Abstract
Nonalcoholic fatty liver disease (NAFLD) is the most common chronic liver disease. Nonalcoholic steatohepatitis (NASH) is an advanced form of NAFLD can progress to liver cirrhosis and hepatocellular carcinoma (HCC). Recently, the prognosis of NAFLD/NASH has been reported to be dependent on liver fibrosis degree. Liver biopsy remains the gold standard, but it has several issues that must be addressed, including its invasiveness, cost, and inter-observer diagnosis variability. To solve these issues, a variety of noninvasive tests (NITs) have been in development for the assessment of NAFLD progression, including blood biomarkers and imaging methods, although the use of NITs varies around the world. The aim of the Japan NASH NIT (JANIT) Forum organized in 2020 is to advance the development of various NITs to assess disease severity and/or response to treatment in NAFLD patients from a scientific perspective through multi-stakeholder dialogue with open innovation, including clinicians with expertise in NAFLD/NASH, companies that develop medical devices and biomarkers, and professionals in the pharmaceutical industry. In addition to conventional NITs, artificial intelligence will soon be deployed in many areas of the NAFLD landscape. To discuss the characteristics of each NIT, we conducted a SWOT (strengths, weaknesses, opportunities, and threats) analysis in this study with the 36 JANIT Forum members (16 physicians and 20 company representatives). Based on this SWOT analysis, the JANIT Forum identified currently available NITs able to accurately select NAFLD patients at high risk of NASH for HCC surveillance/therapeutic intervention and evaluate the effectiveness of therapeutic interventions.
Keywords: NAFLD/NASH, Scoring system, Biomarker, Elastography, Artificial intelligence
Introduction
Nonalcoholic fatty liver disease (NAFLD) is the most common liver disease worldwide, and its progression to nonalcoholic steatohepatitis (NASH) and fibrosis contribute to a growing proportion of the population with cirrhosis and hepatocellular carcinoma (HCC) [1]. Currently, liver biopsy remains the gold standard for diagnosis of NAFLD/NASH, although it has several issues that must be addressed, such as its invasiveness [2] and cost, sampling errors [3], and inter-observer variability. Hepatic fibrosis evaluated by liver histology is independently associated with overall mortality or liver-related events in the US, Europe, and Japan [4, 5]. Therefore, noninvasive tests (NITs) should be required to identify the disease severity of NAFLD.
The Japanese Society of Gastroenterology and the Japanese Society of Hepatology established the Japanese NAFLD/NASH guidelines in 2014 [6, 7] and revised these guidelines in 2020 [8, 9]. The guidelines have received considerable attention and have been widely used in clinical applications, including NITs. They recommend the fibrosis-4 index (FIB-4) and/or the NAFLD fibrosis score (NFS) for classifying high-risk NAFLD patients. As a first step, family physicians or general practitioners at medical check-ups examine liver fibrosis–related markers (FIB-4, NFS, platelet count, enhanced liver fibrosis [ELF] test, Mac-2 binding protein glycosylation isomer [M2BPGi], autotaxin [ATX], type 4 collagen 7S [T4C7S], hyaluronic acid [HA], etc.) in patients with fatty liver for the primary screening. A neo-epitope pro-peptide of type III collagen formation (PRO-C3) is also a useful liver fibrosis biomarker. An algorithm incorporating PRO-C3 has been reported to better identify patients with NAFLD and advanced fibrosis than either the NFS or FIB-4 index alone [10]. However, PRO-C3 testing is not currently covered by insurance in Japan, and insurance coverage is long awaited. Patients with a low risk of advanced hepatic fibrosis (FIB-4 < 1.3 or NFS < − 1.455) do not need further assessment. If a patient is diagnosed with possible advanced hepatic fibrosis (FIB-4 ≥ 1.3, NFS ≥ − 1.455, or platelet count < 200,000/mm3), general practitioners should consult with a hepatologist, who conducts the second step. Hepatologists first check FIB-4 or NFS. If intermediate risk for liver fibrosis (FIB-4 1.3–2.66 or NFS − 1.455–0.674) or severe liver fibrosis (FIB-4 ≥ 2.67 or NFS ≥ 0.675) are suspected, liver biopsy or elastography (ultrasonography, magnetic resonance imaging [MRI]) is recommended. Surveillance for HCC and cardiovascular disease (CVD) are also recommended for patients with possible advanced hepatic fibrosis.
Various NITs are available for NAFLD, including biomarkers and imaging tests, but each NIT has strengths and weaknesses. It is necessary to sort out the strengths and weaknesses of the NITs and combine them or create novel NITs. To achieve this goal, we held a SWOT (strengths, weaknesses, opportunities, and threats) analysis discussion at the Japan NASH NIT (JANIT) Forum, which was organized in 2020. A SWOT analysis is a useful strategy for optimizing resource management in response to changes in the business environment by analyzing external and internal environments in four categories and projecting which organizations and individuals need to make decisions to achieve specific goals. Recently, this method has also been used in the field of gastroenterology [11]. The JANIT Forum aims to advance the development of various NITs to diagnose and assess the response to treatment for NAFLD from a scientific perspective through multi-stakeholder dialogue with open innovation including clinicians with expertise in NAFLD, companies developing medical devices and biomarkers, and professionals in the pharmaceutical industry.
In JANIT Forum, each member was a professional from a healthcare-related company or administrative organization or a healthcare professional involved in the treatment of NAFLD/NASH, who agreed to the purpose of the JANIT Forum and committed themself to discussing the information obtained at the JANIT Forum from a scientific point of view without giving priority to the interests of their own organization. This SWOT analysis discussion was a joint initiative of physicians and professionals from medical device companies, pharmaceutical companies, and diagnostics companies. Although the SWOT framework is most commonly employed in business to analyze the factors that influence a company’s position in the marketplace with a focus on the future, it can also be useful for other domains, such as in the scientific field [12]. The SWOT analysis discussion had 36 participants: 16 physicians from 15 hepatology centers and 20 company representatives from 10 companies. The method of analyzing SWOT was not restricted but freely discussed; it included initial individual SWOT analyses, bringing the results to the group, setting subgroups for various diagnostic methods and creating SWOT in each team, cross-SWOT analysis, selecting key success factors from cross-SWOT analysis, and prioritizing. Our discussion took place primarily online using tools such as Zoom, Microsoft Teams, Facebook, and Slack due to the COVID-19 situation.
Strengths and weaknesses of each NIT
We first presented the strengths and weaknesses of each NIT used in Japan (Table 1). The approval status and price of each NIT are demonstrated in Table 2.
Simple index (scoring system)
-
FIB-4 index
The strengths of the FIB-4 are its simplicity, accuracy, and validation: (i) FIB-4 is based only on the combination of four parameters—age, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and platelets—which are measured as part of the liver blood test [13, 14]. FIB-4 can be easily calculated and is widely available in clinical settings at a low cost. (ii) The diagnostic accuracy of FIB-4 for advanced fibrosis is superior to that of other blood-based NITs, such as NFS, AST to platelet ratio index (APRI), and the body mass index (BMI), AST/ALT ratio, and diabetes (BARD) score [15–20]. In addition, FIB-4 can act as a predictor of incident HCC [21–24], CVD [25, 26], liver-related events [27–29], and mortality. (iii) FIB-4 is the most validated in the prediction of NAFLD with severe liver fibrosis, and some clinical practice guidelines have recommended it as a first triaging tool in clinical practice [8, 30, 31].
A weakness of FIB-4 is that its sensitivity to predict advanced fibrosis is lower in certain populations: (i) Age affects the accuracy of FIB-4, which might lead to overpredicting fibrosis in older adults (> 65 years) [32, 33]. (ii) FIB-4 has shown lower performance in predicting advanced fibrosis in obese NAFLD patients than in non-obese patients [34]. (iii) FIB-4 may less accurately predict fibrosis in NAFLD patients with type 2 diabetes mellitus (T2D) compared to those without T2D [35, 36]. (iv) As FIB-4 was validated in populations with a high prevalence of chronic liver diseases, lower positive predictive values have been reported in low-prevalence populations, such as the general population [30, 37].
-
NFS
NFS is a validated, noninvasive tool for identifying patients whose NAFLD has advanced to liver fibrosis and is based on six available variables: age, BMI, hyperglycemia, platelet count, albumin, and the AST/ALT ratio [38]. A published formula is also available at https://nafldscore.com/.
Its strengths are as follows: i) The NFS variables consist of routine clinical and laboratory data [38]. ii) The diagnostic accuracy of NFS is almost the same as that of FIB-4 [39]. iii) NFS is listed and recommended as a scoring system to screen for advanced liver fibrosis/HCC, alongside FIB-4, in the clinical practice guidelines of Japan [8, 9]. iv) NFS is recommended by the clinical practice guidelines of both the European Association for the Study of the Liver and American Association for the Study of Liver Diseases [30, 31]. (v) NFS is useful in identifying NAFLD/NASH patients with T2D at low or high risk for advanced fibrosis [31]. (vi) NFS is one of the most popular noninvasive blood-based serum tests; therefore, a huge amount of data has been published.
In contrast, the weaknesses of NFS are as follows: (i) Obesity affects the performance of NFS [40, 41]. (ii) The diagnostic accuracy of NFS is not very high compared with other NITs [42]. iii) NFS has reduced specificity in elder patients [32]. (iv) In T2D patients, the NFS tends to be high and difficult to use for exclusion diagnosis [43]. (v) The NFS formula is complicated [38].
-
Hepamet fibrosis scoring (HFS)
Recently, the Hepamet fibrosis scoring (HFS) system was developed based on clinical and laboratory test results, such as age, sex, levels of AST and albumin, homeostatic model assessment score (HOMA), presence of diabetes mellitus, and platelet count. HFS shows greater accuracy than the FIB-4 and NFS scoring systems among European NAFLD patients with advanced fibrosis [17][17]. By contrast, HFS has been reported to have lower diagnostic efficacy for F3–4 than FIB-4 among patients with biopsy-confirmed NAFLD from Asia [45].
Liver-specific fibrosis markers
-
ELF test
The ELF test is a scoring system that diagnoses liver fibrosis and gives prognostic insight into the occurrence of liver-related events. It is calculated from serum values of HA, type III procollagen-N-peptide, and tissue inhibitor of metalloproteinase 1. As with other serum markers, the advantages of the ELF test are that it is minimally invasive and can be performed easily and repeatedly and without the installation of special equipment. The National Institute for Health and Care Excellence guidelines recommend the ELF test for identifying advanced liver fibrosis patients [46]. In Europe, the ELF test has been proposed as one of the patented serum fibrosis markers to be measured after FIB-4 and transient elastography (FibroScan) in the patient selection algorithm [30]. Measuring FIB-4 followed by the ELF test has resulted in an 85% reduction in unnecessary referrals compared with when FIB-4 and ELF test were not used [47]. In Japan, the ELF test has not yet been approved for clinical settings; thus, evidence regarding Japanese patients is limited. However, high diagnostic performance was reported as the areas under the curve (AUCs) of NAFLD fibrosis stages ≥ F2 and ≥ F3 were 0.826 and 0.812, respectively, and the diagnostic accuracy of the ELF test is comparable to that of FibroScan [48].
-
T4C7S
T4C7S is a major component of the lamina densa of the basement membrane. The basement membrane is formed with liver fibrillation, causing the T4C7S concentration in the blood to rise. It is higher in chronic hepatitis and liver cirrhosis patients than in acute hepatitis patients, especially in cases with high inflammatory activity. T4C7S has been used since 1989 and was introduced in the Japanese NAFLD/NASH guidelines in 2014 [6, 7]. The T4C7S assay method has historically been radio immunoassay (RIA) [49], although it recently changed to chemiluminescent enzyme immunoassay (CLEIA). The sensitivity and specificity of CLEIA for the detection of the fibrosis degree of NAFLD patients have been improved compared with RIA [50]. The AUC of T4C7S (CLEIA) for diagnosing liver fibrosis stages ≥ 2 in NAFLD patients was 0.882 and that of RIA was 0.855, making it an important fibrosis marker for early fibrosis. Studies of NAFLD patients with or without T2D, especially in the NAFLD group with T2D, have reported that this marker is superior to other hepatic fibrosis markers [35]. In a report from Shinshu University, the AUCs for fibrosis stages ≥ 3 were 0.87 for all subjects, 0.81 for men, and 0.89 for women [51]. In a report at Yokohama City University, the AUC for fibrosis stages ≥ 2 was 0.83 for both men and women [52]. Insurance fees in Japan for T4C7S are low among other noninvasive markers, including other fibrosis markers and imaging, and can contribute to the healthcare economy. Although T4C7S is widely used in Japan, it is not used in other countries, so its future utilization is expected to grow.
-
M2BPGi
Mac-2 (galectin-3) binding protein (M2BP) is a glycoprotein that has seven potential N-glycosylation sites [53, 54]. M2BP is barely detectable in a normal liver but is strongly detected in hepatocytes from chronic hepatitis type C (CHC) patients as liver fibrosis progresses [55, 56]. In addition, the structure of M2BP glycans has been reported to be markedly altered by fibrosis progression in the liver [57]. M2BPGi is a serum liver fibrosis biomarker and a glycosylation isomer that is recognized by Wisteria floribunda lectin (also known as WFA[ +]-M2BP) [57]. This marker is a useful predictor of NAFLD at fibrosis stages ≥ 2 and ≥ 3 [58], is not affected by age, and can be judged by a single cutoff point [59]. In addition, M2BPGi can differentiate patients at high risk for severe fibrosis from a healthy control group [60], and it may be a predictor of hepatocarcinogenesis, though further studies are required [61]. The M2BPGi clinical test is reimbursable in Japan, but limited data are available in other Asian-Pacific countries as highlighted in the 2016 Asian Pacific Association for the Study of the Liver consensus guidelines. [62]
Because M2BPGi was identified and developed as a fibrosis marker from the serum of patients with CHC [57], its behavior differs based on the level of fibrosis progression against the background of other etiologies. Therefore, cutoffs for different etiologies should be established [63]. Also, the pathophysiological mechanism of M2BPGi is unclear [61]. M2BPGi is a dedicated reagent for the HISCL system (Sysmex Co., Hyogo, Japan) and is currently registered only in Asia.
-
ATX
ATX is a secreted enzyme that produces lysophosphatidate from extracellular lysophosphatidylcholine. Metabolized by liver sinusoidal endothelial cells, ATX is considered to be associated with liver damage. Serum ATX is a useful marker for diagnosing liver fibrosis in patients with NAFLD [51, 52]. As ATX levels are less affected by inflammation, they can be used to detect liver fibrosis at an early stage in Japanese patients with NAFLD [52]. Fujimori et al. reported an AUC of 0.75 for the efficacy of serum ATX in diagnosing liver fibrosis stages ≥ 3 for all patients with NAFLD (AUC 0.74 for male patients and 0.78 for female patients) [51]. Honda et al. also reported AUCs of 0.75 and 0.81 for the efficacy of serum ATX in diagnosing liver fibrosis stages ≥ 2 in male and female NAFLD patients, respectively [52]. However, it should be noted that the reference values of ATX are different between men and women, higher values are observed in pregnant women and patients with follicular lymphoma, and ATX levels are not generally measured in Europe or the US for diagnostic purposes.
-
HA
HA is an acidic mucopolysaccharide obtained by polymerizing D-glucuronic acid and N-acetyl-D-glucosamine, which are mainly produced in fibroblasts and synovial cells. Due to the decrease in HA receptors with liver fibrosis progression, serum HA levels become high. HA has long been known to be a useful marker of liver fibrosis. Loomba et al. reported an AUC of 0.812 for the efficacy of serum HA in differentiating between liver fibrosis stages 0–2 and 3–4 in patients with NAFLD in the US [64]. Fujimori et al. reported an AUC of 0.82 for the efficacy of serum HA in diagnosing liver fibrosis stages ≥ 3 for Japanese patients with NAFLD [51]. It has also been reported that the combination of FIB-4 and serum HA is a better marker than FIB-4 alone with respect to predicting the occurrence of cirrhosis and HCC in patients with diabetes [65]. Furthermore, serum HA levels can be used to predict hepatic fibrosis in pediatric patients with NAFLD [66]. However, it should be noted that serum HA levels are elevated in patients with renal dysfunction, joint disorders (e.g., rheumatoid arthritis, osteoarthritis), scleroderma, dermatomyositis, vasculitis, and malignant cancers (e.g., malignant lymphoma, breast cancer).
-
Cytokeratin-18 fragment
Active caspases in NASH specimens have been reported to be strongly correlated with hepatocyte apoptosis and NASH progression [67]. Hepatocyte ballooning, a form of hepatocyte apoptosis, is a prominent pathological feature of NASH and an important component of the NAFLD activity score (NAS). Cytokeratin 18 (CK18), the major intermediate filament protein in the liver, is cleaved by caspases during hepatocyte apoptosis. Cleaved CK18 shed into the blood has been reported as a biomarker of hepatocyte apoptosis [68]. Feldstein et al. first demonstrated that circulating levels of CK18 fragment (CK18-F/M30) were a predictor of NASH in NAFLD patients [69]. Since then, the usefulness of this marker in differentiating between simple steatosis and NASH has been demonstrated in several clinical studies [70, 71].
However, subsequent studies have revealed its limited sensitivity at the individual level and concluded that it is inadequate as a screening test for diagnosis and staging of NASH [72, 73]. Even still, the involvement of CK18 in the specific disease pathway of NASH suggests the potential for CK18-F to be used in combination with other NITs. Recent studies have shown that the accuracy of NASH diagnosis is improved by the combination of CK18-F with other biomarkers (e.g., hyaluronic acid) or scoring systems (e.g., FIB-4) [74–76]. It is noteworthy that we can more easily diagnose NASH in combination with CK18-F even in cases with a low FIB-4, NFS score, or TE value [75–77], suggesting its ability to rule in NASH among patients rated at low or intermediate risk by clinically established NITs.
The CK18-M30 enzyme-linked immunosorbent assay (ELISA) kit, commercially available for research use only, has not been readily translatable to clinical settings due to variations in disease marker cutoff values and diagnostic performance issues [31]. Based on data showing that adding CK18-F to fibrosis markers can be useful for screening NAFLD patients for NASH, an ELISA kit for CK18-F measurement was finally approved as an in vitro diagnostic reagent in Japan in 2021. It is expected that the significance of this marker will become clear as this reagent becomes widely used in clinical settings in the future.
-
Elastography
As of recently, we can use various liver stiffness measurement (LSM) methods that are about to replace liver biopsy. Vibration-controlled transient elastography (VCTE, or FibroScan), point shear wave elastography (p-SWE), 2-dimensional SWE (2D-SWE), and magnetic resonance elastography (MRE) are available in Japan. We summarized the respective characteristics, advantages, and limitations of the four available elastography techniques for liver fibrosis staging (Table 3). In addition, applications are being developed by each manufacturer as a quantitative evaluation method for hepatic steatosis. They have been newly reimbursed since 2022. There are methods for measuring the attenuation coefficient—e.g., the controlled attenuation parameter (CAP; Echosens), ultrasound-derived fat fraction (Siemens Healthcare), attenuation imaging (Canon Medical Systems), attenuation coefficient measurement (Fujifilm), and ultrasound-guided attenuation parameter (GE Healthcare)—and some vendors add the backscatter coefficient to measure it.
-
VCTE
VCTE (FibroScan) is an NIT that has been widely validated around the world since it was launched in Europe in 2003. In Japan, it was launched and reimbursed in October 2011. On April 16, 2013, Echosens announced that its FibroScan device received 510(k) clearance from the US Food and Drug Administration (FDA). For NAFLD, the utility of LSM by VCTE to assess liver fibrosis was first validated in Japan in 2008 by Yoneda et al. [78]. A recent meta-analysis [79] (VCTE: 53 papers) reported that VCTE has excellent diagnostic performance with an AUC of 0.82 for fibrosis stages ≥ 1, 0.83 for stages ≥ 2, 0.85 for stages ≥ 3, and 0.89 for stage 4. As a quantitative steatosis assessment method, CAP was developed and installed into FibroScan to measure ultrasound attenuation and has been globally validated since 2010 [80, 81].
VCTE is a safe and simple method that also can be used with pregnant patients [82, 83]. The use of VCTE is limited in patients with ascites and narrow intercostals [84, 85]. For obese patients, VCTE can be conducted using an XL probe, but this is difficult in patients with severe obesity [86, 87]. SmartExam, which has recently launched, is expected to extend VCTE usage among severely obese patients [88] and improve the reliability and precision of CAP with reduced variability by the continuous CAP method [89].
Reported confounding factors for LSM by VCTE to assess fibrosis include not only obesity [86, 87, 90–92] but also inflammation [92], food intake s, biliary obstruction [93], heart failure [94], amyloidosis [95], solitary liver lesions [96], and portal hypertension (PH) [97]. Elevated LSM by PH is significantly correlated with the hepatic venous pressure gradient in patients with advanced chronic liver disease/compensated cirrhosis and has been applied to predict the presence of esophageal varices [97]. Spleen stiffness measurement (SSM) by VCTE is reported to be more accurate for prediction than LSM by VCTE [98] and a more specific model for SSM (FibroScan630Expert) has recently been developed [99]. Operator experience might influence the diagnostic performance of VCTE as well [100].
FibroScan-AST (FAST) score which combined LSM by VCTE, CAP for a quantitative steatosis assessment method, and AST increases the diagnostic accuracy to identify active fibrotic NASH patients which is defined NASH with significant fibrosis (stages ≥ 2) and NAS ≥ 4 [101, 102]. In pharmaceutical trials for NASH drug pipelines, LSM and CAP have been referred to as alternative methods for liver biopsy [103], and LSM by VCTE, CAP and FAST score has been adopted in many trials [104–108].
-
p-SWE/2D-SWE
Ultrasound SWE uses acoustic radiation force impulses (ARFI) or mechanical impulse to stimulate liver tissue to produce shear waves that propagate through the liver. The shear wave velocity (SWV) increases with the severity of fibrosis. The ARFI method uses both p-SWE, which measures the region of interest (ROI) by setting one point [109], and 2D-SWE, which measures the SWV by color mapping [110]. In other words, p-SWE generates displacement at a single focal point, whereas 2D-SWE is a dynamic displacement method that can generate stress in multiple focal zones with the same ARFI technique. In Japan, p-SWE and 2D-SWE are approved for the examination of patients with cirrhosis or suspected cirrhosis and reimbursed in October 2016. Both p-SWE and 2D-SWE can be performed at the same time as ultrasound imaging, which is an advantage in that it can be easily introduced at a facility. In the mechanical impulse method, VCTE is recommended in Europe to exclude and diagnose compensated advanced chronic liver disease, which is defined as fibrosis stages ≥ 3 [111]. p-SWE and 2D-SWE may perform similarly to VCTE, and direct comparisons of p-SWE and 2D-SWE with VCTE have been reported [112]. Similar to VCTE, p-SWE and 2D-SWE have been reported to be useful for evaluating hepatic fibrosis in NAFLD [113, 114]. In addition, 2D-SWE and MRE have demonstrated excellent accuracy in diagnosing liver fibrosis in NAFLD [114] and alcoholic liver disease [113]. Furthermore, 2D-SWE has been used in conjunction with the FIB-4 index to assess hepatic fibrosis in NAFLD, metabolic-associated fatty liver disease (MAFLD), and health checkup examinees [113, 115, 116]. The measurement value of chronic liver disease is different by manufacturer and model, so attention to this is necessary [30]. Confounders other than stiffness include non-fasting conditions, elevated aminotransferases, congestive heart failure, and extrahepatic cholestasis.
-
MRE/proton density fat fraction
MRE is an MRI-based technique for the quantitative imaging of liver stiffness [117]. Liver stiffness maps can be obtained with one breath-hold and can be easily included in routine liver MRI protocols. MRE has been shown to be the most accurate imaging tool to assess liver fibrosis [118] in a geographically distinct cohort [119], even in the early stages [120] and in patients with ascites or obesity [121]. Because of this variety of evidence, the FDA approved MRE in 2009, and MRE has been newly reimbursed since 2022 in Japan. Optimal MRE thresholds for the detection of liver fibrosis stages are 2.61 kPa (stages ≥ 1), 2.97 kPa (stages ≥ 2), 3.62 kPa (stages ≥ 3), and 4.69 kPa (stages ≥ 4) [122]. Moreover, MRE can visualize whole-liver stiffness, resulting in reduced sampling error [123], and be readily combined with other quantitative maps, such as proton density fat fraction (PDFF) and R2* [124]. However, MRE also has weaknesses—it is inaccessible, costly, and time-consuming compared with ultrasound methods. Inter-observer bias in ROI placement may be one of the most critical issues for MRE quantification, but an automatic ROI-drawing tool using artificial intelligence (AI) [125] is expected in the near future.
PDFF is also an important MRI-based biomarker to quantitatively measure hepatic fat accumulation, which correlates with the histologically determined steatosis grade [126]. It exploits the chemical shift–encoded MRI method to accurately quantify the relative amount of water and fat signal and calculates the ratio of the density of protons from triglycerides and the total density of protons from both mobile triglycerides and water [127]. PDFF is expressed as an absolute percentage (%), and its thresholds for the detection of liver steatosis grades are: 5.2% (grades ≥ 1), 11.3% (grades ≥ 2), and 17.1% (grades ≥ 3) [118]. Combining MRE with PDFF has been shown to improve the diagnosis of NASH [128], and the accuracy of these MRI-based imaging biomarkers can contribute to evaluating the efficacy of clinical trials [129].
AI
Background
Table 4.
Opportunities and Threats of NITs for NAFLD
| PEST | Opportunities (O) | Threats (T) |
|---|---|---|
| Politics |
The MHLW has attempted to increase the rate of acceptance of Specific Health Checkups and promote regional coordination of local clinics and hospitals There is a need for NITs that can be easily used by primary care doctors to correctly identify people with advanced liver fibrosis |
Authorities might consider NITs insufficient as a complete substitute for liver biopsy due to the lack of evidence Platelet count is not available for health checkup examinees covered by National Health Insurance, meaning some scores of NITs are not calculated |
| Economics |
The MHLW attempts to reduce total health expenditures to maintain the universal insurance system The development of an inexpensive NIT using blood samples for correct prognosis of NAFLD is expected |
Current NITs may not be used any longer if cheap and easy-to-use NITs are developed in the future Facilities equipped with elastography are limited, especially in rural areas with few patients and limited budgets Overall medical costs will soar with frequent use of expensive NITs for NAFLD screening |
| Society |
The number of new subscribers for health apps is increasing Simple and highly accurate NITs are required for non-specialist and primary care doctors |
Physicians are less motivated to use NITs for reasons that include the lack of therapeutic agents for NAFLD Insufficient cooperation between hepatologists, diabetologists, cardiologists, and primary care clinicians will make the use of NITs challenging Physicians cannot use NITs measured at other institutes for same-day diagnosis If different NITs are established by region or country, it will be difficult to find a consensus between regions |
| Technology |
With the spread of 5G networks, advanced imaging technology and online medical care are more accessible Doctors and patients need NITs that allow simple visualization and easily understanding of NAFLD status |
Physicians may stop using current NITs if novel NITs with higher diagnostic performance or NITs without blood sampling (e.g., wearable devices) are developed in the future |
MHLW, Ministry of Health, Labour and Welfare; NIT, noninvasive therapy; NAFLD, nonalcoholic fatty liver disease
Table 1.
Strengths and Weaknesses of NITs for NAFLD available in Japan
| Strengths | Weaknesses | ||
|---|---|---|---|
| Scoring system | FIB-4 |
Easy calculation with low cost High negative predictive value for advanced fibrosis Possible predictor of incident HCC, CVD, and mortality Widely validated score recommended as first triaging tool for clinical practice Rich evidence |
Low performance in older patients (> 65 years) Lower performance for advanced fibrosis in obese NAFLD patients than for nonobese NAFLD patients Unlikely to be accurate for fibrosis in NAFLD patients with T2D compared with those without T2D Lower positive predictive values in low-prevalence populations, such as the general population Existence of indeterminate group |
| NFS |
Easy utilization with clinical and laboratory data Recommended in the clinical practice guidelines of both EASL and AASLD Identification of NAFLD/NASH patients with T2D at low or high risk of advanced fibrosis Rich evidence |
Low performance in obese patients Lower diagnostic accuracy than other NITs Low performance in older patients Complex formula Existence of indeterminate group |
|
| HFS |
Easy utilization with clinical and laboratory data Possible predictor of mortality in European populations |
Less evidence Lower diagnostic efficacy than FIB-4 index in Asian populations Not well known in Japan |
|
| Biomarker | T4C7S |
Well measured in Japan Reflect fibrosis formation in the liver Low insurance fee |
Not generally measured outside of Japan due to its low awareness |
| ATX |
Less affected by inflammation Can be used to detect liver fibrosis at an early stage in Japanese patients with NAFLD |
Difference between men and women Not generally measured outside of Japan |
|
| HA |
Well known to be a useful marker of liver fibrosis Useful in pediatric patients with NAFLD |
Elevation of serum HA level in patients with renal dysfunction, joint disorders, and malignant cancers | |
| CK-18F (M30) |
Predictor of hepatocyte apoptosis Recently approved as NASH diagnosis marker in Japan |
Less evidence Cutoff values not established for the diagnosis of NASH |
|
| M2BPGi |
Better predictor of fibrosis stages ≥ 2 and ≥ 3 Single cutoff value independent of age High performance of differentiating high-risk patients with advanced fibrosis from the general population Possible predictor of hepatocarcinogenesis |
Different cutoffs for different etiologies Unclear mechanism of action Dedicated equipment required (HISCL Series system by Sysmex Co.) Not a quantitative assay |
|
| ELF test |
Easy to use (repeatable, minimally invasive, no equipment installation or special training required) Recommended in Europe as a patented fibrosis marker Approved by the FDA as a NASH prognosis marker (used to identify high-risk NASH patients) |
Not approved for clinical use in Japan Limited evidence in Japanese patients Dedicated equipment is required for in-hospital diagnosis (Atellica or Centar series by Siemens Healthcare Diagnostics Co.) |
|
| Elastography | VCTE |
Excellent diagnostic performance for the assessment of liver fibrosis Widely validated method around the world Easy to learn Quantitative assessment of steatosis using CAP Assessment of progressive NASH using FAST score |
Limited in patients with ascites, narrow intercostal space, and severe obesity Confounders other than stiffness include nonfasting conditions, elevated aminotransferases, congestive heart failure, and extrahepatic cholestasis |
| p-/2D-SWE |
Approved for the examination of patients with cirrhosis or suspected cirrhosis in Japan Both p-SWE and 2D-SWE may be conducted concurrently with ultrasound imaging |
Difference by manufacturer and model Factors other than stiffness include nonfasting conditions, elevated aminotransferases, congestive heart failure, and extrahepatic cholestasis Not an evaluation of the liver as a whole |
|
| MRE |
Best Accuracy for the assessment of liver fibrosis degree Good visibility of the whole liver Can be combined with fat (PDFF), corrected T1, and iron quantification (R2*) Can be applied to patients with ascites or obesity |
(Compared to ultrasound) Inter-observer variability of ROI placement Inaccessibility Costly and time consuming Artifacts due to iron overload |
|
| Others | AI |
Numerous analyses are possible using easily available information Reductions in cost, time, and human resources High accuracy |
Black box nature Potential for leaks of private information Need for good training data |
NIT, noninvasive test; NAFLD, nonalcoholic fatty liver disease; T2D, type 2 diabetes mellitus; EASL, European Association for the Study of the Liver; AASLD, American Association for the Study of Liver Diseases; FIB-4, Fibrosis-4; NFS, NAFLD fibrosis score; HFS, Hepamet fibrosis score; HCC, hepatocellular carcinoma; T4C7S, type 4 collagen 7S; ATX, autotaxin; HA, hyaluronic acid; CK-18F, cytokeratin-18 fragment; M2BPGi, Mac-2 binding protein glycosylation isomer; ELF, enhanced liver fibrosis; VCTE, vibration controlled transient elastography; CAP, controlled attenuation parameter; SWE, shear wave elastography; p-SWE, point SWE; 2D-SWE, 2-dimensional SWE; MRE, magnetic resonance elastography; PDFF, proton density fat fraction; AI, artificial intelligence; ROI, region of interest; T2D, type 2 diabetes
Table 2.
Approval status in USA, EU, and Japan, and price of each NIT in Japan
| NITs | Registration/Approval | Status in Japan | ||||
|---|---|---|---|---|---|---|
| USA | EU | Japan | Reimbursement | Fee (JPY) | ||
| Scoring system | FIB-4 | N/A | N/A | N/A | N/A | N/A |
| NFS | N/A | N/A | N/A | N/A | N/A | |
| Liver-specific fibrosis markers | ELF test | ○ | ○ | - | - | - |
| T4C7S | - | - | ○ | ○ | 1,480 | |
| M2BPGi | - | - | ○ | ○ | 1,940 | |
| ATX | - | - | ○ | ○ | 1,940 | |
| HA | - | ○ | ○ | ○ | 1,790 | |
| Apoptosis marker | CK-18F (M30) | - | - | ○ | - | - |
| Liver stiffness measurement | VCTE | ○ | ○* | ○ | ○ | 2,000 |
| p-/2D-SWE | ○ | ○ | ○ | ○ | 2,000 | |
| MRE | ○ | ○ | ○ | ○ | 6,000 | |
| Liver fat measurement | Attenuation Coefficient (CAP, etc.) | ○ | ○* | ○ | ○ | 2,000 |
| PDFF | ○ | ○ | ○ | - | - | |
(As of April 2022)
Annotation. ○ indicates “Available,”—indicates “Not available.”
Registration/Approval means FDA approval in the USA, CE marking in the EU, and Ministry of Health, Labour and Welfare or Registered Certification Bodies approval in Japan
*FibroScan, which measures LSM by VCTE and CAP, is a CE-marked class IIa ultrasound diagnostic medical device (hepatic and/or splenic applications)
Table 3.
Respective characteristics, advantages, and limitations of the 4 available elastography techniques for liver fibrosis staging
| Imaging | Range (units) | Steatosis grading | Quality criteria | Confounders | |||
|---|---|---|---|---|---|---|---|
| Inflammation | Obesity | Others | |||||
| VCTE | 1.5 ~ 75.0 | kPa | Yes (CAP) | IQR/M ≤ 30% | + | + |
Food intake Biliary obstruction Heart failure Amyloidosis Solitary liver lesions Portal hypertension Operator experience |
| p-/2D-SWE | 0.5 ~ 6.5 | m/s | Yes (UDFF, ATI, ATT, UGAP) | IQR/M ≤ 15% | + | + |
Food intake Obstructive cholestasis Liver congestion Acute hepatitis Infiltrative liver disease |
| MRE | 0 ~ 20 | kPa | Yes (PDFF) | Based on QIBA consensus statement | + | + |
Hemochromatosis/ Hemosiderosis Claustrophobia Metal implant |
QIBA, Quantitative Imaging Biomarkers Alliance; UDFF, ultrasound-derived fat fraction (Siemens Healthcare); ATI, attenuation imaging (Canon Medical Systems); ATT, attenuation measurement method (Fujifilm); UGAP, ultrasound-guided attenuation parameter (GE Healthcare)
AI is going to be deployed in many areas of the NAFLD landscape [130]. The origin of AI for healthcare was developed in 1954 [131], and there have been several booms and chasms since then [132]. Information and communication technology has been making drastic changes since 2000 [133]. Although AI needs big data and faster computers, the past weaknesses and limitations were resolved by an advance in the environment around AI models [134]. Currently, the need for AI in NAFLD-related diagnostics is expanding.
-
(2)
Strengths of AI in the NAFLD/NASH area
The overall strengths of AI include (i) the possibility of performing numerous analyses using easily available information; (ii) reductions in cost, time, and human resource needs; and (iii) high accuracy.
Although NITs are expected to identify patients with advanced NAFLD, AI can expand the possible analyses [135], such as comparing healthy patients with patients diagnosed with NAFLD subjects or comparing NAFLD patients with comorbidities to those without comorbidities. Thus, AI has the potential to both identify NAFLD cases and assess NASH severity, including comorbidities such as HCC or cardiovascular disease.
Various information can be used to obtain an “AI diagnosis,” including the electronic health record (EHR), laboratory data, and imaging examinations. However, assessments of these data have been largely researcher-dependent. In addition, processing large amounts of data can cause physicians to be overworked, leading to human error [136, 137]. By contrast, AI enables us to make highly reproducible diagnoses without heavy workloads, leading to low intra- and inter-rater variability. The EHR is rich in information for the diagnosis of NAFLD. Fialoke et al. and Docherty et al. developed AI models isolating clinically meaningful values from the EHR under HIPAA compliance [138, 139]. A combination of AI and EHR data has been used not only for the diagnosis of NASH but also for the assessment of drugs used for NASH treatment. In addition, many AI models use clinical parameters, including physical examinations and laboratory data [140–142]. In general, radiological diagnosis for NASH entails heterogenous image reconstruction, segmentation, and quantification. In addition, shape, texture, volume, diffusion, and other parameters must be processed. AI automatically processes a large amount of digital data and increases the accuracy of diagnosis. Mojtahed et al. showed that Hepatica (Perspectrum, UK), a deep-learning system, could shorten the time required to assess the detailed hepatic volume and hepatic condition while maintaining high reproducibility compared with a conventional method. Conventional ultrasonography is a typical example of observer-dependent examination. AI can automatically classify ultrasound images [143] and SWE images [144] to reduce manual workload.
Although early-stage “AI diagnosis” was not always accurate, current AI models provide amazing results. Zamanian et al. reported that the AUC for AI-equipped ultrasonography was 0.9999 for diagnosing NAFLD [145]. Okanoue et al. developed AI models using physical examinations and common laboratory data [146, 147]. The AUC was 0.995 when AI was applied to discriminate NAFLD from non-NAFLD. In addition, the AUC was 0.960 for the discrimination between NASH with and without fibrosis. Furthermore, the AI model can discriminate fibrosis staging with high accuracy.
-
(3)
Weakness of AI in NAFLD/NASH areas
AI has some weaknesses, including (i) its black-box nature, (ii) the potential for leaks of private information, and (iii) the need for good teachers. First, it is difficult to know the decision-making process of an AI algorithm, which is an eternal weakness of AI. Second, it is crucial to protect privacy because private information in healthcare systems is sensitive and confidential. Although AI and the digital data of patients are inseparable, the FDA ensures that federal standards are maintained when the EHR is used for AI analyses [148]. Compliance with regulations can be the biggest barrier for regulatory approval. In addition, privacy should be protected from outsiders. Several Japanese hospitals have been attacked by hackers, resulting in potential breaches of data. To better safeguard these files, the Cyber Security Framework was issued by the National Institute of Standards and Technology in 2014. In addition, the Cyber Risk Intelligence Cross-Sector Forum was founded to execute cybersecurity in Japan. These systems now collaborate with each other and function globally to reduce weaknesses in data privacy. When information for AI analyses is restricted, privacy issues are reduced. Third, AI needs good-quality test data. Most test data have been based on liver biopsy, which has sampling variability [149] and other limitations [150]. The histologic scoring systems are semiquantitative with marked inter- and intra-observer variation. Thus, in this case, experienced teachers are not always good teachers. We should grow good teachers by using digital pathology and other clinical parameters, including imaging examinations.
Opportunities and threats
Next, we analyzed the opportunities and threats in NITs based on the PEST (Politics, Economy, Society, Technology) perspective (Table 4) [151]. In Table 4, we discuss the opportunities and threats for all NITs.
-
Opportunities for NITs
The Japanese Ministry of Health, Labour and Welfare (MHLW) has attempted to increase the rate of acceptance for Specific Health Checkups and promote regional coordination among local clinics and hospitals. The MHLW also attempts to reduce total health expenditures to maintain the universal insurance system. Therefore, the increasing development of NITs for NAFLD patients in Japan may be carefully considered. In addition, the number of new health app subscribers is increasing, which may result in increased NAFLD awareness, especially for the young to middle-aged population. Additionally, early diagnostic imaging for NAFLD is required to increase NAFLD awareness among non-specialist and primary care doctors. Furthermore, with the spread of 5G networks, advanced imaging technology and online medical care for NAFLD may be more accessible. Based on these opportunities for NITs, the following actions will be needed.
To calculate the FIB-4 and NFS indexes for their primary screening described in the Japanese NAFLD/NASH guidelines [8, 9], attempts are required to enable non-specialist doctors to measure platelet counts and albumin for such calculations and enable hospitals and institutes to automatically calculate the indexes. Moreover, to correctly capture NAFLD and NASH status, we must ask MHLW to include measurements such as platelet count and albumin as diagnostic items based on the Industrial Safety and Health Act. In addition, new indexes calculated on the basis of measurements from current medical checkup items should be investigated.
After patients diagnosed with liver fibrosis by screening are referred to a specialist, a simple imaging technique is required to provide clear diagnostic information. In particular, after new agents that provide indications for NAFLD are approved, a further simple imaging technique is expected such that non-specialist and primary care doctors can make diagnoses. Furthermore, making people aware of not only a liver disease itself but also the development of liver fibrosis is clinically important. Increasing awareness of imaging techniques that provide visually understandable information and health apps that allow users to check liver fibrosis progression from noninvasive indicators would be effective.
Threats of NITs
Currently, liver biopsy remains the gold standard for diagnosing NAFLD/NASH. In many clinical trials conducted on NASH patients, the primary outcome evaluation has been based on liver biopsy. MRE has been used instead of liver biopsy in some recent clinical trials, and the use of NITs is being considered for defining the trial population, assessing early treatment responses, and evaluating outcomes [152]. However, some NITs are expensive, and their frequent use will increase overall medical costs. These issues would make it difficult to use NITs for the assessment of NAFLD progression in patients.
To reduce the risk of death and poor prognosis due to NAFLD and reduce the burden on patients in the future, there is an urgent need to establish NITs that are highly diagnostic, inexpensive, easy-to-use, and compatible with global activities. To achieve this goal, we must understand the strengths and weaknesses of each NIT, develop combinations of NITs that complement each other, and accumulate evidence. Furthermore, a continuous educational campaign is needed so that patients have a high awareness of NASH and physicians understand the importance of identifying patients at high risk of NASH by using NITs.
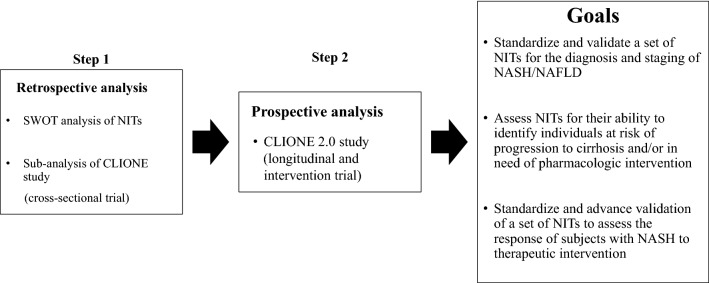
Future perspective (Fig. 1)
Fig. 1.
The JANIT Forum project plan Based on this SWOT analysis of NITs, a sub-analysis of the CLIONE study (cross-sectional trial in Japan) is underway. The next step of the JANIT Forum is the prospective CLIONE 2.0 study (longitudinal and intervention trial). Our goal is to establish standardized NITs for the assessment of NAFLD, which will enable us to diagnose disease severity and assess treatment response in NAFLD patients
Recently, our study group (Japan Study Group of NAFLD) disseminated data from the CLIONE study of a large cohort of Asian NAFLD patients [5]. We will perform sub-analyses of the CLIONE study to establish NITs in collaboration with companies in the JANIT Forum under a nondisclosure agreement for the next 3 years. We are currently planning the CLIONE 2.0 study for longitudinal and intervention trials. The JANIT Forum will not only validate established NITs but also explore novel NITs and/or combinations of them under the guidance of statistical experts. Innovative NITs will facilitate the selection of the right patients for clinical trials and improve the identification of patients at risk for NASH (fibrosis stages ≥ 2 and NAS ≥ 4) and access to care in clinical settings. The JANIT Forum will continue to educate patient associations and the public about NITs to expand public knowledge of NASH/NAFLD.
Conclusion
Based on this SWOT analysis, the JANIT Forum aims to develop effective NITs to select patients in the high-risk group of NAFLD patients (those with a high NAS and advanced fibrosis) for HCC surveillance/therapeutic intervention and to determine the effectiveness of therapeutic interventions. The developed NITs will be beneficial for the increasing number of patients with NAFLD as it will allow us to determine the severity of NAFLD and the efficacy of treatment without resorting to liver biopsy.
Acknowledgements
We thank Kenichi Itou (Sysmex Corporation) for attending the SWOT analysis discussion. We also thank BioScience Writers (https://www.biosciencewriters.com/EditingAccess.aspx) for English language editing.
Atsushi Nakajima—Representative of JANIT Forum.
Abbreviations
- NAFLD
Nonalcoholic fatty liver disease
- NASH
Nonalcoholic steatohepatitis
- HCC
Hepatocellular carcinoma
- NIT
Noninvasive test
- FIB-4
Fibrosis-4 index
- NFS
NAFLD fibrosis score
- ELF test
Enhanced liver fibrosis test
- M2BPGi
Mac-2 binding protein glycosylation isomer
- ATX
Autotaxin
- T4C7S
Type IV collagen 7S
- HA
Hyaluronic acid
- MRI
Magnetic resonance imaging
- CVD
Cardiovascular disease
- SWOT
Strengths, weaknesses, opportunities, and threats
- JANIT
Japan NASH NIT
- AST
Aspartate aminotransferase
- ALT
Alanine aminotransferase
- APRI
AST to platelet ratio index
- BMI
Body mass index
- BARD
BMI, AST/ALT ratio, diabetes
- T2D
Type 2 diabetes mellitus
- AUC
Area under the curve
- RIA
Radio immunoassay
- CLEIA
Chemiluminescent enzyme immunoassay
- M2BP
Mac-2 (galectin-3) binding protein
- CHC
Chronic hepatitis type C
- CK18-F
Cytokeratin 18 fragment
- ELISA
Enzyme-linked immunosorbent assay
- LSM
Liver stiffness measurement
- VCTE
Vibration-controlled transient elastography
- p-SWE
Point shear wave elastography
- 2D-SWE
2-Dimensional SWE
- MRE
MR elastography
- CAP
Controlled attenuation parameter
- FDA
US Food and Drug Administration
- PH
Portal hypertension
- SSM
Spleen stiffness measurement
- FAST
FibroScan-AST
- ARFI
Acoustic radiation force impulses
- SWV
Shear wave velocity
- ROI
Region of interest
- PDFF
Proton density fat fraction
- AI
Artificial intelligence
- EHR
Electronic health record
- PEST
Politics, Economy, Society, Technology
Author contributions
YK, TN, SI, KH, YS, YO, AN, NY, SM, KM, TY, TH, AY, IK, HF, MK, AU, YK, KF, TM: Drafting the manuscript. YS: Conceptualization. YS: Funding acquisition. YK, TN, SI, KH, YS, KM, TY, AY, IK, AU, HF, YY, MK, HH, AM, HH, HT, KT, TI, HT, MY, DWJ, YS: Review and editing of the manuscript. YK, MY, DWJ, YS, TO, AN: Supervision.
Funding
This research was supported by Japan Agency for Medical Research and Development (AMED) under Grant Number JP22fk0210090.
Conflict of interests
TN and TH are employees of Nippon Boehringer Ingelheim Co., Ltd. SI and SM are employees of Integral Corporation. YK and KH are employees of Novartis Pharma KK. YS and TM are employees of the Institute of Immunology Co., Ltd. YO and KF are employees of Fujirebio Inc. AN is an employee of GE Healthcare Japan. NY is an employee of Siemens Healthcare KK. TY and AY are employees of Kowa Company, Ltd. IK and AU are employees of EA Pharma Co., Ltd. HF is an employee of Siemens Healthcare Diagnostics KK. MK is an employee of H.U. Frontier, Inc.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yoshihiro Kamada, Email: ykamada@sahs.med.osaka-u.ac.jp.
Takahiro Nakamura, Email: takahiro.nakamura@boehringer-ingelheim.com.
Satoko Isobe, Email: s.isobe@integralcorp.jp.
Kumiko Hosono, Email: kumiko.hosono@novartis.com.
Yukiko Suama, Email: ysuama@tokumen.co.jp.
Yukie Ohtakaki, Email: yukie.ohtakaki@hugp.com.
Arihito Nauchi, Email: arihito.nauchi@ge.com.
Naoto Yasuda, Email: naoto.yasuda@siemens-healthineers.com.
Soh Mitsuta, Email: s.mitsuta@integralcorp.jp.
Kouichi Miura, Email: miura385@jichi.ac.jp.
Takuma Yamamoto, Email: takuma-yamamoto@kowa.co.jp.
Tatsunori Hosono, Email: tatsunori.hosono@boehringer-ingelheim.com.
Akihiro Yoshida, Email: ak-yoshida@kowa.co.jp.
Ippei Kawanishi, Email: ippei_kawanishi@eapharma.co.jp.
Hideaki Fukushima, Email: hideaki.fukushima@siemens-healthineers.com.
Masao Kinoshita, Email: Masao.kinoshita@hugp.com.
Atsushi Umeda, Email: atsushi_umeda@eapharma.co.jp.
Yuichi Kinoshita, Email: yuichi.kinoshita@novartis.com.
Kana Fukami, Email: kana.fukami@hugp.com.
Toshio Miyawaki, Email: tmiyawaki@tokumen.co.jp.
Hideki Fujii, Email: fujiirola@yahoo.co.jp.
Yuichi Yoshida, Email: yu1yoshida@gmail.com.
Miwa Kawanaka, Email: m.kawanaka@med.kawasaki-m.ac.jp.
Hideyuki Hyogo, Email: hidehyogo@ae.auone-net.jp.
Asahiro Morishita, Email: asahiro@med.kagawa-u.ac.jp.
Hideki Hayashi, Email: hide-hayashi@umin.ac.jp.
Hiroshi Tobita, Email: ht1020@med.shimane-u.ac.jp.
Kengo Tomita, Email: kengo@ndmc.ac.jp.
Tadashi Ikegami, Email: ikegamit@tokyo-med.ac.jp.
Hirokazu Takahashi, Email: takahas2@cc.saga-u.ac.jp.
Masato Yoneda, Email: yoneda@yokohama-cu.ac.jp.
Dae Won Jun, Email: gongori1004@gmail.com.
Yoshio Sumida, Email: sumida19701106@yahoo.co.jp.
Takeshi Okanoue, Email: okanoue@suita.saiseikai.or.jp.
Atsushi Nakajima, Email: nakajima-tky@umin.ac.jp.
References
- 1.Estes C, Razavi H, Loomba R, et al. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67:123–133. doi: 10.1002/hep.29466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thomaides-Brears HB, Alkhouri N, Allende D, et al. Incidence of complications from percutaneous biopsy in chronic liver disease: a systematic review and meta-analysis. Digest Dis Scie. 2021;45:23. doi: 10.1007/s10620-021-07089-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou JH, Cai JJ, She ZG, et al. Noninvasive evaluation of nonalcoholic fatty liver disease: Current evidence and practice. World J Gastroenterol. 2019;25:1307–1326. doi: 10.3748/wjg.v25.i11.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dulai PS, Singh S, Patel J, et al. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: Systematic review and meta-analysis. Hepatology. 2017;65:1557–1565. doi: 10.1002/hep.29085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fujii H, Iwaki M, Hayashi H, et al. Clinical outcomes in biopsy-proven nonalcoholic fatty liver disease patients: a multicenter registry-based cohort study. Clin Gastroenterol Hepatol. 2022;7:934. doi: 10.1016/j.cgh.2022.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Watanabe S, Hashimoto E, Ikejima K, et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. J Gastroenterol. 2015;50:364–377. doi: 10.1007/s00535-015-1050-7. [DOI] [PubMed] [Google Scholar]
- 7.Watanabe S, Hashimoto E, Ikejima K, et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. Hepatol Res. 2015;45:363–377. doi: 10.1111/hepr.12511. [DOI] [PubMed] [Google Scholar]
- 8.Tokushige K, Ikejima K, Ono M, et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis 2020. J Gastroenterol. 2021;56:951–963. doi: 10.1007/s00535-021-01796-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tokushige K, Ikejima K, Ono M, et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis 2020. Hepatol Res. 2021;51:1013–1025. doi: 10.1111/hepr.13688. [DOI] [PubMed] [Google Scholar]
- 10.Daniels SJ, Leeming DJ, Eslam M, et al. ADAPT: An Algorithm Incorporating PRO-C3 Accurately Identifies Patients With NAFLD and Advanced Fibrosis. Hepatology. 2019;69:1075–1086. doi: 10.1002/hep.30163. [DOI] [PubMed] [Google Scholar]
- 11.De-Madaria E, Mira JJ, Carrillo I, et al. The present and future of gastroenterology and hepatology: an international SWOT analysis (the GASTROSWOT project) Lancet Gastroenterol Hepatol. 2022;7:485–494. doi: 10.1016/S2468-1253(21)00442-8. [DOI] [PubMed] [Google Scholar]
- 12.Kim GJ. A SWOT analysis of the field of virtual reality rehabilitation and therapy. Presence. 2005;14:119–146. doi: 10.1162/1054746053967094. [DOI] [Google Scholar]
- 13.Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43:1317–1325. doi: 10.1002/hep.21178. [DOI] [PubMed] [Google Scholar]
- 14.Shah AG, Lydecker A, Murray K, et al. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7:1104–1112. doi: 10.1016/j.cgh.2009.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xiao G, Zhu S, Xiao X, et al. Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: A meta-analysis. Hepatology. 2017;66:1486–1501. doi: 10.1002/hep.29302. [DOI] [PubMed] [Google Scholar]
- 16.Peleg N, Issachar A, Sneh-Arbib O, et al. AST to Platelet Ratio Index and fibrosis 4 calculator scores for non-invasive assessment of hepatic fibrosis in patients with non-alcoholic fatty liver disease. Dig Liver Dis. 2017;49:1133–1138. doi: 10.1016/j.dld.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 17.Patel YA, Gifford EJ, Glass LM, et al. Identifying nonalcoholic fatty liver disease advanced fibrosis in the veterans health administration. Dig Dis Sci. 2018;63:2259–2266. doi: 10.1007/s10620-018-5123-3. [DOI] [PubMed] [Google Scholar]
- 18.de Carli MA, de Carli LA, Correa MB, et al. Performance of noninvasive scores for the diagnosis of advanced liver fibrosis in morbidly obese with nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol. 2020;32:420–425. doi: 10.1097/MEG.0000000000001519. [DOI] [PubMed] [Google Scholar]
- 19.Younes R, Caviglia GP, Govaere O, et al. Long-term outcomes and predictive ability of non-invasive scoring systems in patients with non-alcoholic fatty liver disease. J Hepatol. 2021;75:786–794. doi: 10.1016/j.jhep.2021.05.008. [DOI] [PubMed] [Google Scholar]
- 20.Sumida Y, Yoneda M, Hyogo H, et al. Validation of the FIB4 index in a Japanese nonalcoholic fatty liver disease population. BMC Gastroenterol. 2012;12:2. doi: 10.1186/1471-230X-12-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanwal F, Kramer JR, Mapakshi S, et al. Risk of hepatocellular cancer in patients with non-alcoholic fatty liver disease. Gastroenterology. 2018;155:1828–37.e2. doi: 10.1053/j.gastro.2018.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim GA, Lee HC, Choe J, et al. Association between non-alcoholic fatty liver disease and cancer incidence rate. J Hepatol. 2017;56:23. doi: 10.1016/j.jhep.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 23.Ioannou GN, Green P, Kerr KF, et al. Models estimating risk of hepatocellular carcinoma in patients with alcohol or NAFLD-related cirrhosis for risk stratification. J Hepatol. 2019;71:523–533. doi: 10.1016/j.jhep.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Loosen SH, Kostev K, Keitel V, et al. An elevated FIB-4 score predicts liver cancer development: A longitudinal analysis from 29,999 patients with NAFLD. J Hepatol. 2022;76:247–248. doi: 10.1016/j.jhep.2021.08.030. [DOI] [PubMed] [Google Scholar]
- 25.Baratta F, Pastori D, Angelico F, et al. Nonalcoholic fatty liver disease and fibrosis associated with increased risk of cardiovascular events in a prospective study. Clin Gastroenterol Hepatol. 2020;18:2324–31.e4. doi: 10.1016/j.cgh.2019.12.026. [DOI] [PubMed] [Google Scholar]
- 26.Saito Y, Okumura Y, Nagashima K, et al. Impact of the Fibrosis-4 Index on Risk Stratification of Cardiovascular Events and Mortality in Patients with Atrial Fibrillation: Findings from a Japanese Multicenter Registry. J Clin Med. 2020;9:78. doi: 10.3390/jcm9020584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peleg N, Sneh Arbib O, Issachar A, et al. Noninvasive scoring systems predict hepatic and extra-hepatic cancers in patients with nonalcoholic fatty liver disease. PLoS ONE. 2018;13:e0202393. doi: 10.1371/journal.pone.0202393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hagström H, Nasr P, Ekstedt M, et al. Accuracy of noninvasive scoring systems in assessing risk of death and liver-related endpoints in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2019;17:1148–56.e4. doi: 10.1016/j.cgh.2018.11.030. [DOI] [PubMed] [Google Scholar]
- 29.Önnerhag K, Hartman H, Nilsson PM, et al. Non-invasive fibrosis scoring systems can predict future metabolic complications and overall mortality in non-alcoholic fatty liver disease (NAFLD) Scand J Gastroenterol. 2019;54:328–334. doi: 10.1080/00365521.2019.1583366. [DOI] [PubMed] [Google Scholar]
- 30.Clinical Practice Guidelines EASL, on non-invasive tests for evaluation of liver disease severity and prognosis -, update. J Hepatol. 2021;2021(75):659–689. doi: 10.1016/j.jhep.2021.05.025. [DOI] [PubMed] [Google Scholar]
- 31.Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 32.McPherson S, Hardy T, Dufour JF, et al. Age as a confounding factor for the accurate non-invasive diagnosis of advanced NAFLD Fibrosis. Am J Gastroenterol. 2017;112:740–751. doi: 10.1038/ajg.2016.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ishiba H, Sumida Y, Tanaka S, et al. The novel cutoff points for the FIB4 index categorized by age increase the diagnostic accuracy in NAFLD: a multi-center study. J Gastroenterol. 2018;53:1216–1224. doi: 10.1007/s00535-018-1474-y. [DOI] [PubMed] [Google Scholar]
- 34.Joo SK, Kim W, Kim D, et al. Steatosis severity affects the diagnostic performances of noninvasive fibrosis tests in nonalcoholic fatty liver disease. Liver Int. 2018;38:331–341. doi: 10.1111/liv.13549. [DOI] [PubMed] [Google Scholar]
- 35.Ishiba H, Sumida Y, Seko Y, et al. Type IV Collagen 7S Is the Most Accurate Test For Identifying Advanced Fibrosis in NAFLD With Type 2 Diabetes. Hepatol Commun. 2021;5:559–572. doi: 10.1002/hep4.1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boursier J, Canivet CM, Costentin C, et al. Impact of type 2 diabetes on the accuracy of non-invasive tests of liver fibrosis with resulting clinical implications. Clin Gastroenterol Hepatol. 2022;89:8. doi: 10.1016/j.cgh.2022.02.059. [DOI] [PubMed] [Google Scholar]
- 37.Loomba R, Adams LA. Advances in non-invasive assessment of hepatic fibrosis. Gut. 2020;69:1343–1352. doi: 10.1136/gutjnl-2018-317593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45:846–854. doi: 10.1002/hep.21496. [DOI] [PubMed] [Google Scholar]
- 39.Angulo P, Bugianesi E, Bjornsson ES, et al. Simple noninvasive systems predict long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2013;145:782–9.e4. doi: 10.1053/j.gastro.2013.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ooi GJ, Burton PR, Doyle L, et al. Modified thresholds for fibrosis risk scores in nonalcoholic fatty liver disease are necessary in the obese. Obes Surg. 2017;27:115–125. doi: 10.1007/s11695-016-2246-5. [DOI] [PubMed] [Google Scholar]
- 41.Qadri S, Ahlholm N, Lønsmann I, et al. Obesity Modifies the Performance of Fibrosis Biomarkers in Nonalcoholic Fatty Liver Disease. The Journal of clinical endocrinology and metabolism. 2021. [DOI] [PMC free article] [PubMed]
- 42.Mikolasevic I, Domislovic V, Krznaric-Zrnic I, et al. The Accuracy of Serum Biomarkers in the Diagnosis of Steatosis, Fibrosis, and Inflammation in Patients with Nonalcoholic Fatty Liver Disease in Comparison to a Liver Biopsy. Medicina (Kaunas) 2022;58:78. doi: 10.3390/medicina58020252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boursier J, Tsochatzis EA. Case-finding strategies in non-alcoholic fatty liver disease. JHEP Rep. 2021;3:100219. doi: 10.1016/j.jhepr.2020.100219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ampuero J, Pais R, Aller R, et al. Development and validation of hepamet fibrosis scoring system-a simple, noninvasive test to identify patients with nonalcoholic fatty liver disease with advanced fibrosis. Clin Gastroenterol Hepatol. 2020;18:216–25.e5. doi: 10.1016/j.cgh.2019.05.051. [DOI] [PubMed] [Google Scholar]
- 45.Ito T, Nguyen VH, Tanaka T, et al. Poor Diagnostic Efficacy of Noninvasive Tests for Advanced Fibrosis in Obese or Younger Than 60 Diabetic NAFLD patients. Clin Gastroenterol Hepatol. 2022. [DOI] [PubMed]
- 46.Glen J, Floros L, Day C, et al. Non-alcoholic fatty liver disease (NAFLD): summary of NICE guidance. BMJ. 2016;354:i4428. doi: 10.1136/bmj.i4428. [DOI] [PubMed] [Google Scholar]
- 47.Srivastava A, Jong S, Gola A, et al. Cost-comparison analysis of FIB-4, ELF and fibroscan in community pathways for non-alcoholic fatty liver disease. BMC Gastroenterol. 2019;19:122. doi: 10.1186/s12876-019-1039-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Inadomi C, Takahashi H, Ogawa Y, et al. Accuracy of the Enhanced Liver Fibrosis test, and combination of the Enhanced Liver Fibrosis and non-invasive tests for the diagnosis of advanced liver fibrosis in patients with non-alcoholic fatty liver disease. Hepatol Res. 2020;50:682–692. doi: 10.1111/hepr.13495. [DOI] [PubMed] [Google Scholar]
- 49.Murawaki Y, Ikuta Y, Koda M, et al. Serum type III procollagen peptide, type IV collagen 7S domain, central triple-helix of type IV collagen and tissue inhibitor of metalloproteinases in patients with chronic viral liver disease: relationship to liver histology. Hepatology. 1994;20:780–787. doi: 10.1002/hep.1840200403. [DOI] [PubMed] [Google Scholar]
- 50.Shima T, Ohtakaki Y, Kikuchi H, et al. A novel rapid immunoassay of serum type IV collagen 7S for the diagnosis of fibrosis stage of nonalcoholic fatty liver diseases. Hepatol Res. 2021;51:263–276. doi: 10.1111/hepr.13605. [DOI] [PubMed] [Google Scholar]
- 51.Fujimori N, Umemura T, Kimura T, et al. Serum autotaxin levels are correlated with hepatic fibrosis and ballooning in patients with non-alcoholic fatty liver disease. World J Gastroenterol. 2018;24:1239–1249. doi: 10.3748/wjg.v24.i11.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Honda Y, Imajo K, Kobayashi T, et al. Autotaxin is a valuable biomarker for the prediction of liver fibrosis in patients with non-alcoholic fatty liver disease. Hepatol Res. 2019;49:1136–1146. doi: 10.1111/hepr.13382. [DOI] [PubMed] [Google Scholar]
- 53.Grassadonia A, Tinari N, Iurisci I, et al. 90K (Mac-2 BP) and galectins in tumor progression and metastasis. Glycoconj J. 2004;19:551–556. doi: 10.1023/B:GLYC.0000014085.00706.d4. [DOI] [PubMed] [Google Scholar]
- 54.Przybylo M, Martuszewska D, Pochec E, et al. Identification of proteins bearing beta1-6 branched N-glycans in human melanoma cell lines from different progression stages by tandem mass spectrometry analysis. Biochim Biophys Acta. 2007;1770:1427–1435. doi: 10.1016/j.bbagen.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 55.Artini M, Natoli C, Tinari N, et al. Elevated serum levels of 90K/MAC-2 BP predict unresponsiveness to alpha-interferon therapy in chronic HCV hepatitis patients. J Hepatol. 1996;25:212–217. doi: 10.1016/S0168-8278(96)80076-6. [DOI] [PubMed] [Google Scholar]
- 56.Cheung KJ, Tilleman K, Deforce D, et al. The HCV serum proteome: a search for fibrosis protein markers. J Viral Hepat. 2009;16:418–429. doi: 10.1111/j.1365-2893.2009.01083.x. [DOI] [PubMed] [Google Scholar]
- 57.Kuno A, Ikehara Y, Tanaka Y, et al. A serum "sweet-doughnut" protein facilitates fibrosis evaluation and therapy assessment in patients with viral hepatitis. Sci Rep. 2013;3:1065. doi: 10.1038/srep01065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jang SY, Tak WY, Park SY, et al. Diagnostic Efficacy of Serum Mac-2 binding protein glycosylation isomer and other markers for liver fibrosis in non-alcoholic fatty liver diseases. Ann Lab Med. 2021;41:302–309. doi: 10.3343/alm.2021.41.3.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tamaki N, Higuchi M, Kurosaki M, et al. Wisteria floribunda agglutinin-positive mac-2 binding protein as an age-independent fibrosis marker in nonalcoholic fatty liver disease. Sci Rep. 2019;9:10109. doi: 10.1038/s41598-019-46172-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tamaki N, Kurosaki M, Takahashi Y, et al. Wisteria floribunda Agglutinin-Positive Mac-2 Binding Protein as a Screening Tool for Significant Liver Fibrosis in Health Checkup. Int J Mol Sci. 2020;22:78. doi: 10.3390/ijms22010040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sumida Y, Yoneda M, Seko Y, et al. Surveillance of Hepatocellular Carcinoma in Nonalcoholic Fatty Liver Disease. Diagnostics (Basel). 2020;10:68. doi: 10.3390/diagnostics10080579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shiha G, Ibrahim A, Helmy A, et al. Asian-Pacific Association for the Study of the Liver (APASL) consensus guidelines on invasive and non-invasive assessment of hepatic fibrosis: a 2016 update. Hepatol Int. 2017;11:1–30. doi: 10.1007/s12072-016-9760-3. [DOI] [PubMed] [Google Scholar]
- 63.Pham TTT, Ho DT, Nguyen T. Usefulness of Mac-2 binding protein glycosylation isomer in non-invasive probing liver disease in the Vietnamese population. World J Hepatol. 2020;12:220–229. doi: 10.4254/wjh.v12.i5.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Loomba R, Jain A, Diehl AM, et al. Validation of serum test for advanced liver fibrosis in patients with nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol. 2019;17:1867–76.e3. doi: 10.1016/j.cgh.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 65.Grecian SM, McLachlan S, Fallowfield JA, et al. Addition of hyaluronic acid to the FIB-4 liver fibrosis score improves prediction of incident cirrhosis and hepatocellular carcinoma in type 2 diabetes: The Edinburgh Type 2 Diabetes Study. Obes Sci Pract. 2021;7:497–508. doi: 10.1002/osp4.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lebensztejn DM, Wierzbicka A, Socha P, et al. Cytokeratin-18 and hyaluronic acid levels predict liver fibrosis in children with non-alcoholic fatty liver disease. Acta Biochim Pol. 2011;58:8. doi: 10.18388/abp.2011_2225. [DOI] [PubMed] [Google Scholar]
- 67.Feldstein AE, Canbay A, Angulo P, et al. Hepatocyte apoptosis and fas expression are prominent features of human nonalcoholic steatohepatitis. Gastroenterology. 2003;125:437–443. doi: 10.1016/S0016-5085(03)00907-7. [DOI] [PubMed] [Google Scholar]
- 68.Wieckowska A, Zein NN, Yerian LM, et al. In vivo assessment of liver cell apoptosis as a novel biomarker of disease severity in nonalcoholic fatty liver disease. Hepatology. 2006;44:27–33. doi: 10.1002/hep.21223. [DOI] [PubMed] [Google Scholar]
- 69.Feldstein AE, Wieckowska A, Lopez AR, et al. Cytokeratin-18 fragment levels as noninvasive biomarkers for nonalcoholic steatohepatitis: a multicenter validation study. Hepatology. 2009;50:1072–1078. doi: 10.1002/hep.23050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chen J, Zhu Y, Zheng Q, et al. Serum cytokeratin-18 in the diagnosis of non-alcoholic steatohepatitis: A meta-analysis. Hepatol Res. 2014;44:854–862. doi: 10.1111/hepr.12197. [DOI] [PubMed] [Google Scholar]
- 71.Musso G, Gambino R, Cassader M, et al. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med. 2011;43:617–649. doi: 10.3109/07853890.2010.518623. [DOI] [PubMed] [Google Scholar]
- 72.Cusi K, Chang Z, Harrison S, et al. Limited value of plasma cytokeratin-18 as a biomarker for NASH and fibrosis in patients with non-alcoholic fatty liver disease. J Hepatol. 2014;60:167–174. doi: 10.1016/j.jhep.2013.07.042. [DOI] [PubMed] [Google Scholar]
- 73.Lee J, Vali Y, Boursier J, et al. Accuracy of cytokeratin 18 (M30 and M65) in detecting non-alcoholic steatohepatitis and fibrosis: A systematic review and meta-analysis. PLoS ONE. 2020;15:e0238717. doi: 10.1371/journal.pone.0238717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tada T, Kumada T, Toyoda H, et al. New scoring system combining the FIB-4 index and cytokeratin-18 fragments for predicting steatohepatitis and liver fibrosis in patients with nonalcoholic fatty liver disease. Biomarkers. 2018;23:328–334. doi: 10.1080/1354750X.2018.1425915. [DOI] [PubMed] [Google Scholar]
- 75.Kobayashi N, Kumada T, Toyoda H, et al. Ability of Cytokeratin-18 Fragments and FIB-4 index to diagnose overall and mild fibrosis nonalcoholic steatohepatitis in japanese nonalcoholic fatty liver disease patients. Dig Dis. 2017;35:521–530. doi: 10.1159/000480142. [DOI] [PubMed] [Google Scholar]
- 76.Tada T, Saibara T, Ono M, et al. Predictive value of cytokeratin-18 fragment levels for diagnosing steatohepatitis in patients with nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol. 2021;33:1451–1458. doi: 10.1097/MEG.0000000000002176. [DOI] [PubMed] [Google Scholar]
- 77.Liebig S, Stoeckmann N, Geier A, et al. Multicenter validation study of a diagnostic algorithm to detect NASH and Fibrosis in NAFLD Patients With Low NAFLD Fibrosis Score or Liver Stiffness. Clin Transl Gastroenterol. 2019;10:e00066. doi: 10.14309/ctg.0000000000000066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yoneda M, Yoneda M, Mawatari H, et al. Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with nonalcoholic fatty liver disease (NAFLD) Dig Liver Dis. 2008;40:371–378. doi: 10.1016/j.dld.2007.10.019. [DOI] [PubMed] [Google Scholar]
- 79.Selvaraj EA, Mózes FE, Jayaswal ANA, et al. Diagnostic accuracy of elastography and magnetic resonance imaging in patients with NAFLD: a systematic review and meta-analysis. J Hepatol. 2021;75:770–785. doi: 10.1016/j.jhep.2021.04.044. [DOI] [PubMed] [Google Scholar]
- 80.Petroff D, Blank V, Newsome PN, et al. Assessment of hepatic steatosis by controlled attenuation parameter using the M and XL probes: an individual patient data meta-analysis. Lancet Gastroenterol Hepatol. 2021;6:185–198. doi: 10.1016/S2468-1253(20)30357-5. [DOI] [PubMed] [Google Scholar]
- 81.Gu Q, Cen L, Lai J, et al. A meta-analysis on the diagnostic performance of magnetic resonance imaging and transient elastography in nonalcoholic fatty liver disease. Eur J Clin Invest. 2021;51:e13446. doi: 10.1111/eci.13446. [DOI] [PubMed] [Google Scholar]
- 82.Ammon FJ, Kohlhaas A, Elshaarawy O, et al. Liver stiffness reversibly increases during pregnancy and independently predicts preeclampsia. World J Gastroenterol. 2018;24:4393–4402. doi: 10.3748/wjg.v24.i38.4393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stenberg Ribeiro M, Hagström H, Stål P, et al. Transient liver elastography in normal pregnancy - a longitudinal cohort study. Scand J Gastroenterol. 2019;54:761–765. doi: 10.1080/00365521.2019.1629007. [DOI] [PubMed] [Google Scholar]
- 84.Sandrin L, Fourquet B, Hasquenoph JM, et al. Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol. 2003;29:1705–1713. doi: 10.1016/j.ultrasmedbio.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 85.Ji D, Shao Q, Han P, et al. The frequency and determinants of liver stiffness measurement failure: a retrospective study of "real-life" 38,464 examinations. PLoS ONE. 2014;9:e105183. doi: 10.1371/journal.pone.0105183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Oeda S, Takahashi H, Imajo K, et al. Accuracy of liver stiffness measurement and controlled attenuation parameter using FibroScan(®) M/XL probes to diagnose liver fibrosis and steatosis in patients with nonalcoholic fatty liver disease: a multicenter prospective study. J Gastroenterol. 2020;55:428–440. doi: 10.1007/s00535-019-01635-0. [DOI] [PubMed] [Google Scholar]
- 87.Caussy C, Chen J, Alquiraish MH, et al. Association between obesity and discordance in fibrosis stage determination by magnetic resonance vs transient elastography in patients with nonalcoholic liver disease. Clin Gastroenterol Hepatol. 2018;16:1974–82.e7. doi: 10.1016/j.cgh.2017.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Newsome PN, Clet M, Czernichow S, et al. Expanding the use of the vibration controlled transient elastography in morbid obese patients: validation of a new automated adaptive measurement depths algorithm in a large pooled NAFLD cohort. J Hepatol. 2020;73:S430–S431. doi: 10.1016/S0168-8278(20)31343-X. [DOI] [Google Scholar]
- 89.Audière S, Labourdette A, Miette V, et al. Improved ultrasound attenuation measurement method for the non-invasive evaluation of hepatic steatosis using FibroScan. Ultrasound Med Biol. 2021;47:3181–3195. doi: 10.1016/j.ultrasmedbio.2021.07.007. [DOI] [PubMed] [Google Scholar]
- 90.Petta S, Wong VW, Cammà C, et al. Improved noninvasive prediction of liver fibrosis by liver stiffness measurement in patients with nonalcoholic fatty liver disease accounting for controlled attenuation parameter values. Hepatology. 2017;65:1145–1155. doi: 10.1002/hep.28843. [DOI] [PubMed] [Google Scholar]
- 91.Wong VW, Irles M, Wong GL, et al. Unified interpretation of liver stiffness measurement by M and XL probes in non-alcoholic fatty liver disease. Gut. 2019;68:2057–2064. doi: 10.1136/gutjnl-2018-317334. [DOI] [PubMed] [Google Scholar]
- 92.Siddiqui MS, Vuppalanchi R, Van Natta ML, et al. Vibration-controlled transient elastography to assess fibrosis and steatosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2019;17:156–63.e2. doi: 10.1016/j.cgh.2018.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Millonig G, Reimann FM, Friedrich S, et al. Extrahepatic cholestasis increases liver stiffness (FibroScan) irrespective of fibrosis. Hepatology. 2008;48:1718–1723. doi: 10.1002/hep.22577. [DOI] [PubMed] [Google Scholar]
- 94.Taniguchi T, Ohtani T, Kioka H, et al. Liver stiffness reflecting right-sided filling pressure can predict adverse outcomes in patients with heart failure. JACC Cardiovasc Imaging. 2019;12:955–964. doi: 10.1016/j.jcmg.2017.10.022. [DOI] [PubMed] [Google Scholar]
- 95.Loustaud-Ratti VR, Cypierre A, Rousseau A, et al. Non-invasive detection of hepatic amyloidosis: FibroScan, a new tool. Amyloid. 2011;18:19–24. doi: 10.3109/13506129.2010.543443. [DOI] [PubMed] [Google Scholar]
- 96.Wong GL, Kwok R, Wong VW. Huge adrenal hemangioma: a rare cause of deceivingly high liver stiffness measurement by transient elastography. Clin Gastroenterol Hepatol. 2015;13:e37–e38. doi: 10.1016/j.cgh.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 97.Kim G, Kim MY, Baik SK. Transient elastography versus hepatic venous pressure gradient for diagnosing portal hypertension: a systematic review and meta-analysis. Clin Mol Hepatol. 2017;23:34–41. doi: 10.3350/cmh.2016.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Colecchia A, Ravaioli F, Marasco G, et al. A combined model based on spleen stiffness measurement and Baveno VI criteria to rule out high-risk varices in advanced chronic liver disease. J Hepatol. 2018;69:308–317. doi: 10.1016/j.jhep.2018.04.023. [DOI] [PubMed] [Google Scholar]
- 99.Stefanescu H, Marasco G, Calès P, et al. A novel spleen-dedicated stiffness measurement by FibroScan® improves the screening of high-risk oesophageal varices. Liver Int. 2020;40:175–185. doi: 10.1111/liv.14228. [DOI] [PubMed] [Google Scholar]
- 100.Perazzo H, Fernandes FF, Soares JC, et al. Learning curve and intra/interobserver agreement of transient elastography in chronic hepatitis C patients with or without HIV co-infection. Clin Res Hepatol Gastroenterol. 2016;40:73–82. doi: 10.1016/j.clinre.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 101.Newsome PN, Sasso M, Deeks JJ, et al. FibroScan-AST (FAST) score for the non-invasive identification of patients with non-alcoholic steatohepatitis with significant activity and fibrosis: a prospective derivation and global validation study. Lancet Gastroenterol Hepatol. 2020;5:362–373. doi: 10.1016/S2468-1253(19)30383-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Oeda S, Takahashi H, Imajo K, et al. Diagnostic accuracy of FibroScan-AST score to identify non-alcoholic steatohepatitis with significant activity and fibrosis in Japanese patients with non-alcoholic fatty liver disease: Comparison between M and XL probes. Hepatol Res. 2020;50:831–839. doi: 10.1111/hepr.13508. [DOI] [PubMed] [Google Scholar]
- 103.Konerman MA, Jones JC, Harrison SA. Pharmacotherapy for NASH: Current and emerging. J Hepatol. 2018;68:362–375. doi: 10.1016/j.jhep.2017.10.015. [DOI] [PubMed] [Google Scholar]
- 104.Rinella ME, Dufour JF, Anstee QM, et al. Non-invasive evaluation of response to obeticholic acid in patients with NASH: Results from the REGENERATE study. J Hepatol. 2021;89:56. doi: 10.1016/j.jhep.2021.10.029. [DOI] [PubMed] [Google Scholar]
- 105.Younossi ZM, Stepanova M, Noureddin M, et al. Improvements of fibrosis and disease activity are associated with improvement of patient-reported outcomes in patients with advanced fibrosis due to nonalcoholic steatohepatitis. Hepatology communications. 2021;5:1201–1211. doi: 10.1002/hep4.1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Scorletti E, Afolabi PR, Miles EA, et al. Synbiotics alter fecal microbiomes, but not liver fat or fibrosis, in a randomized trial of patients with nonalcoholic fatty liver disease. Gastroenterology. 2020;158:1597–610.e7. doi: 10.1053/j.gastro.2020.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Patel K, Harrison SA, Elkhashab M, et al. Cilofexor, a Nonsteroidal FXR Agonist, in patients with noncirrhotic NASH: A Phase 2 Randomized Controlled Trial. Hepatology. 2020;72:58–71. doi: 10.1002/hep.31205. [DOI] [PubMed] [Google Scholar]
- 108.Loomba R, Noureddin M, Kowdley KV, et al. Combination therapies including cilofexor and firsocostat for bridging fibrosis and cirrhosis attributable to NASH. Hepatology. 2021;73:625–643. doi: 10.1002/hep.31622. [DOI] [PubMed] [Google Scholar]
- 109.Lin Y, Li H, Jin C, et al. The diagnostic accuracy of liver fibrosis in non-viral liver diseases using acoustic radiation force impulse elastography: A systematic review and meta-analysis. PLoS ONE. 2020;15:e0227358. doi: 10.1371/journal.pone.0227358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Herrmann E, de Lédinghen V, Cassinotto C, et al. Assessment of biopsy-proven liver fibrosis by two-dimensional shear wave elastography: An individual patient data-based meta-analysis. Hepatology. 2018;67:260–272. doi: 10.1002/hep.29179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Papatheodoridi M, Hiriart JB, Lupsor-Platon M, et al. Refining the Baveno VI elastography criteria for the definition of compensated advanced chronic liver disease. J Hepatol. 2021;74:1109–1116. doi: 10.1016/j.jhep.2020.11.050. [DOI] [PubMed] [Google Scholar]
- 112.Foncea CG, Popescu A, Lupusoru R, et al. Comparative study between pSWE and 2D-SWE techniques integrated in the same ultrasound machine, with Transient Elastography as the reference method. Med Ultrason. 2020;22:13–19. doi: 10.11152/mu-2179. [DOI] [PubMed] [Google Scholar]
- 113.Kiani A, Brun V, Lainé F, et al. Acoustic radiation force impulse imaging for assessing liver fibrosis in alcoholic liver disease. World J Gastroenterol. 2016;22:4926–4935. doi: 10.3748/wjg.v22.i20.4926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Imajo K, Honda Y, Kobayashi T, et al. Direct Comparison of US and MR elastography for staging liver fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2022;20:908–17.e11. doi: 10.1016/j.cgh.2020.12.016. [DOI] [PubMed] [Google Scholar]
- 115.Yamamura S, Eslam M, Kawaguchi T, et al. MAFLD identifies patients with significant hepatic fibrosis better than NAFLD. Liver Int. 2020;40:3018–3030. doi: 10.1111/liv.14675. [DOI] [PubMed] [Google Scholar]
- 116.Yamamura S, Kawaguchi T, Nakano D, et al. Profiles of advanced hepatic fibrosis evaluated by FIB-4 index and shear wave elastography in health checkup examinees. Hepatol Res. 2020;50:199–213. doi: 10.1111/hepr.13436. [DOI] [PubMed] [Google Scholar]
- 117.Muthupillai R, Lomas DJ, Rossman PJ, et al. Magnetic resonance elastography by direct visualization of propagating acoustic strain waves. Science. 1995;269:1854–1857. doi: 10.1126/science.7569924. [DOI] [PubMed] [Google Scholar]
- 118.Imajo K, Kessoku T, Honda Y, et al. Magnetic resonance imaging more accurately classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient elastography. Gastroenterology. 2016;150:626–37.e7. doi: 10.1053/j.gastro.2015.11.048. [DOI] [PubMed] [Google Scholar]
- 119.Jung J, Loomba RR, Imajo K, et al. MRE combined with FIB-4 (MEFIB) index in detection of candidates for pharmacological treatment of NASH-related fibrosis. Gut. 2021;70:1946–1953. doi: 10.1136/gutjnl-2020-322976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Loomba R, Wolfson T, Ang B, et al. Magnetic resonance elastography predicts advanced fibrosis in patients with nonalcoholic fatty liver disease: a prospective study. Hepatology. 2014;60:1920–1928. doi: 10.1002/hep.27362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Venkatesh SK, Yin M, Ehman RL. Magnetic resonance elastography of liver: technique, analysis, and clinical applications. J Magn Reson Imaging. 2013;37:544–555. doi: 10.1002/jmri.23731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hsu C, Caussy C, Imajo K, et al. Magnetic resonance vs transient elastography analysis of patients with nonalcoholic fatty liver disease: a systematic review and pooled analysis of individual participants. Clin Gastroenterol Hepatol. 2019;17:630–7.e8. doi: 10.1016/j.cgh.2018.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kawamura N, Imajo K, Kalutkiewicz KJ, et al. Influence of liver stiffness heterogeneity on staging fibrosis in patients with nonalcoholic fatty liver disease. Hepatology. 2021;89:7. doi: 10.1002/hep.32302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Imajo K, Kessoku T, Honda Y, et al. MRI-Based Quantitative R2(*) Mapping at 3 Tesla reflects hepatic iron overload and pathogenesis in nonalcoholic fatty liver disease patients. J Magn Reson Imaging. 2022;55:111–125. doi: 10.1002/jmri.27810. [DOI] [PubMed] [Google Scholar]
- 125.Hoodeshenas S, Welle CL, Navin PJ, et al. Magnetic resonance elastography in primary sclerosing cholangitis: interobserver agreement for liver stiffness measurement with manual and automated methods. Acad Radiol. 2019;26:1625–1632. doi: 10.1016/j.acra.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 126.Permutt Z, Le TA, Peterson MR, et al. Correlation between liver histology and novel magnetic resonance imaging in adult patients with non-alcoholic fatty liver disease - MRI accurately quantifies hepatic steatosis in NAFLD. Aliment Pharmacol Ther. 2012;36:22–29. doi: 10.1111/j.1365-2036.2012.05121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Yu H, McKenzie CA, Shimakawa A, et al. Multiecho reconstruction for simultaneous water-fat decomposition and T2* estimation. J Magn Reson Imaging. 2007;26:1153–1161. doi: 10.1002/jmri.21090. [DOI] [PubMed] [Google Scholar]
- 128.Alsaqal S, Hockings P, Ahlström H, et al. The Combination of MR elastography and proton density fat fraction improves diagnosis of nonalcoholic steatohepatitis. J Magn Reson Imaging. 2021;78:457. doi: 10.1002/jmri.28040. [DOI] [PubMed] [Google Scholar]
- 129.Nakajima A, Eguchi Y, Yoneda M, et al. Randomised clinical trial: Pemafibrate, a novel selective peroxisome proliferator-activated receptor α modulator (SPPARMα), versus placebo in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2021;54:1263–1277. doi: 10.1111/apt.16596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Christou CD, Tsoulfas G. Challenges and opportunities in the application of artificial intelligence in gastroenterology and hepatology. World J Gastroenterol. 2021;27:6191–6223. doi: 10.3748/wjg.v27.i37.6191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Nash FA. Differential diagnosis, an apparatus to assist the logical faculties. Lancet. 1954;266:874–875. doi: 10.1016/S0140-6736(54)91437-3. [DOI] [PubMed] [Google Scholar]
- 132.Miller RA. Medical diagnostic decision support systems–past, present, and future: a threaded bibliography and brief commentary. J Am Med Inform Assoc. 1994;1:8–27. doi: 10.1136/jamia.1994.95236141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Jiang F, Jiang Y, Zhi H, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017;2:230–243. doi: 10.1136/svn-2017-000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Development W. Information and Communication Technology: An enabler for inclusive business solutions. 2012; https://docs.wbcsd.org/2012/08/Information_Communication_Technology.pdf.
- 135.Wong GL, Yuen PC, Ma AJ, et al. Artificial intelligence in prediction of non-alcoholic fatty liver disease and fibrosis. J Gastroenterol Hepatol. 2021;36:543–550. doi: 10.1111/jgh.15385. [DOI] [PubMed] [Google Scholar]
- 136.Popa SL, Ismaiel A, Cristina P, et al. Non-alcoholic fatty liver disease: implementing complete automated diagnosis and staging: a systematic review. Diagnostics (Basel). 2021;11:9. doi: 10.3390/diagnostics11061078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Decharatanachart P, Chaiteerakij R, Tiyarattanachai T, et al. Application of artificial intelligence in non-alcoholic fatty liver disease and liver fibrosis: a systematic review and meta-analysis. Ther Adv Gastroenterol. 2021;14:17562848211062807. doi: 10.1177/17562848211062807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Fialoke S, Malarstig A, Miller MR, et al. Application of Machine Learning Methods to Predict Non-Alcoholic Steatohepatitis (NASH) in Non-Alcoholic Fatty Liver (NAFL) Patients. AMIA Annu Symp Proc. 2018;2018:430–439. [PMC free article] [PubMed] [Google Scholar]
- 139.Docherty M, Regnier SA, Capkun G, et al. Development of a novel machine learning model to predict presence of nonalcoholic steatohepatitis. J Am Med Inform Assoc. 2021;28:1235–1241. doi: 10.1093/jamia/ocab003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ma H, Xu CF, Shen Z, et al. Application of Machine Learning Techniques for Clinical Predictive Modeling: A Cross-Sectional Study on Nonalcoholic Fatty Liver Disease in China. Biomed Res Int. 2018;2018:4304376. doi: 10.1155/2018/4304376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Liu YX, Liu X, Cen C, et al. Comparison and development of advanced machine learning tools to predict nonalcoholic fatty liver disease: An extended study. Hepatobiliary Pancreat Dis Int. 2021;20:409–415. doi: 10.1016/j.hbpd.2021.08.004. [DOI] [PubMed] [Google Scholar]
- 142.Atabaki-Pasdar N, Ohlsson M, Viñuela A, et al. Predicting and elucidating the etiology of fatty liver disease: A machine learning modeling and validation study in the IMI DIRECT cohorts. PLoS Med. 2020;17:e1003149. doi: 10.1371/journal.pmed.1003149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Constantinescu EC, Udristoiu AL, Udristoiu C, et al. Transfer learning with pre-trained deep convolutional neural networks for the automatic assessment of liver steatosis in ultrasound images. Med Ultrason. 2021;23:135–139. doi: 10.11152/mu-2746. [DOI] [PubMed] [Google Scholar]
- 144.Brattain LJ, Telfer BA, Dhyani M, et al. Objective liver fibrosis estimation from shear wave elastography. Annu Int Conf IEEE Eng Med Biol Soc. 2018;2018:1–5. doi: 10.1109/EMBC.2018.8513011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Zamanian H, Mostaar A, Azadeh P, et al. Implementation of Combinational Deep Learning Algorithm for Non-alcoholic Fatty Liver Classification in Ultrasound Images. J Biomed Phys Eng. 2021;11:73–84. doi: 10.31661/jbpe.v0i0.2009-1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Okanoue T, Shima T, Mitsumoto Y, et al. Artificial intelligence/neural network system for the screening of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatol Res. 2021;51:554–569. doi: 10.1111/hepr.13628. [DOI] [PubMed] [Google Scholar]
- 147.Okanoue T, Shima T, Mitsumoto Y, et al. Novel artificial intelligent/neural network system for staging of nonalcoholic steatohepatitis. Hepatol Res. 2021;51:1044–1057. doi: 10.1111/hepr.13681. [DOI] [PubMed] [Google Scholar]
- 148.Food U, Administration D. Manufacturers Sharing Patient-Specific Information from Medical Devices Upon Request: Guidance for Industry and Food and Drug Administration Staff. Silver Spring, MD: US Food and Drug Administration; 2017.
- 149.Ratziu V, Charlotte F, Heurtier A, et al. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128:1898–1906. doi: 10.1053/j.gastro.2005.03.084. [DOI] [PubMed] [Google Scholar]
- 150.Sumida Y, Nakajima A, Itoh Y. Limitations of liver biopsy and non-invasive diagnostic tests for the diagnosis of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J Gastroenterol. 2014;20:475–485. doi: 10.3748/wjg.v20.i2.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Aguilar FJ. Scanning the business environment: Macmillan; 1967.
- 152.Ratziu V, Francque S, Sanyal A. Breakthroughs in therapies for NASH and remaining challenges. J Hepatol. 2022;76:1263–1278. doi: 10.1016/j.jhep.2022.04.002. [DOI] [PubMed] [Google Scholar]