Abstract
Objective:
This study aims to determine quantitatively the mediation effects of multiple cardiovascular risk factors on the associations of childhood body mass index (BMI) and its cumulative burden with adult carotid intima-media thickness (cIMT).
Methods:
The longitudinal cohort consisted of 1391 adults who had been examined for BMI 4–15 times over 35.0 years on average since childhood and had data on adult cIMT, systolic blood pressure (SBP), low-density lipoprotein cholesterol (LDLC), atherogenic index of plasma (AIP) and serum glucose. The area under the curve (AUC) was used as a measure of cumulative burden of BMI.
Results:
After adjusting for covariates, the total effects (standardized regression coefficient) of childhood BMI (0.138), adult BMI (0.111) and BMI AUC (0.150) on cIMT were all significant (P<0.001) without mediators included in the model. The mediation effects of adult SBP, glucose, AIP and LDLC were 8.0%, 4.3%, 3.6% and 0.0%, respectively, in the model with childhood BMI as the predictor, 23.4%, 15.3%, 12.6% and 7.2%, respectively, with adult BMI as the predictor, and 14.7%, 8.7%, 6.0% and 2.0%, respectively, with BMI AUC as the predictor. The direct effects on cIMT were 0.117 (P<0.001) for childhood BMI, 0.046 (P=0.224) for adult BMI and 0.103 (P<0.001) for BMI AUC after removing the mediation effects.
Conclusions:
The long-term deleterious impact of adiposity on subclinical changes in vascular structure begins early in life and is accumulated over lifetime. Excess adiposity and higher cIMT are linked partly through other cardiovascular risk factors in later life, especially elevated BP and glucose.
Keywords: childhood, obesity, cumulative burden, intima-media thickness, mediation effect
Graphical Abstract
INTRODUCTION
Increased arterial wall thickness, a surrogate marker of early atherosclerosis, is associated with cardiovascular (C-V) morbidity and mortality. The carotid intima-media thickness (cIMT) measured noninvasively by ultrasound has been widely used to assess C-V risk (1–4). Extensive data have established a strong association between cIMT and traditional C-V risk factors, including adverse levels of body mass index (BMI), blood pressure (BP), triglycerides (TG), lipoproteins and glucose (5–9).
Numerous studies have demonstrated that obesity is one of the major predictors of cIMT (5–9). Obesity is associated with high cIMT even in children and predicts increased adult cIMT (10–14). Moreover, obesity is also an independent predictor of other C-V risk factors (15–17). These observations indicate that C-V risk factors are intermediate variables between obesity and increased cIMT. Although the concept has been generally accepted that obesity and subclinical changes in the C-V system are linked through other C-V risk factors (18–20), the degree of the mediation effects of intermediate variables on the obesity-cIMT association has not been reported.
Atherosclerosis and its risk factors originate early in life (10–12,21,22). Generally, abnormal cIMT is considered subclinical changes in vascular structure and is thought to be the result of lifespan cumulative exposure to multiple C-V risk factors and their complex interactions (23–25). It is well known that childhood obesity persists into later life (26–28), and increased adult BMI is strongly associated with hypertension, dyslipidemia and hyperglycemia (15–17). To date, no studies have focused on the mediation effects of traditional C-V risk factors on the obesity-cIMT association in terms of early life body weight and its lifelong cumulative burden from childhood to adulthood. Further, it is not clear whether obesity is directly associated with increased cIMT independent of other risk factors.
In the current study, we aimed to determine quantitatively the mediation effects of multiple C-V risk factors on the association of childhood and adulthood BMI and its lifetime burden with adult cIMT in a longitudinal cohort enrolled in the Bogalusa Heart Study.
METHODS
The data and materials have been made publicly available at the National Heart, Lung and Blood Institute Biologic Specimen and Data Repository and can be accessed at https://biolincc.nhlbi.nih.gov/studies/bhs.
Study Cohort
The Bogalusa Heart Study is a series of long-term epidemiologic studies in a semi-rural biracial (65% white and 35% black) community in Bogalusa, Louisiana beginning from 1973. This study focuses on the early natural history of C-V disease since childhood (29). In the community of Bogalusa, 9 cross-sectional surveys of children aged 4–19 years and 12 cross-sectional surveys of adults aged 20–58 years who had been previously examined as children were conducted between 1973 and 2016. Linking these repeated cross-sectional surveys conducted every 2–3 years has resulted in serial observations from childhood to adulthood. The current longitudinal study cohort consisted of 1391 adult subjects (929 whites and 462 blacks; 42.7% males; age range=23.8–56.8 years and mean age=44.4 years at follow-up) who had BMI measured for 4–15 times (at least 2 times in childhood and adulthood each). The mean number of visits was 8.8, and the mean follow-up period was 35.0 years. This cohort also had data on ultrasonography of cIMT and C-V risk factors, including BMI, BP, TG, low-density (LDLC) and high-density (HDLC) lipoprotein cholesterol, and serum fasting glucose collected in three adult surveys during 2001–2016. For the participants who had cIMT and C-V risk factors measured more than once, the values in the last survey were used for analysis.
All subjects in this study gave informed consent at each examination, and for those under 18 years of age, consent of a parent/guardian was obtained. Study protocols were approved by the Institutional Review Board of the Tulane University Health Sciences Center.
General Examinations
Standardized protocols were used by trained examiners across all surveys since 1973 (29). BMI (weight in kilograms divided by the square of the height in meters) was used as a measure of adiposity. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded between 8:00 AM and 10:00 AM on the right arm in a relaxed, sitting position by 2 trained observers (3 replicates each). The mean values of the 6 readings were used for analysis. Subjects were instructed to fast for 12 hours before screening. Serum TG, LDLC, HDLC and glucose were measured as part of a multiple chemistry profile (SMA20; Laboratory Corporation of America, Burlington, NC). Atherogenic index of plasma (AIP) defined as TG/HDLC was used as a measure of dyslipidemia (30) and log-transformed for analysis due to its skewed distribution. Information on anti-hypertensive, lipid-lowering and anti-diabetic medications, smoking and alcohol use was obtained by means of a staff administered standardized questionnaire. Current smoking and drinking were defined as smoking at least 1 cigarette per day and consuming alcohol ≥3 days per week, respectively, during last 12 months.
Carotid Ultrasonography
Carotid artery ultrasound images were obtained by trained sonographers using a Toshiba digital ultrasound instrument with a 7.5-MHz linear array transducer. The images were recorded at common carotid, carotid bulb and internal carotid arteries bilaterally according to the previously developed protocol for the Atherosclerosis Risk in Communities study (31). The mean of the maximum cIMT readings of the 3 right and 3 left far walls for the common, bulb and internal segments was used to determine the composite cIMT for analysis.
Statistical Methods
Long-term burden of BMI was measured as the area under the curve (AUC) which was calculated using statistical models we previously described (32,33). In brief, growth curves of BMI measured multiple times from childhood to adulthood were constructed using a random-effects model with R package “nlme” (version 3.1–148). A cubic curve was fitted in race-sex groups. The AUC was calculated as the integral on the curve parameters during the follow-up period for each subject (Figure 1). Because subjects had different follow-up periods, the AUC values were divided by the number of follow-up years.
Figure 1.
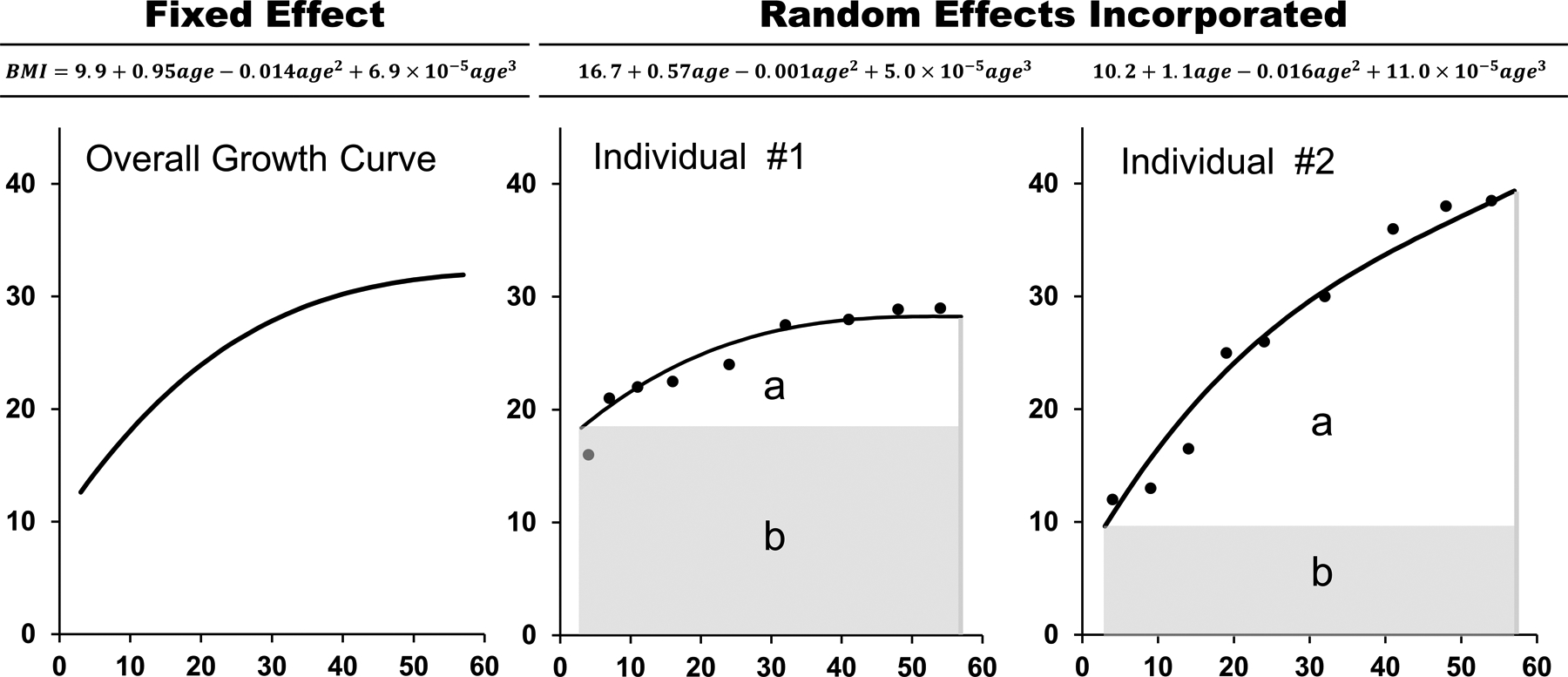
The area under the curve (AUC) of body mass index with two individuals as an example
a = incremental AUC; b = baseline AUC
Total AUC = incremental AUC + baseline AUC
The general mediation analysis model (34,35), also known as third variable model (36), was constructed to examine the mediation effects through SBP, LDLC, AIP and glucose on the BMI-cIMT association. The mediators were selected based on the biological mechanisms underlying the relationships between obesity, hypertension, dyslipidemia, diabetes and atherosclerosis (Figure S1 in the Supplement). Covariates included in the mediation models for adjustment were race, sex, age, smoking, alcohol drinking in the last adult survey and follow-up years. These covariates were chosen to make the results comparable to the reports from our previous (11,14) and other longitudinal cohorts followed since childhood (12,13,24). The mediation parameters were also estimated in the models with additional adjustment for antihypertensive, lipid-lowering and antidiabetic medications in a sensitivity analysis. As shown in Figure 2, BMI was the predictor variable (X), SBP, LDLC, AIP and glucose the mediators (M), and cIMT the dependent variable (Y). The product method (35) was used to estimate the mediation model parameters for continuous variables. Multiple mediators were included in one model as well as in separate models with individual mediators. In general, there are four steps for the mediation analysis: 1) showing that BMI determines cIMT (Model Y = c X) where c is total effect; 2) showing that BMI affects the mediators (Model M = β1 X) where β1 is indirect effect 1; 3) showing that BMI determines cIMT controlling for the mediators (Model Y = β2 Ms + c’ X) where β2 is indirect effect 2, and c’ is direct effect; 4) indirect effect (βInd) is calculated as β1 × β2. Then mediation effect (%) is determined by βInd/c × 100%. Percentile bootstrap 95% confidence intervals of βInd, c’ and mediation effect were calculated using 1000 times bootstrap sampling. Significance of βInd was tested using the method previously described (37). Prior to mediation analyses, childhood BMI and BMI AUC values were adjusted for childhood age and average age, respectively, by regression residual analyses and then standardized with Z-transformation to avoid collinearity of childhood age, follow-up years and adult age in the same model. Mediation analyses were performed using R package “bruceR” (version 0.8.9). The mediation effect of adult BMI on the childhood BMI-adult cIMT association was examined in a separate mediation model. Covariate-adjusted mean values of adult cIMT were compared between subgroups classified by the combination of low/high childhood BMI and low/high adult mediators. Low and high levels were defined as below and above their race- and sex-specific medians, respectively.
Figure 2.
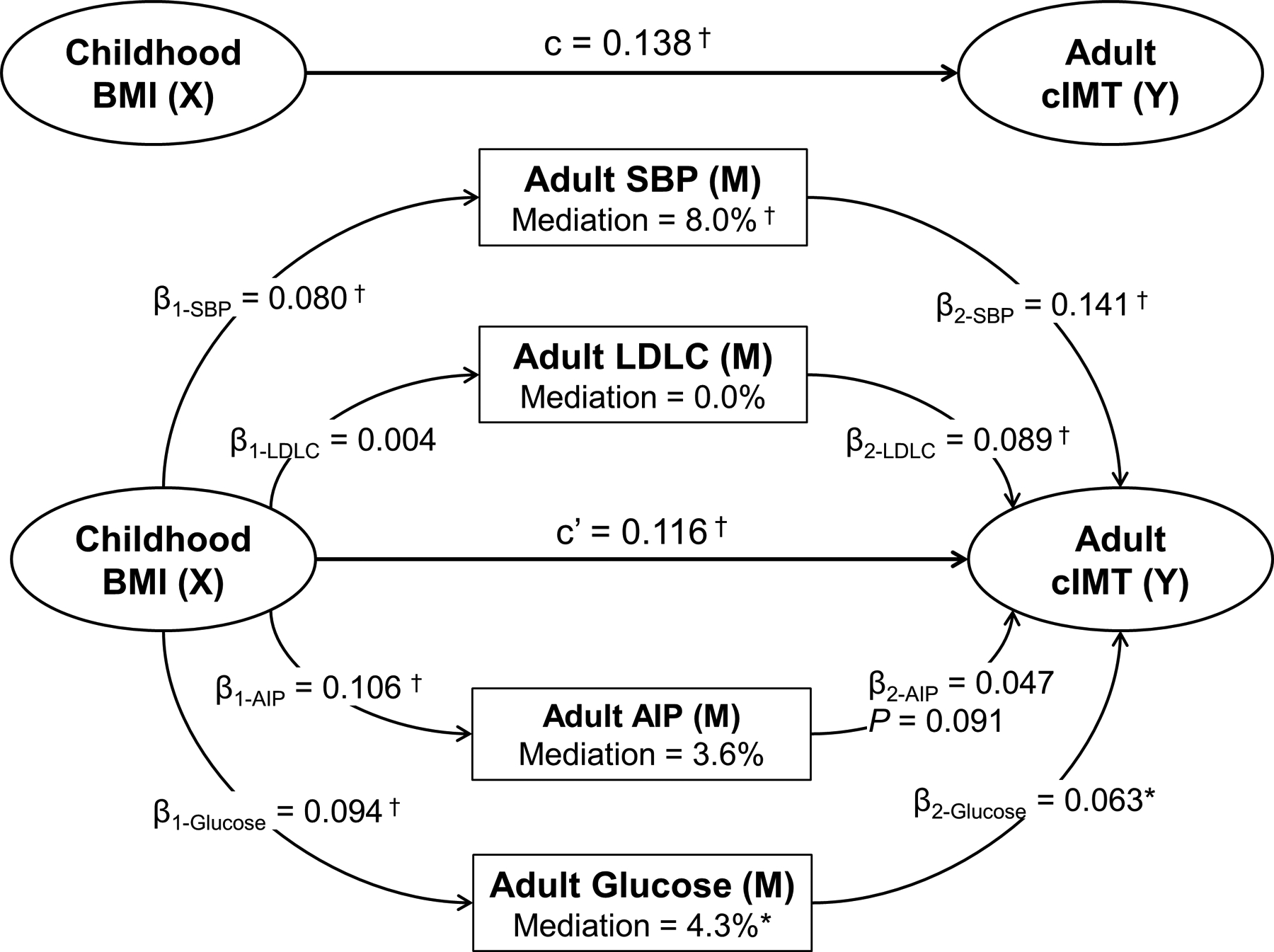
Mediation effects of multiple adult risk factors on the childhood BMI-adult cIMT association
β, c and c’ are standardized regression coefficients.
c=total effect; c’=direct effect; β1=indirect effect 1; β2=indirect effect 2; βInd=indirect effect; BMI=body mass index; cIMT=carotid intima-media thickness; SBP=systolic blood pressure; LDLC=low-density lipoprotein cholesterol; AIP=atherogenic index of plasma
Total βInd= 0.021, P < 0.001 (the sum of the four indirect effects)
* P < 0.05 and † P < 0.01 for being different from 0
RESULTS
Table 1 summarizes the study variables by race and sex. Childhood BMI (values at the first exam) did not show significant race and sex differences, while adult BMI (values at the last exam) and BMI AUC had significant sex differences in whites (males>females) and blacks (males<females), and race difference in females (blacks>whites). Adult SBP, DBP, TG, AIP and composite cIMT showed significant race and sex differences. Other variables did not differ significantly and consistently between race and sex groups.
Table 1.
Characteristics of study variables by race and sex
| Characteristic | Whites (n = 929) | Blacks (n = 462) | P for Race Difference | |||
|---|---|---|---|---|---|---|
| Males (n = 408) |
Females (n = 521) |
Males (n = 186) |
Females (n = 276) |
Males | Females | |
| Childhood | ||||||
| Age (yr) | 9.7 (3.0) | 9.3 (3.1) | 9.6 (2.9) | 9.2 (2.9) | 0.887 | 0.729 |
| BMI (kg/m2) | 17.6 (3.42) | 17.4 (3.3) | 17.2 (3.3) | 17.4 (3.7) | 0.238 | 0.736 |
| Adulthood | ||||||
| Age (yr) | 44.4 (7.3) | 44.3 (7.0) | 44.5 (6.9) | 44.7 (7.5) | 0.933 | 0.461 |
| Follow-up years | 34.8 (6.2) | 35.0 (5.9) | 34.9 (6.0) | 35.5 (6.2) | 0.868 | 0.292 |
| BMI (kg/m2) | 30.5 (6.3) | 29.4 (7.3)* | 30.3 (8.0) | 33.5 (8.6)* | 0.760 | <0.001 |
| SBP (mmHg) | 122.8 (13.1) | 115.0 (12.9)* | 130.8 (17.1) | 124.9 (18.9)* | <0.001 | <0.001 |
| DBP (mmHg) | 79.8 (9.6) | 75.1 (9.5)* | 84.2 (12.6) | 81.1 (11.9)* | <0.001 | <0.001 |
| LDL-C (mg/dL) | 122.0 (37.2) | 121.9 (33.3) | 113.8 (37.7) | 114.1 (36.3) | 0.014 | 0.002 |
| HDL-C (mg/dL) | 41.9 (11.6) | 54.3 (15.2)* | 52.1 (16.4) | 54.9 (15.0) | <0.001 | 0.570 |
| TG (mg/dL) | 152.1 (85.7) | 125.9 (69.1)* | 120.8 (79.9) | 100.4 (54.6)* | <0.001 | <0.001 |
| AIP† | 3.2 [2.0, 5.3] | 2.1 [1.3, 3.3]* | 2.0 [1.3, 3.2] | 1.6 [1.1, 2.5]* | <0.001 | <0.001 |
| Glucose (mg/dL) | 101.2 (27.1) | 94.9 (24.9)* | 100.9 (31.0) | 101.0 (33.6) | 0.889 | 0.003 |
| Smoker, n (%) | 127 (31.1) | 177 (34.0) | 80 (43.0) | 80 (29.0)* | 0.006 | 0.176 |
| Drinker, n (%) | 194 (47.6) | 220 (42.2) | 102 (54.8) | 114 (41.3)* | 0.119 | 0.861 |
| AUC | ||||||
| Average age (yr) | 24.9 (4.5) | 24.5 (4.6) | 24.1 (4.6) | 24.0 (4.6) | 0.050 | 0.134 |
| BMI AUC (kg/m2) | 26.0 (4.6) | 25.1 (5.4)* | 25.8 (5.6) | 27.7 (6.3)* | 0.642 | <0.001 |
| Adult cIMT (mm) | ||||||
| Composite | 0.80 (0.19) | 0.71 (0.14)* | 0.84 (0.17) | 0.80 (0.19)* | 0.036 | <0.001 |
| Internal | 0.85 (0.35) | 0.76 (0.35)* | 0.88 (0.38) | 0.81 (0.38) | 0.394 | 0.061 |
| Bulb | 1.21 (0.55) | 1.06 (0.45)* | 1.12 (0.41) | 1.10 (0.39) | 0.054 | 0.183 |
| Common | 0.95 (0.30) | 0.84 (0.25)* | 0.95 (0.27) | 0.90 (0.25) | 0.742 | 0.002 |
Data are presented as mean (SD) or median [interquartile range].
BMI=body mass index; SBP=systolic blood pressure; DBP=diastolic blood pressure; LDLC=low-density lipoprotein cholesterol; HDLC=high-density lipoprotein cholesterol; TG=Triglycerides; AIP=atherogenic index of plasma (TG/HDLC); AUC=area under the curve; cIMT=carotid intima-media thickness
, P < 0.05 for sex difference within racial groups
, median [interquartile range]
Figure 2 presents the mediation model parameters with childhood BMI as the predictor, adult risk factors as the mediators and cIMT as the outcome, adjusting for age, race, sex, smoking, alcohol use and follow-up years. The mediation effects of adult SBP, glucose, AIP and LDLC were 8.0%, 4.3%, 3.6% and 0.0%, respectively. In Figure 3 with adult BMI as the predictor, the mediation effects of adult SBP, glucose, AIP and LDLC were 23.4%, 15.3%, 12.6% and 7.2%, respectively. In Figure 4 with BMI AUC as the predictor, the mediation effects of adult SBP, glucose, AIP and LDLC were 14.7%, 8.7%, 6.0% and 2.0%, respectively. The standard errors and 95% confidence intervals of the mediation parameters are provided in Table S1 in the Supplement. The results of mediation analyses with additional adjustment for antihypertensive, lipid-lowering and antidiabetic medications are presented in Table S2 in the Supplement. In general, the mediation parameters were slightly weaker than those in Table S1 in the Supplement, but their trends remained considerably similar.
Figure 3.
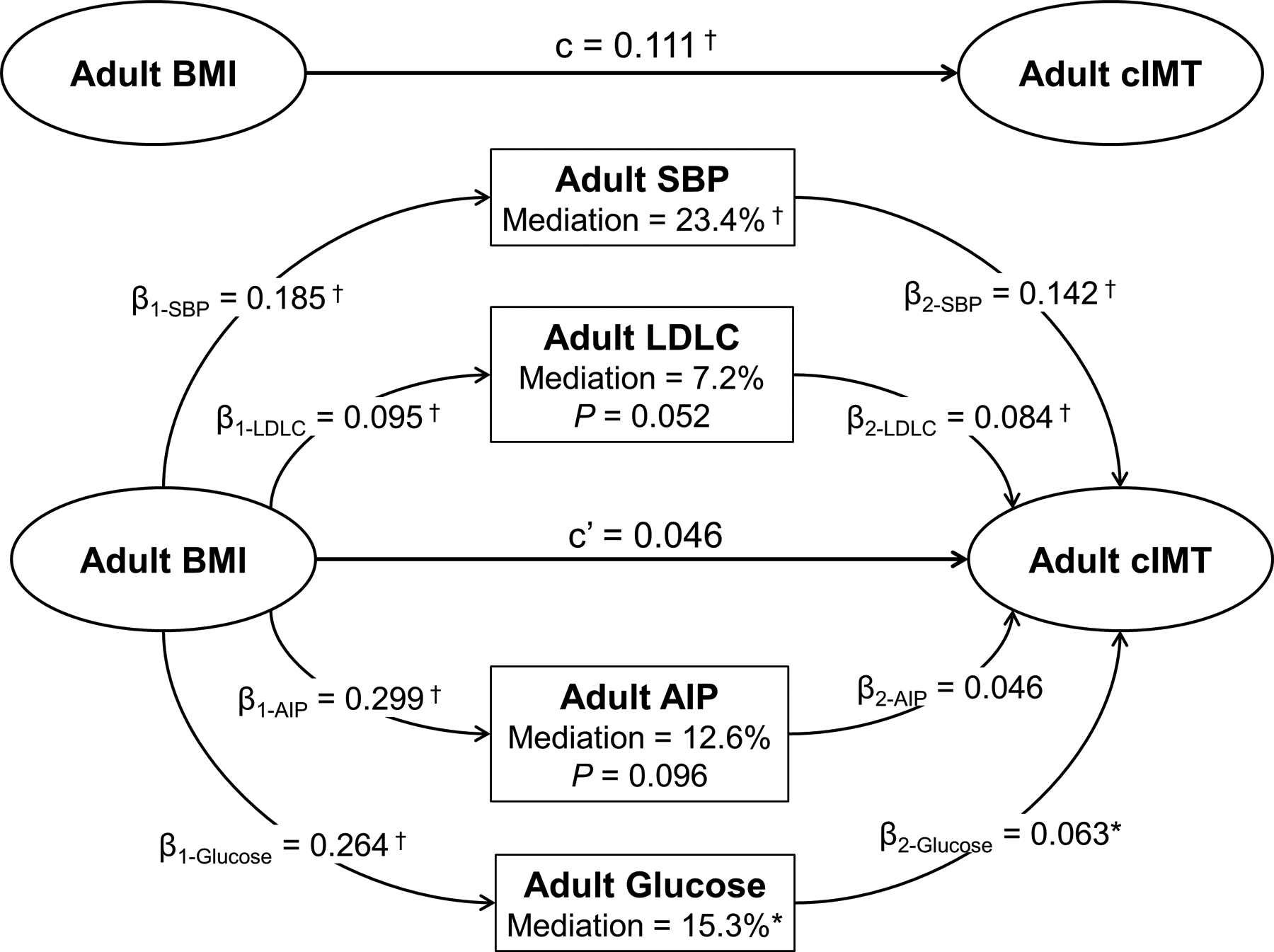
Mediation effects of multiple adult risk factors on the adult BMI-cIMT association
β, c and c’ are standardized regression coefficients.
c=total effect; c’=direct effect; β1=indirect effect 1; β2=indirect effect 2; βInd=indirect effect; BMI=body mass index; cIMT=carotid intima-media thickness; SBP=systolic blood pressure; LDLC=low-density lipoprotein cholesterol; AIP=atherogenic index of plasma
Total βInd= 0.065, P < 0.001 (the sum of the four indirect effects)
* P < 0.05 and † P < 0.01 for being different from 0
Figure 4.
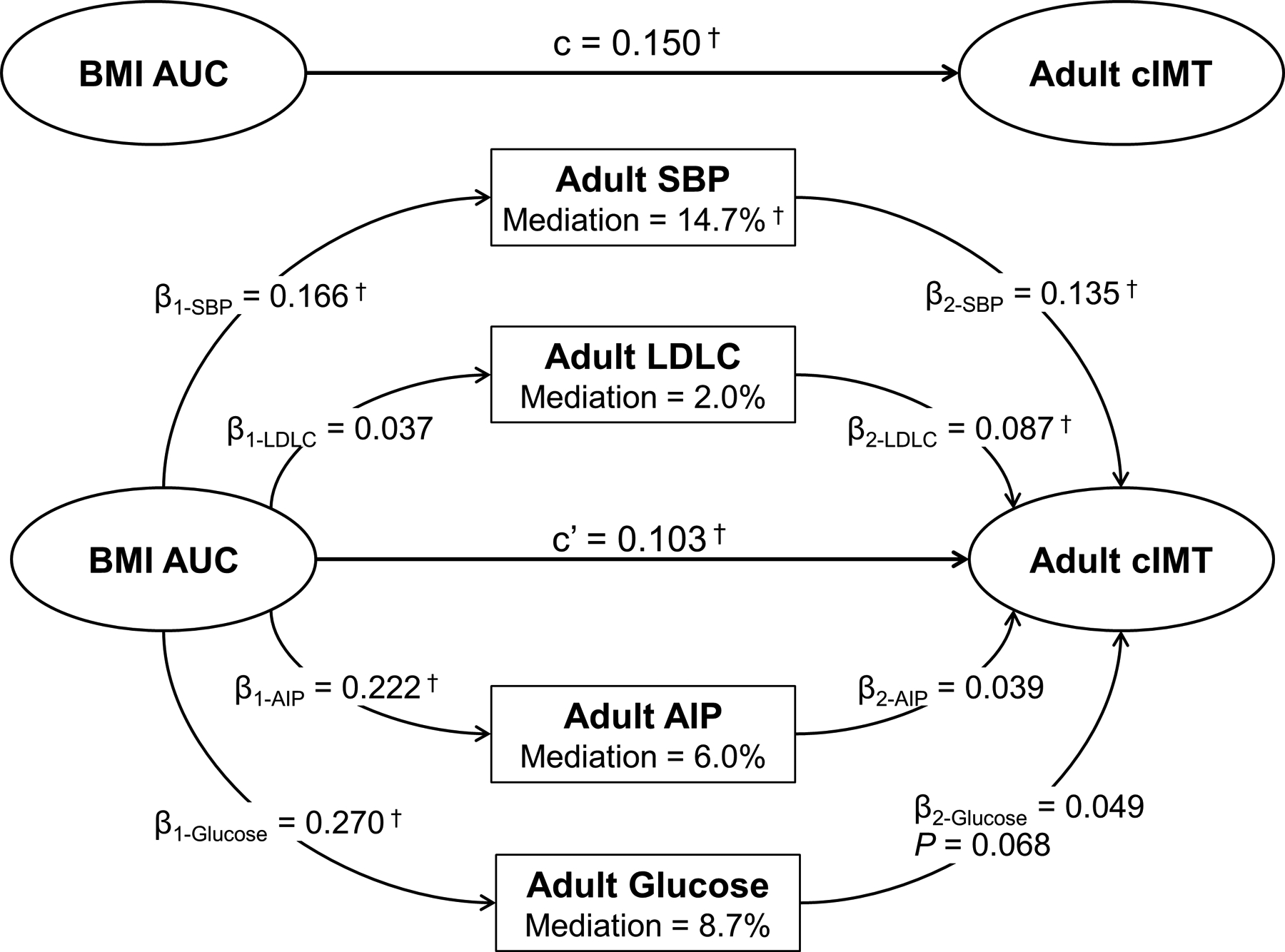
Mediation effects of multiple adult risk factors on the BMI AUC-adult cIMT association
β, c and c’ are standardized regression coefficients.
c=total effect; c’=direct effect; β1=indirect effect 1; β2=indirect effect 2; βInd=indirect effect; BMI=body mass index; AUC=area under the curve; cIMT=carotid intima-media thickness; SBP=systolic blood pressure; LDLC=low-density lipoprotein cholesterol; AIP=atherogenic index of plasma
Total βInd= 0.047, P < 0.001 (the sum of the four indirect effects)
* P < 0.05 and † P < 0.01 for being different from 0
In summary, Figures 2–4 show that the total effects (standardized regression coefficient) of childhood BMI (c=0.138), adult BMI (c=0.111) and BMI AUC (c=0.150) on cIMT were all significant (P<0.001) without mediators included in the model. Adult SBP, glucose, AIP and LDLC had the same order of their mediation effect sizes in the three models. Multiple mediators showed a mediating effect of 58.5% in total on the adult BMI-cIMT association, 31.4% in total on the BMI AUC-cIMT association and 15.9% in total on the childhood BMI-cIMT association. The direct effects on cIMT were c’=0.117 (P<0.001) for childhood BMI, c’=0.046 (P=0.224) for adult BMI and c’=0.103 (P<0.001) for BMI AUC after excluding the mediation effects.
Table 2 shows mediation analyses in separate models with individual mediators to assess the influence of inter-correlation between multiple mediators on the parameter estimation. Compared to the multiple mediator model, individual mediator mediation analyses had relatively greater magnitude of the mediation effects but similar trends in the parameters, with SBP having the highest and LDLC having the lowest mediation effects.
Table 2.
Mediation effect parameters in separate models with a single mediator and with adult cIMT as the outcome
| Predictor | Mediator | c | β1 | β2 | βInd | c’ | Mediation effect (%) |
|---|---|---|---|---|---|---|---|
| Childhood BMI | Adult SBP | 0.138 (0.025)* | 0.080 (0.025)* | 0.166 (0.027)* | 0.013 [0.005, 0.025]* |
0.125 [0.066, 0.185]* |
9.4 [2.2, 16.6]* |
| Adult LDLC | 0.138 (0.025)* | 0.004 (0.027) | 0.110 (0.025)* | 0.000 [−0.007, 0.008] |
0.137 [0.079, 0.198]* |
0.0 [−5.1, 5.8] |
|
| Adult AIP | 0.138 (0.025)* | 0.106 (0.025)* | 0.101 (0.027)* | 0.011 [0.005, 0.019]* |
0.127 [0.068, 0.189]* |
8.0 [2.0, 13.9]* |
|
| Adult Glucose | 0.138 (0.025)* | 0.094 (0.026)* | 0.096 (0.025)* | 0.009 [0.003, 0.018]* |
0.129 [0.068, 0.193]* |
6.5 [0.7, 12.3]* |
|
| Adult BMI | Adult SBP | 0.111 (0.025)* | 0.185 (0.025)* | 0.161 (0.027)* | 0.030 [0.016, 0.048]* |
0.081 [0.017, 0.156]* |
27.0 [11.7, 42.3]* |
| Adult LDLC | 0.111 (0.025)* | 0.095 (0.027)* | 0.102 (0.025)* | 0.010 [0.003, 0.020]* |
0.101 [0.040, 0.169]* |
9.0 [1.5, 16.5]* |
|
| Adult AIP | 0.111 (0.025)* | 0.299 (0.024)* | 0.089 (0.028)* | 0.027 [0.010, 0.045]* |
0.084 [0.018, 0.156]* |
24.3 [8.7, 40.0]* |
|
| Adult Glucose | 0.111 (0.025)* | 0.264 (0.026)* | 0.088 (0.027)* | 0.023 [0.007, 0.041]* |
0.088 [0.027, 0.158]* |
20.7 [5.5, 35.9]* |
|
| BMI AUC | Adult SBP | 0.150 (0.025)* | 0.166 (0.024)* | 0.154 (0.027)* | 0.026 [0.013, 0.041]* |
0.125 [0.062, 0.197]* |
17.3 [8.0, 26.6]* |
| Adult LDLC | 0.150 (0.025)* | 0.037 (0.027) | 0.105 (0.025)* | 0.004 [−0.002, 0.012] |
0.146 [0.086, 0.216]* | 2.7 [−2.5, 7.8] |
|
| Adult AIP | 0.150 (0.025)* | 0.222 (0.024)* | 0.084 (0.027)* | 0.019 [0.006, 0.033]* |
0.132 [0.068, 0.203]* | 12.7 [3.7, 21.6]* |
|
| Adult Glucose | 0.150 (0.025)* | 0.270 (0.025)* | 0.074 (0.027)* | 0.020 [0.004, 0.039]* |
0.130 [0.069, 0.201]* | 13.3 [2.4, 24.3]* |
c, β1, and β2 are standardized regression coefficients (standardized errors). βInd and c’ are standardized regression coefficients [95% confidence intervals]. Mediation effects are percentages [95% confidence intervals].
c=total effect; c’=direct effect; β1=indirect effect 1; β2=indirect effect 2; βInd=indirect effect (β1 × β2)
, P < 0.05 for being different from 0
cIMT=carotid intima-media thickness; BMI=body mass index; SBP=systolic blood pressure; LDLC=low-density lipoprotein cholesterol; AIP=atherogenic index of plasma; AUC=area under the curve
In Figure S2, childhood BMI was highly correlated with adult BMI, whereas adult BMI was not significantly correlated with adult cIMT. The mediation effect of adult BMI (17.7%) on the childhood BMI-adult cIMT association was not significant (P=0.242). In Figures S3 and S4, covariate-adjusted mean values of adult cIMT showed consistently increasing trends across subgroups of low/low, high/low, low/high and high/high of childhood BMI/adult mediators.
DISCUSSION
The key findings of the present study are that childhood BMI, adult BMI and the cumulative burden of BMI were significantly (P<0.001) associated with adult cIMT without mediators included in the model in asymptomatic healthy middle-aged adults; adult SBP, glucose, AIP and LDLC had the same order of their mediation effect sizes in the three models, with multiple mediators showing mediating effects of 15.9%−58.5% in total; childhood and adulthood BMI, and BMI AUC were directly associated with cIMT after removing the mediation effects. These data indicate that the long-term adverse impact of increased BMI on subclinical changes in vascular structure begins early in life and is accumulated over lifetime. Excess adiposity and high cIMT are linked substantially through other C-V risk factors in later life, especially elevated BP and glucose.
It has been widely accepted that roots of C-V disease extend back into early life, even in utero (22,29,38–41). The theory of developmental origins is supported by numerous publications from large population-based C-V study cohorts followed since childhood (8–14,19–21,24,26–28,32,33,41). We found in the current study that early life BMI was associated with subclinical changes in vascular structure measured as cIMT in later life, and this association still existed after removing the mediation effects of intermediate factors, indicating that early life adiposity has direct effects on adult cIMT independent of other C-V risk variables. The findings from this study provide additional evidence for the concept of childhood origins of atherosclerosis.
BP, LDLC, AIP and glucose are, by definition (36,42), intermediate variables instead of confounders in the association analysis between obesity and cIMT because they are located in the pathway between the predictor and the outcome. The Bogalusa Heart Study has reported that the long-term exposure to obesity is associated with increased adult arterial wall stiffness and left ventricular mass partly through elevated BP (19,20). However, data are not available in previous studies regarding the mediating effects of well-established C-V risk factors on the BMI-cIMT association. In the current study, the mediation effects of adult SBP, glucose, AIP and LDLC were 58.5%, 31.4% and 15.9% (P<0.001 for all) in total in the three models with adult BMI, BMI AUC and childhood BMI as predictors, respectively. These observations indicate that the BMI-cIMT association is substantially mediated through intermediate C-V risk factors, suggesting the pathophysiological process of obesity, mediators (hypertension, hyperglycemia, dyslipidemia) and development of atherosclerosis.
The Bogalusa Heart Study has reported the associations of childhood and adulthood C-V risk factors and their long-term burden with adult cIMT in 486 participants aged 25–37 years, which examined individual effects of adverse levels of BMI, SBP, LDLC, HDLC and TG on increased adult cIMT (11). In contrast, the current study focused on whether and to what extent BMI is associated with cIMT through other C-V risk factors. In our previous and current studies, higher SBP and LDLC were noted to be significantly and consistently associated with higher cIMT. An interesting finding in this study is that childhood BMI and its cumulative burden were associated with adult cIMT substantially through adult SBP, but not through adult LDLC due to the weak association between childhood BMI and adult LDLC.
We noted in this study that adult intermediate variables measured concurrently with adult BMI and cIMT had the greatest mediating effects in both multiple and individual mediator models. Adverse adulthood levels of the outcome are the result of long-term deleterious influence of the cumulative risk factor burden since childhood. In this study, BMI AUC showed a stronger total effect on adult cIMT without mediators in the model, compared to childhood and adulthood BMI. The Cardiovascular Risk in Young Finns Study has shown that the cumulative load of SBP and males’ BMI since childhood is more strongly associated with adult cIMT than their current measurements (12). In the Framingham longitudinal cohort followed during adulthood, the cumulative risk factor burden was more predictive of carotid stenosis than the variables concurrently measured, especially BP (23). On the other hand, in the Muscatine cohort, the cumulative risk factor load from childhood did not improve the predictive value for adult cIMT, compared with adult risk factors (24). The cumulative burden is a long-term average of risk factor values over time which reduces measurement error (32,33). The cumulative burden is expected to have a stronger predictive value than a single measurement at a time point. The inconsistency regarding association parameters in the current and previous studies may be explained by several reasons, such as study protocols, the number of visits, exposure during age periods, methodology to calculate the cumulative burden, and covariates adjusted in the model.
Based on our data, childhood and adulthood BMI, and BMI AUC were directly associated with cIMT after removing the mediating effects of multiple intermediate variables. The direct effect of BMI on cIMT indicates that there exist other mechanisms linking obesity with C-V disease. Excess body fat may potentiate early atherosclerosis through its adverse effect on other atherogenic mediators, such as hyperinsulinemia/insulin resistance and alterations in proinflammatory cytokines, fibrinolysis and oxidative stress (18,43,44).
There were a few limitations in this study. Firstly, adult participants under antihypertensive, lipid-lowering and hypoglycemic treatment represent a subgroup who would be expected, without treatment, to have the highest risk variable levels. The use of currently observed variable values of these participants might result in differences in estimating the mediation parameters compared to using the variable values without treatment. In fact, these original values without imputation reflect the long-term influence of real levels of risk factors on cIMT under control by the pharmaceutical treatment. Secondly, diet, physical activity and sleep disorder were not included for adjustment in the mediation analysis models in the present study because because they had more missing values in the three adult surveys. Inclusion of these covariates would result in a substantial reduction of the sample size. Lastly, sex and race differences in the mediation effect parameters were not examined due to the limited sample size in race and sex subgroups. Based on the mediation analysis rules, a significant total effect is required for further mediation analyses. The total effects of childhood BMI, adulthood BMI and BMI AUC on cIMT were, although all positive, not significant in some models and subgroups in this study cohort. Future studies with sufficient samples are needed to assess the race- and sex-specific mediation effects in this regard.
PERSPECTIVES
The current study demonstrates that intermediate C-V risk factors play significant roles in mediating the BMI-cIMT association in terms of childhood and adulthood BMI, and its lifelong cumulative burden, with adult BP and glucose having stronger mediation effects than LDLC and AIP. The early life BMI and the cumulative burden are directly associated with cIMT independent of the intermediate risk variables. The novel findings of this study provide additional evidence for early life origins of C-V disease and have clinical implications for devising prevention strategies for obesity-related atherosclerosis in early life. The quantification of the multiple mediation effects will help clinicians better understand the underlying mechanistic process of obesity, atherogenic mediators and atherosclerosis. Specifically, weight control beginning in childhood can serve as an essential intervention strategy to mitigate hypertension, dyslipidemia and diabetes and thus reduce the future risk of C-V disease.
Supplementary Material
Novelty and Relevance.
What Is New?
Early life body mass index and its cumulative burden were associated with midlife carotid intima-media thickness mainly through elevated blood pressure, but not through dyslipidemia.
Later life hyperglycemia was another important mediator on the association between body mass index and carotid intima-media thickness.
What Is Relevant?
These findings suggest that the long-term deleterious impact of adiposity on atherosclerosis begins early in life and is accumulated over lifetime. Excess adiposity and higher artery wall thickness are linked partly through elevated blood pressure and glucose in later life.
Clinical/Pathophysiological Implications
The quantification of multiple mediation effects will help clinicians better understand the biological process of causal factors, atherogenic mediators and the development of atherosclerosis and develop preventive strategies for obesity-related C-V disease in early life.
Sources of Funding
This work was supported by grants RF1AG041200, R01AG077000 and R01AG077497 from National Institute on Aging, P20GM109036 from the National Institute of General Medical Sciences of the National Institutes of Health, 82073572, 81973147 and 82222064 from National Natural Science Foundation of China and Z201100006820008 from the Beijing Nova Program.
Non-standard Abbreviations and Acronyms
- AIP
atherogenic index of plasma
- AUC
area under the curve
- BMI
body mass index
- BP
blood pressure
- cIMT
carotid intima-media thickness
- C-V
cardiovascular
- DBP
diastolic blood pressure
- HDLC
high-density lipoprotein cholesterol
- LDLC
low-density lipoprotein cholesterol
- SBP
systolic blood pressure
- TG
triglycerides
Footnotes
Disclosure
The authors declare that they have no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
REFERENCES
- 1.Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corra U, Cosyns B, Deaton C, Ian Graham I, Hall MS, Hobbs FDR, Løchen ML, Lollgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WMM. 2016 European guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2016;37:2315–2381.27222591 [Google Scholar]
- 2.Urbina EM, Williams RV, Alpert BS, Collins RT, Daniels SR, Hayman L, Jacobson M, Mahoney L, Mietus-Snyder M, Rocchini A, Steinberger J, McCrindle B: American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young. Noninvasive assessment of subclinical atherosclerosis in children and adolescents: recommendations for standard assessment for clinical research: a scientific statement from the American Heart Association. Hypertension. 2009;54:919–950. [DOI] [PubMed] [Google Scholar]
- 3.Carpenter M, Sinclair H, Kunadian V. Carotid intima media thickness and its utility as a predictor of cardiovascular disease: a review of evidence. Cardiol Rev. 2016;24:70–75. [DOI] [PubMed] [Google Scholar]
- 4.Grobbee DE, Bots ML. Carotid artery intima-media thickness as an indicator of generalized atherosclerosis. J Intern Med. 1994;236:567–573. [DOI] [PubMed] [Google Scholar]
- 5.Koskinen J, Kähönen M, Viikari JSA, Taittonen L, Laitinen M, Rönnemaa T, Lehtimäki T, Hutri-Kähönen N, Pietikäinen M, Jokinen E, Helenius H, Mattsson N, Raitakari OT, Juonala M. Conventional cardiovascular risk factors and metabolic syndrome in predicting carotid intima-media thickness progression in young adults: the cardiovascular risk in Young Finns Study. Circulation. 2009;120:229–236. [DOI] [PubMed] [Google Scholar]
- 6.Urbina EM, Srinivasan SR, Tang R, Bond MG, Kieltyka L, Berenson GS. Impact of multiple coronary risk factors on the intima-media thickness of different segments of carotid artery in healthy young adults (The Bogalusa Heart Study). Am J Cardiol. 2002;90:953–958. [DOI] [PubMed] [Google Scholar]
- 7.Cecelja M, Sriswan R, Kulkarni B, Kinra S, Nitsch D. Association of pulse wave velocity and intima-media thickness with cardiovascular risk factors in young adults. J Clin Hypertens (Greenwich). 2020;22:174–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Juonala M, Viikari JS, Rönnemaa T, Marniemi J, Jula A, Loo BM, Raitakari OT. Associations of dyslipidemias from childhood to adulthood with carotid intima-media thickness, elasticity, and brachial flow-mediated dilatation in adulthood: the Cardiovascular Risk in Young Finns Study. Arterioscler Thromb Vasc Biol. 2008;28:1012–1017. [DOI] [PubMed] [Google Scholar]
- 9.Juonala M, Magnussen CG, Venn A, Dwyer T, Burns TL, Davis PH, Chen W, Srinivasan SR, Daniels SR, Kähönen M, Laitinen T, Taittonen L, Berenson GS, Viikari JS, Raitakari OT. Influence of age on associations between childhood risk factors and carotid intima-media thickness in adulthood: The Cardiovascular Risk in Young Finns Study, the Childhood Determinants of Adult Health Study, the Bogalusa Heart Study, and the Muscatine Study for the International Childhood Cardiovascular Cohort (i3C) Consortium. Circulation. 2010;122:2514–2520. [DOI] [PubMed] [Google Scholar]
- 10.Berenson GS, Srinivasan SR, Bao W, Newman WP 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338:1650–1656. [DOI] [PubMed] [Google Scholar]
- 11.Li S, Chen W, Srinivasan SR, Bond MG, Tang R, Urbina EM, Berenson GS. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA. 2003;290:2271–2276. [DOI] [PubMed] [Google Scholar]
- 12.Raitakari OT, Juonala M, Kähönen M, Taittonen L, Laitinen T, Mäki-Torkko N, Järvisalo MJ, Uhari M, Jokinen E, Rönnemaa T, Akerblom HK, Viikari JSA. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA. 2003;290:2277–2283. [DOI] [PubMed] [Google Scholar]
- 13.Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W, Sun C, Cheung M, Viikari JS, Dwyer T, Raitakari OT. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876–1885. [DOI] [PubMed] [Google Scholar]
- 14.Freedman DS, Patel DA, Srinivasan SR, Chen W, Tang R, Bond MG, Berenson GS. The contribution of childhood obesity to adult carotid intima-media thickness: the Bogalusa Heart Study. Int J Obes (Lond) 2008;32:749–756. [DOI] [PubMed] [Google Scholar]
- 15.Chen W, Srinivasan SR, Li S, Xu J, Berenson GS. Clustering of long-term trends in metabolic syndrome variables from childhood to adulthood in blacks and whites: the Bogalusa Heart Study. Am J Epidemiol. 2007;166:527–533. [DOI] [PubMed] [Google Scholar]
- 16.Mokha JS, Srinivasan SS, Dasmahapatra P, Fernandez C, Chen W, Xu J, Berenson GS. Utility of waist-to-height ratio in assessing the status of central obesity and related cardiometabolic risk profile among normal weight and overweight/obese children: The Bogalusa Heart Study. BMC Pediatr. 2010;10:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Srinivasan SR, Wang R, Chen W, Wei CY, Xu J, Berenson GS. Utility of waist-to-height ratio in detecting central obesity and related adverse cardiovascular risk profile among normal weight younger adults (from the Bogalusa Heart Study). Am J Cardiol. 2009;104:721–724. [DOI] [PubMed] [Google Scholar]
- 18.Van Gaal LF, Mertens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444:875–880. [DOI] [PubMed] [Google Scholar]
- 19.Zhang H, Zhang T, Li S, Guo Y, Shen W, Fernandez C, Harville EW, Bazzano LA, Urbina EM, He J, Chen W. Long-term excessive body weight and adult left ventricular hypertrophy are linked through later life body size and blood pressure: The Bogalusa Heart Study. Circ Res. 2017;120:1614–1621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu Y, Yan Y, Yang X, Li S, Bazzano L, He J, Chen W. Long-term burden of higher body mass Index and adult arterial stiffness are linked predominantly through elevated blood pressure. Hypertension. 2019;73:229–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Newman WP 3rd, Freedman DS, Voors AW, Gard PD, Srinivasan SR, Cresanta JL, Williamson GD, Webber LS, Berenson GS. Relation of serum lipoprotein levels and systolic blood pressure to early atherosclerosis. The Bogalusa Heart Study. N Engl J Med. 1986;314:138–144. [DOI] [PubMed] [Google Scholar]
- 22.Singhal A The early origins of atherosclerosis. Adv Exp Med Biol. 2009;646:51–58. [DOI] [PubMed] [Google Scholar]
- 23.Wilson PW, Hoeg JM, D’Agostino RB, Silbershatz H, Belanger AM, Poehlmann H, O’Leary D, Wolf PA. Cumulative effects of high cholesterol levels, high blood pressure, and cigarette smoking on carotid stenosis. N Engl J Med. 1997;337:516–522. [DOI] [PubMed] [Google Scholar]
- 24.Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intima-medial thickness is related to cardiovascular risk factors measured from childhood through middle age. The Muscatine Study. Circulation. 2001;104:2815–2819 [DOI] [PubMed] [Google Scholar]
- 25.Lynch J, Smith GD. A life course approach to chronic disease epidemiology. Annu Rev Public Health. 2005;26:1–35. [DOI] [PubMed] [Google Scholar]
- 26.Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9:474–488. [DOI] [PubMed] [Google Scholar]
- 27.Bao W, Srinivasan SR, Wattigney WA, Berenson GS. Persistence of multiple cardiovascular risk clustering related to syndrome X from childhood to young adulthood. The Bogalusa Heart Study. Arch Intern Med. 1994;154:1842–1847. [PubMed] [Google Scholar]
- 28.Li S, Chen W, Sun D, Fernandez C, Li J, Kelly T, He J, Krousel-Wood M, Whelton PK. Variability and rapid increase in body mass index during childhood are associated with adult obesity. Int J Epidemiol. 2015;44:1943–1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berenson GS, McMahan CA, Andrews C, Hester HE. Cardiovascular risk factors in children: the early natural history of atherosclerosis and essential hypertension. New York: Oxford University Press; 1980. [Google Scholar]
- 30.Fernández-Macías JC, Ochoa-Martínez AC, Varela-Silva JA, Pérez-Maldonado IN. Atherogenic index of plasma: novel predictive biomarker for cardiovascular illnesses. Arch Med Res. 2019;50:285–294. [DOI] [PubMed] [Google Scholar]
- 31.High-resolution B-mode ultrasound reading methods in the Atherosclerosis Risk in Communities (ARIC) cohort. The ARIC Study Group. J Neuroimaging. 1991;1:168–172. [PubMed] [Google Scholar]
- 32.Cook NR, Rosner BA, Chen W, Srinivasan SR, Berenson GS. Using the area under the curve to reduce measurement error in predicting young adult blood pressure from childhood measures. Stat Med. 2004;23:3421–3435. [DOI] [PubMed] [Google Scholar]
- 33.Chen W, Li S, Cook NR, Rosner BA, Srinivasan SR, Boerwinkle E, Berenson GS. An autosomal genome scan for loci influencing longitudinal burden of body mass index from childhood to young adulthood in white sibships: the Bogalusa Heart Study. Int J Obes Relat Metab Disord. 2004;28:462–469. [DOI] [PubMed] [Google Scholar]
- 34.Baron RM, Kenny DA. The moderator-mediator distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. [DOI] [PubMed] [Google Scholar]
- 35.VanderWeele TJ. Mediation Analysis: A Practitioner’s Guide. Annu Rev Public Health. 2016;37:2.1–2.16. [DOI] [PubMed] [Google Scholar]
- 36.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1:173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cameron N, Demerath E. Critical periods in human growth and their relationship to diseases of aging. Yrbk Phys Anthropol. 2002;45:159–184. [DOI] [PubMed] [Google Scholar]
- 39.Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med. 2008;359:61–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barker DJ. Fetal origins of coronary heart disease. BMJ. 1995;311:171–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dwyer T, Sun C, Magnussen CG, Raitakari OT, Schork NJ, Venn A, Burns TL, Juonala M, Steinberger J, Sinaiko AR, Prineas RJ, Davis PH, Woo JG, Morrison JA, Daniels SR, Chen W, Srinivasan SR, Viikari JS, Berenson GS. Cohort Profile: The International Childhood Cardiovascular Cohort (i3C) Consortium. Int J Epidemiol. 2013;42:86–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weinberg CR. Toward a clearer definition of confounding. Am J Epidemiol. 1993;137:1–8. [DOI] [PubMed] [Google Scholar]
- 43.Ross R Atherosclerosis-an inflammatory disease. N Engl J Med 1999;340:115–126. [DOI] [PubMed] [Google Scholar]
- 44.Dubois-Deruy E, Peugnet V, Turkieh A, Pinet F. Oxidative stress in cardiovascular diseases. Antioxidants (Basel). 2020;9:864–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


