Abstract
Purpose
The prevalence of mental health problems has rapidly increased over time. The extent to which this captures changes in self-reporting due to decreasing stigma is unclear. We explore this by comparing time trends in mental health and stigma-related indicators across English regions.
Methods
We produced annual estimates of self-reported mental disorders (SRMDs) across waves of the Health Survey for England (2009–18, n = 78,226) and three stigma-related indicators (knowledge, attitudes, and intended behaviour) across waves of the Attitudes Towards Mental Illness survey (2009–19, n = 17,287). Differences in trends were tested across nine Government Office Regions using linear models, adjusting for age, sex, ethnicity, marital status, and social class.
Results
In 2009, SRMDs did not vary by region (p = 0.916), whereas stigma-related indicators did (p < 0.001), with London having the highest level of stigma and the North East having lowest level of stigma. Between 2009 and 2018, the prevalence of SRMDs increased from 4.3 to 9.1%. SRMDs increased and stigma-related indicators improved at different rates across regions over time (SRMDs p = 0.024; stigma-related indicators p < 0.001). London reported the lowest increase in SRMDs (+ 0.3 percentage point per year) yet among the largest improvements in attitudes and intended behaviour across regions.
Conclusions
Improvements in attitudes towards mental illness did not mirror changes in self-reported mental health problems across English regions over the past decade. The findings do not support the argument that changes in public stigma, at least when defined at this regional scale, have been driving the increase in self-reported mental health indicators in recent years.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00127-022-02388-7.
Keywords: England, Mental health, Self-report, Stigma, Health Survey for England
Introduction
Multiple studies in the United Kingdom (UK) have found a large increase in the prevalence of mental health problems over the past 2 decades that intensified in the years leading to the COVID-19 pandemic, particularly among young people [1–4]. A key inferential issue has been the extent to which these time trends capture meaningful increases in the burden of mental health or changes in self-report practices. In particular, many point to increased awareness and reduced stigma over time as an alternative hypothesis for changes in individuals’ propensity to self-report mental health problems [4]. The experience of stigma has already been linked to feelings of distress and shame, and a lower capacity to seek treatment [5]. Discussions about its impact on time trends, however, have often been restricted to limitations sections, and no study that we know of has sought to disentangle the extent to which this may be true.
Stigma around mental illness operates at individual, interpersonal, and societal levels [6]. An appropriate design to test this hypothesis may look at changes in self-reported problems and attitudes towards mental health at the micro- (e.g., household), meso- (e.g., network, community), and macro-level (e.g. region, country) scale over time. While attitudes towards mental health have been measured across a number of UK surveys, it is relatively difficult to derive a comprehensive portrait of trends, because attitudes have been measured either once or with different items over time [7–9]. While surveys on attitudes have been run in other countries and trends have been derived using meta-analytic methods, this work remains limited by the lack of repeated measurements, non-representative sampling methods, and/or small sample sizes [10–12].
One key exception is the national Attitudes Towards Mental Illness (AMI) survey, an annual survey of approx. 1,700 people repeated multiple times since 1994 across England [7, 8, 13]. Supporting the argument that attitudes towards mental health have improved over time, studies using AMI data found that both knowledge and attitudes towards people with mental illness improved over the last 2 decades, together with a reduced desire for social distance from people with mental illness [13, 14]. Further analyses in the AMI survey found that changes in these outcomes over time varied by age, improving more rapidly in younger adults, and by region, improving more rapidly in the region of London [13, 14]. While regional differences have declined over time, they remained significant in 2017–19, with London continuing to show a higher level of stigma around mental illness [13]. Analyses in the 2014 HSE dataset, which included a one-time module on attitudes towards mental illness, also supported the idea that regional differences remained meaningful even after taking into account differences in inhabitants’ age, sex, ethnicity, education, and income across regions [15].
To examine the “self-report bias” hypothesis, we therefore propose to examine how self-reported mental health problems may vary as a function of changes in public stigma towards mental illness across English regions over time. We examine this in four steps: (1) reporting estimates of self-reported mental disorders and stigma-related indicators at two points over the last decade (2009 and 2017–19) and testing cross-sectional differences across regions at both time points; (2) estimating annual change rates in each region and testing differences in these rates between regions; (3) testing the role of socio-demographic composition (and its change over time) through statistical adjustment; (4) testing the relevance of region as an analytic scale by estimating the proportion of the variance in these variables that may be explained at the region level (i.e., context) [16]. If the “self-report bias” hypothesis holds, we expect to see larger increases in the prevalence of self-reported mental health problems in regions that also had larger improvements in stigma-related indicators over time.
Methods
Data
We used two datasets to compare time trends over the past decade: the Health Survey for England (HSE) (2009–18) and Attitudes Towards Mental Illness (AMI) survey (2009–19).
The HSE represents a series of annual surveys started in 1991 and designed to monitor trends in the nation's health [17]. HSE adult samples over the past decade averaged 8000 participants aged 16 + , except in 2009 (n = 4645) where it was made smaller to include a larger sample of children. Data collection is done across three interviews (household, individual, and nurse) and a self-completed questionnaire. As a reference point, the estimated individual response rates in 2009 and 2018 were 61% and 54%. Sampling errors are calculated by integrating cluster and stratification variables into the analyses.
The AMI survey has been carried out in England every year from 2008 to 2017, and once again in 2019, by the agency Kantar TNS [13]. There are approximately 1700 participants aged 16 + for each survey year. A quota sampling frame was used to ensure that the survey sample included sufficient numbers of participants across English regions, with sample points selected by a random location methodology. Sampling errors are calculated on the assumption of a simple random sampling method.
Measures
Mental health outcome
We used one measure to capture self-reported mental disorders (SRMDs) in the HSE, derived by the data management team based on open responses during the main individual interview with regard to long-standing health conditions (Yes/No). The filter question was “Do you have any long-standing illness, disability or infirmity? By long-standing I mean anything that has troubled you over a period of time, or that is likely to affect you over a period of time?” in 2009–11 and “Do you have any physical or mental health conditions or illnesses lasting or expected to last 12 months or more?” in 2012–18. The coding frame used in the derived variable available for the time period included both mental illnesses (e.g., alcoholism, drug addiction, anxiety, depression, and schizophrenia) and handicaps (see conditions in Supplementary Table 1).
Stigma-related indicators
Based on the assumption that stigma can be conceptualized as comprised of three constructs, i.e., knowledge (ignorance), attitudes (prejudice), and behaviour (discrimination), we used three separate measures to capture changes in public stigma over time in the AMI survey (see items in Supplementary Table 2) [13]:
1. The Mental Health Knowledge Schedule (MAKS) scale was developed in the late 2000s to assess stigma-related knowledge about mental health problems among the general public [18]. The scale is composed of six Likert-type items asking whether participants agree with knowledge-related statements (e.g., “If a friend had a mental health problem, I know what advice to give them to get professional help”). MAKS items’ response scale vary from 1—Strongly Disagree to 5—Strongly Agree and include an “I do not know” option. Item responses were recoded into a composite score ranging from 6 to 30, with the “I do not know” responses recoded as the mid-point “Neither agree nor disagree” (Cronbach’s alpha in the 2019 sample = 0.60).
2. The 27-item Community Attitudes towards Mental Illness (CAMI) scale is shortened version of a long-standing item battery initially developed to capture neighbourhood opposition to community-based mental health facilities in the 1970s [19]. CAMI items’ response scale vary from 1—Strongly Disagree to 5—Strongly Agree, and item responses were recoded into a composite score ranging from 27 to 135 (Cronbach’s alpha in the 2019 sample = 0.88).
3. The Reported and Intended Behaviour Scale (RIBS) for desire for social distance was developed in the late 2000s based on the Social Distance Scale to assess intended stigmatising and discriminatory behaviours towards people with mental health problems [20]. The scale is composed of four Likert-type items asking whether participants agree that they would be willing to live with, work with, live nearby, and be friends with someone with a mental health problem. RIBS items’ response scale vary from 1—Strongly Disagree to 5—Strongly Agree, and item responses were recoded into a composite score ranging from 4 to 20 (Cronbach’s alpha in the 2019 sample = 0.86).
Region and covariates
Region was defined using the nine-category Government Office Region classification (i.e., North East, North West, Yorkshire and the Humber, East Midlands, West Midlands, East of England, London, South East, and South West). The robustness of regional differences was tested using five covariates: (1) age (16–24, 25–44, 45–64, and 65 +); (2) sex (male or female); (3) ethnicity (White, Black, Asian, and Other); (4) marital status (never married, married, and separated, divorced or widowed); (5) social class of the person responsible for the household. Social class in the AMI was defined using the Market Research Society’s classification system (AB—Managerial and professional occupations, C1—Skilled non-manual occupations, C2—Skilled manual occupations, and DE—Unskilled manual occupations and not in paid work). Social class in the HSE was defined using the National Statistics Socioeconomic classification (1—Managerial and professional occupations; 2—Intermediate occupations; 3—Routine and manual occupations, 4—Not in paid work) [21].
Statistical analysis
We first report the distribution of SRMDs and stigma-related indicators across annual waves at the national level and across the nine regions. We tested cross-sectional regional differences in variables in the 2009 and 2018 samples for the HSE, and in the 2009 and 2017–2019 samples for the AMI survey. We then report unadjusted and adjusted estimates of annual change in these variables using linear (probability) models. Differences in annual change across regions were examined by adding interaction terms and running a Wald-type test for the joint significance of interaction terms. Finally, we explored the amount of variance in outcomes that was explainable at the region level by estimating intraclass correlation coefficients (ICCs) from random-intercept linear models that nested participants in regions for SRMDs and stigma-related indicators (ICCs are detailed in Supplementary Table 3).
Analyses were done with the survey weights provided in the HSE and AMI to derive nationally representative estimates. Analyses were done in the complete-case samples of 78,226 participants (98.9% of whole sample) in the HSE and 17,287 participants (99.3% of whole sample) in the AMI with data on all variables in Stata 17 and R 4.1.2. Models in the HSE dataset were reproduced to show annual relative change, using prevalence ratios from Poisson regression, in Supplementary Table 4.
Results
Self-reported mental disorders (SRMDs) across English regions
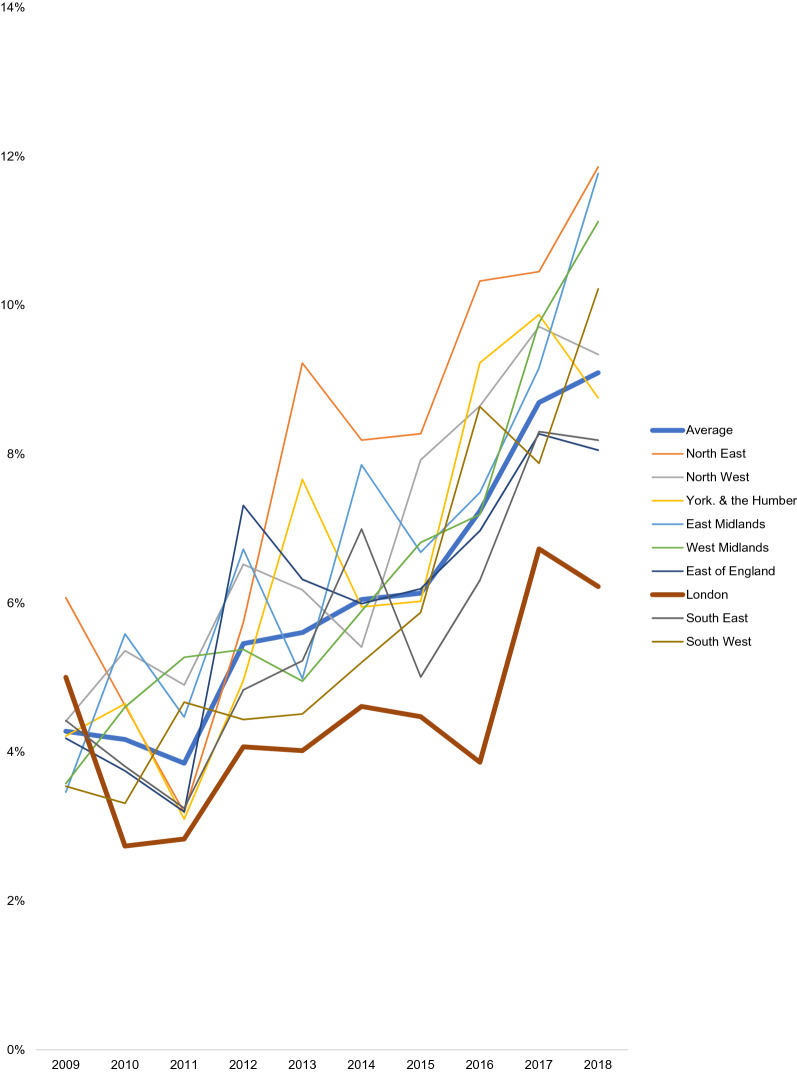
Table 1 presents the prevalence of SRMDs in 2009 and 2018, and annual changes in prevalence between 2009 and 18, at the national level and across the nine regions. Figure 1 presents time trends in the prevalence of SRMDs across regions between 2009 and 18.
Table 1.
Time trends in self-reported mental disorders in England, ages 16 +
| 2009 N = 4618 |
2018 N = 8052 |
Annual absolute change (in percentage points) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| % | 95%CI | % | 95%CI | Bivariate | Adjusted* | ||||
| B | 95%CI | B | 95%CI | ||||||
| Average | 4.3 | 3.6–5.0 | 9.1 | 8.3–9.9 | 0.6 | 0.5–0.7 | 0.6 | 0.5–0.7 | |
| 1 | North East | 6.1 | 3.5–10.3 | 11.9 | 9.3–15.0 | 0.9 | 0.6–1.1 | 0.9 | 0.6–1.2 |
| 2 | North West | 4.4 | 2.9–6.7 | 9.3 | 7.1–12.2 | 0.6 | 0.4–0.8 | 0.6 | 0.4–0.8 |
| 3 | Yorkshire and the Humberlands | 4.2 | 2.9–6.1 | 8.8 | 6.8–11.3 | 0.7 | 0.5–0.9 | 0.7 | 0.5–0.9 |
| 4 | East Midlands | 3.5 | 2.0–6.1 | 11.8 | 9.4–14.7 | 0.7 | 0.4–1.0 | 0.7 | 0.5–1.0 |
| 5 | West Midlands | 3.6 | 2.0–6.2 | 11.1 | 8.1–15.0 | 0.7 | 0.4–1.0 | 0.7 | 0.5–1.0 |
| 6 | East of England | 4.2 | 2.7–6.4 | 8.1 | 6.3–10.3 | 0.5 | 0.3–0.7 | 0.5 | 0.3–0.8 |
| 7 | London | 5.0 | 3.2–7.7 | 6.2 | 5.0–7.7 | 0.3 | 0.2–0.5 | 0.4 | 0.2–0.5 |
| 8 | South East | 4.4 | 2.7–7.2 | 8.2 | 6.3–10.6 | 0.5 | 0.3–0.8 | 0.6 | 0.3–0.8 |
| 9 | South West | 3.5 | 2.2–5.6 | 10.2 | 7.7–13.5 | 0.7 | 0.5–1.0 | 0.8 | 0.5–1.0 |
| Difference (p) | 0.916 | 0.001 | 0.024 | ||||||
| Difference, adjusted* (p) | 0.874 | 0.013 | 0.025 | ||||||
Health Survey for England (HSE), 2009–18 (n = 78,226). P values represent Wald-type tests for the joint significance of (1) region dummy terms and (2) region-by-year interaction dummy terms based on linear probability models. Adjusted models also include age, sex, ethnicity, marital status, and social class of the person responsible for the household. Bolded estimates are statistically significant at the 0.05 level
Fig. 1.
Time trends in self-reported mental disorders (%) across English regions, ages 16 + . Health Survey for England, 2009–18 (n = 78,226)
The overall prevalence of SRMDs in those aged 16 + in England increased from 4.3% in 2009 to 9.1% in 2018. The prevalence of SRMDs did not vary much by region in 2009, but did in 2018. In 2009, the prevalence of SRMDs varied from a low of 3.5% in the East Midlands and South West regions to a high of 6.1% in the North East region (unadjusted p = 0.916, adjusted p = 0.874). In 2018, the prevalence of SRMDs varied between 6.2% in the London region to 11.9% in the North East region (unadjusted p = 0.001, adjusted p = 0.013).
Comparing trends across regions, whereas the annual change rate was significant in all regions, there was significant variability across them (p = 0.024): the annual absolute increase in percentage points was lowest in the London region (0.3 p.p.) and highest in the North East (0.9 p.p.). Adjusting for the five demographic covariates did not meaningfully affect these results.
Stigma-related indicators across English regions
Tables 2, 3 and 4 present the average scores for stigma-related indicators in 2009 and 2017–19, and annual change rates between 2009 and 19, at the national level and across the nine regions. Supplementary Fig. 2 presents the time trends in stigma-related indicators across regions between 2009 and 19.
Table 2.
Time trends in mental health knowledge (MAKS) in England, ages 16 +
| 2009 N = 1743 |
2017–19 N = 3417 |
Annual absolute change | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Bivariate | Adjusted* | ||||||||
| Mean | 95%CI | Mean | 95%CI | B | 95%CI | B | 95%CI | ||
| Average | 22.2 | 22.1, 22.4 | 23.0 | 22.9, 23.1 | 0.11 | 0.09, 0.12 | 0.11 | 0.09, 0.12 | |
| 1 | North East | 22.9 | 22.2, 23.6 | 23.0 | 22.3, 23.5 | 0.05 | − 0.03, 0.12 | 0.06 | − 0.02, 0.13 |
| 2 | North West | 22.1 | 21.7, 22.5 | 23.1 | 22.8, 23.4 | 0.15 | 0.10, 0.19 | 0.15 | 0.11, 0.19 |
| 3 | Yorkshire and the Humberlands | 22.4 | 21.9, 23.0 | 23.5 | 23.1, 23.9 | 0.12 | 0.07, 0.18 | 0.11 | 0.06, 0.17 |
| 4 | East Midlands | 22.3 | 21.8, 22.9 | 23.1 | 22.7, 23.4 | 0.08 | 0.02, 0.13 | 0.08 | 0.02, 0.13 |
| 5 | West Midlands | 22.3 | 21.8, 22.8 | 22.7 | 22.4, 23.0 | 0.07 | 0.02, 0.12 | 0.06 | 0.01, 0.10 |
| 6 | East of England | 22.8 | 22.3, 23.2 | 23.3 | 23.0, 23.6 | 0.10 | 0.05, 0.15 | 0.10 | 0.06, 0.15 |
| 7 | London | 21.7 | 21.4, 22.0 | 22.3 | 22.0, 22.6 | 0.10 | 0.06, 0.14 | 0.07 | 0.03, 0.11 |
| 8 | South East | 22.0 | 21.6, 22.3 | 23.2 | 22.9, 23.4 | 0.14 | 0.10, 0.18 | 0.14 | 0.11, 0.18 |
| 9 | South West | 22.5 | 22.0, 23.0 | 23.3 | 22.9, 23.7 | 0.13 | 0.08, 0.19 | 0.13 | 0.08, 0.19 |
| Difference (p) | 0.007 | < 0.001 | 0.106 | ||||||
| Difference, adjusted* (p) | 0.025 | < 0.001 | 0.007 | ||||||
Attitudes towards Mental Illness (AMI) survey, 2009–19 (n = 17,287). The 6-item MAKS score can vary from 6 to 30; the observed range was 10–30. A higher score indicates more knowledge. As a reference point, the weighted mean was 22.6 and weighted standard deviation was 3.2 in the full complete-case sample. P values represent Wald-type tests for the joint significance of (1) region dummy terms and (2) region-by-year interaction dummy terms based on linear probability models. Adjusted models include age, sex, ethnicity, marital status, and social class of the person responsible for the household
Table 3.
Time trends in attitudes towards mental illness (CAMI) in England, ages 16 +
| 2009 N = 1743 |
2017–19 N = 3417 |
Annual absolute change | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Unadjusted | Bivariate | Adjusted* | ||||||
| Mean | 95%CI | Mean | 95%CI | B | 95%CI | B | 95%CI | ||
| Average | 105.5 | 104.8, 106.2 | 110.2 | 109.7, 110.6 | 0.56 | 0.49, 0.64 | 0.57 | 0.50, 0.63 | |
| 1 | North East | 113.5 | 110.5, 116.4 | 110.7 | 108.6, 112.7 | − 0.16 | − 0.47, 0.15 | − 0.03 | − 0.33, 0.27 |
| 2 | North West | 105.4 | 103.6, 107.2 | 112.1 | 110.8, 113.4 | 0.79 | 0.60, 0.98 | 0.84 | 0.66, 1.02 |
| 3 | Yorkshire and the Humberlands | 106.5 | 104.3, 108.8 | 111.1 | 109.6, 112.7 | 0.29 | 0.06, 0.52 | 0.25 | 0.03, 0.47 |
| 4 | East Midlands | 104.7 | 102.5, 107.0 | 111.2 | 109.5, 112.9 | 0.65 | 0.40, 0.91 | 0.59 | 0.35, 0.83 |
| 5 | West Midlands | 105.2 | 103.2, 107.2 | 110.3 | 108.9, 111.6 | 0.60 | 0.39, 0.80 | 0.57 | 0.38, 0.76 |
| 6 | East of England | 109.5 | 107.5, 111.5 | 110.1 | 108.6, 111.6 | 0.14 | − 0.07, 0.35 | 0.23 | 0.03, 0.43 |
| 7 | London | 97.7 | 95.8, 99.5 | 104.5 | 103.3, 105.8 | 0.88 | 0.69, 1.06 | 0.70 | 0.52, 0.87 |
| 8 | South East | 106.1 | 104.5, 107.8 | 111.7 | 110.4, 112.9 | 0.75 | 0.58, 0.93 | 0.81 | 0.65, 0.98 |
| 9 | South West | 107.8 | 105.6, 110.0 | 112.1 | 110.6, 113.5 | 0.56 | 0.34, 0.78 | 0.58 | 0.37, 0.80 |
| Difference (p) | < 0.001 | < 0.001 | < 0.001 | ||||||
| Difference, adjusted* (p) | < 0.001 | < 0.001 | < 0.001 | ||||||
Attitudes towards Mental Illness (AMI) survey, 2009–19 (n = 17,287). The 27-item CAMI score can vary from 27 to 135; the observed range was 35–135. A higher score indicates less stigmatising attitudes. As a reference point, the weighted mean was 107.8 and weighted standard deviation was 14.0 in the full complete-case sample. P values represent Wald-type tests for the joint significance of (1) region dummy terms and (2) region-by-year interaction dummy terms based on linear probability models. Adjusted models include age, sex, ethnicity, marital status, and social class of the person responsible for the household
Table 4.
Time trends in desire for social distance (RIBS) in England, ages 16 +
| 2009 N = 1743 |
2017–19 N = 3417 |
Annual absolute change | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Bivariate | Adjusted* | ||||||||
| Mean | 95%CI | Mean | 95%CI | B | 95%CI | B | 95%CI | ||
| Average | 15.9 | 15.7, 16.1 | 17.1 | 17.0, 17.2 | 0.13 | 0.11, 0.15 | 0.13 | 0.11, 0.14 | |
| 1 | North East | 17.5 | 16.8, 18.2 | 17.0 | 16.4, 17.7 | 0.00 | − 0.09, 0.09 | 0.02 | − 0.06, 0.10 |
| 2 | North West | 15.9 | 15.5, 16.4 | 17.5 | 17.2, 17.8 | 0.18 | 0.14, 0.23 | 0.20 | 0.16, 0.24 |
| 3 | Yorkshire and the Humberlands | 16.6 | 16.1, 17.1 | 17.3 | 17.0, 17.7 | 0.06 | 0.00, 0.11 | 0.05 | 0.00, 0.10 |
| 4 | East Midlands | 15.8 | 15.2, 16.4 | 17.3 | 16.9, 17.6 | 0.13 | 0.07, 0.18 | 0.11 | 0.06, 0.17 |
| 5 | West Midlands | 15.9 | 15.3, 16.5 | 17.1 | 16.8, 17.4 | 0.12 | 0.07, 0.17 | 0.11 | 0.06, 0.16 |
| 6 | East of England | 16.5 | 16.1, 17.0 | 17.3 | 16.9, 17.6 | 0.11 | 0.06, 0.16 | 0.11 | 0.07, 0.16 |
| 7 | London | 14.0 | 13.5, 14.5 | 16.0 | 15.7, 16.3 | 0.20 | 0.15, 0.24 | 0.16 | 0.11, 0.21 |
| 8 | South East | 16.0 | 15.6, 16.4 | 17.2 | 16.9, 17.5 | 0.14 | 0.09, 0.18 | 0.15 | 0.11, 0.19 |
| 9 | South West | 16.2 | 15.7, 16.7 | 17.3 | 17.0, 17.7 | 0.13 | 0.08, 0.18 | 0.12 | 0.07, 0.17 |
| Difference (p) | < 0.001 | < 0.001 | < 0.001 | ||||||
| Difference, adjusted* (p) | < 0.001 | < 0.001 | < 0.001 | ||||||
Attitudes towards Mental Illness (AMI) survey, 2009–19 (n = 17,287). The 4-item RIBS score can vary from 4 to 20; the observed range was 4–20. A higher score indicates less desire for social distance. As a reference point, the weighted mean was 16.5 and weighted standard deviation was 3.4 in the full complete-case sample. P values represent Wald-type tests for the joint significance of (1) region dummy terms and (2) region-by-year interaction dummy terms based on linear probability models. Adjusted models include age, sex, ethnicity, marital status, and social class of the person responsible for the household
All three indicators significantly varied across regions in 2009 and 2017–19. In 2009, mean scores were each lowest in London (MAKS = 21.7, CAMI = 97.7, RIBS = 14.0) and highest in the North East region (MAKS = 22.9, CAMI = 113.5, RIBS = 17.5). Using standard deviations (SD) from the 2009 sample as a reference point, differences between these two regions represented a 0.39 SD difference for the MAKS, 1.10 SD for the CAMI, and 0.97 SD for the RIBS.
In 2017–19, scores were still lowest in London (MAKS = 22.3, CAMI = 104.5, RIBS = 16.0). The North East region, however, no longer had the most positive indicator scores; Yorkshire and the Humber reported the highest knowledge score (MAKS = 23.5) and North West reported the highest attitude score (CAMI = 112.1) and intended behaviour score (RIBS = 17.5). Using standard deviations in the 2017–19 sample as a reference point, differences between London and regions with the most positive scores represented a 0.39 SD difference for the MAKS, 0.56 SD for the CAMI, and 0.44 SD for the RIBS.
Examining change over time, all three indicators—i.e., MAKS (B = 0.11, 95%CI 0.09, 0.12), CAMI (B = 0.56, 95%CI 0.49, 0.64), and RIBS (B = 0.13, 95%CI 0.11, 0.15)—showed a significant annual improvement rate at the national level. Using standard deviations from the full complete-case sample as a reference point, average differences between 2007 and 2019 could be likened to a 0.41 SD increase for the MAKS, 0.48 SD for the CAMI, and 0.46 SD for the RIBS.
As with SRMDs, annual change rates significantly varied across regions for all indicators in adjusted models (p < 0.01). MAKS. In unadjusted models, MAKS scores improved most rapidly in the North West (B = 0.15, 95%CI 0.10, 0.19) and did not improve in one region: North East (B = 0.05, 95%CI − 0.03, 0.12). There were no change in statistical significance for regions’ change rate between unadjusted and adjusted models. London had a relatively small improvement rate for knowledge (adjusted model: B = 0.07, 95%CI 0.03, 0.11). CAMI. In unadjusted models, CAMI scores improved most rapidly in London (B = 0.56, 95%CI 0.49, 0.64) and did not improve in two regions: North East (B = − 0.16, 95%CI − 0.47, 0.15) and East of England (B = 0.14, 95%CI − 0.07, 0.35). In adjusted models, the annual change rate in East of England increased and became significant (B = 0.23, 95%CI 0.03, 0.43). RIBS. In unadjusted models, RIBS scores improved most rapidly in London (B = 0.20, 95%CI 0.15, 0.24) and did not improve in one region: North East (B = 0.00, 95%CI − 0.09, 0.09). In adjusted models, a second region—Yorkshire & the Humber—no longer showed a significant improvement (B = 0.05, 95% 0.00–0.10).
Examining variation in regional differences with intraclass correlation coefficients
Finally, we explored the extent to which regional differences in SRMDs and stigma-related indicators may be explained by contextual or compositional factors using multilevel modelling. Using unadjusted models only including dummy terms for year in the pooled HSE and AMI samples, intraclass correlation coefficients for the region level were very low for SRMDs (0.1%) and MAKS (0.8%), CAMI (3.6%), and RIBS (2.1%) scores. This supports the idea that contextual effects (including stigma at the regional level) are unlikely to be driving differences in SRMDs across regions.
Discussion
This paper explored the extent to which self-reporting practices may have been sensitive to changes in public stigma by comparing time trends in self-reported mental disorders and attitudes across English regions. During this period, a national campaign—Time to Change—ran across the country to reduce stigma and discrimination against people with mental health disorders [22–24]. Its components varied in scale, including a social marketing campaign, events in public spaces where people could find out more about mental health problems and hear from people with lived experience, and work with employers to improve workplace support for mental health. There had not been any major differences between regions in terms of the coverage of the programme.
We provide new evidence corroborating the worrying pace at which mental health problems have increased in prevalence across English regions in the 2010s. Our statistical adjustment strategy supports the idea that time trends have been insensitive to changes in ethnicity and some living arrangements (i.e., marital status and social class at the household level) during this period. Multilevel modelling also supports that these differences are likely to result from regions’ composition than from contextual effects specific to the regional scale. Importantly, in keeping with austerity responses made by the English government after the 2008 Great Recession, these regional differences may result from cuts in health care and other social services across local authorities within regions [25].
Lack of support for the “self-report bias” hypothesis
Public stigma towards mental illness has been unequally distributed across English regions for a long period of time. Supporting the body of work using the AMI survey, we found that improvements in stigma-related indicators between 2009 and 2019 substantially varied across regions. North West, London, and the South East showed the most improvements, whereas North East and the Yorkshire & Humber showed the least improvements (or no change at all). Notably, the annual change rate across indicators in London was attenuated by 20–30% when adjusting for covariates, supporting the hypothesis that improvements in this region could be explained in part by changes in socio-demographic composition over time.
These trends largely failed to support the “self-report bias” hypothesis, which predicted a corresponding increase in the prevalence of self-reported mental disorders. Instead, London showed the lowest increase in SRMDs across the nine regions and the North West and South East showed an increase matching the national average. At the other end, the North East showed the largest increase in SRMDs across regions and the Yorkshire and Humber showed a slightly above-average increase. We explore three reasons that may explain this negative finding.
The first concerns the nature of the relationship between public stigma and self-reporting. First, substantial levels of improvement may be required before it can start having an impact. The role of attitudes in behaviour change is likely to be non-linear for many behaviours, and this may also be the case for the perception of shared attitudes in one’s environment [26]. While London showed above-average improvements over time, it remained in 2019 behind where most regions were in terms of attitudes and intended behaviours in 2009. It is possible that it is only once a region has a sufficiently high proportion of inhabitants with positive attitudes that it starts seeing a shift in self-reporting practices, and regions such as London may have yet to reach this point. Second, it is possible that the role of public stigma in self-reporting varies across regions: whereas its change had no overlap with self-reported mental health problems in London; it is possible that a substantive change in public stigma in another region with a different regional culture would have a more meaningful impact. Finally, psychological literature suggests that attitudes have a larger impact once they become stable over time [27]. Therefore, it is also possible that changes in the perception of shared attitudes have a lagged effect, and that the changes observed in some English regions will have an impact on self-reporting in the years to come.
A second issue concerns the scale of analysis. The use of the nine regions was done out of convenience given the design and sample sizes of the HSE and AMI surveys. However, the stigma-related processes that influence practices such as self-reporting may work at more interpersonal levels. For instance, one study found in the HSE that knowing someone with a mental health problem was associated with better help seeking practices [28]. Supporting this, another study also found in the HSE no variance in attitudes at the local area level (across geographical units averaging 1500 inhabitants), but a meaningful degree of variance at the household level [29]. Changes in interpersonal stigma (e.g., parents and other family members having more positive attitudes over time) may therefore have a more meaningful impact on self-reporting compared with the changes in public stigma examined here.
A third reason may be that public stigma has a larger impact on self-reporting in some groups, and that our analyses failed to assess this heterogeneity. A small US study among older adults found that perceived public stigma had a stronger impact in those living in rural areas compared with urban areas [30]. In another analysis of the AMI dataset, researchers found that familiarity of someone with a mental health problem had a different impact across socioeconomic groups: compared with those in a higher social class, those in a routine job or unemployed were more likely to have positive attitudes and less desire for social distance if they knew someone with a problem or had a problem themselves [31]. Whereas the sample size of the AMI precludes us from reliably stratifying within regions (e.g., test the three-level interaction between time, region, and urbanicity), it is possible that improvements in public stigma in regions such as London have had a meaningful impact on self-reporting in some groups.
Towards disentangling the relationship between stigma and self-reporting
To the best of our knowledge, this study represents one of the few attempts to examine the role of changes in stigma on the self-reporting of mental health problems over time. This research programme, however, requires a range of studies to fully test this.
A first step includes using other analytic scales to examine how interpersonal and structural stigma may operate to influence self-reporting. Since our findings did not support using region as a meaningful scale, relevant scales may be more micro (i.e., households or networks) or macro (i.e., countries) [32]. Surveys using a household design with information on attitudes and mental health, such as the 2014 HSE, may offer additional insight in the role of peers’ attitudes, including parents and partners, in the self-reporting of mental health problems. On the other end, the role of structural stigma can be examined by looking at cross-country differences. Most studies have relied on the analysis of traditional media to assess national trends in public stigma, which could be contrasted with trends in self-reported mental health outcomes [33, 34]. The same could be done with social media, which is also likely to differ across countries [35, 36]. The estimation of changes in attitudes based on surveys is largely unavailable in other countries, yet cross-national comparisons support the potential for variability [37]. To support this work, other countries need to develop appropriate survey programmes to assess changes in attitudes over time. Examples include data collection done between 2007 and 2013 in the U.S. Behavioral Risk Factor Surveillance System, and in 1996, 2006, and 2018 in the U.S. General Social Survey [10, 11].
Strength and limitations
We remind that with an ecological design (i.e., comparing aggregate levels of self-reported problems and stigma-related indicators across regions), we cannot confirm that associations at the region level match those at the individual level [38]. The decision to use similar covariates across the HSE and AMI surveys may have also led us to omit important covariates for correctly modelling change over time. A cross-sectional design also precludes us from drawing causal interpretations. Reflecting on temporal ordering, it may be increases in psychiatric morbidity that are driving improvements in public stigma over time. Since mental health is a multi-faceted concept, our findings are limited by the use of only one mental health outcome, which was the only variable measured consistently across HSE waves between 2009 and 2018. Other behaviours, such as seeking health care services, may also be more affected by stigma compared with the self-reporting of mental health problems. Using other outcomes related to mental health and stigma would likely yield a more comprehensive portrait of changes across regions over time. Finally, the lack of a repeated survey collecting data on both mental health and attitudes over time precludes us from considering how people may differently report their attitudes if they mis-report their condition, and whether this affects the estimation of time trends. For example, reported stigma may be greater among those who do not accept their mental health condition (i.e., defensive projection) [39].
Conclusion
In 2018, the proportion of those with mental disorders reached nearly 10% of the adult population. Its prevalence increased across all regions since 2009, with some regions such as the Midlands and the South West seeing a threefold increase in prevalence. Understanding the decline in population levels of mental health, its drivers, and the policies that may tackle them represent a clear public health priority. The magnitude of this time trend has led many to consider changes in public stigma over time—“de-stigmatisation”—as an alternative explanation. We shed some light on this issue by comparing time trends in self-reported mental disorders and stigma-related indicators across English regions, which provided no support for this hypothesis. Whereas public stigma and self-reporting behaviour are likely to be related, this should not be used to downplay this public health crisis.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The HSE dataset was accessed on the UK Data Service platform.
Author contributions
TG designed the study, analysed the data, interpreted the findings, and wrote the first draft. CH provided access to the AMI dataset. CH and AM contributed to the analytic strategy, the interpretation of findings, and the writing of the paper. All authors contributed to the final version of the manuscript.
Funding
TG holds a Banting Postdoctoral Fellowship award from the Canadian Institutes of Health Research, and was also funded by the Fonds de Recherche du Québec-Santé during the start of this project. AM is funded by the UK Economic and Social Research Council (ES/W001454/1). The Time to Change evaluation was funded by the UK Government Department of Health and Social Care, Comic Relief, and Big Lottery Fund. CH was supported by these grants from 2008 to 21.
Data availability
The HSE datasets used in this project can be accessed online on the UK Data Service. The AMI dataset can be accessed by contacting the authors.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Slee A, Nazareth I, Freemantle N, Horsfall L. Trends in generalised anxiety disorders and symptoms in primary care: UK population-based cohort study. Br J Psychiatry. 2020 doi: 10.1192/bjp.2020.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gagné T, Schoon I, McMunn A, Sacker A. Mental distress among young adults in Great Britain: long-term trends and early changes during the COVID-19 pandemic. Soc Psychiatry Psychiatr Epidemiol. 2021 doi: 10.1007/s00127-021-02194-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Archer C, Turner K, Kessler D, Mars B, Wiles N. Trends in the recording of anxiety in UK primary care: a multi-method approach. Soc Psychiatry Psychiatr Epidemiol. 2022;57:375–386. doi: 10.1007/s00127-021-02131-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cybulski L, Ashcroft DM, Carr MJ, Garg S, Chew-Graham CA, Kapur N, Webb RT. Temporal trends in annual incidence rates for psychiatric disorders and self-harm among children and adolescents in the UK, 2003–2018. BMC Psychiatry. 2021;21:229. doi: 10.1186/s12888-021-03235-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller PK, Cuthbertson CA, Loveridge S. Social status influence on stigma towards mental illness and substance use disorder in the United States. Community Ment Health J. 2022;58:249–260. doi: 10.1007/s10597-021-00817-6. [DOI] [PubMed] [Google Scholar]
- 6.Hatzenbuehler ML. Structural stigma and health inequalities: research evidence and implications for psychological science. Am Psychol. 2016;71:742–751. doi: 10.1037/amp0000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dean L, Phillips M (2015) Attitudes to mental health problems and mental wellbeing. Findings from the 2015 British Social Attitudes survey
- 8.Ilic N, Henderson H, Henderson C, Evans-Lacko S, Thornicroft G (2015) Attitudes towards mental illness. Health Survey for England, vol 1, Chapter 3
- 9.Reid S, Hinchliffe S, Waterton J, Scotland, Social Research (2014) Attitudes to mental health in Scotland: Scottish social attitudes survey 2013
- 10.Kobau R, Zack MM. Attitudes toward mental illness in adults by mental illness-related factors and chronic disease status: 2007 and 2009 behavioral risk factor surveillance system. Am J Public Health. 2013;103:2078–2089. doi: 10.2105/AJPH.2013.301321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pescosolido BA, Halpern-Manners A, Luo L, Perry B. Trends in public stigma of mental illness in the US, 1996–2018. JAMA Netw Open. 2021;4:e2140202. doi: 10.1001/jamanetworkopen.2021.40202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schomerus G, Schwahn C, Holzinger A, Corrigan PW, Grabe HJ, Carta MG, Angermeyer MC. Evolution of public attitudes about mental illness: a systematic review and meta-analysis. Acta Psychiatr Scand. 2012;125:440–452. doi: 10.1111/j.1600-0447.2012.01826.x. [DOI] [PubMed] [Google Scholar]
- 13.Henderson C, Potts L, Robinson EJ. Mental illness stigma after a decade of Time to Change England: inequalities as targets for further improvement. Eur J Public Health. 2020;30:497–503. doi: 10.1093/eurpub/ckaa013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robinson EJ, Henderson C. Public knowledge, attitudes, social distance and reporting contact with people with mental illness 2009–2017. Psychol Med. 2019;49:2717–2726. doi: 10.1017/S0033291718003677. [DOI] [PubMed] [Google Scholar]
- 15.Bhavsar V, Schofield P, Das-Munshi J, Henderson C. Regional differences in mental health stigma—analysis of nationally representative data from the Health Survey for England, 2014. PLoS ONE. 2019;14:e0210834. doi: 10.1371/journal.pone.0210834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roux AVD. A glossary for multilevel analysis. J Epidemiol Community Health. 2002;56:588–594. doi: 10.1136/jech.56.8.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.NatCen Social Research, University College London, Department of Epidemiology and Public Health (2022) Health survey for England, 2018 [data collection], 2nd edn. UK Data Service, SN: 8649. 10.5255/UKDA-SN-8649-2
- 18.Evans-Lacko S, Little K, Meltzer H, Rose D, Rhydderch D, Henderson C, Thornicroft G. Development and psychometric properties of the mental health knowledge schedule. Can J Psychiatry. 2010;55:440–448. doi: 10.1177/070674371005500707. [DOI] [PubMed] [Google Scholar]
- 19.Taylor SM, Dear MJ. Scaling community attitudes toward the mentally ill. Schizophr Bull. 1981;7:225–240. doi: 10.1093/schbul/7.2.225. [DOI] [PubMed] [Google Scholar]
- 20.Evans-Lacko S, Rose D, Little K, Flach C, Rhydderch D, Henderson C, Thornicroft G. Development and psychometric properties of the reported and intended behaviour scale (RIBS): a stigma-related behaviour measure. Epidemiol Psychiatr Sci. 2011;20:263–271. doi: 10.1017/s2045796011000308. [DOI] [PubMed] [Google Scholar]
- 21.Office for National Statistics (2013) The National Statistics Socio-economic classification (NS-SEC) - Office for National Statistics. https://www.ons.gov.uk/methodology/classificationsandstandards/otherclassifications/thenationalstatisticssocioeconomicclassificationnssecrebasedonsoc2010. Accessed 10 Dec 2021
- 22.Henderson C, Thornicroft G. Stigma and discrimination in mental illness: time to Change. Lancet. 2009;373:1928–1930. doi: 10.1016/S0140-6736(09)61046-1. [DOI] [PubMed] [Google Scholar]
- 23.Evans-Lacko S, Malcolm E, West K, Rose D, London J, Rüsch N, Little K, Henderson C, Thornicroft G. Influence of Time to Change’s social marketing interventions on stigma in England 2009–2011. Br J Psychiatry Suppl. 2013;55:s77–88. doi: 10.1192/bjp.bp.113.126672. [DOI] [PubMed] [Google Scholar]
- 24.Sampogna G, Bakolis I, Evans-Lacko S, Robinson E, Thornicroft G, Henderson C. The impact of social marketing campaigns on reducing mental health stigma: results from the 2009–2014 time to change programme. Eur Psychiatry. 2017;40:116–122. doi: 10.1016/j.eurpsy.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 25.Stuckler D, Reeves A, Loopstra R, Karanikolos M, McKee M. Austerity and health: the impact in the UK and Europe. Eur J Public Health. 2017;27:18–21. doi: 10.1093/eurpub/ckx167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Doorn J, Verhoef PC, Bijmolt THA. The importance of non-linear relationships between attitude and behaviour in policy research. J Consum Policy. 2007;30:75–90. doi: 10.1007/s10603-007-9028-3. [DOI] [Google Scholar]
- 27.Glasman LR, Albarracín D. Forming attitudes that predict future behavior: a meta-analysis of the attitude-behavior relation. Psychol Bull. 2006;132:778–822. doi: 10.1037/0033-2909.132.5.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manescu EA, Robinson EJ, Henderson C. Attitudinal and demographic factors associated with seeking help and receiving antidepressant medication for symptoms of common mental disorder. BMC Psychiatry. 2020;20:579. doi: 10.1186/s12888-020-02971-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ingram E, Jones R, Schofield P, Henderson C. Small area deprivation and stigmatising attitudes towards mental illness: a multilevel analysis of Health Survey for England (2014) data. Soc Psychiatry Psychiatr Epidemiol. 2019;54:1379–1389. doi: 10.1007/s00127-019-01722-w. [DOI] [PubMed] [Google Scholar]
- 30.Stewart H, Jameson JP, Curtin L. The relationship between stigma and self-reported willingness to use mental health services among rural and urban older adults. Psychol Serv. 2015;12:141–148. doi: 10.1037/a0038651. [DOI] [PubMed] [Google Scholar]
- 31.Potts LC, Henderson C. Moderation by socioeconomic status of the relationship between familiarity with mental illness and stigma outcomes. SSM - Popul Health. 2020;11:100611. doi: 10.1016/j.ssmph.2020.100611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duncan C, Jones K, Moon G. Psychiatric morbidity: a multilevel approach to regional variations in the UK. J Epidemiol Community Health. 1995;49:290–295. doi: 10.1136/jech.49.3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Whitley R, Wang J. Good News? A longitudinal analysis of newspaper portrayals of mental illness in Canada 2005 to 2015. Can J Psychiatry Rev Can Psychiatr. 2017;62:278–285. doi: 10.1177/0706743716675856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hildersley R, Potts L, Anderson C, Henderson C. Improvement for most, but not all: changes in newspaper coverage of mental illness from 2008 to 2019 in England. Epidemiol Psychiatr Sci. 2020 doi: 10.1017/S204579602000089X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Poushter J (2017) Not everyone in advanced economies is using social media. In: Pew Res. Cent. https://www.pewresearch.org/fact-tank/2017/04/20/not-everyone-in-advanced-economies-is-using-social-media/. Accessed 27 Jun 2022
- 36.Cheng J, Burke M, Gant B. Country differences in social comparison on social media. Proc ACM Hum-Comput Interact. 2021 doi: 10.1145/3434179. [DOI] [Google Scholar]
- 37.Manago B, Pescosolido BA, Olafsdottir S. Icelandic inclusion, German hesitation and American fear: a cross-cultural comparison of mental-health stigma and the media. Scand J Public Health. 2019;47:90–98. doi: 10.1177/1403494817750337. [DOI] [PubMed] [Google Scholar]
- 38.Blakely TA, Woodward AJ. Ecological effects in multi-level studies. J Epidemiol Community Health. 2000;54:367–374. doi: 10.1136/jech.54.5.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zoubaa S, Dure S, Yanos PT. Is there evidence for defensive projection? The impact of subclinical mental disorder and self-identification on endorsement of stigma. Stigma Health. 2020;5:434–441. doi: 10.1037/sah0000217. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The HSE datasets used in this project can be accessed online on the UK Data Service. The AMI dataset can be accessed by contacting the authors.