55%) of firefighters reported using fragrances (cologne or perfume). Of these, 7 reported fragrance use off-duty, 1 used it during an on-duty shift where they did not respond to a fire event, and 3 reported fragrance use while on-duty in a shift where they responded to a fire event. While these numbers were too low to evaluate differences statistically, the higher proportion of firefighters using fragrances while off-duty may explain observed patterns for some low molecular weight phthalates used in these applications (e.g. DEP). It is worth noting that not all phthalates measured are associated with fragrances, as the most abundant phthalates measured here are high molecular weight phthalates that are most often used as plasticizers associated with building materials, plastics, and consumer products, though the same pattern of lower exposures while on-duty was observed across all phthalates measured.
OPEs
OPEs were measured at the second highest concentrations on wristbands overall. Of the 36 OPEs quantified in this investigation, 23 were measured in >50% of the total samples. EHDPP was measured at the highest median concentration, which was observed in on-duty wristbands with no fire event.
TPHP, EHDPP, TEHP, 4tBDPP, B4IPPP, T4tBPP, TDMPP, and B4tBPPP were all associated with firefighter occupational exposures. Two of these OPEs had lower detection frequencies in off-duty wristbands: T4tBPP (43%) and TDMPP (38%) (SI Table S4), which may demonstrate that these exposures are associated with exposures experienced at a firehouse, rather than exposures experienced while responding to fires. Exposure to T4tBPP and TDMPP were 23 – 73 times higher for firefighters while on-duty; however, we caution again the over interpretation of these data due to the lower detection frequency of these compounds in off-duty bands. Exposure to the rest of the OPEs listed above were 0.8 – 4.4 times higher in wristbands worn while on-duty without a fire event, and between 0.4 – 11.3 times higher in wristbands worn while on-duty with a fire event, both as compared to off-duty wristbands (p<0.05) (Figure 5). In the case of TiBP, significant and lower exposures were observed on wristbands worn on-duty without a fire event (Figure 5), signifying that TiBP exposures are not occupationally driven for firefighters. Of note, the low detection frequencies associated with off-duty wristbands (for T4tBPP and TDMPP, as noted above) may have influenced the multiplicative change trends noted in Figure 5.
Figure 5.
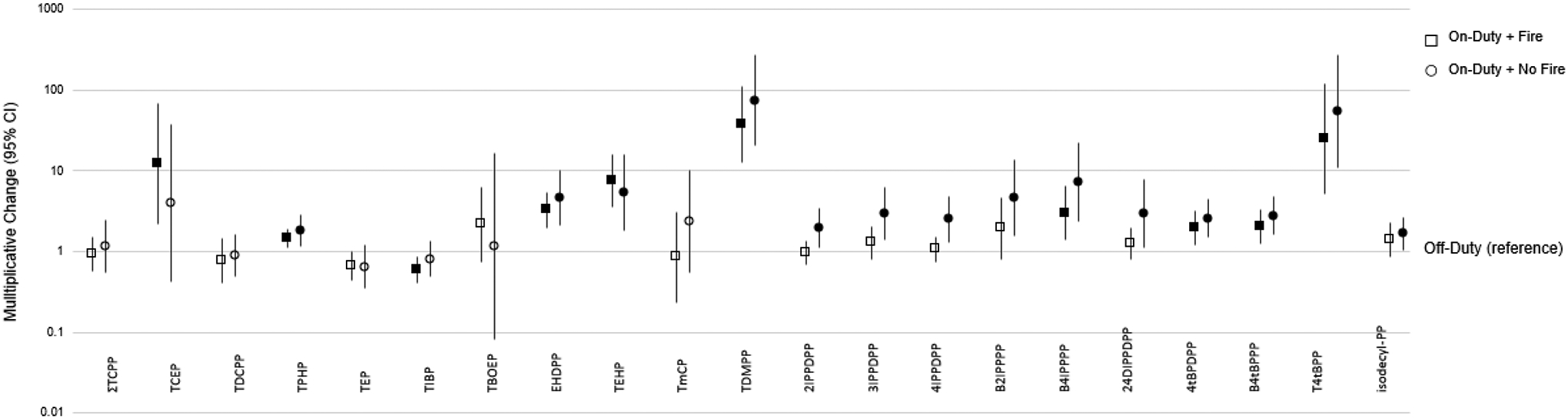
Multiplicative change (10β) in silicone wristband OPE measurements while on-duty (with fire event and without fire event) as compared to off-duty. Exponentiated beta coefficients from these regression analyses represent the multiplicative change in log10-transformed mass of chemical(s) found on on-duty wristbands relative to the reference category of off-duty wristbands. Measurements of tris(1-chloro-2-propyl) phosphate (TCPP) isomers, TCPP1, TCPP2, and TCPP3, on each wristband were summed to a single value (ΣTCPP). Filled shapes indicate p<0.05. Acronyms: TCEP = tris(2-chloroethyl) phosphate; TDCPP = tris(1,3-dichloro-2-propyl) phosphate; TPHP = triphenyl phosphate; TEP = triethyl phosphate; TiBP = tri-iso-butylphosphate; TBOEP = tris(2-butoxyethyl) phosphate; EHDPP = 2-ethylhexyl diphenyl phosphate; TEHP = tris(2-ethylhexyl) phosphate; TmCP = tri-m-cresyl phosphate; TDMPP = tris(3,5-dimethylphenyl) phosphate; 2IPPDPP = 2- isopropylphenyl diphenyl phosphate; 3IPPDPP = 3-isopropylphenyl diphenyl phosphate; 4IPPDPP = 4-isopropylphenyl diphenyl phosphate; B2IPPPP = bis(2-isopropylphenyl) phenyl phosphate; B4IPPPP = bis(4-isopropylphenyl) phenyl phosphate; 24DIPPDPP = bis(2,4-diisopropylphenyl) phenyl phosphate; 4tBPDPP = 4-tert-butylphenyl diphenyl phosphate; B4tBPPP = bis(4-tert-butylphenyl) phenyl phosphate; T4tBPP = Tris(4-tert-butylphenyl) phosphate; isodecyl-PP = isodecyl diphenyl phosphate.
OPEs tend to come from a much wider range of applications and have many more uses than the other chemical classes detailed herein, such as their uses as flame retardants and plasticizers in building materials. For example, TPHP is commonly found in a variety of commercial flame retardant mixtures which are used in furniture but TPHP has also been used in personal care products (e.g. nail polish), electrical industrial equipment, as a plasticizer, in artificial leather products, in varnishes, and as a phthalate substitute.36–41 Additionally, EHDPP is associated with food packaging,42 and TCEP is associated with insulation material.43 The ubiquity of these exposures make OPE exposure sources difficult to ascertain, though it is clear from the high concentrations measured on these wristbands that some of these OPEs seem to be associated with on-duty exposures, though not with responding to fire events. These differences in exposure experienced on-duty may be due to building materials, and/or materials found within the firehouses such as furniture.
PFAS
Of the 18 PFAS compounds quantified, 7 were detected in >50% of samples. 6:2 diPAP had the highest median value of all PFAS measured (Table 2) though PFAS values were generally measured at lower levels on all firefighter wristbands compared to other classes of SVOC evaluated.
Generally, little difference was observed between off-duty and on-duty exposures for each PFAS (Figure 6). Of note, the fire departments in this study did not use firefighting foams, such as aqueous film forming foam (AFFF), while responding to fires during this study collection period. Significantly higher concentrations were observed for PFOS when on-duty and responding to a fire, which may be associated with firefighting gear.44 Interestingly, 6:2 diPAP, a perfluoroalkyl acid (PFAA) precursor which degrades into less-persistent PFAA compounds, was significantly higher when off-duty as compared to on-duty. Though many PFAS precursors degrade in the environment due to their different chemical structures, these precursors unfortunately degrade into more persistent PFAAs. 6:2 diPAP has previously been observed in high levels in dust in fire stations and residential settings in North America.9 The US EPA reports that 6:2 diPAP is typically used as a flame retardant, an emulsion stabilizer, and a surfactant,45 and is found in products such as paper and board-finishing agents,46 fast food packaging, and floor coatings.47–49
Figure 6.
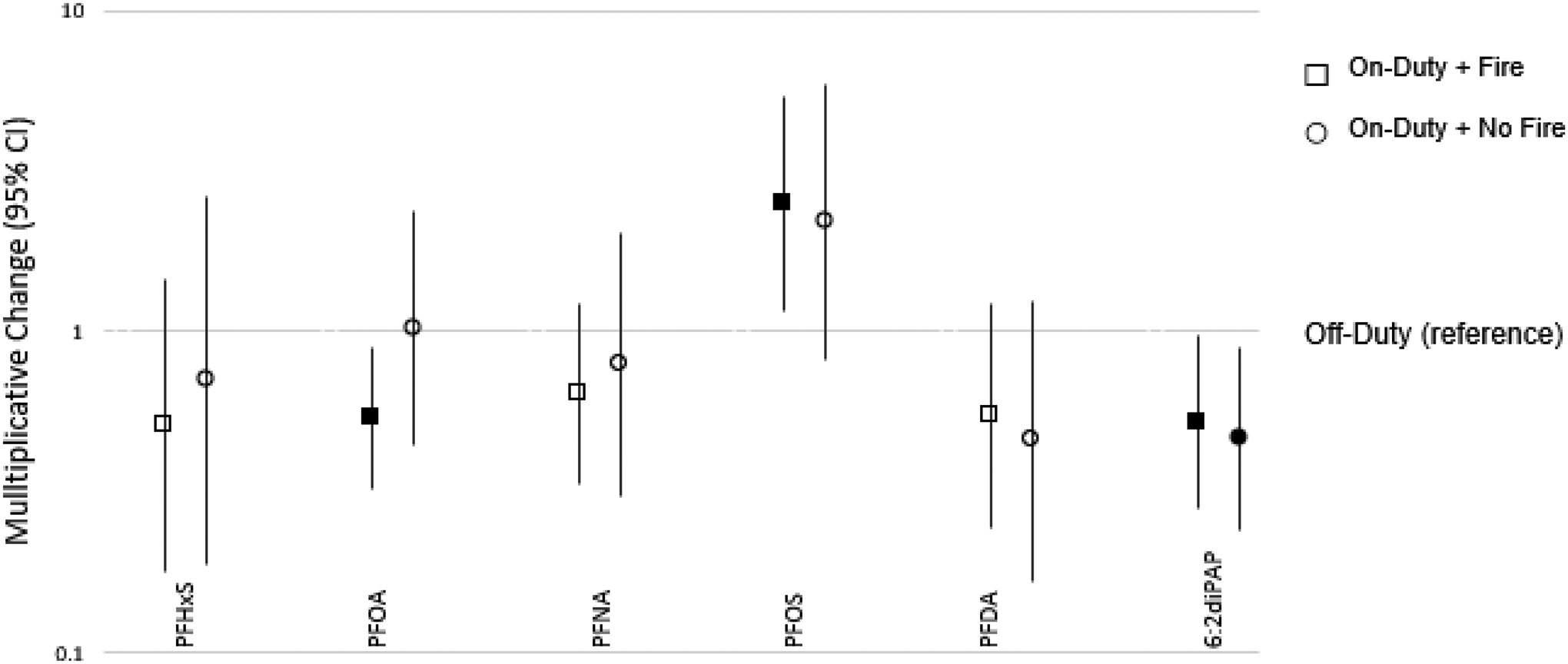
Multiplicative change (10β) in silicone wristband PFAS measurements while on-duty (with fire event and without fire event) as compared to off-duty. Exponentiated beta coefficients from these regression analyses represent the multiplicative change in log10-transformed mass of chemical(s) found on on-duty wristbands relative to the reference category of off-duty wristbands. Filled shapes indicate p<0.05. Acronyms: PFHxS = Perfluorohexanesulfonic acid; PFOA = Perfluorooctanoic acid; PFNA = Perfluorononanoic acid; PFOS = Perfluorooctane sulfonic acid; PFDA = Perfluorodecanoic acid; 6:2 diPAP = 6:2 Fluorotelomer phosphate diester.
Pesticides
Pesticide exposure was not associated with firefighting, and little difference was observed between off-duty and on-duty exposures for any individual compound. A small number of pesticides commonly found in indoor environments were targeted in our methods, and only six of these were found in at least 50% of firefighter wristbands. Cis- and trans-permethrin were found at the highest levels among all pesticides and were the only two pesticides found on 100% of all firefighter wristbands. Pyrethroid pesticides such as permethrin are often associated with indoor pesticide use, in particular products such as insect control sprays, pet products, and lice treatment and shampoos.50–52 As such, both cis- and trans-permethrin were found at significantly higher levels while off-duty as compared to on-duty (SI Figure S3).
Limitations and Strengths
While this study provided insight into differences in chemical exposures experienced by firefighters, there were several limitations that should be considered. Our convenience sample of firefighters was relatively small and consisted of primarily White men from central North Carolina. These municipal firefighter’s exposures may not be representative of all exposures experienced by all types of firefighters (such as those of wildfire fighters, firefighters in more urban or more rural settings, or those in industrial settings). However, the individuals included in our study responded to a range of fire calls (including residential fires, vehicle fires, business fires, and controlled burns for training purposes). Limited information was collected regarding showering and hand washing throughout each period while wearing a wristband, although, in general, bathing patterns were similar across all three time periods based on the survey responses collected. As such, we cannot comment on the impact of hand washing or showering on wristband loading at this time. This small cohort was unfortunately not large enough to draw conclusions regarding how product use or behavioral habits may impact exposure to these firefighters. For example, some firefighters had second jobs while off-duty, though we were unable to comment on the effect these secondary exposures, they may have contributed to off-duty exposures. Importantly, exposure at second jobs would likely mask any suggestion of occupational exposure during firefighting.
Strengths of this study include the study design, which captured differences in exposure based on the type of shift experienced by the firefighter. Though silicone passive samplers have been used to investigate firefighter exposures, these previous investigations have done so either through investigations of a single 24 hour day wearing the passive sampling device14,15 or through suspect screening of a wide range of chemicals. Our study focuses on the widest targeted screening, which typically has higher sensitivity than non-targeted analyses, of compounds of interest. As such, for the compounds quantified herein as compared to those analyzed through suspect screening on silicone dog tags,28 our detection frequencies are considerably higher. Our ability to compare between three different events (i.e., on duty fire/no fire or off duty) means that the occupational exposures specific to firefighters can be further elucidated. Importantly, in this investigation, we observed statistically significant differences related to occupational task in a small population of firefighters that responded to only one or two fires over the 6 days while they wore a wristband. Of the 20 firefighters that wore their wristbands during fire events, 13 of these firefighters only responded to one fire event and 7 responded to two fire events. However, the median amount of total time spent at a fire was about 1.5h regardless of if firefighters experienced one or two fires during that work shift. This demonstrates that the short duration of time spent near a fire significantly increases exposure to several chemical classes, and particularly PAHs, and this difference in exposure can be detected with silicone wristbands. Though more data is needed, this suggests that wristbands are a sensitive passive exposure sampling method for picking up hazardous chemicals to which firefighters may be exposed. Additionally, this is the first targeted analysis of firefighter occupational exposure using silicone wristbands that has measured such a wide range of semi-volatile organic compounds and is the first study to use silicone wristbands to monitor exposure to PFAS. Silicone wristbands are thought to measure the potential exposure that may be experienced through both dermal exposure and inhalation exposure, not only one specific exposure route.53–56 This means that chemical exposure associated with a particular exposure pathway cannot necessarily be isolated using our current study design, but the ability to measure non-dietary exposure routes through a single exposure matrix is a strength for estimating occupational exposures
Conclusion
Firefighters’ occupational exposures were measured on wristbands at higher levels than in previous studies of the general adult population, particularly for PAHs and BFRs.29,57 Specifically, elevated BFRs and PAHs are associated with firefighter on-duty exposure, and firefighters are exposed to PAHs at higher levels while specifically responding to fire events. Using silicone wristbands, we compared occupational and off-duty exposures to investigate firefighter occupational exposures.
By understanding firefighter occupational exposures, we can better hypothesize which exposures may warrant further research for their role as potential risk factors in cancer development. In the future, silicone wristbands may be utilized to further inform the science regarding chemical exposures associated with firefighting, such as other combustion related exposures.58 Additionally, silicone wristbands can be used in larger, epidemiological studies to evaluate associations between health effects and multi-chemical exposure(s). Though silicone wristbands have not yet been investigated for their ability to measure combustion related exposures such as environmentally persistent free radicals, these relatively new passive sampling devices may be instrumental in further characterizing firefighter occupational exposures.
Supplementary Material
Acknowledgements
Funding for this research was provided by The Duke Cancer Institute and the National Institute of Health [U2C-ES030857]. We would like to thank all employees of the Durham Firefighter’s Department who participated in our study. We would particularly like to thank and acknowledge Analia Alvarez, Wayne Cheek, Anna Hoxie, and Corey Miller for their coordination at the firehouses and for their continued support. Jessica L. Levasseur is a Health Policy Research Scholar, a national leadership program supported by the Robert Wood Johnson Foundation. (www.healthpolicyresearch-scholars.org).
Footnotes
Supplemental Information
Additional information on analytic methods, more detailed summary statistics, and pesticide measurements are provided in the supplemental information.
The authors declare no competing financial interests.
References
- 1.Savitz DA, Oxman RT, Metzger KB, et al. Epidemiologic research on man-made disasters: Strategies and implications of cohort definition for World Trade Center worker and volunteer surveillance program. Mt Sinai J Med A J Transl Pers Med. 2008;75(2):77–87. doi: 10.1002/MSJ.20023 [DOI] [PubMed] [Google Scholar]
- 2.National Institute for Occupational Safety and Health (NIOSH) (CDC). World Trade Center Health Program. Atlanta, GA: US Department of Health and Human Services, CDC, National Institute for Occupational Safety and Health. Published 2020. Accessed December 1, 2021. https://www.cdc.gov/wtc/index.html [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) CDC NI for OS and H. World Trade Center Health Program Member Handbook, Version III.; 2020.
- 4.Shapiro M, Wallenstein S, Dasaro C, et al. Cancer in General Responders Participating in World Trade Center Health Programs, 2003–2013. JNCI cancer Spectr. 2019;4(1). doi: 10.1093/JNCICS/PKZ090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.IARC. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans VOLUME 98 Painting, Firefighting, and Shiftwork. Vol 98.; 2010. [PMC free article] [PubMed] [Google Scholar]
- 6.Poutasse CM, Poston WSC, Jahnke SA, et al. Discovery of firefighter chemical exposures using military-style silicone dog tags. Environ Int. 2020;142(May):105818. doi: 10.1016/j.envint.2020.105818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waldman JM, Gavin Q, Anderson M, et al. Exposures to environmental phenols in Southern California firefighters and findings of elevated urinary benzophenone-3 levels. Environ Int. 2016;88:281–287. doi: 10.1016/J.ENVINT.2015.11.014 [DOI] [PubMed] [Google Scholar]
- 8.Alexander BM, Baxter CS. Flame-retardant contamination of firefighter personal protective clothing – A potential health risk for firefighters. J Occup Environ Hyg. 2016;13(9):D148–D155. doi: 10.1080/15459624.2016.1183016 [DOI] [PubMed] [Google Scholar]
- 9.Hall SM, Patton S, Petreas M, et al. Per- And Polyfluoroalkyl Substances in Dust Collected from Residential Homes and Fire Stations in North America. Environ Sci Technol. 2020;54(22):14558–14567. doi: 10.1021/ACS.EST.0C04869/SUPPL_FILE/ES0C04869_SI_001.PDF [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dobraca D, Israel L, McNeel S, et al. Biomonitoring in California Firefighters: Metals and Perfluorinated Chemicals. J Occup Environ Med. 2015;57(1):88. doi: 10.1097/JOM.0000000000000307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaw SD, Berger ML, Harris JH, et al. Persistent organic pollutants including polychlorinated and polybrominated dibenzo-p-dioxins and dibenzofurans in firefighters from Northern California. Chemosphere. 2013;91(10):1386–1394. doi: 10.1016/J.CHEMOSPHERE.2012.12.070 [DOI] [PubMed] [Google Scholar]
- 12.Mayer AC, Fent KW, Chen IC, et al. Characterizing exposures to flame retardants, dioxins, and furans among firefighters responding to controlled residential fires. Int J Hyg Environ Health. 2021;236. doi: 10.1016/J.IJHEH.2021.113782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fent KW, Toennis C, Sammons D, et al. Firefighters’ absorption of PAHs and VOCs during controlled residential fires by job assignment and fire attack tactic. J Expo Sci Environ Epidemiol 2019 302. 2019;30(2):338–349. doi: 10.1038/s41370-019-0145-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baum JLRR, Bakali C, Killawala C, et al. Evaluation of silicone-based wristbands as passive sampling systems using PAHs as an exposure proxy for carcinogen monitoring in firefighters: Evidence from the firefighter cancer initiative. Ecotoxicol Environ Saf. 2020;205:111100. doi: 10.1016/j.ecoenv.2020.111100 [DOI] [PubMed] [Google Scholar]
- 15.Caban-Martinez AJ, Louzado-Feliciano P, Santiago KM, et al. Objective Measurement of Carcinogens Among Dominican Republic Firefighters Using Silicone-Based Wristbands. J Occup Environ Med. 2020;62(11):e611–e615. doi: 10.1097/JOM.0000000000002006 [DOI] [PubMed] [Google Scholar]
- 16.Yilmaz B, Terekeci H, Sandal S, Kelestimur F. Endocrine disrupting chemicals: exposure, effects on human health, mechanism of action, models for testing and strategies for prevention. Rev Endocr Metab Disord 2019 211. 2019;21(1):127–147. doi: 10.1007/S11154-019-09521-Z [DOI] [PubMed] [Google Scholar]
- 17.Weschler CJ, Nazaroff WW. Semivolatile organic compounds in indoor environments. Atmos Environ. 2008;42(40):9018–9040. doi: 10.1016/j.atmosenv.2008.09.052 [DOI] [Google Scholar]
- 18.Kabir ER, Rahman MS, Rahman I. A review on endocrine disruptors and their possible impacts on human health. Environ Toxicol Pharmacol. 2015;40(1):241–258. doi: 10.1016/j.etap.2015.06.009 [DOI] [PubMed] [Google Scholar]
- 19.Giulivo M, Lopez de Alda M, Capri E, Barceló D. Human exposure to endocrine disrupting compounds: Their role in reproductive systems, metabolic syndrome and breast cancer. A review. Environ Res. 2016;151:251–264. doi: 10.1016/j.envres.2016.07.011 [DOI] [PubMed] [Google Scholar]
- 20.Predieri B, Bruzzi P, Bigi E, et al. Endocrine Disrupting Chemicals and Type 1 Diabetes. Int J Mol Sci. 2020;21(8). doi: 10.3390/ijms21082937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hammel SC, Hoffman K, Webster TF, Anderson KA, Stapleton HM. Measuring Personal Exposure to Organophosphate Flame Retardants Using Silicone Wristbands and Hand Wipes. Environ Sci Technol. 2016;50(8):4483–4491. doi: 10.1021/acs.est.6b00030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wise CF, Hammel SC, Herkert N, et al. Comparative Exposure Assessment Using Silicone Passive Samplers Indicates That Domestic Dogs Are Sentinels To Support Human Health Research. Environ Sci Technol. 2020;54(12):7409–7419. doi: 10.1021/acs.est.9b06605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reddam A, Tait G, Herkert N, Hammel SC, Stapleton HM, Volz DC. Longer commutes are associated with increased human exposure to tris(1,3-dichloro-2-propyl) phosphate. Environ Int. 2020;136:105499. doi: 10.1016/j.envint.2020.105499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hammel SC, Hoffman K, Phillips AL, et al. Comparing the Use of Silicone Wristbands, Hand Wipes, And Dust to Evaluate Children’s Exposure to Flame Retardants and Plasticizers. Environ Sci Technol. 2020;54(7):4484–4494. doi: 10.1021/acs.est.9b07909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Herkert NJ, Merrill J, Peters C, et al. Assessing the Effectiveness of Point-of-Use Residential Drinking Water Filters for Perfluoroalkyl Substances (PFASs). Environ Sci Technol Lett. 2020;7(3):178–184. doi: 10.1021/ACS.ESTLETT.0C00004 [DOI] [Google Scholar]
- 26.Poutasse CM. New Configurations of Silicone Passive Sampling Devices: Quantifying Feline and Firefighter Chemical Exposures. Published online February 19, 2020. Accessed July 9, 2021. https://ir.library.oregonstate.edu/concern/graduate_thesis_or_dissertations/ks65hk80h?locale=en
- 27.Hoffman K, Levasseur JL, Zhang S, Hay D, Herkert NJ, Stapleton HM. Monitoring Human Exposure to Organophosphate Esters: Comparing Silicone Wristbands with Spot Urine Samples as Predictors of Internal Dose. Cite This Environ Sci Technol Lett. 2021;8:45. doi: 10.1021/acs.estlett.1c00629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Poutasse CM, Haddock CK, Poston WSC, et al. Firefighter exposures to potential endocrine disrupting chemicals measured by military-style silicone dog tags. Environ Int. 2022;158:106914. doi: 10.1016/J.ENVINT.2021.106914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hammel SC, Phillips AL, Hoffman K, Stapleton HM. Evaluating the Use of Silicone Wristbands to Measure Personal Exposure to Brominated Flame Retardants. Environ Sci Technol. 2018;52(20):11875–11885. doi: 10.1021/acs.est.8b03755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kassotis CD, Herkert NJ, Hammel SC, et al. Thyroid Receptor Antagonism of Chemicals Extracted from Personal Silicone Wristbands within a Papillary Thyroid Cancer Pilot Study. Environ Sci Technol. 2020;54(23):15296–15312. doi: 10.1021/acs.est.0c05972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gong M, Zhang Y, Weschler CJ. Measurement of Phthalates in Skin Wipes: Estimating Exposure from Dermal Absorption. Published online 2014. doi: 10.1021/es501700u [DOI] [PubMed]
- 32.Guo Y, Kannan K. A survey of phthalates and parabens in personal care products from the United States and its implications for human exposure. Environ Sci Technol. 2013;47(24):14442–14449. doi: 10.1021/es4042034 [DOI] [PubMed] [Google Scholar]
- 33.Api A Toxicological profile of diethyl phthalate: a vehicle for fragrance and cosmetic ingredients. Food Chem Toxicol. 2001;39(s):97–108. doi: 10.1016/S0278-6915(00)00124-1. [DOI] [PubMed] [Google Scholar]
- 34.Alexander BM, Baxter CS. Plasticizer Contamination of Firefighter Personal Protective Clothing: A Potential Factor in Increased Health Risks in Firefighters. J Occup Environ Hyg. 2014;11(5):D43–48. [DOI] [PubMed] [Google Scholar]
- 35.Alexander BM. Contamination of Firefighter Personal Protective Gear. Published online 2012.
- 36.Stapleton HM, Sharma S, Getzinger G, et al. Novel and high volume use flame retardants in US couches reflective of the 2005 PentaBDE phase out. Environ Sci Technol. 2012;46(24):13432–13439. doi: 10.1021/ES303471D/SUPPL_FILE/ES303471D_SI_001.PDF [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stapleton HM, Eagle S, Sjödin A, Webster TF. Serum PBDEs in a North Carolina toddler cohort: Associations with handwipes, house dust, and socioeconomic variables. Environ Health Perspect. 2012;120(7):1049–1054. doi: 10.1289/ehp.1104802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bergh C, Torgrip R, Emenius G, Östman C. Organophosphate and phthalate esters in air and settled dust – a multi-location indoor study. Indoor Air. 2011;21(1):67–76. doi: 10.1111/J.1600-0668.2010.00684.X [DOI] [PubMed] [Google Scholar]
- 39.Marklund A, Andersson B, Haglund P. Screening of organophosphorus compounds and their distribution in various indoor environments. Chemosphere. 2003;53(9):1137–1146. doi: 10.1016/S0045-6535(03)00666-0 [DOI] [PubMed] [Google Scholar]
- 40.Van den Eede N, Dirtu AC, Neels H, Covaci A. Analytical developments and preliminary assessment of human exposure to organophosphate flame retardants from indoor dust. Environ Int. 2011;37(2):454–461. doi: 10.1016/J.ENVINT.2010.11.010 [DOI] [PubMed] [Google Scholar]
- 41.Young AS, Allen JG, Kim U-J, et al. Phthalate and Organophosphate Plasticizers in Nail Polish: Evaluation of Labels and Ingredients. Environ Sci Technol. 2018;52:12841–12850. doi: 10.1021/acs.est.8b04495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li J, Zhao L, Letcher RJ, et al. A review on organophosphate Ester (OPE) flame retardants and plasticizers in foodstuffs: Levels, distribution, human dietary exposure, and future directions. Environ Int. 2019;127:35–51. doi: 10.1016/J.ENVINT.2019.03.009 [DOI] [PubMed] [Google Scholar]
- 43.Office of Environmental Health Hazard Assessment. Tris(2-chloroethyl) Phosphate (TCEP). Accessed July 20, 2021. www.P65Warnings.ca.gov
- 44.Peaslee GF, Wilkinson JT, McGuinness SR, et al. Another Pathway for Firefighter Exposure to Per- A nd Polyfluoroalkyl Substances: Firefighter Textiles. Environ Sci Technol Lett. 2020;7(8):594–599. doi: 10.1021/acs.estlett.0c00410 [DOI] [Google Scholar]
- 45.US EPA. CompTox Chemicals Dashboard. Published 2015. Accessed July 20, 2021. https://comptox.epa.gov/dashboard/dsstoxdb/results?search=DTXSID50561590#exposure
- 46.Zweigle J, Bugsel B, Schmitt M, Zwiener C. Electrochemical Oxidation of 6:2 Polyfluoroalkyl Phosphate Diester-Simulation of Transformation Pathways and Reaction Kinetics with Hydroxyl Radicals. Cite This Environ Sci Technol. 2021;55:11070–11079. doi: 10.1021/acs.est.1c02106 [DOI] [PubMed] [Google Scholar]
- 47.Chen P, Yang J, Chen G, Yi S, Liu M, Zhu L. Thyroid-Disrupting Effects of 6:2 and 8:2 Polyfluoroalkyl Phosphate Diester (diPAPs) at Environmentally Relevant Concentrations from Integrated in Silico and in Vivo Studies. Environ Sci Technol Lett. 2020;7(5):330–336. doi: 10.1021/ACS.ESTLETT.0C00191/SUPPL_FILE/EZ0C00191_SI_001.PDF [DOI] [Google Scholar]
- 48.De Silva AO, Allard CN, Spencer C, Webster GM, Shoeib M. Phosphorus-containing fluorinated organics: Polyfluoroalkyl phosphoric acid diesters (diPAPs), perfluorophosphonates (PFPAs), and perfluorophosphinates (PFPIAs) in residential indoor dust. Environ Sci Technol. 2012;46(22):12575–12582. doi: 10.1021/ES303172P/SUPPL_FILE/ES303172P_SI_001.PDF [DOI] [PubMed] [Google Scholar]
- 49.Schaider LA, Balan SA, Blum A, et al. Fluorinated Compounds in U.S. Fast Food Packaging. Environ Sci Technol Lett. 2017;4(3):105–111. doi: 10.1021/ACS.ESTLETT.6B00435/SUPPL_FILE/EZ6B00435_SI_001.PDF [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barr DB, Baker SE, Whitehead RDJ, Wong L, Needham LL. Urinary Concentrations of Pyrethroid Metabolites in the Gene… : Epidemiology. Epidemiology. doi: 10.1097/01.ede.0000340081.01840.c5 [DOI] [Google Scholar]
- 51.Donald CE, Scott RP, Blaustein KL, et al. Silicone wristbands detect individuals’ pesticide exposures in West Africa. R Soc Open Sci. 2016;3(8). doi: 10.1098/rsos.160433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rodzaj W, Wileńska M, Klimowska A, et al. Concentrations of urinary biomarkers and predictors of exposure to pyrethroid insecticides in young, Polish, urban-dwelling men. Sci Total Environ. 2021;773. doi: 10.1016/j.scitotenv.2021.145666 [DOI] [PubMed] [Google Scholar]
- 53.Dixon HM, Armstrong G, Barton M, et al. Discovery of common chemical exposures across three continents using silicone wristbands. R Soc Open Sci. 2019;6(2). doi: 10.1098/rsos.181836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang S, Romanak KA, Tarallo S, et al. The use of silicone wristbands to evaluate personal exposure to semi-volatile organic chemicals (SVOCs) in France and Italy. Environ Pollut. 2020;267:115490. doi: 10.1016/j.envpol.2020.115490 [DOI] [PubMed] [Google Scholar]
- 55.Aerts R, Joly L, Szternfeld P, et al. Silicone Wristband Passive Samplers Yield Highly Individualized Pesticide Residue Exposure Profiles. Environ Sci Technol. 2018;52(1):298–307. doi: 10.1021/acs.est.7b05039 [DOI] [PubMed] [Google Scholar]
- 56.Weschler CJ, Nazaroff WW. Dermal uptake of organic vapors commonly found in indoor air. Environ Sci Technol. 2014;48(2):1230–1237. doi: 10.1021/es405490a [DOI] [PubMed] [Google Scholar]
- 57.Wang S, Romanak KA, Tarallo S, et al. The use of silicone wristbands to evaluate personal exposure to semi-volatile organic chemicals (SVOCs) in France and Italy. Environ Pollut. 2020;267. doi: 10.1016/J.ENVPOL.2020.115490 [DOI] [PubMed] [Google Scholar]
- 58.Lomnicki S, Gullett B, Stöger T, et al. Combustion By-Products and their Health Effects - Combustion Engineering and Global Health in the 21st Century: Issues and Challenges. Int J Toxicol. 2014;33(1):3. doi: 10.1177/1091581813519686 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


