Abstract
Background
Although some adolescents managed to cope well with the challenges brought on by the COVID-19 pandemic, the well-being of many was adversely affected due to school closures, distance education, restrictions on gathering with friends, and limited access to mental health services. Many adolescents reported increased anxiety and depression as well as decreased psychological wellbeing due to the pandemic. Consequently, there is a need for psychological support that exceeds the strained resources available to schools to support young people during times of crisis and societal pressure.
Objective
The present study aimed to explore the effects of an online-delivered ACT intervention to promote adolescent psychological flexibility and self-compassion and decrease psychological distress during the second wave of COVID-19 in the fall of 2020.
Methods
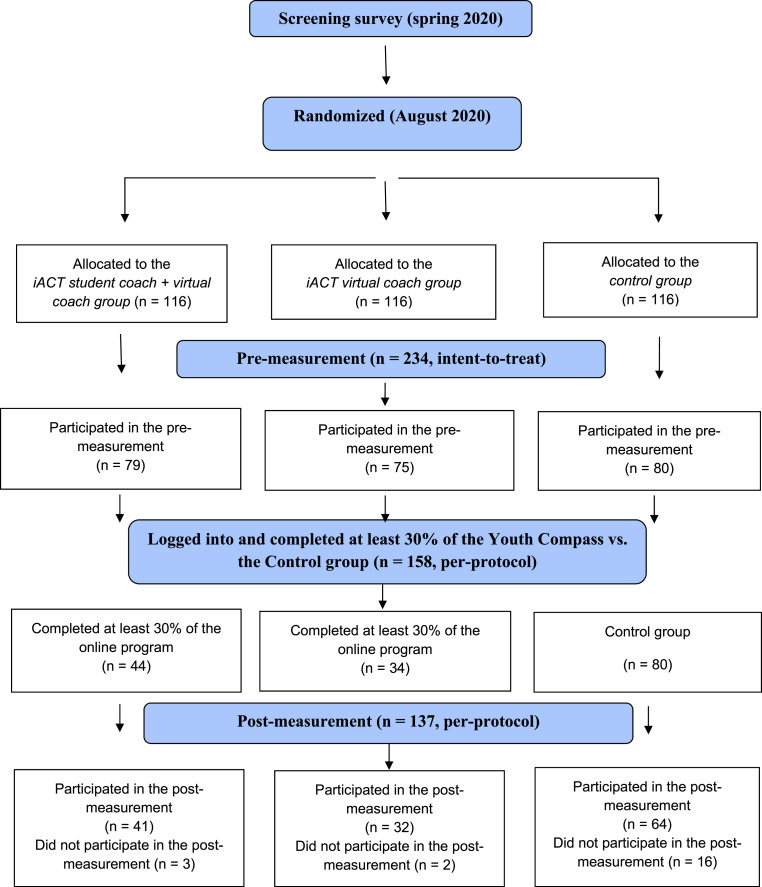
A total of 348 adolescents aged 15–16 were randomly divided into three equal groups: 1) the iACT student coach + virtual coach group, n = 116; 2) the iACT virtual coach group, n = 116; and 3) the control group with no intervention, n = 116). Among these adolescents, 234 participated in a pre-measurement (iACT, n = 154; control, n = 80; intent-to-treat) and completed measures of psychological flexibility, self-compassion, anxiety, and depression.
Results
An investigation of all the adolescents who participated in the pre-measurement (intent-to-treat analysis, n = 234) revealed no significant differences between the three groups with regard to psychological flexibility, self-compassion, and symptoms of anxiety and depression. However, upon combining the two intervention groups and examining the adolescents who completed at least 30% of the Youth Compass program (per-protocol analysis, n = 137), small but significant differences between the iACT intervention and control groups were found regarding the psychological flexibility subscale valued action, self-compassion, and anxiety in favor of the intervention group.
Conclusions
Active use of an ACT-based online intervention under adverse circumstances may decrease symptoms of anxiety and increase psychological flexibility skills in adolescents.
Keywords: ACT, Adolescents, Web-based intervention, Psychological flexibility, Self-compassion, Anxiety
1. Introduction
Stressful conditions have been shown to be a significant risk factor for adolescent mental health (Mastrotheodoros, 2021). One of the most recent challenges faced by adolescents was the COVID-19 pandemic, which resulted in school closures, remote learning, and limited access to mental health services. Longitudinal studies suggest increased mental health symptoms and decreased well-being among adolescents during the pandemic (Mastrotheodoros, 2021). For example, a German study found that of the 1586 children and adolescents examined, two-thirds reported significantly lower quality of life and more mental health problems, such as higher levels of anxiety, compared to the pre-pandemic situation (Ravens-Sieberer et al., 2021). Similar results regarding adolescents have been reported in other studies (e.g., Hafstad et al., 2020, 2021; Hawke et al., 2020; Parola et al., 2020). Maladaptive coping strategies (e.g., rumination) under stressful conditions, pre-existing mental health problems, inadequate family support, and isolation from peers are some of the factors that may have worsened adolescent mental health during the pandemic (Branje & Morris, 2021). Conversely, adaptive coping responses (e.g., acceptance, self-compassion) may have helped some adolescents alleviate COVID-19-related distress (She et al., 2022). In particular, it has been suggested that psychological flexibility protects against the detrimental effects of the COVID-19 pandemic (e.g., Dawson & Golijani-Moghaddam, 2020; McCracken et al., 2021).
Psychological flexibility is defined as acting in accordance with personal goals and values in the presence of potentially intrusive thoughts and feelings (Hayes et al., 2012). It plays an essential role in determining how people cope with and adapt to changing and often challenging life circumstances (Hayes et al., 2012). Stressful events, such as the distress caused by the COVID-19 pandemic, may increase the likelihood of psychological inflexibility (Hayes et al., 1996). For example, an adolescent may engage in attempts to control painful thoughts and emotions related to the pandemic, which may result in further stress and a range of emotional difficulties (Biglan et al., 2008; Hayes et al., 2006). Based on these considerations, it is reasonable to believe that those high in psychological flexibility may be less affected by the adverse consequences of the COVID-19 pandemic. In other words, psychological flexibility may act as a resilience factor against stressful experiences such as the COVID-19 pandemic (Fonseca et al., 2019; Gloster et al., 2017; McCracken et al., 2021). Dawson and Golijani-Moghaddam (2020) found that psychological flexibility was significantly associated with greater well-being and inversely associated with higher levels of depression, anxiety, and COVID-19-related distress. Similar findings have been reported by other researchers (Crasta et al., 2020; Daks et al., 2020; Kroska et al., 2020; Mallett et al., 2021; McCracken et al., 2021; Pakenham et al., 2020; Peltz et al., 2020; Smith et al., 2020) showing the protective role of psychological flexibility in adapting to new and changing circumstances during the pandemic (Presti et al., 2020). However, little is known about whether a psychological intervention can increase psychological flexibility which in turn can mitigate the detrimental effects of the pandemic on adolescents’ mental health.
Along with psychological flexibility, self-compassion may protect against the adverse effects of the pandemic. Self-compassion is not a psychological flexibility process as such; rather, its components are involved in each of the processes of psychological flexibility (Gillanders et al., 2014; Neff & Tirch, 2013, pp. 78–106). According to Neff and Dahm (2015, pp. 121–137), self-compassion is composed of three interrelated aspects: self-kindness, that is, treating oneself kindly; common humanity, that is, seeing personal struggles as something that all human beings share; and mindfulness, that is, holding one's painful thoughts and feelings mindfully. Self-compassion has been found to be positively associated with well-being, life satisfaction, happiness, and coping skills and negatively correlated with psychopathology in adults (e.g., Breines & Chen, 2012; Neff, 2003; Neff et al., 2005; for a review, see Ferrari et al., 2019) and adolescents (Bluth & Eisenlohr-Moul, 2017; Bluth et al., 2016; Neff et al., 2007; for a meta-analysis, see Marsh et al., 2018). Adolescence is a period of change in life in which self-compassion may be particularly low, as adolescents are prone to critical self-evaluations, comparisons to others, and overidentification with emotions (Neff, 2003). Therefore, self-compassion may be particularly relevant during adolescence (Neff, 2003). Furthermore, self-compassion has been found to act as a protective factor in high-stress situations (Gilbert & Procter, 2006; Hofmann et al., 2011), suggesting that people with higher levels of self-compassion react to adverse events with better emotional regulation (Zeng et al., 2015). Correspondingly, Lau et al. (2020) and Gutiérrez-Hernández et al. (2021) found that during the COVID-19 pandemic, higher levels of self-compassion in adult populations were related to lower levels of anxiety, depression, and stress.
A promising approach in promoting psychological flexibility and self-compassion and offering adaptive skills to deal with adverse events is acceptance and commitment therapy (ACT; Hayes et al., 2012). According to meta-analyses, ACT may improve mental and behavioral problems, quality of life, and psychological flexibility in adolescents (Fang & Ding, 2020; Swain et al., 2015). In addition, before the COVID-19 pandemic, our studies suggest that web-based ACT can help increase adolescents’ academic buoyancy and life satisfaction and reduce stress and depressive symptoms (Lappalainen et al., 2021, Puolakanaho et al., 2019). This is in line with evidence showing that web-based interventions are effective at decreasing symptoms of depression and anxiety among adolescents (Das et al., 2016; Välimäki et al., 2017).
However, adolescents have been found not to be fully engaged in using web-based interventions (Välimäki et al., 2017), which is a critical factor in digital interventions, as active usage, and time investment have been associated with improved treatment outcomes in both adult and adolescent populations (Calear et al., 2013; Enrique et al., 2019; Mattila et al., 2016). For example, Enrique et al. (2019) found that 50% of program completion in an Internet-based intervention for individuals with depressive symptoms was associated with clinically meaningful change.
Given that psychological well-being is highly associated with psychological flexibility (Levin et al., 2014) and self-compassion (Marshall et al., 2015), the aim of the current study was to explore whether an online ACT intervention Youth Compass would have an impact on adolescent distress, psychological flexibility, and self-compassion during the COVID-19 pandemic. More specifically, the online Youth Compass intervention offered to 15–16-year-old adolescents was compared to a no-treatment control group, with the goal of exploring whether the intervention would decrease the adolescents’ symptoms of anxiety and depression and enhance their psychological flexibility and self-compassion skills during the second COVID-19 lockdown. Based on our earlier finding, we hypothesized that adolescents completing at least 30% of the program content would show positive changes, that is, their distress would decrease, and their psychological flexibility and self-compassion would increase significantly more in comparison with those in the control condition.
2. Method
2.1. Recruitment
In the spring of 2020, a total of 348 eighth-grade 14–16-year-old adolescents from lower secondary schools (n = 17) in Central Finland filled in a short screening questionnaire and stated their willingness to participate in the Youth Compass study. Participation in the trial was voluntary, and no pre-defined inclusion or exclusion criteria were applied. Thus, the intervention could be categorized as universal, that is, it was offered to all interested adolescents in the eight grade. We therefore followed the recommendation of World Health Organization (2020), according to which universally delivered interventions should be provided for all (unselected) adolescents (10–19 years), with the goal to promote positive mental health, and prevent and reduce suicidal behavior, mental disorders, aggressive and disruptive behaviors, and substance use.
2.2. Randomization
The 348 adolescents were randomly allocated in the SPSS program by a researcher outside of the study to three conditions: 1) a five-week Youth Compass online intervention with two 45-min video call from a student coach and support from a virtual coach (iACT student coach + virtual coach group, n = 116); 2) a five-week Youth Compass online intervention with one 15-min video call from a student coach and support from a virtual coach (iACT virtual coach group, n = 116); and 3) a no-intervention group (control group, n = 116; Fig. 1 ). The three randomized groups were balanced in terms of the levels of stress and depression, including approximately equal amounts of adolescents above (PSS score ≥14 or DEPS score ≥9) and below the cutoff scores for PSS and DEPS.
Fig. 1.
Participant flow diagram.
2.3. Procedure and participants
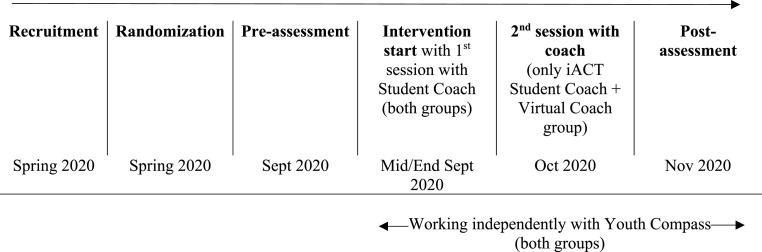
The pre-measurement was administered online in early September 2020 and was filled in by a total of 234 (67%) of the 348 adolescents. An online post-assessment was conducted after seven to eight weeks. A total of 110 (71%) adolescents (of 154) logged into the Youth Compass program mid-September 2020. The mean age of the adolescents (n = 234) was 15.01 years (SD = 0.14, range 14–16 years), a slight majority of whom were female (n = 156, 67%). The demographic characteristics are provided in Table 1 and the timeline for the intervention in Fig. 2 .
Table 1.
Participant Characteristics (inclu. adolescents who filled in the pre-measurement (intent-to-treat analysis, n = 234)).
| Baseline characteristics | All (n = 234) | iACT student coach + virtual coach (n = 79) | iACT virtual coach (n = 75) | Control (n = 80) |
| Age M (SD) | 15.01 (0.15) | 15.04 (0.20) n = 70 | 14.98 (0.12) n = 66 | 15.01 (0.12) n = 67 |
| Gender | ||||
| Female | 156 (66.7%) | 48 (60.8%) | 54 (72%) | 54 (67.5%) |
| Male | 77 (32.9%) | 30 (38%) | 21 (28%) | 26 (32.5%) |
| Other/does not want to tell | 1 (0.4%) | 1 (1.3%) | – | – |
| Mother tonguea | ||||
| Finnish | 226 (97%) | 75 (94.9%) | 73 (97.3%) | 78 (98.7%) |
| Other than Finnish | 7 (3%) | 4 (5.1%) | 2 (2.7%) | 1 (1.3%) |
| Mother's educationb | ||||
| Prim./second. level | 92 (42.7%) | 30 (41%) | 27 (38.5%) | 35 (48%) |
| University level | 124 (57.4%) | 43 (58.8%) | 43 (61.4%) | 38 (52.1%) |
| Father's educationc | ||||
| Prim./second. level | 115 (54.3%) | 42 (59.1%) | 34 (49.2%) | 39 (54.1%) |
| University level | 97 (45.8%) | 29 (40.8%) | 35 (50.7%) | 33 (45.9%) |
| Elevated symptoms of depression (DEPS)d | 90 (39%) | 30 (38.5%) | 31 (42.5%) | 29 (36.3%) |
Others = Living in foster care or approved home.
Missing information, n = 1.
Primary >9 years; secondary 9–12 years; university 12 > years (university, polytechnic, college, etc.); missing information, n = 18.
Missing information, n = 22.
DEPS = The Depression Scale (Salokangas et al., 1995), missing information, n = 3.
Fig. 2.
Timeline for the intervention.
The study procedures were conducted online during the COVID-19 pandemic (the second wave of COVID-19 occurred from September to October 2020), suggesting that the adolescents were presumably burdened not only by occasional quarantine periods, social distancing, and other restrictions but also by the stress associated with pre-transition challenges (exams, etc.).
This study was conducted in compliance with APA ethical standards. Ethical approval was obtained from the Ethical Committee of the University of Jyväskylä on November 20, 2019, registered at www.clinicaltrials.gov in September 2017 and updated in April 2020 (ClinicalTrials.gov Identifier: NCT04340206 ). A signed informed consent form was first obtained from parents, after which the researchers invited the adolescents to consent.
2.4. Intervention and control groups
We investigated two different delivery forms of the Youth Compass intervention: Combined student and virtual coach vs virtual coach only (including 90 min vs. 15 min video call). Our previous studies have shown comparable effects in depressive symptoms regardless of the delivery form of the Youth Compass (e.g., with or without two face-to-face meetings; Lappalainen et al., 2021). Thus, we were open to the possibility that there would be no additional contact-related impact from the 90-min-video call.
The iACT Student Coach + Virtual Coach Group. The adolescents who were randomly assigned to the iACT student coach + virtual coach group received support from a student coach and a built-in virtual coach (chatbot and SMS coaching). Using the doxy. me telemedicine application, the adolescent received the first video call (45 min) from the student coach and was interviewed based on the psychosocial interview template (Strosahl et al., 2012), which included 14 questions adapted for adolescents (e.g., How are you doing in school?). The aim of the interview was to understand the current life situation of each participant. A second videoconferencing meeting (45 min) was arranged two weeks later. The goal of the second meeting was to encourage the adolescent to keep working on the online program. The adolescents were also supported by the virtual coach (see below). Throughout the intervention, the student coach monitored the progress of the participants and sent an SMS message when they showed no progress (Table 2 ).
Table 2.
The youth compass intervention: Modules, module content, and examples of virtual coach messages (SMS).
| Content/message | The Student Coach and Virtual Coach Group | The Virtual Coach Group |
| 1st video conferencing session (doxy.me) | Duration: 45 min Registration for the Youth Compass Introduction Interview with 14 questions |
Duration: 15 min Registration for the Youth Compass Introduction and information on three weekly reminders by the virtual coach No interview |
| Virtual coach SMS message: |
Well, the first module of the Youth Compass is now open! We hope that you enjoy the exercises and chat! |
|
| Introduction | ||
| Getting started: Introduction | ||
| Game: Interrail adventure trip, part I | ||
| Module 1: Direction For Life | ||
| Values: Taking a step toward what brings energy, well-being, and joy. | ||
| Level 1: What Is Important To Me | ||
| Level 2: What Do I Want To Achieve? | ||
| Level 3: What Stops Me? | ||
| Game: Interrail adventure trip, part II | ||
| Virtual coach SMS message: | Hello, I noticed that you have completed some of the exercises in the Youth Compass! Great! | |
| Virtual coach SMS message: |
The second module in the Youth Compass is now open! It's about thoughts this week. I hope you like it!https://nuortenkompassi.fi/programme/nk/e2/minamieli/ |
|
| Module 2: Me And My Mind | ||
| Cognitive defusion: | ||
| Exploring the kinds of automatic thoughts and feelings I have. | ||
| Level 1: Mind Is Like … | ||
| Level 2: Distance to Thoughts | ||
| Level 3: Testing Thoughts | ||
| Game: Interrail adventure trip, part I | ||
| 2nd videoconferencing session (doxy.me) | Duration: 45 min How are you doing? Interview covering values, value-based actions, and cognitive defusion |
No session |
| Virtual coach SMS message (Reminder): | Hi! Just to remind you of the Youth Compass exercises. Listen to some of the recordings a couple of times; they are really good! For example:https://nuortenkompassi.fi/programme/nk/e2/mielikuin/ferrari/ | |
| Virtual coach SMS message (Notification): | The third module is now open in the Youth Compass! So you are now halfway through. There will be some nice exercises this week to help you focus and calm down. | |
| Module 3: Me in the Now | ||
| Present moment and acceptance: Taking a new stance toward my thoughts and feelings | ||
| Level 1: Observe | ||
| Game: Interrail adventure trip, part III | ||
| Level 2. In This Moment: | ||
| Level 3: Testing Out In Practice | ||
| Virtual coach SMS message (Notification): | Hello! I noticed that you have already done many exercises this week! You may want to try them without sound, for example, while you're taking a walk. | |
| Virtual coach SMS message (Notification): |
Hi! The next to last module is now open! If you sometimes feel insecure or are terribly self-critical, we will talk about it this week:https://nuortenkompassi.fi/vara/nk/e4/Good luck in the Youth Compass and otherwise! |
|
| Module 4: Me Myself | ||
| Self-as-a-context and self-compassion: Perceptions of myself and learning to take a different perspective on them. | ||
| Level 1: My Own Story: | ||
| Level 2: Changing the Perspective | ||
| Game: Interrail adventure trip, part IV | ||
| Level 3: Friend To Yourself | ||
| Virtual coach SMS message (Reminder): | I'd like to remind you that there are now super nice exercises in the Youth Compass dealing with not being so harsh on yourself. I really like this one:https://nuortenkompassi.fi/program//kk/e4/tarina/tunnistatarina/ | |
| Virtual coach SMS message (Notification): |
The last module is now open in the Youth Compass! This week is the last:(I hope you liked the program and will also like this final module! |
|
| Module 5: Me And Other PeopleLevel 3: Testing Out In Practice | ||
| ACT-process: Value-based actions, compassion toward others | ||
| Promoting good relationships with my friends and other people | ||
| Level 1: Friend To Yourself and Others | ||
| Level 2: In The World | ||
| Level 3: Challenging Situations | ||
| Game: Interrail adventure trip, part V | ||
| Virtual coach SMS message (Reminder): | Hi, be sure to try the last week's exercises in the Youth Compass. There's a nice one about friends; seehttps://nuortenkompassi.fi/program//kk/e5/ystava/viest/ | |
| A closing SMS message sent by the coach: Thank you for joining the Youth Compass! I wish you all the best! | ||
| Closing feedback | Feedback in writing for the whole program | Feedback in writing for the whole program |
The iACT Virtual Coach Group. The adolescents who were allocated to the iACT virtual coach group received a 15-min video call from the student coach using the doxy. me telemedicine application, in which they received a description of the virtual coaching procedures and an introduction to the built-in virtual coach. Thus, compared to the above described iACT student coach + virtual coach group, the support in this group was mainly technical. The coaches helped the participants log into the program, introduced basic functionalities, and gave an overview on the content. The adolescents were informed that the virtual coach would send them three weekly coaching SMS messages and asked to work independently in the Youth Compass program, supported only by conversations and SMS messages from the virtual coach. The messages from the virtual coach were adapted based on the adolescents’ progress in the program (Table 2).
The No-intervention Control Group. The control group followed the usual curriculum and was not offered additional intervention.
2.5. Coaches
The student coaches were ACT-trained psychology students (n = 27), each responsible for coaching approximately eight randomly chosen adolescents (four from either intervention group). They were final-year bachelor's or master's students with a mean age of 25.04 years (SD = 5.21, range 20–43 years). Except for one male student, the coaches were female (n = 26). The coaches were provided 11 h of training in the ACT methods (7 h of ACT methods and 4 h of the Youth Compass program). They had access to weekly group supervision (2 h) by a licensed psychologist and had to participate in a minimum of two supervision sessions (totaling 4 h). A total of 10 supervision sessions were offered during the intervention period. The purpose of the supervision was to ensure that all coaches followed the procedure as instructed and solve problems arising during the intervention.
2.6. Measures
2.6.1. Outcome measures
Anxiety. The short-form of the Spielberger State-Trait Anxiety Inventory (STAI; Spielberger et al., 1983; Marteau & Bekker, 1992) was used as main outcome measure to measure the adolescents' general anxiety. The inventory is based on a four-point Likert scale ranging from 0 (not at all) to 3 (very much so) and consists of six items. The scores range from 6 to 24, with higher scores indicating greater anxiety. To create scores compatible with the original STAI scores, the STAI-6 scores will be divided by 6 and multiplied by 20 to give a range from 20 to 80. The short-form of the STAI shows acceptable reliability and validity compared to the full-form (Marteau & Bekker, 1992). In this study, Cronbach's alpha was .80 at the pre- and 0.81 at the post-measurement.
Depressive Symptoms. The participants completed the Depression Scale (DEPS; Salokangas et al., 1995; see Kiuru et al., 2012), which consists of 10 items describing depressive symptoms experienced in the last month. The item response categories range from 0 (not at all) to 3 (very much). The total score ranges between 0 and 30, with higher scores indicating more depressive symptoms. A cut-off score of 9 or higher identified 85% of cases of elevated depression symptoms, and the proportion of correctly diagnosed cases of clinical depression was 74% (Salokangas et al., 1995). In the present study, Cronbach's alpha was .93 at the pre- and 0.91 at the post-measurement.
2.6.2. Processes of change measures
Psychological Flexibility. Psychological flexibility was measured by the Comprehensive assessment of Acceptance and Commitment Therapy processes (CompACT), which, in addition to the total score, measures three sub-processes of psychological flexibility: openness to experience (OE; acceptance, defusion), behavioral awareness (BA; present moment, self-as-context), and valued action (VA; values, committed action; Francis et al., 2016). Participants rate 23 items on a seven-point Likert scale ranging from 0 (strongly disagree) to 6 (strongly agree). The total score ranges between 0 and 138, with higher scores indicating greater psychological flexibility. In this study, the scale demonstrated adequate internal consistency (OE, pre, α = 0.77; post, α = 0.79, BA, pre, α = 0.77; post α = .81, and VA, pre, α = 0.84; post, α = 0.88).
Self-Compassion. The Self-Compassion Scale–Short Form (SCS-SF; Raes et al., 2011) is a 12-item questionnaire that includes six subscales, with two items for each subscale: self-kindness versus self-judgment; common humanity versus isolation; and mindfulness versus over-identification. Responses are given on a five-point scale from 1 (almost never) to 5 (almost always). Higher scores indicate higher self-compassion. The SCS-SF is a reliable alternative to the long-form version, when looking at overall self-compassion scores (Raes et al., 2011). In the present study, Cronbach's alpha reliability coefficient was 0.79 at the pre- and 0.83 at the post-measurement.
2.6.3. Adherence
Our results before the pandemic suggested that Youth Compass was helpful for increasing academic buoyancy and life satisfaction as well as reducing stress and depression in adolescents who had completed at least three of the five intervention modules (Lappalainen et al., 2021, Puolakanaho et al., 2019). Thus, in the present study, the adolescents were instructed to complete at least six recommended exercises in each of the five weekly modules; therefore, the minimum intended use (see Sieverink et al., 2017) totaled 30 exercises, which was at least 30% of the program content.
To investigate the impact of the intervention, subgroup analyses were conducted with respect to the adolescents allocated to the two iACT intervention groups who completed the pre-measurements (n = 154), and at least 30% of all the program content (n = 78). Thus, those who did not log in or completed only a part of the first and second module (n = 76, 49%; see Fig. 1) were excluded when completing the per-protocol analyses. Those who filled the adherence criteria (51%) had completed at least one module and half of an additional module or had made the minimum intended use of the program, defined by the completion of six recommended exercises in each weekly module. The recommendation for the minimal intended use was based on our previous study (Lappalainen et al., 2021) in which we investigated the former version of the Youth Compass.
2.6.4. Statistical analyses
Statistical analyses were conducted using SPSS and Mplus (version 8, Muthén & Muthén, 1998 – 2020–2020). Differences between the groups at baseline were investigated using SPSS. Pre-to post-measurement changes from the intervention and control groups were studied using latent change score (SEM) models. These models are equivalent to SPSS repeated measures ANOVA (Gardner, 2006), with the advantage of including all the available data in the analyses (also including participants with some missing values). The intervention results were analyzed using intention-to-treat and per-protocol analyses (Ranganathan et al., 2016). We investigated the effects of the two iACT interventions in comparison with the control group using intention-to-treat analyses, including adolescents who had filled in the pre-measurements (n = 234), and per-protocol analyses, including adolescents who had filled in the pre-measurements, signed into and completed (as recommended) at least 30% of the Youth Compass online program (n = 78 total, in the two iACT intervention groups), and those in the no-intervention control group (n = 80). We examined differences in the changes in psychological flexibility, self-compassion, anxiety, and depression in the three groups. The interaction effects were indicated in the form of Wald-test values (W) and p-values. Effect sizes (ES) regarding changes from the pre-to post-measurement were reported using Cohen's d. An effect size of d = 0.20 was considered small, d = 0.50 moderate, and above d = 0.80 large (Cohen & Williamson, 1988). Further, we investigated whether gender would explain the observed changes from the pre-to post-measurements. Thus, pre-to post-measurement changes from the intervention and control groups were studied using latent change score (SEM) models and testing whether the changes differed depending on gender. The differences in the background variables between the drop-outs and non-drop-outs were analyzed using t- and chi-square tests.
3. Results
3.1. Adherence
A total of 348 adolescents were randomly assigned to the iACT student coach + virtual coach group (n = 116), the iACT virtual coach group (n = 116), and the no-intervention control condition (n = 116; Fig. 1). Of these, 234 (67%) filled in the pre-measurement (iACT student coach + virtual coach group, n = 79; iACT virtual coach group, n = 75; control, n = 80). As 114 (33%) participants withdrew from the study between the randomization (n = 348) and pre-measurement (n = 243), chi-square tests were conducted to compare those who participated in the pre-measurement and those who withdrew from the study before completing the pre-measurement. We found a gender difference between the groups. Significantly more females participated in the pre-measurement (80.7%; n = 159) compared to males (53.4%, n = 79; chi-square 30.284, df = 3, p < 0.01). Further, 110 of the 154 adolescents (71%) from the two intervention groups logged into the Youth Compass online program, among whom 88 (80%) fulfilled the adherence criteria and completed at least 30% of the Youth Compass online program. A closer examination of user activity during the intervention period revealed that most of the adolescents (n = 64) completed 60–100% of the Youth Compass program. However, we detected that 78 of the 88 adolescents who fulfilled the adherence criteria had completed the pre-measurements, and therefore, the iACT student coach + virtual coach group ended up with 44 adolescents; the iACT virtual coach group had 34 adolescents; and the control group comprised 80 adolescents (totaling n = 158). Post-measurement data were available from 137 adolescents in total, indicating that close to 60% (58.5%) of those who participated in the pre-measurement also completed the post-measurement (Fig. 1). The intervention group completing at least 30% of the program (n = 78) included fewer boys than in the control group (chi-square 6.484, df = 2, p = 0.039). The adolescents gave no reasons for dropping out of the study.
3.2. Intervention effects
An analysis of the adolescent sample, that is, those who had filled in the pre-measurements (intent-to-treat analysis, n = 234) revealed that neither of the two intervention groups (iACT student coach + virtual coach; iACT virtual coach) changed significantly differently compared to the control group with regard to psychological flexibility (CompACT total; W = 1.731, df = 2, p = 0.421), self-compassion (SCS-SF; W = 2.998, df = 2, p = 0.112), anxiety (STAI; W = 3.861, df = 2, p = 0.073), and depressive symptoms (DEPS; W = 2.052, df = 2, p = 0.179). In addition, the two intervention groups did not change significantly differently in terms of the abovementioned outcomes.
We then combined the two intervention groups and examined whether there were any changes among adolescents who had logged into the Youth Compass program and met the adherence criteria of completing at least 30% of the program (per-protocol analysis, intervention group, n = 78; control group, n = 80; total n = 158). We found that the iACT group showed a different change compared to the control group regarding to valued action (W = 4.19, df = 1, p = 0.020), self-compassion (SCS-SF; W = 3.55, df = 1, p = 0.030), and anxiety (STAI; W = 3.00, df = 1, p = 0.042, Table 3 ). Thus, a slight increase in the iACT group was found both in terms of valued action and self-compassion (within ES, VA: d = 0.08; SCS: d = 0.12), but they decreased in the control condition (within ES, VA: d = 0.17; SCS: d = 0.05). Anxiety showed a slight increase in the iACT group (within ES, d = 0.05); however, the symptoms of anxiety in the control group increased more significantly (within ES, d = 0.34). There was a similar trend in depression, but the interaction effect was not significant. The corrected between-group ES of all variables were very small or small (d = 0.03–0.30; Table 3).
Table 3.
Changes in psychological flexibility, self-compassion, anxiety and depression in the combined iACT intervention group (n = 78), and the Control group (n = 80) among the adolescents who completed at least 30% of the Youth Compass program.
| Pre |
Post |
|||||
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | W (df = 1) | p | db | dw | |
| CompACT Total | 2.08 | 0.072 | −0.19 | |||
| iACT Intervention | 82.35 (18.13) | 82.72 (21.41) | −0.02 | |||
| Control | 83.35 (17.73) | 80.40 (20.18) | −0.16 | |||
| CompACT VA | 4.19 | 0.020 | −0.26 | |||
| iACT Intervention | 33.42 (7.77) | 34.09 (7.94) | −0.08 | |||
| Control | 33.09 (7.40) | 31.78 (7.76) | 0.17 | |||
| CompACT BA | 0.05 | 0.415 | −0.03 | |||
| iACT Intervention | 17.96 (6.11) | 17.47 (6.18) | 0.08 | |||
| Control | 19.04 (6.38) | 18.37 (6.42) | 0.11 | |||
| CompACT OE | 0.63 | 0.213 | −0.15 | |||
| iACT Intervention | 30.96 (8.06) | 31.30 (10.90) | −0.04 | |||
| Control | 31.19 (8.03) | 30.34 (10.18) | 0.09 | |||
| SelfCompassion (SCS) | 3.55 | 0.030 | −0.17 | |||
| iACT Intervention | 38.42 (7.75) | 39.35 (7.74) | −0.12 | |||
| Control | 39.53 (8.14) | 39.11 (7.66) | 0.05 | |||
| Anxiety | 3.00 | 0.042 | 0.30 | |||
| iACT Intervention | 12.07 (3.55) | 12.26 (3.50) | −0.05 | |||
| Control | 11.77 (3.71) | 13.04 (3.85) | −0.34 | |||
| Depression | 0.57 | 0.224 | 0.10 | |||
| iACT Intervention | 7.73 (6.69) | 7.79 (6.06) | −0.01 | |||
| Control | 7.02 (6.07) | 7.71 (6.92) | −0.11 |
db = between-group effect size dw = within-group effect size.
CompACT Total = Comprehensive assessment of acceptance and commitment therapy processes.
CompACT VA = CompACT Valued action.
CompACT BA = CompACT Behavioral Awareness.
CompACT OE = Comp ACT Openess to Experiences.
Self-Compassion = The Self-Compassion Scale–Short form (SCS-SF).
Since the intervention group that completed at least 30% of the program (n = 78) included fewer boys than in the control group, we performed further analyses and investigated whether boys and girls changed differently during the intervention. The analyses indicated that adolescent boys and girls showed similar changes regarding the measured variables from the pre-to post-measurement.
We investigated more closely those adolescents who had provided complete data in the pre- and post-measurements as well as their user activity (n = 71). Interestingly, all those who did not fulfill our adherence criteria (at least 30% usage) belonged to the virtual coach group (chi-square 7.550, df = 1, p = 0.006). Further, we investigated whether those who had received a greater proportion of the intervention (80–100% usage, n = 35) would show larger changes (effect sizes) in the process variables compared to those with a lower user percentage (0–79%, n = 36, and 30–79%, n = 29). The cutoff was the median value (79; see Table 4 ). Compared to the control group, the high-usage group (80–100%) showed larger changes in total CompACT and openness to experiences than the lower-usage group (0–79% and 30–79%). In value-based action, both the low- and high-usage groups showed larger changes compared to the control group. A comparison between the high- and lower-usage groups revealed that the high-usage group showed larger changes in total CompACT and openness to experiences. Thus, those who received a greater proportion of the intervention showed larger changes, especially in openness to experiences. Further, there was a dose-response between the level of use of the program and the magnitude of changes in symptoms of depression and anxiety. Higher levels of exposure to the program were associated with larger positive changes in symptoms. Change from pre to post in anxiety: User category 0–29% (n = 7), pre-post change = −1.29 (increase in symptoms); user category 30–79% (n = 29), pre-post change = −0.83 (increase in symptoms); user category 80–100% (n = 35), pre-post change = 0.34 (decrease in symptoms). Change from pre to post in depression: User category 0–29% (n = 7), pre-post change = −1.14 (increase in symptoms); user category 30–79% (n = 29), pre-post change = −0.48 (increase in symptoms); user category 80–100% (n = 35), pre-post change = 0.00 (no change).
Table 4.
Between group effect sizes of user activity. Left: Comparison between the control group (n = 80) and the intervention group divided into the low usage groups (0–79% and 30–79%), and the high usage group (80–100%). Right: Comparisons between high usage (80–100%) and the low usage groups (0–79% and 30–79%).
| Control group (n = 80) vs. Intervention use categories |
High usage group (80–100%, n = 35) vs. lower usage categories |
||||
|---|---|---|---|---|---|
| 0–79% (n = 36) | 30–79% (n = 29) | 80–100% (n = 35) | 0–79% (n = 36) | 30–79% (n = 29) | |
| CompACT Total | 0.06 | 0.05 | 0.28 | 0.24 | 0.25 |
| CompACT VA | 0.35 | 0.32 | 0.21 | 0.12 | −0.09 |
| CompACT BA | 0.04 | −0.08 | 0.07 | 0.12 | 0.15 |
| CompACT OE | −0.20a | −0.17a | 0.38 | 0.62 | 0.58 |
| SelfComp (SCS) | 0.14 | 0.17 | 0.17 | 0.04 | 0.02 |
CompACT Total = Comprehensive assessment of acceptance and commitment therapy processes.
CompACT VA = CompACT Valued action.
CompACT BA = CompACT Behavioral Awareness.
CompACT OE = Comp ACT Openess to Experiences.
Self-Compassion = The Self-Compassion Scale–Short form (SCS-SF).
= change larger in the control group.
In addition, we investigated whether levels of psychological flexibility (CompACT Total) and self-compassion (SCS) predicted changes in depression and anxiety. The analyses suggested that the level of psychological flexibility but not the level of self-compassion predicted changes in symptoms of depression (F (1,69) = 5.911, p = 0.18, Adjusted R Square = 0.066). Lower levels of psychological flexibility at pre-measurement were associated with larger changes in depression symptoms (r = −0.28, p = 0.018, n = 71). Thus, those adolescents who had lower levels of psychological flexibility benefitted more of the intervention in respect of depression. Neither levels of psychological flexibility nor self-compassion predicted the changes in anxiety.
4. Discussion
The aim of this study was to examine the effects of an ACT-based online intervention Youth Compass on symptoms of anxiety and depression, psychological flexibility, and self-compassion during the COVID-19 pandemic among 15-16-year-olds. No significantly different changes between the two intervention groups compared with the no-treatment control group were detected in the randomized sample. As our earlier studies (Lappalainen et al., 2021, Puolakanaho et al., 2019) suggested, a more intense use of or engagement with the intervention was needed to obtain beneficial effects. Our hypothesis was that meeting the minimum adherence criteria (i.e., completing 30% of the program) would be associated with significant decreases in psychological symptoms and increases in psychological flexibility and self-compassion. This hypothesis was partially supported. When investigating the adolescents who met the adherence criteria, we found that valued action remained at the same level in the iACT intervention group, while the no-intervention group recorded a reduction in value-based action. Also, there was a slight increase in self-compassion in the iACT group and a slight decrease among the adolescents in the no-intervention group, with the latter also reporting an increase in anxiety and the former reporting significantly smaller increase in anxiety. Further, those who received a greater proportion of the intervention showed larger changes, especially in openness to experiences. There was also a dose-response between the level of use of the program and the magnitude of changes in symptoms of depression and anxiety. Higher levels of exposure to the program were associated with larger positive changes in symptoms.
Based on these results and consistent with recent studies on psychological flexibility in the context of COVID-19 (e.g., Crasta et al., 2020; Daks et al., 2020; Dawson & Golijani-Moghaddam, 2020; Xu et al., 2021), we propose that the psychological flexibility and self-compassion skills that the adolescents learned in the Youth Compass intervention may have protected against psychological distress caused by COVID-19. This was confirmed by the observation that anxiety increased only slightly in the iACT group, showing a significant, albeit small, effect on symptoms of anxiety in comparison to the control condition. Because of COVID-19 and the associated threats and fears regarding the future, the adolescents may have experienced more anxiety, which is in line with Ravens-Sieberer et al. (2021), who found higher levels of generalized anxiety in children and adolescents before versus during the pandemic but no significant increase in the prevalence of depressive symptoms. Indeed, those who engaged in the Youth Compass showed only a minor increase in anxiety compared to a larger increase in the control group. It is noteworthy that the data collection was carried out during the second wave of COVID-19. This potentially explains the increase in symptoms of anxiety among the adolescents. Fear and anxiety are natural reactions under stressful circumstances such as the COVID-19. Anxiety-induced rigidity may excessively narrow behavioral repertoires and restrict engagement in meaningful activities (Presti et al., 2020), whereas psychological flexibility skills may lessen entanglement with worry and anxious thoughts and, despite anxiety, lead to engagement in valued actions. Our results support this view and are consistent with those of Smith et al. (2020), who suggested that high levels of psychological flexibility and tolerance of uncertainty had a protective effect on participants’ anxiety during the pandemic (see also Pakenham et al., 2020).
Studies have shown that increasing young people's engagement in meaningful activities, that is, living consistently with their personal values, may protect against the effects of various stressors on psychosocial functioning and help them improve their well-being (Grégoire et al., 2021; Miller & Orsillo, 2020; Murrell & Kapadia, 2011). After all, the ultimate goal of ACT is behavior change, and other ACT processes are subordinated to helping individuals live according to their chosen values (Hayes et al., 1999; Zhang et al., 2018). In this sense, it is an encouraging finding that the ACT-based intervention positively impacted the adolescents' engagement in value-based actions during the pandemic, that is, in the face of external obstacles. However, partaking in meaningful actions during a lockdown situation may have been more challenging for adolescents than in normal circumstances as their social contacts were sparse and often limited to their immediate family and, occasionally, online contact with teachers and schoolmates. Nevertheless, more information about whether the adolescents in fact conducted meaningful actions and how would be valuable. Some studies conducted during the pandemic (e.g., Ellis et al., 2020; Gadermann et al., 2022; McArthur et al., 2021) found that adolescents who reported spending more time with family also reported less loneliness and fewer mental health symptoms; therefore, it would have been valuable to ascertain whether an increase in valued actions in our adolescent sample was associated with increased interaction and connectedness with family or peers or whether meaningful actions were related to increased exercise or more time for activities that they had not been able to pursue earlier, which were elsewhere reported by adolescents as positive impacts of the pandemic (Kerekes et al., 2021). Momentary data collection methods would have better captured the adolescents' actions on a daily basis and assess their clarity regarding their values, how committed they were to these values, and how consistently they put these values into action on a daily basis. Therefore, there is a need for future studies to track daily behaviors using methodologies such as ecological momentary assessments (EMAs) in order to examine psychological flexibility processes and assess adolescents' experiences when they are engaged in their daily routines.
The results indicate that among the adolescents who completed at least 30% of the Youth Compass program, the intervention had a positive impact on their self-compassion skills compared to those in the no-intervention condition. This suggests that self-compassion may be an important protective factor in alleviating the adverse impacts of the pandemic (see Jiménez et al., 2020; Lau et al., 2020). Self-compassion fosters emotional resilience, that is, psychological flexibility (Jiménez et al., 2020), which may increase the ability to respond more adequately to stressful situations, thereby helping adolescents deal effectively with the challenges posed by global emergencies such as COVID-19. Congruent with previous studies that have shown that brief compassion training via mobile applications and webpages can enhance well-being and self-compassion (Donovan et al., 2016; Eriksson et al., 2018), the findings of the present study suggest that an ACT-based program such as Youth Compass may offer promise in teaching adolescents ways to be kind to themselves in challenging situations, enabling them to see the global pandemic as something that they experience with other people around the world.
It should be noted that this was a universal study that included all interested adolescents. Therefore, some adolescents' psychological flexibility and self-compassion may have been on a relatively high level prior to the intervention. Another potential reason for not obtaining larger effects or significant results on the other variables of psychological flexibility and symptoms may be that the intervention period was relatively short, and engagement in the online program relied mainly on the adolescents' own activity. We used a rough 30% adherence measure, and we do not know de facto how engaged the adolescents really were. We can only speculate as to why the changes in the iACT group, which received more support (2 × 45 min), were not significantly larger than in the virtual coach group (15 min). Nevertheless, it is an important finding that more extensive support in online interventions does not automatically lead to better results, although brief contact with a coach was associated with fewer adolescents reporting low program usage. A short video call from a contact person combined with a virtual coach that keeps the adolescent engaged may be sufficient to produce a beneficial impact on well-being. However, follow-up studies are needed to ensure that the results will be maintained and will have a long-term protective effect on adolescents’ overall well-being.
Interestingly, openness to experiences increased for the adolescents who received a greater proportion of the intervention. This could be explained by the fact that modules 3 and 4 included materials related to observing skills, present moment awareness, acceptance, self-as-context, and self-compassion. Based on these findings, it is recommended that adolescents complete at least 80% of the intervention since the level of use is related to the benefits received from the program.
Regarding the drop-out rate in the study, the context of the COVID-19 pandemic meant that we were obliged to administer all the assessments online instead of the planned in-person paper-and-pencil assessment in schools. In addition, engaging in an online intervention mostly alone, with only a 15-min or 2 × 45-min video calls from a coach may not have been a compelling option for adolescents who occasionally attended school virtually and spent a great deal of time online. However, our drop-out rates were in line with those of other studies investigating digital mental health interventions. Drop-out rates above 20% are fairly common, as reported in a meta-analytic review by Garrido et al. (2019). In our sample, 30% of the adolescents did not log into the program, and among those who logged in, 80% fulfilled our adherence criteria. For example, a meta-analytic review suggested an attrition rate of 24% for a short-term follow-up in smartphone-delivered interventions for mental health problems (Linardon & Fuller-Tyszkiewicz, 2020).
The following limitations must be observed. First, withdrawals and drop-out rates of the magnitude experienced in the current study may threaten the validity and generalizability of our results. Over 80% of the randomized adolescents who participated in the pre-measurement were female, including most of the completers of the study (72%; intent-to-treat). Therefore, our results may not generalize to male adolescents. Second, it should be noted that the adolescents in the current study came from families in which parents were mostly well educated, with around half of the parents having undertaken university-level education. It is important to consider that our findings may not generalize to adolescents from more disadvantaged backgrounds. Future research should be conducted, for example, with a sample of adolescents belonging to less-educated families of a lower socioeconomic status. Finally, the use of self-report questionnaires should be considered a limitation. It is possible that some adolescents may not have been able to answer realistically, particularly in the CompACT measure of psychological flexibility.
Despite these limitations, the present study contributes to the body of knowledge in the field of interventions for adolescent populations. As noted earlier, only a few studies have applied ACT to adolescents during the COVID-19 lockdown. COVID-19 propelled important changes to mental health delivery, suggesting that brief and low-intensity interventions should become a priority in research and clinical practice (Gruber et al., 2021). According to the World Health Organization (2020), universally delivered psychosocial interventions should be provided to all adolescents and implemented in diverse settings or through digital platforms. In terms of delivery, schools are in the unique position of being able to reach young people and provide them with early interventions to promote their emotional health; thus, their role should be strengthened (see also Gee et al., 2021). The online-delivered Youth Compass program enabled us to reach the adolescents and offer them support during the pandemic when traditionally delivered support was unavailable. ACT approaches such as the Youth Compass arguably enable adolescents to acquire important psychological flexibility and self-compassion skills and support them in engaging with meaningful actions and acquiring a compassionate stance toward themselves under stressful circumstances. Building these skills may help adolescents develop strategies to cope with their struggles in challenging times, which they will be able to use throughout their lives.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The study was funded with grants from the XXX (No. 324638) and the Center for Research for Learning and Teaching (MultiLeTe2).
Footnotes
The study reported in this manuscript is part of an intervention study called the Youth Compass plus, which was funded with grants from the Academy of Finland (No. 324638) and the Center for Research for Learning and Teaching (MultiLeTe2). The research plan of the Youth Compass plus was evaluated and approved by the ethics committee of the University of Jyväskylä (Nov. 20, 2019), and the Youth Compass plus intervention was registered at ClinicalTrials.gov.
Data is available upon reasonable request.
References
- Biglan A., Hayes S.C., Pistorello J. Acceptance and commitment: Implications for prevention science. Prevention Science: The Official Journal of the Society for Prevention Research. 2008;9(3):139–152. doi: 10.1007/s11121-008-0099-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluth K., Eisenlohr-Moul T.A. Response to a mindful self-compassion intervention in teens: A within-person association of mindfulness, self-compassion, and emotional well-being outcomes. Journal of Adolescence. 2017;57:108–118. doi: 10.1016/j.adolescence.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluth K., Gaylord S.A., Campo R.A., Mullarkey M.C., Hobbs L. Making friends with yourself: A mixed methods pilot study of a mindful self-compassion program for adolescents. Mindfulness. 2016;7(2):479–492. doi: 10.1007/s12671-015-0476-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branje S., Morris A.S. The impact of the COVID-19 pandemic on adolescent emotional, social, and academic adjustment. Journal of Research on Adolescence : The Official Journal of the Society for Research on Adolescence. 2021;31(3):486–499. doi: 10.1111/jora.12668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breines J.G., Chen S. Self-compassion increases self-improvement motivation. Personality and Social Psychology Bulletin. 2012;38(9):1133–1143. doi: 10.1177/0146167212445599. [DOI] [PubMed] [Google Scholar]
- Calear A.L., Christensen H., Mackinnon A., Griffiths K.M. Adherence to the MoodGYM program: Outcomes and predictors for an adolescent school-based population. Journal of Affective Disorders. 2013;147(1–3):338–344. doi: 10.1016/j.jad.2012.11.036. [DOI] [PubMed] [Google Scholar]
- Cohen S., Williamson G. In: The social psychology of health: Claremont Symposium on applied social psychology. Spacapam S., Oskamp S., editors. 1988. Perceived stress in a probability sample of the US. [Google Scholar]
- Crasta D., Daks J.S., Rogge R.D. Modeling suicide risk among parents during the COVID-19 pandemic: Psychological inflexibility exacerbates the impact of COVID-19 stressors on interpersonal risk factors for suicide. Journal of Contextual Behavioral Science. 2020;18:117–127. doi: 10.1016/j.jcbs.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daks J.S., Peltz J.S., Rogge R.D. Psychological flexibility and inflexibility as sources of resiliency and risk during a pandemic: Modeling the cascade of COVID-19 stress on family systems with a contextual behavioral science lens. Journal of Contextual Behavioral Science. 2020;18:16–27. doi: 10.1016/j.jcbs.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das J.K., Salam R.A., Lassi Z.S., Khan M.N., Mahmood W., Patel V., Bhutta Z.A. Interventions for adolescent mental health: An overview of systematic reviews. The journal of adolescent health. Official Publication of the Society for Adolescent Medicine. 2016;59(4S):S49–S60. doi: 10.1016/j.jadohealth.2016.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson D.L., Golijani-Moghaddam N. COVID-19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. Journal of Contextual Behavioral Science. 2020;17:126–134. doi: 10.1016/j.jcbs.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan E., Rodgers R.F., Cousineau T.M., McGowan K.M., Luk S., Yates K., Franko D.L. Brief report: Feasibility of a mindfulness and self-compassion based mobile intervention for adolescents. Journal of Adolescents. 2016;53:217–221. doi: 10.1016/j.adolescence.2016.09.009. [DOI] [PubMed] [Google Scholar]
- Ellis W.E., Dumas T.M., Forbes L.M. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canadian Journal of Behavioral Science. 2020;52:177–187. doi: 10.1037/cbs0000215. [DOI] [Google Scholar]
- Enrique A., Palacios J.E., Ryan H., Richards D. Exploring the relationship between usage and outcomes of an Internet-based intervention for individuals with depressive symptoms: Secondary analysis of data from a randomized controlled trial. Journal of Medical Internet Research. 2019;21(8) doi: 10.2196/12775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eriksson T., Germundsjö L., Åström E., Rönnlund M. Mindful self-compassion training reduces stress and burnout symptoms among practicing psychologists: A randomized controlled trial of a brief web-based intervention. Frontiers in Psychology. 2018;9:2340–2349. doi: 10.3389/fpsyg.2018.02340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang S., Ding D. A meta-analysis of the efficacy of acceptance and commitment therapy for children. Journal of Contextual Behavioral Science. 2020;15:225–234. [Google Scholar]
- Ferrari M., Hunt C., Harrysunker A., Abbott M.J., Beath A.P., Einstein D.A. Self-compassion interventions and psychosocial outcomes: A meta-analysis of RCTs. Mindfulness. 2019;10:1455–1473. doi: 10.1007/s12671-019-01134-6. [DOI] [Google Scholar]
- Fonseca S., Trindade I.A., Mendes A.L., Ferreira C. The buffer role of psychological flexibility against the impact of major life events on depression symptoms. Clinical Psychologist. 2019;24(1) doi: 10.1111/cp.12194. [DOI] [Google Scholar]
- Francis A.W.L., Dawson D.L., Golijani-Moghaddam N. The development and validation of the comprehensive assessment of acceptance and commitment therapy processes (CompACT) Journal of Contextual Behavioral Science. 2016;5(3):134–145. doi: 10.1016/j.jcbs.2016.05.003. [DOI] [Google Scholar]
- Gadermann A., Thomson K., Gill R., Schonert-Reichl K.A., Gagné Petteni M., Guhn M.…Oberle E. Early Adolescents’ Experiences During the COVID-19 Pandemic and Changes in Their Well-Being. Frontiers in public health. 2022;10:823303. doi: 10.3389/fpubh.2022.823303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner R.C. Hierarchical Linear Modeling: A Primer1 (People within Groups) 2006 https://publish.uwo.ca/∼gardner/DataAnalysisDotCalm/Manuscripts/daHLMREMLpeoplewithingroupsNEWSPAIN.pdf Retrieved from. [Google Scholar]
- Garrido, et al. 2019. What works and what doesn't work? A systematic review of digital mental health interventions for depression and anxiety in young people. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee B., Wilson J., Clarke T., Farthing S., Carroll B., Jackson C., King K., Murdoch J., Fonagy P., Notley C. Review: Delivering mental health support within schools and colleges – a thematic synthesis of barriers and facilitators to implementation of indicated psychological interventions for adolescents. Child and Adolescent Mental Health. 2021;26(1):34–46. doi: 10.1111/camh.12381. [DOI] [PubMed] [Google Scholar]
- Gilbert P., Procter S. Compassionate mind training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy. 2006;13:353–379. [Google Scholar]
- Gillanders D.T., Bolderston H., Bond F.W., Dempster M., Flaxman P.E., Campbell L., Kerr S., Tansey L., Noel P., Ferenbach C., Masley S., Roach L., Lloyd J., May L., Clarke S., Remington B. The development and initial validation of the cognitive fusion questionnaire. Behavior Therapy. 2014;45(1):83–101. doi: 10.1016/j.beth.2013.09.001. [DOI] [PubMed] [Google Scholar]
- Gloster A.T., Meyer A.H., Lieb R. Psychological flexibility as a malleable public health target: Evidence from a representative sample. Journal of Contextual Behavioral Science. 2017;6(2):166–171. doi: 10.1016/j.jcbs.2017.02.003. [DOI] [Google Scholar]
- Grégoire S., Doucerain M., Morin L., Finkelstein-Fox L. The relationship between value-based actions, psychological distress and well-being: A multilevel diary study. Journal of Contextual Behavioral Science. 2021;20:79–88. doi: 10.1016/j.jcbs.2021.03.006. [DOI] [Google Scholar]
- Gruber J., Prinstein M.J., Clark L.A., Rottenberg J., Abramowitz J.S., Albano A.M.…Weinstock L.M. Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. American Psychologist. 2021;76(3):409–426. doi: 10.1037/amp0000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutiérrez-Hernández M.E., Fanjul L.F., Díaz-Megolla A., Reyes-Hurtado P., Herrera-Rodríguez J.F., Enjuto-Castellanos M., Peñate W. COVID-19 lockdown and mental health in a sample population in Spain: The role of self-compassion. International Journal of Environmental Research and Public Health. 2021;18(4):2103. doi: 10.3390/ijerph18042103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafstad G.S., Sætren S.S., Wentzel-Larsen T., Augusti E.-M. Longitudinal change in adolescent mental health during the COVID-19 outbreak – A prospective population-based study of teenagers in Norway (SSRN Scholarly Paper ID 3727297); 2020. Social science research network. [DOI] [Google Scholar]
- Hawke L.D., Barbic S.P., Voineskos A., Szatmari P., Cleverley K., Hayes E., Relihan J., Daley M., Courtney D., Cheung A., Darnay K., Henderson J.L. Impacts of COVID-19 on youth mental health, substance use, and well-being: A rapid survey of clinical and community samples: Répercussions de la COVID-19 sur la santé mentale, l’utilisation de substances et le bien-être des adolescents: Un sondage rapide 19 d’échantillons cliniques et communautaires. Canadian Journal of Psychiatry. 2020;65(10):701–709. doi: 10.1177/0706743720940562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes S.C., Luoma J.B., Bond F.W., Masuda A., Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hayes S.C., Strosahl K.D., Wilson K.G. Guilford Press; 1999. Acceptance and commitment therapy: An experiential approach to behavior change. [Google Scholar]
- Hayes S.C., Strosahl K.D., Wilson K.G. 2nd ed. Guilford Press; 2012. Acceptance and commitment therapy: The process and practice of mindful change. [Google Scholar]
- Hayes S.C., Wilson K.G., Gifford E.V., Follette V.M., Strosahl K. Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology. 1996;64(6):1152–1168. doi: 10.1037/0022–006X.64.6.1152. [DOI] [PubMed] [Google Scholar]
- Hofmann S.G., Grossman P., Hinton D.E. Loving-kindness and compassion meditation: Potential for psychological interventions. Clinical Psychology Review. 2011;31:1126–1132. doi: 10.1016/j.cpr.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiménez Ó., Sánchez-Sánchez L.C., García-Montes J.M. Psychological impact of COVID-19 confinement and its relationship with meditation. International Journal of Environmental Research and Public Health. 2020;17:6642. doi: 10.3390/ijerph17186642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerekes N., Bador K., Sfendla A., Belaatar M., El Mzadi A., Jovic V., et al. Changes in adolescents' psychosocial functioning and well-being as a consequence of long-term covid-19 restrictions. International Journal of Environmental Research and Public Health. 2021;18:8755. doi: 10.3390/ijerph18168755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiuru N., Burk W.J., Laursen B., Nurmi J.E., Salmela-Aro K. Is depression contagious? A test of alternative peer socialization mechanisms of depressive symptoms in adolescent peer networks. Journal of Adolescent Health. 2012;50(3):250–255. doi: 10.1016/j.jadohealth.2011.06.013. [DOI] [PubMed] [Google Scholar]
- Kroska E.B., Roche A.I., Adamowicz J.L., Stegall M.S. Psychological flexibility in the context of COVID-19 adversity: Associations with distress. Journal of Contextual Behavioral Science. 2020;18:28–33. doi: 10.1016/j.jcbs.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lappalainen R., Lappalainen P., Puolakanaho A., Hirvonen R., Eklund K., Ahonen T., Muotka J., Kiuru N. The youth compass – the effectiveness of an online acceptance and commitment therapy program to promote adolescent mental health: A randomized controlled trial. Journal of Contextual Behavioral Science. 2021;20:1–12. doi: 10.1016/j.jcbs.2021.01.007. [DOI] [Google Scholar]
- Lau B.H.-P., Chan C.L.W., Siu-Man N. Self-compassion buffers the adverse mental health impacts of COVID-19-related threats: Results from a cross-sectional survey at the first peak of Hong Kong's outbreak. Frontiers in Psychiatry. 2020;11:1203. doi: 10.3389/fpsyt.2020.585270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin M.E., MacLane C., Daflos S., Seeley J., Hayes S.C., Biglan A., Pistorello J. Examining psychological inflexibility as a transdiagnostic process across psychological disorders. Journal of Contextual Behavioral Science. 2014;3(3):155–163. doi: 10.1016/j.jcbs.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linardon J., Fuller-Tyszkiewicz M. Attrition and adherence in smartphone-delivered interventions for mental health problems: A systematic and meta-analytic review. Journal of Consulting and Clinical Psychology. 2020;88(1):1–13. doi: 10.1037/ccp0000459. [DOI] [PubMed] [Google Scholar]
- Mallett R., Coyle C., Kuang Y., Gillanders D.T. Behind the masks: A cross-sectional study on intolerance of uncertainty, perceived vulnerability to disease and psychological flexibility in relation to state anxiety and wellbeing during the COVID-19 pandemic. Journal of Contextual Behavioral Science. 2021;22:52–62. doi: 10.1016/j.jcbs.2021.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall S.L., Parker P.D., Ciarrochi J., Sahdra B., Jackson C.J., Heaven P.C.L. Self-compassion protects against the negative effects of low self-esteem: A longitudinal study in a large adolescent sample. Personality and Individual Differences. 2015;74:116–121. doi: 10.1016/j.paid.2014.09.013. [DOI] [Google Scholar]
- Marsh I.C., Chan S.W.Y., MacBeth A. Self-compassion and psychological distress in adolescents—a meta-analysis. Mindfulness. 2018;9:1011–1027. doi: 10.1007/s12671-017-0850-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marteau T.M., Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI) British Journal of Clinical Psychology. 1992;31(3):301–306. doi: 10.1111/j.2044-8260.1992.tb00997.x. [DOI] [PubMed] [Google Scholar]
- Mastrotheodoros S. 2021. The effects of COVID-19 on young people's mental health and psychological well-being. Youth partnership between the European Commission and the Council of Europe in the field of youth.https://pjp-eu.coe.int/documents/42128013/72351197/Effects-COVID-Youth-Mental-Health-Psychological-Well-Being.pdf/b2bc0c32-9fd5-0816-bce5-da9289cfca8c [Google Scholar]
- Mattila E., Lappalainen R., Välkkynen P., Sairanen E., Lappalainen P., Karhunen L., Peuhkuri K., Korpela R., Kolehmainen M., Ermes M. Usage and dose response of a mobile acceptance and commitment therapy app: Secondary analysis of the intervention arm of a randomized controlled trial. JMIR Mhealth Uhealth. 2016;4(3):e90. doi: 10.2196/mhealth.5241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArthur B.A., Racine N., McDonald S., Tough S., Madigan S. Child and family factors associated with child mental health and well-being during COVID-19. European Child & Adolescent Psychiatry. 2021:1–11. doi: 10.1007/s00787-021-01849-9. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken L.M., Badinlou F., Buhrman M., Brocki K.C. The role of psychological flexibility in the context of COVID-19: Associations with depression, anxiety, and insomnia. Journal of Contextual Behavioral Science. 2021;19:28–35. doi: 10.1016/j.jcbs.2020.11.003. [DOI] [Google Scholar]
- Miller A.N., Orsillo S.M. Values, acceptance, and belonginess in graduate school: Perspectives from underrepresented minority students. Journal of Contextual Behavioral Science. 2020;15:197–206. doi: 10.1016/j.jcbs.2020.01.002. [DOI] [Google Scholar]
- Murrell A.R., Kapadia V. Brief report on experiential avoidance and valuing in at-risk adolescents. Behavioral Development Bulletin. 2011;17(1):38–42. doi: 10.1037/h0100600. [DOI] [Google Scholar]
- Muthén L., Muthén B.O. 1998–2020. Mplus version 8 & Mplus users' guide.http://www.statmodel.com [Google Scholar]
- Neff K.D. The development and validation of a scale to measure self-compassion. Self and Identity. 2003;2(3):223–250. doi: 10.1080/15298860309027. [DOI] [Google Scholar]
- Neff K.D., Dahm K.A. In: Ostafin B.D., Robinson M.D., Meier B.P., editors. Handbook of mindfulness and self-regulation; 2015. Self-compassion: What it is, what it does, and how it relates to mindfulness. Springer Science + Business Media. [DOI] [Google Scholar]
- Neff K.D., Hsieh Y.-P., Dejitterat K. Self-compassion, achievement goals, and coping with academic failure. Self and Identity. 2005;4(3):263–287. doi: 10.1080/13576500444000317. [DOI] [Google Scholar]
- Neff K.D., Kirkpatrick K.L., Rude S.S. Self-compassion and adaptive psychological functioning. Journal of Research in Personality. 2007;41:139–154. https://doi.org/10.1016/j.jrp.2006.03.004. [Google Scholar]
- Neff K., Tirch D., Self-compassion and ACT. In: Kashdan T.B., Ciarrochi J., editors. New Harbinger Publications, Inc; 2013. Mindfulness, acceptance, and positive psychology: The seven foundations of well-being. [Google Scholar]
- Pakenham K.I., Landi G., Boccolini G., Furlani A., Grandi S., Tossani E. The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID-19 pandemic and lockdown in Italy. Journal of Contextual Behavioral Science. 2020;17:109–118. doi: 10.1016/j.jcbs.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parola A., Rossi A., Tessitore F., Troisi G., Mannarini S. Mental health through the COVID-19 quarantine: A growth curve analysis on Italian young adults. Frontiers in Psychology. 2020;11 doi: 10.3389/fpsyg.2020.567484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltz J.S., Daks J.S., Rogge R.D. Mediators of the association between COVID-19-related stressors and parents' psychological flexibility and inflexibility: The roles of perceived sleep quality and energy. Journal of Contextual Behavioral Science. 2020;17:168–176. doi: 10.1016/j.jcbs.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Presti G., McHugh L., Gloster A., Karekla M., Hayes S.C. The dynamics of fear at the time of COVID-19: A contextual behavioral science perspective. Clinical Neuropsychiatry. 2020;17(2):65–71. doi: 10.36131/CN20200206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puolakanaho A., Lappalainen R., Lappalainen P., Muotka J.S., Hirvonen R., Eklund K.M., Ahonen T., Kiuru N. Reducing stress and enhancing academic buoyancy among adolescents using a brief web-based program based on acceptance and commitment therapy: A randomized controlled trial. Journal of Youth and Adolescence. 2019;48(2):287–305. doi: 10.1007/s10964-018-0973-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raes F., Pommier E., Neff K.D., Van Gucht D. Construction and factorial validation of a short form of the self-compassion scale. Clinical Psychology & Psychotherapy. 2011;18:250–255. doi: 10.1002/cpp.702. [DOI] [PubMed] [Google Scholar]
- Ranganathan P., Pramesh C.S., Aggarwal R. Common pitfalls in statistical analysis: Intention-to-treat versus per-protocol analysis. Perspectives in Clinical Research. 2016;7(3):144–146. doi: 10.4103/2229-3485.184823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravens-Sieberer U., Kaman A., Erhart M., Devine J., Schlack R., Otto C. Vols. 1–11. European Child & Adolescent Psychiatry; 2021. (Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany). Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salokangas R.K., Poutanen O., Stengård E. Screening for depression in primary care. Development and validation of the depression scale, a screening instrument for depression. Acta Psychiatrica Scandinavica. 1995;92(1):10–16. doi: 10.1111/j.1600-0447.1995.tb09536.x. [DOI] [PubMed] [Google Scholar]
- She R., Wong K., Lin J., Zhang Y., Leung K., Yang X. Profiles of stress and coping associated with mental, behavioral, and Internet use problems among adolescents during the COVID-19 pandemic: A stratified random sampling and cluster analysis. Frontiers in Public Health. 2022;10 doi: 10.3389/fpubh.2022.826911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sieverink F., Kelders S.M., van Gemert-Pijnen J.E. Clarifying the concept of adherence to eHealth technology: Systematic review on when usage becomes adherence. Journal of Medical Internet Research. 2017;19(12) doi: 10.2196/jmir.8578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.M., Twohy A.J., Smith G.S. Psychological inflexibility and intolerance of uncertainty moderate the relationship between social isolation and mental health outcomes during COVID-19. Journal of Contextual Behavioral Science. 2020;18:162–174. doi: 10.1016/j.jcbs.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger C.D., Gorsuch R.L., Lushene R., Vagg P.R., Jacobs G.A. Consulting Psychologists Press; 1983. Manual for the state-trait anxiety inventory. [Google Scholar]
- Strosahl K., Robinson P., Gustavsson T. New Harbinger Publications; 2012. Brief interventions for radical change: Principles and practice of focused acceptance and commitment therapy. [Google Scholar]
- Swain J., Hancock K., Hainsworth H.C., Bowman J. Mechanisms of change: Exploratory outcomes from a randomised controlled trial of acceptance and commitment therapy for anxious adolescents. Journal of Contextual Behavioral Science. 2015;4(1):56–67. [Google Scholar]
- Välimäki M., Anttila K., Anttila M., Lahti M. Web-Based Interventions Supporting Adolescents and Young People With Depressive Symptoms: Systematic Review and Meta-Analysis. JMIR mHealth and uHealth. 2017;5(12):e180. doi: 10.2196/mhealth.8624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. Guidelines on mental health promotive and preventive interventions for adolescents: Helping adolescents thrive.https://www.who.int/docs/default-source/mental-health/guidelines-on-mental-health-promotive-and-preventive-interventions-for-adolescents-hat.pdf [PubMed] [Google Scholar]
- Xu W., Shen W., Wang S. Intervention of adolescent’ mental health during the outbreak of COVID-19 using aerobic exercise combined with acceptance and commitment therapy. Children and Youth Services Review. 2021;124 doi: 10.1016/j.childyouth.2021.105960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng X., Chiu C.P.K., Wang R., Oei T.P.S., Leung F.Y.K. The effect of loving-kindness meditation on positive emotions: A meta-analytic review. Frontiers in Psychology. 2015;6:1–14. doi: 10.3389/fpsyg.2015.01693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C.Q., Leeming E., Smith P., Chung P.K., Hagger M.S., Hayes S.C. Acceptance and commitment therapy for health behavior change: A contextually-driven approach. Frontiers in Psychology. 2018;8:2350. doi: 10.3389/fpsyg.2017.02350. [DOI] [PMC free article] [PubMed] [Google Scholar]