Abstract
The provision of palliative care in the intensive care unit (ICU) is increasing. While some scholars have suggested the goals of palliative care to not be aligned with the ICU, some evidence show benefits of the integration. This review aimed to explore and synthesize research that identified barriers and facilitators in the provision of palliative care in the ICU. This review utilized Preferred Reporting Items for Systematic Reviews and Meta-Analyses Scoping Review guidelines based on population, concept, and context. We searched for eligible studies in five electronic databases (Scopus, PubMed, ProQuest, Science Direct, and Sage) and included studies on the provision of palliative care (concept) in the ICU (context) that were published in English between 2005–2021. We describe the provision of palliative care in terms of barriers and facilitators. We also describe the study design and context. A total of 14 papers was included. Several barriers and facilitators in providing palliative care in the ICU were identified and include lack of capabilities, family boundaries, practical issues, cultural differences. Facilitators of the provision of palliative care in an ICU include greater experience and supportive behaviors, i.e., collaborations between health care professionals. This scoping review demonstrates the breadth of barriers and facilitators of palliative care in the ICU. Hospital management can consider findings of the current review to better integrate palliative care in the ICU.
Keywords: critical care, end-of-life care, hospitals, intensive care unit, palliative care, terminal care
INTRODUCTION
Palliative care (PC) is an interprofessional approach to care for patients with serious and complex illness aimed to optimize their quality of life by anticipating, preventing, and treating suffering when the patients are no longer responsive to curative therapies [1]. The provision of PC has shown many benefits including improved quality of life and reduced hospital admission and hospital stays [2]. Due to its benefits, the provision of PC is encouraged to be integrated into a health system, including in the intensive care unit (ICU) [3-5]. The provision of PC in the ICU is increasing, and all patients admitted to ICU should receive PC, which includes symptom management, patient-centered care, and shared-decision making [1,6,7].
Initially, provision of PC in the ICU aimed to improve end-of-life (EOL) care, which includes symptom management and shared decision-making [8]. A previous study showed that up to 20% of patients in an ICU were eligible for PC consultation [9]. Such a PC consultation is available to patients with the following conditions: (1) multisystem organ failure, (2) stage IV malignancy, (3) a stay 10 days or longer in the ICU, (4) intracerebral hemorrhage that requires ventilation, or (5) post cardiac arrest [9]. Thus, ICU-based PC could support patients and families and can provide a more comfortable environment, better healing, and increased awareness of EOL care [10]. It has been shown that PC can be an important component of care for all patients with life-limiting illness [11]. In addition, a current systematic review identified positive outcomes of PC provision in the ICU that include reduced length of hospital stay and reduced time on life-sustaining treatment [12].
The literature search found limited studies focusing on the barriers and facilitators of PC integration in the ICU. Therefore, this scoping review aimed to explore and map barriers and facilitators experienced by health care providers in addressing PC provision in the ICU.
MATERIALS AND METHODS
This scoping review was conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Review (PRISMA-ScR) guidelines [13]. We followed Arksey and O’Malley’s steps for conducting a scoping review: (1) identifying the research questions, (2) identifying relevant studies, (3) study selection, (4) charting data, (5) collating, summarizing, and reporting results, and (6) consultation with the experts [14].
Identifying the Research Questions
In a scoping review, it is fundamental to have a well-defined research question that includes the scope of the study, because it will allow researchers to conduct a more practical and efficient review [15]. There were two research questions for the present review: (1) What are barriers of PC provision in the ICU? and (2) What are facilitators of PC provision in the ICU?
Identifying Relevant Studies
We searched the five electronic databases PubMed (Medline), Science Direct, ProQuest, Scopus, and Sage to identify published studies that met the inclusion criteria. We searched using keywords that were developed based on our questions: “palliative care,” “end-of-life care,” “terminal care,” “intensive care,” “ICU,” and “critical care.” We exported all identified records to Endnote 20 Software (Clarivate Analytics, Philadelphia, PA, USA) and used it to remove duplicates automatically.
Study Selection
Each title and abstract of the retrieved articles were screened independently by two reviewers (ER and SA) to assess adherence to the inclusion criteria. Inclusion criteria were (1) studies about PC or EOL care in adult ICU, (2) studies with quantitative, qualitative, or mixed method designs, (3) publication year 2005–2021, and (4) published in English. Review articles and protocols were excluded. Full-text articles were reviewed independently and then discussed to confirm if the full-text articles met the inclusion criteria. Any discrepancies between the two reviewers at any stage of the selection process were discussed and settled with a third reviewer.
Charting the data
The fourth step was charting the data. A table for extracting details, characteristics, and results of studies based on the Joanna Briggs model was developed [16]. Each of the 14 included studies was read several times by four reviewers (CE, YO, SA, and ER) to ensure that all information was included. We developed a table to chart and capture all relevant important information. Categories included in the charting data stage were: (1) author and publication year, (2) aim of the study, (3) context of the study (country, type of ICU), (4) study design, and (5) respondents (number of participants, characteristics) and study findings.
Consultation to Expert
The consultants’ roles were to provide additional references on potential studies for inclusion in the review, as well as valuable insights into the issues identified. In this study, the process involved an experienced critical care nurse and an anesthetic doctor who served in the ICU as a consultant; both were asked for their opinions regarding the study findings. Both experts agreed with the findings and highlighted the importance of hospital policy related to the provision of PC in an ICU.
RESULTS
Search Results
We found 5,499 studies during the literature search. After removing 531 duplicate articles, the remaining 4,985 articles were further examined based on inclusion criteria by titles and abstracts. In the title and abstract screening, articles that did not meet the inclusion criteria were removed. A total of 149 full text articles was screened independently and discussed to determine relevance. The research flow of articles through identification of final papers is represented in Figure 1.
Figure 1.
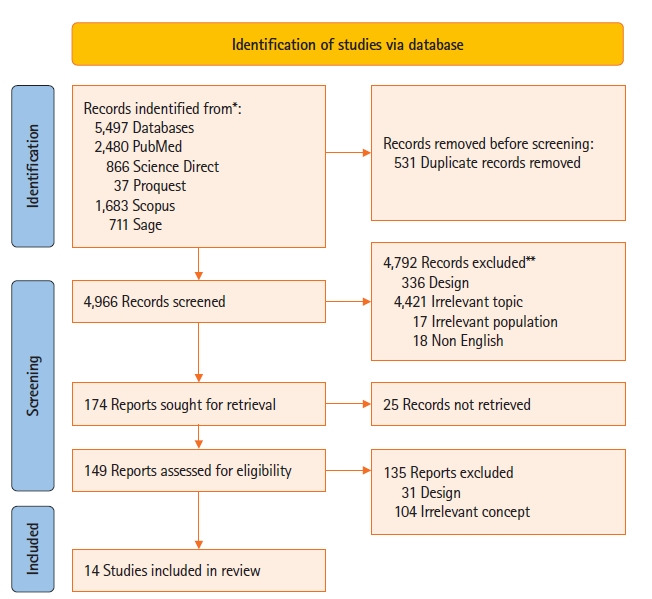
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Review (PRISMA-ScR) search flowchart.
Characteristics of the Included Studies
A total of 14 papers was reviewed in the current scoping review (Table 1) [17-30]. The included studies were performed in nine countries: Egypt (n=1), United States (n=5), Brazil (n=2), Israel (n=1), Germany (n=1), Canada (n=1), Poland (n=1), Scotland (n=1), and Jordan (n=1). The total number of participants was 2,015, comprising patients and relatives (n=324) and health care professionals (HCPs) that included nurses (n=1.499), physicians (n=159), and other HCPs (n=33). The papers explored the provision of EOL care (n=10) in intensive and critical care (n=4) units.
Table 1.
Data extraction of included studies
| Study | Purpose | Design | Context |
Respondent |
Result | ||
|---|---|---|---|---|---|---|---|
| Country | Type of ICU | Characteristics | Total | ||||
| Santos et al. (2017) [17] | To explore perceptions of health professional related with end-of-life care and discuss they goals when planning a palliative care | Qualitative approach | Brazil | Oncology ICUs | Nurses (n=12), physicians (n=8), nutritionists (n=2), and physiotherapists (n=3) | 25 Professionals participated | Barriers doing palliative care in oncology intensive care unit consist of prognostic disease of patient, lack of knowledge and interest in palliative care and reluctance to accept that it is no longer possible to keep seeking for a cure |
| Espinosa et al. (2010) [18] | To understand the experience of ICU nurses in providing end of life care is important first step to improving terminal care in the ICU | Phenomenological research study | United States | Adult ICUs | Participants consisted of women (n=15) and men (n=3) of nurses and with experience providing terminal care | 18 Nurses | Lack of involvement, education, experience of nurses in the plan of care, disagreement and differences practice models among physicians and other healthcare team members, perception of futile care and unnecessary suffering, family unrealistic expectation |
| Ganz and Sapir (2019) [27] | To describe perceptions of Israeli ICU nurses about end-of-life nursing care (include palliative care), the intensity and frequency of barriers to providing quality end-of-life care and the correlation between them | Quantitative approach with personal and work characteristics questionnaire, the quality of palliative care in the ICU And a revised ICU version of the survey of oncology nurses’ perceptions of end-of-life care (sonpelc) | Israel | General/medical, respiratory/surgical, cardiovascular and neurological ICUs | Nurses from 2 hospitals | 124 ICU nurses | Barriers providing end of life care in ICU such as communication between family, physicians and patients, and cultural differences leading to a lack of end-of-life discussions, and lack of palliative care education |
| Graw et al. (2012) [29] | To know advance directives influenced decision making of EOL on the ICU | Retrospective study | Germany | Surgical ICUs | Patients with terminal illness | 224 Patients | Lack of communication and inadequate of documentation being challenges in providing end of life care |
| Kyeremanteng et al. (2020) [19] | To explore barriers towards palliative care-ICU integration | Online survey through email | Canada | Cardiac ICUs | Physicians (n=16), nurses (n=154), ICU fellow (n=5), palliative care staff physician (n=6) | 181 Health workers | unrealistic patient or family expectations, disagreement about goals of care, different opinion of physician, and lack of communication skills as barriers to providing palliative care in ICU |
| Festic et al. (2012) [20] | To explore the differences of physicians and nurses on EOLC in the ICU and how these differences vary according to self-reported proficiency level and primary work unit | A cross-sectional study | United States | Adult ICUs | Physicians (n=50) and nurses (n=331) | 381 Health professionals | Significant differences between physicians and nurses were noted in the following areas: ability to safely raise concerns, DNR decision making, discussion of health care directives, timely hospice referral, spiritual assessment documentation, utilization of social services, and the availability of EOLC education. In every domain of EOLC, physicians reported a more positive perception than nurses. Additional differences were noted among physicians based on experience, as well as among nurses based on their primary work unit and self-reported proficiency level. |
| McKeown et al. (2011) [21] | To explore in depth the Stirling Royal Infirmary ICU team’s views and experiences of the difficulties of providing palliative care in an intensive care setting, and identification of the dying patient | Qualitative interview-based study | Scotland, United Kingdom | Adult ICUs | Participants consisted of consultants (n=5), nursing staffs (n=10) and junior medical staffs (n=10), none of who were known to the interviewing researcher in advance | A total of 25 interviews were undertaken | The ICU team reported there to be a number of advantages to providing EOLC in the ICU in terms of access to nursing and medical care. They also reported there to be issues surrounding training, identification of palliative care patients and over-aggressive management. Further collaboration between ICU and palliative medicine is required to develop understanding between the two specialties and expand provision of palliative care in this unique clinical setting. |
| Friedenberg et al. (2012) [22] | To identify training- and discipline-based barriers among ICU nurses and physicians in attending training | Survey | United States | Medical ICUs | Residents (n=125), fellows (n=20), attendings (n=13), and nurses (n=60) | 218 Participants | There were significant differences in reported barriers to EOL care by level of training, discipline, and institution, particularly in the education-training domain. Nurses’ perceptions of barriers to EOL care varied between institutions. Barriers that varied significantly between nurses included difficulty communicating due to language, inadequate training in recognition of pain and anxiety |
| Atwood et al. (2014) [28] | To compare oncology and CCPs' attitudes regarding palliative care | Electronic survey assessed using simulated patient description to identify respondents’ opinions of whether, when, and why palliative care should be utilized | United States | General ICU in academic hospitals | CCP (n=80), age ranged: 31–>60, years of experience 0–20 years, oncologist (n=72) | 152 Professionals participated | The trained CCP were more likely to integrate PC based on patients' risk and morbidity. |
| Women were more likely to incorporate PC in earlier the illness trajectory. | |||||||
| Attia et al. (2013) [23] | To investigate critical care nurses’ perceptions of barriers and supportive behaviors in providing EOL care to dying patients and their families. | Descriptive design | Egypt | Oncology, cardiology, hepatic and surgical ICUs | Nurses who involved in caring for critically ill patients | 70 ICU nurses | Several barriers were perceived: environment; family members, nurses’ knowledge and skills, physicians’ attitudes and treatment policy. |
| Oncology ICU (n=20) | |||||||
| Cardiology ICU (n=15) | |||||||
| Hepatic ICU (n=15) | |||||||
| Surgical ICU (n=20) | |||||||
| Bluck et al. (2019) [24] | To identify perspectives of HCP at EOL in ICU and barriers to provide palliative care | Mixed method approach: open ended survey | United States | ICU | Resident and fellows (n=18), | 39 Participants | Barriers providing palliative care in ICU included lack of care coordination, limited time, excessive paperwork, having a narrow knowledge base. |
| nurses (n=10), | |||||||
| attending physicians (n=6), | |||||||
| advanced practitioners (n=2), quality improvement specialist (n=2), case manager (n=1) | |||||||
| Ozga et al. (2020) [25] | To understand barriers to EOLC in ICUs, and to identify difficulties perceived by ICU nurses providing EOL care in Poland | Qualitative approach | Poland | Adult ICUs | The participants of the study included register nurses from various ICUs from across Poland with at least 2-year experience working at an ICU | 31 Individuals participated | The main issues raised during the interviews included (1) barriers attributable to the hospital, (2) barriers related to the patient’s family, and (3) barriers related to the ICU personnel providing direct EOLC. The interviewed nurses considered the lack of support from managers to be the main barrier. We found that ICU nurses in Poland dealt with end-of-life aspects that were emotionally and psychologically taxing. In addition, they lacked specialized training in this area, especially with regard to family care and care provision. |
| Silveira et al. (2016) [26] | To know the feelings of nurses regarding palliative care in adult intensive care units | Qualitative approach | Brazil | ICU | Participants of this study consisted of female (n=26) and male (n=4) nurses exercising their labor activities in the period of data collection and have at least one year experience in assisting adult palliative care patients in ICU, which may be current or past experience | 30 Nurses participated in this study | The results showed how central ideas are related to feelings of comfort, frustration, insecurity and anguish, in addition to the feeling that the professional training and performance are focused on the cure. |
| Sharour et al. (2019) [30] | To explore the obstacles and strategies for improvement from nurses' perception of EOLC | Quantitative study with a multisite cross-sectional descriptive design | Jordan | ICU | critical care nurse from different governmental and private hospitals | 163 Critical care nurses | The highest obstacles from the nurses’ perception were family and friends who continually call the nurse wanting an update on the patient’s condition rather than calling the designated family member for information. Furthermore, the highest three supportive behaviors from the nurses’ perception were physicians agreeing about direction of patient care, family members accept that patient is dying, family designating one family member as contact person for the rest of the family. |
ICU: intensive care unit; EOL: end-of-life; EOLC: end-of-life care; DNR: do not resuscitate; CCP: critical care provider; PC: palliative care; HCP: health care professional.
Barriers on the Provision of PC in the ICU
After reviewing the literature, barriers and facilitators were identified. The barriers were lack of capabilities, family boundaries, practical issues, and cultural differences. Further analysis of each barrier found in this review is described below.
Lack of capabilities
There are several barriers to the provision of PC in an ICU. The limited capabilities of HCPs were the most significant barrier [17-28], due in part to shortcomings in PC training [17,28]. In addition, a study conducted by Ozga et al. [25] highlighted the absence of hospital management support in providing training on EOL care. This hinders nurses from acquiring a better understanding of PC, particularly in EOL care. The inadequacy of educational and training for EOL care was perceived as a barrier to integrate PC into the ICU, dealing with death and dying issues, and lack of communication. A study conducted by McKeown et al. [21] stated that education could equip an ICU team to deal with issues surrounding PC as well as death and dying. Four studies found insufficient communication between medical teams and family members [17-19,23]. Evidence from included studies showed lack of communication with patients and families related to decision-making by HCPs [18,19,29].
Family boundaries
Another barrier is family boundaries, an enduring problem in the integration of PC into ICU protocols [18,19,24,27,29-31]. Many families in such situations have unrealistic expectations, which can lead to difficulties for HCPs in applying PC principles based on comfort care and may lead to aggressive treatment for the patients [18,19,23]. A study conducted by Kyeremanteng et al. [19] found unrealistic patient or family expectations as a barrier in providing EOL care in the ICU. This is because the family lacked the necessary medical knowledge and did not fully understand the condition of the dying patient. Unrealistic expectations also were found by Espinosa et al. [18], who identified unrealistic expectations as barriers to PC, particularly during EOL care.
Practical issues
Practical issues are also a considerable barrier to PC delivery in the ICU [18-20,23,29,32]. These issues include limited time for administrative tasks and documentation, disagreement about goals of care between HCPs, differences in nursing and medical approaches, and administrative policy treatment. During providing PC in the ICU there are often agreements and disagreements between HCPs. For example, agreement between HCP was found in Festic et al.’s study [20] that both physicians and nurses agree if patient’s death was not the result of treatment failure. In addition, they thought that providing EOL care for dying patients and their families is a rewarding experience. Meanwhile, disagreement among physicians and nurses is common when providing EOL care in the ICU. Nurses often feel uninvolved in the treatment plan for dying patients, simply carrying out actions discussed and decided only by doctors and families [18,19]. Inadequate policies and practices were identified as barriers to EOL care in the ICU [20].
Differences between medical and nursing models, which were reported as barriers, showed that medical models are focused more on disease or dysfunction, while most nurses are trained in a holistic model to consider all aspects of the patient. The difference between these two models can create difficulty when nurses try to implement physician directions, resulting in nurse frustration, especially in providing EOL care [18]. Practical issues also can be caused by lack of documentation; a study conducted by Graw et al. [29] found that lack of documentation related to advance directives was a significant barrier for health workers in providing care as desired by patients. In addition, barriers including lack of coordination, limited time and staff, and ethical issues were identified [31].
Cultural differences
Cultural difference is another barrier in the provision of PC in the ICU. In this review, only one paper highlighted cultural differences [27]. Ganz and Sapir [27] state that doctors in Asia are more aggressive in their treatment than those in the West. This finding may be due to cultural differences, as death is often not openly discussed in Asia, which can lead to lack of discussion about EOL decisions.
Facilitators in the Provision of PC in ICU
Several facilitators have been identified and include experiences and supportive behavior. Further analysis of each facilitator found in this study is described below.
Supportive behaviors
Sharour et al. [30] identified some supportive behaviors in providing EOL care, including collaboration among physicians and other HCPs to stop aggressive treatment and start EOL care, thereby improving family acceptance. In addition, family acceptance regarding patient death can reduce suffering and psychosocial distress and improve the quality of life for families and their time with patients. Another helpful behavior is appointing one of the family members to communicate with the nurse. This can make it easier for nurses to explain the patient’s condition and EOL care, possibly increasing the effectiveness of treatment and reducing the nurses’ workload.
Previous experiences
Another facilitator is experience, which was identified in a previous study. Festic et al. [20] found that nurses and attending physicians who have longer working experience state have higher agreement on conducting EOL discussion than fellow physicians. Experience is influenced by length of working and the context where the HCP works Experience can lead HCPs in providing EOL care, and ample experience could result in better quality of EOL care [20].
DISCUSSION
This study provides a comprehensive review of the research evidence on the barriers and facilitators in PC provision in the ICU. Further, this review highlights barriers to such provision, including lack of capabilities (knowledge, skills, communications), family boundaries, practical issues, and cultural differences. Facilitators of previous experience and supportive behavior also were identified from the included studies. While, in theory, the ICU and PC principles and practices may seem to be opposites, the two share a similar fundamental goal to provide quality care to patients [1]. PC is increasingly accepted as an essential component of comprehensive care for critically ill patients, regardless of age, diagnosis, and prognosis [33]. The provision of PC has grown exponentially during the last decade. In this regard, data regarding implementation of PC in the ICU setting is lacking due to the common practice of referring PC patients to hospice care, which is commonly offered in a non-hospital setting [1]. In the coming decades, evidence and knowledge translation in PC, intensive care, and their integration will expand further [34].
Barriers in the Provision of PC
Ongoing barriers for optimal integration of PC in the ICU setting have been identified. The provision of a high quality of care for patients who are nearing their EOL is the professional responsibility of health care workers [35]. Therefore, it is crucial for health professionals who work in the hospital to be competent in basic PC and EOL care. However, physicians and nurses continue to lack knowledge in the necessary communication skills, including communicating with family and patients about outcomes and managing clinical aspects of poor outcomes [36]. This limitation may be caused by limited availability of training and education [37]. A study found that a lack of knowledge was more prevalent in female compared to male healthcare professionals and less frequently in physicians [38]. In addition, knowledge deficits were more prevalent in healthcare professionals who had little contact with dying patients [38]. Healthcare professionals who worked with seriously ill or dying patients had higher motivation for quality care compared to those who did not have such contact [38]. However, one study found that critical care nurses felt inadequate and unprepared to provide quality EOL care in the ICU [39]. Regarding EOL decision making skills, a study found that European physicians had no difficulty in making EOL decisions in 81%–93% of cases. In contrast, such decisions were perceived to be difficult by Indian physicians due to barriers of lack of awareness of ethical issues, culture of heroic “fighting till the end,” and lack of PC orientation [40].
Another study supported our findings that the main obstacles of EOL care by doctors and nurses in critical care units were lack of education and training regarding family grieving and quality of EOL care [41]. Training on implementation of PC in the ICU could improve the capabilities of nurses and physicians. For example, two studies reported that training can improve PC knowledge and skills, particularly in symptom management and communication [42,43].
Another barrier in EOL care is cultural differences. Our study confirmed previous findings from Asia that physicians in ICUs frequently withheld but rarely withdrew life-sustaining treatment [44,45]. A study from Asia reported an ethical dilemma involved in withholding and withdrawal of treatment among Asian nurses, where withholding is considered more ethical than withdrawing treatment [46].
While there were several barriers identified, we found previous experiences of HCPs facilitate the provision of PC in the ICU. This finding aligns with a previous study among ICU nurses in which the respondents were classified into two groups based on work experience. Jang et al. [47] reported that the more experienced group tended to consider EOL care.
In addition to experience, supportive behaviors also facilitate the provision of PC. Supportive behaviors such as transformational leadership and supportive inquiry conditions were also reported in two previous studies. For example, the application of transformational leadership was able to create good daily working environments including adequate staffing and has been suggested as contributing to successful implementation. Moreover, facilitation, in the sense of individuals or strategies that make change easier, has recently been strengthened as a crucial component for implementation of EOL care. Another study reported that peer emotional support has a facilitating role for EOL care in the ICU [31].
This literature review applied the six steps of Arksey and O’Malley guidelines, including the sixth step of consulting experts. The experts validated that all articles met the criteria and examined both clinical and practical related contexts. The keywords used were broader compared to PC articles in the ICU setting and included PC, end of life care, and terminal care. This resulted in a large number of identified articles.
CONCLUSIONS
Implementing PC in the ICU is increasingly recognized. However, the implementation of this PC care in the ICU settings has faced some barriers such as lack of capabilities among doctors and nurses, family boundaries, and cultural differences. The facilitators in implementing PC in the ICU setting include health care provider experience and supportive behavior within the organization.
KEY MESSAGES
▪ The provision of palliative care in intensive care units (ICUs) is advocated to improve end-of-life care and patient’ quality of life, and to reduce hospital admission and hospital stays.
▪ This review maps a lack of capabilities and family boundaries as barriers in the integration of palliative care in the ICU
▪ Experiences and supportive behaviors are identified as facilitators in the provision of palliative care in ICUs.
Acknowledgments
This was part of a larger study funded by the Institute of Research and Innovation, Universitas Muhammadiyah Yogyakarta. The authors thank the Institute of Research and Innovation, Universitas Muhammadiyah Yogyakarta.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: CE, YY, ER, Data curation: ER, SA. Formal analysis: ER, SA. Funding acquisition: ER. Methodology: CE, YY, ER. Project administration: SA. Writing–original draft: all authors. Writing–review & editing: all authors.
REFERENCES
- 1.Mercadante S, Gregoretti C, Cortegiani A. Palliative care in intensive care units: why, where, what, who, when, how. BMC Anesthesiol. 2018;18:106. doi: 10.1186/s12871-018-0574-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yosick L, Crook RE, Gatto M, Maxwell TL, Duncan I, Ahmed T, et al. Effects of a population health community-based palliative care program on cost and utilization. J Palliat Med. 2019;22:1075–81. doi: 10.1089/jpm.2018.0489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hua M, Wunsch H. Integrating palliative care in the ICU. Curr Opin Crit Care. 2014;20:673–80. doi: 10.1097/MCC.0000000000000149. [DOI] [PubMed] [Google Scholar]
- 4.Munro CL, Savel RH. Aggressive care AND palliative care. Am J Crit Care. 2018;27:84–6. doi: 10.4037/ajcc2018757. [DOI] [PubMed] [Google Scholar]
- 5.Ito K, George N, Wilson J, Bowman J, Aaronson E, Ouchi K. Primary palliative care recommendations for critical care clinicians. J Intensive Care. 2022;10:20. doi: 10.1186/s40560-022-00612-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aslakson RA, Curtis JR, Nelson JE. The changing role of palliative care in the ICU. Crit Care Med. 2014;42:2418–28. doi: 10.1097/CCM.0000000000000573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan H, Shi W, Zhou Q, Chen G, Pan P. Palliative care in the intensive care unit: not just end-of-life care. Intensive Care Res. 2022:1–6. [Google Scholar]
- 8.Ganz FD, Ben Nun M, Raanan O. Introducing palliative care into the intensive care unit: an interventional study. Heart Lung. 2020;49:915–21. doi: 10.1016/j.hrtlng.2020.07.006. [DOI] [PubMed] [Google Scholar]
- 9.Hua MS, Li G, Blinderman CD, Wunsch H. Estimates of the need for palliative care consultation across united states intensive care units using a trigger-based model. Am J Respir Crit Care Med. 2014;189:428–36. doi: 10.1164/rccm.201307-1229OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coelho CB, Yankaskas JR. New concepts in palliative care in the intensive care unit. Rev Bras Ter Intensiva. 2017;29:222–30. doi: 10.5935/0103-507X.20170031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown CE, Engelberg RA, Nielsen EL, Curtis JR. Palliative care for patients dying in the intensive care unit with chronic lung disease compared with metastatic cancer. Ann Am Thorac Soc. 2016;13:684–9. doi: 10.1513/AnnalsATS.201510-667OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Metaxa V, Anagnostou D, Vlachos S, Arulkumaran N, Bensemmane S, van Dusseldorp I, et al. Palliative care interventions in intensive care unit patients. Intensive Care Med. 2021;47:1415–25. doi: 10.1007/s00134-021-06544-6. [DOI] [PubMed] [Google Scholar]
- 13.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 14.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. [Google Scholar]
- 15.Khalil H, Peters M, Godfrey CM, McInerney P, Soares CB, Parker D. An evidence-based approach to scoping reviews. Worldviews Evid Based Nurs. 2016;13:118–23. doi: 10.1111/wvn.12144. [DOI] [PubMed] [Google Scholar]
- 16. Peters MD, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Scoping reviews. In: Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. Adelaide: Joanna Briggs Institute; 2020. [Google Scholar]
- 17.Santos DC, da Silva MM, Moreira MC, Zepeda KG, Gaspar RB. Care planning for patients receiving palliative care in an oncology intensive care unit. Acta Paul Enferm. 2017;30:295–300. [Google Scholar]
- 18.Espinosa L, Young A, Symes L, Haile B, Walsh T. ICU nurses' experiences in providing terminal care. Crit Care Nurs Q. 2010;33:273–81. doi: 10.1097/CNQ.0b013e3181d91424. [DOI] [PubMed] [Google Scholar]
- 19.Kyeremanteng K, Beckerleg W, Wan C, Vanderspank-Wright B, D'Egidio G, Sutherland S, et al. Survey on barriers to critical care and palliative care integration. Am J Hosp Palliat Care. 2020;37:108–16. doi: 10.1177/1049909119867658. [DOI] [PubMed] [Google Scholar]
- 20.Festic E, Wilson ME, Gajic O, Divertie GD, Rabatin JT. Perspectives of physicians and nurses regarding end-of-life care in the intensive care unit. J Intensive Care Med. 2012;27:45–54. doi: 10.1177/0885066610393465. [DOI] [PubMed] [Google Scholar]
- 21.McKeown A, Booth MG, Strachan L, Calder A, Keeley PW. Unsuitable for the intensive care unit: what happens next? J Palliat Med. 2011;14:899–903. doi: 10.1089/jpm.2011.0064. [DOI] [PubMed] [Google Scholar]
- 22.Friedenberg AS, Levy MM, Ross S, Evans LE. Barriers to end-of-life care in the intensive care unit: perceptions vary by level of training, discipline, and institution. J Palliat Med. 2012;15:404–11. doi: 10.1089/jpm.2011.0261. [DOI] [PubMed] [Google Scholar]
- 23.Attia AK, Abd-Elaziz WW, Kandeel NA. Critical care nurses' perception of barriers and supportive behaviors in end-of-life care. Am J Hosp Palliat Care. 2013;30:297–304. doi: 10.1177/1049909112450067. [DOI] [PubMed] [Google Scholar]
- 24.Bluck S, Mroz EL, Baron-Lee J. Providers' perspectives on palliative care in a neuromedicine-intensive care unit: end-of-life expertise and barriers to referral. J Palliat Med. 2019;22:364–9. doi: 10.1089/jpm.2018.0282. [DOI] [PubMed] [Google Scholar]
- 25.Ozga D, Woźniak K, Gurowiec PJ. Difficulties perceived by ICU nurses providing end-of-life care: a qualitative study. Glob Adv Health Med. 2020;9:2164956120916176. doi: 10.1177/2164956120916176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Silveira NR, Nascimento ER, Rosa LM, Jung W, Martins SR, Fontes MD. Palliative care and the intensive care nurses: feelings that endure. Rev Bras Enferm. 2016;69:1074–81. doi: 10.1590/0034-7167-2016-0267. [DOI] [PubMed] [Google Scholar]
- 27.Ganz FD, Sapir B. Nurses' perceptions of intensive care unit palliative care at end of life. Nurs Crit Care. 2019;24:141–8. doi: 10.1111/nicc.12395. [DOI] [PubMed] [Google Scholar]
- 28.Atwood MA, Hoffmann RG, Yan K, Lee KJ. Attitudes about palliative care: a comparison of pediatric critical care and oncology providers. Am J Hosp Palliat Care. 2014;31:665–71. doi: 10.1177/1049909113500844. [DOI] [PubMed] [Google Scholar]
- 29.Graw JA, Spies CD, Wernecke KD, Braun JP. Managing end-of-life decision making in intensive care medicine: a perspective from Charité Hospital, Germany. PLoS One. 2012;7:e46446. doi: 10.1371/journal.pone.0046446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sharour LA, Subih M, Salameh O, Alrshoud M. End-of-life care (EOLC) in Jordanian critical care units: barriers and strategies for improving. Crit Care Shock. 2019;22:88–97. [Google Scholar]
- 31.Riegel M, Randall S, Ranse K, Buckley T. Healthcare professionals' values about and experience with facilitating end-of-life care in the adult intensive care unit. Intensive Crit Care Nurs. 2021;65:103057. doi: 10.1016/j.iccn.2021.103057. [DOI] [PubMed] [Google Scholar]
- 32.Albert M, Herlitz J, Rawshani A, Ringh M, Claesson A, Djärv T, et al. Cardiac arrest after pulmonary aspiration in hospitalised patients: a national observational study. BMJ Open. 2020;10:e032264. doi: 10.1136/bmjopen-2019-032264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Edwards JD, Voigt LP, Nelson JE. Ten key points about ICU palliative care. Intensive Care Med. 2017;43:83–5. doi: 10.1007/s00134-016-4481-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mathews KS, Nelson JE. Palliative care in the ICU of 2050: past is prologue. Intensive Care Med. 2017;43:1850–2. doi: 10.1007/s00134-017-4828-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Price DM, Strodtman L, Montagnini M, Smith HM, Miller J, Zybert J, et al. Palliative and end-of-life care education needs of nurses across inpatient care settings. J Contin Educ Nurs. 2017;48:329–36. doi: 10.3928/00220124-20170616-10. [DOI] [PubMed] [Google Scholar]
- 36.Aslakson R, Cheng J, Vollenweider D, Galusca D, Smith TJ, Pronovost PJ. Evidence-based palliative care in the intensive care unit: a systematic review of interventions. J Palliat Med. 2014;17:219–35. doi: 10.1089/jpm.2013.0409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brooks LA, Manias E, Nicholson P. Barriers, enablers and challenges to initiating end-of-life care in an Australian intensive care unit context. Aust Crit Care. 2017;30:161–6. doi: 10.1016/j.aucc.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 38.Kalies H, Schöttmer R, Simon ST, Voltz R, Crispin A, Bausewein C. Barriers for the implementation of guidelines in palliative care-results from a national survey of professionals. Support Care Cancer. 2018;26:1943–52. doi: 10.1007/s00520-017-4030-z. [DOI] [PubMed] [Google Scholar]
- 39.Hall JB. Making recommendations for limiting care in the ICU based on sound prognosis. JAMA. 2017;317:2170–1. doi: 10.1001/jama.2017.4327. [DOI] [PubMed] [Google Scholar]
- 40.Mani RK, Amin P, Chawla R, Divatia JV, Kapadia F, Khilnani P, et al. Guidelines for end-of-life and palliative care in Indian intensive care units' ISCCM consensus ethical position statement. Indian J Crit Care Med. 2012;16:166–81. doi: 10.4103/0972-5229.102112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Almansour I, Seymour JE, Aubeeluck A. Staff perception of obstacles and facilitators when providing end of life care in critical care units of two teaching hospitals: a survey design. Intensive Crit Care Nurs. 2019;53:8–14. doi: 10.1016/j.iccn.2019.04.003. [DOI] [PubMed] [Google Scholar]
- 42.Lind R. Sense of responsibility in ICU end-of-life decision-making: relatives' experiences. Nurs Ethics. 2019;26:270–9. doi: 10.1177/0969733017703697. [DOI] [PubMed] [Google Scholar]
- 43.Graham R, Lepage C, Boitor M, Petizian S, Fillion L, Gélinas C. Acceptability and feasibility of an interprofessional end-of-life/palliative care educational intervention in the intensive care unit: a mixed-methods study. Intensive Crit Care Nurs. 2018;48:75–84. doi: 10.1016/j.iccn.2018.04.011. [DOI] [PubMed] [Google Scholar]
- 44.Phua J, Joynt GM, Nishimura M, Deng Y, Myatra SN, Chan YH, et al. Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Intern Med. 2015;175:363–71. doi: 10.1001/jamainternmed.2014.7386. [DOI] [PubMed] [Google Scholar]
- 45.Phua J, Joynt GM, Nishimura M, Deng Y, Myatra SN, Chan YH, et al. Withholding and withdrawal of life-sustaining treatments in low-middle-income versus high-income Asian countries and regions. Intensive Care Med. 2016;42:1118–27. doi: 10.1007/s00134-016-4347-y. [DOI] [PubMed] [Google Scholar]
- 46.Tripathy S, Routray PK, Mishra JC. Intensive care nurses' attitude on palliative and end of life care. Indian J Crit Care Med. 2017;21:655–9. doi: 10.4103/ijccm.IJCCM_240_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jang SK, Park WH, Kim HI, Chang SO. Exploring nurses' end-of-life care for dying patients in the ICU using focus group interviews. Intensive Crit Care Nurs. 2019;52:3–8. doi: 10.1016/j.iccn.2018.09.007. [DOI] [PubMed] [Google Scholar]


