Dear Editor,
We read with interest the research results of Li et al.1 and Zhou et al.2 published on this journal, which reported the decline of Streptococcus pneumoniae and Haemophilus influenzae infection in children under the impact of COVID-19 pandemic. Li et al.3 compared the effect of COVID-19 on the incidence of Escherichia coli infections in respiratory system and digestive system in children, the results indicated larger effect on the respiratory system infection. However, no data were available on the prevalence of Acinetobacter baumannii causing lower respiratory infections especially in the bronchoalveolar lavage fluid (BALF) samples of children before and after the COVID-19 pandemic.
Pneumonia is a leading cause of death among children under five years old globally, which accounted for 12.8% causing about 920,000 deaths every year.4 The pathogens causing pneumonia varied, hence identification of pneumonia etiology is critical for the management and treatment of the disease. Multiple samples were used to detect the pathogens, whereas BALF is the ideal specimen for detecting the causative pathogen apart from lung tissue or aspirate.5 A. baumannii is a Gram negative opportunistic human pathogen, which could cause a wide spectrum of illness including bloodstream infection, pneumonia, and endocarditis.6 It has a remarkable capacity to develop antimicrobial resistance, and multidrug resistant strains may account for ∼45% of all isolates, which made them a serious health threat.7 The outbreak of COVID-19 pandemic has changed the lifestyles of human beings, and the measures to control the transmission of SARS-CoV-2 may also affect the prevalence of other respiratory pathogens.1, 2, 3 , 8 Hence, analysis of the pathogen distributions in the BALF cultures and the prevalence trend of A.baumannii infection in children before and after the COVID-19 pandemic is critical for hospital infection prevention and control.
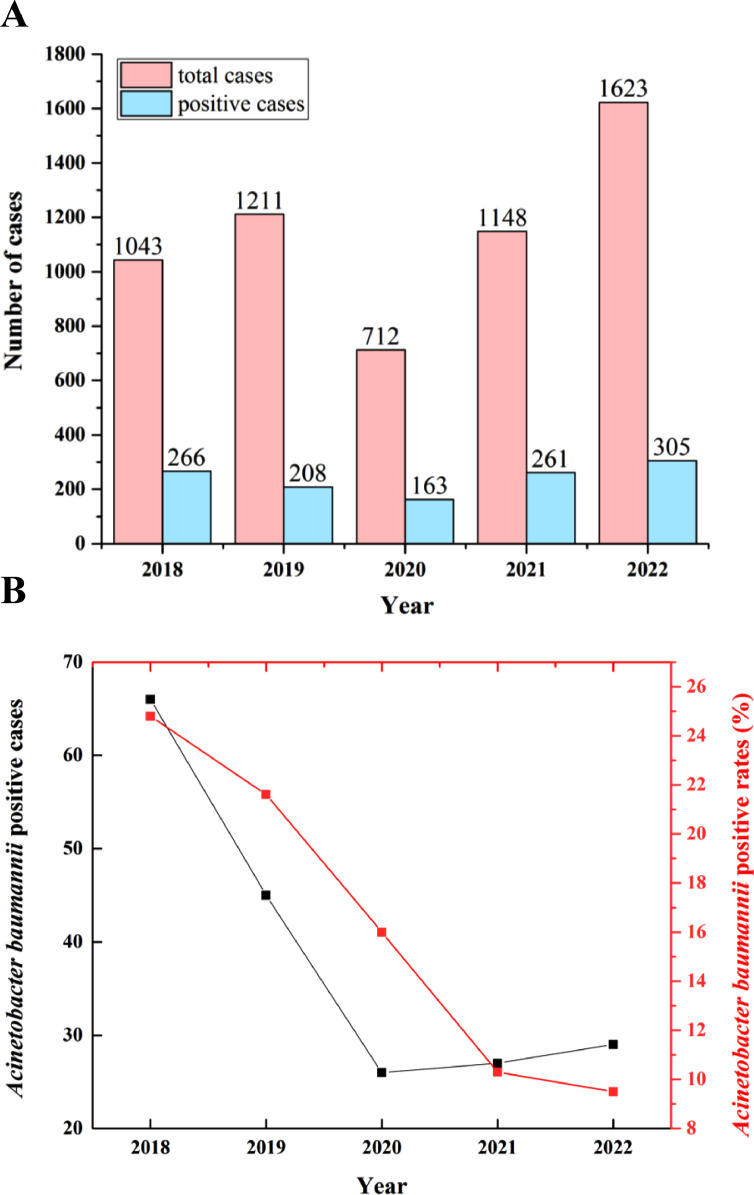
In this study, we firstly compared the total numbers of BALF cultures and the total positive numbers to analyze the impact of COVID-19 pandemic on the pathogen prevalence of children in Henan Children's hospital between January 2018 and November 2022. A total of 5737 children were included (n = 1043 in 2018, n = 1211 in 2019, n = 712 in 2020, n = 1148 in 2021 and n = 1623 in 2022) (Fig. 1 A). The total positive numbers with reported pathogen were 1203 (n = 266 in 2018, n = 208 in 2019, n = 163 in 2020, n = 261 in 2021 and n = 305 in 2022). A significant decrease in the total numbers and positive numbers was found in 2020, the first year of COVID-19 pandemic. However, the total positive rates were not following the decreasing trend.
Fig. 1.
The total numbers of BALF cultures and the total positive numbers (A) and the total number and the positive rates of A. baumannii infection (B) in children from 2018 to 2022.
Further, the pathogen distributions were analyzed with positive culture results before and after the COVID-19 pandemic. Among the positive BALF cultures, the most common pathogens included A. baumannii, S. pneumoniae, Klebsiella pneumoniae, Burkholderia cepacia complex, Staphylococcus aureus, Candida albicans, Pseudomonas aeruginosa and E. coli (Table 1 ), which accounted for over 75% of the total pathogens detected. Among the most common pathogens, a decrease in A. baumannii infections was indicated by the data from 2018 to 2022 (Fig. 1B). The positive rates of S. pneumoniae decreased from 2018 to 2020, while increased in 2021 and 2022. S. pneumoniae was not detected in 2020, whereas a very high rate (40.66%) was detected in 2022. P. aeruginosa increased from 2018 to 2020, while decreased in 2021 and 2022. Other pathogens kept a relatively stable state. Hence, our data indicated significant effect of COVID-19 on the prevalence of A. baumannii infections, which accounted for a high proportion among the positive BALF pathogens before COVID-19 pandemic.
Table 1.
The pathogen distribution of BAFL cultures in children from 2018 to 2022.
| Pathogen | 2018 (n = 266) | 2019 (n = 208) | 2020 (n = 163) | 2021 (n = 261) | 2022 (n = 305) |
|---|---|---|---|---|---|
| Acinetobacter baumannii | 66 (24.81%) | 45 (21.63%) | 26 (15.95%) | 27 (10.34%) | 29 (9.51%) |
| Streptococcus pneumoniae | 65 (24.43%) | 20 (9.62%) | 0 (0%) | 37 (14.18%) | 124 (40.66%) |
| Klebsiella pneumoniae | 28 (10.53%) | 21 (10.10%) | 26 (15.95%) | 43 (16.48%) | 14 (4.59%) |
| Burkholderia cepacia complex | 25 (9.40%) | 20 (9.62%) | 19 (11.66%) | 28 (10.73%) | 24 (7.87%) |
| Staphylococcus aureus | 16 (6.02%) | 16 (7.69%) | 11 (6.75%) | 16 (6.13%) | 33 (10.82%) |
| Candida albicans | 17 (6.40%) | 29 (13.94%) | 17 (10.43%) | 30 (11.49%) | 25 (8.20%) |
| Pseudomonas aeruginosa | 14 (5.26%) | 16 (7.69%) | 16 (9.82%) | 12 (4.60%) | 14 (4.59%) |
| E. coli | 8 (3.01%) | 8 (3.85%) | 7 (4.29%) | 12 (4.60%) | 6 (1.97%) |
| Other pathogens | 27 (10.15%) | 33 (15.87%) | 41 (25.15%) | 56 (21.46%) | 36 (11.80%) |
In conclusion, our data indicated that the distribution of the pathogens may vary in different regions and for different pathogens. Among the pathogens detected, A. baumannii decreased gradually in the COVID-19 pandemic. Hence, continuous observations are required to reveal the epidemiology information to provide clues for the prevention and control of related diseases.
Declaration of Competing Interest
The authors declare no conflict of interests.
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (31900116) and the Medical Science and Technology Projects of Henan Province (LHGJ20190955).
References
- 1.Li Y., Guo Y., Duan Y. Changes in Streptococcus pneumoniae infection in children before and after the COVID-19 pandemic in Zhengzhou, China. J Infect. 2022;85(3):e80–e81. doi: 10.1016/j.jinf.2022.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou J., Zhao P., Nie M., Gao K., Yang J., Sun J. Changes of Haemophilus influenzae infection in children before and after the COVID-19 pandemic, Henan, China. J Infect. 2022 doi: 10.1016/j.jinf.2022.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Liping, Song Chunlan, Li Peng, Li Y. Changes of Escherichia coli infection in children before and after the COVID-19 pandemic in Zhengzhou, China. J Infect. 2022 doi: 10.1016/j.jinf.2022.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu L., Oza S., Hogan D., Chu Y., Perin J., Zhu J., et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. The Lancet. 2016;388(10063):3027–3035. doi: 10.1016/S0140-6736(16)31593-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang R., Wu Y., Deng G., Deng J. Value of sputum Gram stain, sputum culture, and bronchoalveolar lavage fluid Gram stain in predicting single bacterial pathogen among children with community-acquired pneumonia. BMC Pulm Med. 2022;22(1):427. doi: 10.1186/s12890-022-02234-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jalal D., Elzayat M.G., Diab A.A., El-Shqanqery H.E., Samir O., Bakry U., et al. Deciphering Multidrug-Resistant Acinetobacter baumannii from a Pediatric Cancer Hospital in Egypt. mSphere. 2021;6(6) doi: 10.1128/mSphere.00725-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harding C.M., Hennon S.W., Feldman M.F. Uncovering the mechanisms of Acinetobacter baumannii virulence. Nat Rev Microbiol. 2018;16(2):91–102. doi: 10.1038/nrmicro.2017.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meyer Sauteur P.M., Beeton M.L., Uldum S.A., Bossuyt N., Vermeulen M., Loens K., et al. Mycoplasma pneumoniae detections before and during the COVID-19 pandemic: results of a global survey, 2017 to 2021. Euro Surveill. 2022;27(19) doi: 10.2807/1560-7917.ES.2022.27.19.2100746. [DOI] [PMC free article] [PubMed] [Google Scholar]