Abstract
Background:
The Unified Protocol (UP) is a promising transdisgnostic treatment for emotional disorders; limited data exists with trauma-exposed populations. This study compared effectiveness of the UP, Presented Centered Therapy (PCT), and treatment as usual (TAU) in trauma-exposed veterans presenting to routine care.
Method:
Trauma-exposed veterans with one or more emotional disorder diagnoses participated in a pilot hybrid-1 effectiveness/pre-implementation study. Thirty-seven male and female veterans were randomized to one of three conditions.
Results:
Multilevel growth curve modeling demonstrated improvement over time across conditions with large effect sizes (range: −2.15 to −3.32), with the UP demonstrating the greatest change. The between group effect sizes for reductions in number of comorbid diagnoses were medium to small and statistically significant (TAU and UP, d = 0.49, p = .056; TAU and PCT d = 0.18, p = .166, UP and PCT d = 0.31, p = .229). Only the UP led to a decrease in the number of comorbid diagnoses (d = −.71). Psychosocial functioning varied by group, with slight increases in impairment in PCT and TAU, and medium effect size reduction in the UP. Only the UP exhibited significant decreases in self-reported anxiety and depression. Between group differences for UP and PCT were medium to large and statistically significant for depression across two measures (d = −.72 to d = −1.40).
Conclusions:
This represents the first trial examining effectiveness of the UP, PCT and TAU in trauma-exposed veterans. Despite a small sample, large effect size differences demonstrated promising advantages for the UP.
Keywords: transdiagnostic, comorbidity, trauma, PTSD, depression, anxiety, veteran
Complex mental health presentations are costly, debilitating (Kessler & Greenberg, 2002; McHugh et al., 2009), and often result in drift from evidence-based approaches toward eclectic approaches (Von Ranson et al., 2013) to treat multiple co-occurring concerns. The Veterans Health Administration (VHA) has completed various evidence-based mental health treatment rollouts that are largely disorder specific (Karlin et al., 2010, 2012, 2013), which can create challenges for treating common comorbidity and complexity (Kessler at al., 2005; Rytwinski et al., 2013).
Transdiagnostic cognitive behavioral therapies (CBTs) have the potential to meet the diverse needs by utilizing one protocol for a range of primary and comorbid disorders (McHugh et al., 2009). Furthermore, a transdiagnostic approach that targets common neurobiological mechanisms (Barlow et al., 2014) may optimize both patient and clinician time (Barlow, et al., 2020). The Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders (UP; Barlow et al., 2017; Barlow et al., 2017; Farchione et al., 2012) has demonstrated promise across a range of emotional disorders compared to single diagnosis protocols (SDPs). The strongest data are in White females with anxiety and depressive disorders, which is not representative of the larger population, and underscores the need for research representative of routine care (Cassiello-Robins et al., 2020). Additionally, trauma-exposed populations have been under-represented in UP trials and other transdiagnostic treatments despite the frequent cooccurrence with other emotional disorders (Gutner & Presseau, 2019). Evidence on the UP and trauma-exposed populations is limited because it has not been the focus of prior trials.
The VHA provides mental health treatment to a range of veterans presenting with PTSD and trauma exposure that results in other diagnoses including, but not limited to anxiety, depressive and obsessive-compulsive disorders. The diverse presentations to mental health services including diagnoses that are common in trauma-exposed populations suggest that there may be benefits to providing the UP in VHA mental health service settings. A treatment that can address symptoms and underlying problems that occur after trauma exposure (e.g., depression, anxiety, post-traumatic stress) may be effective and efficient in treatment settings that serve diverse diagnostic and treatment needs. This study examined the effectiveness of the UP in trauma-exposed veterans presenting for routine mental health care within the VHA, who agreed to participate in a pilot hybrid type-1 effectiveness-implementation study (Curran et al., 2012; see Gutner et al., 2019 for qualitative implementation-related findings). The aims of the study were to evaluate the UP for a trauma-exposed veteran population with a range of emotional disorders, and examine changes in primary diagnosis and functioning after treatment with the UP compared to transdiagnostic present centered therapy (PCT; Lang et al., 2017), or treatment as usual (TAU). Given the promise of PCT with trauma-exposed populations, we predicted that the UP would outperform TAU, but not PCT, and that the UP would demonstrate advantages in terms of changes in comorbid symptoms (clinical severity rating [CSR], comorbid diagnoses, depression, anxiety) and functioning.
Materials & Methods
Participants
Participants were part of a pilot hybrid type 1 trial that examined clinical outcomes, feasibility, and acceptability of the UP. Thirty-seven trauma-exposed veterans presenting for routine care were recruited via clinician referral between January 2017 and July 2018.
Recruitment was intended to be inclusive and reflect routine care. Participants were included if they were: 18 years of age or older, enrolled in the VA Boston Healthcare System (VABHS); met current criteria for a DSM-5 diagnosis (APA, 2013) for one or more of the following: anxiety disorders, PTSD, or unipolar depression (depressive disorder, not otherwise specified diagnoses were included); experienced trauma exposure during their lifetime (civilian or military); and were willing to discontinue current psychotherapy for emotional disorders if randomized to the UP or PCT condition. Participants were excluded if they: exhibited significant cognitive impairment; had current substance dependence (not abuse) diagnosis requiring medical attention; were seeking treatment for a primary diagnosis of bipolar disorder; had a current diagnosis of psychosis; were at high suicide risk, assessed by the MINI suicidal risk module (Sheehan et al., 1998); or had changed their psychotropic medication within the month prior.
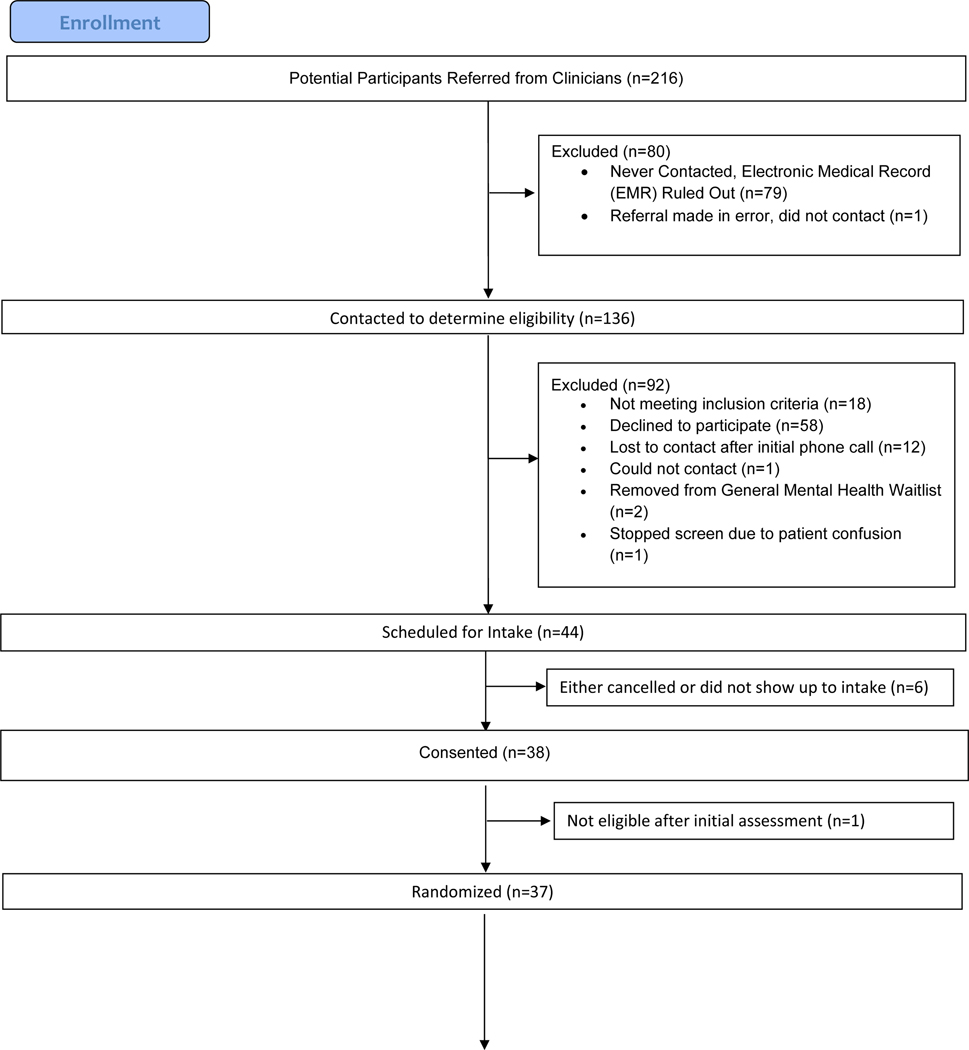
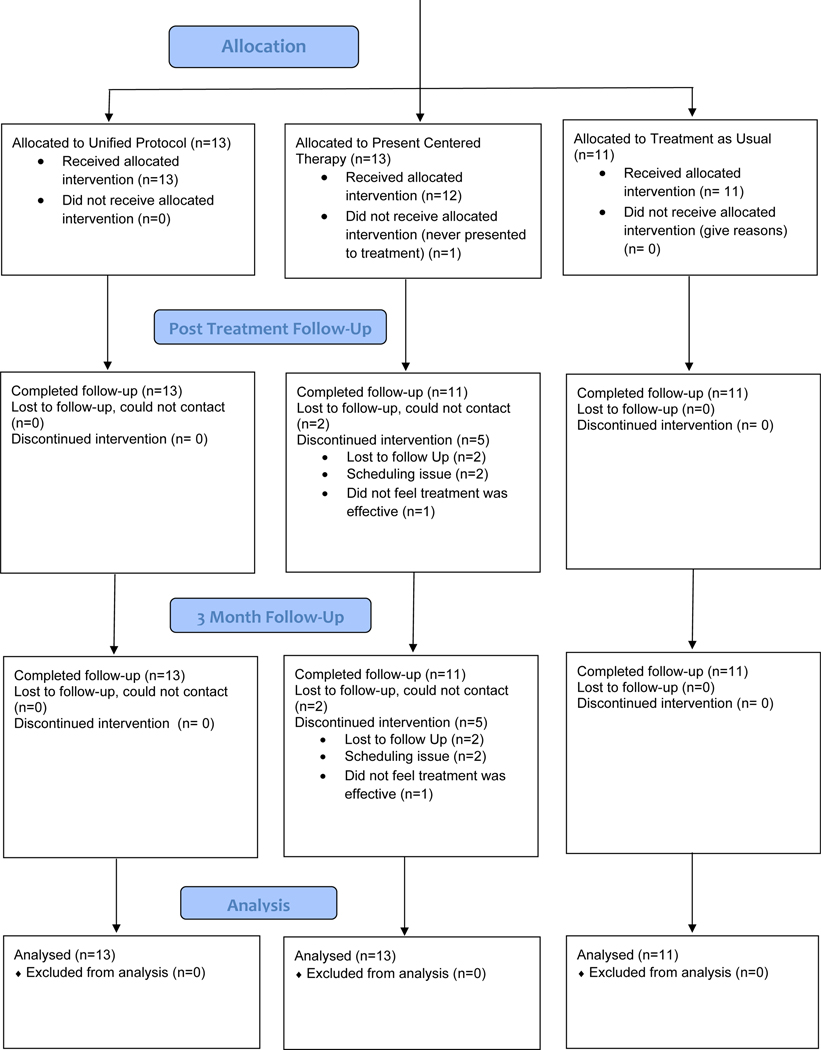
A CONSORT chart (Figure 1) describes participant flow. Demographic information is provided in Table 1 for the intent to treat (ITT) sample who were randomized to UP (n = 13), PCT (n = 13), or TAU (n = 11). Most of the ITT sample was male (81.1%), White (73.3%), and non-Hispanic (83.3%) with a mean age of 46.85 (SD = 13.70).
Figure 1.
CONSORT Diagram
Table 1.
Descriptive information on mental health services received in TAU Group
| Participants | Average number of sessions | ||
|---|---|---|---|
| n | % | Mean (SD) | |
| Individual treatment only | 5 | 62.5 | 8.3 (7.29) |
| Group treatment only | 1 | 12.5 | 5.7 (4.04) |
| Both individual and group treatment | 2 | 18.2 | -- |
| Psychiatry/medication management | 3 | 27.3 | 4.0 (0.0) |
Procedures
Following clinician referral, participants completed a telephone pre-screen for initial eligibility. All initially eligible individuals were scheduled for an intake appointment, which included written informed consent and a comprehensive diagnostic assessment. Once final eligibility was determined, participants were randomized to treatment condition. All participants were assessed at baseline, posttreatment (3–4 months after baseline), and at 3-month follow-up. Participants were compensated $75 for the baseline assessment, and $50 each for the posttreatment and the 3-month follow-up assessments. Weekly self-report measures were collected from participants randomized to UP and PCT. Participants randomized to the UP and PCT group were offered 12-weekly individual therapy sessions and were asked to complete all 12 sessions within 21 weeks of the baseline assessment. All procedures comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and all procedures were approved by VABHS Institutional Review Board.
Randomization
A research assistant who was uninformed of participants’ study condition scheduled baseline assessments. After consent and eligibility was confirmed, participants were randomized to one of the three conditions using a computerized block randomization with an equal chance of being randomized to each condition. The study assessors remained uninformed of randomization through 3-month follow-up.
Interventions
UP and PCT treatment sessions each lasted 50-minutes and participants were asked to refrain from additional psychotherapy. The TAU condition allowed flexibility in treatment that participants received within routine care.
Unified Protocol (Barlow et al., 2017).
The UP is a modular-transdiagnostic CBT treatment. The UP contains similar treatment components to traditional CBT protocols; however, these strategies are applied to the reactions to emotional experiences regardless of diagnosis. It consists of 8 modules: (1) enhancing motivation, (2) psychoeducation on the adaptive nature of emotions, (3) mindful emotion awareness, (4) cognitive flexibility, (5) identifying and preventing patterns of emotional avoidance, (6) increasing awareness and tolerance of emotion-related physical sensations, (7) emotion-focused exposures, and (8) relapse prevention. In this hybrid study, adaptations were first made to the UP manual and patient workbook to improve fit with a veteran population based on previously collected qualitative data that demonstrated examples were not relatable for veterans and the amount of workbook text was too lengthy. Adaptations included veteran relevant worksheet examples, shorter text in the patient workbook, and simplified language and sentence complexity. All core UP elements were retained.
Present Centered Therapy (Lang et al., 2017).
PCT is a manualized supportive therapy that focuses on current symptoms and functioning. PCT was used as a comparison condition because it has been successfully used in trauma-exposed veterans with varied diagnoses before (Lang et al., 2017), and it allows for the control of nonspecific effects of psychotherapy (Schnurr et al., 2007). PCT involves: (1) education about responses to distressing symptoms, (2) daily monitoring of problems, (3) and active problem-solving of day-to-day difficulties. Therapist provide support and empathetic acceptance of the patients’ concerns throughout treatment.
Treatment as Usual.
Participants were randomized into TAU to allow an evaluation of whether the UP and/or PCT yielded additional benefits to veterans above and beyond what is commonly received in routine care. Participants randomized to TAU were instructed to continue to seek care within VABHS and/or in the community without limitations on treatment type or duration (Table 1). TAU occurred in VABHS routine care and ranged from monthly psychiatry appointments to weekly individual and/or group psychotherapy. Because treatment occurred outside of the study, collection of weekly data was not feasible.
Therapists & Treatment Fidelity.
To eliminate differences in experience, therapists administered both the UP and PCT. They included psychology interns, postdoctoral fellows, and licensed psychologists at VABHS. One therapist had previous experience with PCT and one had previous experience with the UP; however, most were new to both interventions. Therapists ranged from 0 to 10+ years of manualized treatment experience. UP and PCT therapists attended gold standard trainings and received weekly supervision for both treatments throughout the study. Fifteen percent of treatment sessions were rated for fidelity by a team of external expert raters using standardized fidelity measures for each of the protocols. Average fidelity for UP and PCT was good to excellent (4.34/5 and 4.32/5, respectively).
Measures
Clinician-Rated Symptom Severity.
Participants completed clinician-administered semi-structured interviews to assess symptom severity at baseline, posttreatment, and 3-month follow-up. The Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5; Brown & Barlow, 2014) was used to diagnose anxiety, mood, obsessive compulsive, and related disorders (e.g., somatic symptom, substance use). The ADIS-5 provides a continuous measure of symptom presentation for differential diagnoses and results in a 0–8 dimensional clinical severity rating (CSR), where CSRs 4 and above are indicative of clinical diagnoses. The PTSD section of the ADIS was replaced with the Clinician Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2012). The CAPS-5 assessed for the presence and severity of PTSD or a diagnosis of otherwise specified traumatic stress disorders if full PTSD diagnostic criteria was not present. This data was also rated on the CSR scale to align with the ADIS-5 diagnoses.
Self-report Measures.
Several self-report measures were included at all timepoints. At baseline, trauma exposure and index trauma were assessed with the Life Events Checklist for DSM-5 (LEC-5; Weathers et al., 2013). Psychosocial functioning was measured by the Inventory of Psychosocial Functioning (IPF; Rodriguez et al., 2012), an 80-item measure that assesses impairment over the past 30 days across 7 domains. The PHQ-9 (Kroenke & Spritzer, 2002) was administered as a brief validated depression measure. Participants in the UP and PCT condition also completed two 5-item weekly measures, the Overall Anxiety Severity and Impairment Scale (OASIS; Norman et al., 2006) and the Overall Depression Severity and Impairment Scale (ODSIS; Bentley et al., 2014), to assess clinical and nonclinical levels of anxiety symptoms and mood impairment. The 5-item client satisfaction questionnaire (CSQ; Larsen et al., 1979) was administered at posttreatment to assess overall treatment satisfaction.
Analytic Plan
To examine change in outcome from baseline to three-month follow-up, and whether these changes significantly varied across conditions, we conducted multilevel modeling in R (R Core Team, 2018) using the lme4 (Bates et al., 2015) and lmerTest (Kuznetsova et al., 2017) packages. The lmer function’s maximum likelihood estimation allowed for the ITT analyses without data imputation procedures. We included the nesting level of patients (random effects) and modeled time as the number of days between baseline and each assessment. Prior to examining the impact of treatment condition on change, we evaluated various unconditional growth models to determine the most reliable manner to model time. After we compared the log-likelihood estimates to identify the most appropriate unconditional growth model, we added the interaction of treatment condition by time to test the impact of treatment condition on change in outcome variables. We computed effect sizes (d) for differences in change between the treatment conditions following the procedures described by Feingold (2009), with d = 0.20, 0.50, 0.80 indicating small, medium, and large effect sizes, respectively.
Results
Index trauma information is available in Table 3, and primary diagnoses across time are presented in Table 4. The average number of traumas experienced by the participants at baseline was 17 (SD = 7.53). Figure 1 reports that 5/13 (38.5%) veterans in PCT dropped out, while none dropped out of UP (X2 (1, N = 26) = 3.96, p = .047). Missing data were minimal, with only two participants from the PCT condition lost to follow-up. At posttreatment, a slightly larger proportion of participants did not meet diagnostic criteria on their primary diagnosis in the PCT (45.5%) and UP (46.2%) conditions relative to the TAU condition (36.4%), but a chi-squared test indicated that this proportion did not significantly vary across conditions, χ2 (2, N = 35) = 0.73, p = .693 (Table 2). There was only one change between posttreatment and follow-up; one participant in the UP condition who did not meet criteria for diagnostic criteria at the posttreatment assessment did meet criteria at the follow-up assessment, changing the proportion in this group to 53.8%. At the follow-up, the proportion did not significantly vary across groups, χ2 (2, N = 35) = 0.28, p = .871. At the posttreatment assessment, mean CSQ scores were 29.88 (SD = 2.75) for PCT and 30.15 (SD = 2.85) for UP, with no statistically significant difference, t(19) = .22, p = .828, d = 0.10.
Table 3.
Index Trauma and Diagnoses at Pretreatment, Posttreatment, and Follow-up
| Index trauma | Treatment condition |
||
|---|---|---|---|
| TAU | PCT | UP | |
|
| |||
| Natural disaster | 0 (0.0) | 1 (7.7) | 2 (15.4) |
| Transportation accident | 0 (0.0) | 0 (0.0) | 1 (7.7) |
| Assault with a weapon | 0 (0.0) | 1 (7.7) | 0 (0.0) |
| Sexual assault | 0 (0.0) | 5 (45.5) | 1 (7.7) |
| Combat or exposure to a war-zone | 0 (0.0) | 1 (7.7) | 2 (15.4) |
| Life-threatening illness or injury | 3 (27.3) | 1 (7.7) | 0 (0.0) |
| Severe human suffering | 1 (9.1) | 1 (7.7) | 2 (15.4) |
| Sudden violent death | 3 (27.3) | 1 (7.7) | 1 (7.7) |
| Sudden accidental death | 1 (9.1) | 1 (7.7) | 1 (7.7) |
| Other | 3 (27.3) | 1 (7.7) | 1 (7.7) |
Note. TAU = Treatment as Usual, PCT = Present Centered Therapy, UP = Unified Protocol.
Table 4.
Index Trauma and Diagnoses at Pretreatment, Posttreatment, and Follow-up
| Assessment | Primary diagnosis | Treatment condition |
||
|---|---|---|---|---|
| TAU | PCT | UP | ||
|
| ||||
| Pre | Adjustment disorder | 0 (0.0) | 0 (0.0) | 1 (7.7) |
| Generalized anxiety disorder | 1 (9.1) | 1 (7.7) | 1 (7.7) | |
| Major depressive disorder | 3 (27.3) | 4 (30.8) | 4 (30.8) | |
| Other-specified trauma & stress related disorder |
0 (0.0) | 1 (7.7) | 0 (0.0) | |
| Other-specified depressive disorder | 1 (9.1) | 0 (0.0) | 1 (7.7) | |
| Panic disorder | 0 (0.0) | 0 (0.0) | 1 (7.7) | |
| Persistent depressive disorder | 3 (27.3) | 2 (15.4) | 1 (7.7) | |
| Posttraumatic stress disorder | 2 (18.2) | 5 (38.5) | 2 (15.4) | |
| Social anxiety disorder | 1 (9.1) | 0 (0.0) | 1 (7.7) | |
| Substance use disorder | 0 (0.0) | 0 (0.0) | 1 (7.7) | |
| Post | Adjustment disorder | 0 (0.0) | 0 (0.0) | 1 (7.7) |
| Generalized anxiety disorder | 1 (9.1) | 1 (9.1) | 1 (7.7) | |
| Major depressive disorder | 3 (27.3) | 3 (27.3) | 4 (30.8) | |
| Other-specified trauma & stress related disorder |
1 (9.1) | 1 (9.1) | 0 (0.0) | |
| Other-specified depressive disorder | 0 (0.0) | 0 (0.0) | 1 (7.7) | |
| Panic disorder | 0 (0.0) | 0 (0.0) | 1 (7.7) | |
| Persistent depressive disorder | 3 (27.3) | 1 (9.1) | 1 (7.7) | |
| Posttraumatic stress disorder | 2 (18.2) | 5 (45.5) | 2 (15.4) | |
| Social anxiety disorder | 1 (9.1) | 0 (0.0) | 1 (7.7) | |
| Substance use disorder | 0 (0.0) | 0 (0.0) | 1 (7.7) | |
| 3MFU | Adjustment disorder | 0 (0.0) | 0 (0.0) | 1 (7.7) |
| Generalized anxiety disorder | 1 (9.1) | 1 (9.1) | 1 (7.7) | |
| Major depressive disorder | 3 (27.3) | 3 (27.3) | 4 (30.8) | |
| Other-specified trauma & stress related disorder |
1 (9.1) | 1 (9.1) | 0 (0.0) | |
| Other-specified depressive disorder | 0 (0.0) | 0 (0.0) | 1 (7.7) | |
| Panic disorder | 0 (0.0) | 0 (0.0) | 1 (7.7) | |
| Persistent depressive disorder | 3 (27.3) | 1 (9.1) | 1 (7.7) | |
| Posttraumatic stress disorder | 2 (18.2) | 5 (45.5) | 2 (15.4) | |
| Social anxiety disorder | 1 (9.1) | 0 (0.0) | 1 (7.7) | |
| Substance use disorder | 0 (0.0) | 0 (0.0) | 1 (7.7) | |
Note. TAU = Treatment as Usual, PCT = Present Centered Therapy, UP = Unified Protocol, Pre = pretreatment assessment, Post = posttreatment assessment, 3MFU = 3 month follow-up assessment.
Table 2.
Descriptive Information and Primary Diagnosis Status at Pretreatment, Posttreatment, and Follow-up
| Assessment | Variable | Treatment condition |
||
|---|---|---|---|---|
| TAU | PCT | UP | ||
|
| ||||
| Pre | Sample Size, n | 11 | 13 | 13 |
| Age, M (SD) | 51.04 (12.65) | 48.08 (13.08) | 42.08 (14.72) | |
| Gender, n (%) | ||||
| Female | 0 (0.0) | 2 (15.4) | 5 (38.5) | |
| Male | 11 (100.0) | 11 (84.6) | 8 (61.5) | |
| Race, n (%) | ||||
| Asian | 0 (00) | 0 (0.0) | 1 (7.7) | |
| Black | 5 (45.5) | 3 (23.1) | 1 (7.7) | |
| White | 6 (54.5) | 10 (76.9) | 11 (84.6) | |
| Ethnicity, n (%) | ||||
| Hispanic/Latino | 1 (9.1) | 0 (0.0) | 2 (15.4) | |
| Non-Hispanic/Latino | 7 (63.6) | 10 (76.9) | 8 (61.5) | |
| Unknown | 3 (27.3) | 3 (23.1) | 3 (23.1) | |
| Number of traumas | 14.27 (5.89) | 16.77 (6.58) | 19.54 (9.16) | |
| Post | Sample Size, n | 11 | 11 | 13 |
| Primary dx, n (%) | ||||
| CSR < 4 | 4 (36.4) | 5 (45.5) | 7 (46.2) | |
| CSR >= 4 | 7 (63.6) | 6 (54.5) | 6 (53.8) | |
| 3MFU | Sample Size, n | 11 | 11 | 13 |
| Primary dx, n (%) | ||||
| CSR < 4 | 4 (36.4) | 5 (45.5) | 6 (53.8) | |
| CSR >= 4 | 7 (63.6) | 6 (54.5) | 7 (46.2) | |
Note: TAU = Treatment as Usual, PCT = Present Centered Therapy, UP = Unified Protocol, Pre = pretreatment assessment, Post = posttreatment assessment, 3MFU = 3 month follow-up assessment, CSR = Clinical Severity Rating, n = sample size per condition, M = Mean, SD = Standard Deviation.
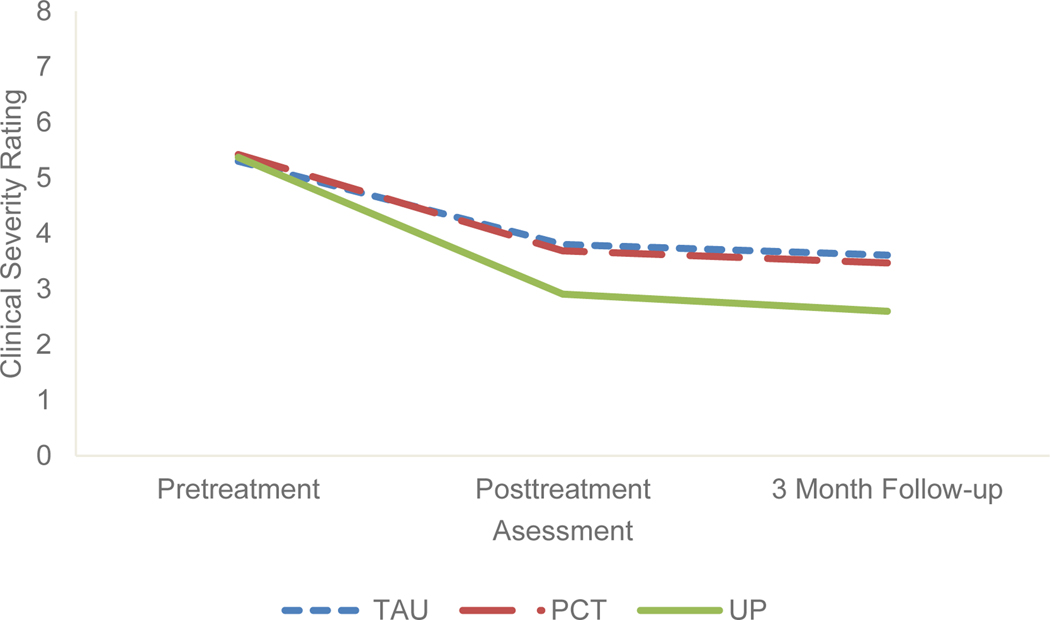
Preliminary unconditional change models indicated that a non-linear change model using the natural log transformation fit the data best at baseline, posttreatment, and follow-up (CSR, PHQ-9, number of comorbid diagnoses, IPF) and a linear change model for session-level outcomes (OASIS, ODSIS). The results of multilevel modeling with the interaction of treatment condition by time are in Table 5, with the results of the CSR analyses in Figure 2. As hypothesized,the between-group effect sizes for the differences in change were large and significant for TAU-UP (d = 1.26, p = .043), large but nonsignificant for UP-PCT (d = 0.95, p = .086), and small-to-medium but nonsignificant for TAU-PCT (d = 0.31, p = .641). All three conditions exhibited large within-group effect size decreases in CSRs (d’s ranging from −1.97 [TAU] to −3.23 [UP]).
Table 5.
Summary of Growth Curve Analyses
| Outcome | Condition | Pre | Post | 3MFU | Change per ln(day) | ΔPre-3MFU | |
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Estimate [95% CI] | Estimate [95% CI] | Estimate [95% CI] | b [95% CI] | Estimate [95% CI] | d | ||
|
| |||||||
| CSR | |||||||
| TAU | 5.30 [4.96, 5.63] | 3.80 [2.60, 5.00] | 3.61 [2.30, 4.92] | −0.32 [−0.50, −0.13] | −1.69 [−2.66, −0.72] | −1.97 | |
| PCT | 5.42 [5.17, 5.67] | 3.69 [2.75, 4.64] | 3.47 [2.43, 4.51] | −0.37 [−0.56, −0.17] | −1.95 [−2.74, −1.17] | −2.28 | |
| UP | 5.37 [4.95, 5.79] | 2.91 [1.96, 3.87] | 2.60 [1.58, 3.63] | −0.52 [−0.69, −0.35] | −2.77 [−3.37, −2.16] | −3.23 | |
| Number of comorbid diagnoses | TAU | 0.63 [0.28, 0.99] | 0.46 [0.12, 0.81] | 0.44 [0.10, 0.79] | −0.04 [−0.09, 0.02] | −0.19 [−0.21, −0.18] | −0.17 |
| PCT | 1.62 [0.90, 2.34] | 1.27 [0.53, 2.01] | 1.23 [0.48, 1.98] | −0.07 [−0.15, 0.00] | −0.39 [−0.68, −0.11] | −0.35 | |
| UP | 1.16 [0.49, 1.82] | 0.50 [0.11, 0.89] | 0.41 [0.03, 0.80] | −0.14 [−0.24, −0.04] | −0.74 [−1.29, −0.20] | −0.66 | |
| Impairment in functioning (IPF) | TAU | 34.30 [26.20, 42.39] | 34.55 [27.00, 42.11] | 34.59 [27.10, 42.07] | 0.05 [−1.06, 1.17] | 0.29 [−0.32, 0.91] | 0.02 |
| PCT | 33.06 [27.01, 39.11] | 34.11 [26.64, 41.58] | 34.24 [26.59, 41.90] | 0.22 [−0.80, 1.25] | 1.19 [−0.60, 2.97] | 0.09 | |
| UP | 37.15 [29.59, 44.72] | 30.59 [22.87, 38.31] | 29.74 [21.88, 37.61] | −1.39 [−2.39, −0.38] | −7.41 [−11.51, −3.31] | −0.55 | |
| Depression (PHQ-9) | |||||||
| TAU | 15.17 [11.62, 18.73] | 12.41 [9.16, 15.67] | 12.06 [8.84, 15.28] | −0.58 [−1.07, −0.10] | −3.11 [−3.46, −2.78] | −0.56 | |
| PCT | 10.92 [8.67, 13.18] | 11.76 [8.55, 14.96] | 11.86 [8.53, 15.19] | 0.18 [−0.30, 0.65] | 0.94 [−0.14, 2.02] | 0.17 | |
| UP | 16.95 [13.54, 20.35] | 9.30 [6.03, 12.57] | 8.31 [4.93, 11.70] | −1.62 [−2.25, −0.99] | −8.63 [−11.37, −5.89] | −1.55 | |
| Weekly anxiety | Session 1 | Session 12 | Change per day | ΔSession 1-Session 12 | |||
| (OASIS) | PCT | 9.02 [6.92, 11.12] | 9.18 [7.36, 11.01] | 0.00 [−0.01, 0.02] | 0.16 [−0.11. 0.44] | 0.04 | |
| UP | 9.44 [7.15, 11.73] | 7.22 [4.68, 9.76] | −0.02 [−0.04, 0.00] | −2.22 [−3.68, −0.76] | −0.48 | ||
| Weekly depression | |||||||
| (ODSIS) | PCT | 9.68 [7.90, 11.46] | 10.08 [8.69, 11.47] | 0.00 [−0.01, 0.02] | 0.40 [0.01, 0.79] | 0.08 | |
| UP | 8.14 [4.96, 11.33] | 5.22 [2.18, 8.26] | −0.03 [−0.04, −0.01] | −2.92 [−3.66, −2.18] | −0.60 | ||
Note. Pre = pretreatment assessment, Post = posttreatment assessment, 3MFU = 3 month follow-up assessment, TAU = Treatment as Usual, PCT = Present Centered Therapy, UP = Unified Protocol, CSR = Clinical Severity Rating, IPF = Inventory of Psychosocial Functioning, PHQ-9 = Patient Health Questionnaire, OASIS = Overall Anxiety Severity and Impairment Scale, ODSIS = Overall Depression Severity and Impairment Scale, b = unstandardized regression coefficient, 95% CI = 95% Confidence Interval, d = Cohen’s d.
Figure 2.
Trajectories of Clinical Severity Ratings (CSR) for Primary Diagnosis as a Function of Treatment Condition
Note. TAU = Treatment as Usual, PCT = Present Centered Therapy, UP = Unified Protocol.
The between-group effect sizes for reductions in number of comorbid diagnoses were small and nonsignificant for TAU-PCT (d = 0.18, p = .166) and contrary to our hypothesis, for the UP-PCT (d = 0.31, p = .229). However, the TAU-UP difference was medium and approached statistical significance (d = 0.49, p = .056). All three conditions exhibited significant within-group reductions in number of comorbid diagnoses which ranged from small to medium effect sizes, d’s = −0.17, −0.35, and −0.66 for the TAU, PCT, and UP, respectively (p < .001, p’s = .010, .012, for the TAU, PCT, and UP; Table 5).
The between-group effect size estimates for change in functional impairments on the IPF fell in the medium range and as we predicted, were significant for TAU-UP (d = 0.57, p = .001) and PCT-UP (d = 0.64, p < .001). The TAU-PCT difference was small and nonsignificant (d = 0.07, p = .347). The TAU (d = 0.02, p = .313) and PCT (d = 0.09, p = .173) conditions exhibited slight increases in functional impairments that were not statistically significant, while the UP condition exhibited a medium, statistically significant reduction (d = −0.55, p = .002).
As we expected, the between-group differences in depression symptom reduction were larger and statistically significant for UP-PCT (d = 1.72, p = <.001), UP-TAU (d = 0.99, p < .001), and were lower forTAU than forPCT (d = 0.73, p < .001), and. The UP (d = −1.55) and TAU (d = −0.56) conditions both exhibited statistically significant (p < .001) decreases in the PHQ-9 from baseline to 3-month follow-up. The PCT condition exhibited minimal and nonsignificant change (d = 0.17, p = .081).
The between group effect size estimates for PCT-UP were medium to large and statistically significant for both anxiety (d = 0.52, p = .003) and depression (d = 0.68, p < .001). Consistent with our hypothesis, only the UP condition exhibited medium to large decreases in self-report weekly anxiety (d = −0.48, p = .006) and depression (d = −0.60, p = < .001). Individuals receiving PCT exhibited minimal changes in weekly OASIS (d = 0.04, p = .214) and minimal but significant increase in weekly ODISIS (d = 0.08, p = .044).
Discussion
The current study represents the first randomized effectiveness study of the UP for trauma-exposed veterans. Although designed as a pilot, results demonstrate great promise for the UP in diagnostically complex trauma-exposed individuals. We anticipated that the UP would outperform TAU but not PCT and that the UP would demonstrate some advantages in comorbidity and functioning. However, the UP and PCT did not to perform equally. Importantly, results suggest that PCT, which was originally developed as an active, non-trauma-focused treatment for PTSD, might not be optimal for people with multiple presenting problems.While TAU can help trauma-exposed populations with depression, anxiety, or PTSD, our findings suggest that, structured treatments targeting emotional disorders may be more beneficial.
The intention of this pilot was to examine differences in effect sizes between groups. When examining change over time, the UP, compared to the TAU group, demonstrated a large effect size difference, with greater change in primary diagnosis occurring in the UP group. The difference between the UP and PCT also approached a large effect size, whereas the difference between PCT and TAU only approached a medium effect size. Thus, preliminary data suggest an advantage of the UP in this population, which is notable for several reasons. First, the UP has traditionally been examined in efficacy studies (Barlow et al., 2017; Farchione et al., 2012) with samples that have primary diagnoses of anxiety disorders and low or unreported rates of trauma. As a result, when patients seek treatment for symptoms common in trauma-exposed populations including PTSD, anxiety, and depression, the UP is rarely considered. These data suggest it could be an effective treatment option to consider, and further, fully-powered studies to evaluate its benefits for trauma-exposed populations are warranted.
Second, PCT has shown lower dropout for trauma-exposed groups compared to trauma-focused treatments (Imel et al., 2013) and has been used transdiagnostically (Lang et al., 2017). Our results suggest that the UP may outperform PCT and TAU for trauma-exposed veterans with a variety of presenting symptoms. This points to a need for more research to consider the UP as a strong viable option for trauma-exposed populations, especially for people who may not want to focus only on their traumatic event(s). The UP also had significantly less dropout compared to PCT which is an important factor to consider and research further.
Participants in the UP group experienced the largest reduction in comorbid diagnoses, though the differences from the other groups were nonsignificant. One of the UP’s goals is to address multiple diagnoses by targeting core mechanisms responsible for disorder development and maintenance. The data provide evidence that the UP can achieve what it is theorized to do, although importantly this study does not test the hypothesized mechanisms. From an implementation perspective, training clinicians to deliver one protocol that effectively reduces symptoms across all diagnoses is highly efficient compared to training in multiple SDPs.
An advantage of the UP was seen with psychosocial functioning with significantly greater change for individuals in UP than those in PCT. Previous studies have demonstrated that following PTSD treatment functional impairment remains an issue (Feingold, 2009). Although most trials focus on reduction in symptom severity as a key indicator of success, functioning and quality of life are arguably equally or more important.
As we expected, this study also demonstrated an advantage of the UP with respect to reductions in weekly anxiety and depression measures. Comparison was not possible with TAU because those participants did not attend weekly study visits. However, compared to PCT, participants who received UP demonstrated significantly greater change during treatment in anxiety across one measure and in depression across two measures. This differential response is notable because the UP has limited published data on mood symptoms. This strong preliminary data suggests the UP can decrease symptoms across emotional disorders, including symptoms related to mood and trauma-exposure. It also supports exploratory research demonstrating that UP reduces depressive symptoms in adults with depressive disorders (Sauzer-Zavala et al., 2020).
A common criticism of clinical trials is that the therapists do not represent those who deliver routine psychotherapy. Importantly, this study utllized clinicians in routine care clinics who represented a vast range of training and experience--from trainees who had never used a manualized treatment to experienced licensed psychologists who regularly provide manualized treatments. The range in therapeutic experience demonstrates that the UP and PCT can be delivered by clinicians in routine care settings with strong fidelity and result in large effect size differences between treatments when trained and supervised by experienced clinicians.
Despite the strong preliminary support for transdiagnostic treatment in trauma-exposed veterans in routine care, there are several notable limitations. First, the study has a small sample size and was not powered to detect small differences in effect sizes. Rather, it was designed to examine a potential signal of effectiveness across treatments. The large effect size differences between conditions suggest that further research on the UP is warranted. Future studies will require a larger sample size to examine potentially important, but smaller differences in effects between the UP and comparison conditions. Although TAU is an important comparison group, another limitation is the variability in the treatment received in the TAU group. Although TAU patients experienced some symptom reduction, the current services may not be structured to produce optimal change. The choice to compare the UP to another transdiagnostic treatment versus an SDP for PTSD allowed exploration about whether this approach may be beneficial where comorbidity is common. Future research should include SDPs for PTSD to elucidate potential non-inferiority for those with PTSD as a primary diagnosis. Finally, although the study oversampled women relative to their representation in the VA patient population, it was challenging to recruit female veterans. Female representation in studies with the veteran population is necessary, as 9.4% of the United States veteran population are women (Department of Veterans Affairs, 2017). Additionally, representation of veterans of color is lacking and is important in future research.
This study demonstrates the promise of the UP for trauma-exposed individuals with multiple diagnoses. It also represents the first attempt to systematically examine the UP in a routine care setting. If replicated with a larger sample, the findings may suggest that the UP can serve as a transdiagnostic protocol to train clinicians in one evidence-based CBT that can be applied across diverse patient populations. Thus, the UP may provide an important solution for challenges that are encountered when implementing SDPs.
Acknowledgement:
The authors would like to thank David H. Barlow, PhD, for his consultation on this study including his input on adaptations to the UP to best fit the current population, and Denise M. Sloan, PhD for her consultation on study design and mentorship on writing the grant that supported this research. The authors submit this work in honor of their colleague Michael K. Suvak, PhD.
Author Note:
This work was supported by National Institute of Health grant K23MH103396 awarded to Dr. Gutner. We would also like to acknowledge the Implementation Research Institute (IRI; NIMH 5R25MH08091607), of which Drs. Gutner and Wiltsey-Stirman are past fellows.
Footnotes
Known Conflict of Interest: None
Trial Registration Number: NCT02944994
Reference
- Bates D, Mächler M, Bolker B, & Walker S.(2015). Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1), 1–48. 10.18637/jss.v067.i01 [DOI] [Google Scholar]
- Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, & Ellard KK (2014). The nature, diagnosis, and treatment of neuroticism: Back to the future. Clinical Psychological Science, 2(3), 344–365. 10.1177/2167702613505532 [DOI] [Google Scholar]
- Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S, ... & Cassiello-Robbins C. (2017). The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: A randomized clinical trial. JAMA psychiatry, 74(9), 875–884. 10.1001/jamapsychiatry.2017.2164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Sauer-Zavala S, Latin HM, Ellard KK, Bullis JR, Bently KH, Boettcher HT, & Cassiello-Robbins. (2017) Unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. Oxford University Press. [Google Scholar]
- Barlow DH, Harris BA, Eustis EH, & Farchione TJ (2020). The unified protocol for transdiagnostic treatment of emotional disorders. World Psychiatry, 19(2), 245–246. 10.1002/wps.20748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley KH, Gallagher MW, Carl JR, & Barlow DH (2014). Development and validation of the Overall Depression Severity and Impairment Scale. Psychological assessment, 26(3), 815–830. 10.1037/a0036216 [DOI] [PubMed] [Google Scholar]
- Brown TA, & Barlow DH Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5) – Adult Version: Client Interview. (2014). Oxford University Press. [Google Scholar]
- Cassiello-Robbins C, Southward MW, Tirpak JW, & Sauer-Zavala S.(2020). A systematic review of Unified Protocol applications with adult populations: Facilitating widespread dissemination via adaptability. Clinical Psychology Review, 78, 101852. [DOI] [PubMed] [Google Scholar]
- Curran GM, Bauer M, Mittman B, Pyne JM, & Stetler C.(2012). Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical care, 50(3), 217–226. https://dx.doi.org/10.1097%2FMLR.0b013e3182408812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Veterans Affairs. Women Veteran Population. Department of Veterans Affairs. (2017). https://www.va.gov/womenvet/docs/womenveteranspopulationfactsheet.pdf.
- Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Thompson-Hollands J, Carl JR, Gallagher MW, & Barlow DH (2012). Unified protocol for transdiagnostic treatment of emotional disorders: a randomized controlled trial. Behavior Therapy. 43(3): 666–678. 10.1016/j.beth.2012.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feingold A.(2009). Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological methods. 2009; 14(1): 43–53. 10.1037/a0014699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green LW, Ottoson JM, Garcia C, & Hiatt RA (2009). Diffusion theory and knowledge dissemination, utilization, and integration in public health. Annual review of public health, 30, 151–174. 10.1146/annurev.publhealth.031308.100049 [DOI] [PubMed] [Google Scholar]
- Gutner CA, & Presseau C.(2019). Dealing with complexity and comorbidity: opportunity for transdiagnostic treatment for PTSD. Current Treatment Options in Psychiatry. 6(2): 119–131. 10.1007/s40501-019-00170-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Yehuda R, Castro CA, McFarlane AC, Vermetten E, Jetly R, Koenen KC, Greenberg N, Shalev AY, Rauch SAM, Marmar CR, & Rothbaum BO (2016). Unintended consequences of changing the definition of posttraumatic stress disorder in DSM-5: critique and call for action. JAMA Psychiatry. 73(7): 750–752. Doi: 10.1001/jamapsychiatry.2016.0647 [DOI] [PubMed] [Google Scholar]
- Imel ZE, Laska K, Jakupcak M, & Simpson TL (2013). Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting & Clinical Psychology. 81(3): 394–404. 10.1037/a0031474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, & Greenberg PE (2002). The economic burden of anxiety and stress disorders. Neuropsychopharmacology: The Fifth Generation of Progress. 981–92. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. Doi: 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kroenke K, & Spitzer RL (2002). The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Annals. 32(9): 509–515. [Google Scholar]
- Kuznetsova A, Brockhoff PB, & Christensen RHB (2017). lmerTest Package: Tests in Linear Mixed Effects Models. Journal of Statistical Software, 82(1), 1–26. 10.18637/jss.v082.i13 [DOI] [Google Scholar]
- Lang AJ, Schnurr PP, Jain S, He F, Walser RD, Bolton E, Benedeck DM, Norman SB, Sylvers P, Flashman L, Strauss J, Ramand R, & Chard KM (2017). Randomized controlled trial of acceptance and commitment therapy for distress and impairment in OEF/OIF/OND veterans. Psychological Trauma: Theory, Research, Practice, and Policy. 9(S1): 74–84. 10.1037/tra0000127 [DOI] [PubMed] [Google Scholar]
- Larsen D, Attkisson CC, Hargreaves WA, & Nguyen TD (1979). Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning. 2, 197–207. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Murray HW, & Barlow DH (2009). Balancing fidelity and adaptation in the dissemination of empirically-supported treatments: The promise of transdiagnostic interventions. Behaviour Research and Therapy. 47(11): 946–953. 10.1016/j.brat.2009.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman SB, Hami Cissell S, Means‐Christensen AJ, & Stein MB (2006) Development and validation of an overall anxiety severity and impairment scale (OASIS). Depression and Anxiety. 23(4): 245–9. 10.1002/da.20182 [DOI] [PubMed] [Google Scholar]
- R Core Team (2018). R: A language and environment for statistical computing [Computer software]. R Foundation for Statistical Computing. https://www.R-project.org/. [Google Scholar]
- Rodriguez P, Holowka DW, & Marx BP (2012) Assessment of posttraumatic stress disorder-related functional impairment: A review. Journal of Rehabilitation Research and Development. 49(5): 649–65. [DOI] [PubMed] [Google Scholar]
- Rytwinski NK, Scur MD, Feeny NC, & Youngstrom EA (2013). The co‐occurrence of major depressive disorder among individuals with posttraumatic stress disorder: A meta‐analysis. Journal of traumatic stress, 26(3), 299–309. [DOI] [PubMed] [Google Scholar]
- Sauer-Zavala S, Bentley KH, Steele SJ, Tirpak JW, Ametaj AA, Nauphal M, Cardona N, Wang M, Farchione TJ & Barlow DH (2020). Treating depressive disorders with the Unified Protocol: A preliminary randomized evaluation. Journal of Affective Disorders, 264, 438–445. 10.1016/j.jad.2019.11.072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, Resick PA, Thurston V, Orsillo SM, Haug R, Turner C, & Bernardy N.(2007). Cognitive Behavioral Therapy for Posttraumatic Stress Disorder in Women: A Randomized Controlled Trial. Journla of the American Medical Association. 297(8): 820–830. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, & Dunbar GC (1998). The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 59: 22–33. [PubMed] [Google Scholar]
- Von Ranson KM, Wallace LM, & Stevenson A.(2013). Psychotherapies provided for eating disorders by community clinicians: Infrequent use of evidence-based treatment. Psychotherapy Research. 23(3): 333–343. 10.1080/10503307.2012.735377 [DOI] [PubMed] [Google Scholar]
- Weathers F, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM Clinician Administered PTSD Scale for DSM 5. Unpublished manuscript. 2012. [Google Scholar]
- Weathers F, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM The Life Events Checklist for DSM-5 (LEC-5) – Extended. 2013. https://www.ptsd.va.gov/professional/assessment/documents/LEC5_Extended_Self-report.PDF