Abstract
Background
The relevance and importance of using racial and ethnic categories in medical education is an area requiring richer discussion and engagement among all health professions educators.
Objectives
There is a genuine need to identify opportunities for leveraging social and structural determinants of health to address health disparities within medical education. We designed a focus session led by a team of diverse clinical and basic science faculty to analyze how medical curricula can integrate racial/ethnic identity as a clinical indicator. We sought to develop strategies to empower medical students and teachers to integrate race as a social rather than a biological construct.
Methods
The 90-minute focus session included an interactive presentation reviewing the literature related to the use of racial identity in medical education, small group case-based discussions in breakout rooms, a large group debrief, and an optional activity for participants to apply the knowledge gained. The study was approved by the Nova Southeastern University Institutional Review Board (IRB #: 2021-185-NSU).
Results
Thirty-three participants attended the session at the 2021 International Association of Medical Science Educators (IAMSE) Conference. Eleven (33%) participated in both pre-session and post-session surveys. Survey data revealed significant pre-/post-changes in the knowledge of the advantages and disadvantages of using race in medical education. Qualitative data indicated that participants acquired new knowledge related to the integration of racial identity as a clinical indicator and they were willing to incorporate strategies learned into their teaching.
Conclusion
Our study data suggests that this focus session equipped faculty with new knowledge and resources to effectively incorporate racial/ethnic identity into medical school curricula to increase awareness of healthcare disparities.
Keywords: medical teaching, diagnostic medicine, clinical skills, ethnicity, race
Introduction
Race, ethnicity, and their relevance in medical education and the practice of medicine continue to be a topic that is heavily discussed in academia. In the past several years, much emphasis has been placed on the topic at academic conferences, with emphasis on ways to identify and mitigate implicit bias at the forefront. Racial categories and their connection with health equity and healthcare outcomes have been intertwined within the practice of medicine for decades, and this has shaped the way in which knowledge is imparted in medical school curricula, clinical research, and textbooks. There are varying opinions among medical educators, where some are averse to the use of racial categories and race-based guidelines due to concerns that when medical school curricula train students to consider racial categories for patients’ healthcare, this perpetuates systemic issues such as microaggressions and stereotyping [1,2]. On the other hand, some medical educators including physicians of color often support the integration of racial categories into diagnostic medicine and clinical care on the basis that there is value and benefit to patients of color when the aim of racial integration is to highlight social and structural rather than genetic explanations [2-5]. Generally, those in support of leveraging race and ethnicity information for better patient outcomes propose that racial identity can be useful for identifying different disease mechanisms and planning relevant clinical interventions when disease etiology is related to social affiliations and environments [2-5]. This interactive workshop was designed and facilitated by clinical faculty, basic science faculty, and medical students. The overarching goal of the session was to generate a robust discussion around the historical and sociological context of race and ethnicity and openly share ideas and expertise on the best approaches to educating medical students about this topic. This was a focus session presented at the 2021 International Association of Medical Science Educators (IAMSE) Conference. The focus session was led by a team of diverse clinical and basic science faculty with the relevant expertise to direct and stimulate discussions. The specific objectives of the session were to review the literature related to the use of racial identity in medical education, analyze the pros and cons of integrating racial categories into case-based learning and clinical skills and diagnostic medicine teaching, and discuss effective strategies for incorporating racial identity into medical education without misidentifying healthcare needs for vulnerable patients.
Materials and methods
Ethical approval
The study was approved by the Nova Southeastern University Institutional Review Board (IRB #: 2021-185-NSU).
Participants
Thirty-three (33) conference attendees participated in the focus session on June 16th during the 2021 International Association of Medical Science Educators (IAMSE) Conference. Of the 33 participants, 23 completed the pre-session surveys, 11 completed both the pre-session and post-session surveys, and eight completed the anonymous commitment activity. These participants had diverse backgrounds based on voluntarily self-disclosed demographic information from the pre-post surveys.
Session structure and context
The 90-minute focus session was presented virtually at the 2021 IAMSE Conference, which had the theme of “Global Perspectives on Health Sciences Education.” A didactic literature review-based presentation centered around teaching racial categories in medical education was followed by a small group case-based discussion. Participants worked through cases that promoted discussion on the advantages and disadvantages of integrating racial categories into active learning cases and integrating this information with the social and structural determinants of health. Participants were then brought back to the large group for debriefing and the optional commitment activity. Pre- and post-activity surveys were utilized as a measure of the effectiveness of the presentation and case-based activity by assessing for changes in knowledge and attitudes about racial identity in medical education. Participants were also invited to participate in an anonymous commitment activity. In this activity, participants were prompted to think of an action item that they could implement in the near future to help increase their self-awareness of using racial identity and avoiding microaggressions, based on the examples given in the session and ideas sparked by discussion.
Cases and facilitators
Two short cases with accompanying questions were developed by the research team with the intention of highlighting the use of racial categories in case-based learning. The experiences of the physicians on the research team who were also individuals of color were integrated into the cases to represent realistic scenarios. Four faculty members and a second-year medical student facilitated the small group discussions. Three of the faculty were females who identified as African American, with one being a basic scientist and two being physicians. The fourth physician facilitator and the student were male, and both were persons of color.
Statistical analysis
A paired Student’s t-test was used to assess the statistical significance of the data obtained from the pre- and post-session surveys, with a p-value less than 0.05 being considered statistically significant.
Results
Demographic characteristics of participants
The demographic characteristics of participants who completed the pre- and post-session surveys are presented in Table 1.
Table 1. Demographic characteristics of the participants (n=23) who completed the pre- and post-session surveys.
| Category | # of respondents (n=23) | % of respondents |
| Professional title | ||
| Basic science faculty | 8 | 34.78 |
| Physician educator | 6 | 26.09 |
| Other health professions faculty | 3 | 13.04 |
| Administrator | 3 | 13.04 |
| Medical student | 2 | 8.70 |
| Other health professions student | 1 | 4.35 |
| Gender | ||
| Females | 19 | 82.61 |
| Males | 3 | 13.04 |
| Prefer not to answer | 1 | 4.35 |
| Sexual orientation | ||
| Straight or heterosexual | 18 | 78.26 |
| Bisexual | 3 | 13.04 |
| Prefer not to answer | 2 | 8.70 |
| Age (years) | ||
| 25-29 | 2 | 8.70 |
| 35-44 | 9 | 39.13 |
| 45-54 | 6 | 26.09 |
| 55-64 | 4 | 17.38 |
| 65 and over | 2 | 8.70 |
| Race/ethnicity | ||
| Asian | 5 | 21.74 |
| Black, non-Hispanic | 1 | 4.35 |
| Hispanic | 3 | 13.04 |
| White, non-Hispanic | 14 | 60.87 |
Pre-/post-surveys
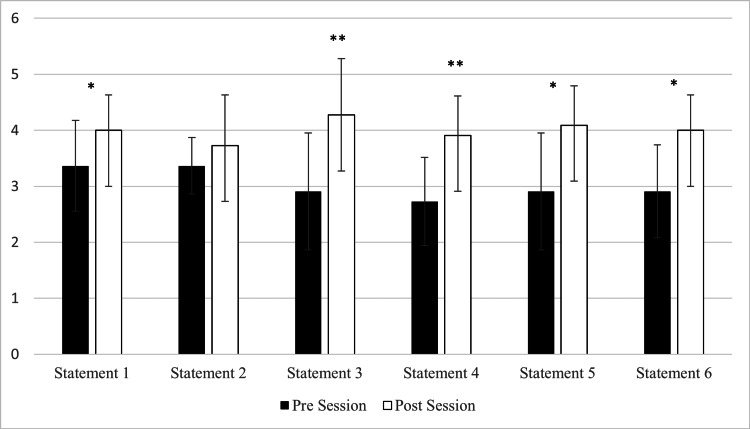
For the pre- and post-session surveys (n=11), the participants responded to the six statements shown in Table 2, on a Likert scale of 5 indicating strongly agree, 4 agree, 3 somewhat agree, 2 disagree, and 1 strongly disagree. Participants showed a significantly favorable increase in five of the six statements. Figure 1 depicts the pre- and post-changes for all six statements.
Table 2. Pre- and post-survey responses.
SD: standard deviation
| Statement | Mean pre-survey responses (SD) | Mean post-survey responses (SD) | Pre- and post-change P value |
| Statement 1: “I am confident in my ability to define race and ethnicity” | 3.36 (0.81) | 4 (0.63) | p=0.026 |
| Statement 2: “I understand and can describe the historical context of race” | 3.36 (0.50) | 3.73 (0.90) | p=0.341 |
| Statement 3: “I am confident in my ability to discuss race as a biologic versus social construct” | 2.91 (1.04) | 4.27 (1.01) | p=0.005 |
| Statement 4: “I am confident in my ability to identify advantages of integrating racial categories into medical teaching” | 2.73 (0.79) | 3.91 (0.70) | p=0.007 |
| Statement 5: “I am confident in my ability to identify disadvantages of integrating racial categories into medical teaching” | 2.91 (1.04) | 4.09 (0.70) | p=0.011 |
| Statement 6: “I am knowledgeable about effective strategies for incorporating racial identity into medical education” | 2.91 (0.83) | 4.00 (0.63) | p=0.014 |
Figure 1. Change in confidence and knowledge.
Results of the pre- and post-survey responses (n=11) to statements 1-6 as shown in Table 2. Data are represented as the mean value ± the standard deviation. * represents p<0.05; ** represents p<0.01.
Anonymous commitment activity
Individuals who participated in the voluntary anonymous commitment activity responded with a wide variety of action items. These items reflected responses to the prompt “I would like to commit to the following personal goal regarding the use of racial identity and/or perpetuating racial microaggression in teaching and in my educational interactions.” The collected narrative responses (n=11) are included in Table 3.
Table 3. Anonymous commitment activity participant responses.
eGFR: estimated glomerular filtration rate; CKD: chronic kidney disease; SDOH: social determinants of health
| Responses |
| I will discuss with my curriculum leadership team whether or how to re-incorporate racial self-identity in a consistent and unbiased manner back into patient cases from which that aspect of identity has been removed, to be able to reflect the diversity of our patient population and seed discussions like we have just had. |
| I will not propagate physician bias and promote stereotypes by the use of outdated, inappropriate question stems or case presentations. I will discuss implicit bias with my students and encourage self-reflection. |
| I agree with the statement. |
| I will give my students tools to help them reflect on their implicit bias and use of racial microaggressions in my courses. |
| I will make sure that the eGFR in our CKD case contains a discussion of the controversy and potential harms of the continued use of race adjustment. |
| I would like to commit to being open and aware of how our institution’s cases may include content about racial identity that perpetuates racial microaggressions in teaching and alter the cases with the use of the relevant social context of race to promote equity in healthcare. |
| I will use race and ethnicity for patient advocacy and SDOH. |
| I will ask questions about the activation of bias or detecting implicit bias in questions, cases, and presentations. |
Discussion
This workshop was intentionally designed to engage medical educators and medical students in the discussion about the use of racial and ethnic categories in medical education. The goal of the activity was to enhance understanding of race-based health disparities and encourage participants to critically analyze the opportunities for appropriate and effective use of racial and ethnic identifiers in medical teaching. There are numerous examples of race-based disparities in medicine that have been refuted in recent years. A traditional example includes the race-based adjustment of spirometer values during pulmonary function testing for Black American patients [6]. Historically, this practice stems from data produced through comparisons of the lungs of Black and White soldiers by physicians during the civil war [1]. However, there is no biological basis for this adjustment as evidenced by recent studies that find no foundation for such corrections [7]. Furthermore, these clinical guidelines place Black Americans specifically at a disadvantage in obtaining disability benefits because of overestimated lung function and might potentially be biasing COVID-19 care by undermining the severity of lung damage and the need for more aggressive recovery treatment plans [8,9]. Other examples of race-based clinical guidelines include the correction of glomerular filtration rate (GFR) for Black Americans and the differential approach to hypertension treatment in Black patients typified by the approval of the drug BiDil (a fixed dose of isosorbide dinitrate plus hydralazine) for the treatment of advanced heart failure in Black patients despite concerns and controversy around the process of its discovery, clinical trials, and marketing [10-13].
Many discussions around race and ethnicity in the medical education literature have focused on the disadvantages of including race and ethnicity in medical decision-making, particularly highlighting that there is significant overlap across racial groups that render race inconsequential for improving diagnosis and care for any one group of individuals [3,14]. Furthermore, the presentation of race in a normalized way in the diagnostic medicine curriculum has been purported to put persons of color at risk for misdiagnoses through racial profiling in the clinical system [2,3].
In this focus session, the participants disclosed through the pre-session survey that there was a need to have more skills and knowledge on how to leverage race and ethnicity information to address the above-highlighted health disparities. Following the didactic session and the case discussions, the participants showed a significant increase in confidence and knowledge about race and medical teaching. This data highlights that sessions of this nature can be beneficial in enhancing the cultural competence of faculty and staff involved in the development and delivery of medical school curricula. This innovative nature of this session also provides a starting point for other medical schools to adapt and customize the presented activities to promote cultural shifts in medical education that will eventually translate into the positive changes that are needed to reduce the systemic barriers faced by individuals of color regarding their healthcare.
Physicians and medical educators are often uncomfortable with discussing race both in preclinical teaching and on the wards, and there is a need for more training for faculty in this regard [15,16]. Population health data categorized by race can be useful for sharpening the diagnostic skills of learners when time is taken to elaborate on the history of racial categories, the concerns around holding race as a biological construct, and the advantages and limits of their utility, especially in the development of case-based learning clinical scenarios that are used routinely in pre-clerkship education [17]. This was highlighted in a recent initiative by the Association of American Medical Colleges (AAMC) to develop “Diversity, Equity, and Inclusion Competencies Across the Learning Continuum,” a framework to help guide faculty development to provide and teach culturally responsive care, including those related to racial disparities [18]. It is therefore imperative that faculty development opportunities are provided for medical educators to enhance their skills and capacity toward addressing race, in order to reduce biases of both learners and faculty [16,19,20].
Limitations
Participation in the session and pre- and post-survey was voluntary with a limited number of participants, which allows for a possible selection bias. However, with the target audience being all faculty in medical education, the representation of the sample should not misrepresent the population as a whole. Although the data was anonymous, it was collected and analyzed by the workshop authors. Demographic information, including professional title, gender, sexual orientation, age, and race/ethnicity, were collected, allowing for analysis of these characteristics for further potentially significant differences. However, as one participant noted, the limited options for providing information about gender and sexual orientation were not inclusive of the spectrum that participants may self-identify on. Opting to use language such as biological sex or separating the two prompts in the future would promote inclusivity.
Conclusions
The meaningful use of racial categories as a social construct is a timely topic of discussion in medical education and clinical practice. The topic by nature is a sensitive one that might generate passionate responses from both learners and educators. Continued implementation of faculty development sessions of this nature can help medical educators especially to be more informed and confident in their ability to appropriately discuss and utilize racial categories in medical education.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. The Nova Southeastern University Institutional Review Board issued approval 2021-185-NSU
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Racial categories in medical practice: how useful are they? Braun L, Fausto-Sterling A, Fullwiley D, et al. PLoS Med. 2007;4:0. doi: 10.1371/journal.pmed.0040271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.From race-based to race-conscious medicine: how anti-racist uprisings call us to act. Cerdeña JP, Plaisime MV, Tsai J. Lancet. 2020;396:1125–1128. doi: 10.1016/S0140-6736(20)32076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Misrepresenting race - the role of medical schools in propagating physician bias. Amutah C, Greenidge K, Mante A, et al. N Engl J Med. 2021;384:872–878. doi: 10.1056/NEJMms2025768. [DOI] [PubMed] [Google Scholar]
- 4.Race, ethnicity, and culture in the medical record: implicit bias or patient advocacy? Fadus MC, Odunsi OT, Squeglia LM. Acad Psychiatry. 2019;43:532–536. doi: 10.1007/s40596-019-01035-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Race, genetic ancestry, and estimating kidney function in CKD. Hsu CY, Yang W, Parikh RV, et al. N Engl J Med. 2021;385:1750–1760. doi: 10.1056/NEJMoa2103753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Defining race/ethnicity and explaining difference in research studies on lung function. Braun L, Wolfgang M, Dickersin K. Eur Respir J. 2013;41:1362–1370. doi: 10.1183/09031936.00091612. [DOI] [PubMed] [Google Scholar]
- 7.Addressing race in pulmonary function testing by aligning intent and evidence with practice and perception. Bhakta NR, Kaminsky DA, Bime C, Thakur N, Hall GL, McCormack MC, Stanojevic S. Chest. 2022;161:288–297. doi: 10.1016/j.chest.2021.08.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Race, ethnicity and lung function: a brief history. Braun L. https://pubmed.ncbi.nlm.nih.gov/26566381/ Can J Respir Ther. 2015;51:99–101. [PMC free article] [PubMed] [Google Scholar]
- 9.Could routine race-adjustment of spirometers exacerbate racial disparities in COVID-19 recovery? Anderson MA, Malhotra A, Non AL. Lancet Respir Med. 2021;9:124–125. doi: 10.1016/S2213-2600(20)30571-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. Ann Intern Med. 1999;130:461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 11.Reassessing the inclusion of race in diagnosing kidney diseases: an interim report from the NKF-ASN task force. Delgado C, Baweja M, Burrows NR, et al. Am J Kidney Dis. 2021;78:103–115. doi: 10.1053/j.ajkd.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. Taylor AL, Ziesche S, Yancy C, et al. N Engl J Med. 2004;351:2049–2057. doi: 10.1056/NEJMoa042934. [DOI] [PubMed] [Google Scholar]
- 13.BiDil: assessing a race-based pharmaceutical. Brody H, Hunt LM. Ann Fam Med. 2006;4:556–560. doi: 10.1370/afm.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Use of racial and ethnic categories in medical testing and diagnosis: primum non nocere. Kaufman JS, Merckx J, Cooper RS. Clin Chem. 2021;67:1456–1465. doi: 10.1093/clinchem/hvab164. [DOI] [PubMed] [Google Scholar]
- 15.Avoiding racial essentialism in medical science curricula. Braun L, Saunders B. AMA J Ethics. 2017;19:518–527. doi: 10.1001/journalofethics.2017.19.6.peer1-1706. [DOI] [PubMed] [Google Scholar]
- 16.When race matters on the wards: talking about racial health disparities and racism in the clinical setting. Brooks KC, Rougas S, George P. MedEdPORTAL. 2016;12:10523. doi: 10.15766/mep_2374-8265.10523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Addressing race, culture, and structural inequality in medical education: a guide for revising teaching cases. Krishnan A, Rabinowitz M, Ziminsky A, Scott SM, Chretien KC. Acad Med. 2019;94:550–555. doi: 10.1097/ACM.0000000000002589. [DOI] [PubMed] [Google Scholar]
- 18.Association of American Medical Colleges: Diversity, equity, and inclusion competencies across the learning continuum. [ Aug; 2022 ]. 2022. https://www.aamc.org/data-reports/report/diversity-equity-and-inclusion-competencies-across-learning-continuum https://www.aamc.org/data-reports/report/diversity-equity-and-inclusion-competencies-across-learning-continuum
- 19.Exploring unconscious bias in disparities research and medical education. van Ryn M, Saha S. JAMA. 2011;306:995–996. doi: 10.1001/jama.2011.1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Addressing racism in medical education an interactive training module. White-Davis T, Edgoose J, Brown Speights JS, Fraser K, Ring JM, Guh J, Saba GW. Fam Med. 2018;50:364–368. doi: 10.22454/FamMed.2018.875510. [DOI] [PubMed] [Google Scholar]